User login
Concentrated Insulins: A Review and Recommendations (FULL)
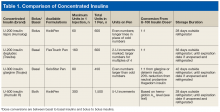
For a long time, 500 U/mL (U-500) insulin was the only concentrated insulin available on the market. With many diabetes mellitus (DM) patients requiring larger doses, additional 200 U/mL (U-200) and 300 U/mL (U-300) concentrations became available. As clinical guidelines lack specific recommendations for optimal use of U-200 and U-300 insulins, clinical discretion is warranted in identifying patients for whom use of these insulins is appropriate. U-500 insulin is recommended in cases that require ≥ 200 U/d or > 2 U/kg/d. Given the ongoing DM and obesity epidemics, increased use of concentrated insulins is likely. Clinicians must stay well informed about the characteristics and benefits of concentrated insulins to remain confident recommending, prescribing, and adjusting these medications.
U-200 Insulin Lispro
Pharmacokinetics/Pharmacodynamics
The amino acid structure of U-200 insulin lispro is different from that of endogenous insulin. In U-200 lispro, lysine replaces a proline at position B28, and proline replaces a lysine at position B29.
In a euglycemic clamp study of patients without DM, a 20-U dose of U-200 lispro and a single 20-U dose of U-100 lispro were found to have similar mean area under the glucose infusion rate curves, mean area under the serum insulin concentration-time curves from time 0 to infinity, mean peak serum insulin levels, and time to maximum glucose-lowering effects.1 For both U-200 lispro and U-100 lispro, time to maximum effect was 1 hour.2
Even numbers are marked on the dial of the pen. Odd numbers are not marked, but longer lines appear in their place. U-200 lispro should not be mixed with any other insulin, whereas U-100 lispro can be mixed with neutral protamine Hagedorn insulin.
Safety/Efficacy
There has been 1 bioequivalence study of euglycemic patients without type 2 DM (T2DM) but no studies of the safety or efficacy of U-200 lispro in patients with DM.3,4 U-100 lispro converts 1:1 to U-200 lispro (eg, 60 U of U-100 lispro converts to 60 U of U-200 lispro).1 The volume of U-200 lispro would be smaller than that of U-100 lispro.
Economic Analysis
There are no published U-200 lispro economic analyses.
Dosing
U-200 lispro should be converted from other bolus insulins in a 1:1 ratio.1
Recommendations
Definitive recommendations await efficacy trials comparing use of U-200 lispro and other bolus insulins in patients with DM. Currently, U-200 lispro may be considered for patients with DM who require high doses of bolus insulin and who may benefit from smaller volumes of lispro.
U-200 Insulin Degludec
Pharmacokinetics/Pharmacodynamics
The basal insulin degludec (Tresiba) is available in U-100 and U-200 concentrations in a pen. After subcutaneous injection, degludec forms gradually dissociating multihexamer chains, which account for its flat and stable PK/PD profile. U-100 degludec and U-200 degludec have similar duration of action (≥ 42 hours) and time to steady state (2-3 days).5,6 A patient who misses a regularly scheduled dose should allow at least 8 hours between injections. Taking degludec at variable times does not decrease efficacy as long as this 8-hour minimum interval is observed.7
Safety/Efficacy
During its development, degludec was evaluated in more than 5,000 patients across 11 therapeutic trials.8 The key studies that led to the approval of degludec used insulin glargine as a comparator. In a 52-week study of 1,030 insulin-naïve patients with T2DM, degludec was noninferior to glargine in hemoglobin A1c (HbA1c) reduction (1.06% vs 1.19%). Overall hypoglycemia rates were similar, though there were fewer nocturnal hypoglycemia episodes with degludec than with glargine (0.25 vs 0.39 per patient-year of exposure; P = .38).9
The BEGIN Basal-Bolus trial series evaluated use of degludec combined with bolus insulin aspart in insulin-experienced patients with T2DM (n = 992) and type 1 DM (T1DM) (n = 629) over 52 weeks.10,11 Both trials found noninferiority in A1c reduction: 1.1% (degludec) and 1.18% (glargine) in patients with T2DM and 0.4% (degludec) and 0.39% (glargine) in those with T1DM.10,11 Significantly fewer episodes of overall hypoglycemia (11.09 vs 13.63 per patient-year) and nocturnal hypoglycemia (1.39 vs 1.84 per patient-year) were found with degludec in patients with T2DM.5 Overall hypoglycemia rates were similar, though there was a 25% lower rate of nocturnal hypoglycemia with degludec in patients with T1DM.11
A meta-analysis of 7 phase 3a trials that compared degludec with glargine revealed significantly lower rates of overall, nocturnal, and severe hypoglycemia with degludec in insulin-naïve patients.12 The analysis confirmed findings of significantly lower rates of overall and nocturnal hypoglycemia with degludec in the overall T2DM population and significantly lower rates of nocturnal hypoglycemia in the T1DM population.12
In the DEVOTE trial, which included 7,637 T2DM patients at high risk for a cardiovascular event, degludec and glargine were compared on the composite primary outcome of death with a cardiovascular cause, nonfatal myocardial infarction, or nonfatal stroke. After a median of 1.99 years, the primary outcome occurred in 8.5% of degludec patients and 9.3% of glargine patients (hazard ratio, 0.91; 95% confidence interval, 0.78-1.06; P < .001 for noninferiority). Mean HbA1c level was 7.5 in both groups; severe hypoglycemia occurred more often in the glargine group (odds ratio, 0.73; P < .001 for superiority).13 Findings from the randomized, crossover SWITCH 1 and SWITCH 2 trials confirmed lower rates of symptomatic hypoglycemia with degludec compared with glargine in patients with T1DM and T2DM, respectively.14,15 No statistically significant differences in weight gain were observed in the clinical trials comparing degludec and glargine.
Economic Analysis
Weatherall and colleagues used a budget impact model to evaluate the costs of degludec and glargine for commercially insured patients with DM in the U.S.16 Three treatment groups were analyzed: basal/bolus combination in T1DM and T2DM, and basal/oral combination in T2DM. Although degludec cost more, overall cost was reduced in T1DM because of reduced insulin usage and fewer hypoglycemic episodes in T2DM with basal/oral combination therapy. The authors acknowledged the many assumptions needed and the potential oversimplification of their model.16 In other countries, economic analyses had similar findings.17-19
Dosing
Degludec converts 1:1 to other basal insulins. Recommended starting doses for U-200 degludec are 10 U once daily for insulin-naïve adults with T2DM and one-third to one-half the total weight-based daily insulin dose for insulin-naïve adults with T1DM.4
Recommendations
For some patients, lower PD variability may make degludec a desirable alternative. As degludec retains its efficacy with variable dosing times, it may be ideal for patients who have difficulty with a once-daily dosing schedule. It is important to inform patients that the degludec pen allows for 2-U increments. Given the lower frequency of nocturnal hypoglycemic events with degludec compared with glargine, degludec is an appropriate basal insulin option for patients with nocturnal hypoglycemia. In addition, U-200 degludec may be considered for DM patients who require high doses of basal insulin and who may benefit from smaller volumes of degludec.
U-300 Isulin Glargine
Pharmacokinetics/Pharmacodynamics
U-300 glargine is a concentrated basal insulin. There are notable differences between its U-100 and U-300 concentrations. For U-300 glargine dosed at 0.4 U/kg, duration of action is 24 hours; for U-300 glargine dosed at 0.6 U/kg or higher, longer duration is expected.20 Steady state is reached after 5 days.21 The U-300 glargine pen contains 1.5 mL, less than the 3 mL in the U-100 pen. U-300 glargine typically is administered in 1 injection once daily if the dose is < 80 U; 2 injections are required if the dose is > 80 U.
Safety/Efficacy
In the EDITION trials, which compared U-300 and U-100 glargine in patients with T1DM and T2DM, the primary endpoint was 6-month HbA1c reduction.22-24 Comparable HbA1c reductions were found in all of the studies. In EDITION 1, in which 2,474 patients with T2DM were taking concomitant bolus insulin with or without metformin, 11% more U-300 glargine than U-100 glargine was needed to achieve similar results.22 In EDITION 4, in which bolus insulin was used in combination in 546 patients with T1DM, 17.5% more U-300 glargine than U-100 glargine was needed to achieve similar glycemic goals.25
Economic Analysis
Compared with other insulins, U-300 glargine has limited published data and economic analyses. Using a cost-utility model to compare U-300 with U-100 glargine in Spanish patients with T2DM, and reporting results in euros per quality-adjusted life years, Monero and colleagues concluded that the hypoglycemia reduction and possible time-of-dose flexibility found with U-300 glargine may contribute to its cost-effectiveness.26
Dosing
U-300 glargine should be converted in a 1:1 ratio from U-100 glargine or detemir. The U-300 glargine dose should be reduced by 20% when switching from NPH insulin.21
Recommendations
A meta-analysis of the EDITION trials 1 to 3 revealed a lower incidence of daytime and nocturnal hypoglycemia with use of U-300 glargine over U-100 glargine and a beneficial shorter hold time after injection of U-300 glargine (5 seconds) compared with U-100 glargine (10 seconds).27 There was statistically lower weight gain with U-300 glargine compared with U-100 glargine however weight gain was < 1 kg in both groups.27 These characteristics of U-300 glargine may prove advantageous for individual patients.
U-500 Insulin
Pharmacokinetics/Pharmacodynamics
U-500 insulin (Humulin R) has been available in a vial since 1997, but other formulations have been used therapeutically since 1952.28 The U-500 KwikPen device, recently added to the market, has improved the vial and syringe dosing. The new U-500 BD (Becton, Dickinson, Franklin Lakes, NJ) syringes allow doses up to 250 U, and the U-500 KwikPens provide up to 300 U per injection.29 When it was first introduced, U-500 insulin had no dedicated delivery device and dose conversion was required to deliver the appropriate dose using an allergy or TB syringe. As a consequence, confusion often resulted between prescribers, pharmacists and patients.30,31 U-500 insulin acts as basal and bolus insulins do. Onset of action is ~15 minutes, time to peak is 4 to 8 hours, and duration of action is ≤ 21 hours.32 As its onset of action is similar to that of U-100, U-500 should be injected 30 minutes before meals.
A single-site, randomized, double-blind, crossover euglycemic clamp study that compared equivalent doses of U-500 and U-100 in healthy obese patients found the formulations had similar overall exposures and effects—the only differences were that U-500 had an extended time to peak and a prolonged post-peak effect. The longer post-peak effect contributes to longer duration of action and allows for fewer daily injections.33
Safety/Efficacy
In the Humulin R U-500 Initiation trial, both of these algorithms improved glycemic control and were associated with a low incidence of severe hypoglycemia. In addition, the associated weight gains were similar. Last, the rate of nonsevere hypoglycemia was slightly lower for the 3-times-daily than for the 2-times-daily regimen.34 A real-world outcome analysis of U-500 initiation confirmed the benefits of switching from U-100 to U-500. A clinically significant improvement in glycemic control was found in all the study participants. Dose and frequency of administration, however, were not reported.35
According to a secondary analysis in the Humulin R U-500 Initiation trial, baseline U-100 total daily dose did not yield a difference in efficacy or safety between the 2-times-a-day and 3-times-a-day arms—allowing use of a simpler 2-times-a-day schedule without regard to baseline total daily dose.28,36 The 2-times-a-day regimen is preferred in clinical practice given that the 2 regimens are equivalent in safety and efficacy and that the 2-times-a-day regimen is simpler, allows for easier titrations, improves patient perceptions of the effect of insulin on daily life function and psychological health, lowers daily injection burden, and maximizes adherence.37
Economic Analysis
A retrospective database analysis revealed lower overall cost and lower pharmacy cost associated with U-500 in comparison with high-dose U-100, as well as reduced hypoglycemia-specific costs or resource utilization, even though U-500 was associated with a slightly higher incidence of hypoglycemia.28 However, the fact that hypoglycemia was reported with a billing code (ICD-9) implies the hypoglycemic event was severe enough to require medical attention. Given these findings, 2-times-a-day U-500 seems more cost-effective than high-dose U-100.
Dosing
The U-500 Humulin R package insert recommends converting a dose to U-500 on the basis of most recent HbA1c level. U-500 can be dosed 2 times daily (60%, 40%) or 3 times daily (40%, 30%, 30%). If HbA1c is > 8%, then the starting total daily dose (TDD) of U-500 is 100% of the U-100 TDD. If HbA1c is ≤ 8%, then the starting TDD of U-500 is 80% of the final U-100 TDD (20% reduction). Dose adjustments may range from 5% to 10% depending on subsequent blood glucose readings.32
Recommendations
U-500 is a safe and effective monotherapy alternative for patients who require high doses of U-100. Initial conversion from U-100 is based on HbA1c level. The total daily dose of U-500 is then divided by 2 (60%, 40%) or 3 (40%, 30%, 30%). The 2-times-a-day regimen enhances adherence and thus may be preferred.
Discussion
It has been suggested that large volumes or depots of insulin approaching 100 units impedes absorption and are more painful compared with smaller volume injections.37 For patients with DM who require higher doses of insulin, concentrated insulins offer the advantage of smaller volumes. Also smaller volumes are a substantial benefit in addressing the growing epidemic of DM and the progressive nature of insulin resistance. Furthermore, concentrated insulins are available in pens. Compared with syringes and vials, pens are associated with a lower risk of dosing errors. The major advantages to the use of concentrated insulins include patient acceptability and the potential for decreased volumes and frequency of injections.
Potential disadvantages also exist for the use of concentrated insulins. Depending on insurance coverage, concentrated insulins may be more expensive than U-100 insulin options. Additionally, thorough counseling and education are of paramount importance when concentrated insulins are initiated or switched in patients with DM. The dosing errors that occur with concentrated insulins could increase the risk of hypoglycemia. Pharmacists should provide detailed counseling to DM patients initiating or switching concentrated insulins. It is important to implement or revise institution and clinic safe practices for concentrated insulins to avoid errors in prescribing, distributing, administering, and monitoring these medications.
Conclusion
Concentrated insulins provide expanded treatment options for patients with DM. Clinicians must stay well informed about concentrated insulin characteristics and dosing strategies to optimize DM treatment. As more evidence becomes available, standardized recommendations can be developed to guide clinicians in the appropriate use of concentrated insulins.
Click here to read the digital edition.
1. Humalog [package insert]. Indianapolis, IN: Eli Lilly & Co; 2015.
2. de la Peña A, Seger M, Soon D, et al. Bioequivalence and comparative pharmacodynamics of insulin lispro 200 U/mL relative to insulin lispro (Humalog®) 100 U/mL. Clin Pharmacol Drug Dev. 2016;5(1):69-75.
3. VA Pharmacy Benefits Management Services, Medical Advisory Panel, VISN Phar macist Executives. Insulin Lispro 200units/mL (Humalog) KwikPen abbreviated review. https://www.pbm.va.gov/PBM/clinicalguidance/abbreviatedre views/Insu lin_Lispro_200units_per_mL_Abbreviated_Review.pdf. Published February 2016. Accessed August 22, 2017.
4. Painter NA, Sisson E. An overview of concentrated insulin products. Diabetes Spectr. 2016;29(3):136-140.
5. Korsatko S, Deller S, Koehler G, et al. A comparison of the steady-state pharmacokinetic and pharmacodynamic profiles of 100 and 200 U/mL formulations of ultra-long-acting insulin degludec. Clin Drug Investig. 2013;33(7):515-521.
6. Goldman-Levine JD, Patel DK, Schnee DM. Insulin degludec: a novel basal insulin analogue. Ann Pharmacother. 2013;47(2):269-277.
7. Meneghini L, Atkin SL, Gouch SC, et al; NN1250-3668 (BEGIN FLEX) Trial Investigators. The efficacy and safety of insulin degludec given in variable once-daily dosing intervals compared with insulin glargine and insulin degludec dosed at the same time daily: a 26-week, randomized, open-label, parallel-group, treat-to-target trial in individuals with type 2 diabetes. Diabetes Care. 2013;36(4):858-864.
8. Rendell M. United States experience of insulin degludec alone or in combination for type 1 and type 2 diabetes. Drug Des Dev Ther. 2017;11:1209-1220.
9. Zinman B, Philis-Tsimikas A, Caropi B, et al; NN1250-3579 (BEGIN Once Long) Trial Investigators. Insulin degludec versus insulin glargine in insulin-naive patients with type 2 diabetes: a 1-year, randomized, treat-to-target trial (BEGIN Once Long). Diabetes Care. 2012;35(12):2464-2471.
10. Garber AJ, King AB, Del Prato S, et al; NN1250-3582 (BEGIN BB T2D) Trial Investigators. Insulin degludec, an ultra-longacting basal insulin, versus insulin glargine in basal-bolus treatment with mealtime insulin aspart in type 2 diabetes (BEGIN Basal-Bolus Type 2): a phase 3, randomised, open-label, treat-to-target non-inferiority trial. Lancet. 2012;379(9825):1498-1507.
11. Heller S, Buse J, Fisher M, et al; BEGIN Basal-Bolus Type 1 Trial Investigators. Insulin degludec, an ultra-longacting basal insulin, versus insulin glargine in basal-bolus treatment with mealtime insulin aspart in type 1 diabetes (BEGIN Basal-Bolus Type 1): a phase 3, randomised, open-label, treat-to-target non-inferiority trial. Lancet. 2012;379(9825):1489-1497.
12. Ratner RE, Gough SC, Mathieu C, et al. Hypoglycaemia risk with insulin degludec compared with insulin glargine in type 2 and type 1 diabetes: a pre-planned meta-analysis of phase 3 trials. Diabetes Obes Metab. 2013;15(2):175-184.
13. Marso SP, McGuire DK, Zinman B, et al; DEVOTE Study Group. Efficacy and safety of degludec versus glargine in type 2 diabetes. N Engl J Med. 2017;377(8):723-732.
14. Lane W, Bailey TS, Gerety G, et al; Group Information; SWITCH 1. Effect of insulin degludec vs insulin glargine U100 on hypoglycemia in patients with type 1 diabetes: the SWITCH 1 randomized clinical trial. JAMA. 2017;318(1):33-44.
15. Wysham C, Bhargava A, Chaykin L, et al. Effect of insulin degludec vs insulin glargine U100 on hypoglycemia in patients with type 2 diabetes: the SWITCH 2 randomized clinical trial. JAMA. 2017;318(1):45-56.
16. Weatherall J, Bludek L, Buchs S. Budget impact of treating commercially insured type 1 and type 2 diabetes patients in the United States with insulin degludec compared to insulin glargine. Curr Med Res Opin. 2017;33(2):231-238.
17. Mezquita-Raya P, Darbà J, Ascanio M, Ramírez de Arellano A. Cost-effectiveness analysis of insulin degludec compared with insulin glargine u100 for the management of type 1 and type 2 diabetes mellitus—from the Spanish National Health System perspective. Expert Rev Pharmacoecon Outcomes Res. 2017:1-9. [Epub ahead of print.]
18. Landstedt-Hallin L, Gundgaard J, Ericsson Å, Ellfors-Zetterlund S. Cost-effectiveness of switching to insulin degludec from other basal insulins: evidence from Swedish real-world data. Curr Med Res Opin. 2017;33(4):647-655.
19. Pollock RF, Tikkanen CK. A short-term cost-utility analysis of insulin degludec versus insulin glargine U100 in patients with type 1 or type 2 diabetes in Denmark. J Med Econ. 2017;20(3):213-220.
20. Becker RH, Dahmen R, Bergmann K, Lehmann A, Jax T, Heise T. New insulin glargine 300 units · mL-1 provides a more even activity profile and prolonged glycemic control at steady state compared with insulin glargine 100 units · mL-1. Diabetes Care. 2015;38(4):637-643.
21. Toujeo [package insert]. Bridgewater, NJ: Sanofi-Aventis; 2015.
22. Riddle MC, Bolli GB, Ziemen M, Muehlen-Bartmer I, Bizet F, Home PD; EDITION 1 Study Investigators. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 2 diabetes using basal and mealtime insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 1). Diabetes Care. 2014;37(10):2755-2762.
23. Yki-Järvinen H, Bergenstal R, Ziemen M, et al; EDITION 2 Study Investigators. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 2 diabetes using oral agents and basal insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 2). Diabetes Care. 2014;37(12):3235-3243.
24. Bolli GB, Riddle MC, Bergenstal RM, et al; on behalf of the EDITION 3 Study Investigators. New insulin glargine 300 U/ml compared with glargine 100 U/ml in insulin-naïve people with type 2 diabetes on oral glucose-lowering drugs: a randomized controlled trial (EDITION 3). Diabetes Obes Metab. 2015;17(4):386-394.
25. Home PD, Bergenstal RM, Bolli GB, et al. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 1 diabetes: a randomized, phase 3a, open-label clinical trial (EDITION 4). Diabetes Care. 2015;38(12):2217-2225.
26. Monero S, Delgado M, Rubio M, Gasche D, Fournier M. Cost-utility evaluation of insulin glargine 300 (GLA-300) versus insulin glargine 100 (GLA-100) in patients with type 2 diabetes mellitus (T2DM). Poster presented at: International Society for Pharmacoeconomics and Outcomes Research (ISPOR) 19th Annual European Congress; October 29-November 2, 2016; Vienna, Austria.
27. Ritzel R, Roussel R, Bolli GB, et al. Patient-level meta-analysis of the EDITION 1, 2 and 3 studies: glycaemic control and hypoglycaemia with new insulin glargine 300 U/ml versus glargine 100 U/ml in people with type 2 diabetes. Diabetes Obes Metab. 2015;17(9):859-867.
28. Eby EL, Wang P, Curtis BH, et al. Cost, healthcare resource utilization, and adherence of individuals with diabetes using U-500 or U-100 insulin: a retrospective database analysis. J Med Econ. 2013;16(4):529-538.
29. Lilly USA. Pharmacy tips about Humulin R U-500 KwikPen syringe and vial. http://www.humulin.com/pharmacy-tips.aspx#about-the-u500-syringe_and_vial. Accessed
30. Meneghini, L. New insulin preparations: a primer for the clinician. Cleve Clin J Med. 2016;83(5 suppl 1):S27-S33.
31. Humulin R U-500 KwikPen [package insert]. Indianapolis, IN: Eli Lilly & Co; 2016.
32. de la Peña A, Riddle M, Morrow LA, et al. Pharmacokinetics and pharmacodynamics of high-dose human regular U-500 insulin versus human regular U-100 insulin in healthy obese subjects. Diabetes Care. 2011;34(12):2496-2501.
33. Hood RC, Arakaki RF, Wysham C, Li YG, Settles JA, Jackson JA. Two treatment approaches for human regular U-500 insulin in patients with type 2 diabetes not achieving adequate glycemic control on high-dose U-100 insulin therapy with or without oral agents: a randomized, titration-to-target clinical trial. Endocr Pract. 2015;21(7):782-793.
34. Eby EL, Curtis BH, Gelwicks SC, et al. Initiation of human regular U-500 insulin use is associated with improved glycemic control: a real-world US cohort study. BMJ Open Diabetes Res Care. 2015;3(1):e000074.
35. Wysham C, Hood RC, Warren ML, Wang T, Morwick TM, Jackson JA. Effect of total daily dose on efficacy, dosing, and safety of 2 dose titration regimens of human regular U500 insulin in severely insulin-resistant patients with type 2 diabetes. Endocr Pract. 2016;22(6):653-665.
36. Kabul S, Hood RC, Duan R, DeLozier AM, Settles J. Patient-reported outcomes in transition from high-dose U-100 insulin to human regular U-500 insulin in severely insulin-resistant patients with type 2 diabetes: analysis of a randomized clinical trial. Health Qual Life Outcomes. 2016;14(1):139.
37. Hirsch IB. Lipodystrophy: metabolic and clinical aspects. https://www.endo crine.org/~/media/endosociety/files/education/lypodystrophy-files/hirsch_tdeg-2013_lrc_final.pdf?la=en. Accessed September 7, 2017.
For a long time, 500 U/mL (U-500) insulin was the only concentrated insulin available on the market. With many diabetes mellitus (DM) patients requiring larger doses, additional 200 U/mL (U-200) and 300 U/mL (U-300) concentrations became available. As clinical guidelines lack specific recommendations for optimal use of U-200 and U-300 insulins, clinical discretion is warranted in identifying patients for whom use of these insulins is appropriate. U-500 insulin is recommended in cases that require ≥ 200 U/d or > 2 U/kg/d. Given the ongoing DM and obesity epidemics, increased use of concentrated insulins is likely. Clinicians must stay well informed about the characteristics and benefits of concentrated insulins to remain confident recommending, prescribing, and adjusting these medications.
U-200 Insulin Lispro
Pharmacokinetics/Pharmacodynamics
The amino acid structure of U-200 insulin lispro is different from that of endogenous insulin. In U-200 lispro, lysine replaces a proline at position B28, and proline replaces a lysine at position B29.
In a euglycemic clamp study of patients without DM, a 20-U dose of U-200 lispro and a single 20-U dose of U-100 lispro were found to have similar mean area under the glucose infusion rate curves, mean area under the serum insulin concentration-time curves from time 0 to infinity, mean peak serum insulin levels, and time to maximum glucose-lowering effects.1 For both U-200 lispro and U-100 lispro, time to maximum effect was 1 hour.2
Even numbers are marked on the dial of the pen. Odd numbers are not marked, but longer lines appear in their place. U-200 lispro should not be mixed with any other insulin, whereas U-100 lispro can be mixed with neutral protamine Hagedorn insulin.
Safety/Efficacy
There has been 1 bioequivalence study of euglycemic patients without type 2 DM (T2DM) but no studies of the safety or efficacy of U-200 lispro in patients with DM.3,4 U-100 lispro converts 1:1 to U-200 lispro (eg, 60 U of U-100 lispro converts to 60 U of U-200 lispro).1 The volume of U-200 lispro would be smaller than that of U-100 lispro.
Economic Analysis
There are no published U-200 lispro economic analyses.
Dosing
U-200 lispro should be converted from other bolus insulins in a 1:1 ratio.1
Recommendations
Definitive recommendations await efficacy trials comparing use of U-200 lispro and other bolus insulins in patients with DM. Currently, U-200 lispro may be considered for patients with DM who require high doses of bolus insulin and who may benefit from smaller volumes of lispro.
U-200 Insulin Degludec
Pharmacokinetics/Pharmacodynamics
The basal insulin degludec (Tresiba) is available in U-100 and U-200 concentrations in a pen. After subcutaneous injection, degludec forms gradually dissociating multihexamer chains, which account for its flat and stable PK/PD profile. U-100 degludec and U-200 degludec have similar duration of action (≥ 42 hours) and time to steady state (2-3 days).5,6 A patient who misses a regularly scheduled dose should allow at least 8 hours between injections. Taking degludec at variable times does not decrease efficacy as long as this 8-hour minimum interval is observed.7
Safety/Efficacy
During its development, degludec was evaluated in more than 5,000 patients across 11 therapeutic trials.8 The key studies that led to the approval of degludec used insulin glargine as a comparator. In a 52-week study of 1,030 insulin-naïve patients with T2DM, degludec was noninferior to glargine in hemoglobin A1c (HbA1c) reduction (1.06% vs 1.19%). Overall hypoglycemia rates were similar, though there were fewer nocturnal hypoglycemia episodes with degludec than with glargine (0.25 vs 0.39 per patient-year of exposure; P = .38).9
The BEGIN Basal-Bolus trial series evaluated use of degludec combined with bolus insulin aspart in insulin-experienced patients with T2DM (n = 992) and type 1 DM (T1DM) (n = 629) over 52 weeks.10,11 Both trials found noninferiority in A1c reduction: 1.1% (degludec) and 1.18% (glargine) in patients with T2DM and 0.4% (degludec) and 0.39% (glargine) in those with T1DM.10,11 Significantly fewer episodes of overall hypoglycemia (11.09 vs 13.63 per patient-year) and nocturnal hypoglycemia (1.39 vs 1.84 per patient-year) were found with degludec in patients with T2DM.5 Overall hypoglycemia rates were similar, though there was a 25% lower rate of nocturnal hypoglycemia with degludec in patients with T1DM.11
A meta-analysis of 7 phase 3a trials that compared degludec with glargine revealed significantly lower rates of overall, nocturnal, and severe hypoglycemia with degludec in insulin-naïve patients.12 The analysis confirmed findings of significantly lower rates of overall and nocturnal hypoglycemia with degludec in the overall T2DM population and significantly lower rates of nocturnal hypoglycemia in the T1DM population.12
In the DEVOTE trial, which included 7,637 T2DM patients at high risk for a cardiovascular event, degludec and glargine were compared on the composite primary outcome of death with a cardiovascular cause, nonfatal myocardial infarction, or nonfatal stroke. After a median of 1.99 years, the primary outcome occurred in 8.5% of degludec patients and 9.3% of glargine patients (hazard ratio, 0.91; 95% confidence interval, 0.78-1.06; P < .001 for noninferiority). Mean HbA1c level was 7.5 in both groups; severe hypoglycemia occurred more often in the glargine group (odds ratio, 0.73; P < .001 for superiority).13 Findings from the randomized, crossover SWITCH 1 and SWITCH 2 trials confirmed lower rates of symptomatic hypoglycemia with degludec compared with glargine in patients with T1DM and T2DM, respectively.14,15 No statistically significant differences in weight gain were observed in the clinical trials comparing degludec and glargine.
Economic Analysis
Weatherall and colleagues used a budget impact model to evaluate the costs of degludec and glargine for commercially insured patients with DM in the U.S.16 Three treatment groups were analyzed: basal/bolus combination in T1DM and T2DM, and basal/oral combination in T2DM. Although degludec cost more, overall cost was reduced in T1DM because of reduced insulin usage and fewer hypoglycemic episodes in T2DM with basal/oral combination therapy. The authors acknowledged the many assumptions needed and the potential oversimplification of their model.16 In other countries, economic analyses had similar findings.17-19
Dosing
Degludec converts 1:1 to other basal insulins. Recommended starting doses for U-200 degludec are 10 U once daily for insulin-naïve adults with T2DM and one-third to one-half the total weight-based daily insulin dose for insulin-naïve adults with T1DM.4
Recommendations
For some patients, lower PD variability may make degludec a desirable alternative. As degludec retains its efficacy with variable dosing times, it may be ideal for patients who have difficulty with a once-daily dosing schedule. It is important to inform patients that the degludec pen allows for 2-U increments. Given the lower frequency of nocturnal hypoglycemic events with degludec compared with glargine, degludec is an appropriate basal insulin option for patients with nocturnal hypoglycemia. In addition, U-200 degludec may be considered for DM patients who require high doses of basal insulin and who may benefit from smaller volumes of degludec.
U-300 Isulin Glargine
Pharmacokinetics/Pharmacodynamics
U-300 glargine is a concentrated basal insulin. There are notable differences between its U-100 and U-300 concentrations. For U-300 glargine dosed at 0.4 U/kg, duration of action is 24 hours; for U-300 glargine dosed at 0.6 U/kg or higher, longer duration is expected.20 Steady state is reached after 5 days.21 The U-300 glargine pen contains 1.5 mL, less than the 3 mL in the U-100 pen. U-300 glargine typically is administered in 1 injection once daily if the dose is < 80 U; 2 injections are required if the dose is > 80 U.
Safety/Efficacy
In the EDITION trials, which compared U-300 and U-100 glargine in patients with T1DM and T2DM, the primary endpoint was 6-month HbA1c reduction.22-24 Comparable HbA1c reductions were found in all of the studies. In EDITION 1, in which 2,474 patients with T2DM were taking concomitant bolus insulin with or without metformin, 11% more U-300 glargine than U-100 glargine was needed to achieve similar results.22 In EDITION 4, in which bolus insulin was used in combination in 546 patients with T1DM, 17.5% more U-300 glargine than U-100 glargine was needed to achieve similar glycemic goals.25
Economic Analysis
Compared with other insulins, U-300 glargine has limited published data and economic analyses. Using a cost-utility model to compare U-300 with U-100 glargine in Spanish patients with T2DM, and reporting results in euros per quality-adjusted life years, Monero and colleagues concluded that the hypoglycemia reduction and possible time-of-dose flexibility found with U-300 glargine may contribute to its cost-effectiveness.26
Dosing
U-300 glargine should be converted in a 1:1 ratio from U-100 glargine or detemir. The U-300 glargine dose should be reduced by 20% when switching from NPH insulin.21
Recommendations
A meta-analysis of the EDITION trials 1 to 3 revealed a lower incidence of daytime and nocturnal hypoglycemia with use of U-300 glargine over U-100 glargine and a beneficial shorter hold time after injection of U-300 glargine (5 seconds) compared with U-100 glargine (10 seconds).27 There was statistically lower weight gain with U-300 glargine compared with U-100 glargine however weight gain was < 1 kg in both groups.27 These characteristics of U-300 glargine may prove advantageous for individual patients.
U-500 Insulin
Pharmacokinetics/Pharmacodynamics
U-500 insulin (Humulin R) has been available in a vial since 1997, but other formulations have been used therapeutically since 1952.28 The U-500 KwikPen device, recently added to the market, has improved the vial and syringe dosing. The new U-500 BD (Becton, Dickinson, Franklin Lakes, NJ) syringes allow doses up to 250 U, and the U-500 KwikPens provide up to 300 U per injection.29 When it was first introduced, U-500 insulin had no dedicated delivery device and dose conversion was required to deliver the appropriate dose using an allergy or TB syringe. As a consequence, confusion often resulted between prescribers, pharmacists and patients.30,31 U-500 insulin acts as basal and bolus insulins do. Onset of action is ~15 minutes, time to peak is 4 to 8 hours, and duration of action is ≤ 21 hours.32 As its onset of action is similar to that of U-100, U-500 should be injected 30 minutes before meals.
A single-site, randomized, double-blind, crossover euglycemic clamp study that compared equivalent doses of U-500 and U-100 in healthy obese patients found the formulations had similar overall exposures and effects—the only differences were that U-500 had an extended time to peak and a prolonged post-peak effect. The longer post-peak effect contributes to longer duration of action and allows for fewer daily injections.33
Safety/Efficacy
In the Humulin R U-500 Initiation trial, both of these algorithms improved glycemic control and were associated with a low incidence of severe hypoglycemia. In addition, the associated weight gains were similar. Last, the rate of nonsevere hypoglycemia was slightly lower for the 3-times-daily than for the 2-times-daily regimen.34 A real-world outcome analysis of U-500 initiation confirmed the benefits of switching from U-100 to U-500. A clinically significant improvement in glycemic control was found in all the study participants. Dose and frequency of administration, however, were not reported.35
According to a secondary analysis in the Humulin R U-500 Initiation trial, baseline U-100 total daily dose did not yield a difference in efficacy or safety between the 2-times-a-day and 3-times-a-day arms—allowing use of a simpler 2-times-a-day schedule without regard to baseline total daily dose.28,36 The 2-times-a-day regimen is preferred in clinical practice given that the 2 regimens are equivalent in safety and efficacy and that the 2-times-a-day regimen is simpler, allows for easier titrations, improves patient perceptions of the effect of insulin on daily life function and psychological health, lowers daily injection burden, and maximizes adherence.37
Economic Analysis
A retrospective database analysis revealed lower overall cost and lower pharmacy cost associated with U-500 in comparison with high-dose U-100, as well as reduced hypoglycemia-specific costs or resource utilization, even though U-500 was associated with a slightly higher incidence of hypoglycemia.28 However, the fact that hypoglycemia was reported with a billing code (ICD-9) implies the hypoglycemic event was severe enough to require medical attention. Given these findings, 2-times-a-day U-500 seems more cost-effective than high-dose U-100.
Dosing
The U-500 Humulin R package insert recommends converting a dose to U-500 on the basis of most recent HbA1c level. U-500 can be dosed 2 times daily (60%, 40%) or 3 times daily (40%, 30%, 30%). If HbA1c is > 8%, then the starting total daily dose (TDD) of U-500 is 100% of the U-100 TDD. If HbA1c is ≤ 8%, then the starting TDD of U-500 is 80% of the final U-100 TDD (20% reduction). Dose adjustments may range from 5% to 10% depending on subsequent blood glucose readings.32
Recommendations
U-500 is a safe and effective monotherapy alternative for patients who require high doses of U-100. Initial conversion from U-100 is based on HbA1c level. The total daily dose of U-500 is then divided by 2 (60%, 40%) or 3 (40%, 30%, 30%). The 2-times-a-day regimen enhances adherence and thus may be preferred.
Discussion
It has been suggested that large volumes or depots of insulin approaching 100 units impedes absorption and are more painful compared with smaller volume injections.37 For patients with DM who require higher doses of insulin, concentrated insulins offer the advantage of smaller volumes. Also smaller volumes are a substantial benefit in addressing the growing epidemic of DM and the progressive nature of insulin resistance. Furthermore, concentrated insulins are available in pens. Compared with syringes and vials, pens are associated with a lower risk of dosing errors. The major advantages to the use of concentrated insulins include patient acceptability and the potential for decreased volumes and frequency of injections.
Potential disadvantages also exist for the use of concentrated insulins. Depending on insurance coverage, concentrated insulins may be more expensive than U-100 insulin options. Additionally, thorough counseling and education are of paramount importance when concentrated insulins are initiated or switched in patients with DM. The dosing errors that occur with concentrated insulins could increase the risk of hypoglycemia. Pharmacists should provide detailed counseling to DM patients initiating or switching concentrated insulins. It is important to implement or revise institution and clinic safe practices for concentrated insulins to avoid errors in prescribing, distributing, administering, and monitoring these medications.
Conclusion
Concentrated insulins provide expanded treatment options for patients with DM. Clinicians must stay well informed about concentrated insulin characteristics and dosing strategies to optimize DM treatment. As more evidence becomes available, standardized recommendations can be developed to guide clinicians in the appropriate use of concentrated insulins.
Click here to read the digital edition.
For a long time, 500 U/mL (U-500) insulin was the only concentrated insulin available on the market. With many diabetes mellitus (DM) patients requiring larger doses, additional 200 U/mL (U-200) and 300 U/mL (U-300) concentrations became available. As clinical guidelines lack specific recommendations for optimal use of U-200 and U-300 insulins, clinical discretion is warranted in identifying patients for whom use of these insulins is appropriate. U-500 insulin is recommended in cases that require ≥ 200 U/d or > 2 U/kg/d. Given the ongoing DM and obesity epidemics, increased use of concentrated insulins is likely. Clinicians must stay well informed about the characteristics and benefits of concentrated insulins to remain confident recommending, prescribing, and adjusting these medications.
U-200 Insulin Lispro
Pharmacokinetics/Pharmacodynamics
The amino acid structure of U-200 insulin lispro is different from that of endogenous insulin. In U-200 lispro, lysine replaces a proline at position B28, and proline replaces a lysine at position B29.
In a euglycemic clamp study of patients without DM, a 20-U dose of U-200 lispro and a single 20-U dose of U-100 lispro were found to have similar mean area under the glucose infusion rate curves, mean area under the serum insulin concentration-time curves from time 0 to infinity, mean peak serum insulin levels, and time to maximum glucose-lowering effects.1 For both U-200 lispro and U-100 lispro, time to maximum effect was 1 hour.2
Even numbers are marked on the dial of the pen. Odd numbers are not marked, but longer lines appear in their place. U-200 lispro should not be mixed with any other insulin, whereas U-100 lispro can be mixed with neutral protamine Hagedorn insulin.
Safety/Efficacy
There has been 1 bioequivalence study of euglycemic patients without type 2 DM (T2DM) but no studies of the safety or efficacy of U-200 lispro in patients with DM.3,4 U-100 lispro converts 1:1 to U-200 lispro (eg, 60 U of U-100 lispro converts to 60 U of U-200 lispro).1 The volume of U-200 lispro would be smaller than that of U-100 lispro.
Economic Analysis
There are no published U-200 lispro economic analyses.
Dosing
U-200 lispro should be converted from other bolus insulins in a 1:1 ratio.1
Recommendations
Definitive recommendations await efficacy trials comparing use of U-200 lispro and other bolus insulins in patients with DM. Currently, U-200 lispro may be considered for patients with DM who require high doses of bolus insulin and who may benefit from smaller volumes of lispro.
U-200 Insulin Degludec
Pharmacokinetics/Pharmacodynamics
The basal insulin degludec (Tresiba) is available in U-100 and U-200 concentrations in a pen. After subcutaneous injection, degludec forms gradually dissociating multihexamer chains, which account for its flat and stable PK/PD profile. U-100 degludec and U-200 degludec have similar duration of action (≥ 42 hours) and time to steady state (2-3 days).5,6 A patient who misses a regularly scheduled dose should allow at least 8 hours between injections. Taking degludec at variable times does not decrease efficacy as long as this 8-hour minimum interval is observed.7
Safety/Efficacy
During its development, degludec was evaluated in more than 5,000 patients across 11 therapeutic trials.8 The key studies that led to the approval of degludec used insulin glargine as a comparator. In a 52-week study of 1,030 insulin-naïve patients with T2DM, degludec was noninferior to glargine in hemoglobin A1c (HbA1c) reduction (1.06% vs 1.19%). Overall hypoglycemia rates were similar, though there were fewer nocturnal hypoglycemia episodes with degludec than with glargine (0.25 vs 0.39 per patient-year of exposure; P = .38).9
The BEGIN Basal-Bolus trial series evaluated use of degludec combined with bolus insulin aspart in insulin-experienced patients with T2DM (n = 992) and type 1 DM (T1DM) (n = 629) over 52 weeks.10,11 Both trials found noninferiority in A1c reduction: 1.1% (degludec) and 1.18% (glargine) in patients with T2DM and 0.4% (degludec) and 0.39% (glargine) in those with T1DM.10,11 Significantly fewer episodes of overall hypoglycemia (11.09 vs 13.63 per patient-year) and nocturnal hypoglycemia (1.39 vs 1.84 per patient-year) were found with degludec in patients with T2DM.5 Overall hypoglycemia rates were similar, though there was a 25% lower rate of nocturnal hypoglycemia with degludec in patients with T1DM.11
A meta-analysis of 7 phase 3a trials that compared degludec with glargine revealed significantly lower rates of overall, nocturnal, and severe hypoglycemia with degludec in insulin-naïve patients.12 The analysis confirmed findings of significantly lower rates of overall and nocturnal hypoglycemia with degludec in the overall T2DM population and significantly lower rates of nocturnal hypoglycemia in the T1DM population.12
In the DEVOTE trial, which included 7,637 T2DM patients at high risk for a cardiovascular event, degludec and glargine were compared on the composite primary outcome of death with a cardiovascular cause, nonfatal myocardial infarction, or nonfatal stroke. After a median of 1.99 years, the primary outcome occurred in 8.5% of degludec patients and 9.3% of glargine patients (hazard ratio, 0.91; 95% confidence interval, 0.78-1.06; P < .001 for noninferiority). Mean HbA1c level was 7.5 in both groups; severe hypoglycemia occurred more often in the glargine group (odds ratio, 0.73; P < .001 for superiority).13 Findings from the randomized, crossover SWITCH 1 and SWITCH 2 trials confirmed lower rates of symptomatic hypoglycemia with degludec compared with glargine in patients with T1DM and T2DM, respectively.14,15 No statistically significant differences in weight gain were observed in the clinical trials comparing degludec and glargine.
Economic Analysis
Weatherall and colleagues used a budget impact model to evaluate the costs of degludec and glargine for commercially insured patients with DM in the U.S.16 Three treatment groups were analyzed: basal/bolus combination in T1DM and T2DM, and basal/oral combination in T2DM. Although degludec cost more, overall cost was reduced in T1DM because of reduced insulin usage and fewer hypoglycemic episodes in T2DM with basal/oral combination therapy. The authors acknowledged the many assumptions needed and the potential oversimplification of their model.16 In other countries, economic analyses had similar findings.17-19
Dosing
Degludec converts 1:1 to other basal insulins. Recommended starting doses for U-200 degludec are 10 U once daily for insulin-naïve adults with T2DM and one-third to one-half the total weight-based daily insulin dose for insulin-naïve adults with T1DM.4
Recommendations
For some patients, lower PD variability may make degludec a desirable alternative. As degludec retains its efficacy with variable dosing times, it may be ideal for patients who have difficulty with a once-daily dosing schedule. It is important to inform patients that the degludec pen allows for 2-U increments. Given the lower frequency of nocturnal hypoglycemic events with degludec compared with glargine, degludec is an appropriate basal insulin option for patients with nocturnal hypoglycemia. In addition, U-200 degludec may be considered for DM patients who require high doses of basal insulin and who may benefit from smaller volumes of degludec.
U-300 Isulin Glargine
Pharmacokinetics/Pharmacodynamics
U-300 glargine is a concentrated basal insulin. There are notable differences between its U-100 and U-300 concentrations. For U-300 glargine dosed at 0.4 U/kg, duration of action is 24 hours; for U-300 glargine dosed at 0.6 U/kg or higher, longer duration is expected.20 Steady state is reached after 5 days.21 The U-300 glargine pen contains 1.5 mL, less than the 3 mL in the U-100 pen. U-300 glargine typically is administered in 1 injection once daily if the dose is < 80 U; 2 injections are required if the dose is > 80 U.
Safety/Efficacy
In the EDITION trials, which compared U-300 and U-100 glargine in patients with T1DM and T2DM, the primary endpoint was 6-month HbA1c reduction.22-24 Comparable HbA1c reductions were found in all of the studies. In EDITION 1, in which 2,474 patients with T2DM were taking concomitant bolus insulin with or without metformin, 11% more U-300 glargine than U-100 glargine was needed to achieve similar results.22 In EDITION 4, in which bolus insulin was used in combination in 546 patients with T1DM, 17.5% more U-300 glargine than U-100 glargine was needed to achieve similar glycemic goals.25
Economic Analysis
Compared with other insulins, U-300 glargine has limited published data and economic analyses. Using a cost-utility model to compare U-300 with U-100 glargine in Spanish patients with T2DM, and reporting results in euros per quality-adjusted life years, Monero and colleagues concluded that the hypoglycemia reduction and possible time-of-dose flexibility found with U-300 glargine may contribute to its cost-effectiveness.26
Dosing
U-300 glargine should be converted in a 1:1 ratio from U-100 glargine or detemir. The U-300 glargine dose should be reduced by 20% when switching from NPH insulin.21
Recommendations
A meta-analysis of the EDITION trials 1 to 3 revealed a lower incidence of daytime and nocturnal hypoglycemia with use of U-300 glargine over U-100 glargine and a beneficial shorter hold time after injection of U-300 glargine (5 seconds) compared with U-100 glargine (10 seconds).27 There was statistically lower weight gain with U-300 glargine compared with U-100 glargine however weight gain was < 1 kg in both groups.27 These characteristics of U-300 glargine may prove advantageous for individual patients.
U-500 Insulin
Pharmacokinetics/Pharmacodynamics
U-500 insulin (Humulin R) has been available in a vial since 1997, but other formulations have been used therapeutically since 1952.28 The U-500 KwikPen device, recently added to the market, has improved the vial and syringe dosing. The new U-500 BD (Becton, Dickinson, Franklin Lakes, NJ) syringes allow doses up to 250 U, and the U-500 KwikPens provide up to 300 U per injection.29 When it was first introduced, U-500 insulin had no dedicated delivery device and dose conversion was required to deliver the appropriate dose using an allergy or TB syringe. As a consequence, confusion often resulted between prescribers, pharmacists and patients.30,31 U-500 insulin acts as basal and bolus insulins do. Onset of action is ~15 minutes, time to peak is 4 to 8 hours, and duration of action is ≤ 21 hours.32 As its onset of action is similar to that of U-100, U-500 should be injected 30 minutes before meals.
A single-site, randomized, double-blind, crossover euglycemic clamp study that compared equivalent doses of U-500 and U-100 in healthy obese patients found the formulations had similar overall exposures and effects—the only differences were that U-500 had an extended time to peak and a prolonged post-peak effect. The longer post-peak effect contributes to longer duration of action and allows for fewer daily injections.33
Safety/Efficacy
In the Humulin R U-500 Initiation trial, both of these algorithms improved glycemic control and were associated with a low incidence of severe hypoglycemia. In addition, the associated weight gains were similar. Last, the rate of nonsevere hypoglycemia was slightly lower for the 3-times-daily than for the 2-times-daily regimen.34 A real-world outcome analysis of U-500 initiation confirmed the benefits of switching from U-100 to U-500. A clinically significant improvement in glycemic control was found in all the study participants. Dose and frequency of administration, however, were not reported.35
According to a secondary analysis in the Humulin R U-500 Initiation trial, baseline U-100 total daily dose did not yield a difference in efficacy or safety between the 2-times-a-day and 3-times-a-day arms—allowing use of a simpler 2-times-a-day schedule without regard to baseline total daily dose.28,36 The 2-times-a-day regimen is preferred in clinical practice given that the 2 regimens are equivalent in safety and efficacy and that the 2-times-a-day regimen is simpler, allows for easier titrations, improves patient perceptions of the effect of insulin on daily life function and psychological health, lowers daily injection burden, and maximizes adherence.37
Economic Analysis
A retrospective database analysis revealed lower overall cost and lower pharmacy cost associated with U-500 in comparison with high-dose U-100, as well as reduced hypoglycemia-specific costs or resource utilization, even though U-500 was associated with a slightly higher incidence of hypoglycemia.28 However, the fact that hypoglycemia was reported with a billing code (ICD-9) implies the hypoglycemic event was severe enough to require medical attention. Given these findings, 2-times-a-day U-500 seems more cost-effective than high-dose U-100.
Dosing
The U-500 Humulin R package insert recommends converting a dose to U-500 on the basis of most recent HbA1c level. U-500 can be dosed 2 times daily (60%, 40%) or 3 times daily (40%, 30%, 30%). If HbA1c is > 8%, then the starting total daily dose (TDD) of U-500 is 100% of the U-100 TDD. If HbA1c is ≤ 8%, then the starting TDD of U-500 is 80% of the final U-100 TDD (20% reduction). Dose adjustments may range from 5% to 10% depending on subsequent blood glucose readings.32
Recommendations
U-500 is a safe and effective monotherapy alternative for patients who require high doses of U-100. Initial conversion from U-100 is based on HbA1c level. The total daily dose of U-500 is then divided by 2 (60%, 40%) or 3 (40%, 30%, 30%). The 2-times-a-day regimen enhances adherence and thus may be preferred.
Discussion
It has been suggested that large volumes or depots of insulin approaching 100 units impedes absorption and are more painful compared with smaller volume injections.37 For patients with DM who require higher doses of insulin, concentrated insulins offer the advantage of smaller volumes. Also smaller volumes are a substantial benefit in addressing the growing epidemic of DM and the progressive nature of insulin resistance. Furthermore, concentrated insulins are available in pens. Compared with syringes and vials, pens are associated with a lower risk of dosing errors. The major advantages to the use of concentrated insulins include patient acceptability and the potential for decreased volumes and frequency of injections.
Potential disadvantages also exist for the use of concentrated insulins. Depending on insurance coverage, concentrated insulins may be more expensive than U-100 insulin options. Additionally, thorough counseling and education are of paramount importance when concentrated insulins are initiated or switched in patients with DM. The dosing errors that occur with concentrated insulins could increase the risk of hypoglycemia. Pharmacists should provide detailed counseling to DM patients initiating or switching concentrated insulins. It is important to implement or revise institution and clinic safe practices for concentrated insulins to avoid errors in prescribing, distributing, administering, and monitoring these medications.
Conclusion
Concentrated insulins provide expanded treatment options for patients with DM. Clinicians must stay well informed about concentrated insulin characteristics and dosing strategies to optimize DM treatment. As more evidence becomes available, standardized recommendations can be developed to guide clinicians in the appropriate use of concentrated insulins.
Click here to read the digital edition.
1. Humalog [package insert]. Indianapolis, IN: Eli Lilly & Co; 2015.
2. de la Peña A, Seger M, Soon D, et al. Bioequivalence and comparative pharmacodynamics of insulin lispro 200 U/mL relative to insulin lispro (Humalog®) 100 U/mL. Clin Pharmacol Drug Dev. 2016;5(1):69-75.
3. VA Pharmacy Benefits Management Services, Medical Advisory Panel, VISN Phar macist Executives. Insulin Lispro 200units/mL (Humalog) KwikPen abbreviated review. https://www.pbm.va.gov/PBM/clinicalguidance/abbreviatedre views/Insu lin_Lispro_200units_per_mL_Abbreviated_Review.pdf. Published February 2016. Accessed August 22, 2017.
4. Painter NA, Sisson E. An overview of concentrated insulin products. Diabetes Spectr. 2016;29(3):136-140.
5. Korsatko S, Deller S, Koehler G, et al. A comparison of the steady-state pharmacokinetic and pharmacodynamic profiles of 100 and 200 U/mL formulations of ultra-long-acting insulin degludec. Clin Drug Investig. 2013;33(7):515-521.
6. Goldman-Levine JD, Patel DK, Schnee DM. Insulin degludec: a novel basal insulin analogue. Ann Pharmacother. 2013;47(2):269-277.
7. Meneghini L, Atkin SL, Gouch SC, et al; NN1250-3668 (BEGIN FLEX) Trial Investigators. The efficacy and safety of insulin degludec given in variable once-daily dosing intervals compared with insulin glargine and insulin degludec dosed at the same time daily: a 26-week, randomized, open-label, parallel-group, treat-to-target trial in individuals with type 2 diabetes. Diabetes Care. 2013;36(4):858-864.
8. Rendell M. United States experience of insulin degludec alone or in combination for type 1 and type 2 diabetes. Drug Des Dev Ther. 2017;11:1209-1220.
9. Zinman B, Philis-Tsimikas A, Caropi B, et al; NN1250-3579 (BEGIN Once Long) Trial Investigators. Insulin degludec versus insulin glargine in insulin-naive patients with type 2 diabetes: a 1-year, randomized, treat-to-target trial (BEGIN Once Long). Diabetes Care. 2012;35(12):2464-2471.
10. Garber AJ, King AB, Del Prato S, et al; NN1250-3582 (BEGIN BB T2D) Trial Investigators. Insulin degludec, an ultra-longacting basal insulin, versus insulin glargine in basal-bolus treatment with mealtime insulin aspart in type 2 diabetes (BEGIN Basal-Bolus Type 2): a phase 3, randomised, open-label, treat-to-target non-inferiority trial. Lancet. 2012;379(9825):1498-1507.
11. Heller S, Buse J, Fisher M, et al; BEGIN Basal-Bolus Type 1 Trial Investigators. Insulin degludec, an ultra-longacting basal insulin, versus insulin glargine in basal-bolus treatment with mealtime insulin aspart in type 1 diabetes (BEGIN Basal-Bolus Type 1): a phase 3, randomised, open-label, treat-to-target non-inferiority trial. Lancet. 2012;379(9825):1489-1497.
12. Ratner RE, Gough SC, Mathieu C, et al. Hypoglycaemia risk with insulin degludec compared with insulin glargine in type 2 and type 1 diabetes: a pre-planned meta-analysis of phase 3 trials. Diabetes Obes Metab. 2013;15(2):175-184.
13. Marso SP, McGuire DK, Zinman B, et al; DEVOTE Study Group. Efficacy and safety of degludec versus glargine in type 2 diabetes. N Engl J Med. 2017;377(8):723-732.
14. Lane W, Bailey TS, Gerety G, et al; Group Information; SWITCH 1. Effect of insulin degludec vs insulin glargine U100 on hypoglycemia in patients with type 1 diabetes: the SWITCH 1 randomized clinical trial. JAMA. 2017;318(1):33-44.
15. Wysham C, Bhargava A, Chaykin L, et al. Effect of insulin degludec vs insulin glargine U100 on hypoglycemia in patients with type 2 diabetes: the SWITCH 2 randomized clinical trial. JAMA. 2017;318(1):45-56.
16. Weatherall J, Bludek L, Buchs S. Budget impact of treating commercially insured type 1 and type 2 diabetes patients in the United States with insulin degludec compared to insulin glargine. Curr Med Res Opin. 2017;33(2):231-238.
17. Mezquita-Raya P, Darbà J, Ascanio M, Ramírez de Arellano A. Cost-effectiveness analysis of insulin degludec compared with insulin glargine u100 for the management of type 1 and type 2 diabetes mellitus—from the Spanish National Health System perspective. Expert Rev Pharmacoecon Outcomes Res. 2017:1-9. [Epub ahead of print.]
18. Landstedt-Hallin L, Gundgaard J, Ericsson Å, Ellfors-Zetterlund S. Cost-effectiveness of switching to insulin degludec from other basal insulins: evidence from Swedish real-world data. Curr Med Res Opin. 2017;33(4):647-655.
19. Pollock RF, Tikkanen CK. A short-term cost-utility analysis of insulin degludec versus insulin glargine U100 in patients with type 1 or type 2 diabetes in Denmark. J Med Econ. 2017;20(3):213-220.
20. Becker RH, Dahmen R, Bergmann K, Lehmann A, Jax T, Heise T. New insulin glargine 300 units · mL-1 provides a more even activity profile and prolonged glycemic control at steady state compared with insulin glargine 100 units · mL-1. Diabetes Care. 2015;38(4):637-643.
21. Toujeo [package insert]. Bridgewater, NJ: Sanofi-Aventis; 2015.
22. Riddle MC, Bolli GB, Ziemen M, Muehlen-Bartmer I, Bizet F, Home PD; EDITION 1 Study Investigators. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 2 diabetes using basal and mealtime insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 1). Diabetes Care. 2014;37(10):2755-2762.
23. Yki-Järvinen H, Bergenstal R, Ziemen M, et al; EDITION 2 Study Investigators. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 2 diabetes using oral agents and basal insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 2). Diabetes Care. 2014;37(12):3235-3243.
24. Bolli GB, Riddle MC, Bergenstal RM, et al; on behalf of the EDITION 3 Study Investigators. New insulin glargine 300 U/ml compared with glargine 100 U/ml in insulin-naïve people with type 2 diabetes on oral glucose-lowering drugs: a randomized controlled trial (EDITION 3). Diabetes Obes Metab. 2015;17(4):386-394.
25. Home PD, Bergenstal RM, Bolli GB, et al. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 1 diabetes: a randomized, phase 3a, open-label clinical trial (EDITION 4). Diabetes Care. 2015;38(12):2217-2225.
26. Monero S, Delgado M, Rubio M, Gasche D, Fournier M. Cost-utility evaluation of insulin glargine 300 (GLA-300) versus insulin glargine 100 (GLA-100) in patients with type 2 diabetes mellitus (T2DM). Poster presented at: International Society for Pharmacoeconomics and Outcomes Research (ISPOR) 19th Annual European Congress; October 29-November 2, 2016; Vienna, Austria.
27. Ritzel R, Roussel R, Bolli GB, et al. Patient-level meta-analysis of the EDITION 1, 2 and 3 studies: glycaemic control and hypoglycaemia with new insulin glargine 300 U/ml versus glargine 100 U/ml in people with type 2 diabetes. Diabetes Obes Metab. 2015;17(9):859-867.
28. Eby EL, Wang P, Curtis BH, et al. Cost, healthcare resource utilization, and adherence of individuals with diabetes using U-500 or U-100 insulin: a retrospective database analysis. J Med Econ. 2013;16(4):529-538.
29. Lilly USA. Pharmacy tips about Humulin R U-500 KwikPen syringe and vial. http://www.humulin.com/pharmacy-tips.aspx#about-the-u500-syringe_and_vial. Accessed
30. Meneghini, L. New insulin preparations: a primer for the clinician. Cleve Clin J Med. 2016;83(5 suppl 1):S27-S33.
31. Humulin R U-500 KwikPen [package insert]. Indianapolis, IN: Eli Lilly & Co; 2016.
32. de la Peña A, Riddle M, Morrow LA, et al. Pharmacokinetics and pharmacodynamics of high-dose human regular U-500 insulin versus human regular U-100 insulin in healthy obese subjects. Diabetes Care. 2011;34(12):2496-2501.
33. Hood RC, Arakaki RF, Wysham C, Li YG, Settles JA, Jackson JA. Two treatment approaches for human regular U-500 insulin in patients with type 2 diabetes not achieving adequate glycemic control on high-dose U-100 insulin therapy with or without oral agents: a randomized, titration-to-target clinical trial. Endocr Pract. 2015;21(7):782-793.
34. Eby EL, Curtis BH, Gelwicks SC, et al. Initiation of human regular U-500 insulin use is associated with improved glycemic control: a real-world US cohort study. BMJ Open Diabetes Res Care. 2015;3(1):e000074.
35. Wysham C, Hood RC, Warren ML, Wang T, Morwick TM, Jackson JA. Effect of total daily dose on efficacy, dosing, and safety of 2 dose titration regimens of human regular U500 insulin in severely insulin-resistant patients with type 2 diabetes. Endocr Pract. 2016;22(6):653-665.
36. Kabul S, Hood RC, Duan R, DeLozier AM, Settles J. Patient-reported outcomes in transition from high-dose U-100 insulin to human regular U-500 insulin in severely insulin-resistant patients with type 2 diabetes: analysis of a randomized clinical trial. Health Qual Life Outcomes. 2016;14(1):139.
37. Hirsch IB. Lipodystrophy: metabolic and clinical aspects. https://www.endo crine.org/~/media/endosociety/files/education/lypodystrophy-files/hirsch_tdeg-2013_lrc_final.pdf?la=en. Accessed September 7, 2017.
1. Humalog [package insert]. Indianapolis, IN: Eli Lilly & Co; 2015.
2. de la Peña A, Seger M, Soon D, et al. Bioequivalence and comparative pharmacodynamics of insulin lispro 200 U/mL relative to insulin lispro (Humalog®) 100 U/mL. Clin Pharmacol Drug Dev. 2016;5(1):69-75.
3. VA Pharmacy Benefits Management Services, Medical Advisory Panel, VISN Phar macist Executives. Insulin Lispro 200units/mL (Humalog) KwikPen abbreviated review. https://www.pbm.va.gov/PBM/clinicalguidance/abbreviatedre views/Insu lin_Lispro_200units_per_mL_Abbreviated_Review.pdf. Published February 2016. Accessed August 22, 2017.
4. Painter NA, Sisson E. An overview of concentrated insulin products. Diabetes Spectr. 2016;29(3):136-140.
5. Korsatko S, Deller S, Koehler G, et al. A comparison of the steady-state pharmacokinetic and pharmacodynamic profiles of 100 and 200 U/mL formulations of ultra-long-acting insulin degludec. Clin Drug Investig. 2013;33(7):515-521.
6. Goldman-Levine JD, Patel DK, Schnee DM. Insulin degludec: a novel basal insulin analogue. Ann Pharmacother. 2013;47(2):269-277.
7. Meneghini L, Atkin SL, Gouch SC, et al; NN1250-3668 (BEGIN FLEX) Trial Investigators. The efficacy and safety of insulin degludec given in variable once-daily dosing intervals compared with insulin glargine and insulin degludec dosed at the same time daily: a 26-week, randomized, open-label, parallel-group, treat-to-target trial in individuals with type 2 diabetes. Diabetes Care. 2013;36(4):858-864.
8. Rendell M. United States experience of insulin degludec alone or in combination for type 1 and type 2 diabetes. Drug Des Dev Ther. 2017;11:1209-1220.
9. Zinman B, Philis-Tsimikas A, Caropi B, et al; NN1250-3579 (BEGIN Once Long) Trial Investigators. Insulin degludec versus insulin glargine in insulin-naive patients with type 2 diabetes: a 1-year, randomized, treat-to-target trial (BEGIN Once Long). Diabetes Care. 2012;35(12):2464-2471.
10. Garber AJ, King AB, Del Prato S, et al; NN1250-3582 (BEGIN BB T2D) Trial Investigators. Insulin degludec, an ultra-longacting basal insulin, versus insulin glargine in basal-bolus treatment with mealtime insulin aspart in type 2 diabetes (BEGIN Basal-Bolus Type 2): a phase 3, randomised, open-label, treat-to-target non-inferiority trial. Lancet. 2012;379(9825):1498-1507.
11. Heller S, Buse J, Fisher M, et al; BEGIN Basal-Bolus Type 1 Trial Investigators. Insulin degludec, an ultra-longacting basal insulin, versus insulin glargine in basal-bolus treatment with mealtime insulin aspart in type 1 diabetes (BEGIN Basal-Bolus Type 1): a phase 3, randomised, open-label, treat-to-target non-inferiority trial. Lancet. 2012;379(9825):1489-1497.
12. Ratner RE, Gough SC, Mathieu C, et al. Hypoglycaemia risk with insulin degludec compared with insulin glargine in type 2 and type 1 diabetes: a pre-planned meta-analysis of phase 3 trials. Diabetes Obes Metab. 2013;15(2):175-184.
13. Marso SP, McGuire DK, Zinman B, et al; DEVOTE Study Group. Efficacy and safety of degludec versus glargine in type 2 diabetes. N Engl J Med. 2017;377(8):723-732.
14. Lane W, Bailey TS, Gerety G, et al; Group Information; SWITCH 1. Effect of insulin degludec vs insulin glargine U100 on hypoglycemia in patients with type 1 diabetes: the SWITCH 1 randomized clinical trial. JAMA. 2017;318(1):33-44.
15. Wysham C, Bhargava A, Chaykin L, et al. Effect of insulin degludec vs insulin glargine U100 on hypoglycemia in patients with type 2 diabetes: the SWITCH 2 randomized clinical trial. JAMA. 2017;318(1):45-56.
16. Weatherall J, Bludek L, Buchs S. Budget impact of treating commercially insured type 1 and type 2 diabetes patients in the United States with insulin degludec compared to insulin glargine. Curr Med Res Opin. 2017;33(2):231-238.
17. Mezquita-Raya P, Darbà J, Ascanio M, Ramírez de Arellano A. Cost-effectiveness analysis of insulin degludec compared with insulin glargine u100 for the management of type 1 and type 2 diabetes mellitus—from the Spanish National Health System perspective. Expert Rev Pharmacoecon Outcomes Res. 2017:1-9. [Epub ahead of print.]
18. Landstedt-Hallin L, Gundgaard J, Ericsson Å, Ellfors-Zetterlund S. Cost-effectiveness of switching to insulin degludec from other basal insulins: evidence from Swedish real-world data. Curr Med Res Opin. 2017;33(4):647-655.
19. Pollock RF, Tikkanen CK. A short-term cost-utility analysis of insulin degludec versus insulin glargine U100 in patients with type 1 or type 2 diabetes in Denmark. J Med Econ. 2017;20(3):213-220.
20. Becker RH, Dahmen R, Bergmann K, Lehmann A, Jax T, Heise T. New insulin glargine 300 units · mL-1 provides a more even activity profile and prolonged glycemic control at steady state compared with insulin glargine 100 units · mL-1. Diabetes Care. 2015;38(4):637-643.
21. Toujeo [package insert]. Bridgewater, NJ: Sanofi-Aventis; 2015.
22. Riddle MC, Bolli GB, Ziemen M, Muehlen-Bartmer I, Bizet F, Home PD; EDITION 1 Study Investigators. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 2 diabetes using basal and mealtime insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 1). Diabetes Care. 2014;37(10):2755-2762.
23. Yki-Järvinen H, Bergenstal R, Ziemen M, et al; EDITION 2 Study Investigators. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 2 diabetes using oral agents and basal insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 2). Diabetes Care. 2014;37(12):3235-3243.
24. Bolli GB, Riddle MC, Bergenstal RM, et al; on behalf of the EDITION 3 Study Investigators. New insulin glargine 300 U/ml compared with glargine 100 U/ml in insulin-naïve people with type 2 diabetes on oral glucose-lowering drugs: a randomized controlled trial (EDITION 3). Diabetes Obes Metab. 2015;17(4):386-394.
25. Home PD, Bergenstal RM, Bolli GB, et al. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 1 diabetes: a randomized, phase 3a, open-label clinical trial (EDITION 4). Diabetes Care. 2015;38(12):2217-2225.
26. Monero S, Delgado M, Rubio M, Gasche D, Fournier M. Cost-utility evaluation of insulin glargine 300 (GLA-300) versus insulin glargine 100 (GLA-100) in patients with type 2 diabetes mellitus (T2DM). Poster presented at: International Society for Pharmacoeconomics and Outcomes Research (ISPOR) 19th Annual European Congress; October 29-November 2, 2016; Vienna, Austria.
27. Ritzel R, Roussel R, Bolli GB, et al. Patient-level meta-analysis of the EDITION 1, 2 and 3 studies: glycaemic control and hypoglycaemia with new insulin glargine 300 U/ml versus glargine 100 U/ml in people with type 2 diabetes. Diabetes Obes Metab. 2015;17(9):859-867.
28. Eby EL, Wang P, Curtis BH, et al. Cost, healthcare resource utilization, and adherence of individuals with diabetes using U-500 or U-100 insulin: a retrospective database analysis. J Med Econ. 2013;16(4):529-538.
29. Lilly USA. Pharmacy tips about Humulin R U-500 KwikPen syringe and vial. http://www.humulin.com/pharmacy-tips.aspx#about-the-u500-syringe_and_vial. Accessed
30. Meneghini, L. New insulin preparations: a primer for the clinician. Cleve Clin J Med. 2016;83(5 suppl 1):S27-S33.
31. Humulin R U-500 KwikPen [package insert]. Indianapolis, IN: Eli Lilly & Co; 2016.
32. de la Peña A, Riddle M, Morrow LA, et al. Pharmacokinetics and pharmacodynamics of high-dose human regular U-500 insulin versus human regular U-100 insulin in healthy obese subjects. Diabetes Care. 2011;34(12):2496-2501.
33. Hood RC, Arakaki RF, Wysham C, Li YG, Settles JA, Jackson JA. Two treatment approaches for human regular U-500 insulin in patients with type 2 diabetes not achieving adequate glycemic control on high-dose U-100 insulin therapy with or without oral agents: a randomized, titration-to-target clinical trial. Endocr Pract. 2015;21(7):782-793.
34. Eby EL, Curtis BH, Gelwicks SC, et al. Initiation of human regular U-500 insulin use is associated with improved glycemic control: a real-world US cohort study. BMJ Open Diabetes Res Care. 2015;3(1):e000074.
35. Wysham C, Hood RC, Warren ML, Wang T, Morwick TM, Jackson JA. Effect of total daily dose on efficacy, dosing, and safety of 2 dose titration regimens of human regular U500 insulin in severely insulin-resistant patients with type 2 diabetes. Endocr Pract. 2016;22(6):653-665.
36. Kabul S, Hood RC, Duan R, DeLozier AM, Settles J. Patient-reported outcomes in transition from high-dose U-100 insulin to human regular U-500 insulin in severely insulin-resistant patients with type 2 diabetes: analysis of a randomized clinical trial. Health Qual Life Outcomes. 2016;14(1):139.
37. Hirsch IB. Lipodystrophy: metabolic and clinical aspects. https://www.endo crine.org/~/media/endosociety/files/education/lypodystrophy-files/hirsch_tdeg-2013_lrc_final.pdf?la=en. Accessed September 7, 2017.