User login
AMA Town Hall: Doctors call for meaningful use delay
Stage 3 of meaningful use should be delayed until Medicare value-based care programs are developed.
To move the Centers for Medicare & Medicaid Services toward that goal, the American Medical Association has created a new website – Break the Red Tape – where physicians can share their good and bad experiences with electronic health records (EHRs) in an effort to help policymakers understand the landscape.
“We want to hear … both what is working so that we can help try to make that happen, but we also need to hear what is not working so that we can send a clear message through our stories, through our real-world experience, to those in policymaking so that they can help us to craft better policies and a better program that will make electronic health records and the policies that the federal government that seek to advance and support the adoption of those tools more effective,” Dr. Stephen Stack, AMA president said July 20 during a town hall event in Atlanta.
At the event, physicians shared how EHRs have affected their practices; many of the comments were negative, though a few bright spots, including electronic prescribing, were highlighted.
Dr. Stack summed up the majority of comments under two key points – usability and interoperability.
“We’ve got to fix the usability, and you all have clearly shown through your stories that information is not being exchanged and that’s not our fault because we didn’t write the code and we didn’t build the wires that connect it,” he said.
Usability issues have translated to decreased productivity, even for those who are experienced in with EHRs. Dr. Melissa Rhodes, a pulmonary, critical care, and sleep physician at Respiratory Consultants of Georgia, said that even though she has been using EHRs since 2006, she still faces a loss of patient care time.
“Every time they have more regulations, more things that I have to answer, takes time away from the patient,” Dr. Rhodes said. She said that she currently sees two-thirds of the patients she could see, and added that she is now asking prospective employees if they know how to type, acknowledging that without that skill, her work flow would be even less productive.
Another comment on usability came from Dr. Albert Johary, a solo-practice internist in Dunwoody, Ga., who has participated in meaningful use for 4 years. He highlighted smoking cessation to illustrate how EHRs are making things more challenging. Prior to EHRs, he would chart that a patient was wanting help to quit smoking and note a prescription for varenicline.
With the EHR he is using now, which he did not identify, he said that he must account for a number of different steps.
“What I’ve started doing is I am doing this in front of the patients,” Dr. Johary said. “I am trying to work with it. I think meaningful use is not necessarily a bad thing,” but even giving notes to a patient is “a four- or five-step process.”
Interoperability “is a major issue” as well, he said, noting that he is part of the Emory Integrated Health Network and now is having to switch EHRs because of the lack of interoperability with the network.
Dr. Stack noted that the AMA supports the alignment of meaningful use with the coming value-based payment reforms. “We do believe that we should pause Stage 3 meaningful use so that it can align with these other new payment delivery models as we go forward,” he said. “We are now going to have the MIPS [Merit-based Incentive Payment System] program, which is going to have meaningful use as a substantial portion of it,” Dr. Stack continued. “We think that the rule making for these two should happen concurrently so that it makes sense when it comes out, not that we do them wrong the first time and have to redo them again to make it all make sense.”
Stage 3 of meaningful use should be delayed until Medicare value-based care programs are developed.
To move the Centers for Medicare & Medicaid Services toward that goal, the American Medical Association has created a new website – Break the Red Tape – where physicians can share their good and bad experiences with electronic health records (EHRs) in an effort to help policymakers understand the landscape.
“We want to hear … both what is working so that we can help try to make that happen, but we also need to hear what is not working so that we can send a clear message through our stories, through our real-world experience, to those in policymaking so that they can help us to craft better policies and a better program that will make electronic health records and the policies that the federal government that seek to advance and support the adoption of those tools more effective,” Dr. Stephen Stack, AMA president said July 20 during a town hall event in Atlanta.
At the event, physicians shared how EHRs have affected their practices; many of the comments were negative, though a few bright spots, including electronic prescribing, were highlighted.
Dr. Stack summed up the majority of comments under two key points – usability and interoperability.
“We’ve got to fix the usability, and you all have clearly shown through your stories that information is not being exchanged and that’s not our fault because we didn’t write the code and we didn’t build the wires that connect it,” he said.
Usability issues have translated to decreased productivity, even for those who are experienced in with EHRs. Dr. Melissa Rhodes, a pulmonary, critical care, and sleep physician at Respiratory Consultants of Georgia, said that even though she has been using EHRs since 2006, she still faces a loss of patient care time.
“Every time they have more regulations, more things that I have to answer, takes time away from the patient,” Dr. Rhodes said. She said that she currently sees two-thirds of the patients she could see, and added that she is now asking prospective employees if they know how to type, acknowledging that without that skill, her work flow would be even less productive.
Another comment on usability came from Dr. Albert Johary, a solo-practice internist in Dunwoody, Ga., who has participated in meaningful use for 4 years. He highlighted smoking cessation to illustrate how EHRs are making things more challenging. Prior to EHRs, he would chart that a patient was wanting help to quit smoking and note a prescription for varenicline.
With the EHR he is using now, which he did not identify, he said that he must account for a number of different steps.
“What I’ve started doing is I am doing this in front of the patients,” Dr. Johary said. “I am trying to work with it. I think meaningful use is not necessarily a bad thing,” but even giving notes to a patient is “a four- or five-step process.”
Interoperability “is a major issue” as well, he said, noting that he is part of the Emory Integrated Health Network and now is having to switch EHRs because of the lack of interoperability with the network.
Dr. Stack noted that the AMA supports the alignment of meaningful use with the coming value-based payment reforms. “We do believe that we should pause Stage 3 meaningful use so that it can align with these other new payment delivery models as we go forward,” he said. “We are now going to have the MIPS [Merit-based Incentive Payment System] program, which is going to have meaningful use as a substantial portion of it,” Dr. Stack continued. “We think that the rule making for these two should happen concurrently so that it makes sense when it comes out, not that we do them wrong the first time and have to redo them again to make it all make sense.”
Stage 3 of meaningful use should be delayed until Medicare value-based care programs are developed.
To move the Centers for Medicare & Medicaid Services toward that goal, the American Medical Association has created a new website – Break the Red Tape – where physicians can share their good and bad experiences with electronic health records (EHRs) in an effort to help policymakers understand the landscape.
“We want to hear … both what is working so that we can help try to make that happen, but we also need to hear what is not working so that we can send a clear message through our stories, through our real-world experience, to those in policymaking so that they can help us to craft better policies and a better program that will make electronic health records and the policies that the federal government that seek to advance and support the adoption of those tools more effective,” Dr. Stephen Stack, AMA president said July 20 during a town hall event in Atlanta.
At the event, physicians shared how EHRs have affected their practices; many of the comments were negative, though a few bright spots, including electronic prescribing, were highlighted.
Dr. Stack summed up the majority of comments under two key points – usability and interoperability.
“We’ve got to fix the usability, and you all have clearly shown through your stories that information is not being exchanged and that’s not our fault because we didn’t write the code and we didn’t build the wires that connect it,” he said.
Usability issues have translated to decreased productivity, even for those who are experienced in with EHRs. Dr. Melissa Rhodes, a pulmonary, critical care, and sleep physician at Respiratory Consultants of Georgia, said that even though she has been using EHRs since 2006, she still faces a loss of patient care time.
“Every time they have more regulations, more things that I have to answer, takes time away from the patient,” Dr. Rhodes said. She said that she currently sees two-thirds of the patients she could see, and added that she is now asking prospective employees if they know how to type, acknowledging that without that skill, her work flow would be even less productive.
Another comment on usability came from Dr. Albert Johary, a solo-practice internist in Dunwoody, Ga., who has participated in meaningful use for 4 years. He highlighted smoking cessation to illustrate how EHRs are making things more challenging. Prior to EHRs, he would chart that a patient was wanting help to quit smoking and note a prescription for varenicline.
With the EHR he is using now, which he did not identify, he said that he must account for a number of different steps.
“What I’ve started doing is I am doing this in front of the patients,” Dr. Johary said. “I am trying to work with it. I think meaningful use is not necessarily a bad thing,” but even giving notes to a patient is “a four- or five-step process.”
Interoperability “is a major issue” as well, he said, noting that he is part of the Emory Integrated Health Network and now is having to switch EHRs because of the lack of interoperability with the network.
Dr. Stack noted that the AMA supports the alignment of meaningful use with the coming value-based payment reforms. “We do believe that we should pause Stage 3 meaningful use so that it can align with these other new payment delivery models as we go forward,” he said. “We are now going to have the MIPS [Merit-based Incentive Payment System] program, which is going to have meaningful use as a substantial portion of it,” Dr. Stack continued. “We think that the rule making for these two should happen concurrently so that it makes sense when it comes out, not that we do them wrong the first time and have to redo them again to make it all make sense.”
Joint Commission launches hospital acute stroke certification
The Joint Commission and the American Heart Association/American Stroke Association have launched a new Disease-Specific Care Advanced Certification Program for Acute Stroke Ready Hospitals.
The certification program targets accredited hospitals that would not otherwise be candidates for Primary Stroke Center or Comprehensive Stroke Center certification.
Eligible hospitals must have a dedicated stroke-focused program, be staffed by medical professionals trained in stroke care, be able to perform rapid diagnostic and laboratory testing 24/7, be able to administer clot-busting medications, have access to telemedicine services, and have established transfer agreements/protocols with facilities that provide primary or comprehensive stroke services.
“This new certification acts as an important bridge and will be a key component in an evolving system of stroke care,” Wendi Roberts, executive director of certification programs for the Joint Commission, said in a statement. “An Acute Stroke Ready Hospital will be the foundation for acute stroke care in many communities, allowing it to be the first step on a patient’s acute stroke journey before being transferred to a Primary Stroke Center or Comprehensive Stroke Center.”
Hospitals could apply for certification beginning July 1.
The Joint Commission and the American Heart Association/American Stroke Association have launched a new Disease-Specific Care Advanced Certification Program for Acute Stroke Ready Hospitals.
The certification program targets accredited hospitals that would not otherwise be candidates for Primary Stroke Center or Comprehensive Stroke Center certification.
Eligible hospitals must have a dedicated stroke-focused program, be staffed by medical professionals trained in stroke care, be able to perform rapid diagnostic and laboratory testing 24/7, be able to administer clot-busting medications, have access to telemedicine services, and have established transfer agreements/protocols with facilities that provide primary or comprehensive stroke services.
“This new certification acts as an important bridge and will be a key component in an evolving system of stroke care,” Wendi Roberts, executive director of certification programs for the Joint Commission, said in a statement. “An Acute Stroke Ready Hospital will be the foundation for acute stroke care in many communities, allowing it to be the first step on a patient’s acute stroke journey before being transferred to a Primary Stroke Center or Comprehensive Stroke Center.”
Hospitals could apply for certification beginning July 1.
The Joint Commission and the American Heart Association/American Stroke Association have launched a new Disease-Specific Care Advanced Certification Program for Acute Stroke Ready Hospitals.
The certification program targets accredited hospitals that would not otherwise be candidates for Primary Stroke Center or Comprehensive Stroke Center certification.
Eligible hospitals must have a dedicated stroke-focused program, be staffed by medical professionals trained in stroke care, be able to perform rapid diagnostic and laboratory testing 24/7, be able to administer clot-busting medications, have access to telemedicine services, and have established transfer agreements/protocols with facilities that provide primary or comprehensive stroke services.
“This new certification acts as an important bridge and will be a key component in an evolving system of stroke care,” Wendi Roberts, executive director of certification programs for the Joint Commission, said in a statement. “An Acute Stroke Ready Hospital will be the foundation for acute stroke care in many communities, allowing it to be the first step on a patient’s acute stroke journey before being transferred to a Primary Stroke Center or Comprehensive Stroke Center.”
Hospitals could apply for certification beginning July 1.
GI societies prepare to fight colonoscopy Medicare rate cuts
Once again, gastroenterologists are preparing to challenge the Centers for Medicare & Medicaid Services (CMS) on proposed cuts to reimbursement for colonoscopies and related services.
The payment update is included in the recent proposed update to the physician fee schedule and will involve various payment cuts, including a 19% reduction in payments for colonoscopy with biopsy, a 12% reduction for colonoscopy with snare polypectomy, and an 11% reduction for colonoscopy with no other ancillary services.
“These reductions are based on flawed methodology,” said Dr. Rajeev Jain, chief of gastroenterology at Presbyterian Hospital of Dallas and a member of the American Gastroenterological Association (AGA) governing board. “They did not use all the survey data that was provided by gastroenterologists. Rather, they used data from other specialties.”
Dr. Jain noted that in 2014, the AGA, along with the American College of Gastroenterology (ACG) and the American Society for Gastrointestinal Endoscopy, (ASGE), were able to convince the CMS to hold off putting the rate cuts into effect for the 2015 calendar year because there was a lack of transparency in the data that prevented the medical societies from properly responding to the rate cuts.
But the agency is relying on the same data sources as in the previous year, and “to use the same flawed logic doesn’t make any sense,” Dr. Jain said.
The CMS in 2012 identified colonoscopy among other procedures as being potentially misvalued. The AGA, ACG, and ASGE provided survey data and recommendations to support proper reimbursement, but they contend that the American Medical Association/Specialty Society Relative Value Scale Update Committee (RUC) ultimately used data from another specialty to determine the value of colonoscopy services, resulting in the payment cut recommendations. The RUC recently was criticized in a Government Accountability Office report for its members having conflicts of interest that could affect how physician services are valued.
Dr. Jain said that what gastroenterologists are getting paid right now from Medicare “barely covers the costs of that care,” and he suggested that if these “draconian” cuts are implemented, patient access could suffer, and it could have an unintended consequence of driving colonoscopy costs higher overall.
The cuts could lead to gastroenterologists limiting their performing of this procedure within their Medicare population or withdrawing from Medicare altogether, he said. The cuts could also lead to more procedures being conducted in the hospital outpatient setting, where Medicare pays more for the procedure than in ambulatory surgical centers, which he said can be more cost effective and are a more patient-friendly environment.
Comments on the proposal are due to the CMS by Sept. 8.
Once again, gastroenterologists are preparing to challenge the Centers for Medicare & Medicaid Services (CMS) on proposed cuts to reimbursement for colonoscopies and related services.
The payment update is included in the recent proposed update to the physician fee schedule and will involve various payment cuts, including a 19% reduction in payments for colonoscopy with biopsy, a 12% reduction for colonoscopy with snare polypectomy, and an 11% reduction for colonoscopy with no other ancillary services.
“These reductions are based on flawed methodology,” said Dr. Rajeev Jain, chief of gastroenterology at Presbyterian Hospital of Dallas and a member of the American Gastroenterological Association (AGA) governing board. “They did not use all the survey data that was provided by gastroenterologists. Rather, they used data from other specialties.”
Dr. Jain noted that in 2014, the AGA, along with the American College of Gastroenterology (ACG) and the American Society for Gastrointestinal Endoscopy, (ASGE), were able to convince the CMS to hold off putting the rate cuts into effect for the 2015 calendar year because there was a lack of transparency in the data that prevented the medical societies from properly responding to the rate cuts.
But the agency is relying on the same data sources as in the previous year, and “to use the same flawed logic doesn’t make any sense,” Dr. Jain said.
The CMS in 2012 identified colonoscopy among other procedures as being potentially misvalued. The AGA, ACG, and ASGE provided survey data and recommendations to support proper reimbursement, but they contend that the American Medical Association/Specialty Society Relative Value Scale Update Committee (RUC) ultimately used data from another specialty to determine the value of colonoscopy services, resulting in the payment cut recommendations. The RUC recently was criticized in a Government Accountability Office report for its members having conflicts of interest that could affect how physician services are valued.
Dr. Jain said that what gastroenterologists are getting paid right now from Medicare “barely covers the costs of that care,” and he suggested that if these “draconian” cuts are implemented, patient access could suffer, and it could have an unintended consequence of driving colonoscopy costs higher overall.
The cuts could lead to gastroenterologists limiting their performing of this procedure within their Medicare population or withdrawing from Medicare altogether, he said. The cuts could also lead to more procedures being conducted in the hospital outpatient setting, where Medicare pays more for the procedure than in ambulatory surgical centers, which he said can be more cost effective and are a more patient-friendly environment.
Comments on the proposal are due to the CMS by Sept. 8.
Once again, gastroenterologists are preparing to challenge the Centers for Medicare & Medicaid Services (CMS) on proposed cuts to reimbursement for colonoscopies and related services.
The payment update is included in the recent proposed update to the physician fee schedule and will involve various payment cuts, including a 19% reduction in payments for colonoscopy with biopsy, a 12% reduction for colonoscopy with snare polypectomy, and an 11% reduction for colonoscopy with no other ancillary services.
“These reductions are based on flawed methodology,” said Dr. Rajeev Jain, chief of gastroenterology at Presbyterian Hospital of Dallas and a member of the American Gastroenterological Association (AGA) governing board. “They did not use all the survey data that was provided by gastroenterologists. Rather, they used data from other specialties.”
Dr. Jain noted that in 2014, the AGA, along with the American College of Gastroenterology (ACG) and the American Society for Gastrointestinal Endoscopy, (ASGE), were able to convince the CMS to hold off putting the rate cuts into effect for the 2015 calendar year because there was a lack of transparency in the data that prevented the medical societies from properly responding to the rate cuts.
But the agency is relying on the same data sources as in the previous year, and “to use the same flawed logic doesn’t make any sense,” Dr. Jain said.
The CMS in 2012 identified colonoscopy among other procedures as being potentially misvalued. The AGA, ACG, and ASGE provided survey data and recommendations to support proper reimbursement, but they contend that the American Medical Association/Specialty Society Relative Value Scale Update Committee (RUC) ultimately used data from another specialty to determine the value of colonoscopy services, resulting in the payment cut recommendations. The RUC recently was criticized in a Government Accountability Office report for its members having conflicts of interest that could affect how physician services are valued.
Dr. Jain said that what gastroenterologists are getting paid right now from Medicare “barely covers the costs of that care,” and he suggested that if these “draconian” cuts are implemented, patient access could suffer, and it could have an unintended consequence of driving colonoscopy costs higher overall.
The cuts could lead to gastroenterologists limiting their performing of this procedure within their Medicare population or withdrawing from Medicare altogether, he said. The cuts could also lead to more procedures being conducted in the hospital outpatient setting, where Medicare pays more for the procedure than in ambulatory surgical centers, which he said can be more cost effective and are a more patient-friendly environment.
Comments on the proposal are due to the CMS by Sept. 8.
21st Century Cures bill passes House
The House has overwhemingly passed the 21st Century Cures Act, H.R. 6, a broad piece of legislation aimed at streamlining the approval process for medical drugs and devices.
The bill, passed by a 344-77 vote on July 10, also aims to spur innovation in biomedical research and to boost funding to the National Institutes of Health.
Changes made prior to the bill’s introduction to the House floor raised the ire of some legislators and included a reduction in NIH funding and the inclusion of Hyde Amendment language that prohibits the use of federal funds for abortions except in the case of rape, incest, or to save the life of the mother. The bill as it stands is not expected to be picked up in the Senate, which is expected to craft its own legislation.
“I am concerned that the very goal of this legislation set out to achieve, to encourage biomedical innovation and the development of new treatment and cures is undermined somewhat by the reduction in funding for NIH from $10 billion to $8.75 billion,” House Energy and Commerce Committee Ranking Member Frank Pallone, D-N.J., said during the floor debate on July 9.
Despite the concerns over the changes to the bill, support for the bill was overwhelmingly voiced throughout the debate.
“It is time now that we as a nation got serious about curing the major diseases – not treating the diseases, but curing the major diseases – that are affecting this country and affecting us personally,” said House Republican Doctors’ Caucus Chairman Phil Roe, R-Tenn. “I am more passionate about this bill and excited about passing the 21st Century Cures bill than anything I have voted on since I have been in the Congress.”
The House has overwhemingly passed the 21st Century Cures Act, H.R. 6, a broad piece of legislation aimed at streamlining the approval process for medical drugs and devices.
The bill, passed by a 344-77 vote on July 10, also aims to spur innovation in biomedical research and to boost funding to the National Institutes of Health.
Changes made prior to the bill’s introduction to the House floor raised the ire of some legislators and included a reduction in NIH funding and the inclusion of Hyde Amendment language that prohibits the use of federal funds for abortions except in the case of rape, incest, or to save the life of the mother. The bill as it stands is not expected to be picked up in the Senate, which is expected to craft its own legislation.
“I am concerned that the very goal of this legislation set out to achieve, to encourage biomedical innovation and the development of new treatment and cures is undermined somewhat by the reduction in funding for NIH from $10 billion to $8.75 billion,” House Energy and Commerce Committee Ranking Member Frank Pallone, D-N.J., said during the floor debate on July 9.
Despite the concerns over the changes to the bill, support for the bill was overwhelmingly voiced throughout the debate.
“It is time now that we as a nation got serious about curing the major diseases – not treating the diseases, but curing the major diseases – that are affecting this country and affecting us personally,” said House Republican Doctors’ Caucus Chairman Phil Roe, R-Tenn. “I am more passionate about this bill and excited about passing the 21st Century Cures bill than anything I have voted on since I have been in the Congress.”
The House has overwhemingly passed the 21st Century Cures Act, H.R. 6, a broad piece of legislation aimed at streamlining the approval process for medical drugs and devices.
The bill, passed by a 344-77 vote on July 10, also aims to spur innovation in biomedical research and to boost funding to the National Institutes of Health.
Changes made prior to the bill’s introduction to the House floor raised the ire of some legislators and included a reduction in NIH funding and the inclusion of Hyde Amendment language that prohibits the use of federal funds for abortions except in the case of rape, incest, or to save the life of the mother. The bill as it stands is not expected to be picked up in the Senate, which is expected to craft its own legislation.
“I am concerned that the very goal of this legislation set out to achieve, to encourage biomedical innovation and the development of new treatment and cures is undermined somewhat by the reduction in funding for NIH from $10 billion to $8.75 billion,” House Energy and Commerce Committee Ranking Member Frank Pallone, D-N.J., said during the floor debate on July 9.
Despite the concerns over the changes to the bill, support for the bill was overwhelmingly voiced throughout the debate.
“It is time now that we as a nation got serious about curing the major diseases – not treating the diseases, but curing the major diseases – that are affecting this country and affecting us personally,” said House Republican Doctors’ Caucus Chairman Phil Roe, R-Tenn. “I am more passionate about this bill and excited about passing the 21st Century Cures bill than anything I have voted on since I have been in the Congress.”
Hospitals vary widely in low-risk delivery costs
The cost of a low-risk childbirth varies widely across the country, but research is lacking to fully understand why, according to new report in Health Affairs.
Overall, the average hospital facility cost for a maternity stay with a low-risk delivery ranged from $1,189 to $11,986 across 463 hospitals, with a mean of $4,485. There was more than a twofold difference between the 10th and 90th percentiles, Xiao Xu, Ph. D., from Yale University, New Haven, Conn., and her colleagues reported.
“Contrary to the common belief that spending more leads to improved outcomes or at least maintains quality of care, we found a significant positive association between estimated hospital facility cost and serious maternal morbidity rate for low-risk childbirths,” the researchs wrote.
The variation remained regardless of the method of delivery, though the range was wider for cesarean delivery. The average cost of vaginal childbirths ranged from $1,183 to $11,819, and costs associated with a cesarean delivery ranged from $1,249 to $13,688 (Health Aff. 2015; 34: 1212-19 [doi:10.1377/hltaff.2014.1088]).
The findings are based on an analysis of discharge data from the 2011 Nationwide Inpatient Sample, which includes data on nonfederal short-term hospitals in 46 states. The researchers focused on low-risk childbirths and excluded deliveries with identified maternal comorbidities, such as preeclampsia, hypertensive disorders, diabetes, and obesity. They also excluded birth with obstetric risk factors, such as multiple gestation or previous cesarean delivery. The final sample included 463 hospitals and 267,120 births. After weighting the sample, the researchers estimated that the sample represented 1.3 million births nationwide.
Researchers found that hospital characteristics accounted for only 13% of the variation in average costs. For example, research showed that costs were significantly higher at rural hospitals (all were nonteaching facilities) than at urban nonteaching hospitals, but costs between urban teaching and urban nonteaching hospitals were comparable. Additionally, compared with investor-owned private hospitals, nonfederal government hospitals and nonprofit private hospitals had significantly higher facility costs.
After other hospital factors were adjusted for, the researchers found that a 1% increase in the serious maternal morbidity rate was associated with a $296 increase in the average facility cost for a maternity stay across low-risk births.
The rate of cesarean deliveries in the study hospitals ranged from 2% to 39% for low-risk births. In one model, researchers estimated that average facility costs for maternity stays were about $432 higher in hospitals with high cesarean delivery rates than in those with low rates. But after the researchers adjusted for mean length of stay, the association was no longer significant.
The researchers recommended establishing standard definitions and management guidelines for common indications for cesarean delivery, such as labor dystocia and abnormal fetal heart rate tracing to help bring down cesarean rates. “The safe reduction of cesarean deliveries may help reduce facility costs and cost variation for childbirth-related hospitalizations,” Dr. Xu and her colleagues wrote.
The wide variation in maternity stay facility costs presents an opportunity for overall cost containment, the researchers wrote, noting that if hospitals above the 75th percentile could reduce costs to the 75th percentile, it would have generated savings of $290 million in 2011 for costs associated with low-risk childbirths.
The study was supported by an award from the Blue Cross Blue Shield of Michigan Foundation. Dr. Harlan Krumholz, one of the study authors, is chair of the Cardiac Scientific Advisory Board for UnitedHealthcare and has contracts with Medtronic Inc. and Johnson and Johnson.
The cost of a low-risk childbirth varies widely across the country, but research is lacking to fully understand why, according to new report in Health Affairs.
Overall, the average hospital facility cost for a maternity stay with a low-risk delivery ranged from $1,189 to $11,986 across 463 hospitals, with a mean of $4,485. There was more than a twofold difference between the 10th and 90th percentiles, Xiao Xu, Ph. D., from Yale University, New Haven, Conn., and her colleagues reported.
“Contrary to the common belief that spending more leads to improved outcomes or at least maintains quality of care, we found a significant positive association between estimated hospital facility cost and serious maternal morbidity rate for low-risk childbirths,” the researchs wrote.
The variation remained regardless of the method of delivery, though the range was wider for cesarean delivery. The average cost of vaginal childbirths ranged from $1,183 to $11,819, and costs associated with a cesarean delivery ranged from $1,249 to $13,688 (Health Aff. 2015; 34: 1212-19 [doi:10.1377/hltaff.2014.1088]).
The findings are based on an analysis of discharge data from the 2011 Nationwide Inpatient Sample, which includes data on nonfederal short-term hospitals in 46 states. The researchers focused on low-risk childbirths and excluded deliveries with identified maternal comorbidities, such as preeclampsia, hypertensive disorders, diabetes, and obesity. They also excluded birth with obstetric risk factors, such as multiple gestation or previous cesarean delivery. The final sample included 463 hospitals and 267,120 births. After weighting the sample, the researchers estimated that the sample represented 1.3 million births nationwide.
Researchers found that hospital characteristics accounted for only 13% of the variation in average costs. For example, research showed that costs were significantly higher at rural hospitals (all were nonteaching facilities) than at urban nonteaching hospitals, but costs between urban teaching and urban nonteaching hospitals were comparable. Additionally, compared with investor-owned private hospitals, nonfederal government hospitals and nonprofit private hospitals had significantly higher facility costs.
After other hospital factors were adjusted for, the researchers found that a 1% increase in the serious maternal morbidity rate was associated with a $296 increase in the average facility cost for a maternity stay across low-risk births.
The rate of cesarean deliveries in the study hospitals ranged from 2% to 39% for low-risk births. In one model, researchers estimated that average facility costs for maternity stays were about $432 higher in hospitals with high cesarean delivery rates than in those with low rates. But after the researchers adjusted for mean length of stay, the association was no longer significant.
The researchers recommended establishing standard definitions and management guidelines for common indications for cesarean delivery, such as labor dystocia and abnormal fetal heart rate tracing to help bring down cesarean rates. “The safe reduction of cesarean deliveries may help reduce facility costs and cost variation for childbirth-related hospitalizations,” Dr. Xu and her colleagues wrote.
The wide variation in maternity stay facility costs presents an opportunity for overall cost containment, the researchers wrote, noting that if hospitals above the 75th percentile could reduce costs to the 75th percentile, it would have generated savings of $290 million in 2011 for costs associated with low-risk childbirths.
The study was supported by an award from the Blue Cross Blue Shield of Michigan Foundation. Dr. Harlan Krumholz, one of the study authors, is chair of the Cardiac Scientific Advisory Board for UnitedHealthcare and has contracts with Medtronic Inc. and Johnson and Johnson.
The cost of a low-risk childbirth varies widely across the country, but research is lacking to fully understand why, according to new report in Health Affairs.
Overall, the average hospital facility cost for a maternity stay with a low-risk delivery ranged from $1,189 to $11,986 across 463 hospitals, with a mean of $4,485. There was more than a twofold difference between the 10th and 90th percentiles, Xiao Xu, Ph. D., from Yale University, New Haven, Conn., and her colleagues reported.
“Contrary to the common belief that spending more leads to improved outcomes or at least maintains quality of care, we found a significant positive association between estimated hospital facility cost and serious maternal morbidity rate for low-risk childbirths,” the researchs wrote.
The variation remained regardless of the method of delivery, though the range was wider for cesarean delivery. The average cost of vaginal childbirths ranged from $1,183 to $11,819, and costs associated with a cesarean delivery ranged from $1,249 to $13,688 (Health Aff. 2015; 34: 1212-19 [doi:10.1377/hltaff.2014.1088]).
The findings are based on an analysis of discharge data from the 2011 Nationwide Inpatient Sample, which includes data on nonfederal short-term hospitals in 46 states. The researchers focused on low-risk childbirths and excluded deliveries with identified maternal comorbidities, such as preeclampsia, hypertensive disorders, diabetes, and obesity. They also excluded birth with obstetric risk factors, such as multiple gestation or previous cesarean delivery. The final sample included 463 hospitals and 267,120 births. After weighting the sample, the researchers estimated that the sample represented 1.3 million births nationwide.
Researchers found that hospital characteristics accounted for only 13% of the variation in average costs. For example, research showed that costs were significantly higher at rural hospitals (all were nonteaching facilities) than at urban nonteaching hospitals, but costs between urban teaching and urban nonteaching hospitals were comparable. Additionally, compared with investor-owned private hospitals, nonfederal government hospitals and nonprofit private hospitals had significantly higher facility costs.
After other hospital factors were adjusted for, the researchers found that a 1% increase in the serious maternal morbidity rate was associated with a $296 increase in the average facility cost for a maternity stay across low-risk births.
The rate of cesarean deliveries in the study hospitals ranged from 2% to 39% for low-risk births. In one model, researchers estimated that average facility costs for maternity stays were about $432 higher in hospitals with high cesarean delivery rates than in those with low rates. But after the researchers adjusted for mean length of stay, the association was no longer significant.
The researchers recommended establishing standard definitions and management guidelines for common indications for cesarean delivery, such as labor dystocia and abnormal fetal heart rate tracing to help bring down cesarean rates. “The safe reduction of cesarean deliveries may help reduce facility costs and cost variation for childbirth-related hospitalizations,” Dr. Xu and her colleagues wrote.
The wide variation in maternity stay facility costs presents an opportunity for overall cost containment, the researchers wrote, noting that if hospitals above the 75th percentile could reduce costs to the 75th percentile, it would have generated savings of $290 million in 2011 for costs associated with low-risk childbirths.
The study was supported by an award from the Blue Cross Blue Shield of Michigan Foundation. Dr. Harlan Krumholz, one of the study authors, is chair of the Cardiac Scientific Advisory Board for UnitedHealthcare and has contracts with Medtronic Inc. and Johnson and Johnson.
FROM HEALTH AFFAIRS
Key clinical point: The cost of maternity hospital stays varies widely at U.S. hospitals even among low-risk deliveries.
Major finding: The overall average hospital facility cost for a low-risk delivery ranged from $1,189 to $11,986, with a mean cost of $4,485.
Data source: An analysis of discharge data from the 2011 Nationwide Inpatient Sample, including 463 hospitals and 267,120 births.
Disclosures: The study was supported by an award from the Blue Cross Blue Shield of Michigan Foundation. Dr. Harlan Krumholz, one of the study authors, is chair of the Cardiac Scientific Advisory Board for UnitedHealthcare and has contracts with Medtronic Inc. and Johnson & Johnson.
Contraceptive costs drop 20% under ACA
Women have seen a 20% decrease in their out-of-pocket expenses for oral contraceptives and intrauterine devices since the implementation of the Affordable Care Act’s mandate to cover contraceptives without consumer cost sharing, according to a new analysis published in Health Affairs.
The average adjusted per claim out-of-pocket expense for oral contraceptive pills fell from $33.58 in June 2012 to $19.84 in June 2013, after the mandate took effect for most private health plans. For the insertion of an IUD, the average, per claim, out-of-pocket cost fell from $293.28 to $145.24 during the same time period, the researchers reported.
The researchers estimated that the average pill user saved about $255 a year, while the average savings on IUD insertions was about $248 per woman.
The findings are based on an analysis of pharmacy and medical claims data from nearly 791,000 women aged 13-45 who were enrolled in private insurance for at least 1 month between January 2008 and June 2013 (Health Aff. 2015;34:1204-11 [doi:10.1377/hltaff.2015.0127]).
The ACA requires most private health plans to cover all methods of contraception approved by the Food and Drug Administration with no cost sharing as part of the preventive services mandate, although in practice, other studies have found some access issues remain despite the mandate. Many plans began implementing the contraceptive coverage mandate in January 2013, though in 2013 about a third of insured workers were still in a grandfathered plans that are not subject to the ACA’s requirements.
Within 10 months of implementation of the ACA’s contraception mandate, median spending for almost all contraceptive methods fell to zero and the average spending dropped by 38%-93%, depending on the method, according to the researchers. The reason that average spending remained above zero is that not all brands are required to be covered with no cost sharing, and some women in the study were enrolled in grandfathered plans.
“Our findings suggest the ACA mandate will likely significantly reduce the out-of-pocket expenditures of contraceptive users, in some cases to nothing,” Nora Becker and Daniel Polsky, Ph. D., both of the Wharton School at the University of Pennsylvania in Philadelphia, wrote. “But it is still too early to predict the final impact of the mandate on health care use and spending, or the mandate’s impact on other health and socioeconomic outcomes for women.”
Since many women are unaware of the ACA’s contraception coverage mandate, the impact of the mandate will “depend on how sensitive consumers are to out-of-pocket expenses for contraceptives and how many women were dissuaded from using contraceptive products by that expense before the mandate’s implementation,” they wrote.
The researchers reported having no financial disclosures.
Women have seen a 20% decrease in their out-of-pocket expenses for oral contraceptives and intrauterine devices since the implementation of the Affordable Care Act’s mandate to cover contraceptives without consumer cost sharing, according to a new analysis published in Health Affairs.
The average adjusted per claim out-of-pocket expense for oral contraceptive pills fell from $33.58 in June 2012 to $19.84 in June 2013, after the mandate took effect for most private health plans. For the insertion of an IUD, the average, per claim, out-of-pocket cost fell from $293.28 to $145.24 during the same time period, the researchers reported.
The researchers estimated that the average pill user saved about $255 a year, while the average savings on IUD insertions was about $248 per woman.
The findings are based on an analysis of pharmacy and medical claims data from nearly 791,000 women aged 13-45 who were enrolled in private insurance for at least 1 month between January 2008 and June 2013 (Health Aff. 2015;34:1204-11 [doi:10.1377/hltaff.2015.0127]).
The ACA requires most private health plans to cover all methods of contraception approved by the Food and Drug Administration with no cost sharing as part of the preventive services mandate, although in practice, other studies have found some access issues remain despite the mandate. Many plans began implementing the contraceptive coverage mandate in January 2013, though in 2013 about a third of insured workers were still in a grandfathered plans that are not subject to the ACA’s requirements.
Within 10 months of implementation of the ACA’s contraception mandate, median spending for almost all contraceptive methods fell to zero and the average spending dropped by 38%-93%, depending on the method, according to the researchers. The reason that average spending remained above zero is that not all brands are required to be covered with no cost sharing, and some women in the study were enrolled in grandfathered plans.
“Our findings suggest the ACA mandate will likely significantly reduce the out-of-pocket expenditures of contraceptive users, in some cases to nothing,” Nora Becker and Daniel Polsky, Ph. D., both of the Wharton School at the University of Pennsylvania in Philadelphia, wrote. “But it is still too early to predict the final impact of the mandate on health care use and spending, or the mandate’s impact on other health and socioeconomic outcomes for women.”
Since many women are unaware of the ACA’s contraception coverage mandate, the impact of the mandate will “depend on how sensitive consumers are to out-of-pocket expenses for contraceptives and how many women were dissuaded from using contraceptive products by that expense before the mandate’s implementation,” they wrote.
The researchers reported having no financial disclosures.
Women have seen a 20% decrease in their out-of-pocket expenses for oral contraceptives and intrauterine devices since the implementation of the Affordable Care Act’s mandate to cover contraceptives without consumer cost sharing, according to a new analysis published in Health Affairs.
The average adjusted per claim out-of-pocket expense for oral contraceptive pills fell from $33.58 in June 2012 to $19.84 in June 2013, after the mandate took effect for most private health plans. For the insertion of an IUD, the average, per claim, out-of-pocket cost fell from $293.28 to $145.24 during the same time period, the researchers reported.
The researchers estimated that the average pill user saved about $255 a year, while the average savings on IUD insertions was about $248 per woman.
The findings are based on an analysis of pharmacy and medical claims data from nearly 791,000 women aged 13-45 who were enrolled in private insurance for at least 1 month between January 2008 and June 2013 (Health Aff. 2015;34:1204-11 [doi:10.1377/hltaff.2015.0127]).
The ACA requires most private health plans to cover all methods of contraception approved by the Food and Drug Administration with no cost sharing as part of the preventive services mandate, although in practice, other studies have found some access issues remain despite the mandate. Many plans began implementing the contraceptive coverage mandate in January 2013, though in 2013 about a third of insured workers were still in a grandfathered plans that are not subject to the ACA’s requirements.
Within 10 months of implementation of the ACA’s contraception mandate, median spending for almost all contraceptive methods fell to zero and the average spending dropped by 38%-93%, depending on the method, according to the researchers. The reason that average spending remained above zero is that not all brands are required to be covered with no cost sharing, and some women in the study were enrolled in grandfathered plans.
“Our findings suggest the ACA mandate will likely significantly reduce the out-of-pocket expenditures of contraceptive users, in some cases to nothing,” Nora Becker and Daniel Polsky, Ph. D., both of the Wharton School at the University of Pennsylvania in Philadelphia, wrote. “But it is still too early to predict the final impact of the mandate on health care use and spending, or the mandate’s impact on other health and socioeconomic outcomes for women.”
Since many women are unaware of the ACA’s contraception coverage mandate, the impact of the mandate will “depend on how sensitive consumers are to out-of-pocket expenses for contraceptives and how many women were dissuaded from using contraceptive products by that expense before the mandate’s implementation,” they wrote.
The researchers reported having no financial disclosures.
FROM HEALTH AFFAIRS
Key clinical point: The Affordable Care Act has significantly reduced out-of-pockets costs for contraceptives.
Major finding: Under the ACA, the average, per claim, out-of-pocket cost for oral contraceptives dropped from $33.58 to $19.84, while the average intrauterine device cost fell from $293.28 to $145.24 per claim.
Data source: A claims analysis of 791,000 women aged 13-45 conducted between January 2008 and June 2013.
Disclosures: The researchers reported having no financial disclosures.
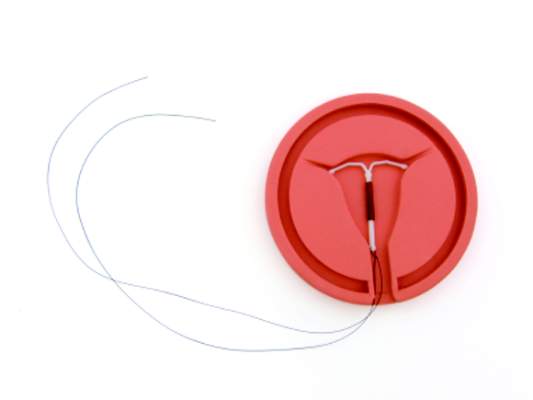
Gaining immediate postpartum IUD coverage one state at a time
As more physicians and women consider immediate postpartum insertion of an intrauterine device as a way to prevent rapid repeat pregnancy, the next step is getting the procedure covered by Medicaid.
Already, 12 state Medicaid agencies offer coverage for this procedure immediately postpartum, with California being the latest to join Alabama, Colorado, Georgia, Iowa, Louisiana, Maryland, Montana, New Mexico, New York, Oklahoma, and South Carolina.
The Association of State and Territorial Health Officials (ASTHO) has been working with state Medicaid agencies and physicians to expand that roster. So far, states have been receptive to the idea, said Dr. Lisa F. Waddell, ASTHO’s chief program officer for community health and prevention, adding that as more states make the necessary policy change to cover the device and insertion procedure, it becomes easier for other states to follow suit.
“Medicaid was a partner at the table and continues to be,” she said. “I really believe they’re wanting to get better outcomes for their dollars they are investing and therefore are opening up to listening to partners and the providers in the state.”
The key challenge is defining the economics of this policy change. Normally, birth services are paid under a flat fee, which does not include coverage of immediate postpartum IUD insertion.
“Any time you make any type of change where there is going to be a cost incurred, people want to know that there will be a return on investment,” Dr. Waddell said.
They are making the case from an outcomes perspective, arguing that the Medicaid program will save money by preventing unplanned rapid repeat pregnancies. And by paying physicians to insert immediate postpartum IUDs, it promotes planned pregnancies in the future, which in turn promotes healthy babies and mothers, another way to help rein in overall costs and improve overall outcomes, she said.
The other challenge is training physicians on the policies and codes in their state, as well the actual IUD insertion protocols.
“There is a lot of emphasis on provider training,” Dr. Waddell said.
Education has been a key emphasis in New Mexico, said Dr. Eve Espey, chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque, who noted that her university hospital is the only location in the state that “very routinely” does this procedure.
“What I’d like to do is through our perinatal collaborative is take the show on the road and talk to other hospitals about how to deal with the reimbursement mechanism and then train providers to be able to offer it to women with Medicaid,” Dr. Espey said. “Then I think an important next step is to talk to private insurers. We have a lot of work to do and I think starting with Medicaid does make a lot of sense.”
ASTHO is also focusing on gaining coverage in the Medicaid setting first. If they can help get the majority of state Medicaid agencies to cover the procedure, it will be easier to convince private insurers to follow suit, as coverage is also not common in the private sector, Dr. Waddell said.
In New Mexico, the state Medicaid program had covered IUD devices and insertion but didn’t pay for immediate postpartum insertion. But with “substantial” no-show rates for follow-up postpartum appointments to insert the devices, it became important to gain that coverage so that patients could have the procedure when they were the most motivated, Dr. Espey said.
In Georgia, the experience has been similar. Dr. Melissa Kottke, director of the Jane Fonda Center for Adolescent Reproductive Health at Emory University in Atlanta said there was a lot of hospital-level coordination needed once the state-approved coverage.
“The changes that have to get instituted are really at a particular institution or organizational level,” Dr. Kottke said. “There are a lot of stakeholders that need to be involved,” from clinicians to coding staff to electronic health record vendors and other key personnel.
“There is a lot of education and a lot of cooperation that is necessary, but it’s certainly something that’s definitely doable,” she said.
Dr. Kottke said there have not been any issues with the adequacy of payment for this procedure and the state Medicaid agency has been “really supportive of this approach,” particularly since there had already been a number of states that had instituted coverage and have seen improved outcomes, both clinical and financial.
“It’s a huge opportunity for taking really good care of women,” Dr. Kottke said. “We know that the immediate postpartum period is a time of unmet contraceptive need and to remove the financial barrier is really exciting to see.”
As more physicians and women consider immediate postpartum insertion of an intrauterine device as a way to prevent rapid repeat pregnancy, the next step is getting the procedure covered by Medicaid.
Already, 12 state Medicaid agencies offer coverage for this procedure immediately postpartum, with California being the latest to join Alabama, Colorado, Georgia, Iowa, Louisiana, Maryland, Montana, New Mexico, New York, Oklahoma, and South Carolina.
The Association of State and Territorial Health Officials (ASTHO) has been working with state Medicaid agencies and physicians to expand that roster. So far, states have been receptive to the idea, said Dr. Lisa F. Waddell, ASTHO’s chief program officer for community health and prevention, adding that as more states make the necessary policy change to cover the device and insertion procedure, it becomes easier for other states to follow suit.
“Medicaid was a partner at the table and continues to be,” she said. “I really believe they’re wanting to get better outcomes for their dollars they are investing and therefore are opening up to listening to partners and the providers in the state.”
The key challenge is defining the economics of this policy change. Normally, birth services are paid under a flat fee, which does not include coverage of immediate postpartum IUD insertion.
“Any time you make any type of change where there is going to be a cost incurred, people want to know that there will be a return on investment,” Dr. Waddell said.
They are making the case from an outcomes perspective, arguing that the Medicaid program will save money by preventing unplanned rapid repeat pregnancies. And by paying physicians to insert immediate postpartum IUDs, it promotes planned pregnancies in the future, which in turn promotes healthy babies and mothers, another way to help rein in overall costs and improve overall outcomes, she said.
The other challenge is training physicians on the policies and codes in their state, as well the actual IUD insertion protocols.
“There is a lot of emphasis on provider training,” Dr. Waddell said.
Education has been a key emphasis in New Mexico, said Dr. Eve Espey, chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque, who noted that her university hospital is the only location in the state that “very routinely” does this procedure.
“What I’d like to do is through our perinatal collaborative is take the show on the road and talk to other hospitals about how to deal with the reimbursement mechanism and then train providers to be able to offer it to women with Medicaid,” Dr. Espey said. “Then I think an important next step is to talk to private insurers. We have a lot of work to do and I think starting with Medicaid does make a lot of sense.”
ASTHO is also focusing on gaining coverage in the Medicaid setting first. If they can help get the majority of state Medicaid agencies to cover the procedure, it will be easier to convince private insurers to follow suit, as coverage is also not common in the private sector, Dr. Waddell said.
In New Mexico, the state Medicaid program had covered IUD devices and insertion but didn’t pay for immediate postpartum insertion. But with “substantial” no-show rates for follow-up postpartum appointments to insert the devices, it became important to gain that coverage so that patients could have the procedure when they were the most motivated, Dr. Espey said.
In Georgia, the experience has been similar. Dr. Melissa Kottke, director of the Jane Fonda Center for Adolescent Reproductive Health at Emory University in Atlanta said there was a lot of hospital-level coordination needed once the state-approved coverage.
“The changes that have to get instituted are really at a particular institution or organizational level,” Dr. Kottke said. “There are a lot of stakeholders that need to be involved,” from clinicians to coding staff to electronic health record vendors and other key personnel.
“There is a lot of education and a lot of cooperation that is necessary, but it’s certainly something that’s definitely doable,” she said.
Dr. Kottke said there have not been any issues with the adequacy of payment for this procedure and the state Medicaid agency has been “really supportive of this approach,” particularly since there had already been a number of states that had instituted coverage and have seen improved outcomes, both clinical and financial.
“It’s a huge opportunity for taking really good care of women,” Dr. Kottke said. “We know that the immediate postpartum period is a time of unmet contraceptive need and to remove the financial barrier is really exciting to see.”
As more physicians and women consider immediate postpartum insertion of an intrauterine device as a way to prevent rapid repeat pregnancy, the next step is getting the procedure covered by Medicaid.
Already, 12 state Medicaid agencies offer coverage for this procedure immediately postpartum, with California being the latest to join Alabama, Colorado, Georgia, Iowa, Louisiana, Maryland, Montana, New Mexico, New York, Oklahoma, and South Carolina.
The Association of State and Territorial Health Officials (ASTHO) has been working with state Medicaid agencies and physicians to expand that roster. So far, states have been receptive to the idea, said Dr. Lisa F. Waddell, ASTHO’s chief program officer for community health and prevention, adding that as more states make the necessary policy change to cover the device and insertion procedure, it becomes easier for other states to follow suit.
“Medicaid was a partner at the table and continues to be,” she said. “I really believe they’re wanting to get better outcomes for their dollars they are investing and therefore are opening up to listening to partners and the providers in the state.”
The key challenge is defining the economics of this policy change. Normally, birth services are paid under a flat fee, which does not include coverage of immediate postpartum IUD insertion.
“Any time you make any type of change where there is going to be a cost incurred, people want to know that there will be a return on investment,” Dr. Waddell said.
They are making the case from an outcomes perspective, arguing that the Medicaid program will save money by preventing unplanned rapid repeat pregnancies. And by paying physicians to insert immediate postpartum IUDs, it promotes planned pregnancies in the future, which in turn promotes healthy babies and mothers, another way to help rein in overall costs and improve overall outcomes, she said.
The other challenge is training physicians on the policies and codes in their state, as well the actual IUD insertion protocols.
“There is a lot of emphasis on provider training,” Dr. Waddell said.
Education has been a key emphasis in New Mexico, said Dr. Eve Espey, chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque, who noted that her university hospital is the only location in the state that “very routinely” does this procedure.
“What I’d like to do is through our perinatal collaborative is take the show on the road and talk to other hospitals about how to deal with the reimbursement mechanism and then train providers to be able to offer it to women with Medicaid,” Dr. Espey said. “Then I think an important next step is to talk to private insurers. We have a lot of work to do and I think starting with Medicaid does make a lot of sense.”
ASTHO is also focusing on gaining coverage in the Medicaid setting first. If they can help get the majority of state Medicaid agencies to cover the procedure, it will be easier to convince private insurers to follow suit, as coverage is also not common in the private sector, Dr. Waddell said.
In New Mexico, the state Medicaid program had covered IUD devices and insertion but didn’t pay for immediate postpartum insertion. But with “substantial” no-show rates for follow-up postpartum appointments to insert the devices, it became important to gain that coverage so that patients could have the procedure when they were the most motivated, Dr. Espey said.
In Georgia, the experience has been similar. Dr. Melissa Kottke, director of the Jane Fonda Center for Adolescent Reproductive Health at Emory University in Atlanta said there was a lot of hospital-level coordination needed once the state-approved coverage.
“The changes that have to get instituted are really at a particular institution or organizational level,” Dr. Kottke said. “There are a lot of stakeholders that need to be involved,” from clinicians to coding staff to electronic health record vendors and other key personnel.
“There is a lot of education and a lot of cooperation that is necessary, but it’s certainly something that’s definitely doable,” she said.
Dr. Kottke said there have not been any issues with the adequacy of payment for this procedure and the state Medicaid agency has been “really supportive of this approach,” particularly since there had already been a number of states that had instituted coverage and have seen improved outcomes, both clinical and financial.
“It’s a huge opportunity for taking really good care of women,” Dr. Kottke said. “We know that the immediate postpartum period is a time of unmet contraceptive need and to remove the financial barrier is really exciting to see.”
CMS pledges flexibility during first year of ICD-10
Physicians will have a year to learn how to properly code under ICD-10 before facing potential penalties or withheld payments, according to a joint announcement from the Centers for Medicare & Medicaid Services and the American Medical Association.
During that first year using the new coding system, Medicare will not deny claims based solely on the specificity of diagnosis codes, provided they are in the appropriate family of ICD-10 codes. However, physicians still will not be able to use ICD-9 codes after Sept. 30, 2015.
“This means that Medicare will not deny payment for these unintentional errors as practices become accustomed to ICD-10 coding,” Dr. Steven Stack, AMA president, wrote in a blog post on the AMA website. “This transition period will give physicians and their practice teams time to get up to speed on the more complicated code set.”
Similarly, physicians will not face penalties under the Physician Quality Reporting System, the value-based modifier, or the meaningful use program based on the specificity of diagnosis codes if the appropriate family of ICD-10 codes are used, according to the AMA. Finally, if a Medicare contractor is unable to process a claim due to coding issues, CMS will authorize an advance payment to the physician.
CMS also plans to create an ICD-10 coordination center and appoint an ombudsman to answer questions about claims submission using ICD-10.
“With easy-to-use tools, a new ICD-10 ombudsman, and added flexibility in our claims audit and quality reporting process, CMS is committed to working with the physician community to work through this transition.” Andy Slavitt, CMS Acting Administrator, said in a statement.
Physicians will have a year to learn how to properly code under ICD-10 before facing potential penalties or withheld payments, according to a joint announcement from the Centers for Medicare & Medicaid Services and the American Medical Association.
During that first year using the new coding system, Medicare will not deny claims based solely on the specificity of diagnosis codes, provided they are in the appropriate family of ICD-10 codes. However, physicians still will not be able to use ICD-9 codes after Sept. 30, 2015.
“This means that Medicare will not deny payment for these unintentional errors as practices become accustomed to ICD-10 coding,” Dr. Steven Stack, AMA president, wrote in a blog post on the AMA website. “This transition period will give physicians and their practice teams time to get up to speed on the more complicated code set.”
Similarly, physicians will not face penalties under the Physician Quality Reporting System, the value-based modifier, or the meaningful use program based on the specificity of diagnosis codes if the appropriate family of ICD-10 codes are used, according to the AMA. Finally, if a Medicare contractor is unable to process a claim due to coding issues, CMS will authorize an advance payment to the physician.
CMS also plans to create an ICD-10 coordination center and appoint an ombudsman to answer questions about claims submission using ICD-10.
“With easy-to-use tools, a new ICD-10 ombudsman, and added flexibility in our claims audit and quality reporting process, CMS is committed to working with the physician community to work through this transition.” Andy Slavitt, CMS Acting Administrator, said in a statement.
Physicians will have a year to learn how to properly code under ICD-10 before facing potential penalties or withheld payments, according to a joint announcement from the Centers for Medicare & Medicaid Services and the American Medical Association.
During that first year using the new coding system, Medicare will not deny claims based solely on the specificity of diagnosis codes, provided they are in the appropriate family of ICD-10 codes. However, physicians still will not be able to use ICD-9 codes after Sept. 30, 2015.
“This means that Medicare will not deny payment for these unintentional errors as practices become accustomed to ICD-10 coding,” Dr. Steven Stack, AMA president, wrote in a blog post on the AMA website. “This transition period will give physicians and their practice teams time to get up to speed on the more complicated code set.”
Similarly, physicians will not face penalties under the Physician Quality Reporting System, the value-based modifier, or the meaningful use program based on the specificity of diagnosis codes if the appropriate family of ICD-10 codes are used, according to the AMA. Finally, if a Medicare contractor is unable to process a claim due to coding issues, CMS will authorize an advance payment to the physician.
CMS also plans to create an ICD-10 coordination center and appoint an ombudsman to answer questions about claims submission using ICD-10.
“With easy-to-use tools, a new ICD-10 ombudsman, and added flexibility in our claims audit and quality reporting process, CMS is committed to working with the physician community to work through this transition.” Andy Slavitt, CMS Acting Administrator, said in a statement.
Survey: Most Health Care Organizations Had a Recent Security Breach
More than two-thirds of health care organizations responding to a survey have experienced a significant and recent security event, according to the Health Information and Management Systems Society (HIMSS).
The single largest source of significant security incidents were negligent insiders, defined as well-meaning individuals who unwittingly caused a breach. However, 64% of respondents reported that their organization had been the victim of an attack from an external actor – usually an online scam artist. The results are part of the 2015 HIMSS Cybersecurity Survey, which polled 297 health care leaders and information security officers.
Most of the security incidents resulted in limited disruption of IT systems with limited impact on clinical care, according to the report. The majority of respondents said security incidents were detected within 24 hours of occurrence, “approximately 20% of these security incidents ultimately resulted in loss of patient, financial, or operational data.”
While security breaches may seem like an IT issue, Jennifer Horowitz, senior director of research at HIMSS, said physicians need to be aware of what they can do to help keep their systems secure.
“This is a rapidly changing environment and I think that physicians also need ... to do their part: adhering to the security policies and protocols as their organization,” Ms. Horowitz said in an interivew, highlighting particularly that physicians need to be aware of potential phishing scams sent via email that could comprompise data security.
More than two-thirds of health care organizations responding to a survey have experienced a significant and recent security event, according to the Health Information and Management Systems Society (HIMSS).
The single largest source of significant security incidents were negligent insiders, defined as well-meaning individuals who unwittingly caused a breach. However, 64% of respondents reported that their organization had been the victim of an attack from an external actor – usually an online scam artist. The results are part of the 2015 HIMSS Cybersecurity Survey, which polled 297 health care leaders and information security officers.
Most of the security incidents resulted in limited disruption of IT systems with limited impact on clinical care, according to the report. The majority of respondents said security incidents were detected within 24 hours of occurrence, “approximately 20% of these security incidents ultimately resulted in loss of patient, financial, or operational data.”
While security breaches may seem like an IT issue, Jennifer Horowitz, senior director of research at HIMSS, said physicians need to be aware of what they can do to help keep their systems secure.
“This is a rapidly changing environment and I think that physicians also need ... to do their part: adhering to the security policies and protocols as their organization,” Ms. Horowitz said in an interivew, highlighting particularly that physicians need to be aware of potential phishing scams sent via email that could comprompise data security.
More than two-thirds of health care organizations responding to a survey have experienced a significant and recent security event, according to the Health Information and Management Systems Society (HIMSS).
The single largest source of significant security incidents were negligent insiders, defined as well-meaning individuals who unwittingly caused a breach. However, 64% of respondents reported that their organization had been the victim of an attack from an external actor – usually an online scam artist. The results are part of the 2015 HIMSS Cybersecurity Survey, which polled 297 health care leaders and information security officers.
Most of the security incidents resulted in limited disruption of IT systems with limited impact on clinical care, according to the report. The majority of respondents said security incidents were detected within 24 hours of occurrence, “approximately 20% of these security incidents ultimately resulted in loss of patient, financial, or operational data.”
While security breaches may seem like an IT issue, Jennifer Horowitz, senior director of research at HIMSS, said physicians need to be aware of what they can do to help keep their systems secure.
“This is a rapidly changing environment and I think that physicians also need ... to do their part: adhering to the security policies and protocols as their organization,” Ms. Horowitz said in an interivew, highlighting particularly that physicians need to be aware of potential phishing scams sent via email that could comprompise data security.
Survey: Most health care organizations had a recent security breach
More than two-thirds of health care organizations responding to a survey have experienced a significant and recent security event, according to the Health Information and Management Systems Society (HIMSS).
The single largest source of significant security incidents were negligent insiders, defined as well-meaning individuals who unwittingly caused a breach. However, 64% of respondents reported that their organization had been the victim of an attack from an external actor – usually an online scam artist. The results are part of the 2015 HIMSS Cybersecurity Survey, which polled 297 health care leaders and information security officers.
Most of the security incidents resulted in limited disruption of IT systems with limited impact on clinical care, according to the report. The majority of respondents said security incidents were detected within 24 hours of occurrence, “approximately 20% of these security incidents ultimately resulted in loss of patient, financial, or operational data.”
While security breaches may seem like an IT issue, Jennifer Horowitz, senior director of research at HIMSS, said physicians need to be aware of what they can do to help keep their systems secure.
“This is a rapidly changing environment and I think that physicians also need ... to do their part: adhering to the security policies and protocols as their organization,” Ms. Horowitz said in an interivew, highlighting particularly that physicians need to be aware of potential phishing scams sent via email that could comprompise data security.
More than two-thirds of health care organizations responding to a survey have experienced a significant and recent security event, according to the Health Information and Management Systems Society (HIMSS).
The single largest source of significant security incidents were negligent insiders, defined as well-meaning individuals who unwittingly caused a breach. However, 64% of respondents reported that their organization had been the victim of an attack from an external actor – usually an online scam artist. The results are part of the 2015 HIMSS Cybersecurity Survey, which polled 297 health care leaders and information security officers.
Most of the security incidents resulted in limited disruption of IT systems with limited impact on clinical care, according to the report. The majority of respondents said security incidents were detected within 24 hours of occurrence, “approximately 20% of these security incidents ultimately resulted in loss of patient, financial, or operational data.”
While security breaches may seem like an IT issue, Jennifer Horowitz, senior director of research at HIMSS, said physicians need to be aware of what they can do to help keep their systems secure.
“This is a rapidly changing environment and I think that physicians also need ... to do their part: adhering to the security policies and protocols as their organization,” Ms. Horowitz said in an interivew, highlighting particularly that physicians need to be aware of potential phishing scams sent via email that could comprompise data security.
More than two-thirds of health care organizations responding to a survey have experienced a significant and recent security event, according to the Health Information and Management Systems Society (HIMSS).
The single largest source of significant security incidents were negligent insiders, defined as well-meaning individuals who unwittingly caused a breach. However, 64% of respondents reported that their organization had been the victim of an attack from an external actor – usually an online scam artist. The results are part of the 2015 HIMSS Cybersecurity Survey, which polled 297 health care leaders and information security officers.
Most of the security incidents resulted in limited disruption of IT systems with limited impact on clinical care, according to the report. The majority of respondents said security incidents were detected within 24 hours of occurrence, “approximately 20% of these security incidents ultimately resulted in loss of patient, financial, or operational data.”
While security breaches may seem like an IT issue, Jennifer Horowitz, senior director of research at HIMSS, said physicians need to be aware of what they can do to help keep their systems secure.
“This is a rapidly changing environment and I think that physicians also need ... to do their part: adhering to the security policies and protocols as their organization,” Ms. Horowitz said in an interivew, highlighting particularly that physicians need to be aware of potential phishing scams sent via email that could comprompise data security.