User login
Employer health insurance: Deductibles rising faster than wages
Health insurance deductibles have risen much faster than average wages over the last 10 years, according to the latest Employer Health Benefit Survey released by the Kaiser Family Foundation.
“The share of workers in plans with a general annual deductible has gone from 59% to 85%, and I think even more notably, the average deductible has more than doubled from $735 to $1,573 and deductibles have risen more markedly in smaller firms,” Drew Altman, president and CEO of the KFF said during an Oct. 3 press conference.
“These two trends combine for an effective 212% increase in worker deductibles over the past decade, and that is 8 times the increase in workers’ wages during the same period, which for me is the most important number,” he said.
Employer health care costs generally have remained stable, according to the annual survey, now in its 20th year. Annual family premiums for employer-sponsored health insurance rose 5% to an average $19,616 in 2018, extending a 7-year run of moderate increases. The average premium paid by the employee is $5,547.
For a single individual, the average premium increased 3% to $6,896, with employees contributing an average of $1,186.
Although the year-over-year comparison has a premiums increase comparable to that of wages (2.6%) and inflation ($2.5%), over time, premiums are rising much faster.
KFF noted that 85% of employees have a deductible in their plan, up from 81% last year and 59% a decade ago. About 152 million Americans are covered by an employer-sponsored plan.
“Health care costs absolutely remain a burden for employers, but they are a bigger problem for workers as their cost sharing has been rising much faster than their wages have been rising in recent years,” Mr. Altman said.
The survey found that 70% of large employers offer some kind of complete health risk assessments and 38% offer incentives for workers to participate in these programs, with the value of incentives reaching $500 or more.
SOURCE: Kaiser Family Foundation, 2018 Employer Health Benefits.
Health insurance deductibles have risen much faster than average wages over the last 10 years, according to the latest Employer Health Benefit Survey released by the Kaiser Family Foundation.
“The share of workers in plans with a general annual deductible has gone from 59% to 85%, and I think even more notably, the average deductible has more than doubled from $735 to $1,573 and deductibles have risen more markedly in smaller firms,” Drew Altman, president and CEO of the KFF said during an Oct. 3 press conference.
“These two trends combine for an effective 212% increase in worker deductibles over the past decade, and that is 8 times the increase in workers’ wages during the same period, which for me is the most important number,” he said.
Employer health care costs generally have remained stable, according to the annual survey, now in its 20th year. Annual family premiums for employer-sponsored health insurance rose 5% to an average $19,616 in 2018, extending a 7-year run of moderate increases. The average premium paid by the employee is $5,547.
For a single individual, the average premium increased 3% to $6,896, with employees contributing an average of $1,186.
Although the year-over-year comparison has a premiums increase comparable to that of wages (2.6%) and inflation ($2.5%), over time, premiums are rising much faster.
KFF noted that 85% of employees have a deductible in their plan, up from 81% last year and 59% a decade ago. About 152 million Americans are covered by an employer-sponsored plan.
“Health care costs absolutely remain a burden for employers, but they are a bigger problem for workers as their cost sharing has been rising much faster than their wages have been rising in recent years,” Mr. Altman said.
The survey found that 70% of large employers offer some kind of complete health risk assessments and 38% offer incentives for workers to participate in these programs, with the value of incentives reaching $500 or more.
SOURCE: Kaiser Family Foundation, 2018 Employer Health Benefits.
Health insurance deductibles have risen much faster than average wages over the last 10 years, according to the latest Employer Health Benefit Survey released by the Kaiser Family Foundation.
“The share of workers in plans with a general annual deductible has gone from 59% to 85%, and I think even more notably, the average deductible has more than doubled from $735 to $1,573 and deductibles have risen more markedly in smaller firms,” Drew Altman, president and CEO of the KFF said during an Oct. 3 press conference.
“These two trends combine for an effective 212% increase in worker deductibles over the past decade, and that is 8 times the increase in workers’ wages during the same period, which for me is the most important number,” he said.
Employer health care costs generally have remained stable, according to the annual survey, now in its 20th year. Annual family premiums for employer-sponsored health insurance rose 5% to an average $19,616 in 2018, extending a 7-year run of moderate increases. The average premium paid by the employee is $5,547.
For a single individual, the average premium increased 3% to $6,896, with employees contributing an average of $1,186.
Although the year-over-year comparison has a premiums increase comparable to that of wages (2.6%) and inflation ($2.5%), over time, premiums are rising much faster.
KFF noted that 85% of employees have a deductible in their plan, up from 81% last year and 59% a decade ago. About 152 million Americans are covered by an employer-sponsored plan.
“Health care costs absolutely remain a burden for employers, but they are a bigger problem for workers as their cost sharing has been rising much faster than their wages have been rising in recent years,” Mr. Altman said.
The survey found that 70% of large employers offer some kind of complete health risk assessments and 38% offer incentives for workers to participate in these programs, with the value of incentives reaching $500 or more.
SOURCE: Kaiser Family Foundation, 2018 Employer Health Benefits.
Key clinical point: The average employee deductible rose from $735 to $1,573 in the last decade.
Major finding: Deductibles have risen 8 times faster than wages since 2008.
Study details: Kaiser Family Foundation surveyed 4,070 randomly selected nonfederal public and private firms with three or more employees; 2,160 responded to the full survey and 1,910 responded to a single question about offering coverage.
Disclosures: No financial conflicts of interest reported.
Source: Kaiser Family Foundation, 2018 Employer Health Benefits.
ACOG lends support to bill promoting maternal mortality review committees
The Preventing Maternal Deaths Act of 2018 (H.R. 1318) was the subject of a Sept. 27 hearing of the House Energy and Commerce Health Subcommittee. The bill comes at a time when 700 women a year die as a result of pregnancy or pregnancy-related complications with a rate that is increasing, while 157 of 183 countries around the world are reporting decreasing rates of maternal mortality, according to ACOG.
The bill, authored by Rep. Jamie Herrera Beutler (R-Wash.) and Diana DeGette (D-Colo.) would allocate $58 million for each fiscal year from 2019 through 2023 to support the 33 existing states with maternal mortality review committees (MMRCs) and help the remaining 17 states develop them, as well as to standardize data collection across the nation.
The goal of having these committees in place is to “improve data collection and reporting around maternal mortality, and to develop or support surveillance systems at the local, state, and national level in order to better understand the burden of maternal complications,” a background memo on the hearing noted. “These surveillance efforts include identifying groups of women with disproportionately high rates of maternal mortality and identifying the determinants of disparities in maternal care, health risks, and health outcomes.”
Necessitating this legislation was a data point that was reiterated throughout the course of the hearing – that maternal mortality rates in the United States were on the rise.
“What’s both surprising and devastating is that, despite massive innovation and advances in health care and technology, we’ve experienced recent reports that have indicated that the number of women dying due to pregnancy complications is actually increasing,” Full Committee Chairman Greg Walden (R-Ore.) said in his opening remarks at the hearing. “According to the Centers for Disease Control and Prevention, maternal mortality rates in America have more than doubled since 1987. I think we are asking, how can that be? This is not a statistic any of us wants to hear.”
Chairman Walden acknowledged that there are questions as to whether the increase was a function of better data collection or whether it was an issue with the delivery of health care.
“The bill before us today will help us answer these really important questions and hopefully ensure that expectant newborn mothers receive even better care,” he said.
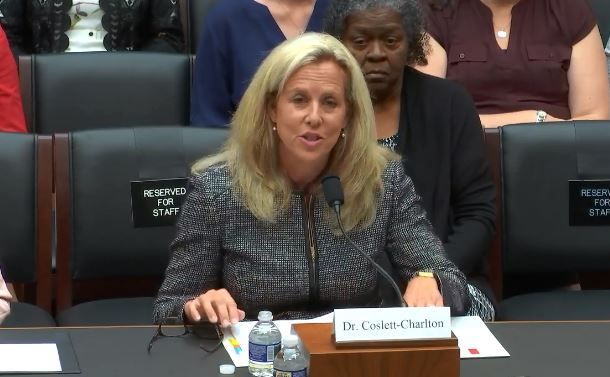
Lynne M. Coslett-Charlton, MD, ACOG Pennsylvania District legislative chair, offered the organization’s support for the bill.
MMRCs “are multidisciplinary groups of local experts in maternal and public health, as well as patient and community advocates, that closely examine maternal death cases and identify locally relevant ways to prevent future deaths,” she testified before the committee. “While traditional public health surveillance using vital statistics can tell us about trends and disparities, MMRCs are best positioned to comprehensively assess maternal deaths and identify opportunities for prevention.”
Dr. Coslett-Charlton added that to clearly understand why women are dying from preventable maternal complications, which she noted that 60% of maternal deaths are, “every state must have a robust MMRC. The Preventing Maternal Deaths Act will help us reach that goal, and ultimately improve maternal health across this nation,” as these committees review every maternal death and can make a determination as to whether they could have been preventable.
Additionally, the fact that black women face a significantly higher rate of maternal mortality was another data point highlighted during the hearing, further adding to the need for this bill that has bipartisan support and more than 170 cosponsors.
Rep. DeGette called it “one of the most striking aspects” that black women “are nearly four times as likely to experience a pregnancy-related death.”
Stacey D. Stewart, president of the March of Dimes, in her written testimony praised the inclusion in H.R. 1318 of a “demonstration project to determine how best to address disparities in maternal health outcomes.”
The Preventing Maternal Deaths Act of 2018 (H.R. 1318) was the subject of a Sept. 27 hearing of the House Energy and Commerce Health Subcommittee. The bill comes at a time when 700 women a year die as a result of pregnancy or pregnancy-related complications with a rate that is increasing, while 157 of 183 countries around the world are reporting decreasing rates of maternal mortality, according to ACOG.
The bill, authored by Rep. Jamie Herrera Beutler (R-Wash.) and Diana DeGette (D-Colo.) would allocate $58 million for each fiscal year from 2019 through 2023 to support the 33 existing states with maternal mortality review committees (MMRCs) and help the remaining 17 states develop them, as well as to standardize data collection across the nation.
The goal of having these committees in place is to “improve data collection and reporting around maternal mortality, and to develop or support surveillance systems at the local, state, and national level in order to better understand the burden of maternal complications,” a background memo on the hearing noted. “These surveillance efforts include identifying groups of women with disproportionately high rates of maternal mortality and identifying the determinants of disparities in maternal care, health risks, and health outcomes.”
Necessitating this legislation was a data point that was reiterated throughout the course of the hearing – that maternal mortality rates in the United States were on the rise.
“What’s both surprising and devastating is that, despite massive innovation and advances in health care and technology, we’ve experienced recent reports that have indicated that the number of women dying due to pregnancy complications is actually increasing,” Full Committee Chairman Greg Walden (R-Ore.) said in his opening remarks at the hearing. “According to the Centers for Disease Control and Prevention, maternal mortality rates in America have more than doubled since 1987. I think we are asking, how can that be? This is not a statistic any of us wants to hear.”
Chairman Walden acknowledged that there are questions as to whether the increase was a function of better data collection or whether it was an issue with the delivery of health care.
“The bill before us today will help us answer these really important questions and hopefully ensure that expectant newborn mothers receive even better care,” he said.
Lynne M. Coslett-Charlton, MD, ACOG Pennsylvania District legislative chair, offered the organization’s support for the bill.
MMRCs “are multidisciplinary groups of local experts in maternal and public health, as well as patient and community advocates, that closely examine maternal death cases and identify locally relevant ways to prevent future deaths,” she testified before the committee. “While traditional public health surveillance using vital statistics can tell us about trends and disparities, MMRCs are best positioned to comprehensively assess maternal deaths and identify opportunities for prevention.”
Dr. Coslett-Charlton added that to clearly understand why women are dying from preventable maternal complications, which she noted that 60% of maternal deaths are, “every state must have a robust MMRC. The Preventing Maternal Deaths Act will help us reach that goal, and ultimately improve maternal health across this nation,” as these committees review every maternal death and can make a determination as to whether they could have been preventable.
Additionally, the fact that black women face a significantly higher rate of maternal mortality was another data point highlighted during the hearing, further adding to the need for this bill that has bipartisan support and more than 170 cosponsors.
Rep. DeGette called it “one of the most striking aspects” that black women “are nearly four times as likely to experience a pregnancy-related death.”
Stacey D. Stewart, president of the March of Dimes, in her written testimony praised the inclusion in H.R. 1318 of a “demonstration project to determine how best to address disparities in maternal health outcomes.”
The Preventing Maternal Deaths Act of 2018 (H.R. 1318) was the subject of a Sept. 27 hearing of the House Energy and Commerce Health Subcommittee. The bill comes at a time when 700 women a year die as a result of pregnancy or pregnancy-related complications with a rate that is increasing, while 157 of 183 countries around the world are reporting decreasing rates of maternal mortality, according to ACOG.
The bill, authored by Rep. Jamie Herrera Beutler (R-Wash.) and Diana DeGette (D-Colo.) would allocate $58 million for each fiscal year from 2019 through 2023 to support the 33 existing states with maternal mortality review committees (MMRCs) and help the remaining 17 states develop them, as well as to standardize data collection across the nation.
The goal of having these committees in place is to “improve data collection and reporting around maternal mortality, and to develop or support surveillance systems at the local, state, and national level in order to better understand the burden of maternal complications,” a background memo on the hearing noted. “These surveillance efforts include identifying groups of women with disproportionately high rates of maternal mortality and identifying the determinants of disparities in maternal care, health risks, and health outcomes.”
Necessitating this legislation was a data point that was reiterated throughout the course of the hearing – that maternal mortality rates in the United States were on the rise.
“What’s both surprising and devastating is that, despite massive innovation and advances in health care and technology, we’ve experienced recent reports that have indicated that the number of women dying due to pregnancy complications is actually increasing,” Full Committee Chairman Greg Walden (R-Ore.) said in his opening remarks at the hearing. “According to the Centers for Disease Control and Prevention, maternal mortality rates in America have more than doubled since 1987. I think we are asking, how can that be? This is not a statistic any of us wants to hear.”
Chairman Walden acknowledged that there are questions as to whether the increase was a function of better data collection or whether it was an issue with the delivery of health care.
“The bill before us today will help us answer these really important questions and hopefully ensure that expectant newborn mothers receive even better care,” he said.
Lynne M. Coslett-Charlton, MD, ACOG Pennsylvania District legislative chair, offered the organization’s support for the bill.
MMRCs “are multidisciplinary groups of local experts in maternal and public health, as well as patient and community advocates, that closely examine maternal death cases and identify locally relevant ways to prevent future deaths,” she testified before the committee. “While traditional public health surveillance using vital statistics can tell us about trends and disparities, MMRCs are best positioned to comprehensively assess maternal deaths and identify opportunities for prevention.”
Dr. Coslett-Charlton added that to clearly understand why women are dying from preventable maternal complications, which she noted that 60% of maternal deaths are, “every state must have a robust MMRC. The Preventing Maternal Deaths Act will help us reach that goal, and ultimately improve maternal health across this nation,” as these committees review every maternal death and can make a determination as to whether they could have been preventable.
Additionally, the fact that black women face a significantly higher rate of maternal mortality was another data point highlighted during the hearing, further adding to the need for this bill that has bipartisan support and more than 170 cosponsors.
Rep. DeGette called it “one of the most striking aspects” that black women “are nearly four times as likely to experience a pregnancy-related death.”
Stacey D. Stewart, president of the March of Dimes, in her written testimony praised the inclusion in H.R. 1318 of a “demonstration project to determine how best to address disparities in maternal health outcomes.”
REPORTING FROM A HOUSE ENERGY AND COMMERCE HEALTH SUBCOMMITTEE HEARING
Red flag raised on CMS indication-based formulary policy
Physician groups are expressing concerns regarding a new policy that will allow indication-based formulary design in the Medicare Part D prescription drug benefit.
The Centers for Medicare & Medicaid Services announced the new policy in an Aug. 29 memo to Part D plan sponsors.
According to a fact sheet issued by CMS on the same day, indication-based formulary design “is a formulary management tool that allows health plans to tailor on-formulary coverage of drugs predicated on specific indications.”
Current Part D policy requires plan sponsors to cover all Food and Drug Administration–approved indications for each drug that is on a plan formulary. Sponsors can begin to implement the new indication-based formulary design policy for plans issued in 2020.
The memo notes that, if a Part D plan sponsor chooses to opt into this policy, “it must ensure that there is another therapeutically similar drug on formulary for the nonformulary indication. For example, if a tumor necrosis factor (TNF) blocker is FDA-approved for both Crohn’s disease and plaque psoriasis, but the Part D plan will include it on formulary for plaque psoriasis only, the plan must ensure that there is another TNF blocker on formulary that will be covered for Crohn’s disease.”
Beneficiaries can use the exceptions process to get coverage for a drug that has an indication not on the formulary.
“By allowing Medicare’s prescription drug plans to cover the best drug for each patient condition, plans will have more negotiating power with drug companies, which will result in lower prices for Medicare beneficiaries,” CMS Administrator Seema Verma said in a statement.
However, physician groups should be concerned about the definition of “best drug.” Is this definition based upon efficacy, results of clinical trials, clinical effectiveness research, or just cost? Will there be transparenecy surrounding rebates?
The “proposed changes will exacerbate many of the access issues patients currently face with plan usage of existing utilization management practices, such as step therapy,” the American College of Rheumatology said in a statement. “Unlike step therapy, which often delays effective treatments, this proposal would go even further and allow plans to remove therapies from the formulary altogether, leaving patients completely unable to access treatments that doctors and patients choose together. ... We also have concerns on what this would mean for work being done on compendia inclusion to secure off-label drug coverage if plans don’t have to cover all FDA-approved indications.”
A similar situation exists in patients with inflammatory bowel disease in which step therapy has largely been replaced by risk assessments. The AGA Crohn’s and UC Care Pathways are based on this principle.
Under the plan, Medicare patients will face increased challenges as they navigate health plans to make sure that their needed drug is on their selected formulary, which can change based on what health conditions they have,” AMA President Barbara McAneny, MD, said in a statement. Dr. McAneny added that it will be even more difficult for physicians who are working with patients to get them on the best medicines covered by the patient’s formulary.
“Physicians already lack ready access to accurate formulary information – preferred/tier status, on/off formulary, PA [prior authorization] and step therapy requirements – at the point of care in their EHRs,” she said. “These transparency problems will expand by an order of magnitude by the complications this change introduces.”
Physician groups are expressing concerns regarding a new policy that will allow indication-based formulary design in the Medicare Part D prescription drug benefit.
The Centers for Medicare & Medicaid Services announced the new policy in an Aug. 29 memo to Part D plan sponsors.
According to a fact sheet issued by CMS on the same day, indication-based formulary design “is a formulary management tool that allows health plans to tailor on-formulary coverage of drugs predicated on specific indications.”
Current Part D policy requires plan sponsors to cover all Food and Drug Administration–approved indications for each drug that is on a plan formulary. Sponsors can begin to implement the new indication-based formulary design policy for plans issued in 2020.
The memo notes that, if a Part D plan sponsor chooses to opt into this policy, “it must ensure that there is another therapeutically similar drug on formulary for the nonformulary indication. For example, if a tumor necrosis factor (TNF) blocker is FDA-approved for both Crohn’s disease and plaque psoriasis, but the Part D plan will include it on formulary for plaque psoriasis only, the plan must ensure that there is another TNF blocker on formulary that will be covered for Crohn’s disease.”
Beneficiaries can use the exceptions process to get coverage for a drug that has an indication not on the formulary.
“By allowing Medicare’s prescription drug plans to cover the best drug for each patient condition, plans will have more negotiating power with drug companies, which will result in lower prices for Medicare beneficiaries,” CMS Administrator Seema Verma said in a statement.
However, physician groups should be concerned about the definition of “best drug.” Is this definition based upon efficacy, results of clinical trials, clinical effectiveness research, or just cost? Will there be transparenecy surrounding rebates?
The “proposed changes will exacerbate many of the access issues patients currently face with plan usage of existing utilization management practices, such as step therapy,” the American College of Rheumatology said in a statement. “Unlike step therapy, which often delays effective treatments, this proposal would go even further and allow plans to remove therapies from the formulary altogether, leaving patients completely unable to access treatments that doctors and patients choose together. ... We also have concerns on what this would mean for work being done on compendia inclusion to secure off-label drug coverage if plans don’t have to cover all FDA-approved indications.”
A similar situation exists in patients with inflammatory bowel disease in which step therapy has largely been replaced by risk assessments. The AGA Crohn’s and UC Care Pathways are based on this principle.
Under the plan, Medicare patients will face increased challenges as they navigate health plans to make sure that their needed drug is on their selected formulary, which can change based on what health conditions they have,” AMA President Barbara McAneny, MD, said in a statement. Dr. McAneny added that it will be even more difficult for physicians who are working with patients to get them on the best medicines covered by the patient’s formulary.
“Physicians already lack ready access to accurate formulary information – preferred/tier status, on/off formulary, PA [prior authorization] and step therapy requirements – at the point of care in their EHRs,” she said. “These transparency problems will expand by an order of magnitude by the complications this change introduces.”
Physician groups are expressing concerns regarding a new policy that will allow indication-based formulary design in the Medicare Part D prescription drug benefit.
The Centers for Medicare & Medicaid Services announced the new policy in an Aug. 29 memo to Part D plan sponsors.
According to a fact sheet issued by CMS on the same day, indication-based formulary design “is a formulary management tool that allows health plans to tailor on-formulary coverage of drugs predicated on specific indications.”
Current Part D policy requires plan sponsors to cover all Food and Drug Administration–approved indications for each drug that is on a plan formulary. Sponsors can begin to implement the new indication-based formulary design policy for plans issued in 2020.
The memo notes that, if a Part D plan sponsor chooses to opt into this policy, “it must ensure that there is another therapeutically similar drug on formulary for the nonformulary indication. For example, if a tumor necrosis factor (TNF) blocker is FDA-approved for both Crohn’s disease and plaque psoriasis, but the Part D plan will include it on formulary for plaque psoriasis only, the plan must ensure that there is another TNF blocker on formulary that will be covered for Crohn’s disease.”
Beneficiaries can use the exceptions process to get coverage for a drug that has an indication not on the formulary.
“By allowing Medicare’s prescription drug plans to cover the best drug for each patient condition, plans will have more negotiating power with drug companies, which will result in lower prices for Medicare beneficiaries,” CMS Administrator Seema Verma said in a statement.
However, physician groups should be concerned about the definition of “best drug.” Is this definition based upon efficacy, results of clinical trials, clinical effectiveness research, or just cost? Will there be transparenecy surrounding rebates?
The “proposed changes will exacerbate many of the access issues patients currently face with plan usage of existing utilization management practices, such as step therapy,” the American College of Rheumatology said in a statement. “Unlike step therapy, which often delays effective treatments, this proposal would go even further and allow plans to remove therapies from the formulary altogether, leaving patients completely unable to access treatments that doctors and patients choose together. ... We also have concerns on what this would mean for work being done on compendia inclusion to secure off-label drug coverage if plans don’t have to cover all FDA-approved indications.”
A similar situation exists in patients with inflammatory bowel disease in which step therapy has largely been replaced by risk assessments. The AGA Crohn’s and UC Care Pathways are based on this principle.
Under the plan, Medicare patients will face increased challenges as they navigate health plans to make sure that their needed drug is on their selected formulary, which can change based on what health conditions they have,” AMA President Barbara McAneny, MD, said in a statement. Dr. McAneny added that it will be even more difficult for physicians who are working with patients to get them on the best medicines covered by the patient’s formulary.
“Physicians already lack ready access to accurate formulary information – preferred/tier status, on/off formulary, PA [prior authorization] and step therapy requirements – at the point of care in their EHRs,” she said. “These transparency problems will expand by an order of magnitude by the complications this change introduces.”
House, Senate agree on broad opioid legislation
Leaders in the House and the Senate have agreed to a final legislative package to address the opioid crisis.
The consensus legislation, called the Substance Use–Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (H.R. 6), combines a House bill of the same name passed in June with the Opioid Crisis Response Act (S. 2680), passed by the Senate by a 99-1 vote on Sept. 17.
A number of provisions would affect medical practice directly, by:
- Allowing Medicare to pay clinicians to provide substance-use disorder treatment via telemedicine.
- Adding to the Welcome to Medicare exam as well as the annual physical a review of beneficiary’s opioid prescriptions, screening for potential abuse, and referral to appropriate treatment services, if necessary.
- Requiring controlled substance prescriptions covered by Part D to be transmitted electronically beginning Jan. 1, 2021.
- Allowing physicians who recently graduated in good standing from an accredited school and who have appropriate training to prescribe medication-assisted therapy.
- Requiring CMS to notify prescribers if they are identified as statistical outliers when it comes to prescribing opioids, as compared with their peers.
“The bill will make a real difference in Medicare, a program in which one in three beneficiaries is prescribed an opioid,” Senate Finance Committee Chairman Orrin Hatch (R-Utah) said Sept .17 during Senate floor debate.
“It will empower patients through information on pain treatment alternatives. It will expand treatment options for patients suffering from addiction, including through increased access to care via telehealth,” he said. “The bill also increases the ability to track opioid prescriptions to prevent misuse and diversion, while also ensuring that beneficiaries promptly get the medications they need.”
The bill also requires the Food and Drug Administration to issue guidance on expedited pathways for approval of new nonaddictive pain treatments and on the appropriate use of pain endpoints across agency divisions as well as clarification on requirements on how opioid-sparing data is to be used on labels.
The combined legislation also clarifies the FDA’s authority to require drug manufacturers to package opioids in three- and seven-supply blister packs, as well as requiring manufacturers to provide patients with simple and safe options to dispose of unused opioids.
The combined bill addresses one of the criticisms of the Senate-passed version.
Sen. Edward Markey (D-Mass.) noted the absence of a provision that would have given nurse practitioners and physician assistants permanent prescribing authority for medication-assisted therapies.
“This is a missed opportunity to build upon our commitment to treatment,” he said on the Senate floor.
The final version of H.R. 6 that will be voted on by both chambers includes the House-passed provision.
At press time, votes on the combined bill had not been scheduled.
Sen. Margaret Wood Hassan (D-N.H.) warned the Congress not to get complacent.
“This legislation is a vital next step in our efforts to combat this crisis,” she said. “The biggest mistake anyone could make is thinking that our efforts are anywhere close to being done.”
A section-by-section summary of the bill can be found here.
Leaders in the House and the Senate have agreed to a final legislative package to address the opioid crisis.
The consensus legislation, called the Substance Use–Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (H.R. 6), combines a House bill of the same name passed in June with the Opioid Crisis Response Act (S. 2680), passed by the Senate by a 99-1 vote on Sept. 17.
A number of provisions would affect medical practice directly, by:
- Allowing Medicare to pay clinicians to provide substance-use disorder treatment via telemedicine.
- Adding to the Welcome to Medicare exam as well as the annual physical a review of beneficiary’s opioid prescriptions, screening for potential abuse, and referral to appropriate treatment services, if necessary.
- Requiring controlled substance prescriptions covered by Part D to be transmitted electronically beginning Jan. 1, 2021.
- Allowing physicians who recently graduated in good standing from an accredited school and who have appropriate training to prescribe medication-assisted therapy.
- Requiring CMS to notify prescribers if they are identified as statistical outliers when it comes to prescribing opioids, as compared with their peers.
“The bill will make a real difference in Medicare, a program in which one in three beneficiaries is prescribed an opioid,” Senate Finance Committee Chairman Orrin Hatch (R-Utah) said Sept .17 during Senate floor debate.
“It will empower patients through information on pain treatment alternatives. It will expand treatment options for patients suffering from addiction, including through increased access to care via telehealth,” he said. “The bill also increases the ability to track opioid prescriptions to prevent misuse and diversion, while also ensuring that beneficiaries promptly get the medications they need.”
The bill also requires the Food and Drug Administration to issue guidance on expedited pathways for approval of new nonaddictive pain treatments and on the appropriate use of pain endpoints across agency divisions as well as clarification on requirements on how opioid-sparing data is to be used on labels.
The combined legislation also clarifies the FDA’s authority to require drug manufacturers to package opioids in three- and seven-supply blister packs, as well as requiring manufacturers to provide patients with simple and safe options to dispose of unused opioids.
The combined bill addresses one of the criticisms of the Senate-passed version.
Sen. Edward Markey (D-Mass.) noted the absence of a provision that would have given nurse practitioners and physician assistants permanent prescribing authority for medication-assisted therapies.
“This is a missed opportunity to build upon our commitment to treatment,” he said on the Senate floor.
The final version of H.R. 6 that will be voted on by both chambers includes the House-passed provision.
At press time, votes on the combined bill had not been scheduled.
Sen. Margaret Wood Hassan (D-N.H.) warned the Congress not to get complacent.
“This legislation is a vital next step in our efforts to combat this crisis,” she said. “The biggest mistake anyone could make is thinking that our efforts are anywhere close to being done.”
A section-by-section summary of the bill can be found here.
Leaders in the House and the Senate have agreed to a final legislative package to address the opioid crisis.
The consensus legislation, called the Substance Use–Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (H.R. 6), combines a House bill of the same name passed in June with the Opioid Crisis Response Act (S. 2680), passed by the Senate by a 99-1 vote on Sept. 17.
A number of provisions would affect medical practice directly, by:
- Allowing Medicare to pay clinicians to provide substance-use disorder treatment via telemedicine.
- Adding to the Welcome to Medicare exam as well as the annual physical a review of beneficiary’s opioid prescriptions, screening for potential abuse, and referral to appropriate treatment services, if necessary.
- Requiring controlled substance prescriptions covered by Part D to be transmitted electronically beginning Jan. 1, 2021.
- Allowing physicians who recently graduated in good standing from an accredited school and who have appropriate training to prescribe medication-assisted therapy.
- Requiring CMS to notify prescribers if they are identified as statistical outliers when it comes to prescribing opioids, as compared with their peers.
“The bill will make a real difference in Medicare, a program in which one in three beneficiaries is prescribed an opioid,” Senate Finance Committee Chairman Orrin Hatch (R-Utah) said Sept .17 during Senate floor debate.
“It will empower patients through information on pain treatment alternatives. It will expand treatment options for patients suffering from addiction, including through increased access to care via telehealth,” he said. “The bill also increases the ability to track opioid prescriptions to prevent misuse and diversion, while also ensuring that beneficiaries promptly get the medications they need.”
The bill also requires the Food and Drug Administration to issue guidance on expedited pathways for approval of new nonaddictive pain treatments and on the appropriate use of pain endpoints across agency divisions as well as clarification on requirements on how opioid-sparing data is to be used on labels.
The combined legislation also clarifies the FDA’s authority to require drug manufacturers to package opioids in three- and seven-supply blister packs, as well as requiring manufacturers to provide patients with simple and safe options to dispose of unused opioids.
The combined bill addresses one of the criticisms of the Senate-passed version.
Sen. Edward Markey (D-Mass.) noted the absence of a provision that would have given nurse practitioners and physician assistants permanent prescribing authority for medication-assisted therapies.
“This is a missed opportunity to build upon our commitment to treatment,” he said on the Senate floor.
The final version of H.R. 6 that will be voted on by both chambers includes the House-passed provision.
At press time, votes on the combined bill had not been scheduled.
Sen. Margaret Wood Hassan (D-N.H.) warned the Congress not to get complacent.
“This legislation is a vital next step in our efforts to combat this crisis,” she said. “The biggest mistake anyone could make is thinking that our efforts are anywhere close to being done.”
A section-by-section summary of the bill can be found here.
Proposal to change Part B drug WAC-based reimbursement draws criticism
Some physician groups are pushing back on a proposal to lower the add-on percentage for reimbursement of new Part B drugs paid using the wholesale acquisition cost (WAC) when an average sales price (ASP) has not yet been established.
Under current regulation, physicians are reimbursed at WAC plus 6% for newly approved drugs. The Centers for Medicare & Medicaid Services is looking to reduce the add-on to 3% in the proposed update to the physician fee schedule for 2019.
In Sept. 6 comments to the agency, the American College of Rheumatology took on a neutral stance to the proposal as a whole, stating only that it appreciates “that the proposed rule does clarify that the change in reimbursement would not apply to new biosimilars, whose reimbursement would remain at the drug’s WAC plus 6% of the reference drug’s ASP.”
The American Society of Clinical Oncology took a more hard-line stance.
“CMS should not finalize the proposed reduction in the add-on rate for Part B drugs subject to payment through the wholesale acquisition cost methodology and should instead focus on pursuing comprehensive solutions that drive value-based cancer care,” ASCO said in Sept. 10 comments to the agency. It acknowledged CMS’ pursuit to lower drug spending, but suggested this will not have any meaningful impact “since most drugs are paid through a WAC-based methodology on a temporary basis only.”
The American Medical Association argued in Sept. 10 comments to the agency that, when accounting for the budget sequester that is in effect, physicians would only be getting reimbursed with a 1.4% add-on and that enactment of this proposal “would trigger reimbursement cuts for new drugs that will preclude their use in most physician offices and hinder Medicare patients’ access to new and innovated therapies that are more effective and/or less debilitating than existing drugs. AMA strongly believes that this proposal should not be finalized.”
Some physician groups are pushing back on a proposal to lower the add-on percentage for reimbursement of new Part B drugs paid using the wholesale acquisition cost (WAC) when an average sales price (ASP) has not yet been established.
Under current regulation, physicians are reimbursed at WAC plus 6% for newly approved drugs. The Centers for Medicare & Medicaid Services is looking to reduce the add-on to 3% in the proposed update to the physician fee schedule for 2019.
In Sept. 6 comments to the agency, the American College of Rheumatology took on a neutral stance to the proposal as a whole, stating only that it appreciates “that the proposed rule does clarify that the change in reimbursement would not apply to new biosimilars, whose reimbursement would remain at the drug’s WAC plus 6% of the reference drug’s ASP.”
The American Society of Clinical Oncology took a more hard-line stance.
“CMS should not finalize the proposed reduction in the add-on rate for Part B drugs subject to payment through the wholesale acquisition cost methodology and should instead focus on pursuing comprehensive solutions that drive value-based cancer care,” ASCO said in Sept. 10 comments to the agency. It acknowledged CMS’ pursuit to lower drug spending, but suggested this will not have any meaningful impact “since most drugs are paid through a WAC-based methodology on a temporary basis only.”
The American Medical Association argued in Sept. 10 comments to the agency that, when accounting for the budget sequester that is in effect, physicians would only be getting reimbursed with a 1.4% add-on and that enactment of this proposal “would trigger reimbursement cuts for new drugs that will preclude their use in most physician offices and hinder Medicare patients’ access to new and innovated therapies that are more effective and/or less debilitating than existing drugs. AMA strongly believes that this proposal should not be finalized.”
Some physician groups are pushing back on a proposal to lower the add-on percentage for reimbursement of new Part B drugs paid using the wholesale acquisition cost (WAC) when an average sales price (ASP) has not yet been established.
Under current regulation, physicians are reimbursed at WAC plus 6% for newly approved drugs. The Centers for Medicare & Medicaid Services is looking to reduce the add-on to 3% in the proposed update to the physician fee schedule for 2019.
In Sept. 6 comments to the agency, the American College of Rheumatology took on a neutral stance to the proposal as a whole, stating only that it appreciates “that the proposed rule does clarify that the change in reimbursement would not apply to new biosimilars, whose reimbursement would remain at the drug’s WAC plus 6% of the reference drug’s ASP.”
The American Society of Clinical Oncology took a more hard-line stance.
“CMS should not finalize the proposed reduction in the add-on rate for Part B drugs subject to payment through the wholesale acquisition cost methodology and should instead focus on pursuing comprehensive solutions that drive value-based cancer care,” ASCO said in Sept. 10 comments to the agency. It acknowledged CMS’ pursuit to lower drug spending, but suggested this will not have any meaningful impact “since most drugs are paid through a WAC-based methodology on a temporary basis only.”
The American Medical Association argued in Sept. 10 comments to the agency that, when accounting for the budget sequester that is in effect, physicians would only be getting reimbursed with a 1.4% add-on and that enactment of this proposal “would trigger reimbursement cuts for new drugs that will preclude their use in most physician offices and hinder Medicare patients’ access to new and innovated therapies that are more effective and/or less debilitating than existing drugs. AMA strongly believes that this proposal should not be finalized.”
Is CMS becoming more open to PTAC recommendations?
Recommendations on potential physician-focused alternative payment models so far have gained little traction with officials at the Centers for Medicare & Medicaid Services, but that could be changing.
At a recent meeting of the Physician-Focused Payment Model Technical Advisory Committee (PTAC), Alex Azar, secretary of the Department of Health & Human Services, and Seema Verma, administrator of the Centers for Medicare & Medicaid Services, attended briefly, according to officials at the American College of Emergency Physicians. ACEP was having its proposal evaluated by PTAC.
Physician organizations have been puzzled as to why federal health officials have yet to approve a physician-developed alternative payment model (APM) under the Quality Payment Program, despite several being recommended by PTAC. In fact, no physician-developed APM has even been sent to the Center for Medicare and Medicaid Innovation for further testing and refinement.
ACEP’s model, the Acute Unscheduled Care Model, “provides incentives to safely discharge Medicare beneficiaries from the ED by facilitating and rewarding postdischarge care coordination,” the organizations notes in the model description submitted to PTAC. “The model ensures that emergency physicians who make the decision to provide safe, efficient outpatient care have the necessary tools to support this transformation and are rewarded for their decision making.”
Going into the meeting, the preliminary evaluation report had the PTAC reviewers agreeing unanimously that the model met 7 of the secretary’s 10 criteria for a physician-focused APM, that the majority agreed on the 8th criterion, and a majority agreed that the model did not meet criteria on the remaining two items.
PTAC reviewers “thought that we met all 10 criteria for models that the secretary put forth for evaluating physician-focused payment models,” Jeffrey Davis, ACEP Director of Regulatory Affairs, said in an interview, adding that the attendance of Mr. Azar and Ms. Verma at the meeting was a positive development.
“I think we were especially inspired by the fact that Secretary Azar, Administrator Verma, and Adam Boehler, the new head of [Center for Medicare and Medicaid Innovation], spoke at the beginning of the PTAC meeting,” he said, adding that while no models have been formally implemented or even designated for testing, they said that ideas are being incorporated into model development going on at the CMS.
Ms. Verma went so far as to tweet that “this group of leading experts volunteer their time to improve our healthcare system, and we greatly value their input.”
“We still think [PTAC] is a great avenue to get our model into the public arena,” Mr. Davis said. “We are optimistic.”
Recommendations on potential physician-focused alternative payment models so far have gained little traction with officials at the Centers for Medicare & Medicaid Services, but that could be changing.
At a recent meeting of the Physician-Focused Payment Model Technical Advisory Committee (PTAC), Alex Azar, secretary of the Department of Health & Human Services, and Seema Verma, administrator of the Centers for Medicare & Medicaid Services, attended briefly, according to officials at the American College of Emergency Physicians. ACEP was having its proposal evaluated by PTAC.
Physician organizations have been puzzled as to why federal health officials have yet to approve a physician-developed alternative payment model (APM) under the Quality Payment Program, despite several being recommended by PTAC. In fact, no physician-developed APM has even been sent to the Center for Medicare and Medicaid Innovation for further testing and refinement.
ACEP’s model, the Acute Unscheduled Care Model, “provides incentives to safely discharge Medicare beneficiaries from the ED by facilitating and rewarding postdischarge care coordination,” the organizations notes in the model description submitted to PTAC. “The model ensures that emergency physicians who make the decision to provide safe, efficient outpatient care have the necessary tools to support this transformation and are rewarded for their decision making.”
Going into the meeting, the preliminary evaluation report had the PTAC reviewers agreeing unanimously that the model met 7 of the secretary’s 10 criteria for a physician-focused APM, that the majority agreed on the 8th criterion, and a majority agreed that the model did not meet criteria on the remaining two items.
PTAC reviewers “thought that we met all 10 criteria for models that the secretary put forth for evaluating physician-focused payment models,” Jeffrey Davis, ACEP Director of Regulatory Affairs, said in an interview, adding that the attendance of Mr. Azar and Ms. Verma at the meeting was a positive development.
“I think we were especially inspired by the fact that Secretary Azar, Administrator Verma, and Adam Boehler, the new head of [Center for Medicare and Medicaid Innovation], spoke at the beginning of the PTAC meeting,” he said, adding that while no models have been formally implemented or even designated for testing, they said that ideas are being incorporated into model development going on at the CMS.
Ms. Verma went so far as to tweet that “this group of leading experts volunteer their time to improve our healthcare system, and we greatly value their input.”
“We still think [PTAC] is a great avenue to get our model into the public arena,” Mr. Davis said. “We are optimistic.”
Recommendations on potential physician-focused alternative payment models so far have gained little traction with officials at the Centers for Medicare & Medicaid Services, but that could be changing.
At a recent meeting of the Physician-Focused Payment Model Technical Advisory Committee (PTAC), Alex Azar, secretary of the Department of Health & Human Services, and Seema Verma, administrator of the Centers for Medicare & Medicaid Services, attended briefly, according to officials at the American College of Emergency Physicians. ACEP was having its proposal evaluated by PTAC.
Physician organizations have been puzzled as to why federal health officials have yet to approve a physician-developed alternative payment model (APM) under the Quality Payment Program, despite several being recommended by PTAC. In fact, no physician-developed APM has even been sent to the Center for Medicare and Medicaid Innovation for further testing and refinement.
ACEP’s model, the Acute Unscheduled Care Model, “provides incentives to safely discharge Medicare beneficiaries from the ED by facilitating and rewarding postdischarge care coordination,” the organizations notes in the model description submitted to PTAC. “The model ensures that emergency physicians who make the decision to provide safe, efficient outpatient care have the necessary tools to support this transformation and are rewarded for their decision making.”
Going into the meeting, the preliminary evaluation report had the PTAC reviewers agreeing unanimously that the model met 7 of the secretary’s 10 criteria for a physician-focused APM, that the majority agreed on the 8th criterion, and a majority agreed that the model did not meet criteria on the remaining two items.
PTAC reviewers “thought that we met all 10 criteria for models that the secretary put forth for evaluating physician-focused payment models,” Jeffrey Davis, ACEP Director of Regulatory Affairs, said in an interview, adding that the attendance of Mr. Azar and Ms. Verma at the meeting was a positive development.
“I think we were especially inspired by the fact that Secretary Azar, Administrator Verma, and Adam Boehler, the new head of [Center for Medicare and Medicaid Innovation], spoke at the beginning of the PTAC meeting,” he said, adding that while no models have been formally implemented or even designated for testing, they said that ideas are being incorporated into model development going on at the CMS.
Ms. Verma went so far as to tweet that “this group of leading experts volunteer their time to improve our healthcare system, and we greatly value their input.”
“We still think [PTAC] is a great avenue to get our model into the public arena,” Mr. Davis said. “We are optimistic.”
Medicare gets input on revamping Part B drug program
The Centers for Medicare & Medicaid Services has an uphill climb if it is hoping to sell the idea of a revamped competitive acquisition program (CAP) for prescription drugs administered in the office under Medicare Part B.
The CMS has been seeking comments on bringing the program back. Given the responses to the proposal for simply revising the program without specific operational details as presented in the American Patients First blueprint for lowering drug prices and costs, the final program design will need to be something special to attract physicians to participate.
Under the original CAP, participating physicians would order drugs from an approved vendor, who would then bill Medicare and collect copayments from the beneficiary. The original program was in effect for 18 months and ended on Dec. 31, 2008, after it had little participation and faced other concerns.
More recently, the Medicare Payment Advisory Committee (MedPAC) recommended a revised version of the program, which they dubbed the Part B Drug Value Program (DVP). Under this proposal, private vendors would acquire drugs at lower prices using various negotiation tools, and physicians would be encouraged to make more value-based use decisions based on opportunities for shared savings under Part B.
The CMS is asking for feedback in its proposed 2019 update to the outpatient prospective payment system on a wide range of questions on how the revamped CAP program should be designed, including program design, which suppliers and drugs to include, how to encourage participation, how to structure outcomes-based arrangements, and whether indication-based pricing should be used.
Any demonstration project to test the provisions of a revised CAP program “must be voluntary, as we cannot predict the outcome and the impacts on patients and practice,” officials from the American College of Rheumatology insisted in a July 13 comment letter. “Making any programs and demonstrations voluntary, rather than compulsory, is centrally important to protecting patients.”
The ACR noted that it has “concerns regarding recreating a [CAP] for Part B drugs that was previously unworkable,” adding that it would “oppose a CAP program if it were unchanged or similar to the previous program, or if it would not ensure adequate protections for patient access to medicines.”
The ACR expressly opposed any CAP program that would include utilization management techniques such as prior authorization, step therapy, or other formulary limitation methods.
The American Medical Association said in July 16 comments on the blueprint that a “hasty resurrection of the original CAP with a few cosmetic changes is bound to fail. A CAP descendant cannot succeed without a significant redesign, consultation with earlier program participants, and adequate public input. Any successful redesign will need to provide physicians with a true choice of whether to participate or not; ensure that patient access to necessary drugs is not harmed; and avoid the temptation to add burdensome new administrative procedures aimed at enhancing CAP vendors’ negotiating power and cost-constraints.”
The AMA raised a number of questions that would need to be addressed to get the program up and running in the areas of patient protections and operational issues.
The American Academy of Dermatology Association offered support for the current Part B payment scheme of average sales price plus 6%, but said simply on CAP that it “should be restructured to provide greater flexibility and appeal to providers and vendors.”
The Alliance of Specialty Physicians offered a suggestions in its comments, including
- Allowing physicians to remain in the current buy-and-bill system.
- Ensuring a minimum of three vendor choices per physician.
- Allowing physicians to easily switch between vendors and/or back to the current buy-and-bill system.
- Prohibiting CAP vendors from engaging in any utilization management techniques or medical review work.
The American Gastroenterological Association, which also supported to the Alliance of Specialty Physicians suggestions, said in separately filed comments that it is “unclear that the marketplace has changed in ways that would support the success of a new CAP program,” though the AGA “does not oppose” the idea of a new, voluntary CAP program.
The AGA noted that consolidation has improved the negotiation and purchasing power of physicians in the Part B space, while practices that remained independent as small and mid-sized groups “mostly shifted their Part B drug and biologic patients to hospital outpatient–based departments and infusion clinics because of the significant upfront costs of administering Part B drugs and biologics.”
The Centers for Medicare & Medicaid Services has an uphill climb if it is hoping to sell the idea of a revamped competitive acquisition program (CAP) for prescription drugs administered in the office under Medicare Part B.
The CMS has been seeking comments on bringing the program back. Given the responses to the proposal for simply revising the program without specific operational details as presented in the American Patients First blueprint for lowering drug prices and costs, the final program design will need to be something special to attract physicians to participate.
Under the original CAP, participating physicians would order drugs from an approved vendor, who would then bill Medicare and collect copayments from the beneficiary. The original program was in effect for 18 months and ended on Dec. 31, 2008, after it had little participation and faced other concerns.
More recently, the Medicare Payment Advisory Committee (MedPAC) recommended a revised version of the program, which they dubbed the Part B Drug Value Program (DVP). Under this proposal, private vendors would acquire drugs at lower prices using various negotiation tools, and physicians would be encouraged to make more value-based use decisions based on opportunities for shared savings under Part B.
The CMS is asking for feedback in its proposed 2019 update to the outpatient prospective payment system on a wide range of questions on how the revamped CAP program should be designed, including program design, which suppliers and drugs to include, how to encourage participation, how to structure outcomes-based arrangements, and whether indication-based pricing should be used.
Any demonstration project to test the provisions of a revised CAP program “must be voluntary, as we cannot predict the outcome and the impacts on patients and practice,” officials from the American College of Rheumatology insisted in a July 13 comment letter. “Making any programs and demonstrations voluntary, rather than compulsory, is centrally important to protecting patients.”
The ACR noted that it has “concerns regarding recreating a [CAP] for Part B drugs that was previously unworkable,” adding that it would “oppose a CAP program if it were unchanged or similar to the previous program, or if it would not ensure adequate protections for patient access to medicines.”
The ACR expressly opposed any CAP program that would include utilization management techniques such as prior authorization, step therapy, or other formulary limitation methods.
The American Medical Association said in July 16 comments on the blueprint that a “hasty resurrection of the original CAP with a few cosmetic changes is bound to fail. A CAP descendant cannot succeed without a significant redesign, consultation with earlier program participants, and adequate public input. Any successful redesign will need to provide physicians with a true choice of whether to participate or not; ensure that patient access to necessary drugs is not harmed; and avoid the temptation to add burdensome new administrative procedures aimed at enhancing CAP vendors’ negotiating power and cost-constraints.”
The AMA raised a number of questions that would need to be addressed to get the program up and running in the areas of patient protections and operational issues.
The American Academy of Dermatology Association offered support for the current Part B payment scheme of average sales price plus 6%, but said simply on CAP that it “should be restructured to provide greater flexibility and appeal to providers and vendors.”
The Alliance of Specialty Physicians offered a suggestions in its comments, including
- Allowing physicians to remain in the current buy-and-bill system.
- Ensuring a minimum of three vendor choices per physician.
- Allowing physicians to easily switch between vendors and/or back to the current buy-and-bill system.
- Prohibiting CAP vendors from engaging in any utilization management techniques or medical review work.
The American Gastroenterological Association, which also supported to the Alliance of Specialty Physicians suggestions, said in separately filed comments that it is “unclear that the marketplace has changed in ways that would support the success of a new CAP program,” though the AGA “does not oppose” the idea of a new, voluntary CAP program.
The AGA noted that consolidation has improved the negotiation and purchasing power of physicians in the Part B space, while practices that remained independent as small and mid-sized groups “mostly shifted their Part B drug and biologic patients to hospital outpatient–based departments and infusion clinics because of the significant upfront costs of administering Part B drugs and biologics.”
The Centers for Medicare & Medicaid Services has an uphill climb if it is hoping to sell the idea of a revamped competitive acquisition program (CAP) for prescription drugs administered in the office under Medicare Part B.
The CMS has been seeking comments on bringing the program back. Given the responses to the proposal for simply revising the program without specific operational details as presented in the American Patients First blueprint for lowering drug prices and costs, the final program design will need to be something special to attract physicians to participate.
Under the original CAP, participating physicians would order drugs from an approved vendor, who would then bill Medicare and collect copayments from the beneficiary. The original program was in effect for 18 months and ended on Dec. 31, 2008, after it had little participation and faced other concerns.
More recently, the Medicare Payment Advisory Committee (MedPAC) recommended a revised version of the program, which they dubbed the Part B Drug Value Program (DVP). Under this proposal, private vendors would acquire drugs at lower prices using various negotiation tools, and physicians would be encouraged to make more value-based use decisions based on opportunities for shared savings under Part B.
The CMS is asking for feedback in its proposed 2019 update to the outpatient prospective payment system on a wide range of questions on how the revamped CAP program should be designed, including program design, which suppliers and drugs to include, how to encourage participation, how to structure outcomes-based arrangements, and whether indication-based pricing should be used.
Any demonstration project to test the provisions of a revised CAP program “must be voluntary, as we cannot predict the outcome and the impacts on patients and practice,” officials from the American College of Rheumatology insisted in a July 13 comment letter. “Making any programs and demonstrations voluntary, rather than compulsory, is centrally important to protecting patients.”
The ACR noted that it has “concerns regarding recreating a [CAP] for Part B drugs that was previously unworkable,” adding that it would “oppose a CAP program if it were unchanged or similar to the previous program, or if it would not ensure adequate protections for patient access to medicines.”
The ACR expressly opposed any CAP program that would include utilization management techniques such as prior authorization, step therapy, or other formulary limitation methods.
The American Medical Association said in July 16 comments on the blueprint that a “hasty resurrection of the original CAP with a few cosmetic changes is bound to fail. A CAP descendant cannot succeed without a significant redesign, consultation with earlier program participants, and adequate public input. Any successful redesign will need to provide physicians with a true choice of whether to participate or not; ensure that patient access to necessary drugs is not harmed; and avoid the temptation to add burdensome new administrative procedures aimed at enhancing CAP vendors’ negotiating power and cost-constraints.”
The AMA raised a number of questions that would need to be addressed to get the program up and running in the areas of patient protections and operational issues.
The American Academy of Dermatology Association offered support for the current Part B payment scheme of average sales price plus 6%, but said simply on CAP that it “should be restructured to provide greater flexibility and appeal to providers and vendors.”
The Alliance of Specialty Physicians offered a suggestions in its comments, including
- Allowing physicians to remain in the current buy-and-bill system.
- Ensuring a minimum of three vendor choices per physician.
- Allowing physicians to easily switch between vendors and/or back to the current buy-and-bill system.
- Prohibiting CAP vendors from engaging in any utilization management techniques or medical review work.
The American Gastroenterological Association, which also supported to the Alliance of Specialty Physicians suggestions, said in separately filed comments that it is “unclear that the marketplace has changed in ways that would support the success of a new CAP program,” though the AGA “does not oppose” the idea of a new, voluntary CAP program.
The AGA noted that consolidation has improved the negotiation and purchasing power of physicians in the Part B space, while practices that remained independent as small and mid-sized groups “mostly shifted their Part B drug and biologic patients to hospital outpatient–based departments and infusion clinics because of the significant upfront costs of administering Part B drugs and biologics.”
FDA issues new REMS for immediate-release opioids
Opioid prescribers will need to be mindful of a new, expanded Risk Evaluation and Mitigation Strategy issued Sept. 18 by the Food and Drug Administration, covering immediate-release opioid analgesics used in the outpatient setting. The strategy also applies to extended-release and long-acting opioids, which have been subject to REMS since 2012.
The new REMS program requires for the first time that training be made available to health care providers who are involved in pain management. For the purposes of this REMS program, the training is not limited to just the prescriber, but includes nurses and pharmacists.
, including alternatives to opioids for pain management.
The FDA said it is in the process of approving a new label for opioids that will contain information about health care provider education that is now a part of the REMS.
“Our new effort is aimed at arming providers with the most current and comprehensive information on the appropriate management of pain,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “Appropriate prescribing practices and education are important steps that we are prioritizing to help address the human and financial toll of this crisis.”
Dr. Gottlieb added that the goal of the new REMS is to help prescribers with the latest evidence on the appropriate amount of doses that should be prescribed for a given condition and that the “aim is to reduce overall dispensing as a way to further reduce exposure to these drugs. Our goal is to help prevent patients from becoming addicted by decreasing unnecessary or inappropriate exposure to opioids and fostering rational prescribing to enable appropriate access to those patients who have legitimate medical need for these medicines.”
The FDA also approved a new guidance document that includes updated educational content.
Opioid prescribers will need to be mindful of a new, expanded Risk Evaluation and Mitigation Strategy issued Sept. 18 by the Food and Drug Administration, covering immediate-release opioid analgesics used in the outpatient setting. The strategy also applies to extended-release and long-acting opioids, which have been subject to REMS since 2012.
The new REMS program requires for the first time that training be made available to health care providers who are involved in pain management. For the purposes of this REMS program, the training is not limited to just the prescriber, but includes nurses and pharmacists.
, including alternatives to opioids for pain management.
The FDA said it is in the process of approving a new label for opioids that will contain information about health care provider education that is now a part of the REMS.
“Our new effort is aimed at arming providers with the most current and comprehensive information on the appropriate management of pain,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “Appropriate prescribing practices and education are important steps that we are prioritizing to help address the human and financial toll of this crisis.”
Dr. Gottlieb added that the goal of the new REMS is to help prescribers with the latest evidence on the appropriate amount of doses that should be prescribed for a given condition and that the “aim is to reduce overall dispensing as a way to further reduce exposure to these drugs. Our goal is to help prevent patients from becoming addicted by decreasing unnecessary or inappropriate exposure to opioids and fostering rational prescribing to enable appropriate access to those patients who have legitimate medical need for these medicines.”
The FDA also approved a new guidance document that includes updated educational content.
Opioid prescribers will need to be mindful of a new, expanded Risk Evaluation and Mitigation Strategy issued Sept. 18 by the Food and Drug Administration, covering immediate-release opioid analgesics used in the outpatient setting. The strategy also applies to extended-release and long-acting opioids, which have been subject to REMS since 2012.
The new REMS program requires for the first time that training be made available to health care providers who are involved in pain management. For the purposes of this REMS program, the training is not limited to just the prescriber, but includes nurses and pharmacists.
, including alternatives to opioids for pain management.
The FDA said it is in the process of approving a new label for opioids that will contain information about health care provider education that is now a part of the REMS.
“Our new effort is aimed at arming providers with the most current and comprehensive information on the appropriate management of pain,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “Appropriate prescribing practices and education are important steps that we are prioritizing to help address the human and financial toll of this crisis.”
Dr. Gottlieb added that the goal of the new REMS is to help prescribers with the latest evidence on the appropriate amount of doses that should be prescribed for a given condition and that the “aim is to reduce overall dispensing as a way to further reduce exposure to these drugs. Our goal is to help prevent patients from becoming addicted by decreasing unnecessary or inappropriate exposure to opioids and fostering rational prescribing to enable appropriate access to those patients who have legitimate medical need for these medicines.”
The FDA also approved a new guidance document that includes updated educational content.
E/M comments may fall on deaf ears at CMS
Doctors’ dismay at the proposed flattening of evaluation and management (E/M) payments seems to be falling on deaf ears.
More than 170 medical societies and organizations expressed their concern about the new payment structure for E/M codes proposed as part of the 2019 Medicare Physician Fee Schedule (PFS) in comments on the draft rule.
Yet, in the final days of the comment period, Seema Verma, administrator of the Centers for Medicare & Medicaid Services, took to Twitter to defend her agency’s plan.

The controversial proposal would set the payment rate for a level 1 E/M office visit for a new patient at $44, down from the current $45. Payment for levels 2-5 would be $135. Currently, payments for level 2 new patient visits are set at $76, level 3 at $110, level 4 at $167, and level 5 at $211.
For E/M office visits with established patients, the proposed rate would be $24 for level 1, up from the current $22. Payment for levels 2-5 would be $93. Under the current methodology, payments for established patient level 2 visits are set at $45, level 3 at $74, level 4 at $109, and level 5 at $148.
Offsetting the changes in payment are several new proposed add-on codes, according to CMS.
Despite the lower payment for more complex patient care, Ms. Verma touted the scheme’s budget neutrality.

Ms. Verma’s tweets come as medical societies filed their formal complaints on the proposal, mirroring concerns expressed in two letters sent to the agency ahead of the comment deadline. The letters, sent at the end of August and between the two of them signed by more than 170 medical associations, aimed to preempt the comment process. They called for the E/M proposal to be rescinded, claiming that the cuts would reduce access to Medicare services by patients and hurt physicians that treat the sickest patients and those who provide comprehensive primary care because the expected lower reimbursement. One suggested that the changes exacerbate workforce shortages.
In its formal comments, the American Medical Association said that given “the groundswell of opposition from individual physicians and nearly every physician and health professional organization in the country, including the AMA, we ask that CMS set aside its proposal to restructure payment and coding for E/M office and other outpatient visits while an expert physician work group, with input from a broad spectrum of physicians and other health professionals, develops an alternative that could be implemented in 2020.”
The proposed E/M changes “are not an improvement over the current documentation requirements and payment structure. The structure is flawed, and the proposal to reduce payments when E/M services are reported with procedures fails to account for fee schedule reductions that have already been taken on these codes,” according to comments submitted by the American Academy of Dermatology Association.
The American Society of Clinical Oncology said it “supports the Agency’s proposal to reduce documentation burdens for E&M services but pairing it with reductions in payment will negatively impact patient access and should be avoided.”
ASCO also called on the agency to withdraw its proposal to consolidate E/M payments, noting that offsetting payments from add-on codes do “not appear to fully offset the direct and indirect cuts to oncology reimbursement, is ambiguous, and lacks assurances of long-term durability.”
Surgeons “cannot support the collapse of work RVU [relative value unit] values into one single rate under the [physician fee schedule] that would be paid for services using the current CPT codes for level 2 through 5 E/M visits because this single rate is a calculation of several values that were resourced-based, but in and of itself is not a resource-based value. There is no assurance that the underlying math used to derive this single value correctly reflects the resources used to deliver care across a wide spectrum of providers in America,” according to comments submitted by the American College of Surgeons.
ACS also argued that it is “not possible to fully analyze the repercussions and potential distortions to the PFS from these policies individually or taken as a whole during the 60-day comment period.” The comments noted that ACS favors documentation reduction efforts included in the proposal, but urged CMS to delay finalizing any E/M changes until more work can be done in tandem with stakeholders to craft a better solution.
The American College of Cardiology voiced support for the documentation reduction aspects of the E/M proposal but urged CMS to “not finalize any E/M payment changes for 2019. The Agency makes it clear it believes documentation proposals are intrinsically linked to the payment proposals. It is not clear to the ACC exactly why that must be the case.”
ACC also voiced concern over a provision that would halve the least-expensive procedure or the E/M visit code when a physician bills for both simultaneously. “No data are described to indicate that 50% is a correct reduction. Instead, it appears that CMS chose 50% because the reduction is equivalent to the 6.7 million RVUs needed to offset other proposed changes for compressing E/M payment into single levels and allowing use of the new add-on codes.”
A key concern for the American Academy of Family Physicians was collapsing the levels 2 through 5 E/M visits into a single payment level.
Instead, AAFP recommended that CMS work with it and other medical societies to develop new codes and values to ensure proper payment for services. Instead of a primary care add-on code, CMS should increase E/M payments by 15% for services provided “by physicians who list their primary practice designation as family medicine, internal medicine, or geriatrics,” according to the comments.
AAFP is “concerned that the changes included in the proposed rule may harm the quality and cost of care for Medicare beneficiaries,” the comment letter states, adding that it is “possible that beneficiary out-of-pocket costs would increase due to more frequent physician or clinician visits.”
The American College of Rheumatology voiced its support for the focus “on reducing physician burden by simplifying documentation requirements,” but said it had “serious concerns about the changes to evaluation and management (E/M) codes that result in cuts in reimbursement to cognitive specialists for the complex services they provide.” It added that while there is support for the documentation reduction efforts, “we are skeptical that this proposal will simplify the reporting burden on providers in the Quality Payment Program. As proposed, the new plan proposes several ‘add-on’ codes that would likely prevent reduction in audits or documentation.”
The estimated 51 hours per doctor per year of time saved “are insufficient to offset the proposed cuts to reimbursement. For example, if a physician sees around 100 patients a week, this translates to under 40 seconds per patient, which is not a benefit that outweighs the proposed reduction in reimbursement.”
The American College of Physicians voiced its opposition to the E/M proposal, noting that it “strongly believes that cognitive care of more complex patients must be appropriately recognized with higher allowed payment rates than less complex care patients.” ACP said the even with the proposed add-on codes, the proposed changes undervalue cognitive care for the most complex patients.
Doctors’ dismay at the proposed flattening of evaluation and management (E/M) payments seems to be falling on deaf ears.
More than 170 medical societies and organizations expressed their concern about the new payment structure for E/M codes proposed as part of the 2019 Medicare Physician Fee Schedule (PFS) in comments on the draft rule.
Yet, in the final days of the comment period, Seema Verma, administrator of the Centers for Medicare & Medicaid Services, took to Twitter to defend her agency’s plan.

The controversial proposal would set the payment rate for a level 1 E/M office visit for a new patient at $44, down from the current $45. Payment for levels 2-5 would be $135. Currently, payments for level 2 new patient visits are set at $76, level 3 at $110, level 4 at $167, and level 5 at $211.
For E/M office visits with established patients, the proposed rate would be $24 for level 1, up from the current $22. Payment for levels 2-5 would be $93. Under the current methodology, payments for established patient level 2 visits are set at $45, level 3 at $74, level 4 at $109, and level 5 at $148.
Offsetting the changes in payment are several new proposed add-on codes, according to CMS.
Despite the lower payment for more complex patient care, Ms. Verma touted the scheme’s budget neutrality.

Ms. Verma’s tweets come as medical societies filed their formal complaints on the proposal, mirroring concerns expressed in two letters sent to the agency ahead of the comment deadline. The letters, sent at the end of August and between the two of them signed by more than 170 medical associations, aimed to preempt the comment process. They called for the E/M proposal to be rescinded, claiming that the cuts would reduce access to Medicare services by patients and hurt physicians that treat the sickest patients and those who provide comprehensive primary care because the expected lower reimbursement. One suggested that the changes exacerbate workforce shortages.
In its formal comments, the American Medical Association said that given “the groundswell of opposition from individual physicians and nearly every physician and health professional organization in the country, including the AMA, we ask that CMS set aside its proposal to restructure payment and coding for E/M office and other outpatient visits while an expert physician work group, with input from a broad spectrum of physicians and other health professionals, develops an alternative that could be implemented in 2020.”
The proposed E/M changes “are not an improvement over the current documentation requirements and payment structure. The structure is flawed, and the proposal to reduce payments when E/M services are reported with procedures fails to account for fee schedule reductions that have already been taken on these codes,” according to comments submitted by the American Academy of Dermatology Association.
The American Society of Clinical Oncology said it “supports the Agency’s proposal to reduce documentation burdens for E&M services but pairing it with reductions in payment will negatively impact patient access and should be avoided.”
ASCO also called on the agency to withdraw its proposal to consolidate E/M payments, noting that offsetting payments from add-on codes do “not appear to fully offset the direct and indirect cuts to oncology reimbursement, is ambiguous, and lacks assurances of long-term durability.”
Surgeons “cannot support the collapse of work RVU [relative value unit] values into one single rate under the [physician fee schedule] that would be paid for services using the current CPT codes for level 2 through 5 E/M visits because this single rate is a calculation of several values that were resourced-based, but in and of itself is not a resource-based value. There is no assurance that the underlying math used to derive this single value correctly reflects the resources used to deliver care across a wide spectrum of providers in America,” according to comments submitted by the American College of Surgeons.
ACS also argued that it is “not possible to fully analyze the repercussions and potential distortions to the PFS from these policies individually or taken as a whole during the 60-day comment period.” The comments noted that ACS favors documentation reduction efforts included in the proposal, but urged CMS to delay finalizing any E/M changes until more work can be done in tandem with stakeholders to craft a better solution.
The American College of Cardiology voiced support for the documentation reduction aspects of the E/M proposal but urged CMS to “not finalize any E/M payment changes for 2019. The Agency makes it clear it believes documentation proposals are intrinsically linked to the payment proposals. It is not clear to the ACC exactly why that must be the case.”
ACC also voiced concern over a provision that would halve the least-expensive procedure or the E/M visit code when a physician bills for both simultaneously. “No data are described to indicate that 50% is a correct reduction. Instead, it appears that CMS chose 50% because the reduction is equivalent to the 6.7 million RVUs needed to offset other proposed changes for compressing E/M payment into single levels and allowing use of the new add-on codes.”
A key concern for the American Academy of Family Physicians was collapsing the levels 2 through 5 E/M visits into a single payment level.
Instead, AAFP recommended that CMS work with it and other medical societies to develop new codes and values to ensure proper payment for services. Instead of a primary care add-on code, CMS should increase E/M payments by 15% for services provided “by physicians who list their primary practice designation as family medicine, internal medicine, or geriatrics,” according to the comments.
AAFP is “concerned that the changes included in the proposed rule may harm the quality and cost of care for Medicare beneficiaries,” the comment letter states, adding that it is “possible that beneficiary out-of-pocket costs would increase due to more frequent physician or clinician visits.”
The American College of Rheumatology voiced its support for the focus “on reducing physician burden by simplifying documentation requirements,” but said it had “serious concerns about the changes to evaluation and management (E/M) codes that result in cuts in reimbursement to cognitive specialists for the complex services they provide.” It added that while there is support for the documentation reduction efforts, “we are skeptical that this proposal will simplify the reporting burden on providers in the Quality Payment Program. As proposed, the new plan proposes several ‘add-on’ codes that would likely prevent reduction in audits or documentation.”
The estimated 51 hours per doctor per year of time saved “are insufficient to offset the proposed cuts to reimbursement. For example, if a physician sees around 100 patients a week, this translates to under 40 seconds per patient, which is not a benefit that outweighs the proposed reduction in reimbursement.”
The American College of Physicians voiced its opposition to the E/M proposal, noting that it “strongly believes that cognitive care of more complex patients must be appropriately recognized with higher allowed payment rates than less complex care patients.” ACP said the even with the proposed add-on codes, the proposed changes undervalue cognitive care for the most complex patients.
Doctors’ dismay at the proposed flattening of evaluation and management (E/M) payments seems to be falling on deaf ears.
More than 170 medical societies and organizations expressed their concern about the new payment structure for E/M codes proposed as part of the 2019 Medicare Physician Fee Schedule (PFS) in comments on the draft rule.
Yet, in the final days of the comment period, Seema Verma, administrator of the Centers for Medicare & Medicaid Services, took to Twitter to defend her agency’s plan.

The controversial proposal would set the payment rate for a level 1 E/M office visit for a new patient at $44, down from the current $45. Payment for levels 2-5 would be $135. Currently, payments for level 2 new patient visits are set at $76, level 3 at $110, level 4 at $167, and level 5 at $211.
For E/M office visits with established patients, the proposed rate would be $24 for level 1, up from the current $22. Payment for levels 2-5 would be $93. Under the current methodology, payments for established patient level 2 visits are set at $45, level 3 at $74, level 4 at $109, and level 5 at $148.
Offsetting the changes in payment are several new proposed add-on codes, according to CMS.
Despite the lower payment for more complex patient care, Ms. Verma touted the scheme’s budget neutrality.

Ms. Verma’s tweets come as medical societies filed their formal complaints on the proposal, mirroring concerns expressed in two letters sent to the agency ahead of the comment deadline. The letters, sent at the end of August and between the two of them signed by more than 170 medical associations, aimed to preempt the comment process. They called for the E/M proposal to be rescinded, claiming that the cuts would reduce access to Medicare services by patients and hurt physicians that treat the sickest patients and those who provide comprehensive primary care because the expected lower reimbursement. One suggested that the changes exacerbate workforce shortages.
In its formal comments, the American Medical Association said that given “the groundswell of opposition from individual physicians and nearly every physician and health professional organization in the country, including the AMA, we ask that CMS set aside its proposal to restructure payment and coding for E/M office and other outpatient visits while an expert physician work group, with input from a broad spectrum of physicians and other health professionals, develops an alternative that could be implemented in 2020.”
The proposed E/M changes “are not an improvement over the current documentation requirements and payment structure. The structure is flawed, and the proposal to reduce payments when E/M services are reported with procedures fails to account for fee schedule reductions that have already been taken on these codes,” according to comments submitted by the American Academy of Dermatology Association.
The American Society of Clinical Oncology said it “supports the Agency’s proposal to reduce documentation burdens for E&M services but pairing it with reductions in payment will negatively impact patient access and should be avoided.”
ASCO also called on the agency to withdraw its proposal to consolidate E/M payments, noting that offsetting payments from add-on codes do “not appear to fully offset the direct and indirect cuts to oncology reimbursement, is ambiguous, and lacks assurances of long-term durability.”
Surgeons “cannot support the collapse of work RVU [relative value unit] values into one single rate under the [physician fee schedule] that would be paid for services using the current CPT codes for level 2 through 5 E/M visits because this single rate is a calculation of several values that were resourced-based, but in and of itself is not a resource-based value. There is no assurance that the underlying math used to derive this single value correctly reflects the resources used to deliver care across a wide spectrum of providers in America,” according to comments submitted by the American College of Surgeons.
ACS also argued that it is “not possible to fully analyze the repercussions and potential distortions to the PFS from these policies individually or taken as a whole during the 60-day comment period.” The comments noted that ACS favors documentation reduction efforts included in the proposal, but urged CMS to delay finalizing any E/M changes until more work can be done in tandem with stakeholders to craft a better solution.
The American College of Cardiology voiced support for the documentation reduction aspects of the E/M proposal but urged CMS to “not finalize any E/M payment changes for 2019. The Agency makes it clear it believes documentation proposals are intrinsically linked to the payment proposals. It is not clear to the ACC exactly why that must be the case.”
ACC also voiced concern over a provision that would halve the least-expensive procedure or the E/M visit code when a physician bills for both simultaneously. “No data are described to indicate that 50% is a correct reduction. Instead, it appears that CMS chose 50% because the reduction is equivalent to the 6.7 million RVUs needed to offset other proposed changes for compressing E/M payment into single levels and allowing use of the new add-on codes.”
A key concern for the American Academy of Family Physicians was collapsing the levels 2 through 5 E/M visits into a single payment level.
Instead, AAFP recommended that CMS work with it and other medical societies to develop new codes and values to ensure proper payment for services. Instead of a primary care add-on code, CMS should increase E/M payments by 15% for services provided “by physicians who list their primary practice designation as family medicine, internal medicine, or geriatrics,” according to the comments.
AAFP is “concerned that the changes included in the proposed rule may harm the quality and cost of care for Medicare beneficiaries,” the comment letter states, adding that it is “possible that beneficiary out-of-pocket costs would increase due to more frequent physician or clinician visits.”
The American College of Rheumatology voiced its support for the focus “on reducing physician burden by simplifying documentation requirements,” but said it had “serious concerns about the changes to evaluation and management (E/M) codes that result in cuts in reimbursement to cognitive specialists for the complex services they provide.” It added that while there is support for the documentation reduction efforts, “we are skeptical that this proposal will simplify the reporting burden on providers in the Quality Payment Program. As proposed, the new plan proposes several ‘add-on’ codes that would likely prevent reduction in audits or documentation.”
The estimated 51 hours per doctor per year of time saved “are insufficient to offset the proposed cuts to reimbursement. For example, if a physician sees around 100 patients a week, this translates to under 40 seconds per patient, which is not a benefit that outweighs the proposed reduction in reimbursement.”
The American College of Physicians voiced its opposition to the E/M proposal, noting that it “strongly believes that cognitive care of more complex patients must be appropriately recognized with higher allowed payment rates than less complex care patients.” ACP said the even with the proposed add-on codes, the proposed changes undervalue cognitive care for the most complex patients.
SCOTUS: Kavanaugh suggests precedent will govern future abortion decisions
Supreme Court justice nominee Brett Kavanaugh suggested precedent would guide his thinking when it comes to deliberating on any Roe v. Wade challenges, but he came short of saying that he would not support overturning the landmark abortion rights case.
Testifying Sept. 5 before the Senate Judiciary Committee during a confirmation hearing, Judge Kavanaugh noted that the decision of Roe v. Wade has been reaffirmed in follow-up cases, and that would play a significant role in his approach to future challenges.
Sen. Dianne Feinstein (D-Calif.), the ranking Democrat on the panel, asked Judge Kavanaugh if he agreed with Justice Sandra Day O’Connor that “a woman’s right to control her reproductive life impacts her ability to ‘participate equally in the economic and social life of the nation?’ ”
“As a general proposition, I understand the importance of the precedent set forth in Roe v. Wade,” Judge Kavanaugh replied. “So Roe v. Wade held, of course, and is reaffirmed in Planned Parenthood v. Casey, that a woman has a constitutional right to obtain an abortion before viability, subject to reasonable regulation by the state up to the point where that regulation constitutes an undue burden on the woman’s right to obtain an abortion. One of the reasons for that holding, as explained by the court in Roe and also in Planned Parenthood v. Casey more fully, is along the lines of what you said, Sen. Feinstein, about the quote from Justice O’Connor.”
He continued: “That’s one of the rationales that undergirds Roe v. Wade. It’s one of the rationales that undergirds Planned Parenthood v. Casey.”
Sen. Feinstein followed by noting reports quoting Judge Kavanaugh as saying Roe v. Wade was “settled law,” inquired what that term means, and asked for further clarification as to whether it was settled precedent and whether it could be overturned.
“Senator, I said that it’s settled as a precedent of the Supreme Court, entitled the respect of principles of stare decisis,” he responded, referencing the legal principle of determining points in litigation according to precedent. “One of the important things to keep in mind about Roe v. Wade is that it has been reaffirmed many times over the past 45 years, as you know, and most prominently, most importantly reaffirmed in Planned Parenthood v. Casey in 1992. And as you well recall, Senator, I know when that case came up, the Supreme Court didn’t just reaffirm it in passing, the court specifically went through all factors of stare decisis in considering whether to overrule it.”
He noted that the joint opinion of Justice Anthony Kennedy, Justice O’Connor, and Justice David Souter, went to “great length” to go through those factors.
Judge Kavanaugh called Planned Parenthood v. Casey a “precedent-on-precedent. It is not as if it’s just a run-of-the-mill case that was decided and never been reconsidered. Casey specifically reconsidered [Roe v. Wade], applied the stare decisis factors and decided to reaffirm it. That makes Casey precedent-on-precedent.”
That said, Judge Kavanaugh did not say outright that Row v. Wade would not be overturned because of these factors.
The first 2 days of Judge Kavanaugh’s confirmation hearing were frequently interrupted by protesters shouting objections to his nomination. At press time, more than 120 protesters had been arrested, according to the U.S. Capitol Police.
Health care did surface in questions about the Affordable Care Act and in specific the current legal action in Texas that is looking to kill the health care law, but Judge Kavanaugh declined to answer any questions surrounding it, stating that he did not want to prejudge any potential case that could come before him.
Much of the questioning he faced was more geared toward opinions on presidential powers, including whether presidents could avoid subpoenas and whether a president could pardon himself, but he declined to answer those questions because they are ones that could come before him given the current political environment.
Judge Kavanaugh painted himself as of independent thought, pushing back at those who are saying that he will serve to protect the president and act as his puppet on the bench, citing cases where he went against former President George W. Bush, for whom he served as White House staff secretary and who eventually was appointed him to the D.C. Circuit Court in May 2006.
Supreme Court justice nominee Brett Kavanaugh suggested precedent would guide his thinking when it comes to deliberating on any Roe v. Wade challenges, but he came short of saying that he would not support overturning the landmark abortion rights case.
Testifying Sept. 5 before the Senate Judiciary Committee during a confirmation hearing, Judge Kavanaugh noted that the decision of Roe v. Wade has been reaffirmed in follow-up cases, and that would play a significant role in his approach to future challenges.
Sen. Dianne Feinstein (D-Calif.), the ranking Democrat on the panel, asked Judge Kavanaugh if he agreed with Justice Sandra Day O’Connor that “a woman’s right to control her reproductive life impacts her ability to ‘participate equally in the economic and social life of the nation?’ ”
“As a general proposition, I understand the importance of the precedent set forth in Roe v. Wade,” Judge Kavanaugh replied. “So Roe v. Wade held, of course, and is reaffirmed in Planned Parenthood v. Casey, that a woman has a constitutional right to obtain an abortion before viability, subject to reasonable regulation by the state up to the point where that regulation constitutes an undue burden on the woman’s right to obtain an abortion. One of the reasons for that holding, as explained by the court in Roe and also in Planned Parenthood v. Casey more fully, is along the lines of what you said, Sen. Feinstein, about the quote from Justice O’Connor.”
He continued: “That’s one of the rationales that undergirds Roe v. Wade. It’s one of the rationales that undergirds Planned Parenthood v. Casey.”
Sen. Feinstein followed by noting reports quoting Judge Kavanaugh as saying Roe v. Wade was “settled law,” inquired what that term means, and asked for further clarification as to whether it was settled precedent and whether it could be overturned.
“Senator, I said that it’s settled as a precedent of the Supreme Court, entitled the respect of principles of stare decisis,” he responded, referencing the legal principle of determining points in litigation according to precedent. “One of the important things to keep in mind about Roe v. Wade is that it has been reaffirmed many times over the past 45 years, as you know, and most prominently, most importantly reaffirmed in Planned Parenthood v. Casey in 1992. And as you well recall, Senator, I know when that case came up, the Supreme Court didn’t just reaffirm it in passing, the court specifically went through all factors of stare decisis in considering whether to overrule it.”
He noted that the joint opinion of Justice Anthony Kennedy, Justice O’Connor, and Justice David Souter, went to “great length” to go through those factors.
Judge Kavanaugh called Planned Parenthood v. Casey a “precedent-on-precedent. It is not as if it’s just a run-of-the-mill case that was decided and never been reconsidered. Casey specifically reconsidered [Roe v. Wade], applied the stare decisis factors and decided to reaffirm it. That makes Casey precedent-on-precedent.”
That said, Judge Kavanaugh did not say outright that Row v. Wade would not be overturned because of these factors.
The first 2 days of Judge Kavanaugh’s confirmation hearing were frequently interrupted by protesters shouting objections to his nomination. At press time, more than 120 protesters had been arrested, according to the U.S. Capitol Police.
Health care did surface in questions about the Affordable Care Act and in specific the current legal action in Texas that is looking to kill the health care law, but Judge Kavanaugh declined to answer any questions surrounding it, stating that he did not want to prejudge any potential case that could come before him.
Much of the questioning he faced was more geared toward opinions on presidential powers, including whether presidents could avoid subpoenas and whether a president could pardon himself, but he declined to answer those questions because they are ones that could come before him given the current political environment.
Judge Kavanaugh painted himself as of independent thought, pushing back at those who are saying that he will serve to protect the president and act as his puppet on the bench, citing cases where he went against former President George W. Bush, for whom he served as White House staff secretary and who eventually was appointed him to the D.C. Circuit Court in May 2006.
Supreme Court justice nominee Brett Kavanaugh suggested precedent would guide his thinking when it comes to deliberating on any Roe v. Wade challenges, but he came short of saying that he would not support overturning the landmark abortion rights case.
Testifying Sept. 5 before the Senate Judiciary Committee during a confirmation hearing, Judge Kavanaugh noted that the decision of Roe v. Wade has been reaffirmed in follow-up cases, and that would play a significant role in his approach to future challenges.
Sen. Dianne Feinstein (D-Calif.), the ranking Democrat on the panel, asked Judge Kavanaugh if he agreed with Justice Sandra Day O’Connor that “a woman’s right to control her reproductive life impacts her ability to ‘participate equally in the economic and social life of the nation?’ ”
“As a general proposition, I understand the importance of the precedent set forth in Roe v. Wade,” Judge Kavanaugh replied. “So Roe v. Wade held, of course, and is reaffirmed in Planned Parenthood v. Casey, that a woman has a constitutional right to obtain an abortion before viability, subject to reasonable regulation by the state up to the point where that regulation constitutes an undue burden on the woman’s right to obtain an abortion. One of the reasons for that holding, as explained by the court in Roe and also in Planned Parenthood v. Casey more fully, is along the lines of what you said, Sen. Feinstein, about the quote from Justice O’Connor.”
He continued: “That’s one of the rationales that undergirds Roe v. Wade. It’s one of the rationales that undergirds Planned Parenthood v. Casey.”
Sen. Feinstein followed by noting reports quoting Judge Kavanaugh as saying Roe v. Wade was “settled law,” inquired what that term means, and asked for further clarification as to whether it was settled precedent and whether it could be overturned.
“Senator, I said that it’s settled as a precedent of the Supreme Court, entitled the respect of principles of stare decisis,” he responded, referencing the legal principle of determining points in litigation according to precedent. “One of the important things to keep in mind about Roe v. Wade is that it has been reaffirmed many times over the past 45 years, as you know, and most prominently, most importantly reaffirmed in Planned Parenthood v. Casey in 1992. And as you well recall, Senator, I know when that case came up, the Supreme Court didn’t just reaffirm it in passing, the court specifically went through all factors of stare decisis in considering whether to overrule it.”
He noted that the joint opinion of Justice Anthony Kennedy, Justice O’Connor, and Justice David Souter, went to “great length” to go through those factors.
Judge Kavanaugh called Planned Parenthood v. Casey a “precedent-on-precedent. It is not as if it’s just a run-of-the-mill case that was decided and never been reconsidered. Casey specifically reconsidered [Roe v. Wade], applied the stare decisis factors and decided to reaffirm it. That makes Casey precedent-on-precedent.”
That said, Judge Kavanaugh did not say outright that Row v. Wade would not be overturned because of these factors.
The first 2 days of Judge Kavanaugh’s confirmation hearing were frequently interrupted by protesters shouting objections to his nomination. At press time, more than 120 protesters had been arrested, according to the U.S. Capitol Police.
Health care did surface in questions about the Affordable Care Act and in specific the current legal action in Texas that is looking to kill the health care law, but Judge Kavanaugh declined to answer any questions surrounding it, stating that he did not want to prejudge any potential case that could come before him.
Much of the questioning he faced was more geared toward opinions on presidential powers, including whether presidents could avoid subpoenas and whether a president could pardon himself, but he declined to answer those questions because they are ones that could come before him given the current political environment.
Judge Kavanaugh painted himself as of independent thought, pushing back at those who are saying that he will serve to protect the president and act as his puppet on the bench, citing cases where he went against former President George W. Bush, for whom he served as White House staff secretary and who eventually was appointed him to the D.C. Circuit Court in May 2006.