User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Gun policy reform related to mental illness ‘a complex puzzle’
LAS VEGAS – On April 16, 2007, a 23-year-old man shot 32 people to death and injured 23 others during a massacre on the campus of Virginia Tech University in Blacksburg, before taking his own life. On the same day, 231 other gun casualties occurred in other areas of the United States, 83 of them fatal and 148 nonfatal, according to Jeffrey W. Swanson, PhD.
“These were domestic violence incidents, suicides, some unintentional injuries, and a few law enforcement actions,” he said at an annual psychopharmacology update held by the Nevada Psychiatric Association. “This is the daily drip, drip, drip of gun violence in our country.”
According to data from the Substance Abuse and Mental Health Services Administration, 9.8 million adults in the United States have a serious mental illness, 2.5 million have a co-occurring substance use disorder, 1.9 million have no insurance, 3.1 million go without treatment for their mental illness, 100,000 are homeless, and about 1 million find themselves in jail or in prison. “We probably have more people with a serious mental illness in one of our big-city jails every day than we ever had in the largest asylum in the middle of the 20th century,” said Dr. Swanson, professor of psychiatry and behavioral sciences at Duke University, Durham, N.C. “I think that’s scandalous. It probably costs our society $318 billion per year. On the other hand, we have gun-related violence that claims 36,000 lives each year. One economist estimates that costs our society $174 billion per year. Those are two different public health problems that come together on their edges.”
Americans tend to think about mental illness and gun violence after all-too-frequent mass shootings at schools, workplaces, or concert events, he continued. “A mass shooting at a public place is so terrifying, and destructing and irrational,” he said. “It’s everything we don’t want our ordinary lives to be. We want our lives to be safe and to make sense. A mass shooting is none of those things. The act of going out and shooting a bunch of strangers is not the act of a healthy mind.
“But that person is very atypical in two ways: atypical of people with serious mental illnesses, most of whom are not violent and never will be, and atypical of the perpetrators of gun violence, the vast majority of whom do not have serious mental illnesses. But talking about both of these problems together in the aftermath of a mass shooting is too often the conversation that we’re stuck with.”
In 2015, there were 36,252 gun-related deaths in the United States. Of these, 61% were suicides, 36% were homicides, 2% were police-related, and 1% were unintentional. “We hear prominent voices in the public square today telling us that this is a problem related to mental health, and that the logical solution is to fix the mental health care system,” Dr. Swanson said. “As a mental health services researcher who has spent my career trying to build evidence for better policies to improve outcomes for people with serious mental illnesses, and knowing that the mental health care system we have is fragmented and overburdened – that the treatments we have don’t work very well for some people – I firmly believe we need to invest in and improve the mental health care system. But the idea that this alone is going to solve our problem of gun violence is misguided, in my opinion.”
Homicide data from the International Crime Victim Survey, conducted by Gallup Europe in 2000, found that in the United States, assaults are three more times likely to involve guns than in 14 other industrialized countries, including France, the United Kingdom, Canada, Spain, Belgium, and Australia. Moreover, there is an average of 97 guns for every 100 people in the United States, compared with an average of 17 guns per 100 people in all other industrialized countries. The violent crime rate in the United States is close to the average in 15 other industrialized countries in Western Europe, the United Kingdom, Canada, Australia, and Japan: 5.5%, compared with 6.3%.
At the same time, the United States has a homicide rate several times higher than the rate in these other countries. “How can you have this paradox where our crime rate is about average, but our homicide rate is not average?” Dr. Swanson asked. “It has something to do with our unique relationship with firearms.” The way he sees it, after the Supreme Court decision in District of Columbia v. Heller, confirming the individual right to bear arms under the Second Amendment, “gun control is really ‘people control.’ It focuses on dangerous people. We can’t broadly limit legal access to guns. We have to figure out, ‘Who are the people so dangerous that it is justified to limit their Second Amendment right?’ That’s very hard to do. Why? Because gun violence is very complicated. It’s caused by many factors that interact with each other, and they are nonspecific – meaning that they apply to many more people who are not going to do the thing you’re trying to prevent than who will.
“Serious mental illness may be one factor – particularly in terms of gun suicide – but it contributes very little (only about 4%) to overall interpersonal violence. People with serious mental illnesses are far more likely to be victims of violence than they are to be perpetrators.”
Factors linked to a propensity for violence include being young and male, poverty, exposure to violence, being abused as a child, and substance abuse. “,” he said.
Recently, Dr. Swanson led a team of researchers that set out to analyze descriptive information on 762 individuals subjected to gun removal in Connecticut between 1999 and 2013, as part of that state’s “risk warrant” gun law (Law Contemp Probl. 2017;[80]179-208). Enacted in 1999, the statute allows police, after independently investigating and determining probable cause, to obtain a court warrant and remove guns from anyone who is found to pose an imminent risk of harming someone else or himself or herself.
Dr. Swanson and his associates found that the individuals had an average of seven guns, 92% were male, and their mean age was 47 years. Most (81%) were married or cohabitating, 46% had a mental health or substance abuse record, 12% had an arrest leading to conviction in the year before or after, 61% were considered a risk of harm to self, 49% of calls to police about the individual came from family members or acquaintances, and 55% were transported to the emergency department or hospital. The researchers found that the proportion of people in treatment in the public behavioral health care system increased from 12% before the gun removal event to 29% after the gun removal event.
When they matched the death records, they found 21 suicides among these 762 patients, which was about 40 times greater than the suicide rate in the general adult population in Connecticut, 12 per 100,000. “That’s important, because if you think about suicide as a needle in a haystack, this law provides a way to identify a much smaller haystack with a lot more needles in it,” Dr. Swanson said. “So it’s more efficient to try to intervene to prevent gun suicide or violence in a group like that, and it shows that this policy is narrowly tailored.” When the researchers examined the method of suicide, they found that only 6 out of 21 individuals used a firearm, and none of the gun-involved suicides happened during the year when the firearms were retained. “They all happened when the person became eligible to get their guns back,” he said. “Using information on the fatality rate for each method of suicide, we estimated that for every 10-12 gun removals, one life was saved. Is that high or low? It depends on where you stand. If you’re someone who cares a lot about the right to own firearms, you might think that’s unacceptable. If you’re like me and you have had three gun suicides in your extended family, every one is a tragedy, a life cut short. We want to put this kind of calculation in the hands of lawmakers so they can see what is in the balance between risks and rights.”
Dr. Swanson ended his presentation by offering five principles aimed at guiding gun policy reforms related to mental illness:
- Prioritize contemporaneous risk assessment based on evidence of behaviors that correlate with violence and self-harm at specific times, not mental illness or treatment history per se as a category of exclusion.
- Preempt existing gun access, rather than simply thwarting a new gun purchase by a dangerous person.
- Provide legal due process for deprivation of gun rights.
- Preserve confidential therapeutic relationships. “You don’t want a crisis-driven law that requires doctors to report any patient who talks with them about suicide, because that can have a chilling effect and keep people away from seeking treatment, and also inhibit their disclosures in therapy,” he said.
Prevent the unpredictable through comprehensive background checks, but also by reducing the social determinant of violence and investing in improved access to mental health and substance abuse services.
“This is a complex puzzle, with maybe a couple of pieces hidden under the rug,” Dr. Swanson said.
He reported having no financial disclosures.
LAS VEGAS – On April 16, 2007, a 23-year-old man shot 32 people to death and injured 23 others during a massacre on the campus of Virginia Tech University in Blacksburg, before taking his own life. On the same day, 231 other gun casualties occurred in other areas of the United States, 83 of them fatal and 148 nonfatal, according to Jeffrey W. Swanson, PhD.
“These were domestic violence incidents, suicides, some unintentional injuries, and a few law enforcement actions,” he said at an annual psychopharmacology update held by the Nevada Psychiatric Association. “This is the daily drip, drip, drip of gun violence in our country.”
According to data from the Substance Abuse and Mental Health Services Administration, 9.8 million adults in the United States have a serious mental illness, 2.5 million have a co-occurring substance use disorder, 1.9 million have no insurance, 3.1 million go without treatment for their mental illness, 100,000 are homeless, and about 1 million find themselves in jail or in prison. “We probably have more people with a serious mental illness in one of our big-city jails every day than we ever had in the largest asylum in the middle of the 20th century,” said Dr. Swanson, professor of psychiatry and behavioral sciences at Duke University, Durham, N.C. “I think that’s scandalous. It probably costs our society $318 billion per year. On the other hand, we have gun-related violence that claims 36,000 lives each year. One economist estimates that costs our society $174 billion per year. Those are two different public health problems that come together on their edges.”
Americans tend to think about mental illness and gun violence after all-too-frequent mass shootings at schools, workplaces, or concert events, he continued. “A mass shooting at a public place is so terrifying, and destructing and irrational,” he said. “It’s everything we don’t want our ordinary lives to be. We want our lives to be safe and to make sense. A mass shooting is none of those things. The act of going out and shooting a bunch of strangers is not the act of a healthy mind.
“But that person is very atypical in two ways: atypical of people with serious mental illnesses, most of whom are not violent and never will be, and atypical of the perpetrators of gun violence, the vast majority of whom do not have serious mental illnesses. But talking about both of these problems together in the aftermath of a mass shooting is too often the conversation that we’re stuck with.”
In 2015, there were 36,252 gun-related deaths in the United States. Of these, 61% were suicides, 36% were homicides, 2% were police-related, and 1% were unintentional. “We hear prominent voices in the public square today telling us that this is a problem related to mental health, and that the logical solution is to fix the mental health care system,” Dr. Swanson said. “As a mental health services researcher who has spent my career trying to build evidence for better policies to improve outcomes for people with serious mental illnesses, and knowing that the mental health care system we have is fragmented and overburdened – that the treatments we have don’t work very well for some people – I firmly believe we need to invest in and improve the mental health care system. But the idea that this alone is going to solve our problem of gun violence is misguided, in my opinion.”
Homicide data from the International Crime Victim Survey, conducted by Gallup Europe in 2000, found that in the United States, assaults are three more times likely to involve guns than in 14 other industrialized countries, including France, the United Kingdom, Canada, Spain, Belgium, and Australia. Moreover, there is an average of 97 guns for every 100 people in the United States, compared with an average of 17 guns per 100 people in all other industrialized countries. The violent crime rate in the United States is close to the average in 15 other industrialized countries in Western Europe, the United Kingdom, Canada, Australia, and Japan: 5.5%, compared with 6.3%.
At the same time, the United States has a homicide rate several times higher than the rate in these other countries. “How can you have this paradox where our crime rate is about average, but our homicide rate is not average?” Dr. Swanson asked. “It has something to do with our unique relationship with firearms.” The way he sees it, after the Supreme Court decision in District of Columbia v. Heller, confirming the individual right to bear arms under the Second Amendment, “gun control is really ‘people control.’ It focuses on dangerous people. We can’t broadly limit legal access to guns. We have to figure out, ‘Who are the people so dangerous that it is justified to limit their Second Amendment right?’ That’s very hard to do. Why? Because gun violence is very complicated. It’s caused by many factors that interact with each other, and they are nonspecific – meaning that they apply to many more people who are not going to do the thing you’re trying to prevent than who will.
“Serious mental illness may be one factor – particularly in terms of gun suicide – but it contributes very little (only about 4%) to overall interpersonal violence. People with serious mental illnesses are far more likely to be victims of violence than they are to be perpetrators.”
Factors linked to a propensity for violence include being young and male, poverty, exposure to violence, being abused as a child, and substance abuse. “,” he said.
Recently, Dr. Swanson led a team of researchers that set out to analyze descriptive information on 762 individuals subjected to gun removal in Connecticut between 1999 and 2013, as part of that state’s “risk warrant” gun law (Law Contemp Probl. 2017;[80]179-208). Enacted in 1999, the statute allows police, after independently investigating and determining probable cause, to obtain a court warrant and remove guns from anyone who is found to pose an imminent risk of harming someone else or himself or herself.
Dr. Swanson and his associates found that the individuals had an average of seven guns, 92% were male, and their mean age was 47 years. Most (81%) were married or cohabitating, 46% had a mental health or substance abuse record, 12% had an arrest leading to conviction in the year before or after, 61% were considered a risk of harm to self, 49% of calls to police about the individual came from family members or acquaintances, and 55% were transported to the emergency department or hospital. The researchers found that the proportion of people in treatment in the public behavioral health care system increased from 12% before the gun removal event to 29% after the gun removal event.
When they matched the death records, they found 21 suicides among these 762 patients, which was about 40 times greater than the suicide rate in the general adult population in Connecticut, 12 per 100,000. “That’s important, because if you think about suicide as a needle in a haystack, this law provides a way to identify a much smaller haystack with a lot more needles in it,” Dr. Swanson said. “So it’s more efficient to try to intervene to prevent gun suicide or violence in a group like that, and it shows that this policy is narrowly tailored.” When the researchers examined the method of suicide, they found that only 6 out of 21 individuals used a firearm, and none of the gun-involved suicides happened during the year when the firearms were retained. “They all happened when the person became eligible to get their guns back,” he said. “Using information on the fatality rate for each method of suicide, we estimated that for every 10-12 gun removals, one life was saved. Is that high or low? It depends on where you stand. If you’re someone who cares a lot about the right to own firearms, you might think that’s unacceptable. If you’re like me and you have had three gun suicides in your extended family, every one is a tragedy, a life cut short. We want to put this kind of calculation in the hands of lawmakers so they can see what is in the balance between risks and rights.”
Dr. Swanson ended his presentation by offering five principles aimed at guiding gun policy reforms related to mental illness:
- Prioritize contemporaneous risk assessment based on evidence of behaviors that correlate with violence and self-harm at specific times, not mental illness or treatment history per se as a category of exclusion.
- Preempt existing gun access, rather than simply thwarting a new gun purchase by a dangerous person.
- Provide legal due process for deprivation of gun rights.
- Preserve confidential therapeutic relationships. “You don’t want a crisis-driven law that requires doctors to report any patient who talks with them about suicide, because that can have a chilling effect and keep people away from seeking treatment, and also inhibit their disclosures in therapy,” he said.
Prevent the unpredictable through comprehensive background checks, but also by reducing the social determinant of violence and investing in improved access to mental health and substance abuse services.
“This is a complex puzzle, with maybe a couple of pieces hidden under the rug,” Dr. Swanson said.
He reported having no financial disclosures.
LAS VEGAS – On April 16, 2007, a 23-year-old man shot 32 people to death and injured 23 others during a massacre on the campus of Virginia Tech University in Blacksburg, before taking his own life. On the same day, 231 other gun casualties occurred in other areas of the United States, 83 of them fatal and 148 nonfatal, according to Jeffrey W. Swanson, PhD.
“These were domestic violence incidents, suicides, some unintentional injuries, and a few law enforcement actions,” he said at an annual psychopharmacology update held by the Nevada Psychiatric Association. “This is the daily drip, drip, drip of gun violence in our country.”
According to data from the Substance Abuse and Mental Health Services Administration, 9.8 million adults in the United States have a serious mental illness, 2.5 million have a co-occurring substance use disorder, 1.9 million have no insurance, 3.1 million go without treatment for their mental illness, 100,000 are homeless, and about 1 million find themselves in jail or in prison. “We probably have more people with a serious mental illness in one of our big-city jails every day than we ever had in the largest asylum in the middle of the 20th century,” said Dr. Swanson, professor of psychiatry and behavioral sciences at Duke University, Durham, N.C. “I think that’s scandalous. It probably costs our society $318 billion per year. On the other hand, we have gun-related violence that claims 36,000 lives each year. One economist estimates that costs our society $174 billion per year. Those are two different public health problems that come together on their edges.”
Americans tend to think about mental illness and gun violence after all-too-frequent mass shootings at schools, workplaces, or concert events, he continued. “A mass shooting at a public place is so terrifying, and destructing and irrational,” he said. “It’s everything we don’t want our ordinary lives to be. We want our lives to be safe and to make sense. A mass shooting is none of those things. The act of going out and shooting a bunch of strangers is not the act of a healthy mind.
“But that person is very atypical in two ways: atypical of people with serious mental illnesses, most of whom are not violent and never will be, and atypical of the perpetrators of gun violence, the vast majority of whom do not have serious mental illnesses. But talking about both of these problems together in the aftermath of a mass shooting is too often the conversation that we’re stuck with.”
In 2015, there were 36,252 gun-related deaths in the United States. Of these, 61% were suicides, 36% were homicides, 2% were police-related, and 1% were unintentional. “We hear prominent voices in the public square today telling us that this is a problem related to mental health, and that the logical solution is to fix the mental health care system,” Dr. Swanson said. “As a mental health services researcher who has spent my career trying to build evidence for better policies to improve outcomes for people with serious mental illnesses, and knowing that the mental health care system we have is fragmented and overburdened – that the treatments we have don’t work very well for some people – I firmly believe we need to invest in and improve the mental health care system. But the idea that this alone is going to solve our problem of gun violence is misguided, in my opinion.”
Homicide data from the International Crime Victim Survey, conducted by Gallup Europe in 2000, found that in the United States, assaults are three more times likely to involve guns than in 14 other industrialized countries, including France, the United Kingdom, Canada, Spain, Belgium, and Australia. Moreover, there is an average of 97 guns for every 100 people in the United States, compared with an average of 17 guns per 100 people in all other industrialized countries. The violent crime rate in the United States is close to the average in 15 other industrialized countries in Western Europe, the United Kingdom, Canada, Australia, and Japan: 5.5%, compared with 6.3%.
At the same time, the United States has a homicide rate several times higher than the rate in these other countries. “How can you have this paradox where our crime rate is about average, but our homicide rate is not average?” Dr. Swanson asked. “It has something to do with our unique relationship with firearms.” The way he sees it, after the Supreme Court decision in District of Columbia v. Heller, confirming the individual right to bear arms under the Second Amendment, “gun control is really ‘people control.’ It focuses on dangerous people. We can’t broadly limit legal access to guns. We have to figure out, ‘Who are the people so dangerous that it is justified to limit their Second Amendment right?’ That’s very hard to do. Why? Because gun violence is very complicated. It’s caused by many factors that interact with each other, and they are nonspecific – meaning that they apply to many more people who are not going to do the thing you’re trying to prevent than who will.
“Serious mental illness may be one factor – particularly in terms of gun suicide – but it contributes very little (only about 4%) to overall interpersonal violence. People with serious mental illnesses are far more likely to be victims of violence than they are to be perpetrators.”
Factors linked to a propensity for violence include being young and male, poverty, exposure to violence, being abused as a child, and substance abuse. “,” he said.
Recently, Dr. Swanson led a team of researchers that set out to analyze descriptive information on 762 individuals subjected to gun removal in Connecticut between 1999 and 2013, as part of that state’s “risk warrant” gun law (Law Contemp Probl. 2017;[80]179-208). Enacted in 1999, the statute allows police, after independently investigating and determining probable cause, to obtain a court warrant and remove guns from anyone who is found to pose an imminent risk of harming someone else or himself or herself.
Dr. Swanson and his associates found that the individuals had an average of seven guns, 92% were male, and their mean age was 47 years. Most (81%) were married or cohabitating, 46% had a mental health or substance abuse record, 12% had an arrest leading to conviction in the year before or after, 61% were considered a risk of harm to self, 49% of calls to police about the individual came from family members or acquaintances, and 55% were transported to the emergency department or hospital. The researchers found that the proportion of people in treatment in the public behavioral health care system increased from 12% before the gun removal event to 29% after the gun removal event.
When they matched the death records, they found 21 suicides among these 762 patients, which was about 40 times greater than the suicide rate in the general adult population in Connecticut, 12 per 100,000. “That’s important, because if you think about suicide as a needle in a haystack, this law provides a way to identify a much smaller haystack with a lot more needles in it,” Dr. Swanson said. “So it’s more efficient to try to intervene to prevent gun suicide or violence in a group like that, and it shows that this policy is narrowly tailored.” When the researchers examined the method of suicide, they found that only 6 out of 21 individuals used a firearm, and none of the gun-involved suicides happened during the year when the firearms were retained. “They all happened when the person became eligible to get their guns back,” he said. “Using information on the fatality rate for each method of suicide, we estimated that for every 10-12 gun removals, one life was saved. Is that high or low? It depends on where you stand. If you’re someone who cares a lot about the right to own firearms, you might think that’s unacceptable. If you’re like me and you have had three gun suicides in your extended family, every one is a tragedy, a life cut short. We want to put this kind of calculation in the hands of lawmakers so they can see what is in the balance between risks and rights.”
Dr. Swanson ended his presentation by offering five principles aimed at guiding gun policy reforms related to mental illness:
- Prioritize contemporaneous risk assessment based on evidence of behaviors that correlate with violence and self-harm at specific times, not mental illness or treatment history per se as a category of exclusion.
- Preempt existing gun access, rather than simply thwarting a new gun purchase by a dangerous person.
- Provide legal due process for deprivation of gun rights.
- Preserve confidential therapeutic relationships. “You don’t want a crisis-driven law that requires doctors to report any patient who talks with them about suicide, because that can have a chilling effect and keep people away from seeking treatment, and also inhibit their disclosures in therapy,” he said.
Prevent the unpredictable through comprehensive background checks, but also by reducing the social determinant of violence and investing in improved access to mental health and substance abuse services.
“This is a complex puzzle, with maybe a couple of pieces hidden under the rug,” Dr. Swanson said.
He reported having no financial disclosures.
REPORTING FROM NPA 2018
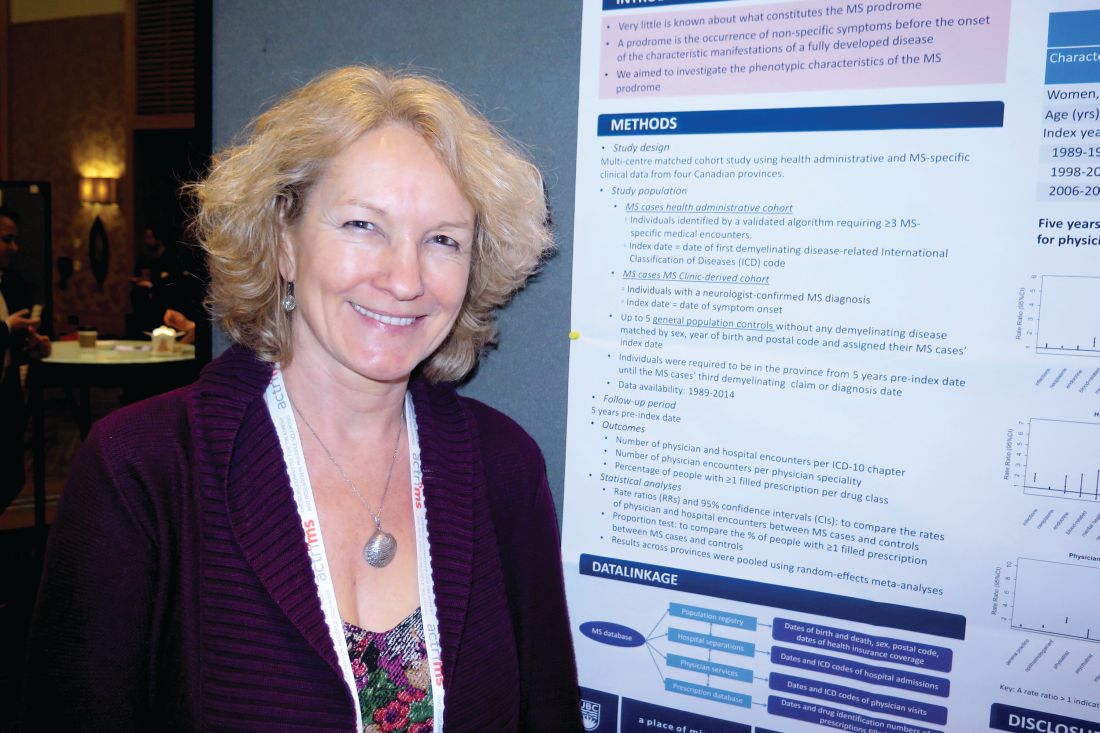
High dose of novel compound for relapsing-remitting MS shows promise
SAN DIEGO – Early results of the novel human endogenous retrovirus-W antagonist GNbAC1 in a phase 2 trial of patients with relapsing-remitting multiple sclerosis demonstrated evidence of remyelination at week 24 among high-dose users, but it did not meet its primary endpoint of active lesions seen on MRI.
In an interview at ACTRIMS Forum 2018, held by the Americas Committee for Treatment and Research in Multiple Sclerosis, study author Robert Glanzman, MD, said that GNbAC1 is a monoclonal antibody that targets and blocks the envelope protein pHER-W ENV, a potent agonist of Toll-like receptor 4. It thereby inhibits TLR4-mediated pathogenicity, which includes activation of macrophages and microglia into proinflammatory phenotypes and direct inhibition of remyelination via TLR4.
In a study known as CHANGE-MS, 270 patients with relapsing-remitting MS were randomized to one of three doses of the GNbAC1 (6, 12, or 18 mg/kg), or placebo via monthly IV infusion over 6 months. The study was conducted at 70 centers in 13 European countries over the past 3 years. It had a 24-week, double-blind, placebo-controlled period, followed by a 24-week, dose-blind, active-only treatment period, with placebo patients randomized to the three different doses of GNbA1C. Brain MRI scans were performed at weeks 12, 16, 20, 24, and 48, to look for evidence of remyelination.
The mean age of patients was 38 years and 65% were female. The researchers observed no safety concerns and no significant effect on inflammatory measures over weeks 12-24, even though the absolute number of lesions was reduced by about 50%. Although the primary endpoint of the cumulative number of gadolinium-enhancing lesions seen on brain MRI scans every 4 weeks during weeks 12-24 was not met, post hoc analyses suggest a decrease in neuroinflammation in the 18 mg/kg GNbA1C group at week 24, compared with placebo (P = .008). “A consistent increase in MT [magnetization transfer] ratio signal was observed in normal-appearing white matter and cerebral cortex at the highest dose, suggesting remyelination,” Dr. Glanzman added. “We gained about a quarter or half of percent in normal-appearing white matter at the cerebral cortex at the high dose. Normally, MS patients lose white matter over time, both in the cortex and in gray matter. We’re actually showing evidence of remyelination, which is really exciting. If these data are replicated and confirmed at week 48, we think we really have an exciting compound.”
GeNeuro sponsored the study.
Full 48-week analyses from CHANGE-MS are expected to be unveiled at the 2018 annual meeting American Academy of Neurology.
SOURCE: Glanzman R et al. Abstract P034.
SAN DIEGO – Early results of the novel human endogenous retrovirus-W antagonist GNbAC1 in a phase 2 trial of patients with relapsing-remitting multiple sclerosis demonstrated evidence of remyelination at week 24 among high-dose users, but it did not meet its primary endpoint of active lesions seen on MRI.
In an interview at ACTRIMS Forum 2018, held by the Americas Committee for Treatment and Research in Multiple Sclerosis, study author Robert Glanzman, MD, said that GNbAC1 is a monoclonal antibody that targets and blocks the envelope protein pHER-W ENV, a potent agonist of Toll-like receptor 4. It thereby inhibits TLR4-mediated pathogenicity, which includes activation of macrophages and microglia into proinflammatory phenotypes and direct inhibition of remyelination via TLR4.
In a study known as CHANGE-MS, 270 patients with relapsing-remitting MS were randomized to one of three doses of the GNbAC1 (6, 12, or 18 mg/kg), or placebo via monthly IV infusion over 6 months. The study was conducted at 70 centers in 13 European countries over the past 3 years. It had a 24-week, double-blind, placebo-controlled period, followed by a 24-week, dose-blind, active-only treatment period, with placebo patients randomized to the three different doses of GNbA1C. Brain MRI scans were performed at weeks 12, 16, 20, 24, and 48, to look for evidence of remyelination.
The mean age of patients was 38 years and 65% were female. The researchers observed no safety concerns and no significant effect on inflammatory measures over weeks 12-24, even though the absolute number of lesions was reduced by about 50%. Although the primary endpoint of the cumulative number of gadolinium-enhancing lesions seen on brain MRI scans every 4 weeks during weeks 12-24 was not met, post hoc analyses suggest a decrease in neuroinflammation in the 18 mg/kg GNbA1C group at week 24, compared with placebo (P = .008). “A consistent increase in MT [magnetization transfer] ratio signal was observed in normal-appearing white matter and cerebral cortex at the highest dose, suggesting remyelination,” Dr. Glanzman added. “We gained about a quarter or half of percent in normal-appearing white matter at the cerebral cortex at the high dose. Normally, MS patients lose white matter over time, both in the cortex and in gray matter. We’re actually showing evidence of remyelination, which is really exciting. If these data are replicated and confirmed at week 48, we think we really have an exciting compound.”
GeNeuro sponsored the study.
Full 48-week analyses from CHANGE-MS are expected to be unveiled at the 2018 annual meeting American Academy of Neurology.
SOURCE: Glanzman R et al. Abstract P034.
SAN DIEGO – Early results of the novel human endogenous retrovirus-W antagonist GNbAC1 in a phase 2 trial of patients with relapsing-remitting multiple sclerosis demonstrated evidence of remyelination at week 24 among high-dose users, but it did not meet its primary endpoint of active lesions seen on MRI.
In an interview at ACTRIMS Forum 2018, held by the Americas Committee for Treatment and Research in Multiple Sclerosis, study author Robert Glanzman, MD, said that GNbAC1 is a monoclonal antibody that targets and blocks the envelope protein pHER-W ENV, a potent agonist of Toll-like receptor 4. It thereby inhibits TLR4-mediated pathogenicity, which includes activation of macrophages and microglia into proinflammatory phenotypes and direct inhibition of remyelination via TLR4.
In a study known as CHANGE-MS, 270 patients with relapsing-remitting MS were randomized to one of three doses of the GNbAC1 (6, 12, or 18 mg/kg), or placebo via monthly IV infusion over 6 months. The study was conducted at 70 centers in 13 European countries over the past 3 years. It had a 24-week, double-blind, placebo-controlled period, followed by a 24-week, dose-blind, active-only treatment period, with placebo patients randomized to the three different doses of GNbA1C. Brain MRI scans were performed at weeks 12, 16, 20, 24, and 48, to look for evidence of remyelination.
The mean age of patients was 38 years and 65% were female. The researchers observed no safety concerns and no significant effect on inflammatory measures over weeks 12-24, even though the absolute number of lesions was reduced by about 50%. Although the primary endpoint of the cumulative number of gadolinium-enhancing lesions seen on brain MRI scans every 4 weeks during weeks 12-24 was not met, post hoc analyses suggest a decrease in neuroinflammation in the 18 mg/kg GNbA1C group at week 24, compared with placebo (P = .008). “A consistent increase in MT [magnetization transfer] ratio signal was observed in normal-appearing white matter and cerebral cortex at the highest dose, suggesting remyelination,” Dr. Glanzman added. “We gained about a quarter or half of percent in normal-appearing white matter at the cerebral cortex at the high dose. Normally, MS patients lose white matter over time, both in the cortex and in gray matter. We’re actually showing evidence of remyelination, which is really exciting. If these data are replicated and confirmed at week 48, we think we really have an exciting compound.”
GeNeuro sponsored the study.
Full 48-week analyses from CHANGE-MS are expected to be unveiled at the 2018 annual meeting American Academy of Neurology.
SOURCE: Glanzman R et al. Abstract P034.
REPORTING FROM ACTRIMS FORUM 2018
Key clinical point:
Major finding: Although the primary endpoint was not met, post hoc analyses suggest a decrease in neuroinflammation in the 18 mg/kg GNbA1C group at week 24, compared with placebo (P = .008).
Study details: A phase 2 study of 270 patients with relapsing-remitting MS who were randomized to one of three doses of GNbAC1.
Disclosures: Dr. Glanzman is chief medical officer for GeNeuro, which sponsored the study.
Source: Glanzman R et al. Abstract P034.
Long-term effects of ketamine uncertain
LAS VEGAS – Low doses of ketamine, an N-methyl-D-asparate glutamate receptor antagonist, can produce benefits that are unprecedented in the history of treating major depression, according to David Feifel, MD, PhD.
“When have we ever had the ability to be sitting in front of a patient who is extremely suicidal and have an intervention that will work within [an] hour that will remediate that?” he asked at an annual psychopharmacology update held by the Nevada Psychiatric Association. “Ketamine is that tool. If nothing else, that’s what ketamine already presents to us in this field.”
Then there’s the potential for abuse. he asked. “What about other long-term side effects?”
A recent consensus statement authored by Gerard Sanacora, PhD, MD, and associates acknowledged that data on the long-term effects of using ketamine in psychiatry practice are limited or nonexistent (JAMA Psychiatry. 2017 Apr 1;74[4]:399-405), even though an increasing number of clinicians are providing off-label ketamine for depression and other psychiatric disorders. First synthesized in the 1960s, ketamine’s primary site of action in the central nervous system seems to be the thalamocortical projection system, said Dr. Feifel, who has been providing the drug to patients since 2008. In a handout that accompanied his talk, he wrote that ketamine “selectively depresses neuronal function in parts of the cortex and thalamus while stimulating parts of the limbic system, including the hippocampus. This process creates what is termed a functional disorganization of nonspecific pathways in midbrain and thalamic areas.”
Ketamine creates acute subjective experiences that vary with doses, including a sense of “melting into people or things” at lower doses, and visions and hallucinations at higher doses. “Patients will tell me that they deliberately tried to move their hands and feet, to make sure they were still connected to their bodies,” Dr. Feifel said. “There’s often a sensation of moving through space. At higher doses, they often experience a profound sense of connection to all things, an ineffable universal unity that can change their perspective on themselves and their depression. It’s very profound.”
Antidepressant benefits with ketamine are usually dramatic, said Dr. Feifel, who also is founder and director of the Kadima Neuropsychiatry Institute in La Jolla, Calif. The drug is most commonly administered as an IV infusion over a 40 minute period at a dosage of 0.5 mg/kg. It also can be administered orally, intranasally, and intramuscularly. “Patients may achieve response and even remission of depression within a day, even when the depression was previously medication refractory,” he said. “The benefits are usually lost in 3-21 days. Maintenance treatment with ketamine, scheduled once every 2-4 weeks, can maintain the treatment gains. Dissociative and psychotomimetic effects are common but very seldom problematic.”
Dr. Feifel noted that ketamine’s remarkable results have piqued the interest of pharmaceutical companies. “But it is off patent – non proprietary,” he said. “Several novel agents by different pharmaceutical companies quickly have been developed and are in development. Some have modified pharmacology and are claimed to produce less acute dissociative/psychedelic effects. Janssen is developing intranasal esketamine for acutely suicidal patients that has been fast-tracked by the FDA.”
Dr. Feifel reported having no financial disclosures.
LAS VEGAS – Low doses of ketamine, an N-methyl-D-asparate glutamate receptor antagonist, can produce benefits that are unprecedented in the history of treating major depression, according to David Feifel, MD, PhD.
“When have we ever had the ability to be sitting in front of a patient who is extremely suicidal and have an intervention that will work within [an] hour that will remediate that?” he asked at an annual psychopharmacology update held by the Nevada Psychiatric Association. “Ketamine is that tool. If nothing else, that’s what ketamine already presents to us in this field.”
Then there’s the potential for abuse. he asked. “What about other long-term side effects?”
A recent consensus statement authored by Gerard Sanacora, PhD, MD, and associates acknowledged that data on the long-term effects of using ketamine in psychiatry practice are limited or nonexistent (JAMA Psychiatry. 2017 Apr 1;74[4]:399-405), even though an increasing number of clinicians are providing off-label ketamine for depression and other psychiatric disorders. First synthesized in the 1960s, ketamine’s primary site of action in the central nervous system seems to be the thalamocortical projection system, said Dr. Feifel, who has been providing the drug to patients since 2008. In a handout that accompanied his talk, he wrote that ketamine “selectively depresses neuronal function in parts of the cortex and thalamus while stimulating parts of the limbic system, including the hippocampus. This process creates what is termed a functional disorganization of nonspecific pathways in midbrain and thalamic areas.”
Ketamine creates acute subjective experiences that vary with doses, including a sense of “melting into people or things” at lower doses, and visions and hallucinations at higher doses. “Patients will tell me that they deliberately tried to move their hands and feet, to make sure they were still connected to their bodies,” Dr. Feifel said. “There’s often a sensation of moving through space. At higher doses, they often experience a profound sense of connection to all things, an ineffable universal unity that can change their perspective on themselves and their depression. It’s very profound.”
Antidepressant benefits with ketamine are usually dramatic, said Dr. Feifel, who also is founder and director of the Kadima Neuropsychiatry Institute in La Jolla, Calif. The drug is most commonly administered as an IV infusion over a 40 minute period at a dosage of 0.5 mg/kg. It also can be administered orally, intranasally, and intramuscularly. “Patients may achieve response and even remission of depression within a day, even when the depression was previously medication refractory,” he said. “The benefits are usually lost in 3-21 days. Maintenance treatment with ketamine, scheduled once every 2-4 weeks, can maintain the treatment gains. Dissociative and psychotomimetic effects are common but very seldom problematic.”
Dr. Feifel noted that ketamine’s remarkable results have piqued the interest of pharmaceutical companies. “But it is off patent – non proprietary,” he said. “Several novel agents by different pharmaceutical companies quickly have been developed and are in development. Some have modified pharmacology and are claimed to produce less acute dissociative/psychedelic effects. Janssen is developing intranasal esketamine for acutely suicidal patients that has been fast-tracked by the FDA.”
Dr. Feifel reported having no financial disclosures.
LAS VEGAS – Low doses of ketamine, an N-methyl-D-asparate glutamate receptor antagonist, can produce benefits that are unprecedented in the history of treating major depression, according to David Feifel, MD, PhD.
“When have we ever had the ability to be sitting in front of a patient who is extremely suicidal and have an intervention that will work within [an] hour that will remediate that?” he asked at an annual psychopharmacology update held by the Nevada Psychiatric Association. “Ketamine is that tool. If nothing else, that’s what ketamine already presents to us in this field.”
Then there’s the potential for abuse. he asked. “What about other long-term side effects?”
A recent consensus statement authored by Gerard Sanacora, PhD, MD, and associates acknowledged that data on the long-term effects of using ketamine in psychiatry practice are limited or nonexistent (JAMA Psychiatry. 2017 Apr 1;74[4]:399-405), even though an increasing number of clinicians are providing off-label ketamine for depression and other psychiatric disorders. First synthesized in the 1960s, ketamine’s primary site of action in the central nervous system seems to be the thalamocortical projection system, said Dr. Feifel, who has been providing the drug to patients since 2008. In a handout that accompanied his talk, he wrote that ketamine “selectively depresses neuronal function in parts of the cortex and thalamus while stimulating parts of the limbic system, including the hippocampus. This process creates what is termed a functional disorganization of nonspecific pathways in midbrain and thalamic areas.”
Ketamine creates acute subjective experiences that vary with doses, including a sense of “melting into people or things” at lower doses, and visions and hallucinations at higher doses. “Patients will tell me that they deliberately tried to move their hands and feet, to make sure they were still connected to their bodies,” Dr. Feifel said. “There’s often a sensation of moving through space. At higher doses, they often experience a profound sense of connection to all things, an ineffable universal unity that can change their perspective on themselves and their depression. It’s very profound.”
Antidepressant benefits with ketamine are usually dramatic, said Dr. Feifel, who also is founder and director of the Kadima Neuropsychiatry Institute in La Jolla, Calif. The drug is most commonly administered as an IV infusion over a 40 minute period at a dosage of 0.5 mg/kg. It also can be administered orally, intranasally, and intramuscularly. “Patients may achieve response and even remission of depression within a day, even when the depression was previously medication refractory,” he said. “The benefits are usually lost in 3-21 days. Maintenance treatment with ketamine, scheduled once every 2-4 weeks, can maintain the treatment gains. Dissociative and psychotomimetic effects are common but very seldom problematic.”
Dr. Feifel noted that ketamine’s remarkable results have piqued the interest of pharmaceutical companies. “But it is off patent – non proprietary,” he said. “Several novel agents by different pharmaceutical companies quickly have been developed and are in development. Some have modified pharmacology and are claimed to produce less acute dissociative/psychedelic effects. Janssen is developing intranasal esketamine for acutely suicidal patients that has been fast-tracked by the FDA.”
Dr. Feifel reported having no financial disclosures.
REPORTING FROM NPA 2018
Embrace the complexity of marijuana use in adolescents
Las Vegas – When talking with adolescents and their families about marijuana use, Kevin M. Gray, MD, recommends embracing the complexity of the issue.
“Avoid polarizing this topic and avoid vilifying cannabis,” he advised at an annual psychopharmacology update held by the Nevada Psychiatric Association. “Take an interest in what they have to say about cannabis. Work in a gentle, nonconfrontational way where you avoid polarization and find some common ground where you can agree that maybe there’s some good and some bad [about cannabis], but the overwhelming evidence in adolescents is that there’s more harm than good with cannabis use, particularly recreationally.”
Dr. Gray, professor and director of child and adolescent psychiatry at the Medical University of South Carolina, Charleston, acknowledged that clinicians face a delicate balance between risk and benefit, even among Food and Drug Administration–approved medications. However, teens and families may struggle with these nuances, especially in light of the term “medical marijuana.” Some assume that “medical” implies “beneficial.” Others may equate “marijuana” with “natural,” which they may, in turn, equate with being “harmless.”
“Perception is critically important,” Dr. Gray said at an annual psychopharmacology update held by the Nevada Psychiatric Association.
Cannabis initiation typically occurs during adolescence, and rates of initiation and use are increasing. According to Dr. Gray, 55% of U.S. high school seniors have used marijuana, 23% use currently, and 6% use daily. “Those are the ones who have adverse outcomes,” he said. Young users are particularly prone to dependence symptoms and an inability to cut back their use. The odds of meeting criteria for cannabis use disorder are substantially greater in adolescent users than they are in adults regardless of time frame or intensity of use.
“In a dose-dependent manner, adolescent cannabis use is associated with adverse academic, occupational, cognitive, psychiatric, and substance use outcomes,” Dr. Gray said, adding that the average potency of delta-9-tetrahydrocannabinol (THC) in seized cannabis increased from 3% in 1992 to 11% in 2010. “Cannabis use in adolescence is associated with increased incidence and worsened course of psychotic, mood, and anxiety disorders. Serious cannabis-associated risks are well recognized and are particularly striking in adolescents. Adult-onset cannabis users may experience fewer adverse effects.”
Evidence-based psychosocial approaches for adolescents with cannabis use disorder include motivational enhancement therapy, which involves building rapport in a gentle way, with phrasing such as “Tell me what you like about marijuana use” and “What don’t you like about it?” Dr. Gray described motivational enhancement therapy as “a gentle nudge for behavior change” that serves as a bridge to cognitive-behavioral therapy, family therapy, and contingency management. “That said, long-term abstinence outcomes are generally poor,” he said. “People tend to go back to use.”
N-acetylcysteine (NAC) shows promise as a medication for adolescents with cannabis use disorder. NAC activates the cystine/glutamate exchanger and upregulates the GLT-1 receptor, which leads to reduction in reinstatement of drug seeking in animal models. One trial of NAC supported efficacy in 116 cannabis-dependent adolescents (Am J Psychiatry. 2012 Aug;169[8]:805-12). Led by Dr. Gray, the trial consisted of 8 weeks of active treatment on placebo or NAC 1,200 mg BID. All participants received weekly brief cessation counseling and twice-weekly contingency management. The researchers found that adolescents in the NAC group were more than twice as likely to submit a negative urine specimen during treatment than were their counterparts in the placebo group (odds ratio, 2.4; P = .029). In addition, those in the NAC group also were significantly more likely than were those in the placebo group to achieve end-of-treatment abstinence, which was defined as self-reported abstinence confirmed by negative urine testing throughout the last 2 weeks of treatment (OR, 2.3; P = .054).
A similarly designed adult trial indicated that adolescent findings did not translate to adults (Drug Alcohol Depend. 2017 Aug 1;177:249-57). “Whether this may be due to developmental differences in the course and phenomenology of cannabis use disorder, we don’t know,” Dr. Gray said. “For now, NAC remains the only pharmacotherapy with positive published intent-to-treat clinical trial abstinence findings for cannabis use disorder in adolescents. Positive adolescent findings must be replicated, but the necessary behavioral treatment platform must be clarified to translate successfully to real-world practice.”
Dr. Gray disclosed that he receives research funding from the National Institutes of Health.
[email protected]
Las Vegas – When talking with adolescents and their families about marijuana use, Kevin M. Gray, MD, recommends embracing the complexity of the issue.
“Avoid polarizing this topic and avoid vilifying cannabis,” he advised at an annual psychopharmacology update held by the Nevada Psychiatric Association. “Take an interest in what they have to say about cannabis. Work in a gentle, nonconfrontational way where you avoid polarization and find some common ground where you can agree that maybe there’s some good and some bad [about cannabis], but the overwhelming evidence in adolescents is that there’s more harm than good with cannabis use, particularly recreationally.”
Dr. Gray, professor and director of child and adolescent psychiatry at the Medical University of South Carolina, Charleston, acknowledged that clinicians face a delicate balance between risk and benefit, even among Food and Drug Administration–approved medications. However, teens and families may struggle with these nuances, especially in light of the term “medical marijuana.” Some assume that “medical” implies “beneficial.” Others may equate “marijuana” with “natural,” which they may, in turn, equate with being “harmless.”
“Perception is critically important,” Dr. Gray said at an annual psychopharmacology update held by the Nevada Psychiatric Association.
Cannabis initiation typically occurs during adolescence, and rates of initiation and use are increasing. According to Dr. Gray, 55% of U.S. high school seniors have used marijuana, 23% use currently, and 6% use daily. “Those are the ones who have adverse outcomes,” he said. Young users are particularly prone to dependence symptoms and an inability to cut back their use. The odds of meeting criteria for cannabis use disorder are substantially greater in adolescent users than they are in adults regardless of time frame or intensity of use.
“In a dose-dependent manner, adolescent cannabis use is associated with adverse academic, occupational, cognitive, psychiatric, and substance use outcomes,” Dr. Gray said, adding that the average potency of delta-9-tetrahydrocannabinol (THC) in seized cannabis increased from 3% in 1992 to 11% in 2010. “Cannabis use in adolescence is associated with increased incidence and worsened course of psychotic, mood, and anxiety disorders. Serious cannabis-associated risks are well recognized and are particularly striking in adolescents. Adult-onset cannabis users may experience fewer adverse effects.”
Evidence-based psychosocial approaches for adolescents with cannabis use disorder include motivational enhancement therapy, which involves building rapport in a gentle way, with phrasing such as “Tell me what you like about marijuana use” and “What don’t you like about it?” Dr. Gray described motivational enhancement therapy as “a gentle nudge for behavior change” that serves as a bridge to cognitive-behavioral therapy, family therapy, and contingency management. “That said, long-term abstinence outcomes are generally poor,” he said. “People tend to go back to use.”
N-acetylcysteine (NAC) shows promise as a medication for adolescents with cannabis use disorder. NAC activates the cystine/glutamate exchanger and upregulates the GLT-1 receptor, which leads to reduction in reinstatement of drug seeking in animal models. One trial of NAC supported efficacy in 116 cannabis-dependent adolescents (Am J Psychiatry. 2012 Aug;169[8]:805-12). Led by Dr. Gray, the trial consisted of 8 weeks of active treatment on placebo or NAC 1,200 mg BID. All participants received weekly brief cessation counseling and twice-weekly contingency management. The researchers found that adolescents in the NAC group were more than twice as likely to submit a negative urine specimen during treatment than were their counterparts in the placebo group (odds ratio, 2.4; P = .029). In addition, those in the NAC group also were significantly more likely than were those in the placebo group to achieve end-of-treatment abstinence, which was defined as self-reported abstinence confirmed by negative urine testing throughout the last 2 weeks of treatment (OR, 2.3; P = .054).
A similarly designed adult trial indicated that adolescent findings did not translate to adults (Drug Alcohol Depend. 2017 Aug 1;177:249-57). “Whether this may be due to developmental differences in the course and phenomenology of cannabis use disorder, we don’t know,” Dr. Gray said. “For now, NAC remains the only pharmacotherapy with positive published intent-to-treat clinical trial abstinence findings for cannabis use disorder in adolescents. Positive adolescent findings must be replicated, but the necessary behavioral treatment platform must be clarified to translate successfully to real-world practice.”
Dr. Gray disclosed that he receives research funding from the National Institutes of Health.
[email protected]
Las Vegas – When talking with adolescents and their families about marijuana use, Kevin M. Gray, MD, recommends embracing the complexity of the issue.
“Avoid polarizing this topic and avoid vilifying cannabis,” he advised at an annual psychopharmacology update held by the Nevada Psychiatric Association. “Take an interest in what they have to say about cannabis. Work in a gentle, nonconfrontational way where you avoid polarization and find some common ground where you can agree that maybe there’s some good and some bad [about cannabis], but the overwhelming evidence in adolescents is that there’s more harm than good with cannabis use, particularly recreationally.”
Dr. Gray, professor and director of child and adolescent psychiatry at the Medical University of South Carolina, Charleston, acknowledged that clinicians face a delicate balance between risk and benefit, even among Food and Drug Administration–approved medications. However, teens and families may struggle with these nuances, especially in light of the term “medical marijuana.” Some assume that “medical” implies “beneficial.” Others may equate “marijuana” with “natural,” which they may, in turn, equate with being “harmless.”
“Perception is critically important,” Dr. Gray said at an annual psychopharmacology update held by the Nevada Psychiatric Association.
Cannabis initiation typically occurs during adolescence, and rates of initiation and use are increasing. According to Dr. Gray, 55% of U.S. high school seniors have used marijuana, 23% use currently, and 6% use daily. “Those are the ones who have adverse outcomes,” he said. Young users are particularly prone to dependence symptoms and an inability to cut back their use. The odds of meeting criteria for cannabis use disorder are substantially greater in adolescent users than they are in adults regardless of time frame or intensity of use.
“In a dose-dependent manner, adolescent cannabis use is associated with adverse academic, occupational, cognitive, psychiatric, and substance use outcomes,” Dr. Gray said, adding that the average potency of delta-9-tetrahydrocannabinol (THC) in seized cannabis increased from 3% in 1992 to 11% in 2010. “Cannabis use in adolescence is associated with increased incidence and worsened course of psychotic, mood, and anxiety disorders. Serious cannabis-associated risks are well recognized and are particularly striking in adolescents. Adult-onset cannabis users may experience fewer adverse effects.”
Evidence-based psychosocial approaches for adolescents with cannabis use disorder include motivational enhancement therapy, which involves building rapport in a gentle way, with phrasing such as “Tell me what you like about marijuana use” and “What don’t you like about it?” Dr. Gray described motivational enhancement therapy as “a gentle nudge for behavior change” that serves as a bridge to cognitive-behavioral therapy, family therapy, and contingency management. “That said, long-term abstinence outcomes are generally poor,” he said. “People tend to go back to use.”
N-acetylcysteine (NAC) shows promise as a medication for adolescents with cannabis use disorder. NAC activates the cystine/glutamate exchanger and upregulates the GLT-1 receptor, which leads to reduction in reinstatement of drug seeking in animal models. One trial of NAC supported efficacy in 116 cannabis-dependent adolescents (Am J Psychiatry. 2012 Aug;169[8]:805-12). Led by Dr. Gray, the trial consisted of 8 weeks of active treatment on placebo or NAC 1,200 mg BID. All participants received weekly brief cessation counseling and twice-weekly contingency management. The researchers found that adolescents in the NAC group were more than twice as likely to submit a negative urine specimen during treatment than were their counterparts in the placebo group (odds ratio, 2.4; P = .029). In addition, those in the NAC group also were significantly more likely than were those in the placebo group to achieve end-of-treatment abstinence, which was defined as self-reported abstinence confirmed by negative urine testing throughout the last 2 weeks of treatment (OR, 2.3; P = .054).
A similarly designed adult trial indicated that adolescent findings did not translate to adults (Drug Alcohol Depend. 2017 Aug 1;177:249-57). “Whether this may be due to developmental differences in the course and phenomenology of cannabis use disorder, we don’t know,” Dr. Gray said. “For now, NAC remains the only pharmacotherapy with positive published intent-to-treat clinical trial abstinence findings for cannabis use disorder in adolescents. Positive adolescent findings must be replicated, but the necessary behavioral treatment platform must be clarified to translate successfully to real-world practice.”
Dr. Gray disclosed that he receives research funding from the National Institutes of Health.
[email protected]
REPORTING FROM NPA 2018
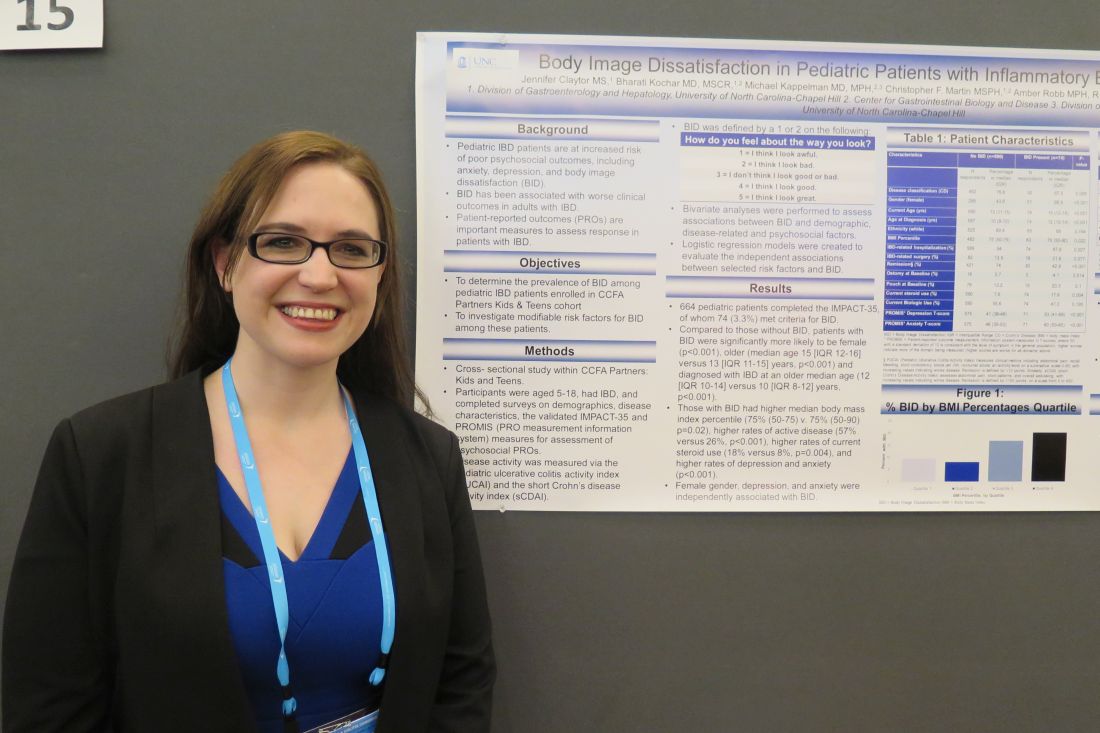
Expert shares tips for positioning biologics in IBD patient treatment
LAS VEGAS – In the clinical opinion of Edward V. Loftus Jr., MD, biologics for inflammatory bowel disease (IBD) patients are best positioned based on age, personal medical history, and the presence of extraintestinal manifestations.
“ and is the way to go if you’re trying to change the trajectory of illness,” Dr. Loftus said at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
In general, patients who are younger at diagnosis are going to have more severe disease than patients diagnosed older, said Dr. Loftus, professor of medicine at the Mayo Clinic, Rochester, Minn. “For CD [Crohn’s disease], the presence of fistulizing disease, especially internal fistulas, and to a lesser extent perianal fistulas, and then the presence of small-bowel disease or proximal GI disease, are all harbingers of more aggressive disease,” he said. “Multiple studies show that the time interval between diagnosis and development of intestinal complications is shorter in patients with small-bowel disease relative to colonic disease. When you add up those factors, you’re talking about 70% of CD patients, if not more. Most Crohn’s patients are going to be high-risk patients.”
For ulcerative colitis (UC), being male is a risk factor for hospitalization, surgery, and for developing colon cancer. On average, males are twice as likely as females to require surgery, and they’re twice as likely to develop colon cancer. Other predictors in UC for high-risk disease include early need for hospitalization, early need for corticosteroids, and extensive colitis at diagnosis. “You’re thinking about these things because how you’re going to treat these patients is going to differ,” he said.
According to Dr. Loftus, aminosalicylate (5-ASA) drugs are the frontline drugs of choice for low-risk UC patients with mild symptoms. “If they’re having moderate symptoms, you might initially start with a corticosteroid taper,” he noted. “That can be either prednisone or budesonide MMX. In a patient with really active symptoms, they’re going to go to IV steroids or maybe directly to anti-TNF [tumor necrosis factor] therapy.” For low-risk CD patients, consider budesonide taper then observation. “If they don’t flare again, maybe monitor that patient periodically,” he advised. “For high-risk patients, consider biologic therapy with or without thiopurine or methotrexate.”
A recent analysis of Medicare and Medicaid data from 2006 to 2013 found a significantly higher rate of mortality in IBD patients treated with prolonged corticosteroids than that seen in those treated with anti-TNF therapy (Am J Gastroenterol. Jan 16, 2018. doi: 10.1038/ajg2017.479). “That should give you pause,” Dr. Loftus said. “Don’t just put your patient on prednisone because you think it’s the easiest and safest thing to do. It’s not. It’s much more dangerous and has implications [for] the patient’s life expectancy.”
Some data are beginning to emerge about the use of biosimilars in IBD, mostly from Europe. Investigators of one randomized, controlled trial of biosimilar CT-P13 vs. originator infliximab in CD presented at the 2017 Digestive Disease Week meeting; they found in their trial that at week 6 all clinical endpoints were similar between the two agents. “If you’re forced to change your patient to this particular biosimilar, I wouldn’t be too worried about it,” Dr. Loftus said. “Of course, I’m not necessarily going to switch unless my institution or a particular third-party payer mandate it.”
In a published study funded by the Norwegian government, researchers conducted a prospective trial of switching from infliximab to CT-P13 in patients with a variety of conditions (Lancet. 2017;389:2304-16). Overall, the clinical failure rate was the same for both agents. Among CD patients, the researchers observed a nonsignificant trend toward disease worsening among those on the biosimilar, “but there was essentially no difference,” Dr. Loftus said.
He went on to discuss vedolizumab, a monoclonal antibody to alpha4beta7 integrin approved in 2014 for patients with moderate to severely active UC or CD. Phase 3 data from GEMINI I in moderate to severe UC found that relevant clinical endpoints were met by week 6 and they persisted at week 52 at both doses (N Engl J Med. 2013;369[8]:699-710). “For CD, the use of vedolizumab is a bit of a mixed picture,” Dr. Loftus said. “In GEMINI II, some of the primary endpoints were met at week 6, but at least one was missed (N Engl J Med. 2013;369[8]:711-21). The same thing was seen in GEMINI III. There’s a sense here that vedolizumab takes a little bit longer to work in CD.”
Integrated safety analyses of the GEMINI trials found no signal for increased rates of serious adverse events, and no cases of progressive multifocal leukoencephalopathy have been reported (J Crohns Colitis. 2017;11[2]:185-90). “The risk factors for serious infections were prior anti-TNF failure and opioid analgesic use in UC patients and younger age, steroid use, and opioid analgesic use in CD patients,” Dr. Loftus said.
In a trial of CD patients failing anti-TNF therapy, researchers observed a robust clinical response with ustekinumab, compared with placebo, at week 6 (N Engl J Med. 2016;375:1946-60). Even greater effects were observed in UNITI-2, a trial of ustekinumab in CD patients who hadn’t failed anti-TNFs.
Dr. Loftus cautioned that elderly and immunocompromised patients face an increased risk for infections when they’re placed on anti-TNF therapy. At the same time, researchers used a French database to determine the risk of lymphoma in IBD patients stratified by medication. For patients unexposed to such therapies, the risk of lymphoma was 1:4,000. For patients on thiopurine monotherapy, the risk was about 1:2,000; it was about 1:2,500 for those on anti-TNF monotherapy and about 1:1,000 for those on combination therapy (JAMA. 2017;318:1679-86). “One of the messages in this study is we can reassure our more risk-averse patients that the absolute risk of lymphoma is very low, even among patients on combination therapy,” he said.
Dr. Loftus called for head-to-head trials comparing the individual biologic agents and shared his recommendations on how to position currently available therapies. “I would say that for the average ‘bread and butter’ Crohn’s patient, anti-TNF therapy is the way to go,” he said. “For perianal fistulizing patients, I’m going to go with anti-TNF therapy, such as infliximab or adalimumab. For a patient with active extraintestinal manifestations, such as spondyloarthropathy, uveitis, and pyoderma, anti-TNF therapy is the way to go. However, with an elderly or immunosuppressed patient, consider vedolizumab or ustekinumab. For patients with a personal history of malignancy, an anti-TNF is very reasonable, but it may be easier to convince them to consider vedolizumab or ustekinumab.”
Recommendations for UC are largely similar, he continued. “However, I think we have enough data from GEMINI I and the integrated safety data with vedolizumab to say that, for the average ‘bread and butter’ UC patient, anti-TNF therapy or vedolizumab are appropriate. For a patient with extraintestinal manifestations I would avoid vedolizumab initially and try anti-TNF therapy. For patients with acute severe colitis, we have the bulk of evidence for efficacy resting with infliximab, so I would go with that. For the elderly or immunosuppressed patient, I would go with vedolizumab. For the person with a history of malignancy, an anti-TNF agent is reasonable, but consider vedolizumab.”
Dr. Loftus disclosed that he has consulted for AbbVie, Takeda Pharmaceutical, Janssen Pharmaceutica, UCB, Pfizer, Amgen, Eli Lilly, Celltrion Healthcare, Napo Pharmaceuticals. He has also received research support from AbbVie, Takeda Pharmaceutical, Janssen Pharmaceutica, UCB, Pfizer, Amgen, Genentech, Seres Pharmaceuticals, MedImmune, Allergan, and Robarts Clinical Trials.
*This story was updated on 3/26.
LAS VEGAS – In the clinical opinion of Edward V. Loftus Jr., MD, biologics for inflammatory bowel disease (IBD) patients are best positioned based on age, personal medical history, and the presence of extraintestinal manifestations.
“ and is the way to go if you’re trying to change the trajectory of illness,” Dr. Loftus said at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
In general, patients who are younger at diagnosis are going to have more severe disease than patients diagnosed older, said Dr. Loftus, professor of medicine at the Mayo Clinic, Rochester, Minn. “For CD [Crohn’s disease], the presence of fistulizing disease, especially internal fistulas, and to a lesser extent perianal fistulas, and then the presence of small-bowel disease or proximal GI disease, are all harbingers of more aggressive disease,” he said. “Multiple studies show that the time interval between diagnosis and development of intestinal complications is shorter in patients with small-bowel disease relative to colonic disease. When you add up those factors, you’re talking about 70% of CD patients, if not more. Most Crohn’s patients are going to be high-risk patients.”
For ulcerative colitis (UC), being male is a risk factor for hospitalization, surgery, and for developing colon cancer. On average, males are twice as likely as females to require surgery, and they’re twice as likely to develop colon cancer. Other predictors in UC for high-risk disease include early need for hospitalization, early need for corticosteroids, and extensive colitis at diagnosis. “You’re thinking about these things because how you’re going to treat these patients is going to differ,” he said.
According to Dr. Loftus, aminosalicylate (5-ASA) drugs are the frontline drugs of choice for low-risk UC patients with mild symptoms. “If they’re having moderate symptoms, you might initially start with a corticosteroid taper,” he noted. “That can be either prednisone or budesonide MMX. In a patient with really active symptoms, they’re going to go to IV steroids or maybe directly to anti-TNF [tumor necrosis factor] therapy.” For low-risk CD patients, consider budesonide taper then observation. “If they don’t flare again, maybe monitor that patient periodically,” he advised. “For high-risk patients, consider biologic therapy with or without thiopurine or methotrexate.”
A recent analysis of Medicare and Medicaid data from 2006 to 2013 found a significantly higher rate of mortality in IBD patients treated with prolonged corticosteroids than that seen in those treated with anti-TNF therapy (Am J Gastroenterol. Jan 16, 2018. doi: 10.1038/ajg2017.479). “That should give you pause,” Dr. Loftus said. “Don’t just put your patient on prednisone because you think it’s the easiest and safest thing to do. It’s not. It’s much more dangerous and has implications [for] the patient’s life expectancy.”
Some data are beginning to emerge about the use of biosimilars in IBD, mostly from Europe. Investigators of one randomized, controlled trial of biosimilar CT-P13 vs. originator infliximab in CD presented at the 2017 Digestive Disease Week meeting; they found in their trial that at week 6 all clinical endpoints were similar between the two agents. “If you’re forced to change your patient to this particular biosimilar, I wouldn’t be too worried about it,” Dr. Loftus said. “Of course, I’m not necessarily going to switch unless my institution or a particular third-party payer mandate it.”
In a published study funded by the Norwegian government, researchers conducted a prospective trial of switching from infliximab to CT-P13 in patients with a variety of conditions (Lancet. 2017;389:2304-16). Overall, the clinical failure rate was the same for both agents. Among CD patients, the researchers observed a nonsignificant trend toward disease worsening among those on the biosimilar, “but there was essentially no difference,” Dr. Loftus said.
He went on to discuss vedolizumab, a monoclonal antibody to alpha4beta7 integrin approved in 2014 for patients with moderate to severely active UC or CD. Phase 3 data from GEMINI I in moderate to severe UC found that relevant clinical endpoints were met by week 6 and they persisted at week 52 at both doses (N Engl J Med. 2013;369[8]:699-710). “For CD, the use of vedolizumab is a bit of a mixed picture,” Dr. Loftus said. “In GEMINI II, some of the primary endpoints were met at week 6, but at least one was missed (N Engl J Med. 2013;369[8]:711-21). The same thing was seen in GEMINI III. There’s a sense here that vedolizumab takes a little bit longer to work in CD.”
Integrated safety analyses of the GEMINI trials found no signal for increased rates of serious adverse events, and no cases of progressive multifocal leukoencephalopathy have been reported (J Crohns Colitis. 2017;11[2]:185-90). “The risk factors for serious infections were prior anti-TNF failure and opioid analgesic use in UC patients and younger age, steroid use, and opioid analgesic use in CD patients,” Dr. Loftus said.
In a trial of CD patients failing anti-TNF therapy, researchers observed a robust clinical response with ustekinumab, compared with placebo, at week 6 (N Engl J Med. 2016;375:1946-60). Even greater effects were observed in UNITI-2, a trial of ustekinumab in CD patients who hadn’t failed anti-TNFs.
Dr. Loftus cautioned that elderly and immunocompromised patients face an increased risk for infections when they’re placed on anti-TNF therapy. At the same time, researchers used a French database to determine the risk of lymphoma in IBD patients stratified by medication. For patients unexposed to such therapies, the risk of lymphoma was 1:4,000. For patients on thiopurine monotherapy, the risk was about 1:2,000; it was about 1:2,500 for those on anti-TNF monotherapy and about 1:1,000 for those on combination therapy (JAMA. 2017;318:1679-86). “One of the messages in this study is we can reassure our more risk-averse patients that the absolute risk of lymphoma is very low, even among patients on combination therapy,” he said.
Dr. Loftus called for head-to-head trials comparing the individual biologic agents and shared his recommendations on how to position currently available therapies. “I would say that for the average ‘bread and butter’ Crohn’s patient, anti-TNF therapy is the way to go,” he said. “For perianal fistulizing patients, I’m going to go with anti-TNF therapy, such as infliximab or adalimumab. For a patient with active extraintestinal manifestations, such as spondyloarthropathy, uveitis, and pyoderma, anti-TNF therapy is the way to go. However, with an elderly or immunosuppressed patient, consider vedolizumab or ustekinumab. For patients with a personal history of malignancy, an anti-TNF is very reasonable, but it may be easier to convince them to consider vedolizumab or ustekinumab.”
Recommendations for UC are largely similar, he continued. “However, I think we have enough data from GEMINI I and the integrated safety data with vedolizumab to say that, for the average ‘bread and butter’ UC patient, anti-TNF therapy or vedolizumab are appropriate. For a patient with extraintestinal manifestations I would avoid vedolizumab initially and try anti-TNF therapy. For patients with acute severe colitis, we have the bulk of evidence for efficacy resting with infliximab, so I would go with that. For the elderly or immunosuppressed patient, I would go with vedolizumab. For the person with a history of malignancy, an anti-TNF agent is reasonable, but consider vedolizumab.”
Dr. Loftus disclosed that he has consulted for AbbVie, Takeda Pharmaceutical, Janssen Pharmaceutica, UCB, Pfizer, Amgen, Eli Lilly, Celltrion Healthcare, Napo Pharmaceuticals. He has also received research support from AbbVie, Takeda Pharmaceutical, Janssen Pharmaceutica, UCB, Pfizer, Amgen, Genentech, Seres Pharmaceuticals, MedImmune, Allergan, and Robarts Clinical Trials.
*This story was updated on 3/26.
LAS VEGAS – In the clinical opinion of Edward V. Loftus Jr., MD, biologics for inflammatory bowel disease (IBD) patients are best positioned based on age, personal medical history, and the presence of extraintestinal manifestations.
“ and is the way to go if you’re trying to change the trajectory of illness,” Dr. Loftus said at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
In general, patients who are younger at diagnosis are going to have more severe disease than patients diagnosed older, said Dr. Loftus, professor of medicine at the Mayo Clinic, Rochester, Minn. “For CD [Crohn’s disease], the presence of fistulizing disease, especially internal fistulas, and to a lesser extent perianal fistulas, and then the presence of small-bowel disease or proximal GI disease, are all harbingers of more aggressive disease,” he said. “Multiple studies show that the time interval between diagnosis and development of intestinal complications is shorter in patients with small-bowel disease relative to colonic disease. When you add up those factors, you’re talking about 70% of CD patients, if not more. Most Crohn’s patients are going to be high-risk patients.”
For ulcerative colitis (UC), being male is a risk factor for hospitalization, surgery, and for developing colon cancer. On average, males are twice as likely as females to require surgery, and they’re twice as likely to develop colon cancer. Other predictors in UC for high-risk disease include early need for hospitalization, early need for corticosteroids, and extensive colitis at diagnosis. “You’re thinking about these things because how you’re going to treat these patients is going to differ,” he said.
According to Dr. Loftus, aminosalicylate (5-ASA) drugs are the frontline drugs of choice for low-risk UC patients with mild symptoms. “If they’re having moderate symptoms, you might initially start with a corticosteroid taper,” he noted. “That can be either prednisone or budesonide MMX. In a patient with really active symptoms, they’re going to go to IV steroids or maybe directly to anti-TNF [tumor necrosis factor] therapy.” For low-risk CD patients, consider budesonide taper then observation. “If they don’t flare again, maybe monitor that patient periodically,” he advised. “For high-risk patients, consider biologic therapy with or without thiopurine or methotrexate.”
A recent analysis of Medicare and Medicaid data from 2006 to 2013 found a significantly higher rate of mortality in IBD patients treated with prolonged corticosteroids than that seen in those treated with anti-TNF therapy (Am J Gastroenterol. Jan 16, 2018. doi: 10.1038/ajg2017.479). “That should give you pause,” Dr. Loftus said. “Don’t just put your patient on prednisone because you think it’s the easiest and safest thing to do. It’s not. It’s much more dangerous and has implications [for] the patient’s life expectancy.”
Some data are beginning to emerge about the use of biosimilars in IBD, mostly from Europe. Investigators of one randomized, controlled trial of biosimilar CT-P13 vs. originator infliximab in CD presented at the 2017 Digestive Disease Week meeting; they found in their trial that at week 6 all clinical endpoints were similar between the two agents. “If you’re forced to change your patient to this particular biosimilar, I wouldn’t be too worried about it,” Dr. Loftus said. “Of course, I’m not necessarily going to switch unless my institution or a particular third-party payer mandate it.”
In a published study funded by the Norwegian government, researchers conducted a prospective trial of switching from infliximab to CT-P13 in patients with a variety of conditions (Lancet. 2017;389:2304-16). Overall, the clinical failure rate was the same for both agents. Among CD patients, the researchers observed a nonsignificant trend toward disease worsening among those on the biosimilar, “but there was essentially no difference,” Dr. Loftus said.
He went on to discuss vedolizumab, a monoclonal antibody to alpha4beta7 integrin approved in 2014 for patients with moderate to severely active UC or CD. Phase 3 data from GEMINI I in moderate to severe UC found that relevant clinical endpoints were met by week 6 and they persisted at week 52 at both doses (N Engl J Med. 2013;369[8]:699-710). “For CD, the use of vedolizumab is a bit of a mixed picture,” Dr. Loftus said. “In GEMINI II, some of the primary endpoints were met at week 6, but at least one was missed (N Engl J Med. 2013;369[8]:711-21). The same thing was seen in GEMINI III. There’s a sense here that vedolizumab takes a little bit longer to work in CD.”
Integrated safety analyses of the GEMINI trials found no signal for increased rates of serious adverse events, and no cases of progressive multifocal leukoencephalopathy have been reported (J Crohns Colitis. 2017;11[2]:185-90). “The risk factors for serious infections were prior anti-TNF failure and opioid analgesic use in UC patients and younger age, steroid use, and opioid analgesic use in CD patients,” Dr. Loftus said.
In a trial of CD patients failing anti-TNF therapy, researchers observed a robust clinical response with ustekinumab, compared with placebo, at week 6 (N Engl J Med. 2016;375:1946-60). Even greater effects were observed in UNITI-2, a trial of ustekinumab in CD patients who hadn’t failed anti-TNFs.
Dr. Loftus cautioned that elderly and immunocompromised patients face an increased risk for infections when they’re placed on anti-TNF therapy. At the same time, researchers used a French database to determine the risk of lymphoma in IBD patients stratified by medication. For patients unexposed to such therapies, the risk of lymphoma was 1:4,000. For patients on thiopurine monotherapy, the risk was about 1:2,000; it was about 1:2,500 for those on anti-TNF monotherapy and about 1:1,000 for those on combination therapy (JAMA. 2017;318:1679-86). “One of the messages in this study is we can reassure our more risk-averse patients that the absolute risk of lymphoma is very low, even among patients on combination therapy,” he said.
Dr. Loftus called for head-to-head trials comparing the individual biologic agents and shared his recommendations on how to position currently available therapies. “I would say that for the average ‘bread and butter’ Crohn’s patient, anti-TNF therapy is the way to go,” he said. “For perianal fistulizing patients, I’m going to go with anti-TNF therapy, such as infliximab or adalimumab. For a patient with active extraintestinal manifestations, such as spondyloarthropathy, uveitis, and pyoderma, anti-TNF therapy is the way to go. However, with an elderly or immunosuppressed patient, consider vedolizumab or ustekinumab. For patients with a personal history of malignancy, an anti-TNF is very reasonable, but it may be easier to convince them to consider vedolizumab or ustekinumab.”
Recommendations for UC are largely similar, he continued. “However, I think we have enough data from GEMINI I and the integrated safety data with vedolizumab to say that, for the average ‘bread and butter’ UC patient, anti-TNF therapy or vedolizumab are appropriate. For a patient with extraintestinal manifestations I would avoid vedolizumab initially and try anti-TNF therapy. For patients with acute severe colitis, we have the bulk of evidence for efficacy resting with infliximab, so I would go with that. For the elderly or immunosuppressed patient, I would go with vedolizumab. For the person with a history of malignancy, an anti-TNF agent is reasonable, but consider vedolizumab.”
Dr. Loftus disclosed that he has consulted for AbbVie, Takeda Pharmaceutical, Janssen Pharmaceutica, UCB, Pfizer, Amgen, Eli Lilly, Celltrion Healthcare, Napo Pharmaceuticals. He has also received research support from AbbVie, Takeda Pharmaceutical, Janssen Pharmaceutica, UCB, Pfizer, Amgen, Genentech, Seres Pharmaceuticals, MedImmune, Allergan, and Robarts Clinical Trials.
*This story was updated on 3/26.
EXPERT ANALYSIS FROM THE CROHN’S & COLITIS CONGRESS
Study identifies characteristics that may constitute the MS prodrome
SAN DIEGO – Compared with controls, patients who developed MS were more frequently admitted to the hospital or visited a physician for problems related to the nervous system, sensory organs, musculoskeletal system, and genitourinary system in the 5 years prior to MS onset, a multicenter matched cohort study found.
“People are seeking help for different conditions that are most likely related to their MS,” one of the study authors, Elaine Kingwell, PhD, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “It suggests there could be opportunity to recognize and possibly diagnose and treat MS earlier.”
In a previously published study (Lancet Neurol. 2017;16[6]:445-51) led by Helen Tremlett, PhD, and first author Jose Wijnands, PhD, the team found increased health care utilization in people with MS across all health sectors – physician, hospital, and pharmacy (prescriptions filled).
For the current study, the team set out to identify early signs and symptoms that could define the MS prodrome. “We wanted to know why people went to the hospital, why people went to their physician, what kind of drugs they were prescribed, and what kind of specialists they saw,” explained Dr. Kingwell, an epidemiologist in the department of neurology at the University of British Columbia, Vancouver.
The researchers used health administrative and MS-specific data from four Canadian provinces to conduct a multicenter matched cohort study. Individuals were required to be in the province from 5 years pre-index date, measured as either the first demyelinating event in health administrative data or MS onset as determined by the treating neurologist, until the MS cases’ third demyelinating claim or diagnosis date. The potential for a prodromal period was examined in the 5 years pre-index date, and outcomes of interest were number of physician and hospital encounters per ICD-10 chapter, number of physician encounters per physician specialty, and percentage of people with one or more filled prescription per drug class.
The researchers used rate ratios and 95% confidence intervals to compare the rates of physician and hospital encounters between MS cases and controls and the proportion test to compare the percentage of people with one or more filled prescriptions between MS cases and controls. They used random-effects meta-analyses to pool results across Canadian provinces.
The population consisted of 13,951 MS patients and 66,940 controls derived from a health administration cohort and 3,202 MS patients and 16,006 controls derived from MS clinics. Compared with controls, in the 5 years before the first demyelinating claim or symptom onset, cases had more physician and hospital encounters for the nervous system (rate ratio = 1.70-4.75), sensory organs (RR = 1.40-2.28), musculoskeletal system (RR = 1.19-1.70), and genitourinary system (RR = 1.17-1.59), Dr. Kingwell and her associates reported.
Cases also had more encounters with psychiatrists (RR = 1.48-1.66) and urologists (RR = 1.49-1.80), and a higher proportion of filled prescriptions for hormonal preparations and drugs related to the musculoskeletal or genitourinary systems (ranging from 1.1 to 1.5 times higher; P less than .02 for all associations). “While we did not examine each individual drug, we did group drugs by their therapeutic class,” Dr. Wijnands noted in an interview after the meeting. “As for the increased number of visits to psychiatrists, it is intriguing. We don’t necessarily know all the reasons why. It opens up a lot of questions for people to follow up on.”
In contrast, MS cases had fewer pregnancy-related encounters, compared with controls (RR = 0.78-0.88).
Dr. Wijnands acknowledged certain limitations of the study, including its reliance on administrative data to measure the prodromal period. “When we described the prodrome itself, we relied on ICD codes from the physician and hospital data as well as prescriptions filled. Issues or problems for which individuals do not seek medical attention, for instance, would not be captured in our study,” she said.
The study was funded by the National MS Society. Dr. Wijnands receives salary support from the Michael Smith Foundation for Health Research /The Koehle Family Foundation, coauthor Ruth Ann Marrie, MD, PhD, holds the Waugh Family Chair in Multiple Sclerosis, and Dr. Tremlett is funded by the Canada Research Chair Program. Dr. Kingwell reported having no financial disclosures.
[email protected]
SOURCE: Kingwell E et al. ACTRIMS Forum 2018, late-breaking poster 254.
SAN DIEGO – Compared with controls, patients who developed MS were more frequently admitted to the hospital or visited a physician for problems related to the nervous system, sensory organs, musculoskeletal system, and genitourinary system in the 5 years prior to MS onset, a multicenter matched cohort study found.
“People are seeking help for different conditions that are most likely related to their MS,” one of the study authors, Elaine Kingwell, PhD, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “It suggests there could be opportunity to recognize and possibly diagnose and treat MS earlier.”
In a previously published study (Lancet Neurol. 2017;16[6]:445-51) led by Helen Tremlett, PhD, and first author Jose Wijnands, PhD, the team found increased health care utilization in people with MS across all health sectors – physician, hospital, and pharmacy (prescriptions filled).
For the current study, the team set out to identify early signs and symptoms that could define the MS prodrome. “We wanted to know why people went to the hospital, why people went to their physician, what kind of drugs they were prescribed, and what kind of specialists they saw,” explained Dr. Kingwell, an epidemiologist in the department of neurology at the University of British Columbia, Vancouver.
The researchers used health administrative and MS-specific data from four Canadian provinces to conduct a multicenter matched cohort study. Individuals were required to be in the province from 5 years pre-index date, measured as either the first demyelinating event in health administrative data or MS onset as determined by the treating neurologist, until the MS cases’ third demyelinating claim or diagnosis date. The potential for a prodromal period was examined in the 5 years pre-index date, and outcomes of interest were number of physician and hospital encounters per ICD-10 chapter, number of physician encounters per physician specialty, and percentage of people with one or more filled prescription per drug class.
The researchers used rate ratios and 95% confidence intervals to compare the rates of physician and hospital encounters between MS cases and controls and the proportion test to compare the percentage of people with one or more filled prescriptions between MS cases and controls. They used random-effects meta-analyses to pool results across Canadian provinces.
The population consisted of 13,951 MS patients and 66,940 controls derived from a health administration cohort and 3,202 MS patients and 16,006 controls derived from MS clinics. Compared with controls, in the 5 years before the first demyelinating claim or symptom onset, cases had more physician and hospital encounters for the nervous system (rate ratio = 1.70-4.75), sensory organs (RR = 1.40-2.28), musculoskeletal system (RR = 1.19-1.70), and genitourinary system (RR = 1.17-1.59), Dr. Kingwell and her associates reported.
Cases also had more encounters with psychiatrists (RR = 1.48-1.66) and urologists (RR = 1.49-1.80), and a higher proportion of filled prescriptions for hormonal preparations and drugs related to the musculoskeletal or genitourinary systems (ranging from 1.1 to 1.5 times higher; P less than .02 for all associations). “While we did not examine each individual drug, we did group drugs by their therapeutic class,” Dr. Wijnands noted in an interview after the meeting. “As for the increased number of visits to psychiatrists, it is intriguing. We don’t necessarily know all the reasons why. It opens up a lot of questions for people to follow up on.”
In contrast, MS cases had fewer pregnancy-related encounters, compared with controls (RR = 0.78-0.88).
Dr. Wijnands acknowledged certain limitations of the study, including its reliance on administrative data to measure the prodromal period. “When we described the prodrome itself, we relied on ICD codes from the physician and hospital data as well as prescriptions filled. Issues or problems for which individuals do not seek medical attention, for instance, would not be captured in our study,” she said.
The study was funded by the National MS Society. Dr. Wijnands receives salary support from the Michael Smith Foundation for Health Research /The Koehle Family Foundation, coauthor Ruth Ann Marrie, MD, PhD, holds the Waugh Family Chair in Multiple Sclerosis, and Dr. Tremlett is funded by the Canada Research Chair Program. Dr. Kingwell reported having no financial disclosures.
[email protected]
SOURCE: Kingwell E et al. ACTRIMS Forum 2018, late-breaking poster 254.
SAN DIEGO – Compared with controls, patients who developed MS were more frequently admitted to the hospital or visited a physician for problems related to the nervous system, sensory organs, musculoskeletal system, and genitourinary system in the 5 years prior to MS onset, a multicenter matched cohort study found.
“People are seeking help for different conditions that are most likely related to their MS,” one of the study authors, Elaine Kingwell, PhD, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “It suggests there could be opportunity to recognize and possibly diagnose and treat MS earlier.”
In a previously published study (Lancet Neurol. 2017;16[6]:445-51) led by Helen Tremlett, PhD, and first author Jose Wijnands, PhD, the team found increased health care utilization in people with MS across all health sectors – physician, hospital, and pharmacy (prescriptions filled).
For the current study, the team set out to identify early signs and symptoms that could define the MS prodrome. “We wanted to know why people went to the hospital, why people went to their physician, what kind of drugs they were prescribed, and what kind of specialists they saw,” explained Dr. Kingwell, an epidemiologist in the department of neurology at the University of British Columbia, Vancouver.
The researchers used health administrative and MS-specific data from four Canadian provinces to conduct a multicenter matched cohort study. Individuals were required to be in the province from 5 years pre-index date, measured as either the first demyelinating event in health administrative data or MS onset as determined by the treating neurologist, until the MS cases’ third demyelinating claim or diagnosis date. The potential for a prodromal period was examined in the 5 years pre-index date, and outcomes of interest were number of physician and hospital encounters per ICD-10 chapter, number of physician encounters per physician specialty, and percentage of people with one or more filled prescription per drug class.
The researchers used rate ratios and 95% confidence intervals to compare the rates of physician and hospital encounters between MS cases and controls and the proportion test to compare the percentage of people with one or more filled prescriptions between MS cases and controls. They used random-effects meta-analyses to pool results across Canadian provinces.
The population consisted of 13,951 MS patients and 66,940 controls derived from a health administration cohort and 3,202 MS patients and 16,006 controls derived from MS clinics. Compared with controls, in the 5 years before the first demyelinating claim or symptom onset, cases had more physician and hospital encounters for the nervous system (rate ratio = 1.70-4.75), sensory organs (RR = 1.40-2.28), musculoskeletal system (RR = 1.19-1.70), and genitourinary system (RR = 1.17-1.59), Dr. Kingwell and her associates reported.
Cases also had more encounters with psychiatrists (RR = 1.48-1.66) and urologists (RR = 1.49-1.80), and a higher proportion of filled prescriptions for hormonal preparations and drugs related to the musculoskeletal or genitourinary systems (ranging from 1.1 to 1.5 times higher; P less than .02 for all associations). “While we did not examine each individual drug, we did group drugs by their therapeutic class,” Dr. Wijnands noted in an interview after the meeting. “As for the increased number of visits to psychiatrists, it is intriguing. We don’t necessarily know all the reasons why. It opens up a lot of questions for people to follow up on.”
In contrast, MS cases had fewer pregnancy-related encounters, compared with controls (RR = 0.78-0.88).
Dr. Wijnands acknowledged certain limitations of the study, including its reliance on administrative data to measure the prodromal period. “When we described the prodrome itself, we relied on ICD codes from the physician and hospital data as well as prescriptions filled. Issues or problems for which individuals do not seek medical attention, for instance, would not be captured in our study,” she said.
The study was funded by the National MS Society. Dr. Wijnands receives salary support from the Michael Smith Foundation for Health Research /The Koehle Family Foundation, coauthor Ruth Ann Marrie, MD, PhD, holds the Waugh Family Chair in Multiple Sclerosis, and Dr. Tremlett is funded by the Canada Research Chair Program. Dr. Kingwell reported having no financial disclosures.
[email protected]
SOURCE: Kingwell E et al. ACTRIMS Forum 2018, late-breaking poster 254.
REPORTING FROM ACTRIMS FORUM 2018
Key clinical point: Several phenotypic characteristics may constitute the MS prodrome.
Major finding: Compared with controls, in the 5 years before the first demyelinating claim or symptom onset, MS cases had more physician and hospital encounters for the nervous system (rate ratio = 1.70-4.75), sensory organs (RR = 1.40-2.28), and musculoskeletal system (RR = 1.19-1.70).
Study details: A multicenter matched cohort study of 13,951 MS patients and 66,940 controls derived from a health administration cohort and 3,202 MS patients and 16,006 controls derived from MS clinics.
Disclosures: The study was funded by the National MS Society. Dr. Wijnands receives salary support from the Michael Smith Foundation for Health Research /The Koehle Family Foundation, coauthor Ruth Ann Marrie, MD, PhD, holds the Waugh Family Chair in Multiple Sclerosis, and Dr. Tremlett is funded by the Canada Research Chair Program. Dr. Kingwell reported having no financial disclosures.
Source: Kingwell E et al. ACTRIMS Forum 2018, late-breaking poster 254.
Study spotlights body image dissatisfaction in pediatric IBD
LAS VEGAS – Among current steroid use, higher body mass index percentile, and comorbid mood disorder.
The findings come from a cross-sectional study of 664 patients enrolled in the Crohn’s & Colitis Foundation’s Partners Kids & Teens cohort, presented by Jennifer Claytor, MS, at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
Ms. Claytor, a fourth-year medical student at the University of North Carolina at Chapel Hill, and her associates asked study participants aged 5-18 years to complete surveys on demographics, disease characteristics, and the IMPACT-35 questionnaire and Patient-Reported Outcomes Measurement Information System (PROMIS) tools for assessment of psychological patient-reported outcomes. The pediatric ulcerative colitis activity index and the short Crohn’s disease activity index were used to measure disease activity.
The researchers classified body image dissatisfaction as being present if the patients selected “I look awful” or “I look bad” from the list of possible responses to the question, “How do you feel about the way you look?” Next, they performed bivariate analyses to assess associations between body image dissatisfaction and demographic, disease-related, and psychosocial factors and created logistic regression models to evaluate independent associations between selected risk factors and body image dissatisfaction. “There has been some literature which suggests that for boys, weight and not body image dissatisfaction predicts worse psychosocial outcomes,” Ms. Claytor said. “But for girls it’s body image dissatisfaction, irrespective of weight.”
Of the 664 patients, 74 (3.3%) met criteria for body image dissatisfaction. Compared with patients who did not meet criteria for body image dissatisfaction, those who did were significantly more likely to be female (69% vs. 44%, respectively; P less than .001), older (mean age of 15 vs. 13 years; P less than .001), and diagnosed with IBD an older age (median of 12 vs. 10 years; P less than .001). Ms. Claytor and her associates also found that individuals with body image dissatisfaction had a higher median BMI percentile (P = .02), higher rates of active disease (57% vs. 26%; P less than .001), higher rates of current steroid use (18% vs. 8%; P = .004), and higher rates of depression and anxiety (P less than .001).
After adjusting for age, body mass index, remission, steroid use, and other factors, the odds for developing body image dissatisfaction was highest among those with anxiety (odds ratio, 5.42), followed by depression (OR, 4.73), female gender (OR, 2.31), and current steroid use (OR, 1.59). “I think this points to the need for enhanced counseling services and being aware of these characteristics,” Ms. Claytor said. She reported having no financial disclosures.
SOURCE: Claytor J et al. Crohn’s & Colitis Congress, Poster 15.
*This story was updated on 3/26.
LAS VEGAS – Among current steroid use, higher body mass index percentile, and comorbid mood disorder.
The findings come from a cross-sectional study of 664 patients enrolled in the Crohn’s & Colitis Foundation’s Partners Kids & Teens cohort, presented by Jennifer Claytor, MS, at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
Ms. Claytor, a fourth-year medical student at the University of North Carolina at Chapel Hill, and her associates asked study participants aged 5-18 years to complete surveys on demographics, disease characteristics, and the IMPACT-35 questionnaire and Patient-Reported Outcomes Measurement Information System (PROMIS) tools for assessment of psychological patient-reported outcomes. The pediatric ulcerative colitis activity index and the short Crohn’s disease activity index were used to measure disease activity.
The researchers classified body image dissatisfaction as being present if the patients selected “I look awful” or “I look bad” from the list of possible responses to the question, “How do you feel about the way you look?” Next, they performed bivariate analyses to assess associations between body image dissatisfaction and demographic, disease-related, and psychosocial factors and created logistic regression models to evaluate independent associations between selected risk factors and body image dissatisfaction. “There has been some literature which suggests that for boys, weight and not body image dissatisfaction predicts worse psychosocial outcomes,” Ms. Claytor said. “But for girls it’s body image dissatisfaction, irrespective of weight.”
Of the 664 patients, 74 (3.3%) met criteria for body image dissatisfaction. Compared with patients who did not meet criteria for body image dissatisfaction, those who did were significantly more likely to be female (69% vs. 44%, respectively; P less than .001), older (mean age of 15 vs. 13 years; P less than .001), and diagnosed with IBD an older age (median of 12 vs. 10 years; P less than .001). Ms. Claytor and her associates also found that individuals with body image dissatisfaction had a higher median BMI percentile (P = .02), higher rates of active disease (57% vs. 26%; P less than .001), higher rates of current steroid use (18% vs. 8%; P = .004), and higher rates of depression and anxiety (P less than .001).
After adjusting for age, body mass index, remission, steroid use, and other factors, the odds for developing body image dissatisfaction was highest among those with anxiety (odds ratio, 5.42), followed by depression (OR, 4.73), female gender (OR, 2.31), and current steroid use (OR, 1.59). “I think this points to the need for enhanced counseling services and being aware of these characteristics,” Ms. Claytor said. She reported having no financial disclosures.
SOURCE: Claytor J et al. Crohn’s & Colitis Congress, Poster 15.
*This story was updated on 3/26.
LAS VEGAS – Among current steroid use, higher body mass index percentile, and comorbid mood disorder.
The findings come from a cross-sectional study of 664 patients enrolled in the Crohn’s & Colitis Foundation’s Partners Kids & Teens cohort, presented by Jennifer Claytor, MS, at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
Ms. Claytor, a fourth-year medical student at the University of North Carolina at Chapel Hill, and her associates asked study participants aged 5-18 years to complete surveys on demographics, disease characteristics, and the IMPACT-35 questionnaire and Patient-Reported Outcomes Measurement Information System (PROMIS) tools for assessment of psychological patient-reported outcomes. The pediatric ulcerative colitis activity index and the short Crohn’s disease activity index were used to measure disease activity.
The researchers classified body image dissatisfaction as being present if the patients selected “I look awful” or “I look bad” from the list of possible responses to the question, “How do you feel about the way you look?” Next, they performed bivariate analyses to assess associations between body image dissatisfaction and demographic, disease-related, and psychosocial factors and created logistic regression models to evaluate independent associations between selected risk factors and body image dissatisfaction. “There has been some literature which suggests that for boys, weight and not body image dissatisfaction predicts worse psychosocial outcomes,” Ms. Claytor said. “But for girls it’s body image dissatisfaction, irrespective of weight.”
Of the 664 patients, 74 (3.3%) met criteria for body image dissatisfaction. Compared with patients who did not meet criteria for body image dissatisfaction, those who did were significantly more likely to be female (69% vs. 44%, respectively; P less than .001), older (mean age of 15 vs. 13 years; P less than .001), and diagnosed with IBD an older age (median of 12 vs. 10 years; P less than .001). Ms. Claytor and her associates also found that individuals with body image dissatisfaction had a higher median BMI percentile (P = .02), higher rates of active disease (57% vs. 26%; P less than .001), higher rates of current steroid use (18% vs. 8%; P = .004), and higher rates of depression and anxiety (P less than .001).
After adjusting for age, body mass index, remission, steroid use, and other factors, the odds for developing body image dissatisfaction was highest among those with anxiety (odds ratio, 5.42), followed by depression (OR, 4.73), female gender (OR, 2.31), and current steroid use (OR, 1.59). “I think this points to the need for enhanced counseling services and being aware of these characteristics,” Ms. Claytor said. She reported having no financial disclosures.
SOURCE: Claytor J et al. Crohn’s & Colitis Congress, Poster 15.
*This story was updated on 3/26.
REPORTING FROM CROHN’S & COLITIS CONGRESS
Key clinical point: Interventions to target modifiable risk factors for body image dissatisfaction may improve quality of life in pediatric IBD patients.
Major finding: The odds for developing body image dissatisfaction were highest among those with anxiety (odds ratio, 5.42), followed by depression (OR, 4.73) and female gender (OR, 2.31).
Study details: A cross-sectional study of 664 patients enrolled in the Crohn’s & Colitis Foundation’s Partners Kids & Teens cohort.
Disclosures: Ms. Claytor reported having no financial disclosures.
Source: Claytor J et al. Crohn’s & Colitis Congress, Poster 15.
High patient activation linked to clinical remission in IBD
LAS VEGAS – results from a longitudinal analysis suggest.
“Patient activation is defined as understanding one’s role in the health care process and having the knowledge, skills, and confidence to manage one’s health,” Edward L. Barnes, MD, MPH, said at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “It emphasizes an individual’s willingness to take independent actions and manage their own health care. In many chronic conditions, higher levels of patient activation have been linked to improved health outcomes, better patient experiences related to health care, higher quality of life scores, and lower overall health care costs.”
A 13-question survey known as the Patient Activation Measure from Insignia Health can be used to assess patient activation (Health Serv Res 2005;4096 Pt 1:1918-30). This measure is scored from zero to 100 and allows the categorization of individuals into four levels of activation. In level 1, the patient believes an active role is important. In level 2, the patient has the confidence and knowledge to take action. In level 3 the patient takes action, and in level 4, the patient stays the course during stress.
Dr. Barnes and his associates set out to evaluate the demographic and clinical characteristics associated with higher patient activation in patients with IBD. A secondary aim was to determine whether higher levels of patient care are associated with decreased frequency of relapse or flare. They performed a prospective cohort study of individuals who participated in the Crohn’s and Colitis Foundation’s Partners Internet cohort. Consecutive participants who completed a Partners survey between June 2, 2016, and Jan. 5, 2017, were asked to complete the Patient Activation Measure as an optional module. Clinical remission was defined via the short Crohn’s Disease Activity Index (a score of 150 or lower) and the Simple Clinical Colitis Activity Index (a score of 2 or less).
High patient activation was defined as level 3 or level 4 on the Patient Activation Measure, and multivariable logistic regression was used to evaluate predictors of patient activation level and the relationship between level of patient activation and clinical remission. All covariates included in the multivariable analyses were identified a priori based on prior association with patient activation or clinical disease activity in IBD.
The survey was administered to 1,486 participants. Of these, 1,082 (73%) completed follow-up surveys, including assessments of disease activity. The mean age of respondents was 44 years, 74% were female, 5% were nonwhite, and 77% reported their highest education level as college or graduate school. The mean disease duration was 14.4 years.
Patients with less than a 12th grade education were significantly associated with a decreased odds of having patient activation (adjusted odds ratio 0.25 [95% confidence interval, 0.07-0.94]). Although nonsignificant after adjustment for potential confounders, nonwhite race was also associated with decreased odds of high patient activation (aOR 0.64). Meanwhile, there was a trend among those who graduated from college or graduate school in predicting high patient activation level (aOR of 1.44 and 1.36, respectively).
After adjustment for race, educational status, time since diagnosis, smoking status, and history of IBD-related surgery among patients with Crohn’s disease, patients with higher patient activation were more likely to be in clinical remission at follow-up for both Crohn’s disease (71% vs. 62%; aOR of 1.60 [95% CI, 1.00-2.57], P = .05) and ulcerative colitis (54% vs. 34%; aOR 2.23, respectively; [95% CI, 1.15-4.19], P = .01).
Dr. Barnes acknowledged certain limitations of the study, including the fact that study participants comprised a voluntary, Internet-based cohort. “Participants may exhibit higher levels of patient activation than the general population of patients with IBD,” he said. “There may be an overrepresentation of college graduates in this sample, and the racial and ethnic makeup of this cohort may be different from that of a clinic-based population or the general population of patients with IBD.” He added that there might be unmeasured confounders in the relationship between patient activation and remission that the researchers could not assess.
“Patient activation appears to impact the disease course in patients with CD [Crohn’s disease] and UC [ulcerative colitis],” Dr. Barnes concluded. “The effect of patient activation on the disease course may be larger in UC than in CD. Efforts to improve patient activation in patients with IBD may have the ability to ultimately improve clinical outcomes.”
He reported having no financial disclosures.
*This story was updated on 3/26.
SOURCE: Barnes EL et al. Crohn’s & Colitis Congress, Clinical Abstract 12.
LAS VEGAS – results from a longitudinal analysis suggest.
“Patient activation is defined as understanding one’s role in the health care process and having the knowledge, skills, and confidence to manage one’s health,” Edward L. Barnes, MD, MPH, said at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “It emphasizes an individual’s willingness to take independent actions and manage their own health care. In many chronic conditions, higher levels of patient activation have been linked to improved health outcomes, better patient experiences related to health care, higher quality of life scores, and lower overall health care costs.”
A 13-question survey known as the Patient Activation Measure from Insignia Health can be used to assess patient activation (Health Serv Res 2005;4096 Pt 1:1918-30). This measure is scored from zero to 100 and allows the categorization of individuals into four levels of activation. In level 1, the patient believes an active role is important. In level 2, the patient has the confidence and knowledge to take action. In level 3 the patient takes action, and in level 4, the patient stays the course during stress.
Dr. Barnes and his associates set out to evaluate the demographic and clinical characteristics associated with higher patient activation in patients with IBD. A secondary aim was to determine whether higher levels of patient care are associated with decreased frequency of relapse or flare. They performed a prospective cohort study of individuals who participated in the Crohn’s and Colitis Foundation’s Partners Internet cohort. Consecutive participants who completed a Partners survey between June 2, 2016, and Jan. 5, 2017, were asked to complete the Patient Activation Measure as an optional module. Clinical remission was defined via the short Crohn’s Disease Activity Index (a score of 150 or lower) and the Simple Clinical Colitis Activity Index (a score of 2 or less).
High patient activation was defined as level 3 or level 4 on the Patient Activation Measure, and multivariable logistic regression was used to evaluate predictors of patient activation level and the relationship between level of patient activation and clinical remission. All covariates included in the multivariable analyses were identified a priori based on prior association with patient activation or clinical disease activity in IBD.
The survey was administered to 1,486 participants. Of these, 1,082 (73%) completed follow-up surveys, including assessments of disease activity. The mean age of respondents was 44 years, 74% were female, 5% were nonwhite, and 77% reported their highest education level as college or graduate school. The mean disease duration was 14.4 years.
Patients with less than a 12th grade education were significantly associated with a decreased odds of having patient activation (adjusted odds ratio 0.25 [95% confidence interval, 0.07-0.94]). Although nonsignificant after adjustment for potential confounders, nonwhite race was also associated with decreased odds of high patient activation (aOR 0.64). Meanwhile, there was a trend among those who graduated from college or graduate school in predicting high patient activation level (aOR of 1.44 and 1.36, respectively).
After adjustment for race, educational status, time since diagnosis, smoking status, and history of IBD-related surgery among patients with Crohn’s disease, patients with higher patient activation were more likely to be in clinical remission at follow-up for both Crohn’s disease (71% vs. 62%; aOR of 1.60 [95% CI, 1.00-2.57], P = .05) and ulcerative colitis (54% vs. 34%; aOR 2.23, respectively; [95% CI, 1.15-4.19], P = .01).
Dr. Barnes acknowledged certain limitations of the study, including the fact that study participants comprised a voluntary, Internet-based cohort. “Participants may exhibit higher levels of patient activation than the general population of patients with IBD,” he said. “There may be an overrepresentation of college graduates in this sample, and the racial and ethnic makeup of this cohort may be different from that of a clinic-based population or the general population of patients with IBD.” He added that there might be unmeasured confounders in the relationship between patient activation and remission that the researchers could not assess.
“Patient activation appears to impact the disease course in patients with CD [Crohn’s disease] and UC [ulcerative colitis],” Dr. Barnes concluded. “The effect of patient activation on the disease course may be larger in UC than in CD. Efforts to improve patient activation in patients with IBD may have the ability to ultimately improve clinical outcomes.”
He reported having no financial disclosures.
*This story was updated on 3/26.
SOURCE: Barnes EL et al. Crohn’s & Colitis Congress, Clinical Abstract 12.
LAS VEGAS – results from a longitudinal analysis suggest.
“Patient activation is defined as understanding one’s role in the health care process and having the knowledge, skills, and confidence to manage one’s health,” Edward L. Barnes, MD, MPH, said at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “It emphasizes an individual’s willingness to take independent actions and manage their own health care. In many chronic conditions, higher levels of patient activation have been linked to improved health outcomes, better patient experiences related to health care, higher quality of life scores, and lower overall health care costs.”
A 13-question survey known as the Patient Activation Measure from Insignia Health can be used to assess patient activation (Health Serv Res 2005;4096 Pt 1:1918-30). This measure is scored from zero to 100 and allows the categorization of individuals into four levels of activation. In level 1, the patient believes an active role is important. In level 2, the patient has the confidence and knowledge to take action. In level 3 the patient takes action, and in level 4, the patient stays the course during stress.
Dr. Barnes and his associates set out to evaluate the demographic and clinical characteristics associated with higher patient activation in patients with IBD. A secondary aim was to determine whether higher levels of patient care are associated with decreased frequency of relapse or flare. They performed a prospective cohort study of individuals who participated in the Crohn’s and Colitis Foundation’s Partners Internet cohort. Consecutive participants who completed a Partners survey between June 2, 2016, and Jan. 5, 2017, were asked to complete the Patient Activation Measure as an optional module. Clinical remission was defined via the short Crohn’s Disease Activity Index (a score of 150 or lower) and the Simple Clinical Colitis Activity Index (a score of 2 or less).
High patient activation was defined as level 3 or level 4 on the Patient Activation Measure, and multivariable logistic regression was used to evaluate predictors of patient activation level and the relationship between level of patient activation and clinical remission. All covariates included in the multivariable analyses were identified a priori based on prior association with patient activation or clinical disease activity in IBD.
The survey was administered to 1,486 participants. Of these, 1,082 (73%) completed follow-up surveys, including assessments of disease activity. The mean age of respondents was 44 years, 74% were female, 5% were nonwhite, and 77% reported their highest education level as college or graduate school. The mean disease duration was 14.4 years.
Patients with less than a 12th grade education were significantly associated with a decreased odds of having patient activation (adjusted odds ratio 0.25 [95% confidence interval, 0.07-0.94]). Although nonsignificant after adjustment for potential confounders, nonwhite race was also associated with decreased odds of high patient activation (aOR 0.64). Meanwhile, there was a trend among those who graduated from college or graduate school in predicting high patient activation level (aOR of 1.44 and 1.36, respectively).
After adjustment for race, educational status, time since diagnosis, smoking status, and history of IBD-related surgery among patients with Crohn’s disease, patients with higher patient activation were more likely to be in clinical remission at follow-up for both Crohn’s disease (71% vs. 62%; aOR of 1.60 [95% CI, 1.00-2.57], P = .05) and ulcerative colitis (54% vs. 34%; aOR 2.23, respectively; [95% CI, 1.15-4.19], P = .01).
Dr. Barnes acknowledged certain limitations of the study, including the fact that study participants comprised a voluntary, Internet-based cohort. “Participants may exhibit higher levels of patient activation than the general population of patients with IBD,” he said. “There may be an overrepresentation of college graduates in this sample, and the racial and ethnic makeup of this cohort may be different from that of a clinic-based population or the general population of patients with IBD.” He added that there might be unmeasured confounders in the relationship between patient activation and remission that the researchers could not assess.
“Patient activation appears to impact the disease course in patients with CD [Crohn’s disease] and UC [ulcerative colitis],” Dr. Barnes concluded. “The effect of patient activation on the disease course may be larger in UC than in CD. Efforts to improve patient activation in patients with IBD may have the ability to ultimately improve clinical outcomes.”
He reported having no financial disclosures.
*This story was updated on 3/26.
SOURCE: Barnes EL et al. Crohn’s & Colitis Congress, Clinical Abstract 12.
REPORTING FROM THE CROHN’S & COLITIS CONGRESS
Key clinical point: Patient activation appears to impact the disease course in IBD patients.
Major finding: Individuals with higher patient activation were more likely to be in clinical remission at follow-up for both CD and UC (adjusted OR of 1.60 vs. adjusted OR of 2.23, respectively).
Study details: Responses from 1,082 IBD patients who participated in the Crohn’s and Colitis Foundation’s Partners Internet cohort.
Disclosures: Dr. Barnes reported having no financial disclosures.
Source: Barnes EL et al. Crohn’s & Colitis Congress, Clinical Abstract 12.
‘Real-world evidence’ used to compare agents for relapsing-remitting MS
SAN DIEGO – Delayed-release dimethyl fumarate did not show any differences versus fingolimod in relapse rate over a 1-year, “real-world” study of patients with relapsing-remitting multiple sclerosis, but a significantly greater proportion of patients taking delayed-release dimethyl fumarate achieved relapse-free status and a lower annualized relapsed rate, compared with patients on glatiramer acetate
“There is a need for real-world data that compares the effectiveness of the growing number of MS [multiple sclerosis] treatment options,” Christophe Hotermans, MD, vice president of Global Medical Therapeutic Areas at Boston-based Biogen, said in an interview during ACTRIMS Forum 2018, held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “These results were consistent with previous analyses of efficacy of these treatments in people with relapsing-remitting MS, which showed no significant differences in efficacy between delayed-release dimethyl fumarate [DMF, Tecfidera] versus fingolimod [FTY, Gilenya] and greater efficacy with dimethyl fumarate, compared with glatiramer acetate [GA].”
The findings come from EFFECT (Observational Study to Characterize Real-world Clinical Outcomes With Relapsing-remitting Multiple Sclerosis), a multicenter, international, retrospective, single-time-point medical record review study comparing the effectiveness of DMF vs. other disease-modifying therapies, including FTY and GA in patients with relapsing-remitting MS.
Endpoints included the Kaplan-Meier estimated proportion of patients who relapsed at 12 months and annualized relapse rate. Baseline covariates were used in estimating propensity scores. The data were divided into four strata using quartiles of propensity scores. After assessing for balance in baseline covariates between the treatment groups, Kaplan-Meier estimates of relapse and estimates of treatment effects were pooled across the four strata.
At the meeting, Jinny Min, PharmD, a medical postdoctoral research fellow at Biogen, reported results from 816 DMF patients, 781 FTY patients, and 1,042 GA patients. In the trimmed analysis set, the estimated proportion of DMF and FTY patients who relapsed at 12 months after treatment initiation was 12% vs. 13%, respectively (hazard ratio, 1.07, P = .693; the adjusted rate ratio for annualized relapse was 1.09, P = .617). In the analysis of DMF vs. GA patients, the estimated proportion of DMF patients that relapsed at 12 months was 12% vs. 21%, respectively (HR, 0.71), which represented a significant decrease of 29% (P less than .02). The adjusted rate ratio for annualized relapse was 0.69, representing a significant decrease of 31% (P less than .01).
“We hope that these data help health care providers and people living with MS as they consider their treatment options,” Dr. Hotermans said. “The limitations of this study are similar to those that would be present in other retrospective studies that utilize real-world data. However, we worked to mitigate many of those limitations through a propensity-score estimation approach to adjust for confounders. An additional limitation that is inherent to the study design (retrospective chart review) is that patients’ medical history, MS disease, treatment history, and relapse history were limited to the information available in the medical records.”
The study was supported by Biogen, which markets DMF. Dr. Hotermans and Dr. Min are employees of the company.
SOURCE: Min J et al. ACTRIMS Forum 2018, Abstract P016.
SAN DIEGO – Delayed-release dimethyl fumarate did not show any differences versus fingolimod in relapse rate over a 1-year, “real-world” study of patients with relapsing-remitting multiple sclerosis, but a significantly greater proportion of patients taking delayed-release dimethyl fumarate achieved relapse-free status and a lower annualized relapsed rate, compared with patients on glatiramer acetate
“There is a need for real-world data that compares the effectiveness of the growing number of MS [multiple sclerosis] treatment options,” Christophe Hotermans, MD, vice president of Global Medical Therapeutic Areas at Boston-based Biogen, said in an interview during ACTRIMS Forum 2018, held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “These results were consistent with previous analyses of efficacy of these treatments in people with relapsing-remitting MS, which showed no significant differences in efficacy between delayed-release dimethyl fumarate [DMF, Tecfidera] versus fingolimod [FTY, Gilenya] and greater efficacy with dimethyl fumarate, compared with glatiramer acetate [GA].”
The findings come from EFFECT (Observational Study to Characterize Real-world Clinical Outcomes With Relapsing-remitting Multiple Sclerosis), a multicenter, international, retrospective, single-time-point medical record review study comparing the effectiveness of DMF vs. other disease-modifying therapies, including FTY and GA in patients with relapsing-remitting MS.
Endpoints included the Kaplan-Meier estimated proportion of patients who relapsed at 12 months and annualized relapse rate. Baseline covariates were used in estimating propensity scores. The data were divided into four strata using quartiles of propensity scores. After assessing for balance in baseline covariates between the treatment groups, Kaplan-Meier estimates of relapse and estimates of treatment effects were pooled across the four strata.
At the meeting, Jinny Min, PharmD, a medical postdoctoral research fellow at Biogen, reported results from 816 DMF patients, 781 FTY patients, and 1,042 GA patients. In the trimmed analysis set, the estimated proportion of DMF and FTY patients who relapsed at 12 months after treatment initiation was 12% vs. 13%, respectively (hazard ratio, 1.07, P = .693; the adjusted rate ratio for annualized relapse was 1.09, P = .617). In the analysis of DMF vs. GA patients, the estimated proportion of DMF patients that relapsed at 12 months was 12% vs. 21%, respectively (HR, 0.71), which represented a significant decrease of 29% (P less than .02). The adjusted rate ratio for annualized relapse was 0.69, representing a significant decrease of 31% (P less than .01).
“We hope that these data help health care providers and people living with MS as they consider their treatment options,” Dr. Hotermans said. “The limitations of this study are similar to those that would be present in other retrospective studies that utilize real-world data. However, we worked to mitigate many of those limitations through a propensity-score estimation approach to adjust for confounders. An additional limitation that is inherent to the study design (retrospective chart review) is that patients’ medical history, MS disease, treatment history, and relapse history were limited to the information available in the medical records.”
The study was supported by Biogen, which markets DMF. Dr. Hotermans and Dr. Min are employees of the company.
SOURCE: Min J et al. ACTRIMS Forum 2018, Abstract P016.
SAN DIEGO – Delayed-release dimethyl fumarate did not show any differences versus fingolimod in relapse rate over a 1-year, “real-world” study of patients with relapsing-remitting multiple sclerosis, but a significantly greater proportion of patients taking delayed-release dimethyl fumarate achieved relapse-free status and a lower annualized relapsed rate, compared with patients on glatiramer acetate
“There is a need for real-world data that compares the effectiveness of the growing number of MS [multiple sclerosis] treatment options,” Christophe Hotermans, MD, vice president of Global Medical Therapeutic Areas at Boston-based Biogen, said in an interview during ACTRIMS Forum 2018, held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “These results were consistent with previous analyses of efficacy of these treatments in people with relapsing-remitting MS, which showed no significant differences in efficacy between delayed-release dimethyl fumarate [DMF, Tecfidera] versus fingolimod [FTY, Gilenya] and greater efficacy with dimethyl fumarate, compared with glatiramer acetate [GA].”
The findings come from EFFECT (Observational Study to Characterize Real-world Clinical Outcomes With Relapsing-remitting Multiple Sclerosis), a multicenter, international, retrospective, single-time-point medical record review study comparing the effectiveness of DMF vs. other disease-modifying therapies, including FTY and GA in patients with relapsing-remitting MS.
Endpoints included the Kaplan-Meier estimated proportion of patients who relapsed at 12 months and annualized relapse rate. Baseline covariates were used in estimating propensity scores. The data were divided into four strata using quartiles of propensity scores. After assessing for balance in baseline covariates between the treatment groups, Kaplan-Meier estimates of relapse and estimates of treatment effects were pooled across the four strata.
At the meeting, Jinny Min, PharmD, a medical postdoctoral research fellow at Biogen, reported results from 816 DMF patients, 781 FTY patients, and 1,042 GA patients. In the trimmed analysis set, the estimated proportion of DMF and FTY patients who relapsed at 12 months after treatment initiation was 12% vs. 13%, respectively (hazard ratio, 1.07, P = .693; the adjusted rate ratio for annualized relapse was 1.09, P = .617). In the analysis of DMF vs. GA patients, the estimated proportion of DMF patients that relapsed at 12 months was 12% vs. 21%, respectively (HR, 0.71), which represented a significant decrease of 29% (P less than .02). The adjusted rate ratio for annualized relapse was 0.69, representing a significant decrease of 31% (P less than .01).
“We hope that these data help health care providers and people living with MS as they consider their treatment options,” Dr. Hotermans said. “The limitations of this study are similar to those that would be present in other retrospective studies that utilize real-world data. However, we worked to mitigate many of those limitations through a propensity-score estimation approach to adjust for confounders. An additional limitation that is inherent to the study design (retrospective chart review) is that patients’ medical history, MS disease, treatment history, and relapse history were limited to the information available in the medical records.”
The study was supported by Biogen, which markets DMF. Dr. Hotermans and Dr. Min are employees of the company.
SOURCE: Min J et al. ACTRIMS Forum 2018, Abstract P016.
REPORTING FROM ACTRIMS FORUM 2018
Key clinical point:
Major finding: Delayed-release dimethyl fumarate had a 29% lower risk of relapse during the 12-month period vs. glatiramer acetate.
Study details: Results from a multicenter study of 816 delayed-release dimethyl fumarate patients, 781 fingolimod patients, and 1,042 glatiramer acetate patients with relapsing-remitting MS.
Disclosures: The study was supported by Biogen, which markets delayed-release dimethyl fumarate. Dr. Hotermans and Dr. Min are employees of the company.
Source: Min J et al. ACTRIMS Forum 2018, Abstract P016.
Switching RRMS patients to daclizumab beta appears safe
SAN DIEGO – Switching relapsing-remitting multiple sclerosis patients from glatiramer acetate to daclizumab beta resulted in no increase in the adverse event profile and was associated with superior efficacy, a post hoc analysis of data from the DECIDE study showed.
“There is always a challenge in transitioning patients from one therapeutic agent to another, with concerns for adequate efficacy to justify the switch, and heightened risks of toxicity or adverse events,” lead study author Stanley L. Cohan, MD, PhD, said in an interview prior to the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “Daclizumab is not a first-line or platform therapeutic agent, but has clearly superior efficacy to first-line medication, and, based upon the current data presented, safety and efficacy are not adversely influenced by prior treatment history with a first-line agent.”
In the phase 3 DECIDE trial, daclizumab beta 150 mg demonstrated greater efficacy versus intramuscular (IM) interferon (IFN) beta-1a 30 mcg on several clinical, radiographic, and patient-centered outcomes in patients with relapsing-remitting multiple sclerosis (N Engl J Med 2015; 373:1418-28). The purpose of the current study was to examine the efficacy and safety of daclizumab beta vs. IM IFN beta-1a in the subgroup of RRMS patients treated with glatiramer acetate (GA) as their only previous disease-modifying therapy (DMT) before entering DECIDE.
Dr. Cohan, a neurologist who directs the Providence MS Center at the Providence Brain and Spine Institute in Portland, Ore., and his associates reported data from 42 of 922 (5%) IM IFN beta-1a and 50 of 919 (5%) daclizumab beta patients who had received treatment with GA only prior to DECIDE. Baseline characteristics were balanced between treatment groups, including duration of prior treatment with GA, reasons for discontinuing GA, and time between GA discontinuation and start of treatment in DECIDE. The annualized relapse rate was 42% lower in patients treated with daclizumab beta vs. IM IFN beta-1a (rate ratio of 0.58). Daclizumab beta also reduced risk of relapse by 53% (hazard ratio of 0.47; P = .048) and the mean number of new or newly-enlarging T2-hyperintense lesions at week 96 by 58% (lesion mean ratio, 0.42; P = .021) vs. IM IFN beta-1a.
In patients treated with GA only before DECIDE, 98% of IM IFN beta-1a patients and 94% of daclizumab beta patients reported any adverse event (AE). In all, 2% of IM IFN beta-1a patients and 16% of daclizumab beta patients had a serious AE (excluding MS relapse), and 10% of IM IFN beta-1a and 12% of daclizumab beta patients discontinued treatment because of an AE (excluding MS relapse).
The incidence of elevations of alanine aminotransferase or aspartate aminotransferase three times the upper limit of normal or greater was 10% in the IM IFN beta-1a group and 8% in the daclizumab beta, while the ALT and AST elevations were greater than five times the ULN in 0% and 4% of patients, respectively.
Serious adverse events were reported in eight participants in the daclizumab beta group (including abortion induced, ankle fracture, anal fistula, anxiety, appendicitis perforated, convulsion, pelvic abscess, inguinal hernia, abnormal cervix smear), and one participant in the IM IFN beta-1a group (ligament rupture).
“This post hoc analysis demonstrates that in switching from glatiramer to daclizumab there was no unanticipated or increase in the AE profile, and that a switch from glatiramer to daclizumab was associated with superior efficacy, again in line with overall efficacy observed for daclizumab in this study,” Dr. Cohan said.
He acknowledged certain limitations of the study, including the post hoc nature of the analysis. “The small glatiramer cohort size, and the large percentage of former glatiramer patients who entered DECIDE because of lack of glatiramer efficacy may have introduced a selection bias which would magnify the seeming efficacy of daclizumab, and interferon-beta,” he added.
Dr. Cohan reported that he receives research support from Biogen, Novartis, Roche, Sanofi, and Mallinckrodt, and speaking honoraria from Acorda, Biogen, Roche, and Sanofi. He has served on advisory boards for Biogen, Sanofi, and Novartis.
SOURCE: Cohan et al. ACTRIMS Forum 2018, Poster 42.
SAN DIEGO – Switching relapsing-remitting multiple sclerosis patients from glatiramer acetate to daclizumab beta resulted in no increase in the adverse event profile and was associated with superior efficacy, a post hoc analysis of data from the DECIDE study showed.
“There is always a challenge in transitioning patients from one therapeutic agent to another, with concerns for adequate efficacy to justify the switch, and heightened risks of toxicity or adverse events,” lead study author Stanley L. Cohan, MD, PhD, said in an interview prior to the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “Daclizumab is not a first-line or platform therapeutic agent, but has clearly superior efficacy to first-line medication, and, based upon the current data presented, safety and efficacy are not adversely influenced by prior treatment history with a first-line agent.”
In the phase 3 DECIDE trial, daclizumab beta 150 mg demonstrated greater efficacy versus intramuscular (IM) interferon (IFN) beta-1a 30 mcg on several clinical, radiographic, and patient-centered outcomes in patients with relapsing-remitting multiple sclerosis (N Engl J Med 2015; 373:1418-28). The purpose of the current study was to examine the efficacy and safety of daclizumab beta vs. IM IFN beta-1a in the subgroup of RRMS patients treated with glatiramer acetate (GA) as their only previous disease-modifying therapy (DMT) before entering DECIDE.
Dr. Cohan, a neurologist who directs the Providence MS Center at the Providence Brain and Spine Institute in Portland, Ore., and his associates reported data from 42 of 922 (5%) IM IFN beta-1a and 50 of 919 (5%) daclizumab beta patients who had received treatment with GA only prior to DECIDE. Baseline characteristics were balanced between treatment groups, including duration of prior treatment with GA, reasons for discontinuing GA, and time between GA discontinuation and start of treatment in DECIDE. The annualized relapse rate was 42% lower in patients treated with daclizumab beta vs. IM IFN beta-1a (rate ratio of 0.58). Daclizumab beta also reduced risk of relapse by 53% (hazard ratio of 0.47; P = .048) and the mean number of new or newly-enlarging T2-hyperintense lesions at week 96 by 58% (lesion mean ratio, 0.42; P = .021) vs. IM IFN beta-1a.
In patients treated with GA only before DECIDE, 98% of IM IFN beta-1a patients and 94% of daclizumab beta patients reported any adverse event (AE). In all, 2% of IM IFN beta-1a patients and 16% of daclizumab beta patients had a serious AE (excluding MS relapse), and 10% of IM IFN beta-1a and 12% of daclizumab beta patients discontinued treatment because of an AE (excluding MS relapse).
The incidence of elevations of alanine aminotransferase or aspartate aminotransferase three times the upper limit of normal or greater was 10% in the IM IFN beta-1a group and 8% in the daclizumab beta, while the ALT and AST elevations were greater than five times the ULN in 0% and 4% of patients, respectively.
Serious adverse events were reported in eight participants in the daclizumab beta group (including abortion induced, ankle fracture, anal fistula, anxiety, appendicitis perforated, convulsion, pelvic abscess, inguinal hernia, abnormal cervix smear), and one participant in the IM IFN beta-1a group (ligament rupture).
“This post hoc analysis demonstrates that in switching from glatiramer to daclizumab there was no unanticipated or increase in the AE profile, and that a switch from glatiramer to daclizumab was associated with superior efficacy, again in line with overall efficacy observed for daclizumab in this study,” Dr. Cohan said.
He acknowledged certain limitations of the study, including the post hoc nature of the analysis. “The small glatiramer cohort size, and the large percentage of former glatiramer patients who entered DECIDE because of lack of glatiramer efficacy may have introduced a selection bias which would magnify the seeming efficacy of daclizumab, and interferon-beta,” he added.
Dr. Cohan reported that he receives research support from Biogen, Novartis, Roche, Sanofi, and Mallinckrodt, and speaking honoraria from Acorda, Biogen, Roche, and Sanofi. He has served on advisory boards for Biogen, Sanofi, and Novartis.
SOURCE: Cohan et al. ACTRIMS Forum 2018, Poster 42.
SAN DIEGO – Switching relapsing-remitting multiple sclerosis patients from glatiramer acetate to daclizumab beta resulted in no increase in the adverse event profile and was associated with superior efficacy, a post hoc analysis of data from the DECIDE study showed.
“There is always a challenge in transitioning patients from one therapeutic agent to another, with concerns for adequate efficacy to justify the switch, and heightened risks of toxicity or adverse events,” lead study author Stanley L. Cohan, MD, PhD, said in an interview prior to the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “Daclizumab is not a first-line or platform therapeutic agent, but has clearly superior efficacy to first-line medication, and, based upon the current data presented, safety and efficacy are not adversely influenced by prior treatment history with a first-line agent.”
In the phase 3 DECIDE trial, daclizumab beta 150 mg demonstrated greater efficacy versus intramuscular (IM) interferon (IFN) beta-1a 30 mcg on several clinical, radiographic, and patient-centered outcomes in patients with relapsing-remitting multiple sclerosis (N Engl J Med 2015; 373:1418-28). The purpose of the current study was to examine the efficacy and safety of daclizumab beta vs. IM IFN beta-1a in the subgroup of RRMS patients treated with glatiramer acetate (GA) as their only previous disease-modifying therapy (DMT) before entering DECIDE.
Dr. Cohan, a neurologist who directs the Providence MS Center at the Providence Brain and Spine Institute in Portland, Ore., and his associates reported data from 42 of 922 (5%) IM IFN beta-1a and 50 of 919 (5%) daclizumab beta patients who had received treatment with GA only prior to DECIDE. Baseline characteristics were balanced between treatment groups, including duration of prior treatment with GA, reasons for discontinuing GA, and time between GA discontinuation and start of treatment in DECIDE. The annualized relapse rate was 42% lower in patients treated with daclizumab beta vs. IM IFN beta-1a (rate ratio of 0.58). Daclizumab beta also reduced risk of relapse by 53% (hazard ratio of 0.47; P = .048) and the mean number of new or newly-enlarging T2-hyperintense lesions at week 96 by 58% (lesion mean ratio, 0.42; P = .021) vs. IM IFN beta-1a.
In patients treated with GA only before DECIDE, 98% of IM IFN beta-1a patients and 94% of daclizumab beta patients reported any adverse event (AE). In all, 2% of IM IFN beta-1a patients and 16% of daclizumab beta patients had a serious AE (excluding MS relapse), and 10% of IM IFN beta-1a and 12% of daclizumab beta patients discontinued treatment because of an AE (excluding MS relapse).
The incidence of elevations of alanine aminotransferase or aspartate aminotransferase three times the upper limit of normal or greater was 10% in the IM IFN beta-1a group and 8% in the daclizumab beta, while the ALT and AST elevations were greater than five times the ULN in 0% and 4% of patients, respectively.
Serious adverse events were reported in eight participants in the daclizumab beta group (including abortion induced, ankle fracture, anal fistula, anxiety, appendicitis perforated, convulsion, pelvic abscess, inguinal hernia, abnormal cervix smear), and one participant in the IM IFN beta-1a group (ligament rupture).
“This post hoc analysis demonstrates that in switching from glatiramer to daclizumab there was no unanticipated or increase in the AE profile, and that a switch from glatiramer to daclizumab was associated with superior efficacy, again in line with overall efficacy observed for daclizumab in this study,” Dr. Cohan said.
He acknowledged certain limitations of the study, including the post hoc nature of the analysis. “The small glatiramer cohort size, and the large percentage of former glatiramer patients who entered DECIDE because of lack of glatiramer efficacy may have introduced a selection bias which would magnify the seeming efficacy of daclizumab, and interferon-beta,” he added.
Dr. Cohan reported that he receives research support from Biogen, Novartis, Roche, Sanofi, and Mallinckrodt, and speaking honoraria from Acorda, Biogen, Roche, and Sanofi. He has served on advisory boards for Biogen, Sanofi, and Novartis.
SOURCE: Cohan et al. ACTRIMS Forum 2018, Poster 42.
REPORTING FROM ACTRIMS FORUM 2018
Key clinical point:
Major finding: The annualized relapse rate was 42% lower in patients treated with daclizumab beta vs. IM IFN beta-1a (rate ratio of 0.58).
Study details: A post hoc analysis of 42 of 922 (5%) IM IFN beta-1a and 50 of 919 (5%) daclizumab beta patients who had received treatment with glatiramer acetate only prior to the DECIDE trial.
Disclosures: Dr. Cohan reported that he receives research support from Biogen, Novartis, Roche, Sanofi, and Mallinckrodt, and speaking honoraria from Acorda, Biogen, Roche, and Sanofi. He has served on advisory boards for Biogen, Sanofi, and Novartis.
Source: Cohan S et al. ACTRIMS Forum 2018 Poster 42.