User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Expert discusses risks of biosimilars in rheumatology
SAN DIEGO – If you perceive that the use of biosimilars for rheumatic diseases hasn’t gained the traction one would expect, you’re not alone. In the opinion of J. Eugene Huffstutter, MD, the expected risks of biosimilar products have clinicians concerned, especially when it comes to immunologic characteristics.
“We’ve all had patients on biologics for years: Everything’s fine, but then the patient has an infusion reaction,” Dr. Huffstutter said at the annual meeting of the American College of Rheumatology. “I’ve had it happen with the first infusion of a biologic and I’ve had it with the 20th infusion of that same biologic product. It’s impossible to predict.”
Other unforeseen risks of biosimilars include the impact on pharmacovigilance, manufacturing, and politics. “What if our government says we want to use this agent or that agent? Or, what if it advises everyone to use the bio-originator? Then there are coverage challenges,” he said. “How are the insurance companies going to look at this? Then there are corporate impacts. The companies that make biosimilars have invested a tremendous amount of resources to bring these to market. We have a huge market in the U.S., but the uptake has been very slow. So are they going to say, ‘We’re going to take our resources and do something else?’ ”
Practice protocols for using biosimilars vary depending on your practice environment. For example, if biosimilars are administered by a freestanding practice, “you have to depend a lot on your state laws in terms of what the pharmacist is able to do,” said Dr. Huffstutter, who is also the past president of the Tennessee Rheumatology Society. “What are the patient support programs available for that biosimilar compared with bio-originator? What do the insurance contracts say in terms of can you get this filled or not? What’s the formulary status? How well do physicians in your community accept biosimilars? More importantly, how do your patients feel about biosimilars? I think they’ve been left out of this whole discussion.”
Dr. Huffstutter disclosed that he has received research support from GlaxoSmithKline, Pfizer, and UCB. He is also a member of the speakers bureau and/or is an adviser to Janssen, Lilly, Pfizer, Genentech, Novartis, Regeneron, and UCB.
SAN DIEGO – If you perceive that the use of biosimilars for rheumatic diseases hasn’t gained the traction one would expect, you’re not alone. In the opinion of J. Eugene Huffstutter, MD, the expected risks of biosimilar products have clinicians concerned, especially when it comes to immunologic characteristics.
“We’ve all had patients on biologics for years: Everything’s fine, but then the patient has an infusion reaction,” Dr. Huffstutter said at the annual meeting of the American College of Rheumatology. “I’ve had it happen with the first infusion of a biologic and I’ve had it with the 20th infusion of that same biologic product. It’s impossible to predict.”
Other unforeseen risks of biosimilars include the impact on pharmacovigilance, manufacturing, and politics. “What if our government says we want to use this agent or that agent? Or, what if it advises everyone to use the bio-originator? Then there are coverage challenges,” he said. “How are the insurance companies going to look at this? Then there are corporate impacts. The companies that make biosimilars have invested a tremendous amount of resources to bring these to market. We have a huge market in the U.S., but the uptake has been very slow. So are they going to say, ‘We’re going to take our resources and do something else?’ ”
Practice protocols for using biosimilars vary depending on your practice environment. For example, if biosimilars are administered by a freestanding practice, “you have to depend a lot on your state laws in terms of what the pharmacist is able to do,” said Dr. Huffstutter, who is also the past president of the Tennessee Rheumatology Society. “What are the patient support programs available for that biosimilar compared with bio-originator? What do the insurance contracts say in terms of can you get this filled or not? What’s the formulary status? How well do physicians in your community accept biosimilars? More importantly, how do your patients feel about biosimilars? I think they’ve been left out of this whole discussion.”
Dr. Huffstutter disclosed that he has received research support from GlaxoSmithKline, Pfizer, and UCB. He is also a member of the speakers bureau and/or is an adviser to Janssen, Lilly, Pfizer, Genentech, Novartis, Regeneron, and UCB.
SAN DIEGO – If you perceive that the use of biosimilars for rheumatic diseases hasn’t gained the traction one would expect, you’re not alone. In the opinion of J. Eugene Huffstutter, MD, the expected risks of biosimilar products have clinicians concerned, especially when it comes to immunologic characteristics.
“We’ve all had patients on biologics for years: Everything’s fine, but then the patient has an infusion reaction,” Dr. Huffstutter said at the annual meeting of the American College of Rheumatology. “I’ve had it happen with the first infusion of a biologic and I’ve had it with the 20th infusion of that same biologic product. It’s impossible to predict.”
Other unforeseen risks of biosimilars include the impact on pharmacovigilance, manufacturing, and politics. “What if our government says we want to use this agent or that agent? Or, what if it advises everyone to use the bio-originator? Then there are coverage challenges,” he said. “How are the insurance companies going to look at this? Then there are corporate impacts. The companies that make biosimilars have invested a tremendous amount of resources to bring these to market. We have a huge market in the U.S., but the uptake has been very slow. So are they going to say, ‘We’re going to take our resources and do something else?’ ”
Practice protocols for using biosimilars vary depending on your practice environment. For example, if biosimilars are administered by a freestanding practice, “you have to depend a lot on your state laws in terms of what the pharmacist is able to do,” said Dr. Huffstutter, who is also the past president of the Tennessee Rheumatology Society. “What are the patient support programs available for that biosimilar compared with bio-originator? What do the insurance contracts say in terms of can you get this filled or not? What’s the formulary status? How well do physicians in your community accept biosimilars? More importantly, how do your patients feel about biosimilars? I think they’ve been left out of this whole discussion.”
Dr. Huffstutter disclosed that he has received research support from GlaxoSmithKline, Pfizer, and UCB. He is also a member of the speakers bureau and/or is an adviser to Janssen, Lilly, Pfizer, Genentech, Novartis, Regeneron, and UCB.
EXPERT ANALYSIS FROM ACR 2017
Study explores why RA patients discontinue methotrexate
SAN DIEGO – Despite the well-recognized role of methotrexate in the management of rheumatoid arthritis, about 30% of patients with RA discontinue treatment with methotrexate 1-2 years after starting it, according to results from a registry study.
“We know that methotrexate is an acceptable and certainly well-characterized treatment for RA,” study author Jeffrey R. Curtis, MD, said at the annual meeting of the American College of Rheumatology. “Despite, this, though, patterns of persistence, intolerance, and inadequate response with methotrexate [MTX] are not well characterized in real-world settings. We all get the sense that there are patients who greatly dislike it.”
The researchers analyzed patients not previously treated with a biologic DMARD (bDMARD) or a targeted synthetic DMARD (tsDMARD). They compared 1,488 patients who initiated MTX monotherapy with 656 patients who initiated MTX in combination with csDMARDs during October 2001 through February 2017 and had at least one follow-up visit after treatment initiation.
The mean age of patients was 57 years, 75% were female, and 84% were white. Patients in the MTX combination therapy group were more likely to be white, better educated, and employed, but were slightly less likely to have active disease. Dr. Curtis reported that the proportion of MTX monotherapy patients who discontinued MTX was 24% at 1 year, 37% at 2 years, and 46% at 3 years, and was not significantly different from the figures for the combination MTX therapy group (P = .99). “The survival curve was overlapping and nonsignificant,” said Dr. Curtis, professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham. “For example, at 12 months, 24.4% of people stopped methotrexate if they had started it alone, but it was 26% if they were on combination therapy. Flipping that around, 75% stayed on MTX at 1 year’s time.”
In contrast, the researchers also found that patients in the MTX monotherapy group were significantly more likely to start a bDMARD or a tsDMARD earlier than patients in the MTX combination therapy group (P less than .001). In an adjusted Cox proportional hazards model, higher risk for MTX discontinuation was associated with being disabled (hazard ratio, 1.33), being retired (HR, 1.37), or using alcohol regularly (the HR ranged from 1.22 to 2.03 depending on the mean units consumed per day). MTX discontinuation was less likely in patients with older age (HR, 0.94), longer duration of RA (HR, 0.92), or higher baseline Clinical Disease Activity Index score (HR, 0.96).
About 20% of physicians in the registry provided reasons for discontinuation of MTX. The top reasons they gave were the presence of infection and cancer (about 85% and 15%, respectively). The reasons patients gave for discontinuation of MTX were wide ranging and included unusual fatigue (about 67%), followed by stomach problems (48%), hair loss (about 36%), mental fog (about 29%), sores in the mouth (about 25%), nausea (about 19%), and diarrhea (about 19%). “Patients are telling us very different things about why this drug is being stopped,” Dr. Curtis said. “Doctors in this registry could specify a reason for stopping that would map to these reasons, and yet they didn’t.”
He acknowledged certain limitations of the study, including the potential for missing data and the possibility that some of the patients may have reinitiated MTX. “We know from other data that people may stop MTX for a period of time but then may resume it,” Dr. Curtis said. Going forward, he called for strategies “to better identify patients with suboptimal persistence to MTX and predict those most likely to not tolerate MTX, to optimize overall RA treatment.”
The study was supported by Corrona, and the analysis was funded by Pfizer. Dr. Curtis reported that he has received research grants from Amgen, Corrona, Crescendo Bioscience, and Pfizer, and consulting fees from AbbVie, Amgen, Bristol-Myers Squibb, Corrona, Myriad, Pfizer, Roche/Genentech, and UCB.
SAN DIEGO – Despite the well-recognized role of methotrexate in the management of rheumatoid arthritis, about 30% of patients with RA discontinue treatment with methotrexate 1-2 years after starting it, according to results from a registry study.
“We know that methotrexate is an acceptable and certainly well-characterized treatment for RA,” study author Jeffrey R. Curtis, MD, said at the annual meeting of the American College of Rheumatology. “Despite, this, though, patterns of persistence, intolerance, and inadequate response with methotrexate [MTX] are not well characterized in real-world settings. We all get the sense that there are patients who greatly dislike it.”
The researchers analyzed patients not previously treated with a biologic DMARD (bDMARD) or a targeted synthetic DMARD (tsDMARD). They compared 1,488 patients who initiated MTX monotherapy with 656 patients who initiated MTX in combination with csDMARDs during October 2001 through February 2017 and had at least one follow-up visit after treatment initiation.
The mean age of patients was 57 years, 75% were female, and 84% were white. Patients in the MTX combination therapy group were more likely to be white, better educated, and employed, but were slightly less likely to have active disease. Dr. Curtis reported that the proportion of MTX monotherapy patients who discontinued MTX was 24% at 1 year, 37% at 2 years, and 46% at 3 years, and was not significantly different from the figures for the combination MTX therapy group (P = .99). “The survival curve was overlapping and nonsignificant,” said Dr. Curtis, professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham. “For example, at 12 months, 24.4% of people stopped methotrexate if they had started it alone, but it was 26% if they were on combination therapy. Flipping that around, 75% stayed on MTX at 1 year’s time.”
In contrast, the researchers also found that patients in the MTX monotherapy group were significantly more likely to start a bDMARD or a tsDMARD earlier than patients in the MTX combination therapy group (P less than .001). In an adjusted Cox proportional hazards model, higher risk for MTX discontinuation was associated with being disabled (hazard ratio, 1.33), being retired (HR, 1.37), or using alcohol regularly (the HR ranged from 1.22 to 2.03 depending on the mean units consumed per day). MTX discontinuation was less likely in patients with older age (HR, 0.94), longer duration of RA (HR, 0.92), or higher baseline Clinical Disease Activity Index score (HR, 0.96).
About 20% of physicians in the registry provided reasons for discontinuation of MTX. The top reasons they gave were the presence of infection and cancer (about 85% and 15%, respectively). The reasons patients gave for discontinuation of MTX were wide ranging and included unusual fatigue (about 67%), followed by stomach problems (48%), hair loss (about 36%), mental fog (about 29%), sores in the mouth (about 25%), nausea (about 19%), and diarrhea (about 19%). “Patients are telling us very different things about why this drug is being stopped,” Dr. Curtis said. “Doctors in this registry could specify a reason for stopping that would map to these reasons, and yet they didn’t.”
He acknowledged certain limitations of the study, including the potential for missing data and the possibility that some of the patients may have reinitiated MTX. “We know from other data that people may stop MTX for a period of time but then may resume it,” Dr. Curtis said. Going forward, he called for strategies “to better identify patients with suboptimal persistence to MTX and predict those most likely to not tolerate MTX, to optimize overall RA treatment.”
The study was supported by Corrona, and the analysis was funded by Pfizer. Dr. Curtis reported that he has received research grants from Amgen, Corrona, Crescendo Bioscience, and Pfizer, and consulting fees from AbbVie, Amgen, Bristol-Myers Squibb, Corrona, Myriad, Pfizer, Roche/Genentech, and UCB.
SAN DIEGO – Despite the well-recognized role of methotrexate in the management of rheumatoid arthritis, about 30% of patients with RA discontinue treatment with methotrexate 1-2 years after starting it, according to results from a registry study.
“We know that methotrexate is an acceptable and certainly well-characterized treatment for RA,” study author Jeffrey R. Curtis, MD, said at the annual meeting of the American College of Rheumatology. “Despite, this, though, patterns of persistence, intolerance, and inadequate response with methotrexate [MTX] are not well characterized in real-world settings. We all get the sense that there are patients who greatly dislike it.”
The researchers analyzed patients not previously treated with a biologic DMARD (bDMARD) or a targeted synthetic DMARD (tsDMARD). They compared 1,488 patients who initiated MTX monotherapy with 656 patients who initiated MTX in combination with csDMARDs during October 2001 through February 2017 and had at least one follow-up visit after treatment initiation.
The mean age of patients was 57 years, 75% were female, and 84% were white. Patients in the MTX combination therapy group were more likely to be white, better educated, and employed, but were slightly less likely to have active disease. Dr. Curtis reported that the proportion of MTX monotherapy patients who discontinued MTX was 24% at 1 year, 37% at 2 years, and 46% at 3 years, and was not significantly different from the figures for the combination MTX therapy group (P = .99). “The survival curve was overlapping and nonsignificant,” said Dr. Curtis, professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham. “For example, at 12 months, 24.4% of people stopped methotrexate if they had started it alone, but it was 26% if they were on combination therapy. Flipping that around, 75% stayed on MTX at 1 year’s time.”
In contrast, the researchers also found that patients in the MTX monotherapy group were significantly more likely to start a bDMARD or a tsDMARD earlier than patients in the MTX combination therapy group (P less than .001). In an adjusted Cox proportional hazards model, higher risk for MTX discontinuation was associated with being disabled (hazard ratio, 1.33), being retired (HR, 1.37), or using alcohol regularly (the HR ranged from 1.22 to 2.03 depending on the mean units consumed per day). MTX discontinuation was less likely in patients with older age (HR, 0.94), longer duration of RA (HR, 0.92), or higher baseline Clinical Disease Activity Index score (HR, 0.96).
About 20% of physicians in the registry provided reasons for discontinuation of MTX. The top reasons they gave were the presence of infection and cancer (about 85% and 15%, respectively). The reasons patients gave for discontinuation of MTX were wide ranging and included unusual fatigue (about 67%), followed by stomach problems (48%), hair loss (about 36%), mental fog (about 29%), sores in the mouth (about 25%), nausea (about 19%), and diarrhea (about 19%). “Patients are telling us very different things about why this drug is being stopped,” Dr. Curtis said. “Doctors in this registry could specify a reason for stopping that would map to these reasons, and yet they didn’t.”
He acknowledged certain limitations of the study, including the potential for missing data and the possibility that some of the patients may have reinitiated MTX. “We know from other data that people may stop MTX for a period of time but then may resume it,” Dr. Curtis said. Going forward, he called for strategies “to better identify patients with suboptimal persistence to MTX and predict those most likely to not tolerate MTX, to optimize overall RA treatment.”
The study was supported by Corrona, and the analysis was funded by Pfizer. Dr. Curtis reported that he has received research grants from Amgen, Corrona, Crescendo Bioscience, and Pfizer, and consulting fees from AbbVie, Amgen, Bristol-Myers Squibb, Corrona, Myriad, Pfizer, Roche/Genentech, and UCB.
AT ACR 2017
Key clinical point: Nearly one-third of patients with RA discontinue methotrexate 1–2 years after initiation.
Major finding: The proportion of MTX monotherapy patients who discontinued MTX was 24% at 1 year, 37% at 2 years, and 46% at 3 years, and was not significantly different from the combination MTX therapy group (P = .99).
Study details: A registry study that compared 1,488 patients who initiated MTX monotherapy with 656 patients who initiated MTX in combination with conventional synthetic DMARDs.
Disclosures: The study was supported by Corrona, and the analysis was funded by Pfizer. Dr. Curtis reported that he has received research grants from Amgen, Corrona, Crescendo Bioscience, and Pfizer, and consulting fees from AbbVie, Amgen, Bristol-Myers Squibb, Corrona, Myriad, Pfizer, Roche/Genentech, and UCB.
Anabasum shows promise in treating skin-predominant dermatomyositis, systemic sclerosis
SAN DIEGO – Results from two phase 2 studies of the investigational agent anabasum provide evidence supporting its safety and efficacy in patients with refractory skin-predominant dermatomyositis or diffuse cutaneous systemic sclerosis.
Anabasum (JBT-101) is a nonimmunosuppressive, synthetic, oral cannabinoid receptor type 2 agonist being developed by Norwood, Mass.–based Corbus Pharmaceuticals. It works by triggering resolution of innate immune responses, said Barbara White, MD, a rheumatologist who is chief medical officer for Corbus. “It restores homeostasis, gets rid of inflammation, turns off active fibrotic processes, and helps clear bacteria if it is present – all without immunosuppression,” she explained in an interview at the annual meeting of the American College of Rheumatology. “A drug that would restore homeostasis in the setting of an ongoing immune response has the potential to be helpful in multiple autoimmune diseases.”
The mean age of the study participants was 53 years and most were white. Even though 19 of the patients were on immunosuppressants at baseline, both cohorts had mean CDASI scores in the 33-35 range, which can be considered severe.
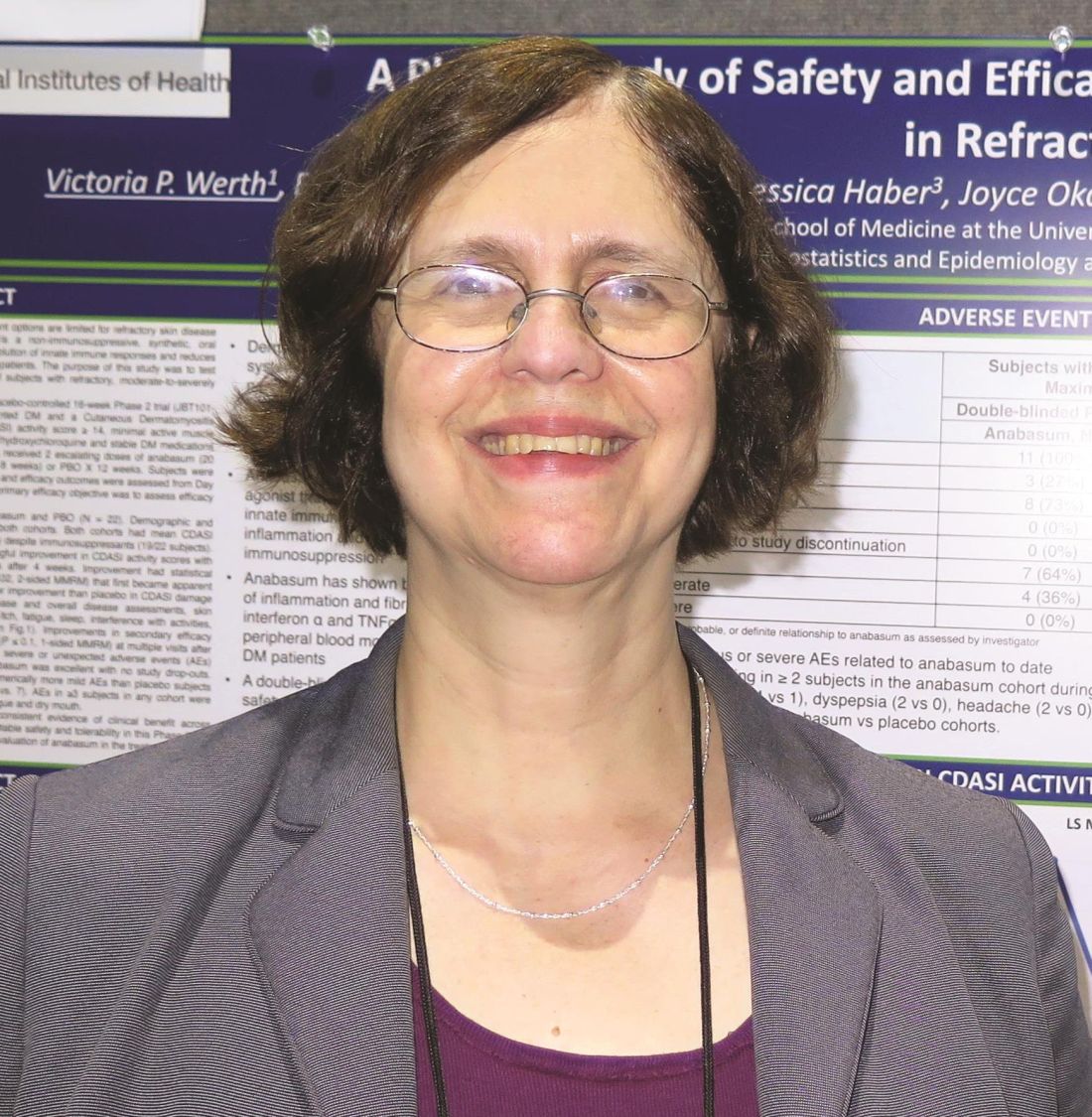
The investigators, led by Victoria P. Werth, MD, of the University of Pennsylvania, Philadelphia, reported that anabasum-treated subjects experienced a medically meaningful improvement in mean CDASI scores, with a reduction of at least 5 points at all visits after week 4 and reaching –9.3 at the end of the study, compared with –3.7 points in the placebo group (P = .02). They also found that 56% of subjects in the anabasum group had a 10-point reduction or more in CDASI score, compared with only 18% in the placebo group (P = .09). In addition, no subjects in the anabasum group developed skin erosions during the active dosing period, compared with 36% of subjects in the placebo group (P = .05).
The researchers also observed that, compared with subjects in the placebo group, those in the anabasum group had greater improvement in patient-reported global skin disease and overall disease assessments, skin symptoms (including photosensitivity and itch), fatigue, sleep, interference with activities, pain, and physical function. No serious, severe, or unexpected adverse events occurred in the anabasum group. Adverse events included dizziness, dyspepsia, headache, and increased appetite.
There is not a Food and Drug Administration or European Medicines Agency–approved drug for refractory skin-predominant dermatomyositis, “so this is encouraging,” Dr. White said.
Dr. Spiera reported that patients in the anabasum group had greater improvement in ACR CRISS, compared with placebo-treated subjects over 16 weeks (P = .044). They also had greater improvement and less worsening in individual CRISS core measures, including modified Rodnan Skin Score, Patient Global Assessment, Physician Global Assessment, and the Health Assessment Questionnaire Disability Index. Patient-reported outcomes of systemic sclerosis skin symptoms, itch, and the Patient-Reported Outcomes Measurement Information System–29 (PROMIS-29) domains of physical function, pain interference, and sleep also improved for the anabasum group, compared with the placebo group (P less than .05 for all).
An analysis of paired skin biopsies before and after treatment with the assessor blinded to treatment assignment demonstrated that patients treated with anabasum were more likely to show improvement in fibrosis and inflammation and less likely to show worsening than were those treated with placebo, consistent with what was observed clinically. In a related poster presented at the meeting, gene expression analysis from specimens before and after treatment also revealed that anabasum treatment (as opposed to treatment with placebo) was associated with changes relevant to pathways involved in fibrosis and inflammation.
“This is the first double-blind, randomized, placebo controlled trial in diffuse cutaneous systemic sclerosis to demonstrate a clinical benefit using the CRISS as an endpoint, with a drug that was safe and well tolerated in the trial,” Dr. Spiera said. “These results bring hope to patients and their physicians that anabasum may be an effective drug for systemic sclerosis where currently there are no proven treatments.”
Both studies were sponsored by Corbus, and the dermatomyositis study was also sponsored by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Some of the investigators in both studies were employees of Corbus. Dr. Spiera reported receiving research support from Corbus and many other pharmaceutical companies. He also is a consultant to Roche-Genentech, GlaxoSmithKline, Boehringer Ingelheim, and CSL Behring. He is a member of the Rheumatology News editorial advisory board.
SAN DIEGO – Results from two phase 2 studies of the investigational agent anabasum provide evidence supporting its safety and efficacy in patients with refractory skin-predominant dermatomyositis or diffuse cutaneous systemic sclerosis.
Anabasum (JBT-101) is a nonimmunosuppressive, synthetic, oral cannabinoid receptor type 2 agonist being developed by Norwood, Mass.–based Corbus Pharmaceuticals. It works by triggering resolution of innate immune responses, said Barbara White, MD, a rheumatologist who is chief medical officer for Corbus. “It restores homeostasis, gets rid of inflammation, turns off active fibrotic processes, and helps clear bacteria if it is present – all without immunosuppression,” she explained in an interview at the annual meeting of the American College of Rheumatology. “A drug that would restore homeostasis in the setting of an ongoing immune response has the potential to be helpful in multiple autoimmune diseases.”
The mean age of the study participants was 53 years and most were white. Even though 19 of the patients were on immunosuppressants at baseline, both cohorts had mean CDASI scores in the 33-35 range, which can be considered severe.
The investigators, led by Victoria P. Werth, MD, of the University of Pennsylvania, Philadelphia, reported that anabasum-treated subjects experienced a medically meaningful improvement in mean CDASI scores, with a reduction of at least 5 points at all visits after week 4 and reaching –9.3 at the end of the study, compared with –3.7 points in the placebo group (P = .02). They also found that 56% of subjects in the anabasum group had a 10-point reduction or more in CDASI score, compared with only 18% in the placebo group (P = .09). In addition, no subjects in the anabasum group developed skin erosions during the active dosing period, compared with 36% of subjects in the placebo group (P = .05).
The researchers also observed that, compared with subjects in the placebo group, those in the anabasum group had greater improvement in patient-reported global skin disease and overall disease assessments, skin symptoms (including photosensitivity and itch), fatigue, sleep, interference with activities, pain, and physical function. No serious, severe, or unexpected adverse events occurred in the anabasum group. Adverse events included dizziness, dyspepsia, headache, and increased appetite.
There is not a Food and Drug Administration or European Medicines Agency–approved drug for refractory skin-predominant dermatomyositis, “so this is encouraging,” Dr. White said.
Dr. Spiera reported that patients in the anabasum group had greater improvement in ACR CRISS, compared with placebo-treated subjects over 16 weeks (P = .044). They also had greater improvement and less worsening in individual CRISS core measures, including modified Rodnan Skin Score, Patient Global Assessment, Physician Global Assessment, and the Health Assessment Questionnaire Disability Index. Patient-reported outcomes of systemic sclerosis skin symptoms, itch, and the Patient-Reported Outcomes Measurement Information System–29 (PROMIS-29) domains of physical function, pain interference, and sleep also improved for the anabasum group, compared with the placebo group (P less than .05 for all).
An analysis of paired skin biopsies before and after treatment with the assessor blinded to treatment assignment demonstrated that patients treated with anabasum were more likely to show improvement in fibrosis and inflammation and less likely to show worsening than were those treated with placebo, consistent with what was observed clinically. In a related poster presented at the meeting, gene expression analysis from specimens before and after treatment also revealed that anabasum treatment (as opposed to treatment with placebo) was associated with changes relevant to pathways involved in fibrosis and inflammation.
“This is the first double-blind, randomized, placebo controlled trial in diffuse cutaneous systemic sclerosis to demonstrate a clinical benefit using the CRISS as an endpoint, with a drug that was safe and well tolerated in the trial,” Dr. Spiera said. “These results bring hope to patients and their physicians that anabasum may be an effective drug for systemic sclerosis where currently there are no proven treatments.”
Both studies were sponsored by Corbus, and the dermatomyositis study was also sponsored by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Some of the investigators in both studies were employees of Corbus. Dr. Spiera reported receiving research support from Corbus and many other pharmaceutical companies. He also is a consultant to Roche-Genentech, GlaxoSmithKline, Boehringer Ingelheim, and CSL Behring. He is a member of the Rheumatology News editorial advisory board.
SAN DIEGO – Results from two phase 2 studies of the investigational agent anabasum provide evidence supporting its safety and efficacy in patients with refractory skin-predominant dermatomyositis or diffuse cutaneous systemic sclerosis.
Anabasum (JBT-101) is a nonimmunosuppressive, synthetic, oral cannabinoid receptor type 2 agonist being developed by Norwood, Mass.–based Corbus Pharmaceuticals. It works by triggering resolution of innate immune responses, said Barbara White, MD, a rheumatologist who is chief medical officer for Corbus. “It restores homeostasis, gets rid of inflammation, turns off active fibrotic processes, and helps clear bacteria if it is present – all without immunosuppression,” she explained in an interview at the annual meeting of the American College of Rheumatology. “A drug that would restore homeostasis in the setting of an ongoing immune response has the potential to be helpful in multiple autoimmune diseases.”
The mean age of the study participants was 53 years and most were white. Even though 19 of the patients were on immunosuppressants at baseline, both cohorts had mean CDASI scores in the 33-35 range, which can be considered severe.
The investigators, led by Victoria P. Werth, MD, of the University of Pennsylvania, Philadelphia, reported that anabasum-treated subjects experienced a medically meaningful improvement in mean CDASI scores, with a reduction of at least 5 points at all visits after week 4 and reaching –9.3 at the end of the study, compared with –3.7 points in the placebo group (P = .02). They also found that 56% of subjects in the anabasum group had a 10-point reduction or more in CDASI score, compared with only 18% in the placebo group (P = .09). In addition, no subjects in the anabasum group developed skin erosions during the active dosing period, compared with 36% of subjects in the placebo group (P = .05).
The researchers also observed that, compared with subjects in the placebo group, those in the anabasum group had greater improvement in patient-reported global skin disease and overall disease assessments, skin symptoms (including photosensitivity and itch), fatigue, sleep, interference with activities, pain, and physical function. No serious, severe, or unexpected adverse events occurred in the anabasum group. Adverse events included dizziness, dyspepsia, headache, and increased appetite.
There is not a Food and Drug Administration or European Medicines Agency–approved drug for refractory skin-predominant dermatomyositis, “so this is encouraging,” Dr. White said.
Dr. Spiera reported that patients in the anabasum group had greater improvement in ACR CRISS, compared with placebo-treated subjects over 16 weeks (P = .044). They also had greater improvement and less worsening in individual CRISS core measures, including modified Rodnan Skin Score, Patient Global Assessment, Physician Global Assessment, and the Health Assessment Questionnaire Disability Index. Patient-reported outcomes of systemic sclerosis skin symptoms, itch, and the Patient-Reported Outcomes Measurement Information System–29 (PROMIS-29) domains of physical function, pain interference, and sleep also improved for the anabasum group, compared with the placebo group (P less than .05 for all).
An analysis of paired skin biopsies before and after treatment with the assessor blinded to treatment assignment demonstrated that patients treated with anabasum were more likely to show improvement in fibrosis and inflammation and less likely to show worsening than were those treated with placebo, consistent with what was observed clinically. In a related poster presented at the meeting, gene expression analysis from specimens before and after treatment also revealed that anabasum treatment (as opposed to treatment with placebo) was associated with changes relevant to pathways involved in fibrosis and inflammation.
“This is the first double-blind, randomized, placebo controlled trial in diffuse cutaneous systemic sclerosis to demonstrate a clinical benefit using the CRISS as an endpoint, with a drug that was safe and well tolerated in the trial,” Dr. Spiera said. “These results bring hope to patients and their physicians that anabasum may be an effective drug for systemic sclerosis where currently there are no proven treatments.”
Both studies were sponsored by Corbus, and the dermatomyositis study was also sponsored by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Some of the investigators in both studies were employees of Corbus. Dr. Spiera reported receiving research support from Corbus and many other pharmaceutical companies. He also is a consultant to Roche-Genentech, GlaxoSmithKline, Boehringer Ingelheim, and CSL Behring. He is a member of the Rheumatology News editorial advisory board.
AT ACR 2017
Key clinical point: Anabasum had a favorable safety profile and was well tolerated in patients with either refractory skin-predominant dermatomyositis or diffuse cutaneous systemic sclerosis.
Major finding: Treatment with anabasum resulted in greater improvement in the Cutaneous Dermatomyositis Disease Area and Severity Index (CDASI) score at 12 weeks, compared with placebo (–9.3 vs. –3.7 points, respectively; P = .02) and also in the ACR Combined Response Index in Systemic Sclerosis (CRISS) at 16 weeks, compared with placebo (P = .044).
Study details: Two 12-week, phase 2 studies of anabasum in patients with dermatomyositis or systemic sclerosis.
Disclosures: The studies were funded by Corbus, and the dermatomyositis study was additionally supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Spiera reported receiving research support from Corbus and many other pharmaceutical companies. He is a consultant to Roche-Genentech, GlaxoSmithKline, Boehringer Ingelheim, and CSL Behring. Some of the investigators in both studies were employees of Corbus.
Novel agent found to benefit Sjögren’s patients
SAN DIEGO – according to results of a proof-of-concept study.
CFZ533 is a novel monoclonal antibody being developed by Novartis that potently and selectively blocks CD40, a costimulatory pathway receptor essential for germinal center reactions and other immune-mediated functions implicated in primary Sjögren’s syndrome pathogenesis.
“Sjögren’s syndrome is characterized by focal infiltration of lymphocytes in a periductal distribution in exocrine glands,” lead study author Benjamin Fisher, MD, said at the annual meeting of the American College of Rheumatology.
“These lymphocytic foci often show organization and a proportion will show a germinal center formation. The lymphocytic infiltrates are associated with profound dryness, conjunctival erosions, fatigue that’s disabling, and in at least one-third of patients, systemic manifestations. There are no proven immunomodulatory treatments for this Sjögren’s syndrome. The lymphocytic infiltrates are also characterized by the expression of the costimulatory molecule CD40 and its ligand, also known as CD154,” he said.
For the study, subjects with an ESSDAI (EULAR Sjögren’s Syndrome Disease Activity Index) score of 6 or more were randomized 2:1 to receive 10 mg/kg of CFZ533 or placebo over a 12-week period. Four additional doses were administered in an open-label extension for 12 weeks. The primary goals were to evaluate the drug’s safety and tolerability as assessed by adverse events, and also to assess disease activity, with the primary outcome being the ESSDAI score. “The proof-of-concept criteria were stringent,” Dr. Fisher said. They “required a reduction in the ESSDAI score after 12 weeks to be 5 or more points greater in the CFZ533 group than the placebo group. The minimal clinically important difference is 3 points.”
He reported results from 21 patients in the CFZ533 and 11 in the placebo group. The baseline ESSDAI scores were 10.6 and 11 in the CFZ533 group and placebo groups, respectively. Patients also showed high symptomatic burden as assessed by the ESSPRI (EULAR Sjögren’s Syndrome Patient Reported Index), which measures dryness, fatigue, and pain on a 0-10 scale (mean scores of 6.7 and 7.2, respectively).
At 24 weeks, CFZ533 was found to be well tolerated, with no unexpected safety findings. “There were no serious infectious complications and there were no thromboembolic events,” Dr. Fisher said. “We did have one serious adverse event at the end of the open-label period. It occurred on the last day of that subject’s follow-up period. This was a case of atrial fibrillation. However, the patient had a predisposing medical condition and it was thought to be unrelated to the study drug.” Evaluation of pharmacokinetic data revealed that plasma levels throughout the study were above the level which previous data suggest is associated with inhibition of the CD40 pathway in tissue. “These plasma levels are also associated with inhibition of germinal center formation and with inhibition of T-dependent antigen response,” he said.
At the end of 12 weeks, CFZ533 was associated with a statistically significant reduction in ESSDAI scores, compared with the placebo group. The difference between groups was 5.6 points, which exceeded the proof-of-concept criteria. “This response was maintained through the open-label period,” Dr. Fisher said. “We also saw a reduction in the placebo group once they’d been switched to CFZ533 in the open-label period.”
The researchers also observed clinically meaningful improvements in other measures that favored CFZ533 over placebo, including the Physician Global Assessment, the physician and patient ratings on the Visual Analog Scale, and the Short Form–36 physical and mental health measures. “These data support continuation of the CFZ533 clinical program in primary Sjögren’s syndrome,” Dr. Fisher concluded.
Novartis sponsored the study. Dr. Fisher disclosed having received research support from Novartis, Roche, Bristol-Myers Squibb, and Virtualscopics.
SAN DIEGO – according to results of a proof-of-concept study.
CFZ533 is a novel monoclonal antibody being developed by Novartis that potently and selectively blocks CD40, a costimulatory pathway receptor essential for germinal center reactions and other immune-mediated functions implicated in primary Sjögren’s syndrome pathogenesis.
“Sjögren’s syndrome is characterized by focal infiltration of lymphocytes in a periductal distribution in exocrine glands,” lead study author Benjamin Fisher, MD, said at the annual meeting of the American College of Rheumatology.
“These lymphocytic foci often show organization and a proportion will show a germinal center formation. The lymphocytic infiltrates are associated with profound dryness, conjunctival erosions, fatigue that’s disabling, and in at least one-third of patients, systemic manifestations. There are no proven immunomodulatory treatments for this Sjögren’s syndrome. The lymphocytic infiltrates are also characterized by the expression of the costimulatory molecule CD40 and its ligand, also known as CD154,” he said.
For the study, subjects with an ESSDAI (EULAR Sjögren’s Syndrome Disease Activity Index) score of 6 or more were randomized 2:1 to receive 10 mg/kg of CFZ533 or placebo over a 12-week period. Four additional doses were administered in an open-label extension for 12 weeks. The primary goals were to evaluate the drug’s safety and tolerability as assessed by adverse events, and also to assess disease activity, with the primary outcome being the ESSDAI score. “The proof-of-concept criteria were stringent,” Dr. Fisher said. They “required a reduction in the ESSDAI score after 12 weeks to be 5 or more points greater in the CFZ533 group than the placebo group. The minimal clinically important difference is 3 points.”
He reported results from 21 patients in the CFZ533 and 11 in the placebo group. The baseline ESSDAI scores were 10.6 and 11 in the CFZ533 group and placebo groups, respectively. Patients also showed high symptomatic burden as assessed by the ESSPRI (EULAR Sjögren’s Syndrome Patient Reported Index), which measures dryness, fatigue, and pain on a 0-10 scale (mean scores of 6.7 and 7.2, respectively).
At 24 weeks, CFZ533 was found to be well tolerated, with no unexpected safety findings. “There were no serious infectious complications and there were no thromboembolic events,” Dr. Fisher said. “We did have one serious adverse event at the end of the open-label period. It occurred on the last day of that subject’s follow-up period. This was a case of atrial fibrillation. However, the patient had a predisposing medical condition and it was thought to be unrelated to the study drug.” Evaluation of pharmacokinetic data revealed that plasma levels throughout the study were above the level which previous data suggest is associated with inhibition of the CD40 pathway in tissue. “These plasma levels are also associated with inhibition of germinal center formation and with inhibition of T-dependent antigen response,” he said.
At the end of 12 weeks, CFZ533 was associated with a statistically significant reduction in ESSDAI scores, compared with the placebo group. The difference between groups was 5.6 points, which exceeded the proof-of-concept criteria. “This response was maintained through the open-label period,” Dr. Fisher said. “We also saw a reduction in the placebo group once they’d been switched to CFZ533 in the open-label period.”
The researchers also observed clinically meaningful improvements in other measures that favored CFZ533 over placebo, including the Physician Global Assessment, the physician and patient ratings on the Visual Analog Scale, and the Short Form–36 physical and mental health measures. “These data support continuation of the CFZ533 clinical program in primary Sjögren’s syndrome,” Dr. Fisher concluded.
Novartis sponsored the study. Dr. Fisher disclosed having received research support from Novartis, Roche, Bristol-Myers Squibb, and Virtualscopics.
SAN DIEGO – according to results of a proof-of-concept study.
CFZ533 is a novel monoclonal antibody being developed by Novartis that potently and selectively blocks CD40, a costimulatory pathway receptor essential for germinal center reactions and other immune-mediated functions implicated in primary Sjögren’s syndrome pathogenesis.
“Sjögren’s syndrome is characterized by focal infiltration of lymphocytes in a periductal distribution in exocrine glands,” lead study author Benjamin Fisher, MD, said at the annual meeting of the American College of Rheumatology.
“These lymphocytic foci often show organization and a proportion will show a germinal center formation. The lymphocytic infiltrates are associated with profound dryness, conjunctival erosions, fatigue that’s disabling, and in at least one-third of patients, systemic manifestations. There are no proven immunomodulatory treatments for this Sjögren’s syndrome. The lymphocytic infiltrates are also characterized by the expression of the costimulatory molecule CD40 and its ligand, also known as CD154,” he said.
For the study, subjects with an ESSDAI (EULAR Sjögren’s Syndrome Disease Activity Index) score of 6 or more were randomized 2:1 to receive 10 mg/kg of CFZ533 or placebo over a 12-week period. Four additional doses were administered in an open-label extension for 12 weeks. The primary goals were to evaluate the drug’s safety and tolerability as assessed by adverse events, and also to assess disease activity, with the primary outcome being the ESSDAI score. “The proof-of-concept criteria were stringent,” Dr. Fisher said. They “required a reduction in the ESSDAI score after 12 weeks to be 5 or more points greater in the CFZ533 group than the placebo group. The minimal clinically important difference is 3 points.”
He reported results from 21 patients in the CFZ533 and 11 in the placebo group. The baseline ESSDAI scores were 10.6 and 11 in the CFZ533 group and placebo groups, respectively. Patients also showed high symptomatic burden as assessed by the ESSPRI (EULAR Sjögren’s Syndrome Patient Reported Index), which measures dryness, fatigue, and pain on a 0-10 scale (mean scores of 6.7 and 7.2, respectively).
At 24 weeks, CFZ533 was found to be well tolerated, with no unexpected safety findings. “There were no serious infectious complications and there were no thromboembolic events,” Dr. Fisher said. “We did have one serious adverse event at the end of the open-label period. It occurred on the last day of that subject’s follow-up period. This was a case of atrial fibrillation. However, the patient had a predisposing medical condition and it was thought to be unrelated to the study drug.” Evaluation of pharmacokinetic data revealed that plasma levels throughout the study were above the level which previous data suggest is associated with inhibition of the CD40 pathway in tissue. “These plasma levels are also associated with inhibition of germinal center formation and with inhibition of T-dependent antigen response,” he said.
At the end of 12 weeks, CFZ533 was associated with a statistically significant reduction in ESSDAI scores, compared with the placebo group. The difference between groups was 5.6 points, which exceeded the proof-of-concept criteria. “This response was maintained through the open-label period,” Dr. Fisher said. “We also saw a reduction in the placebo group once they’d been switched to CFZ533 in the open-label period.”
The researchers also observed clinically meaningful improvements in other measures that favored CFZ533 over placebo, including the Physician Global Assessment, the physician and patient ratings on the Visual Analog Scale, and the Short Form–36 physical and mental health measures. “These data support continuation of the CFZ533 clinical program in primary Sjögren’s syndrome,” Dr. Fisher concluded.
Novartis sponsored the study. Dr. Fisher disclosed having received research support from Novartis, Roche, Bristol-Myers Squibb, and Virtualscopics.
AT ACR 2017
Key clinical point: Data support continuation of CFZ533 in clinical trials.
Major finding: At the end of 12 weeks, patients in the treatment group had a mean improvement of 5.6 points on the EULAR Sjögren’s Syndrome Disease Activity Index (ESSDAI) score.
Study details: A proof of concept study of 42 Sjögren’s patients.
Disclosures: Novartis sponsored the study. Dr. Fisher disclosed having received research support from Novartis, Roche, Bristol-Myers Squibb, and Virtualscopics.
Race may transcend social, geographical parameters in lupus mortality
SAN DIEGO – Blacks with systemic lupus erythematosus (SLE) who share the same social and geographic contexts as whites with the disease were disproportionately more likely to die young and to show severe patterns of mortality, according to a study of death certificate data.
“One of the most salient aspects of the epidemiology of lupus is the predilection of the disease for women and racial minorities,” lead study author Titilola Falasinnu, PhD, said at the annual meeting of the American College of Rheumatology.
Dr. Falasinnu, a postdoctoral fellow in Stanford (Calif.) University’s department of health research and policy, and her associates examined SLE mortality across eight groups of race-county combinations published in 2006 and known as the “Eight Americas” (PLoS Med. 2006 Sep 12;3[9]:e260). This seminal work, which has been validated across multiple disease states, jointly characterized race, socioeconomic status, and geographical location in relation to health disparities in the United States to demonstrate the most important factors accounting for these disparities within the Eight Americas.
For the current analysis, Dr. Falasinnu and her associates were most interested in America 6 (black middle America), America 7 (Southern low-income rural blacks), and America 8 (high-risk urban blacks). “The question we wanted to ask is whether, on average, poorer individuals have more severe SLE mortality experiences, compared with richer individuals in the black community,” she said. “What happens when you hold race constant and you vary socioeconomic indices?” Using death certificate data from the National Center for Health Statistics Multiple Causes of Death database, they identified SLE-related deaths between 2003 and 2014. Next, they compared these data with mortality statistics from each of the Eight Americas.
In all, there were nearly 25,000 SLE-related deaths, of which 85% were female. More than one-third of deaths occurred among those aged 45-64 years, and the mean age at death was 57 years. More than half of deaths (64%) occurred among whites, and 31% among blacks. Among SLE decedents, northern rural whites in America 2 had the lowest mortality rates. Blacks in America 6, 7, and 8 had the highest mortality, yet there were no significant differences in the death rates among those three groups. “We found that in general, blacks were three times more likely to die with SLE, compared with those in America 3 [middle America],” Dr. Falasinnu said.
Asians, Native Americans, and blacks with SLE died at an average age of 48-49 years, regardless of their social context, while Northern whites had the highest life expectancy: an average age of 69 years. They also found that 17% of SLE deaths in America 2 occurred before the age of 50 years, compared with more than 50% in Americas 6, 7, and 8. The most frequently reported associated causes of death were cardiovascular disease (about 50% of all SLE-related deaths) and kidney manifestations (about 20% of all SLE-related deaths). Compared with those in America 3, racial minorities had a 23%-53% higher risk of infections, a 5%-64% higher risk of kidney disease, a 7%-23% lower risk of cardiovascular disease, and a 20%-52% lower risk of cancers.
“Although blacks inhabited three vastly different geographical and social contexts, SLE mortality parameters did not vary among socially advantaged and disadvantaged black Americas,” Dr. Falasinnu concluded. “Blacks sharing the same social and geographical contexts as whites were disproportionately more likely to die young and exhibit patterns of mortality associated with active SLE disease.”
She acknowledged certain limitations of the study, including that differences in the degree of underreporting on death certificates across racial groups could bias the results. “The Eight Americas framework does not allow for evaluation of ethnicity,” she added. “We were also unable to examine causes for the disparities in SLE mortality. One could argue that there are a lot of other social factors that are likely race related that are not necessarily captured by the Eight Americas. Also, as with most epidemiological studies, we cannot rule out the role that ecological fallacy may play where the population average may not be appropriate in estimating an individual’s risk of mortality.”
One of the study coauthors reported receiving partial salary support through the Dr. Elaine Lambert Lupus Foundation via the John and Marcia Goldman Foundation and previously receiving salary support through a lupus-related grant from the Genomics Institute of the Novartis Research Foundation. The other coauthors reported having no relevant disclosures.
[email protected]
SAN DIEGO – Blacks with systemic lupus erythematosus (SLE) who share the same social and geographic contexts as whites with the disease were disproportionately more likely to die young and to show severe patterns of mortality, according to a study of death certificate data.
“One of the most salient aspects of the epidemiology of lupus is the predilection of the disease for women and racial minorities,” lead study author Titilola Falasinnu, PhD, said at the annual meeting of the American College of Rheumatology.
Dr. Falasinnu, a postdoctoral fellow in Stanford (Calif.) University’s department of health research and policy, and her associates examined SLE mortality across eight groups of race-county combinations published in 2006 and known as the “Eight Americas” (PLoS Med. 2006 Sep 12;3[9]:e260). This seminal work, which has been validated across multiple disease states, jointly characterized race, socioeconomic status, and geographical location in relation to health disparities in the United States to demonstrate the most important factors accounting for these disparities within the Eight Americas.
For the current analysis, Dr. Falasinnu and her associates were most interested in America 6 (black middle America), America 7 (Southern low-income rural blacks), and America 8 (high-risk urban blacks). “The question we wanted to ask is whether, on average, poorer individuals have more severe SLE mortality experiences, compared with richer individuals in the black community,” she said. “What happens when you hold race constant and you vary socioeconomic indices?” Using death certificate data from the National Center for Health Statistics Multiple Causes of Death database, they identified SLE-related deaths between 2003 and 2014. Next, they compared these data with mortality statistics from each of the Eight Americas.
In all, there were nearly 25,000 SLE-related deaths, of which 85% were female. More than one-third of deaths occurred among those aged 45-64 years, and the mean age at death was 57 years. More than half of deaths (64%) occurred among whites, and 31% among blacks. Among SLE decedents, northern rural whites in America 2 had the lowest mortality rates. Blacks in America 6, 7, and 8 had the highest mortality, yet there were no significant differences in the death rates among those three groups. “We found that in general, blacks were three times more likely to die with SLE, compared with those in America 3 [middle America],” Dr. Falasinnu said.
Asians, Native Americans, and blacks with SLE died at an average age of 48-49 years, regardless of their social context, while Northern whites had the highest life expectancy: an average age of 69 years. They also found that 17% of SLE deaths in America 2 occurred before the age of 50 years, compared with more than 50% in Americas 6, 7, and 8. The most frequently reported associated causes of death were cardiovascular disease (about 50% of all SLE-related deaths) and kidney manifestations (about 20% of all SLE-related deaths). Compared with those in America 3, racial minorities had a 23%-53% higher risk of infections, a 5%-64% higher risk of kidney disease, a 7%-23% lower risk of cardiovascular disease, and a 20%-52% lower risk of cancers.
“Although blacks inhabited three vastly different geographical and social contexts, SLE mortality parameters did not vary among socially advantaged and disadvantaged black Americas,” Dr. Falasinnu concluded. “Blacks sharing the same social and geographical contexts as whites were disproportionately more likely to die young and exhibit patterns of mortality associated with active SLE disease.”
She acknowledged certain limitations of the study, including that differences in the degree of underreporting on death certificates across racial groups could bias the results. “The Eight Americas framework does not allow for evaluation of ethnicity,” she added. “We were also unable to examine causes for the disparities in SLE mortality. One could argue that there are a lot of other social factors that are likely race related that are not necessarily captured by the Eight Americas. Also, as with most epidemiological studies, we cannot rule out the role that ecological fallacy may play where the population average may not be appropriate in estimating an individual’s risk of mortality.”
One of the study coauthors reported receiving partial salary support through the Dr. Elaine Lambert Lupus Foundation via the John and Marcia Goldman Foundation and previously receiving salary support through a lupus-related grant from the Genomics Institute of the Novartis Research Foundation. The other coauthors reported having no relevant disclosures.
[email protected]
SAN DIEGO – Blacks with systemic lupus erythematosus (SLE) who share the same social and geographic contexts as whites with the disease were disproportionately more likely to die young and to show severe patterns of mortality, according to a study of death certificate data.
“One of the most salient aspects of the epidemiology of lupus is the predilection of the disease for women and racial minorities,” lead study author Titilola Falasinnu, PhD, said at the annual meeting of the American College of Rheumatology.
Dr. Falasinnu, a postdoctoral fellow in Stanford (Calif.) University’s department of health research and policy, and her associates examined SLE mortality across eight groups of race-county combinations published in 2006 and known as the “Eight Americas” (PLoS Med. 2006 Sep 12;3[9]:e260). This seminal work, which has been validated across multiple disease states, jointly characterized race, socioeconomic status, and geographical location in relation to health disparities in the United States to demonstrate the most important factors accounting for these disparities within the Eight Americas.
For the current analysis, Dr. Falasinnu and her associates were most interested in America 6 (black middle America), America 7 (Southern low-income rural blacks), and America 8 (high-risk urban blacks). “The question we wanted to ask is whether, on average, poorer individuals have more severe SLE mortality experiences, compared with richer individuals in the black community,” she said. “What happens when you hold race constant and you vary socioeconomic indices?” Using death certificate data from the National Center for Health Statistics Multiple Causes of Death database, they identified SLE-related deaths between 2003 and 2014. Next, they compared these data with mortality statistics from each of the Eight Americas.
In all, there were nearly 25,000 SLE-related deaths, of which 85% were female. More than one-third of deaths occurred among those aged 45-64 years, and the mean age at death was 57 years. More than half of deaths (64%) occurred among whites, and 31% among blacks. Among SLE decedents, northern rural whites in America 2 had the lowest mortality rates. Blacks in America 6, 7, and 8 had the highest mortality, yet there were no significant differences in the death rates among those three groups. “We found that in general, blacks were three times more likely to die with SLE, compared with those in America 3 [middle America],” Dr. Falasinnu said.
Asians, Native Americans, and blacks with SLE died at an average age of 48-49 years, regardless of their social context, while Northern whites had the highest life expectancy: an average age of 69 years. They also found that 17% of SLE deaths in America 2 occurred before the age of 50 years, compared with more than 50% in Americas 6, 7, and 8. The most frequently reported associated causes of death were cardiovascular disease (about 50% of all SLE-related deaths) and kidney manifestations (about 20% of all SLE-related deaths). Compared with those in America 3, racial minorities had a 23%-53% higher risk of infections, a 5%-64% higher risk of kidney disease, a 7%-23% lower risk of cardiovascular disease, and a 20%-52% lower risk of cancers.
“Although blacks inhabited three vastly different geographical and social contexts, SLE mortality parameters did not vary among socially advantaged and disadvantaged black Americas,” Dr. Falasinnu concluded. “Blacks sharing the same social and geographical contexts as whites were disproportionately more likely to die young and exhibit patterns of mortality associated with active SLE disease.”
She acknowledged certain limitations of the study, including that differences in the degree of underreporting on death certificates across racial groups could bias the results. “The Eight Americas framework does not allow for evaluation of ethnicity,” she added. “We were also unable to examine causes for the disparities in SLE mortality. One could argue that there are a lot of other social factors that are likely race related that are not necessarily captured by the Eight Americas. Also, as with most epidemiological studies, we cannot rule out the role that ecological fallacy may play where the population average may not be appropriate in estimating an individual’s risk of mortality.”
One of the study coauthors reported receiving partial salary support through the Dr. Elaine Lambert Lupus Foundation via the John and Marcia Goldman Foundation and previously receiving salary support through a lupus-related grant from the Genomics Institute of the Novartis Research Foundation. The other coauthors reported having no relevant disclosures.
[email protected]
AT ACR 2017
Key clinical point: Blacks sharing the same social and geographical contexts as whites were more likely to die young and exhibit patterns of mortality associated with active SLE disease.
Major finding: Blacks in three race-geographic contexts were about three times more likely than whites in middle America to die with SLE.
Study details: An analysis of nearly 25,000 SLE-related deaths from the National Center for Health Statistics Multiple Causes of Death database.
Disclosures: One of the study coauthors reported receiving partial salary support through the Dr. Elaine Lambert Lupus Foundation via the John and Marcia Goldman Foundation and previously receiving salary support through a lupus-related grant from the Genomics Institute of the Novartis Research Foundation. The other coauthors reported having no relevant disclosures.
Proposed SLE classification criteria prove highly sensitive, specific
SAN DIEGO – yielded a sensitivity of 98% and a specificity of 97%.
The development is part of a four-phase joint effort by the American College of Rheumatology and the European League Against Rheumatism, first launched in 2014, to improve classification of patients with SLE for the purposes of clinical trials of new therapies and clinical research into the causes and outcomes of the disease. “The ACR and EULAR have long recognized the importance of classification criteria, so that we have more homogeneous groups in these research studies, and then we can compare results from studies,” Sindhu Johnson, MD, PhD, said during a press briefing at the annual meeting of the American College of Rheumatology.
A synopsis of the first three phases from the ongoing effort was presented at the June 2017 EULAR meeting. It included results from a systematic review of the literature and a meta-regression analysis to determine whether antinuclear autoantibodies should be required in the classification of SLE. The analysis showed that an antinuclear antibody titer of greater than or equal to 1:80 by immunofluorescence on human epithelial type 2 cells had a sensitivity of 98.4% for correctly capturing SLE. This prompted the EULAR/ACR steering committee to propose this titer as an “entry criterion” for SLE classification.
At the ACR meeting, Dr. Johnson, a rheumatologist at the University of Toronto who also cochairs the ACR Classification and Response Criteria subcommittee, discussed the fourth phase of the collaboration, which involves fine-tuning and validating the proposed SLE classification criteria.
To date, 189 investigators and more than 3,500 patients have contributed to the effort. “In the most recent phase, 36 international lupus centers were approached to contribute 100 cases and 100 controls,” she explained. “We then had each case independently adjudicated by three lupus experts at three different lupus centers to make sure there was consensus on the diagnosis. Next, we randomly selected 500 cases and 500 controls, resulting in a derivation cohort of 1,000 subjects to test our draft criteria system.”
Dr. Johnson and her associates found that the proposed SLE criteria had a sensitivity of 98% and a specificity of 97%, which exceeds that of the old ACR criteria. “We have defined a system of criteria which produces a measure of the relative probability that a particular case with a combination of clinical symptoms or features has SLE,” she said.
Dr. Johnson emphasized that the proposed criteria are intended for the classification of SLE, not for diagnosing the condition. “The diagnosis of lupus still remains in the hands of the physician, who will take into account all of the symptoms, signs, and other investigations,” she said. “We have identified the highest yield of those, but there will be some people who do not fulfill classification criteria yet do have a diagnosis of SLE.”
The next few weeks is a period to solicit feedback from stakeholders, after which members of the EULAR/ACR steering committee will be weighing feedback on the proposed criteria. “After that, we will see if there are any final revisions that need to be made,” Dr. Johnson said. “If we’re happy with the product, then the final validation will occur. We still have more than 1,000 patients from the validation core that has been reserved for that final validation.”
Data from the final validation are expected to be presented at the June 2018 EULAR meeting and ultimately published in Arthritis and Rheumatism and the Annals of Rheumatic Diseases. “Before we can get there, though, it needs to be formally reviewed by the ACR and EULAR for their formal endorsement. We expect that will take another 6 months.” She reported having no disclosures.
SAN DIEGO – yielded a sensitivity of 98% and a specificity of 97%.
The development is part of a four-phase joint effort by the American College of Rheumatology and the European League Against Rheumatism, first launched in 2014, to improve classification of patients with SLE for the purposes of clinical trials of new therapies and clinical research into the causes and outcomes of the disease. “The ACR and EULAR have long recognized the importance of classification criteria, so that we have more homogeneous groups in these research studies, and then we can compare results from studies,” Sindhu Johnson, MD, PhD, said during a press briefing at the annual meeting of the American College of Rheumatology.
A synopsis of the first three phases from the ongoing effort was presented at the June 2017 EULAR meeting. It included results from a systematic review of the literature and a meta-regression analysis to determine whether antinuclear autoantibodies should be required in the classification of SLE. The analysis showed that an antinuclear antibody titer of greater than or equal to 1:80 by immunofluorescence on human epithelial type 2 cells had a sensitivity of 98.4% for correctly capturing SLE. This prompted the EULAR/ACR steering committee to propose this titer as an “entry criterion” for SLE classification.
At the ACR meeting, Dr. Johnson, a rheumatologist at the University of Toronto who also cochairs the ACR Classification and Response Criteria subcommittee, discussed the fourth phase of the collaboration, which involves fine-tuning and validating the proposed SLE classification criteria.
To date, 189 investigators and more than 3,500 patients have contributed to the effort. “In the most recent phase, 36 international lupus centers were approached to contribute 100 cases and 100 controls,” she explained. “We then had each case independently adjudicated by three lupus experts at three different lupus centers to make sure there was consensus on the diagnosis. Next, we randomly selected 500 cases and 500 controls, resulting in a derivation cohort of 1,000 subjects to test our draft criteria system.”
Dr. Johnson and her associates found that the proposed SLE criteria had a sensitivity of 98% and a specificity of 97%, which exceeds that of the old ACR criteria. “We have defined a system of criteria which produces a measure of the relative probability that a particular case with a combination of clinical symptoms or features has SLE,” she said.
Dr. Johnson emphasized that the proposed criteria are intended for the classification of SLE, not for diagnosing the condition. “The diagnosis of lupus still remains in the hands of the physician, who will take into account all of the symptoms, signs, and other investigations,” she said. “We have identified the highest yield of those, but there will be some people who do not fulfill classification criteria yet do have a diagnosis of SLE.”
The next few weeks is a period to solicit feedback from stakeholders, after which members of the EULAR/ACR steering committee will be weighing feedback on the proposed criteria. “After that, we will see if there are any final revisions that need to be made,” Dr. Johnson said. “If we’re happy with the product, then the final validation will occur. We still have more than 1,000 patients from the validation core that has been reserved for that final validation.”
Data from the final validation are expected to be presented at the June 2018 EULAR meeting and ultimately published in Arthritis and Rheumatism and the Annals of Rheumatic Diseases. “Before we can get there, though, it needs to be formally reviewed by the ACR and EULAR for their formal endorsement. We expect that will take another 6 months.” She reported having no disclosures.
SAN DIEGO – yielded a sensitivity of 98% and a specificity of 97%.
The development is part of a four-phase joint effort by the American College of Rheumatology and the European League Against Rheumatism, first launched in 2014, to improve classification of patients with SLE for the purposes of clinical trials of new therapies and clinical research into the causes and outcomes of the disease. “The ACR and EULAR have long recognized the importance of classification criteria, so that we have more homogeneous groups in these research studies, and then we can compare results from studies,” Sindhu Johnson, MD, PhD, said during a press briefing at the annual meeting of the American College of Rheumatology.
A synopsis of the first three phases from the ongoing effort was presented at the June 2017 EULAR meeting. It included results from a systematic review of the literature and a meta-regression analysis to determine whether antinuclear autoantibodies should be required in the classification of SLE. The analysis showed that an antinuclear antibody titer of greater than or equal to 1:80 by immunofluorescence on human epithelial type 2 cells had a sensitivity of 98.4% for correctly capturing SLE. This prompted the EULAR/ACR steering committee to propose this titer as an “entry criterion” for SLE classification.
At the ACR meeting, Dr. Johnson, a rheumatologist at the University of Toronto who also cochairs the ACR Classification and Response Criteria subcommittee, discussed the fourth phase of the collaboration, which involves fine-tuning and validating the proposed SLE classification criteria.
To date, 189 investigators and more than 3,500 patients have contributed to the effort. “In the most recent phase, 36 international lupus centers were approached to contribute 100 cases and 100 controls,” she explained. “We then had each case independently adjudicated by three lupus experts at three different lupus centers to make sure there was consensus on the diagnosis. Next, we randomly selected 500 cases and 500 controls, resulting in a derivation cohort of 1,000 subjects to test our draft criteria system.”
Dr. Johnson and her associates found that the proposed SLE criteria had a sensitivity of 98% and a specificity of 97%, which exceeds that of the old ACR criteria. “We have defined a system of criteria which produces a measure of the relative probability that a particular case with a combination of clinical symptoms or features has SLE,” she said.
Dr. Johnson emphasized that the proposed criteria are intended for the classification of SLE, not for diagnosing the condition. “The diagnosis of lupus still remains in the hands of the physician, who will take into account all of the symptoms, signs, and other investigations,” she said. “We have identified the highest yield of those, but there will be some people who do not fulfill classification criteria yet do have a diagnosis of SLE.”
The next few weeks is a period to solicit feedback from stakeholders, after which members of the EULAR/ACR steering committee will be weighing feedback on the proposed criteria. “After that, we will see if there are any final revisions that need to be made,” Dr. Johnson said. “If we’re happy with the product, then the final validation will occur. We still have more than 1,000 patients from the validation core that has been reserved for that final validation.”
Data from the final validation are expected to be presented at the June 2018 EULAR meeting and ultimately published in Arthritis and Rheumatism and the Annals of Rheumatic Diseases. “Before we can get there, though, it needs to be formally reviewed by the ACR and EULAR for their formal endorsement. We expect that will take another 6 months.” She reported having no disclosures.
AT ACR 2017
For women with RA, small-joint surgery rate nearly twice that of men
SAN DIEGO – but the rate of small-joint procedures is declining for both sexes. However, no differences in rates of large-joint procedures between sexes were observed during the same time period.
Those are key findings from a retrospective study which set out to determine if there are sex differences in the incidence and trends of large- versus small-joint surgery rates in rheumatoid arthritis over time. “Why is orthopedic surgery important to rheumatology? The main reason is because it’s a surrogate for failed medical management,” lead study author Michael D. Richter, MD, said at the annual meeting of the American College of Rheumatology.
Dr. Richter, an internal medicine resident at Mayo Clinic, Rochester, Minn., said that women with RA generally present with more severe symptoms and higher rates of disability, while men have a better treatment response and a higher remission rate. For example, results from the multinational Quantitative Standard Monitoring of Patients with RA study found that remission rates were around 30% in men and 17% in women (Arthritis Res Ther. 2009;11[1]:R7). “However, a lot of these studies are criticized because it’s thought that gender can play a role in the disease measures,” he said. “By looking at joint surgery we have an objective outcome, and we can look at differences in treatment efficacy.”
Dr. Richter and his associates drew from the Rochester Epidemiology Project to identify 1,077 patients from Olmstead County, Minn., who fulfilled ACR criteria for RA between 1980 and 2013, and who were followed up until death, migration, or July 1, 2016. They classified surgeries as small joint (wrist, hand, or foot) or large joint (shoulder, elbow, hip, knee, or ankle). A majority of the patients (70%) were women. Compared with women, men were slightly older at diagnosis (a mean of 58 years vs. 55 years, respectively), were more likely to have a history of smoking (67% vs. 46%), and were more likely to have large-joint swelling upon initial presentation (49% vs. 42%). The mean follow-up was 12 years. No differences between men and women were noted in obesity, inflammatory biomarkers, or seropositivity.
During the study period, 112 patients underwent at least one small-joint surgery, 90 of whom were women (80%). The cumulative incidence of small-joint surgery at 15 years was nearly double that of men: 14.4% vs. 7.6%, respectively (P = .008). “Prior to the year 2000 there were no significant trends in the rate of small-joint surgery but it was more common in women,” he said. “After 2000 there was a significant decline for men and women (P = .002), but no significant difference between sexes.”
At the same time, 204 patients underwent at least one large-joint surgery during the time period, 141 of whom were women (69%). The cumulative incidence of large-joint surgery at 15 years was 20.2% for women and 18.8% for men, which was statistically similar (P = .55). “We saw no significant change over time in the rate of large-joint surgery from 1980 to 2016,” Dr. Richter said. “This is in contrast to what we see in the general population, where orthopedic procedures for osteoarthritis are more common.”
He acknowledged certain limitations of the study, including its retrospective design and the fact that the researchers were unable to include specific surgical indications in the analysis. “This becomes particularly important for the large-joint procedures,” he said. “We don’t know if osteoarthritis or chronic inflammatory arthritis is leading to the large-joint procedure.”
The National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Institute on Aging funded the study. Dr. Richter reported having no financial disclosures.
SAN DIEGO – but the rate of small-joint procedures is declining for both sexes. However, no differences in rates of large-joint procedures between sexes were observed during the same time period.
Those are key findings from a retrospective study which set out to determine if there are sex differences in the incidence and trends of large- versus small-joint surgery rates in rheumatoid arthritis over time. “Why is orthopedic surgery important to rheumatology? The main reason is because it’s a surrogate for failed medical management,” lead study author Michael D. Richter, MD, said at the annual meeting of the American College of Rheumatology.
Dr. Richter, an internal medicine resident at Mayo Clinic, Rochester, Minn., said that women with RA generally present with more severe symptoms and higher rates of disability, while men have a better treatment response and a higher remission rate. For example, results from the multinational Quantitative Standard Monitoring of Patients with RA study found that remission rates were around 30% in men and 17% in women (Arthritis Res Ther. 2009;11[1]:R7). “However, a lot of these studies are criticized because it’s thought that gender can play a role in the disease measures,” he said. “By looking at joint surgery we have an objective outcome, and we can look at differences in treatment efficacy.”
Dr. Richter and his associates drew from the Rochester Epidemiology Project to identify 1,077 patients from Olmstead County, Minn., who fulfilled ACR criteria for RA between 1980 and 2013, and who were followed up until death, migration, or July 1, 2016. They classified surgeries as small joint (wrist, hand, or foot) or large joint (shoulder, elbow, hip, knee, or ankle). A majority of the patients (70%) were women. Compared with women, men were slightly older at diagnosis (a mean of 58 years vs. 55 years, respectively), were more likely to have a history of smoking (67% vs. 46%), and were more likely to have large-joint swelling upon initial presentation (49% vs. 42%). The mean follow-up was 12 years. No differences between men and women were noted in obesity, inflammatory biomarkers, or seropositivity.
During the study period, 112 patients underwent at least one small-joint surgery, 90 of whom were women (80%). The cumulative incidence of small-joint surgery at 15 years was nearly double that of men: 14.4% vs. 7.6%, respectively (P = .008). “Prior to the year 2000 there were no significant trends in the rate of small-joint surgery but it was more common in women,” he said. “After 2000 there was a significant decline for men and women (P = .002), but no significant difference between sexes.”
At the same time, 204 patients underwent at least one large-joint surgery during the time period, 141 of whom were women (69%). The cumulative incidence of large-joint surgery at 15 years was 20.2% for women and 18.8% for men, which was statistically similar (P = .55). “We saw no significant change over time in the rate of large-joint surgery from 1980 to 2016,” Dr. Richter said. “This is in contrast to what we see in the general population, where orthopedic procedures for osteoarthritis are more common.”
He acknowledged certain limitations of the study, including its retrospective design and the fact that the researchers were unable to include specific surgical indications in the analysis. “This becomes particularly important for the large-joint procedures,” he said. “We don’t know if osteoarthritis or chronic inflammatory arthritis is leading to the large-joint procedure.”
The National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Institute on Aging funded the study. Dr. Richter reported having no financial disclosures.
SAN DIEGO – but the rate of small-joint procedures is declining for both sexes. However, no differences in rates of large-joint procedures between sexes were observed during the same time period.
Those are key findings from a retrospective study which set out to determine if there are sex differences in the incidence and trends of large- versus small-joint surgery rates in rheumatoid arthritis over time. “Why is orthopedic surgery important to rheumatology? The main reason is because it’s a surrogate for failed medical management,” lead study author Michael D. Richter, MD, said at the annual meeting of the American College of Rheumatology.
Dr. Richter, an internal medicine resident at Mayo Clinic, Rochester, Minn., said that women with RA generally present with more severe symptoms and higher rates of disability, while men have a better treatment response and a higher remission rate. For example, results from the multinational Quantitative Standard Monitoring of Patients with RA study found that remission rates were around 30% in men and 17% in women (Arthritis Res Ther. 2009;11[1]:R7). “However, a lot of these studies are criticized because it’s thought that gender can play a role in the disease measures,” he said. “By looking at joint surgery we have an objective outcome, and we can look at differences in treatment efficacy.”
Dr. Richter and his associates drew from the Rochester Epidemiology Project to identify 1,077 patients from Olmstead County, Minn., who fulfilled ACR criteria for RA between 1980 and 2013, and who were followed up until death, migration, or July 1, 2016. They classified surgeries as small joint (wrist, hand, or foot) or large joint (shoulder, elbow, hip, knee, or ankle). A majority of the patients (70%) were women. Compared with women, men were slightly older at diagnosis (a mean of 58 years vs. 55 years, respectively), were more likely to have a history of smoking (67% vs. 46%), and were more likely to have large-joint swelling upon initial presentation (49% vs. 42%). The mean follow-up was 12 years. No differences between men and women were noted in obesity, inflammatory biomarkers, or seropositivity.
During the study period, 112 patients underwent at least one small-joint surgery, 90 of whom were women (80%). The cumulative incidence of small-joint surgery at 15 years was nearly double that of men: 14.4% vs. 7.6%, respectively (P = .008). “Prior to the year 2000 there were no significant trends in the rate of small-joint surgery but it was more common in women,” he said. “After 2000 there was a significant decline for men and women (P = .002), but no significant difference between sexes.”
At the same time, 204 patients underwent at least one large-joint surgery during the time period, 141 of whom were women (69%). The cumulative incidence of large-joint surgery at 15 years was 20.2% for women and 18.8% for men, which was statistically similar (P = .55). “We saw no significant change over time in the rate of large-joint surgery from 1980 to 2016,” Dr. Richter said. “This is in contrast to what we see in the general population, where orthopedic procedures for osteoarthritis are more common.”
He acknowledged certain limitations of the study, including its retrospective design and the fact that the researchers were unable to include specific surgical indications in the analysis. “This becomes particularly important for the large-joint procedures,” he said. “We don’t know if osteoarthritis or chronic inflammatory arthritis is leading to the large-joint procedure.”
The National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Institute on Aging funded the study. Dr. Richter reported having no financial disclosures.
AT ACR 2017
Key clinical point: Women with RA had a higher rate of small-joint surgery, compared with men.
Major finding: The cumulative incidence of small-joint surgery was significantly higher among women, compared with men (14.4% vs. 7.6%, respectively), but there were no differences between sexes in the rates of large-joint surgery.
Study details: A retrospective, population-based study of 1,077 patients with RA.
Disclosures: The National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Institute on Aging funded the study. Dr. Richter reported having no financial disclosures.
Injectable agent found to improve knee function in OA patients
SAN DIEGO – Among patients with mild to moderate patellofemoral osteoarthritis, intra-articular administration of the novel agent TPX-100 was safe and associated with functional benefits up to 1 year, a proof-of-concept study showed.
“We don’t yet have a disease-modifying drug for osteoarthritis [OA]; that’s sort of the holy grail for researchers,” lead study author Dawn McGuire, MD, said in an interview at the annual meeting of the American College of Rheumatology. “All of the patient-reported outcome and patient function indices that we studied moved in the same direction, showing a benefit of TPX-100. I think this is very promising.”
The study consisted of two parts. In Part A, four dose cohorts ranging from 20 mg to 200 mg per injection were enrolled. There were no dose-limiting toxicities or safety concerns at any dose, and the 200-mg dose was selected dose for Part B of the study.
The median age of the 118 patients was 60 years and their median body mass index was 29.2 kg/m2. No drug-related serious adverse events and no dose-limiting toxicities occurred across doses ranging from 20 mg to 200 mg per injection. The incidence of common adverse events such as knee pain was similar between placebo- and TPX-100-treated knees.
Quantitative MRI showed no measurable between-knee differences in cartilage thickness or volume at 6 or 12 months. However, statistically significant and clinically meaningful differences in knee function were observed in favor of TPX-100-treated knees, compared with controls, including KOOS activities of daily living (P = .008 at 6 and 12 months), KOOS knee-related quality of life (P = .21 at 6 months and P = .03 at 12 months), and a significant reduction in pain going up or down stairs (P = .004 at 12 months). Subjects’ use of nonsteroidal anti-inflammatory medications declined by 63% during the study.
“In this study, we see some terrific, long-term results in knee-related core activities, which certainly were disease modifying from the patients’ perspective,” said Dr. McGuire, who noted that a phase 3 study is being planned. “In addition, patient’s pain going up and down stairs improved significantly, with a marked reduction in analgesic use. Any of us who are experienced in these tough areas of medicine know that early results can look extremely promising, but we have to do larger confirmatory studies.”
SAN DIEGO – Among patients with mild to moderate patellofemoral osteoarthritis, intra-articular administration of the novel agent TPX-100 was safe and associated with functional benefits up to 1 year, a proof-of-concept study showed.
“We don’t yet have a disease-modifying drug for osteoarthritis [OA]; that’s sort of the holy grail for researchers,” lead study author Dawn McGuire, MD, said in an interview at the annual meeting of the American College of Rheumatology. “All of the patient-reported outcome and patient function indices that we studied moved in the same direction, showing a benefit of TPX-100. I think this is very promising.”
The study consisted of two parts. In Part A, four dose cohorts ranging from 20 mg to 200 mg per injection were enrolled. There were no dose-limiting toxicities or safety concerns at any dose, and the 200-mg dose was selected dose for Part B of the study.
The median age of the 118 patients was 60 years and their median body mass index was 29.2 kg/m2. No drug-related serious adverse events and no dose-limiting toxicities occurred across doses ranging from 20 mg to 200 mg per injection. The incidence of common adverse events such as knee pain was similar between placebo- and TPX-100-treated knees.
Quantitative MRI showed no measurable between-knee differences in cartilage thickness or volume at 6 or 12 months. However, statistically significant and clinically meaningful differences in knee function were observed in favor of TPX-100-treated knees, compared with controls, including KOOS activities of daily living (P = .008 at 6 and 12 months), KOOS knee-related quality of life (P = .21 at 6 months and P = .03 at 12 months), and a significant reduction in pain going up or down stairs (P = .004 at 12 months). Subjects’ use of nonsteroidal anti-inflammatory medications declined by 63% during the study.
“In this study, we see some terrific, long-term results in knee-related core activities, which certainly were disease modifying from the patients’ perspective,” said Dr. McGuire, who noted that a phase 3 study is being planned. “In addition, patient’s pain going up and down stairs improved significantly, with a marked reduction in analgesic use. Any of us who are experienced in these tough areas of medicine know that early results can look extremely promising, but we have to do larger confirmatory studies.”
SAN DIEGO – Among patients with mild to moderate patellofemoral osteoarthritis, intra-articular administration of the novel agent TPX-100 was safe and associated with functional benefits up to 1 year, a proof-of-concept study showed.
“We don’t yet have a disease-modifying drug for osteoarthritis [OA]; that’s sort of the holy grail for researchers,” lead study author Dawn McGuire, MD, said in an interview at the annual meeting of the American College of Rheumatology. “All of the patient-reported outcome and patient function indices that we studied moved in the same direction, showing a benefit of TPX-100. I think this is very promising.”
The study consisted of two parts. In Part A, four dose cohorts ranging from 20 mg to 200 mg per injection were enrolled. There were no dose-limiting toxicities or safety concerns at any dose, and the 200-mg dose was selected dose for Part B of the study.
The median age of the 118 patients was 60 years and their median body mass index was 29.2 kg/m2. No drug-related serious adverse events and no dose-limiting toxicities occurred across doses ranging from 20 mg to 200 mg per injection. The incidence of common adverse events such as knee pain was similar between placebo- and TPX-100-treated knees.
Quantitative MRI showed no measurable between-knee differences in cartilage thickness or volume at 6 or 12 months. However, statistically significant and clinically meaningful differences in knee function were observed in favor of TPX-100-treated knees, compared with controls, including KOOS activities of daily living (P = .008 at 6 and 12 months), KOOS knee-related quality of life (P = .21 at 6 months and P = .03 at 12 months), and a significant reduction in pain going up or down stairs (P = .004 at 12 months). Subjects’ use of nonsteroidal anti-inflammatory medications declined by 63% during the study.
“In this study, we see some terrific, long-term results in knee-related core activities, which certainly were disease modifying from the patients’ perspective,” said Dr. McGuire, who noted that a phase 3 study is being planned. “In addition, patient’s pain going up and down stairs improved significantly, with a marked reduction in analgesic use. Any of us who are experienced in these tough areas of medicine know that early results can look extremely promising, but we have to do larger confirmatory studies.”
AT ACR 2017
Key clinical point:
Major finding: Statistically significant differences in knee function were observed in favor of TPX-100-treated knees, compared with controls, using Knee Injury and Osteoarthritis Outcome Score activities of daily living (P = .008 at 6 and 12 months) and a significant reduction in pain going up or down stairs (P = .004 at 12 months).
Study details: A randomized, proof-of-concept study involving 118 patients with patellofemoral knee OA.
Disclosures: OrthoTrophix sponsored the study. Dr. McGuire is chief medical officer and a cofounder of the company.
Blindness linked to HCQ use rare in rheumatic patients
SAN DIEGO – Out of a cohort of nearly 2,900 rheumatic patients, none developed blindness attributable to toxic maculopathy from using hydroxychloroquine, in a single-center retrospective study.
“That’s very reassuring,” lead study author Dilpreet K. Singh, MD, said in an interview at the annual meeting of the American College of Rheumatology. “It’s still important to be vigilant with our screening and also to take note of the hydroxychloroquine dose that they’re on, because a lot of our patients have been on hydroxychloroquine for 10 or 15 years and there may not have been a dose adjustment. It’s also important to focus on the patients’ comorbidities and get them under better control.”
In an effort to assess the prevalence of blindness in a cohort of rheumatic patients and to identify the characteristics and comorbidities of those with HCQ retinal toxicity, Dr. Singh and her associates retrospectively evaluated 2,898 patients at MetroHealth Medical Center between January 1999 and August of 2017 with diagnoses of rheumatoid arthritis, inflammatory polyarthritis, systemic lupus erythematosus, subacute cutaneous lupus, and discoid lupus erythematosus who had a prescription written for HCQ.
In all, 31 had a diagnosis of “blindness” or “toxic maculopathy,” and these cases were further assessed for patient demographics, comorbidities, use of tamoxifen, weight and dose at initiation and discontinuation of HCQ, and duration of HCQ. Nearly 70% of these patients had hypertension, about 60% had chronic kidney disease, and 35% had cataracts. The researchers confirmed that in each of the cases the blindness was not caused by HCQ ocular toxicity, but instead by stroke, preexisting macular disease, diabetic retinopathy, hypertensive retinopathy, or cataracts.
Only 3 of the 31 patients were found to have HCQ retinal toxicity, each without blindness or change in vision. Two patients had bull’s-eye maculopathy and one had HCQ toxic maculopathy. Each of the three patients had received HCQ for more than 18 years at doses that ranged from 6.3 to 8.2 mg/kg based on documented weight, and none had functional vision loss at diagnosis.
“It’s reassuring to know that there’s a very small percentage of patients that will have HCQ-related toxicity,” Dr. Singh concluded. “We should also be focusing on the comorbidities [such as] diabetes, hypertension, and stroke-related vision loss that are common in our population of rheumatic patients, because these are contributing to visual impairment and blindness.”
She reported having no disclosures.
[email protected]
SAN DIEGO – Out of a cohort of nearly 2,900 rheumatic patients, none developed blindness attributable to toxic maculopathy from using hydroxychloroquine, in a single-center retrospective study.
“That’s very reassuring,” lead study author Dilpreet K. Singh, MD, said in an interview at the annual meeting of the American College of Rheumatology. “It’s still important to be vigilant with our screening and also to take note of the hydroxychloroquine dose that they’re on, because a lot of our patients have been on hydroxychloroquine for 10 or 15 years and there may not have been a dose adjustment. It’s also important to focus on the patients’ comorbidities and get them under better control.”
In an effort to assess the prevalence of blindness in a cohort of rheumatic patients and to identify the characteristics and comorbidities of those with HCQ retinal toxicity, Dr. Singh and her associates retrospectively evaluated 2,898 patients at MetroHealth Medical Center between January 1999 and August of 2017 with diagnoses of rheumatoid arthritis, inflammatory polyarthritis, systemic lupus erythematosus, subacute cutaneous lupus, and discoid lupus erythematosus who had a prescription written for HCQ.
In all, 31 had a diagnosis of “blindness” or “toxic maculopathy,” and these cases were further assessed for patient demographics, comorbidities, use of tamoxifen, weight and dose at initiation and discontinuation of HCQ, and duration of HCQ. Nearly 70% of these patients had hypertension, about 60% had chronic kidney disease, and 35% had cataracts. The researchers confirmed that in each of the cases the blindness was not caused by HCQ ocular toxicity, but instead by stroke, preexisting macular disease, diabetic retinopathy, hypertensive retinopathy, or cataracts.
Only 3 of the 31 patients were found to have HCQ retinal toxicity, each without blindness or change in vision. Two patients had bull’s-eye maculopathy and one had HCQ toxic maculopathy. Each of the three patients had received HCQ for more than 18 years at doses that ranged from 6.3 to 8.2 mg/kg based on documented weight, and none had functional vision loss at diagnosis.
“It’s reassuring to know that there’s a very small percentage of patients that will have HCQ-related toxicity,” Dr. Singh concluded. “We should also be focusing on the comorbidities [such as] diabetes, hypertension, and stroke-related vision loss that are common in our population of rheumatic patients, because these are contributing to visual impairment and blindness.”
She reported having no disclosures.
[email protected]
SAN DIEGO – Out of a cohort of nearly 2,900 rheumatic patients, none developed blindness attributable to toxic maculopathy from using hydroxychloroquine, in a single-center retrospective study.
“That’s very reassuring,” lead study author Dilpreet K. Singh, MD, said in an interview at the annual meeting of the American College of Rheumatology. “It’s still important to be vigilant with our screening and also to take note of the hydroxychloroquine dose that they’re on, because a lot of our patients have been on hydroxychloroquine for 10 or 15 years and there may not have been a dose adjustment. It’s also important to focus on the patients’ comorbidities and get them under better control.”
In an effort to assess the prevalence of blindness in a cohort of rheumatic patients and to identify the characteristics and comorbidities of those with HCQ retinal toxicity, Dr. Singh and her associates retrospectively evaluated 2,898 patients at MetroHealth Medical Center between January 1999 and August of 2017 with diagnoses of rheumatoid arthritis, inflammatory polyarthritis, systemic lupus erythematosus, subacute cutaneous lupus, and discoid lupus erythematosus who had a prescription written for HCQ.
In all, 31 had a diagnosis of “blindness” or “toxic maculopathy,” and these cases were further assessed for patient demographics, comorbidities, use of tamoxifen, weight and dose at initiation and discontinuation of HCQ, and duration of HCQ. Nearly 70% of these patients had hypertension, about 60% had chronic kidney disease, and 35% had cataracts. The researchers confirmed that in each of the cases the blindness was not caused by HCQ ocular toxicity, but instead by stroke, preexisting macular disease, diabetic retinopathy, hypertensive retinopathy, or cataracts.
Only 3 of the 31 patients were found to have HCQ retinal toxicity, each without blindness or change in vision. Two patients had bull’s-eye maculopathy and one had HCQ toxic maculopathy. Each of the three patients had received HCQ for more than 18 years at doses that ranged from 6.3 to 8.2 mg/kg based on documented weight, and none had functional vision loss at diagnosis.
“It’s reassuring to know that there’s a very small percentage of patients that will have HCQ-related toxicity,” Dr. Singh concluded. “We should also be focusing on the comorbidities [such as] diabetes, hypertension, and stroke-related vision loss that are common in our population of rheumatic patients, because these are contributing to visual impairment and blindness.”
She reported having no disclosures.
[email protected]
AT ACR 2017
Key clinical point: The incidence of blindness due to hydroxychloroquine toxicity is very low.
Major finding: No patients developed blindness attributable to toxic maculopathy from using hydroxychloroquine.
Study details: A single-center retrospective study of 2,898 rheumatic patients.
Disclosures: Dr. Singh reported having no disclosures.
VIDEO: New PsA guideline expected in 2018
SAN DIEGO – For the first time, a forthcoming evidence-based guideline for the management of psoriatic arthritis recommends tumor necrosis factor inhibitor biologics as first-line therapy.
“Guidelines that have been around for the last several years have been skirting around the fact that there’s really no evidence that methotrexate works for PsA,” Dafna D. Gladman, MD, said during a press briefing at the annual meeting of the American College of Rheumatology. “So it’s refreshing and reassuring that when you do an appropriate, evidence-based approach, you finally find the truth in front of you, and you have TNF inhibitors as the first-line treatment. Obviously, they’re not for everybody. There are patients in whom we cannot use TNF inhibitors, either because they don’t like needles, or because they have contraindications to getting these particular needles, but at least we have a recommendation for the use of these drugs as a first-line treatment.”

“At first, I wasn’t a big fan of the idea of the GRADE guidelines because the number of questions blows up so fast, [but] it really makes you focus on what the most common [clinical] settings are,” said another core oversight team member, Alexis Ogdie, MD, a rheumatologist at the University of Pennsylvania, Philadelphia. “These guidelines also reveal the major gap of no head-to-head studies. I think we’ve known that, but this really called that out as important. When we’re making a treatment decision between [drugs] A and B, we need those studies to be able to better understand how to treat our patients, rather than using the data from one trial to make a decision. ... For my patients, I’m excited that I can now use a TNF inhibitor as a first-line agent. When we have patients come in with very severe disease, occasionally they also have severe psoriasis, so we’ve been able to use TNF inhibitors as first-line treatment in some of our patients in Pennsylvania. This differs state by state. But the exciting thing is that they get better so fast and you don’t have to tell them to wait 12 weeks for methotrexate to work.”
The ACR/NPF guideline is currently under peer review and is expected to be published in Arthritis & Rheumatology, Arthritis Care & Research, and the Journal of Psoriasis and Psoriatic Arthritis in the spring or summer of 2018. It focuses on common PsA patients, not exceptional cases. It includes recommendations on the management of patients with active PsA that is defined by the patients’ self-report and judged by the examining clinician to be caused by PsA, based on the on the presence of at least one of the following: actively inflamed joints; dactylitis; enthesitis; axial disease; active skin and/or nail involvement; and/or extra-articular manifestations such as uveitis or inflammatory bowel disease. Authors of the guideline considered cost as one of many possible factors affecting the use of the recommendations, but explicit cost-effectiveness analyses were not conducted. Also, since the NPF and the American Academy of Dermatology are concurrently developing a psoriasis treatment guideline, the treatment of skin psoriasis was not included in the guideline.
According to the guideline’s principal investigator Jasvinder Singh, MD, professor of medicine and epidemiology at the University of Alabama at Birmingham, the guideline will include 80 recommendations, 75 (94%) that are rated as “conditional,” and 5 (6%) that are rated as “strong,” based on the quality of evidence in the existing medical literature. “Most of our treatment guidelines rely on very low-to-moderate quality evidence, which means that there needs to be an active discussion between the physician and the patient with regard to which treatment to choose,” said Dr. Singh, who is also a staff rheumatologist at the Birmingham Veterans Affairs Medical Center and who led development of the 2012 and 2015 ACR treatment guidelines for RA. “When you’re not choosing the preferred treatment, there are defined specific recommendations under which that second treatment may be preferred over the first treatment.”
During a separate session at the meeting, Dr. Singh unveiled a few of the draft recommendations. One calls for using a treat-to-target strategy over not using one. In the setting of immunizing patients who are receiving a biologic, another recommendation calls for clinicians to start the indicated biologic and administer killed vaccines (as indicated) in patients with active PsA rather than delaying the biologic to give the killed vaccines. In addition, delaying the start of the indicated biologic is recommended over not delaying in order to administer a live attenuated vaccine in patients with active PsA. When patients continue to have with active PsA despite being on a TNF inhibitor, the draft guideline recommends switching to a different TNF inhibitor rather than an IL-17 inhibitor, an IL-12/IL-23 inhibitor, abatacept (Orencia), tofacitinib (Xeljanz), or adding methotrexate. If PsA is still active, the guideline recommends switching to an IL-17 inhibitor instead of an IL-12/IL-23 inhibitor, abatacept, or tofacitinib. If PsA is still active, the guideline recommends switching to an IL-12/IL-23 inhibitor over abatacept or tofacitinib.
The guideline also includes suggestions for nonpharmacologic treatments, including recommending low-impact exercise over high-impact exercise, occupational therapy, physical therapy, and weight loss. It also includes a strong recommendation to provide smoking cessation advice to patients.
Dr. Singh acknowledged significant research gaps in the current PsA medical literature, including no head-to-head comparisons of treatments. He said that the field also could benefit from specific studies for enthesitis, axial disease, and arthritis mutilans; randomized trials of nonpharmacologic interventions; more trials of monotherapy vs. combination therapy; vaccination trials for live attenuated vaccines; trials and registry studies of patients with common comorbidities, and studies of NSAIDs and glucocorticoids, to define their role.
Possible topics for future PsA guidelines, he continued, include treatment options for patients for whom biologic medication is not an option; use of therapies in pregnancy and conception; incorporation of high-quality cost or cost-effectiveness analysis into recommendations; and the role of other comorbidities, such as fibromyalgia, hepatitis, depression/anxiety, malignancy, and cardiovascular disease.
“Evidence-based medicine needs to be practiced, even in situations where it’s difficult to get a drug,” Dr. Gladman said. “One of the things we hope will happen in the near future is that companies will start doing head-to-head studies, to help us support evidence-based recommendations in the future.”
None of the speakers reported having relevant financial disclosures.
SAN DIEGO – For the first time, a forthcoming evidence-based guideline for the management of psoriatic arthritis recommends tumor necrosis factor inhibitor biologics as first-line therapy.
“Guidelines that have been around for the last several years have been skirting around the fact that there’s really no evidence that methotrexate works for PsA,” Dafna D. Gladman, MD, said during a press briefing at the annual meeting of the American College of Rheumatology. “So it’s refreshing and reassuring that when you do an appropriate, evidence-based approach, you finally find the truth in front of you, and you have TNF inhibitors as the first-line treatment. Obviously, they’re not for everybody. There are patients in whom we cannot use TNF inhibitors, either because they don’t like needles, or because they have contraindications to getting these particular needles, but at least we have a recommendation for the use of these drugs as a first-line treatment.”

“At first, I wasn’t a big fan of the idea of the GRADE guidelines because the number of questions blows up so fast, [but] it really makes you focus on what the most common [clinical] settings are,” said another core oversight team member, Alexis Ogdie, MD, a rheumatologist at the University of Pennsylvania, Philadelphia. “These guidelines also reveal the major gap of no head-to-head studies. I think we’ve known that, but this really called that out as important. When we’re making a treatment decision between [drugs] A and B, we need those studies to be able to better understand how to treat our patients, rather than using the data from one trial to make a decision. ... For my patients, I’m excited that I can now use a TNF inhibitor as a first-line agent. When we have patients come in with very severe disease, occasionally they also have severe psoriasis, so we’ve been able to use TNF inhibitors as first-line treatment in some of our patients in Pennsylvania. This differs state by state. But the exciting thing is that they get better so fast and you don’t have to tell them to wait 12 weeks for methotrexate to work.”
The ACR/NPF guideline is currently under peer review and is expected to be published in Arthritis & Rheumatology, Arthritis Care & Research, and the Journal of Psoriasis and Psoriatic Arthritis in the spring or summer of 2018. It focuses on common PsA patients, not exceptional cases. It includes recommendations on the management of patients with active PsA that is defined by the patients’ self-report and judged by the examining clinician to be caused by PsA, based on the on the presence of at least one of the following: actively inflamed joints; dactylitis; enthesitis; axial disease; active skin and/or nail involvement; and/or extra-articular manifestations such as uveitis or inflammatory bowel disease. Authors of the guideline considered cost as one of many possible factors affecting the use of the recommendations, but explicit cost-effectiveness analyses were not conducted. Also, since the NPF and the American Academy of Dermatology are concurrently developing a psoriasis treatment guideline, the treatment of skin psoriasis was not included in the guideline.
According to the guideline’s principal investigator Jasvinder Singh, MD, professor of medicine and epidemiology at the University of Alabama at Birmingham, the guideline will include 80 recommendations, 75 (94%) that are rated as “conditional,” and 5 (6%) that are rated as “strong,” based on the quality of evidence in the existing medical literature. “Most of our treatment guidelines rely on very low-to-moderate quality evidence, which means that there needs to be an active discussion between the physician and the patient with regard to which treatment to choose,” said Dr. Singh, who is also a staff rheumatologist at the Birmingham Veterans Affairs Medical Center and who led development of the 2012 and 2015 ACR treatment guidelines for RA. “When you’re not choosing the preferred treatment, there are defined specific recommendations under which that second treatment may be preferred over the first treatment.”
During a separate session at the meeting, Dr. Singh unveiled a few of the draft recommendations. One calls for using a treat-to-target strategy over not using one. In the setting of immunizing patients who are receiving a biologic, another recommendation calls for clinicians to start the indicated biologic and administer killed vaccines (as indicated) in patients with active PsA rather than delaying the biologic to give the killed vaccines. In addition, delaying the start of the indicated biologic is recommended over not delaying in order to administer a live attenuated vaccine in patients with active PsA. When patients continue to have with active PsA despite being on a TNF inhibitor, the draft guideline recommends switching to a different TNF inhibitor rather than an IL-17 inhibitor, an IL-12/IL-23 inhibitor, abatacept (Orencia), tofacitinib (Xeljanz), or adding methotrexate. If PsA is still active, the guideline recommends switching to an IL-17 inhibitor instead of an IL-12/IL-23 inhibitor, abatacept, or tofacitinib. If PsA is still active, the guideline recommends switching to an IL-12/IL-23 inhibitor over abatacept or tofacitinib.
The guideline also includes suggestions for nonpharmacologic treatments, including recommending low-impact exercise over high-impact exercise, occupational therapy, physical therapy, and weight loss. It also includes a strong recommendation to provide smoking cessation advice to patients.
Dr. Singh acknowledged significant research gaps in the current PsA medical literature, including no head-to-head comparisons of treatments. He said that the field also could benefit from specific studies for enthesitis, axial disease, and arthritis mutilans; randomized trials of nonpharmacologic interventions; more trials of monotherapy vs. combination therapy; vaccination trials for live attenuated vaccines; trials and registry studies of patients with common comorbidities, and studies of NSAIDs and glucocorticoids, to define their role.
Possible topics for future PsA guidelines, he continued, include treatment options for patients for whom biologic medication is not an option; use of therapies in pregnancy and conception; incorporation of high-quality cost or cost-effectiveness analysis into recommendations; and the role of other comorbidities, such as fibromyalgia, hepatitis, depression/anxiety, malignancy, and cardiovascular disease.
“Evidence-based medicine needs to be practiced, even in situations where it’s difficult to get a drug,” Dr. Gladman said. “One of the things we hope will happen in the near future is that companies will start doing head-to-head studies, to help us support evidence-based recommendations in the future.”
None of the speakers reported having relevant financial disclosures.
SAN DIEGO – For the first time, a forthcoming evidence-based guideline for the management of psoriatic arthritis recommends tumor necrosis factor inhibitor biologics as first-line therapy.
“Guidelines that have been around for the last several years have been skirting around the fact that there’s really no evidence that methotrexate works for PsA,” Dafna D. Gladman, MD, said during a press briefing at the annual meeting of the American College of Rheumatology. “So it’s refreshing and reassuring that when you do an appropriate, evidence-based approach, you finally find the truth in front of you, and you have TNF inhibitors as the first-line treatment. Obviously, they’re not for everybody. There are patients in whom we cannot use TNF inhibitors, either because they don’t like needles, or because they have contraindications to getting these particular needles, but at least we have a recommendation for the use of these drugs as a first-line treatment.”

“At first, I wasn’t a big fan of the idea of the GRADE guidelines because the number of questions blows up so fast, [but] it really makes you focus on what the most common [clinical] settings are,” said another core oversight team member, Alexis Ogdie, MD, a rheumatologist at the University of Pennsylvania, Philadelphia. “These guidelines also reveal the major gap of no head-to-head studies. I think we’ve known that, but this really called that out as important. When we’re making a treatment decision between [drugs] A and B, we need those studies to be able to better understand how to treat our patients, rather than using the data from one trial to make a decision. ... For my patients, I’m excited that I can now use a TNF inhibitor as a first-line agent. When we have patients come in with very severe disease, occasionally they also have severe psoriasis, so we’ve been able to use TNF inhibitors as first-line treatment in some of our patients in Pennsylvania. This differs state by state. But the exciting thing is that they get better so fast and you don’t have to tell them to wait 12 weeks for methotrexate to work.”
The ACR/NPF guideline is currently under peer review and is expected to be published in Arthritis & Rheumatology, Arthritis Care & Research, and the Journal of Psoriasis and Psoriatic Arthritis in the spring or summer of 2018. It focuses on common PsA patients, not exceptional cases. It includes recommendations on the management of patients with active PsA that is defined by the patients’ self-report and judged by the examining clinician to be caused by PsA, based on the on the presence of at least one of the following: actively inflamed joints; dactylitis; enthesitis; axial disease; active skin and/or nail involvement; and/or extra-articular manifestations such as uveitis or inflammatory bowel disease. Authors of the guideline considered cost as one of many possible factors affecting the use of the recommendations, but explicit cost-effectiveness analyses were not conducted. Also, since the NPF and the American Academy of Dermatology are concurrently developing a psoriasis treatment guideline, the treatment of skin psoriasis was not included in the guideline.
According to the guideline’s principal investigator Jasvinder Singh, MD, professor of medicine and epidemiology at the University of Alabama at Birmingham, the guideline will include 80 recommendations, 75 (94%) that are rated as “conditional,” and 5 (6%) that are rated as “strong,” based on the quality of evidence in the existing medical literature. “Most of our treatment guidelines rely on very low-to-moderate quality evidence, which means that there needs to be an active discussion between the physician and the patient with regard to which treatment to choose,” said Dr. Singh, who is also a staff rheumatologist at the Birmingham Veterans Affairs Medical Center and who led development of the 2012 and 2015 ACR treatment guidelines for RA. “When you’re not choosing the preferred treatment, there are defined specific recommendations under which that second treatment may be preferred over the first treatment.”
During a separate session at the meeting, Dr. Singh unveiled a few of the draft recommendations. One calls for using a treat-to-target strategy over not using one. In the setting of immunizing patients who are receiving a biologic, another recommendation calls for clinicians to start the indicated biologic and administer killed vaccines (as indicated) in patients with active PsA rather than delaying the biologic to give the killed vaccines. In addition, delaying the start of the indicated biologic is recommended over not delaying in order to administer a live attenuated vaccine in patients with active PsA. When patients continue to have with active PsA despite being on a TNF inhibitor, the draft guideline recommends switching to a different TNF inhibitor rather than an IL-17 inhibitor, an IL-12/IL-23 inhibitor, abatacept (Orencia), tofacitinib (Xeljanz), or adding methotrexate. If PsA is still active, the guideline recommends switching to an IL-17 inhibitor instead of an IL-12/IL-23 inhibitor, abatacept, or tofacitinib. If PsA is still active, the guideline recommends switching to an IL-12/IL-23 inhibitor over abatacept or tofacitinib.
The guideline also includes suggestions for nonpharmacologic treatments, including recommending low-impact exercise over high-impact exercise, occupational therapy, physical therapy, and weight loss. It also includes a strong recommendation to provide smoking cessation advice to patients.
Dr. Singh acknowledged significant research gaps in the current PsA medical literature, including no head-to-head comparisons of treatments. He said that the field also could benefit from specific studies for enthesitis, axial disease, and arthritis mutilans; randomized trials of nonpharmacologic interventions; more trials of monotherapy vs. combination therapy; vaccination trials for live attenuated vaccines; trials and registry studies of patients with common comorbidities, and studies of NSAIDs and glucocorticoids, to define their role.
Possible topics for future PsA guidelines, he continued, include treatment options for patients for whom biologic medication is not an option; use of therapies in pregnancy and conception; incorporation of high-quality cost or cost-effectiveness analysis into recommendations; and the role of other comorbidities, such as fibromyalgia, hepatitis, depression/anxiety, malignancy, and cardiovascular disease.
“Evidence-based medicine needs to be practiced, even in situations where it’s difficult to get a drug,” Dr. Gladman said. “One of the things we hope will happen in the near future is that companies will start doing head-to-head studies, to help us support evidence-based recommendations in the future.”
None of the speakers reported having relevant financial disclosures.
AT ACR 2017