User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Emergent colectomies for ulcerative colitis declining
LAS VEGAS – , a large database analysis has shown.
“Despite advances in medical therapy for ulcerative colitis (UC), many patients still need surgery,” Ryan C. Ungaro, MD, said at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “Prior epidemiologic studies have demonstrated a decline in colectomy rates over time, particularly comparing the pre- and postbiologic eras, but less is known about rates of emergent colectomy over time,” he said. In particular, he continued, data on UC colectomy and ileal pouch anal anastomosis (IPAA) surgery rates in the United States are limited.
In an effort to examine UC emergent colectomy rates and IPAA over time, Dr. Ungaro, of the division of gastroenterology at the Icahn School of Medicine at Mount Sinai, New York, and his associates analyzed data from the U.S. Nationwide Inpatient Sample from 2000 through 2014. They defined emergent colectomy cases as admission through the emergency department and used the ICD-9-CM code for subtotal colectomy (45.8) as the outcome variable, and defined a second cohort of UC patients admitted electively with an outcome variable of ICD-9-CM code for IPAA (45.95). To evaluate temporal trends of colectomy and IPAA, the researchers used joinpoint regression analysis with calculation of annual percentage change.
They also observed disparities in IPAA surgery rates based on race and insurance type. Specifically, whites had higher rates of elective IPAA during the study period, compared with black or Hispanic patients (P less than .01), while patients with private insurance had higher rates of elective IPAA, compared with those insured by Medicare or Medicaid (P less than .01). Dr. Ungaro acknowledged certain limitations of the study, including the fact that the Nationwide Inpatient Sample relies on administrative codes, “which may increase risk of misclassification bias,” he said. They were also unable to track individual patients across time and lacked data on medication use and disease severity.
“There has been a significant decline in emergency colectomy for ulcerative colitis in the United States,” Dr. Ungaro concluded. “We expect that this is due to more effective inpatient care. However, the overall need for surgery in UC appears to be stable given unchanged IPAA rates. This suggests a limited impact on overall surgery rates with a shift from emergent to elective procedures.” He reported having no relevant financial disclosures.
*This story was updated on 3/26.
SOURCE: Ungaro RC et al. Crohn’s & Colitis Congress, Clinical Abstract 23.
LAS VEGAS – , a large database analysis has shown.
“Despite advances in medical therapy for ulcerative colitis (UC), many patients still need surgery,” Ryan C. Ungaro, MD, said at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “Prior epidemiologic studies have demonstrated a decline in colectomy rates over time, particularly comparing the pre- and postbiologic eras, but less is known about rates of emergent colectomy over time,” he said. In particular, he continued, data on UC colectomy and ileal pouch anal anastomosis (IPAA) surgery rates in the United States are limited.
In an effort to examine UC emergent colectomy rates and IPAA over time, Dr. Ungaro, of the division of gastroenterology at the Icahn School of Medicine at Mount Sinai, New York, and his associates analyzed data from the U.S. Nationwide Inpatient Sample from 2000 through 2014. They defined emergent colectomy cases as admission through the emergency department and used the ICD-9-CM code for subtotal colectomy (45.8) as the outcome variable, and defined a second cohort of UC patients admitted electively with an outcome variable of ICD-9-CM code for IPAA (45.95). To evaluate temporal trends of colectomy and IPAA, the researchers used joinpoint regression analysis with calculation of annual percentage change.
They also observed disparities in IPAA surgery rates based on race and insurance type. Specifically, whites had higher rates of elective IPAA during the study period, compared with black or Hispanic patients (P less than .01), while patients with private insurance had higher rates of elective IPAA, compared with those insured by Medicare or Medicaid (P less than .01). Dr. Ungaro acknowledged certain limitations of the study, including the fact that the Nationwide Inpatient Sample relies on administrative codes, “which may increase risk of misclassification bias,” he said. They were also unable to track individual patients across time and lacked data on medication use and disease severity.
“There has been a significant decline in emergency colectomy for ulcerative colitis in the United States,” Dr. Ungaro concluded. “We expect that this is due to more effective inpatient care. However, the overall need for surgery in UC appears to be stable given unchanged IPAA rates. This suggests a limited impact on overall surgery rates with a shift from emergent to elective procedures.” He reported having no relevant financial disclosures.
*This story was updated on 3/26.
SOURCE: Ungaro RC et al. Crohn’s & Colitis Congress, Clinical Abstract 23.
LAS VEGAS – , a large database analysis has shown.
“Despite advances in medical therapy for ulcerative colitis (UC), many patients still need surgery,” Ryan C. Ungaro, MD, said at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “Prior epidemiologic studies have demonstrated a decline in colectomy rates over time, particularly comparing the pre- and postbiologic eras, but less is known about rates of emergent colectomy over time,” he said. In particular, he continued, data on UC colectomy and ileal pouch anal anastomosis (IPAA) surgery rates in the United States are limited.
In an effort to examine UC emergent colectomy rates and IPAA over time, Dr. Ungaro, of the division of gastroenterology at the Icahn School of Medicine at Mount Sinai, New York, and his associates analyzed data from the U.S. Nationwide Inpatient Sample from 2000 through 2014. They defined emergent colectomy cases as admission through the emergency department and used the ICD-9-CM code for subtotal colectomy (45.8) as the outcome variable, and defined a second cohort of UC patients admitted electively with an outcome variable of ICD-9-CM code for IPAA (45.95). To evaluate temporal trends of colectomy and IPAA, the researchers used joinpoint regression analysis with calculation of annual percentage change.
They also observed disparities in IPAA surgery rates based on race and insurance type. Specifically, whites had higher rates of elective IPAA during the study period, compared with black or Hispanic patients (P less than .01), while patients with private insurance had higher rates of elective IPAA, compared with those insured by Medicare or Medicaid (P less than .01). Dr. Ungaro acknowledged certain limitations of the study, including the fact that the Nationwide Inpatient Sample relies on administrative codes, “which may increase risk of misclassification bias,” he said. They were also unable to track individual patients across time and lacked data on medication use and disease severity.
“There has been a significant decline in emergency colectomy for ulcerative colitis in the United States,” Dr. Ungaro concluded. “We expect that this is due to more effective inpatient care. However, the overall need for surgery in UC appears to be stable given unchanged IPAA rates. This suggests a limited impact on overall surgery rates with a shift from emergent to elective procedures.” He reported having no relevant financial disclosures.
*This story was updated on 3/26.
SOURCE: Ungaro RC et al. Crohn’s & Colitis Congress, Clinical Abstract 23.
REPORTING FROM THE CROHN’S & COLITIS CONGRESS
Key clinical point: There has been a significant decline in emergent ulcerative colitis colectomies in the United States.
Major finding: Between 2000 and 2014, the colectomy rate among patients emergently admitted to the hospital declined more than 7% annually (P less than .05).
Study details: An analysis of 470,720 hospital admissions from the Nationwide Inpatient Sample.
Disclosures: Dr. Ungaro reported having no financial disclosures.
Source: Ungaro RC et al. Crohn’s & Colitis Congress, Clinical Abstract 23.
Three in 10 diabetic patients may have liver fibrosis
LOS ANGELES – For every 10 adult patients with type 2 diabetes, three are likely to have moderate to severe liver fibrosis, according to Kenneth Cusi, MD, FACP, FACE.
“The question is, How are we going to tackle this problem? My academic goal is that we incorporate screening for NASH [nonalcoholic steatohepatitis], or for fibrosis more specifically, in the same way we do for retinopathy or nephropathy [in diabetes], because we do have a way to treat it,” he said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease.
Dr. Cusi, chief of the division of endocrinology, diabetes, and metabolism at the University of Florida, Gainesville, predicted that obesity will become the No. 1 cause of liver transplantation. “It’s a real epidemic; you’re not seeing it because the inflexion of obesity happened just 2 decades ago,” he said. “Patients with diabetes face the greatest risk of fatty liver and of fibrosis. Untreated, it’s the equivalent of having macroalbuminuria. If you do nothing and they don’t die of cardiovascular disease, they’re going to have a good chance of getting fibrosis.”
As part of the large population-based Rotterdam study of individuals aged 45 years and older, researchers found that liver stiffness of 8 kPa or more by transient elastography was present in 5.6% of the study participants and was strongly associated with steatosis and diabetes (Hepatology. 2016;63:138-47). According to Dr. Cusi, individuals who have steatosis without diabetes face a 5%-10% risk of fibrosis, while those with steatosis and diabetes face a 15%-20% risk. “It’s well established in a number of studies that if you have fibrosis, you’re at high risk not only of cirrhosis, but also of hepatocellular carcinoma,” he said. “The key thing is not detecting fat, which is not really the target. The target is if there’s fibrosis or not.” Three ways to assess for fibrosis include MR elastography, transient elastography (which is the most commonly used), and fibrosis marker panels.
Liver fibrosis likely starts with adipose tissue dysfunction, said Dr. Cusi, who authored a review on the pathophysiology of interactions between adipose tissue and target organs in obesity and the resulting clinical implications for the management of nonalcoholic steatohepatitis (Gastroenterology. 2012;142[4]:711-25.e6). “When you have insulin-resistant, sick adipose tissue, that leads to the accumulation of fat in the liver,” he said. “. Even if you get people who are matched for BMIs [body mass indexes] between 30 and 35 kg/m2, there is a spectrum in which some individuals have very insulin-resistant adipose tissue and others less so. I would say that 1 out of 10 are metabolically healthy, and we don’t understand exactly why.”
In a recent cross-sectional analysis of 352 healthy individuals, Dr. Cusi and his associates found that intrahepatic triglyceride (IHTG) accumulation is strongly associated with adipose tissue insulin resistance, supporting the current theory of lipotoxicity as a driver of IHTG accumulation (Hepatology. 2017;65[4]:1132-44). The researchers observed that once IHTG accumulation reaches about 6%, skeletal muscle insulin resistance, hypertriglyceridemia, and low HDL cholesterol become fully established. “The next question is, How does this correlate with NASH?” Dr. Cusi said. “Our take is that there is a threshold effect. Once you have a critical amount of triglycerides in your liver, some individuals are going to activate pathways that are harmful. NASH is not something exclusive to individuals who are obese. Lean people can also develop NASH. The key feature is insulin resistance, not metabolic syndrome. Once you develop a fatty liver, your chances of NASH are comparable to that of an obese individual. The paradox is that lean individuals get a fatty liver, but when they get a fatty liver, they are at risk for NASH and for fibrosis.”
Why lean individuals develop NASH is not fully understood, but Dr. Cusi said he suspects that the problem develops at the mitochondrial level. Results from an unpublished animal model in which mice were fed a high–trans-fat diet for 24 weeks showed that the mice developed steatosis by week 8 and NASH by week 24. The mice had an increase in the tricarboxylic acid (TCA) cycle, which is typical of the NASH period, as well as an increase in ceramides. “Perhaps a unifying hypothesis would be that the development of NASH is linked to inflammation and to insulin signaling,” Dr. Cusi said. “Not surprisingly, it had a number of effects on the mitochondria, and in this animal model it decreases the TCA.” He noted that the biology of fibrosis remains unknown in humans. “What we have been familiar with is the high-triglyceride, low-HDL pattern,” he said. “If you look at how that correlates with the amount of liver fat, it is basically a threshold effect. Once you have steatosis, you don’t see much worse dyslipidemia, which is typical of these patients.”
Recently published guidance from the American Association for the Study of Liver Diseases on the diagnosis and management of nonalcoholic fatty liver disease (NAFLD) suggests that patients require a weight loss of 3%-5% to improve steatosis, but a loss of 7%-10% to improve most histologic features of NASH, including fibrosis (Hepatology. 2018;67[1]:328-57). Exercise alone may prevent or reduce steatosis, but its ability to improve other aspects of liver histology remains unknown. Bariatric surgery can be considered in otherwise eligible obese individuals with NAFLD or NASH. The procedure’s impact on fibrosis is unknown.
The AASLD practice guideline notes that metformin is not recommended for treating NASH in adult patients, but pioglitazone improves liver histology in patients with and without type 2 diabetes with biopsy-proven NASH. “Pioglitazone has had the greatest benefit in terms of treatment effect, compared to placebo,” Dr. Cusi said. “It’s a generic drug; at the VA [Veterans Affairs], it costs 8 cents per tablet. I think that pioglitazone will be to NASH what metformin has been to type 2 diabetes. The most common side effect is weight gain, typically between 4 and 9 lb. Risks and benefits should be discussed with each patient. It should not be used for NAFLD without biopsy-proven NASH.” The guideline goes on to say that it’s currently premature to consider GLP-1 (glucagonlike peptide–1) agonists for treating liver disease in patients with NAFLD or NASH. Meanwhile, vitamin E at 800 IU has been shown to improve liver histology in nondiabetic adults with NASH, but the risks and benefits should be discussed with each patient. Vitamin E is not recommended for NASH in diabetic patients, NAFLD without a liver biopsy, NASH cirrhosis, or cryptogenic cirrhosis.
The AASLD practice guideline also states that the best evidence for using SGLT2 (sodium-glucose cotransporter–2) inhibitors in NAFLD comes from animal studies, which report a reduction in steatosis with and without weight loss. Clinical studies reporting a reduction in steatosis are limited. There are positive observational studies with a reduction in alanine aminotransferase and some studies that have shown a reduction in liver fat. “For me, the best option is to tailor treatment to the pathophysiology of the disease,” Dr. Cusi said. “You reduce fat by weight loss in some way, or you change the biology of fat with a thiazolidinedione.”
Dr. Cusi reported that he has received grant support from the Burroughs Wellcome Fund, the American Diabetes Association, and the National Institutes of Health.
LOS ANGELES – For every 10 adult patients with type 2 diabetes, three are likely to have moderate to severe liver fibrosis, according to Kenneth Cusi, MD, FACP, FACE.
“The question is, How are we going to tackle this problem? My academic goal is that we incorporate screening for NASH [nonalcoholic steatohepatitis], or for fibrosis more specifically, in the same way we do for retinopathy or nephropathy [in diabetes], because we do have a way to treat it,” he said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease.
Dr. Cusi, chief of the division of endocrinology, diabetes, and metabolism at the University of Florida, Gainesville, predicted that obesity will become the No. 1 cause of liver transplantation. “It’s a real epidemic; you’re not seeing it because the inflexion of obesity happened just 2 decades ago,” he said. “Patients with diabetes face the greatest risk of fatty liver and of fibrosis. Untreated, it’s the equivalent of having macroalbuminuria. If you do nothing and they don’t die of cardiovascular disease, they’re going to have a good chance of getting fibrosis.”
As part of the large population-based Rotterdam study of individuals aged 45 years and older, researchers found that liver stiffness of 8 kPa or more by transient elastography was present in 5.6% of the study participants and was strongly associated with steatosis and diabetes (Hepatology. 2016;63:138-47). According to Dr. Cusi, individuals who have steatosis without diabetes face a 5%-10% risk of fibrosis, while those with steatosis and diabetes face a 15%-20% risk. “It’s well established in a number of studies that if you have fibrosis, you’re at high risk not only of cirrhosis, but also of hepatocellular carcinoma,” he said. “The key thing is not detecting fat, which is not really the target. The target is if there’s fibrosis or not.” Three ways to assess for fibrosis include MR elastography, transient elastography (which is the most commonly used), and fibrosis marker panels.
Liver fibrosis likely starts with adipose tissue dysfunction, said Dr. Cusi, who authored a review on the pathophysiology of interactions between adipose tissue and target organs in obesity and the resulting clinical implications for the management of nonalcoholic steatohepatitis (Gastroenterology. 2012;142[4]:711-25.e6). “When you have insulin-resistant, sick adipose tissue, that leads to the accumulation of fat in the liver,” he said. “. Even if you get people who are matched for BMIs [body mass indexes] between 30 and 35 kg/m2, there is a spectrum in which some individuals have very insulin-resistant adipose tissue and others less so. I would say that 1 out of 10 are metabolically healthy, and we don’t understand exactly why.”
In a recent cross-sectional analysis of 352 healthy individuals, Dr. Cusi and his associates found that intrahepatic triglyceride (IHTG) accumulation is strongly associated with adipose tissue insulin resistance, supporting the current theory of lipotoxicity as a driver of IHTG accumulation (Hepatology. 2017;65[4]:1132-44). The researchers observed that once IHTG accumulation reaches about 6%, skeletal muscle insulin resistance, hypertriglyceridemia, and low HDL cholesterol become fully established. “The next question is, How does this correlate with NASH?” Dr. Cusi said. “Our take is that there is a threshold effect. Once you have a critical amount of triglycerides in your liver, some individuals are going to activate pathways that are harmful. NASH is not something exclusive to individuals who are obese. Lean people can also develop NASH. The key feature is insulin resistance, not metabolic syndrome. Once you develop a fatty liver, your chances of NASH are comparable to that of an obese individual. The paradox is that lean individuals get a fatty liver, but when they get a fatty liver, they are at risk for NASH and for fibrosis.”
Why lean individuals develop NASH is not fully understood, but Dr. Cusi said he suspects that the problem develops at the mitochondrial level. Results from an unpublished animal model in which mice were fed a high–trans-fat diet for 24 weeks showed that the mice developed steatosis by week 8 and NASH by week 24. The mice had an increase in the tricarboxylic acid (TCA) cycle, which is typical of the NASH period, as well as an increase in ceramides. “Perhaps a unifying hypothesis would be that the development of NASH is linked to inflammation and to insulin signaling,” Dr. Cusi said. “Not surprisingly, it had a number of effects on the mitochondria, and in this animal model it decreases the TCA.” He noted that the biology of fibrosis remains unknown in humans. “What we have been familiar with is the high-triglyceride, low-HDL pattern,” he said. “If you look at how that correlates with the amount of liver fat, it is basically a threshold effect. Once you have steatosis, you don’t see much worse dyslipidemia, which is typical of these patients.”
Recently published guidance from the American Association for the Study of Liver Diseases on the diagnosis and management of nonalcoholic fatty liver disease (NAFLD) suggests that patients require a weight loss of 3%-5% to improve steatosis, but a loss of 7%-10% to improve most histologic features of NASH, including fibrosis (Hepatology. 2018;67[1]:328-57). Exercise alone may prevent or reduce steatosis, but its ability to improve other aspects of liver histology remains unknown. Bariatric surgery can be considered in otherwise eligible obese individuals with NAFLD or NASH. The procedure’s impact on fibrosis is unknown.
The AASLD practice guideline notes that metformin is not recommended for treating NASH in adult patients, but pioglitazone improves liver histology in patients with and without type 2 diabetes with biopsy-proven NASH. “Pioglitazone has had the greatest benefit in terms of treatment effect, compared to placebo,” Dr. Cusi said. “It’s a generic drug; at the VA [Veterans Affairs], it costs 8 cents per tablet. I think that pioglitazone will be to NASH what metformin has been to type 2 diabetes. The most common side effect is weight gain, typically between 4 and 9 lb. Risks and benefits should be discussed with each patient. It should not be used for NAFLD without biopsy-proven NASH.” The guideline goes on to say that it’s currently premature to consider GLP-1 (glucagonlike peptide–1) agonists for treating liver disease in patients with NAFLD or NASH. Meanwhile, vitamin E at 800 IU has been shown to improve liver histology in nondiabetic adults with NASH, but the risks and benefits should be discussed with each patient. Vitamin E is not recommended for NASH in diabetic patients, NAFLD without a liver biopsy, NASH cirrhosis, or cryptogenic cirrhosis.
The AASLD practice guideline also states that the best evidence for using SGLT2 (sodium-glucose cotransporter–2) inhibitors in NAFLD comes from animal studies, which report a reduction in steatosis with and without weight loss. Clinical studies reporting a reduction in steatosis are limited. There are positive observational studies with a reduction in alanine aminotransferase and some studies that have shown a reduction in liver fat. “For me, the best option is to tailor treatment to the pathophysiology of the disease,” Dr. Cusi said. “You reduce fat by weight loss in some way, or you change the biology of fat with a thiazolidinedione.”
Dr. Cusi reported that he has received grant support from the Burroughs Wellcome Fund, the American Diabetes Association, and the National Institutes of Health.
LOS ANGELES – For every 10 adult patients with type 2 diabetes, three are likely to have moderate to severe liver fibrosis, according to Kenneth Cusi, MD, FACP, FACE.
“The question is, How are we going to tackle this problem? My academic goal is that we incorporate screening for NASH [nonalcoholic steatohepatitis], or for fibrosis more specifically, in the same way we do for retinopathy or nephropathy [in diabetes], because we do have a way to treat it,” he said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease.
Dr. Cusi, chief of the division of endocrinology, diabetes, and metabolism at the University of Florida, Gainesville, predicted that obesity will become the No. 1 cause of liver transplantation. “It’s a real epidemic; you’re not seeing it because the inflexion of obesity happened just 2 decades ago,” he said. “Patients with diabetes face the greatest risk of fatty liver and of fibrosis. Untreated, it’s the equivalent of having macroalbuminuria. If you do nothing and they don’t die of cardiovascular disease, they’re going to have a good chance of getting fibrosis.”
As part of the large population-based Rotterdam study of individuals aged 45 years and older, researchers found that liver stiffness of 8 kPa or more by transient elastography was present in 5.6% of the study participants and was strongly associated with steatosis and diabetes (Hepatology. 2016;63:138-47). According to Dr. Cusi, individuals who have steatosis without diabetes face a 5%-10% risk of fibrosis, while those with steatosis and diabetes face a 15%-20% risk. “It’s well established in a number of studies that if you have fibrosis, you’re at high risk not only of cirrhosis, but also of hepatocellular carcinoma,” he said. “The key thing is not detecting fat, which is not really the target. The target is if there’s fibrosis or not.” Three ways to assess for fibrosis include MR elastography, transient elastography (which is the most commonly used), and fibrosis marker panels.
Liver fibrosis likely starts with adipose tissue dysfunction, said Dr. Cusi, who authored a review on the pathophysiology of interactions between adipose tissue and target organs in obesity and the resulting clinical implications for the management of nonalcoholic steatohepatitis (Gastroenterology. 2012;142[4]:711-25.e6). “When you have insulin-resistant, sick adipose tissue, that leads to the accumulation of fat in the liver,” he said. “. Even if you get people who are matched for BMIs [body mass indexes] between 30 and 35 kg/m2, there is a spectrum in which some individuals have very insulin-resistant adipose tissue and others less so. I would say that 1 out of 10 are metabolically healthy, and we don’t understand exactly why.”
In a recent cross-sectional analysis of 352 healthy individuals, Dr. Cusi and his associates found that intrahepatic triglyceride (IHTG) accumulation is strongly associated with adipose tissue insulin resistance, supporting the current theory of lipotoxicity as a driver of IHTG accumulation (Hepatology. 2017;65[4]:1132-44). The researchers observed that once IHTG accumulation reaches about 6%, skeletal muscle insulin resistance, hypertriglyceridemia, and low HDL cholesterol become fully established. “The next question is, How does this correlate with NASH?” Dr. Cusi said. “Our take is that there is a threshold effect. Once you have a critical amount of triglycerides in your liver, some individuals are going to activate pathways that are harmful. NASH is not something exclusive to individuals who are obese. Lean people can also develop NASH. The key feature is insulin resistance, not metabolic syndrome. Once you develop a fatty liver, your chances of NASH are comparable to that of an obese individual. The paradox is that lean individuals get a fatty liver, but when they get a fatty liver, they are at risk for NASH and for fibrosis.”
Why lean individuals develop NASH is not fully understood, but Dr. Cusi said he suspects that the problem develops at the mitochondrial level. Results from an unpublished animal model in which mice were fed a high–trans-fat diet for 24 weeks showed that the mice developed steatosis by week 8 and NASH by week 24. The mice had an increase in the tricarboxylic acid (TCA) cycle, which is typical of the NASH period, as well as an increase in ceramides. “Perhaps a unifying hypothesis would be that the development of NASH is linked to inflammation and to insulin signaling,” Dr. Cusi said. “Not surprisingly, it had a number of effects on the mitochondria, and in this animal model it decreases the TCA.” He noted that the biology of fibrosis remains unknown in humans. “What we have been familiar with is the high-triglyceride, low-HDL pattern,” he said. “If you look at how that correlates with the amount of liver fat, it is basically a threshold effect. Once you have steatosis, you don’t see much worse dyslipidemia, which is typical of these patients.”
Recently published guidance from the American Association for the Study of Liver Diseases on the diagnosis and management of nonalcoholic fatty liver disease (NAFLD) suggests that patients require a weight loss of 3%-5% to improve steatosis, but a loss of 7%-10% to improve most histologic features of NASH, including fibrosis (Hepatology. 2018;67[1]:328-57). Exercise alone may prevent or reduce steatosis, but its ability to improve other aspects of liver histology remains unknown. Bariatric surgery can be considered in otherwise eligible obese individuals with NAFLD or NASH. The procedure’s impact on fibrosis is unknown.
The AASLD practice guideline notes that metformin is not recommended for treating NASH in adult patients, but pioglitazone improves liver histology in patients with and without type 2 diabetes with biopsy-proven NASH. “Pioglitazone has had the greatest benefit in terms of treatment effect, compared to placebo,” Dr. Cusi said. “It’s a generic drug; at the VA [Veterans Affairs], it costs 8 cents per tablet. I think that pioglitazone will be to NASH what metformin has been to type 2 diabetes. The most common side effect is weight gain, typically between 4 and 9 lb. Risks and benefits should be discussed with each patient. It should not be used for NAFLD without biopsy-proven NASH.” The guideline goes on to say that it’s currently premature to consider GLP-1 (glucagonlike peptide–1) agonists for treating liver disease in patients with NAFLD or NASH. Meanwhile, vitamin E at 800 IU has been shown to improve liver histology in nondiabetic adults with NASH, but the risks and benefits should be discussed with each patient. Vitamin E is not recommended for NASH in diabetic patients, NAFLD without a liver biopsy, NASH cirrhosis, or cryptogenic cirrhosis.
The AASLD practice guideline also states that the best evidence for using SGLT2 (sodium-glucose cotransporter–2) inhibitors in NAFLD comes from animal studies, which report a reduction in steatosis with and without weight loss. Clinical studies reporting a reduction in steatosis are limited. There are positive observational studies with a reduction in alanine aminotransferase and some studies that have shown a reduction in liver fat. “For me, the best option is to tailor treatment to the pathophysiology of the disease,” Dr. Cusi said. “You reduce fat by weight loss in some way, or you change the biology of fat with a thiazolidinedione.”
Dr. Cusi reported that he has received grant support from the Burroughs Wellcome Fund, the American Diabetes Association, and the National Institutes of Health.
EXPERT ANALYSIS FROM WCIRDC 2017
Study IDs predictors of nonmelanoma skin cancer in IBD
LAS VEGAS – , a large national analysis showed.
“Some studies have shown that patients with IBD may be at increased risk for nonmelanoma skin cancer (NMSC) because of the immunomodulators that they take for the management of their disease,” Zubair Khan, MD, said in an interview at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “But these are mostly small, single-center studies.” In an effort to determine the epidemiology of NMSC in patients hospitalized with IBD, Dr. Khan, associate chief resident in the internal medicine department at the University of Toledo (Ohio) Medical Center and his associates analyzed the National Inpatient Sample (NIS) database for all subjects who had a primary or secondary discharge diagnosis of IBD during 2002-2014. Next, they used ICD-9 codes to identify the rate of NMSC in this population.
Compared with IBD patients without NMSC, most of the IBD patients with NMSC were males (54% vs. 42%; P less than 0.001), covered by Medicare (65% vs. 37%), were white (96% vs. 81%; P less than .001), lived in the Midwest or Western United States (27% and 26% vs. 22% and 17%), were admitted to urban teaching hospitals (57% vs. 51%; P less than .001), were discharged to skilled nursing facilities (16% vs. 10%; P less than .001), required home health care (17% vs. 11%), and were admitted electively (27% vs. 20%). The researchers observed no significant difference in mortality among IBD patients with and without NMSC (1.61% vs. 1.53%; P = .22).
Multivariate analysis revealed that the following factors were predictive of NMSC in IBD: comorbid diagnosis of rheumatoid arthritis, collagen vasculature diseases, male sex, and white race. “Patients with those risk factors should be made more aware of their risk for developing NMSC,” Dr. Khan said. “They shouldn’t be taken lightly.”
Dr. Khan reported having no financial disclosures.
*This story was updated on 3/26.
SOURCE: Khan Z et al. Crohn’s & Colitis Congress, Poster 209.
LAS VEGAS – , a large national analysis showed.
“Some studies have shown that patients with IBD may be at increased risk for nonmelanoma skin cancer (NMSC) because of the immunomodulators that they take for the management of their disease,” Zubair Khan, MD, said in an interview at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “But these are mostly small, single-center studies.” In an effort to determine the epidemiology of NMSC in patients hospitalized with IBD, Dr. Khan, associate chief resident in the internal medicine department at the University of Toledo (Ohio) Medical Center and his associates analyzed the National Inpatient Sample (NIS) database for all subjects who had a primary or secondary discharge diagnosis of IBD during 2002-2014. Next, they used ICD-9 codes to identify the rate of NMSC in this population.
Compared with IBD patients without NMSC, most of the IBD patients with NMSC were males (54% vs. 42%; P less than 0.001), covered by Medicare (65% vs. 37%), were white (96% vs. 81%; P less than .001), lived in the Midwest or Western United States (27% and 26% vs. 22% and 17%), were admitted to urban teaching hospitals (57% vs. 51%; P less than .001), were discharged to skilled nursing facilities (16% vs. 10%; P less than .001), required home health care (17% vs. 11%), and were admitted electively (27% vs. 20%). The researchers observed no significant difference in mortality among IBD patients with and without NMSC (1.61% vs. 1.53%; P = .22).
Multivariate analysis revealed that the following factors were predictive of NMSC in IBD: comorbid diagnosis of rheumatoid arthritis, collagen vasculature diseases, male sex, and white race. “Patients with those risk factors should be made more aware of their risk for developing NMSC,” Dr. Khan said. “They shouldn’t be taken lightly.”
Dr. Khan reported having no financial disclosures.
*This story was updated on 3/26.
SOURCE: Khan Z et al. Crohn’s & Colitis Congress, Poster 209.
LAS VEGAS – , a large national analysis showed.
“Some studies have shown that patients with IBD may be at increased risk for nonmelanoma skin cancer (NMSC) because of the immunomodulators that they take for the management of their disease,” Zubair Khan, MD, said in an interview at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “But these are mostly small, single-center studies.” In an effort to determine the epidemiology of NMSC in patients hospitalized with IBD, Dr. Khan, associate chief resident in the internal medicine department at the University of Toledo (Ohio) Medical Center and his associates analyzed the National Inpatient Sample (NIS) database for all subjects who had a primary or secondary discharge diagnosis of IBD during 2002-2014. Next, they used ICD-9 codes to identify the rate of NMSC in this population.
Compared with IBD patients without NMSC, most of the IBD patients with NMSC were males (54% vs. 42%; P less than 0.001), covered by Medicare (65% vs. 37%), were white (96% vs. 81%; P less than .001), lived in the Midwest or Western United States (27% and 26% vs. 22% and 17%), were admitted to urban teaching hospitals (57% vs. 51%; P less than .001), were discharged to skilled nursing facilities (16% vs. 10%; P less than .001), required home health care (17% vs. 11%), and were admitted electively (27% vs. 20%). The researchers observed no significant difference in mortality among IBD patients with and without NMSC (1.61% vs. 1.53%; P = .22).
Multivariate analysis revealed that the following factors were predictive of NMSC in IBD: comorbid diagnosis of rheumatoid arthritis, collagen vasculature diseases, male sex, and white race. “Patients with those risk factors should be made more aware of their risk for developing NMSC,” Dr. Khan said. “They shouldn’t be taken lightly.”
Dr. Khan reported having no financial disclosures.
*This story was updated on 3/26.
SOURCE: Khan Z et al. Crohn’s & Colitis Congress, Poster 209.
REPORTING FROM THE CROHN’S & COLITIS CONGRESS
Key clinical point: Many factors predict which IBD patients are at risk for developing nonmelanoma skin cancer.
Major finding: Compared with IBD patients without NMSC, most of the IBD patients with NMSC were males (54% vs. 42%; P less than .001) and white (96% vs. 81%; P less than .001).
Study details: An analysis of 22,620 patients who had a primary or secondary discharge diagnosis of IBD during 2002-2014.
Disclosures: Dr. Khan reported having no financial disclosures.
Source: Khan Z et al. Crohn’s & Colitis Congress, Poster 209.
Three in 10 of your diabetic patients may have liver fibrosis
LOS ANGELES – For every 10 of your adult patients with type 2 diabetes, three are likely to have moderate to severe liver fibrosis, according to Kenneth Cusi, MD, FACP, FACE.
“If in the last 10 patients, you didn’t diagnose anybody with fibrosis, you probably missed it,” he said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “The question is, How are we going to tackle this problem? My academic goal is that we incorporate screening for NASH [nonalcoholic steatohepatitis], or for fibrosis more specifically, in the same way we do for retinopathy or nephropathy, because we do have a way to treat it.”
As part of the large population-based Rotterdam study of individuals aged 45 years and older, researchers found that liver stiffness of 8 kPa or more by transient elastography was present in 5.6% of the study participants and was strongly associated with steatosis and diabetes (Hepatology. 2016;63:138-47). According to Dr. Cusi, individuals who have steatosis without diabetes face a 5%-10% risk of fibrosis, while those with steatosis and diabetes face a 15%-20% risk.
“It’s well established in a number of studies that if you have fibrosis, you’re at high risk not only of cirrhosis, but also of hepatocellular carcinoma,” he said. “The key thing is not detecting fat, which is not really the target. The target is if there’s fibrosis or not.” Three ways to assess for fibrosis include MR elastography, transient elastography (which is the most commonly used), and fibrosis marker panels.
Liver fibrosis likely starts with adipose tissue dysfunction, said Dr. Cusi, who authored a review on the pathophysiology of interactions between adipose tissue and target organs in obesity and the resulting clinical implications for the management of nonalcoholic steatohepatitis (Gastroenterology. 2012;142[4]:711-25.e6).
“When you have insulin-resistant, sick adipose tissue, that leads to the accumulation of fat in the liver,” he said. “. Even if you get people who are matched for BMIs [body mass indexes] between 30 and 35 kg/m2, there is a spectrum in which some individuals have very insulin-resistant adipose tissue and others less so. I would say that 1 out of 10 are metabolically healthy, and we don’t understand exactly why.”
In a recent cross-sectional analysis of 352 healthy individuals, Dr. Cusi and his associates found that intrahepatic triglyceride (IHTG) accumulation is strongly associated with adipose tissue insulin resistance, supporting the current theory of lipotoxicity as a driver of IHTG accumulation (Hepatology. 2017;65[4]:1132-44). The researchers observed that once IHTG accumulation reaches about 6%, skeletal muscle insulin resistance, hypertriglyceridemia, and low HDL cholesterol become fully established.
“The next question is, How does this correlate with NASH?” Dr. Cusi said. “Our take is that there is a threshold effect. Once you have a critical amount of triglycerides in your liver, some individuals are going to activate pathways that are harmful. NASH is not something exclusive to individuals who are obese. Lean people can also develop NASH. The key feature is insulin resistance, not metabolic syndrome. Once you develop a fatty liver, your chances of NASH are comparable to that of an obese individual. The paradox is that lean individuals get a fatty liver, but when they get a fatty liver, they are at risk for NASH and for fibrosis.”
Why lean individuals develop NASH is not fully understood, but Dr. Cusi said he suspects that the problem develops at the mitochondrial level.
Results from an unpublished animal model in which mice were fed a high–trans-fat diet for 24 weeks showed that the mice developed steatosis by week 8 and NASH by week 24. The mice had an increase in the tricarboxylic acid (TCA) cycle, which is typical of the NASH period, as well as an increase in ceramides.
“Perhaps a unifying hypothesis would be that the development of NASH is linked to inflammation and to insulin signaling,” Dr. Cusi said. “Not surprisingly, it had a number of effects on the mitochondria, and in this animal model it decreases the TCA.” He noted that the biology of fibrosis remains unknown in humans. “What we have been familiar with is the high-triglyceride, low-HDL pattern,” he said. “If you look at how that correlates with the amount of liver fat, it is basically a threshold effect. Once you have steatosis, you don’t see much worse dyslipidemia, which is typical of these patients.”
Recently published guidance from the American Association for the Study of Liver Diseases on the diagnosis and management of nonalcoholic fatty liver disease (NAFLD) suggests that patients require a weight loss of 3%-5% to improve steatosis, but a loss of 7%-10% to improve most histologic features of NASH, including fibrosis (Hepatology. 2018;67[1]:328-57). Exercise alone may prevent or reduce steatosis, but its ability to improve other aspects of liver histology remains unknown. Bariatric surgery can be considered in otherwise eligible obese individuals with NAFLD or NASH. The procedure’s impact on fibrosis is unknown.
The AASLD practice guideline notes that metformin is not recommended for treating NASH in adult patients, but pioglitazone improves liver histology in patients with and without type 2 diabetes with biopsy-proven NASH.
“Pioglitazone has had the greatest benefit in terms of treatment effect, compared to placebo,” Dr. Cusi said. “It’s a generic drug; at the VA [Veterans Affairs], it costs 8 cents per tablet. I think that pioglitazone will be to NASH what metformin has been to type 2 diabetes. The most common side effect is weight gain, typically between 4 and 9 lb. Risks and benefits should be discussed with each patient. It should not be used for NAFLD without biopsy-proven NASH.”
The guideline goes on to say that it’s currently premature to consider GLP-1 (glucagonlike peptide–1) agonists for treating liver disease in patients with NAFLD or NASH. Meanwhile, vitamin E at 800 IU has been shown to improve liver histology in nondiabetic adults with NASH, but the risks and benefits should be discussed with each patient. Vitamin E is not recommended for NASH in diabetic patients, NAFLD without a liver biopsy, NASH cirrhosis, or cryptogenic cirrhosis.
The AASLD practice guideline also states that the best evidence for using SGLT2 (sodium-glucose cotransporter–2) inhibitors in NAFLD comes from animal studies, which report a reduction in steatosis with and without weight loss. Clinical studies reporting a reduction in steatosis are limited. There are positive observational studies with a reduction in alanine aminotransferase and some studies that have shown a reduction in liver fat. “For me, the best option is to tailor treatment to the pathophysiology of the disease,” Dr. Cusi said. “You reduce fat by weight loss in some way, or you change the biology of fat with a thiazolidinedione.”
Dr. Cusi reported that he has received grant support from the Burroughs Wellcome Fund, the American Diabetes Association, and the National Institutes of Health.
LOS ANGELES – For every 10 of your adult patients with type 2 diabetes, three are likely to have moderate to severe liver fibrosis, according to Kenneth Cusi, MD, FACP, FACE.
“If in the last 10 patients, you didn’t diagnose anybody with fibrosis, you probably missed it,” he said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “The question is, How are we going to tackle this problem? My academic goal is that we incorporate screening for NASH [nonalcoholic steatohepatitis], or for fibrosis more specifically, in the same way we do for retinopathy or nephropathy, because we do have a way to treat it.”
As part of the large population-based Rotterdam study of individuals aged 45 years and older, researchers found that liver stiffness of 8 kPa or more by transient elastography was present in 5.6% of the study participants and was strongly associated with steatosis and diabetes (Hepatology. 2016;63:138-47). According to Dr. Cusi, individuals who have steatosis without diabetes face a 5%-10% risk of fibrosis, while those with steatosis and diabetes face a 15%-20% risk.
“It’s well established in a number of studies that if you have fibrosis, you’re at high risk not only of cirrhosis, but also of hepatocellular carcinoma,” he said. “The key thing is not detecting fat, which is not really the target. The target is if there’s fibrosis or not.” Three ways to assess for fibrosis include MR elastography, transient elastography (which is the most commonly used), and fibrosis marker panels.
Liver fibrosis likely starts with adipose tissue dysfunction, said Dr. Cusi, who authored a review on the pathophysiology of interactions between adipose tissue and target organs in obesity and the resulting clinical implications for the management of nonalcoholic steatohepatitis (Gastroenterology. 2012;142[4]:711-25.e6).
“When you have insulin-resistant, sick adipose tissue, that leads to the accumulation of fat in the liver,” he said. “. Even if you get people who are matched for BMIs [body mass indexes] between 30 and 35 kg/m2, there is a spectrum in which some individuals have very insulin-resistant adipose tissue and others less so. I would say that 1 out of 10 are metabolically healthy, and we don’t understand exactly why.”
In a recent cross-sectional analysis of 352 healthy individuals, Dr. Cusi and his associates found that intrahepatic triglyceride (IHTG) accumulation is strongly associated with adipose tissue insulin resistance, supporting the current theory of lipotoxicity as a driver of IHTG accumulation (Hepatology. 2017;65[4]:1132-44). The researchers observed that once IHTG accumulation reaches about 6%, skeletal muscle insulin resistance, hypertriglyceridemia, and low HDL cholesterol become fully established.
“The next question is, How does this correlate with NASH?” Dr. Cusi said. “Our take is that there is a threshold effect. Once you have a critical amount of triglycerides in your liver, some individuals are going to activate pathways that are harmful. NASH is not something exclusive to individuals who are obese. Lean people can also develop NASH. The key feature is insulin resistance, not metabolic syndrome. Once you develop a fatty liver, your chances of NASH are comparable to that of an obese individual. The paradox is that lean individuals get a fatty liver, but when they get a fatty liver, they are at risk for NASH and for fibrosis.”
Why lean individuals develop NASH is not fully understood, but Dr. Cusi said he suspects that the problem develops at the mitochondrial level.
Results from an unpublished animal model in which mice were fed a high–trans-fat diet for 24 weeks showed that the mice developed steatosis by week 8 and NASH by week 24. The mice had an increase in the tricarboxylic acid (TCA) cycle, which is typical of the NASH period, as well as an increase in ceramides.
“Perhaps a unifying hypothesis would be that the development of NASH is linked to inflammation and to insulin signaling,” Dr. Cusi said. “Not surprisingly, it had a number of effects on the mitochondria, and in this animal model it decreases the TCA.” He noted that the biology of fibrosis remains unknown in humans. “What we have been familiar with is the high-triglyceride, low-HDL pattern,” he said. “If you look at how that correlates with the amount of liver fat, it is basically a threshold effect. Once you have steatosis, you don’t see much worse dyslipidemia, which is typical of these patients.”
Recently published guidance from the American Association for the Study of Liver Diseases on the diagnosis and management of nonalcoholic fatty liver disease (NAFLD) suggests that patients require a weight loss of 3%-5% to improve steatosis, but a loss of 7%-10% to improve most histologic features of NASH, including fibrosis (Hepatology. 2018;67[1]:328-57). Exercise alone may prevent or reduce steatosis, but its ability to improve other aspects of liver histology remains unknown. Bariatric surgery can be considered in otherwise eligible obese individuals with NAFLD or NASH. The procedure’s impact on fibrosis is unknown.
The AASLD practice guideline notes that metformin is not recommended for treating NASH in adult patients, but pioglitazone improves liver histology in patients with and without type 2 diabetes with biopsy-proven NASH.
“Pioglitazone has had the greatest benefit in terms of treatment effect, compared to placebo,” Dr. Cusi said. “It’s a generic drug; at the VA [Veterans Affairs], it costs 8 cents per tablet. I think that pioglitazone will be to NASH what metformin has been to type 2 diabetes. The most common side effect is weight gain, typically between 4 and 9 lb. Risks and benefits should be discussed with each patient. It should not be used for NAFLD without biopsy-proven NASH.”
The guideline goes on to say that it’s currently premature to consider GLP-1 (glucagonlike peptide–1) agonists for treating liver disease in patients with NAFLD or NASH. Meanwhile, vitamin E at 800 IU has been shown to improve liver histology in nondiabetic adults with NASH, but the risks and benefits should be discussed with each patient. Vitamin E is not recommended for NASH in diabetic patients, NAFLD without a liver biopsy, NASH cirrhosis, or cryptogenic cirrhosis.
The AASLD practice guideline also states that the best evidence for using SGLT2 (sodium-glucose cotransporter–2) inhibitors in NAFLD comes from animal studies, which report a reduction in steatosis with and without weight loss. Clinical studies reporting a reduction in steatosis are limited. There are positive observational studies with a reduction in alanine aminotransferase and some studies that have shown a reduction in liver fat. “For me, the best option is to tailor treatment to the pathophysiology of the disease,” Dr. Cusi said. “You reduce fat by weight loss in some way, or you change the biology of fat with a thiazolidinedione.”
Dr. Cusi reported that he has received grant support from the Burroughs Wellcome Fund, the American Diabetes Association, and the National Institutes of Health.
LOS ANGELES – For every 10 of your adult patients with type 2 diabetes, three are likely to have moderate to severe liver fibrosis, according to Kenneth Cusi, MD, FACP, FACE.
“If in the last 10 patients, you didn’t diagnose anybody with fibrosis, you probably missed it,” he said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “The question is, How are we going to tackle this problem? My academic goal is that we incorporate screening for NASH [nonalcoholic steatohepatitis], or for fibrosis more specifically, in the same way we do for retinopathy or nephropathy, because we do have a way to treat it.”
As part of the large population-based Rotterdam study of individuals aged 45 years and older, researchers found that liver stiffness of 8 kPa or more by transient elastography was present in 5.6% of the study participants and was strongly associated with steatosis and diabetes (Hepatology. 2016;63:138-47). According to Dr. Cusi, individuals who have steatosis without diabetes face a 5%-10% risk of fibrosis, while those with steatosis and diabetes face a 15%-20% risk.
“It’s well established in a number of studies that if you have fibrosis, you’re at high risk not only of cirrhosis, but also of hepatocellular carcinoma,” he said. “The key thing is not detecting fat, which is not really the target. The target is if there’s fibrosis or not.” Three ways to assess for fibrosis include MR elastography, transient elastography (which is the most commonly used), and fibrosis marker panels.
Liver fibrosis likely starts with adipose tissue dysfunction, said Dr. Cusi, who authored a review on the pathophysiology of interactions between adipose tissue and target organs in obesity and the resulting clinical implications for the management of nonalcoholic steatohepatitis (Gastroenterology. 2012;142[4]:711-25.e6).
“When you have insulin-resistant, sick adipose tissue, that leads to the accumulation of fat in the liver,” he said. “. Even if you get people who are matched for BMIs [body mass indexes] between 30 and 35 kg/m2, there is a spectrum in which some individuals have very insulin-resistant adipose tissue and others less so. I would say that 1 out of 10 are metabolically healthy, and we don’t understand exactly why.”
In a recent cross-sectional analysis of 352 healthy individuals, Dr. Cusi and his associates found that intrahepatic triglyceride (IHTG) accumulation is strongly associated with adipose tissue insulin resistance, supporting the current theory of lipotoxicity as a driver of IHTG accumulation (Hepatology. 2017;65[4]:1132-44). The researchers observed that once IHTG accumulation reaches about 6%, skeletal muscle insulin resistance, hypertriglyceridemia, and low HDL cholesterol become fully established.
“The next question is, How does this correlate with NASH?” Dr. Cusi said. “Our take is that there is a threshold effect. Once you have a critical amount of triglycerides in your liver, some individuals are going to activate pathways that are harmful. NASH is not something exclusive to individuals who are obese. Lean people can also develop NASH. The key feature is insulin resistance, not metabolic syndrome. Once you develop a fatty liver, your chances of NASH are comparable to that of an obese individual. The paradox is that lean individuals get a fatty liver, but when they get a fatty liver, they are at risk for NASH and for fibrosis.”
Why lean individuals develop NASH is not fully understood, but Dr. Cusi said he suspects that the problem develops at the mitochondrial level.
Results from an unpublished animal model in which mice were fed a high–trans-fat diet for 24 weeks showed that the mice developed steatosis by week 8 and NASH by week 24. The mice had an increase in the tricarboxylic acid (TCA) cycle, which is typical of the NASH period, as well as an increase in ceramides.
“Perhaps a unifying hypothesis would be that the development of NASH is linked to inflammation and to insulin signaling,” Dr. Cusi said. “Not surprisingly, it had a number of effects on the mitochondria, and in this animal model it decreases the TCA.” He noted that the biology of fibrosis remains unknown in humans. “What we have been familiar with is the high-triglyceride, low-HDL pattern,” he said. “If you look at how that correlates with the amount of liver fat, it is basically a threshold effect. Once you have steatosis, you don’t see much worse dyslipidemia, which is typical of these patients.”
Recently published guidance from the American Association for the Study of Liver Diseases on the diagnosis and management of nonalcoholic fatty liver disease (NAFLD) suggests that patients require a weight loss of 3%-5% to improve steatosis, but a loss of 7%-10% to improve most histologic features of NASH, including fibrosis (Hepatology. 2018;67[1]:328-57). Exercise alone may prevent or reduce steatosis, but its ability to improve other aspects of liver histology remains unknown. Bariatric surgery can be considered in otherwise eligible obese individuals with NAFLD or NASH. The procedure’s impact on fibrosis is unknown.
The AASLD practice guideline notes that metformin is not recommended for treating NASH in adult patients, but pioglitazone improves liver histology in patients with and without type 2 diabetes with biopsy-proven NASH.
“Pioglitazone has had the greatest benefit in terms of treatment effect, compared to placebo,” Dr. Cusi said. “It’s a generic drug; at the VA [Veterans Affairs], it costs 8 cents per tablet. I think that pioglitazone will be to NASH what metformin has been to type 2 diabetes. The most common side effect is weight gain, typically between 4 and 9 lb. Risks and benefits should be discussed with each patient. It should not be used for NAFLD without biopsy-proven NASH.”
The guideline goes on to say that it’s currently premature to consider GLP-1 (glucagonlike peptide–1) agonists for treating liver disease in patients with NAFLD or NASH. Meanwhile, vitamin E at 800 IU has been shown to improve liver histology in nondiabetic adults with NASH, but the risks and benefits should be discussed with each patient. Vitamin E is not recommended for NASH in diabetic patients, NAFLD without a liver biopsy, NASH cirrhosis, or cryptogenic cirrhosis.
The AASLD practice guideline also states that the best evidence for using SGLT2 (sodium-glucose cotransporter–2) inhibitors in NAFLD comes from animal studies, which report a reduction in steatosis with and without weight loss. Clinical studies reporting a reduction in steatosis are limited. There are positive observational studies with a reduction in alanine aminotransferase and some studies that have shown a reduction in liver fat. “For me, the best option is to tailor treatment to the pathophysiology of the disease,” Dr. Cusi said. “You reduce fat by weight loss in some way, or you change the biology of fat with a thiazolidinedione.”
Dr. Cusi reported that he has received grant support from the Burroughs Wellcome Fund, the American Diabetes Association, and the National Institutes of Health.
EXPERT ANALYSIS FROM WCIRDC 2017
Study probes predictors of response to vedolizumab
LAS VEGAS – , a small, single-center study showed.
“Right now there are a variety of medications to treat Crohn’s disease, but there isn’t a set criteria [for] what [drug] works for which kind of patient,” Adam A. Dhedhi, MD, said in an interview at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “We’re trying to figure out if we can find a predictor of response to vedolizumab.” Manufactured by Millennium Pharmaceuticals, vedolizumab is a gut-selective monoclonal antibody to alpha4beta7 integrin that prevents transportation of leukocytes into gastrointestinal mucosa.
He and his associates reported that a low CRP value at time of initiation (a mean of 6.6 mg/L) was found to be a positive predictor of both response and remission (odds ratio, 0.3045; P = .001), while the mean CRP value for nonresponders was 29.9 mg/L. In addition, any smoking history was a predictor of poor response to vedolizumab (OR, 0.0008; P = .009). “That was surprising and useful information to carry forward,” Dr. Dhedhi said. “If you’re making a decision between an anti-TNF [tumor necrosis factor] agent and vedolizumab, [and] if the patient is a smoker or has a higher active disease state, that may help tip the scales one way or the other.” In their abstract, the researchers noted that cigarette smoke “has been found to be involved in beta-2 integrin activation and neutrophil migration in lung tissue and may play a similar role in the gut” (Respiratory Research 2011;12[1]:75). Dr. Dhedhi and his associates also found that more than half of patients who had previously used two or more anti-TNF therapies (58%) achieved remission, compared with 47% who had used one prior anti-TNF drug and 43% who were anti-TNF naive.
He acknowledged certain limitations of the study, including its retrospective design and small sample size. Dr. Dhedhi reported having no financial disclosures.
*This story was updated on 3/26.
SOURCE: Dhedhi AA et al. Crohn’s & Colitis Congress, Poster 207.
LAS VEGAS – , a small, single-center study showed.
“Right now there are a variety of medications to treat Crohn’s disease, but there isn’t a set criteria [for] what [drug] works for which kind of patient,” Adam A. Dhedhi, MD, said in an interview at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “We’re trying to figure out if we can find a predictor of response to vedolizumab.” Manufactured by Millennium Pharmaceuticals, vedolizumab is a gut-selective monoclonal antibody to alpha4beta7 integrin that prevents transportation of leukocytes into gastrointestinal mucosa.
He and his associates reported that a low CRP value at time of initiation (a mean of 6.6 mg/L) was found to be a positive predictor of both response and remission (odds ratio, 0.3045; P = .001), while the mean CRP value for nonresponders was 29.9 mg/L. In addition, any smoking history was a predictor of poor response to vedolizumab (OR, 0.0008; P = .009). “That was surprising and useful information to carry forward,” Dr. Dhedhi said. “If you’re making a decision between an anti-TNF [tumor necrosis factor] agent and vedolizumab, [and] if the patient is a smoker or has a higher active disease state, that may help tip the scales one way or the other.” In their abstract, the researchers noted that cigarette smoke “has been found to be involved in beta-2 integrin activation and neutrophil migration in lung tissue and may play a similar role in the gut” (Respiratory Research 2011;12[1]:75). Dr. Dhedhi and his associates also found that more than half of patients who had previously used two or more anti-TNF therapies (58%) achieved remission, compared with 47% who had used one prior anti-TNF drug and 43% who were anti-TNF naive.
He acknowledged certain limitations of the study, including its retrospective design and small sample size. Dr. Dhedhi reported having no financial disclosures.
*This story was updated on 3/26.
SOURCE: Dhedhi AA et al. Crohn’s & Colitis Congress, Poster 207.
LAS VEGAS – , a small, single-center study showed.
“Right now there are a variety of medications to treat Crohn’s disease, but there isn’t a set criteria [for] what [drug] works for which kind of patient,” Adam A. Dhedhi, MD, said in an interview at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “We’re trying to figure out if we can find a predictor of response to vedolizumab.” Manufactured by Millennium Pharmaceuticals, vedolizumab is a gut-selective monoclonal antibody to alpha4beta7 integrin that prevents transportation of leukocytes into gastrointestinal mucosa.
He and his associates reported that a low CRP value at time of initiation (a mean of 6.6 mg/L) was found to be a positive predictor of both response and remission (odds ratio, 0.3045; P = .001), while the mean CRP value for nonresponders was 29.9 mg/L. In addition, any smoking history was a predictor of poor response to vedolizumab (OR, 0.0008; P = .009). “That was surprising and useful information to carry forward,” Dr. Dhedhi said. “If you’re making a decision between an anti-TNF [tumor necrosis factor] agent and vedolizumab, [and] if the patient is a smoker or has a higher active disease state, that may help tip the scales one way or the other.” In their abstract, the researchers noted that cigarette smoke “has been found to be involved in beta-2 integrin activation and neutrophil migration in lung tissue and may play a similar role in the gut” (Respiratory Research 2011;12[1]:75). Dr. Dhedhi and his associates also found that more than half of patients who had previously used two or more anti-TNF therapies (58%) achieved remission, compared with 47% who had used one prior anti-TNF drug and 43% who were anti-TNF naive.
He acknowledged certain limitations of the study, including its retrospective design and small sample size. Dr. Dhedhi reported having no financial disclosures.
*This story was updated on 3/26.
SOURCE: Dhedhi AA et al. Crohn’s & Colitis Congress, Poster 207.
REPORTING FROM THE CROHN’S & COLITIS CONGRESS
Key clinical point: More aggressive Crohn’s disease or highly active disease is less likely to respond to vedolizumab therapy.
Major finding: A low baseline CRP level significantly predicted response and remission with vedolizumab (P = .001), while a history of smoking was a negative predictor of response and remission (P = .009).
Study details: A single-center, retrospective analysis of 45 Crohn’s patients treated with vedolizumab between 2014 and 2017.
Disclosures: Dr. Dhedhi reported having no financial disclosures.
Source: Dhedhi AA et al. Crohn’s & Colitis Congress, Poster 207.
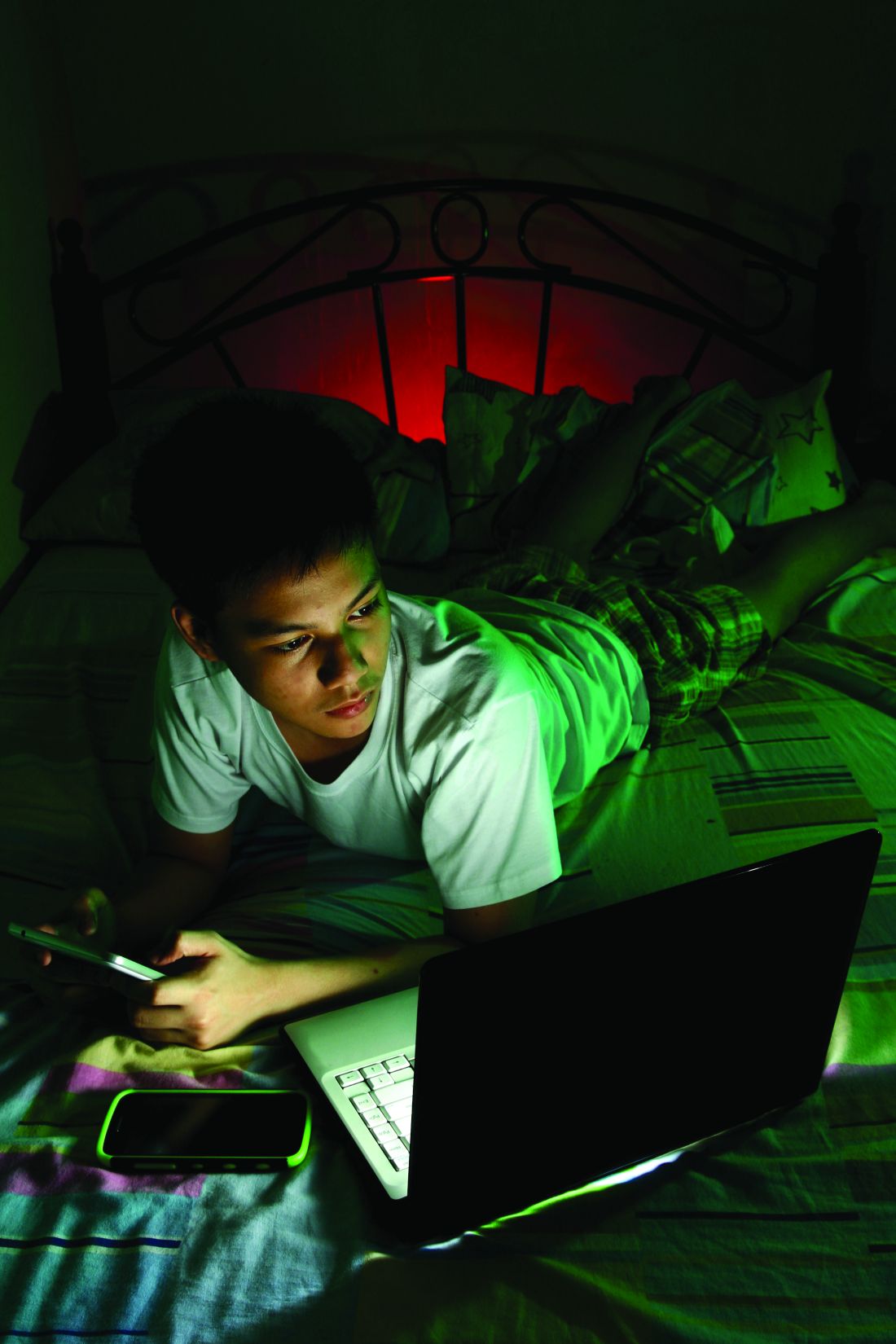
Pathological video game use can be ‘life-dominating’
SAN DIEGO – As a medical student, David L. Atkinson, MD, learned about a group of five adult men who played EverQuest, which bills itself as a 3D online world that “offers endless excitement, adventure, battle, and discovery.” They shared an apartment in Austin, Tex., and rotated which one would hold a full-time job while the other four spent their waking hours playing EverQuest.
“It was a little concerning,” recalled Dr. Atkinson, now a psychiatrist and the medical director of the teen recovery program at Children’s Health, Dallas. “EverQuest had a button in the game where you could order a pizza without interrupting your game play. Pathological video game use can be incredibly life-dominating.”
Many terms are used for pathological video game use, including problematic video game use, gaming disorder, and Internet gaming disorder, which is the term used in section III of DSM-5. Whether chronic video game use is a societal problem or an individual problem “is a very big question,” Dr. Atkinson said. “When we look at some of the prevalence data from Monitoring the Future, we have seen reductions in all kinds of substance use. We have seen reductions in teenage motor vehicle accidents and in teen pregnancy. If kids are playing video games and they’re all getting out of shape, that’s a cultural challenge. A clinician, though, may advocate against it as part of good health care.
“For instance, underage drinking in some American subcultures is normative. It doesn’t mean it’s a good idea.”
Most youth do not develop addictive behavior from playing games like EverQuest. “Substance use and gaming are different,” Dr. Atkinson said. “The amount of time spent at the expense of other things is one of the primary harms of video gaming, but financial concerns are not irrelevant. The new Star Wars Battlefront game would cost $2,100 if someone were to buy all of the available extras for the video game. Otherwise, it would take several hundred hours of game play to achieve all of these unlocked features.” While video games do not induce supraphysiologic dopamine release in the way drugs like cocaine do, the addictive potential is measured by an equation of reward versus effort. Obtaining a video game is not dependent upon social interactions, unlike drug use in states where the drug in question is illegal. In fact, the fewer social connections, the greater the risk of developing a video game use disorder.
“The perception of harm of video game addiction is very low, and parents do not consider the potential for developing an addiction before they buy a computer, handheld device, or video game console,” he said. “It is viewed as something that has to be limited ... not as something that is impossible to limit.” However, when parents begin to detect problems, they often find themselves unable to control their children’s or teens’ use of gaming, according to Dr. Atkinson.
In the DSM-5, Internet gaming disorder is defined as being preoccupied with games and withdrawn when not playing them, including irritability, anxiety, and sadness. Tolerance manifests as needing to spend more time playing the game. Typically, gamers cannot reduce their use despite effort, and there is a loss of interest in other activities and hobbies, Dr. Atkinson said. They may continue to engage in overuse of games despite knowing it’s a problem; they may lie about usage, may use games to escape anxiety or guilt, and may have lost or risked lose or risk relationships or career opportunities because of games.
“Not all gamers will do all of these things,” he emphasized. “For example, some gamers have disordered use and lose interest in other things, but don’t lie about it.” DSM-5 criteria also note that the video gaming itself must cause clinically significant impairment and must not be a manifestation of another disorder.
Tools aimed at helping in the diagnosis include the Problem Video Game Playing Questionnaire, the Internet Gaming Disorder Scale, the Internet Gaming Disorder Scale–Short-Form, the Problematic Online Gaming Questionnaire, the Game Addiction Scale, and the Electronic Gaming Motives Questionnaire, which measures enhancement, coping, social, and self-gratification motives.
According to Dr. Atkinson, 90% of children in Japan, Korea, North America, and Europe play video games. However, the prevalence of Internet gaming disorder is estimated to be 1% in the United States, 1.14% in Germany, and 5.9% in South Korea. Males have higher rates of pathological video game use, while afflicted females tend to have more problems. Pathological gaming use is associated with high levels of previous truancy and few leisure activities. It’s also associated with depression, poor impulse control, narcissistic traits, high anxiety, poor social competence, and less religiosity.
“The overlap with depression is very interesting,” Dr. Atkinson said. “ When they get rejected in a peer group or for a job, they tend to take it harder than people who don’t game. The gaming world is a place where you can be safe from rejection. If your credit card goes through, you’re allowed in.”
Anhedonia is another factor within the clinical syndrome of depression that is associated with video game use. A nationwide community sample of individuals in Korea showed that gaming and depression have their overlap most strongly with the “escape from negative emotions” model (J Nerv Ment Dis. 2017;205[7]:568-73). Other associated problems include greater obesity; metabolic indicators, such as high triglycerides and cholesterol; and sleep deprivation. Chronic gamers also tend to have less social support, less health promotion, and heightened social phobia. “When you’re gaming all the time, you’re going to have less opportunity to engage in an exposure paradigm to help you get over your social phobia,” Dr. Atkinson said. “Problem gamers are also more likely to have pathological use of pornography, poor impulse control, and ADHD symptoms.”
Studies of biobehavioral characteristics of those with pathological video game use suggest that there is a decreased dopamine striatal response (Neurosci Biobehav Rev. 2017 Apr;75:314-30). They also suggest decreased functional connectivity across areas of the brain, including decreased resting-state functional connectivity between ventral tegmental area and the nucleus accumbens, and lower tonic dopamine firing.
Parental management training can be successful at setting gaming limits in children under 12 years of age, he said. Pathological video game use is associated with physiologic stress in the family problem-solving task. One study of a brief 3-week family therapy intervention as measured by functional MRI showed that improvement in perceived family cohesion was associated with an increase in the activity of the caudate nucleus in response to the gamer’s viewing images of family cohesion and was inversely correlated with changes in online game playing time (Psychiatry Res. 2012 May 31;202[2]:126-31). “Bringing the family together may give them something to do besides gaming,” Dr. Atkinson said. “That can help them put games in a more balanced perspective.”
The largest evidence base supports cognitive-behavioral therapy for Internet gaming disorder, but there is insufficient evidence to make a clear statement of benefit (Clin Psychol Rev. 2017 Jun;54:123-33). Gaming-related cognitions accounted for a large portion of the variance in treatment response.
“Does the gaming cause the thoughts? Or do the thoughts cause the gaming?” Dr. Atkinson asked. “The cognitive model of CBT would tell you there’s a bidirectional relationship.”
As for medications, bupropion has been shown to reduce online gaming in depressed individuals, and escitalopram also may be efficacious. One comparative analysis showed that there were greater effects from using bupropion than for using escitalopram (Clin Psychopharmacol Neurosci. 2017 Nov 30;15[4]:361-8). Methylphenidate also has been shown to reduce online gaming (Compr Psychiatry. 2009 May-Jun;50[3]:251-6).
Parents who take video games away from their children often are met with a burst of aggression. “There’s an attempt to reestablish dominance in the situation, to obtain the old reinforcer or to reestablish control,” Dr. Atkinson said. “It’s different from tapering a drug; this is something that you have to plan for. Tapering video games is difficult to do. If the kid plays longer than they’re supposed to, what do you do then? You may have a fight to discontinue the video game. That’s one of the practical problems.”
Dr. Atkinson reported having no financial disclosures.
SOURCE: Atkinson DL. AAAP 2017.
SAN DIEGO – As a medical student, David L. Atkinson, MD, learned about a group of five adult men who played EverQuest, which bills itself as a 3D online world that “offers endless excitement, adventure, battle, and discovery.” They shared an apartment in Austin, Tex., and rotated which one would hold a full-time job while the other four spent their waking hours playing EverQuest.
“It was a little concerning,” recalled Dr. Atkinson, now a psychiatrist and the medical director of the teen recovery program at Children’s Health, Dallas. “EverQuest had a button in the game where you could order a pizza without interrupting your game play. Pathological video game use can be incredibly life-dominating.”
Many terms are used for pathological video game use, including problematic video game use, gaming disorder, and Internet gaming disorder, which is the term used in section III of DSM-5. Whether chronic video game use is a societal problem or an individual problem “is a very big question,” Dr. Atkinson said. “When we look at some of the prevalence data from Monitoring the Future, we have seen reductions in all kinds of substance use. We have seen reductions in teenage motor vehicle accidents and in teen pregnancy. If kids are playing video games and they’re all getting out of shape, that’s a cultural challenge. A clinician, though, may advocate against it as part of good health care.
“For instance, underage drinking in some American subcultures is normative. It doesn’t mean it’s a good idea.”
Most youth do not develop addictive behavior from playing games like EverQuest. “Substance use and gaming are different,” Dr. Atkinson said. “The amount of time spent at the expense of other things is one of the primary harms of video gaming, but financial concerns are not irrelevant. The new Star Wars Battlefront game would cost $2,100 if someone were to buy all of the available extras for the video game. Otherwise, it would take several hundred hours of game play to achieve all of these unlocked features.” While video games do not induce supraphysiologic dopamine release in the way drugs like cocaine do, the addictive potential is measured by an equation of reward versus effort. Obtaining a video game is not dependent upon social interactions, unlike drug use in states where the drug in question is illegal. In fact, the fewer social connections, the greater the risk of developing a video game use disorder.
“The perception of harm of video game addiction is very low, and parents do not consider the potential for developing an addiction before they buy a computer, handheld device, or video game console,” he said. “It is viewed as something that has to be limited ... not as something that is impossible to limit.” However, when parents begin to detect problems, they often find themselves unable to control their children’s or teens’ use of gaming, according to Dr. Atkinson.
In the DSM-5, Internet gaming disorder is defined as being preoccupied with games and withdrawn when not playing them, including irritability, anxiety, and sadness. Tolerance manifests as needing to spend more time playing the game. Typically, gamers cannot reduce their use despite effort, and there is a loss of interest in other activities and hobbies, Dr. Atkinson said. They may continue to engage in overuse of games despite knowing it’s a problem; they may lie about usage, may use games to escape anxiety or guilt, and may have lost or risked lose or risk relationships or career opportunities because of games.
“Not all gamers will do all of these things,” he emphasized. “For example, some gamers have disordered use and lose interest in other things, but don’t lie about it.” DSM-5 criteria also note that the video gaming itself must cause clinically significant impairment and must not be a manifestation of another disorder.
Tools aimed at helping in the diagnosis include the Problem Video Game Playing Questionnaire, the Internet Gaming Disorder Scale, the Internet Gaming Disorder Scale–Short-Form, the Problematic Online Gaming Questionnaire, the Game Addiction Scale, and the Electronic Gaming Motives Questionnaire, which measures enhancement, coping, social, and self-gratification motives.
According to Dr. Atkinson, 90% of children in Japan, Korea, North America, and Europe play video games. However, the prevalence of Internet gaming disorder is estimated to be 1% in the United States, 1.14% in Germany, and 5.9% in South Korea. Males have higher rates of pathological video game use, while afflicted females tend to have more problems. Pathological gaming use is associated with high levels of previous truancy and few leisure activities. It’s also associated with depression, poor impulse control, narcissistic traits, high anxiety, poor social competence, and less religiosity.
“The overlap with depression is very interesting,” Dr. Atkinson said. “ When they get rejected in a peer group or for a job, they tend to take it harder than people who don’t game. The gaming world is a place where you can be safe from rejection. If your credit card goes through, you’re allowed in.”
Anhedonia is another factor within the clinical syndrome of depression that is associated with video game use. A nationwide community sample of individuals in Korea showed that gaming and depression have their overlap most strongly with the “escape from negative emotions” model (J Nerv Ment Dis. 2017;205[7]:568-73). Other associated problems include greater obesity; metabolic indicators, such as high triglycerides and cholesterol; and sleep deprivation. Chronic gamers also tend to have less social support, less health promotion, and heightened social phobia. “When you’re gaming all the time, you’re going to have less opportunity to engage in an exposure paradigm to help you get over your social phobia,” Dr. Atkinson said. “Problem gamers are also more likely to have pathological use of pornography, poor impulse control, and ADHD symptoms.”
Studies of biobehavioral characteristics of those with pathological video game use suggest that there is a decreased dopamine striatal response (Neurosci Biobehav Rev. 2017 Apr;75:314-30). They also suggest decreased functional connectivity across areas of the brain, including decreased resting-state functional connectivity between ventral tegmental area and the nucleus accumbens, and lower tonic dopamine firing.
Parental management training can be successful at setting gaming limits in children under 12 years of age, he said. Pathological video game use is associated with physiologic stress in the family problem-solving task. One study of a brief 3-week family therapy intervention as measured by functional MRI showed that improvement in perceived family cohesion was associated with an increase in the activity of the caudate nucleus in response to the gamer’s viewing images of family cohesion and was inversely correlated with changes in online game playing time (Psychiatry Res. 2012 May 31;202[2]:126-31). “Bringing the family together may give them something to do besides gaming,” Dr. Atkinson said. “That can help them put games in a more balanced perspective.”
The largest evidence base supports cognitive-behavioral therapy for Internet gaming disorder, but there is insufficient evidence to make a clear statement of benefit (Clin Psychol Rev. 2017 Jun;54:123-33). Gaming-related cognitions accounted for a large portion of the variance in treatment response.
“Does the gaming cause the thoughts? Or do the thoughts cause the gaming?” Dr. Atkinson asked. “The cognitive model of CBT would tell you there’s a bidirectional relationship.”
As for medications, bupropion has been shown to reduce online gaming in depressed individuals, and escitalopram also may be efficacious. One comparative analysis showed that there were greater effects from using bupropion than for using escitalopram (Clin Psychopharmacol Neurosci. 2017 Nov 30;15[4]:361-8). Methylphenidate also has been shown to reduce online gaming (Compr Psychiatry. 2009 May-Jun;50[3]:251-6).
Parents who take video games away from their children often are met with a burst of aggression. “There’s an attempt to reestablish dominance in the situation, to obtain the old reinforcer or to reestablish control,” Dr. Atkinson said. “It’s different from tapering a drug; this is something that you have to plan for. Tapering video games is difficult to do. If the kid plays longer than they’re supposed to, what do you do then? You may have a fight to discontinue the video game. That’s one of the practical problems.”
Dr. Atkinson reported having no financial disclosures.
SOURCE: Atkinson DL. AAAP 2017.
SAN DIEGO – As a medical student, David L. Atkinson, MD, learned about a group of five adult men who played EverQuest, which bills itself as a 3D online world that “offers endless excitement, adventure, battle, and discovery.” They shared an apartment in Austin, Tex., and rotated which one would hold a full-time job while the other four spent their waking hours playing EverQuest.
“It was a little concerning,” recalled Dr. Atkinson, now a psychiatrist and the medical director of the teen recovery program at Children’s Health, Dallas. “EverQuest had a button in the game where you could order a pizza without interrupting your game play. Pathological video game use can be incredibly life-dominating.”
Many terms are used for pathological video game use, including problematic video game use, gaming disorder, and Internet gaming disorder, which is the term used in section III of DSM-5. Whether chronic video game use is a societal problem or an individual problem “is a very big question,” Dr. Atkinson said. “When we look at some of the prevalence data from Monitoring the Future, we have seen reductions in all kinds of substance use. We have seen reductions in teenage motor vehicle accidents and in teen pregnancy. If kids are playing video games and they’re all getting out of shape, that’s a cultural challenge. A clinician, though, may advocate against it as part of good health care.
“For instance, underage drinking in some American subcultures is normative. It doesn’t mean it’s a good idea.”
Most youth do not develop addictive behavior from playing games like EverQuest. “Substance use and gaming are different,” Dr. Atkinson said. “The amount of time spent at the expense of other things is one of the primary harms of video gaming, but financial concerns are not irrelevant. The new Star Wars Battlefront game would cost $2,100 if someone were to buy all of the available extras for the video game. Otherwise, it would take several hundred hours of game play to achieve all of these unlocked features.” While video games do not induce supraphysiologic dopamine release in the way drugs like cocaine do, the addictive potential is measured by an equation of reward versus effort. Obtaining a video game is not dependent upon social interactions, unlike drug use in states where the drug in question is illegal. In fact, the fewer social connections, the greater the risk of developing a video game use disorder.
“The perception of harm of video game addiction is very low, and parents do not consider the potential for developing an addiction before they buy a computer, handheld device, or video game console,” he said. “It is viewed as something that has to be limited ... not as something that is impossible to limit.” However, when parents begin to detect problems, they often find themselves unable to control their children’s or teens’ use of gaming, according to Dr. Atkinson.
In the DSM-5, Internet gaming disorder is defined as being preoccupied with games and withdrawn when not playing them, including irritability, anxiety, and sadness. Tolerance manifests as needing to spend more time playing the game. Typically, gamers cannot reduce their use despite effort, and there is a loss of interest in other activities and hobbies, Dr. Atkinson said. They may continue to engage in overuse of games despite knowing it’s a problem; they may lie about usage, may use games to escape anxiety or guilt, and may have lost or risked lose or risk relationships or career opportunities because of games.
“Not all gamers will do all of these things,” he emphasized. “For example, some gamers have disordered use and lose interest in other things, but don’t lie about it.” DSM-5 criteria also note that the video gaming itself must cause clinically significant impairment and must not be a manifestation of another disorder.
Tools aimed at helping in the diagnosis include the Problem Video Game Playing Questionnaire, the Internet Gaming Disorder Scale, the Internet Gaming Disorder Scale–Short-Form, the Problematic Online Gaming Questionnaire, the Game Addiction Scale, and the Electronic Gaming Motives Questionnaire, which measures enhancement, coping, social, and self-gratification motives.
According to Dr. Atkinson, 90% of children in Japan, Korea, North America, and Europe play video games. However, the prevalence of Internet gaming disorder is estimated to be 1% in the United States, 1.14% in Germany, and 5.9% in South Korea. Males have higher rates of pathological video game use, while afflicted females tend to have more problems. Pathological gaming use is associated with high levels of previous truancy and few leisure activities. It’s also associated with depression, poor impulse control, narcissistic traits, high anxiety, poor social competence, and less religiosity.
“The overlap with depression is very interesting,” Dr. Atkinson said. “ When they get rejected in a peer group or for a job, they tend to take it harder than people who don’t game. The gaming world is a place where you can be safe from rejection. If your credit card goes through, you’re allowed in.”
Anhedonia is another factor within the clinical syndrome of depression that is associated with video game use. A nationwide community sample of individuals in Korea showed that gaming and depression have their overlap most strongly with the “escape from negative emotions” model (J Nerv Ment Dis. 2017;205[7]:568-73). Other associated problems include greater obesity; metabolic indicators, such as high triglycerides and cholesterol; and sleep deprivation. Chronic gamers also tend to have less social support, less health promotion, and heightened social phobia. “When you’re gaming all the time, you’re going to have less opportunity to engage in an exposure paradigm to help you get over your social phobia,” Dr. Atkinson said. “Problem gamers are also more likely to have pathological use of pornography, poor impulse control, and ADHD symptoms.”
Studies of biobehavioral characteristics of those with pathological video game use suggest that there is a decreased dopamine striatal response (Neurosci Biobehav Rev. 2017 Apr;75:314-30). They also suggest decreased functional connectivity across areas of the brain, including decreased resting-state functional connectivity between ventral tegmental area and the nucleus accumbens, and lower tonic dopamine firing.
Parental management training can be successful at setting gaming limits in children under 12 years of age, he said. Pathological video game use is associated with physiologic stress in the family problem-solving task. One study of a brief 3-week family therapy intervention as measured by functional MRI showed that improvement in perceived family cohesion was associated with an increase in the activity of the caudate nucleus in response to the gamer’s viewing images of family cohesion and was inversely correlated with changes in online game playing time (Psychiatry Res. 2012 May 31;202[2]:126-31). “Bringing the family together may give them something to do besides gaming,” Dr. Atkinson said. “That can help them put games in a more balanced perspective.”
The largest evidence base supports cognitive-behavioral therapy for Internet gaming disorder, but there is insufficient evidence to make a clear statement of benefit (Clin Psychol Rev. 2017 Jun;54:123-33). Gaming-related cognitions accounted for a large portion of the variance in treatment response.
“Does the gaming cause the thoughts? Or do the thoughts cause the gaming?” Dr. Atkinson asked. “The cognitive model of CBT would tell you there’s a bidirectional relationship.”
As for medications, bupropion has been shown to reduce online gaming in depressed individuals, and escitalopram also may be efficacious. One comparative analysis showed that there were greater effects from using bupropion than for using escitalopram (Clin Psychopharmacol Neurosci. 2017 Nov 30;15[4]:361-8). Methylphenidate also has been shown to reduce online gaming (Compr Psychiatry. 2009 May-Jun;50[3]:251-6).
Parents who take video games away from their children often are met with a burst of aggression. “There’s an attempt to reestablish dominance in the situation, to obtain the old reinforcer or to reestablish control,” Dr. Atkinson said. “It’s different from tapering a drug; this is something that you have to plan for. Tapering video games is difficult to do. If the kid plays longer than they’re supposed to, what do you do then? You may have a fight to discontinue the video game. That’s one of the practical problems.”
Dr. Atkinson reported having no financial disclosures.
SOURCE: Atkinson DL. AAAP 2017.
REPORTING FROM AAAP
Shedding light on shift work’s influence on cardiometabolic risk
LOS ANGELES – Current and previous night workers had significantly increased levels of hemoglobin A1c, compared with diurnal workers, preliminary results from an ongoing study showed. The finding sheds further insight into the link between environmental light, circadian rhythms, and metabolic disorders.
“To date, observational studies on bright light have revealed that evening bright light is associated with increased appetite and that bedroom light intensity is correlated with obesity,” Massimo Federici, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “It’s also been reported that artificial light is correlated with type 2 diabetes in the home setting and that daytime light exposure is positively correlated with body mass index. However, no studies have directly investigated the effect of acute light on human glucose metabolism.”
Although few metabolic intervention studies using light have been done, Dr. Federici mentioned three of note. One, in patients with seasonal affective disorder and type 2 diabetes, showed reduced insulin requirements after light therapy (Lancet. 1992;339[8800]:1065-6). Another, a short-term study of 25 obese subjects treated with 5,000 lux bright light therapy in addition to exercise, showed reduced body fat after 6 weeks (Obesity 2007; 15[7]:1749-57). A third, in 34 obese subjects who were exposed to 1,300 lux bright light every morning for 3 weeks, showed a small but significant reduction in fat mass (Obes Facts 2013;6:28-38).
As part of an ongoing project known as EuRhythDia, researchers including Dr. Federici set out to identify metabolic and molecular variables associated with shift work, and to test the effect of a lifestyle intervention that comprised light exposure, exercise, and melatonin. He presented unpublished results from one aspect of the trial: a cross-sectional analysis of 273 nurses divided into one of three groups: 64 diurnal workers (DW), 111 active night shift workers (aNW), and 98 prior night shift workers (pNW). Those with diabetes or taking oral antidiabetic drugs were excluded from the study.
The analysis showed that nurses in the pNW group were significantly older, at a mean of 39.7 years, than those in the DW group, whose mean age was 37 years, and the aNW group, who averaged 36.1 years. Those in the pNW group also had a significantly greater body mass index, compared with their counterparts in the aNW and DW groups (a mean of 25.7 kg/m2, vs. 24.8 and 23.7, respectively) as well has a higher mean waist circumference (a mean of 87.2 cm, vs. 84.6 cm and 82 cm).
The mean HbA1c was higher in the nurses with prior and active night shift work, at 5.3% each, than in the diurnal workers (5.1%, P less than .001).
When Pittsburgh Sleep Quality Index scores were used to evaluate sleep quality independent of work status, more than half of the study subjects (163) were classified as being “good sleepers,” while 110 were considered to be “bad sleepers.” Bad sleepers had a significantly higher mean HbA1c level compared with good sleepers (5.3% vs. 5.2%). Bad sleepers also had higher levels of HDL cholesterol (a mean of 60.8 mg/dL vs. 56.3 mg/dL).
Dr. Federici highlighted preliminary findings from a study of 32 aNW subjects who were assigned to treatment with warm light therapy at 1,000 lux for 30 minutes at 30 cm every morning for 3 months. They observed a mild improvement in the area under the curve of the oral glucose tolerance test at 24 weeks (12 weeks’ washout after 12 weeks of light therapy). “However, the effect was obtained not at the end of the intervention but at the end of the washout period,” he said.
He called for more studies going forward that take into account the effect of seasons as well as the effects of diet and exercise.
Dr. Federici disclosed that he receives editorial fees from Springer Nature group.
LOS ANGELES – Current and previous night workers had significantly increased levels of hemoglobin A1c, compared with diurnal workers, preliminary results from an ongoing study showed. The finding sheds further insight into the link between environmental light, circadian rhythms, and metabolic disorders.
“To date, observational studies on bright light have revealed that evening bright light is associated with increased appetite and that bedroom light intensity is correlated with obesity,” Massimo Federici, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “It’s also been reported that artificial light is correlated with type 2 diabetes in the home setting and that daytime light exposure is positively correlated with body mass index. However, no studies have directly investigated the effect of acute light on human glucose metabolism.”
Although few metabolic intervention studies using light have been done, Dr. Federici mentioned three of note. One, in patients with seasonal affective disorder and type 2 diabetes, showed reduced insulin requirements after light therapy (Lancet. 1992;339[8800]:1065-6). Another, a short-term study of 25 obese subjects treated with 5,000 lux bright light therapy in addition to exercise, showed reduced body fat after 6 weeks (Obesity 2007; 15[7]:1749-57). A third, in 34 obese subjects who were exposed to 1,300 lux bright light every morning for 3 weeks, showed a small but significant reduction in fat mass (Obes Facts 2013;6:28-38).
As part of an ongoing project known as EuRhythDia, researchers including Dr. Federici set out to identify metabolic and molecular variables associated with shift work, and to test the effect of a lifestyle intervention that comprised light exposure, exercise, and melatonin. He presented unpublished results from one aspect of the trial: a cross-sectional analysis of 273 nurses divided into one of three groups: 64 diurnal workers (DW), 111 active night shift workers (aNW), and 98 prior night shift workers (pNW). Those with diabetes or taking oral antidiabetic drugs were excluded from the study.
The analysis showed that nurses in the pNW group were significantly older, at a mean of 39.7 years, than those in the DW group, whose mean age was 37 years, and the aNW group, who averaged 36.1 years. Those in the pNW group also had a significantly greater body mass index, compared with their counterparts in the aNW and DW groups (a mean of 25.7 kg/m2, vs. 24.8 and 23.7, respectively) as well has a higher mean waist circumference (a mean of 87.2 cm, vs. 84.6 cm and 82 cm).
The mean HbA1c was higher in the nurses with prior and active night shift work, at 5.3% each, than in the diurnal workers (5.1%, P less than .001).
When Pittsburgh Sleep Quality Index scores were used to evaluate sleep quality independent of work status, more than half of the study subjects (163) were classified as being “good sleepers,” while 110 were considered to be “bad sleepers.” Bad sleepers had a significantly higher mean HbA1c level compared with good sleepers (5.3% vs. 5.2%). Bad sleepers also had higher levels of HDL cholesterol (a mean of 60.8 mg/dL vs. 56.3 mg/dL).
Dr. Federici highlighted preliminary findings from a study of 32 aNW subjects who were assigned to treatment with warm light therapy at 1,000 lux for 30 minutes at 30 cm every morning for 3 months. They observed a mild improvement in the area under the curve of the oral glucose tolerance test at 24 weeks (12 weeks’ washout after 12 weeks of light therapy). “However, the effect was obtained not at the end of the intervention but at the end of the washout period,” he said.
He called for more studies going forward that take into account the effect of seasons as well as the effects of diet and exercise.
Dr. Federici disclosed that he receives editorial fees from Springer Nature group.
LOS ANGELES – Current and previous night workers had significantly increased levels of hemoglobin A1c, compared with diurnal workers, preliminary results from an ongoing study showed. The finding sheds further insight into the link between environmental light, circadian rhythms, and metabolic disorders.
“To date, observational studies on bright light have revealed that evening bright light is associated with increased appetite and that bedroom light intensity is correlated with obesity,” Massimo Federici, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “It’s also been reported that artificial light is correlated with type 2 diabetes in the home setting and that daytime light exposure is positively correlated with body mass index. However, no studies have directly investigated the effect of acute light on human glucose metabolism.”
Although few metabolic intervention studies using light have been done, Dr. Federici mentioned three of note. One, in patients with seasonal affective disorder and type 2 diabetes, showed reduced insulin requirements after light therapy (Lancet. 1992;339[8800]:1065-6). Another, a short-term study of 25 obese subjects treated with 5,000 lux bright light therapy in addition to exercise, showed reduced body fat after 6 weeks (Obesity 2007; 15[7]:1749-57). A third, in 34 obese subjects who were exposed to 1,300 lux bright light every morning for 3 weeks, showed a small but significant reduction in fat mass (Obes Facts 2013;6:28-38).
As part of an ongoing project known as EuRhythDia, researchers including Dr. Federici set out to identify metabolic and molecular variables associated with shift work, and to test the effect of a lifestyle intervention that comprised light exposure, exercise, and melatonin. He presented unpublished results from one aspect of the trial: a cross-sectional analysis of 273 nurses divided into one of three groups: 64 diurnal workers (DW), 111 active night shift workers (aNW), and 98 prior night shift workers (pNW). Those with diabetes or taking oral antidiabetic drugs were excluded from the study.
The analysis showed that nurses in the pNW group were significantly older, at a mean of 39.7 years, than those in the DW group, whose mean age was 37 years, and the aNW group, who averaged 36.1 years. Those in the pNW group also had a significantly greater body mass index, compared with their counterparts in the aNW and DW groups (a mean of 25.7 kg/m2, vs. 24.8 and 23.7, respectively) as well has a higher mean waist circumference (a mean of 87.2 cm, vs. 84.6 cm and 82 cm).
The mean HbA1c was higher in the nurses with prior and active night shift work, at 5.3% each, than in the diurnal workers (5.1%, P less than .001).
When Pittsburgh Sleep Quality Index scores were used to evaluate sleep quality independent of work status, more than half of the study subjects (163) were classified as being “good sleepers,” while 110 were considered to be “bad sleepers.” Bad sleepers had a significantly higher mean HbA1c level compared with good sleepers (5.3% vs. 5.2%). Bad sleepers also had higher levels of HDL cholesterol (a mean of 60.8 mg/dL vs. 56.3 mg/dL).
Dr. Federici highlighted preliminary findings from a study of 32 aNW subjects who were assigned to treatment with warm light therapy at 1,000 lux for 30 minutes at 30 cm every morning for 3 months. They observed a mild improvement in the area under the curve of the oral glucose tolerance test at 24 weeks (12 weeks’ washout after 12 weeks of light therapy). “However, the effect was obtained not at the end of the intervention but at the end of the washout period,” he said.
He called for more studies going forward that take into account the effect of seasons as well as the effects of diet and exercise.
Dr. Federici disclosed that he receives editorial fees from Springer Nature group.
EXPERT ANALYSIS FROM WCIRDC 2017
Early psychotherapy may predict buprenorphine treatment retention
SAN DIEGO – an observational study found.
“Opioid use disorder and overdose deaths are devastating many communities across the country,” lead study author Ajay Manhapra, MD, said at the annual meeting and scientific symposium of the American Academy of Addiction Psychiatry. “We know that engagement in opioid agonist treatment with buprenorphine/methadone is associated with a two-thirds reduction in mortality and lower morbidity. However, 1-year retention rates are generally less than 50%.”
As part of a larger study on 3-year buprenorphine retention, Dr. Manhapra and his associates set out to investigate what factors predict long-term retention in buprenorphine treatment. From patients with an OUD diagnosis in the Marketscan database, they identified 16,190 individuals who filled their prescription of buprenorphine after the first 60 days of 2011 as new starts and calculated the treatment retention period as the time between the date of their first prescription to the last prescription until the end of 2014. The researchers used CPT codes to identify the receipt of any outpatient psychotherapy and multivariate Cox survival analysis to examine the effect of psychotherapy receipt on buprenorphine retention.
Dr. Manhapra reported that of the 16,190 patients, 15% were engaged in buprenorphine treatment for 30 days or fewer, 40% were engaged for 31 days to 1 year, 31% were engaged between 1 and 3 years, and 14% were engaged for more than 3 years. The mean duration of retention was 1.23 years. At the same time, the outpatient psychotherapy receipt rate in 2011 was 30.29% among those retained for 0-30 days, 35.30% among those retained for 31-364 days, 37.59% among those retained for 1-3 years, and 39.20% among those retained for more than 3 years.
Multivariate Cox survival analysis revealed that receipt of any psychotherapy in 2011 was associated with a lower risk of discontinuation of buprenorphine treatment (hazard ratio, 0.86; P less than .0001). “Is this a direct effect of psychotherapy? I don’t know,” said Dr. Manhapra, who also practices at the Hampton (Virginia) VA Medical Center. “Is this a selection bias not accounted for by the variables available? That is, those who have a better chance of sustained retention might have been selected for or chosen to receive psychotherapy. Those are possibilities. We need further observational and qualitative studies, and maybe more randomized trials.”
Dr. Manhapra disclosed that he has received support from the VA Interprofessional Fellowship in Addiction Treatment and from Research in Addiction Medicine Scholars.
SOURCE: Manhapra A et al. AAAP 2017. Paper session A5.
SAN DIEGO – an observational study found.
“Opioid use disorder and overdose deaths are devastating many communities across the country,” lead study author Ajay Manhapra, MD, said at the annual meeting and scientific symposium of the American Academy of Addiction Psychiatry. “We know that engagement in opioid agonist treatment with buprenorphine/methadone is associated with a two-thirds reduction in mortality and lower morbidity. However, 1-year retention rates are generally less than 50%.”
As part of a larger study on 3-year buprenorphine retention, Dr. Manhapra and his associates set out to investigate what factors predict long-term retention in buprenorphine treatment. From patients with an OUD diagnosis in the Marketscan database, they identified 16,190 individuals who filled their prescription of buprenorphine after the first 60 days of 2011 as new starts and calculated the treatment retention period as the time between the date of their first prescription to the last prescription until the end of 2014. The researchers used CPT codes to identify the receipt of any outpatient psychotherapy and multivariate Cox survival analysis to examine the effect of psychotherapy receipt on buprenorphine retention.
Dr. Manhapra reported that of the 16,190 patients, 15% were engaged in buprenorphine treatment for 30 days or fewer, 40% were engaged for 31 days to 1 year, 31% were engaged between 1 and 3 years, and 14% were engaged for more than 3 years. The mean duration of retention was 1.23 years. At the same time, the outpatient psychotherapy receipt rate in 2011 was 30.29% among those retained for 0-30 days, 35.30% among those retained for 31-364 days, 37.59% among those retained for 1-3 years, and 39.20% among those retained for more than 3 years.
Multivariate Cox survival analysis revealed that receipt of any psychotherapy in 2011 was associated with a lower risk of discontinuation of buprenorphine treatment (hazard ratio, 0.86; P less than .0001). “Is this a direct effect of psychotherapy? I don’t know,” said Dr. Manhapra, who also practices at the Hampton (Virginia) VA Medical Center. “Is this a selection bias not accounted for by the variables available? That is, those who have a better chance of sustained retention might have been selected for or chosen to receive psychotherapy. Those are possibilities. We need further observational and qualitative studies, and maybe more randomized trials.”
Dr. Manhapra disclosed that he has received support from the VA Interprofessional Fellowship in Addiction Treatment and from Research in Addiction Medicine Scholars.
SOURCE: Manhapra A et al. AAAP 2017. Paper session A5.
SAN DIEGO – an observational study found.
“Opioid use disorder and overdose deaths are devastating many communities across the country,” lead study author Ajay Manhapra, MD, said at the annual meeting and scientific symposium of the American Academy of Addiction Psychiatry. “We know that engagement in opioid agonist treatment with buprenorphine/methadone is associated with a two-thirds reduction in mortality and lower morbidity. However, 1-year retention rates are generally less than 50%.”
As part of a larger study on 3-year buprenorphine retention, Dr. Manhapra and his associates set out to investigate what factors predict long-term retention in buprenorphine treatment. From patients with an OUD diagnosis in the Marketscan database, they identified 16,190 individuals who filled their prescription of buprenorphine after the first 60 days of 2011 as new starts and calculated the treatment retention period as the time between the date of their first prescription to the last prescription until the end of 2014. The researchers used CPT codes to identify the receipt of any outpatient psychotherapy and multivariate Cox survival analysis to examine the effect of psychotherapy receipt on buprenorphine retention.
Dr. Manhapra reported that of the 16,190 patients, 15% were engaged in buprenorphine treatment for 30 days or fewer, 40% were engaged for 31 days to 1 year, 31% were engaged between 1 and 3 years, and 14% were engaged for more than 3 years. The mean duration of retention was 1.23 years. At the same time, the outpatient psychotherapy receipt rate in 2011 was 30.29% among those retained for 0-30 days, 35.30% among those retained for 31-364 days, 37.59% among those retained for 1-3 years, and 39.20% among those retained for more than 3 years.
Multivariate Cox survival analysis revealed that receipt of any psychotherapy in 2011 was associated with a lower risk of discontinuation of buprenorphine treatment (hazard ratio, 0.86; P less than .0001). “Is this a direct effect of psychotherapy? I don’t know,” said Dr. Manhapra, who also practices at the Hampton (Virginia) VA Medical Center. “Is this a selection bias not accounted for by the variables available? That is, those who have a better chance of sustained retention might have been selected for or chosen to receive psychotherapy. Those are possibilities. We need further observational and qualitative studies, and maybe more randomized trials.”
Dr. Manhapra disclosed that he has received support from the VA Interprofessional Fellowship in Addiction Treatment and from Research in Addiction Medicine Scholars.
SOURCE: Manhapra A et al. AAAP 2017. Paper session A5.
REPORTING FROM AAAP
Key clinical point: Psychotherapy at the beginning of buprenorphine treatment may affect retention in patients with opioid use disorder.
Major finding: Receipt of any psychotherapy in 2011 was associated with a lower risk of discontinuation of buprenorphine treatment by 2014 (hazard ratio, 0.86; P less than .0001).
Study details: An observational study of 16,190 individuals with OUD.
Disclosures: Dr. Manhapra disclosed that he has received support from the VA Interprofessional Fellowship in Addiction Treatment and from Research in Addiction Medicine Scholars.
Source: Manhapra A et al. AAAP 2017. Paper session A5.
Internet addiction ‘an impairing but treatable problem’
SAN DIEGO – The concept of Internet addiction is imperfect, but it has validity and describes an impairing but treatable problem, according to Diana D. Deister, MD.
“Timely diagnosis can lead to good treatment and symptom improvement,” she said at the annual meeting and scientific symposium of the American Academy of Addiction Psychiatry.
Frameworks for the diagnosis of Internet addiction (IA)/pathological Internet use (PIU) vary but are based mostly on DSM-IV substance abuse and dependency criteria, DSM-IV pathological gambling, or other models. “There are many different checklists and diagnostic instruments you can use, and common synonyms include pathological Internet use, problematic Internet use, and compulsive Internet use,” said Dr. Deister, a child and adolescent psychiatrist at Boston Children’s Hospital. “They may not all refer to the exact same problem you might encounter in clinical practice.”
The Internet Addiction Diagnostic Questionnaire, developed in 1998 by Kimberly S. Young, PsyD, is widely used in research and consists of eight yes or no questions (Cyberpsychol Behav. 1998;1[3]:237-44). Answering “yes” to five out of the eight questions gives you a diagnosis of IA. “There are no preferred symptoms that everybody has to have in order to make the diagnosis, so this is more like the current SUD diagnosis for DSM-5,” Dr. Deister explained. “And there’s no time criteria.”
Clinicians can secure a more detailed assessment of IA symptoms by using the Internet Addiction Test (IAT), which Dr. Young developed in 2013. This tool consists of 20 questions rated on a five-point Likert scale based on frequency, where 0 stands for “not applicable” and 5 stands for “always.” Questions include “How often do you find that you stay online longer than you intended?” “How often do you block out disturbing thoughts about your life with soothing thoughts of the Internet?” And “How often do you feel depressed, moody, or nervous when you are offline, which goes away once you are back online?” A score of 80-100 is considered to meet criteria for IA, a score of 50-79 is considered borderline IA, while a score of below 50 is considered not pathological. Variations of this test can be found in the medical literature, including the Internet Process Addiction Test (Behav Sci. 2015;5:341-52), which contains subscales of Internet use: surfing, online gaming, social networking, and sex.
Dr. Deister noted that imaging studies of brain pathways in IA have demonstrated that mesolimbic dopaminergic projections to the nucleus accumbens from the ventral tegmental area are involved, as well as diminished activity of the ventral medial prefrontal cortex. In a tract-based spatial statistics study, researchers used diffusor tensor imaging (DTI) to study the white matter integrity in 18 adolescents with IA, and 18 age- and gender-matched controls (PLoS ONE. 7[1]:e30253. doi:10.1371/journal.pone.0030253). Compared with controls, the IA group scored higher in the IAT, the Strengths and Difficulties Questionnaire, the Screen for Child Anxiety Related Emotional Disorders scale, and Family Assessment Device measure. DTI scans demonstrated widespread reductions of fractional anisotropy (FA; a measure of white matter health) in major white matter pathways. In addition, significantly negative correlations were found between FA values in the left genu of the corpus callosum and the Screen for Child Anxiety Related Emotional Disorders, and between FA values in the left external capsule and in the IAT.
“The reason these white matter tracts could be important is that there have been previous studies showing that you can improve the health of your white matter tracks through exercise and physical therapy,” Dr. Deister said. “So it may be that this knowledge could lead to new treatments for some of these patients.”
One study of the dose dependence of IA symptoms found that adolescents who met criteria for addictive Internet use, compared with those who met criteria for borderline-addictive Internet use, had higher rates of peer problems (adjusted odds ratio, 7.14 vs. AOR, 5.28); conduct problems (AOR, 22.31 vs. AOR, 4.77); hyperactivity (AOR, 9.49 vs. AOR, 5.58); and emotional symptoms (AOR, 19.06 vs. AOR, 2.85; Int J Adolesc Med. 2014;26[3]:369-75). Multivariate regression analysis revealed that Internet addictive behavior was independently associated with using the Internet for retrieving sexual information (AOR, 1.17) and for participating in games with monetary rewards (AOR, 1.90).
Dr. Deister said IA and aggression go hand in hand. A study of 714 middle school students in Seoul, South Korea, showed a linear association between aggression and IA (Cyberpsychol Behav Soc Netw. 2015;18[5]:260-7). A separate qualitative study of 27 university students in the United States found that the consequences of Internet use led to decreased physical activity, decreased sleep, decreased face-to-face time with other people, and poorer academic performance and concentration (PLoS ONE. 2015;10[2]:e0117372). Another study found that trait anhedonia at baseline predicted greater levels of compulsive Internet use, addiction to online activities, and greater likelihood of addiction to online/offline games (Comput Human Behav. 2016;62:475-9).
Treatment for IA takes all the usual forms, but outcome studies are limited. Cognitive-behavioral therapy for IA was first developed as a 12-week model with a familiar design of behavior modification, cognitive restructuring, harm reduction, and relapse prevention, Dr. Deister said. One study of treatment outcomes that used CBT in 128 IA patients found that 95% of patients were able to manage symptoms at the end of 12 weeks of treatment, while 78% sustained recovery 6 months after treatment (J Behav Addict. 2013;2[4]:209-15). Meanwhile, a meta-analysis of 12 studies related to IA found that medications and psychotherapy were found to be effective for improving IA status, time spent online, and depression and anxiety symptoms (Clin Psychol Rev. 2013;33:317-29). A more recent intention-to-treat analysis of IA disorders in adolescents and adults found that patients referred to treatment showed significant improvements in compulsive Internet use over time (J Behav Addict. 2017;6[4]:579-92). Differential effects were found depending on patients’ compliance, with high compliance generally resulting in significantly higher rates of change.
Dr. Deister reported having no financial disclosures.
SAN DIEGO – The concept of Internet addiction is imperfect, but it has validity and describes an impairing but treatable problem, according to Diana D. Deister, MD.
“Timely diagnosis can lead to good treatment and symptom improvement,” she said at the annual meeting and scientific symposium of the American Academy of Addiction Psychiatry.
Frameworks for the diagnosis of Internet addiction (IA)/pathological Internet use (PIU) vary but are based mostly on DSM-IV substance abuse and dependency criteria, DSM-IV pathological gambling, or other models. “There are many different checklists and diagnostic instruments you can use, and common synonyms include pathological Internet use, problematic Internet use, and compulsive Internet use,” said Dr. Deister, a child and adolescent psychiatrist at Boston Children’s Hospital. “They may not all refer to the exact same problem you might encounter in clinical practice.”
The Internet Addiction Diagnostic Questionnaire, developed in 1998 by Kimberly S. Young, PsyD, is widely used in research and consists of eight yes or no questions (Cyberpsychol Behav. 1998;1[3]:237-44). Answering “yes” to five out of the eight questions gives you a diagnosis of IA. “There are no preferred symptoms that everybody has to have in order to make the diagnosis, so this is more like the current SUD diagnosis for DSM-5,” Dr. Deister explained. “And there’s no time criteria.”
Clinicians can secure a more detailed assessment of IA symptoms by using the Internet Addiction Test (IAT), which Dr. Young developed in 2013. This tool consists of 20 questions rated on a five-point Likert scale based on frequency, where 0 stands for “not applicable” and 5 stands for “always.” Questions include “How often do you find that you stay online longer than you intended?” “How often do you block out disturbing thoughts about your life with soothing thoughts of the Internet?” And “How often do you feel depressed, moody, or nervous when you are offline, which goes away once you are back online?” A score of 80-100 is considered to meet criteria for IA, a score of 50-79 is considered borderline IA, while a score of below 50 is considered not pathological. Variations of this test can be found in the medical literature, including the Internet Process Addiction Test (Behav Sci. 2015;5:341-52), which contains subscales of Internet use: surfing, online gaming, social networking, and sex.
Dr. Deister noted that imaging studies of brain pathways in IA have demonstrated that mesolimbic dopaminergic projections to the nucleus accumbens from the ventral tegmental area are involved, as well as diminished activity of the ventral medial prefrontal cortex. In a tract-based spatial statistics study, researchers used diffusor tensor imaging (DTI) to study the white matter integrity in 18 adolescents with IA, and 18 age- and gender-matched controls (PLoS ONE. 7[1]:e30253. doi:10.1371/journal.pone.0030253). Compared with controls, the IA group scored higher in the IAT, the Strengths and Difficulties Questionnaire, the Screen for Child Anxiety Related Emotional Disorders scale, and Family Assessment Device measure. DTI scans demonstrated widespread reductions of fractional anisotropy (FA; a measure of white matter health) in major white matter pathways. In addition, significantly negative correlations were found between FA values in the left genu of the corpus callosum and the Screen for Child Anxiety Related Emotional Disorders, and between FA values in the left external capsule and in the IAT.
“The reason these white matter tracts could be important is that there have been previous studies showing that you can improve the health of your white matter tracks through exercise and physical therapy,” Dr. Deister said. “So it may be that this knowledge could lead to new treatments for some of these patients.”
One study of the dose dependence of IA symptoms found that adolescents who met criteria for addictive Internet use, compared with those who met criteria for borderline-addictive Internet use, had higher rates of peer problems (adjusted odds ratio, 7.14 vs. AOR, 5.28); conduct problems (AOR, 22.31 vs. AOR, 4.77); hyperactivity (AOR, 9.49 vs. AOR, 5.58); and emotional symptoms (AOR, 19.06 vs. AOR, 2.85; Int J Adolesc Med. 2014;26[3]:369-75). Multivariate regression analysis revealed that Internet addictive behavior was independently associated with using the Internet for retrieving sexual information (AOR, 1.17) and for participating in games with monetary rewards (AOR, 1.90).
Dr. Deister said IA and aggression go hand in hand. A study of 714 middle school students in Seoul, South Korea, showed a linear association between aggression and IA (Cyberpsychol Behav Soc Netw. 2015;18[5]:260-7). A separate qualitative study of 27 university students in the United States found that the consequences of Internet use led to decreased physical activity, decreased sleep, decreased face-to-face time with other people, and poorer academic performance and concentration (PLoS ONE. 2015;10[2]:e0117372). Another study found that trait anhedonia at baseline predicted greater levels of compulsive Internet use, addiction to online activities, and greater likelihood of addiction to online/offline games (Comput Human Behav. 2016;62:475-9).
Treatment for IA takes all the usual forms, but outcome studies are limited. Cognitive-behavioral therapy for IA was first developed as a 12-week model with a familiar design of behavior modification, cognitive restructuring, harm reduction, and relapse prevention, Dr. Deister said. One study of treatment outcomes that used CBT in 128 IA patients found that 95% of patients were able to manage symptoms at the end of 12 weeks of treatment, while 78% sustained recovery 6 months after treatment (J Behav Addict. 2013;2[4]:209-15). Meanwhile, a meta-analysis of 12 studies related to IA found that medications and psychotherapy were found to be effective for improving IA status, time spent online, and depression and anxiety symptoms (Clin Psychol Rev. 2013;33:317-29). A more recent intention-to-treat analysis of IA disorders in adolescents and adults found that patients referred to treatment showed significant improvements in compulsive Internet use over time (J Behav Addict. 2017;6[4]:579-92). Differential effects were found depending on patients’ compliance, with high compliance generally resulting in significantly higher rates of change.
Dr. Deister reported having no financial disclosures.
SAN DIEGO – The concept of Internet addiction is imperfect, but it has validity and describes an impairing but treatable problem, according to Diana D. Deister, MD.
“Timely diagnosis can lead to good treatment and symptom improvement,” she said at the annual meeting and scientific symposium of the American Academy of Addiction Psychiatry.
Frameworks for the diagnosis of Internet addiction (IA)/pathological Internet use (PIU) vary but are based mostly on DSM-IV substance abuse and dependency criteria, DSM-IV pathological gambling, or other models. “There are many different checklists and diagnostic instruments you can use, and common synonyms include pathological Internet use, problematic Internet use, and compulsive Internet use,” said Dr. Deister, a child and adolescent psychiatrist at Boston Children’s Hospital. “They may not all refer to the exact same problem you might encounter in clinical practice.”
The Internet Addiction Diagnostic Questionnaire, developed in 1998 by Kimberly S. Young, PsyD, is widely used in research and consists of eight yes or no questions (Cyberpsychol Behav. 1998;1[3]:237-44). Answering “yes” to five out of the eight questions gives you a diagnosis of IA. “There are no preferred symptoms that everybody has to have in order to make the diagnosis, so this is more like the current SUD diagnosis for DSM-5,” Dr. Deister explained. “And there’s no time criteria.”
Clinicians can secure a more detailed assessment of IA symptoms by using the Internet Addiction Test (IAT), which Dr. Young developed in 2013. This tool consists of 20 questions rated on a five-point Likert scale based on frequency, where 0 stands for “not applicable” and 5 stands for “always.” Questions include “How often do you find that you stay online longer than you intended?” “How often do you block out disturbing thoughts about your life with soothing thoughts of the Internet?” And “How often do you feel depressed, moody, or nervous when you are offline, which goes away once you are back online?” A score of 80-100 is considered to meet criteria for IA, a score of 50-79 is considered borderline IA, while a score of below 50 is considered not pathological. Variations of this test can be found in the medical literature, including the Internet Process Addiction Test (Behav Sci. 2015;5:341-52), which contains subscales of Internet use: surfing, online gaming, social networking, and sex.
Dr. Deister noted that imaging studies of brain pathways in IA have demonstrated that mesolimbic dopaminergic projections to the nucleus accumbens from the ventral tegmental area are involved, as well as diminished activity of the ventral medial prefrontal cortex. In a tract-based spatial statistics study, researchers used diffusor tensor imaging (DTI) to study the white matter integrity in 18 adolescents with IA, and 18 age- and gender-matched controls (PLoS ONE. 7[1]:e30253. doi:10.1371/journal.pone.0030253). Compared with controls, the IA group scored higher in the IAT, the Strengths and Difficulties Questionnaire, the Screen for Child Anxiety Related Emotional Disorders scale, and Family Assessment Device measure. DTI scans demonstrated widespread reductions of fractional anisotropy (FA; a measure of white matter health) in major white matter pathways. In addition, significantly negative correlations were found between FA values in the left genu of the corpus callosum and the Screen for Child Anxiety Related Emotional Disorders, and between FA values in the left external capsule and in the IAT.
“The reason these white matter tracts could be important is that there have been previous studies showing that you can improve the health of your white matter tracks through exercise and physical therapy,” Dr. Deister said. “So it may be that this knowledge could lead to new treatments for some of these patients.”
One study of the dose dependence of IA symptoms found that adolescents who met criteria for addictive Internet use, compared with those who met criteria for borderline-addictive Internet use, had higher rates of peer problems (adjusted odds ratio, 7.14 vs. AOR, 5.28); conduct problems (AOR, 22.31 vs. AOR, 4.77); hyperactivity (AOR, 9.49 vs. AOR, 5.58); and emotional symptoms (AOR, 19.06 vs. AOR, 2.85; Int J Adolesc Med. 2014;26[3]:369-75). Multivariate regression analysis revealed that Internet addictive behavior was independently associated with using the Internet for retrieving sexual information (AOR, 1.17) and for participating in games with monetary rewards (AOR, 1.90).
Dr. Deister said IA and aggression go hand in hand. A study of 714 middle school students in Seoul, South Korea, showed a linear association between aggression and IA (Cyberpsychol Behav Soc Netw. 2015;18[5]:260-7). A separate qualitative study of 27 university students in the United States found that the consequences of Internet use led to decreased physical activity, decreased sleep, decreased face-to-face time with other people, and poorer academic performance and concentration (PLoS ONE. 2015;10[2]:e0117372). Another study found that trait anhedonia at baseline predicted greater levels of compulsive Internet use, addiction to online activities, and greater likelihood of addiction to online/offline games (Comput Human Behav. 2016;62:475-9).
Treatment for IA takes all the usual forms, but outcome studies are limited. Cognitive-behavioral therapy for IA was first developed as a 12-week model with a familiar design of behavior modification, cognitive restructuring, harm reduction, and relapse prevention, Dr. Deister said. One study of treatment outcomes that used CBT in 128 IA patients found that 95% of patients were able to manage symptoms at the end of 12 weeks of treatment, while 78% sustained recovery 6 months after treatment (J Behav Addict. 2013;2[4]:209-15). Meanwhile, a meta-analysis of 12 studies related to IA found that medications and psychotherapy were found to be effective for improving IA status, time spent online, and depression and anxiety symptoms (Clin Psychol Rev. 2013;33:317-29). A more recent intention-to-treat analysis of IA disorders in adolescents and adults found that patients referred to treatment showed significant improvements in compulsive Internet use over time (J Behav Addict. 2017;6[4]:579-92). Differential effects were found depending on patients’ compliance, with high compliance generally resulting in significantly higher rates of change.
Dr. Deister reported having no financial disclosures.
REPORTING FROM AAAP
Two MS diagnostic criteria found to have similar accuracy
The 2016 Magnetic Resonance Imaging in Multiple Sclerosis (MAGNIMS) criteria showed accuracy similar to that of the 2010 McDonald criteria in predicting the development of clinically definite multiple sclerosis, a retrospective study found.
“Among the different modifications proposed, our results support removal of the distinction between symptomatic and asymptomatic lesions, which simplifies the clinical use of MRI criteria, and suggest that further consideration is given to increasing the number of lesions needed to define periventricular involvement from one to three, because this might slightly increase specificity,” wrote researchers led by Massimo Filippi, MD. The report was published Dec. 21, 2017, in The Lancet Neurology. “Further effort is still needed to improve cortical lesion assessment and more studies should be done to evaluate the effect of including optic nerve assessment as an additional DIS [dissemination in space] criterion.”
Dr. Filippi, of the neuroimaging research unit in the division of neuroscience at San Raffaele Scientific Institute at Vita-Salute San Raffaele University, Milan, and his coauthors at eight centers reported that of the 368 patients, 189 (51%) developed clinically definite MS at the last evaluation, which occurred at a median of 50 months. At 36 months, DIS alone showed high sensitivity in the 2010 McDonald and 2016 MAGNIMS criteria (91% vs. 93%, respectively), similar specificity (33% vs. 32%), and similar area under the curve values (AUC, 0.62 vs. 0.63). Inclusion of symptomatic lesions did not alter performance. The researchers also found that requiring three periventricular lesions reduced sensitivity to 85% and increased specificity to 40%, but did not affect AUC values (it stood at 0.63). When optic nerve evaluation was included, sensitivity was similar (92%), while specificity fell to 26% and AUC dropped to 0.59.
The 2016 MAGNIMS and 2010 McDonald criteria achieved similar sensitivity, specificity, and AUC values when compared on the performance of DIT criteria and DIS plus DIT criteria.
“For both sets of criteria, specificity was lower than that of previous studies that evaluated the diagnostic performance of the 2010 McDonald criteria,” the authors wrote. “Several factors could help explain our findings, including the different follow-up durations, the statistical methods (e.g., using a time-to-event analysis in our study), and the effect of treatment, which might have delayed or prevented the occurrence of the second attack during the study period.” They acknowledged certain limitations of the study, including its retrospective design and the fact that patients were recruited in highly specialized centers, which may have resulted in the selection of patients at higher risk of conversion to clinically definite multiple sclerosis.
The study was funded by the U.K. MS Society, the National Institute for Health Research University College London Hospitals Biomedical Research Centre, and the Dutch MS Research Foundation. The authors reported having numerous financial disclosures with the pharmaceutical industry.
SOURCE: Filippi M et al., Lancet Neurol. 2017 Dec 21. doi: 10.1016/S1474-4422(17)30469-6.
As multiple sclerosis diagnosis evolves, revisions to existing diagnostic criteria have increased sensitivity, which in turn has helped clinicians establish earlier diagnosis. In an editorial published online Dec. 21, 2017, in The Lancet Neurology (doi: 10.1016/S1474-4422(17)30459-3), Anne H. Cross, MD, and Robert N. Naismith, MD, point out that while the study by Dr. Filippi et al. showed that for both sets of MRI criteria sensitivity was greater than specificity for predicting clinically definite multiple sclerosis, the modest specificity is cause for concern. They cited one study (Neurology 2016;87:1393-9) that emphasized the importance of not misdiagnosing other CNS diseases as multiple sclerosis. “In that study at four academic medical centers, 110 people seen over a period of less than 1.5 years were found to have been misdiagnosed,” wrote Dr. Cross and Dr. Naismith, both with the department of neurology at Washington University, St. Louis. “[Seventy percent] of the 110 individuals had received disease-modifying therapy and 31% had unnecessary morbidity. Leading factors contributing to erroneous diagnosis in the study included overreliance on MRI abnormalities in patients with non-specific neurological symptoms.”
The authors noted that vascular and other diseases can cause MRI abnormalities that could meet the 2016 Magnetic Resonance Imaging in Multiple Sclerosis (MAGNIMS) recommendations or the 2010 and 2017 McDonald MRI criteria. For example, patients with monophasic inflammatory and infectious diseases might have gadolinium-enhancing lesions that meet the 2017 McDonald criteria for dissemination in time, which require only the simultaneous presence of gadolinium-enhancing and gadolinium-negative lesions in the proper locations. For patients with an atypical presentation who meet the 2010 and 2017 McDonald or 2016 MAGNIMS recommendations, they advise clinicians to weigh all of the observed imaging features (including the number of periventricular lesions, along with lesion size, shape, and location) to improve diagnostic specificity and help to limit misdiagnoses.
Dr. Cross has received consulting fees from AbbVie, Bayer, Biogen, EMD Serono, Genentech/Roche, Genzyme/Sanofi, Mallinckodt, Novartis, and Teva. Dr. Naismith has consulted for Acorda, Alkermes, Bayer, Biogen, EMD Serono, Genentech, Genzyme, Novartis, and Teva.
As multiple sclerosis diagnosis evolves, revisions to existing diagnostic criteria have increased sensitivity, which in turn has helped clinicians establish earlier diagnosis. In an editorial published online Dec. 21, 2017, in The Lancet Neurology (doi: 10.1016/S1474-4422(17)30459-3), Anne H. Cross, MD, and Robert N. Naismith, MD, point out that while the study by Dr. Filippi et al. showed that for both sets of MRI criteria sensitivity was greater than specificity for predicting clinically definite multiple sclerosis, the modest specificity is cause for concern. They cited one study (Neurology 2016;87:1393-9) that emphasized the importance of not misdiagnosing other CNS diseases as multiple sclerosis. “In that study at four academic medical centers, 110 people seen over a period of less than 1.5 years were found to have been misdiagnosed,” wrote Dr. Cross and Dr. Naismith, both with the department of neurology at Washington University, St. Louis. “[Seventy percent] of the 110 individuals had received disease-modifying therapy and 31% had unnecessary morbidity. Leading factors contributing to erroneous diagnosis in the study included overreliance on MRI abnormalities in patients with non-specific neurological symptoms.”
The authors noted that vascular and other diseases can cause MRI abnormalities that could meet the 2016 Magnetic Resonance Imaging in Multiple Sclerosis (MAGNIMS) recommendations or the 2010 and 2017 McDonald MRI criteria. For example, patients with monophasic inflammatory and infectious diseases might have gadolinium-enhancing lesions that meet the 2017 McDonald criteria for dissemination in time, which require only the simultaneous presence of gadolinium-enhancing and gadolinium-negative lesions in the proper locations. For patients with an atypical presentation who meet the 2010 and 2017 McDonald or 2016 MAGNIMS recommendations, they advise clinicians to weigh all of the observed imaging features (including the number of periventricular lesions, along with lesion size, shape, and location) to improve diagnostic specificity and help to limit misdiagnoses.
Dr. Cross has received consulting fees from AbbVie, Bayer, Biogen, EMD Serono, Genentech/Roche, Genzyme/Sanofi, Mallinckodt, Novartis, and Teva. Dr. Naismith has consulted for Acorda, Alkermes, Bayer, Biogen, EMD Serono, Genentech, Genzyme, Novartis, and Teva.
As multiple sclerosis diagnosis evolves, revisions to existing diagnostic criteria have increased sensitivity, which in turn has helped clinicians establish earlier diagnosis. In an editorial published online Dec. 21, 2017, in The Lancet Neurology (doi: 10.1016/S1474-4422(17)30459-3), Anne H. Cross, MD, and Robert N. Naismith, MD, point out that while the study by Dr. Filippi et al. showed that for both sets of MRI criteria sensitivity was greater than specificity for predicting clinically definite multiple sclerosis, the modest specificity is cause for concern. They cited one study (Neurology 2016;87:1393-9) that emphasized the importance of not misdiagnosing other CNS diseases as multiple sclerosis. “In that study at four academic medical centers, 110 people seen over a period of less than 1.5 years were found to have been misdiagnosed,” wrote Dr. Cross and Dr. Naismith, both with the department of neurology at Washington University, St. Louis. “[Seventy percent] of the 110 individuals had received disease-modifying therapy and 31% had unnecessary morbidity. Leading factors contributing to erroneous diagnosis in the study included overreliance on MRI abnormalities in patients with non-specific neurological symptoms.”
The authors noted that vascular and other diseases can cause MRI abnormalities that could meet the 2016 Magnetic Resonance Imaging in Multiple Sclerosis (MAGNIMS) recommendations or the 2010 and 2017 McDonald MRI criteria. For example, patients with monophasic inflammatory and infectious diseases might have gadolinium-enhancing lesions that meet the 2017 McDonald criteria for dissemination in time, which require only the simultaneous presence of gadolinium-enhancing and gadolinium-negative lesions in the proper locations. For patients with an atypical presentation who meet the 2010 and 2017 McDonald or 2016 MAGNIMS recommendations, they advise clinicians to weigh all of the observed imaging features (including the number of periventricular lesions, along with lesion size, shape, and location) to improve diagnostic specificity and help to limit misdiagnoses.
Dr. Cross has received consulting fees from AbbVie, Bayer, Biogen, EMD Serono, Genentech/Roche, Genzyme/Sanofi, Mallinckodt, Novartis, and Teva. Dr. Naismith has consulted for Acorda, Alkermes, Bayer, Biogen, EMD Serono, Genentech, Genzyme, Novartis, and Teva.
The 2016 Magnetic Resonance Imaging in Multiple Sclerosis (MAGNIMS) criteria showed accuracy similar to that of the 2010 McDonald criteria in predicting the development of clinically definite multiple sclerosis, a retrospective study found.
“Among the different modifications proposed, our results support removal of the distinction between symptomatic and asymptomatic lesions, which simplifies the clinical use of MRI criteria, and suggest that further consideration is given to increasing the number of lesions needed to define periventricular involvement from one to three, because this might slightly increase specificity,” wrote researchers led by Massimo Filippi, MD. The report was published Dec. 21, 2017, in The Lancet Neurology. “Further effort is still needed to improve cortical lesion assessment and more studies should be done to evaluate the effect of including optic nerve assessment as an additional DIS [dissemination in space] criterion.”
Dr. Filippi, of the neuroimaging research unit in the division of neuroscience at San Raffaele Scientific Institute at Vita-Salute San Raffaele University, Milan, and his coauthors at eight centers reported that of the 368 patients, 189 (51%) developed clinically definite MS at the last evaluation, which occurred at a median of 50 months. At 36 months, DIS alone showed high sensitivity in the 2010 McDonald and 2016 MAGNIMS criteria (91% vs. 93%, respectively), similar specificity (33% vs. 32%), and similar area under the curve values (AUC, 0.62 vs. 0.63). Inclusion of symptomatic lesions did not alter performance. The researchers also found that requiring three periventricular lesions reduced sensitivity to 85% and increased specificity to 40%, but did not affect AUC values (it stood at 0.63). When optic nerve evaluation was included, sensitivity was similar (92%), while specificity fell to 26% and AUC dropped to 0.59.
The 2016 MAGNIMS and 2010 McDonald criteria achieved similar sensitivity, specificity, and AUC values when compared on the performance of DIT criteria and DIS plus DIT criteria.
“For both sets of criteria, specificity was lower than that of previous studies that evaluated the diagnostic performance of the 2010 McDonald criteria,” the authors wrote. “Several factors could help explain our findings, including the different follow-up durations, the statistical methods (e.g., using a time-to-event analysis in our study), and the effect of treatment, which might have delayed or prevented the occurrence of the second attack during the study period.” They acknowledged certain limitations of the study, including its retrospective design and the fact that patients were recruited in highly specialized centers, which may have resulted in the selection of patients at higher risk of conversion to clinically definite multiple sclerosis.
The study was funded by the U.K. MS Society, the National Institute for Health Research University College London Hospitals Biomedical Research Centre, and the Dutch MS Research Foundation. The authors reported having numerous financial disclosures with the pharmaceutical industry.
SOURCE: Filippi M et al., Lancet Neurol. 2017 Dec 21. doi: 10.1016/S1474-4422(17)30469-6.
The 2016 Magnetic Resonance Imaging in Multiple Sclerosis (MAGNIMS) criteria showed accuracy similar to that of the 2010 McDonald criteria in predicting the development of clinically definite multiple sclerosis, a retrospective study found.
“Among the different modifications proposed, our results support removal of the distinction between symptomatic and asymptomatic lesions, which simplifies the clinical use of MRI criteria, and suggest that further consideration is given to increasing the number of lesions needed to define periventricular involvement from one to three, because this might slightly increase specificity,” wrote researchers led by Massimo Filippi, MD. The report was published Dec. 21, 2017, in The Lancet Neurology. “Further effort is still needed to improve cortical lesion assessment and more studies should be done to evaluate the effect of including optic nerve assessment as an additional DIS [dissemination in space] criterion.”
Dr. Filippi, of the neuroimaging research unit in the division of neuroscience at San Raffaele Scientific Institute at Vita-Salute San Raffaele University, Milan, and his coauthors at eight centers reported that of the 368 patients, 189 (51%) developed clinically definite MS at the last evaluation, which occurred at a median of 50 months. At 36 months, DIS alone showed high sensitivity in the 2010 McDonald and 2016 MAGNIMS criteria (91% vs. 93%, respectively), similar specificity (33% vs. 32%), and similar area under the curve values (AUC, 0.62 vs. 0.63). Inclusion of symptomatic lesions did not alter performance. The researchers also found that requiring three periventricular lesions reduced sensitivity to 85% and increased specificity to 40%, but did not affect AUC values (it stood at 0.63). When optic nerve evaluation was included, sensitivity was similar (92%), while specificity fell to 26% and AUC dropped to 0.59.
The 2016 MAGNIMS and 2010 McDonald criteria achieved similar sensitivity, specificity, and AUC values when compared on the performance of DIT criteria and DIS plus DIT criteria.
“For both sets of criteria, specificity was lower than that of previous studies that evaluated the diagnostic performance of the 2010 McDonald criteria,” the authors wrote. “Several factors could help explain our findings, including the different follow-up durations, the statistical methods (e.g., using a time-to-event analysis in our study), and the effect of treatment, which might have delayed or prevented the occurrence of the second attack during the study period.” They acknowledged certain limitations of the study, including its retrospective design and the fact that patients were recruited in highly specialized centers, which may have resulted in the selection of patients at higher risk of conversion to clinically definite multiple sclerosis.
The study was funded by the U.K. MS Society, the National Institute for Health Research University College London Hospitals Biomedical Research Centre, and the Dutch MS Research Foundation. The authors reported having numerous financial disclosures with the pharmaceutical industry.
SOURCE: Filippi M et al., Lancet Neurol. 2017 Dec 21. doi: 10.1016/S1474-4422(17)30469-6.
FROM THE LANCET NEUROLOGY
Key clinical point:
Major finding: The 2016 MAGNIMS criteria and 2010 McDonald criteria performed similarly for predicting clinically definite multiple sclerosis (a sensitivity of 91% and 93%, respectively, and a specificity of 33% and 32%).
Study details: A retrospective study of 368 patients with clinically isolated syndrome.
Disclosures: The study was funded by the U.K. MS Society, the National Institute for Health Research University College London Hospitals Biomedical Research Centre, and the Dutch MS Research Foundation. The study authors reported having numerous financial disclosures.
Source: Filippi M et al., Lancet Neurol. 2017 Dec 21. doi: 10.1016/S1474-4422(17)30469-6.