User login
How to adjust drug dosing after bariatric surgery
Bariatric surgery has increased 10-fold in the United States over the past decade.1 Because one-third of bariatric candidates take psychiatric medications, psychiatric input on postoperative management is in demand.2
Despite this surgery’s rising popularity, no data exist to guide psychotropic dosing in patients with altered GI environments and who experience massive postoperative weight loss. Evidence and clinical experience support these recommendations:
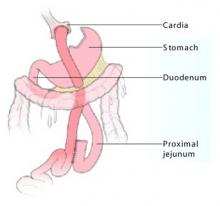
Managing changes in psychotropic absorption. The most common procedure, the Roux-en-Y gastric bypass (RYGB), bypasses the duodenum, proximal jejunum, and all of the stomach except the cardia (Figure). Because ingested food is normally absorbed in the duodenum and jejunum, a bypass results in relative malabsorption of food. Orally ingested food and medications pass into the cardia, where they are not exposed to acid.
One novel in vitro study2 examined the dissolution of 22 psychotropics in a simulated GI environment of control and post-RYGB states. Twelve medications dissolved differently in a postoperative environment than in the control state; 10 dissolved much less than expected.
The effect of bariatric surgery on in vivo absorption of commonly used psychotropics has not been studied. For safe yet effective dosing immediately after surgery, try:
- Using immediate-release psychotropics.3 Time-released medications are designed to dissolve gradually within the full intestinal tract. Extended-release formulations will probably have markedly different pharmacokinetics after RYGB. Coated pills require stomach acid to release active ingredients, so crush oral medications in the immediate postoperative period.
- Monitoring serum drug levels of medications with a narrow therapeutic index. Also measure preoperative blood levels while the patient feels well. This baseline will provide a target to aim for if the patient has a postoperative relapse.
Figure Roux-en-Y gastric bypass
Vertical stapling of the upper stomach creates a small pouch, and a Y-shaped section of small intestine attached to the pouch allows food to bypass the duodenum and part of the jejunum.
Illustration: Jennifer Fairman
Postoperative weight loss. Many physiologic factors influence drug absorption, such as gastric emptying time and the integrity and surface area of the epithelium. The gut has an impressive capacity to compensate for loss of function, so absorption after surgery may eventually normalize. By that time, however, marked weight loss can complicate the clinical picture.
Compared with nonobese persons, obese persons have an increased proportion of adipose tissue, as well as increased total body water, lean body mass, visceral organ mass, and higher glomerular filtration rate.
Postoperative bariatric patients often lose more than 100 pounds of adipose tissue. This type of weight loss mostly affects lipid-soluble drugs with a large volume of distribution (Vd) that readily cross cell membranes, such as fluoxetine. Drugs with a large Vd, such as fluoxetine (Table), reach all major compartments of distribution, which in a normal weight individual include: plasma (5%), interstitial fluid (16%), intracellular fluid (35%), transcellular fluid (2%), and fat (20%). Because the amount of fat in an overweight patient is initially very high but rapidly decreases after bariatric surgery, drugs with a large Vd can shift into other compartments.
For drugs with a small Vd, such as lithium, a lower maintenance dosage may be required because of decreased glomerular filtration following marked weight loss.4
Table
Common drugs’ volume of distribution (Vd)
| Drug | Extent of distribution | Volume of distribution |
|---|---|---|
| Fluoxetine | Large | 10 to 103 L/kg |
| Citalopram | Moderate | 14 to 17 L/kg |
| Venlafaxine | Moderate | 6 to 7 L/kg |
| Oxcarbazepine | Small | 0.7 L/kg |
| Lithium | Small | 0.4 to 0.6 L/kg |
| Valproic acid | Small | 0.1 to 0.4 L/kg |
1. Tsao A. Weighing bariatric surgery’s risks. BusinessWeek Online. Available at: http://www.businessweek.com/bwdaily/dnflash/oct2004/nf20041028_0264_db092.htm. Accessed Nov. 28, 2005.
2. Seaman JS, Bowers SP, Dixon P, Schindler L. Dissolution of common psychiatric medications in a Roux-en-Y gastric bypass model. Psychosomatics 2005;46(3):250-3.
3. Malone M. Altered drug disposition in obesity and after bariatric surgery. Nutr Clin Pract 2003;18(2):131-5.
4. Sproule BA, Hardy BG, Shulman KI. Differential pharmacokinetics of lithium in elderly patients. Drugs Aging 2000;16(3):165-77.
Dr. McAlpine is assistant professor of psychiatry and director of eating disorders services, Mayo Clinic, Rochester, MN.
Bariatric surgery has increased 10-fold in the United States over the past decade.1 Because one-third of bariatric candidates take psychiatric medications, psychiatric input on postoperative management is in demand.2
Despite this surgery’s rising popularity, no data exist to guide psychotropic dosing in patients with altered GI environments and who experience massive postoperative weight loss. Evidence and clinical experience support these recommendations:
Managing changes in psychotropic absorption. The most common procedure, the Roux-en-Y gastric bypass (RYGB), bypasses the duodenum, proximal jejunum, and all of the stomach except the cardia (Figure). Because ingested food is normally absorbed in the duodenum and jejunum, a bypass results in relative malabsorption of food. Orally ingested food and medications pass into the cardia, where they are not exposed to acid.
One novel in vitro study2 examined the dissolution of 22 psychotropics in a simulated GI environment of control and post-RYGB states. Twelve medications dissolved differently in a postoperative environment than in the control state; 10 dissolved much less than expected.
The effect of bariatric surgery on in vivo absorption of commonly used psychotropics has not been studied. For safe yet effective dosing immediately after surgery, try:
- Using immediate-release psychotropics.3 Time-released medications are designed to dissolve gradually within the full intestinal tract. Extended-release formulations will probably have markedly different pharmacokinetics after RYGB. Coated pills require stomach acid to release active ingredients, so crush oral medications in the immediate postoperative period.
- Monitoring serum drug levels of medications with a narrow therapeutic index. Also measure preoperative blood levels while the patient feels well. This baseline will provide a target to aim for if the patient has a postoperative relapse.
Figure Roux-en-Y gastric bypass
Vertical stapling of the upper stomach creates a small pouch, and a Y-shaped section of small intestine attached to the pouch allows food to bypass the duodenum and part of the jejunum.
Illustration: Jennifer Fairman
Postoperative weight loss. Many physiologic factors influence drug absorption, such as gastric emptying time and the integrity and surface area of the epithelium. The gut has an impressive capacity to compensate for loss of function, so absorption after surgery may eventually normalize. By that time, however, marked weight loss can complicate the clinical picture.
Compared with nonobese persons, obese persons have an increased proportion of adipose tissue, as well as increased total body water, lean body mass, visceral organ mass, and higher glomerular filtration rate.
Postoperative bariatric patients often lose more than 100 pounds of adipose tissue. This type of weight loss mostly affects lipid-soluble drugs with a large volume of distribution (Vd) that readily cross cell membranes, such as fluoxetine. Drugs with a large Vd, such as fluoxetine (Table), reach all major compartments of distribution, which in a normal weight individual include: plasma (5%), interstitial fluid (16%), intracellular fluid (35%), transcellular fluid (2%), and fat (20%). Because the amount of fat in an overweight patient is initially very high but rapidly decreases after bariatric surgery, drugs with a large Vd can shift into other compartments.
For drugs with a small Vd, such as lithium, a lower maintenance dosage may be required because of decreased glomerular filtration following marked weight loss.4
Table
Common drugs’ volume of distribution (Vd)
| Drug | Extent of distribution | Volume of distribution |
|---|---|---|
| Fluoxetine | Large | 10 to 103 L/kg |
| Citalopram | Moderate | 14 to 17 L/kg |
| Venlafaxine | Moderate | 6 to 7 L/kg |
| Oxcarbazepine | Small | 0.7 L/kg |
| Lithium | Small | 0.4 to 0.6 L/kg |
| Valproic acid | Small | 0.1 to 0.4 L/kg |
Bariatric surgery has increased 10-fold in the United States over the past decade.1 Because one-third of bariatric candidates take psychiatric medications, psychiatric input on postoperative management is in demand.2
Despite this surgery’s rising popularity, no data exist to guide psychotropic dosing in patients with altered GI environments and who experience massive postoperative weight loss. Evidence and clinical experience support these recommendations:
Managing changes in psychotropic absorption. The most common procedure, the Roux-en-Y gastric bypass (RYGB), bypasses the duodenum, proximal jejunum, and all of the stomach except the cardia (Figure). Because ingested food is normally absorbed in the duodenum and jejunum, a bypass results in relative malabsorption of food. Orally ingested food and medications pass into the cardia, where they are not exposed to acid.
One novel in vitro study2 examined the dissolution of 22 psychotropics in a simulated GI environment of control and post-RYGB states. Twelve medications dissolved differently in a postoperative environment than in the control state; 10 dissolved much less than expected.
The effect of bariatric surgery on in vivo absorption of commonly used psychotropics has not been studied. For safe yet effective dosing immediately after surgery, try:
- Using immediate-release psychotropics.3 Time-released medications are designed to dissolve gradually within the full intestinal tract. Extended-release formulations will probably have markedly different pharmacokinetics after RYGB. Coated pills require stomach acid to release active ingredients, so crush oral medications in the immediate postoperative period.
- Monitoring serum drug levels of medications with a narrow therapeutic index. Also measure preoperative blood levels while the patient feels well. This baseline will provide a target to aim for if the patient has a postoperative relapse.
Figure Roux-en-Y gastric bypass
Vertical stapling of the upper stomach creates a small pouch, and a Y-shaped section of small intestine attached to the pouch allows food to bypass the duodenum and part of the jejunum.
Illustration: Jennifer Fairman
Postoperative weight loss. Many physiologic factors influence drug absorption, such as gastric emptying time and the integrity and surface area of the epithelium. The gut has an impressive capacity to compensate for loss of function, so absorption after surgery may eventually normalize. By that time, however, marked weight loss can complicate the clinical picture.
Compared with nonobese persons, obese persons have an increased proportion of adipose tissue, as well as increased total body water, lean body mass, visceral organ mass, and higher glomerular filtration rate.
Postoperative bariatric patients often lose more than 100 pounds of adipose tissue. This type of weight loss mostly affects lipid-soluble drugs with a large volume of distribution (Vd) that readily cross cell membranes, such as fluoxetine. Drugs with a large Vd, such as fluoxetine (Table), reach all major compartments of distribution, which in a normal weight individual include: plasma (5%), interstitial fluid (16%), intracellular fluid (35%), transcellular fluid (2%), and fat (20%). Because the amount of fat in an overweight patient is initially very high but rapidly decreases after bariatric surgery, drugs with a large Vd can shift into other compartments.
For drugs with a small Vd, such as lithium, a lower maintenance dosage may be required because of decreased glomerular filtration following marked weight loss.4
Table
Common drugs’ volume of distribution (Vd)
| Drug | Extent of distribution | Volume of distribution |
|---|---|---|
| Fluoxetine | Large | 10 to 103 L/kg |
| Citalopram | Moderate | 14 to 17 L/kg |
| Venlafaxine | Moderate | 6 to 7 L/kg |
| Oxcarbazepine | Small | 0.7 L/kg |
| Lithium | Small | 0.4 to 0.6 L/kg |
| Valproic acid | Small | 0.1 to 0.4 L/kg |
1. Tsao A. Weighing bariatric surgery’s risks. BusinessWeek Online. Available at: http://www.businessweek.com/bwdaily/dnflash/oct2004/nf20041028_0264_db092.htm. Accessed Nov. 28, 2005.
2. Seaman JS, Bowers SP, Dixon P, Schindler L. Dissolution of common psychiatric medications in a Roux-en-Y gastric bypass model. Psychosomatics 2005;46(3):250-3.
3. Malone M. Altered drug disposition in obesity and after bariatric surgery. Nutr Clin Pract 2003;18(2):131-5.
4. Sproule BA, Hardy BG, Shulman KI. Differential pharmacokinetics of lithium in elderly patients. Drugs Aging 2000;16(3):165-77.
Dr. McAlpine is assistant professor of psychiatry and director of eating disorders services, Mayo Clinic, Rochester, MN.
1. Tsao A. Weighing bariatric surgery’s risks. BusinessWeek Online. Available at: http://www.businessweek.com/bwdaily/dnflash/oct2004/nf20041028_0264_db092.htm. Accessed Nov. 28, 2005.
2. Seaman JS, Bowers SP, Dixon P, Schindler L. Dissolution of common psychiatric medications in a Roux-en-Y gastric bypass model. Psychosomatics 2005;46(3):250-3.
3. Malone M. Altered drug disposition in obesity and after bariatric surgery. Nutr Clin Pract 2003;18(2):131-5.
4. Sproule BA, Hardy BG, Shulman KI. Differential pharmacokinetics of lithium in elderly patients. Drugs Aging 2000;16(3):165-77.
Dr. McAlpine is assistant professor of psychiatry and director of eating disorders services, Mayo Clinic, Rochester, MN.