User login
Racial Disparities in HIV Diagnoses Persist
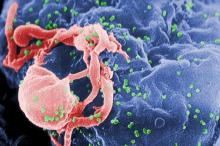
Blacks/African Americans continue to bear a disproportionate burden of HIV diagnoses compared with any other racial or ethnic groups, according to data published Feb. 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report.
Between 2005 and 2008, blacks/African Americans accounted for 50.3% of all HIV diagnoses in 37 states reporting to the CDC through HIV surveillance systems, despite representing just 13.6% of the population in those states, the authors wrote. Additionally, in 2008 alone, the rates of HIV diagnosis among African American males and females, respectively, were 8 and 19 times the rates reported for white males and females and 2 and 4 times the rates reported for Hispanic males and females, they stated.
"In nearly every demographic and transmission category, the largest percentages of HIV diagnoses were among blacks/African Americans," the authors wrote.
For example, during the 4-year reporting period, 56.1% of HIV diagnoses were made in individuals aged 25-44 years, and of this age group, blacks/African Americans accounted for 46.4% of them. Similarly, among adolescent and adult males, blacks/African Americans accounted for the largest percentage of HIV diagnoses overall, at 44.8%, compared with 19% and 33.6% among Hispanic/Latino and white males, respectively. They also accounted for the largest percentage of HIV diagnoses in the South, at 50.1% compared with 16.5% and 31.7% among Hispanic/Latino and white males, and in the Northeast, at 42.1% compared with 28.3% and 25.5% among Hispanic/Latino and white males, the report stated.
Among females over the 4-year period, blacks/African Americans accounted for 50.3% of the HIV diagnoses overall, compared with 17.8% and 29.4% for Hispanic/Latino and white females, respectively, and they also accounted for the majority of HIV diagnoses in the South, Midwest, and Northeast, according to the report (MMWR Morb. Mortal. Wkly. Rep. 2011;60:93-8).
When assessed by transmission category, the racial disparities were most pronounced in the rates of HIV diagnoses attributed to heterosexual contact. Nearly 71% of the males in this transmission category were black/African American, while 16.3% were Hispanic/Latino, and 11% were white. Among the females, 68% of those in the heterosexual transmission category were black/African American, compared with 14.3% who were Hispanic/Latino and 15.2% who were white.
Among black/African American males, HIV transmissions were classified as male-to-male sexual contact in 61.1% of the diagnoses, heterosexual contact in 23.1%, injection drug use in 11.9%, and both male-to-male sexual contact and infection drug use in 3.6%, the analysis showed. In black/African American females, 85.2% of HIV transmissions were through heterosexual contact and 14% were through infection drug use, according to the report.
In a trend analysis for the 4 years covered by the report, rates of HIV diagnoses increased among black/African American males while trends in other race/ethnic groups and gender groups remained stable.
"Lack of knowledge of HIV status and missed opportunities to diagnose HIV in routine clinical settings are contributing factors to the HIV epidemic among blacks/African Americans," the authors wrote in their editorial comment. "Ongoing and increased HIV testing and efforts to ensure referral and access to HIV-related primary medical care are warranted," they stated, as are comprehensive approaches "that take into account patient-specific behavioral risk factors, such as having multiple sex partners and unprotected sex, in addition to underlying factors such as poverty, unequal access to health care, incarceration, lack of education, stigma, homophobia, sexism, and racism."
No conflicts of interest were reported.
Blacks/African Americans continue to bear a disproportionate burden of HIV diagnoses compared with any other racial or ethnic groups, according to data published Feb. 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report.
Between 2005 and 2008, blacks/African Americans accounted for 50.3% of all HIV diagnoses in 37 states reporting to the CDC through HIV surveillance systems, despite representing just 13.6% of the population in those states, the authors wrote. Additionally, in 2008 alone, the rates of HIV diagnosis among African American males and females, respectively, were 8 and 19 times the rates reported for white males and females and 2 and 4 times the rates reported for Hispanic males and females, they stated.
"In nearly every demographic and transmission category, the largest percentages of HIV diagnoses were among blacks/African Americans," the authors wrote.
For example, during the 4-year reporting period, 56.1% of HIV diagnoses were made in individuals aged 25-44 years, and of this age group, blacks/African Americans accounted for 46.4% of them. Similarly, among adolescent and adult males, blacks/African Americans accounted for the largest percentage of HIV diagnoses overall, at 44.8%, compared with 19% and 33.6% among Hispanic/Latino and white males, respectively. They also accounted for the largest percentage of HIV diagnoses in the South, at 50.1% compared with 16.5% and 31.7% among Hispanic/Latino and white males, and in the Northeast, at 42.1% compared with 28.3% and 25.5% among Hispanic/Latino and white males, the report stated.
Among females over the 4-year period, blacks/African Americans accounted for 50.3% of the HIV diagnoses overall, compared with 17.8% and 29.4% for Hispanic/Latino and white females, respectively, and they also accounted for the majority of HIV diagnoses in the South, Midwest, and Northeast, according to the report (MMWR Morb. Mortal. Wkly. Rep. 2011;60:93-8).
When assessed by transmission category, the racial disparities were most pronounced in the rates of HIV diagnoses attributed to heterosexual contact. Nearly 71% of the males in this transmission category were black/African American, while 16.3% were Hispanic/Latino, and 11% were white. Among the females, 68% of those in the heterosexual transmission category were black/African American, compared with 14.3% who were Hispanic/Latino and 15.2% who were white.
Among black/African American males, HIV transmissions were classified as male-to-male sexual contact in 61.1% of the diagnoses, heterosexual contact in 23.1%, injection drug use in 11.9%, and both male-to-male sexual contact and infection drug use in 3.6%, the analysis showed. In black/African American females, 85.2% of HIV transmissions were through heterosexual contact and 14% were through infection drug use, according to the report.
In a trend analysis for the 4 years covered by the report, rates of HIV diagnoses increased among black/African American males while trends in other race/ethnic groups and gender groups remained stable.
"Lack of knowledge of HIV status and missed opportunities to diagnose HIV in routine clinical settings are contributing factors to the HIV epidemic among blacks/African Americans," the authors wrote in their editorial comment. "Ongoing and increased HIV testing and efforts to ensure referral and access to HIV-related primary medical care are warranted," they stated, as are comprehensive approaches "that take into account patient-specific behavioral risk factors, such as having multiple sex partners and unprotected sex, in addition to underlying factors such as poverty, unequal access to health care, incarceration, lack of education, stigma, homophobia, sexism, and racism."
No conflicts of interest were reported.
Blacks/African Americans continue to bear a disproportionate burden of HIV diagnoses compared with any other racial or ethnic groups, according to data published Feb. 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report.
Between 2005 and 2008, blacks/African Americans accounted for 50.3% of all HIV diagnoses in 37 states reporting to the CDC through HIV surveillance systems, despite representing just 13.6% of the population in those states, the authors wrote. Additionally, in 2008 alone, the rates of HIV diagnosis among African American males and females, respectively, were 8 and 19 times the rates reported for white males and females and 2 and 4 times the rates reported for Hispanic males and females, they stated.
"In nearly every demographic and transmission category, the largest percentages of HIV diagnoses were among blacks/African Americans," the authors wrote.
For example, during the 4-year reporting period, 56.1% of HIV diagnoses were made in individuals aged 25-44 years, and of this age group, blacks/African Americans accounted for 46.4% of them. Similarly, among adolescent and adult males, blacks/African Americans accounted for the largest percentage of HIV diagnoses overall, at 44.8%, compared with 19% and 33.6% among Hispanic/Latino and white males, respectively. They also accounted for the largest percentage of HIV diagnoses in the South, at 50.1% compared with 16.5% and 31.7% among Hispanic/Latino and white males, and in the Northeast, at 42.1% compared with 28.3% and 25.5% among Hispanic/Latino and white males, the report stated.
Among females over the 4-year period, blacks/African Americans accounted for 50.3% of the HIV diagnoses overall, compared with 17.8% and 29.4% for Hispanic/Latino and white females, respectively, and they also accounted for the majority of HIV diagnoses in the South, Midwest, and Northeast, according to the report (MMWR Morb. Mortal. Wkly. Rep. 2011;60:93-8).
When assessed by transmission category, the racial disparities were most pronounced in the rates of HIV diagnoses attributed to heterosexual contact. Nearly 71% of the males in this transmission category were black/African American, while 16.3% were Hispanic/Latino, and 11% were white. Among the females, 68% of those in the heterosexual transmission category were black/African American, compared with 14.3% who were Hispanic/Latino and 15.2% who were white.
Among black/African American males, HIV transmissions were classified as male-to-male sexual contact in 61.1% of the diagnoses, heterosexual contact in 23.1%, injection drug use in 11.9%, and both male-to-male sexual contact and infection drug use in 3.6%, the analysis showed. In black/African American females, 85.2% of HIV transmissions were through heterosexual contact and 14% were through infection drug use, according to the report.
In a trend analysis for the 4 years covered by the report, rates of HIV diagnoses increased among black/African American males while trends in other race/ethnic groups and gender groups remained stable.
"Lack of knowledge of HIV status and missed opportunities to diagnose HIV in routine clinical settings are contributing factors to the HIV epidemic among blacks/African Americans," the authors wrote in their editorial comment. "Ongoing and increased HIV testing and efforts to ensure referral and access to HIV-related primary medical care are warranted," they stated, as are comprehensive approaches "that take into account patient-specific behavioral risk factors, such as having multiple sex partners and unprotected sex, in addition to underlying factors such as poverty, unequal access to health care, incarceration, lack of education, stigma, homophobia, sexism, and racism."
No conflicts of interest were reported.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Racial Disparities in HIV Diagnoses Persist
Blacks/African Americans continue to bear a disproportionate burden of HIV diagnoses compared with any other racial or ethnic groups, according to data published Feb. 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report.
Between 2005 and 2008, blacks/African Americans accounted for 50.3% of all HIV diagnoses in 37 states reporting to the CDC through HIV surveillance systems, despite representing just 13.6% of the population in those states, the authors wrote. Additionally, in 2008 alone, the rates of HIV diagnosis among African American males and females, respectively, were 8 and 19 times the rates reported for white males and females and 2 and 4 times the rates reported for Hispanic males and females, they stated.
"In nearly every demographic and transmission category, the largest percentages of HIV diagnoses were among blacks/African Americans," the authors wrote.
For example, during the 4-year reporting period, 56.1% of HIV diagnoses were made in individuals aged 25-44 years, and of this age group, blacks/African Americans accounted for 46.4% of them. Similarly, among adolescent and adult males, blacks/African Americans accounted for the largest percentage of HIV diagnoses overall, at 44.8%, compared with 19% and 33.6% among Hispanic/Latino and white males, respectively. They also accounted for the largest percentage of HIV diagnoses in the South, at 50.1% compared with 16.5% and 31.7% among Hispanic/Latino and white males, and in the Northeast, at 42.1% compared with 28.3% and 25.5% among Hispanic/Latino and white males, the report stated.
Among females over the 4-year period, blacks/African Americans accounted for 50.3% of the HIV diagnoses overall, compared with 17.8% and 29.4% for Hispanic/Latino and white females, respectively, and they also accounted for the majority of HIV diagnoses in the South, Midwest, and Northeast, according to the report (MMWR Morb. Mortal. Wkly. Rep. 2011;60:93-8).
When assessed by transmission category, the racial disparities were most pronounced in the rates of HIV diagnoses attributed to heterosexual contact. Nearly 71% of the males in this transmission category were black/African American, while 16.3% were Hispanic/Latino, and 11% were white. Among the females, 68% of those in the heterosexual transmission category were black/African American, compared with 14.3% who were Hispanic/Latino and 15.2% who were white.
Among black/African American males, HIV transmissions were classified as male-to-male sexual contact in 61.1% of the diagnoses, heterosexual contact in 23.1%, injection drug use in 11.9%, and both male-to-male sexual contact and infection drug use in 3.6%, the analysis showed. In black/African American females, 85.2% of HIV transmissions were through heterosexual contact and 14% were through infection drug use, according to the report.
In a trend analysis for the 4 years covered by the report, rates of HIV diagnoses increased among black/African American males while trends in other race/ethnic groups and gender groups remained stable.
"Lack of knowledge of HIV status and missed opportunities to diagnose HIV in routine clinical settings are contributing factors to the HIV epidemic among blacks/African Americans," the authors wrote in their editorial comment. "Ongoing and increased HIV testing and efforts to ensure referral and access to HIV-related primary medical care are warranted," they stated, as are comprehensive approaches "that take into account patient-specific behavioral risk factors, such as having multiple sex partners and unprotected sex, in addition to underlying factors such as poverty, unequal access to health care, incarceration, lack of education, stigma, homophobia, sexism, and racism."
No conflicts of interest were reported.
Blacks/African Americans continue to bear a disproportionate burden of HIV diagnoses compared with any other racial or ethnic groups, according to data published Feb. 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report.
Between 2005 and 2008, blacks/African Americans accounted for 50.3% of all HIV diagnoses in 37 states reporting to the CDC through HIV surveillance systems, despite representing just 13.6% of the population in those states, the authors wrote. Additionally, in 2008 alone, the rates of HIV diagnosis among African American males and females, respectively, were 8 and 19 times the rates reported for white males and females and 2 and 4 times the rates reported for Hispanic males and females, they stated.
"In nearly every demographic and transmission category, the largest percentages of HIV diagnoses were among blacks/African Americans," the authors wrote.
For example, during the 4-year reporting period, 56.1% of HIV diagnoses were made in individuals aged 25-44 years, and of this age group, blacks/African Americans accounted for 46.4% of them. Similarly, among adolescent and adult males, blacks/African Americans accounted for the largest percentage of HIV diagnoses overall, at 44.8%, compared with 19% and 33.6% among Hispanic/Latino and white males, respectively. They also accounted for the largest percentage of HIV diagnoses in the South, at 50.1% compared with 16.5% and 31.7% among Hispanic/Latino and white males, and in the Northeast, at 42.1% compared with 28.3% and 25.5% among Hispanic/Latino and white males, the report stated.
Among females over the 4-year period, blacks/African Americans accounted for 50.3% of the HIV diagnoses overall, compared with 17.8% and 29.4% for Hispanic/Latino and white females, respectively, and they also accounted for the majority of HIV diagnoses in the South, Midwest, and Northeast, according to the report (MMWR Morb. Mortal. Wkly. Rep. 2011;60:93-8).
When assessed by transmission category, the racial disparities were most pronounced in the rates of HIV diagnoses attributed to heterosexual contact. Nearly 71% of the males in this transmission category were black/African American, while 16.3% were Hispanic/Latino, and 11% were white. Among the females, 68% of those in the heterosexual transmission category were black/African American, compared with 14.3% who were Hispanic/Latino and 15.2% who were white.
Among black/African American males, HIV transmissions were classified as male-to-male sexual contact in 61.1% of the diagnoses, heterosexual contact in 23.1%, injection drug use in 11.9%, and both male-to-male sexual contact and infection drug use in 3.6%, the analysis showed. In black/African American females, 85.2% of HIV transmissions were through heterosexual contact and 14% were through infection drug use, according to the report.
In a trend analysis for the 4 years covered by the report, rates of HIV diagnoses increased among black/African American males while trends in other race/ethnic groups and gender groups remained stable.
"Lack of knowledge of HIV status and missed opportunities to diagnose HIV in routine clinical settings are contributing factors to the HIV epidemic among blacks/African Americans," the authors wrote in their editorial comment. "Ongoing and increased HIV testing and efforts to ensure referral and access to HIV-related primary medical care are warranted," they stated, as are comprehensive approaches "that take into account patient-specific behavioral risk factors, such as having multiple sex partners and unprotected sex, in addition to underlying factors such as poverty, unequal access to health care, incarceration, lack of education, stigma, homophobia, sexism, and racism."
No conflicts of interest were reported.
Blacks/African Americans continue to bear a disproportionate burden of HIV diagnoses compared with any other racial or ethnic groups, according to data published Feb. 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report.
Between 2005 and 2008, blacks/African Americans accounted for 50.3% of all HIV diagnoses in 37 states reporting to the CDC through HIV surveillance systems, despite representing just 13.6% of the population in those states, the authors wrote. Additionally, in 2008 alone, the rates of HIV diagnosis among African American males and females, respectively, were 8 and 19 times the rates reported for white males and females and 2 and 4 times the rates reported for Hispanic males and females, they stated.
"In nearly every demographic and transmission category, the largest percentages of HIV diagnoses were among blacks/African Americans," the authors wrote.
For example, during the 4-year reporting period, 56.1% of HIV diagnoses were made in individuals aged 25-44 years, and of this age group, blacks/African Americans accounted for 46.4% of them. Similarly, among adolescent and adult males, blacks/African Americans accounted for the largest percentage of HIV diagnoses overall, at 44.8%, compared with 19% and 33.6% among Hispanic/Latino and white males, respectively. They also accounted for the largest percentage of HIV diagnoses in the South, at 50.1% compared with 16.5% and 31.7% among Hispanic/Latino and white males, and in the Northeast, at 42.1% compared with 28.3% and 25.5% among Hispanic/Latino and white males, the report stated.
Among females over the 4-year period, blacks/African Americans accounted for 50.3% of the HIV diagnoses overall, compared with 17.8% and 29.4% for Hispanic/Latino and white females, respectively, and they also accounted for the majority of HIV diagnoses in the South, Midwest, and Northeast, according to the report (MMWR Morb. Mortal. Wkly. Rep. 2011;60:93-8).
When assessed by transmission category, the racial disparities were most pronounced in the rates of HIV diagnoses attributed to heterosexual contact. Nearly 71% of the males in this transmission category were black/African American, while 16.3% were Hispanic/Latino, and 11% were white. Among the females, 68% of those in the heterosexual transmission category were black/African American, compared with 14.3% who were Hispanic/Latino and 15.2% who were white.
Among black/African American males, HIV transmissions were classified as male-to-male sexual contact in 61.1% of the diagnoses, heterosexual contact in 23.1%, injection drug use in 11.9%, and both male-to-male sexual contact and infection drug use in 3.6%, the analysis showed. In black/African American females, 85.2% of HIV transmissions were through heterosexual contact and 14% were through infection drug use, according to the report.
In a trend analysis for the 4 years covered by the report, rates of HIV diagnoses increased among black/African American males while trends in other race/ethnic groups and gender groups remained stable.
"Lack of knowledge of HIV status and missed opportunities to diagnose HIV in routine clinical settings are contributing factors to the HIV epidemic among blacks/African Americans," the authors wrote in their editorial comment. "Ongoing and increased HIV testing and efforts to ensure referral and access to HIV-related primary medical care are warranted," they stated, as are comprehensive approaches "that take into account patient-specific behavioral risk factors, such as having multiple sex partners and unprotected sex, in addition to underlying factors such as poverty, unequal access to health care, incarceration, lack of education, stigma, homophobia, sexism, and racism."
No conflicts of interest were reported.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Major Finding: HIV diagnoses in blacks/African Americans continue to be disproportionately high relative to other racial and ethnic groups.
Data Source: Data from the National HIV Surveillance System representing HIV diagnoses rates for 2005-2008 from 37 states with mature surveillance systems.
Disclosures: No conflicts of interest were reported.
Maternal Stroke History Linked to Myocardial Infarction Risk in Women
Women whose mothers had a stroke are at increased risk for both stroke and myocardial infarction, new research has shown.
In a study of sex-of-parent and sex-of-proband interactions for family history of stroke in acute coronary syndrome (ACS) patients, Amitava Banerjee of the University of Oxford, England, and colleagues evaluated the family histories of 1,957 patients who had suffered a stroke, transient ischemic attack, myocardial infarction, or unstable angina. They determined that maternal history of stroke was more than twice as common than paternal stroke history in women with ACS, with an odds ratio of 2.53. Additionally, women with ACS were more likely to have female vs. male first-degree relatives with stroke history (odds ratio 2.09), while the opposite was true for males with ACS (odds ratio 0.69), the authors reported Feb. 1 in Circulation: Cardiovascular Genetics.
Previous studies have shown that women face a higher risk of myocardial infarction before age 65 if their mothers had a myocardial infarction at an early age, and that stroke in female first-degree relatives is a powerful risk factor for ischemic stroke in women; however, this is the first study to point toward sex-specific heritability of vascular disease across different arterial territories, the authors wrote. The current study is also the first to consider "the full spectrum of ACS without age restrictions on the proband or parent at time of vascular event," they stated.
The findings are especially noteworthy because "family history of stroke is omitted from existing MI risk prediction tools, which perform less well in women than in men," the authors stressed.
Among the possible explanations for the excess of maternal stroke vs. paternal stroke in ACS probands include the tendency of women to be more accurate in their reports of family history than males, and the fact that women with myocardial infarction likely have a greater number of genetic risk factors for ACS than do men. Thus, they would potentially transmit more susceptibility genes to their offspring, the authors hypothesized, noting that, "if there were shared risk factors between MI and stroke, a Carter effect might be expected for [family history] of stroke in ACS probands."
It’s also possible that sex-specific associations might be a function of sex-specific genes or sex-specific behaviors "which predispose to vascular disease across arterial territories," the authors wrote. "Future analyses should consider sex-of-parent/sex-of-offspring associations in prospective studies to better understand how sex-specific differences in [family history] lead to sex-specific differences in pathogenesis [such as localization of disease on coronary angiography and prothrombotic markers] and outcomes of CHD."
Because genome-wide scans are yet to produce data useful for clinical risk prediction of vascular disease, "more detailed use of [family history] data may provide a low-cost, low-technology alternative in the interim," they concluded.
The Oxford Vascular Study is funded by the U.K. Medical Research Council, the Dunhill Medical Trust, the Stroke Association, the BUPA Foundation, the National Institute for Health Research (NIHR), the Thames Valley Primary Care Research Partnership and the NIHR Biomedical Research Centre, Oxford. Author A.P. Banning is supported by the NIHR Biomedical Research Centre, Oxford. The authors reported having no financial conflicts of interest.
Women whose mothers had a stroke are at increased risk for both stroke and myocardial infarction, new research has shown.
In a study of sex-of-parent and sex-of-proband interactions for family history of stroke in acute coronary syndrome (ACS) patients, Amitava Banerjee of the University of Oxford, England, and colleagues evaluated the family histories of 1,957 patients who had suffered a stroke, transient ischemic attack, myocardial infarction, or unstable angina. They determined that maternal history of stroke was more than twice as common than paternal stroke history in women with ACS, with an odds ratio of 2.53. Additionally, women with ACS were more likely to have female vs. male first-degree relatives with stroke history (odds ratio 2.09), while the opposite was true for males with ACS (odds ratio 0.69), the authors reported Feb. 1 in Circulation: Cardiovascular Genetics.
Previous studies have shown that women face a higher risk of myocardial infarction before age 65 if their mothers had a myocardial infarction at an early age, and that stroke in female first-degree relatives is a powerful risk factor for ischemic stroke in women; however, this is the first study to point toward sex-specific heritability of vascular disease across different arterial territories, the authors wrote. The current study is also the first to consider "the full spectrum of ACS without age restrictions on the proband or parent at time of vascular event," they stated.
The findings are especially noteworthy because "family history of stroke is omitted from existing MI risk prediction tools, which perform less well in women than in men," the authors stressed.
Among the possible explanations for the excess of maternal stroke vs. paternal stroke in ACS probands include the tendency of women to be more accurate in their reports of family history than males, and the fact that women with myocardial infarction likely have a greater number of genetic risk factors for ACS than do men. Thus, they would potentially transmit more susceptibility genes to their offspring, the authors hypothesized, noting that, "if there were shared risk factors between MI and stroke, a Carter effect might be expected for [family history] of stroke in ACS probands."
It’s also possible that sex-specific associations might be a function of sex-specific genes or sex-specific behaviors "which predispose to vascular disease across arterial territories," the authors wrote. "Future analyses should consider sex-of-parent/sex-of-offspring associations in prospective studies to better understand how sex-specific differences in [family history] lead to sex-specific differences in pathogenesis [such as localization of disease on coronary angiography and prothrombotic markers] and outcomes of CHD."
Because genome-wide scans are yet to produce data useful for clinical risk prediction of vascular disease, "more detailed use of [family history] data may provide a low-cost, low-technology alternative in the interim," they concluded.
The Oxford Vascular Study is funded by the U.K. Medical Research Council, the Dunhill Medical Trust, the Stroke Association, the BUPA Foundation, the National Institute for Health Research (NIHR), the Thames Valley Primary Care Research Partnership and the NIHR Biomedical Research Centre, Oxford. Author A.P. Banning is supported by the NIHR Biomedical Research Centre, Oxford. The authors reported having no financial conflicts of interest.
Women whose mothers had a stroke are at increased risk for both stroke and myocardial infarction, new research has shown.
In a study of sex-of-parent and sex-of-proband interactions for family history of stroke in acute coronary syndrome (ACS) patients, Amitava Banerjee of the University of Oxford, England, and colleagues evaluated the family histories of 1,957 patients who had suffered a stroke, transient ischemic attack, myocardial infarction, or unstable angina. They determined that maternal history of stroke was more than twice as common than paternal stroke history in women with ACS, with an odds ratio of 2.53. Additionally, women with ACS were more likely to have female vs. male first-degree relatives with stroke history (odds ratio 2.09), while the opposite was true for males with ACS (odds ratio 0.69), the authors reported Feb. 1 in Circulation: Cardiovascular Genetics.
Previous studies have shown that women face a higher risk of myocardial infarction before age 65 if their mothers had a myocardial infarction at an early age, and that stroke in female first-degree relatives is a powerful risk factor for ischemic stroke in women; however, this is the first study to point toward sex-specific heritability of vascular disease across different arterial territories, the authors wrote. The current study is also the first to consider "the full spectrum of ACS without age restrictions on the proband or parent at time of vascular event," they stated.
The findings are especially noteworthy because "family history of stroke is omitted from existing MI risk prediction tools, which perform less well in women than in men," the authors stressed.
Among the possible explanations for the excess of maternal stroke vs. paternal stroke in ACS probands include the tendency of women to be more accurate in their reports of family history than males, and the fact that women with myocardial infarction likely have a greater number of genetic risk factors for ACS than do men. Thus, they would potentially transmit more susceptibility genes to their offspring, the authors hypothesized, noting that, "if there were shared risk factors between MI and stroke, a Carter effect might be expected for [family history] of stroke in ACS probands."
It’s also possible that sex-specific associations might be a function of sex-specific genes or sex-specific behaviors "which predispose to vascular disease across arterial territories," the authors wrote. "Future analyses should consider sex-of-parent/sex-of-offspring associations in prospective studies to better understand how sex-specific differences in [family history] lead to sex-specific differences in pathogenesis [such as localization of disease on coronary angiography and prothrombotic markers] and outcomes of CHD."
Because genome-wide scans are yet to produce data useful for clinical risk prediction of vascular disease, "more detailed use of [family history] data may provide a low-cost, low-technology alternative in the interim," they concluded.
The Oxford Vascular Study is funded by the U.K. Medical Research Council, the Dunhill Medical Trust, the Stroke Association, the BUPA Foundation, the National Institute for Health Research (NIHR), the Thames Valley Primary Care Research Partnership and the NIHR Biomedical Research Centre, Oxford. Author A.P. Banning is supported by the NIHR Biomedical Research Centre, Oxford. The authors reported having no financial conflicts of interest.
FROM CIRCULATION: CARDIOVASCULAR GENETICS
Maternal Stroke History Linked to Myocardial Infarction Risk in Women
Women whose mothers had a stroke are at increased risk for both stroke and myocardial infarction, new research has shown.
In a study of sex-of-parent and sex-of-proband interactions for family history of stroke in acute coronary syndrome (ACS) patients, Amitava Banerjee of the University of Oxford, England, and colleagues evaluated the family histories of 1,957 patients who had suffered a stroke, transient ischemic attack, myocardial infarction, or unstable angina. They determined that maternal history of stroke was more than twice as common than paternal stroke history in women with ACS, with an odds ratio of 2.53. Additionally, women with ACS were more likely to have female vs. male first-degree relatives with stroke history (odds ratio 2.09), while the opposite was true for males with ACS (odds ratio 0.69), the authors reported Feb. 1 in Circulation: Cardiovascular Genetics.
Previous studies have shown that women face a higher risk of myocardial infarction before age 65 if their mothers had a myocardial infarction at an early age, and that stroke in female first-degree relatives is a powerful risk factor for ischemic stroke in women; however, this is the first study to point toward sex-specific heritability of vascular disease across different arterial territories, the authors wrote. The current study is also the first to consider "the full spectrum of ACS without age restrictions on the proband or parent at time of vascular event," they stated.
The findings are especially noteworthy because "family history of stroke is omitted from existing MI risk prediction tools, which perform less well in women than in men," the authors stressed.
Among the possible explanations for the excess of maternal stroke vs. paternal stroke in ACS probands include the tendency of women to be more accurate in their reports of family history than males, and the fact that women with myocardial infarction likely have a greater number of genetic risk factors for ACS than do men. Thus, they would potentially transmit more susceptibility genes to their offspring, the authors hypothesized, noting that, "if there were shared risk factors between MI and stroke, a Carter effect might be expected for [family history] of stroke in ACS probands."
It’s also possible that sex-specific associations might be a function of sex-specific genes or sex-specific behaviors "which predispose to vascular disease across arterial territories," the authors wrote. "Future analyses should consider sex-of-parent/sex-of-offspring associations in prospective studies to better understand how sex-specific differences in [family history] lead to sex-specific differences in pathogenesis [such as localization of disease on coronary angiography and prothrombotic markers] and outcomes of CHD."
Because genome-wide scans are yet to produce data useful for clinical risk prediction of vascular disease, "more detailed use of [family history] data may provide a low-cost, low-technology alternative in the interim," they concluded.
The Oxford Vascular Study is funded by the U.K. Medical Research Council, the Dunhill Medical Trust, the Stroke Association, the BUPA Foundation, the National Institute for Health Research (NIHR), the Thames Valley Primary Care Research Partnership and the NIHR Biomedical Research Centre, Oxford. Author A.P. Banning is supported by the NIHR Biomedical Research Centre, Oxford. The authors reported having no financial conflicts of interest.
Women whose mothers had a stroke are at increased risk for both stroke and myocardial infarction, new research has shown.
In a study of sex-of-parent and sex-of-proband interactions for family history of stroke in acute coronary syndrome (ACS) patients, Amitava Banerjee of the University of Oxford, England, and colleagues evaluated the family histories of 1,957 patients who had suffered a stroke, transient ischemic attack, myocardial infarction, or unstable angina. They determined that maternal history of stroke was more than twice as common than paternal stroke history in women with ACS, with an odds ratio of 2.53. Additionally, women with ACS were more likely to have female vs. male first-degree relatives with stroke history (odds ratio 2.09), while the opposite was true for males with ACS (odds ratio 0.69), the authors reported Feb. 1 in Circulation: Cardiovascular Genetics.
Previous studies have shown that women face a higher risk of myocardial infarction before age 65 if their mothers had a myocardial infarction at an early age, and that stroke in female first-degree relatives is a powerful risk factor for ischemic stroke in women; however, this is the first study to point toward sex-specific heritability of vascular disease across different arterial territories, the authors wrote. The current study is also the first to consider "the full spectrum of ACS without age restrictions on the proband or parent at time of vascular event," they stated.
The findings are especially noteworthy because "family history of stroke is omitted from existing MI risk prediction tools, which perform less well in women than in men," the authors stressed.
Among the possible explanations for the excess of maternal stroke vs. paternal stroke in ACS probands include the tendency of women to be more accurate in their reports of family history than males, and the fact that women with myocardial infarction likely have a greater number of genetic risk factors for ACS than do men. Thus, they would potentially transmit more susceptibility genes to their offspring, the authors hypothesized, noting that, "if there were shared risk factors between MI and stroke, a Carter effect might be expected for [family history] of stroke in ACS probands."
It’s also possible that sex-specific associations might be a function of sex-specific genes or sex-specific behaviors "which predispose to vascular disease across arterial territories," the authors wrote. "Future analyses should consider sex-of-parent/sex-of-offspring associations in prospective studies to better understand how sex-specific differences in [family history] lead to sex-specific differences in pathogenesis [such as localization of disease on coronary angiography and prothrombotic markers] and outcomes of CHD."
Because genome-wide scans are yet to produce data useful for clinical risk prediction of vascular disease, "more detailed use of [family history] data may provide a low-cost, low-technology alternative in the interim," they concluded.
The Oxford Vascular Study is funded by the U.K. Medical Research Council, the Dunhill Medical Trust, the Stroke Association, the BUPA Foundation, the National Institute for Health Research (NIHR), the Thames Valley Primary Care Research Partnership and the NIHR Biomedical Research Centre, Oxford. Author A.P. Banning is supported by the NIHR Biomedical Research Centre, Oxford. The authors reported having no financial conflicts of interest.
Women whose mothers had a stroke are at increased risk for both stroke and myocardial infarction, new research has shown.
In a study of sex-of-parent and sex-of-proband interactions for family history of stroke in acute coronary syndrome (ACS) patients, Amitava Banerjee of the University of Oxford, England, and colleagues evaluated the family histories of 1,957 patients who had suffered a stroke, transient ischemic attack, myocardial infarction, or unstable angina. They determined that maternal history of stroke was more than twice as common than paternal stroke history in women with ACS, with an odds ratio of 2.53. Additionally, women with ACS were more likely to have female vs. male first-degree relatives with stroke history (odds ratio 2.09), while the opposite was true for males with ACS (odds ratio 0.69), the authors reported Feb. 1 in Circulation: Cardiovascular Genetics.
Previous studies have shown that women face a higher risk of myocardial infarction before age 65 if their mothers had a myocardial infarction at an early age, and that stroke in female first-degree relatives is a powerful risk factor for ischemic stroke in women; however, this is the first study to point toward sex-specific heritability of vascular disease across different arterial territories, the authors wrote. The current study is also the first to consider "the full spectrum of ACS without age restrictions on the proband or parent at time of vascular event," they stated.
The findings are especially noteworthy because "family history of stroke is omitted from existing MI risk prediction tools, which perform less well in women than in men," the authors stressed.
Among the possible explanations for the excess of maternal stroke vs. paternal stroke in ACS probands include the tendency of women to be more accurate in their reports of family history than males, and the fact that women with myocardial infarction likely have a greater number of genetic risk factors for ACS than do men. Thus, they would potentially transmit more susceptibility genes to their offspring, the authors hypothesized, noting that, "if there were shared risk factors between MI and stroke, a Carter effect might be expected for [family history] of stroke in ACS probands."
It’s also possible that sex-specific associations might be a function of sex-specific genes or sex-specific behaviors "which predispose to vascular disease across arterial territories," the authors wrote. "Future analyses should consider sex-of-parent/sex-of-offspring associations in prospective studies to better understand how sex-specific differences in [family history] lead to sex-specific differences in pathogenesis [such as localization of disease on coronary angiography and prothrombotic markers] and outcomes of CHD."
Because genome-wide scans are yet to produce data useful for clinical risk prediction of vascular disease, "more detailed use of [family history] data may provide a low-cost, low-technology alternative in the interim," they concluded.
The Oxford Vascular Study is funded by the U.K. Medical Research Council, the Dunhill Medical Trust, the Stroke Association, the BUPA Foundation, the National Institute for Health Research (NIHR), the Thames Valley Primary Care Research Partnership and the NIHR Biomedical Research Centre, Oxford. Author A.P. Banning is supported by the NIHR Biomedical Research Centre, Oxford. The authors reported having no financial conflicts of interest.
FROM CIRCULATION: CARDIOVASCULAR GENETICS
Major Finding: Maternal stroke history is linked to myocardial infarction risk in women.
Data Source: A prospective population-based study of 2,200 patients investigating the link between a relative’s stroke and heart disease risk and patient and relative gender.
Disclosures: The authors had no financial conflicts to disclose.
Telbivudine Appears Safe in Pregnancy
BOSTON – Limited use of the antiviral drug telbivudine is safe and effective for pregnant women with active hepatitis B virus infection and reduces perinatal transmission of the virus to their infants, Dr. Calvin Pan reported at the meeting.
In the first open-label case-control trial investigating the safety and efficacy of telbivudine during the second to third trimester of pregnancy, the synthetic nucleoside analogue led to significant increases in rates of complete virologic response and normalization of alanine aminotransferase (ALT) levels in treated vs. untreated pregnant women with hepatitis B virus (HBV) infection, reported Dr. Pan of Mount Sinai School of Medicine in New York.
Additionally, there were no congenital defects identified up to 28 weeks post partum in the infants born to treated mothers.
Dr. Pan and his colleagues at the Second Affiliated Hospital of the Southeast University in Nanjing, China, where the study was conducted, enrolled 88 pregnant women who screened positive for hepatitis B e antigen (HBeAg) between gestational weeks 12 and 23 and who had serum HBV DNA levels greater than 6 log10 copies/mL and elevated ALT levels up to 10 times the upper limit of normal (40 IU/mL). Of the 88 patients, 53 opted to take telbivudine, and the remaining 35 served as the study's control arm, he said.
Women in the treatment arm received 600 mg/day of telbivudine beginning sometime between 20 and 32 weeks' gestation and continuing until a minimum of 4 weeks post partum, and infants born to women in both groups received hepatitis B immunoglobulin within 24 hours of birth and the HBV vaccine at birth, 1 month, and 6 months.
The mean duration of telbivudine treatment was 15.5 weeks, and all of the women who took the drug remained in the study through at least postpartum week 4, compared with 92% of the controls, said Dr. Pan. Physical and laboratory examinations were conducted at baseline, at the time of delivery, and at 4 weeks post partum, he said, noting that a second study looked at infant outcomes through 28 weeks.
At the time of delivery and 4 weeks post partum, a complete virologic response was observed in 53% and 62% of the treated patients, respectively, while no patients in the control arm achieved a complete virologic response at either time point, Dr. Pan reported. “Both the control arm and the telbivudine arm had HBV DNA of approximately 8 logs. At the time of delivery, this was reduced substantially [to 2.35 log10 copies/mL] in the mothers in the treatment arm.”
With respect to ALT levels, 77% of the treatment group achieved normalization compared with 29% of the control group, Dr. Pan said. Also, the levels of HBeAg dropped by 98% in the treatment group, which was a significantly greater decrease than the 60% drop observed in the control group; the latter was likely the result of natural viral clearance, he noted.
An evaluation of newborn outcomes showed no congenital deformities nor any differences in gestational age, infant height and weight, or Apgar scores between the two groups, said Dr. Pan. Significantly fewer babies born to telbivudine-treated mothers vs. untreated mothers had hepatitis B surface antigens or detectable levels of HBV RNA at birth (4% vs. 23%).
Telbivudine appeared to be well tolerated as there were no adverse event–related treatment discontinuations, said Dr. Pan. Also, none of the patients experienced virologic breakthrough.
Despite concerns regarding antiviral treatment during pregnancy because of the potential risks to the fetus, the findings from this study suggest that limited treatment with telbivudine can improve maternal and child outcomes, Dr. Pan concluded.
The study was funded by the Chinese Department of Health with no commercial support. Dr. Pan said he had no relevant financial disclosures.
BOSTON – Limited use of the antiviral drug telbivudine is safe and effective for pregnant women with active hepatitis B virus infection and reduces perinatal transmission of the virus to their infants, Dr. Calvin Pan reported at the meeting.
In the first open-label case-control trial investigating the safety and efficacy of telbivudine during the second to third trimester of pregnancy, the synthetic nucleoside analogue led to significant increases in rates of complete virologic response and normalization of alanine aminotransferase (ALT) levels in treated vs. untreated pregnant women with hepatitis B virus (HBV) infection, reported Dr. Pan of Mount Sinai School of Medicine in New York.
Additionally, there were no congenital defects identified up to 28 weeks post partum in the infants born to treated mothers.
Dr. Pan and his colleagues at the Second Affiliated Hospital of the Southeast University in Nanjing, China, where the study was conducted, enrolled 88 pregnant women who screened positive for hepatitis B e antigen (HBeAg) between gestational weeks 12 and 23 and who had serum HBV DNA levels greater than 6 log10 copies/mL and elevated ALT levels up to 10 times the upper limit of normal (40 IU/mL). Of the 88 patients, 53 opted to take telbivudine, and the remaining 35 served as the study's control arm, he said.
Women in the treatment arm received 600 mg/day of telbivudine beginning sometime between 20 and 32 weeks' gestation and continuing until a minimum of 4 weeks post partum, and infants born to women in both groups received hepatitis B immunoglobulin within 24 hours of birth and the HBV vaccine at birth, 1 month, and 6 months.
The mean duration of telbivudine treatment was 15.5 weeks, and all of the women who took the drug remained in the study through at least postpartum week 4, compared with 92% of the controls, said Dr. Pan. Physical and laboratory examinations were conducted at baseline, at the time of delivery, and at 4 weeks post partum, he said, noting that a second study looked at infant outcomes through 28 weeks.
At the time of delivery and 4 weeks post partum, a complete virologic response was observed in 53% and 62% of the treated patients, respectively, while no patients in the control arm achieved a complete virologic response at either time point, Dr. Pan reported. “Both the control arm and the telbivudine arm had HBV DNA of approximately 8 logs. At the time of delivery, this was reduced substantially [to 2.35 log10 copies/mL] in the mothers in the treatment arm.”
With respect to ALT levels, 77% of the treatment group achieved normalization compared with 29% of the control group, Dr. Pan said. Also, the levels of HBeAg dropped by 98% in the treatment group, which was a significantly greater decrease than the 60% drop observed in the control group; the latter was likely the result of natural viral clearance, he noted.
An evaluation of newborn outcomes showed no congenital deformities nor any differences in gestational age, infant height and weight, or Apgar scores between the two groups, said Dr. Pan. Significantly fewer babies born to telbivudine-treated mothers vs. untreated mothers had hepatitis B surface antigens or detectable levels of HBV RNA at birth (4% vs. 23%).
Telbivudine appeared to be well tolerated as there were no adverse event–related treatment discontinuations, said Dr. Pan. Also, none of the patients experienced virologic breakthrough.
Despite concerns regarding antiviral treatment during pregnancy because of the potential risks to the fetus, the findings from this study suggest that limited treatment with telbivudine can improve maternal and child outcomes, Dr. Pan concluded.
The study was funded by the Chinese Department of Health with no commercial support. Dr. Pan said he had no relevant financial disclosures.
BOSTON – Limited use of the antiviral drug telbivudine is safe and effective for pregnant women with active hepatitis B virus infection and reduces perinatal transmission of the virus to their infants, Dr. Calvin Pan reported at the meeting.
In the first open-label case-control trial investigating the safety and efficacy of telbivudine during the second to third trimester of pregnancy, the synthetic nucleoside analogue led to significant increases in rates of complete virologic response and normalization of alanine aminotransferase (ALT) levels in treated vs. untreated pregnant women with hepatitis B virus (HBV) infection, reported Dr. Pan of Mount Sinai School of Medicine in New York.
Additionally, there were no congenital defects identified up to 28 weeks post partum in the infants born to treated mothers.
Dr. Pan and his colleagues at the Second Affiliated Hospital of the Southeast University in Nanjing, China, where the study was conducted, enrolled 88 pregnant women who screened positive for hepatitis B e antigen (HBeAg) between gestational weeks 12 and 23 and who had serum HBV DNA levels greater than 6 log10 copies/mL and elevated ALT levels up to 10 times the upper limit of normal (40 IU/mL). Of the 88 patients, 53 opted to take telbivudine, and the remaining 35 served as the study's control arm, he said.
Women in the treatment arm received 600 mg/day of telbivudine beginning sometime between 20 and 32 weeks' gestation and continuing until a minimum of 4 weeks post partum, and infants born to women in both groups received hepatitis B immunoglobulin within 24 hours of birth and the HBV vaccine at birth, 1 month, and 6 months.
The mean duration of telbivudine treatment was 15.5 weeks, and all of the women who took the drug remained in the study through at least postpartum week 4, compared with 92% of the controls, said Dr. Pan. Physical and laboratory examinations were conducted at baseline, at the time of delivery, and at 4 weeks post partum, he said, noting that a second study looked at infant outcomes through 28 weeks.
At the time of delivery and 4 weeks post partum, a complete virologic response was observed in 53% and 62% of the treated patients, respectively, while no patients in the control arm achieved a complete virologic response at either time point, Dr. Pan reported. “Both the control arm and the telbivudine arm had HBV DNA of approximately 8 logs. At the time of delivery, this was reduced substantially [to 2.35 log10 copies/mL] in the mothers in the treatment arm.”
With respect to ALT levels, 77% of the treatment group achieved normalization compared with 29% of the control group, Dr. Pan said. Also, the levels of HBeAg dropped by 98% in the treatment group, which was a significantly greater decrease than the 60% drop observed in the control group; the latter was likely the result of natural viral clearance, he noted.
An evaluation of newborn outcomes showed no congenital deformities nor any differences in gestational age, infant height and weight, or Apgar scores between the two groups, said Dr. Pan. Significantly fewer babies born to telbivudine-treated mothers vs. untreated mothers had hepatitis B surface antigens or detectable levels of HBV RNA at birth (4% vs. 23%).
Telbivudine appeared to be well tolerated as there were no adverse event–related treatment discontinuations, said Dr. Pan. Also, none of the patients experienced virologic breakthrough.
Despite concerns regarding antiviral treatment during pregnancy because of the potential risks to the fetus, the findings from this study suggest that limited treatment with telbivudine can improve maternal and child outcomes, Dr. Pan concluded.
The study was funded by the Chinese Department of Health with no commercial support. Dr. Pan said he had no relevant financial disclosures.
From the Annual Meeting of the American Association for the Study of Liver Diseases
Adding Immunoglobulin to HBV Vaccine No Help
Major Finding: The addition of hepatitis B immunoglobulin to hepatitis B prophylaxis with the recombinant HBV vaccine does not confer additional protection to newborns of chronically infected mothers.
Data Source: A randomized controlled trial of 222 infants born to mothers who tested positive for hepatitis B surface antigen.
Disclosures: Dr. Sarin and Dr. Pande reported having no relevant financial disclosures.
BOSTON – The recombinant hepatitis B vaccine confers as much protection when given alone as it does when given together with hepatitis B immunoglobulin to newborns of chronically infected mothers, but neither regimen is optimally effective, a study has shown.
The randomized controlled trial assessed the hepatitis B virus (HBV) status of 222 infants born to mothers who tested positive for hepatitis B surface antigen (HBsAg). The rate of protection observed in infants who received only the vaccine was statistically similar to that of infants who received the vaccine plus hepatitis B immune globulin (HBIG).
A total of 39% of the vaccine-only group and 41% of the combination group remained infection free at a minimum of 18 weeks after birth, Dr. Shiv K. Sarin reported at the meeting noting that nearly half of the babies in both groups developed occult HBV infections.
The current standard of care for preventing HBV infection in babies born to mothers who are HBsAg positive is the recombinant hepatitis B virus vaccine plus HBIG; however, previous studies have suggested the possibility that the vaccine alone may be as effective as the combination therapy, said Dr. Sarin of the Institute of Liver and Biliary Sciences in New Delhi.
To test this hypothesis, Dr. Sarin, along with lead investigator Dr. Chandana Pande, a research associate at G.B. Pant Hospital in New Delhi, and colleagues randomized the newborns of 222 women who screened positive for HBsAg during their prenatal care to receive the 0.5-mL recombinant HBV vaccine at birth, 6 weeks, 10 weeks, and 14 weeks, either alone (116 infants) or with 0.5 mL intramuscular HBIG (106 infants). Mothers on antiviral therapy and those with coinfections were excluded from the investigation, he said.
All of the babies were assessed at a minimum of 18 weeks for HBsAg, HBV-DNA, and antibodies to HBsAg (anti-HBs). The study's primary end point was freedom from overt or occult HBV infection with adequate immune response, defined as anti-HBs titers of at least 10 IU/mL, Dr. Sarin said in a poster presentation.
Babies with overt HBV infection were those whose blood specimens tested positive for HBsAg by enzyme-linked immunosorbent assay, whereas babies with occult infection were negative for HBsAg but positive for HBV-DNA by polymerase chain reaction testing, he said. Babies with no infection but whose anti-HBs titers were less than 10 IU/mL were categorized as having a poor immune response.
At 18 weeks after birth, there were no significant differences between the combination therapy group and monotherapy group with respect to the number of babies meeting the study's primary end point, Dr. Sarin reported. Specifically, 43 babies in the combination group and 45 in the vaccine-only group remained free of overt or occult HBV infection with adequate immune response.
Of the babies not meeting the primary end point, 9 had overt HBV infection, including 2 in the combination group and 7 in the vaccine-only group, and 106 developed occult HBV infection, including 52 in the combination group and 54 in the vaccine-only group, Dr. Sarin said. Neither of these differences attained statistical significance, nor did the between-group difference in the number of infants demonstrating a poor immune response, he said.
Major Finding: The addition of hepatitis B immunoglobulin to hepatitis B prophylaxis with the recombinant HBV vaccine does not confer additional protection to newborns of chronically infected mothers.
Data Source: A randomized controlled trial of 222 infants born to mothers who tested positive for hepatitis B surface antigen.
Disclosures: Dr. Sarin and Dr. Pande reported having no relevant financial disclosures.
BOSTON – The recombinant hepatitis B vaccine confers as much protection when given alone as it does when given together with hepatitis B immunoglobulin to newborns of chronically infected mothers, but neither regimen is optimally effective, a study has shown.
The randomized controlled trial assessed the hepatitis B virus (HBV) status of 222 infants born to mothers who tested positive for hepatitis B surface antigen (HBsAg). The rate of protection observed in infants who received only the vaccine was statistically similar to that of infants who received the vaccine plus hepatitis B immune globulin (HBIG).
A total of 39% of the vaccine-only group and 41% of the combination group remained infection free at a minimum of 18 weeks after birth, Dr. Shiv K. Sarin reported at the meeting noting that nearly half of the babies in both groups developed occult HBV infections.
The current standard of care for preventing HBV infection in babies born to mothers who are HBsAg positive is the recombinant hepatitis B virus vaccine plus HBIG; however, previous studies have suggested the possibility that the vaccine alone may be as effective as the combination therapy, said Dr. Sarin of the Institute of Liver and Biliary Sciences in New Delhi.
To test this hypothesis, Dr. Sarin, along with lead investigator Dr. Chandana Pande, a research associate at G.B. Pant Hospital in New Delhi, and colleagues randomized the newborns of 222 women who screened positive for HBsAg during their prenatal care to receive the 0.5-mL recombinant HBV vaccine at birth, 6 weeks, 10 weeks, and 14 weeks, either alone (116 infants) or with 0.5 mL intramuscular HBIG (106 infants). Mothers on antiviral therapy and those with coinfections were excluded from the investigation, he said.
All of the babies were assessed at a minimum of 18 weeks for HBsAg, HBV-DNA, and antibodies to HBsAg (anti-HBs). The study's primary end point was freedom from overt or occult HBV infection with adequate immune response, defined as anti-HBs titers of at least 10 IU/mL, Dr. Sarin said in a poster presentation.
Babies with overt HBV infection were those whose blood specimens tested positive for HBsAg by enzyme-linked immunosorbent assay, whereas babies with occult infection were negative for HBsAg but positive for HBV-DNA by polymerase chain reaction testing, he said. Babies with no infection but whose anti-HBs titers were less than 10 IU/mL were categorized as having a poor immune response.
At 18 weeks after birth, there were no significant differences between the combination therapy group and monotherapy group with respect to the number of babies meeting the study's primary end point, Dr. Sarin reported. Specifically, 43 babies in the combination group and 45 in the vaccine-only group remained free of overt or occult HBV infection with adequate immune response.
Of the babies not meeting the primary end point, 9 had overt HBV infection, including 2 in the combination group and 7 in the vaccine-only group, and 106 developed occult HBV infection, including 52 in the combination group and 54 in the vaccine-only group, Dr. Sarin said. Neither of these differences attained statistical significance, nor did the between-group difference in the number of infants demonstrating a poor immune response, he said.
Major Finding: The addition of hepatitis B immunoglobulin to hepatitis B prophylaxis with the recombinant HBV vaccine does not confer additional protection to newborns of chronically infected mothers.
Data Source: A randomized controlled trial of 222 infants born to mothers who tested positive for hepatitis B surface antigen.
Disclosures: Dr. Sarin and Dr. Pande reported having no relevant financial disclosures.
BOSTON – The recombinant hepatitis B vaccine confers as much protection when given alone as it does when given together with hepatitis B immunoglobulin to newborns of chronically infected mothers, but neither regimen is optimally effective, a study has shown.
The randomized controlled trial assessed the hepatitis B virus (HBV) status of 222 infants born to mothers who tested positive for hepatitis B surface antigen (HBsAg). The rate of protection observed in infants who received only the vaccine was statistically similar to that of infants who received the vaccine plus hepatitis B immune globulin (HBIG).
A total of 39% of the vaccine-only group and 41% of the combination group remained infection free at a minimum of 18 weeks after birth, Dr. Shiv K. Sarin reported at the meeting noting that nearly half of the babies in both groups developed occult HBV infections.
The current standard of care for preventing HBV infection in babies born to mothers who are HBsAg positive is the recombinant hepatitis B virus vaccine plus HBIG; however, previous studies have suggested the possibility that the vaccine alone may be as effective as the combination therapy, said Dr. Sarin of the Institute of Liver and Biliary Sciences in New Delhi.
To test this hypothesis, Dr. Sarin, along with lead investigator Dr. Chandana Pande, a research associate at G.B. Pant Hospital in New Delhi, and colleagues randomized the newborns of 222 women who screened positive for HBsAg during their prenatal care to receive the 0.5-mL recombinant HBV vaccine at birth, 6 weeks, 10 weeks, and 14 weeks, either alone (116 infants) or with 0.5 mL intramuscular HBIG (106 infants). Mothers on antiviral therapy and those with coinfections were excluded from the investigation, he said.
All of the babies were assessed at a minimum of 18 weeks for HBsAg, HBV-DNA, and antibodies to HBsAg (anti-HBs). The study's primary end point was freedom from overt or occult HBV infection with adequate immune response, defined as anti-HBs titers of at least 10 IU/mL, Dr. Sarin said in a poster presentation.
Babies with overt HBV infection were those whose blood specimens tested positive for HBsAg by enzyme-linked immunosorbent assay, whereas babies with occult infection were negative for HBsAg but positive for HBV-DNA by polymerase chain reaction testing, he said. Babies with no infection but whose anti-HBs titers were less than 10 IU/mL were categorized as having a poor immune response.
At 18 weeks after birth, there were no significant differences between the combination therapy group and monotherapy group with respect to the number of babies meeting the study's primary end point, Dr. Sarin reported. Specifically, 43 babies in the combination group and 45 in the vaccine-only group remained free of overt or occult HBV infection with adequate immune response.
Of the babies not meeting the primary end point, 9 had overt HBV infection, including 2 in the combination group and 7 in the vaccine-only group, and 106 developed occult HBV infection, including 52 in the combination group and 54 in the vaccine-only group, Dr. Sarin said. Neither of these differences attained statistical significance, nor did the between-group difference in the number of infants demonstrating a poor immune response, he said.
From the Annual Meeting of the American Association for the Study of Liver Diseases
AAP Issues New Guidelines for Evaluation of Febrile Seizures
Identifying the cause of fever should be the top priority when evaluating infants or young children after a simple febrile seizure, and the differential diagnosis should always include meningitis, according to a new clinical practice guideline published by the American Academy of Pediatrics.
In most situations, however, “a simple febrile seizure does not usually require further evaluation, specifically electroencephalography, blood studies, or neuroimaging,” the AAP Subcommittee on Febrile Seizures wrote.
The new guideline replaces the 1996 AAP practice parameter for the neurodiagnostic evaluation of healthy infants and children 6–60 months of age who have had a simple febrile seizure and who present for evaluation within 12 hours of the event (Pediatrics 1996;97:769-72).
The new document is based on a comprehensive review of the evidence-based literature published from 1996 to February 2009, with an emphasis on research that differentiated simple febrile seizures from other seizure types. The final recommendations, presented as action statements relating to the use of lumbar puncture, electroencephalography, laboratory testing, and neuroimaging, were developed based on the quality of supporting evidence and the balance of benefit and harm if the given policy is carried out, said lead author Dr. Patricia K. Duffner, professor of neurology and pediatrics at the State University of New York at Buffalo, and her associates (Pediatrics 2011;127:389-94).
Dr. Duffner noted in an interview that the biggest change is in the recommendation regarding lumbar punctures. In the prior guideline, lumbar punctures were strongly considered for children aged 6 – 12 months and considered for those aged 12–18 months. With the advent of routine immunizations for Haemophilus influenzae and Streptococcus pneumoniae, the risk of simple febrile seizures being caused by bacterial meningitis is much reduced, she said. The caveat is the child who has not been immunized and the child who is on antibiotics which may mask the infection. In those cases, the physician will need to be more cautious in his/her evaluation of the child.
Neuroimaging was never recommended for simple febrile seizures, and “I doubt this will change practice for most pediatricians and ER physicians,” she said in an interview.
“I think the guidelines will be well accepted. They are timely and relevant given the evidence base supporting them,” Dr. Duffner concluded.
According to the document:
▸ Lumbar puncture. It is strongly recommended for children who present with febrile seizure and have meningeal signs and symptoms, including neck stiffness, Kernig signs, or Brudzinski signs, or those whose history or exam suggests possible meningitis or intracranial infection. The procedure is optional for infants between 6 and 12 months who have not received scheduled Haemophilus influenzae type b (Hib) or Streptococcus pneumoniae immunizations or when immunization status is unknown, and for children with febrile seizure who have been pretreated with antibiotics, which could potentially mask the signs and symptoms of meningitis.
Since the previous practice parameter was published, there has been widespread immunization in the United States for two of the most common causes of bacterial meningitis in this age range: Hib and S. pneumoniae. Compliance with all recommended immunizations does not completely eliminate the possibility of bacterial meningitis from the differential diagnosis, but “current data no longer support routine lumbar puncture in well-appearing, fully immunized children who present with a simple febrile seizure. Moreover, although approximately 25% of young children with meningitis have seizures as the presenting sign of the disease, some are either obtunded or comatose when evaluated by a physician for the seizure, and the remainder most often have obvious clinical signs of meningitis (focal seizures, recurrent seizures, petechial rash, or nuchal rigidity),” the guideline says.
▸ Electroencephalography (EEG). It should not be used routinely in the evaluation of simple febrile seizures in otherwise neurologically healthy children. “There is no evidence that EEG readings performed either at the time of presentation after a simple febrile seizure or within the following month are predictive of either recurrence of febrile seizures or the development of afebrile seizures/epilepsy within the next 2 years,” the authors wrote.
▸ Measurement of serum electrolytes, calcium, phosphorus, magnesium, blood glucose, or complete blood cell count. Such measurements should not be performed routinely for the sole purpose of identifying the cause of a simple febrile seizure. “When fever is present, the decision regarding the need for laboratory testing should be directed toward identifying the source of the fever rather than as part of the routine evaluation of the seizure itself,” Dr. Duffner and her associates concluded.
▸ Neuroimaging. It is not recommended for the routine evaluation of children who present with simple febrile seizures. “The literature does not support the use of skull films in evaluation of the child with a febrile seizure,” they explained, nor have data been published that support or negate the need for CT or MRI in this population.
Data do show that “CT scanning is associated with radiation exposure that may escalate future cancer risk. MRI is associated with risks from required sedation and high cost,” Dr. Duffner and her associates said. Additionally, extrapolation of data from CT studies in neurologically healthy children with generalized epilepsy “has shown that clinically important intracranial structural abnormalities in this patient population are uncommon,” they noted.
All of the authors filed conflict of interest statements with the AAP, and any conflicts have been resolved through a process approved by the Board of Directors. The AAP reported having neither solicited nor accepted any commercial involvement in the development of the revised guideline.
The guidelines on when to do a lumbar puncture “in the context of
lack of immunization and pretreatment with antibiotics will be most
useful with regard to decision making in this carefully defined patient
population,” Dr. Jeffrey Buchhalter said in an interview. The authors
“were very specific regarding age of inclusion and consideration of only
simple febrile seizures in their recommendation.”
“My general
impression is that many individuals who evaluate children with simple
febrile seizures recognize the very low utility of neuroimaging but
obtain head CT anyway due to concern regarding litigation if anything is
missed. The strong recommendation not to obtain skull films is
appropriate, but in my experience has not been used with any frequency
during the last decade,” he said.
“The guidelines make sense as so
much credence is given to observational studies – what we commonly see
in clinical practice. Furthermore, the recommendations take into account
a benefit/harm consideration that each clinician confronts. Thus,
implementation should occur with a caveat regarding perceived
medical-legal liability regarding neuroimaging and other testing.
“However,
a potential reason not to implement these guidelines is precisely
because of the lack of high-quality evidence proving or disproving each
recommendation. This is an interesting conundrum that we face in
creating guidelines that are truly evidence based yet clinically
relevant,” Dr. Buchhalter concluded.
DR. BUCHHALTER is chief of
neurology at Phoenix Children's Hospital. Dr. Buchhalter has received
personal compensation for activities with the National Institute of
Neurological Disorders and Stroke, and he has received research support
from Ovation Pharmaceuticals, Inc. and Pfizer Inc.
The guidelines on when to do a lumbar puncture “in the context of
lack of immunization and pretreatment with antibiotics will be most
useful with regard to decision making in this carefully defined patient
population,” Dr. Jeffrey Buchhalter said in an interview. The authors
“were very specific regarding age of inclusion and consideration of only
simple febrile seizures in their recommendation.”
“My general
impression is that many individuals who evaluate children with simple
febrile seizures recognize the very low utility of neuroimaging but
obtain head CT anyway due to concern regarding litigation if anything is
missed. The strong recommendation not to obtain skull films is
appropriate, but in my experience has not been used with any frequency
during the last decade,” he said.
“The guidelines make sense as so
much credence is given to observational studies – what we commonly see
in clinical practice. Furthermore, the recommendations take into account
a benefit/harm consideration that each clinician confronts. Thus,
implementation should occur with a caveat regarding perceived
medical-legal liability regarding neuroimaging and other testing.
“However,
a potential reason not to implement these guidelines is precisely
because of the lack of high-quality evidence proving or disproving each
recommendation. This is an interesting conundrum that we face in
creating guidelines that are truly evidence based yet clinically
relevant,” Dr. Buchhalter concluded.
DR. BUCHHALTER is chief of
neurology at Phoenix Children's Hospital. Dr. Buchhalter has received
personal compensation for activities with the National Institute of
Neurological Disorders and Stroke, and he has received research support
from Ovation Pharmaceuticals, Inc. and Pfizer Inc.
The guidelines on when to do a lumbar puncture “in the context of
lack of immunization and pretreatment with antibiotics will be most
useful with regard to decision making in this carefully defined patient
population,” Dr. Jeffrey Buchhalter said in an interview. The authors
“were very specific regarding age of inclusion and consideration of only
simple febrile seizures in their recommendation.”
“My general
impression is that many individuals who evaluate children with simple
febrile seizures recognize the very low utility of neuroimaging but
obtain head CT anyway due to concern regarding litigation if anything is
missed. The strong recommendation not to obtain skull films is
appropriate, but in my experience has not been used with any frequency
during the last decade,” he said.
“The guidelines make sense as so
much credence is given to observational studies – what we commonly see
in clinical practice. Furthermore, the recommendations take into account
a benefit/harm consideration that each clinician confronts. Thus,
implementation should occur with a caveat regarding perceived
medical-legal liability regarding neuroimaging and other testing.
“However,
a potential reason not to implement these guidelines is precisely
because of the lack of high-quality evidence proving or disproving each
recommendation. This is an interesting conundrum that we face in
creating guidelines that are truly evidence based yet clinically
relevant,” Dr. Buchhalter concluded.
DR. BUCHHALTER is chief of
neurology at Phoenix Children's Hospital. Dr. Buchhalter has received
personal compensation for activities with the National Institute of
Neurological Disorders and Stroke, and he has received research support
from Ovation Pharmaceuticals, Inc. and Pfizer Inc.
Identifying the cause of fever should be the top priority when evaluating infants or young children after a simple febrile seizure, and the differential diagnosis should always include meningitis, according to a new clinical practice guideline published by the American Academy of Pediatrics.
In most situations, however, “a simple febrile seizure does not usually require further evaluation, specifically electroencephalography, blood studies, or neuroimaging,” the AAP Subcommittee on Febrile Seizures wrote.
The new guideline replaces the 1996 AAP practice parameter for the neurodiagnostic evaluation of healthy infants and children 6–60 months of age who have had a simple febrile seizure and who present for evaluation within 12 hours of the event (Pediatrics 1996;97:769-72).
The new document is based on a comprehensive review of the evidence-based literature published from 1996 to February 2009, with an emphasis on research that differentiated simple febrile seizures from other seizure types. The final recommendations, presented as action statements relating to the use of lumbar puncture, electroencephalography, laboratory testing, and neuroimaging, were developed based on the quality of supporting evidence and the balance of benefit and harm if the given policy is carried out, said lead author Dr. Patricia K. Duffner, professor of neurology and pediatrics at the State University of New York at Buffalo, and her associates (Pediatrics 2011;127:389-94).
Dr. Duffner noted in an interview that the biggest change is in the recommendation regarding lumbar punctures. In the prior guideline, lumbar punctures were strongly considered for children aged 6 – 12 months and considered for those aged 12–18 months. With the advent of routine immunizations for Haemophilus influenzae and Streptococcus pneumoniae, the risk of simple febrile seizures being caused by bacterial meningitis is much reduced, she said. The caveat is the child who has not been immunized and the child who is on antibiotics which may mask the infection. In those cases, the physician will need to be more cautious in his/her evaluation of the child.
Neuroimaging was never recommended for simple febrile seizures, and “I doubt this will change practice for most pediatricians and ER physicians,” she said in an interview.
“I think the guidelines will be well accepted. They are timely and relevant given the evidence base supporting them,” Dr. Duffner concluded.
According to the document:
▸ Lumbar puncture. It is strongly recommended for children who present with febrile seizure and have meningeal signs and symptoms, including neck stiffness, Kernig signs, or Brudzinski signs, or those whose history or exam suggests possible meningitis or intracranial infection. The procedure is optional for infants between 6 and 12 months who have not received scheduled Haemophilus influenzae type b (Hib) or Streptococcus pneumoniae immunizations or when immunization status is unknown, and for children with febrile seizure who have been pretreated with antibiotics, which could potentially mask the signs and symptoms of meningitis.
Since the previous practice parameter was published, there has been widespread immunization in the United States for two of the most common causes of bacterial meningitis in this age range: Hib and S. pneumoniae. Compliance with all recommended immunizations does not completely eliminate the possibility of bacterial meningitis from the differential diagnosis, but “current data no longer support routine lumbar puncture in well-appearing, fully immunized children who present with a simple febrile seizure. Moreover, although approximately 25% of young children with meningitis have seizures as the presenting sign of the disease, some are either obtunded or comatose when evaluated by a physician for the seizure, and the remainder most often have obvious clinical signs of meningitis (focal seizures, recurrent seizures, petechial rash, or nuchal rigidity),” the guideline says.
▸ Electroencephalography (EEG). It should not be used routinely in the evaluation of simple febrile seizures in otherwise neurologically healthy children. “There is no evidence that EEG readings performed either at the time of presentation after a simple febrile seizure or within the following month are predictive of either recurrence of febrile seizures or the development of afebrile seizures/epilepsy within the next 2 years,” the authors wrote.
▸ Measurement of serum electrolytes, calcium, phosphorus, magnesium, blood glucose, or complete blood cell count. Such measurements should not be performed routinely for the sole purpose of identifying the cause of a simple febrile seizure. “When fever is present, the decision regarding the need for laboratory testing should be directed toward identifying the source of the fever rather than as part of the routine evaluation of the seizure itself,” Dr. Duffner and her associates concluded.
▸ Neuroimaging. It is not recommended for the routine evaluation of children who present with simple febrile seizures. “The literature does not support the use of skull films in evaluation of the child with a febrile seizure,” they explained, nor have data been published that support or negate the need for CT or MRI in this population.
Data do show that “CT scanning is associated with radiation exposure that may escalate future cancer risk. MRI is associated with risks from required sedation and high cost,” Dr. Duffner and her associates said. Additionally, extrapolation of data from CT studies in neurologically healthy children with generalized epilepsy “has shown that clinically important intracranial structural abnormalities in this patient population are uncommon,” they noted.
All of the authors filed conflict of interest statements with the AAP, and any conflicts have been resolved through a process approved by the Board of Directors. The AAP reported having neither solicited nor accepted any commercial involvement in the development of the revised guideline.
Identifying the cause of fever should be the top priority when evaluating infants or young children after a simple febrile seizure, and the differential diagnosis should always include meningitis, according to a new clinical practice guideline published by the American Academy of Pediatrics.
In most situations, however, “a simple febrile seizure does not usually require further evaluation, specifically electroencephalography, blood studies, or neuroimaging,” the AAP Subcommittee on Febrile Seizures wrote.
The new guideline replaces the 1996 AAP practice parameter for the neurodiagnostic evaluation of healthy infants and children 6–60 months of age who have had a simple febrile seizure and who present for evaluation within 12 hours of the event (Pediatrics 1996;97:769-72).
The new document is based on a comprehensive review of the evidence-based literature published from 1996 to February 2009, with an emphasis on research that differentiated simple febrile seizures from other seizure types. The final recommendations, presented as action statements relating to the use of lumbar puncture, electroencephalography, laboratory testing, and neuroimaging, were developed based on the quality of supporting evidence and the balance of benefit and harm if the given policy is carried out, said lead author Dr. Patricia K. Duffner, professor of neurology and pediatrics at the State University of New York at Buffalo, and her associates (Pediatrics 2011;127:389-94).
Dr. Duffner noted in an interview that the biggest change is in the recommendation regarding lumbar punctures. In the prior guideline, lumbar punctures were strongly considered for children aged 6 – 12 months and considered for those aged 12–18 months. With the advent of routine immunizations for Haemophilus influenzae and Streptococcus pneumoniae, the risk of simple febrile seizures being caused by bacterial meningitis is much reduced, she said. The caveat is the child who has not been immunized and the child who is on antibiotics which may mask the infection. In those cases, the physician will need to be more cautious in his/her evaluation of the child.
Neuroimaging was never recommended for simple febrile seizures, and “I doubt this will change practice for most pediatricians and ER physicians,” she said in an interview.
“I think the guidelines will be well accepted. They are timely and relevant given the evidence base supporting them,” Dr. Duffner concluded.
According to the document:
▸ Lumbar puncture. It is strongly recommended for children who present with febrile seizure and have meningeal signs and symptoms, including neck stiffness, Kernig signs, or Brudzinski signs, or those whose history or exam suggests possible meningitis or intracranial infection. The procedure is optional for infants between 6 and 12 months who have not received scheduled Haemophilus influenzae type b (Hib) or Streptococcus pneumoniae immunizations or when immunization status is unknown, and for children with febrile seizure who have been pretreated with antibiotics, which could potentially mask the signs and symptoms of meningitis.
Since the previous practice parameter was published, there has been widespread immunization in the United States for two of the most common causes of bacterial meningitis in this age range: Hib and S. pneumoniae. Compliance with all recommended immunizations does not completely eliminate the possibility of bacterial meningitis from the differential diagnosis, but “current data no longer support routine lumbar puncture in well-appearing, fully immunized children who present with a simple febrile seizure. Moreover, although approximately 25% of young children with meningitis have seizures as the presenting sign of the disease, some are either obtunded or comatose when evaluated by a physician for the seizure, and the remainder most often have obvious clinical signs of meningitis (focal seizures, recurrent seizures, petechial rash, or nuchal rigidity),” the guideline says.
▸ Electroencephalography (EEG). It should not be used routinely in the evaluation of simple febrile seizures in otherwise neurologically healthy children. “There is no evidence that EEG readings performed either at the time of presentation after a simple febrile seizure or within the following month are predictive of either recurrence of febrile seizures or the development of afebrile seizures/epilepsy within the next 2 years,” the authors wrote.
▸ Measurement of serum electrolytes, calcium, phosphorus, magnesium, blood glucose, or complete blood cell count. Such measurements should not be performed routinely for the sole purpose of identifying the cause of a simple febrile seizure. “When fever is present, the decision regarding the need for laboratory testing should be directed toward identifying the source of the fever rather than as part of the routine evaluation of the seizure itself,” Dr. Duffner and her associates concluded.
▸ Neuroimaging. It is not recommended for the routine evaluation of children who present with simple febrile seizures. “The literature does not support the use of skull films in evaluation of the child with a febrile seizure,” they explained, nor have data been published that support or negate the need for CT or MRI in this population.
Data do show that “CT scanning is associated with radiation exposure that may escalate future cancer risk. MRI is associated with risks from required sedation and high cost,” Dr. Duffner and her associates said. Additionally, extrapolation of data from CT studies in neurologically healthy children with generalized epilepsy “has shown that clinically important intracranial structural abnormalities in this patient population are uncommon,” they noted.
All of the authors filed conflict of interest statements with the AAP, and any conflicts have been resolved through a process approved by the Board of Directors. The AAP reported having neither solicited nor accepted any commercial involvement in the development of the revised guideline.
New Epilepsy Treatments Found Safe, Effective in Phase III
SAN ANTONIO – Treatment options for epilepsy may soon be expanding in light of the results of several recently reported phase III trials.
Two drugs, including one that has not yet been approved in any country, demonstrated efficacy and safety as adjunctive treatments for different forms of epilepsy.
Perampanel, a selective, noncompetitive alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor antagonist was tested as an add-on therapy for partial-onset seizures in the first of three multinational, placebo-controlled trials.
Adjunctive therapy with the benzodiazepine derivative clobazam significantly reduced the occurrence of drop seizures in the largest clinical trial to date in patients with Lennox-Gastaut syndrome.
Perampanel
In the Eisai-sponsored study of perampanel, 712 patients aged between 12 and 72 years with refractory partial seizures were randomized to treatment with 2, 4, or 8 mg/day of perampanel or placebo following a 6-week baseline phase. The patients were being treated with one to three concomitant antiepileptic drugs, Dr. Gregory L. Krauss reported.
At the end of the 19-week treatment phase, the median change in seizure frequency from baseline for the intention-to-treat population was significant in the 4-mg and 8-mg groups, with reductions of 28.6% and 33.5%, respectively, compared with nonsignificant reductions of 16.3% and 13.8% in the 2-mg and placebo groups, respectively.
The treatment phase included 6-week titration and 13-week maintenance periods, according to Dr. Krauss, professor of neurology at Johns Hopkins University in Baltimore.
“The responder rates were similar,” he noted, referring to the percentage of patients in each group who experienced at least a 50% reduction in seizure frequency during the maintenance phase relative to baseline. Nearly 29% of the 4-mg group and 35% of the 8-mg group were responders, compared with 21% of the 2-mg group and 17.6% of the placebo group, he said.
Treatment-related adverse events – most often dizziness, somnolence, and headache – caused a low number of patients in each group to withdraw from the trial. The few serious adverse events that occurred also were similarly distributed across the groups, according to Dr. Krauss.
In addition to confirming the safety and efficacy of 4 mg and 8 mg perampanel as an add-on treatment for partial-onset seizures, the findings also “help to establish the range of therapeutic doses and to identify the potential lower dose range for treatment,” he said.
Clobazam
The frequency of drop seizures declined significantly for patients with Lennox-Gastaut Syndrome (LGS) who received the highest doses of clobazam in a double-blind, placebo-controlled trial.
“Patients in the 0.5-mg dose group experienced an average decrease of 47.8% and those in the 1.5-mg group had an average decrease of 69.5%,” said Dr. Joan Conry of Children's National Medical Center in Washington.
Dr. Conry said that the drug “is much needed” because the drop attacks experienced by LGS patients often lead to injury.
In the trial, 238 patients aged 2-60 years with clinical and EEG-confirmed LGS who experienced drop seizures during a 4-week baseline phase were randomized to placebo or 0.25 mg, 0.5 mg, or 1.5 mg of clobazam up to a maximum daily dose of 40 mg. Following the treatment period (a 3-week titration phase and a 12-week maintenance phase), the investigators compared the percentage decrease in mean weekly drop seizures during the maintenance phase against the baseline rate for the modified intention-to-treat population of 217 patients.
Patients who experienced 75% and 50% reductions in drop seizures showed significant decreases relative to placebo in the medium- and low-dosage groups. Seizure frequency was reduced by 75% in 38% of patients who received 0.5 mg and 63% of patients who received 1.5 mg, compared with 11% of placebo-treated patients. Seizure reductions of at least 50% occurred in 59% of the medium-dosage group and 78% of the high-dosage group, compared with 32% of the placebo patients, she said.
The patients who were taking the high dosage of clobazam also had a significant decline in the frequency of nondrop seizures – a secondary study outcome – in comparison with placebo. Physician and caregiver global assessment scores also improved across all three of the dosages, Dr. Conry stated.
The most frequent adverse events observed included somnolence, lethargy, upper respiratory tract infections, drooling, and behavioral abnormalities, she noted.
Lundbeck, the manufacturer of clobazam and sponsor of the trial, will likely submit an application to the Food and Drug Administration in the first quarter of 2011, according to Dr. Conry. The drug is already available in more than 100 countries.
Dr. Krauss reported relationships with UCB Pharma, Bristol-Meyers Squibb, Eisai, SK Biosciences, and Johnson & Johnson. Dr. Conry received compensation from Lundbeck for the clobazam study.
Adjunctive therapy with 8 mg of perampanel decreased the mean frequency of seizures by 33.5%.
Source DR. KRAUSS
SAN ANTONIO – Treatment options for epilepsy may soon be expanding in light of the results of several recently reported phase III trials.
Two drugs, including one that has not yet been approved in any country, demonstrated efficacy and safety as adjunctive treatments for different forms of epilepsy.
Perampanel, a selective, noncompetitive alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor antagonist was tested as an add-on therapy for partial-onset seizures in the first of three multinational, placebo-controlled trials.
Adjunctive therapy with the benzodiazepine derivative clobazam significantly reduced the occurrence of drop seizures in the largest clinical trial to date in patients with Lennox-Gastaut syndrome.
Perampanel
In the Eisai-sponsored study of perampanel, 712 patients aged between 12 and 72 years with refractory partial seizures were randomized to treatment with 2, 4, or 8 mg/day of perampanel or placebo following a 6-week baseline phase. The patients were being treated with one to three concomitant antiepileptic drugs, Dr. Gregory L. Krauss reported.
At the end of the 19-week treatment phase, the median change in seizure frequency from baseline for the intention-to-treat population was significant in the 4-mg and 8-mg groups, with reductions of 28.6% and 33.5%, respectively, compared with nonsignificant reductions of 16.3% and 13.8% in the 2-mg and placebo groups, respectively.
The treatment phase included 6-week titration and 13-week maintenance periods, according to Dr. Krauss, professor of neurology at Johns Hopkins University in Baltimore.
“The responder rates were similar,” he noted, referring to the percentage of patients in each group who experienced at least a 50% reduction in seizure frequency during the maintenance phase relative to baseline. Nearly 29% of the 4-mg group and 35% of the 8-mg group were responders, compared with 21% of the 2-mg group and 17.6% of the placebo group, he said.
Treatment-related adverse events – most often dizziness, somnolence, and headache – caused a low number of patients in each group to withdraw from the trial. The few serious adverse events that occurred also were similarly distributed across the groups, according to Dr. Krauss.
In addition to confirming the safety and efficacy of 4 mg and 8 mg perampanel as an add-on treatment for partial-onset seizures, the findings also “help to establish the range of therapeutic doses and to identify the potential lower dose range for treatment,” he said.
Clobazam
The frequency of drop seizures declined significantly for patients with Lennox-Gastaut Syndrome (LGS) who received the highest doses of clobazam in a double-blind, placebo-controlled trial.
“Patients in the 0.5-mg dose group experienced an average decrease of 47.8% and those in the 1.5-mg group had an average decrease of 69.5%,” said Dr. Joan Conry of Children's National Medical Center in Washington.
Dr. Conry said that the drug “is much needed” because the drop attacks experienced by LGS patients often lead to injury.
In the trial, 238 patients aged 2-60 years with clinical and EEG-confirmed LGS who experienced drop seizures during a 4-week baseline phase were randomized to placebo or 0.25 mg, 0.5 mg, or 1.5 mg of clobazam up to a maximum daily dose of 40 mg. Following the treatment period (a 3-week titration phase and a 12-week maintenance phase), the investigators compared the percentage decrease in mean weekly drop seizures during the maintenance phase against the baseline rate for the modified intention-to-treat population of 217 patients.
Patients who experienced 75% and 50% reductions in drop seizures showed significant decreases relative to placebo in the medium- and low-dosage groups. Seizure frequency was reduced by 75% in 38% of patients who received 0.5 mg and 63% of patients who received 1.5 mg, compared with 11% of placebo-treated patients. Seizure reductions of at least 50% occurred in 59% of the medium-dosage group and 78% of the high-dosage group, compared with 32% of the placebo patients, she said.
The patients who were taking the high dosage of clobazam also had a significant decline in the frequency of nondrop seizures – a secondary study outcome – in comparison with placebo. Physician and caregiver global assessment scores also improved across all three of the dosages, Dr. Conry stated.
The most frequent adverse events observed included somnolence, lethargy, upper respiratory tract infections, drooling, and behavioral abnormalities, she noted.
Lundbeck, the manufacturer of clobazam and sponsor of the trial, will likely submit an application to the Food and Drug Administration in the first quarter of 2011, according to Dr. Conry. The drug is already available in more than 100 countries.
Dr. Krauss reported relationships with UCB Pharma, Bristol-Meyers Squibb, Eisai, SK Biosciences, and Johnson & Johnson. Dr. Conry received compensation from Lundbeck for the clobazam study.
Adjunctive therapy with 8 mg of perampanel decreased the mean frequency of seizures by 33.5%.
Source DR. KRAUSS
SAN ANTONIO – Treatment options for epilepsy may soon be expanding in light of the results of several recently reported phase III trials.
Two drugs, including one that has not yet been approved in any country, demonstrated efficacy and safety as adjunctive treatments for different forms of epilepsy.
Perampanel, a selective, noncompetitive alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor antagonist was tested as an add-on therapy for partial-onset seizures in the first of three multinational, placebo-controlled trials.
Adjunctive therapy with the benzodiazepine derivative clobazam significantly reduced the occurrence of drop seizures in the largest clinical trial to date in patients with Lennox-Gastaut syndrome.
Perampanel
In the Eisai-sponsored study of perampanel, 712 patients aged between 12 and 72 years with refractory partial seizures were randomized to treatment with 2, 4, or 8 mg/day of perampanel or placebo following a 6-week baseline phase. The patients were being treated with one to three concomitant antiepileptic drugs, Dr. Gregory L. Krauss reported.
At the end of the 19-week treatment phase, the median change in seizure frequency from baseline for the intention-to-treat population was significant in the 4-mg and 8-mg groups, with reductions of 28.6% and 33.5%, respectively, compared with nonsignificant reductions of 16.3% and 13.8% in the 2-mg and placebo groups, respectively.
The treatment phase included 6-week titration and 13-week maintenance periods, according to Dr. Krauss, professor of neurology at Johns Hopkins University in Baltimore.
“The responder rates were similar,” he noted, referring to the percentage of patients in each group who experienced at least a 50% reduction in seizure frequency during the maintenance phase relative to baseline. Nearly 29% of the 4-mg group and 35% of the 8-mg group were responders, compared with 21% of the 2-mg group and 17.6% of the placebo group, he said.
Treatment-related adverse events – most often dizziness, somnolence, and headache – caused a low number of patients in each group to withdraw from the trial. The few serious adverse events that occurred also were similarly distributed across the groups, according to Dr. Krauss.
In addition to confirming the safety and efficacy of 4 mg and 8 mg perampanel as an add-on treatment for partial-onset seizures, the findings also “help to establish the range of therapeutic doses and to identify the potential lower dose range for treatment,” he said.
Clobazam
The frequency of drop seizures declined significantly for patients with Lennox-Gastaut Syndrome (LGS) who received the highest doses of clobazam in a double-blind, placebo-controlled trial.
“Patients in the 0.5-mg dose group experienced an average decrease of 47.8% and those in the 1.5-mg group had an average decrease of 69.5%,” said Dr. Joan Conry of Children's National Medical Center in Washington.
Dr. Conry said that the drug “is much needed” because the drop attacks experienced by LGS patients often lead to injury.
In the trial, 238 patients aged 2-60 years with clinical and EEG-confirmed LGS who experienced drop seizures during a 4-week baseline phase were randomized to placebo or 0.25 mg, 0.5 mg, or 1.5 mg of clobazam up to a maximum daily dose of 40 mg. Following the treatment period (a 3-week titration phase and a 12-week maintenance phase), the investigators compared the percentage decrease in mean weekly drop seizures during the maintenance phase against the baseline rate for the modified intention-to-treat population of 217 patients.
Patients who experienced 75% and 50% reductions in drop seizures showed significant decreases relative to placebo in the medium- and low-dosage groups. Seizure frequency was reduced by 75% in 38% of patients who received 0.5 mg and 63% of patients who received 1.5 mg, compared with 11% of placebo-treated patients. Seizure reductions of at least 50% occurred in 59% of the medium-dosage group and 78% of the high-dosage group, compared with 32% of the placebo patients, she said.
The patients who were taking the high dosage of clobazam also had a significant decline in the frequency of nondrop seizures – a secondary study outcome – in comparison with placebo. Physician and caregiver global assessment scores also improved across all three of the dosages, Dr. Conry stated.
The most frequent adverse events observed included somnolence, lethargy, upper respiratory tract infections, drooling, and behavioral abnormalities, she noted.
Lundbeck, the manufacturer of clobazam and sponsor of the trial, will likely submit an application to the Food and Drug Administration in the first quarter of 2011, according to Dr. Conry. The drug is already available in more than 100 countries.
Dr. Krauss reported relationships with UCB Pharma, Bristol-Meyers Squibb, Eisai, SK Biosciences, and Johnson & Johnson. Dr. Conry received compensation from Lundbeck for the clobazam study.
Adjunctive therapy with 8 mg of perampanel decreased the mean frequency of seizures by 33.5%.
Source DR. KRAUSS
Ketogenic Diet May Help Some With Epilepsy : Seizure control may improve with switch from the modified Atkins diet to the stricter ketogenic diet.
SAN ANTONIO – Switching from the modified Atkins diet to the stricter ketogenic diet may improve seizure control in some patients with intractable epilepsy, a multinational, retrospective study has shown. h
In particular, patients with myoclonic-astatic epilepsy, an idiopathic generalized epilepsy syndrome of early childhood, appeared to have the greatest likelihood of further improvement after making the switch, Dr. Eric Kossoff reported at the meetingo
Previous studies have suggested that children who have achieved seizure control with the stringent, high-fat, low-carbohydrate ketogenic diet can maintain that status when they transition to the less-restrictive modified Atkins diet; however, the possibility of achieving additional seizure control by switching from the modified Atkins to the ketogenic diet has not been investigated, said Dr. Kossoff of Johns Hopkins University, Baltimore.
The modified Atkins diet differs from the traditional Atkins program in its further restriction of carbohydrates and stronger encouragement of fat intake. Compared with the ketogenic diet, the modified Atkins diet does not restrict fluid, calories, or protein, and it relies on carbohydrate counts rather than food weight and measurement, Dr. Kossoff explained.
Dr. Kossoff and colleagues from Denmark, Germany, and South Korea found that 9 of 28 patients who made the change reduced the frequency of seizures by more than 10%; 5 of the 9 subsequently became seizure free.
The ketogenic diet did not improve seizures in another five children who previously had no improvement while on the modified Atkins diet.
The likelihood of improvement as a result of the dietary switch was 78% for patients with myoclonic-astatic epilepsy, which was significantly higher than the 11% reported for all other etiologies combined. All five children who became seizure free after transitioning to the ketogenic diet had myoclonic-astatic epilepsy.
“We also observed a trend toward greater likelihood of improvement if a child had fasted at the onset of the ketogenic diet, but this did not reach statistical significance,” he said.
Further research into the mechanisms underlying the anticonvulsant effect of the diets is needed to determine when and in which patients to use them, Dr. Kossoff said.
Some insight into this question was provided at the meeting by Susan Masino, Ph.D., of Trinity College in Hartford, Conn., who presented the findings of a study that confirmed adenosine as a key factor in the anticonvulsant effect of the ketogenic diet.
Dr. Masino and her colleagues found that mice with normal levels of adenosine A1 receptor (A1R) and a transgenic overexpression of adenosine kinase, an intracellular enzyme that negatively influences extracellular levels of adenosine, had a “near complete” reduction in the number and duration of spontaneous seizures. But mice with reduced A1R levels and those that lacked A1Rs were partially or completely resistant to the diet therapy.
“When we injected glucose, which blocks A1Rs, into the mice with reduced seizures from the ketogenic diet, the seizure frequency returned to previous levels within 30-90 minutes,” she said.
The ketogenic diet appears to reduce seizures by increasing A1R-mediated inhibition through its low carbohydrate nature, Dr. Masino said. The suggestion that ketogenic metabolism increases the activity of adenosine at the A1 receptor subtype “may offer insight into new therapies for epilepsy as well as other clinical conditions in which adenosine is known to have clinical benefits.”
Dr. Kossoff has received consultant fees from Atkins Nutritionals Inc. Dr. Masino reported having no relevant financial disclosures.
The chance of improvement as a result of dietary switch was 78% for patients with myoclonic-astatic epilepsy.
Source DR. KOSSOFF
SAN ANTONIO – Switching from the modified Atkins diet to the stricter ketogenic diet may improve seizure control in some patients with intractable epilepsy, a multinational, retrospective study has shown. h
In particular, patients with myoclonic-astatic epilepsy, an idiopathic generalized epilepsy syndrome of early childhood, appeared to have the greatest likelihood of further improvement after making the switch, Dr. Eric Kossoff reported at the meetingo
Previous studies have suggested that children who have achieved seizure control with the stringent, high-fat, low-carbohydrate ketogenic diet can maintain that status when they transition to the less-restrictive modified Atkins diet; however, the possibility of achieving additional seizure control by switching from the modified Atkins to the ketogenic diet has not been investigated, said Dr. Kossoff of Johns Hopkins University, Baltimore.
The modified Atkins diet differs from the traditional Atkins program in its further restriction of carbohydrates and stronger encouragement of fat intake. Compared with the ketogenic diet, the modified Atkins diet does not restrict fluid, calories, or protein, and it relies on carbohydrate counts rather than food weight and measurement, Dr. Kossoff explained.
Dr. Kossoff and colleagues from Denmark, Germany, and South Korea found that 9 of 28 patients who made the change reduced the frequency of seizures by more than 10%; 5 of the 9 subsequently became seizure free.
The ketogenic diet did not improve seizures in another five children who previously had no improvement while on the modified Atkins diet.
The likelihood of improvement as a result of the dietary switch was 78% for patients with myoclonic-astatic epilepsy, which was significantly higher than the 11% reported for all other etiologies combined. All five children who became seizure free after transitioning to the ketogenic diet had myoclonic-astatic epilepsy.
“We also observed a trend toward greater likelihood of improvement if a child had fasted at the onset of the ketogenic diet, but this did not reach statistical significance,” he said.
Further research into the mechanisms underlying the anticonvulsant effect of the diets is needed to determine when and in which patients to use them, Dr. Kossoff said.
Some insight into this question was provided at the meeting by Susan Masino, Ph.D., of Trinity College in Hartford, Conn., who presented the findings of a study that confirmed adenosine as a key factor in the anticonvulsant effect of the ketogenic diet.
Dr. Masino and her colleagues found that mice with normal levels of adenosine A1 receptor (A1R) and a transgenic overexpression of adenosine kinase, an intracellular enzyme that negatively influences extracellular levels of adenosine, had a “near complete” reduction in the number and duration of spontaneous seizures. But mice with reduced A1R levels and those that lacked A1Rs were partially or completely resistant to the diet therapy.
“When we injected glucose, which blocks A1Rs, into the mice with reduced seizures from the ketogenic diet, the seizure frequency returned to previous levels within 30-90 minutes,” she said.
The ketogenic diet appears to reduce seizures by increasing A1R-mediated inhibition through its low carbohydrate nature, Dr. Masino said. The suggestion that ketogenic metabolism increases the activity of adenosine at the A1 receptor subtype “may offer insight into new therapies for epilepsy as well as other clinical conditions in which adenosine is known to have clinical benefits.”
Dr. Kossoff has received consultant fees from Atkins Nutritionals Inc. Dr. Masino reported having no relevant financial disclosures.
The chance of improvement as a result of dietary switch was 78% for patients with myoclonic-astatic epilepsy.
Source DR. KOSSOFF
SAN ANTONIO – Switching from the modified Atkins diet to the stricter ketogenic diet may improve seizure control in some patients with intractable epilepsy, a multinational, retrospective study has shown. h
In particular, patients with myoclonic-astatic epilepsy, an idiopathic generalized epilepsy syndrome of early childhood, appeared to have the greatest likelihood of further improvement after making the switch, Dr. Eric Kossoff reported at the meetingo
Previous studies have suggested that children who have achieved seizure control with the stringent, high-fat, low-carbohydrate ketogenic diet can maintain that status when they transition to the less-restrictive modified Atkins diet; however, the possibility of achieving additional seizure control by switching from the modified Atkins to the ketogenic diet has not been investigated, said Dr. Kossoff of Johns Hopkins University, Baltimore.
The modified Atkins diet differs from the traditional Atkins program in its further restriction of carbohydrates and stronger encouragement of fat intake. Compared with the ketogenic diet, the modified Atkins diet does not restrict fluid, calories, or protein, and it relies on carbohydrate counts rather than food weight and measurement, Dr. Kossoff explained.
Dr. Kossoff and colleagues from Denmark, Germany, and South Korea found that 9 of 28 patients who made the change reduced the frequency of seizures by more than 10%; 5 of the 9 subsequently became seizure free.
The ketogenic diet did not improve seizures in another five children who previously had no improvement while on the modified Atkins diet.
The likelihood of improvement as a result of the dietary switch was 78% for patients with myoclonic-astatic epilepsy, which was significantly higher than the 11% reported for all other etiologies combined. All five children who became seizure free after transitioning to the ketogenic diet had myoclonic-astatic epilepsy.
“We also observed a trend toward greater likelihood of improvement if a child had fasted at the onset of the ketogenic diet, but this did not reach statistical significance,” he said.
Further research into the mechanisms underlying the anticonvulsant effect of the diets is needed to determine when and in which patients to use them, Dr. Kossoff said.
Some insight into this question was provided at the meeting by Susan Masino, Ph.D., of Trinity College in Hartford, Conn., who presented the findings of a study that confirmed adenosine as a key factor in the anticonvulsant effect of the ketogenic diet.
Dr. Masino and her colleagues found that mice with normal levels of adenosine A1 receptor (A1R) and a transgenic overexpression of adenosine kinase, an intracellular enzyme that negatively influences extracellular levels of adenosine, had a “near complete” reduction in the number and duration of spontaneous seizures. But mice with reduced A1R levels and those that lacked A1Rs were partially or completely resistant to the diet therapy.
“When we injected glucose, which blocks A1Rs, into the mice with reduced seizures from the ketogenic diet, the seizure frequency returned to previous levels within 30-90 minutes,” she said.
The ketogenic diet appears to reduce seizures by increasing A1R-mediated inhibition through its low carbohydrate nature, Dr. Masino said. The suggestion that ketogenic metabolism increases the activity of adenosine at the A1 receptor subtype “may offer insight into new therapies for epilepsy as well as other clinical conditions in which adenosine is known to have clinical benefits.”
Dr. Kossoff has received consultant fees from Atkins Nutritionals Inc. Dr. Masino reported having no relevant financial disclosures.
The chance of improvement as a result of dietary switch was 78% for patients with myoclonic-astatic epilepsy.
Source DR. KOSSOFF
AAP Issues New Guidelines for Neuroevaluation of Febrile Seizures
Identifying the cause of fever should be the top priority when evaluating infants or young children after a simple febrile seizure, and the differential diagnosis should always include meningitis, according to a new clinical practice guideline published by the American Academy of Pediatrics.
In most situations, however, "a simple febrile seizure does not usually require further evaluation, specifically electroencephalography, blood studies, or neuroimaging," the AAP Subcommittee on Febrile Seizures wrote in the February 2011 issue of Pediatrics.
The new guideline replaces the 1996 AAP practice parameter for the neurodiagnostic evaluation of healthy infants and children 6-60 months of age who have had a simple febrile seizure and who present for evaluation within 12 hours of the event (Pediatrics 1996;97:769-72).
The new document is based on a comprehensive review of the evidence-based literature published from 1996 to February 2009, with an emphasis on research that differentiated simple febrile seizures from other seizure types. The final recommendations, presented as action statements relating to the use of lumbar puncture, electroencephalography, laboratory testing, and neuroimaging, were developed based on the quality of supporting evidence and the balance of benefit and harm if the given policy is carried out, said lead author Dr. Patricia K. Duffner, professor of neurology and pediatrics at the State University of New York at Buffalo, and associates (Pediatrics 2011 Jan. 31 [doi: 10.1542/peds.2010-3318]).
According to the document:
• Lumbar puncture. It is strongly recommended for children who present with febrile seizure and have meningeal signs and symptoms, including neck stiffness, Kernig signs, or Brudzinski signs, or those whose history or exam suggests possible meningitis or intracranial infection. The procedure is optional for infants between 6 and 12 months who have not received scheduled Haemophilus influenzae type b (Hib) or Streptococcus pneumoniae immunizations or when immunization status is unknown, and for children with febrile seizure who have been pretreated with antibiotics, which could potentially mask the signs and symptoms of meningitis.
Since the previous practice parameter was published, there has been widespread immunization in the United States for two of the most common causes of bacterial meningitis in this age range: Hib and S. pneumoniae. Compliance with all recommended immunizations does not completely eliminate the possibility of bacterial meningitis from the differential diagnosis, but "current data no longer support routine lumbar puncture in well-appearing, fully immunized children who present with a simple febrile seizure. Moreover, although approximately 25% of young children with meningitis have seizures as the presenting sign of the disease, some are either obtunded or comatose when evaluated by a physician for the seizure, and the remainder most often have obvious clinical signs of meningitis (focal seizures, recurrent seizures, petechial rash, or nuchal rigidity)," the guideline says.
• Electroencephalography (EEG). It should not be used routinely in the evaluation of simple febrile seizures in otherwise neurologically healthy children. "There is no evidence that EEG readings performed either at the time of presentation after a simple febrile seizure or within the following month are predictive of either recurrence of febrile seizures or the development of afebrile seizures/epilepsy within the next 2 years," the authors wrote.
• Measurement of serum electrolytes, calcium, phosphorus, magnesium, blood glucose, or complete blood cell count. Such measurements should not be performed routinely for the sole purpose of identifying the cause of a simple febrile seizure. "When fever is present, the decision regarding the need for laboratory testing should be directed toward identifying the source of the fever rather than as part of the routine evaluation of the seizure itself," Dr. Duffner and her associates concluded.
• Neuroimaging. It is not recommended for the routine evaluation of children who present with simple febrile seizures. "The literature does not support the use of skull films in evaluation of the child with a febrile seizure," they explained, nor have data been published that support or negate the need for CT or MRI in this population.
Data do show that "CT scanning is associated with radiation exposure that may escalate future cancer risk. MRI is associated with risks from required sedation and high cost," Dr. Duffner and her associates said. Additionally, extrapolation of data from CT studies in neurologically healthy children with generalized epilepsy "has shown that clinically important intracranial structural abnormalities in this patient population are uncommon," they noted.
All of the authors filed conflict of interest statements with the AAP, and any conflicts have been resolved through a process approved by the Board of Directors. The AAP reported having neither solicited nor accepted any commercial involvement in the development of the revised guideline.
Identifying the cause of fever should be the top priority when evaluating infants or young children after a simple febrile seizure, and the differential diagnosis should always include meningitis, according to a new clinical practice guideline published by the American Academy of Pediatrics.
In most situations, however, "a simple febrile seizure does not usually require further evaluation, specifically electroencephalography, blood studies, or neuroimaging," the AAP Subcommittee on Febrile Seizures wrote in the February 2011 issue of Pediatrics.
The new guideline replaces the 1996 AAP practice parameter for the neurodiagnostic evaluation of healthy infants and children 6-60 months of age who have had a simple febrile seizure and who present for evaluation within 12 hours of the event (Pediatrics 1996;97:769-72).
The new document is based on a comprehensive review of the evidence-based literature published from 1996 to February 2009, with an emphasis on research that differentiated simple febrile seizures from other seizure types. The final recommendations, presented as action statements relating to the use of lumbar puncture, electroencephalography, laboratory testing, and neuroimaging, were developed based on the quality of supporting evidence and the balance of benefit and harm if the given policy is carried out, said lead author Dr. Patricia K. Duffner, professor of neurology and pediatrics at the State University of New York at Buffalo, and associates (Pediatrics 2011 Jan. 31 [doi: 10.1542/peds.2010-3318]).
According to the document:
• Lumbar puncture. It is strongly recommended for children who present with febrile seizure and have meningeal signs and symptoms, including neck stiffness, Kernig signs, or Brudzinski signs, or those whose history or exam suggests possible meningitis or intracranial infection. The procedure is optional for infants between 6 and 12 months who have not received scheduled Haemophilus influenzae type b (Hib) or Streptococcus pneumoniae immunizations or when immunization status is unknown, and for children with febrile seizure who have been pretreated with antibiotics, which could potentially mask the signs and symptoms of meningitis.
Since the previous practice parameter was published, there has been widespread immunization in the United States for two of the most common causes of bacterial meningitis in this age range: Hib and S. pneumoniae. Compliance with all recommended immunizations does not completely eliminate the possibility of bacterial meningitis from the differential diagnosis, but "current data no longer support routine lumbar puncture in well-appearing, fully immunized children who present with a simple febrile seizure. Moreover, although approximately 25% of young children with meningitis have seizures as the presenting sign of the disease, some are either obtunded or comatose when evaluated by a physician for the seizure, and the remainder most often have obvious clinical signs of meningitis (focal seizures, recurrent seizures, petechial rash, or nuchal rigidity)," the guideline says.
• Electroencephalography (EEG). It should not be used routinely in the evaluation of simple febrile seizures in otherwise neurologically healthy children. "There is no evidence that EEG readings performed either at the time of presentation after a simple febrile seizure or within the following month are predictive of either recurrence of febrile seizures or the development of afebrile seizures/epilepsy within the next 2 years," the authors wrote.
• Measurement of serum electrolytes, calcium, phosphorus, magnesium, blood glucose, or complete blood cell count. Such measurements should not be performed routinely for the sole purpose of identifying the cause of a simple febrile seizure. "When fever is present, the decision regarding the need for laboratory testing should be directed toward identifying the source of the fever rather than as part of the routine evaluation of the seizure itself," Dr. Duffner and her associates concluded.
• Neuroimaging. It is not recommended for the routine evaluation of children who present with simple febrile seizures. "The literature does not support the use of skull films in evaluation of the child with a febrile seizure," they explained, nor have data been published that support or negate the need for CT or MRI in this population.
Data do show that "CT scanning is associated with radiation exposure that may escalate future cancer risk. MRI is associated with risks from required sedation and high cost," Dr. Duffner and her associates said. Additionally, extrapolation of data from CT studies in neurologically healthy children with generalized epilepsy "has shown that clinically important intracranial structural abnormalities in this patient population are uncommon," they noted.
All of the authors filed conflict of interest statements with the AAP, and any conflicts have been resolved through a process approved by the Board of Directors. The AAP reported having neither solicited nor accepted any commercial involvement in the development of the revised guideline.
Identifying the cause of fever should be the top priority when evaluating infants or young children after a simple febrile seizure, and the differential diagnosis should always include meningitis, according to a new clinical practice guideline published by the American Academy of Pediatrics.
In most situations, however, "a simple febrile seizure does not usually require further evaluation, specifically electroencephalography, blood studies, or neuroimaging," the AAP Subcommittee on Febrile Seizures wrote in the February 2011 issue of Pediatrics.
The new guideline replaces the 1996 AAP practice parameter for the neurodiagnostic evaluation of healthy infants and children 6-60 months of age who have had a simple febrile seizure and who present for evaluation within 12 hours of the event (Pediatrics 1996;97:769-72).
The new document is based on a comprehensive review of the evidence-based literature published from 1996 to February 2009, with an emphasis on research that differentiated simple febrile seizures from other seizure types. The final recommendations, presented as action statements relating to the use of lumbar puncture, electroencephalography, laboratory testing, and neuroimaging, were developed based on the quality of supporting evidence and the balance of benefit and harm if the given policy is carried out, said lead author Dr. Patricia K. Duffner, professor of neurology and pediatrics at the State University of New York at Buffalo, and associates (Pediatrics 2011 Jan. 31 [doi: 10.1542/peds.2010-3318]).
According to the document:
• Lumbar puncture. It is strongly recommended for children who present with febrile seizure and have meningeal signs and symptoms, including neck stiffness, Kernig signs, or Brudzinski signs, or those whose history or exam suggests possible meningitis or intracranial infection. The procedure is optional for infants between 6 and 12 months who have not received scheduled Haemophilus influenzae type b (Hib) or Streptococcus pneumoniae immunizations or when immunization status is unknown, and for children with febrile seizure who have been pretreated with antibiotics, which could potentially mask the signs and symptoms of meningitis.
Since the previous practice parameter was published, there has been widespread immunization in the United States for two of the most common causes of bacterial meningitis in this age range: Hib and S. pneumoniae. Compliance with all recommended immunizations does not completely eliminate the possibility of bacterial meningitis from the differential diagnosis, but "current data no longer support routine lumbar puncture in well-appearing, fully immunized children who present with a simple febrile seizure. Moreover, although approximately 25% of young children with meningitis have seizures as the presenting sign of the disease, some are either obtunded or comatose when evaluated by a physician for the seizure, and the remainder most often have obvious clinical signs of meningitis (focal seizures, recurrent seizures, petechial rash, or nuchal rigidity)," the guideline says.
• Electroencephalography (EEG). It should not be used routinely in the evaluation of simple febrile seizures in otherwise neurologically healthy children. "There is no evidence that EEG readings performed either at the time of presentation after a simple febrile seizure or within the following month are predictive of either recurrence of febrile seizures or the development of afebrile seizures/epilepsy within the next 2 years," the authors wrote.
• Measurement of serum electrolytes, calcium, phosphorus, magnesium, blood glucose, or complete blood cell count. Such measurements should not be performed routinely for the sole purpose of identifying the cause of a simple febrile seizure. "When fever is present, the decision regarding the need for laboratory testing should be directed toward identifying the source of the fever rather than as part of the routine evaluation of the seizure itself," Dr. Duffner and her associates concluded.
• Neuroimaging. It is not recommended for the routine evaluation of children who present with simple febrile seizures. "The literature does not support the use of skull films in evaluation of the child with a febrile seizure," they explained, nor have data been published that support or negate the need for CT or MRI in this population.
Data do show that "CT scanning is associated with radiation exposure that may escalate future cancer risk. MRI is associated with risks from required sedation and high cost," Dr. Duffner and her associates said. Additionally, extrapolation of data from CT studies in neurologically healthy children with generalized epilepsy "has shown that clinically important intracranial structural abnormalities in this patient population are uncommon," they noted.
All of the authors filed conflict of interest statements with the AAP, and any conflicts have been resolved through a process approved by the Board of Directors. The AAP reported having neither solicited nor accepted any commercial involvement in the development of the revised guideline.