User login
Repeat Laparoscopic Cholecystectomy for Duplicated Gallbladder After 16-Year Interval
Gallbladder duplication is a congenital abnormality of the hepatobiliary system and often is not considered in the evaluation of a patient with right upper quadrant pain. Accuracy of the most commonly used imaging study to assess for biliary disease, abdominal ultrasound, is highly dependent on the skills of the ultrasonographer, and given its relative rarity, this condition is often not considered prior to planned cholecystectomy.1 Small case reviews found that < 50% of gallbladder duplications are diagnosed preoperatively despite use of ultrasound or computed tomography (CT) scan.2-4 Failure to recognize duplicate gallbladder anatomy in symptomatic patients may result in incomplete surgical management, an increase in perioperative complications, and years of morbidity due to unresolved symptoms. Once a patient has had a cholecystectomy, symptoms are presumed to be due to a nonbiliary etiology and an extensive, often repetitive, workup is pursued before “repeat cholecystectomy” is considered.5
Case Presentation
A 63-year-old man was referred to gastroenterology for recurrent episodic right upper quadrant pain. He reported intermittent both right and left upper abdominal pain that was variable in quality. At times it was associated with an empty stomach prior to meals; at other times, onset was 30 to 60 minutes after meals. The patient also reported significant flatulence and bloating and intermittent loose stools. Sixteen years before, he underwent a laparoscopic cholecystectomy. He reported that the pain he experienced before the cholecystectomy never resolved after surgery but occurred less frequently. For the next 16 years, the patient did not seek evaluation of his ongoing but infrequent symptoms until his pain became a daily occurrence. The patient’s surgical history included a remote open vagotomy and antrectomy for peptic ulcer disease, laparoscopic appendectomy, and a laparoscopic cholecystectomy for reported biliary colic.
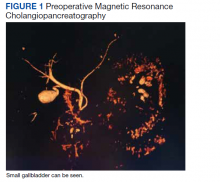
The gastroenterology evaluation included a colonoscopy and esophagogastroduodenoscopy (EGD); both were benign and without findings specific to identify the etiology for the patient’s pain. The patient was given a course of rifaximin 1200 mg daily for 7 days for possible bacterial overgrowth and placed on a proton pump inhibitor twice daily. Neither of these interventions helped resolve the patient’s symptoms. Further workup was pursued by gastroenterology to include a right upper quadrant ultrasound that showed a structure most consistent with a small gallbladder containing a small polyp vs stone. Magnetic resonance cholangiopancreatography (MRCP) also was performed and showed the presence of a small gallbladder with a small 2-mm filling defect and an otherwise benign biliary tree. MRCP images and EGD documented a Billroth 1 reconstruction at the time of his remote antrectomy and vagotomy (Figure 1).
The patient was referred to general surgery for consideration of a repeat cholecystectomy. He confirmed the history of intermittent upper abdominal pain for the past 16 years, which was similar to the symptoms he had experienced before his original laparoscopic cholecystectomy. On examination, the patient had a body mass index of 38, had a large upper midline incision from his prior antrectomy and vagotomy procedure, and several scars presumed to be port incision scars to the right lateral abdominal wall. Hospital records were obtained from the patient’s prior workup for biliary colic and cholecystectomy 16 years before. The preoperative abdominal ultrasound examination showed a mildly distended gallbladder but was notably described as “quite limited due to patient’s body habitus and liver is not well seen.” No additional imaging was documented in his presurgical evaluation notes and imaging records.
The operative report described a gallbladder that was densely adherent to adjacent fat and omental tissue with significant adhesions secondary to the prior vagotomy and antrectomy procedure. The cystic duct and artery were dissected free at the level of their junction with the gallbladder infundibulum. The cystic artery was divided with a harmonic scalpel. Following this the gallbladder body was dissected free from the liver bed in top-down fashion. A 0 Vicryl Endoloop suture was placed over the gallbladder and secured just past the origin of the cystic duct on the gallbladder infundibulum and the cystic duct divided above this suture. No surgical clips were used, which corresponded with the lack of surgical clips seen in imaging in his recent gastroenterology workup. No documentation of an intraoperative cholangiogram existed or was considered in the operative report.
The pathology report from this first cholecystectomy procedure noted the removed specimen to be an unopened 6-cm gallbladder containing 2 small yellow stones that otherwise were benign. At the time of this patient’s re-presentation to general surgery, there was suspicion that the patient’s prior surgical procedure had not been a cholecystectomy but rather a subtotal cholecystectomy. However, after appropriate workup and review of prior records, the patient had, indeed, previously undergone cholecystectomy and represented a rare case of gallbladder duplication resulting in abdominal pain for 16 years after his index operation.
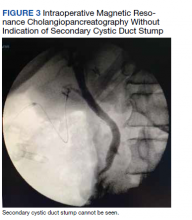
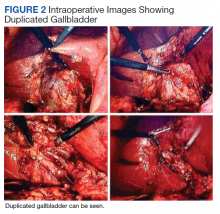
The patient was consented for repeat cholecystectomy and underwent a laparoscopic lysis of adhesions, cholecystectomy, and intraoperative cholangiogram. Significant scarring was found at the liver undersurface that would have been exposed during the original laparoscopic resection of the gallbladder from its liver bed. Deeper to this, a small saccular structure was identified as the duplicate gallbladder (Figure 2). Though the visualized gallbladder was small with a deep intrahepatic lie, the critical view of safety was achieved and was without additional variation. An intraoperative cholangiogram was performed to determine whether residual ductal stumps or other additional evidence of the previously removed gallbladder could be identified. The cholangiogram showed clear visualization of the cystic duct, common bile duct, right and left hepatic ducts, and contrast into the duodenum without abnormal variants. There was no visualized accessory or secondary cystic duct stump seen on the cholangiogram (Figure 3). Pathology of the repeat cholecystectomy specimen confirmed a 3-cm gallbladder with a distinct duct leading out of the gallbladder and the presence of several gallstones. The patient had an uneventful recovery after the repeat laparoscopic cholecystectomy with complete resolution of his upper abdominal pain.
Discussion
The first reported human case of gallbladder duplication was noted in a sacrificial victim of Emperor Augustus in 31 BCE. Sherren reported the first documented case of double accessory gallbladder in a living human in 1911.1,6 Though the exact incidence of gallbladder duplication is not fully known due to primary documentation from case reports, incidence is approximately 1 in 4000 to 5000 people. It was first formally classified by Boyden in 1926.7 Further anatomic classification based on morphology and embryogenesis was delineated by Harlaftis and colleagues in 1977, establishing type 1 and 2 structures of a duplicated gallbladder.8 Type 1 duplicated gallbladder anatomy shares a single cystic duct, whereas in type 2 each gallbladder has its own cystic duct. Later reports and studies identified triple gallbladders as well as trabecular variants with the most common classification used currently being the modified Harlaftis classification.9,10
The case presented here most likely represents either a Y-shaped type 1 primordial gallbladder or a type 2 accessory gallbladder based on historical data and intraoperative cholangiogram findings at the time of repeat cholecystectomy. Gallbladder duplication is clinically indistinguishable from regular gallbladder pathology preoperatively and can only be identified on imaging or intraoperatively.11 Prior case reports and studies have found that it is frequently missed on preoperative abdominal ultrasonography and CT in up to 50% of cases.12-14
The differential diagnosis of gallbladder duplication seen on preoperative imaging includes a gallbladder diverticulum, choledochal cyst, focal adenonomyomatosis, Phrygian cap, or folded gallbladder.1,2 Historically, the most definitive test for gallbladder duplication has been either intraoperative cholangiography, which can also clarify biliary anatomy, or endoscopic retrograde cholangiopancreatography with cholangiography.1,3 The debate over routine use of intraoperative cholangiography has been ongoing for the past several decades.15 Though intraoperative cholangiogram remains one of the most definitive tests for gallbladder duplication, given the overall low incidence of this variant, recommendation for routine intraoperative cholangiography solely to rule out gallbladder duplication cannot be definitively recommended based on our review of the literature. Currently, preoperative MRCP is the study of choice when there is concern from historical facts or from other imaging of gallbladder duplication as it is noninvasive and has a high degree of detail, particularly with 3D reconstructions.14,16 At the time of surgery, the most critical step to avoid inadvertent ductal injury is clear visualization of ductal anatomy and obtaining the critical view of safety.17 Though this will also assist in identifying some cases of gallbladder duplication, given the great variation of duplication, it will not prevent missing some variants. In our case, extensive local scarring from the patient’s prior antrectomy and vagotomy along with lack of the use of intraoperative cholangiography likely contributed to missing his duplication at the time of his index cholecystectomy.
Undiagnosed gallbladder duplication can lead to additional morbidity related to common entities associated with gallbladder pathology, such as biliary colic, cholecystitis, cholangitis, and pancreatitis. Additionally, case reports in the literature have documented more rare associations, such as empyema, carcinoma, cholecystoenteric fistula, and torsion, all associated with a duplicated gallbladder.18-21 Once identified pre- or intraoperatively, it is generally recommended that all gallbladders be removed in symptomatic patients and that intraoperative cholangiography be done to assure complete resection of the duplicated gallbladders and to avoid injury to the biliary trees.22-25
Conclusions
Gallbladder duplication and other congenital biliary anatomic variations should be considered before a biliary operation and included in the differential diagnosis when evaluating patients who have clinical symptoms consistent with biliary pathology. In addition, intraoperative cholangiogram should be performed during cholecystectomy if the inferior liver edge cannot be visualized well, as in the case of this patient where a prior foregut operation resulted in extensive adhesive disease. Intraoperative cholangiogram also should be considered in patients whose preoperative imaging does not visualize the right upper quadrant well due to patient habitus. Doing so may identify gallbladder duplication and allow for complete cholecystectomy as well as proper identification and management of cystic duct variants. Awareness and consideration of duplicated biliary variants can help prevent intraoperative complications related to biliary anomalies and avoid the morbidity related to recurrent biliary disease and the need for repeat operative procedures.
Acknowledgments
We extend our thanks to Veterans Affairs Puget Sound Healthcare System and the Departments of Surgery and Radiology for their support of this case report, and Lorrie Langdale, MD, and Roger Tatum, MD, for their mentorship of this project
1. Vezakis A, Pantiora E, Giannoulopoulos D, et al. A duplicated gallbladder in a patient presenting with acute cholangitis. A case study and a literature review. Ann Hepatol. 2019;18(1):240-245. doi:10.5604/01.3001.0012.7932
2. Barut Í, Tarhan ÖR, Dog^ru U, Bülbül M. Gallbladder duplication: diagnosed and treated by laparoscopy. Eur J Gen Med. 2006;3(3):142-145. doi:10.29333/ejgm/82396 3. Cozacov Y, Subhas G, Jacobs M, Parikh J. Total laparoscopic removal of accessory gallbladder: a case report and review of literature. World J Gastrointest Surg. 2015;7(12):398-402. doi:10.4240/wjgs.v7.i12.398
4. Musleh MG, Burnett H, Rajashanker B, Ammori BJ. Laparoscopic double cholecystectomy for duplicated gallbladder: a case report. Int J Surg Case Rep. 2017;41:502-504. Published 2017 Nov 27. doi:10.1016/j.ijscr.2017.11.046
5. Walbolt TD, Lalezarzadeh F. Laparoscopic management of a duplicated gallbladder: a case study and anatomic history. Surg Laparosc Endosc Percutan Tech. 2011;21(3):e156-e158. doi:10.1097/SLE.0b013e31821d47ce
6. Sherren J. A double gall-bladder removed by operation. Ann Surg. 1911;54(2):204-205. doi:10.1097/00000658-191108000-00009
7. Boyden EA. The accessory gall-bladder—an embryological and comparative study of aberrant biliary vesicles occurring in man and the domestic mammals. Am J Anat. 1926; 38(2):177-231. doi:10.1002/aja.1000380202
8. Harlaftis N, Gray SW, Skandalakis JE. Multiple gallbladders. Surg Gynecol Obstet. 1977;145(6):928-934.
9. Kim RD, Zendejas I, Velopulos C, et al. Duplicate gallbladder arising from the left hepatic duct: report of a case. Surg Today. 2009;39(6):536-539. doi:10.1007/s00595-008-3878-4
10. Causey MW, Miller S, Fernelius CA, Burgess JR, Brown TA, Newton C. Gallbladder duplication: evaluation, treatment, and classification. J Pediatr Surg. 2010;45(2):443-446. doi:10.1016/j.jpedsurg.2009.12.015
11. Apolo Romero EX, Gálvez Salazar PF, Estrada Chandi JA, et al. Gallbladder duplication and cholecystitis. J Surg Case Rep. 2018;2018(7):rjy158. Published 2018 Jul 3. doi:10.1093/jscr/rjy158
12. Gorecki PJ, Andrei VE, Musacchio T, Schein M. Double gallbladder originating from left hepatic duct: a case report and review of literature. JSLS. 1998;2(4):337-339.
13. Cueto García J, Weber A, Serrano Berry F, Tanur Tatz B. Double gallbladder treated successfully by laparoscopy. J Laparoendosc Surg. 1993;3(2):153-155. doi:10.1089/lps.1993.3.153
14. Fazio V, Damiano G, Palumbo VD, et al. An unexpected surprise at the end of a “quiet” cholecystectomy. A case report and review of the literature. Ann Ital Chir. 2012;83(3):265-267.
15. Flum DR, Dellinger EP, Cheadle A, Chan L, Koepsell T. Intraoperative cholangiography and risk of common bile duct injury during cholecystectomy. JAMA. 2003;289(13):1639-1644. doi:10.1001/jama.289.13.1639
16. Botsford A, McKay K, Hartery A, Hapgood C. MRCP imaging of duplicate gallbladder: a case report and review of the literature. Surg Radiol Anat. 2015;37(5):425-429. doi:10.1007/s00276-015-1456-1
17. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180(1):101-125.
18. Raymond SW, Thrift CB. Carcinoma of a duplicated gall bladder. Ill Med J. 1956;110(5):239-240.
19. Cunningham JJ. Empyema of a duplicated gallbladder: echographic findings. J Clin Ultrasound. 1980;8(6):511-512. doi:10.1002/jcu.1870080612
20. Recht W. Torsion of a double gallbladder; a report of a case and a review of the literature. Br J Surg. 1952;39(156):342-344. doi:10.1002/bjs.18003915616
21. Ritchie AW, Crucioli V. Double gallbladder with cholecystocolic fistula: a case report. Br J Surg. 1980;67(2):145-146. doi:10.1002/bjs.1800670226
22. Shapiro T, Rennie W. Duplicate gallbladder cholecystitis after open cholecystectomy. Ann Emerg Med. 1999;33(5):584-587. doi:10.1016/s0196-0644(99)70348-3
23. Hobbs MS, Mai Q, Knuiman MW, Fletcher DR, Ridout SC. Surgeon experience and trends in intraoperative complications in laparoscopic cholecystectomy. Br J Surg. 2006;93(7):844-853. doi:10.1002/bjs.5333
24. Davidoff AM, Pappas TN, Murray EA, et al. Mechanisms of major biliary injury during laparoscopic cholecystectomy. Ann Surg. 1992;215(3):196-202. doi:10.1097/00000658-199203000-00002
25. Flowers JL, Zucker KA, Graham SM, Scovill WA, Imbembo AL, Bailey RW. Laparoscopic cholangiography. Results and indications. Ann Surg. 1992;215(3):209-216. doi:10.1097/00000658-199203000-00004
Gallbladder duplication is a congenital abnormality of the hepatobiliary system and often is not considered in the evaluation of a patient with right upper quadrant pain. Accuracy of the most commonly used imaging study to assess for biliary disease, abdominal ultrasound, is highly dependent on the skills of the ultrasonographer, and given its relative rarity, this condition is often not considered prior to planned cholecystectomy.1 Small case reviews found that < 50% of gallbladder duplications are diagnosed preoperatively despite use of ultrasound or computed tomography (CT) scan.2-4 Failure to recognize duplicate gallbladder anatomy in symptomatic patients may result in incomplete surgical management, an increase in perioperative complications, and years of morbidity due to unresolved symptoms. Once a patient has had a cholecystectomy, symptoms are presumed to be due to a nonbiliary etiology and an extensive, often repetitive, workup is pursued before “repeat cholecystectomy” is considered.5
Case Presentation
A 63-year-old man was referred to gastroenterology for recurrent episodic right upper quadrant pain. He reported intermittent both right and left upper abdominal pain that was variable in quality. At times it was associated with an empty stomach prior to meals; at other times, onset was 30 to 60 minutes after meals. The patient also reported significant flatulence and bloating and intermittent loose stools. Sixteen years before, he underwent a laparoscopic cholecystectomy. He reported that the pain he experienced before the cholecystectomy never resolved after surgery but occurred less frequently. For the next 16 years, the patient did not seek evaluation of his ongoing but infrequent symptoms until his pain became a daily occurrence. The patient’s surgical history included a remote open vagotomy and antrectomy for peptic ulcer disease, laparoscopic appendectomy, and a laparoscopic cholecystectomy for reported biliary colic.
The gastroenterology evaluation included a colonoscopy and esophagogastroduodenoscopy (EGD); both were benign and without findings specific to identify the etiology for the patient’s pain. The patient was given a course of rifaximin 1200 mg daily for 7 days for possible bacterial overgrowth and placed on a proton pump inhibitor twice daily. Neither of these interventions helped resolve the patient’s symptoms. Further workup was pursued by gastroenterology to include a right upper quadrant ultrasound that showed a structure most consistent with a small gallbladder containing a small polyp vs stone. Magnetic resonance cholangiopancreatography (MRCP) also was performed and showed the presence of a small gallbladder with a small 2-mm filling defect and an otherwise benign biliary tree. MRCP images and EGD documented a Billroth 1 reconstruction at the time of his remote antrectomy and vagotomy (Figure 1).
The patient was referred to general surgery for consideration of a repeat cholecystectomy. He confirmed the history of intermittent upper abdominal pain for the past 16 years, which was similar to the symptoms he had experienced before his original laparoscopic cholecystectomy. On examination, the patient had a body mass index of 38, had a large upper midline incision from his prior antrectomy and vagotomy procedure, and several scars presumed to be port incision scars to the right lateral abdominal wall. Hospital records were obtained from the patient’s prior workup for biliary colic and cholecystectomy 16 years before. The preoperative abdominal ultrasound examination showed a mildly distended gallbladder but was notably described as “quite limited due to patient’s body habitus and liver is not well seen.” No additional imaging was documented in his presurgical evaluation notes and imaging records.
The operative report described a gallbladder that was densely adherent to adjacent fat and omental tissue with significant adhesions secondary to the prior vagotomy and antrectomy procedure. The cystic duct and artery were dissected free at the level of their junction with the gallbladder infundibulum. The cystic artery was divided with a harmonic scalpel. Following this the gallbladder body was dissected free from the liver bed in top-down fashion. A 0 Vicryl Endoloop suture was placed over the gallbladder and secured just past the origin of the cystic duct on the gallbladder infundibulum and the cystic duct divided above this suture. No surgical clips were used, which corresponded with the lack of surgical clips seen in imaging in his recent gastroenterology workup. No documentation of an intraoperative cholangiogram existed or was considered in the operative report.
The pathology report from this first cholecystectomy procedure noted the removed specimen to be an unopened 6-cm gallbladder containing 2 small yellow stones that otherwise were benign. At the time of this patient’s re-presentation to general surgery, there was suspicion that the patient’s prior surgical procedure had not been a cholecystectomy but rather a subtotal cholecystectomy. However, after appropriate workup and review of prior records, the patient had, indeed, previously undergone cholecystectomy and represented a rare case of gallbladder duplication resulting in abdominal pain for 16 years after his index operation.
The patient was consented for repeat cholecystectomy and underwent a laparoscopic lysis of adhesions, cholecystectomy, and intraoperative cholangiogram. Significant scarring was found at the liver undersurface that would have been exposed during the original laparoscopic resection of the gallbladder from its liver bed. Deeper to this, a small saccular structure was identified as the duplicate gallbladder (Figure 2). Though the visualized gallbladder was small with a deep intrahepatic lie, the critical view of safety was achieved and was without additional variation. An intraoperative cholangiogram was performed to determine whether residual ductal stumps or other additional evidence of the previously removed gallbladder could be identified. The cholangiogram showed clear visualization of the cystic duct, common bile duct, right and left hepatic ducts, and contrast into the duodenum without abnormal variants. There was no visualized accessory or secondary cystic duct stump seen on the cholangiogram (Figure 3). Pathology of the repeat cholecystectomy specimen confirmed a 3-cm gallbladder with a distinct duct leading out of the gallbladder and the presence of several gallstones. The patient had an uneventful recovery after the repeat laparoscopic cholecystectomy with complete resolution of his upper abdominal pain.
Discussion
The first reported human case of gallbladder duplication was noted in a sacrificial victim of Emperor Augustus in 31 BCE. Sherren reported the first documented case of double accessory gallbladder in a living human in 1911.1,6 Though the exact incidence of gallbladder duplication is not fully known due to primary documentation from case reports, incidence is approximately 1 in 4000 to 5000 people. It was first formally classified by Boyden in 1926.7 Further anatomic classification based on morphology and embryogenesis was delineated by Harlaftis and colleagues in 1977, establishing type 1 and 2 structures of a duplicated gallbladder.8 Type 1 duplicated gallbladder anatomy shares a single cystic duct, whereas in type 2 each gallbladder has its own cystic duct. Later reports and studies identified triple gallbladders as well as trabecular variants with the most common classification used currently being the modified Harlaftis classification.9,10
The case presented here most likely represents either a Y-shaped type 1 primordial gallbladder or a type 2 accessory gallbladder based on historical data and intraoperative cholangiogram findings at the time of repeat cholecystectomy. Gallbladder duplication is clinically indistinguishable from regular gallbladder pathology preoperatively and can only be identified on imaging or intraoperatively.11 Prior case reports and studies have found that it is frequently missed on preoperative abdominal ultrasonography and CT in up to 50% of cases.12-14
The differential diagnosis of gallbladder duplication seen on preoperative imaging includes a gallbladder diverticulum, choledochal cyst, focal adenonomyomatosis, Phrygian cap, or folded gallbladder.1,2 Historically, the most definitive test for gallbladder duplication has been either intraoperative cholangiography, which can also clarify biliary anatomy, or endoscopic retrograde cholangiopancreatography with cholangiography.1,3 The debate over routine use of intraoperative cholangiography has been ongoing for the past several decades.15 Though intraoperative cholangiogram remains one of the most definitive tests for gallbladder duplication, given the overall low incidence of this variant, recommendation for routine intraoperative cholangiography solely to rule out gallbladder duplication cannot be definitively recommended based on our review of the literature. Currently, preoperative MRCP is the study of choice when there is concern from historical facts or from other imaging of gallbladder duplication as it is noninvasive and has a high degree of detail, particularly with 3D reconstructions.14,16 At the time of surgery, the most critical step to avoid inadvertent ductal injury is clear visualization of ductal anatomy and obtaining the critical view of safety.17 Though this will also assist in identifying some cases of gallbladder duplication, given the great variation of duplication, it will not prevent missing some variants. In our case, extensive local scarring from the patient’s prior antrectomy and vagotomy along with lack of the use of intraoperative cholangiography likely contributed to missing his duplication at the time of his index cholecystectomy.
Undiagnosed gallbladder duplication can lead to additional morbidity related to common entities associated with gallbladder pathology, such as biliary colic, cholecystitis, cholangitis, and pancreatitis. Additionally, case reports in the literature have documented more rare associations, such as empyema, carcinoma, cholecystoenteric fistula, and torsion, all associated with a duplicated gallbladder.18-21 Once identified pre- or intraoperatively, it is generally recommended that all gallbladders be removed in symptomatic patients and that intraoperative cholangiography be done to assure complete resection of the duplicated gallbladders and to avoid injury to the biliary trees.22-25
Conclusions
Gallbladder duplication and other congenital biliary anatomic variations should be considered before a biliary operation and included in the differential diagnosis when evaluating patients who have clinical symptoms consistent with biliary pathology. In addition, intraoperative cholangiogram should be performed during cholecystectomy if the inferior liver edge cannot be visualized well, as in the case of this patient where a prior foregut operation resulted in extensive adhesive disease. Intraoperative cholangiogram also should be considered in patients whose preoperative imaging does not visualize the right upper quadrant well due to patient habitus. Doing so may identify gallbladder duplication and allow for complete cholecystectomy as well as proper identification and management of cystic duct variants. Awareness and consideration of duplicated biliary variants can help prevent intraoperative complications related to biliary anomalies and avoid the morbidity related to recurrent biliary disease and the need for repeat operative procedures.
Acknowledgments
We extend our thanks to Veterans Affairs Puget Sound Healthcare System and the Departments of Surgery and Radiology for their support of this case report, and Lorrie Langdale, MD, and Roger Tatum, MD, for their mentorship of this project
Gallbladder duplication is a congenital abnormality of the hepatobiliary system and often is not considered in the evaluation of a patient with right upper quadrant pain. Accuracy of the most commonly used imaging study to assess for biliary disease, abdominal ultrasound, is highly dependent on the skills of the ultrasonographer, and given its relative rarity, this condition is often not considered prior to planned cholecystectomy.1 Small case reviews found that < 50% of gallbladder duplications are diagnosed preoperatively despite use of ultrasound or computed tomography (CT) scan.2-4 Failure to recognize duplicate gallbladder anatomy in symptomatic patients may result in incomplete surgical management, an increase in perioperative complications, and years of morbidity due to unresolved symptoms. Once a patient has had a cholecystectomy, symptoms are presumed to be due to a nonbiliary etiology and an extensive, often repetitive, workup is pursued before “repeat cholecystectomy” is considered.5
Case Presentation
A 63-year-old man was referred to gastroenterology for recurrent episodic right upper quadrant pain. He reported intermittent both right and left upper abdominal pain that was variable in quality. At times it was associated with an empty stomach prior to meals; at other times, onset was 30 to 60 minutes after meals. The patient also reported significant flatulence and bloating and intermittent loose stools. Sixteen years before, he underwent a laparoscopic cholecystectomy. He reported that the pain he experienced before the cholecystectomy never resolved after surgery but occurred less frequently. For the next 16 years, the patient did not seek evaluation of his ongoing but infrequent symptoms until his pain became a daily occurrence. The patient’s surgical history included a remote open vagotomy and antrectomy for peptic ulcer disease, laparoscopic appendectomy, and a laparoscopic cholecystectomy for reported biliary colic.
The gastroenterology evaluation included a colonoscopy and esophagogastroduodenoscopy (EGD); both were benign and without findings specific to identify the etiology for the patient’s pain. The patient was given a course of rifaximin 1200 mg daily for 7 days for possible bacterial overgrowth and placed on a proton pump inhibitor twice daily. Neither of these interventions helped resolve the patient’s symptoms. Further workup was pursued by gastroenterology to include a right upper quadrant ultrasound that showed a structure most consistent with a small gallbladder containing a small polyp vs stone. Magnetic resonance cholangiopancreatography (MRCP) also was performed and showed the presence of a small gallbladder with a small 2-mm filling defect and an otherwise benign biliary tree. MRCP images and EGD documented a Billroth 1 reconstruction at the time of his remote antrectomy and vagotomy (Figure 1).
The patient was referred to general surgery for consideration of a repeat cholecystectomy. He confirmed the history of intermittent upper abdominal pain for the past 16 years, which was similar to the symptoms he had experienced before his original laparoscopic cholecystectomy. On examination, the patient had a body mass index of 38, had a large upper midline incision from his prior antrectomy and vagotomy procedure, and several scars presumed to be port incision scars to the right lateral abdominal wall. Hospital records were obtained from the patient’s prior workup for biliary colic and cholecystectomy 16 years before. The preoperative abdominal ultrasound examination showed a mildly distended gallbladder but was notably described as “quite limited due to patient’s body habitus and liver is not well seen.” No additional imaging was documented in his presurgical evaluation notes and imaging records.
The operative report described a gallbladder that was densely adherent to adjacent fat and omental tissue with significant adhesions secondary to the prior vagotomy and antrectomy procedure. The cystic duct and artery were dissected free at the level of their junction with the gallbladder infundibulum. The cystic artery was divided with a harmonic scalpel. Following this the gallbladder body was dissected free from the liver bed in top-down fashion. A 0 Vicryl Endoloop suture was placed over the gallbladder and secured just past the origin of the cystic duct on the gallbladder infundibulum and the cystic duct divided above this suture. No surgical clips were used, which corresponded with the lack of surgical clips seen in imaging in his recent gastroenterology workup. No documentation of an intraoperative cholangiogram existed or was considered in the operative report.
The pathology report from this first cholecystectomy procedure noted the removed specimen to be an unopened 6-cm gallbladder containing 2 small yellow stones that otherwise were benign. At the time of this patient’s re-presentation to general surgery, there was suspicion that the patient’s prior surgical procedure had not been a cholecystectomy but rather a subtotal cholecystectomy. However, after appropriate workup and review of prior records, the patient had, indeed, previously undergone cholecystectomy and represented a rare case of gallbladder duplication resulting in abdominal pain for 16 years after his index operation.
The patient was consented for repeat cholecystectomy and underwent a laparoscopic lysis of adhesions, cholecystectomy, and intraoperative cholangiogram. Significant scarring was found at the liver undersurface that would have been exposed during the original laparoscopic resection of the gallbladder from its liver bed. Deeper to this, a small saccular structure was identified as the duplicate gallbladder (Figure 2). Though the visualized gallbladder was small with a deep intrahepatic lie, the critical view of safety was achieved and was without additional variation. An intraoperative cholangiogram was performed to determine whether residual ductal stumps or other additional evidence of the previously removed gallbladder could be identified. The cholangiogram showed clear visualization of the cystic duct, common bile duct, right and left hepatic ducts, and contrast into the duodenum without abnormal variants. There was no visualized accessory or secondary cystic duct stump seen on the cholangiogram (Figure 3). Pathology of the repeat cholecystectomy specimen confirmed a 3-cm gallbladder with a distinct duct leading out of the gallbladder and the presence of several gallstones. The patient had an uneventful recovery after the repeat laparoscopic cholecystectomy with complete resolution of his upper abdominal pain.
Discussion
The first reported human case of gallbladder duplication was noted in a sacrificial victim of Emperor Augustus in 31 BCE. Sherren reported the first documented case of double accessory gallbladder in a living human in 1911.1,6 Though the exact incidence of gallbladder duplication is not fully known due to primary documentation from case reports, incidence is approximately 1 in 4000 to 5000 people. It was first formally classified by Boyden in 1926.7 Further anatomic classification based on morphology and embryogenesis was delineated by Harlaftis and colleagues in 1977, establishing type 1 and 2 structures of a duplicated gallbladder.8 Type 1 duplicated gallbladder anatomy shares a single cystic duct, whereas in type 2 each gallbladder has its own cystic duct. Later reports and studies identified triple gallbladders as well as trabecular variants with the most common classification used currently being the modified Harlaftis classification.9,10
The case presented here most likely represents either a Y-shaped type 1 primordial gallbladder or a type 2 accessory gallbladder based on historical data and intraoperative cholangiogram findings at the time of repeat cholecystectomy. Gallbladder duplication is clinically indistinguishable from regular gallbladder pathology preoperatively and can only be identified on imaging or intraoperatively.11 Prior case reports and studies have found that it is frequently missed on preoperative abdominal ultrasonography and CT in up to 50% of cases.12-14
The differential diagnosis of gallbladder duplication seen on preoperative imaging includes a gallbladder diverticulum, choledochal cyst, focal adenonomyomatosis, Phrygian cap, or folded gallbladder.1,2 Historically, the most definitive test for gallbladder duplication has been either intraoperative cholangiography, which can also clarify biliary anatomy, or endoscopic retrograde cholangiopancreatography with cholangiography.1,3 The debate over routine use of intraoperative cholangiography has been ongoing for the past several decades.15 Though intraoperative cholangiogram remains one of the most definitive tests for gallbladder duplication, given the overall low incidence of this variant, recommendation for routine intraoperative cholangiography solely to rule out gallbladder duplication cannot be definitively recommended based on our review of the literature. Currently, preoperative MRCP is the study of choice when there is concern from historical facts or from other imaging of gallbladder duplication as it is noninvasive and has a high degree of detail, particularly with 3D reconstructions.14,16 At the time of surgery, the most critical step to avoid inadvertent ductal injury is clear visualization of ductal anatomy and obtaining the critical view of safety.17 Though this will also assist in identifying some cases of gallbladder duplication, given the great variation of duplication, it will not prevent missing some variants. In our case, extensive local scarring from the patient’s prior antrectomy and vagotomy along with lack of the use of intraoperative cholangiography likely contributed to missing his duplication at the time of his index cholecystectomy.
Undiagnosed gallbladder duplication can lead to additional morbidity related to common entities associated with gallbladder pathology, such as biliary colic, cholecystitis, cholangitis, and pancreatitis. Additionally, case reports in the literature have documented more rare associations, such as empyema, carcinoma, cholecystoenteric fistula, and torsion, all associated with a duplicated gallbladder.18-21 Once identified pre- or intraoperatively, it is generally recommended that all gallbladders be removed in symptomatic patients and that intraoperative cholangiography be done to assure complete resection of the duplicated gallbladders and to avoid injury to the biliary trees.22-25
Conclusions
Gallbladder duplication and other congenital biliary anatomic variations should be considered before a biliary operation and included in the differential diagnosis when evaluating patients who have clinical symptoms consistent with biliary pathology. In addition, intraoperative cholangiogram should be performed during cholecystectomy if the inferior liver edge cannot be visualized well, as in the case of this patient where a prior foregut operation resulted in extensive adhesive disease. Intraoperative cholangiogram also should be considered in patients whose preoperative imaging does not visualize the right upper quadrant well due to patient habitus. Doing so may identify gallbladder duplication and allow for complete cholecystectomy as well as proper identification and management of cystic duct variants. Awareness and consideration of duplicated biliary variants can help prevent intraoperative complications related to biliary anomalies and avoid the morbidity related to recurrent biliary disease and the need for repeat operative procedures.
Acknowledgments
We extend our thanks to Veterans Affairs Puget Sound Healthcare System and the Departments of Surgery and Radiology for their support of this case report, and Lorrie Langdale, MD, and Roger Tatum, MD, for their mentorship of this project
1. Vezakis A, Pantiora E, Giannoulopoulos D, et al. A duplicated gallbladder in a patient presenting with acute cholangitis. A case study and a literature review. Ann Hepatol. 2019;18(1):240-245. doi:10.5604/01.3001.0012.7932
2. Barut Í, Tarhan ÖR, Dog^ru U, Bülbül M. Gallbladder duplication: diagnosed and treated by laparoscopy. Eur J Gen Med. 2006;3(3):142-145. doi:10.29333/ejgm/82396 3. Cozacov Y, Subhas G, Jacobs M, Parikh J. Total laparoscopic removal of accessory gallbladder: a case report and review of literature. World J Gastrointest Surg. 2015;7(12):398-402. doi:10.4240/wjgs.v7.i12.398
4. Musleh MG, Burnett H, Rajashanker B, Ammori BJ. Laparoscopic double cholecystectomy for duplicated gallbladder: a case report. Int J Surg Case Rep. 2017;41:502-504. Published 2017 Nov 27. doi:10.1016/j.ijscr.2017.11.046
5. Walbolt TD, Lalezarzadeh F. Laparoscopic management of a duplicated gallbladder: a case study and anatomic history. Surg Laparosc Endosc Percutan Tech. 2011;21(3):e156-e158. doi:10.1097/SLE.0b013e31821d47ce
6. Sherren J. A double gall-bladder removed by operation. Ann Surg. 1911;54(2):204-205. doi:10.1097/00000658-191108000-00009
7. Boyden EA. The accessory gall-bladder—an embryological and comparative study of aberrant biliary vesicles occurring in man and the domestic mammals. Am J Anat. 1926; 38(2):177-231. doi:10.1002/aja.1000380202
8. Harlaftis N, Gray SW, Skandalakis JE. Multiple gallbladders. Surg Gynecol Obstet. 1977;145(6):928-934.
9. Kim RD, Zendejas I, Velopulos C, et al. Duplicate gallbladder arising from the left hepatic duct: report of a case. Surg Today. 2009;39(6):536-539. doi:10.1007/s00595-008-3878-4
10. Causey MW, Miller S, Fernelius CA, Burgess JR, Brown TA, Newton C. Gallbladder duplication: evaluation, treatment, and classification. J Pediatr Surg. 2010;45(2):443-446. doi:10.1016/j.jpedsurg.2009.12.015
11. Apolo Romero EX, Gálvez Salazar PF, Estrada Chandi JA, et al. Gallbladder duplication and cholecystitis. J Surg Case Rep. 2018;2018(7):rjy158. Published 2018 Jul 3. doi:10.1093/jscr/rjy158
12. Gorecki PJ, Andrei VE, Musacchio T, Schein M. Double gallbladder originating from left hepatic duct: a case report and review of literature. JSLS. 1998;2(4):337-339.
13. Cueto García J, Weber A, Serrano Berry F, Tanur Tatz B. Double gallbladder treated successfully by laparoscopy. J Laparoendosc Surg. 1993;3(2):153-155. doi:10.1089/lps.1993.3.153
14. Fazio V, Damiano G, Palumbo VD, et al. An unexpected surprise at the end of a “quiet” cholecystectomy. A case report and review of the literature. Ann Ital Chir. 2012;83(3):265-267.
15. Flum DR, Dellinger EP, Cheadle A, Chan L, Koepsell T. Intraoperative cholangiography and risk of common bile duct injury during cholecystectomy. JAMA. 2003;289(13):1639-1644. doi:10.1001/jama.289.13.1639
16. Botsford A, McKay K, Hartery A, Hapgood C. MRCP imaging of duplicate gallbladder: a case report and review of the literature. Surg Radiol Anat. 2015;37(5):425-429. doi:10.1007/s00276-015-1456-1
17. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180(1):101-125.
18. Raymond SW, Thrift CB. Carcinoma of a duplicated gall bladder. Ill Med J. 1956;110(5):239-240.
19. Cunningham JJ. Empyema of a duplicated gallbladder: echographic findings. J Clin Ultrasound. 1980;8(6):511-512. doi:10.1002/jcu.1870080612
20. Recht W. Torsion of a double gallbladder; a report of a case and a review of the literature. Br J Surg. 1952;39(156):342-344. doi:10.1002/bjs.18003915616
21. Ritchie AW, Crucioli V. Double gallbladder with cholecystocolic fistula: a case report. Br J Surg. 1980;67(2):145-146. doi:10.1002/bjs.1800670226
22. Shapiro T, Rennie W. Duplicate gallbladder cholecystitis after open cholecystectomy. Ann Emerg Med. 1999;33(5):584-587. doi:10.1016/s0196-0644(99)70348-3
23. Hobbs MS, Mai Q, Knuiman MW, Fletcher DR, Ridout SC. Surgeon experience and trends in intraoperative complications in laparoscopic cholecystectomy. Br J Surg. 2006;93(7):844-853. doi:10.1002/bjs.5333
24. Davidoff AM, Pappas TN, Murray EA, et al. Mechanisms of major biliary injury during laparoscopic cholecystectomy. Ann Surg. 1992;215(3):196-202. doi:10.1097/00000658-199203000-00002
25. Flowers JL, Zucker KA, Graham SM, Scovill WA, Imbembo AL, Bailey RW. Laparoscopic cholangiography. Results and indications. Ann Surg. 1992;215(3):209-216. doi:10.1097/00000658-199203000-00004
1. Vezakis A, Pantiora E, Giannoulopoulos D, et al. A duplicated gallbladder in a patient presenting with acute cholangitis. A case study and a literature review. Ann Hepatol. 2019;18(1):240-245. doi:10.5604/01.3001.0012.7932
2. Barut Í, Tarhan ÖR, Dog^ru U, Bülbül M. Gallbladder duplication: diagnosed and treated by laparoscopy. Eur J Gen Med. 2006;3(3):142-145. doi:10.29333/ejgm/82396 3. Cozacov Y, Subhas G, Jacobs M, Parikh J. Total laparoscopic removal of accessory gallbladder: a case report and review of literature. World J Gastrointest Surg. 2015;7(12):398-402. doi:10.4240/wjgs.v7.i12.398
4. Musleh MG, Burnett H, Rajashanker B, Ammori BJ. Laparoscopic double cholecystectomy for duplicated gallbladder: a case report. Int J Surg Case Rep. 2017;41:502-504. Published 2017 Nov 27. doi:10.1016/j.ijscr.2017.11.046
5. Walbolt TD, Lalezarzadeh F. Laparoscopic management of a duplicated gallbladder: a case study and anatomic history. Surg Laparosc Endosc Percutan Tech. 2011;21(3):e156-e158. doi:10.1097/SLE.0b013e31821d47ce
6. Sherren J. A double gall-bladder removed by operation. Ann Surg. 1911;54(2):204-205. doi:10.1097/00000658-191108000-00009
7. Boyden EA. The accessory gall-bladder—an embryological and comparative study of aberrant biliary vesicles occurring in man and the domestic mammals. Am J Anat. 1926; 38(2):177-231. doi:10.1002/aja.1000380202
8. Harlaftis N, Gray SW, Skandalakis JE. Multiple gallbladders. Surg Gynecol Obstet. 1977;145(6):928-934.
9. Kim RD, Zendejas I, Velopulos C, et al. Duplicate gallbladder arising from the left hepatic duct: report of a case. Surg Today. 2009;39(6):536-539. doi:10.1007/s00595-008-3878-4
10. Causey MW, Miller S, Fernelius CA, Burgess JR, Brown TA, Newton C. Gallbladder duplication: evaluation, treatment, and classification. J Pediatr Surg. 2010;45(2):443-446. doi:10.1016/j.jpedsurg.2009.12.015
11. Apolo Romero EX, Gálvez Salazar PF, Estrada Chandi JA, et al. Gallbladder duplication and cholecystitis. J Surg Case Rep. 2018;2018(7):rjy158. Published 2018 Jul 3. doi:10.1093/jscr/rjy158
12. Gorecki PJ, Andrei VE, Musacchio T, Schein M. Double gallbladder originating from left hepatic duct: a case report and review of literature. JSLS. 1998;2(4):337-339.
13. Cueto García J, Weber A, Serrano Berry F, Tanur Tatz B. Double gallbladder treated successfully by laparoscopy. J Laparoendosc Surg. 1993;3(2):153-155. doi:10.1089/lps.1993.3.153
14. Fazio V, Damiano G, Palumbo VD, et al. An unexpected surprise at the end of a “quiet” cholecystectomy. A case report and review of the literature. Ann Ital Chir. 2012;83(3):265-267.
15. Flum DR, Dellinger EP, Cheadle A, Chan L, Koepsell T. Intraoperative cholangiography and risk of common bile duct injury during cholecystectomy. JAMA. 2003;289(13):1639-1644. doi:10.1001/jama.289.13.1639
16. Botsford A, McKay K, Hartery A, Hapgood C. MRCP imaging of duplicate gallbladder: a case report and review of the literature. Surg Radiol Anat. 2015;37(5):425-429. doi:10.1007/s00276-015-1456-1
17. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180(1):101-125.
18. Raymond SW, Thrift CB. Carcinoma of a duplicated gall bladder. Ill Med J. 1956;110(5):239-240.
19. Cunningham JJ. Empyema of a duplicated gallbladder: echographic findings. J Clin Ultrasound. 1980;8(6):511-512. doi:10.1002/jcu.1870080612
20. Recht W. Torsion of a double gallbladder; a report of a case and a review of the literature. Br J Surg. 1952;39(156):342-344. doi:10.1002/bjs.18003915616
21. Ritchie AW, Crucioli V. Double gallbladder with cholecystocolic fistula: a case report. Br J Surg. 1980;67(2):145-146. doi:10.1002/bjs.1800670226
22. Shapiro T, Rennie W. Duplicate gallbladder cholecystitis after open cholecystectomy. Ann Emerg Med. 1999;33(5):584-587. doi:10.1016/s0196-0644(99)70348-3
23. Hobbs MS, Mai Q, Knuiman MW, Fletcher DR, Ridout SC. Surgeon experience and trends in intraoperative complications in laparoscopic cholecystectomy. Br J Surg. 2006;93(7):844-853. doi:10.1002/bjs.5333
24. Davidoff AM, Pappas TN, Murray EA, et al. Mechanisms of major biliary injury during laparoscopic cholecystectomy. Ann Surg. 1992;215(3):196-202. doi:10.1097/00000658-199203000-00002
25. Flowers JL, Zucker KA, Graham SM, Scovill WA, Imbembo AL, Bailey RW. Laparoscopic cholangiography. Results and indications. Ann Surg. 1992;215(3):209-216. doi:10.1097/00000658-199203000-00004