User login
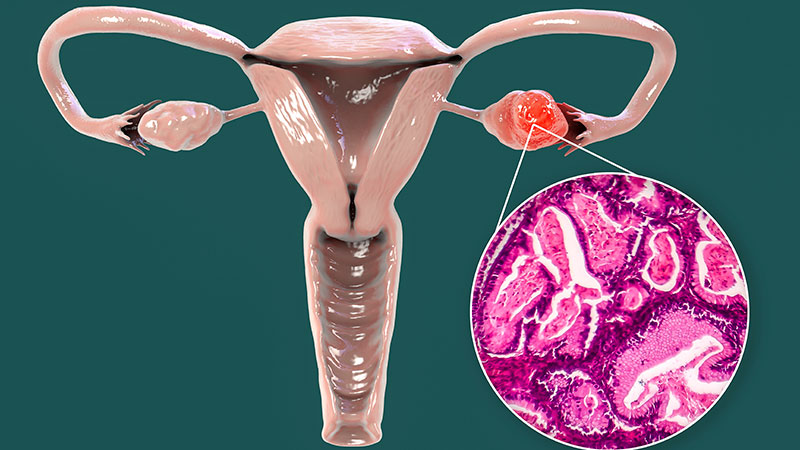
ASCO Updates Treatment Guidance for Newly Diagnosed, Advanced Ovarian Cancer
The American Society of Clinical Oncology (ASCO) has released updated guidelines for neoadjuvant chemotherapy in newly diagnosed advanced ovarian cancer, introducing changes in patient selection and treatment strategies. The changes reflect emerging evidence on racial disparities, treatment outcomes, and quality of life considerations.
The publication of the new guidance follows dramatic shifts in treatment patterns over the past decade.
“There had been a big shift in how we were treating patients in the United States,” explained Stephanie Gaillard, MD, PhD, one of the authors of the updated guidelines. “We saw a substantial drop in the number of patients undergoing primary cytoreductive surgery for ovarian cancer from about 70% of patients in 2010 to only about 37% in 2021.”
The new guidelines maintain the recommendation for platinum/taxane-based neoadjuvant chemotherapy but introduce modifications regarding timing and duration.
“It’s still a recommendation that gynecologic oncologists are involved in determining whether someone is eligible for primary cytoreductive surgery or should undergo neoadjuvant chemotherapy first,” Gaillard noted. “We emphasize that patients who are eligible for primary cytoreductive surgery should undergo surgery as opposed to receiving neoadjuvant chemotherapy.”
Alexander Melamed, MD, MPH, a gynecologic oncologist at Massachusetts General Hospital, Boston, who was not involved in authoring the updated guidelines, noted that additional evidence-based guidance is needed to individualize treatment plans. He pointed to four completed trials comparing neoadjuvant chemotherapy with cytoreductive surgery, noting: “When these trials have been pooled together in meta-analyses, there was a higher risk of mortality associated with primary cytoreductive surgery and a higher risk of severe complications.”
The updated guidelines take this higher risk for mortality with primary cytoreductive surgery into consideration, and patients who are not eligible for primary surgery would receive neoadjuvant chemotherapy, Gaillard noted.
Changes in Patient Selection
The 2025 guidelines describe a more nuanced approach for selecting patients for neoadjuvant chemotherapy vs primary cytoreductive surgery. While the 2016 ASCO guidelines primarily focused on disease burden and surgical resectability when selecting patients for neoadjuvant chemotherapy, the new recommendations incorporate additional factors.
The guidelines discuss recent findings showing that Black patients experience a 38% lower likelihood of undergoing cytoreductive surgery than non-Black patients. In addition, compared with non-Hispanic White women, Asian and Black women more frequently receive neoadjuvant chemotherapy with interval debulking surgery rather than primary cytoreductive surgery. According to the authors, these differences persist even after accounting for clinical factors, suggesting that structural barriers to healthcare access may play a role.
The guidelines discuss how affordability, availability, and accessibility mediate racial disparities in ovarian cancer care. According to the authors, structural inequities in healthcare access influence treatment quality for minority patients. Non-White patients face greater challenges in accessing gynecologic oncology consultations and standard-of-care combination therapy, leading to poorer survival outcomes, the guidelines say.
According to Melamed, the guidelines serve as an important tool for promoting healthcare equity. “Having recommendations and standards is incredibly important for achieving equity because once there is consensus on a best practice, it doesn’t matter if you’re rich, poor, or a patient of a particular racial or ethnic group — if you have the disease, you ought to have access to that standard,” he said.
The 2016 ASCO guidelines focused primarily on disease burden and surgical resectability, whereas the 2024 National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines for ovarian cancer focus more on oncologic outcomes and surgical considerations. Based on the NCCN guidelines, treatment selection for ovarian cancer is primarily determined by the histologic subtype, stage of disease, and whether the patient is a candidate for primary surgery. The 2025 ASCO guidelines, on the other hand, emphasize the importance of quality-of-life outcomes during treatment selection. The authors of the updated ASCO guidelines acknowledged that treatment decisions should consider both the duration and quality of life, particularly for elderly patients or those with multiple comorbidities.
Treatment Timing and Duration
The guidelines maintain the recommendations for platinum/taxane-based neoadjuvant chemotherapy described in the previous ASCO guidelines but introduce modifications regarding treatment timing and duration. The optimal window for interval cytoreductive surgery now falls after three to four chemotherapy cycles, allowing more individualized approaches based on patient response and tolerance.
In addition, postsurgical chemotherapy protocols have become more flexible. Rather than mandating a fixed number of cycles, the guidelines encourage tailoring treatment duration to individual patient factors including response assessment, performance status, and quality-of-life considerations.
The updated guidelines also emphasize the importance of genetic and molecular testing at diagnosis, which Melamed identifies as “absolutely central to treatment and deciding who receives maintenance therapy.” This is also recommended by the NCCN guidelines.
However, he highlighted the following practical challenge in molecular testing after neoadjuvant chemotherapy. “Probably 20% of patients have an exceptional response to neoadjuvant therapy, such that there is insufficient tissue at the time of their cytoreduction to do somatic testing,” he said.
Hyperthermic Intraperitoneal Chemotherapy (HIPEC)
A notable difference between the 2016 and 2025 guidelines is the inclusion of HIPEC in the updated guidelines.
Commenting to this news organization, Gaillard explained the nuanced approach to HIPEC: “The committee discussed HIPEC extensively. We recognize that it may not be available at many centers and requires specially trained staff and dedicated resources. The reason for including HIPEC in the guidelines is to highlight that there have been studies that show a potential overall survival benefit.”
Melamed considers the recommendation of HIPEC to be one of the strongest aspects of the updated guidelines. “There have been two large trials and one smaller one that have shown that for patients treated with neoadjuvant chemotherapy, the addition of HIPEC appears to improve overall survival,” he explained.
Implementation Strategies
The authors acknowledged that barriers to healthcare delivery present significant challenges to the implementation of the guidelines. Limited access to gynecologic oncologists in rural areas, insurance coverage gaps, and varying surgical expertise across institutions complicate the delivery of optimal care. The guidelines also emphasize the need for solutions to ensure equitable access to recommended treatments.
Melamed noted that the decentralized structure of the healthcare system in the United States complicates the uniform adoption of guidelines, particularly in resource-limited settings, adding that “geographic region and local resources and expertise influence both access to treatment and outcomes.”
Although both the updated ASCO guidelines and NCCN guidelines emphasize the importance of evaluation by a gynecologic oncologist for determining the most appropriate treatment strategy, the scarcity of gynecologic oncologists is one of the most significant barriers to accessing optimal care, according to Gaillard. She proposes telemedicine consultations and enhanced communication between medical oncologists and gynecologic oncologists to ensure equitable access.
Gaillard also commented on the challenges in implementing a multidisciplinary treatment approach, the importance of which is emphasized in the updated guidelines.
“There can be a limited availability of the multidisciplinary team to be involved in this decision-making,” she said. “Ideally, patient assessment by a gynecologic oncologist would happen in person, but recognizing that availability is limited, it doesn’t necessarily have to. Sometimes, it can just be a conversation between a medical oncologist and a gynecologic oncologist detailing a treatment plan together.”
Looking Ahead
Gaillard noted that ovarian cancer is a very active field of research and that the guidelines may need to be updated again in the near future to incorporate novel treatment approaches.
“Newer and more effective targeted therapies based on tumor profiling are being developed,” she said. “These will hopefully move earlier in the treatment course for patients. Maybe we will not use chemotherapy in the future because we will have more directed and targeted therapies.”
She also emphasized the importance of early diagnosis in shaping future treatment guidelines for ovarian cancer.
“Neoadjuvant chemotherapy is predominantly used in situations where patients have very advanced disease and may not benefit from primary cytoreductive surgery,” she noted. “If we develop better diagnostic tools that will allow us to diagnose patients earlier, then we may not need to use neoadjuvant chemotherapy.”
All funding for the administration of the guideline development project was provided by ASCO. Gaillard reported receiving consulting or advisory fees from Verastem, Merck, AstraZeneca, and Compugen; research funding from AstraZeneca, Tesaro, Compugen, Genentech/Roche, Clovis Oncology, Tempest Therapeutics, Blueprint Pharmaceutic, Immunogen, Volastra Therapeutics, and Beigene; and patents, royalties, or other intellectual property from US Patent Nos 10,258,604 and 10,905,659, licensed by Duke University to Sermonix. Melamed reported receiving research funding from the National Cancer Institute and the National Institutes of Health.
A version of this article first appeared on Medscape.com.
The American Society of Clinical Oncology (ASCO) has released updated guidelines for neoadjuvant chemotherapy in newly diagnosed advanced ovarian cancer, introducing changes in patient selection and treatment strategies. The changes reflect emerging evidence on racial disparities, treatment outcomes, and quality of life considerations.
The publication of the new guidance follows dramatic shifts in treatment patterns over the past decade.
“There had been a big shift in how we were treating patients in the United States,” explained Stephanie Gaillard, MD, PhD, one of the authors of the updated guidelines. “We saw a substantial drop in the number of patients undergoing primary cytoreductive surgery for ovarian cancer from about 70% of patients in 2010 to only about 37% in 2021.”
The new guidelines maintain the recommendation for platinum/taxane-based neoadjuvant chemotherapy but introduce modifications regarding timing and duration.
“It’s still a recommendation that gynecologic oncologists are involved in determining whether someone is eligible for primary cytoreductive surgery or should undergo neoadjuvant chemotherapy first,” Gaillard noted. “We emphasize that patients who are eligible for primary cytoreductive surgery should undergo surgery as opposed to receiving neoadjuvant chemotherapy.”
Alexander Melamed, MD, MPH, a gynecologic oncologist at Massachusetts General Hospital, Boston, who was not involved in authoring the updated guidelines, noted that additional evidence-based guidance is needed to individualize treatment plans. He pointed to four completed trials comparing neoadjuvant chemotherapy with cytoreductive surgery, noting: “When these trials have been pooled together in meta-analyses, there was a higher risk of mortality associated with primary cytoreductive surgery and a higher risk of severe complications.”
The updated guidelines take this higher risk for mortality with primary cytoreductive surgery into consideration, and patients who are not eligible for primary surgery would receive neoadjuvant chemotherapy, Gaillard noted.
Changes in Patient Selection
The 2025 guidelines describe a more nuanced approach for selecting patients for neoadjuvant chemotherapy vs primary cytoreductive surgery. While the 2016 ASCO guidelines primarily focused on disease burden and surgical resectability when selecting patients for neoadjuvant chemotherapy, the new recommendations incorporate additional factors.
The guidelines discuss recent findings showing that Black patients experience a 38% lower likelihood of undergoing cytoreductive surgery than non-Black patients. In addition, compared with non-Hispanic White women, Asian and Black women more frequently receive neoadjuvant chemotherapy with interval debulking surgery rather than primary cytoreductive surgery. According to the authors, these differences persist even after accounting for clinical factors, suggesting that structural barriers to healthcare access may play a role.
The guidelines discuss how affordability, availability, and accessibility mediate racial disparities in ovarian cancer care. According to the authors, structural inequities in healthcare access influence treatment quality for minority patients. Non-White patients face greater challenges in accessing gynecologic oncology consultations and standard-of-care combination therapy, leading to poorer survival outcomes, the guidelines say.
According to Melamed, the guidelines serve as an important tool for promoting healthcare equity. “Having recommendations and standards is incredibly important for achieving equity because once there is consensus on a best practice, it doesn’t matter if you’re rich, poor, or a patient of a particular racial or ethnic group — if you have the disease, you ought to have access to that standard,” he said.
The 2016 ASCO guidelines focused primarily on disease burden and surgical resectability, whereas the 2024 National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines for ovarian cancer focus more on oncologic outcomes and surgical considerations. Based on the NCCN guidelines, treatment selection for ovarian cancer is primarily determined by the histologic subtype, stage of disease, and whether the patient is a candidate for primary surgery. The 2025 ASCO guidelines, on the other hand, emphasize the importance of quality-of-life outcomes during treatment selection. The authors of the updated ASCO guidelines acknowledged that treatment decisions should consider both the duration and quality of life, particularly for elderly patients or those with multiple comorbidities.
Treatment Timing and Duration
The guidelines maintain the recommendations for platinum/taxane-based neoadjuvant chemotherapy described in the previous ASCO guidelines but introduce modifications regarding treatment timing and duration. The optimal window for interval cytoreductive surgery now falls after three to four chemotherapy cycles, allowing more individualized approaches based on patient response and tolerance.
In addition, postsurgical chemotherapy protocols have become more flexible. Rather than mandating a fixed number of cycles, the guidelines encourage tailoring treatment duration to individual patient factors including response assessment, performance status, and quality-of-life considerations.
The updated guidelines also emphasize the importance of genetic and molecular testing at diagnosis, which Melamed identifies as “absolutely central to treatment and deciding who receives maintenance therapy.” This is also recommended by the NCCN guidelines.
However, he highlighted the following practical challenge in molecular testing after neoadjuvant chemotherapy. “Probably 20% of patients have an exceptional response to neoadjuvant therapy, such that there is insufficient tissue at the time of their cytoreduction to do somatic testing,” he said.
Hyperthermic Intraperitoneal Chemotherapy (HIPEC)
A notable difference between the 2016 and 2025 guidelines is the inclusion of HIPEC in the updated guidelines.
Commenting to this news organization, Gaillard explained the nuanced approach to HIPEC: “The committee discussed HIPEC extensively. We recognize that it may not be available at many centers and requires specially trained staff and dedicated resources. The reason for including HIPEC in the guidelines is to highlight that there have been studies that show a potential overall survival benefit.”
Melamed considers the recommendation of HIPEC to be one of the strongest aspects of the updated guidelines. “There have been two large trials and one smaller one that have shown that for patients treated with neoadjuvant chemotherapy, the addition of HIPEC appears to improve overall survival,” he explained.
Implementation Strategies
The authors acknowledged that barriers to healthcare delivery present significant challenges to the implementation of the guidelines. Limited access to gynecologic oncologists in rural areas, insurance coverage gaps, and varying surgical expertise across institutions complicate the delivery of optimal care. The guidelines also emphasize the need for solutions to ensure equitable access to recommended treatments.
Melamed noted that the decentralized structure of the healthcare system in the United States complicates the uniform adoption of guidelines, particularly in resource-limited settings, adding that “geographic region and local resources and expertise influence both access to treatment and outcomes.”
Although both the updated ASCO guidelines and NCCN guidelines emphasize the importance of evaluation by a gynecologic oncologist for determining the most appropriate treatment strategy, the scarcity of gynecologic oncologists is one of the most significant barriers to accessing optimal care, according to Gaillard. She proposes telemedicine consultations and enhanced communication between medical oncologists and gynecologic oncologists to ensure equitable access.
Gaillard also commented on the challenges in implementing a multidisciplinary treatment approach, the importance of which is emphasized in the updated guidelines.
“There can be a limited availability of the multidisciplinary team to be involved in this decision-making,” she said. “Ideally, patient assessment by a gynecologic oncologist would happen in person, but recognizing that availability is limited, it doesn’t necessarily have to. Sometimes, it can just be a conversation between a medical oncologist and a gynecologic oncologist detailing a treatment plan together.”
Looking Ahead
Gaillard noted that ovarian cancer is a very active field of research and that the guidelines may need to be updated again in the near future to incorporate novel treatment approaches.
“Newer and more effective targeted therapies based on tumor profiling are being developed,” she said. “These will hopefully move earlier in the treatment course for patients. Maybe we will not use chemotherapy in the future because we will have more directed and targeted therapies.”
She also emphasized the importance of early diagnosis in shaping future treatment guidelines for ovarian cancer.
“Neoadjuvant chemotherapy is predominantly used in situations where patients have very advanced disease and may not benefit from primary cytoreductive surgery,” she noted. “If we develop better diagnostic tools that will allow us to diagnose patients earlier, then we may not need to use neoadjuvant chemotherapy.”
All funding for the administration of the guideline development project was provided by ASCO. Gaillard reported receiving consulting or advisory fees from Verastem, Merck, AstraZeneca, and Compugen; research funding from AstraZeneca, Tesaro, Compugen, Genentech/Roche, Clovis Oncology, Tempest Therapeutics, Blueprint Pharmaceutic, Immunogen, Volastra Therapeutics, and Beigene; and patents, royalties, or other intellectual property from US Patent Nos 10,258,604 and 10,905,659, licensed by Duke University to Sermonix. Melamed reported receiving research funding from the National Cancer Institute and the National Institutes of Health.
A version of this article first appeared on Medscape.com.
The American Society of Clinical Oncology (ASCO) has released updated guidelines for neoadjuvant chemotherapy in newly diagnosed advanced ovarian cancer, introducing changes in patient selection and treatment strategies. The changes reflect emerging evidence on racial disparities, treatment outcomes, and quality of life considerations.
The publication of the new guidance follows dramatic shifts in treatment patterns over the past decade.
“There had been a big shift in how we were treating patients in the United States,” explained Stephanie Gaillard, MD, PhD, one of the authors of the updated guidelines. “We saw a substantial drop in the number of patients undergoing primary cytoreductive surgery for ovarian cancer from about 70% of patients in 2010 to only about 37% in 2021.”
The new guidelines maintain the recommendation for platinum/taxane-based neoadjuvant chemotherapy but introduce modifications regarding timing and duration.
“It’s still a recommendation that gynecologic oncologists are involved in determining whether someone is eligible for primary cytoreductive surgery or should undergo neoadjuvant chemotherapy first,” Gaillard noted. “We emphasize that patients who are eligible for primary cytoreductive surgery should undergo surgery as opposed to receiving neoadjuvant chemotherapy.”
Alexander Melamed, MD, MPH, a gynecologic oncologist at Massachusetts General Hospital, Boston, who was not involved in authoring the updated guidelines, noted that additional evidence-based guidance is needed to individualize treatment plans. He pointed to four completed trials comparing neoadjuvant chemotherapy with cytoreductive surgery, noting: “When these trials have been pooled together in meta-analyses, there was a higher risk of mortality associated with primary cytoreductive surgery and a higher risk of severe complications.”
The updated guidelines take this higher risk for mortality with primary cytoreductive surgery into consideration, and patients who are not eligible for primary surgery would receive neoadjuvant chemotherapy, Gaillard noted.
Changes in Patient Selection
The 2025 guidelines describe a more nuanced approach for selecting patients for neoadjuvant chemotherapy vs primary cytoreductive surgery. While the 2016 ASCO guidelines primarily focused on disease burden and surgical resectability when selecting patients for neoadjuvant chemotherapy, the new recommendations incorporate additional factors.
The guidelines discuss recent findings showing that Black patients experience a 38% lower likelihood of undergoing cytoreductive surgery than non-Black patients. In addition, compared with non-Hispanic White women, Asian and Black women more frequently receive neoadjuvant chemotherapy with interval debulking surgery rather than primary cytoreductive surgery. According to the authors, these differences persist even after accounting for clinical factors, suggesting that structural barriers to healthcare access may play a role.
The guidelines discuss how affordability, availability, and accessibility mediate racial disparities in ovarian cancer care. According to the authors, structural inequities in healthcare access influence treatment quality for minority patients. Non-White patients face greater challenges in accessing gynecologic oncology consultations and standard-of-care combination therapy, leading to poorer survival outcomes, the guidelines say.
According to Melamed, the guidelines serve as an important tool for promoting healthcare equity. “Having recommendations and standards is incredibly important for achieving equity because once there is consensus on a best practice, it doesn’t matter if you’re rich, poor, or a patient of a particular racial or ethnic group — if you have the disease, you ought to have access to that standard,” he said.
The 2016 ASCO guidelines focused primarily on disease burden and surgical resectability, whereas the 2024 National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines for ovarian cancer focus more on oncologic outcomes and surgical considerations. Based on the NCCN guidelines, treatment selection for ovarian cancer is primarily determined by the histologic subtype, stage of disease, and whether the patient is a candidate for primary surgery. The 2025 ASCO guidelines, on the other hand, emphasize the importance of quality-of-life outcomes during treatment selection. The authors of the updated ASCO guidelines acknowledged that treatment decisions should consider both the duration and quality of life, particularly for elderly patients or those with multiple comorbidities.
Treatment Timing and Duration
The guidelines maintain the recommendations for platinum/taxane-based neoadjuvant chemotherapy described in the previous ASCO guidelines but introduce modifications regarding treatment timing and duration. The optimal window for interval cytoreductive surgery now falls after three to four chemotherapy cycles, allowing more individualized approaches based on patient response and tolerance.
In addition, postsurgical chemotherapy protocols have become more flexible. Rather than mandating a fixed number of cycles, the guidelines encourage tailoring treatment duration to individual patient factors including response assessment, performance status, and quality-of-life considerations.
The updated guidelines also emphasize the importance of genetic and molecular testing at diagnosis, which Melamed identifies as “absolutely central to treatment and deciding who receives maintenance therapy.” This is also recommended by the NCCN guidelines.
However, he highlighted the following practical challenge in molecular testing after neoadjuvant chemotherapy. “Probably 20% of patients have an exceptional response to neoadjuvant therapy, such that there is insufficient tissue at the time of their cytoreduction to do somatic testing,” he said.
Hyperthermic Intraperitoneal Chemotherapy (HIPEC)
A notable difference between the 2016 and 2025 guidelines is the inclusion of HIPEC in the updated guidelines.
Commenting to this news organization, Gaillard explained the nuanced approach to HIPEC: “The committee discussed HIPEC extensively. We recognize that it may not be available at many centers and requires specially trained staff and dedicated resources. The reason for including HIPEC in the guidelines is to highlight that there have been studies that show a potential overall survival benefit.”
Melamed considers the recommendation of HIPEC to be one of the strongest aspects of the updated guidelines. “There have been two large trials and one smaller one that have shown that for patients treated with neoadjuvant chemotherapy, the addition of HIPEC appears to improve overall survival,” he explained.
Implementation Strategies
The authors acknowledged that barriers to healthcare delivery present significant challenges to the implementation of the guidelines. Limited access to gynecologic oncologists in rural areas, insurance coverage gaps, and varying surgical expertise across institutions complicate the delivery of optimal care. The guidelines also emphasize the need for solutions to ensure equitable access to recommended treatments.
Melamed noted that the decentralized structure of the healthcare system in the United States complicates the uniform adoption of guidelines, particularly in resource-limited settings, adding that “geographic region and local resources and expertise influence both access to treatment and outcomes.”
Although both the updated ASCO guidelines and NCCN guidelines emphasize the importance of evaluation by a gynecologic oncologist for determining the most appropriate treatment strategy, the scarcity of gynecologic oncologists is one of the most significant barriers to accessing optimal care, according to Gaillard. She proposes telemedicine consultations and enhanced communication between medical oncologists and gynecologic oncologists to ensure equitable access.
Gaillard also commented on the challenges in implementing a multidisciplinary treatment approach, the importance of which is emphasized in the updated guidelines.
“There can be a limited availability of the multidisciplinary team to be involved in this decision-making,” she said. “Ideally, patient assessment by a gynecologic oncologist would happen in person, but recognizing that availability is limited, it doesn’t necessarily have to. Sometimes, it can just be a conversation between a medical oncologist and a gynecologic oncologist detailing a treatment plan together.”
Looking Ahead
Gaillard noted that ovarian cancer is a very active field of research and that the guidelines may need to be updated again in the near future to incorporate novel treatment approaches.
“Newer and more effective targeted therapies based on tumor profiling are being developed,” she said. “These will hopefully move earlier in the treatment course for patients. Maybe we will not use chemotherapy in the future because we will have more directed and targeted therapies.”
She also emphasized the importance of early diagnosis in shaping future treatment guidelines for ovarian cancer.
“Neoadjuvant chemotherapy is predominantly used in situations where patients have very advanced disease and may not benefit from primary cytoreductive surgery,” she noted. “If we develop better diagnostic tools that will allow us to diagnose patients earlier, then we may not need to use neoadjuvant chemotherapy.”
All funding for the administration of the guideline development project was provided by ASCO. Gaillard reported receiving consulting or advisory fees from Verastem, Merck, AstraZeneca, and Compugen; research funding from AstraZeneca, Tesaro, Compugen, Genentech/Roche, Clovis Oncology, Tempest Therapeutics, Blueprint Pharmaceutic, Immunogen, Volastra Therapeutics, and Beigene; and patents, royalties, or other intellectual property from US Patent Nos 10,258,604 and 10,905,659, licensed by Duke University to Sermonix. Melamed reported receiving research funding from the National Cancer Institute and the National Institutes of Health.
A version of this article first appeared on Medscape.com.
ImPrint Identifies Patients With Breast Cancer Likely to Respond to Neoadjuvant Immunotherapy
SAN DIEGO — Using ImPrint, an immune-related biomarker, clinicians can identify patients with breast cancer who are likely to respond to neoadjuvant immunotherapy, according to data from the ongoing phase 2 I-SPY2 trial.
Patient selection based on ImPrint class can result in high response rates and spare nonresponders the toxicities of immunotherapy, said Denise M. Wolf, PhD, during her presentation of the study results at the annual meeting of the American Association for Cancer Research (AACR).
“Our results show that patients with ER+/HER2-/ImPrint+ breast cancer have a very high probability of achieving complete response to immunotherapy, whereas those who are ER+/HER2-/ImPrint- have a low probability of responding,” noted Dr. Wolf, PhD, MSc of the University of California, San Francisco (UCSF), in an interview.
She added that, although effective, immunotherapy also carries the risk of serious immune-related toxicities, and knowledge of ImPrint class can help patients and physicians determine whether immunotherapy is a good treatment option. “Many patients will be willing to take the risk of immunotherapy toxicities if their odds of responding are very high, as is the case for ImPrint+ patients, but [are] likely less enthused with a low likelihood of response,” Dr. Wolf said during the interview.
Need for Predictive Biomarkers for Neoadjuvant Immunotherapy
Although neoadjuvant immunotherapy has become the standard treatment for patients with early-stage triple-negative breast cancer (TNBC), chemotherapy remains the mainstay of treatment for patients with hormone receptor–positive (HR+), human epidermal growth factor receptor 2–negative (HER2-) breast cancer. The I-SPY2 clinical trial is the first randomized clinical study to assess the efficacy of immunotherapy in the high-risk population of patients with HR+/HER2-, Dr. Wolf said. Data from this study suggest that a subset of HR+/HER2- patients may also derive substantial benefit from this approach compared with standard chemotherapy.
“We and others have previously observed that a minority of ER+/HER2- breast cancers are enriched for tumor-infiltrating lymphocytes and that high levels of immune-related gene signatures associate with improved survival in this subtype, as well as in TNBC,” noted Dr. Wolf during an interview.
She explained that patients with high-risk ER+/HER2- breast cancer were not responding to any of the experimental agent classes tested in the trial and showed particularly poor outcomes, and that she and her colleagues “wanted to see if immune-oncology agents would impact response in these patients.”
ImPrint, an Immune Expression Signature
Preliminary data from the I-SPY2 trial showed that immune-related gene signatures were associated with pathologic complete response (pCR) in patients with HR+/HER2- breast cancer treated with immunotherapy. This observation allowed investigators to develop a clinically applicable immune classifier, termed ImPrint, to predict response to immunotherapy in this population.
This immune classifier is a 53-gene signature developed using data from the first anti–programmed death-1 (PD-1) arm that included patients treated with pembrolizumab, explained Dr. Wolf.
Performance of ImPrint in Patients With HR+/HER2- Breast Cancer
Dr. Wolf presented new data on the performance of ImPrint in 204 patients with high-risk HR+/HER2- breast cancer from the following five immunotherapy arms of the I-SPY2 trial, at the meeting. These arms included: anti–PD-1, anti–PDL-1 plus PARP inhibitor, anti–PD-1/TLR9 dual immunotherapy, and anti–PD-1 with or without LAG3 inhibitor. Data from 191 patients treated with the current standard of care (paclitaxel followed by adriamycin and cyclophosphamide cytoxan) were included in the analysis as a control.
The pCR in the entire population across these five immunotherapy arms was 33%. The response rate in the control arm was 13.5%.
“The high pCR in the immunotherapy groups is remarkable given the traditionally poor response of HR+/HER2- tumors to standard neoadjuvant chemotherapy,” said Ritu Aneja, PhD, the associate dean for research and innovation at the University of Alabama at Birmingham and a breast cancer expert, who was not involved in the I-SPY2 trial.
When patients were stratified according to ImPrint status, significant differences were observed among the groups. In this analysis, 28% of HR+/HER2- patients were classified as ImPrint positive (likely sensitive) based on ImPrint expression levels in pretreatment mRNA samples, and these individuals achieved pCR rates as high as 76% with immunotherapy.
In comparison, pCR rates were only 16% in ImPrint-negative (likely resistant) patients. The highest response rate was observed in the anti–PD-1/TLR9 dual immunotherapy arm, with a pCR rate of greater than 90% in ImPrint-positive patients. In the control arm, pCR rates were 33% in ImPrint-positive and 8% in ImPrint-negative patients.
“These results suggest that a subset of [patients with] high-risk HR+/HER2- breast cancers is highly sensitive to immunotherapy,” said Dr. Aneja in an interview. “By using a specific and sensitive selection strategy like ImPrint, we may be able to identify patients who can achieve pCR rates similar to what we see with the best neoadjuvant therapies in triple-negative and HER2-positive disease.”
Ability of ImPrint to Predict Long-Term Outcomes
During her talk, Dr. Wolf explained that she and her research team currently do not have sufficient follow-up data to assess the ability of ImPrint to predict long-term outcomes. Therefore, they used the pCR data to predict long-term disease-free survival (DRFS) outcomes. Based on their model, HR+/HER2-/ImPrint+ patients treated with immunotherapy were estimated to have a 91% 5-year DRFS rate, compared with 80% for those receiving standard chemotherapy alone. This represents a 52% reduction in the risk of disease recurrence.
“This suggests not only a higher immediate response rate to therapy but also potential long-term benefits for patients identified as ImPrint+,” Dr. Aneja said, commenting on the significance of the DRFS data, during the interview, She added that the ability to predict longer-term outcomes is a critical advantage in selecting the most effective treatment strategies for patients.
Comparison of ImPrint With Other Biomarkers
The investigators compared ImPrint to other potential biomarkers for immunotherapy response, including MammaPrint (ultra) High2 risk (MP2) and tumor grade. During her talk, Dr. Wolf showed data demonstrating that ImPrint is a more precise predictor of pCR, with higher response rates than either of those other markers.
The pCR rates for MP2 and grade III were 56% and 45%, respectively, which are much smaller than the pCR rates observed for ImPrint+ patients (75%).
“This difference underscores ImPrint’s effectiveness in distinguishing patients who could benefit from immunotherapy, offering a pCR prediction accuracy that is significantly higher than seen with other biomarkers that have been proposed as selection markers for neoadjuvant immunotherapy trials in HR+/HER2- breast cancers, such as MP2 and tumor grade,” said Dr. Aneja, during the interview.
Looking Ahead — Implementation of Imprint for Patient Selection
Dr. Aneja echoed that the findings from the I-SPY2 trial advocate for the integration of biomarker-driven approaches, particularly the use of the ImPrint classifier, into the treatment planning process for high-risk HR+/HER2- breast cancer.
“This approach can enable clinicians to identify patients who are more likely to benefit from immunotherapy, thus personalizing treatment strategies and potentially enhancing treatment efficacy while minimizing exposure to unnecessary toxicity for those unlikely to respond,” she said.
Dr. Aneja added that while the I-SPY2 trial offers promising data on ImPrint’s efficacy, additional prospective studies are needed to validate these findings across diverse patient populations and settings, as well as the correlation between biomarker positivity and long-term clinical outcomes, including DRFS and overall survival. “This will help to better understand the full spectrum of benefits provided by immunotherapies in biomarker-selected patient groups,” she said.
Dr. Wolf and Dr. Aneja reported no relationships with entities whose primary business is producing, marketing, selling, reselling, or distributing healthcare products used by or on patients.
SAN DIEGO — Using ImPrint, an immune-related biomarker, clinicians can identify patients with breast cancer who are likely to respond to neoadjuvant immunotherapy, according to data from the ongoing phase 2 I-SPY2 trial.
Patient selection based on ImPrint class can result in high response rates and spare nonresponders the toxicities of immunotherapy, said Denise M. Wolf, PhD, during her presentation of the study results at the annual meeting of the American Association for Cancer Research (AACR).
“Our results show that patients with ER+/HER2-/ImPrint+ breast cancer have a very high probability of achieving complete response to immunotherapy, whereas those who are ER+/HER2-/ImPrint- have a low probability of responding,” noted Dr. Wolf, PhD, MSc of the University of California, San Francisco (UCSF), in an interview.
She added that, although effective, immunotherapy also carries the risk of serious immune-related toxicities, and knowledge of ImPrint class can help patients and physicians determine whether immunotherapy is a good treatment option. “Many patients will be willing to take the risk of immunotherapy toxicities if their odds of responding are very high, as is the case for ImPrint+ patients, but [are] likely less enthused with a low likelihood of response,” Dr. Wolf said during the interview.
Need for Predictive Biomarkers for Neoadjuvant Immunotherapy
Although neoadjuvant immunotherapy has become the standard treatment for patients with early-stage triple-negative breast cancer (TNBC), chemotherapy remains the mainstay of treatment for patients with hormone receptor–positive (HR+), human epidermal growth factor receptor 2–negative (HER2-) breast cancer. The I-SPY2 clinical trial is the first randomized clinical study to assess the efficacy of immunotherapy in the high-risk population of patients with HR+/HER2-, Dr. Wolf said. Data from this study suggest that a subset of HR+/HER2- patients may also derive substantial benefit from this approach compared with standard chemotherapy.
“We and others have previously observed that a minority of ER+/HER2- breast cancers are enriched for tumor-infiltrating lymphocytes and that high levels of immune-related gene signatures associate with improved survival in this subtype, as well as in TNBC,” noted Dr. Wolf during an interview.
She explained that patients with high-risk ER+/HER2- breast cancer were not responding to any of the experimental agent classes tested in the trial and showed particularly poor outcomes, and that she and her colleagues “wanted to see if immune-oncology agents would impact response in these patients.”
ImPrint, an Immune Expression Signature
Preliminary data from the I-SPY2 trial showed that immune-related gene signatures were associated with pathologic complete response (pCR) in patients with HR+/HER2- breast cancer treated with immunotherapy. This observation allowed investigators to develop a clinically applicable immune classifier, termed ImPrint, to predict response to immunotherapy in this population.
This immune classifier is a 53-gene signature developed using data from the first anti–programmed death-1 (PD-1) arm that included patients treated with pembrolizumab, explained Dr. Wolf.
Performance of ImPrint in Patients With HR+/HER2- Breast Cancer
Dr. Wolf presented new data on the performance of ImPrint in 204 patients with high-risk HR+/HER2- breast cancer from the following five immunotherapy arms of the I-SPY2 trial, at the meeting. These arms included: anti–PD-1, anti–PDL-1 plus PARP inhibitor, anti–PD-1/TLR9 dual immunotherapy, and anti–PD-1 with or without LAG3 inhibitor. Data from 191 patients treated with the current standard of care (paclitaxel followed by adriamycin and cyclophosphamide cytoxan) were included in the analysis as a control.
The pCR in the entire population across these five immunotherapy arms was 33%. The response rate in the control arm was 13.5%.
“The high pCR in the immunotherapy groups is remarkable given the traditionally poor response of HR+/HER2- tumors to standard neoadjuvant chemotherapy,” said Ritu Aneja, PhD, the associate dean for research and innovation at the University of Alabama at Birmingham and a breast cancer expert, who was not involved in the I-SPY2 trial.
When patients were stratified according to ImPrint status, significant differences were observed among the groups. In this analysis, 28% of HR+/HER2- patients were classified as ImPrint positive (likely sensitive) based on ImPrint expression levels in pretreatment mRNA samples, and these individuals achieved pCR rates as high as 76% with immunotherapy.
In comparison, pCR rates were only 16% in ImPrint-negative (likely resistant) patients. The highest response rate was observed in the anti–PD-1/TLR9 dual immunotherapy arm, with a pCR rate of greater than 90% in ImPrint-positive patients. In the control arm, pCR rates were 33% in ImPrint-positive and 8% in ImPrint-negative patients.
“These results suggest that a subset of [patients with] high-risk HR+/HER2- breast cancers is highly sensitive to immunotherapy,” said Dr. Aneja in an interview. “By using a specific and sensitive selection strategy like ImPrint, we may be able to identify patients who can achieve pCR rates similar to what we see with the best neoadjuvant therapies in triple-negative and HER2-positive disease.”
Ability of ImPrint to Predict Long-Term Outcomes
During her talk, Dr. Wolf explained that she and her research team currently do not have sufficient follow-up data to assess the ability of ImPrint to predict long-term outcomes. Therefore, they used the pCR data to predict long-term disease-free survival (DRFS) outcomes. Based on their model, HR+/HER2-/ImPrint+ patients treated with immunotherapy were estimated to have a 91% 5-year DRFS rate, compared with 80% for those receiving standard chemotherapy alone. This represents a 52% reduction in the risk of disease recurrence.
“This suggests not only a higher immediate response rate to therapy but also potential long-term benefits for patients identified as ImPrint+,” Dr. Aneja said, commenting on the significance of the DRFS data, during the interview, She added that the ability to predict longer-term outcomes is a critical advantage in selecting the most effective treatment strategies for patients.
Comparison of ImPrint With Other Biomarkers
The investigators compared ImPrint to other potential biomarkers for immunotherapy response, including MammaPrint (ultra) High2 risk (MP2) and tumor grade. During her talk, Dr. Wolf showed data demonstrating that ImPrint is a more precise predictor of pCR, with higher response rates than either of those other markers.
The pCR rates for MP2 and grade III were 56% and 45%, respectively, which are much smaller than the pCR rates observed for ImPrint+ patients (75%).
“This difference underscores ImPrint’s effectiveness in distinguishing patients who could benefit from immunotherapy, offering a pCR prediction accuracy that is significantly higher than seen with other biomarkers that have been proposed as selection markers for neoadjuvant immunotherapy trials in HR+/HER2- breast cancers, such as MP2 and tumor grade,” said Dr. Aneja, during the interview.
Looking Ahead — Implementation of Imprint for Patient Selection
Dr. Aneja echoed that the findings from the I-SPY2 trial advocate for the integration of biomarker-driven approaches, particularly the use of the ImPrint classifier, into the treatment planning process for high-risk HR+/HER2- breast cancer.
“This approach can enable clinicians to identify patients who are more likely to benefit from immunotherapy, thus personalizing treatment strategies and potentially enhancing treatment efficacy while minimizing exposure to unnecessary toxicity for those unlikely to respond,” she said.
Dr. Aneja added that while the I-SPY2 trial offers promising data on ImPrint’s efficacy, additional prospective studies are needed to validate these findings across diverse patient populations and settings, as well as the correlation between biomarker positivity and long-term clinical outcomes, including DRFS and overall survival. “This will help to better understand the full spectrum of benefits provided by immunotherapies in biomarker-selected patient groups,” she said.
Dr. Wolf and Dr. Aneja reported no relationships with entities whose primary business is producing, marketing, selling, reselling, or distributing healthcare products used by or on patients.
SAN DIEGO — Using ImPrint, an immune-related biomarker, clinicians can identify patients with breast cancer who are likely to respond to neoadjuvant immunotherapy, according to data from the ongoing phase 2 I-SPY2 trial.
Patient selection based on ImPrint class can result in high response rates and spare nonresponders the toxicities of immunotherapy, said Denise M. Wolf, PhD, during her presentation of the study results at the annual meeting of the American Association for Cancer Research (AACR).
“Our results show that patients with ER+/HER2-/ImPrint+ breast cancer have a very high probability of achieving complete response to immunotherapy, whereas those who are ER+/HER2-/ImPrint- have a low probability of responding,” noted Dr. Wolf, PhD, MSc of the University of California, San Francisco (UCSF), in an interview.
She added that, although effective, immunotherapy also carries the risk of serious immune-related toxicities, and knowledge of ImPrint class can help patients and physicians determine whether immunotherapy is a good treatment option. “Many patients will be willing to take the risk of immunotherapy toxicities if their odds of responding are very high, as is the case for ImPrint+ patients, but [are] likely less enthused with a low likelihood of response,” Dr. Wolf said during the interview.
Need for Predictive Biomarkers for Neoadjuvant Immunotherapy
Although neoadjuvant immunotherapy has become the standard treatment for patients with early-stage triple-negative breast cancer (TNBC), chemotherapy remains the mainstay of treatment for patients with hormone receptor–positive (HR+), human epidermal growth factor receptor 2–negative (HER2-) breast cancer. The I-SPY2 clinical trial is the first randomized clinical study to assess the efficacy of immunotherapy in the high-risk population of patients with HR+/HER2-, Dr. Wolf said. Data from this study suggest that a subset of HR+/HER2- patients may also derive substantial benefit from this approach compared with standard chemotherapy.
“We and others have previously observed that a minority of ER+/HER2- breast cancers are enriched for tumor-infiltrating lymphocytes and that high levels of immune-related gene signatures associate with improved survival in this subtype, as well as in TNBC,” noted Dr. Wolf during an interview.
She explained that patients with high-risk ER+/HER2- breast cancer were not responding to any of the experimental agent classes tested in the trial and showed particularly poor outcomes, and that she and her colleagues “wanted to see if immune-oncology agents would impact response in these patients.”
ImPrint, an Immune Expression Signature
Preliminary data from the I-SPY2 trial showed that immune-related gene signatures were associated with pathologic complete response (pCR) in patients with HR+/HER2- breast cancer treated with immunotherapy. This observation allowed investigators to develop a clinically applicable immune classifier, termed ImPrint, to predict response to immunotherapy in this population.
This immune classifier is a 53-gene signature developed using data from the first anti–programmed death-1 (PD-1) arm that included patients treated with pembrolizumab, explained Dr. Wolf.
Performance of ImPrint in Patients With HR+/HER2- Breast Cancer
Dr. Wolf presented new data on the performance of ImPrint in 204 patients with high-risk HR+/HER2- breast cancer from the following five immunotherapy arms of the I-SPY2 trial, at the meeting. These arms included: anti–PD-1, anti–PDL-1 plus PARP inhibitor, anti–PD-1/TLR9 dual immunotherapy, and anti–PD-1 with or without LAG3 inhibitor. Data from 191 patients treated with the current standard of care (paclitaxel followed by adriamycin and cyclophosphamide cytoxan) were included in the analysis as a control.
The pCR in the entire population across these five immunotherapy arms was 33%. The response rate in the control arm was 13.5%.
“The high pCR in the immunotherapy groups is remarkable given the traditionally poor response of HR+/HER2- tumors to standard neoadjuvant chemotherapy,” said Ritu Aneja, PhD, the associate dean for research and innovation at the University of Alabama at Birmingham and a breast cancer expert, who was not involved in the I-SPY2 trial.
When patients were stratified according to ImPrint status, significant differences were observed among the groups. In this analysis, 28% of HR+/HER2- patients were classified as ImPrint positive (likely sensitive) based on ImPrint expression levels in pretreatment mRNA samples, and these individuals achieved pCR rates as high as 76% with immunotherapy.
In comparison, pCR rates were only 16% in ImPrint-negative (likely resistant) patients. The highest response rate was observed in the anti–PD-1/TLR9 dual immunotherapy arm, with a pCR rate of greater than 90% in ImPrint-positive patients. In the control arm, pCR rates were 33% in ImPrint-positive and 8% in ImPrint-negative patients.
“These results suggest that a subset of [patients with] high-risk HR+/HER2- breast cancers is highly sensitive to immunotherapy,” said Dr. Aneja in an interview. “By using a specific and sensitive selection strategy like ImPrint, we may be able to identify patients who can achieve pCR rates similar to what we see with the best neoadjuvant therapies in triple-negative and HER2-positive disease.”
Ability of ImPrint to Predict Long-Term Outcomes
During her talk, Dr. Wolf explained that she and her research team currently do not have sufficient follow-up data to assess the ability of ImPrint to predict long-term outcomes. Therefore, they used the pCR data to predict long-term disease-free survival (DRFS) outcomes. Based on their model, HR+/HER2-/ImPrint+ patients treated with immunotherapy were estimated to have a 91% 5-year DRFS rate, compared with 80% for those receiving standard chemotherapy alone. This represents a 52% reduction in the risk of disease recurrence.
“This suggests not only a higher immediate response rate to therapy but also potential long-term benefits for patients identified as ImPrint+,” Dr. Aneja said, commenting on the significance of the DRFS data, during the interview, She added that the ability to predict longer-term outcomes is a critical advantage in selecting the most effective treatment strategies for patients.
Comparison of ImPrint With Other Biomarkers
The investigators compared ImPrint to other potential biomarkers for immunotherapy response, including MammaPrint (ultra) High2 risk (MP2) and tumor grade. During her talk, Dr. Wolf showed data demonstrating that ImPrint is a more precise predictor of pCR, with higher response rates than either of those other markers.
The pCR rates for MP2 and grade III were 56% and 45%, respectively, which are much smaller than the pCR rates observed for ImPrint+ patients (75%).
“This difference underscores ImPrint’s effectiveness in distinguishing patients who could benefit from immunotherapy, offering a pCR prediction accuracy that is significantly higher than seen with other biomarkers that have been proposed as selection markers for neoadjuvant immunotherapy trials in HR+/HER2- breast cancers, such as MP2 and tumor grade,” said Dr. Aneja, during the interview.
Looking Ahead — Implementation of Imprint for Patient Selection
Dr. Aneja echoed that the findings from the I-SPY2 trial advocate for the integration of biomarker-driven approaches, particularly the use of the ImPrint classifier, into the treatment planning process for high-risk HR+/HER2- breast cancer.
“This approach can enable clinicians to identify patients who are more likely to benefit from immunotherapy, thus personalizing treatment strategies and potentially enhancing treatment efficacy while minimizing exposure to unnecessary toxicity for those unlikely to respond,” she said.
Dr. Aneja added that while the I-SPY2 trial offers promising data on ImPrint’s efficacy, additional prospective studies are needed to validate these findings across diverse patient populations and settings, as well as the correlation between biomarker positivity and long-term clinical outcomes, including DRFS and overall survival. “This will help to better understand the full spectrum of benefits provided by immunotherapies in biomarker-selected patient groups,” she said.
Dr. Wolf and Dr. Aneja reported no relationships with entities whose primary business is producing, marketing, selling, reselling, or distributing healthcare products used by or on patients.