User login
Brendon Shank joined the Society of Hospital Medicine in February 2011 and serves as Associate Vice President of Communications. He is responsible for maintaining a dialogue between SHM and its many audiences, including members, media and others in healthcare.
Healthcare Trailblazers
Younger generations blaze new paths through the American economy. Fifteen years ago, Generation X was fresh out of college and flush with the unimagined potential of the Internet. They helped change the way the world shared information and conducted business. The impact of such innovation and enthusiasm for new technology is still felt today.
The healthcare sector possesses pioneers of its own, many with the same kind of drive and vision as the dot-com entrepreneurs of the 1990s. Fifteen years from now, today’s young hospitalists—shaped by ever-changing demands and healthcare hurdles—will be recognized as an authority in the new ways patient care is delivered.
—Brian Markoff, MD, FHM, associate professor of medicine, Mount Sinai Hospitalist Group, New York City
Bijo Chacko, MD, FHM, former chair of SHM’s Young Physicians Committee, sees energy in the newest generation of hospitalists. He also sees great potential from residents who are finishing their training and considering their job options. Until recently, SHM’s Young Physicians Committee operated as a task force. The group’s growth and increased young-physician representation throughout the society prompted SHM leadership to promote the task force to full committee status.
“The wonderful thing is that we have received lots of input from around the country and dramatically increased membership in the past few years,” says Dr. Chacko, hospital medicine medical director for Preferred Health Partners in New York City. “We have moved from simply gathering information about young physicians in hospital medicine to actively disseminating it, including the new Resident’s Corner [department in The Hospitalist]. It addresses the needs of residents and introduces them to the nuances and specifics of hospital medicine.”
The demand for information has spurred the launch of a young physicians section (www.hospitalmedicine.org/youngdoctor) on SHM’s Web site. Combined with SHM’s online career center (www.hospitalmedicine.org/careercenter), the new microsites provide young physicians a broad range of information about the specialty and—most importantly—HM career options.
Natural Progression
Four out of five large hospitals now use hospitalists, and as more hospitals implement HM programs, more residents will be exposed to the hospitalist model of care. For residents, the allure of an HM career is broad and deep. In many ways, HM is the logical extension of residency training. Brian Markoff, MD, FHM, a hospitalist and associate professor of medicine at Mount Sinai Hospitalist Group in New York City, was a chief resident when he founded the hospitalist program at the University of California at Davis Health System in Sacramento in 1998.
“Creating the hospitalist program at UC-Davis was pretty easy,” Dr. Markoff says. “All of the program’s founders were chief residents at the time. The people involved were warm to the idea, and we could teach without being in the fellowship program. Residents are already very comfortable treating patients in the hospital setting.”
Dr. Markoff says practicing hospitalists are a positive influence on residents who are still undecided on a career path. “If you’re a good role model, they’ll be interested in hospital medicine,” he says.
Diversity of Patients, Issues, Settings
Dr. Markoff and others caution that HM encompasses more than an expansion of a resident’s standard roles and responsibilities. “We’re not just super-residents,” he says. “We’re highly trained specialists in the care of hospitalized patients and the process of making care in hospital better.”
Medical conditions, patient issues, and administrative situations that often are outside a resident’s scope quickly come into focus for a new hospitalist. When Mona Patel, DO, associate director of hospitalist services at Staten Island University Hospital in New York, chose an HM career five years ago, the diversity in opportunities was a major draw. Like many hospitalists, she knew she would enjoy the type of care she provides to patients.
“I liked the acuity of the patients and disease processes; it was much more interesting and exciting for me than ongoing outpatient care of chronic diseases,” Dr. Patel says. “I liked the interaction with the hospital house staff and lots of consultants. If I had questions about a patient, I could easily consult with a specialist within the hospital.”
In addition to providing bedside care, new hospitalists often find themselves at the forefront of a monumental change in how healthcare is provided nationwide. Quality improvement (QI) initiatives, such as reducing preventable diseases in the hospital and reducing readmission rates, attracted Bryan Huang, MD, to hospital medicine at the University of California at San Diego.
“When I interviewed at UCSD, I was very interested in quality improvement,” says Dr. Huang, an assistant clinical professor at UCSD’s Division of Hospital Medicine. “UCSD is well known for glycemic control and VTE prophylaxis. We’re now working on quality improvement for treating delirium and hospital discharge.”
His experience as an academic hospitalist has opened up the QI world to him. “Before this job, I was almost not familiar at all with quality improvement,” Dr. Huang says. “As a resident, I did some quality-improvement work, but not much. Quality improvement was missing from residency training, but it’s getting better.”
Dr. Patel says HM’s biggest selling point is the variety of settings available to a new hospitalist. She’s been working for the past two years in an academic hospital program in a community hospital setting with 20 hospitalists. Before that, she worked in private practice as a hospitalist. Now, when she talks with residents, she talks about their options.
“It’s really important that you figure out what kind of setting you want,” Dr. Patel says. “Hospital medicine has a diversity of settings, from a small community hospital where you do a broad range of inpatient care to a larger academic teaching environment or a private practice group.”
Leadership Opportunities
The continuing demand for hospitalists affords young physicians who are considering an HM career additional freedom in the job market. In comparison to more traditional primary-care models, hospitalist jobs offer flexible hours and competitive salaries.
Dr. Chacko points to another benefit that is a direct result of the high demand for hospitalists: increased opportunities to launch management careers. The average age of a hospitalist is 37 and the average age of an HM group leader is 41, according to SHM’s 2007-2008 Bi-Annual Survey on the State of the Hospital Medicine Movement.
“That’s not that much of a difference,” Dr. Chacko says. “Early-career hospitalists find ample leadership opportunities in the specialty. There are lots of opportunities for young hospitalists.”
How to Get Started
Because most teaching hospitals have hospitalists, most residents are exposed to HM. Many hospitalists relish the opportunity to mentor and provide early-career counseling. “Sometimes, a resident will ask to grab coffee and learn more about hospital medicine,” Dr. Huang says. “I tell them what my job is like. Many ask, ‘How do I get started looking for a job?’ I tell them that connections really help. Word of mouth is very important, so I refer people to other people.”
Margaret Fang, MD, MPH, FHM, assistant professor of medicine at the University of California at San Francisco’s division of hospital medicine and a founding member of the Young Physicians Committee, recommends that residents begin with a vision and work backward. “On a broad level, if you’re a resident, you should think about where you want to be in five years,” she says. “Look around your hospital and find a few people whose job you want.”
For some young physicians, looking ahead five years could mean being part of the healthcare revolution of tomorrow. TH
Brendon Shank is a freelance writer based in Philadelphia.
SHM elects board members
SHM has elected three new members to its Board of Directors and re-elected two members. Board members are nominated and elected by the membership and serve a three-year term.The newly elected members of the board are:



Re-elected board members:


Younger generations blaze new paths through the American economy. Fifteen years ago, Generation X was fresh out of college and flush with the unimagined potential of the Internet. They helped change the way the world shared information and conducted business. The impact of such innovation and enthusiasm for new technology is still felt today.
The healthcare sector possesses pioneers of its own, many with the same kind of drive and vision as the dot-com entrepreneurs of the 1990s. Fifteen years from now, today’s young hospitalists—shaped by ever-changing demands and healthcare hurdles—will be recognized as an authority in the new ways patient care is delivered.
—Brian Markoff, MD, FHM, associate professor of medicine, Mount Sinai Hospitalist Group, New York City
Bijo Chacko, MD, FHM, former chair of SHM’s Young Physicians Committee, sees energy in the newest generation of hospitalists. He also sees great potential from residents who are finishing their training and considering their job options. Until recently, SHM’s Young Physicians Committee operated as a task force. The group’s growth and increased young-physician representation throughout the society prompted SHM leadership to promote the task force to full committee status.
“The wonderful thing is that we have received lots of input from around the country and dramatically increased membership in the past few years,” says Dr. Chacko, hospital medicine medical director for Preferred Health Partners in New York City. “We have moved from simply gathering information about young physicians in hospital medicine to actively disseminating it, including the new Resident’s Corner [department in The Hospitalist]. It addresses the needs of residents and introduces them to the nuances and specifics of hospital medicine.”
The demand for information has spurred the launch of a young physicians section (www.hospitalmedicine.org/youngdoctor) on SHM’s Web site. Combined with SHM’s online career center (www.hospitalmedicine.org/careercenter), the new microsites provide young physicians a broad range of information about the specialty and—most importantly—HM career options.
Natural Progression
Four out of five large hospitals now use hospitalists, and as more hospitals implement HM programs, more residents will be exposed to the hospitalist model of care. For residents, the allure of an HM career is broad and deep. In many ways, HM is the logical extension of residency training. Brian Markoff, MD, FHM, a hospitalist and associate professor of medicine at Mount Sinai Hospitalist Group in New York City, was a chief resident when he founded the hospitalist program at the University of California at Davis Health System in Sacramento in 1998.
“Creating the hospitalist program at UC-Davis was pretty easy,” Dr. Markoff says. “All of the program’s founders were chief residents at the time. The people involved were warm to the idea, and we could teach without being in the fellowship program. Residents are already very comfortable treating patients in the hospital setting.”
Dr. Markoff says practicing hospitalists are a positive influence on residents who are still undecided on a career path. “If you’re a good role model, they’ll be interested in hospital medicine,” he says.
Diversity of Patients, Issues, Settings
Dr. Markoff and others caution that HM encompasses more than an expansion of a resident’s standard roles and responsibilities. “We’re not just super-residents,” he says. “We’re highly trained specialists in the care of hospitalized patients and the process of making care in hospital better.”
Medical conditions, patient issues, and administrative situations that often are outside a resident’s scope quickly come into focus for a new hospitalist. When Mona Patel, DO, associate director of hospitalist services at Staten Island University Hospital in New York, chose an HM career five years ago, the diversity in opportunities was a major draw. Like many hospitalists, she knew she would enjoy the type of care she provides to patients.
“I liked the acuity of the patients and disease processes; it was much more interesting and exciting for me than ongoing outpatient care of chronic diseases,” Dr. Patel says. “I liked the interaction with the hospital house staff and lots of consultants. If I had questions about a patient, I could easily consult with a specialist within the hospital.”
In addition to providing bedside care, new hospitalists often find themselves at the forefront of a monumental change in how healthcare is provided nationwide. Quality improvement (QI) initiatives, such as reducing preventable diseases in the hospital and reducing readmission rates, attracted Bryan Huang, MD, to hospital medicine at the University of California at San Diego.
“When I interviewed at UCSD, I was very interested in quality improvement,” says Dr. Huang, an assistant clinical professor at UCSD’s Division of Hospital Medicine. “UCSD is well known for glycemic control and VTE prophylaxis. We’re now working on quality improvement for treating delirium and hospital discharge.”
His experience as an academic hospitalist has opened up the QI world to him. “Before this job, I was almost not familiar at all with quality improvement,” Dr. Huang says. “As a resident, I did some quality-improvement work, but not much. Quality improvement was missing from residency training, but it’s getting better.”
Dr. Patel says HM’s biggest selling point is the variety of settings available to a new hospitalist. She’s been working for the past two years in an academic hospital program in a community hospital setting with 20 hospitalists. Before that, she worked in private practice as a hospitalist. Now, when she talks with residents, she talks about their options.
“It’s really important that you figure out what kind of setting you want,” Dr. Patel says. “Hospital medicine has a diversity of settings, from a small community hospital where you do a broad range of inpatient care to a larger academic teaching environment or a private practice group.”
Leadership Opportunities
The continuing demand for hospitalists affords young physicians who are considering an HM career additional freedom in the job market. In comparison to more traditional primary-care models, hospitalist jobs offer flexible hours and competitive salaries.
Dr. Chacko points to another benefit that is a direct result of the high demand for hospitalists: increased opportunities to launch management careers. The average age of a hospitalist is 37 and the average age of an HM group leader is 41, according to SHM’s 2007-2008 Bi-Annual Survey on the State of the Hospital Medicine Movement.
“That’s not that much of a difference,” Dr. Chacko says. “Early-career hospitalists find ample leadership opportunities in the specialty. There are lots of opportunities for young hospitalists.”
How to Get Started
Because most teaching hospitals have hospitalists, most residents are exposed to HM. Many hospitalists relish the opportunity to mentor and provide early-career counseling. “Sometimes, a resident will ask to grab coffee and learn more about hospital medicine,” Dr. Huang says. “I tell them what my job is like. Many ask, ‘How do I get started looking for a job?’ I tell them that connections really help. Word of mouth is very important, so I refer people to other people.”
Margaret Fang, MD, MPH, FHM, assistant professor of medicine at the University of California at San Francisco’s division of hospital medicine and a founding member of the Young Physicians Committee, recommends that residents begin with a vision and work backward. “On a broad level, if you’re a resident, you should think about where you want to be in five years,” she says. “Look around your hospital and find a few people whose job you want.”
For some young physicians, looking ahead five years could mean being part of the healthcare revolution of tomorrow. TH
Brendon Shank is a freelance writer based in Philadelphia.
SHM elects board members
SHM has elected three new members to its Board of Directors and re-elected two members. Board members are nominated and elected by the membership and serve a three-year term.The newly elected members of the board are:



Re-elected board members:


Younger generations blaze new paths through the American economy. Fifteen years ago, Generation X was fresh out of college and flush with the unimagined potential of the Internet. They helped change the way the world shared information and conducted business. The impact of such innovation and enthusiasm for new technology is still felt today.
The healthcare sector possesses pioneers of its own, many with the same kind of drive and vision as the dot-com entrepreneurs of the 1990s. Fifteen years from now, today’s young hospitalists—shaped by ever-changing demands and healthcare hurdles—will be recognized as an authority in the new ways patient care is delivered.
—Brian Markoff, MD, FHM, associate professor of medicine, Mount Sinai Hospitalist Group, New York City
Bijo Chacko, MD, FHM, former chair of SHM’s Young Physicians Committee, sees energy in the newest generation of hospitalists. He also sees great potential from residents who are finishing their training and considering their job options. Until recently, SHM’s Young Physicians Committee operated as a task force. The group’s growth and increased young-physician representation throughout the society prompted SHM leadership to promote the task force to full committee status.
“The wonderful thing is that we have received lots of input from around the country and dramatically increased membership in the past few years,” says Dr. Chacko, hospital medicine medical director for Preferred Health Partners in New York City. “We have moved from simply gathering information about young physicians in hospital medicine to actively disseminating it, including the new Resident’s Corner [department in The Hospitalist]. It addresses the needs of residents and introduces them to the nuances and specifics of hospital medicine.”
The demand for information has spurred the launch of a young physicians section (www.hospitalmedicine.org/youngdoctor) on SHM’s Web site. Combined with SHM’s online career center (www.hospitalmedicine.org/careercenter), the new microsites provide young physicians a broad range of information about the specialty and—most importantly—HM career options.
Natural Progression
Four out of five large hospitals now use hospitalists, and as more hospitals implement HM programs, more residents will be exposed to the hospitalist model of care. For residents, the allure of an HM career is broad and deep. In many ways, HM is the logical extension of residency training. Brian Markoff, MD, FHM, a hospitalist and associate professor of medicine at Mount Sinai Hospitalist Group in New York City, was a chief resident when he founded the hospitalist program at the University of California at Davis Health System in Sacramento in 1998.
“Creating the hospitalist program at UC-Davis was pretty easy,” Dr. Markoff says. “All of the program’s founders were chief residents at the time. The people involved were warm to the idea, and we could teach without being in the fellowship program. Residents are already very comfortable treating patients in the hospital setting.”
Dr. Markoff says practicing hospitalists are a positive influence on residents who are still undecided on a career path. “If you’re a good role model, they’ll be interested in hospital medicine,” he says.
Diversity of Patients, Issues, Settings
Dr. Markoff and others caution that HM encompasses more than an expansion of a resident’s standard roles and responsibilities. “We’re not just super-residents,” he says. “We’re highly trained specialists in the care of hospitalized patients and the process of making care in hospital better.”
Medical conditions, patient issues, and administrative situations that often are outside a resident’s scope quickly come into focus for a new hospitalist. When Mona Patel, DO, associate director of hospitalist services at Staten Island University Hospital in New York, chose an HM career five years ago, the diversity in opportunities was a major draw. Like many hospitalists, she knew she would enjoy the type of care she provides to patients.
“I liked the acuity of the patients and disease processes; it was much more interesting and exciting for me than ongoing outpatient care of chronic diseases,” Dr. Patel says. “I liked the interaction with the hospital house staff and lots of consultants. If I had questions about a patient, I could easily consult with a specialist within the hospital.”
In addition to providing bedside care, new hospitalists often find themselves at the forefront of a monumental change in how healthcare is provided nationwide. Quality improvement (QI) initiatives, such as reducing preventable diseases in the hospital and reducing readmission rates, attracted Bryan Huang, MD, to hospital medicine at the University of California at San Diego.
“When I interviewed at UCSD, I was very interested in quality improvement,” says Dr. Huang, an assistant clinical professor at UCSD’s Division of Hospital Medicine. “UCSD is well known for glycemic control and VTE prophylaxis. We’re now working on quality improvement for treating delirium and hospital discharge.”
His experience as an academic hospitalist has opened up the QI world to him. “Before this job, I was almost not familiar at all with quality improvement,” Dr. Huang says. “As a resident, I did some quality-improvement work, but not much. Quality improvement was missing from residency training, but it’s getting better.”
Dr. Patel says HM’s biggest selling point is the variety of settings available to a new hospitalist. She’s been working for the past two years in an academic hospital program in a community hospital setting with 20 hospitalists. Before that, she worked in private practice as a hospitalist. Now, when she talks with residents, she talks about their options.
“It’s really important that you figure out what kind of setting you want,” Dr. Patel says. “Hospital medicine has a diversity of settings, from a small community hospital where you do a broad range of inpatient care to a larger academic teaching environment or a private practice group.”
Leadership Opportunities
The continuing demand for hospitalists affords young physicians who are considering an HM career additional freedom in the job market. In comparison to more traditional primary-care models, hospitalist jobs offer flexible hours and competitive salaries.
Dr. Chacko points to another benefit that is a direct result of the high demand for hospitalists: increased opportunities to launch management careers. The average age of a hospitalist is 37 and the average age of an HM group leader is 41, according to SHM’s 2007-2008 Bi-Annual Survey on the State of the Hospital Medicine Movement.
“That’s not that much of a difference,” Dr. Chacko says. “Early-career hospitalists find ample leadership opportunities in the specialty. There are lots of opportunities for young hospitalists.”
How to Get Started
Because most teaching hospitals have hospitalists, most residents are exposed to HM. Many hospitalists relish the opportunity to mentor and provide early-career counseling. “Sometimes, a resident will ask to grab coffee and learn more about hospital medicine,” Dr. Huang says. “I tell them what my job is like. Many ask, ‘How do I get started looking for a job?’ I tell them that connections really help. Word of mouth is very important, so I refer people to other people.”
Margaret Fang, MD, MPH, FHM, assistant professor of medicine at the University of California at San Francisco’s division of hospital medicine and a founding member of the Young Physicians Committee, recommends that residents begin with a vision and work backward. “On a broad level, if you’re a resident, you should think about where you want to be in five years,” she says. “Look around your hospital and find a few people whose job you want.”
For some young physicians, looking ahead five years could mean being part of the healthcare revolution of tomorrow. TH
Brendon Shank is a freelance writer based in Philadelphia.
SHM elects board members
SHM has elected three new members to its Board of Directors and re-elected two members. Board members are nominated and elected by the membership and serve a three-year term.The newly elected members of the board are:



Re-elected board members:


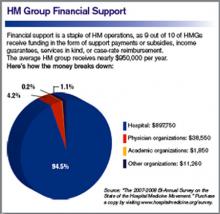
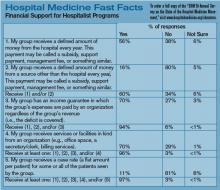
Focused on the Practice
Most HM groups (HMGs) participate in quality initiatives in their hospitals, according to new SHM research. Moreover, 7 out of 10 HMGs participating in QI initiatives are leading those efforts at their hospitals.
The findings are part of SHM’s 2008-2009 Focused Survey, the latest in a series of reports commissioned by the Practice Analysis Committee. The survey and report concentrate on topics of interest from SHM’s comprehensive, biannual survey of its membership.
The survey compiled responses from 145 HMG leaders. In addition to QI initiatives, participants in the survey responded to a variety of questions, including quality-based incentives, hospitalist turnover, and the use of part-time hospitalists.

—Joe Miller, SHM’s executive advisor to the CEO
“This is certain to be a conversation starter for hospitalists, hospital executives, and others,” says Burke Kealey, MD, FHM, medical director for hospital medicine at St. Paul, Minn.-based HealthPartners and chair of SHM’s Practice Analysis Committee. “The Focused Survey is an opportunity for SHM to answer some of the pressing questions that healthcare executives and providers have about managing a hospitalist practice within the larger context of the hospital.”
Hospital executives and hospitalists use SHM survey findings to better understand what is going on in the specialty, says Joe Miller, SHM’s executive advisor to the CEO. “These surveys answer the kinds of questions that often come up when hospitalists and hospitals begin to evaluate their performance and plan for the future,” Miller says. “We use their questions as source material for this survey, so we can help them answer questions like, ‘How are most hospitalists participating in QI?’ or ‘How are other hospitalists using part-time staff members?’ ”
Hospitalists Lead the Way
Hospitalists continue to be at the forefront of QI initiatives within their hospitals, according to the latest survey. Almost all respondents (96.5%) reported that their HMG participated in QI programs; the average HMG has six hospitalists playing an active role in QI within the hospital.
The survey also found that 72.1% of respondents involved in QI activity reported that their hospitalists were “responsible for leading project(s)” on QI initiatives.
“The findings about the active role hospitalists play in QI initiatives may surprise even the most staunch advocate of QI within the hospital medicine specialty,” says Leslie Flores, MHA, SHM’s director of the Practice Management Institute and leader of the Focused Survey research. “In essence, it shows that nearly every hospitalist group is active in promoting QI, and that the vast majority of them are taking a leadership position to improve quality. … It is remarkable and extremely exciting that hospitalists are so deeply involved in QI in their organizations.”
The survey identified patient safety, clinical QI, and quality-related IT initiatives as most popular.
Quality Incentive Compensation
In order to track HMG quality incentive compensation, the 2008-2009 Focused Survey asked similar questions about the topic to questions in the 2006-2007 Focused Survey. Quality incentive compensation—paying bonuses or additional payments for meeting QI measures—not only increased markedly in the past two years, but a majority of HMGs also have adopted the practice. The number of HMGs that have quality incentive compensation plans has increased by 39% since 2006, according to the survey.
Nine out of 10 HMGs that receive performance-based compensation reported that the source of the compensation was the hospital or health system. In most cases, the compensation was paid to an individual hospitalist, which represents a shift from 2006, when more groups reported receiving the compensation directly.
The survey also shows that hospitals and HMGs use a number of process measures to evaluate QI incentives, including participation in quality or safety committees, transition of care measures, or core measures for heart failure, pneumonia, and acute myocardial infarction.
New Numbers Dispel High Turnover Myth
For years, the conventional wisdom throughout the healthcare community has been that HM suffers from a high turnover rate among its hospitalists. Focused Survey findings suggest otherwise. In fact, turnover rates for hospitalist groups have remained constant since 2005. Nearly a third (31.7%) of HMGs reported no turnover at all within the past 12 months.
“Getting an accurate idea about turnover in hospitalist groups has been an ongoing challenge in our research,” Flores says. “In this year’s Focused Survey, we provided clearer definitions and asked more specific questions to improve our measurement of turnover.”
The added specificity only served to reinforce findings from previous surveys that showed relatively low turnover rates. The most recent research revealed a 12.7% turnover rate, compared with 13% in 2007 and 12% in 2005.
The latest Focused Survey also includes detailed findings on turnover among full-time hospitalists compared with part-time hospitalists.
Part-Time vs. Full-Time
The new data challenge long-held assumptions about the role of part-time hospitalists. The survey queried HMGs about full-time and part-time hospitalist staff, and the proportion of time that each employee covers in the hospital.
Although there isn’t a consensus about what constitutes a full-time hospitalist, it is clear that they cover the vast majority (85%) of HMG staff hours. Part-time hospitalists are responsible for 10% of hospitalist staff hours, and “casual” hospitalists—temporary hospitalists or moonlighters—make up the remaining 5%.
Part-time hospitalists share the same responsibilities as their full-time colleagues, according to the report. More than 70% of HMG leaders said their part-time staff is deployed to cover the same shifts and responsibilities as full-time staff. Many HMGs use part-time staff to cover night and weekend shifts.
Trend Today, Initiative Tomorrow
Taken together, SHM’s bi-annual survey and Focused Survey have begun to reveal some of the most prevalent trends within the specialty, including low turnover and a specialty-wide QI emphasis. However, Flores sees room for additional research in the near future.
“There is a lot more to learn about the nature of hospitalists’ involvement in organizational quality initiatives and what benefits that involvement is delivering to their organizations,” she says. “The survey suggests some areas, particularly in the quality arena, where SHM can develop additional programs and services to support hospitalists and the work they do.”
The 10-page 2008-2009 Focused Survey report is available at www.hospitalmedicine.org/shmstore. TH
Brendon Shank is a freelance writer based in Philadelphia.
Most HM groups (HMGs) participate in quality initiatives in their hospitals, according to new SHM research. Moreover, 7 out of 10 HMGs participating in QI initiatives are leading those efforts at their hospitals.
The findings are part of SHM’s 2008-2009 Focused Survey, the latest in a series of reports commissioned by the Practice Analysis Committee. The survey and report concentrate on topics of interest from SHM’s comprehensive, biannual survey of its membership.
The survey compiled responses from 145 HMG leaders. In addition to QI initiatives, participants in the survey responded to a variety of questions, including quality-based incentives, hospitalist turnover, and the use of part-time hospitalists.

—Joe Miller, SHM’s executive advisor to the CEO
“This is certain to be a conversation starter for hospitalists, hospital executives, and others,” says Burke Kealey, MD, FHM, medical director for hospital medicine at St. Paul, Minn.-based HealthPartners and chair of SHM’s Practice Analysis Committee. “The Focused Survey is an opportunity for SHM to answer some of the pressing questions that healthcare executives and providers have about managing a hospitalist practice within the larger context of the hospital.”
Hospital executives and hospitalists use SHM survey findings to better understand what is going on in the specialty, says Joe Miller, SHM’s executive advisor to the CEO. “These surveys answer the kinds of questions that often come up when hospitalists and hospitals begin to evaluate their performance and plan for the future,” Miller says. “We use their questions as source material for this survey, so we can help them answer questions like, ‘How are most hospitalists participating in QI?’ or ‘How are other hospitalists using part-time staff members?’ ”
Hospitalists Lead the Way
Hospitalists continue to be at the forefront of QI initiatives within their hospitals, according to the latest survey. Almost all respondents (96.5%) reported that their HMG participated in QI programs; the average HMG has six hospitalists playing an active role in QI within the hospital.
The survey also found that 72.1% of respondents involved in QI activity reported that their hospitalists were “responsible for leading project(s)” on QI initiatives.
“The findings about the active role hospitalists play in QI initiatives may surprise even the most staunch advocate of QI within the hospital medicine specialty,” says Leslie Flores, MHA, SHM’s director of the Practice Management Institute and leader of the Focused Survey research. “In essence, it shows that nearly every hospitalist group is active in promoting QI, and that the vast majority of them are taking a leadership position to improve quality. … It is remarkable and extremely exciting that hospitalists are so deeply involved in QI in their organizations.”
The survey identified patient safety, clinical QI, and quality-related IT initiatives as most popular.
Quality Incentive Compensation
In order to track HMG quality incentive compensation, the 2008-2009 Focused Survey asked similar questions about the topic to questions in the 2006-2007 Focused Survey. Quality incentive compensation—paying bonuses or additional payments for meeting QI measures—not only increased markedly in the past two years, but a majority of HMGs also have adopted the practice. The number of HMGs that have quality incentive compensation plans has increased by 39% since 2006, according to the survey.
Nine out of 10 HMGs that receive performance-based compensation reported that the source of the compensation was the hospital or health system. In most cases, the compensation was paid to an individual hospitalist, which represents a shift from 2006, when more groups reported receiving the compensation directly.
The survey also shows that hospitals and HMGs use a number of process measures to evaluate QI incentives, including participation in quality or safety committees, transition of care measures, or core measures for heart failure, pneumonia, and acute myocardial infarction.
New Numbers Dispel High Turnover Myth
For years, the conventional wisdom throughout the healthcare community has been that HM suffers from a high turnover rate among its hospitalists. Focused Survey findings suggest otherwise. In fact, turnover rates for hospitalist groups have remained constant since 2005. Nearly a third (31.7%) of HMGs reported no turnover at all within the past 12 months.
“Getting an accurate idea about turnover in hospitalist groups has been an ongoing challenge in our research,” Flores says. “In this year’s Focused Survey, we provided clearer definitions and asked more specific questions to improve our measurement of turnover.”
The added specificity only served to reinforce findings from previous surveys that showed relatively low turnover rates. The most recent research revealed a 12.7% turnover rate, compared with 13% in 2007 and 12% in 2005.
The latest Focused Survey also includes detailed findings on turnover among full-time hospitalists compared with part-time hospitalists.
Part-Time vs. Full-Time
The new data challenge long-held assumptions about the role of part-time hospitalists. The survey queried HMGs about full-time and part-time hospitalist staff, and the proportion of time that each employee covers in the hospital.
Although there isn’t a consensus about what constitutes a full-time hospitalist, it is clear that they cover the vast majority (85%) of HMG staff hours. Part-time hospitalists are responsible for 10% of hospitalist staff hours, and “casual” hospitalists—temporary hospitalists or moonlighters—make up the remaining 5%.
Part-time hospitalists share the same responsibilities as their full-time colleagues, according to the report. More than 70% of HMG leaders said their part-time staff is deployed to cover the same shifts and responsibilities as full-time staff. Many HMGs use part-time staff to cover night and weekend shifts.
Trend Today, Initiative Tomorrow
Taken together, SHM’s bi-annual survey and Focused Survey have begun to reveal some of the most prevalent trends within the specialty, including low turnover and a specialty-wide QI emphasis. However, Flores sees room for additional research in the near future.
“There is a lot more to learn about the nature of hospitalists’ involvement in organizational quality initiatives and what benefits that involvement is delivering to their organizations,” she says. “The survey suggests some areas, particularly in the quality arena, where SHM can develop additional programs and services to support hospitalists and the work they do.”
The 10-page 2008-2009 Focused Survey report is available at www.hospitalmedicine.org/shmstore. TH
Brendon Shank is a freelance writer based in Philadelphia.
Most HM groups (HMGs) participate in quality initiatives in their hospitals, according to new SHM research. Moreover, 7 out of 10 HMGs participating in QI initiatives are leading those efforts at their hospitals.
The findings are part of SHM’s 2008-2009 Focused Survey, the latest in a series of reports commissioned by the Practice Analysis Committee. The survey and report concentrate on topics of interest from SHM’s comprehensive, biannual survey of its membership.
The survey compiled responses from 145 HMG leaders. In addition to QI initiatives, participants in the survey responded to a variety of questions, including quality-based incentives, hospitalist turnover, and the use of part-time hospitalists.

—Joe Miller, SHM’s executive advisor to the CEO
“This is certain to be a conversation starter for hospitalists, hospital executives, and others,” says Burke Kealey, MD, FHM, medical director for hospital medicine at St. Paul, Minn.-based HealthPartners and chair of SHM’s Practice Analysis Committee. “The Focused Survey is an opportunity for SHM to answer some of the pressing questions that healthcare executives and providers have about managing a hospitalist practice within the larger context of the hospital.”
Hospital executives and hospitalists use SHM survey findings to better understand what is going on in the specialty, says Joe Miller, SHM’s executive advisor to the CEO. “These surveys answer the kinds of questions that often come up when hospitalists and hospitals begin to evaluate their performance and plan for the future,” Miller says. “We use their questions as source material for this survey, so we can help them answer questions like, ‘How are most hospitalists participating in QI?’ or ‘How are other hospitalists using part-time staff members?’ ”
Hospitalists Lead the Way
Hospitalists continue to be at the forefront of QI initiatives within their hospitals, according to the latest survey. Almost all respondents (96.5%) reported that their HMG participated in QI programs; the average HMG has six hospitalists playing an active role in QI within the hospital.
The survey also found that 72.1% of respondents involved in QI activity reported that their hospitalists were “responsible for leading project(s)” on QI initiatives.
“The findings about the active role hospitalists play in QI initiatives may surprise even the most staunch advocate of QI within the hospital medicine specialty,” says Leslie Flores, MHA, SHM’s director of the Practice Management Institute and leader of the Focused Survey research. “In essence, it shows that nearly every hospitalist group is active in promoting QI, and that the vast majority of them are taking a leadership position to improve quality. … It is remarkable and extremely exciting that hospitalists are so deeply involved in QI in their organizations.”
The survey identified patient safety, clinical QI, and quality-related IT initiatives as most popular.
Quality Incentive Compensation
In order to track HMG quality incentive compensation, the 2008-2009 Focused Survey asked similar questions about the topic to questions in the 2006-2007 Focused Survey. Quality incentive compensation—paying bonuses or additional payments for meeting QI measures—not only increased markedly in the past two years, but a majority of HMGs also have adopted the practice. The number of HMGs that have quality incentive compensation plans has increased by 39% since 2006, according to the survey.
Nine out of 10 HMGs that receive performance-based compensation reported that the source of the compensation was the hospital or health system. In most cases, the compensation was paid to an individual hospitalist, which represents a shift from 2006, when more groups reported receiving the compensation directly.
The survey also shows that hospitals and HMGs use a number of process measures to evaluate QI incentives, including participation in quality or safety committees, transition of care measures, or core measures for heart failure, pneumonia, and acute myocardial infarction.
New Numbers Dispel High Turnover Myth
For years, the conventional wisdom throughout the healthcare community has been that HM suffers from a high turnover rate among its hospitalists. Focused Survey findings suggest otherwise. In fact, turnover rates for hospitalist groups have remained constant since 2005. Nearly a third (31.7%) of HMGs reported no turnover at all within the past 12 months.
“Getting an accurate idea about turnover in hospitalist groups has been an ongoing challenge in our research,” Flores says. “In this year’s Focused Survey, we provided clearer definitions and asked more specific questions to improve our measurement of turnover.”
The added specificity only served to reinforce findings from previous surveys that showed relatively low turnover rates. The most recent research revealed a 12.7% turnover rate, compared with 13% in 2007 and 12% in 2005.
The latest Focused Survey also includes detailed findings on turnover among full-time hospitalists compared with part-time hospitalists.
Part-Time vs. Full-Time
The new data challenge long-held assumptions about the role of part-time hospitalists. The survey queried HMGs about full-time and part-time hospitalist staff, and the proportion of time that each employee covers in the hospital.
Although there isn’t a consensus about what constitutes a full-time hospitalist, it is clear that they cover the vast majority (85%) of HMG staff hours. Part-time hospitalists are responsible for 10% of hospitalist staff hours, and “casual” hospitalists—temporary hospitalists or moonlighters—make up the remaining 5%.
Part-time hospitalists share the same responsibilities as their full-time colleagues, according to the report. More than 70% of HMG leaders said their part-time staff is deployed to cover the same shifts and responsibilities as full-time staff. Many HMGs use part-time staff to cover night and weekend shifts.
Trend Today, Initiative Tomorrow
Taken together, SHM’s bi-annual survey and Focused Survey have begun to reveal some of the most prevalent trends within the specialty, including low turnover and a specialty-wide QI emphasis. However, Flores sees room for additional research in the near future.
“There is a lot more to learn about the nature of hospitalists’ involvement in organizational quality initiatives and what benefits that involvement is delivering to their organizations,” she says. “The survey suggests some areas, particularly in the quality arena, where SHM can develop additional programs and services to support hospitalists and the work they do.”
The 10-page 2008-2009 Focused Survey report is available at www.hospitalmedicine.org/shmstore. TH
Brendon Shank is a freelance writer based in Philadelphia.
2010: HM Goes to Washington
Enter text here
Enter text here
Enter text here
SHM’s Down with Digital
When hospitalist Robert Wachter, MD, FHM, started his HM blog almost two years ago, he didn’t anticipate that one of his blog entries would be about pop-music icon Britney Spears. Or that it would become his most popular, attracting nearly double the number of readers as his next-most-popular post.
Dr. Wachter—professor and chief of the division of hospital medicine at the University of California at San Francisco, a former SHM president, and author of the blog “Wachter’s World” (www.wachtersworld.com)—attributes the popularity of that post partly to Spears, but also to the fact it touched on a topic that always sparks interest among hospitalists, other healthcare providers, and hospital executives: the relationship between doctors and nurses in a hospital setting. Dr. Wachter’s most-popular post used Spears’ hospitalization in early 2008 and the controversy surrounding care providers who sneaked a peek at her medical records to make a point about how physicians and nurses often are treated differently in a hospital setting.
—Robert Chang, MD, hospitalist, University of Michigan Medical Center, Ann Arbor
But that was just one story. In the first year alone, Dr. Wachter wrote 76 blog posts, each of which easily exceeded 1,000 words. During the first year of blogging, the average post was read more than 1,800 times and the Web site attracted nearly 140,000 views.
“This has been one of the most gratifying things I’ve done in my career,” Dr. Wachter says. “I’ve published hundreds of articles in journals, but something about this form has an immediacy and connection to the audience that feels very important.”
And he isn’t alone. Blogs and HM have experienced similar growth trajectories in recent years. Now they are coming together to help hospitalists understand the most pressing issues in the specialty and provide the best care to hospitalized patients.
A Blog Primer
Blogs are Web sites that feature regular articles, or “posts.” The topic, length, and regularity of the posts are entirely at the discretion of the author, also known as the blogger. Some blogs are updated dozens of times a day; others, such as Wachter’s World, only feature new posts every week or so, but often with more depth and insight.
Although initially dismissed by many as outlets for trivial information, blogs are now recognized by experts in nearly every field as an important and cost-effective way to spark conversation and take positions on issues of the day.
Compared with more traditional media outlets, the ability to create dialogue is perhaps the most distinctive blog characteristic. Bloggers often invite readers to post or e-mail comments, creating interactivity between author and reader. In addition, many blogs automatically e-mail and distribute new blog posts to subscribers.
The “viral” aspect of blogs is a major contributor to their success. For instance, say Dr. Wachter writes a new blog post at 8:30 in the morning. Shortly thereafter, his readers will receive an automatically generated e-mail from the blog informing readers that Dr. Wachter has posted a new blog entry. When the reader visits the blog and reads the new post, they might think it could be of interest to a colleague, so they forward it to a colleague via e-mail. The colleague not only reads the article, but they also are impressed and post a comment for the rest of the blog’s readers to view.
SHM Blogs Advance the Specialty
The feedback loop of blogs isn’t limited to the on-screen world. That’s the lesson learned by clinical hospitalist Danielle Scheurer, MD, MSCR, SHM’s Web editor and director of General Medical Services at Brigham and Women’s Hospital in Boston.
As the author of SHM’s new clinical practice blog, “Hospital Medicine Quick Hits,” Dr. Scheurer knew the fledgling blog provided a valuable resource to busy clinicians, but she didn’t expect it to get back to her. She recalls that one day, “my blog was quoted to me by one of my house staff, who said, ‘I found this great hospital medicine blog today,’ and he didn’t realize I was the author.”
For the blog, Scheurer scours through 50 of the top medical journals for articles that are relevant to practicing clinical hospitalists. She posts concise overviews of the articles, along with links to the original research.
For hospitalists who have an interest in practice management, SHM offers another new blog, “The Hospitalist Leader.” It shares perspectives and ideas on the day-to-day interactions that hospitalists encounter and how best to administer a hospital practice. Four hospitalist co-authors—Robert Chang, MD, FHM, a hospitalist at the University of Michigan Medical Center in Ann Arbor; Rusty Holman, MD, FHM, chief operating officer of Brentwood, Tenn.-based Cogent Healthcare; John Nelson, MD, FHM, principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm; and Robert Bessler, MD, FHM, a hospitalist with Sound Inpatient Physicians in Tacoma, Wash.—use many of their own experiences in the hospital as raw material for the blog.
Dr. Chang views the blog as another way to move HM forward: “I trust and hope that we can use the blog to help the professional status of our profession, as this ultimately will determine the choices we make, large and small,” he says.
What’s Next
If you’re attending HM09 this year, don’t be surprised if you see someone else in the crowd excitedly typing into an iPhone or BlackBerry. You just might find a new blog post on the session you just attended.
Gone are the old images of a blogger in slippers and pajamas stealthily typing on the computer in the basement. These days, posting at or during an event, on site and in real time, is standard practice for many bloggers. In fact, SHM made a concerted effort to invite the most influential bloggers in the industry to HM09.
And if the person typing away isn’t “live blogging,” he may be “tweeting,” or adding super-short updates to the popular Web site Twitter. For many bloggers, it’s a way of communicating instantaneously with their audiences; once they post a blog article, they “tweet”—or send out—the link to thousands of readers.
SHM has its own Twitter account—@SHMLive—and uses the account to keep interested hospitalists updated on new blog posts, society news, and other HM developments.
“Hospital medicine is constantly evolving,” says Heather Abdel-Salam, SHM’s public relations and marketing coordinator, “and so do our efforts t.o communicate the best practices in the specialty. Blogs, Twitter feeds, and other online outreach are a big part of how we promote hospital medicine and help it grow within the healthcare arena.” TH
Brendon Shank is a freelance writer based in Philadelphia.
When hospitalist Robert Wachter, MD, FHM, started his HM blog almost two years ago, he didn’t anticipate that one of his blog entries would be about pop-music icon Britney Spears. Or that it would become his most popular, attracting nearly double the number of readers as his next-most-popular post.
Dr. Wachter—professor and chief of the division of hospital medicine at the University of California at San Francisco, a former SHM president, and author of the blog “Wachter’s World” (www.wachtersworld.com)—attributes the popularity of that post partly to Spears, but also to the fact it touched on a topic that always sparks interest among hospitalists, other healthcare providers, and hospital executives: the relationship between doctors and nurses in a hospital setting. Dr. Wachter’s most-popular post used Spears’ hospitalization in early 2008 and the controversy surrounding care providers who sneaked a peek at her medical records to make a point about how physicians and nurses often are treated differently in a hospital setting.
—Robert Chang, MD, hospitalist, University of Michigan Medical Center, Ann Arbor
But that was just one story. In the first year alone, Dr. Wachter wrote 76 blog posts, each of which easily exceeded 1,000 words. During the first year of blogging, the average post was read more than 1,800 times and the Web site attracted nearly 140,000 views.
“This has been one of the most gratifying things I’ve done in my career,” Dr. Wachter says. “I’ve published hundreds of articles in journals, but something about this form has an immediacy and connection to the audience that feels very important.”
And he isn’t alone. Blogs and HM have experienced similar growth trajectories in recent years. Now they are coming together to help hospitalists understand the most pressing issues in the specialty and provide the best care to hospitalized patients.
A Blog Primer
Blogs are Web sites that feature regular articles, or “posts.” The topic, length, and regularity of the posts are entirely at the discretion of the author, also known as the blogger. Some blogs are updated dozens of times a day; others, such as Wachter’s World, only feature new posts every week or so, but often with more depth and insight.
Although initially dismissed by many as outlets for trivial information, blogs are now recognized by experts in nearly every field as an important and cost-effective way to spark conversation and take positions on issues of the day.
Compared with more traditional media outlets, the ability to create dialogue is perhaps the most distinctive blog characteristic. Bloggers often invite readers to post or e-mail comments, creating interactivity between author and reader. In addition, many blogs automatically e-mail and distribute new blog posts to subscribers.
The “viral” aspect of blogs is a major contributor to their success. For instance, say Dr. Wachter writes a new blog post at 8:30 in the morning. Shortly thereafter, his readers will receive an automatically generated e-mail from the blog informing readers that Dr. Wachter has posted a new blog entry. When the reader visits the blog and reads the new post, they might think it could be of interest to a colleague, so they forward it to a colleague via e-mail. The colleague not only reads the article, but they also are impressed and post a comment for the rest of the blog’s readers to view.
SHM Blogs Advance the Specialty
The feedback loop of blogs isn’t limited to the on-screen world. That’s the lesson learned by clinical hospitalist Danielle Scheurer, MD, MSCR, SHM’s Web editor and director of General Medical Services at Brigham and Women’s Hospital in Boston.
As the author of SHM’s new clinical practice blog, “Hospital Medicine Quick Hits,” Dr. Scheurer knew the fledgling blog provided a valuable resource to busy clinicians, but she didn’t expect it to get back to her. She recalls that one day, “my blog was quoted to me by one of my house staff, who said, ‘I found this great hospital medicine blog today,’ and he didn’t realize I was the author.”
For the blog, Scheurer scours through 50 of the top medical journals for articles that are relevant to practicing clinical hospitalists. She posts concise overviews of the articles, along with links to the original research.
For hospitalists who have an interest in practice management, SHM offers another new blog, “The Hospitalist Leader.” It shares perspectives and ideas on the day-to-day interactions that hospitalists encounter and how best to administer a hospital practice. Four hospitalist co-authors—Robert Chang, MD, FHM, a hospitalist at the University of Michigan Medical Center in Ann Arbor; Rusty Holman, MD, FHM, chief operating officer of Brentwood, Tenn.-based Cogent Healthcare; John Nelson, MD, FHM, principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm; and Robert Bessler, MD, FHM, a hospitalist with Sound Inpatient Physicians in Tacoma, Wash.—use many of their own experiences in the hospital as raw material for the blog.
Dr. Chang views the blog as another way to move HM forward: “I trust and hope that we can use the blog to help the professional status of our profession, as this ultimately will determine the choices we make, large and small,” he says.
What’s Next
If you’re attending HM09 this year, don’t be surprised if you see someone else in the crowd excitedly typing into an iPhone or BlackBerry. You just might find a new blog post on the session you just attended.
Gone are the old images of a blogger in slippers and pajamas stealthily typing on the computer in the basement. These days, posting at or during an event, on site and in real time, is standard practice for many bloggers. In fact, SHM made a concerted effort to invite the most influential bloggers in the industry to HM09.
And if the person typing away isn’t “live blogging,” he may be “tweeting,” or adding super-short updates to the popular Web site Twitter. For many bloggers, it’s a way of communicating instantaneously with their audiences; once they post a blog article, they “tweet”—or send out—the link to thousands of readers.
SHM has its own Twitter account—@SHMLive—and uses the account to keep interested hospitalists updated on new blog posts, society news, and other HM developments.
“Hospital medicine is constantly evolving,” says Heather Abdel-Salam, SHM’s public relations and marketing coordinator, “and so do our efforts t.o communicate the best practices in the specialty. Blogs, Twitter feeds, and other online outreach are a big part of how we promote hospital medicine and help it grow within the healthcare arena.” TH
Brendon Shank is a freelance writer based in Philadelphia.
When hospitalist Robert Wachter, MD, FHM, started his HM blog almost two years ago, he didn’t anticipate that one of his blog entries would be about pop-music icon Britney Spears. Or that it would become his most popular, attracting nearly double the number of readers as his next-most-popular post.
Dr. Wachter—professor and chief of the division of hospital medicine at the University of California at San Francisco, a former SHM president, and author of the blog “Wachter’s World” (www.wachtersworld.com)—attributes the popularity of that post partly to Spears, but also to the fact it touched on a topic that always sparks interest among hospitalists, other healthcare providers, and hospital executives: the relationship between doctors and nurses in a hospital setting. Dr. Wachter’s most-popular post used Spears’ hospitalization in early 2008 and the controversy surrounding care providers who sneaked a peek at her medical records to make a point about how physicians and nurses often are treated differently in a hospital setting.
—Robert Chang, MD, hospitalist, University of Michigan Medical Center, Ann Arbor
But that was just one story. In the first year alone, Dr. Wachter wrote 76 blog posts, each of which easily exceeded 1,000 words. During the first year of blogging, the average post was read more than 1,800 times and the Web site attracted nearly 140,000 views.
“This has been one of the most gratifying things I’ve done in my career,” Dr. Wachter says. “I’ve published hundreds of articles in journals, but something about this form has an immediacy and connection to the audience that feels very important.”
And he isn’t alone. Blogs and HM have experienced similar growth trajectories in recent years. Now they are coming together to help hospitalists understand the most pressing issues in the specialty and provide the best care to hospitalized patients.
A Blog Primer
Blogs are Web sites that feature regular articles, or “posts.” The topic, length, and regularity of the posts are entirely at the discretion of the author, also known as the blogger. Some blogs are updated dozens of times a day; others, such as Wachter’s World, only feature new posts every week or so, but often with more depth and insight.
Although initially dismissed by many as outlets for trivial information, blogs are now recognized by experts in nearly every field as an important and cost-effective way to spark conversation and take positions on issues of the day.
Compared with more traditional media outlets, the ability to create dialogue is perhaps the most distinctive blog characteristic. Bloggers often invite readers to post or e-mail comments, creating interactivity between author and reader. In addition, many blogs automatically e-mail and distribute new blog posts to subscribers.
The “viral” aspect of blogs is a major contributor to their success. For instance, say Dr. Wachter writes a new blog post at 8:30 in the morning. Shortly thereafter, his readers will receive an automatically generated e-mail from the blog informing readers that Dr. Wachter has posted a new blog entry. When the reader visits the blog and reads the new post, they might think it could be of interest to a colleague, so they forward it to a colleague via e-mail. The colleague not only reads the article, but they also are impressed and post a comment for the rest of the blog’s readers to view.
SHM Blogs Advance the Specialty
The feedback loop of blogs isn’t limited to the on-screen world. That’s the lesson learned by clinical hospitalist Danielle Scheurer, MD, MSCR, SHM’s Web editor and director of General Medical Services at Brigham and Women’s Hospital in Boston.
As the author of SHM’s new clinical practice blog, “Hospital Medicine Quick Hits,” Dr. Scheurer knew the fledgling blog provided a valuable resource to busy clinicians, but she didn’t expect it to get back to her. She recalls that one day, “my blog was quoted to me by one of my house staff, who said, ‘I found this great hospital medicine blog today,’ and he didn’t realize I was the author.”
For the blog, Scheurer scours through 50 of the top medical journals for articles that are relevant to practicing clinical hospitalists. She posts concise overviews of the articles, along with links to the original research.
For hospitalists who have an interest in practice management, SHM offers another new blog, “The Hospitalist Leader.” It shares perspectives and ideas on the day-to-day interactions that hospitalists encounter and how best to administer a hospital practice. Four hospitalist co-authors—Robert Chang, MD, FHM, a hospitalist at the University of Michigan Medical Center in Ann Arbor; Rusty Holman, MD, FHM, chief operating officer of Brentwood, Tenn.-based Cogent Healthcare; John Nelson, MD, FHM, principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm; and Robert Bessler, MD, FHM, a hospitalist with Sound Inpatient Physicians in Tacoma, Wash.—use many of their own experiences in the hospital as raw material for the blog.
Dr. Chang views the blog as another way to move HM forward: “I trust and hope that we can use the blog to help the professional status of our profession, as this ultimately will determine the choices we make, large and small,” he says.
What’s Next
If you’re attending HM09 this year, don’t be surprised if you see someone else in the crowd excitedly typing into an iPhone or BlackBerry. You just might find a new blog post on the session you just attended.
Gone are the old images of a blogger in slippers and pajamas stealthily typing on the computer in the basement. These days, posting at or during an event, on site and in real time, is standard practice for many bloggers. In fact, SHM made a concerted effort to invite the most influential bloggers in the industry to HM09.
And if the person typing away isn’t “live blogging,” he may be “tweeting,” or adding super-short updates to the popular Web site Twitter. For many bloggers, it’s a way of communicating instantaneously with their audiences; once they post a blog article, they “tweet”—or send out—the link to thousands of readers.
SHM has its own Twitter account—@SHMLive—and uses the account to keep interested hospitalists updated on new blog posts, society news, and other HM developments.
“Hospital medicine is constantly evolving,” says Heather Abdel-Salam, SHM’s public relations and marketing coordinator, “and so do our efforts t.o communicate the best practices in the specialty. Blogs, Twitter feeds, and other online outreach are a big part of how we promote hospital medicine and help it grow within the healthcare arena.” TH
Brendon Shank is a freelance writer based in Philadelphia.
VTE Awareness Month
Jason Stein, MD, knows he could walk into almost any nursing unit in any hospital in the country, ask a simple question, and get blank stares in return.
“I would ask, ‘Which patients here in the nursing unit don’t have an order for VTE prophylaxis?’ ” says Dr. Stein, associate director for quality improvement and assistant professor of medicine at Emory University School of Medicine in Atlanta. “And they would tell me, ‘What kind of place do you think this is? How can we possibly know that?’ ”
It’s not idle chat. Venous thromboembolism (VTE) is a condition known throughout HM for three things: It runs rampant in hospitals; it can be deadly; and it’s easily preventable.
This month, SHM—along with dozens of other healthcare organizations, including the Agency for Healthcare Research Quality (AHRQ)—is highlighting the dangers of VTE and deep vein thrombosis (DVT), and promoting best practices to prevent them.
“SHM’s leadership of awareness efforts and championing VTE [prevention] has played an important role in keeping this on everybody’s mind,” Dr. Stein says.
VTE: A Hospital-Based Epidemic
Although it is easy to target at-risk populations and prevent it, VTE is widespread and dangerous.
“By published estimates, each year VTE kills more people than HIV, car accidents, and breast cancer combined,” says Gregory A. Maynard, MD, Ms, chief of the division of hospital medicine and clinical professor of medicine at the University of California at San Diego.
The risk of VTE in hospital patients should give hospitalists and their colleagues pause. Here’s why:
- According to the American Heart Association, more than 200,000 cases of VTE are reported each year, and VTE occurs for the first time in approximately 100 out of every 100,000 persons each year;
- Research published last year in The Lancet estimates 52% of hospitalized patients are at risk for VTE;
- 1 in 3 VTE patients experiences a pulmonary embolism;
- 30% of new VTE patients die within three days;
- 20% of new VTE patients die suddenly from pulmonary embolus; and
- DVT is responsible for approximately 8,000 hospital discharges every year. Pulmonary embolism accounts for nearly 100,000.
Risk Factors and Prevention
In a hospital setting, VTE risk factors are especially straightforward to monitor and prevent, but Dr. Maynard sees room for improvement.
“We don’t need to do better things; we need to do things better,” he told colleagues at a recent grand rounds. “Pharmacologic prophylaxis is the preferred way to prevent VTE in the hospital, which can reduce DVT and pulmonary embolism by 50% to 65%.”
Most hospital patients have at least one of these VTE risk factors, which are sorted into three categories:
- Stasis: conditions such as advanced age, immobility, paralysis, or stroke;
- Hypercoaguability: smoking, pregnancy, cancer, or sepsis; and
- Endothelial damage: surgery, prior VTE, central lines, or trauma.
Because the potential VTE risk is so high in hospital patients, the assessment must go hand in hand with prophylaxis, says Dr. Maynard and other hospitalists working with VTE.
Recent research has shown that prescribing medications to prevent VTE before it begins is safe, effective, and cost-effective.
The Hospitalist’s Role
The responsibility for VTE risk assessment and prevention often falls to hospitalists. In its online VTE Resource Room, SHM provides information for hospitalists working to assess and prevent VTE in their patients. It also provides a complete toolkit for hospitalists interested in addressing VTE prevention systematically throughout their hospitals. The toolkit is part of a comprehensive VTE Prevention Collaborative, which provides real-world mentoring and materials to hospitalists as they develop VTE monitoring and prevention programs.
“In 2005, when SHM set up the Quality Improvement resource room, we began with VTE prophylaxis,” Dr. Stein says. “VTE is the No. 1 cause of preventable death in hospitals, and preventing it is a fundamentally simple thing for hospitalists to do. We’re trying to get physicians to order a shot in the abdomen once a day. … If we can’t do that, we’re in trouble. On the flipside, if we can figure that out, we can derive mechanisms that we can apply to more complex problems in care.”
Together with SHM, Drs. Stein and Maynard have pioneered a two-pronged approach known as “measure-vention.” The underlying principal of measure-vention is that monitoring for VTE risk in real time can empower hospital staff to remedy issues in real time. In most hospitals, VTE risk can only be measured retrospectively through quality improvement data, which can take months to collect.
SHM and Dr. Stein have implemented an information technology approach at five of Emory’s hospitals. Each facility assesses patients who don’t have VTE prophylaxis every hour. The data is distributed to nursing stations, where nurses and other providers can apply VTE interventions within minutes. The program has driven Emory’s VTE prophylaxis rates to more than 90%, and Dr. Stein is working to make the program exportable to other hospitals, with the help of funding and assistance from SHM.
“As the leader of the VTE prevention program at Emory hospitals, I hear lots of stories about preventable VTE—not just about patients, but from friends of friends and family members,” he says. “It’s extraordinary.” TH
Brendon Shank is a freelance writer based in Philadelphia.
Jason Stein, MD, knows he could walk into almost any nursing unit in any hospital in the country, ask a simple question, and get blank stares in return.
“I would ask, ‘Which patients here in the nursing unit don’t have an order for VTE prophylaxis?’ ” says Dr. Stein, associate director for quality improvement and assistant professor of medicine at Emory University School of Medicine in Atlanta. “And they would tell me, ‘What kind of place do you think this is? How can we possibly know that?’ ”
It’s not idle chat. Venous thromboembolism (VTE) is a condition known throughout HM for three things: It runs rampant in hospitals; it can be deadly; and it’s easily preventable.
This month, SHM—along with dozens of other healthcare organizations, including the Agency for Healthcare Research Quality (AHRQ)—is highlighting the dangers of VTE and deep vein thrombosis (DVT), and promoting best practices to prevent them.
“SHM’s leadership of awareness efforts and championing VTE [prevention] has played an important role in keeping this on everybody’s mind,” Dr. Stein says.
VTE: A Hospital-Based Epidemic
Although it is easy to target at-risk populations and prevent it, VTE is widespread and dangerous.
“By published estimates, each year VTE kills more people than HIV, car accidents, and breast cancer combined,” says Gregory A. Maynard, MD, Ms, chief of the division of hospital medicine and clinical professor of medicine at the University of California at San Diego.
The risk of VTE in hospital patients should give hospitalists and their colleagues pause. Here’s why:
- According to the American Heart Association, more than 200,000 cases of VTE are reported each year, and VTE occurs for the first time in approximately 100 out of every 100,000 persons each year;
- Research published last year in The Lancet estimates 52% of hospitalized patients are at risk for VTE;
- 1 in 3 VTE patients experiences a pulmonary embolism;
- 30% of new VTE patients die within three days;
- 20% of new VTE patients die suddenly from pulmonary embolus; and
- DVT is responsible for approximately 8,000 hospital discharges every year. Pulmonary embolism accounts for nearly 100,000.
Risk Factors and Prevention
In a hospital setting, VTE risk factors are especially straightforward to monitor and prevent, but Dr. Maynard sees room for improvement.
“We don’t need to do better things; we need to do things better,” he told colleagues at a recent grand rounds. “Pharmacologic prophylaxis is the preferred way to prevent VTE in the hospital, which can reduce DVT and pulmonary embolism by 50% to 65%.”
Most hospital patients have at least one of these VTE risk factors, which are sorted into three categories:
- Stasis: conditions such as advanced age, immobility, paralysis, or stroke;
- Hypercoaguability: smoking, pregnancy, cancer, or sepsis; and
- Endothelial damage: surgery, prior VTE, central lines, or trauma.
Because the potential VTE risk is so high in hospital patients, the assessment must go hand in hand with prophylaxis, says Dr. Maynard and other hospitalists working with VTE.
Recent research has shown that prescribing medications to prevent VTE before it begins is safe, effective, and cost-effective.
The Hospitalist’s Role
The responsibility for VTE risk assessment and prevention often falls to hospitalists. In its online VTE Resource Room, SHM provides information for hospitalists working to assess and prevent VTE in their patients. It also provides a complete toolkit for hospitalists interested in addressing VTE prevention systematically throughout their hospitals. The toolkit is part of a comprehensive VTE Prevention Collaborative, which provides real-world mentoring and materials to hospitalists as they develop VTE monitoring and prevention programs.
“In 2005, when SHM set up the Quality Improvement resource room, we began with VTE prophylaxis,” Dr. Stein says. “VTE is the No. 1 cause of preventable death in hospitals, and preventing it is a fundamentally simple thing for hospitalists to do. We’re trying to get physicians to order a shot in the abdomen once a day. … If we can’t do that, we’re in trouble. On the flipside, if we can figure that out, we can derive mechanisms that we can apply to more complex problems in care.”
Together with SHM, Drs. Stein and Maynard have pioneered a two-pronged approach known as “measure-vention.” The underlying principal of measure-vention is that monitoring for VTE risk in real time can empower hospital staff to remedy issues in real time. In most hospitals, VTE risk can only be measured retrospectively through quality improvement data, which can take months to collect.
SHM and Dr. Stein have implemented an information technology approach at five of Emory’s hospitals. Each facility assesses patients who don’t have VTE prophylaxis every hour. The data is distributed to nursing stations, where nurses and other providers can apply VTE interventions within minutes. The program has driven Emory’s VTE prophylaxis rates to more than 90%, and Dr. Stein is working to make the program exportable to other hospitals, with the help of funding and assistance from SHM.
“As the leader of the VTE prevention program at Emory hospitals, I hear lots of stories about preventable VTE—not just about patients, but from friends of friends and family members,” he says. “It’s extraordinary.” TH
Brendon Shank is a freelance writer based in Philadelphia.
Jason Stein, MD, knows he could walk into almost any nursing unit in any hospital in the country, ask a simple question, and get blank stares in return.
“I would ask, ‘Which patients here in the nursing unit don’t have an order for VTE prophylaxis?’ ” says Dr. Stein, associate director for quality improvement and assistant professor of medicine at Emory University School of Medicine in Atlanta. “And they would tell me, ‘What kind of place do you think this is? How can we possibly know that?’ ”
It’s not idle chat. Venous thromboembolism (VTE) is a condition known throughout HM for three things: It runs rampant in hospitals; it can be deadly; and it’s easily preventable.
This month, SHM—along with dozens of other healthcare organizations, including the Agency for Healthcare Research Quality (AHRQ)—is highlighting the dangers of VTE and deep vein thrombosis (DVT), and promoting best practices to prevent them.
“SHM’s leadership of awareness efforts and championing VTE [prevention] has played an important role in keeping this on everybody’s mind,” Dr. Stein says.
VTE: A Hospital-Based Epidemic
Although it is easy to target at-risk populations and prevent it, VTE is widespread and dangerous.
“By published estimates, each year VTE kills more people than HIV, car accidents, and breast cancer combined,” says Gregory A. Maynard, MD, Ms, chief of the division of hospital medicine and clinical professor of medicine at the University of California at San Diego.
The risk of VTE in hospital patients should give hospitalists and their colleagues pause. Here’s why:
- According to the American Heart Association, more than 200,000 cases of VTE are reported each year, and VTE occurs for the first time in approximately 100 out of every 100,000 persons each year;
- Research published last year in The Lancet estimates 52% of hospitalized patients are at risk for VTE;
- 1 in 3 VTE patients experiences a pulmonary embolism;
- 30% of new VTE patients die within three days;
- 20% of new VTE patients die suddenly from pulmonary embolus; and
- DVT is responsible for approximately 8,000 hospital discharges every year. Pulmonary embolism accounts for nearly 100,000.
Risk Factors and Prevention
In a hospital setting, VTE risk factors are especially straightforward to monitor and prevent, but Dr. Maynard sees room for improvement.
“We don’t need to do better things; we need to do things better,” he told colleagues at a recent grand rounds. “Pharmacologic prophylaxis is the preferred way to prevent VTE in the hospital, which can reduce DVT and pulmonary embolism by 50% to 65%.”
Most hospital patients have at least one of these VTE risk factors, which are sorted into three categories:
- Stasis: conditions such as advanced age, immobility, paralysis, or stroke;
- Hypercoaguability: smoking, pregnancy, cancer, or sepsis; and
- Endothelial damage: surgery, prior VTE, central lines, or trauma.
Because the potential VTE risk is so high in hospital patients, the assessment must go hand in hand with prophylaxis, says Dr. Maynard and other hospitalists working with VTE.
Recent research has shown that prescribing medications to prevent VTE before it begins is safe, effective, and cost-effective.
The Hospitalist’s Role
The responsibility for VTE risk assessment and prevention often falls to hospitalists. In its online VTE Resource Room, SHM provides information for hospitalists working to assess and prevent VTE in their patients. It also provides a complete toolkit for hospitalists interested in addressing VTE prevention systematically throughout their hospitals. The toolkit is part of a comprehensive VTE Prevention Collaborative, which provides real-world mentoring and materials to hospitalists as they develop VTE monitoring and prevention programs.
“In 2005, when SHM set up the Quality Improvement resource room, we began with VTE prophylaxis,” Dr. Stein says. “VTE is the No. 1 cause of preventable death in hospitals, and preventing it is a fundamentally simple thing for hospitalists to do. We’re trying to get physicians to order a shot in the abdomen once a day. … If we can’t do that, we’re in trouble. On the flipside, if we can figure that out, we can derive mechanisms that we can apply to more complex problems in care.”
Together with SHM, Drs. Stein and Maynard have pioneered a two-pronged approach known as “measure-vention.” The underlying principal of measure-vention is that monitoring for VTE risk in real time can empower hospital staff to remedy issues in real time. In most hospitals, VTE risk can only be measured retrospectively through quality improvement data, which can take months to collect.
SHM and Dr. Stein have implemented an information technology approach at five of Emory’s hospitals. Each facility assesses patients who don’t have VTE prophylaxis every hour. The data is distributed to nursing stations, where nurses and other providers can apply VTE interventions within minutes. The program has driven Emory’s VTE prophylaxis rates to more than 90%, and Dr. Stein is working to make the program exportable to other hospitals, with the help of funding and assistance from SHM.
“As the leader of the VTE prevention program at Emory hospitals, I hear lots of stories about preventable VTE—not just about patients, but from friends of friends and family members,” he says. “It’s extraordinary.” TH
Brendon Shank is a freelance writer based in Philadelphia.
Non-Physician Providers: Vital HM Resources
Enter text here
Enter text here
Enter text here
Project BOOST Expands
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions) is an initiative to improve practices in transition care and reduce readmission rates for hospitals across the country. The project’s toolkit, mentoring program, and national advocacy efforts have proven so successful that the program is expanding this year.
In 2008, SHM began the first round of the Project BOOST mentoring program in six pilot hospitals. The first full cycle of Project BOOST mentoring sites began in March at 24 sites. The Hospitalist will feature updates on the full cycle of Project BOOST later this year. For more information about Project BOOST, visit www.hospitalmedicine.org/BOOST or e-mail [email protected].
As a pilot site, Southwestern Vermont Medical Center in Bennington has worked with mentors for the past six months. We caught up with project leader Jennifer Fells, RN, MS, to discuss the institution’s participation.
—Jennifer Fells, RN, MS, Southwestern Vermont Medical Center, Bennington
Question: Why did your group choose to participate in the mentoring program?
Answer: We wanted to reduce our readmission rate, and we knew we weren’t doing a service to patients. This was also a goal of our organization overall; it’s not only a benefit to the hospital, but a larger value when the patient goes back to the community.
Q: How has the BOOST mentoring program benefited your program?
A: It helped us get organized by beginning the process and affirmed our belief that there were ways to address readmissions. The toolkit has proved to be invaluable. The mentors helped us keep on track and offered us guidance. They share the experiences of the other Project BOOST teams, and we benefit from that information.
The changes in the approach to the discharge process were a surprise to us. After we developed our team, we discovered how fragmented the discharge process was throughout the entire organization. Discharges were handled over multiple disciplines, and it was fragmented by design.
For example, our documentation, discharge plans, discharge recommendations, and patient-education materials are in different parts of our documentation system.
Q: What did you learn about your program through the initial Project BOOST step: analyze care delivery?
A: We realized that disciplines were not coordinated with one another and there was not enough time for the physician to complete the discharge plan. The process was cumbersome, awkward, and very time-consuming. We were looking to create efficiency in the information that needs to be coordinated to do those discharge orders.
Q: What additional changes do you hope to see in the remaining time with BOOST mentors?
A: We definitely hope to improve our process. We want to have implemented the tools and have a coordinated discharge process, and a centralized way to communicate the discharge plan. We found a lack of communication creates a barrier among disciplines, and we hope to correct that and become more customer-friendly to patients.
Q: How did your site’s BOOST mentor assist in the implementation process? What was the outcome?
A: Our site mentor helped with the clarification of data to be collected for measurement, keeping us on track with the toolkit, and served as another set of eyes. When you are in an organization, and even when you have the appropriate team, you always need somebody to say, “What do you think about this?” or “Did you think about this item?”
It’s another perspective, sharing gained knowledge from other organizations. That’s very critical.
SHM marketing coordinator Nadia Clenending contributed to this report.
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions) is an initiative to improve practices in transition care and reduce readmission rates for hospitals across the country. The project’s toolkit, mentoring program, and national advocacy efforts have proven so successful that the program is expanding this year.
In 2008, SHM began the first round of the Project BOOST mentoring program in six pilot hospitals. The first full cycle of Project BOOST mentoring sites began in March at 24 sites. The Hospitalist will feature updates on the full cycle of Project BOOST later this year. For more information about Project BOOST, visit www.hospitalmedicine.org/BOOST or e-mail [email protected].
As a pilot site, Southwestern Vermont Medical Center in Bennington has worked with mentors for the past six months. We caught up with project leader Jennifer Fells, RN, MS, to discuss the institution’s participation.
—Jennifer Fells, RN, MS, Southwestern Vermont Medical Center, Bennington
Question: Why did your group choose to participate in the mentoring program?
Answer: We wanted to reduce our readmission rate, and we knew we weren’t doing a service to patients. This was also a goal of our organization overall; it’s not only a benefit to the hospital, but a larger value when the patient goes back to the community.
Q: How has the BOOST mentoring program benefited your program?
A: It helped us get organized by beginning the process and affirmed our belief that there were ways to address readmissions. The toolkit has proved to be invaluable. The mentors helped us keep on track and offered us guidance. They share the experiences of the other Project BOOST teams, and we benefit from that information.
The changes in the approach to the discharge process were a surprise to us. After we developed our team, we discovered how fragmented the discharge process was throughout the entire organization. Discharges were handled over multiple disciplines, and it was fragmented by design.
For example, our documentation, discharge plans, discharge recommendations, and patient-education materials are in different parts of our documentation system.
Q: What did you learn about your program through the initial Project BOOST step: analyze care delivery?
A: We realized that disciplines were not coordinated with one another and there was not enough time for the physician to complete the discharge plan. The process was cumbersome, awkward, and very time-consuming. We were looking to create efficiency in the information that needs to be coordinated to do those discharge orders.
Q: What additional changes do you hope to see in the remaining time with BOOST mentors?
A: We definitely hope to improve our process. We want to have implemented the tools and have a coordinated discharge process, and a centralized way to communicate the discharge plan. We found a lack of communication creates a barrier among disciplines, and we hope to correct that and become more customer-friendly to patients.
Q: How did your site’s BOOST mentor assist in the implementation process? What was the outcome?
A: Our site mentor helped with the clarification of data to be collected for measurement, keeping us on track with the toolkit, and served as another set of eyes. When you are in an organization, and even when you have the appropriate team, you always need somebody to say, “What do you think about this?” or “Did you think about this item?”
It’s another perspective, sharing gained knowledge from other organizations. That’s very critical.
SHM marketing coordinator Nadia Clenending contributed to this report.
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions) is an initiative to improve practices in transition care and reduce readmission rates for hospitals across the country. The project’s toolkit, mentoring program, and national advocacy efforts have proven so successful that the program is expanding this year.
In 2008, SHM began the first round of the Project BOOST mentoring program in six pilot hospitals. The first full cycle of Project BOOST mentoring sites began in March at 24 sites. The Hospitalist will feature updates on the full cycle of Project BOOST later this year. For more information about Project BOOST, visit www.hospitalmedicine.org/BOOST or e-mail [email protected].
As a pilot site, Southwestern Vermont Medical Center in Bennington has worked with mentors for the past six months. We caught up with project leader Jennifer Fells, RN, MS, to discuss the institution’s participation.
—Jennifer Fells, RN, MS, Southwestern Vermont Medical Center, Bennington
Question: Why did your group choose to participate in the mentoring program?
Answer: We wanted to reduce our readmission rate, and we knew we weren’t doing a service to patients. This was also a goal of our organization overall; it’s not only a benefit to the hospital, but a larger value when the patient goes back to the community.
Q: How has the BOOST mentoring program benefited your program?
A: It helped us get organized by beginning the process and affirmed our belief that there were ways to address readmissions. The toolkit has proved to be invaluable. The mentors helped us keep on track and offered us guidance. They share the experiences of the other Project BOOST teams, and we benefit from that information.
The changes in the approach to the discharge process were a surprise to us. After we developed our team, we discovered how fragmented the discharge process was throughout the entire organization. Discharges were handled over multiple disciplines, and it was fragmented by design.
For example, our documentation, discharge plans, discharge recommendations, and patient-education materials are in different parts of our documentation system.
Q: What did you learn about your program through the initial Project BOOST step: analyze care delivery?
A: We realized that disciplines were not coordinated with one another and there was not enough time for the physician to complete the discharge plan. The process was cumbersome, awkward, and very time-consuming. We were looking to create efficiency in the information that needs to be coordinated to do those discharge orders.
Q: What additional changes do you hope to see in the remaining time with BOOST mentors?
A: We definitely hope to improve our process. We want to have implemented the tools and have a coordinated discharge process, and a centralized way to communicate the discharge plan. We found a lack of communication creates a barrier among disciplines, and we hope to correct that and become more customer-friendly to patients.
Q: How did your site’s BOOST mentor assist in the implementation process? What was the outcome?
A: Our site mentor helped with the clarification of data to be collected for measurement, keeping us on track with the toolkit, and served as another set of eyes. When you are in an organization, and even when you have the appropriate team, you always need somebody to say, “What do you think about this?” or “Did you think about this item?”
It’s another perspective, sharing gained knowledge from other organizations. That’s very critical.
SHM marketing coordinator Nadia Clenending contributed to this report.
For the Team
Many speakers at the recent SHM annual meeting in Dallas focused on the many ways hospitalists enhance quality of care. The teamwork necessary to effectively render inpatient services was an especially important topic.
Hospitalists have compiled a significant amount of descriptive material about their working environments and the composition and workloads of hospitalist teams. However, there is not much material available quantifying the ways that various disciplines impact the overall care-delivery metrics of multidisciplinary hospitalist teams.
The SHM Non-Physician Provider Committee is interested in collecting information on multidisciplinary programs, their component disciplines and individual providers to help identify and describe teams that have integrated nurse practitioners, physician assistants, clinical pharmacists and pharmacologists, nurse clinical care coordinators, and other related disciplines into their practices. Our goal is to develop descriptions of successful and unsuccessful implementation models.
We would also like to collect information measuring additional domains of interest to major stakeholders. Such domains might include the clinical utilization of non-physician providers in relationship to both scope-of-practice and delegation of authority, the influence of multidisciplinary integration on patient-centered care and patient satisfaction, process and outcomes quality metrics, throughput and efficiency measures, documentation practices, hospital privileges for non-physicians, medical education in the multidisciplinary environment, risk management and, of course, reimbursement.
One might ask why the collection and analysis of such data should be of interest to hospitalists and to SHM. There are several immediate answers:
- The first reason involves manpower. Hospital medicine has become a growing discipline for physicians—one that did not exist on the radar screens of physician planners 10 years ago. However, given the growing demand for hospitalists there may be a significant shortage. To address this deficit, hospital medicine practices will need to attract new associates in the form of nurse practitioners and physician assistants. It is therefore imperative that hospitalists proactively identify barriers to the integration of non-physician providers into their practices and have successful implementation models to guide this effort.
- The second reason centers on the fact that hospitalists will continue to lead efforts to enhance quality of care. Incorporating a multidisciplinary approach—whether through the pre-rounding and follow-up of nurse clinical care coordinators, the counsel of clinical pharmacists, or the hands-on care of other disciplines—will facilitate throughput and improve quality as well as enhance patient satisfaction and communication. Identifying best practices in these particular domains will provide information crucial to success in these areas.
- The third reason is related to the cost of services. With declining reimbursements coupled with increasing costs, hospital medicine programs must identify and implement measures aimed at expense control and maximization of services. Used appropriately, non-physician providers provide a lower-cost alternative to a physician-only model. When one-to-one pairing occurs, physician/NPP team-care can be delivered in a parallel-versus-linear fashion, thus allowing for increased census as well as expedition of care.
The future of hospital medicine is one of continued growth with the demand for hospital medicine physicians far outstripping the available supply to meet the ever-increasing needs. SHM is committed to researching and sharing best practices, and views the use of multidisciplinary teams as an important model of care. Together, we can all achieve more.
If you are interested in being a part of this project or feel that this data would be of benefit to your practice, please contact the Non-Physician Provider Committee at [email protected].
Chapter Reports
Nashville
Quite a bit of networking took place before the Medtronic-sponsored presentation at Ruth’s Chris in Nashville on April 26. The SHM Nashville Chapter has re-energized itself under the co-direction of Steven Embry, MD, and Kimberly Bell, MD. Eleven Nashville-area healthcare organizations were represented by more than 28 attendees. The attendees were a multidisciplinary mix of physicians, nurses, and administrators. Shashank Desai, MD, engaged the audience with his presentation “Simple to Complex: Advances in the Management of CHF.” Dr. Desai is the medical director of the Heart Failure and Transplant Program at Inova Fairfax Hospital.
Pacific Northwest
The latest Pacific Northwest Chapter meeting of SHM was held in Seattle on May 15. A change of venue and a new focus on speakers provided local hospitalists with information they won’t find elsewhere. Joseph Bennet, MD, former president of the local chapter, gave a presentation detailing his 15 months practicing hospitalist medicine in Dunedin, New Zealand. In addition to stunning photos of the terrain, Dr. Bennet delivered a thought-provoking presentation comparing New Zealand with the United States regarding culture, medical system financing, drug and care delivery, physician training, end-of-life issues, and many more aspects.
Pittsburgh
The Pittsburgh Chapter had a meeting May 10 at Morton’s Steakhouse. The speaker for the event was Rene Alvarez, MD, director of the Critical Care Unit at University of Pittsburgh Medical Center. Dr. Alvarez discussed “Strategies for Optimal Management of Patients with Heart Failure,” which generated an excellent discussion. Various hospital medicine topics including incentives, program structures, and 24/7 programs were also discussed. Attendees included hospitalists from six local hospitals. The next meeting will be held Oct. 30. For more information on the Pittsburgh Chapter, contact Michael Cratty, MD, PhD, at [email protected].
Rocky Mountain
The Rocky Mountain Chapter held its spring meeting May 3 at the Denver Colorado Downtown Aquarium. Chapter President Eugene Chu, MD, welcomed attendees and was followed by an update from the Rocky Mountain Chapter Public Policy Committee presented by Bob Brockmann, MD, MSc. Guest speakers for the night were Edward Maa, MD, who spoke about “Seizure Management in Hospitalized Patients” and Daniel Mogyoros, MD, whose presentation was titled “Updates in Infectious Disease for Hospital Medicine.” Attendees received two AMA PRA [Physician’s Recognition Award] Category 1 credits.
San Diego
At its June 5 meeting, San Diego’s chapter discussed real-time, evidence-based practice as a means to improve patient care and share new clinical evidence with colleagues. Online access during the presentation allowed the group to review several evidence resources: PubMed, the Physician’s Information and Education Resource, the American College of Physicians Journal Club, and National Guideline Clearing House using real patient cases. Dinner was served by Blue Coral Seafood and Spirits, and Novartis sponsored the event.
Upstate South Carolina
The second meeting of the Upstate S.C. Chapter was held May 15, with close to 20 physicians representing five hospitals in upstate South Carolina. Kenneth Leeper, MD, pulmonologist, presented information on ventilator-associated pneumonia. Following the presentation, the business meeting was opened by outgoing President Raja Paladugu, MD.
The following officers were elected for 2007:
- President: Zafar Hossain, MD;
- Vice President: Imran Shaikh, MD; and
- Secretary: Shawn Morrow, MD.
The group decided to meet on a quarterly basis, with the next meeting to be held in September. TH
Many speakers at the recent SHM annual meeting in Dallas focused on the many ways hospitalists enhance quality of care. The teamwork necessary to effectively render inpatient services was an especially important topic.
Hospitalists have compiled a significant amount of descriptive material about their working environments and the composition and workloads of hospitalist teams. However, there is not much material available quantifying the ways that various disciplines impact the overall care-delivery metrics of multidisciplinary hospitalist teams.
The SHM Non-Physician Provider Committee is interested in collecting information on multidisciplinary programs, their component disciplines and individual providers to help identify and describe teams that have integrated nurse practitioners, physician assistants, clinical pharmacists and pharmacologists, nurse clinical care coordinators, and other related disciplines into their practices. Our goal is to develop descriptions of successful and unsuccessful implementation models.
We would also like to collect information measuring additional domains of interest to major stakeholders. Such domains might include the clinical utilization of non-physician providers in relationship to both scope-of-practice and delegation of authority, the influence of multidisciplinary integration on patient-centered care and patient satisfaction, process and outcomes quality metrics, throughput and efficiency measures, documentation practices, hospital privileges for non-physicians, medical education in the multidisciplinary environment, risk management and, of course, reimbursement.
One might ask why the collection and analysis of such data should be of interest to hospitalists and to SHM. There are several immediate answers:
- The first reason involves manpower. Hospital medicine has become a growing discipline for physicians—one that did not exist on the radar screens of physician planners 10 years ago. However, given the growing demand for hospitalists there may be a significant shortage. To address this deficit, hospital medicine practices will need to attract new associates in the form of nurse practitioners and physician assistants. It is therefore imperative that hospitalists proactively identify barriers to the integration of non-physician providers into their practices and have successful implementation models to guide this effort.
- The second reason centers on the fact that hospitalists will continue to lead efforts to enhance quality of care. Incorporating a multidisciplinary approach—whether through the pre-rounding and follow-up of nurse clinical care coordinators, the counsel of clinical pharmacists, or the hands-on care of other disciplines—will facilitate throughput and improve quality as well as enhance patient satisfaction and communication. Identifying best practices in these particular domains will provide information crucial to success in these areas.
- The third reason is related to the cost of services. With declining reimbursements coupled with increasing costs, hospital medicine programs must identify and implement measures aimed at expense control and maximization of services. Used appropriately, non-physician providers provide a lower-cost alternative to a physician-only model. When one-to-one pairing occurs, physician/NPP team-care can be delivered in a parallel-versus-linear fashion, thus allowing for increased census as well as expedition of care.
The future of hospital medicine is one of continued growth with the demand for hospital medicine physicians far outstripping the available supply to meet the ever-increasing needs. SHM is committed to researching and sharing best practices, and views the use of multidisciplinary teams as an important model of care. Together, we can all achieve more.
If you are interested in being a part of this project or feel that this data would be of benefit to your practice, please contact the Non-Physician Provider Committee at [email protected].
Chapter Reports
Nashville
Quite a bit of networking took place before the Medtronic-sponsored presentation at Ruth’s Chris in Nashville on April 26. The SHM Nashville Chapter has re-energized itself under the co-direction of Steven Embry, MD, and Kimberly Bell, MD. Eleven Nashville-area healthcare organizations were represented by more than 28 attendees. The attendees were a multidisciplinary mix of physicians, nurses, and administrators. Shashank Desai, MD, engaged the audience with his presentation “Simple to Complex: Advances in the Management of CHF.” Dr. Desai is the medical director of the Heart Failure and Transplant Program at Inova Fairfax Hospital.
Pacific Northwest
The latest Pacific Northwest Chapter meeting of SHM was held in Seattle on May 15. A change of venue and a new focus on speakers provided local hospitalists with information they won’t find elsewhere. Joseph Bennet, MD, former president of the local chapter, gave a presentation detailing his 15 months practicing hospitalist medicine in Dunedin, New Zealand. In addition to stunning photos of the terrain, Dr. Bennet delivered a thought-provoking presentation comparing New Zealand with the United States regarding culture, medical system financing, drug and care delivery, physician training, end-of-life issues, and many more aspects.
Pittsburgh
The Pittsburgh Chapter had a meeting May 10 at Morton’s Steakhouse. The speaker for the event was Rene Alvarez, MD, director of the Critical Care Unit at University of Pittsburgh Medical Center. Dr. Alvarez discussed “Strategies for Optimal Management of Patients with Heart Failure,” which generated an excellent discussion. Various hospital medicine topics including incentives, program structures, and 24/7 programs were also discussed. Attendees included hospitalists from six local hospitals. The next meeting will be held Oct. 30. For more information on the Pittsburgh Chapter, contact Michael Cratty, MD, PhD, at [email protected].
Rocky Mountain
The Rocky Mountain Chapter held its spring meeting May 3 at the Denver Colorado Downtown Aquarium. Chapter President Eugene Chu, MD, welcomed attendees and was followed by an update from the Rocky Mountain Chapter Public Policy Committee presented by Bob Brockmann, MD, MSc. Guest speakers for the night were Edward Maa, MD, who spoke about “Seizure Management in Hospitalized Patients” and Daniel Mogyoros, MD, whose presentation was titled “Updates in Infectious Disease for Hospital Medicine.” Attendees received two AMA PRA [Physician’s Recognition Award] Category 1 credits.
San Diego
At its June 5 meeting, San Diego’s chapter discussed real-time, evidence-based practice as a means to improve patient care and share new clinical evidence with colleagues. Online access during the presentation allowed the group to review several evidence resources: PubMed, the Physician’s Information and Education Resource, the American College of Physicians Journal Club, and National Guideline Clearing House using real patient cases. Dinner was served by Blue Coral Seafood and Spirits, and Novartis sponsored the event.
Upstate South Carolina
The second meeting of the Upstate S.C. Chapter was held May 15, with close to 20 physicians representing five hospitals in upstate South Carolina. Kenneth Leeper, MD, pulmonologist, presented information on ventilator-associated pneumonia. Following the presentation, the business meeting was opened by outgoing President Raja Paladugu, MD.
The following officers were elected for 2007:
- President: Zafar Hossain, MD;
- Vice President: Imran Shaikh, MD; and
- Secretary: Shawn Morrow, MD.
The group decided to meet on a quarterly basis, with the next meeting to be held in September. TH
Many speakers at the recent SHM annual meeting in Dallas focused on the many ways hospitalists enhance quality of care. The teamwork necessary to effectively render inpatient services was an especially important topic.
Hospitalists have compiled a significant amount of descriptive material about their working environments and the composition and workloads of hospitalist teams. However, there is not much material available quantifying the ways that various disciplines impact the overall care-delivery metrics of multidisciplinary hospitalist teams.
The SHM Non-Physician Provider Committee is interested in collecting information on multidisciplinary programs, their component disciplines and individual providers to help identify and describe teams that have integrated nurse practitioners, physician assistants, clinical pharmacists and pharmacologists, nurse clinical care coordinators, and other related disciplines into their practices. Our goal is to develop descriptions of successful and unsuccessful implementation models.
We would also like to collect information measuring additional domains of interest to major stakeholders. Such domains might include the clinical utilization of non-physician providers in relationship to both scope-of-practice and delegation of authority, the influence of multidisciplinary integration on patient-centered care and patient satisfaction, process and outcomes quality metrics, throughput and efficiency measures, documentation practices, hospital privileges for non-physicians, medical education in the multidisciplinary environment, risk management and, of course, reimbursement.
One might ask why the collection and analysis of such data should be of interest to hospitalists and to SHM. There are several immediate answers:
- The first reason involves manpower. Hospital medicine has become a growing discipline for physicians—one that did not exist on the radar screens of physician planners 10 years ago. However, given the growing demand for hospitalists there may be a significant shortage. To address this deficit, hospital medicine practices will need to attract new associates in the form of nurse practitioners and physician assistants. It is therefore imperative that hospitalists proactively identify barriers to the integration of non-physician providers into their practices and have successful implementation models to guide this effort.
- The second reason centers on the fact that hospitalists will continue to lead efforts to enhance quality of care. Incorporating a multidisciplinary approach—whether through the pre-rounding and follow-up of nurse clinical care coordinators, the counsel of clinical pharmacists, or the hands-on care of other disciplines—will facilitate throughput and improve quality as well as enhance patient satisfaction and communication. Identifying best practices in these particular domains will provide information crucial to success in these areas.
- The third reason is related to the cost of services. With declining reimbursements coupled with increasing costs, hospital medicine programs must identify and implement measures aimed at expense control and maximization of services. Used appropriately, non-physician providers provide a lower-cost alternative to a physician-only model. When one-to-one pairing occurs, physician/NPP team-care can be delivered in a parallel-versus-linear fashion, thus allowing for increased census as well as expedition of care.
The future of hospital medicine is one of continued growth with the demand for hospital medicine physicians far outstripping the available supply to meet the ever-increasing needs. SHM is committed to researching and sharing best practices, and views the use of multidisciplinary teams as an important model of care. Together, we can all achieve more.
If you are interested in being a part of this project or feel that this data would be of benefit to your practice, please contact the Non-Physician Provider Committee at [email protected].
Chapter Reports
Nashville
Quite a bit of networking took place before the Medtronic-sponsored presentation at Ruth’s Chris in Nashville on April 26. The SHM Nashville Chapter has re-energized itself under the co-direction of Steven Embry, MD, and Kimberly Bell, MD. Eleven Nashville-area healthcare organizations were represented by more than 28 attendees. The attendees were a multidisciplinary mix of physicians, nurses, and administrators. Shashank Desai, MD, engaged the audience with his presentation “Simple to Complex: Advances in the Management of CHF.” Dr. Desai is the medical director of the Heart Failure and Transplant Program at Inova Fairfax Hospital.
Pacific Northwest
The latest Pacific Northwest Chapter meeting of SHM was held in Seattle on May 15. A change of venue and a new focus on speakers provided local hospitalists with information they won’t find elsewhere. Joseph Bennet, MD, former president of the local chapter, gave a presentation detailing his 15 months practicing hospitalist medicine in Dunedin, New Zealand. In addition to stunning photos of the terrain, Dr. Bennet delivered a thought-provoking presentation comparing New Zealand with the United States regarding culture, medical system financing, drug and care delivery, physician training, end-of-life issues, and many more aspects.
Pittsburgh
The Pittsburgh Chapter had a meeting May 10 at Morton’s Steakhouse. The speaker for the event was Rene Alvarez, MD, director of the Critical Care Unit at University of Pittsburgh Medical Center. Dr. Alvarez discussed “Strategies for Optimal Management of Patients with Heart Failure,” which generated an excellent discussion. Various hospital medicine topics including incentives, program structures, and 24/7 programs were also discussed. Attendees included hospitalists from six local hospitals. The next meeting will be held Oct. 30. For more information on the Pittsburgh Chapter, contact Michael Cratty, MD, PhD, at [email protected].
Rocky Mountain
The Rocky Mountain Chapter held its spring meeting May 3 at the Denver Colorado Downtown Aquarium. Chapter President Eugene Chu, MD, welcomed attendees and was followed by an update from the Rocky Mountain Chapter Public Policy Committee presented by Bob Brockmann, MD, MSc. Guest speakers for the night were Edward Maa, MD, who spoke about “Seizure Management in Hospitalized Patients” and Daniel Mogyoros, MD, whose presentation was titled “Updates in Infectious Disease for Hospital Medicine.” Attendees received two AMA PRA [Physician’s Recognition Award] Category 1 credits.
San Diego
At its June 5 meeting, San Diego’s chapter discussed real-time, evidence-based practice as a means to improve patient care and share new clinical evidence with colleagues. Online access during the presentation allowed the group to review several evidence resources: PubMed, the Physician’s Information and Education Resource, the American College of Physicians Journal Club, and National Guideline Clearing House using real patient cases. Dinner was served by Blue Coral Seafood and Spirits, and Novartis sponsored the event.
Upstate South Carolina
The second meeting of the Upstate S.C. Chapter was held May 15, with close to 20 physicians representing five hospitals in upstate South Carolina. Kenneth Leeper, MD, pulmonologist, presented information on ventilator-associated pneumonia. Following the presentation, the business meeting was opened by outgoing President Raja Paladugu, MD.
The following officers were elected for 2007:
- President: Zafar Hossain, MD;
- Vice President: Imran Shaikh, MD; and
- Secretary: Shawn Morrow, MD.
The group decided to meet on a quarterly basis, with the next meeting to be held in September. TH
The Inpatient with AIDS: What the Hospitalist Needs to Know
The opinions and assertions contained herein are those of the authors and are not to be construed as official or as reflecting the views of the Department of Defense, the Department of the Navy, or the naval services at large.
Introduction
An estimated 850,000 to 950,000 persons in the United States are living with human immunodeficiency virus (HIV), 280,000 of whom are unaware of their infection and another 43,000 of whom meet the definition of acquired immunodeficiency syndrome (AIDS) (www.cdc.gov). The use of highly active antiretroviral therapy (HAART) has produced significant declines in morbidity and mortality from AIDS. Compared with the first 2 decades of the HIV pandemic, the number of HIV-related hospital admissions has declined. However, recently, this rate of decline has markedly slowed (1-3). The reasons for this plateau are many including a steady number of admissions for complications related to HAART, treatment failures, and the overall increased prevalence of HIV infection. Not only will HIV-infected patients still frequently require admission to the hospital, but the complexity of their inpatient care will continue to increase with the advancements in multiple drug regimens, aging of the HIV-infected population, and the interaction of HIV infection with medical comorbidities, many of which are attributable to HAART.
The hospitalist caring for the inpatient with AIDS is presented with several challenges including not only the diagnosis and management of opportunistic infections, but also the complications of HAART. In this article we review the guidelines for the initiation and continuation of HAART in the hospital, review important clinical complications of antiretroviral therapy, and review conditions that may result in the hospitalization of AIDS patients.
Initiation of HAART in the Hospital
In those who do not have access to health care, the initial diagnosis of HIV infection frequently occurs during a hospitalization for an AIDS-defining illness. Initiation of antiretrovirals is contingent on several issues, including CD4 count, viral load, clinical status, likelihood of continued adherence, and the concurrent treatment of opportunistic infections (OIs). All patients with HIV infection and a CD4 count <200 cells/mm3 or an AIDS-defining illness should receive antiretroviral therapy. Controversy exists as to whether a patient admitted for the treatment of an opportunistic infection should begin antiretroviral therapy immediately, or whether this therapy should be deferred until after acute treatment of the OI. The potential detrimental effects of drug-drug interactions, the need for treatment interruptions, and drug-related toxicity between antiretrovirals and OI-specific therapy may support initiating HAART after control of an OI is achieved. Conversely, for some opportunistic infections, such as cryptosporidiosis, the use of HAART is essential for successful treatment of the infection.
An ongoing randomized controlled trial initiated within the Adult AIDS Clinical Trials Group (ACTG) comparing outcomes between patients who start HAART immediately after presentation with an acute OI and patients who start HAART at least 4 weeks after the OI has resolved should help identify the factors supporting early or delayed initiation of antiretrovirals (4).
Generally speaking, HAART can be administered by combining either a protease inhibitor (PI) or a nonnucleoside reverse transcriptase inhibitor (NNRTI) with 2 nucleoside reverse transcriptase inhibitors (NRTIs). There are currently more than 20 FDA-approved antiretrovirals. Frequent updates on the guidelines for the use of antiretroviral agents in HIV-infected adults are available at www.AIDSinfo.nih.gov, and a discussion of this topic is beyond the scope of this review.
Continuation of HAART in the Hospital
In most cases, every effort should be made to minimize interruption of HAART during a hospitalization. Although some investigators are examining the virologic and immunologic safety of interrupting HAART as a treatment strategy, there are few data on viral replication, CD4 cell count decline, and rate of acquisition of new mutations in hospitalized patients who have unexpected treatment interruptions (5). The long half-life of some antiretrovirals promotes the emergence of resistance once HAART is stopped. For example, once NNRTIs are stopped, subtherapeutic levels remain in the plasma and cells for several days. HIV then replicates in a milieu that may select for resistance mutations.
Because zidovudine is the only antiretroviral available in a parenteral preparation, it is often difficult to continue HAART when a patient cannot take medications by mouth. Drugs given by the enteral route in a hospitalized patient may also be poorly absorbed, and few data exist on the absorption of antiretrovirals administered through a gastrostomy or jejunostomy tube (6).
Prescribing HAART in the Hospital
Antiretroviral prescribing errors occur frequently in the hospitalized AIDS patient. The most common errors include overdosing or underdosing, missing components of multidrug regimens, or missing critical drug-drug interactions (7). Underdosing may lead to resistance, and overdosing contributes to increased toxicity. In one report, prescribing errors occurred in 12% of admissions in the post-HAART era (1998) compared with 2% of admissions in the pre-HAART era (1996) (7). The NRTIs, including didanosine, emtricitabine, lamivudine, stavudine, and zidovudine, require decreased dosing in renal insufficiency. Tenofovir is not recommended for use if the creatine clearance is less than 60 mL/minute. Dosage adjustments in hepatic disease are recommended for amprenavir, fosamprenavir, delavirdine, efavirenz, and nevirapine.
Immune Reconstitution Syndrome
The widespread use of HAART has produced sustained suppression of HIV replication and recovery of CD4 cell counts. It also became evident that HAART resulted in not only a numerical increase in CD4 cells, but also in a functional immune recovery (8-10). This improved T-cell response to antigens results in adequate protection against specific opportunistic infections, allowing for discontinuation of primary and secondary prophylaxis in HIV-infected patients. Immune reconstitution syndrome (IRS), an inflammatory syndrome, is recognized as a potential complication that can occur days to months after starting HAART. The onset of IRS is characterized by a paradoxical worsening of clinical or laboratory parameters despite a favorable response in CD4 cell counts and the suppression of viral replication (9,11,12). IRS has been reported to occur in 10–25% of patients who receive HAART and more commonly in those whose CD4 cell counts are <50 cells/mm3 at the start of HAART (9,11). It is postulated that the inflammatory response is triggered by the recognition of antigens associated with ongoing infection or recognition of persisting antigens associated with past (nonreplicating) infections. Mycobacterial antigens, frequently implicated in IRS, are responsible for about one third of cases. Other antigens associated with IRS include cytomegalovirus and hepatitis B and C (11). In most circumstances, with the management of IRS, HAART should be continued, while specific antimicrobial therapy and steroids should be considered (10).
Medical Conditions that Should Prompt HIV Screening
There are several medical conditions that should prompt screening for HIV infection. Generally, anyone presenting with a fever of unknown etiology who is sexually active or had a blood transfusion prior to 1985 should be screened for HIV infection. Symptoms consistent with acute retroviral syndrome (fever, sore throat, malaise, and skin rash) may be more commonly recognized by clinicians now than previously, and this remains a “golden opportunity” to intervene. Frequently, acute retroviral syndrome will be attributed to Epstein-Barr virus; however, caution should be used in the diagnosis of mononucleosis in those other than teenage populations. It is recommended that all persons presenting with any sexually transmitted disease, unexplained generalized lymphadenopathy, oral candidiasis, or tuberculosis should also be tested. Other conditions where HIV infection should be considered include enigmatic pneumonia, acute hepatitis B infection, herpes zoster infection (particularly in younger, seemingly immunocompetent individuals), idiopathic thrombocytopenic purpura, and nephropathy of unknown cause.
Drug Interactions
Drug interactions are an important consideration in the treatment of HIV infection. Interactions between HAART and other drugs used for the treatment or prophylaxis of opportunistic infections along with those used for the treatment of drug-induced endocrinopathies (hyperlipidemia, diabetes mellitus) are virtually unavoidable. Drug interactions occur either because of drug metabolism or absorption. The multiple metabolic pathways of some drugs make it difficult to predict the outcome of drug interactions. All protease inhibitors and non-nucleoside reverse transcriptase inhibitors are metabolized by the cytochrome P-450 enzyme system and each of these drugs may alter the metabolism of other antiretrovirals and concomitantly administered drugs (13,14). A decrease in trough plasma concentrations of the protease inhibitors to a level below the in vitro concentration required to inhibit replication of 50% of viral strains (IC50) may lead to development of resistance. Because nucleoside analogue reverse transcriptase inhibitors are primarily eliminated by the kidney, they do not interact with other drugs through the cytochrome P-450 system.
One noteworthy interaction that the clinician caring for HIV-infected patients should be aware of is the interaction of ribavirin with zidovudine. Ribavirin decreases the phosphorylation of zidovudine and stavudine in vitro, resulting in decreased concentrations of the active compound. HIV-infected patients who are coinfected with hepatitis C may be treated with regimens that include ribavirin, which may reduce the efficacy of zidovudine (15). Another important interaction is the effect of nevirapine or efavirenz on plasma methadone concentrations. Both drugs can decrease methadone plasma levels by 50%, and patients receiving chronic therapy may need increased methadone doses to prevent withdrawal symptoms (16).
Protease inhibitors are associated with numerous interactions including certain antiarrhythmics, sedatives, hypnotics, ergot derivatives, and several lipid-lowering agents (statins). Not only do protease inhibitors affect the metabolism of certain drugs, but also their own metabolism is altered by other inducers or inhibitors of cytochrome activity that can cause clinically important decreases in serum levels of protease inhibitors. One widely recognized interaction is that of rifampin, which may decrease levels of some protease inhibitors by 80%. The resulting low plasma concentrations may promote viral resistance and result in treatment failure. Patients being treated for tuberculosis, who are also receiving protease inhibitors should be treated with a four-drug regimen that includes rifabutin (at half dose) instead of rifampin. Updated guidelines for the use of rifabutin or rifampin in HIV-infected patients receiving antiretroviral agents have been reviewed recently (17).
Other potent inducers such as phenytoin, phenobarbital, and carbamazepine can cause similar reductions in serum levels of protease inhibitors. Azole antifungal drugs and macrolides also have important interactions that complicate both the treatment and prophylaxis of opportunistic infections.
Interactions that interfere with absorption can also affect plasma drug concentrations. For example, the absorption of fluconazole is unaffected by variations in gastric pH, while itraconazole and ketoconazole require an acidic environment for optimal absorption. The protease inhibitor, atazanavir, also requires a low pH for absorption and thus is contraindicated with the use of proton pump inhibitors; taking atazanavir with acidic beverages is not sufficient to overcome this (18).
New information about drug interactions becomes known on almost a daily basis in patients with HIV infection. The number of documented and theoretical interactions can become overwhelming to the clinician. Clinicians should suspect potential drug interactions in a patient who is failing therapy but who is adherent to HAART. Fortunately, there are extensive tables on Web sites (www.hivatis.org) and product information to aid in the recognition and management of drug interactions.
Complications of HAART
Diabetes mellitus, hyperlipidemias, lipodystrophy, and insulin resistance are among the many complex metabolic abnormalities attributable to the use of HAART. For the most part, these complications are managed conservatively and usually do not mandate the discontinuation of HAART. Pancreatitis, hepatic steatosis, and lactic acidosis are wellrecognized complications of NRTIs. These are usually more acute and may result in hospitalization and necessitate the discontinuation of medications. Cessation of the offending agent (didanosine [ddI], stavudine [d4T], and zalcitabine [ddC) usually results in resolution of pancreatitis, but the episode may limit use of these agents in the future. Hepatic steatosis and lactic acidosis are rare but life-threatening adverse effects associated with the mitochondrial toxicity seen with the NRTIs. Symptoms usually develop insidiously with nausea, vomiting, abdominal pain, weight loss, or dyspnea and can progress rapidly to fatal lactic acidosis. Hepatomegaly, ascites, elevated liver associated enzymes, and an increased anion gap with lactic acidemia are usually present (19,20). Discontinuation of antiretroivirals is imperative.
There is an accumulating body of evidence that suggests that HIV-infected patients receiving HAART may be at risk for accelerated coronary disease (21). In addition, some cohort studies have reported an increased incidence of myocardial infarction (MI) following the introduction of HAART and the risk for MI rose progressively with the number of years on antiretroviral therapy (22,23). However, it is important to note that many traditional risk factors for coronary artery disease contribute more substantially to the risk for a cardiovascular event than does HAART. Therefore, aggressive modification of primary cardiac risk factors is warranted.
Hypersensitivity Drug Reactions
Drug hypersensitivity reactions are life-threatening reactions that result in a systemic illness that usually includes fever and maculopapular rash accompanied by constitutional symptoms (fatigue, myalgias, and arthralgias), visceral involvement (lymphadenopathy, mucositis, pneumonitis, myocarditis, hepatitis, and interstitial nephritis), and hematologic abnormalities (eosinophilia) (24).
Abacavir, an NRTI, is a relatively new antiretroviral agent used in many HAART regimens. Abacavir is associated with a hypersensitivity reaction, which can be fatal if abacavir use is continued despite the reaction, or if re-challenge with the drug takes place after the reaction (25). The overall incidence of this reaction appears to be around 4% (25). Prior antiretroviral experience and being of African descent are associated with a nearly 40% reduction in the risk of this hypersensitivity reaction, while patients of white race are at a significantly greater risk. CD4 cell counts do not appear to be significantly related to abacavir hypersensitivity (26). The exact metabolite that is likely responsible for abacavir hypersensitivity is unknown.
The most common symptoms of abacavir hypersensitivity reaction are fever, rash, nausea, vomiting, and abdominal pain. Occasionally, respiratory symptoms will be present and can mimic influenza. However, gastrointestinal symptoms are the most prominent complaints after fever and rash and help to distinguish between influenza and abacavir hypersensitivity. More than 90% of hypersensitivity reactions occur during the first 6 weeks of treatment, with a median time to development of 8 days. A fever that develops within a few weeks after the initiation of therapy with abacavir may be due to causes other than hypersensitivity. One of the most common situations is the simultaneous initiation of treatment with other drugs, such as trimethoprimsulfamethxazole, efavirenz, or nevirapine, all of which are associated with a higher incidence of hypersensitivity than abacavir (27,28). Symptoms may be sudden and worsen over a few days if abacavir is continued. Symptoms tend to improve in 48 hours after abacavir is discontinued. Supportive therapy includes intravenous hydration and withdrawal of abacavir as well as all other antiretrovirals. Early in the use of this medication, 20% of patients who were re-challenged with the drug experienced unanticipated life-threatening events manifesting as an anaphylactic or immediate type hypersensitivity reaction. Hypotension, renal insufficiency, and bronchospasm have resulted in death. Rechallenge symptoms have been seen with the first dose (29). A discussion of the potential for this hypersensitivity is warranted when prescribing this agent. In the United States, a patient information card warning of this hypersensitivity reaction is distributed to the patient with each bottle of abacavir. Prednisone does not prevent the development of hypersensitivity reaction.
Symptoms of toxicity from TMP-SMX are more likely to occur in the HIV infected than in patients without HIV infection. Fever and rash can occur in up to 50% of HIV-infected patients. The rash can be treatment limiting or severe in up to 20% of HIV-infected patients who receive it. Life-threatening reactions may occur, including fatal Stevens Johnson-type exfoliative skin reactions. Most toxicity in HIV-infected patients appears to be related to metabolites of the sulfamethoxazole component and decreased levels of glutathione. There have been reports of severe systemic reactions that resemble anaphylaxis or septic shock occurring in HIV-infected patients who are re-challenged with TMP-SMX after experiencing toxicity within the previous 6–8 weeks (30).
The NNRTIf nevirapine and efavirenz can cause a delayed hypersensitivity reaction similar to that seen with abacavir. Cutaneous involvement is a prominent component of both nevirapine and efavirenz hypersensitivity reaction, with rash more likely to occur with the use of nevirapine. In addition, female patients have a higher propensity of developing Stevens-Johnson syndrome and symptomatic hepatic events from nevirapine (28,31).
Laboratory Abnormalities Related to Drugs
Hyperbilirubinemia and Atazanavir and Indinavir
Atazanavir, a protease inhibitor, is metabolized by the liver via CYP3A and also inhibits both CTP3A and UGT1A1. UGT1A1 is required for conjugation of bilirubin and inhibition of this enzyme results in elevated levels of unconjugated bilirubin. This effect is similar to what is observed in Gilbert’s syndrome. Asymptomatic indirect hyperbilirubemia may be seen in up to 60% of patients receiving atazanavir. Total bilirubin levels may rise to greater than 5 mg/dL, and more than 17% of patients may experience jaundice (18). Concurrent elevations in hepatic serum transaminases should not be attributed to atazanavir and alternative etiologies for these elevations should be sought. This hyperbilirubinemia is reversible upon discontinuation of the atazanavir.
Similarly, but to a lesser degree, asymptomatic unconjugated hyperbilirubinemia (>2 mg/dL) has been reported in up to 14% of patients treated with indinavir. Elevated serum transaminases were seen in less than 1%.
Renal Abnormalities and Indinavir
Several renal syndromes have been associated with indinavir use, ranging from obstructive uropathy and acute renal failure to asymptomatic pyuria. The range of clinical syndromes is a consequence of indinavir crystals aggregating within or irritating the urinary tract (32). Symptomatic nephrolithiasis (indinavir crystallization) has been reported to affect up to 12% (range, 5–35 %) of patients who receive indinavir, while up to 67% of patients will have asymptomatic crystalluria. The cumulative frequency of nephrolithiasis events increases with increasing exposure to indinavir. Therapy may be continued or interrupted for a few days. Adequate hydration is necessary with the administration of indinavir. Indinavir associated pyuria is frequently associated with interstitial nephritis or urothelial inflammation. Discontinuation of indinavir will lead to resolution of urine abnormalities.
Elevated Mean Corpuscular Volume (MCV) and NRTIs
Elevation of MCV or macrocytosis occurs in more than 90% of patients treated with zidovudine, but is not correlated with the development of anemia. Macrocytosis (MCV values exceeding 110/fl) develops within 2 weeks following the initiation of zidovudine therapy, and its presence can be used as a marker for medical adherence. When anemia does occur it is associated with a dose related bone marrow toxicity manifested as a macrocytic anemia. Serum B12 and folate levels are normal. Stavudine use is also associated with macrocytosis, in non-zidovudine-containing regimens (33).
Drug Screens and Efavirenz
The use of efavirenz, a potent non-nucleoside reverse transcriptase inhibitor, can cause a false-positive urine drug screen for cannabinoid. Efavirenz does not bind to cannabinoid receptors. The false-positive test results are specific to the assay kit used (34).
Evaluation of the AIDS Patient with Fever
Fever is a common symptom in HIV-infected patients, the etiology of which can be identified in more than 80% of cases (35,36). The AIDS patient with fever poses a considerable challenge given that the expanded differential may include a wide range of OIs. The CD4 cell count remains a valuable predictor of risk for infection. Patients with CD4 cell counts greater than 500 cells/mm3 should be evaluated as if immunocompetent. Patients with CD4 cell counts between 200 and 500 cells/mm3 are at increased risk for upper and lower bacterial respiratory infections, tuberculosis, and sinusitis, but overall their risk for opportunistic infection is not increased. In patients with CD4 counts less than 200 cells/mm3, Pneumocystis jiroveci pneumonia, formerly known as Pneumocystis carinii pneumonia, is the most common cause of fever in those not receiving primary prophylaxis. As the CD4 cell count decreases below 100 cells/mm3, the risk for disseminated MAC, toxoplasmosis, CMV, disseminated fungal infections, and lymphoma should be considered possible causes of fever. HIV itself is usually not the cause of fever in patients with advanced immunosuppression (37).
In patients with CD4 counts >200 cells/mm3, the clinician can usually construct a laboratory and radiographic evaluation guided by symptoms, while in patients with severe immunosuppression a broader evaluation is required. A serum cryptococcal antigen should be obtained, as it has high sensitivity and specificity for both systemic disease as well as meningitis (38). Bacterial, mycobacterial, and fungal isolator blood cultures should be performed, as well as a urine culture, despite lack of symptoms. Urine AFB cultures can be added if there is a suspicion for tuberculosis. Sputum should be evaluated with gram stain, AFB smear, and culture, as well as PCP direct fluorescent antibody. If diarrhea is present, stool studies should include bacterial culture, ova and parasites evaluation, an assay for C. difficile, and Cryptosporidia and Giardia stool antigen assays. A serum LDH may be elevated in PCP, disseminated histoplasmosis, or lymphoma. A serum CMV antigen may be useful in the patient with fever and diarrhea, hepatitis, or retinitis.
A chest radiograph should be performed in all febrile AIDS patients. Chest films may be normal in 5–10% of HIV-infected patients with tuberculosis (TB). The typical radiographic appearance of Pneumocystis jiroveci pneumonia is a bilateral interstitial pattern characterized by reticular or ground-glass opacities. However, normal chest radiographs may be seen in one third of AIDS patients with active PCP. High-resolution computed tomography (HRCT) of the chest should be obtained if there is still a clinical suspicion for Pneumocystis. HRCT has been shown in several reports to have a 100% negative predictive value in the evaluation for PCP (39,40).
A lumbar puncture should be performed if the patient is symptomatic or if the serum cryptococcal antigen is reactive. A bone marrow biopsy and culture is also useful particularly in the evaluation of the patient with cytopenias. Bacterial, fungal, and AFB cultures may yield disseminated mycobacterial or fungal disease. Histopathologic evaluation may reveal granulomas with organisms or lymphoma. Bronchoscopy may be pursued in cases of high suspicion for TB or PCP.
Guidelines for the management of opportunistic infections associated with human immunodeficiency virus are available at www.AIDSinfo.nih.gov.
Evaluation of the AIDS Patient with Focal Neurological Disease
Toxoplasma encephalitis (TE) may be distinguished from primary CNS lymphoma without a brain biopsy. TE is caused by reactivation of latent infection by the protozoan Toxoplasma gondii. Almost 90% of patients have CD4 counts less than 200 cells/mm3 and 75% have CD4 counts less than 100 cells/mm3. Serum anti-Toxoplasma IgG antibodies are detected in more than 90% of patients with TE. Lesions on CT or MRI (a more sensitive modality) are typically multiple ring-enhancing lesions with a predilection for the basal ganglia. An emipiric trial of therapy is recommended, and a response confirms a diagnosis in the patient who has a positive Toxoplasma antibody and is not receiving trimethoprim-sulfamethoxazole prophylaxis. A lumbar puncture in this setting is not necessary and maybe ill advised if cerebral edema is present (Figure 1, page 24).
Primary CNS lymphoma (PCNSL) has a similar radiographic appearance as TE. Solitary lesions are more frequent in PCNSL. Positron emission tomography (PET) and single photon emission CT (SPECT) are useful adjunctive imaging modalities as they are positive in PCNSL due to the increased metabolic activity of the tumor. Cytologic analysis of the CSF may show lymphomatous cells. Epstein-Barr virus (EBV) DNA is uniformly detected in PCNSL in AIDS patients and detection of EBV DNA by PCR on the CSF has a sensitivity of 90–100% and a specificity of 87–98% for the diagnosis of PCNSL (41,42). Combining SPECT imaging and EBV PCR provides 100% sensitivity and 100% negative predictive value in the evaluation of AIDS-related primary CNS lymphoma (43), obviating the need for brain biopsy.
Progressive multifocal leukoencephalopathy (PML) is characterized radiographically by multiple and bilateral hypodense lesions of the white matter without mass effect or enhancement on CT. MRI demonstrates areas of hypointensity on T1-weighted images and increased intensity on T2-weighted images. JC virus DNA can be detected by PCR of CSF or brain tissue with sensitivity of approximately 80% and specificity of 95%. Because of the high positive predictive value of a positive PCR, a patient with AIDS who also has a compatible MRI can be diagnosed with PML (44,45).
Other focal neurologic disease seen in AIDS patients includes cryptococcomas, tuberculomas, CMV encephalitis, neurosyphilis, Nocardia and Aspergillus infection, and bacterial brain abscesses (46).
Conclusion
As survival of the HIV-infected population improves, more patients may require hospitalization for HAART treatment failures or complications attributed to antiretroviral therapy. The hospitalist should be familiar with the complications of antiretroviral agents, the interactions between HAART and medications used to treat opportunistic infections, and medical conditions induced by HAART. Evaluation of the HIV-infected patient presenting with fever can be based on the CD4 cell count, which predicts risk for opportunistic infections. Finally, using combined diagnostic approaches along with modern imaging and laboratory assays may preclude the need for more invasive procedures in the HIV-infected hospitalized patient.
Dr. Decker may be reached at [email protected].
References
- Torres RA, Barr M. Impact of combination therapy for HIV infection on inpatient census. N Engl J Med. 1997;336:1531-2.
- Fleishman JA, Hellinger FJ. Trends in HIV-related inpatient admissions from 1993 to 1997: a seven-state study. J Acquir Immune Defic Syndr. 2001;28:73-80.
- Fleishman JA, Hellinger FH. Recent trends in HIV-related inpatient admissions 1996-2000: a 7-state study. J Acquir Immune Defic Syndr. 2003;34:102-10.
- Powderly WG. Should patients with an acute opportunistic infection receive antiretroviral therapy immediately? Advanced Studies in Medicine. 2005;5:S111-S116.
- Fagard C, Oxenius A, Gunthard H, et al. A prospective trial of structured treatment interruptions in human immunodeficiency virus infection. Arch Intern Med. 2003;163:1220-6.
- Soni N, Pozniak A. Continuing HIV therapy in the ICU. Crit Care. 2001;5:247-8.
- Purdy BD, Raymond AM, Lesar TS. Antiretroviral prescribing errors in hospitalized patients. Ann Pharmacother. 2000;34:833-8.
- Autran B, Carcelain G, Li TS, et al. Positive effects of combined antiretroviral therapy on CD4+ T cell homeostasis and function in advanced HIV disease. Science. 1997;277:112-6.
- Cooney EL. Clinical indicators of immune restoration following highly active antiretroviral therapy. Clin Infect Dis. 2002;34:224-33.
- Hirsch HH, Kaufmann G, Sendi P, BaĴegay M. Immune reconstitution in HIV-infected patients. Clin Infect Dis. 2004;38:1159-66.
- Cheng VC, Yuen KY, Chan WM, Wong SS, Ma ES, Chan RM. Immunorestitution disease involving the innate and adaptive response. Clin Infect Dis. 2000;30:882-92.
- Fishman JE, Saraf-Lavi E, Narita M, Hollender ES, Ramsinghani R, Ashkin D. Pulmonary tuberculosis in AIDS patients: transient chest radiographic worsening after initiation of antiretroviral therapy. AJR Am J Roentgenol. 2000;174:43-9.
- Piscitelli SC, Gallicano KD. Interactions among drugs for HIV and opportunistic infections. N Engl J Med. 2001;344:984-96.
- Barry M, Mulcahy F, Merry C, Gibbons S, Back D. Pharmacokinetics and potential interactions amongst antiretroviral agents used to treat patients with HIV infection. Clin Pharmacokinet. 1999;36:289-304.
- Sim SM, Hoggard PG, Sales SD, Phiboonbanakit D, Hart CA, Back DJ. Effect of ribavirin on zidovudine efficacy and toxicity in vitro: a concentration-dependent interaction. AIDS Res Hum Retroviruses. 1998;14:1661-7.
- Clarke SM, Mulcahy FM, Tjia J, et al. The pharmacokinetics of methadone in HIV-positive patients receiving the non-nucleoside reverse transcriptase inhibitor efavirenz. Br J Clin Pharmacol. 2001;51:213-7.
- Centers for Disease Control and Prevention. Updated guidelines for the use of rifabutin or rifampin for the treatment and prevention of tuberculosis among HIV-infected patients taking protease inhibitors or nonnucleoside reverse transcriptase inhibitors. Morb Mortal Wkly Rep. 2000;49:185-9.
- Havlir DV, O’Marro SD. Atazanavir: new option for treatment of HIV infection. Clin Infect Dis. 2004;38:1599-604.
- Sheng WH, Hsieh SM, Lee SC, et al. Fatal lactic acidosis associated with highly active antiretroviral therapy in patients with advanced human immunodeficiency virus infection in Taiwan. Int J STD AIDS. 2004;15:249-53.
- Herman JS, Easterbrook PJ. The metabolic toxicities of antiretroviral therapy. Int J STD AIDS. 2001;12:555-62;quiz 563-4.
- Behrens G, Schmidt H, Meyer D, Stoll M, Schmidt RE. Vascular complications associated with use of HIV protease inhibitors. Lancet. 1998;351:1958.
- Klein D, Hurley LB, Sidney S. Cardiovascular Disease and HIV Infection. N Engl J Med. 2003;349:1869-70; author reply 1869-70.
- Friis-Moller N, Sabin CA, Weber R, et al. Combination antiretroviral therapy and the risk of myocardial infarction. N Engl J Med. 2003;349:1993-2003.
- Anderson JA, Adkinson NF Jr. Allergic reactions to drugs and biologic agents. JAMA. 1987;258:2891-9.
- Hewitt RG. Abacavir hypersensitivity reaction. Clin Infect Dis. 2002;34:1137-42.
- Hetherington S, Hughes AR, Mosteller M, et al. Genetic variations in HLA-B region and hypersensitivity reactions to abacavir. Lancet. 2002;359:1121-2.
- Bossi P, Colin D, Bricaire F, Caumes E. Hypersensitivity syndrome associated with efavirenz therapy. Clin Infect Dis. 2000;30:227-8.
- Bourezane Y, Salard D, Hoen B, Vandel S, Drobacheff C, Laurent R. DRESS (drug rash with eosinophilia and systemic symptoms) syndrome associated with nevirapine therapy. Clin Infect Dis. 1998;27:1321-2.
- Walensky RP, Goldberg JH, Daily JP. Anaphylaxis after rechallenge with abacavir. AIDS. 1999;13:999-1000.
- Martin GJ, Paparello SF, Decker CF. A severe systemic reaction to trimethoprim-sulfamethoxazole in a patient infected with the human immunodeficiency virus. Clin Infect Dis. 1993;16:175-6.
- Bersoff-Matcha SJ, Miller WC, Aberg JA, et al. Sex differences in nevirapine rash. Clin Infect Dis. 2001;32:124-9.
- Kopp JB, Falloon J, Filie A, et al. Indinavir-associated interstitial nephritis and urothelial inflammation: clinical and cytologic findings. Clin Infect Dis. 2002;34:1122-8.
- Geene D, Sudre P, Anwar D, Goehring C, Saaidia A, Hirschel B. Causes of macrocytosis in HIV-infected patients not treated with zidovudine. Swiss HIV Cohort Study. J Infect. 2000;40:160-3.
- Gottesman L. Sustiva may cause false positive on marijuana test. WORLD. 1999:7.
- Sepkowitz KA, Telzak EE, Carrow M, Armstrong D. Fever among outpatients with advanced human immunodeficiency virus infection. Arch Intern Med. 1993;153: 1909-12.
- Barat LM, Gunn JE, Steger KA, Perkins CJ, Craven DE. Causes of fever in patients infected with human immunodeficiency virus who were admitted to Boston City Hospital. Clin Infect Dis. 1996;23:320-8.
- Sepkowitz KA. FUO and AIDS. Curr Clin Top Infect Dis. 1999;19:1-15.
- Asawavichienjinda T, Sitthi-Amorn C, Tanyanont V. Serum cyrptococcal antigen: diagnostic value in the diagnosis of AIDS-related cryptococcal meningitis. J Med Assoc Thai. 1999;82:65-71.
- Richards PJ, Riddell L, Reznek RH, Armstrong P, Pinching AJ, Parkin JM. High resolution computed tomography in HIV patients with suspected Pneumocystis carinii pneumonia and a normal chest radiograph. Clin Radiol. 1996;51:689-93.
- Gruden JF, Huang L, Turner J, et al. High-resolution CT in the evaluation of clinically suspected Pneumocystis carinii pneumonia in AIDS patients with normal, equivocal, or nonspecific radiographic findings. AJR Am J Roentgenol. 1997;169:967-75.
- MacMahon EM, Glass JD, Hayward SD, et al. Association of Epstein-Barr virus with primary central nervous system lymphoma in AIDS. AIDS Res Hum Retroviruses. 1992;8:740-2.
- Rao CR, Jain K, Bhatia K, Laksmaiah KC, Shankar SK. Association of primary central nervous system lymphomas with the Epstein-Barr virus. Neurol India. 2003;51:237-40.
- Antinori A, De Rossi G, Ammassari A, et al. Value of combined approach with thallium-201 single-photon emission computed tomography and Epstein-Barr virus DNA polymerase chain reaction in CSF for the diagnosis of AIDS-related primary CNS lymphoma. J Clin Oncol. 1999;17:554-60.
- Post MJ, Yiannoutsos C, Simpson D, et al. Progressive multifocal leukoencephalopathy in AIDS: are there any MR findings useful to patient management and predictive of patient survival? AIDS Clinical Trials Group, 243 Team. AJNR Am J Neuroradiol. 1999;20:1896-906.
- Weber T. Cerebrospinal fluid analysis for the diagnosis of human immunodeficiency virus-related neurologic diseases. Semin Neurol. 1999;19:223-33.
- Skiest DJ. Focal neurological disease in patients with acquired immunodeficiency syndrome. Clin Infect Dis. 2002;34:103-15.
The opinions and assertions contained herein are those of the authors and are not to be construed as official or as reflecting the views of the Department of Defense, the Department of the Navy, or the naval services at large.
Introduction
An estimated 850,000 to 950,000 persons in the United States are living with human immunodeficiency virus (HIV), 280,000 of whom are unaware of their infection and another 43,000 of whom meet the definition of acquired immunodeficiency syndrome (AIDS) (www.cdc.gov). The use of highly active antiretroviral therapy (HAART) has produced significant declines in morbidity and mortality from AIDS. Compared with the first 2 decades of the HIV pandemic, the number of HIV-related hospital admissions has declined. However, recently, this rate of decline has markedly slowed (1-3). The reasons for this plateau are many including a steady number of admissions for complications related to HAART, treatment failures, and the overall increased prevalence of HIV infection. Not only will HIV-infected patients still frequently require admission to the hospital, but the complexity of their inpatient care will continue to increase with the advancements in multiple drug regimens, aging of the HIV-infected population, and the interaction of HIV infection with medical comorbidities, many of which are attributable to HAART.
The hospitalist caring for the inpatient with AIDS is presented with several challenges including not only the diagnosis and management of opportunistic infections, but also the complications of HAART. In this article we review the guidelines for the initiation and continuation of HAART in the hospital, review important clinical complications of antiretroviral therapy, and review conditions that may result in the hospitalization of AIDS patients.
Initiation of HAART in the Hospital
In those who do not have access to health care, the initial diagnosis of HIV infection frequently occurs during a hospitalization for an AIDS-defining illness. Initiation of antiretrovirals is contingent on several issues, including CD4 count, viral load, clinical status, likelihood of continued adherence, and the concurrent treatment of opportunistic infections (OIs). All patients with HIV infection and a CD4 count <200 cells/mm3 or an AIDS-defining illness should receive antiretroviral therapy. Controversy exists as to whether a patient admitted for the treatment of an opportunistic infection should begin antiretroviral therapy immediately, or whether this therapy should be deferred until after acute treatment of the OI. The potential detrimental effects of drug-drug interactions, the need for treatment interruptions, and drug-related toxicity between antiretrovirals and OI-specific therapy may support initiating HAART after control of an OI is achieved. Conversely, for some opportunistic infections, such as cryptosporidiosis, the use of HAART is essential for successful treatment of the infection.
An ongoing randomized controlled trial initiated within the Adult AIDS Clinical Trials Group (ACTG) comparing outcomes between patients who start HAART immediately after presentation with an acute OI and patients who start HAART at least 4 weeks after the OI has resolved should help identify the factors supporting early or delayed initiation of antiretrovirals (4).
Generally speaking, HAART can be administered by combining either a protease inhibitor (PI) or a nonnucleoside reverse transcriptase inhibitor (NNRTI) with 2 nucleoside reverse transcriptase inhibitors (NRTIs). There are currently more than 20 FDA-approved antiretrovirals. Frequent updates on the guidelines for the use of antiretroviral agents in HIV-infected adults are available at www.AIDSinfo.nih.gov, and a discussion of this topic is beyond the scope of this review.
Continuation of HAART in the Hospital
In most cases, every effort should be made to minimize interruption of HAART during a hospitalization. Although some investigators are examining the virologic and immunologic safety of interrupting HAART as a treatment strategy, there are few data on viral replication, CD4 cell count decline, and rate of acquisition of new mutations in hospitalized patients who have unexpected treatment interruptions (5). The long half-life of some antiretrovirals promotes the emergence of resistance once HAART is stopped. For example, once NNRTIs are stopped, subtherapeutic levels remain in the plasma and cells for several days. HIV then replicates in a milieu that may select for resistance mutations.
Because zidovudine is the only antiretroviral available in a parenteral preparation, it is often difficult to continue HAART when a patient cannot take medications by mouth. Drugs given by the enteral route in a hospitalized patient may also be poorly absorbed, and few data exist on the absorption of antiretrovirals administered through a gastrostomy or jejunostomy tube (6).
Prescribing HAART in the Hospital
Antiretroviral prescribing errors occur frequently in the hospitalized AIDS patient. The most common errors include overdosing or underdosing, missing components of multidrug regimens, or missing critical drug-drug interactions (7). Underdosing may lead to resistance, and overdosing contributes to increased toxicity. In one report, prescribing errors occurred in 12% of admissions in the post-HAART era (1998) compared with 2% of admissions in the pre-HAART era (1996) (7). The NRTIs, including didanosine, emtricitabine, lamivudine, stavudine, and zidovudine, require decreased dosing in renal insufficiency. Tenofovir is not recommended for use if the creatine clearance is less than 60 mL/minute. Dosage adjustments in hepatic disease are recommended for amprenavir, fosamprenavir, delavirdine, efavirenz, and nevirapine.
Immune Reconstitution Syndrome
The widespread use of HAART has produced sustained suppression of HIV replication and recovery of CD4 cell counts. It also became evident that HAART resulted in not only a numerical increase in CD4 cells, but also in a functional immune recovery (8-10). This improved T-cell response to antigens results in adequate protection against specific opportunistic infections, allowing for discontinuation of primary and secondary prophylaxis in HIV-infected patients. Immune reconstitution syndrome (IRS), an inflammatory syndrome, is recognized as a potential complication that can occur days to months after starting HAART. The onset of IRS is characterized by a paradoxical worsening of clinical or laboratory parameters despite a favorable response in CD4 cell counts and the suppression of viral replication (9,11,12). IRS has been reported to occur in 10–25% of patients who receive HAART and more commonly in those whose CD4 cell counts are <50 cells/mm3 at the start of HAART (9,11). It is postulated that the inflammatory response is triggered by the recognition of antigens associated with ongoing infection or recognition of persisting antigens associated with past (nonreplicating) infections. Mycobacterial antigens, frequently implicated in IRS, are responsible for about one third of cases. Other antigens associated with IRS include cytomegalovirus and hepatitis B and C (11). In most circumstances, with the management of IRS, HAART should be continued, while specific antimicrobial therapy and steroids should be considered (10).
Medical Conditions that Should Prompt HIV Screening
There are several medical conditions that should prompt screening for HIV infection. Generally, anyone presenting with a fever of unknown etiology who is sexually active or had a blood transfusion prior to 1985 should be screened for HIV infection. Symptoms consistent with acute retroviral syndrome (fever, sore throat, malaise, and skin rash) may be more commonly recognized by clinicians now than previously, and this remains a “golden opportunity” to intervene. Frequently, acute retroviral syndrome will be attributed to Epstein-Barr virus; however, caution should be used in the diagnosis of mononucleosis in those other than teenage populations. It is recommended that all persons presenting with any sexually transmitted disease, unexplained generalized lymphadenopathy, oral candidiasis, or tuberculosis should also be tested. Other conditions where HIV infection should be considered include enigmatic pneumonia, acute hepatitis B infection, herpes zoster infection (particularly in younger, seemingly immunocompetent individuals), idiopathic thrombocytopenic purpura, and nephropathy of unknown cause.
Drug Interactions
Drug interactions are an important consideration in the treatment of HIV infection. Interactions between HAART and other drugs used for the treatment or prophylaxis of opportunistic infections along with those used for the treatment of drug-induced endocrinopathies (hyperlipidemia, diabetes mellitus) are virtually unavoidable. Drug interactions occur either because of drug metabolism or absorption. The multiple metabolic pathways of some drugs make it difficult to predict the outcome of drug interactions. All protease inhibitors and non-nucleoside reverse transcriptase inhibitors are metabolized by the cytochrome P-450 enzyme system and each of these drugs may alter the metabolism of other antiretrovirals and concomitantly administered drugs (13,14). A decrease in trough plasma concentrations of the protease inhibitors to a level below the in vitro concentration required to inhibit replication of 50% of viral strains (IC50) may lead to development of resistance. Because nucleoside analogue reverse transcriptase inhibitors are primarily eliminated by the kidney, they do not interact with other drugs through the cytochrome P-450 system.
One noteworthy interaction that the clinician caring for HIV-infected patients should be aware of is the interaction of ribavirin with zidovudine. Ribavirin decreases the phosphorylation of zidovudine and stavudine in vitro, resulting in decreased concentrations of the active compound. HIV-infected patients who are coinfected with hepatitis C may be treated with regimens that include ribavirin, which may reduce the efficacy of zidovudine (15). Another important interaction is the effect of nevirapine or efavirenz on plasma methadone concentrations. Both drugs can decrease methadone plasma levels by 50%, and patients receiving chronic therapy may need increased methadone doses to prevent withdrawal symptoms (16).
Protease inhibitors are associated with numerous interactions including certain antiarrhythmics, sedatives, hypnotics, ergot derivatives, and several lipid-lowering agents (statins). Not only do protease inhibitors affect the metabolism of certain drugs, but also their own metabolism is altered by other inducers or inhibitors of cytochrome activity that can cause clinically important decreases in serum levels of protease inhibitors. One widely recognized interaction is that of rifampin, which may decrease levels of some protease inhibitors by 80%. The resulting low plasma concentrations may promote viral resistance and result in treatment failure. Patients being treated for tuberculosis, who are also receiving protease inhibitors should be treated with a four-drug regimen that includes rifabutin (at half dose) instead of rifampin. Updated guidelines for the use of rifabutin or rifampin in HIV-infected patients receiving antiretroviral agents have been reviewed recently (17).
Other potent inducers such as phenytoin, phenobarbital, and carbamazepine can cause similar reductions in serum levels of protease inhibitors. Azole antifungal drugs and macrolides also have important interactions that complicate both the treatment and prophylaxis of opportunistic infections.
Interactions that interfere with absorption can also affect plasma drug concentrations. For example, the absorption of fluconazole is unaffected by variations in gastric pH, while itraconazole and ketoconazole require an acidic environment for optimal absorption. The protease inhibitor, atazanavir, also requires a low pH for absorption and thus is contraindicated with the use of proton pump inhibitors; taking atazanavir with acidic beverages is not sufficient to overcome this (18).
New information about drug interactions becomes known on almost a daily basis in patients with HIV infection. The number of documented and theoretical interactions can become overwhelming to the clinician. Clinicians should suspect potential drug interactions in a patient who is failing therapy but who is adherent to HAART. Fortunately, there are extensive tables on Web sites (www.hivatis.org) and product information to aid in the recognition and management of drug interactions.
Complications of HAART
Diabetes mellitus, hyperlipidemias, lipodystrophy, and insulin resistance are among the many complex metabolic abnormalities attributable to the use of HAART. For the most part, these complications are managed conservatively and usually do not mandate the discontinuation of HAART. Pancreatitis, hepatic steatosis, and lactic acidosis are wellrecognized complications of NRTIs. These are usually more acute and may result in hospitalization and necessitate the discontinuation of medications. Cessation of the offending agent (didanosine [ddI], stavudine [d4T], and zalcitabine [ddC) usually results in resolution of pancreatitis, but the episode may limit use of these agents in the future. Hepatic steatosis and lactic acidosis are rare but life-threatening adverse effects associated with the mitochondrial toxicity seen with the NRTIs. Symptoms usually develop insidiously with nausea, vomiting, abdominal pain, weight loss, or dyspnea and can progress rapidly to fatal lactic acidosis. Hepatomegaly, ascites, elevated liver associated enzymes, and an increased anion gap with lactic acidemia are usually present (19,20). Discontinuation of antiretroivirals is imperative.
There is an accumulating body of evidence that suggests that HIV-infected patients receiving HAART may be at risk for accelerated coronary disease (21). In addition, some cohort studies have reported an increased incidence of myocardial infarction (MI) following the introduction of HAART and the risk for MI rose progressively with the number of years on antiretroviral therapy (22,23). However, it is important to note that many traditional risk factors for coronary artery disease contribute more substantially to the risk for a cardiovascular event than does HAART. Therefore, aggressive modification of primary cardiac risk factors is warranted.
Hypersensitivity Drug Reactions
Drug hypersensitivity reactions are life-threatening reactions that result in a systemic illness that usually includes fever and maculopapular rash accompanied by constitutional symptoms (fatigue, myalgias, and arthralgias), visceral involvement (lymphadenopathy, mucositis, pneumonitis, myocarditis, hepatitis, and interstitial nephritis), and hematologic abnormalities (eosinophilia) (24).
Abacavir, an NRTI, is a relatively new antiretroviral agent used in many HAART regimens. Abacavir is associated with a hypersensitivity reaction, which can be fatal if abacavir use is continued despite the reaction, or if re-challenge with the drug takes place after the reaction (25). The overall incidence of this reaction appears to be around 4% (25). Prior antiretroviral experience and being of African descent are associated with a nearly 40% reduction in the risk of this hypersensitivity reaction, while patients of white race are at a significantly greater risk. CD4 cell counts do not appear to be significantly related to abacavir hypersensitivity (26). The exact metabolite that is likely responsible for abacavir hypersensitivity is unknown.
The most common symptoms of abacavir hypersensitivity reaction are fever, rash, nausea, vomiting, and abdominal pain. Occasionally, respiratory symptoms will be present and can mimic influenza. However, gastrointestinal symptoms are the most prominent complaints after fever and rash and help to distinguish between influenza and abacavir hypersensitivity. More than 90% of hypersensitivity reactions occur during the first 6 weeks of treatment, with a median time to development of 8 days. A fever that develops within a few weeks after the initiation of therapy with abacavir may be due to causes other than hypersensitivity. One of the most common situations is the simultaneous initiation of treatment with other drugs, such as trimethoprimsulfamethxazole, efavirenz, or nevirapine, all of which are associated with a higher incidence of hypersensitivity than abacavir (27,28). Symptoms may be sudden and worsen over a few days if abacavir is continued. Symptoms tend to improve in 48 hours after abacavir is discontinued. Supportive therapy includes intravenous hydration and withdrawal of abacavir as well as all other antiretrovirals. Early in the use of this medication, 20% of patients who were re-challenged with the drug experienced unanticipated life-threatening events manifesting as an anaphylactic or immediate type hypersensitivity reaction. Hypotension, renal insufficiency, and bronchospasm have resulted in death. Rechallenge symptoms have been seen with the first dose (29). A discussion of the potential for this hypersensitivity is warranted when prescribing this agent. In the United States, a patient information card warning of this hypersensitivity reaction is distributed to the patient with each bottle of abacavir. Prednisone does not prevent the development of hypersensitivity reaction.
Symptoms of toxicity from TMP-SMX are more likely to occur in the HIV infected than in patients without HIV infection. Fever and rash can occur in up to 50% of HIV-infected patients. The rash can be treatment limiting or severe in up to 20% of HIV-infected patients who receive it. Life-threatening reactions may occur, including fatal Stevens Johnson-type exfoliative skin reactions. Most toxicity in HIV-infected patients appears to be related to metabolites of the sulfamethoxazole component and decreased levels of glutathione. There have been reports of severe systemic reactions that resemble anaphylaxis or septic shock occurring in HIV-infected patients who are re-challenged with TMP-SMX after experiencing toxicity within the previous 6–8 weeks (30).
The NNRTIf nevirapine and efavirenz can cause a delayed hypersensitivity reaction similar to that seen with abacavir. Cutaneous involvement is a prominent component of both nevirapine and efavirenz hypersensitivity reaction, with rash more likely to occur with the use of nevirapine. In addition, female patients have a higher propensity of developing Stevens-Johnson syndrome and symptomatic hepatic events from nevirapine (28,31).
Laboratory Abnormalities Related to Drugs
Hyperbilirubinemia and Atazanavir and Indinavir
Atazanavir, a protease inhibitor, is metabolized by the liver via CYP3A and also inhibits both CTP3A and UGT1A1. UGT1A1 is required for conjugation of bilirubin and inhibition of this enzyme results in elevated levels of unconjugated bilirubin. This effect is similar to what is observed in Gilbert’s syndrome. Asymptomatic indirect hyperbilirubemia may be seen in up to 60% of patients receiving atazanavir. Total bilirubin levels may rise to greater than 5 mg/dL, and more than 17% of patients may experience jaundice (18). Concurrent elevations in hepatic serum transaminases should not be attributed to atazanavir and alternative etiologies for these elevations should be sought. This hyperbilirubinemia is reversible upon discontinuation of the atazanavir.
Similarly, but to a lesser degree, asymptomatic unconjugated hyperbilirubinemia (>2 mg/dL) has been reported in up to 14% of patients treated with indinavir. Elevated serum transaminases were seen in less than 1%.
Renal Abnormalities and Indinavir
Several renal syndromes have been associated with indinavir use, ranging from obstructive uropathy and acute renal failure to asymptomatic pyuria. The range of clinical syndromes is a consequence of indinavir crystals aggregating within or irritating the urinary tract (32). Symptomatic nephrolithiasis (indinavir crystallization) has been reported to affect up to 12% (range, 5–35 %) of patients who receive indinavir, while up to 67% of patients will have asymptomatic crystalluria. The cumulative frequency of nephrolithiasis events increases with increasing exposure to indinavir. Therapy may be continued or interrupted for a few days. Adequate hydration is necessary with the administration of indinavir. Indinavir associated pyuria is frequently associated with interstitial nephritis or urothelial inflammation. Discontinuation of indinavir will lead to resolution of urine abnormalities.
Elevated Mean Corpuscular Volume (MCV) and NRTIs
Elevation of MCV or macrocytosis occurs in more than 90% of patients treated with zidovudine, but is not correlated with the development of anemia. Macrocytosis (MCV values exceeding 110/fl) develops within 2 weeks following the initiation of zidovudine therapy, and its presence can be used as a marker for medical adherence. When anemia does occur it is associated with a dose related bone marrow toxicity manifested as a macrocytic anemia. Serum B12 and folate levels are normal. Stavudine use is also associated with macrocytosis, in non-zidovudine-containing regimens (33).
Drug Screens and Efavirenz
The use of efavirenz, a potent non-nucleoside reverse transcriptase inhibitor, can cause a false-positive urine drug screen for cannabinoid. Efavirenz does not bind to cannabinoid receptors. The false-positive test results are specific to the assay kit used (34).
Evaluation of the AIDS Patient with Fever
Fever is a common symptom in HIV-infected patients, the etiology of which can be identified in more than 80% of cases (35,36). The AIDS patient with fever poses a considerable challenge given that the expanded differential may include a wide range of OIs. The CD4 cell count remains a valuable predictor of risk for infection. Patients with CD4 cell counts greater than 500 cells/mm3 should be evaluated as if immunocompetent. Patients with CD4 cell counts between 200 and 500 cells/mm3 are at increased risk for upper and lower bacterial respiratory infections, tuberculosis, and sinusitis, but overall their risk for opportunistic infection is not increased. In patients with CD4 counts less than 200 cells/mm3, Pneumocystis jiroveci pneumonia, formerly known as Pneumocystis carinii pneumonia, is the most common cause of fever in those not receiving primary prophylaxis. As the CD4 cell count decreases below 100 cells/mm3, the risk for disseminated MAC, toxoplasmosis, CMV, disseminated fungal infections, and lymphoma should be considered possible causes of fever. HIV itself is usually not the cause of fever in patients with advanced immunosuppression (37).
In patients with CD4 counts >200 cells/mm3, the clinician can usually construct a laboratory and radiographic evaluation guided by symptoms, while in patients with severe immunosuppression a broader evaluation is required. A serum cryptococcal antigen should be obtained, as it has high sensitivity and specificity for both systemic disease as well as meningitis (38). Bacterial, mycobacterial, and fungal isolator blood cultures should be performed, as well as a urine culture, despite lack of symptoms. Urine AFB cultures can be added if there is a suspicion for tuberculosis. Sputum should be evaluated with gram stain, AFB smear, and culture, as well as PCP direct fluorescent antibody. If diarrhea is present, stool studies should include bacterial culture, ova and parasites evaluation, an assay for C. difficile, and Cryptosporidia and Giardia stool antigen assays. A serum LDH may be elevated in PCP, disseminated histoplasmosis, or lymphoma. A serum CMV antigen may be useful in the patient with fever and diarrhea, hepatitis, or retinitis.
A chest radiograph should be performed in all febrile AIDS patients. Chest films may be normal in 5–10% of HIV-infected patients with tuberculosis (TB). The typical radiographic appearance of Pneumocystis jiroveci pneumonia is a bilateral interstitial pattern characterized by reticular or ground-glass opacities. However, normal chest radiographs may be seen in one third of AIDS patients with active PCP. High-resolution computed tomography (HRCT) of the chest should be obtained if there is still a clinical suspicion for Pneumocystis. HRCT has been shown in several reports to have a 100% negative predictive value in the evaluation for PCP (39,40).
A lumbar puncture should be performed if the patient is symptomatic or if the serum cryptococcal antigen is reactive. A bone marrow biopsy and culture is also useful particularly in the evaluation of the patient with cytopenias. Bacterial, fungal, and AFB cultures may yield disseminated mycobacterial or fungal disease. Histopathologic evaluation may reveal granulomas with organisms or lymphoma. Bronchoscopy may be pursued in cases of high suspicion for TB or PCP.
Guidelines for the management of opportunistic infections associated with human immunodeficiency virus are available at www.AIDSinfo.nih.gov.
Evaluation of the AIDS Patient with Focal Neurological Disease
Toxoplasma encephalitis (TE) may be distinguished from primary CNS lymphoma without a brain biopsy. TE is caused by reactivation of latent infection by the protozoan Toxoplasma gondii. Almost 90% of patients have CD4 counts less than 200 cells/mm3 and 75% have CD4 counts less than 100 cells/mm3. Serum anti-Toxoplasma IgG antibodies are detected in more than 90% of patients with TE. Lesions on CT or MRI (a more sensitive modality) are typically multiple ring-enhancing lesions with a predilection for the basal ganglia. An emipiric trial of therapy is recommended, and a response confirms a diagnosis in the patient who has a positive Toxoplasma antibody and is not receiving trimethoprim-sulfamethoxazole prophylaxis. A lumbar puncture in this setting is not necessary and maybe ill advised if cerebral edema is present (Figure 1, page 24).
Primary CNS lymphoma (PCNSL) has a similar radiographic appearance as TE. Solitary lesions are more frequent in PCNSL. Positron emission tomography (PET) and single photon emission CT (SPECT) are useful adjunctive imaging modalities as they are positive in PCNSL due to the increased metabolic activity of the tumor. Cytologic analysis of the CSF may show lymphomatous cells. Epstein-Barr virus (EBV) DNA is uniformly detected in PCNSL in AIDS patients and detection of EBV DNA by PCR on the CSF has a sensitivity of 90–100% and a specificity of 87–98% for the diagnosis of PCNSL (41,42). Combining SPECT imaging and EBV PCR provides 100% sensitivity and 100% negative predictive value in the evaluation of AIDS-related primary CNS lymphoma (43), obviating the need for brain biopsy.
Progressive multifocal leukoencephalopathy (PML) is characterized radiographically by multiple and bilateral hypodense lesions of the white matter without mass effect or enhancement on CT. MRI demonstrates areas of hypointensity on T1-weighted images and increased intensity on T2-weighted images. JC virus DNA can be detected by PCR of CSF or brain tissue with sensitivity of approximately 80% and specificity of 95%. Because of the high positive predictive value of a positive PCR, a patient with AIDS who also has a compatible MRI can be diagnosed with PML (44,45).
Other focal neurologic disease seen in AIDS patients includes cryptococcomas, tuberculomas, CMV encephalitis, neurosyphilis, Nocardia and Aspergillus infection, and bacterial brain abscesses (46).
Conclusion
As survival of the HIV-infected population improves, more patients may require hospitalization for HAART treatment failures or complications attributed to antiretroviral therapy. The hospitalist should be familiar with the complications of antiretroviral agents, the interactions between HAART and medications used to treat opportunistic infections, and medical conditions induced by HAART. Evaluation of the HIV-infected patient presenting with fever can be based on the CD4 cell count, which predicts risk for opportunistic infections. Finally, using combined diagnostic approaches along with modern imaging and laboratory assays may preclude the need for more invasive procedures in the HIV-infected hospitalized patient.
Dr. Decker may be reached at [email protected].
References
- Torres RA, Barr M. Impact of combination therapy for HIV infection on inpatient census. N Engl J Med. 1997;336:1531-2.
- Fleishman JA, Hellinger FJ. Trends in HIV-related inpatient admissions from 1993 to 1997: a seven-state study. J Acquir Immune Defic Syndr. 2001;28:73-80.
- Fleishman JA, Hellinger FH. Recent trends in HIV-related inpatient admissions 1996-2000: a 7-state study. J Acquir Immune Defic Syndr. 2003;34:102-10.
- Powderly WG. Should patients with an acute opportunistic infection receive antiretroviral therapy immediately? Advanced Studies in Medicine. 2005;5:S111-S116.
- Fagard C, Oxenius A, Gunthard H, et al. A prospective trial of structured treatment interruptions in human immunodeficiency virus infection. Arch Intern Med. 2003;163:1220-6.
- Soni N, Pozniak A. Continuing HIV therapy in the ICU. Crit Care. 2001;5:247-8.
- Purdy BD, Raymond AM, Lesar TS. Antiretroviral prescribing errors in hospitalized patients. Ann Pharmacother. 2000;34:833-8.
- Autran B, Carcelain G, Li TS, et al. Positive effects of combined antiretroviral therapy on CD4+ T cell homeostasis and function in advanced HIV disease. Science. 1997;277:112-6.
- Cooney EL. Clinical indicators of immune restoration following highly active antiretroviral therapy. Clin Infect Dis. 2002;34:224-33.
- Hirsch HH, Kaufmann G, Sendi P, BaĴegay M. Immune reconstitution in HIV-infected patients. Clin Infect Dis. 2004;38:1159-66.
- Cheng VC, Yuen KY, Chan WM, Wong SS, Ma ES, Chan RM. Immunorestitution disease involving the innate and adaptive response. Clin Infect Dis. 2000;30:882-92.
- Fishman JE, Saraf-Lavi E, Narita M, Hollender ES, Ramsinghani R, Ashkin D. Pulmonary tuberculosis in AIDS patients: transient chest radiographic worsening after initiation of antiretroviral therapy. AJR Am J Roentgenol. 2000;174:43-9.
- Piscitelli SC, Gallicano KD. Interactions among drugs for HIV and opportunistic infections. N Engl J Med. 2001;344:984-96.
- Barry M, Mulcahy F, Merry C, Gibbons S, Back D. Pharmacokinetics and potential interactions amongst antiretroviral agents used to treat patients with HIV infection. Clin Pharmacokinet. 1999;36:289-304.
- Sim SM, Hoggard PG, Sales SD, Phiboonbanakit D, Hart CA, Back DJ. Effect of ribavirin on zidovudine efficacy and toxicity in vitro: a concentration-dependent interaction. AIDS Res Hum Retroviruses. 1998;14:1661-7.
- Clarke SM, Mulcahy FM, Tjia J, et al. The pharmacokinetics of methadone in HIV-positive patients receiving the non-nucleoside reverse transcriptase inhibitor efavirenz. Br J Clin Pharmacol. 2001;51:213-7.
- Centers for Disease Control and Prevention. Updated guidelines for the use of rifabutin or rifampin for the treatment and prevention of tuberculosis among HIV-infected patients taking protease inhibitors or nonnucleoside reverse transcriptase inhibitors. Morb Mortal Wkly Rep. 2000;49:185-9.
- Havlir DV, O’Marro SD. Atazanavir: new option for treatment of HIV infection. Clin Infect Dis. 2004;38:1599-604.
- Sheng WH, Hsieh SM, Lee SC, et al. Fatal lactic acidosis associated with highly active antiretroviral therapy in patients with advanced human immunodeficiency virus infection in Taiwan. Int J STD AIDS. 2004;15:249-53.
- Herman JS, Easterbrook PJ. The metabolic toxicities of antiretroviral therapy. Int J STD AIDS. 2001;12:555-62;quiz 563-4.
- Behrens G, Schmidt H, Meyer D, Stoll M, Schmidt RE. Vascular complications associated with use of HIV protease inhibitors. Lancet. 1998;351:1958.
- Klein D, Hurley LB, Sidney S. Cardiovascular Disease and HIV Infection. N Engl J Med. 2003;349:1869-70; author reply 1869-70.
- Friis-Moller N, Sabin CA, Weber R, et al. Combination antiretroviral therapy and the risk of myocardial infarction. N Engl J Med. 2003;349:1993-2003.
- Anderson JA, Adkinson NF Jr. Allergic reactions to drugs and biologic agents. JAMA. 1987;258:2891-9.
- Hewitt RG. Abacavir hypersensitivity reaction. Clin Infect Dis. 2002;34:1137-42.
- Hetherington S, Hughes AR, Mosteller M, et al. Genetic variations in HLA-B region and hypersensitivity reactions to abacavir. Lancet. 2002;359:1121-2.
- Bossi P, Colin D, Bricaire F, Caumes E. Hypersensitivity syndrome associated with efavirenz therapy. Clin Infect Dis. 2000;30:227-8.
- Bourezane Y, Salard D, Hoen B, Vandel S, Drobacheff C, Laurent R. DRESS (drug rash with eosinophilia and systemic symptoms) syndrome associated with nevirapine therapy. Clin Infect Dis. 1998;27:1321-2.
- Walensky RP, Goldberg JH, Daily JP. Anaphylaxis after rechallenge with abacavir. AIDS. 1999;13:999-1000.
- Martin GJ, Paparello SF, Decker CF. A severe systemic reaction to trimethoprim-sulfamethoxazole in a patient infected with the human immunodeficiency virus. Clin Infect Dis. 1993;16:175-6.
- Bersoff-Matcha SJ, Miller WC, Aberg JA, et al. Sex differences in nevirapine rash. Clin Infect Dis. 2001;32:124-9.
- Kopp JB, Falloon J, Filie A, et al. Indinavir-associated interstitial nephritis and urothelial inflammation: clinical and cytologic findings. Clin Infect Dis. 2002;34:1122-8.
- Geene D, Sudre P, Anwar D, Goehring C, Saaidia A, Hirschel B. Causes of macrocytosis in HIV-infected patients not treated with zidovudine. Swiss HIV Cohort Study. J Infect. 2000;40:160-3.
- Gottesman L. Sustiva may cause false positive on marijuana test. WORLD. 1999:7.
- Sepkowitz KA, Telzak EE, Carrow M, Armstrong D. Fever among outpatients with advanced human immunodeficiency virus infection. Arch Intern Med. 1993;153: 1909-12.
- Barat LM, Gunn JE, Steger KA, Perkins CJ, Craven DE. Causes of fever in patients infected with human immunodeficiency virus who were admitted to Boston City Hospital. Clin Infect Dis. 1996;23:320-8.
- Sepkowitz KA. FUO and AIDS. Curr Clin Top Infect Dis. 1999;19:1-15.
- Asawavichienjinda T, Sitthi-Amorn C, Tanyanont V. Serum cyrptococcal antigen: diagnostic value in the diagnosis of AIDS-related cryptococcal meningitis. J Med Assoc Thai. 1999;82:65-71.
- Richards PJ, Riddell L, Reznek RH, Armstrong P, Pinching AJ, Parkin JM. High resolution computed tomography in HIV patients with suspected Pneumocystis carinii pneumonia and a normal chest radiograph. Clin Radiol. 1996;51:689-93.
- Gruden JF, Huang L, Turner J, et al. High-resolution CT in the evaluation of clinically suspected Pneumocystis carinii pneumonia in AIDS patients with normal, equivocal, or nonspecific radiographic findings. AJR Am J Roentgenol. 1997;169:967-75.
- MacMahon EM, Glass JD, Hayward SD, et al. Association of Epstein-Barr virus with primary central nervous system lymphoma in AIDS. AIDS Res Hum Retroviruses. 1992;8:740-2.
- Rao CR, Jain K, Bhatia K, Laksmaiah KC, Shankar SK. Association of primary central nervous system lymphomas with the Epstein-Barr virus. Neurol India. 2003;51:237-40.
- Antinori A, De Rossi G, Ammassari A, et al. Value of combined approach with thallium-201 single-photon emission computed tomography and Epstein-Barr virus DNA polymerase chain reaction in CSF for the diagnosis of AIDS-related primary CNS lymphoma. J Clin Oncol. 1999;17:554-60.
- Post MJ, Yiannoutsos C, Simpson D, et al. Progressive multifocal leukoencephalopathy in AIDS: are there any MR findings useful to patient management and predictive of patient survival? AIDS Clinical Trials Group, 243 Team. AJNR Am J Neuroradiol. 1999;20:1896-906.
- Weber T. Cerebrospinal fluid analysis for the diagnosis of human immunodeficiency virus-related neurologic diseases. Semin Neurol. 1999;19:223-33.
- Skiest DJ. Focal neurological disease in patients with acquired immunodeficiency syndrome. Clin Infect Dis. 2002;34:103-15.
The opinions and assertions contained herein are those of the authors and are not to be construed as official or as reflecting the views of the Department of Defense, the Department of the Navy, or the naval services at large.
Introduction
An estimated 850,000 to 950,000 persons in the United States are living with human immunodeficiency virus (HIV), 280,000 of whom are unaware of their infection and another 43,000 of whom meet the definition of acquired immunodeficiency syndrome (AIDS) (www.cdc.gov). The use of highly active antiretroviral therapy (HAART) has produced significant declines in morbidity and mortality from AIDS. Compared with the first 2 decades of the HIV pandemic, the number of HIV-related hospital admissions has declined. However, recently, this rate of decline has markedly slowed (1-3). The reasons for this plateau are many including a steady number of admissions for complications related to HAART, treatment failures, and the overall increased prevalence of HIV infection. Not only will HIV-infected patients still frequently require admission to the hospital, but the complexity of their inpatient care will continue to increase with the advancements in multiple drug regimens, aging of the HIV-infected population, and the interaction of HIV infection with medical comorbidities, many of which are attributable to HAART.
The hospitalist caring for the inpatient with AIDS is presented with several challenges including not only the diagnosis and management of opportunistic infections, but also the complications of HAART. In this article we review the guidelines for the initiation and continuation of HAART in the hospital, review important clinical complications of antiretroviral therapy, and review conditions that may result in the hospitalization of AIDS patients.
Initiation of HAART in the Hospital
In those who do not have access to health care, the initial diagnosis of HIV infection frequently occurs during a hospitalization for an AIDS-defining illness. Initiation of antiretrovirals is contingent on several issues, including CD4 count, viral load, clinical status, likelihood of continued adherence, and the concurrent treatment of opportunistic infections (OIs). All patients with HIV infection and a CD4 count <200 cells/mm3 or an AIDS-defining illness should receive antiretroviral therapy. Controversy exists as to whether a patient admitted for the treatment of an opportunistic infection should begin antiretroviral therapy immediately, or whether this therapy should be deferred until after acute treatment of the OI. The potential detrimental effects of drug-drug interactions, the need for treatment interruptions, and drug-related toxicity between antiretrovirals and OI-specific therapy may support initiating HAART after control of an OI is achieved. Conversely, for some opportunistic infections, such as cryptosporidiosis, the use of HAART is essential for successful treatment of the infection.
An ongoing randomized controlled trial initiated within the Adult AIDS Clinical Trials Group (ACTG) comparing outcomes between patients who start HAART immediately after presentation with an acute OI and patients who start HAART at least 4 weeks after the OI has resolved should help identify the factors supporting early or delayed initiation of antiretrovirals (4).
Generally speaking, HAART can be administered by combining either a protease inhibitor (PI) or a nonnucleoside reverse transcriptase inhibitor (NNRTI) with 2 nucleoside reverse transcriptase inhibitors (NRTIs). There are currently more than 20 FDA-approved antiretrovirals. Frequent updates on the guidelines for the use of antiretroviral agents in HIV-infected adults are available at www.AIDSinfo.nih.gov, and a discussion of this topic is beyond the scope of this review.
Continuation of HAART in the Hospital
In most cases, every effort should be made to minimize interruption of HAART during a hospitalization. Although some investigators are examining the virologic and immunologic safety of interrupting HAART as a treatment strategy, there are few data on viral replication, CD4 cell count decline, and rate of acquisition of new mutations in hospitalized patients who have unexpected treatment interruptions (5). The long half-life of some antiretrovirals promotes the emergence of resistance once HAART is stopped. For example, once NNRTIs are stopped, subtherapeutic levels remain in the plasma and cells for several days. HIV then replicates in a milieu that may select for resistance mutations.
Because zidovudine is the only antiretroviral available in a parenteral preparation, it is often difficult to continue HAART when a patient cannot take medications by mouth. Drugs given by the enteral route in a hospitalized patient may also be poorly absorbed, and few data exist on the absorption of antiretrovirals administered through a gastrostomy or jejunostomy tube (6).
Prescribing HAART in the Hospital
Antiretroviral prescribing errors occur frequently in the hospitalized AIDS patient. The most common errors include overdosing or underdosing, missing components of multidrug regimens, or missing critical drug-drug interactions (7). Underdosing may lead to resistance, and overdosing contributes to increased toxicity. In one report, prescribing errors occurred in 12% of admissions in the post-HAART era (1998) compared with 2% of admissions in the pre-HAART era (1996) (7). The NRTIs, including didanosine, emtricitabine, lamivudine, stavudine, and zidovudine, require decreased dosing in renal insufficiency. Tenofovir is not recommended for use if the creatine clearance is less than 60 mL/minute. Dosage adjustments in hepatic disease are recommended for amprenavir, fosamprenavir, delavirdine, efavirenz, and nevirapine.
Immune Reconstitution Syndrome
The widespread use of HAART has produced sustained suppression of HIV replication and recovery of CD4 cell counts. It also became evident that HAART resulted in not only a numerical increase in CD4 cells, but also in a functional immune recovery (8-10). This improved T-cell response to antigens results in adequate protection against specific opportunistic infections, allowing for discontinuation of primary and secondary prophylaxis in HIV-infected patients. Immune reconstitution syndrome (IRS), an inflammatory syndrome, is recognized as a potential complication that can occur days to months after starting HAART. The onset of IRS is characterized by a paradoxical worsening of clinical or laboratory parameters despite a favorable response in CD4 cell counts and the suppression of viral replication (9,11,12). IRS has been reported to occur in 10–25% of patients who receive HAART and more commonly in those whose CD4 cell counts are <50 cells/mm3 at the start of HAART (9,11). It is postulated that the inflammatory response is triggered by the recognition of antigens associated with ongoing infection or recognition of persisting antigens associated with past (nonreplicating) infections. Mycobacterial antigens, frequently implicated in IRS, are responsible for about one third of cases. Other antigens associated with IRS include cytomegalovirus and hepatitis B and C (11). In most circumstances, with the management of IRS, HAART should be continued, while specific antimicrobial therapy and steroids should be considered (10).
Medical Conditions that Should Prompt HIV Screening
There are several medical conditions that should prompt screening for HIV infection. Generally, anyone presenting with a fever of unknown etiology who is sexually active or had a blood transfusion prior to 1985 should be screened for HIV infection. Symptoms consistent with acute retroviral syndrome (fever, sore throat, malaise, and skin rash) may be more commonly recognized by clinicians now than previously, and this remains a “golden opportunity” to intervene. Frequently, acute retroviral syndrome will be attributed to Epstein-Barr virus; however, caution should be used in the diagnosis of mononucleosis in those other than teenage populations. It is recommended that all persons presenting with any sexually transmitted disease, unexplained generalized lymphadenopathy, oral candidiasis, or tuberculosis should also be tested. Other conditions where HIV infection should be considered include enigmatic pneumonia, acute hepatitis B infection, herpes zoster infection (particularly in younger, seemingly immunocompetent individuals), idiopathic thrombocytopenic purpura, and nephropathy of unknown cause.
Drug Interactions
Drug interactions are an important consideration in the treatment of HIV infection. Interactions between HAART and other drugs used for the treatment or prophylaxis of opportunistic infections along with those used for the treatment of drug-induced endocrinopathies (hyperlipidemia, diabetes mellitus) are virtually unavoidable. Drug interactions occur either because of drug metabolism or absorption. The multiple metabolic pathways of some drugs make it difficult to predict the outcome of drug interactions. All protease inhibitors and non-nucleoside reverse transcriptase inhibitors are metabolized by the cytochrome P-450 enzyme system and each of these drugs may alter the metabolism of other antiretrovirals and concomitantly administered drugs (13,14). A decrease in trough plasma concentrations of the protease inhibitors to a level below the in vitro concentration required to inhibit replication of 50% of viral strains (IC50) may lead to development of resistance. Because nucleoside analogue reverse transcriptase inhibitors are primarily eliminated by the kidney, they do not interact with other drugs through the cytochrome P-450 system.
One noteworthy interaction that the clinician caring for HIV-infected patients should be aware of is the interaction of ribavirin with zidovudine. Ribavirin decreases the phosphorylation of zidovudine and stavudine in vitro, resulting in decreased concentrations of the active compound. HIV-infected patients who are coinfected with hepatitis C may be treated with regimens that include ribavirin, which may reduce the efficacy of zidovudine (15). Another important interaction is the effect of nevirapine or efavirenz on plasma methadone concentrations. Both drugs can decrease methadone plasma levels by 50%, and patients receiving chronic therapy may need increased methadone doses to prevent withdrawal symptoms (16).
Protease inhibitors are associated with numerous interactions including certain antiarrhythmics, sedatives, hypnotics, ergot derivatives, and several lipid-lowering agents (statins). Not only do protease inhibitors affect the metabolism of certain drugs, but also their own metabolism is altered by other inducers or inhibitors of cytochrome activity that can cause clinically important decreases in serum levels of protease inhibitors. One widely recognized interaction is that of rifampin, which may decrease levels of some protease inhibitors by 80%. The resulting low plasma concentrations may promote viral resistance and result in treatment failure. Patients being treated for tuberculosis, who are also receiving protease inhibitors should be treated with a four-drug regimen that includes rifabutin (at half dose) instead of rifampin. Updated guidelines for the use of rifabutin or rifampin in HIV-infected patients receiving antiretroviral agents have been reviewed recently (17).
Other potent inducers such as phenytoin, phenobarbital, and carbamazepine can cause similar reductions in serum levels of protease inhibitors. Azole antifungal drugs and macrolides also have important interactions that complicate both the treatment and prophylaxis of opportunistic infections.
Interactions that interfere with absorption can also affect plasma drug concentrations. For example, the absorption of fluconazole is unaffected by variations in gastric pH, while itraconazole and ketoconazole require an acidic environment for optimal absorption. The protease inhibitor, atazanavir, also requires a low pH for absorption and thus is contraindicated with the use of proton pump inhibitors; taking atazanavir with acidic beverages is not sufficient to overcome this (18).
New information about drug interactions becomes known on almost a daily basis in patients with HIV infection. The number of documented and theoretical interactions can become overwhelming to the clinician. Clinicians should suspect potential drug interactions in a patient who is failing therapy but who is adherent to HAART. Fortunately, there are extensive tables on Web sites (www.hivatis.org) and product information to aid in the recognition and management of drug interactions.
Complications of HAART
Diabetes mellitus, hyperlipidemias, lipodystrophy, and insulin resistance are among the many complex metabolic abnormalities attributable to the use of HAART. For the most part, these complications are managed conservatively and usually do not mandate the discontinuation of HAART. Pancreatitis, hepatic steatosis, and lactic acidosis are wellrecognized complications of NRTIs. These are usually more acute and may result in hospitalization and necessitate the discontinuation of medications. Cessation of the offending agent (didanosine [ddI], stavudine [d4T], and zalcitabine [ddC) usually results in resolution of pancreatitis, but the episode may limit use of these agents in the future. Hepatic steatosis and lactic acidosis are rare but life-threatening adverse effects associated with the mitochondrial toxicity seen with the NRTIs. Symptoms usually develop insidiously with nausea, vomiting, abdominal pain, weight loss, or dyspnea and can progress rapidly to fatal lactic acidosis. Hepatomegaly, ascites, elevated liver associated enzymes, and an increased anion gap with lactic acidemia are usually present (19,20). Discontinuation of antiretroivirals is imperative.
There is an accumulating body of evidence that suggests that HIV-infected patients receiving HAART may be at risk for accelerated coronary disease (21). In addition, some cohort studies have reported an increased incidence of myocardial infarction (MI) following the introduction of HAART and the risk for MI rose progressively with the number of years on antiretroviral therapy (22,23). However, it is important to note that many traditional risk factors for coronary artery disease contribute more substantially to the risk for a cardiovascular event than does HAART. Therefore, aggressive modification of primary cardiac risk factors is warranted.
Hypersensitivity Drug Reactions
Drug hypersensitivity reactions are life-threatening reactions that result in a systemic illness that usually includes fever and maculopapular rash accompanied by constitutional symptoms (fatigue, myalgias, and arthralgias), visceral involvement (lymphadenopathy, mucositis, pneumonitis, myocarditis, hepatitis, and interstitial nephritis), and hematologic abnormalities (eosinophilia) (24).
Abacavir, an NRTI, is a relatively new antiretroviral agent used in many HAART regimens. Abacavir is associated with a hypersensitivity reaction, which can be fatal if abacavir use is continued despite the reaction, or if re-challenge with the drug takes place after the reaction (25). The overall incidence of this reaction appears to be around 4% (25). Prior antiretroviral experience and being of African descent are associated with a nearly 40% reduction in the risk of this hypersensitivity reaction, while patients of white race are at a significantly greater risk. CD4 cell counts do not appear to be significantly related to abacavir hypersensitivity (26). The exact metabolite that is likely responsible for abacavir hypersensitivity is unknown.
The most common symptoms of abacavir hypersensitivity reaction are fever, rash, nausea, vomiting, and abdominal pain. Occasionally, respiratory symptoms will be present and can mimic influenza. However, gastrointestinal symptoms are the most prominent complaints after fever and rash and help to distinguish between influenza and abacavir hypersensitivity. More than 90% of hypersensitivity reactions occur during the first 6 weeks of treatment, with a median time to development of 8 days. A fever that develops within a few weeks after the initiation of therapy with abacavir may be due to causes other than hypersensitivity. One of the most common situations is the simultaneous initiation of treatment with other drugs, such as trimethoprimsulfamethxazole, efavirenz, or nevirapine, all of which are associated with a higher incidence of hypersensitivity than abacavir (27,28). Symptoms may be sudden and worsen over a few days if abacavir is continued. Symptoms tend to improve in 48 hours after abacavir is discontinued. Supportive therapy includes intravenous hydration and withdrawal of abacavir as well as all other antiretrovirals. Early in the use of this medication, 20% of patients who were re-challenged with the drug experienced unanticipated life-threatening events manifesting as an anaphylactic or immediate type hypersensitivity reaction. Hypotension, renal insufficiency, and bronchospasm have resulted in death. Rechallenge symptoms have been seen with the first dose (29). A discussion of the potential for this hypersensitivity is warranted when prescribing this agent. In the United States, a patient information card warning of this hypersensitivity reaction is distributed to the patient with each bottle of abacavir. Prednisone does not prevent the development of hypersensitivity reaction.
Symptoms of toxicity from TMP-SMX are more likely to occur in the HIV infected than in patients without HIV infection. Fever and rash can occur in up to 50% of HIV-infected patients. The rash can be treatment limiting or severe in up to 20% of HIV-infected patients who receive it. Life-threatening reactions may occur, including fatal Stevens Johnson-type exfoliative skin reactions. Most toxicity in HIV-infected patients appears to be related to metabolites of the sulfamethoxazole component and decreased levels of glutathione. There have been reports of severe systemic reactions that resemble anaphylaxis or septic shock occurring in HIV-infected patients who are re-challenged with TMP-SMX after experiencing toxicity within the previous 6–8 weeks (30).
The NNRTIf nevirapine and efavirenz can cause a delayed hypersensitivity reaction similar to that seen with abacavir. Cutaneous involvement is a prominent component of both nevirapine and efavirenz hypersensitivity reaction, with rash more likely to occur with the use of nevirapine. In addition, female patients have a higher propensity of developing Stevens-Johnson syndrome and symptomatic hepatic events from nevirapine (28,31).
Laboratory Abnormalities Related to Drugs
Hyperbilirubinemia and Atazanavir and Indinavir
Atazanavir, a protease inhibitor, is metabolized by the liver via CYP3A and also inhibits both CTP3A and UGT1A1. UGT1A1 is required for conjugation of bilirubin and inhibition of this enzyme results in elevated levels of unconjugated bilirubin. This effect is similar to what is observed in Gilbert’s syndrome. Asymptomatic indirect hyperbilirubemia may be seen in up to 60% of patients receiving atazanavir. Total bilirubin levels may rise to greater than 5 mg/dL, and more than 17% of patients may experience jaundice (18). Concurrent elevations in hepatic serum transaminases should not be attributed to atazanavir and alternative etiologies for these elevations should be sought. This hyperbilirubinemia is reversible upon discontinuation of the atazanavir.
Similarly, but to a lesser degree, asymptomatic unconjugated hyperbilirubinemia (>2 mg/dL) has been reported in up to 14% of patients treated with indinavir. Elevated serum transaminases were seen in less than 1%.
Renal Abnormalities and Indinavir
Several renal syndromes have been associated with indinavir use, ranging from obstructive uropathy and acute renal failure to asymptomatic pyuria. The range of clinical syndromes is a consequence of indinavir crystals aggregating within or irritating the urinary tract (32). Symptomatic nephrolithiasis (indinavir crystallization) has been reported to affect up to 12% (range, 5–35 %) of patients who receive indinavir, while up to 67% of patients will have asymptomatic crystalluria. The cumulative frequency of nephrolithiasis events increases with increasing exposure to indinavir. Therapy may be continued or interrupted for a few days. Adequate hydration is necessary with the administration of indinavir. Indinavir associated pyuria is frequently associated with interstitial nephritis or urothelial inflammation. Discontinuation of indinavir will lead to resolution of urine abnormalities.
Elevated Mean Corpuscular Volume (MCV) and NRTIs
Elevation of MCV or macrocytosis occurs in more than 90% of patients treated with zidovudine, but is not correlated with the development of anemia. Macrocytosis (MCV values exceeding 110/fl) develops within 2 weeks following the initiation of zidovudine therapy, and its presence can be used as a marker for medical adherence. When anemia does occur it is associated with a dose related bone marrow toxicity manifested as a macrocytic anemia. Serum B12 and folate levels are normal. Stavudine use is also associated with macrocytosis, in non-zidovudine-containing regimens (33).
Drug Screens and Efavirenz
The use of efavirenz, a potent non-nucleoside reverse transcriptase inhibitor, can cause a false-positive urine drug screen for cannabinoid. Efavirenz does not bind to cannabinoid receptors. The false-positive test results are specific to the assay kit used (34).
Evaluation of the AIDS Patient with Fever
Fever is a common symptom in HIV-infected patients, the etiology of which can be identified in more than 80% of cases (35,36). The AIDS patient with fever poses a considerable challenge given that the expanded differential may include a wide range of OIs. The CD4 cell count remains a valuable predictor of risk for infection. Patients with CD4 cell counts greater than 500 cells/mm3 should be evaluated as if immunocompetent. Patients with CD4 cell counts between 200 and 500 cells/mm3 are at increased risk for upper and lower bacterial respiratory infections, tuberculosis, and sinusitis, but overall their risk for opportunistic infection is not increased. In patients with CD4 counts less than 200 cells/mm3, Pneumocystis jiroveci pneumonia, formerly known as Pneumocystis carinii pneumonia, is the most common cause of fever in those not receiving primary prophylaxis. As the CD4 cell count decreases below 100 cells/mm3, the risk for disseminated MAC, toxoplasmosis, CMV, disseminated fungal infections, and lymphoma should be considered possible causes of fever. HIV itself is usually not the cause of fever in patients with advanced immunosuppression (37).
In patients with CD4 counts >200 cells/mm3, the clinician can usually construct a laboratory and radiographic evaluation guided by symptoms, while in patients with severe immunosuppression a broader evaluation is required. A serum cryptococcal antigen should be obtained, as it has high sensitivity and specificity for both systemic disease as well as meningitis (38). Bacterial, mycobacterial, and fungal isolator blood cultures should be performed, as well as a urine culture, despite lack of symptoms. Urine AFB cultures can be added if there is a suspicion for tuberculosis. Sputum should be evaluated with gram stain, AFB smear, and culture, as well as PCP direct fluorescent antibody. If diarrhea is present, stool studies should include bacterial culture, ova and parasites evaluation, an assay for C. difficile, and Cryptosporidia and Giardia stool antigen assays. A serum LDH may be elevated in PCP, disseminated histoplasmosis, or lymphoma. A serum CMV antigen may be useful in the patient with fever and diarrhea, hepatitis, or retinitis.
A chest radiograph should be performed in all febrile AIDS patients. Chest films may be normal in 5–10% of HIV-infected patients with tuberculosis (TB). The typical radiographic appearance of Pneumocystis jiroveci pneumonia is a bilateral interstitial pattern characterized by reticular or ground-glass opacities. However, normal chest radiographs may be seen in one third of AIDS patients with active PCP. High-resolution computed tomography (HRCT) of the chest should be obtained if there is still a clinical suspicion for Pneumocystis. HRCT has been shown in several reports to have a 100% negative predictive value in the evaluation for PCP (39,40).
A lumbar puncture should be performed if the patient is symptomatic or if the serum cryptococcal antigen is reactive. A bone marrow biopsy and culture is also useful particularly in the evaluation of the patient with cytopenias. Bacterial, fungal, and AFB cultures may yield disseminated mycobacterial or fungal disease. Histopathologic evaluation may reveal granulomas with organisms or lymphoma. Bronchoscopy may be pursued in cases of high suspicion for TB or PCP.
Guidelines for the management of opportunistic infections associated with human immunodeficiency virus are available at www.AIDSinfo.nih.gov.
Evaluation of the AIDS Patient with Focal Neurological Disease
Toxoplasma encephalitis (TE) may be distinguished from primary CNS lymphoma without a brain biopsy. TE is caused by reactivation of latent infection by the protozoan Toxoplasma gondii. Almost 90% of patients have CD4 counts less than 200 cells/mm3 and 75% have CD4 counts less than 100 cells/mm3. Serum anti-Toxoplasma IgG antibodies are detected in more than 90% of patients with TE. Lesions on CT or MRI (a more sensitive modality) are typically multiple ring-enhancing lesions with a predilection for the basal ganglia. An emipiric trial of therapy is recommended, and a response confirms a diagnosis in the patient who has a positive Toxoplasma antibody and is not receiving trimethoprim-sulfamethoxazole prophylaxis. A lumbar puncture in this setting is not necessary and maybe ill advised if cerebral edema is present (Figure 1, page 24).
Primary CNS lymphoma (PCNSL) has a similar radiographic appearance as TE. Solitary lesions are more frequent in PCNSL. Positron emission tomography (PET) and single photon emission CT (SPECT) are useful adjunctive imaging modalities as they are positive in PCNSL due to the increased metabolic activity of the tumor. Cytologic analysis of the CSF may show lymphomatous cells. Epstein-Barr virus (EBV) DNA is uniformly detected in PCNSL in AIDS patients and detection of EBV DNA by PCR on the CSF has a sensitivity of 90–100% and a specificity of 87–98% for the diagnosis of PCNSL (41,42). Combining SPECT imaging and EBV PCR provides 100% sensitivity and 100% negative predictive value in the evaluation of AIDS-related primary CNS lymphoma (43), obviating the need for brain biopsy.
Progressive multifocal leukoencephalopathy (PML) is characterized radiographically by multiple and bilateral hypodense lesions of the white matter without mass effect or enhancement on CT. MRI demonstrates areas of hypointensity on T1-weighted images and increased intensity on T2-weighted images. JC virus DNA can be detected by PCR of CSF or brain tissue with sensitivity of approximately 80% and specificity of 95%. Because of the high positive predictive value of a positive PCR, a patient with AIDS who also has a compatible MRI can be diagnosed with PML (44,45).
Other focal neurologic disease seen in AIDS patients includes cryptococcomas, tuberculomas, CMV encephalitis, neurosyphilis, Nocardia and Aspergillus infection, and bacterial brain abscesses (46).
Conclusion
As survival of the HIV-infected population improves, more patients may require hospitalization for HAART treatment failures or complications attributed to antiretroviral therapy. The hospitalist should be familiar with the complications of antiretroviral agents, the interactions between HAART and medications used to treat opportunistic infections, and medical conditions induced by HAART. Evaluation of the HIV-infected patient presenting with fever can be based on the CD4 cell count, which predicts risk for opportunistic infections. Finally, using combined diagnostic approaches along with modern imaging and laboratory assays may preclude the need for more invasive procedures in the HIV-infected hospitalized patient.
Dr. Decker may be reached at [email protected].
References
- Torres RA, Barr M. Impact of combination therapy for HIV infection on inpatient census. N Engl J Med. 1997;336:1531-2.
- Fleishman JA, Hellinger FJ. Trends in HIV-related inpatient admissions from 1993 to 1997: a seven-state study. J Acquir Immune Defic Syndr. 2001;28:73-80.
- Fleishman JA, Hellinger FH. Recent trends in HIV-related inpatient admissions 1996-2000: a 7-state study. J Acquir Immune Defic Syndr. 2003;34:102-10.
- Powderly WG. Should patients with an acute opportunistic infection receive antiretroviral therapy immediately? Advanced Studies in Medicine. 2005;5:S111-S116.
- Fagard C, Oxenius A, Gunthard H, et al. A prospective trial of structured treatment interruptions in human immunodeficiency virus infection. Arch Intern Med. 2003;163:1220-6.
- Soni N, Pozniak A. Continuing HIV therapy in the ICU. Crit Care. 2001;5:247-8.
- Purdy BD, Raymond AM, Lesar TS. Antiretroviral prescribing errors in hospitalized patients. Ann Pharmacother. 2000;34:833-8.
- Autran B, Carcelain G, Li TS, et al. Positive effects of combined antiretroviral therapy on CD4+ T cell homeostasis and function in advanced HIV disease. Science. 1997;277:112-6.
- Cooney EL. Clinical indicators of immune restoration following highly active antiretroviral therapy. Clin Infect Dis. 2002;34:224-33.
- Hirsch HH, Kaufmann G, Sendi P, BaĴegay M. Immune reconstitution in HIV-infected patients. Clin Infect Dis. 2004;38:1159-66.
- Cheng VC, Yuen KY, Chan WM, Wong SS, Ma ES, Chan RM. Immunorestitution disease involving the innate and adaptive response. Clin Infect Dis. 2000;30:882-92.
- Fishman JE, Saraf-Lavi E, Narita M, Hollender ES, Ramsinghani R, Ashkin D. Pulmonary tuberculosis in AIDS patients: transient chest radiographic worsening after initiation of antiretroviral therapy. AJR Am J Roentgenol. 2000;174:43-9.
- Piscitelli SC, Gallicano KD. Interactions among drugs for HIV and opportunistic infections. N Engl J Med. 2001;344:984-96.
- Barry M, Mulcahy F, Merry C, Gibbons S, Back D. Pharmacokinetics and potential interactions amongst antiretroviral agents used to treat patients with HIV infection. Clin Pharmacokinet. 1999;36:289-304.
- Sim SM, Hoggard PG, Sales SD, Phiboonbanakit D, Hart CA, Back DJ. Effect of ribavirin on zidovudine efficacy and toxicity in vitro: a concentration-dependent interaction. AIDS Res Hum Retroviruses. 1998;14:1661-7.
- Clarke SM, Mulcahy FM, Tjia J, et al. The pharmacokinetics of methadone in HIV-positive patients receiving the non-nucleoside reverse transcriptase inhibitor efavirenz. Br J Clin Pharmacol. 2001;51:213-7.
- Centers for Disease Control and Prevention. Updated guidelines for the use of rifabutin or rifampin for the treatment and prevention of tuberculosis among HIV-infected patients taking protease inhibitors or nonnucleoside reverse transcriptase inhibitors. Morb Mortal Wkly Rep. 2000;49:185-9.
- Havlir DV, O’Marro SD. Atazanavir: new option for treatment of HIV infection. Clin Infect Dis. 2004;38:1599-604.
- Sheng WH, Hsieh SM, Lee SC, et al. Fatal lactic acidosis associated with highly active antiretroviral therapy in patients with advanced human immunodeficiency virus infection in Taiwan. Int J STD AIDS. 2004;15:249-53.
- Herman JS, Easterbrook PJ. The metabolic toxicities of antiretroviral therapy. Int J STD AIDS. 2001;12:555-62;quiz 563-4.
- Behrens G, Schmidt H, Meyer D, Stoll M, Schmidt RE. Vascular complications associated with use of HIV protease inhibitors. Lancet. 1998;351:1958.
- Klein D, Hurley LB, Sidney S. Cardiovascular Disease and HIV Infection. N Engl J Med. 2003;349:1869-70; author reply 1869-70.
- Friis-Moller N, Sabin CA, Weber R, et al. Combination antiretroviral therapy and the risk of myocardial infarction. N Engl J Med. 2003;349:1993-2003.
- Anderson JA, Adkinson NF Jr. Allergic reactions to drugs and biologic agents. JAMA. 1987;258:2891-9.
- Hewitt RG. Abacavir hypersensitivity reaction. Clin Infect Dis. 2002;34:1137-42.
- Hetherington S, Hughes AR, Mosteller M, et al. Genetic variations in HLA-B region and hypersensitivity reactions to abacavir. Lancet. 2002;359:1121-2.
- Bossi P, Colin D, Bricaire F, Caumes E. Hypersensitivity syndrome associated with efavirenz therapy. Clin Infect Dis. 2000;30:227-8.
- Bourezane Y, Salard D, Hoen B, Vandel S, Drobacheff C, Laurent R. DRESS (drug rash with eosinophilia and systemic symptoms) syndrome associated with nevirapine therapy. Clin Infect Dis. 1998;27:1321-2.
- Walensky RP, Goldberg JH, Daily JP. Anaphylaxis after rechallenge with abacavir. AIDS. 1999;13:999-1000.
- Martin GJ, Paparello SF, Decker CF. A severe systemic reaction to trimethoprim-sulfamethoxazole in a patient infected with the human immunodeficiency virus. Clin Infect Dis. 1993;16:175-6.
- Bersoff-Matcha SJ, Miller WC, Aberg JA, et al. Sex differences in nevirapine rash. Clin Infect Dis. 2001;32:124-9.
- Kopp JB, Falloon J, Filie A, et al. Indinavir-associated interstitial nephritis and urothelial inflammation: clinical and cytologic findings. Clin Infect Dis. 2002;34:1122-8.
- Geene D, Sudre P, Anwar D, Goehring C, Saaidia A, Hirschel B. Causes of macrocytosis in HIV-infected patients not treated with zidovudine. Swiss HIV Cohort Study. J Infect. 2000;40:160-3.
- Gottesman L. Sustiva may cause false positive on marijuana test. WORLD. 1999:7.
- Sepkowitz KA, Telzak EE, Carrow M, Armstrong D. Fever among outpatients with advanced human immunodeficiency virus infection. Arch Intern Med. 1993;153: 1909-12.
- Barat LM, Gunn JE, Steger KA, Perkins CJ, Craven DE. Causes of fever in patients infected with human immunodeficiency virus who were admitted to Boston City Hospital. Clin Infect Dis. 1996;23:320-8.
- Sepkowitz KA. FUO and AIDS. Curr Clin Top Infect Dis. 1999;19:1-15.
- Asawavichienjinda T, Sitthi-Amorn C, Tanyanont V. Serum cyrptococcal antigen: diagnostic value in the diagnosis of AIDS-related cryptococcal meningitis. J Med Assoc Thai. 1999;82:65-71.
- Richards PJ, Riddell L, Reznek RH, Armstrong P, Pinching AJ, Parkin JM. High resolution computed tomography in HIV patients with suspected Pneumocystis carinii pneumonia and a normal chest radiograph. Clin Radiol. 1996;51:689-93.
- Gruden JF, Huang L, Turner J, et al. High-resolution CT in the evaluation of clinically suspected Pneumocystis carinii pneumonia in AIDS patients with normal, equivocal, or nonspecific radiographic findings. AJR Am J Roentgenol. 1997;169:967-75.
- MacMahon EM, Glass JD, Hayward SD, et al. Association of Epstein-Barr virus with primary central nervous system lymphoma in AIDS. AIDS Res Hum Retroviruses. 1992;8:740-2.
- Rao CR, Jain K, Bhatia K, Laksmaiah KC, Shankar SK. Association of primary central nervous system lymphomas with the Epstein-Barr virus. Neurol India. 2003;51:237-40.
- Antinori A, De Rossi G, Ammassari A, et al. Value of combined approach with thallium-201 single-photon emission computed tomography and Epstein-Barr virus DNA polymerase chain reaction in CSF for the diagnosis of AIDS-related primary CNS lymphoma. J Clin Oncol. 1999;17:554-60.
- Post MJ, Yiannoutsos C, Simpson D, et al. Progressive multifocal leukoencephalopathy in AIDS: are there any MR findings useful to patient management and predictive of patient survival? AIDS Clinical Trials Group, 243 Team. AJNR Am J Neuroradiol. 1999;20:1896-906.
- Weber T. Cerebrospinal fluid analysis for the diagnosis of human immunodeficiency virus-related neurologic diseases. Semin Neurol. 1999;19:223-33.
- Skiest DJ. Focal neurological disease in patients with acquired immunodeficiency syndrome. Clin Infect Dis. 2002;34:103-15.