User login
Brendon Shank joined the Society of Hospital Medicine in February 2011 and serves as Associate Vice President of Communications. He is responsible for maintaining a dialogue between SHM and its many audiences, including members, media and others in healthcare.
Stage Presence
For hospitalist Robert Wachter, MD, MHM, the next annual SHM meeting will be particularly poignant, and not just because he’s HM11’s featured speaker.
Next year will mark the 15th anniversary of the New England Journal of Medicine article coauthored by Dr. Wachter that introduced the term “hospitalist” to the American healthcare lexicon. The specialty is growing and developing into adulthood nicely, he says, which will be part of his presentation in Grapevine, Texas.
“At age 15, that’s when you move to adolescence—you’re going to be off on adulthood and on your own,” says Dr. Wachter, professor, chief of the Division of Hospital Medicine, and chief of the Medical Service at the University of California at San Francisco Medical Center, former SHM president and author of the blog Wachter’s World (www.wachtersworld.com).
Like a proud father, Dr. Wachter expects that he will reminisce about the past, speculate about HM’s bright future, and encourage hospitalists to continue their work.
“This will be an optimistic talk,” he says. “The growth has been extraordinary.”
At the outset of the specialty, Dr. Wachter says, he and colleagues predicted some of the current trends, but they underestimated how powerful some would become.
“We couldn’t have predicted that the pressures to increase quality and safety would be as intense as they are today, but we did a good job believing that these areas were important before they hit,” he says.
Looking forward, he says, other emerging forces will join quality and safety at the forefront of HM. “The next five years will likely bring similar pressures on efficiency and throughput,” he says. “I’m going to encourage folks to stay ahead of the curve.”
Having attended every annual conference since the beginning, Dr. Wachter looks forward to “polar things” about each meeting: catching up with the founders of the movement and seeing new faces.
“What’s more fun for me is the amount of youthful energy at the meetings,” he says, especially of the hospitalists he has mentored over the years. “When I come with my group from UCSF, it gives me tremendous pride.” TH
Brendon Shank is a freelance writer based in Philadelphia.
For hospitalist Robert Wachter, MD, MHM, the next annual SHM meeting will be particularly poignant, and not just because he’s HM11’s featured speaker.
Next year will mark the 15th anniversary of the New England Journal of Medicine article coauthored by Dr. Wachter that introduced the term “hospitalist” to the American healthcare lexicon. The specialty is growing and developing into adulthood nicely, he says, which will be part of his presentation in Grapevine, Texas.
“At age 15, that’s when you move to adolescence—you’re going to be off on adulthood and on your own,” says Dr. Wachter, professor, chief of the Division of Hospital Medicine, and chief of the Medical Service at the University of California at San Francisco Medical Center, former SHM president and author of the blog Wachter’s World (www.wachtersworld.com).
Like a proud father, Dr. Wachter expects that he will reminisce about the past, speculate about HM’s bright future, and encourage hospitalists to continue their work.
“This will be an optimistic talk,” he says. “The growth has been extraordinary.”
At the outset of the specialty, Dr. Wachter says, he and colleagues predicted some of the current trends, but they underestimated how powerful some would become.
“We couldn’t have predicted that the pressures to increase quality and safety would be as intense as they are today, but we did a good job believing that these areas were important before they hit,” he says.
Looking forward, he says, other emerging forces will join quality and safety at the forefront of HM. “The next five years will likely bring similar pressures on efficiency and throughput,” he says. “I’m going to encourage folks to stay ahead of the curve.”
Having attended every annual conference since the beginning, Dr. Wachter looks forward to “polar things” about each meeting: catching up with the founders of the movement and seeing new faces.
“What’s more fun for me is the amount of youthful energy at the meetings,” he says, especially of the hospitalists he has mentored over the years. “When I come with my group from UCSF, it gives me tremendous pride.” TH
Brendon Shank is a freelance writer based in Philadelphia.
For hospitalist Robert Wachter, MD, MHM, the next annual SHM meeting will be particularly poignant, and not just because he’s HM11’s featured speaker.
Next year will mark the 15th anniversary of the New England Journal of Medicine article coauthored by Dr. Wachter that introduced the term “hospitalist” to the American healthcare lexicon. The specialty is growing and developing into adulthood nicely, he says, which will be part of his presentation in Grapevine, Texas.
“At age 15, that’s when you move to adolescence—you’re going to be off on adulthood and on your own,” says Dr. Wachter, professor, chief of the Division of Hospital Medicine, and chief of the Medical Service at the University of California at San Francisco Medical Center, former SHM president and author of the blog Wachter’s World (www.wachtersworld.com).
Like a proud father, Dr. Wachter expects that he will reminisce about the past, speculate about HM’s bright future, and encourage hospitalists to continue their work.
“This will be an optimistic talk,” he says. “The growth has been extraordinary.”
At the outset of the specialty, Dr. Wachter says, he and colleagues predicted some of the current trends, but they underestimated how powerful some would become.
“We couldn’t have predicted that the pressures to increase quality and safety would be as intense as they are today, but we did a good job believing that these areas were important before they hit,” he says.
Looking forward, he says, other emerging forces will join quality and safety at the forefront of HM. “The next five years will likely bring similar pressures on efficiency and throughput,” he says. “I’m going to encourage folks to stay ahead of the curve.”
Having attended every annual conference since the beginning, Dr. Wachter looks forward to “polar things” about each meeting: catching up with the founders of the movement and seeing new faces.
“What’s more fun for me is the amount of youthful energy at the meetings,” he says, especially of the hospitalists he has mentored over the years. “When I come with my group from UCSF, it gives me tremendous pride.” TH
Brendon Shank is a freelance writer based in Philadelphia.
Hospitalists Flock to Free HM App for iPhone, BlackBerry, and Other Handhelds
In less than a year, a smartphone application has attracted the attention of hospitalists across the country. Thousands of individuals have accessed the new “Hospitalist Connection” app since it launched in April.
Developed by Epocrates, one of the leaders in mobile applications in healthcare, “Hospitalist Connection” delivers fresh perspectives and unique content about leading research in hospital medicine. Topics include practice management, quality improvement, and care transitions.
Recent articles have covered the effect that financial incentives can have on HM operations and an editorial from Chad Whelan, MD, FHM, physician editor of “Hospitalist Connection,” about the effects of “presenteeism,” or physicians working when the know they are sick.
“When they are on the job, downtime for hospitalists is rare and valuable,” says Dr. Whelan, director of the Division of Hospital Medicine and associate professor of medicine at Loyola University’s Stritch School of Medicine in Chicago.
“‘Hospitalist Connection’ is an easy way to stay informed on best practices in the field—from anywhere at any time.”
To download and subscribe to “Hospitalist Connection,” visit www.hospitalmedicine.org/epocrates.
For SHM, delivering content to smartphones is a logical move.
“This advances the specialty, and we’re thrilled to make it as easy as possible for our members and others to subscribe,” says Todd Von Deak, MBA, CAE, vice president of operations and general manager of SHM. “This is another tangible way that SHM is helping hospitalists improve the quality, safety, and efficiency of care in the hospital.”
In less than a year, a smartphone application has attracted the attention of hospitalists across the country. Thousands of individuals have accessed the new “Hospitalist Connection” app since it launched in April.
Developed by Epocrates, one of the leaders in mobile applications in healthcare, “Hospitalist Connection” delivers fresh perspectives and unique content about leading research in hospital medicine. Topics include practice management, quality improvement, and care transitions.
Recent articles have covered the effect that financial incentives can have on HM operations and an editorial from Chad Whelan, MD, FHM, physician editor of “Hospitalist Connection,” about the effects of “presenteeism,” or physicians working when the know they are sick.
“When they are on the job, downtime for hospitalists is rare and valuable,” says Dr. Whelan, director of the Division of Hospital Medicine and associate professor of medicine at Loyola University’s Stritch School of Medicine in Chicago.
“‘Hospitalist Connection’ is an easy way to stay informed on best practices in the field—from anywhere at any time.”
To download and subscribe to “Hospitalist Connection,” visit www.hospitalmedicine.org/epocrates.
For SHM, delivering content to smartphones is a logical move.
“This advances the specialty, and we’re thrilled to make it as easy as possible for our members and others to subscribe,” says Todd Von Deak, MBA, CAE, vice president of operations and general manager of SHM. “This is another tangible way that SHM is helping hospitalists improve the quality, safety, and efficiency of care in the hospital.”
In less than a year, a smartphone application has attracted the attention of hospitalists across the country. Thousands of individuals have accessed the new “Hospitalist Connection” app since it launched in April.
Developed by Epocrates, one of the leaders in mobile applications in healthcare, “Hospitalist Connection” delivers fresh perspectives and unique content about leading research in hospital medicine. Topics include practice management, quality improvement, and care transitions.
Recent articles have covered the effect that financial incentives can have on HM operations and an editorial from Chad Whelan, MD, FHM, physician editor of “Hospitalist Connection,” about the effects of “presenteeism,” or physicians working when the know they are sick.
“When they are on the job, downtime for hospitalists is rare and valuable,” says Dr. Whelan, director of the Division of Hospital Medicine and associate professor of medicine at Loyola University’s Stritch School of Medicine in Chicago.
“‘Hospitalist Connection’ is an easy way to stay informed on best practices in the field—from anywhere at any time.”
To download and subscribe to “Hospitalist Connection,” visit www.hospitalmedicine.org/epocrates.
For SHM, delivering content to smartphones is a logical move.
“This advances the specialty, and we’re thrilled to make it as easy as possible for our members and others to subscribe,” says Todd Von Deak, MBA, CAE, vice president of operations and general manager of SHM. “This is another tangible way that SHM is helping hospitalists improve the quality, safety, and efficiency of care in the hospital.”
A New Look at Family Medicine Hospitalists
A new survey spearheaded by SHM’s Family Medicine Task Force gives the first glimpse into the demographics, settings, and scopes of practice of this growing HM segment.
The research found that hospitalists trained in family medicine are experienced physicians who likely work directly for their hospital. More than half (51%) completed residency training more than 10 years ago, although the largest single group of respondents (37%) finished residency six to 10 years ago.
Virtually all respondents (96%) work full-time and a third are hospital employees—the most prevalent staffing model found in the survey. In addition to clinical practice, half of family-medicine-trained hospitalists have teaching and other leadership responsibilities.
The survey is based on responses from 81 of the 263 SHM members registered as family medicine physicians.
“As the number of family-medicine-trained physicians grows within hospital medicine, it’s important for us to understand the people behind it,” said research coauthor Claudia Geyer, MD, FHM.
Family-medicine-trained hospitalists are a growing phenomenon in the specialty. Survey data from 2007 to 2008 revealed that 3.7% of U.S. hospitalists are trained in family medicine; however, SHM’s recent membership data show that more than 6% of SHM members are registered as family medicine physicians.
A new survey spearheaded by SHM’s Family Medicine Task Force gives the first glimpse into the demographics, settings, and scopes of practice of this growing HM segment.
The research found that hospitalists trained in family medicine are experienced physicians who likely work directly for their hospital. More than half (51%) completed residency training more than 10 years ago, although the largest single group of respondents (37%) finished residency six to 10 years ago.
Virtually all respondents (96%) work full-time and a third are hospital employees—the most prevalent staffing model found in the survey. In addition to clinical practice, half of family-medicine-trained hospitalists have teaching and other leadership responsibilities.
The survey is based on responses from 81 of the 263 SHM members registered as family medicine physicians.
“As the number of family-medicine-trained physicians grows within hospital medicine, it’s important for us to understand the people behind it,” said research coauthor Claudia Geyer, MD, FHM.
Family-medicine-trained hospitalists are a growing phenomenon in the specialty. Survey data from 2007 to 2008 revealed that 3.7% of U.S. hospitalists are trained in family medicine; however, SHM’s recent membership data show that more than 6% of SHM members are registered as family medicine physicians.
A new survey spearheaded by SHM’s Family Medicine Task Force gives the first glimpse into the demographics, settings, and scopes of practice of this growing HM segment.
The research found that hospitalists trained in family medicine are experienced physicians who likely work directly for their hospital. More than half (51%) completed residency training more than 10 years ago, although the largest single group of respondents (37%) finished residency six to 10 years ago.
Virtually all respondents (96%) work full-time and a third are hospital employees—the most prevalent staffing model found in the survey. In addition to clinical practice, half of family-medicine-trained hospitalists have teaching and other leadership responsibilities.
The survey is based on responses from 81 of the 263 SHM members registered as family medicine physicians.
“As the number of family-medicine-trained physicians grows within hospital medicine, it’s important for us to understand the people behind it,” said research coauthor Claudia Geyer, MD, FHM.
Family-medicine-trained hospitalists are a growing phenomenon in the specialty. Survey data from 2007 to 2008 revealed that 3.7% of U.S. hospitalists are trained in family medicine; however, SHM’s recent membership data show that more than 6% of SHM members are registered as family medicine physicians.
Fellows Program Application Deadline is Jan. 14
Next year’s annual meeting in Dallas marks the third induction of fellows into the SHM Fellows program. Candidates still have a few weeks to submit an application. The deadline for 2011 applications is Jan. 14.
More than 700 fellows and senior fellows have been inducted since the program began in 2009. “The success and enthusiasm for this program has been incredible,” says Todd Von Deak, SHM’s vice president of operations and general manager. “For individual hospitalists, it’s a simple way to demonstrate to patients and hospitals that you take your profession very seriously. For the specialty, it illustrates the growth and accomplishments of hospital medicine to the rest of the healthcare sector.”
In addition to additional rights and privileges from SHM, fellows can append their designation to their name and credentials.
The SHM Fellows program inducts three levels of fellows every year: Fellow in Hospital Medicine (FHM), Senior Fellow in Hospital Medicine (SFHM), and Master in Hospital Medicine (MHM).
To be nominated, both FHM and SFHM designations require five years as a practicing hospitalist and a demonstrated commitment to quality improvement, teamwork, and leadership. An FHM candidate must be an SHM member for at least three years; SFHM candidates must be members for at least five.
Introduced last year, the MHM designation is by invitation only and reserved for the specialty’s leaders and pioneers. The inaugural MHM designees were John Nelson (pictured left), MD, MHM, Robert Watcher (center), MD, MHM, and Winthrop Whitcomb (right), MD, MHM.
For more information or an application, visit www.hospitalmedicine.org/fellows.
FELLOW IN HOSPITAL MEDICINE SPOTLIGHT
Bradley M. Sherman, MD, FACP, FHM
Dr. Sherman, a hospitalist of 15 years, is both chairman and director of quality and performance improvement in the Department of Medicine at Glen Cove (N.Y.) Hospital, part of the North Shore University Health System. He is a clinical associate professor of medicine at New York University School of Medicine and an associate professor of medicine at Hofstra University School of Medicine.
A six-year SHM member, he helped establish the Long Island, N.Y., chapter and led as its president from 2004 to 2007. He served as moderator both for the transitions-in-care discussion and MRSA infections symposium at HM10 in Washington, D.C.
Undergraduate education: Duke University, Durham, N.C.
Graduate education: The Rockefeller University in New York City and New York Medical College in Valhalla, N.Y.
Internship and residency: Northwestern University, Chicago.
Fellowships: Gastroenterology fellowship at University of Pittsburgh from 1994 to 1995; fellowship in quality at Greater New York Hospital Association from 2009 to 2010.
Notable: This year, he completed a 15-month Six Sigma quality project on reducing variation care and standardization for patients admitted with heart failure, as well as a capstone project on reducing 30-day readmissions for patients discharged with heart failure.
Quotable: “Hospital medicine will continue to expand and become an integral part of hospital operations and practice. The comanagement services with surgical specialties will continue to evolve, and hospitalists will be taking a larger role in ensuring that care rendered across the continuum is met at the highest standard, both in and out of the hospital.”
FYI: Dr. Sherman enjoys spending time with his wife and two sons, ages 12 and 9. He is an avid tennis player and a regular at his local gym. —Sarah Gelotte
Next year’s annual meeting in Dallas marks the third induction of fellows into the SHM Fellows program. Candidates still have a few weeks to submit an application. The deadline for 2011 applications is Jan. 14.
More than 700 fellows and senior fellows have been inducted since the program began in 2009. “The success and enthusiasm for this program has been incredible,” says Todd Von Deak, SHM’s vice president of operations and general manager. “For individual hospitalists, it’s a simple way to demonstrate to patients and hospitals that you take your profession very seriously. For the specialty, it illustrates the growth and accomplishments of hospital medicine to the rest of the healthcare sector.”
In addition to additional rights and privileges from SHM, fellows can append their designation to their name and credentials.
The SHM Fellows program inducts three levels of fellows every year: Fellow in Hospital Medicine (FHM), Senior Fellow in Hospital Medicine (SFHM), and Master in Hospital Medicine (MHM).
To be nominated, both FHM and SFHM designations require five years as a practicing hospitalist and a demonstrated commitment to quality improvement, teamwork, and leadership. An FHM candidate must be an SHM member for at least three years; SFHM candidates must be members for at least five.
Introduced last year, the MHM designation is by invitation only and reserved for the specialty’s leaders and pioneers. The inaugural MHM designees were John Nelson (pictured left), MD, MHM, Robert Watcher (center), MD, MHM, and Winthrop Whitcomb (right), MD, MHM.
For more information or an application, visit www.hospitalmedicine.org/fellows.
FELLOW IN HOSPITAL MEDICINE SPOTLIGHT
Bradley M. Sherman, MD, FACP, FHM
Dr. Sherman, a hospitalist of 15 years, is both chairman and director of quality and performance improvement in the Department of Medicine at Glen Cove (N.Y.) Hospital, part of the North Shore University Health System. He is a clinical associate professor of medicine at New York University School of Medicine and an associate professor of medicine at Hofstra University School of Medicine.
A six-year SHM member, he helped establish the Long Island, N.Y., chapter and led as its president from 2004 to 2007. He served as moderator both for the transitions-in-care discussion and MRSA infections symposium at HM10 in Washington, D.C.
Undergraduate education: Duke University, Durham, N.C.
Graduate education: The Rockefeller University in New York City and New York Medical College in Valhalla, N.Y.
Internship and residency: Northwestern University, Chicago.
Fellowships: Gastroenterology fellowship at University of Pittsburgh from 1994 to 1995; fellowship in quality at Greater New York Hospital Association from 2009 to 2010.
Notable: This year, he completed a 15-month Six Sigma quality project on reducing variation care and standardization for patients admitted with heart failure, as well as a capstone project on reducing 30-day readmissions for patients discharged with heart failure.
Quotable: “Hospital medicine will continue to expand and become an integral part of hospital operations and practice. The comanagement services with surgical specialties will continue to evolve, and hospitalists will be taking a larger role in ensuring that care rendered across the continuum is met at the highest standard, both in and out of the hospital.”
FYI: Dr. Sherman enjoys spending time with his wife and two sons, ages 12 and 9. He is an avid tennis player and a regular at his local gym. —Sarah Gelotte
Next year’s annual meeting in Dallas marks the third induction of fellows into the SHM Fellows program. Candidates still have a few weeks to submit an application. The deadline for 2011 applications is Jan. 14.
More than 700 fellows and senior fellows have been inducted since the program began in 2009. “The success and enthusiasm for this program has been incredible,” says Todd Von Deak, SHM’s vice president of operations and general manager. “For individual hospitalists, it’s a simple way to demonstrate to patients and hospitals that you take your profession very seriously. For the specialty, it illustrates the growth and accomplishments of hospital medicine to the rest of the healthcare sector.”
In addition to additional rights and privileges from SHM, fellows can append their designation to their name and credentials.
The SHM Fellows program inducts three levels of fellows every year: Fellow in Hospital Medicine (FHM), Senior Fellow in Hospital Medicine (SFHM), and Master in Hospital Medicine (MHM).
To be nominated, both FHM and SFHM designations require five years as a practicing hospitalist and a demonstrated commitment to quality improvement, teamwork, and leadership. An FHM candidate must be an SHM member for at least three years; SFHM candidates must be members for at least five.
Introduced last year, the MHM designation is by invitation only and reserved for the specialty’s leaders and pioneers. The inaugural MHM designees were John Nelson (pictured left), MD, MHM, Robert Watcher (center), MD, MHM, and Winthrop Whitcomb (right), MD, MHM.
For more information or an application, visit www.hospitalmedicine.org/fellows.
FELLOW IN HOSPITAL MEDICINE SPOTLIGHT
Bradley M. Sherman, MD, FACP, FHM
Dr. Sherman, a hospitalist of 15 years, is both chairman and director of quality and performance improvement in the Department of Medicine at Glen Cove (N.Y.) Hospital, part of the North Shore University Health System. He is a clinical associate professor of medicine at New York University School of Medicine and an associate professor of medicine at Hofstra University School of Medicine.
A six-year SHM member, he helped establish the Long Island, N.Y., chapter and led as its president from 2004 to 2007. He served as moderator both for the transitions-in-care discussion and MRSA infections symposium at HM10 in Washington, D.C.
Undergraduate education: Duke University, Durham, N.C.
Graduate education: The Rockefeller University in New York City and New York Medical College in Valhalla, N.Y.
Internship and residency: Northwestern University, Chicago.
Fellowships: Gastroenterology fellowship at University of Pittsburgh from 1994 to 1995; fellowship in quality at Greater New York Hospital Association from 2009 to 2010.
Notable: This year, he completed a 15-month Six Sigma quality project on reducing variation care and standardization for patients admitted with heart failure, as well as a capstone project on reducing 30-day readmissions for patients discharged with heart failure.
Quotable: “Hospital medicine will continue to expand and become an integral part of hospital operations and practice. The comanagement services with surgical specialties will continue to evolve, and hospitalists will be taking a larger role in ensuring that care rendered across the continuum is met at the highest standard, both in and out of the hospital.”
FYI: Dr. Sherman enjoys spending time with his wife and two sons, ages 12 and 9. He is an avid tennis player and a regular at his local gym. —Sarah Gelotte
Career Challenge
Whether it’s directing a quality-improvement initiative on the hospital floor, training new recruits, or presenting metrics to hospital administrators, demonstrating leadership is a key competency for hospitalists. And, despite how it looks in the movies, most leaders are trained, not born.
That’s the foundation of SHM’s Leadership Academy program, a series of intense, four-day programs designed specifically to help hospitalists develop their leadership skills in a hands-on environment.
The demand for continued leadership training has been so high that SHM has developed a third leadership course for hospitalists who have completed either of the original tracks. CME credits are available for all three Leadership Academy course levels.
The new course, March 11-14 at the Aria Resort & Casino in Las Vegas, will follow the same four-day format as its predecessors. For updates and to register, visit the “Hospitalist Leadership Academies” page of the SHM website, www.hospitalmedicine.org/leadership.
“This is about building skills and growing momentum,” says Tina Budnitz, MPH, senior advisor for quality initiatives at SHM. “Participants walk away from Leadership Academy with newfound tools and the motivation to use them to lead important projects in their hospital.”
For Budnitz, the new academy course is a natural extension of the existing program. “Developing leadership skills is an ongoing process, so it makes sense to provide new material and new insights to hospitalists,” she says.
A Better Way to Communicate
The new course will bring in leadership experts and will help established leaders manage their hospitalist teams, says Leadership Committee chair Patience Agborbesong, MD, SFHM, who plans on attending the Las Vegas academy.
“It came into being because people were asking about other topics,” says Dr. Agborbesong, lead hospitalist at Wake Forest Inpatient Physicians in Winston-Salem, N.C. “We were getting the same questions from attendees asking for more. Hospitalists were saying, ‘Now what? I feel like I still need to develop these skills.’ ”
One of the key sessions in the new course focuses on advanced communications—a critical skill for hospitalists with long-term career aspirations. In the session, scientist-turned-filmmaker and author Randy Olson will offer his unique perspective on how clinicians and scientists can improve their communications with team members, hospital administrators, patients, and the public. After laying the groundwork for better communications, Olson will lead the hospitalists through a highly interactive set of exercises that culminate in participants presenting back to the group.
Published in 2009, Olson’s book Don’t Be Such a Scientist invites scientists to become better communicators and storytellers as a means to getting their points across and influencing audiences.
A full day of the course is devoted to leading and managing teams, including how to build a successful hospitalist program by selecting and investing in the right people. Another portion of the day teaches hospitalists skills they can use to build trust within their teams.
The final day focuses on an often-neglected element of leadership: self-investment. An executive coach will work with hospitalists to understand the importance of investing in their own careers, and help them develop tools to make self-investment easier.
The Originals
Years ago, as it became clear that hospitalists would be on the vanguard of changing healthcare in the hospital, it became equally clear that clinical and diagnostic skills alone would not be sufficient to tackle challenges that were as much about the people involved as they were about the technical requirements of healthcare.
The foundational SHM Leadership Academy course was developed to address the interpersonal dynamics of leadership in the hospital. Since its inception, the principles of hospitalist leadership apply equally to physicians and nonphysicians, including hospital administrators, physician assistants, and other hospital-based caregivers.
The allure for many hospitalists, including Dr. Agborbesong, is its particular relevance to the hospital setting.
“I had been to other leadership trainings, but this one was geared right to me. Everything was focused on the practice of HM and was oriented toward a leader at my level, when I was still new in my leadership position,” she says. “Other courses assumed that I was midway through my career or further.”
The real-world basis of the academy is apparent in the teaching model as well as its subject. Because many of the participants are already active and engaged leaders, the academy’s courses are structured to be interactive, hands-on learning experiences. Participants in the first Leadership Academy program walk away with, among other skill sets, the ability to:
- Evaluate personal leadership strengths and weaknesses and apply them to everyday leadership and management challenges;
- Predict and plan for the near-term challenges affecting the viability of their hospitalist programs;
- Improve patient outcomes through successful planning, allocation of resources, collaboration, teamwork, and execution;
- Understand key hospital drivers and examine how hospital performance metrics are derived, as well as how HM practices can influence and impact these metrics; and
- Implement methods of effective change through leadership, shared vision, and managing the organizational culture.
Participants in the second SHM Leadership Academy course build on those skills and learn to:
- Drive culture change through specific leadership behaviors and actions;
- Use financial reports to drive decision-making in clinical and operational practices;
- Recruit and retain the best physicians for their group;
- Build exceptional physician satisfaction; and
- Engage in effective, professional negotiation activities using proven techniques. TH
Brendon Shank is a freelance writer based in Philadelphia.
HM11 Right Around the Corner
Hospital Medicine 2011, or HM11, the premier event for healthcare professionals who specialize in hospital medicine, is just months away, and includes the specialty’s best opportunities for education, networking, and career advancement.
HM11 will present the future of HM in an authentic Lone Star State setting—the Gaylord Texan Hotel and Convention Center in Grapevine, Texas, May 10-13. The official kickoff to HM11 will be Wednesday morning; educational pre-courses will be offered Tuesday.
In addition to dozens of sessions from the best in the specialty on issues like clinical practice, practice management, new academic research, and quality initiatives, SHM again will present pre-courses specifically designed for in-depth education.
New pre-courses in 2011 include:
- Advanced Interactive Critical Care;
- Portable Ultrasound for the Hospitalist;
- Perioperative Medicine for the Hospitalist; and
- Succeeding in Challenging Times: Advances in Hospital Practice Management.
The continued growth of SHM’s annual conference also means new opportunities for exhibitors and sponsors to reach thousands of the most influential individuals in modern healthcare. Materials for both exhibitors and sponsors are available at the HM11 website.
Discounted early registration is available through April 3. For details and updates, visit www.hospitalmedicine2011.org.
Whether it’s directing a quality-improvement initiative on the hospital floor, training new recruits, or presenting metrics to hospital administrators, demonstrating leadership is a key competency for hospitalists. And, despite how it looks in the movies, most leaders are trained, not born.
That’s the foundation of SHM’s Leadership Academy program, a series of intense, four-day programs designed specifically to help hospitalists develop their leadership skills in a hands-on environment.
The demand for continued leadership training has been so high that SHM has developed a third leadership course for hospitalists who have completed either of the original tracks. CME credits are available for all three Leadership Academy course levels.
The new course, March 11-14 at the Aria Resort & Casino in Las Vegas, will follow the same four-day format as its predecessors. For updates and to register, visit the “Hospitalist Leadership Academies” page of the SHM website, www.hospitalmedicine.org/leadership.
“This is about building skills and growing momentum,” says Tina Budnitz, MPH, senior advisor for quality initiatives at SHM. “Participants walk away from Leadership Academy with newfound tools and the motivation to use them to lead important projects in their hospital.”
For Budnitz, the new academy course is a natural extension of the existing program. “Developing leadership skills is an ongoing process, so it makes sense to provide new material and new insights to hospitalists,” she says.
A Better Way to Communicate
The new course will bring in leadership experts and will help established leaders manage their hospitalist teams, says Leadership Committee chair Patience Agborbesong, MD, SFHM, who plans on attending the Las Vegas academy.
“It came into being because people were asking about other topics,” says Dr. Agborbesong, lead hospitalist at Wake Forest Inpatient Physicians in Winston-Salem, N.C. “We were getting the same questions from attendees asking for more. Hospitalists were saying, ‘Now what? I feel like I still need to develop these skills.’ ”
One of the key sessions in the new course focuses on advanced communications—a critical skill for hospitalists with long-term career aspirations. In the session, scientist-turned-filmmaker and author Randy Olson will offer his unique perspective on how clinicians and scientists can improve their communications with team members, hospital administrators, patients, and the public. After laying the groundwork for better communications, Olson will lead the hospitalists through a highly interactive set of exercises that culminate in participants presenting back to the group.
Published in 2009, Olson’s book Don’t Be Such a Scientist invites scientists to become better communicators and storytellers as a means to getting their points across and influencing audiences.
A full day of the course is devoted to leading and managing teams, including how to build a successful hospitalist program by selecting and investing in the right people. Another portion of the day teaches hospitalists skills they can use to build trust within their teams.
The final day focuses on an often-neglected element of leadership: self-investment. An executive coach will work with hospitalists to understand the importance of investing in their own careers, and help them develop tools to make self-investment easier.
The Originals
Years ago, as it became clear that hospitalists would be on the vanguard of changing healthcare in the hospital, it became equally clear that clinical and diagnostic skills alone would not be sufficient to tackle challenges that were as much about the people involved as they were about the technical requirements of healthcare.
The foundational SHM Leadership Academy course was developed to address the interpersonal dynamics of leadership in the hospital. Since its inception, the principles of hospitalist leadership apply equally to physicians and nonphysicians, including hospital administrators, physician assistants, and other hospital-based caregivers.
The allure for many hospitalists, including Dr. Agborbesong, is its particular relevance to the hospital setting.
“I had been to other leadership trainings, but this one was geared right to me. Everything was focused on the practice of HM and was oriented toward a leader at my level, when I was still new in my leadership position,” she says. “Other courses assumed that I was midway through my career or further.”
The real-world basis of the academy is apparent in the teaching model as well as its subject. Because many of the participants are already active and engaged leaders, the academy’s courses are structured to be interactive, hands-on learning experiences. Participants in the first Leadership Academy program walk away with, among other skill sets, the ability to:
- Evaluate personal leadership strengths and weaknesses and apply them to everyday leadership and management challenges;
- Predict and plan for the near-term challenges affecting the viability of their hospitalist programs;
- Improve patient outcomes through successful planning, allocation of resources, collaboration, teamwork, and execution;
- Understand key hospital drivers and examine how hospital performance metrics are derived, as well as how HM practices can influence and impact these metrics; and
- Implement methods of effective change through leadership, shared vision, and managing the organizational culture.
Participants in the second SHM Leadership Academy course build on those skills and learn to:
- Drive culture change through specific leadership behaviors and actions;
- Use financial reports to drive decision-making in clinical and operational practices;
- Recruit and retain the best physicians for their group;
- Build exceptional physician satisfaction; and
- Engage in effective, professional negotiation activities using proven techniques. TH
Brendon Shank is a freelance writer based in Philadelphia.
HM11 Right Around the Corner
Hospital Medicine 2011, or HM11, the premier event for healthcare professionals who specialize in hospital medicine, is just months away, and includes the specialty’s best opportunities for education, networking, and career advancement.
HM11 will present the future of HM in an authentic Lone Star State setting—the Gaylord Texan Hotel and Convention Center in Grapevine, Texas, May 10-13. The official kickoff to HM11 will be Wednesday morning; educational pre-courses will be offered Tuesday.
In addition to dozens of sessions from the best in the specialty on issues like clinical practice, practice management, new academic research, and quality initiatives, SHM again will present pre-courses specifically designed for in-depth education.
New pre-courses in 2011 include:
- Advanced Interactive Critical Care;
- Portable Ultrasound for the Hospitalist;
- Perioperative Medicine for the Hospitalist; and
- Succeeding in Challenging Times: Advances in Hospital Practice Management.
The continued growth of SHM’s annual conference also means new opportunities for exhibitors and sponsors to reach thousands of the most influential individuals in modern healthcare. Materials for both exhibitors and sponsors are available at the HM11 website.
Discounted early registration is available through April 3. For details and updates, visit www.hospitalmedicine2011.org.
Whether it’s directing a quality-improvement initiative on the hospital floor, training new recruits, or presenting metrics to hospital administrators, demonstrating leadership is a key competency for hospitalists. And, despite how it looks in the movies, most leaders are trained, not born.
That’s the foundation of SHM’s Leadership Academy program, a series of intense, four-day programs designed specifically to help hospitalists develop their leadership skills in a hands-on environment.
The demand for continued leadership training has been so high that SHM has developed a third leadership course for hospitalists who have completed either of the original tracks. CME credits are available for all three Leadership Academy course levels.
The new course, March 11-14 at the Aria Resort & Casino in Las Vegas, will follow the same four-day format as its predecessors. For updates and to register, visit the “Hospitalist Leadership Academies” page of the SHM website, www.hospitalmedicine.org/leadership.
“This is about building skills and growing momentum,” says Tina Budnitz, MPH, senior advisor for quality initiatives at SHM. “Participants walk away from Leadership Academy with newfound tools and the motivation to use them to lead important projects in their hospital.”
For Budnitz, the new academy course is a natural extension of the existing program. “Developing leadership skills is an ongoing process, so it makes sense to provide new material and new insights to hospitalists,” she says.
A Better Way to Communicate
The new course will bring in leadership experts and will help established leaders manage their hospitalist teams, says Leadership Committee chair Patience Agborbesong, MD, SFHM, who plans on attending the Las Vegas academy.
“It came into being because people were asking about other topics,” says Dr. Agborbesong, lead hospitalist at Wake Forest Inpatient Physicians in Winston-Salem, N.C. “We were getting the same questions from attendees asking for more. Hospitalists were saying, ‘Now what? I feel like I still need to develop these skills.’ ”
One of the key sessions in the new course focuses on advanced communications—a critical skill for hospitalists with long-term career aspirations. In the session, scientist-turned-filmmaker and author Randy Olson will offer his unique perspective on how clinicians and scientists can improve their communications with team members, hospital administrators, patients, and the public. After laying the groundwork for better communications, Olson will lead the hospitalists through a highly interactive set of exercises that culminate in participants presenting back to the group.
Published in 2009, Olson’s book Don’t Be Such a Scientist invites scientists to become better communicators and storytellers as a means to getting their points across and influencing audiences.
A full day of the course is devoted to leading and managing teams, including how to build a successful hospitalist program by selecting and investing in the right people. Another portion of the day teaches hospitalists skills they can use to build trust within their teams.
The final day focuses on an often-neglected element of leadership: self-investment. An executive coach will work with hospitalists to understand the importance of investing in their own careers, and help them develop tools to make self-investment easier.
The Originals
Years ago, as it became clear that hospitalists would be on the vanguard of changing healthcare in the hospital, it became equally clear that clinical and diagnostic skills alone would not be sufficient to tackle challenges that were as much about the people involved as they were about the technical requirements of healthcare.
The foundational SHM Leadership Academy course was developed to address the interpersonal dynamics of leadership in the hospital. Since its inception, the principles of hospitalist leadership apply equally to physicians and nonphysicians, including hospital administrators, physician assistants, and other hospital-based caregivers.
The allure for many hospitalists, including Dr. Agborbesong, is its particular relevance to the hospital setting.
“I had been to other leadership trainings, but this one was geared right to me. Everything was focused on the practice of HM and was oriented toward a leader at my level, when I was still new in my leadership position,” she says. “Other courses assumed that I was midway through my career or further.”
The real-world basis of the academy is apparent in the teaching model as well as its subject. Because many of the participants are already active and engaged leaders, the academy’s courses are structured to be interactive, hands-on learning experiences. Participants in the first Leadership Academy program walk away with, among other skill sets, the ability to:
- Evaluate personal leadership strengths and weaknesses and apply them to everyday leadership and management challenges;
- Predict and plan for the near-term challenges affecting the viability of their hospitalist programs;
- Improve patient outcomes through successful planning, allocation of resources, collaboration, teamwork, and execution;
- Understand key hospital drivers and examine how hospital performance metrics are derived, as well as how HM practices can influence and impact these metrics; and
- Implement methods of effective change through leadership, shared vision, and managing the organizational culture.
Participants in the second SHM Leadership Academy course build on those skills and learn to:
- Drive culture change through specific leadership behaviors and actions;
- Use financial reports to drive decision-making in clinical and operational practices;
- Recruit and retain the best physicians for their group;
- Build exceptional physician satisfaction; and
- Engage in effective, professional negotiation activities using proven techniques. TH
Brendon Shank is a freelance writer based in Philadelphia.
HM11 Right Around the Corner
Hospital Medicine 2011, or HM11, the premier event for healthcare professionals who specialize in hospital medicine, is just months away, and includes the specialty’s best opportunities for education, networking, and career advancement.
HM11 will present the future of HM in an authentic Lone Star State setting—the Gaylord Texan Hotel and Convention Center in Grapevine, Texas, May 10-13. The official kickoff to HM11 will be Wednesday morning; educational pre-courses will be offered Tuesday.
In addition to dozens of sessions from the best in the specialty on issues like clinical practice, practice management, new academic research, and quality initiatives, SHM again will present pre-courses specifically designed for in-depth education.
New pre-courses in 2011 include:
- Advanced Interactive Critical Care;
- Portable Ultrasound for the Hospitalist;
- Perioperative Medicine for the Hospitalist; and
- Succeeding in Challenging Times: Advances in Hospital Practice Management.
The continued growth of SHM’s annual conference also means new opportunities for exhibitors and sponsors to reach thousands of the most influential individuals in modern healthcare. Materials for both exhibitors and sponsors are available at the HM11 website.
Discounted early registration is available through April 3. For details and updates, visit www.hospitalmedicine2011.org.
Can You Hear Me Now?
In the past three years, SHM has brought in-depth quality-improvement (QI) programs to nearly every state in the country.
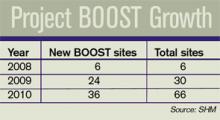
Between its three major mentored implementation projects—Project BOOST (Better Outcomes for Older Adults through Safe Transitions), Glycemic Control Mentored Implemen-tation, and the Venous Thromboembolism (VTE) Collaborative—SHM has worked with more than 100 hospitals across the country and in Canada. SHM is expanding these three programs to additional hospitals and actively developing other QI initiatives.
“SHM’s quality-improvement programs focus on real change, and they have made a substantial impact,” says Joe Miller, SHM’s senior vice president and chief solutions officer. “Hospitalists using SHM’s quality-improvement methods have impacted the care of tens of thousands of hospitalized patients.”
SHM’s programs all use a mix of in-depth mentoring led by national experts and specially designed resource toolkits that enable hospitalists to lead major initiatives within their hospitals. The programs also facilitate “peer learning,” allowing hospitalists to learn from one another.
Project BOOST, which is designed to reduce unplanned readmissions to the hospital, has received national attention. In early 2010, SHM teamed with Blue Cross/Blue Shield of Michigan and the University of Michigan to bring the program to more than a dozen hospitals in that state. SHM also announced a new collaboration with the California HealthCare Foundation to implement Project BOOST in more than 20 hospitals in California.
“Healthcare reform is creating a new focus on quality improvement,” Miller says. “SHM is bringing a multidisciplinary approach to transforming inpatient care to hospitals across the country.” TH
Chapter Updates
Milwaukee/SE Wisconsin
The Milwaukee/SE Wisconsin chapter held a meeting June 10 at Bacchus Restaurant in Milwaukee, at which congratulations were doled out to chapter member Eric Siegal, MD, SFHM, on his election to SHM’s board of directors. As chair of SHM’s Public Policy Committee, Dr. Siegal advocates for such issues as the Physician Quality Reporting Initiative (PQRI).
The chapter also acknowledged Dr. Len Scarpinato of St. Luke’s Hospital, who achieved Senior Fellow in Hospital Medicine (SFHM) designation and was honored at HM10 in April in Washington, D.C. As the regional director of Cogent Healthcare in southeast Wisconsin, Dr. Scarpinato has been instrumental in bringing hospitalists together to network and exchange innovative ideas.
Chapter member Jeanette Kalupa, DNP, ACNP-BC, APNP, of St. Luke’s was mentioned in the opening presentation at HM10 for her work as co-chair of the Nonphysician Providers Committee. Despite a busy HM10 schedule, Drs. Don Lee, Wes Lafferty, Scarpinato, Betty Tucker, and Peter Quandt took time out for a White House tour.
Greater Baltimore Area
The Greater Baltimore Area chapter of SHM met June 16 at Linwood’s Restaurant in Owings Mills, Md. Dr. Suzanne Mitchell spoke on “Relating to the Patient.” The meeting, sponsored by Merck, attracted 50 hospitalists and guests from 10 HM groups.
Los Angeles
The latest Los Angeles chapter meeting was held July 29. The featured speaker was Darrell Harrington, MD, associate medical director for Graduate Medical Education and chief of the division of general internal medicine at Harbor-UCLA Medical Center. Dr. Harrington delivered a presentation about maximizing DVT and PE quality measures. The chapter’s next meeting will be held in the fall.
SHAPE the Landscape of Academic Hospital Medicine: Participate in the Academic Hospitalist Survey
The recently released State of Hospital Medicine: 2010 Report Based on 2009 Data provides an unprecedented look at the factors shaping the specialty. However, for academic hospitalists, the picture can be very different. That is why SHM and the Medical Group Management Association (MGMA) are embarking on their first joint survey of academic hospitalists.
Academic HM groups—including groups at community-based teaching hospitals—can participate in the survey now through Nov. 5 by logging on to www6.mgma.com, or by contacting MGMA’s Survey Operations Department at 877-275-6462, Ext. 1895.
“Academic hospitalists and executive leaders at academic institutions need to know how they stack up against their peers in the field,” says Leslie Flores, SHM’s senior advisor for practice management. “Participating in this survey is the first step in providing an in-depth resource that identifies the major trends in academic hospital medicine.”
Like the new State of Hospital Medicine report, the academic report will provide data on hospitalist compensation and productivity, staffing information, and financial support. It also will examine the organizational structure of academic hospitalist practices and how academic hospitalists allocate their time between clinical, research, and teaching responsibilities. The new report also will feature information about medical-school and research funding.
MGMA will publish its standard academic survey results early next spring. Hospitalist-specific data will also be published in the 2011 State of Hospital Medicine report, to be released next summer.
In the past three years, SHM has brought in-depth quality-improvement (QI) programs to nearly every state in the country.
Between its three major mentored implementation projects—Project BOOST (Better Outcomes for Older Adults through Safe Transitions), Glycemic Control Mentored Implemen-tation, and the Venous Thromboembolism (VTE) Collaborative—SHM has worked with more than 100 hospitals across the country and in Canada. SHM is expanding these three programs to additional hospitals and actively developing other QI initiatives.
“SHM’s quality-improvement programs focus on real change, and they have made a substantial impact,” says Joe Miller, SHM’s senior vice president and chief solutions officer. “Hospitalists using SHM’s quality-improvement methods have impacted the care of tens of thousands of hospitalized patients.”
SHM’s programs all use a mix of in-depth mentoring led by national experts and specially designed resource toolkits that enable hospitalists to lead major initiatives within their hospitals. The programs also facilitate “peer learning,” allowing hospitalists to learn from one another.
Project BOOST, which is designed to reduce unplanned readmissions to the hospital, has received national attention. In early 2010, SHM teamed with Blue Cross/Blue Shield of Michigan and the University of Michigan to bring the program to more than a dozen hospitals in that state. SHM also announced a new collaboration with the California HealthCare Foundation to implement Project BOOST in more than 20 hospitals in California.
“Healthcare reform is creating a new focus on quality improvement,” Miller says. “SHM is bringing a multidisciplinary approach to transforming inpatient care to hospitals across the country.” TH
Chapter Updates
Milwaukee/SE Wisconsin
The Milwaukee/SE Wisconsin chapter held a meeting June 10 at Bacchus Restaurant in Milwaukee, at which congratulations were doled out to chapter member Eric Siegal, MD, SFHM, on his election to SHM’s board of directors. As chair of SHM’s Public Policy Committee, Dr. Siegal advocates for such issues as the Physician Quality Reporting Initiative (PQRI).
The chapter also acknowledged Dr. Len Scarpinato of St. Luke’s Hospital, who achieved Senior Fellow in Hospital Medicine (SFHM) designation and was honored at HM10 in April in Washington, D.C. As the regional director of Cogent Healthcare in southeast Wisconsin, Dr. Scarpinato has been instrumental in bringing hospitalists together to network and exchange innovative ideas.
Chapter member Jeanette Kalupa, DNP, ACNP-BC, APNP, of St. Luke’s was mentioned in the opening presentation at HM10 for her work as co-chair of the Nonphysician Providers Committee. Despite a busy HM10 schedule, Drs. Don Lee, Wes Lafferty, Scarpinato, Betty Tucker, and Peter Quandt took time out for a White House tour.
Greater Baltimore Area
The Greater Baltimore Area chapter of SHM met June 16 at Linwood’s Restaurant in Owings Mills, Md. Dr. Suzanne Mitchell spoke on “Relating to the Patient.” The meeting, sponsored by Merck, attracted 50 hospitalists and guests from 10 HM groups.
Los Angeles
The latest Los Angeles chapter meeting was held July 29. The featured speaker was Darrell Harrington, MD, associate medical director for Graduate Medical Education and chief of the division of general internal medicine at Harbor-UCLA Medical Center. Dr. Harrington delivered a presentation about maximizing DVT and PE quality measures. The chapter’s next meeting will be held in the fall.
SHAPE the Landscape of Academic Hospital Medicine: Participate in the Academic Hospitalist Survey
The recently released State of Hospital Medicine: 2010 Report Based on 2009 Data provides an unprecedented look at the factors shaping the specialty. However, for academic hospitalists, the picture can be very different. That is why SHM and the Medical Group Management Association (MGMA) are embarking on their first joint survey of academic hospitalists.
Academic HM groups—including groups at community-based teaching hospitals—can participate in the survey now through Nov. 5 by logging on to www6.mgma.com, or by contacting MGMA’s Survey Operations Department at 877-275-6462, Ext. 1895.
“Academic hospitalists and executive leaders at academic institutions need to know how they stack up against their peers in the field,” says Leslie Flores, SHM’s senior advisor for practice management. “Participating in this survey is the first step in providing an in-depth resource that identifies the major trends in academic hospital medicine.”
Like the new State of Hospital Medicine report, the academic report will provide data on hospitalist compensation and productivity, staffing information, and financial support. It also will examine the organizational structure of academic hospitalist practices and how academic hospitalists allocate their time between clinical, research, and teaching responsibilities. The new report also will feature information about medical-school and research funding.
MGMA will publish its standard academic survey results early next spring. Hospitalist-specific data will also be published in the 2011 State of Hospital Medicine report, to be released next summer.
In the past three years, SHM has brought in-depth quality-improvement (QI) programs to nearly every state in the country.
Between its three major mentored implementation projects—Project BOOST (Better Outcomes for Older Adults through Safe Transitions), Glycemic Control Mentored Implemen-tation, and the Venous Thromboembolism (VTE) Collaborative—SHM has worked with more than 100 hospitals across the country and in Canada. SHM is expanding these three programs to additional hospitals and actively developing other QI initiatives.
“SHM’s quality-improvement programs focus on real change, and they have made a substantial impact,” says Joe Miller, SHM’s senior vice president and chief solutions officer. “Hospitalists using SHM’s quality-improvement methods have impacted the care of tens of thousands of hospitalized patients.”
SHM’s programs all use a mix of in-depth mentoring led by national experts and specially designed resource toolkits that enable hospitalists to lead major initiatives within their hospitals. The programs also facilitate “peer learning,” allowing hospitalists to learn from one another.
Project BOOST, which is designed to reduce unplanned readmissions to the hospital, has received national attention. In early 2010, SHM teamed with Blue Cross/Blue Shield of Michigan and the University of Michigan to bring the program to more than a dozen hospitals in that state. SHM also announced a new collaboration with the California HealthCare Foundation to implement Project BOOST in more than 20 hospitals in California.
“Healthcare reform is creating a new focus on quality improvement,” Miller says. “SHM is bringing a multidisciplinary approach to transforming inpatient care to hospitals across the country.” TH
Chapter Updates
Milwaukee/SE Wisconsin
The Milwaukee/SE Wisconsin chapter held a meeting June 10 at Bacchus Restaurant in Milwaukee, at which congratulations were doled out to chapter member Eric Siegal, MD, SFHM, on his election to SHM’s board of directors. As chair of SHM’s Public Policy Committee, Dr. Siegal advocates for such issues as the Physician Quality Reporting Initiative (PQRI).
The chapter also acknowledged Dr. Len Scarpinato of St. Luke’s Hospital, who achieved Senior Fellow in Hospital Medicine (SFHM) designation and was honored at HM10 in April in Washington, D.C. As the regional director of Cogent Healthcare in southeast Wisconsin, Dr. Scarpinato has been instrumental in bringing hospitalists together to network and exchange innovative ideas.
Chapter member Jeanette Kalupa, DNP, ACNP-BC, APNP, of St. Luke’s was mentioned in the opening presentation at HM10 for her work as co-chair of the Nonphysician Providers Committee. Despite a busy HM10 schedule, Drs. Don Lee, Wes Lafferty, Scarpinato, Betty Tucker, and Peter Quandt took time out for a White House tour.
Greater Baltimore Area
The Greater Baltimore Area chapter of SHM met June 16 at Linwood’s Restaurant in Owings Mills, Md. Dr. Suzanne Mitchell spoke on “Relating to the Patient.” The meeting, sponsored by Merck, attracted 50 hospitalists and guests from 10 HM groups.
Los Angeles
The latest Los Angeles chapter meeting was held July 29. The featured speaker was Darrell Harrington, MD, associate medical director for Graduate Medical Education and chief of the division of general internal medicine at Harbor-UCLA Medical Center. Dr. Harrington delivered a presentation about maximizing DVT and PE quality measures. The chapter’s next meeting will be held in the fall.
SHAPE the Landscape of Academic Hospital Medicine: Participate in the Academic Hospitalist Survey
The recently released State of Hospital Medicine: 2010 Report Based on 2009 Data provides an unprecedented look at the factors shaping the specialty. However, for academic hospitalists, the picture can be very different. That is why SHM and the Medical Group Management Association (MGMA) are embarking on their first joint survey of academic hospitalists.
Academic HM groups—including groups at community-based teaching hospitals—can participate in the survey now through Nov. 5 by logging on to www6.mgma.com, or by contacting MGMA’s Survey Operations Department at 877-275-6462, Ext. 1895.
“Academic hospitalists and executive leaders at academic institutions need to know how they stack up against their peers in the field,” says Leslie Flores, SHM’s senior advisor for practice management. “Participating in this survey is the first step in providing an in-depth resource that identifies the major trends in academic hospital medicine.”
Like the new State of Hospital Medicine report, the academic report will provide data on hospitalist compensation and productivity, staffing information, and financial support. It also will examine the organizational structure of academic hospitalist practices and how academic hospitalists allocate their time between clinical, research, and teaching responsibilities. The new report also will feature information about medical-school and research funding.
MGMA will publish its standard academic survey results early next spring. Hospitalist-specific data will also be published in the 2011 State of Hospital Medicine report, to be released next summer.
SHM+MGMA = Better Survey
As HM continues to grow, the need for clear and accurate data about the specialty will only become more intense. Hospitalists and HM group leaders use survey information to better understand how they compare to other practices across the country, in terms of size and practice characteristics, as well as compensation and productivity.
Increasingly, healthcare executives are turning to survey data—either independently or via their hospitalist group leaders—to get a grasp on the best practices in the industry.
That’s why SHM teamed up with the Medical Group Management Association (MGMA), the industry leader for professional administrators and leaders of medical group practices, to research and develop the State of Hospital Medicine: 2010 Report Based on 2009 Data.
Previously, SHM created and fielded a biannual survey, then analyzed the results independently.

—Leslie A. Flores, MHA, SHM senior advisor for practice management
“Our partnership with MGMA expands our survey population, delivers more information, and brings MGMA’s 90 years of industry credibility in the medical practice management field,” says Leslie A. Flores, MHA, SHM senior advisor for practice management. “The 2010 survey gives hospitalists and hospital administrators an unprecedented snapshot of the state of hospital medicine.”
The 2010 report will be available this month in the “Practice Resources” section of the SHM website (www.hospitalmedicine.org).
The print version will be available to SHM members for $125; for $175, members receive both the print version and the report on CD-ROM.
“This is a first-ever opportunity for hospitalists, group leaders, and healthcare executives to get the clearest picture possible of a rapidly changing industry,” Flores says. TH
Brendon Shank is a freelance writer based in Philadelphia.
SHM Adopts Strict Code for Industry Relations
A long with nearly 20 other organizations, SHM has adopted the Code for Industry Relations (http://cmss.org/) established by the Council on Medical Specialty Societies (CMSS). In an era of digital communication, SHM has created a Web area (www.hospital medicine.org/industry) to continuously update its policies toward industry, display its current partnerships, and disclose the potential conflicts of interest of its board or directors, editors, and CEO.
The message from SHM leadership: SHM is committed to being a leader in an era of transparency and disclosure.
Transparency serves an important role for medical specialty societies, says Norman B. Kahn Jr., MD, executive vice president and CEO of CMSS. The code developed by CMSS and adopted by SHM “assures in interactions with industry that the patients’ needs come first,” Dr. Kahn says. “The bottom line is that this is all about protecting the independence of societies from industry without abrogating the relationship.”
From its early days, SHM has been aware of the need to balance the responsibilities of speaking for HM and the need to disclose any potential conflicts of interests. In 2000, SHM developed its Principles of Organizational Relationships (www.hospitalmedicine.org/OrgRelationships), which have guided the society’s efforts.
The principles call for a clear, bright line that is a barrier between the support of a partner and SHM’s control of content. Among other activities, SHM has applied those principles to meetings and educational initiatives, quality-improvement (QI) projects, and publications.
The principles also were the foundation for the tough conflict-of-interest policies (www.hospital medicine.org/interestpolicies) the board approved in 2005.
Over the last decade, as HM has grown, national hospitalist leaders have become the experts on a wide range of topics and are asked to speak, write, or advise government agencies, foundations, and industry.
As SHM has developed its resources to help hospitalists improve glycemic control, reduce unnecessary DVTs and PEs, and improve the transitions of care, SHM has engaged in partnerships with government agencies, foundations, and industry as well.
“SHM’s leadership recognizes that it has a fiduciary responsibility to its members—a responsibility to provide expert direction, and necessary resources, to enable the hospitalist to ensure the best possible care of his or her patients, and to advance the quality of the hospital system,” says SHM President Jeff Wiese, MD, SFHM. “But SHM cannot do this alone, and when external partnerships are established, it is the organization’s responsibility to enter into these partnerships judiciously, and to be fully transparent to the membership with respect to the arrangements of these partnerships.
“We are confident that no other organization has a more robust disclosure policy than SHM.”
Today’s Nominations, Tomorrow’s Leaders
HM leaders aren’t born that way—they’re nominated.
SHM is accepting nominations for its board election; new members will take office in May at HM11 in Dallas.
The nomination deadline is Oct. 31. Online ballots will be available to all SHM members in late 2010. The results of the election will be announced online in early 2011.
Nominees must be SHM members in good standing. SHM members may nominate themselves or be nominated by another SHM member. Nominations must include a letter of nomination, a one-page CV, and a recent photo.
The nomination committee considers candidates based on length of SHM membership, activity as a hospitalist and SHM member, the prominence of the candidate within the specialty, and a number of other factors.
Board members serve a three-year term and normally serve on one or more committees.
“Participating in SHM’s leadership is one of the best ways to help guide the future of hospital medicine,” says Larry Wellikson, MD, SFHM, CEO of SHM. “That begins by submitting a board nomination to SHM this year.”
Chapter Updates
Chicago
The Chicago chapter met May 19 at Sullivan’s Steakhouse. Twenty-five hospitalists from the Chicago area, including hospitalists at Loyola Hospital, Lutheran General Hospital, Illinois Masonic Medical Center, Trinity Hospital, Silver Cross, and Evanston Hospital, as well as hospitalist groups like Cogent and Vista, attended the meeting.
Dr. Robin Ross of Season Hospice and Palliative Care, which sponsored the event, presented clinical pearls for end-of-life care for the busy hospitalist. The meeting also featured a town-hall discussion, with topics relevant to everyday hospitalist practice—coding, consultations, and the use of observation units. Notification of chapter elections were summated to all chapter members in July and August.
Harrisburg/South Central Pennsylvania
Thirty hospitalists representing six HM programs attended the Harrisburg/South Central Pennsylvania chapter of SHM June 9 at Passage to India in Harrisburg.
Eric Kupersmith, MD, SFHM, division head of the hospitalist program at Cooper University Hospital in Camden, N.J., led an open discussion regarding “Transition of Care and the Hospitalist’s Role.” Chapter members had the opportunity to discuss how each individual program actively seeks to decrease readmission rates. Discharge-planning specifics generated group discussion, and a handful of hospitalists offered testimonials about what is working in their practices.
The meeting was sponsored by Merck.
A BOOST for all seasons: Discharge improvement resources now available year round
When Project BOOST (Better Outcomes for Older Adults through Safer Transitions), SHM’s groundbreaking program to reduce readmissions, first began in 2008, hospital sites applied to participate in a yearlong program of one-on-one mentorships, regular sessions to share best practices, and a resource toolkit.
Since then, Project BOOST has grown and evolved. Some BOOST iterations now include third parties, such as the University of Michigan, Blue Cross/Blue Shield of Michigan, and the California HealthCare Foundation. SHM also recently introduced a nationwide, tuition-based version of the BOOST initiative.
Now, SHM is announcing that new resources are available to all hospitals, regardless of their participation in Project BOOST, all year. Some resources were previously available only to Project BOOST participants; others are brand-new materials available to any hospital or hospitalist trying to reduce unplanned readmissions to their hospital.
“No matter where you are in the hospital, you have an opportunity to improve discharge,” says Tina Budnitz, MPH, senior advisor for quality improvement. “The response to Project BOOST has been overwhelmingly positive. That’s why we’re so excited to make these new materials available to anyone responsible for lowering readmissions.”
Individuals can download the Project BOOST implementation course, a new training program specifically designed to help nurses use the proven “teachback” method, and the Project BOOST patient PASS form.
Budnitz and Project BOOST organizers also plan to launch supplemental products for self-implementers, including access to Project BOOST e-mail listservs, data centers, and webinars.
Prepare Now for Flu Season
With most of the country still enjoying warm weather, it’s easy to forget that flu season is right around the corner. Hospitals can either be part of the solution—or part of the problem.
Compared to friends and family outside of the hospital, patients in the hospital are especially at risk. The chances of contracting the flu are higher, given decreased immune responses and increased proximity to caregivers and other potentially infected patients. Plus, the impact of the flu on healthcare providers can be significantly more severe.
By now, most hospitals have protocols for preparing for flu season and isolating infected patients, says Danielle Scheurer, MD, MSc, SFHM, assistant professor of medicine at Harvard Medical School in Boston and director of general medical service at Brigham and Women’s Hospitalist Service. Hospitalists play a special role within those protocols, she adds.
“Hospitalists can be instrumental in preventing the spread of flu within the hospital by having a low threshold for diagnostic testing of patients, immediate isolation of those patients, and strict adherence to infection-control measures in those with suspected influenza,” Dr. Scheurer says.
Dr. Scheurer also emphasizes the fact that flu prevention doesn’t end with better clinical practices. Patient education is key.
“Hospitalists can be vital in educating patients about how to avoid symptomatic contacts,” she says, “and how to advocate for themselves in insisting that all care providers use strict handwashing protocols to avoid transmitting influenza among patients.” TH
As HM continues to grow, the need for clear and accurate data about the specialty will only become more intense. Hospitalists and HM group leaders use survey information to better understand how they compare to other practices across the country, in terms of size and practice characteristics, as well as compensation and productivity.
Increasingly, healthcare executives are turning to survey data—either independently or via their hospitalist group leaders—to get a grasp on the best practices in the industry.
That’s why SHM teamed up with the Medical Group Management Association (MGMA), the industry leader for professional administrators and leaders of medical group practices, to research and develop the State of Hospital Medicine: 2010 Report Based on 2009 Data.
Previously, SHM created and fielded a biannual survey, then analyzed the results independently.

—Leslie A. Flores, MHA, SHM senior advisor for practice management
“Our partnership with MGMA expands our survey population, delivers more information, and brings MGMA’s 90 years of industry credibility in the medical practice management field,” says Leslie A. Flores, MHA, SHM senior advisor for practice management. “The 2010 survey gives hospitalists and hospital administrators an unprecedented snapshot of the state of hospital medicine.”
The 2010 report will be available this month in the “Practice Resources” section of the SHM website (www.hospitalmedicine.org).
The print version will be available to SHM members for $125; for $175, members receive both the print version and the report on CD-ROM.
“This is a first-ever opportunity for hospitalists, group leaders, and healthcare executives to get the clearest picture possible of a rapidly changing industry,” Flores says. TH
Brendon Shank is a freelance writer based in Philadelphia.
SHM Adopts Strict Code for Industry Relations
A long with nearly 20 other organizations, SHM has adopted the Code for Industry Relations (http://cmss.org/) established by the Council on Medical Specialty Societies (CMSS). In an era of digital communication, SHM has created a Web area (www.hospital medicine.org/industry) to continuously update its policies toward industry, display its current partnerships, and disclose the potential conflicts of interest of its board or directors, editors, and CEO.
The message from SHM leadership: SHM is committed to being a leader in an era of transparency and disclosure.
Transparency serves an important role for medical specialty societies, says Norman B. Kahn Jr., MD, executive vice president and CEO of CMSS. The code developed by CMSS and adopted by SHM “assures in interactions with industry that the patients’ needs come first,” Dr. Kahn says. “The bottom line is that this is all about protecting the independence of societies from industry without abrogating the relationship.”
From its early days, SHM has been aware of the need to balance the responsibilities of speaking for HM and the need to disclose any potential conflicts of interests. In 2000, SHM developed its Principles of Organizational Relationships (www.hospitalmedicine.org/OrgRelationships), which have guided the society’s efforts.
The principles call for a clear, bright line that is a barrier between the support of a partner and SHM’s control of content. Among other activities, SHM has applied those principles to meetings and educational initiatives, quality-improvement (QI) projects, and publications.
The principles also were the foundation for the tough conflict-of-interest policies (www.hospital medicine.org/interestpolicies) the board approved in 2005.
Over the last decade, as HM has grown, national hospitalist leaders have become the experts on a wide range of topics and are asked to speak, write, or advise government agencies, foundations, and industry.
As SHM has developed its resources to help hospitalists improve glycemic control, reduce unnecessary DVTs and PEs, and improve the transitions of care, SHM has engaged in partnerships with government agencies, foundations, and industry as well.
“SHM’s leadership recognizes that it has a fiduciary responsibility to its members—a responsibility to provide expert direction, and necessary resources, to enable the hospitalist to ensure the best possible care of his or her patients, and to advance the quality of the hospital system,” says SHM President Jeff Wiese, MD, SFHM. “But SHM cannot do this alone, and when external partnerships are established, it is the organization’s responsibility to enter into these partnerships judiciously, and to be fully transparent to the membership with respect to the arrangements of these partnerships.
“We are confident that no other organization has a more robust disclosure policy than SHM.”
Today’s Nominations, Tomorrow’s Leaders
HM leaders aren’t born that way—they’re nominated.
SHM is accepting nominations for its board election; new members will take office in May at HM11 in Dallas.
The nomination deadline is Oct. 31. Online ballots will be available to all SHM members in late 2010. The results of the election will be announced online in early 2011.
Nominees must be SHM members in good standing. SHM members may nominate themselves or be nominated by another SHM member. Nominations must include a letter of nomination, a one-page CV, and a recent photo.
The nomination committee considers candidates based on length of SHM membership, activity as a hospitalist and SHM member, the prominence of the candidate within the specialty, and a number of other factors.
Board members serve a three-year term and normally serve on one or more committees.
“Participating in SHM’s leadership is one of the best ways to help guide the future of hospital medicine,” says Larry Wellikson, MD, SFHM, CEO of SHM. “That begins by submitting a board nomination to SHM this year.”
Chapter Updates
Chicago
The Chicago chapter met May 19 at Sullivan’s Steakhouse. Twenty-five hospitalists from the Chicago area, including hospitalists at Loyola Hospital, Lutheran General Hospital, Illinois Masonic Medical Center, Trinity Hospital, Silver Cross, and Evanston Hospital, as well as hospitalist groups like Cogent and Vista, attended the meeting.
Dr. Robin Ross of Season Hospice and Palliative Care, which sponsored the event, presented clinical pearls for end-of-life care for the busy hospitalist. The meeting also featured a town-hall discussion, with topics relevant to everyday hospitalist practice—coding, consultations, and the use of observation units. Notification of chapter elections were summated to all chapter members in July and August.
Harrisburg/South Central Pennsylvania
Thirty hospitalists representing six HM programs attended the Harrisburg/South Central Pennsylvania chapter of SHM June 9 at Passage to India in Harrisburg.
Eric Kupersmith, MD, SFHM, division head of the hospitalist program at Cooper University Hospital in Camden, N.J., led an open discussion regarding “Transition of Care and the Hospitalist’s Role.” Chapter members had the opportunity to discuss how each individual program actively seeks to decrease readmission rates. Discharge-planning specifics generated group discussion, and a handful of hospitalists offered testimonials about what is working in their practices.
The meeting was sponsored by Merck.
A BOOST for all seasons: Discharge improvement resources now available year round
When Project BOOST (Better Outcomes for Older Adults through Safer Transitions), SHM’s groundbreaking program to reduce readmissions, first began in 2008, hospital sites applied to participate in a yearlong program of one-on-one mentorships, regular sessions to share best practices, and a resource toolkit.
Since then, Project BOOST has grown and evolved. Some BOOST iterations now include third parties, such as the University of Michigan, Blue Cross/Blue Shield of Michigan, and the California HealthCare Foundation. SHM also recently introduced a nationwide, tuition-based version of the BOOST initiative.
Now, SHM is announcing that new resources are available to all hospitals, regardless of their participation in Project BOOST, all year. Some resources were previously available only to Project BOOST participants; others are brand-new materials available to any hospital or hospitalist trying to reduce unplanned readmissions to their hospital.
“No matter where you are in the hospital, you have an opportunity to improve discharge,” says Tina Budnitz, MPH, senior advisor for quality improvement. “The response to Project BOOST has been overwhelmingly positive. That’s why we’re so excited to make these new materials available to anyone responsible for lowering readmissions.”
Individuals can download the Project BOOST implementation course, a new training program specifically designed to help nurses use the proven “teachback” method, and the Project BOOST patient PASS form.
Budnitz and Project BOOST organizers also plan to launch supplemental products for self-implementers, including access to Project BOOST e-mail listservs, data centers, and webinars.
Prepare Now for Flu Season
With most of the country still enjoying warm weather, it’s easy to forget that flu season is right around the corner. Hospitals can either be part of the solution—or part of the problem.
Compared to friends and family outside of the hospital, patients in the hospital are especially at risk. The chances of contracting the flu are higher, given decreased immune responses and increased proximity to caregivers and other potentially infected patients. Plus, the impact of the flu on healthcare providers can be significantly more severe.
By now, most hospitals have protocols for preparing for flu season and isolating infected patients, says Danielle Scheurer, MD, MSc, SFHM, assistant professor of medicine at Harvard Medical School in Boston and director of general medical service at Brigham and Women’s Hospitalist Service. Hospitalists play a special role within those protocols, she adds.
“Hospitalists can be instrumental in preventing the spread of flu within the hospital by having a low threshold for diagnostic testing of patients, immediate isolation of those patients, and strict adherence to infection-control measures in those with suspected influenza,” Dr. Scheurer says.
Dr. Scheurer also emphasizes the fact that flu prevention doesn’t end with better clinical practices. Patient education is key.
“Hospitalists can be vital in educating patients about how to avoid symptomatic contacts,” she says, “and how to advocate for themselves in insisting that all care providers use strict handwashing protocols to avoid transmitting influenza among patients.” TH
As HM continues to grow, the need for clear and accurate data about the specialty will only become more intense. Hospitalists and HM group leaders use survey information to better understand how they compare to other practices across the country, in terms of size and practice characteristics, as well as compensation and productivity.
Increasingly, healthcare executives are turning to survey data—either independently or via their hospitalist group leaders—to get a grasp on the best practices in the industry.
That’s why SHM teamed up with the Medical Group Management Association (MGMA), the industry leader for professional administrators and leaders of medical group practices, to research and develop the State of Hospital Medicine: 2010 Report Based on 2009 Data.
Previously, SHM created and fielded a biannual survey, then analyzed the results independently.

—Leslie A. Flores, MHA, SHM senior advisor for practice management
“Our partnership with MGMA expands our survey population, delivers more information, and brings MGMA’s 90 years of industry credibility in the medical practice management field,” says Leslie A. Flores, MHA, SHM senior advisor for practice management. “The 2010 survey gives hospitalists and hospital administrators an unprecedented snapshot of the state of hospital medicine.”
The 2010 report will be available this month in the “Practice Resources” section of the SHM website (www.hospitalmedicine.org).
The print version will be available to SHM members for $125; for $175, members receive both the print version and the report on CD-ROM.
“This is a first-ever opportunity for hospitalists, group leaders, and healthcare executives to get the clearest picture possible of a rapidly changing industry,” Flores says. TH
Brendon Shank is a freelance writer based in Philadelphia.
SHM Adopts Strict Code for Industry Relations
A long with nearly 20 other organizations, SHM has adopted the Code for Industry Relations (http://cmss.org/) established by the Council on Medical Specialty Societies (CMSS). In an era of digital communication, SHM has created a Web area (www.hospital medicine.org/industry) to continuously update its policies toward industry, display its current partnerships, and disclose the potential conflicts of interest of its board or directors, editors, and CEO.
The message from SHM leadership: SHM is committed to being a leader in an era of transparency and disclosure.
Transparency serves an important role for medical specialty societies, says Norman B. Kahn Jr., MD, executive vice president and CEO of CMSS. The code developed by CMSS and adopted by SHM “assures in interactions with industry that the patients’ needs come first,” Dr. Kahn says. “The bottom line is that this is all about protecting the independence of societies from industry without abrogating the relationship.”
From its early days, SHM has been aware of the need to balance the responsibilities of speaking for HM and the need to disclose any potential conflicts of interests. In 2000, SHM developed its Principles of Organizational Relationships (www.hospitalmedicine.org/OrgRelationships), which have guided the society’s efforts.
The principles call for a clear, bright line that is a barrier between the support of a partner and SHM’s control of content. Among other activities, SHM has applied those principles to meetings and educational initiatives, quality-improvement (QI) projects, and publications.
The principles also were the foundation for the tough conflict-of-interest policies (www.hospital medicine.org/interestpolicies) the board approved in 2005.
Over the last decade, as HM has grown, national hospitalist leaders have become the experts on a wide range of topics and are asked to speak, write, or advise government agencies, foundations, and industry.
As SHM has developed its resources to help hospitalists improve glycemic control, reduce unnecessary DVTs and PEs, and improve the transitions of care, SHM has engaged in partnerships with government agencies, foundations, and industry as well.
“SHM’s leadership recognizes that it has a fiduciary responsibility to its members—a responsibility to provide expert direction, and necessary resources, to enable the hospitalist to ensure the best possible care of his or her patients, and to advance the quality of the hospital system,” says SHM President Jeff Wiese, MD, SFHM. “But SHM cannot do this alone, and when external partnerships are established, it is the organization’s responsibility to enter into these partnerships judiciously, and to be fully transparent to the membership with respect to the arrangements of these partnerships.
“We are confident that no other organization has a more robust disclosure policy than SHM.”
Today’s Nominations, Tomorrow’s Leaders
HM leaders aren’t born that way—they’re nominated.
SHM is accepting nominations for its board election; new members will take office in May at HM11 in Dallas.
The nomination deadline is Oct. 31. Online ballots will be available to all SHM members in late 2010. The results of the election will be announced online in early 2011.
Nominees must be SHM members in good standing. SHM members may nominate themselves or be nominated by another SHM member. Nominations must include a letter of nomination, a one-page CV, and a recent photo.
The nomination committee considers candidates based on length of SHM membership, activity as a hospitalist and SHM member, the prominence of the candidate within the specialty, and a number of other factors.
Board members serve a three-year term and normally serve on one or more committees.
“Participating in SHM’s leadership is one of the best ways to help guide the future of hospital medicine,” says Larry Wellikson, MD, SFHM, CEO of SHM. “That begins by submitting a board nomination to SHM this year.”
Chapter Updates
Chicago
The Chicago chapter met May 19 at Sullivan’s Steakhouse. Twenty-five hospitalists from the Chicago area, including hospitalists at Loyola Hospital, Lutheran General Hospital, Illinois Masonic Medical Center, Trinity Hospital, Silver Cross, and Evanston Hospital, as well as hospitalist groups like Cogent and Vista, attended the meeting.
Dr. Robin Ross of Season Hospice and Palliative Care, which sponsored the event, presented clinical pearls for end-of-life care for the busy hospitalist. The meeting also featured a town-hall discussion, with topics relevant to everyday hospitalist practice—coding, consultations, and the use of observation units. Notification of chapter elections were summated to all chapter members in July and August.
Harrisburg/South Central Pennsylvania
Thirty hospitalists representing six HM programs attended the Harrisburg/South Central Pennsylvania chapter of SHM June 9 at Passage to India in Harrisburg.
Eric Kupersmith, MD, SFHM, division head of the hospitalist program at Cooper University Hospital in Camden, N.J., led an open discussion regarding “Transition of Care and the Hospitalist’s Role.” Chapter members had the opportunity to discuss how each individual program actively seeks to decrease readmission rates. Discharge-planning specifics generated group discussion, and a handful of hospitalists offered testimonials about what is working in their practices.
The meeting was sponsored by Merck.
A BOOST for all seasons: Discharge improvement resources now available year round
When Project BOOST (Better Outcomes for Older Adults through Safer Transitions), SHM’s groundbreaking program to reduce readmissions, first began in 2008, hospital sites applied to participate in a yearlong program of one-on-one mentorships, regular sessions to share best practices, and a resource toolkit.
Since then, Project BOOST has grown and evolved. Some BOOST iterations now include third parties, such as the University of Michigan, Blue Cross/Blue Shield of Michigan, and the California HealthCare Foundation. SHM also recently introduced a nationwide, tuition-based version of the BOOST initiative.
Now, SHM is announcing that new resources are available to all hospitals, regardless of their participation in Project BOOST, all year. Some resources were previously available only to Project BOOST participants; others are brand-new materials available to any hospital or hospitalist trying to reduce unplanned readmissions to their hospital.
“No matter where you are in the hospital, you have an opportunity to improve discharge,” says Tina Budnitz, MPH, senior advisor for quality improvement. “The response to Project BOOST has been overwhelmingly positive. That’s why we’re so excited to make these new materials available to anyone responsible for lowering readmissions.”
Individuals can download the Project BOOST implementation course, a new training program specifically designed to help nurses use the proven “teachback” method, and the Project BOOST patient PASS form.
Budnitz and Project BOOST organizers also plan to launch supplemental products for self-implementers, including access to Project BOOST e-mail listservs, data centers, and webinars.
Prepare Now for Flu Season
With most of the country still enjoying warm weather, it’s easy to forget that flu season is right around the corner. Hospitals can either be part of the solution—or part of the problem.
Compared to friends and family outside of the hospital, patients in the hospital are especially at risk. The chances of contracting the flu are higher, given decreased immune responses and increased proximity to caregivers and other potentially infected patients. Plus, the impact of the flu on healthcare providers can be significantly more severe.
By now, most hospitals have protocols for preparing for flu season and isolating infected patients, says Danielle Scheurer, MD, MSc, SFHM, assistant professor of medicine at Harvard Medical School in Boston and director of general medical service at Brigham and Women’s Hospitalist Service. Hospitalists play a special role within those protocols, she adds.
“Hospitalists can be instrumental in preventing the spread of flu within the hospital by having a low threshold for diagnostic testing of patients, immediate isolation of those patients, and strict adherence to infection-control measures in those with suspected influenza,” Dr. Scheurer says.
Dr. Scheurer also emphasizes the fact that flu prevention doesn’t end with better clinical practices. Patient education is key.
“Hospitalists can be vital in educating patients about how to avoid symptomatic contacts,” she says, “and how to advocate for themselves in insisting that all care providers use strict handwashing protocols to avoid transmitting influenza among patients.” TH
Join the Club
Every year, hospitalists across the country receive SHM membership renewal notices in the mail. For the vast majority of them, the decision to renew is an easy one.
For the others, hospitalist Mike Hawkins, MD, FACP, FHM, recommends a tried-and-true approach in the field: Evaluate the risk-to-benefit ratio.
“As they say in medicine, the risk-to-benefit ratio is a no-brainer,” says Dr. Hawkins, the Southeast region medical director for Brentwood, Tenn.-based Cogent Healthcare.
Dr. Hawkins should know about membership benefits; he’s been an SHM member since 1996. In fact, he was one of the first 200 members of SHM’s original incarnation, the National Association of Inpatient Physicians. He joined for the resources that helped his new hospitalist program grow and for the access to people who were doing the same thing he was in his hospital. He also recognized the potential for networking and the sharing of ideas from such industry leaders as Bob Wachter, MD, MHM, and John Nelson, MD, MHM.
Since then, the membership benefits that Dr. Hawkins and more than 10,000 other hospitalists receive have evolved along with their careers and the specialty as a whole.
SHM membership and the HM specialty have become nearly synonymous to most hospitalists. “I can’t imagine a true hospitalist that wouldn’t be an SHM member,” Dr. Hawkins says. “Most of the hospitalists on my teams are members. As a company, we strongly encourage our physicians to be SHM members.”
Membership: The Basics
Hawkins’ enthusiasm for becoming an SHM member is no surprise to Todd Von Deak, MBA, CAE, vice president of operations and general manager for SHM.
“Thousands of hospitalists join SHM for the many tangible benefits like discounts or subscriptions to the Journal of Hospital Medicine and The Hospitalist,” Von Deak says.
As SHM has evolved, so have the benefits it offers to members. The original society publication sent to members was only four pages; today, members receive both The Hospitalist and the Journal of Hospital Medicine, one of the top peer-reviewed journals in healthcare—and the only peer-reviewed journal for HM.
The evolution of services to members has helped members establish credibility with their peers. Last year, SHM introduced the Fellow in Hospital Medicine designation to its members. This year, it expanded the fellowship program to include the new Senior Fellow in Hospital Medicine and the Master in Hospital Medicine programs.
“Many of our members are younger than the average physician, and in an emerging specialty,” Von Deak says. “That’s why so many of SHM’s benefits help members to establish themselves within healthcare. Our fellowship program has only been around for two years and we’ve already inducted nearly 1,000 members.”
The products and events—all offered to members at reduced rates—have all grown with SHM and its members. This year’s annual meeting attracted more than 2,500 of the most dedicated hospitalists from around the world.
Eugene Chu, MD, FHM, hospitalist and director of hospital medicine at the Denver Health Medical Center, remembers when he first joined SHM eight years ago. At the time, he says the member discount for the annual meeting was one of the deciding factors. “Financially, it made a lot of sense. The meeting discount and the member fee were close,” he says. “I’m glad it did, as SHM has offered a lot of additional benefits since then.”
Join the Movement
Over time, Dr. Chu found that the discounts for events and products were just the beginning. He now sees value in the energy that SHM brings to its members.
“Being a member brings you into the community of hospitalists,” he says. “It’s hard to quantify, but every time I come back from the spring meeting, I come back really charged up and enthusiastic about where hospital medicine is going.”
Dr. Chu isn’t alone. Many hospitalists become SHM members for financial reasons but end up renewing for the intangibles, Von Deak says.
“As members, they discover a lot more: the ability to network with peers in a growing specialty, a unified voice on critical issues, and, above all, the feeling that they are part of a real movement made up of dedicated professionals just like them,” Von Deak says.
The movement is equal parts human capital and mission. In recent years, SHM members and leadership have created new quality-improvement (QI) programs that have benefited hospitals and patients alike. The Project BOOST (Better Outcomes for Older Adults through Safer Transitions) initiative, for example, is helping more than 60 hospitals improve their discharge processes. Programs like Project BOOST, which was created in 2008, have raised the profiles of both SHM and its members within hospitals and all of healthcare.
SHM members also have ample opportunities for leadership development; like the movement, those opportunities go beyond HM. SHM’s online resource centers and mentored QI programs bring the very best of the specialty to aspiring hospitalist leaders in hospitals across the country.
For Aziz Ansari, DO, an assistant professor in hospital medicine and associate director for Loyola University Medical Center’s hospital medicine practice in Chicago, joining SHM was part of the natural progression in his career. He became an SHM member near the end of his first year as a hospitalist. Since then, Ansari’s appreciation of SHM membership has changed.
“As I progressed into leadership positions in hospital medicine, I found that the society brings credibility to the specialty,” Dr. Ansari explains. “To be established, the society needs members.”
Dr. Ansari can’t imagine not being an active member. “In fact, I haven’t met a nonmember who is as invested in their career and the specialty as SHM’s members are,” he says. TH
Brendon Shank is a freelance writer based in Philadelphia.
Every year, hospitalists across the country receive SHM membership renewal notices in the mail. For the vast majority of them, the decision to renew is an easy one.
For the others, hospitalist Mike Hawkins, MD, FACP, FHM, recommends a tried-and-true approach in the field: Evaluate the risk-to-benefit ratio.
“As they say in medicine, the risk-to-benefit ratio is a no-brainer,” says Dr. Hawkins, the Southeast region medical director for Brentwood, Tenn.-based Cogent Healthcare.
Dr. Hawkins should know about membership benefits; he’s been an SHM member since 1996. In fact, he was one of the first 200 members of SHM’s original incarnation, the National Association of Inpatient Physicians. He joined for the resources that helped his new hospitalist program grow and for the access to people who were doing the same thing he was in his hospital. He also recognized the potential for networking and the sharing of ideas from such industry leaders as Bob Wachter, MD, MHM, and John Nelson, MD, MHM.
Since then, the membership benefits that Dr. Hawkins and more than 10,000 other hospitalists receive have evolved along with their careers and the specialty as a whole.
SHM membership and the HM specialty have become nearly synonymous to most hospitalists. “I can’t imagine a true hospitalist that wouldn’t be an SHM member,” Dr. Hawkins says. “Most of the hospitalists on my teams are members. As a company, we strongly encourage our physicians to be SHM members.”
Membership: The Basics
Hawkins’ enthusiasm for becoming an SHM member is no surprise to Todd Von Deak, MBA, CAE, vice president of operations and general manager for SHM.
“Thousands of hospitalists join SHM for the many tangible benefits like discounts or subscriptions to the Journal of Hospital Medicine and The Hospitalist,” Von Deak says.
As SHM has evolved, so have the benefits it offers to members. The original society publication sent to members was only four pages; today, members receive both The Hospitalist and the Journal of Hospital Medicine, one of the top peer-reviewed journals in healthcare—and the only peer-reviewed journal for HM.
The evolution of services to members has helped members establish credibility with their peers. Last year, SHM introduced the Fellow in Hospital Medicine designation to its members. This year, it expanded the fellowship program to include the new Senior Fellow in Hospital Medicine and the Master in Hospital Medicine programs.
“Many of our members are younger than the average physician, and in an emerging specialty,” Von Deak says. “That’s why so many of SHM’s benefits help members to establish themselves within healthcare. Our fellowship program has only been around for two years and we’ve already inducted nearly 1,000 members.”
The products and events—all offered to members at reduced rates—have all grown with SHM and its members. This year’s annual meeting attracted more than 2,500 of the most dedicated hospitalists from around the world.
Eugene Chu, MD, FHM, hospitalist and director of hospital medicine at the Denver Health Medical Center, remembers when he first joined SHM eight years ago. At the time, he says the member discount for the annual meeting was one of the deciding factors. “Financially, it made a lot of sense. The meeting discount and the member fee were close,” he says. “I’m glad it did, as SHM has offered a lot of additional benefits since then.”
Join the Movement
Over time, Dr. Chu found that the discounts for events and products were just the beginning. He now sees value in the energy that SHM brings to its members.
“Being a member brings you into the community of hospitalists,” he says. “It’s hard to quantify, but every time I come back from the spring meeting, I come back really charged up and enthusiastic about where hospital medicine is going.”
Dr. Chu isn’t alone. Many hospitalists become SHM members for financial reasons but end up renewing for the intangibles, Von Deak says.
“As members, they discover a lot more: the ability to network with peers in a growing specialty, a unified voice on critical issues, and, above all, the feeling that they are part of a real movement made up of dedicated professionals just like them,” Von Deak says.
The movement is equal parts human capital and mission. In recent years, SHM members and leadership have created new quality-improvement (QI) programs that have benefited hospitals and patients alike. The Project BOOST (Better Outcomes for Older Adults through Safer Transitions) initiative, for example, is helping more than 60 hospitals improve their discharge processes. Programs like Project BOOST, which was created in 2008, have raised the profiles of both SHM and its members within hospitals and all of healthcare.
SHM members also have ample opportunities for leadership development; like the movement, those opportunities go beyond HM. SHM’s online resource centers and mentored QI programs bring the very best of the specialty to aspiring hospitalist leaders in hospitals across the country.
For Aziz Ansari, DO, an assistant professor in hospital medicine and associate director for Loyola University Medical Center’s hospital medicine practice in Chicago, joining SHM was part of the natural progression in his career. He became an SHM member near the end of his first year as a hospitalist. Since then, Ansari’s appreciation of SHM membership has changed.
“As I progressed into leadership positions in hospital medicine, I found that the society brings credibility to the specialty,” Dr. Ansari explains. “To be established, the society needs members.”
Dr. Ansari can’t imagine not being an active member. “In fact, I haven’t met a nonmember who is as invested in their career and the specialty as SHM’s members are,” he says. TH
Brendon Shank is a freelance writer based in Philadelphia.
Every year, hospitalists across the country receive SHM membership renewal notices in the mail. For the vast majority of them, the decision to renew is an easy one.
For the others, hospitalist Mike Hawkins, MD, FACP, FHM, recommends a tried-and-true approach in the field: Evaluate the risk-to-benefit ratio.
“As they say in medicine, the risk-to-benefit ratio is a no-brainer,” says Dr. Hawkins, the Southeast region medical director for Brentwood, Tenn.-based Cogent Healthcare.
Dr. Hawkins should know about membership benefits; he’s been an SHM member since 1996. In fact, he was one of the first 200 members of SHM’s original incarnation, the National Association of Inpatient Physicians. He joined for the resources that helped his new hospitalist program grow and for the access to people who were doing the same thing he was in his hospital. He also recognized the potential for networking and the sharing of ideas from such industry leaders as Bob Wachter, MD, MHM, and John Nelson, MD, MHM.
Since then, the membership benefits that Dr. Hawkins and more than 10,000 other hospitalists receive have evolved along with their careers and the specialty as a whole.
SHM membership and the HM specialty have become nearly synonymous to most hospitalists. “I can’t imagine a true hospitalist that wouldn’t be an SHM member,” Dr. Hawkins says. “Most of the hospitalists on my teams are members. As a company, we strongly encourage our physicians to be SHM members.”
Membership: The Basics
Hawkins’ enthusiasm for becoming an SHM member is no surprise to Todd Von Deak, MBA, CAE, vice president of operations and general manager for SHM.
“Thousands of hospitalists join SHM for the many tangible benefits like discounts or subscriptions to the Journal of Hospital Medicine and The Hospitalist,” Von Deak says.
As SHM has evolved, so have the benefits it offers to members. The original society publication sent to members was only four pages; today, members receive both The Hospitalist and the Journal of Hospital Medicine, one of the top peer-reviewed journals in healthcare—and the only peer-reviewed journal for HM.
The evolution of services to members has helped members establish credibility with their peers. Last year, SHM introduced the Fellow in Hospital Medicine designation to its members. This year, it expanded the fellowship program to include the new Senior Fellow in Hospital Medicine and the Master in Hospital Medicine programs.
“Many of our members are younger than the average physician, and in an emerging specialty,” Von Deak says. “That’s why so many of SHM’s benefits help members to establish themselves within healthcare. Our fellowship program has only been around for two years and we’ve already inducted nearly 1,000 members.”
The products and events—all offered to members at reduced rates—have all grown with SHM and its members. This year’s annual meeting attracted more than 2,500 of the most dedicated hospitalists from around the world.
Eugene Chu, MD, FHM, hospitalist and director of hospital medicine at the Denver Health Medical Center, remembers when he first joined SHM eight years ago. At the time, he says the member discount for the annual meeting was one of the deciding factors. “Financially, it made a lot of sense. The meeting discount and the member fee were close,” he says. “I’m glad it did, as SHM has offered a lot of additional benefits since then.”
Join the Movement
Over time, Dr. Chu found that the discounts for events and products were just the beginning. He now sees value in the energy that SHM brings to its members.
“Being a member brings you into the community of hospitalists,” he says. “It’s hard to quantify, but every time I come back from the spring meeting, I come back really charged up and enthusiastic about where hospital medicine is going.”
Dr. Chu isn’t alone. Many hospitalists become SHM members for financial reasons but end up renewing for the intangibles, Von Deak says.
“As members, they discover a lot more: the ability to network with peers in a growing specialty, a unified voice on critical issues, and, above all, the feeling that they are part of a real movement made up of dedicated professionals just like them,” Von Deak says.
The movement is equal parts human capital and mission. In recent years, SHM members and leadership have created new quality-improvement (QI) programs that have benefited hospitals and patients alike. The Project BOOST (Better Outcomes for Older Adults through Safer Transitions) initiative, for example, is helping more than 60 hospitals improve their discharge processes. Programs like Project BOOST, which was created in 2008, have raised the profiles of both SHM and its members within hospitals and all of healthcare.
SHM members also have ample opportunities for leadership development; like the movement, those opportunities go beyond HM. SHM’s online resource centers and mentored QI programs bring the very best of the specialty to aspiring hospitalist leaders in hospitals across the country.
For Aziz Ansari, DO, an assistant professor in hospital medicine and associate director for Loyola University Medical Center’s hospital medicine practice in Chicago, joining SHM was part of the natural progression in his career. He became an SHM member near the end of his first year as a hospitalist. Since then, Ansari’s appreciation of SHM membership has changed.
“As I progressed into leadership positions in hospital medicine, I found that the society brings credibility to the specialty,” Dr. Ansari explains. “To be established, the society needs members.”
Dr. Ansari can’t imagine not being an active member. “In fact, I haven’t met a nonmember who is as invested in their career and the specialty as SHM’s members are,” he says. TH
Brendon Shank is a freelance writer based in Philadelphia.
California Dreamin’
Project BOOST, SHM’s popular mentorship program designed to help hospitals reduce readmissions, is headed to the most populous state in the country. In a joint venture with the California HealthCare Foundation, Project BOOST (Better Outcomes for Older Adults through Safe Transitions) will launch a groundbreaking, two-year program in 20 hospitals in the Golden State.
The California HealthCare Founda-tion will cover almost half of the $28,000 in tuition costs for each hospital accepted into the collaborative program. Individual sites will be responsible for the other $14,500.
In year one, hospitals will begin improving their discharge procedures using Project BOOST’s toolkit and one-on-one mentorships with leaders in the field. The second year of the project will focus on training additional mentors in California. The foundation has committed not only to improving outcomes in the first 20 sites, but also building a sustainable infrastructure that will allow gains to quickly spread throughout the state.
Recruiting for the California sites has just begun. Potential applicants can visit www.hospitalmedicine.org/boost for more information.
“California is a microcosm for the challenges and opportunities for hospitalized care in our healthcare system,” says Janet Nagamine, RN, MD, SFHM, program leader for the California BOOST program and an SHM board member. “We are very excited to work with the California HealthCare Foundation, one of the state’s leaders in healthcare quality improvement. … Their support will help California’s hospitals and primary-care physicians [PCPs] safely transition patients from hospital to home during that vulnerable period.”
Project BOOST’s Continued Expansion
The California program will be SHM’s largest state-specific program to date, representing the fourth wave of BOOST’s continued expansion. With the support of the John A. Hartford Foundation, the program began with six pilot sites throughout the country in 2008. In 2009, Hartford funded 24 additional sites.
In January, SHM, the University of Michigan, and Blue Cross Blue Shield of Michigan announced the first state-specific Project BOOST program. The three organizations announced Michigan’s 14 participating sites in May.
Two other hospital sites began implementing Project BOOST on a tuition-based model in May.
Readmission Challenge
Most hospitalists are intimately familiar with the challenges involved with transitions of care. Research in the April 2009 New England Journal of Medicine by Stephen F. Jencks, MD, MPH, Mark V. Williams, MD, FHM, and Eric A. Coleman, MD, MPH, indicates that 1 in 5 hospitalized patients is readmitted to the hospital within a month of their discharge.1
Balancing the three-legged stool of communication between the hospitalist, PCP, and patient can be demanding. For the individual hospitalist or PCP, it requires intense attention to detail, strong communication skills, and patience. For hospitals, safe transitions require a systemic, team-based approach.
But the alternative—continued or increased readmissions after discharge—is even more taxing. The study found that unplanned readmissions cost Medicare $17.4 billion each year, making estimates of the total cost even higher.1
Looking beyond the costs directly associated with readmissions, the study’s authors see the issue as a potential vital sign that could assess overall healthcare quality. “Although the readmission rate is often presented as a measure of the performance of hospitals, it may also be a useful indicator of the performance of our healthcare system,” they write.
The Approach: Gain Traction, Results
Rather than forcing a one-size-fits-all process on every hospital site, Project BOOST provides individual hospitals with the capacity and experience necessary to implement processes that best fit their unique situation.
Project BOOST sites participate in a two-pronged program consisting of a yearlong, one-on-one mentorship with the leaders in the field. It begins with an intensive, two-day conference and the Project BOOST toolkit.
The toolkit includes printed materials and a new DVD for use by hospitalists and other care providers to facilitate communication with patients and caregivers during discharge.
New case studies published by SHM document some of the program’s earliest successes.
At Piedmont Hospital, a 481-bed acute-care hospital near Atlanta, the full implementation of Project BOOST in one hospital unit has improved many of its “vital signs” in comparison with units that have not implemented BOOST, including decreased length of stay and lower 30-day readmissions (see “Piedmont Hospital: Project BOOST unit vs. regular hospital units,” p. 6).
For St. Mary’s Medical Center, a 582-bed community teaching hospital in St. Louis, hospitalists implementing Project BOOST made a major difference in just three months:
Not only did the Project BOOST unit nearly halve 30-day readmissions (7% from 12%), but the program also increased patient satisfaction, to 68% from 52%.
BOOSTing into the Future
Project BOOST benefits haven’t been limited to program sites and their patients. New innovations from the mentored implementation program have led to resources that all hospitals can use.
SHM recently introduced a new DVD and curriculum package that teaches nurses and discharge planners to use the “teachback” method to communicate with patients during the discharge process. It helps ensure that patients fully understand their care plans and post-discharge instructions.
The teachback package is available at the SHM online store (www.hospitalmedicine.org); it is $85 for SHM members and $125 for nonmembers.
SHM has also launched a BOOST data center and a BOOST community site. The data center enables sites to enter, track, and benchmark key outcomes, which can then be evaluated against comparison units at their own hospitals, BOOST averages, and subsets of hospitals with similar characteristics. The BOOST community site facilitates the sharing of ideas and documents between BOOST hospitals.
New funding approaches will help Project BOOST to continue to reach more hospitals. Since its inception, third parties have provided financial resources for the program.
Now, SHM is offering a tuition-based model, open to hospitals nationwide, which is set to begin this fall.
SHM is accepting applications at www.hospitalmedicine.org/boost. TH
Brendon Shank is a freelance writer based in Philadelphia.
Reference
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Eng J Med. 2009:360:1418-1428.
Project BOOST, SHM’s popular mentorship program designed to help hospitals reduce readmissions, is headed to the most populous state in the country. In a joint venture with the California HealthCare Foundation, Project BOOST (Better Outcomes for Older Adults through Safe Transitions) will launch a groundbreaking, two-year program in 20 hospitals in the Golden State.
The California HealthCare Founda-tion will cover almost half of the $28,000 in tuition costs for each hospital accepted into the collaborative program. Individual sites will be responsible for the other $14,500.
In year one, hospitals will begin improving their discharge procedures using Project BOOST’s toolkit and one-on-one mentorships with leaders in the field. The second year of the project will focus on training additional mentors in California. The foundation has committed not only to improving outcomes in the first 20 sites, but also building a sustainable infrastructure that will allow gains to quickly spread throughout the state.
Recruiting for the California sites has just begun. Potential applicants can visit www.hospitalmedicine.org/boost for more information.
“California is a microcosm for the challenges and opportunities for hospitalized care in our healthcare system,” says Janet Nagamine, RN, MD, SFHM, program leader for the California BOOST program and an SHM board member. “We are very excited to work with the California HealthCare Foundation, one of the state’s leaders in healthcare quality improvement. … Their support will help California’s hospitals and primary-care physicians [PCPs] safely transition patients from hospital to home during that vulnerable period.”
Project BOOST’s Continued Expansion
The California program will be SHM’s largest state-specific program to date, representing the fourth wave of BOOST’s continued expansion. With the support of the John A. Hartford Foundation, the program began with six pilot sites throughout the country in 2008. In 2009, Hartford funded 24 additional sites.
In January, SHM, the University of Michigan, and Blue Cross Blue Shield of Michigan announced the first state-specific Project BOOST program. The three organizations announced Michigan’s 14 participating sites in May.
Two other hospital sites began implementing Project BOOST on a tuition-based model in May.
Readmission Challenge
Most hospitalists are intimately familiar with the challenges involved with transitions of care. Research in the April 2009 New England Journal of Medicine by Stephen F. Jencks, MD, MPH, Mark V. Williams, MD, FHM, and Eric A. Coleman, MD, MPH, indicates that 1 in 5 hospitalized patients is readmitted to the hospital within a month of their discharge.1
Balancing the three-legged stool of communication between the hospitalist, PCP, and patient can be demanding. For the individual hospitalist or PCP, it requires intense attention to detail, strong communication skills, and patience. For hospitals, safe transitions require a systemic, team-based approach.
But the alternative—continued or increased readmissions after discharge—is even more taxing. The study found that unplanned readmissions cost Medicare $17.4 billion each year, making estimates of the total cost even higher.1
Looking beyond the costs directly associated with readmissions, the study’s authors see the issue as a potential vital sign that could assess overall healthcare quality. “Although the readmission rate is often presented as a measure of the performance of hospitals, it may also be a useful indicator of the performance of our healthcare system,” they write.
The Approach: Gain Traction, Results
Rather than forcing a one-size-fits-all process on every hospital site, Project BOOST provides individual hospitals with the capacity and experience necessary to implement processes that best fit their unique situation.
Project BOOST sites participate in a two-pronged program consisting of a yearlong, one-on-one mentorship with the leaders in the field. It begins with an intensive, two-day conference and the Project BOOST toolkit.
The toolkit includes printed materials and a new DVD for use by hospitalists and other care providers to facilitate communication with patients and caregivers during discharge.
New case studies published by SHM document some of the program’s earliest successes.
At Piedmont Hospital, a 481-bed acute-care hospital near Atlanta, the full implementation of Project BOOST in one hospital unit has improved many of its “vital signs” in comparison with units that have not implemented BOOST, including decreased length of stay and lower 30-day readmissions (see “Piedmont Hospital: Project BOOST unit vs. regular hospital units,” p. 6).
For St. Mary’s Medical Center, a 582-bed community teaching hospital in St. Louis, hospitalists implementing Project BOOST made a major difference in just three months:
Not only did the Project BOOST unit nearly halve 30-day readmissions (7% from 12%), but the program also increased patient satisfaction, to 68% from 52%.
BOOSTing into the Future
Project BOOST benefits haven’t been limited to program sites and their patients. New innovations from the mentored implementation program have led to resources that all hospitals can use.
SHM recently introduced a new DVD and curriculum package that teaches nurses and discharge planners to use the “teachback” method to communicate with patients during the discharge process. It helps ensure that patients fully understand their care plans and post-discharge instructions.
The teachback package is available at the SHM online store (www.hospitalmedicine.org); it is $85 for SHM members and $125 for nonmembers.
SHM has also launched a BOOST data center and a BOOST community site. The data center enables sites to enter, track, and benchmark key outcomes, which can then be evaluated against comparison units at their own hospitals, BOOST averages, and subsets of hospitals with similar characteristics. The BOOST community site facilitates the sharing of ideas and documents between BOOST hospitals.
New funding approaches will help Project BOOST to continue to reach more hospitals. Since its inception, third parties have provided financial resources for the program.
Now, SHM is offering a tuition-based model, open to hospitals nationwide, which is set to begin this fall.
SHM is accepting applications at www.hospitalmedicine.org/boost. TH
Brendon Shank is a freelance writer based in Philadelphia.
Reference
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Eng J Med. 2009:360:1418-1428.
Project BOOST, SHM’s popular mentorship program designed to help hospitals reduce readmissions, is headed to the most populous state in the country. In a joint venture with the California HealthCare Foundation, Project BOOST (Better Outcomes for Older Adults through Safe Transitions) will launch a groundbreaking, two-year program in 20 hospitals in the Golden State.
The California HealthCare Founda-tion will cover almost half of the $28,000 in tuition costs for each hospital accepted into the collaborative program. Individual sites will be responsible for the other $14,500.
In year one, hospitals will begin improving their discharge procedures using Project BOOST’s toolkit and one-on-one mentorships with leaders in the field. The second year of the project will focus on training additional mentors in California. The foundation has committed not only to improving outcomes in the first 20 sites, but also building a sustainable infrastructure that will allow gains to quickly spread throughout the state.
Recruiting for the California sites has just begun. Potential applicants can visit www.hospitalmedicine.org/boost for more information.
“California is a microcosm for the challenges and opportunities for hospitalized care in our healthcare system,” says Janet Nagamine, RN, MD, SFHM, program leader for the California BOOST program and an SHM board member. “We are very excited to work with the California HealthCare Foundation, one of the state’s leaders in healthcare quality improvement. … Their support will help California’s hospitals and primary-care physicians [PCPs] safely transition patients from hospital to home during that vulnerable period.”
Project BOOST’s Continued Expansion
The California program will be SHM’s largest state-specific program to date, representing the fourth wave of BOOST’s continued expansion. With the support of the John A. Hartford Foundation, the program began with six pilot sites throughout the country in 2008. In 2009, Hartford funded 24 additional sites.
In January, SHM, the University of Michigan, and Blue Cross Blue Shield of Michigan announced the first state-specific Project BOOST program. The three organizations announced Michigan’s 14 participating sites in May.
Two other hospital sites began implementing Project BOOST on a tuition-based model in May.
Readmission Challenge
Most hospitalists are intimately familiar with the challenges involved with transitions of care. Research in the April 2009 New England Journal of Medicine by Stephen F. Jencks, MD, MPH, Mark V. Williams, MD, FHM, and Eric A. Coleman, MD, MPH, indicates that 1 in 5 hospitalized patients is readmitted to the hospital within a month of their discharge.1
Balancing the three-legged stool of communication between the hospitalist, PCP, and patient can be demanding. For the individual hospitalist or PCP, it requires intense attention to detail, strong communication skills, and patience. For hospitals, safe transitions require a systemic, team-based approach.
But the alternative—continued or increased readmissions after discharge—is even more taxing. The study found that unplanned readmissions cost Medicare $17.4 billion each year, making estimates of the total cost even higher.1
Looking beyond the costs directly associated with readmissions, the study’s authors see the issue as a potential vital sign that could assess overall healthcare quality. “Although the readmission rate is often presented as a measure of the performance of hospitals, it may also be a useful indicator of the performance of our healthcare system,” they write.
The Approach: Gain Traction, Results
Rather than forcing a one-size-fits-all process on every hospital site, Project BOOST provides individual hospitals with the capacity and experience necessary to implement processes that best fit their unique situation.
Project BOOST sites participate in a two-pronged program consisting of a yearlong, one-on-one mentorship with the leaders in the field. It begins with an intensive, two-day conference and the Project BOOST toolkit.
The toolkit includes printed materials and a new DVD for use by hospitalists and other care providers to facilitate communication with patients and caregivers during discharge.
New case studies published by SHM document some of the program’s earliest successes.
At Piedmont Hospital, a 481-bed acute-care hospital near Atlanta, the full implementation of Project BOOST in one hospital unit has improved many of its “vital signs” in comparison with units that have not implemented BOOST, including decreased length of stay and lower 30-day readmissions (see “Piedmont Hospital: Project BOOST unit vs. regular hospital units,” p. 6).
For St. Mary’s Medical Center, a 582-bed community teaching hospital in St. Louis, hospitalists implementing Project BOOST made a major difference in just three months:
Not only did the Project BOOST unit nearly halve 30-day readmissions (7% from 12%), but the program also increased patient satisfaction, to 68% from 52%.
BOOSTing into the Future
Project BOOST benefits haven’t been limited to program sites and their patients. New innovations from the mentored implementation program have led to resources that all hospitals can use.
SHM recently introduced a new DVD and curriculum package that teaches nurses and discharge planners to use the “teachback” method to communicate with patients during the discharge process. It helps ensure that patients fully understand their care plans and post-discharge instructions.
The teachback package is available at the SHM online store (www.hospitalmedicine.org); it is $85 for SHM members and $125 for nonmembers.
SHM has also launched a BOOST data center and a BOOST community site. The data center enables sites to enter, track, and benchmark key outcomes, which can then be evaluated against comparison units at their own hospitals, BOOST averages, and subsets of hospitals with similar characteristics. The BOOST community site facilitates the sharing of ideas and documents between BOOST hospitals.
New funding approaches will help Project BOOST to continue to reach more hospitals. Since its inception, third parties have provided financial resources for the program.
Now, SHM is offering a tuition-based model, open to hospitals nationwide, which is set to begin this fall.
SHM is accepting applications at www.hospitalmedicine.org/boost. TH
Brendon Shank is a freelance writer based in Philadelphia.
Reference
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Eng J Med. 2009:360:1418-1428.
FPHM: Open for Business
2010 could be called the year of recognition for hospitalists. For the hundreds of hospitalists who were inducted as fellows, senior fellows, or master fellows in April, it has already been a momentous year. For some of them—and others, too—their journey toward full recognition of their efforts in the hospital will continue by taking the inaugural Focused Practice in Hospital Medicine (FPHM) Maintenance of Certification (MOC) secure examination administered by the American Board of Internal Medicine (ABIM).
Registration opened for eligible candidates May 1.
The registration period ends Aug. 1.
The first exam is Oct. 25.
In order to qualify for the FPHM MOC program, candidates must submit attestations to ABIM—both from themselves and a supervisor—that demonstrate that the applicant “meets thresholds for internal medicine practice in the hospital setting and professional commitment to hospital medicine,” according to ABIM’s Q&A document about the program.
In addition to attestations, program entrants must have served as a hospitalist for at least three years and fulfill ABIM’s basic requirements for the MOC (see “FPHM Eligibility Requirements,” p. 10).
Why Do It?
While HM has been gaining recognition in the healthcare arena for more than a decade, the FPHM MOC pathway is the first of its kind—and it represents the first time hospitalists will be recognized on an individual level by an independent evaluation organization like ABIM.
“This is a momentous opportunity at every level,” says SHM vice president of operations and general manager Todd Von Deak. “For the individual members, it provides a new kind of recognition of their expertise in a growing specialty. At a higher level, every applicant in the Hospital Medicine MOC program is helping to elevate the specialty among their peers and patients.”
For its part, SHM is helping to promote the program to its membership through informational e-mails to members and additional visibility on the website, www.hospitalmedicine. org.
“We are thrilled to introduce this program to our members,” Von Deak says. “We already have seen strong initial support for the program from SHM members, and we’re confident that even more will apply soon.”
Why Do It Now?
Participation in the first year of the FPHM program can influence the support the program receives in subsequent years, according to Von Deak. “A robust launch year is important to the success of a program like this,” he says. “SHM members can demonstrate to ABIM that this is a valuable program within the specialty by signing up soon. Strength in numbers is critical.”
Plus, hospitalists aren’t required to wait until their ABIM certification expires before registering for the FPHM program. While ABIM certification, which must be renewed every 10 years, is a prerequisite for the FPHM MOC, ABIM-certified hospitalists can register for the program at any time.
Hospitalists who don’t register soon will have to wait for more than 18 months before they can be recognized for their work by ABIM. Certificates for successful applicants in this year’s program will be distributed to hospitalists in early 2011.
For more details, visit www.abim.org, click the “Get Information by Specialty” box, then click the “Hospital Medicine, Focused Practice” section. TH
Brendon Shank is a freelance writer based in Philadelphia.
2010 could be called the year of recognition for hospitalists. For the hundreds of hospitalists who were inducted as fellows, senior fellows, or master fellows in April, it has already been a momentous year. For some of them—and others, too—their journey toward full recognition of their efforts in the hospital will continue by taking the inaugural Focused Practice in Hospital Medicine (FPHM) Maintenance of Certification (MOC) secure examination administered by the American Board of Internal Medicine (ABIM).
Registration opened for eligible candidates May 1.
The registration period ends Aug. 1.
The first exam is Oct. 25.
In order to qualify for the FPHM MOC program, candidates must submit attestations to ABIM—both from themselves and a supervisor—that demonstrate that the applicant “meets thresholds for internal medicine practice in the hospital setting and professional commitment to hospital medicine,” according to ABIM’s Q&A document about the program.
In addition to attestations, program entrants must have served as a hospitalist for at least three years and fulfill ABIM’s basic requirements for the MOC (see “FPHM Eligibility Requirements,” p. 10).
Why Do It?
While HM has been gaining recognition in the healthcare arena for more than a decade, the FPHM MOC pathway is the first of its kind—and it represents the first time hospitalists will be recognized on an individual level by an independent evaluation organization like ABIM.
“This is a momentous opportunity at every level,” says SHM vice president of operations and general manager Todd Von Deak. “For the individual members, it provides a new kind of recognition of their expertise in a growing specialty. At a higher level, every applicant in the Hospital Medicine MOC program is helping to elevate the specialty among their peers and patients.”
For its part, SHM is helping to promote the program to its membership through informational e-mails to members and additional visibility on the website, www.hospitalmedicine. org.
“We are thrilled to introduce this program to our members,” Von Deak says. “We already have seen strong initial support for the program from SHM members, and we’re confident that even more will apply soon.”
Why Do It Now?
Participation in the first year of the FPHM program can influence the support the program receives in subsequent years, according to Von Deak. “A robust launch year is important to the success of a program like this,” he says. “SHM members can demonstrate to ABIM that this is a valuable program within the specialty by signing up soon. Strength in numbers is critical.”
Plus, hospitalists aren’t required to wait until their ABIM certification expires before registering for the FPHM program. While ABIM certification, which must be renewed every 10 years, is a prerequisite for the FPHM MOC, ABIM-certified hospitalists can register for the program at any time.
Hospitalists who don’t register soon will have to wait for more than 18 months before they can be recognized for their work by ABIM. Certificates for successful applicants in this year’s program will be distributed to hospitalists in early 2011.
For more details, visit www.abim.org, click the “Get Information by Specialty” box, then click the “Hospital Medicine, Focused Practice” section. TH
Brendon Shank is a freelance writer based in Philadelphia.
2010 could be called the year of recognition for hospitalists. For the hundreds of hospitalists who were inducted as fellows, senior fellows, or master fellows in April, it has already been a momentous year. For some of them—and others, too—their journey toward full recognition of their efforts in the hospital will continue by taking the inaugural Focused Practice in Hospital Medicine (FPHM) Maintenance of Certification (MOC) secure examination administered by the American Board of Internal Medicine (ABIM).
Registration opened for eligible candidates May 1.
The registration period ends Aug. 1.
The first exam is Oct. 25.
In order to qualify for the FPHM MOC program, candidates must submit attestations to ABIM—both from themselves and a supervisor—that demonstrate that the applicant “meets thresholds for internal medicine practice in the hospital setting and professional commitment to hospital medicine,” according to ABIM’s Q&A document about the program.
In addition to attestations, program entrants must have served as a hospitalist for at least three years and fulfill ABIM’s basic requirements for the MOC (see “FPHM Eligibility Requirements,” p. 10).
Why Do It?
While HM has been gaining recognition in the healthcare arena for more than a decade, the FPHM MOC pathway is the first of its kind—and it represents the first time hospitalists will be recognized on an individual level by an independent evaluation organization like ABIM.
“This is a momentous opportunity at every level,” says SHM vice president of operations and general manager Todd Von Deak. “For the individual members, it provides a new kind of recognition of their expertise in a growing specialty. At a higher level, every applicant in the Hospital Medicine MOC program is helping to elevate the specialty among their peers and patients.”
For its part, SHM is helping to promote the program to its membership through informational e-mails to members and additional visibility on the website, www.hospitalmedicine. org.
“We are thrilled to introduce this program to our members,” Von Deak says. “We already have seen strong initial support for the program from SHM members, and we’re confident that even more will apply soon.”
Why Do It Now?
Participation in the first year of the FPHM program can influence the support the program receives in subsequent years, according to Von Deak. “A robust launch year is important to the success of a program like this,” he says. “SHM members can demonstrate to ABIM that this is a valuable program within the specialty by signing up soon. Strength in numbers is critical.”
Plus, hospitalists aren’t required to wait until their ABIM certification expires before registering for the FPHM program. While ABIM certification, which must be renewed every 10 years, is a prerequisite for the FPHM MOC, ABIM-certified hospitalists can register for the program at any time.
Hospitalists who don’t register soon will have to wait for more than 18 months before they can be recognized for their work by ABIM. Certificates for successful applicants in this year’s program will be distributed to hospitalists in early 2011.
For more details, visit www.abim.org, click the “Get Information by Specialty” box, then click the “Hospital Medicine, Focused Practice” section. TH
Brendon Shank is a freelance writer based in Philadelphia.