User login
Project BOOST, SHM’s popular mentorship program designed to help hospitals reduce readmissions, is headed to the most populous state in the country. In a joint venture with the California HealthCare Foundation, Project BOOST (Better Outcomes for Older Adults through Safe Transitions) will launch a groundbreaking, two-year program in 20 hospitals in the Golden State.
The California HealthCare Founda-tion will cover almost half of the $28,000 in tuition costs for each hospital accepted into the collaborative program. Individual sites will be responsible for the other $14,500.
In year one, hospitals will begin improving their discharge procedures using Project BOOST’s toolkit and one-on-one mentorships with leaders in the field. The second year of the project will focus on training additional mentors in California. The foundation has committed not only to improving outcomes in the first 20 sites, but also building a sustainable infrastructure that will allow gains to quickly spread throughout the state.
Recruiting for the California sites has just begun. Potential applicants can visit www.hospitalmedicine.org/boost for more information.
“California is a microcosm for the challenges and opportunities for hospitalized care in our healthcare system,” says Janet Nagamine, RN, MD, SFHM, program leader for the California BOOST program and an SHM board member. “We are very excited to work with the California HealthCare Foundation, one of the state’s leaders in healthcare quality improvement. … Their support will help California’s hospitals and primary-care physicians [PCPs] safely transition patients from hospital to home during that vulnerable period.”
Project BOOST’s Continued Expansion
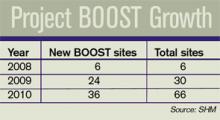
The California program will be SHM’s largest state-specific program to date, representing the fourth wave of BOOST’s continued expansion. With the support of the John A. Hartford Foundation, the program began with six pilot sites throughout the country in 2008. In 2009, Hartford funded 24 additional sites.
In January, SHM, the University of Michigan, and Blue Cross Blue Shield of Michigan announced the first state-specific Project BOOST program. The three organizations announced Michigan’s 14 participating sites in May.
Two other hospital sites began implementing Project BOOST on a tuition-based model in May.
Readmission Challenge
Most hospitalists are intimately familiar with the challenges involved with transitions of care. Research in the April 2009 New England Journal of Medicine by Stephen F. Jencks, MD, MPH, Mark V. Williams, MD, FHM, and Eric A. Coleman, MD, MPH, indicates that 1 in 5 hospitalized patients is readmitted to the hospital within a month of their discharge.1
Balancing the three-legged stool of communication between the hospitalist, PCP, and patient can be demanding. For the individual hospitalist or PCP, it requires intense attention to detail, strong communication skills, and patience. For hospitals, safe transitions require a systemic, team-based approach.
But the alternative—continued or increased readmissions after discharge—is even more taxing. The study found that unplanned readmissions cost Medicare $17.4 billion each year, making estimates of the total cost even higher.1
Looking beyond the costs directly associated with readmissions, the study’s authors see the issue as a potential vital sign that could assess overall healthcare quality. “Although the readmission rate is often presented as a measure of the performance of hospitals, it may also be a useful indicator of the performance of our healthcare system,” they write.
The Approach: Gain Traction, Results
Rather than forcing a one-size-fits-all process on every hospital site, Project BOOST provides individual hospitals with the capacity and experience necessary to implement processes that best fit their unique situation.
Project BOOST sites participate in a two-pronged program consisting of a yearlong, one-on-one mentorship with the leaders in the field. It begins with an intensive, two-day conference and the Project BOOST toolkit.
The toolkit includes printed materials and a new DVD for use by hospitalists and other care providers to facilitate communication with patients and caregivers during discharge.
New case studies published by SHM document some of the program’s earliest successes.
At Piedmont Hospital, a 481-bed acute-care hospital near Atlanta, the full implementation of Project BOOST in one hospital unit has improved many of its “vital signs” in comparison with units that have not implemented BOOST, including decreased length of stay and lower 30-day readmissions (see “Piedmont Hospital: Project BOOST unit vs. regular hospital units,” p. 6).
For St. Mary’s Medical Center, a 582-bed community teaching hospital in St. Louis, hospitalists implementing Project BOOST made a major difference in just three months:
Not only did the Project BOOST unit nearly halve 30-day readmissions (7% from 12%), but the program also increased patient satisfaction, to 68% from 52%.
BOOSTing into the Future
Project BOOST benefits haven’t been limited to program sites and their patients. New innovations from the mentored implementation program have led to resources that all hospitals can use.
SHM recently introduced a new DVD and curriculum package that teaches nurses and discharge planners to use the “teachback” method to communicate with patients during the discharge process. It helps ensure that patients fully understand their care plans and post-discharge instructions.
The teachback package is available at the SHM online store (www.hospitalmedicine.org); it is $85 for SHM members and $125 for nonmembers.
SHM has also launched a BOOST data center and a BOOST community site. The data center enables sites to enter, track, and benchmark key outcomes, which can then be evaluated against comparison units at their own hospitals, BOOST averages, and subsets of hospitals with similar characteristics. The BOOST community site facilitates the sharing of ideas and documents between BOOST hospitals.
New funding approaches will help Project BOOST to continue to reach more hospitals. Since its inception, third parties have provided financial resources for the program.
Now, SHM is offering a tuition-based model, open to hospitals nationwide, which is set to begin this fall.
SHM is accepting applications at www.hospitalmedicine.org/boost. TH
Brendon Shank is a freelance writer based in Philadelphia.
Reference
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Eng J Med. 2009:360:1418-1428.
Project BOOST, SHM’s popular mentorship program designed to help hospitals reduce readmissions, is headed to the most populous state in the country. In a joint venture with the California HealthCare Foundation, Project BOOST (Better Outcomes for Older Adults through Safe Transitions) will launch a groundbreaking, two-year program in 20 hospitals in the Golden State.
The California HealthCare Founda-tion will cover almost half of the $28,000 in tuition costs for each hospital accepted into the collaborative program. Individual sites will be responsible for the other $14,500.
In year one, hospitals will begin improving their discharge procedures using Project BOOST’s toolkit and one-on-one mentorships with leaders in the field. The second year of the project will focus on training additional mentors in California. The foundation has committed not only to improving outcomes in the first 20 sites, but also building a sustainable infrastructure that will allow gains to quickly spread throughout the state.
Recruiting for the California sites has just begun. Potential applicants can visit www.hospitalmedicine.org/boost for more information.
“California is a microcosm for the challenges and opportunities for hospitalized care in our healthcare system,” says Janet Nagamine, RN, MD, SFHM, program leader for the California BOOST program and an SHM board member. “We are very excited to work with the California HealthCare Foundation, one of the state’s leaders in healthcare quality improvement. … Their support will help California’s hospitals and primary-care physicians [PCPs] safely transition patients from hospital to home during that vulnerable period.”
Project BOOST’s Continued Expansion
The California program will be SHM’s largest state-specific program to date, representing the fourth wave of BOOST’s continued expansion. With the support of the John A. Hartford Foundation, the program began with six pilot sites throughout the country in 2008. In 2009, Hartford funded 24 additional sites.
In January, SHM, the University of Michigan, and Blue Cross Blue Shield of Michigan announced the first state-specific Project BOOST program. The three organizations announced Michigan’s 14 participating sites in May.
Two other hospital sites began implementing Project BOOST on a tuition-based model in May.
Readmission Challenge
Most hospitalists are intimately familiar with the challenges involved with transitions of care. Research in the April 2009 New England Journal of Medicine by Stephen F. Jencks, MD, MPH, Mark V. Williams, MD, FHM, and Eric A. Coleman, MD, MPH, indicates that 1 in 5 hospitalized patients is readmitted to the hospital within a month of their discharge.1
Balancing the three-legged stool of communication between the hospitalist, PCP, and patient can be demanding. For the individual hospitalist or PCP, it requires intense attention to detail, strong communication skills, and patience. For hospitals, safe transitions require a systemic, team-based approach.
But the alternative—continued or increased readmissions after discharge—is even more taxing. The study found that unplanned readmissions cost Medicare $17.4 billion each year, making estimates of the total cost even higher.1
Looking beyond the costs directly associated with readmissions, the study’s authors see the issue as a potential vital sign that could assess overall healthcare quality. “Although the readmission rate is often presented as a measure of the performance of hospitals, it may also be a useful indicator of the performance of our healthcare system,” they write.
The Approach: Gain Traction, Results
Rather than forcing a one-size-fits-all process on every hospital site, Project BOOST provides individual hospitals with the capacity and experience necessary to implement processes that best fit their unique situation.
Project BOOST sites participate in a two-pronged program consisting of a yearlong, one-on-one mentorship with the leaders in the field. It begins with an intensive, two-day conference and the Project BOOST toolkit.
The toolkit includes printed materials and a new DVD for use by hospitalists and other care providers to facilitate communication with patients and caregivers during discharge.
New case studies published by SHM document some of the program’s earliest successes.
At Piedmont Hospital, a 481-bed acute-care hospital near Atlanta, the full implementation of Project BOOST in one hospital unit has improved many of its “vital signs” in comparison with units that have not implemented BOOST, including decreased length of stay and lower 30-day readmissions (see “Piedmont Hospital: Project BOOST unit vs. regular hospital units,” p. 6).
For St. Mary’s Medical Center, a 582-bed community teaching hospital in St. Louis, hospitalists implementing Project BOOST made a major difference in just three months:
Not only did the Project BOOST unit nearly halve 30-day readmissions (7% from 12%), but the program also increased patient satisfaction, to 68% from 52%.
BOOSTing into the Future
Project BOOST benefits haven’t been limited to program sites and their patients. New innovations from the mentored implementation program have led to resources that all hospitals can use.
SHM recently introduced a new DVD and curriculum package that teaches nurses and discharge planners to use the “teachback” method to communicate with patients during the discharge process. It helps ensure that patients fully understand their care plans and post-discharge instructions.
The teachback package is available at the SHM online store (www.hospitalmedicine.org); it is $85 for SHM members and $125 for nonmembers.
SHM has also launched a BOOST data center and a BOOST community site. The data center enables sites to enter, track, and benchmark key outcomes, which can then be evaluated against comparison units at their own hospitals, BOOST averages, and subsets of hospitals with similar characteristics. The BOOST community site facilitates the sharing of ideas and documents between BOOST hospitals.
New funding approaches will help Project BOOST to continue to reach more hospitals. Since its inception, third parties have provided financial resources for the program.
Now, SHM is offering a tuition-based model, open to hospitals nationwide, which is set to begin this fall.
SHM is accepting applications at www.hospitalmedicine.org/boost. TH
Brendon Shank is a freelance writer based in Philadelphia.
Reference
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Eng J Med. 2009:360:1418-1428.
Project BOOST, SHM’s popular mentorship program designed to help hospitals reduce readmissions, is headed to the most populous state in the country. In a joint venture with the California HealthCare Foundation, Project BOOST (Better Outcomes for Older Adults through Safe Transitions) will launch a groundbreaking, two-year program in 20 hospitals in the Golden State.
The California HealthCare Founda-tion will cover almost half of the $28,000 in tuition costs for each hospital accepted into the collaborative program. Individual sites will be responsible for the other $14,500.
In year one, hospitals will begin improving their discharge procedures using Project BOOST’s toolkit and one-on-one mentorships with leaders in the field. The second year of the project will focus on training additional mentors in California. The foundation has committed not only to improving outcomes in the first 20 sites, but also building a sustainable infrastructure that will allow gains to quickly spread throughout the state.
Recruiting for the California sites has just begun. Potential applicants can visit www.hospitalmedicine.org/boost for more information.
“California is a microcosm for the challenges and opportunities for hospitalized care in our healthcare system,” says Janet Nagamine, RN, MD, SFHM, program leader for the California BOOST program and an SHM board member. “We are very excited to work with the California HealthCare Foundation, one of the state’s leaders in healthcare quality improvement. … Their support will help California’s hospitals and primary-care physicians [PCPs] safely transition patients from hospital to home during that vulnerable period.”
Project BOOST’s Continued Expansion
The California program will be SHM’s largest state-specific program to date, representing the fourth wave of BOOST’s continued expansion. With the support of the John A. Hartford Foundation, the program began with six pilot sites throughout the country in 2008. In 2009, Hartford funded 24 additional sites.
In January, SHM, the University of Michigan, and Blue Cross Blue Shield of Michigan announced the first state-specific Project BOOST program. The three organizations announced Michigan’s 14 participating sites in May.
Two other hospital sites began implementing Project BOOST on a tuition-based model in May.
Readmission Challenge
Most hospitalists are intimately familiar with the challenges involved with transitions of care. Research in the April 2009 New England Journal of Medicine by Stephen F. Jencks, MD, MPH, Mark V. Williams, MD, FHM, and Eric A. Coleman, MD, MPH, indicates that 1 in 5 hospitalized patients is readmitted to the hospital within a month of their discharge.1
Balancing the three-legged stool of communication between the hospitalist, PCP, and patient can be demanding. For the individual hospitalist or PCP, it requires intense attention to detail, strong communication skills, and patience. For hospitals, safe transitions require a systemic, team-based approach.
But the alternative—continued or increased readmissions after discharge—is even more taxing. The study found that unplanned readmissions cost Medicare $17.4 billion each year, making estimates of the total cost even higher.1
Looking beyond the costs directly associated with readmissions, the study’s authors see the issue as a potential vital sign that could assess overall healthcare quality. “Although the readmission rate is often presented as a measure of the performance of hospitals, it may also be a useful indicator of the performance of our healthcare system,” they write.
The Approach: Gain Traction, Results
Rather than forcing a one-size-fits-all process on every hospital site, Project BOOST provides individual hospitals with the capacity and experience necessary to implement processes that best fit their unique situation.
Project BOOST sites participate in a two-pronged program consisting of a yearlong, one-on-one mentorship with the leaders in the field. It begins with an intensive, two-day conference and the Project BOOST toolkit.
The toolkit includes printed materials and a new DVD for use by hospitalists and other care providers to facilitate communication with patients and caregivers during discharge.
New case studies published by SHM document some of the program’s earliest successes.
At Piedmont Hospital, a 481-bed acute-care hospital near Atlanta, the full implementation of Project BOOST in one hospital unit has improved many of its “vital signs” in comparison with units that have not implemented BOOST, including decreased length of stay and lower 30-day readmissions (see “Piedmont Hospital: Project BOOST unit vs. regular hospital units,” p. 6).
For St. Mary’s Medical Center, a 582-bed community teaching hospital in St. Louis, hospitalists implementing Project BOOST made a major difference in just three months:
Not only did the Project BOOST unit nearly halve 30-day readmissions (7% from 12%), but the program also increased patient satisfaction, to 68% from 52%.
BOOSTing into the Future
Project BOOST benefits haven’t been limited to program sites and their patients. New innovations from the mentored implementation program have led to resources that all hospitals can use.
SHM recently introduced a new DVD and curriculum package that teaches nurses and discharge planners to use the “teachback” method to communicate with patients during the discharge process. It helps ensure that patients fully understand their care plans and post-discharge instructions.
The teachback package is available at the SHM online store (www.hospitalmedicine.org); it is $85 for SHM members and $125 for nonmembers.
SHM has also launched a BOOST data center and a BOOST community site. The data center enables sites to enter, track, and benchmark key outcomes, which can then be evaluated against comparison units at their own hospitals, BOOST averages, and subsets of hospitals with similar characteristics. The BOOST community site facilitates the sharing of ideas and documents between BOOST hospitals.
New funding approaches will help Project BOOST to continue to reach more hospitals. Since its inception, third parties have provided financial resources for the program.
Now, SHM is offering a tuition-based model, open to hospitals nationwide, which is set to begin this fall.
SHM is accepting applications at www.hospitalmedicine.org/boost. TH
Brendon Shank is a freelance writer based in Philadelphia.
Reference
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Eng J Med. 2009:360:1418-1428.