User login
Brendon Shank joined the Society of Hospital Medicine in February 2011 and serves as Associate Vice President of Communications. He is responsible for maintaining a dialogue between SHM and its many audiences, including members, media and others in healthcare.
SQUINT Is Looking Out For You
Starting a new, hospital-based quality-improvement (QI) program can be a lonely task for hospitalists. What can begin with a rush of enthusiasm to solve a critical problem on your hospital floor quickly can lead to a single hospitalist in front of a computer screen wondering, "Has anyone else ever done this before?"
Unlike clinical knowledge, most of which comes from years of specialized formal training and volumes of peer-reviewed evidence on procedures, starting QI programs often presents a special challenge: a blank page and limited access to those who’ve taken on similar projects.
Those challenges, and the need to better understand what other hospitalists have already tried, motivated SHM’s Center for Hospital Innovation & Improvement, also known as The Center, to develop SQUINT, a new user-generated online repository of hospital-based QI programs.
"Being asked to lead a quality-improvement project is a daunting and difficult task," says Andrew Dunn, MD, FACP, professor of medicine and acting chief for Mount Sinai School of Medicine’s hospital medicine division in New York City. "Getting ideas on methods that have worked elsewhere is a great way to start. SQUINT is an easy way for hospitalists to get a head start on a project rather than start from scratch."
Access to SQUINT (SHM’s QUality Improve-ment NeTwork) is free to SHM members. Log in and gain access to summaries of QI programs from around the country. Because the summaries are searchable based on type, size, location, and specific kinds of topics, hospitalists can quickly find out whether projects similar to theirs are available through SQUINT.
For instance, a user could search for projects specifically related to transitions of care during discharge at community hospitals with 200-299 beds; a user in Oklahoma could search for all QI projects that have been uploaded from hospitals in the Sooner State. SQUINT also affords users keyword searches and browsing options.
For Hasan F. Shabbir, MD, SFHM, chief quality officer at Emory Johns Creek Hospital and assistant professor of medicine for Emory University School of Medicine’s division of hospital medicine in Atlanta, the ability to search user-generated, user-posted project files is especially important. Dr. Shabbir is no stranger to starting a QI project cold, or poring through literature and searching the Internet, worried that the materials don’t always explain the outcomes of a QI project that can be found through Google.
"You may just find a PDF on the Web and not know if it was a success," he says. "What’s unique about SQUINT is that it gives you a product, describes how it was utilized, and describes how it was—or wasn’t—effective. A lot of the work that needs to be done doesn’t always achieve the intended result."
Understanding the pitfalls and challenges of QI programs can save time and effort, he explains. "It’s equally important," he says. "Typically, only the successful stuff gets published in journals."
One of the first projects shared via SQUINT is a case study in using local resources to improve transitions of care for diabetic patients, submitted by medical director Jordan Messler, MD, SFHM, and his colleagues at Morton Plant Hospital in Clearwater, Fla.
"This was a project that we have done that we were probably not going to publish, but came up with some neat process things that we can share," says Dr. Messler, who hopes his team’s progress could help others get started. "If just one other program finds it and it saves them some time, that would be great."
Uploading descriptions of the QI programs can take as little as 15 minutes. Once project details and supporting documents are loaded into SQUINT, submissions are reviewed by members of SHM’s Health Quality and Patient Safety committee for clarity, the involvement of multidisciplinary team members, presentation of details, and the description of impacts and barriers to success.
Dr. Messler found the process of uploading simple and easy to use. He plans to add more.
"We have a variety of programs that we’ll probably upload," he says, including other recent QI programs addressing diabetes and DVT. "There’s no harm in putting them up there."
—Andrew Dunn, MD, FACP, professor, acting chief, hospital medicine division, Mount Sinai School of Medicine, New York City
Like other online user-submitted forums, submitting accepted content has added benefits: increased visibility among a community dedicated to improving the care of hospitalized patients and career advancement.
"This is a portal for you to spread what you’ve learned," Dr. Messler says. "Then, over time, this could be something that could be added to a resume or get to the point that folks will be proud of having a list of submissions to SQUINT."
For Dr. Shabbir, the utility of SQUINT extends beyond his own use.
"I have a junior colleague who is working on a new quality-improvement program. I’m going to tell her to look into SQUINT to see if others have worked on similar programs," he says. "If they have, that will put you two or three steps forward. For the novice, it also teaches the language and structure of how quality improvement happens."
Teaching and changing patient safety is a big part of SQUINT’s goal, according to Dr. Dunn.
"Hospitals should not need to start at ground zero, take months to get started and re-create every mistake made at other institutions," he says. "By sharing successful projects and learning from our errors, we can move patient safety initiatives along faster and better. … And that will, hopefully, improve outcomes across the country."
Brendon Shank is associate vice president of communications at SHM.
Starting a new, hospital-based quality-improvement (QI) program can be a lonely task for hospitalists. What can begin with a rush of enthusiasm to solve a critical problem on your hospital floor quickly can lead to a single hospitalist in front of a computer screen wondering, "Has anyone else ever done this before?"
Unlike clinical knowledge, most of which comes from years of specialized formal training and volumes of peer-reviewed evidence on procedures, starting QI programs often presents a special challenge: a blank page and limited access to those who’ve taken on similar projects.
Those challenges, and the need to better understand what other hospitalists have already tried, motivated SHM’s Center for Hospital Innovation & Improvement, also known as The Center, to develop SQUINT, a new user-generated online repository of hospital-based QI programs.
"Being asked to lead a quality-improvement project is a daunting and difficult task," says Andrew Dunn, MD, FACP, professor of medicine and acting chief for Mount Sinai School of Medicine’s hospital medicine division in New York City. "Getting ideas on methods that have worked elsewhere is a great way to start. SQUINT is an easy way for hospitalists to get a head start on a project rather than start from scratch."
Access to SQUINT (SHM’s QUality Improve-ment NeTwork) is free to SHM members. Log in and gain access to summaries of QI programs from around the country. Because the summaries are searchable based on type, size, location, and specific kinds of topics, hospitalists can quickly find out whether projects similar to theirs are available through SQUINT.
For instance, a user could search for projects specifically related to transitions of care during discharge at community hospitals with 200-299 beds; a user in Oklahoma could search for all QI projects that have been uploaded from hospitals in the Sooner State. SQUINT also affords users keyword searches and browsing options.
For Hasan F. Shabbir, MD, SFHM, chief quality officer at Emory Johns Creek Hospital and assistant professor of medicine for Emory University School of Medicine’s division of hospital medicine in Atlanta, the ability to search user-generated, user-posted project files is especially important. Dr. Shabbir is no stranger to starting a QI project cold, or poring through literature and searching the Internet, worried that the materials don’t always explain the outcomes of a QI project that can be found through Google.
"You may just find a PDF on the Web and not know if it was a success," he says. "What’s unique about SQUINT is that it gives you a product, describes how it was utilized, and describes how it was—or wasn’t—effective. A lot of the work that needs to be done doesn’t always achieve the intended result."
Understanding the pitfalls and challenges of QI programs can save time and effort, he explains. "It’s equally important," he says. "Typically, only the successful stuff gets published in journals."
One of the first projects shared via SQUINT is a case study in using local resources to improve transitions of care for diabetic patients, submitted by medical director Jordan Messler, MD, SFHM, and his colleagues at Morton Plant Hospital in Clearwater, Fla.
"This was a project that we have done that we were probably not going to publish, but came up with some neat process things that we can share," says Dr. Messler, who hopes his team’s progress could help others get started. "If just one other program finds it and it saves them some time, that would be great."
Uploading descriptions of the QI programs can take as little as 15 minutes. Once project details and supporting documents are loaded into SQUINT, submissions are reviewed by members of SHM’s Health Quality and Patient Safety committee for clarity, the involvement of multidisciplinary team members, presentation of details, and the description of impacts and barriers to success.
Dr. Messler found the process of uploading simple and easy to use. He plans to add more.
"We have a variety of programs that we’ll probably upload," he says, including other recent QI programs addressing diabetes and DVT. "There’s no harm in putting them up there."
—Andrew Dunn, MD, FACP, professor, acting chief, hospital medicine division, Mount Sinai School of Medicine, New York City
Like other online user-submitted forums, submitting accepted content has added benefits: increased visibility among a community dedicated to improving the care of hospitalized patients and career advancement.
"This is a portal for you to spread what you’ve learned," Dr. Messler says. "Then, over time, this could be something that could be added to a resume or get to the point that folks will be proud of having a list of submissions to SQUINT."
For Dr. Shabbir, the utility of SQUINT extends beyond his own use.
"I have a junior colleague who is working on a new quality-improvement program. I’m going to tell her to look into SQUINT to see if others have worked on similar programs," he says. "If they have, that will put you two or three steps forward. For the novice, it also teaches the language and structure of how quality improvement happens."
Teaching and changing patient safety is a big part of SQUINT’s goal, according to Dr. Dunn.
"Hospitals should not need to start at ground zero, take months to get started and re-create every mistake made at other institutions," he says. "By sharing successful projects and learning from our errors, we can move patient safety initiatives along faster and better. … And that will, hopefully, improve outcomes across the country."
Brendon Shank is associate vice president of communications at SHM.
Starting a new, hospital-based quality-improvement (QI) program can be a lonely task for hospitalists. What can begin with a rush of enthusiasm to solve a critical problem on your hospital floor quickly can lead to a single hospitalist in front of a computer screen wondering, "Has anyone else ever done this before?"
Unlike clinical knowledge, most of which comes from years of specialized formal training and volumes of peer-reviewed evidence on procedures, starting QI programs often presents a special challenge: a blank page and limited access to those who’ve taken on similar projects.
Those challenges, and the need to better understand what other hospitalists have already tried, motivated SHM’s Center for Hospital Innovation & Improvement, also known as The Center, to develop SQUINT, a new user-generated online repository of hospital-based QI programs.
"Being asked to lead a quality-improvement project is a daunting and difficult task," says Andrew Dunn, MD, FACP, professor of medicine and acting chief for Mount Sinai School of Medicine’s hospital medicine division in New York City. "Getting ideas on methods that have worked elsewhere is a great way to start. SQUINT is an easy way for hospitalists to get a head start on a project rather than start from scratch."
Access to SQUINT (SHM’s QUality Improve-ment NeTwork) is free to SHM members. Log in and gain access to summaries of QI programs from around the country. Because the summaries are searchable based on type, size, location, and specific kinds of topics, hospitalists can quickly find out whether projects similar to theirs are available through SQUINT.
For instance, a user could search for projects specifically related to transitions of care during discharge at community hospitals with 200-299 beds; a user in Oklahoma could search for all QI projects that have been uploaded from hospitals in the Sooner State. SQUINT also affords users keyword searches and browsing options.
For Hasan F. Shabbir, MD, SFHM, chief quality officer at Emory Johns Creek Hospital and assistant professor of medicine for Emory University School of Medicine’s division of hospital medicine in Atlanta, the ability to search user-generated, user-posted project files is especially important. Dr. Shabbir is no stranger to starting a QI project cold, or poring through literature and searching the Internet, worried that the materials don’t always explain the outcomes of a QI project that can be found through Google.
"You may just find a PDF on the Web and not know if it was a success," he says. "What’s unique about SQUINT is that it gives you a product, describes how it was utilized, and describes how it was—or wasn’t—effective. A lot of the work that needs to be done doesn’t always achieve the intended result."
Understanding the pitfalls and challenges of QI programs can save time and effort, he explains. "It’s equally important," he says. "Typically, only the successful stuff gets published in journals."
One of the first projects shared via SQUINT is a case study in using local resources to improve transitions of care for diabetic patients, submitted by medical director Jordan Messler, MD, SFHM, and his colleagues at Morton Plant Hospital in Clearwater, Fla.
"This was a project that we have done that we were probably not going to publish, but came up with some neat process things that we can share," says Dr. Messler, who hopes his team’s progress could help others get started. "If just one other program finds it and it saves them some time, that would be great."
Uploading descriptions of the QI programs can take as little as 15 minutes. Once project details and supporting documents are loaded into SQUINT, submissions are reviewed by members of SHM’s Health Quality and Patient Safety committee for clarity, the involvement of multidisciplinary team members, presentation of details, and the description of impacts and barriers to success.
Dr. Messler found the process of uploading simple and easy to use. He plans to add more.
"We have a variety of programs that we’ll probably upload," he says, including other recent QI programs addressing diabetes and DVT. "There’s no harm in putting them up there."
—Andrew Dunn, MD, FACP, professor, acting chief, hospital medicine division, Mount Sinai School of Medicine, New York City
Like other online user-submitted forums, submitting accepted content has added benefits: increased visibility among a community dedicated to improving the care of hospitalized patients and career advancement.
"This is a portal for you to spread what you’ve learned," Dr. Messler says. "Then, over time, this could be something that could be added to a resume or get to the point that folks will be proud of having a list of submissions to SQUINT."
For Dr. Shabbir, the utility of SQUINT extends beyond his own use.
"I have a junior colleague who is working on a new quality-improvement program. I’m going to tell her to look into SQUINT to see if others have worked on similar programs," he says. "If they have, that will put you two or three steps forward. For the novice, it also teaches the language and structure of how quality improvement happens."
Teaching and changing patient safety is a big part of SQUINT’s goal, according to Dr. Dunn.
"Hospitals should not need to start at ground zero, take months to get started and re-create every mistake made at other institutions," he says. "By sharing successful projects and learning from our errors, we can move patient safety initiatives along faster and better. … And that will, hopefully, improve outcomes across the country."
Brendon Shank is associate vice president of communications at SHM.
Discharge improvement
If you’re a hospitalist interested in reducing readmissions in your hospital, the time to act is now.
Project BOOST (Better Outcomes for Older Adults through Safe Transitions), SHM’s groundbreaking program designed to help hospitals reduce unplanned readmissions, is now accepting applications for two new cohorts: one national and another specific to California. The deadline for applications is August 1.
Now with 85 sites as part of the national community, Project BOOST will introduce new sites across the country in the fall. In addition to the national cohort, Project BOOST will also establish a new cohort in California, with discounted tuition through grants from three healthcare groups in the state.
“It’s a great time to apply,” says Stephanie Rennke, MD, assistant clinical professor of medicine at the University of California San Francisco Medical Center. “We are at the cusp of a lot of big changes in health reform. The time to address readmissions is now. Hospitals will have to address this, and BOOST is one way to do that.”

—Stephanie Rennke, MD, assistant clinical professor of medicine, University of California San Francisco Medical Center
Applications are submitted online (www.hospitalmedicine.org/boost) and evaluated based on whether improving discharge and care transitions is a high priority at the institution. Applications must be accompanied by a letter of support from an executive sponsor within the applicant’s hospital.
Once accepted into the program, BOOST participants pay a tuition fee of $28,000. Thanks to the support of the California HealthCare Foundation, the L.A. Care Health Plan, and the Hospital Association of Southern California, sites in California are eligible for reduced tuition based on site location and availability of funds.
For Dr. Rennke, the link between healthcare reform and readmissions is clear, along with the repercussions for hospitals. Most notably, the discharge process affects multiple quality issues, including “patient satisfaction, provider satisfaction and improving communication from hospital to home.”
“Hospitals need to realize healthcare reform is coming,” says Dr. Rennke, who previously served as a Project BOOST site team member and now works as a BOOST mentor. “Not only is reducing readmissions the right thing to do, it will also have a financial impact for hospitals that don’t address it. … It’s going to be of paramount importance to address the discharge process.”
National Growth
Since it was initially developed through a grant from the John A. Hartford Foundation, Project BOOST has spread to hospitals across the country and received widespread attention throughout the healthcare community.
At the time of Project BOOST’s inception in 2008, readmissions already were an intractable and costly issue for hospitals. The next year, research coauthored by Project BOOST principal investigator Mark V. Williams, MD, FHM, and published in the New England Journal of Medicine revealed that unplanned readmissions cost Medicare $17.4 billion annually.
Project BOOST’s pilot cohort consisted of six hospital sites. The program’s growth accelerated quickly, and it soon added another 24 sites and, later, two statewide programs in Michigan and Illinois.
The popularity of Project BOOST among hospitals has captured the attention of media and other organizations as well:
- This year, Kaiser Health News featured the work of Atlanta’s Piedmont Hospital to reduce readmissions using Project BOOST in an article focusing on the impact of healthcare reform laws on hospital readmissions.
- The Bassett Healthcare Network, a Project BOOST site in upstate New York, has earned the Hospital Association of New York State’s prestigious 2011 HANYS Pinnacle Award for Quality and Safety for the group’s care-transition work. The award was presented to Bassett Healthcare Network chief executives in June.
- In California, the Kaiser Permanente West LA BOOST Team was recognized with an award from Dr. Benjamin Chu, president of Southern California Kaiser Foundation Health Plan.
- In December 2010, Dr. Williams and hospitalist Matthew Schreiber, CMO of Piedmont Hospital, shared their experiences with Project BOOST at a national conference hosted by the Centers for Medicare & Medicaid Services (CMS).
The Project BOOST Process
Once a site is accepted as a Project BOOST site, the site leader receives an information package and access to the Project BOOST online repository for recording and uploading readmission data. Then, each Project BOOST cohort performs an in-person conference. Networking and personal interaction are an important part of sharing challenges and successes in reducing readmissions. The conference also includes training on root-cause analysis and process mapping, a required step for application of the new Community Based Care Transitions Program (CCTP), part of the Affordable Care Act.
Each site leader is assigned a Project BOOST mentor, a national expert on reducing readmissions to the hospital. The mentor conducts a site visit to the hospital to meet the entire team in person and better understand the discharge challenges first-hand.
Over the course of the year, through regularly scheduled telephone calls, the mentor works with the Project BOOST team to best apply the program to the needs of the specific hospital. Mentors also help answer questions related to project planning, toolkit materials, data collection, implementation, and analysis.
In Dr. Rennke’s case, the process helped augment and guide UCSF’s current discharge program. Having multiple team members from different disciplines made distributing the work and implementation easier.
“Overall, we knew this was going to be doable because we incorporated Project BOOST into an already existing discharge process,” Dr. Rennke says.
Readmissions in the Crosshairs
The impacts of preventable readmissions on patient safety and efficiency of care in the hospital have made the issue a heated one in public policy. Earlier this year, the U.S. Department of Health and Human Services announced the creation of Partnership for Patients, a $1 billion initiative to address “quality, safety, and affordability of healthcare for all Americans.” SHM was one of the first medical societies to sign on to the “Partnership for Patients Pledge.”
One of the partnership’s two major goals is to reduce hospital readmissions by 20%. According to the Partnership for Patients website, “achieving this goal would mean more than 1.6 million patients would recover from illness without suffering a preventable complication requiring rehospitalization within 30 days of discharge.”
The government is backing up this goal with funding for hospitals with concrete plans to reduce readmissions. Under the Affordable Care Act of 2010—commonly known as the healthcare reform law—Medicare created the five-year CCTP earlier this year. The program provides $500 million to collaborative partnerships between hospitals and community-based organizations to implement care-transition services for Medicare beneficiaries, many of whom are at high risk of readmission.
To Dr. Rennke, the attention to reducing readmissions is an extension of her responsibility as a caregiver. “Our responsibility doesn’t end when the patient leaves the hospital,” she says. TH
Brendon Shank is SHM’s assistant vice president of communications.
If you’re a hospitalist interested in reducing readmissions in your hospital, the time to act is now.
Project BOOST (Better Outcomes for Older Adults through Safe Transitions), SHM’s groundbreaking program designed to help hospitals reduce unplanned readmissions, is now accepting applications for two new cohorts: one national and another specific to California. The deadline for applications is August 1.
Now with 85 sites as part of the national community, Project BOOST will introduce new sites across the country in the fall. In addition to the national cohort, Project BOOST will also establish a new cohort in California, with discounted tuition through grants from three healthcare groups in the state.
“It’s a great time to apply,” says Stephanie Rennke, MD, assistant clinical professor of medicine at the University of California San Francisco Medical Center. “We are at the cusp of a lot of big changes in health reform. The time to address readmissions is now. Hospitals will have to address this, and BOOST is one way to do that.”

—Stephanie Rennke, MD, assistant clinical professor of medicine, University of California San Francisco Medical Center
Applications are submitted online (www.hospitalmedicine.org/boost) and evaluated based on whether improving discharge and care transitions is a high priority at the institution. Applications must be accompanied by a letter of support from an executive sponsor within the applicant’s hospital.
Once accepted into the program, BOOST participants pay a tuition fee of $28,000. Thanks to the support of the California HealthCare Foundation, the L.A. Care Health Plan, and the Hospital Association of Southern California, sites in California are eligible for reduced tuition based on site location and availability of funds.
For Dr. Rennke, the link between healthcare reform and readmissions is clear, along with the repercussions for hospitals. Most notably, the discharge process affects multiple quality issues, including “patient satisfaction, provider satisfaction and improving communication from hospital to home.”
“Hospitals need to realize healthcare reform is coming,” says Dr. Rennke, who previously served as a Project BOOST site team member and now works as a BOOST mentor. “Not only is reducing readmissions the right thing to do, it will also have a financial impact for hospitals that don’t address it. … It’s going to be of paramount importance to address the discharge process.”
National Growth
Since it was initially developed through a grant from the John A. Hartford Foundation, Project BOOST has spread to hospitals across the country and received widespread attention throughout the healthcare community.
At the time of Project BOOST’s inception in 2008, readmissions already were an intractable and costly issue for hospitals. The next year, research coauthored by Project BOOST principal investigator Mark V. Williams, MD, FHM, and published in the New England Journal of Medicine revealed that unplanned readmissions cost Medicare $17.4 billion annually.
Project BOOST’s pilot cohort consisted of six hospital sites. The program’s growth accelerated quickly, and it soon added another 24 sites and, later, two statewide programs in Michigan and Illinois.
The popularity of Project BOOST among hospitals has captured the attention of media and other organizations as well:
- This year, Kaiser Health News featured the work of Atlanta’s Piedmont Hospital to reduce readmissions using Project BOOST in an article focusing on the impact of healthcare reform laws on hospital readmissions.
- The Bassett Healthcare Network, a Project BOOST site in upstate New York, has earned the Hospital Association of New York State’s prestigious 2011 HANYS Pinnacle Award for Quality and Safety for the group’s care-transition work. The award was presented to Bassett Healthcare Network chief executives in June.
- In California, the Kaiser Permanente West LA BOOST Team was recognized with an award from Dr. Benjamin Chu, president of Southern California Kaiser Foundation Health Plan.
- In December 2010, Dr. Williams and hospitalist Matthew Schreiber, CMO of Piedmont Hospital, shared their experiences with Project BOOST at a national conference hosted by the Centers for Medicare & Medicaid Services (CMS).
The Project BOOST Process
Once a site is accepted as a Project BOOST site, the site leader receives an information package and access to the Project BOOST online repository for recording and uploading readmission data. Then, each Project BOOST cohort performs an in-person conference. Networking and personal interaction are an important part of sharing challenges and successes in reducing readmissions. The conference also includes training on root-cause analysis and process mapping, a required step for application of the new Community Based Care Transitions Program (CCTP), part of the Affordable Care Act.
Each site leader is assigned a Project BOOST mentor, a national expert on reducing readmissions to the hospital. The mentor conducts a site visit to the hospital to meet the entire team in person and better understand the discharge challenges first-hand.
Over the course of the year, through regularly scheduled telephone calls, the mentor works with the Project BOOST team to best apply the program to the needs of the specific hospital. Mentors also help answer questions related to project planning, toolkit materials, data collection, implementation, and analysis.
In Dr. Rennke’s case, the process helped augment and guide UCSF’s current discharge program. Having multiple team members from different disciplines made distributing the work and implementation easier.
“Overall, we knew this was going to be doable because we incorporated Project BOOST into an already existing discharge process,” Dr. Rennke says.
Readmissions in the Crosshairs
The impacts of preventable readmissions on patient safety and efficiency of care in the hospital have made the issue a heated one in public policy. Earlier this year, the U.S. Department of Health and Human Services announced the creation of Partnership for Patients, a $1 billion initiative to address “quality, safety, and affordability of healthcare for all Americans.” SHM was one of the first medical societies to sign on to the “Partnership for Patients Pledge.”
One of the partnership’s two major goals is to reduce hospital readmissions by 20%. According to the Partnership for Patients website, “achieving this goal would mean more than 1.6 million patients would recover from illness without suffering a preventable complication requiring rehospitalization within 30 days of discharge.”
The government is backing up this goal with funding for hospitals with concrete plans to reduce readmissions. Under the Affordable Care Act of 2010—commonly known as the healthcare reform law—Medicare created the five-year CCTP earlier this year. The program provides $500 million to collaborative partnerships between hospitals and community-based organizations to implement care-transition services for Medicare beneficiaries, many of whom are at high risk of readmission.
To Dr. Rennke, the attention to reducing readmissions is an extension of her responsibility as a caregiver. “Our responsibility doesn’t end when the patient leaves the hospital,” she says. TH
Brendon Shank is SHM’s assistant vice president of communications.
If you’re a hospitalist interested in reducing readmissions in your hospital, the time to act is now.
Project BOOST (Better Outcomes for Older Adults through Safe Transitions), SHM’s groundbreaking program designed to help hospitals reduce unplanned readmissions, is now accepting applications for two new cohorts: one national and another specific to California. The deadline for applications is August 1.
Now with 85 sites as part of the national community, Project BOOST will introduce new sites across the country in the fall. In addition to the national cohort, Project BOOST will also establish a new cohort in California, with discounted tuition through grants from three healthcare groups in the state.
“It’s a great time to apply,” says Stephanie Rennke, MD, assistant clinical professor of medicine at the University of California San Francisco Medical Center. “We are at the cusp of a lot of big changes in health reform. The time to address readmissions is now. Hospitals will have to address this, and BOOST is one way to do that.”

—Stephanie Rennke, MD, assistant clinical professor of medicine, University of California San Francisco Medical Center
Applications are submitted online (www.hospitalmedicine.org/boost) and evaluated based on whether improving discharge and care transitions is a high priority at the institution. Applications must be accompanied by a letter of support from an executive sponsor within the applicant’s hospital.
Once accepted into the program, BOOST participants pay a tuition fee of $28,000. Thanks to the support of the California HealthCare Foundation, the L.A. Care Health Plan, and the Hospital Association of Southern California, sites in California are eligible for reduced tuition based on site location and availability of funds.
For Dr. Rennke, the link between healthcare reform and readmissions is clear, along with the repercussions for hospitals. Most notably, the discharge process affects multiple quality issues, including “patient satisfaction, provider satisfaction and improving communication from hospital to home.”
“Hospitals need to realize healthcare reform is coming,” says Dr. Rennke, who previously served as a Project BOOST site team member and now works as a BOOST mentor. “Not only is reducing readmissions the right thing to do, it will also have a financial impact for hospitals that don’t address it. … It’s going to be of paramount importance to address the discharge process.”
National Growth
Since it was initially developed through a grant from the John A. Hartford Foundation, Project BOOST has spread to hospitals across the country and received widespread attention throughout the healthcare community.
At the time of Project BOOST’s inception in 2008, readmissions already were an intractable and costly issue for hospitals. The next year, research coauthored by Project BOOST principal investigator Mark V. Williams, MD, FHM, and published in the New England Journal of Medicine revealed that unplanned readmissions cost Medicare $17.4 billion annually.
Project BOOST’s pilot cohort consisted of six hospital sites. The program’s growth accelerated quickly, and it soon added another 24 sites and, later, two statewide programs in Michigan and Illinois.
The popularity of Project BOOST among hospitals has captured the attention of media and other organizations as well:
- This year, Kaiser Health News featured the work of Atlanta’s Piedmont Hospital to reduce readmissions using Project BOOST in an article focusing on the impact of healthcare reform laws on hospital readmissions.
- The Bassett Healthcare Network, a Project BOOST site in upstate New York, has earned the Hospital Association of New York State’s prestigious 2011 HANYS Pinnacle Award for Quality and Safety for the group’s care-transition work. The award was presented to Bassett Healthcare Network chief executives in June.
- In California, the Kaiser Permanente West LA BOOST Team was recognized with an award from Dr. Benjamin Chu, president of Southern California Kaiser Foundation Health Plan.
- In December 2010, Dr. Williams and hospitalist Matthew Schreiber, CMO of Piedmont Hospital, shared their experiences with Project BOOST at a national conference hosted by the Centers for Medicare & Medicaid Services (CMS).
The Project BOOST Process
Once a site is accepted as a Project BOOST site, the site leader receives an information package and access to the Project BOOST online repository for recording and uploading readmission data. Then, each Project BOOST cohort performs an in-person conference. Networking and personal interaction are an important part of sharing challenges and successes in reducing readmissions. The conference also includes training on root-cause analysis and process mapping, a required step for application of the new Community Based Care Transitions Program (CCTP), part of the Affordable Care Act.
Each site leader is assigned a Project BOOST mentor, a national expert on reducing readmissions to the hospital. The mentor conducts a site visit to the hospital to meet the entire team in person and better understand the discharge challenges first-hand.
Over the course of the year, through regularly scheduled telephone calls, the mentor works with the Project BOOST team to best apply the program to the needs of the specific hospital. Mentors also help answer questions related to project planning, toolkit materials, data collection, implementation, and analysis.
In Dr. Rennke’s case, the process helped augment and guide UCSF’s current discharge program. Having multiple team members from different disciplines made distributing the work and implementation easier.
“Overall, we knew this was going to be doable because we incorporated Project BOOST into an already existing discharge process,” Dr. Rennke says.
Readmissions in the Crosshairs
The impacts of preventable readmissions on patient safety and efficiency of care in the hospital have made the issue a heated one in public policy. Earlier this year, the U.S. Department of Health and Human Services announced the creation of Partnership for Patients, a $1 billion initiative to address “quality, safety, and affordability of healthcare for all Americans.” SHM was one of the first medical societies to sign on to the “Partnership for Patients Pledge.”
One of the partnership’s two major goals is to reduce hospital readmissions by 20%. According to the Partnership for Patients website, “achieving this goal would mean more than 1.6 million patients would recover from illness without suffering a preventable complication requiring rehospitalization within 30 days of discharge.”
The government is backing up this goal with funding for hospitals with concrete plans to reduce readmissions. Under the Affordable Care Act of 2010—commonly known as the healthcare reform law—Medicare created the five-year CCTP earlier this year. The program provides $500 million to collaborative partnerships between hospitals and community-based organizations to implement care-transition services for Medicare beneficiaries, many of whom are at high risk of readmission.
To Dr. Rennke, the attention to reducing readmissions is an extension of her responsibility as a caregiver. “Our responsibility doesn’t end when the patient leaves the hospital,” she says. TH
Brendon Shank is SHM’s assistant vice president of communications.
Virtual Mentorship
With more than 250 hospitals adopting them in the last three years, SHM’s mentored implementation programs make a compelling case for the need to address care transitions, improve the management of diabetes, and prevent VTEs in hospitalized patients. And early results from the sites show that the mentored implementation model, with its combination of a best-practices toolkit and individualized support from national experts, can make a real difference.
“Quality improvement (QI) is the niche of hospital medicine; our mentored implementation programs have achieved both the goals of improving care in a clinical area nationwide as well as creating quality improvement leaders within our ranks,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, associate professor of medicine and hospital medicine section chief at the University of New Mexico Health Sciences Center’s Department of Internal Medicine.
That’s the reasoning behind SHM’s new eQUIPS program. In essence, eQUIPS (Electronic Quality Improvement Programs) is SHM’s proven mentored implementation program, but without the mentor. Participants can access the same educational tools and resources, the same data center for tracking performance, and participate in the same online collaborative available to mentored implementation sites.

“SHM’s eQUIPS program takes the collective knowledge from the programs and offers it as a self-guided program that includes robust data collection and display programs,” Dr. Rogers says. “It will allow hospital quality-improvement teams more time to focus on driving change through the effective use of data, rather than spending their time trying to get the data.”
eQUIPS empowers hospitalists to move forward on valuable QI programs at their own pace, at any time. Hospitalists begin with the confidence that an entire community of likeminded physicians is supporting them, sharing their information, challenges, and successes.
Now, hospitalists can bring best practices to their hospitals and show their directors and executive leadership that they are on the cutting edge of addressing some of the most pervasive challenges in today’s hospitals.
Although they share a similar approach, each of eQUIPS’ three programs tackles the individual challenges of care transitions, VTE, and glycemic control separately. Hospitals can subscribe to any combination of the three topics.
Because eQUIPS is meant for year-after-year use and designed so that its utility grows along with its user base, access to eQUIPS is based on a yearly subscription model. The first year of access to eQUIPS is $2,500, which includes a one-time technology start-up fee. Each following year’s subscription is $1,500.
Hospitalists can apply for eQUIPS at www.hospitalmedicine.org/equips.
Educational Resources Get eQUIPS Users Started
Regardless of how far a hospital has advanced its programs, the educational materials that come with the subscription take hospitalists through the best in evidence-based medicine to address care transitions, VTE, and glycemic control, essentially forming a toolkit of relevant journal articles, presentations, step-by-step implementation guides, clinical tools, program files submitted by participants, and on-demand educational webinars facilitated by content experts.
Analysis and Reporting
Most experts agree that tracking and reporting results are the linchpins of QI programs. eQUIPS makes it easier with secure online tools for recording, benchmarking, process management, and tracking milestones.
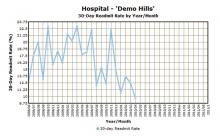
Plus, eQUIPS enables hospitalists to compare their programs to others across the country. By uploading performance data to the secure eQUIPS data center for performance tracking, hospitals can analyze and compare outcomes from their programs to other eQUIPS sites and national norms (see Figure 1).
And hospitalists can assure their hospitals’ legal staffs that SHM has taken steps to ensure HIPAA compliance through third-party reviews. eQUIPS subscribers log into the site through a secured-password authentication similar to those of other online public health and financial institutions. In addition, SHM’s QI programs have earned the Patient Safety Organization (PSO) designation from the Agency for Healthcare Research and Quality (AHRQ), which makes it easier for hospitals to share performance data with SHM.
Real-Time Collaboration
Every hospital faces unique challenges, but they also have much in common when it comes to implementing new programs. As eQUIPS subscribers join, they can share their QI experiences and ask others for feedback in finding solutions.
The eQUIPS community website feature serves as a central, on-demand repository for sharing documents and educational materials, while the online workspace enables hospitalists to collaborate in real time by posting documents and editing them with other participating eQUIPS sites.
eQUIPS also brings collaboration right to users’ inboxes. Access to QI listservs has been a productive way for hospitalists to connect and benefit from the collective experience of the group; it’s a key component of the eQUIPS programs.
For Rogers, eQUIPS and its collaborative tools are a logistical extension of SHM’s successful QI track record. TH
Brendon Shank is assistant vice president of communications for SHM.
With more than 250 hospitals adopting them in the last three years, SHM’s mentored implementation programs make a compelling case for the need to address care transitions, improve the management of diabetes, and prevent VTEs in hospitalized patients. And early results from the sites show that the mentored implementation model, with its combination of a best-practices toolkit and individualized support from national experts, can make a real difference.
“Quality improvement (QI) is the niche of hospital medicine; our mentored implementation programs have achieved both the goals of improving care in a clinical area nationwide as well as creating quality improvement leaders within our ranks,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, associate professor of medicine and hospital medicine section chief at the University of New Mexico Health Sciences Center’s Department of Internal Medicine.
That’s the reasoning behind SHM’s new eQUIPS program. In essence, eQUIPS (Electronic Quality Improvement Programs) is SHM’s proven mentored implementation program, but without the mentor. Participants can access the same educational tools and resources, the same data center for tracking performance, and participate in the same online collaborative available to mentored implementation sites.

“SHM’s eQUIPS program takes the collective knowledge from the programs and offers it as a self-guided program that includes robust data collection and display programs,” Dr. Rogers says. “It will allow hospital quality-improvement teams more time to focus on driving change through the effective use of data, rather than spending their time trying to get the data.”
eQUIPS empowers hospitalists to move forward on valuable QI programs at their own pace, at any time. Hospitalists begin with the confidence that an entire community of likeminded physicians is supporting them, sharing their information, challenges, and successes.
Now, hospitalists can bring best practices to their hospitals and show their directors and executive leadership that they are on the cutting edge of addressing some of the most pervasive challenges in today’s hospitals.
Although they share a similar approach, each of eQUIPS’ three programs tackles the individual challenges of care transitions, VTE, and glycemic control separately. Hospitals can subscribe to any combination of the three topics.
Because eQUIPS is meant for year-after-year use and designed so that its utility grows along with its user base, access to eQUIPS is based on a yearly subscription model. The first year of access to eQUIPS is $2,500, which includes a one-time technology start-up fee. Each following year’s subscription is $1,500.
Hospitalists can apply for eQUIPS at www.hospitalmedicine.org/equips.
Educational Resources Get eQUIPS Users Started
Regardless of how far a hospital has advanced its programs, the educational materials that come with the subscription take hospitalists through the best in evidence-based medicine to address care transitions, VTE, and glycemic control, essentially forming a toolkit of relevant journal articles, presentations, step-by-step implementation guides, clinical tools, program files submitted by participants, and on-demand educational webinars facilitated by content experts.
Analysis and Reporting
Most experts agree that tracking and reporting results are the linchpins of QI programs. eQUIPS makes it easier with secure online tools for recording, benchmarking, process management, and tracking milestones.
Plus, eQUIPS enables hospitalists to compare their programs to others across the country. By uploading performance data to the secure eQUIPS data center for performance tracking, hospitals can analyze and compare outcomes from their programs to other eQUIPS sites and national norms (see Figure 1).
And hospitalists can assure their hospitals’ legal staffs that SHM has taken steps to ensure HIPAA compliance through third-party reviews. eQUIPS subscribers log into the site through a secured-password authentication similar to those of other online public health and financial institutions. In addition, SHM’s QI programs have earned the Patient Safety Organization (PSO) designation from the Agency for Healthcare Research and Quality (AHRQ), which makes it easier for hospitals to share performance data with SHM.
Real-Time Collaboration
Every hospital faces unique challenges, but they also have much in common when it comes to implementing new programs. As eQUIPS subscribers join, they can share their QI experiences and ask others for feedback in finding solutions.
The eQUIPS community website feature serves as a central, on-demand repository for sharing documents and educational materials, while the online workspace enables hospitalists to collaborate in real time by posting documents and editing them with other participating eQUIPS sites.
eQUIPS also brings collaboration right to users’ inboxes. Access to QI listservs has been a productive way for hospitalists to connect and benefit from the collective experience of the group; it’s a key component of the eQUIPS programs.
For Rogers, eQUIPS and its collaborative tools are a logistical extension of SHM’s successful QI track record. TH
Brendon Shank is assistant vice president of communications for SHM.
With more than 250 hospitals adopting them in the last three years, SHM’s mentored implementation programs make a compelling case for the need to address care transitions, improve the management of diabetes, and prevent VTEs in hospitalized patients. And early results from the sites show that the mentored implementation model, with its combination of a best-practices toolkit and individualized support from national experts, can make a real difference.
“Quality improvement (QI) is the niche of hospital medicine; our mentored implementation programs have achieved both the goals of improving care in a clinical area nationwide as well as creating quality improvement leaders within our ranks,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, associate professor of medicine and hospital medicine section chief at the University of New Mexico Health Sciences Center’s Department of Internal Medicine.
That’s the reasoning behind SHM’s new eQUIPS program. In essence, eQUIPS (Electronic Quality Improvement Programs) is SHM’s proven mentored implementation program, but without the mentor. Participants can access the same educational tools and resources, the same data center for tracking performance, and participate in the same online collaborative available to mentored implementation sites.

“SHM’s eQUIPS program takes the collective knowledge from the programs and offers it as a self-guided program that includes robust data collection and display programs,” Dr. Rogers says. “It will allow hospital quality-improvement teams more time to focus on driving change through the effective use of data, rather than spending their time trying to get the data.”
eQUIPS empowers hospitalists to move forward on valuable QI programs at their own pace, at any time. Hospitalists begin with the confidence that an entire community of likeminded physicians is supporting them, sharing their information, challenges, and successes.
Now, hospitalists can bring best practices to their hospitals and show their directors and executive leadership that they are on the cutting edge of addressing some of the most pervasive challenges in today’s hospitals.
Although they share a similar approach, each of eQUIPS’ three programs tackles the individual challenges of care transitions, VTE, and glycemic control separately. Hospitals can subscribe to any combination of the three topics.
Because eQUIPS is meant for year-after-year use and designed so that its utility grows along with its user base, access to eQUIPS is based on a yearly subscription model. The first year of access to eQUIPS is $2,500, which includes a one-time technology start-up fee. Each following year’s subscription is $1,500.
Hospitalists can apply for eQUIPS at www.hospitalmedicine.org/equips.
Educational Resources Get eQUIPS Users Started
Regardless of how far a hospital has advanced its programs, the educational materials that come with the subscription take hospitalists through the best in evidence-based medicine to address care transitions, VTE, and glycemic control, essentially forming a toolkit of relevant journal articles, presentations, step-by-step implementation guides, clinical tools, program files submitted by participants, and on-demand educational webinars facilitated by content experts.
Analysis and Reporting
Most experts agree that tracking and reporting results are the linchpins of QI programs. eQUIPS makes it easier with secure online tools for recording, benchmarking, process management, and tracking milestones.
Plus, eQUIPS enables hospitalists to compare their programs to others across the country. By uploading performance data to the secure eQUIPS data center for performance tracking, hospitals can analyze and compare outcomes from their programs to other eQUIPS sites and national norms (see Figure 1).
And hospitalists can assure their hospitals’ legal staffs that SHM has taken steps to ensure HIPAA compliance through third-party reviews. eQUIPS subscribers log into the site through a secured-password authentication similar to those of other online public health and financial institutions. In addition, SHM’s QI programs have earned the Patient Safety Organization (PSO) designation from the Agency for Healthcare Research and Quality (AHRQ), which makes it easier for hospitals to share performance data with SHM.
Real-Time Collaboration
Every hospital faces unique challenges, but they also have much in common when it comes to implementing new programs. As eQUIPS subscribers join, they can share their QI experiences and ask others for feedback in finding solutions.
The eQUIPS community website feature serves as a central, on-demand repository for sharing documents and educational materials, while the online workspace enables hospitalists to collaborate in real time by posting documents and editing them with other participating eQUIPS sites.
eQUIPS also brings collaboration right to users’ inboxes. Access to QI listservs has been a productive way for hospitalists to connect and benefit from the collective experience of the group; it’s a key component of the eQUIPS programs.
For Rogers, eQUIPS and its collaborative tools are a logistical extension of SHM’s successful QI track record. TH
Brendon Shank is assistant vice president of communications for SHM.
NEW SHM MEMBERS: May 2011
Enter text here
Enter text here
Enter text here
Pediatric Palooza
As a specialty within the broader field of HM, pediatric HM (PHM) has a dedicated and active following. That devotion is apparent at its annual meeting, to be held this year July 27-31 in Kansas City, Mo. The conference is cosponsored by SHM, the American Academy of Pediatrics (AAP), the AAP Section on Hospital Medicine (SOHM), and the Academic Pediatric Association (APA).
Pediatric hospitalists can register though the “Events” section at www.hospitalmedicine.org. Fees for SHM, AAP, and APA members who register before June 30 are $650. After June 30, rates increase to $700. Discounts are available for residents.
Jack Percelay, MD, SFHM, has been to almost every PHM annual meeting since the event began in 1998. He continually is impressed with the increase in stature, quality, and community at each meeting.

“These meetings have been absolutely stupendous,” says Dr. Percelay, MD, SFHM, pediatric hospitalist at Hunterdon Medical Center in New York City. “This is our fifth consecutive year and each one has been bigger and better than the one before. Previous years have sold out early, so it’s important to register and book a hotel early. And I hear the barbecue is good in Kansas City, too.”
Whether it’s the opportunity to network with other hospitalists dedicated to caring for children, the importance of the discussions, or the smoked ribs, PHM has become a draw—not just for pediatric hospitalists, but also for high-profile speakers.
This year’s keynote speaker—Carolyn Clancy, MD, director of the Agency for Healthcare Research and Quality (AHRQ)—will be especially timely. With the continued public dialogue surrounding the role of hospitals—and hospitalists—in the Affordable Care Act (known widely as the health reform law), Dr. Clancy’s presentation will help link the day-to-day work of pediatric hospitalists to the long-term changes they can expect in their hospitals.
For Dr. Percelay, the annual meeting for pediatric hospitalists is still about the people who attend and helping each other in a growing specialty.
“We’re young enough as a field that this is a great way to make established personal connections,” he says. “You can approach people and connect a face to an email and get more involved.
“If you haven’t been to one of these before and your program is struggling with infectious-disease issues, or you don’t know what else is out there, networking helps to define the potential in terms of growing program. If you’re a growing program, it’s much easier to copy an example than to invent a program anew. We share very well, so there are opportunities at all levels.”
In addition to the people, of course, there are opportunities for educational and professional development, including two clinical tracks, a track for educators, and three separate tracks for practice management, quality, and research. The schedule also features a “potpourri” track, which will offer topics on PHM programs in community hospitals, ultrasound, and hunger, homelessness, and violence. TH
Brendon Shank is SHM’s assistant vice president of communications.
As a specialty within the broader field of HM, pediatric HM (PHM) has a dedicated and active following. That devotion is apparent at its annual meeting, to be held this year July 27-31 in Kansas City, Mo. The conference is cosponsored by SHM, the American Academy of Pediatrics (AAP), the AAP Section on Hospital Medicine (SOHM), and the Academic Pediatric Association (APA).
Pediatric hospitalists can register though the “Events” section at www.hospitalmedicine.org. Fees for SHM, AAP, and APA members who register before June 30 are $650. After June 30, rates increase to $700. Discounts are available for residents.
Jack Percelay, MD, SFHM, has been to almost every PHM annual meeting since the event began in 1998. He continually is impressed with the increase in stature, quality, and community at each meeting.

“These meetings have been absolutely stupendous,” says Dr. Percelay, MD, SFHM, pediatric hospitalist at Hunterdon Medical Center in New York City. “This is our fifth consecutive year and each one has been bigger and better than the one before. Previous years have sold out early, so it’s important to register and book a hotel early. And I hear the barbecue is good in Kansas City, too.”
Whether it’s the opportunity to network with other hospitalists dedicated to caring for children, the importance of the discussions, or the smoked ribs, PHM has become a draw—not just for pediatric hospitalists, but also for high-profile speakers.
This year’s keynote speaker—Carolyn Clancy, MD, director of the Agency for Healthcare Research and Quality (AHRQ)—will be especially timely. With the continued public dialogue surrounding the role of hospitals—and hospitalists—in the Affordable Care Act (known widely as the health reform law), Dr. Clancy’s presentation will help link the day-to-day work of pediatric hospitalists to the long-term changes they can expect in their hospitals.
For Dr. Percelay, the annual meeting for pediatric hospitalists is still about the people who attend and helping each other in a growing specialty.
“We’re young enough as a field that this is a great way to make established personal connections,” he says. “You can approach people and connect a face to an email and get more involved.
“If you haven’t been to one of these before and your program is struggling with infectious-disease issues, or you don’t know what else is out there, networking helps to define the potential in terms of growing program. If you’re a growing program, it’s much easier to copy an example than to invent a program anew. We share very well, so there are opportunities at all levels.”
In addition to the people, of course, there are opportunities for educational and professional development, including two clinical tracks, a track for educators, and three separate tracks for practice management, quality, and research. The schedule also features a “potpourri” track, which will offer topics on PHM programs in community hospitals, ultrasound, and hunger, homelessness, and violence. TH
Brendon Shank is SHM’s assistant vice president of communications.
As a specialty within the broader field of HM, pediatric HM (PHM) has a dedicated and active following. That devotion is apparent at its annual meeting, to be held this year July 27-31 in Kansas City, Mo. The conference is cosponsored by SHM, the American Academy of Pediatrics (AAP), the AAP Section on Hospital Medicine (SOHM), and the Academic Pediatric Association (APA).
Pediatric hospitalists can register though the “Events” section at www.hospitalmedicine.org. Fees for SHM, AAP, and APA members who register before June 30 are $650. After June 30, rates increase to $700. Discounts are available for residents.
Jack Percelay, MD, SFHM, has been to almost every PHM annual meeting since the event began in 1998. He continually is impressed with the increase in stature, quality, and community at each meeting.

“These meetings have been absolutely stupendous,” says Dr. Percelay, MD, SFHM, pediatric hospitalist at Hunterdon Medical Center in New York City. “This is our fifth consecutive year and each one has been bigger and better than the one before. Previous years have sold out early, so it’s important to register and book a hotel early. And I hear the barbecue is good in Kansas City, too.”
Whether it’s the opportunity to network with other hospitalists dedicated to caring for children, the importance of the discussions, or the smoked ribs, PHM has become a draw—not just for pediatric hospitalists, but also for high-profile speakers.
This year’s keynote speaker—Carolyn Clancy, MD, director of the Agency for Healthcare Research and Quality (AHRQ)—will be especially timely. With the continued public dialogue surrounding the role of hospitals—and hospitalists—in the Affordable Care Act (known widely as the health reform law), Dr. Clancy’s presentation will help link the day-to-day work of pediatric hospitalists to the long-term changes they can expect in their hospitals.
For Dr. Percelay, the annual meeting for pediatric hospitalists is still about the people who attend and helping each other in a growing specialty.
“We’re young enough as a field that this is a great way to make established personal connections,” he says. “You can approach people and connect a face to an email and get more involved.
“If you haven’t been to one of these before and your program is struggling with infectious-disease issues, or you don’t know what else is out there, networking helps to define the potential in terms of growing program. If you’re a growing program, it’s much easier to copy an example than to invent a program anew. We share very well, so there are opportunities at all levels.”
In addition to the people, of course, there are opportunities for educational and professional development, including two clinical tracks, a track for educators, and three separate tracks for practice management, quality, and research. The schedule also features a “potpourri” track, which will offer topics on PHM programs in community hospitals, ultrasound, and hunger, homelessness, and violence. TH
Brendon Shank is SHM’s assistant vice president of communications.
HM11 PREVIEW: Insider’s Viewpoint
Robert Kocher, MD, is not a household name for hospitalists who aren’t policy wonks. That’s not to say he shouldn’t be.
Dr. Kocher, a former special assistant to President Obama on healthcare and economic policy who is now the director of the McKinsey Center for U.S. Health System Reform in Washington, D.C., was a behind-the-scenes player in the landmark healthcare reform legislation signed into law last year. After a two-year stint in the White House, he transitioned back to the private sector late in 2010, landing at McKinsey & Co., a powerhouse consulting firm in the nation’s capital.
On May 11, Dr. Kocher will give HM11’s first keynote speech, “Coming to Your Hospital: Healthcare Reform. What Does This Mean for Hospitalists.” His talk will be an inside look at how the reform package came together and point out how hospitalists can be “the solution that hospitals will want to deploy to allow them to capitalize” on reform.
“Instead of hospitalists being a de facto link [between different departments of a given hospital], I think hospitalists will be a value-creating link,” Dr. Kocher says. “There’s going to be much more information that’s going to have to flow between the inpatient side and the outpatient side if you’re going to manage population health and lower per capita costs. … It’s going to require more specialization, which hospitalists are in the right position to really take on and to deliver.”
Dr. Kocher (pronounced “coacher”) joined the reform fight in January 2009, taking a post at the National Economic Council as special assistant to the president for healthcare. He left that job last fall and rejoined McKinsey, the firm he had been with for seven years before joining the Obama administration. His career began with a medical degree from George Washington University and internal-medicine residency at Beth Israel Deaconess Medical Center in Boston.

He followed that with a stint as a clinical fellow and instructor at Harvard Medical School. In addition to his role as a principal at McKinsey, Dr. Kocher is a nonresident senior fellow at the Brookings Institution Engleberg Center for Health Reform.
He is a well-known speaker on healthcare topics and a frequent writer who has authored pieces for major outlets, including the New England Journal of Medicine, the Washington Post and The New York Times. The White House last year filmed him as part of its “Reality Check” Web series (www.whitehouse.gov/realitycheck/31), which is aimed at “debunking the myths” swirling around reform.
Dr. Kocher says all of his career stops pale in comparison to being part of once-in-a-generation talks that shaped the future of U.S. healthcare.
“Certainly, [it was] the most impactful thing I’ll ever get to actually do, because we were able to shape the lasting policies that will change the way healthcare is delivered for years to come,” he says. “It was an incredible privilege to get to observe and take part in that policy-making process and understand that some compromises have to happen to make successful legislation.”
Brendon Shank, SHM’s assistant vice president of communications, says that having a White House participant in the reform negotiations as a featured speaker is a treat for hospitalists.
“This is exciting because it’s someone who helped define policy,” Shank says. “This is someone who knows the inside of it. He’s been in the room for discussions that will affect hospitalists for years down the road.”
Exactly what those effects will be will take time to understand. But Dr. Kocher sees reform as a chance for HM to make itself indispensable to hospitals looking to improve quality, efficiency, and transitional-care outcomes.
More HM11 Preview
HM11’s visiting professor to serve as mentor, stimulate discussion
Hospitalists come from all walks; HM11 has a place for all of them
HM11 attendees can earn as many as 18.75 CME credits
Industry pioneer recounts HM’s meteoric rise, sees bright future for hospitalists
Lots to See, Lots to Do in ‘Big D’
From sports to culture to Tex-Mex, Dallas metroplex has something for every visitor
You may also
HM11 PREVIEW SUPPLEMENT
in pdf format.
The responsibility will, of course, come with the challenge of actually proving that HM can deliver on the pledge of better care at better prices.
“For hospitals, as the payment system evolves and matures, we’re going to be paying more often for outcomes,” Dr. Kocher says. “That change is going to require hospitalists to become much more reliable.
“It’s a more specialized skill that doctors who are part-time hospital doctors are going to have a hard time developing. It clearly makes the system more dependent on hospitalists. … That said, I think that it’s the responsibility of hospitalists to prove they can deliver.”
Dr. Kocher is optimistic that the political squabbling the reform process has sparked will have little lasting impact. He understands HM leaders might be nervous about the potential for political upheaval to translate into medical upheaval, but he doubts that will happen.
“The political rhetoric and scuffling going on in Washington has almost no bearing on the fundamental underlying trend which will drive the market to near-universal use of hospitalists,” he says. “Whether you’re a Republican or Democrat, you share the perspective that the current health system is wildly too expensive.” HM11
Richard Quinn is a freelance writer based in New Jersey.
Robert Kocher, MD, is not a household name for hospitalists who aren’t policy wonks. That’s not to say he shouldn’t be.
Dr. Kocher, a former special assistant to President Obama on healthcare and economic policy who is now the director of the McKinsey Center for U.S. Health System Reform in Washington, D.C., was a behind-the-scenes player in the landmark healthcare reform legislation signed into law last year. After a two-year stint in the White House, he transitioned back to the private sector late in 2010, landing at McKinsey & Co., a powerhouse consulting firm in the nation’s capital.
On May 11, Dr. Kocher will give HM11’s first keynote speech, “Coming to Your Hospital: Healthcare Reform. What Does This Mean for Hospitalists.” His talk will be an inside look at how the reform package came together and point out how hospitalists can be “the solution that hospitals will want to deploy to allow them to capitalize” on reform.
“Instead of hospitalists being a de facto link [between different departments of a given hospital], I think hospitalists will be a value-creating link,” Dr. Kocher says. “There’s going to be much more information that’s going to have to flow between the inpatient side and the outpatient side if you’re going to manage population health and lower per capita costs. … It’s going to require more specialization, which hospitalists are in the right position to really take on and to deliver.”
Dr. Kocher (pronounced “coacher”) joined the reform fight in January 2009, taking a post at the National Economic Council as special assistant to the president for healthcare. He left that job last fall and rejoined McKinsey, the firm he had been with for seven years before joining the Obama administration. His career began with a medical degree from George Washington University and internal-medicine residency at Beth Israel Deaconess Medical Center in Boston.

He followed that with a stint as a clinical fellow and instructor at Harvard Medical School. In addition to his role as a principal at McKinsey, Dr. Kocher is a nonresident senior fellow at the Brookings Institution Engleberg Center for Health Reform.
He is a well-known speaker on healthcare topics and a frequent writer who has authored pieces for major outlets, including the New England Journal of Medicine, the Washington Post and The New York Times. The White House last year filmed him as part of its “Reality Check” Web series (www.whitehouse.gov/realitycheck/31), which is aimed at “debunking the myths” swirling around reform.
Dr. Kocher says all of his career stops pale in comparison to being part of once-in-a-generation talks that shaped the future of U.S. healthcare.
“Certainly, [it was] the most impactful thing I’ll ever get to actually do, because we were able to shape the lasting policies that will change the way healthcare is delivered for years to come,” he says. “It was an incredible privilege to get to observe and take part in that policy-making process and understand that some compromises have to happen to make successful legislation.”
Brendon Shank, SHM’s assistant vice president of communications, says that having a White House participant in the reform negotiations as a featured speaker is a treat for hospitalists.
“This is exciting because it’s someone who helped define policy,” Shank says. “This is someone who knows the inside of it. He’s been in the room for discussions that will affect hospitalists for years down the road.”
Exactly what those effects will be will take time to understand. But Dr. Kocher sees reform as a chance for HM to make itself indispensable to hospitals looking to improve quality, efficiency, and transitional-care outcomes.
More HM11 Preview
HM11’s visiting professor to serve as mentor, stimulate discussion
Hospitalists come from all walks; HM11 has a place for all of them
HM11 attendees can earn as many as 18.75 CME credits
Industry pioneer recounts HM’s meteoric rise, sees bright future for hospitalists
Lots to See, Lots to Do in ‘Big D’
From sports to culture to Tex-Mex, Dallas metroplex has something for every visitor
You may also
HM11 PREVIEW SUPPLEMENT
in pdf format.
The responsibility will, of course, come with the challenge of actually proving that HM can deliver on the pledge of better care at better prices.
“For hospitals, as the payment system evolves and matures, we’re going to be paying more often for outcomes,” Dr. Kocher says. “That change is going to require hospitalists to become much more reliable.
“It’s a more specialized skill that doctors who are part-time hospital doctors are going to have a hard time developing. It clearly makes the system more dependent on hospitalists. … That said, I think that it’s the responsibility of hospitalists to prove they can deliver.”
Dr. Kocher is optimistic that the political squabbling the reform process has sparked will have little lasting impact. He understands HM leaders might be nervous about the potential for political upheaval to translate into medical upheaval, but he doubts that will happen.
“The political rhetoric and scuffling going on in Washington has almost no bearing on the fundamental underlying trend which will drive the market to near-universal use of hospitalists,” he says. “Whether you’re a Republican or Democrat, you share the perspective that the current health system is wildly too expensive.” HM11
Richard Quinn is a freelance writer based in New Jersey.
Robert Kocher, MD, is not a household name for hospitalists who aren’t policy wonks. That’s not to say he shouldn’t be.
Dr. Kocher, a former special assistant to President Obama on healthcare and economic policy who is now the director of the McKinsey Center for U.S. Health System Reform in Washington, D.C., was a behind-the-scenes player in the landmark healthcare reform legislation signed into law last year. After a two-year stint in the White House, he transitioned back to the private sector late in 2010, landing at McKinsey & Co., a powerhouse consulting firm in the nation’s capital.
On May 11, Dr. Kocher will give HM11’s first keynote speech, “Coming to Your Hospital: Healthcare Reform. What Does This Mean for Hospitalists.” His talk will be an inside look at how the reform package came together and point out how hospitalists can be “the solution that hospitals will want to deploy to allow them to capitalize” on reform.
“Instead of hospitalists being a de facto link [between different departments of a given hospital], I think hospitalists will be a value-creating link,” Dr. Kocher says. “There’s going to be much more information that’s going to have to flow between the inpatient side and the outpatient side if you’re going to manage population health and lower per capita costs. … It’s going to require more specialization, which hospitalists are in the right position to really take on and to deliver.”
Dr. Kocher (pronounced “coacher”) joined the reform fight in January 2009, taking a post at the National Economic Council as special assistant to the president for healthcare. He left that job last fall and rejoined McKinsey, the firm he had been with for seven years before joining the Obama administration. His career began with a medical degree from George Washington University and internal-medicine residency at Beth Israel Deaconess Medical Center in Boston.

He followed that with a stint as a clinical fellow and instructor at Harvard Medical School. In addition to his role as a principal at McKinsey, Dr. Kocher is a nonresident senior fellow at the Brookings Institution Engleberg Center for Health Reform.
He is a well-known speaker on healthcare topics and a frequent writer who has authored pieces for major outlets, including the New England Journal of Medicine, the Washington Post and The New York Times. The White House last year filmed him as part of its “Reality Check” Web series (www.whitehouse.gov/realitycheck/31), which is aimed at “debunking the myths” swirling around reform.
Dr. Kocher says all of his career stops pale in comparison to being part of once-in-a-generation talks that shaped the future of U.S. healthcare.
“Certainly, [it was] the most impactful thing I’ll ever get to actually do, because we were able to shape the lasting policies that will change the way healthcare is delivered for years to come,” he says. “It was an incredible privilege to get to observe and take part in that policy-making process and understand that some compromises have to happen to make successful legislation.”
Brendon Shank, SHM’s assistant vice president of communications, says that having a White House participant in the reform negotiations as a featured speaker is a treat for hospitalists.
“This is exciting because it’s someone who helped define policy,” Shank says. “This is someone who knows the inside of it. He’s been in the room for discussions that will affect hospitalists for years down the road.”
Exactly what those effects will be will take time to understand. But Dr. Kocher sees reform as a chance for HM to make itself indispensable to hospitals looking to improve quality, efficiency, and transitional-care outcomes.
More HM11 Preview
HM11’s visiting professor to serve as mentor, stimulate discussion
Hospitalists come from all walks; HM11 has a place for all of them
HM11 attendees can earn as many as 18.75 CME credits
Industry pioneer recounts HM’s meteoric rise, sees bright future for hospitalists
Lots to See, Lots to Do in ‘Big D’
From sports to culture to Tex-Mex, Dallas metroplex has something for every visitor
You may also
HM11 PREVIEW SUPPLEMENT
in pdf format.
The responsibility will, of course, come with the challenge of actually proving that HM can deliver on the pledge of better care at better prices.
“For hospitals, as the payment system evolves and matures, we’re going to be paying more often for outcomes,” Dr. Kocher says. “That change is going to require hospitalists to become much more reliable.
“It’s a more specialized skill that doctors who are part-time hospital doctors are going to have a hard time developing. It clearly makes the system more dependent on hospitalists. … That said, I think that it’s the responsibility of hospitalists to prove they can deliver.”
Dr. Kocher is optimistic that the political squabbling the reform process has sparked will have little lasting impact. He understands HM leaders might be nervous about the potential for political upheaval to translate into medical upheaval, but he doubts that will happen.
“The political rhetoric and scuffling going on in Washington has almost no bearing on the fundamental underlying trend which will drive the market to near-universal use of hospitalists,” he says. “Whether you’re a Republican or Democrat, you share the perspective that the current health system is wildly too expensive.” HM11
Richard Quinn is a freelance writer based in New Jersey.
HM11 PREVIEW: HM11 Day-by-Day Schedule
Enter text here
Enter text here
Enter text here
Top Leaders, Hot Topics
Since its inception, SHM’s annual meeting has grown every year, attracting more hospitalists, bringing influential leaders to presentations, and creating a welcome environment for some of the most innovative ideas in healthcare. That growth in influence—and influencers—will be evident at HM11 next month.
This year, HM11 will bring hospitalists closer than ever to the decision-makers. Featured presenters Robert Wachter, MD, MHM, professor, chief of the division of hospital medicine at the University of California at San Francisco, and former White House advisor Robert Kocher, MD, will be joined by Cecil B. Wilson, MD, president of the American Medical Association.
“The Society of Hospital Medicine is a dynamic, growing organization that is very responsive to the interests and needs of hospitalists,” Dr. Wilson told SHM. “So when the SHM leadership offered me the opportunity to speak at Hospital Medicine 2011, I was pleased and honored. … I am hopeful that the AMA and the SHM can continue to work together productively to advance the interests of physicians and our patients.”

In addition to hosting the country’s most influential figures in healthcare, HM11 will present some of its most cutting-edge ideas in improving care. The continued focus on reducing unplanned readmissions in hospitals across the country has turned to a search for solutions. A new session will put the spotlight on SHM’s own program, Project BOOST (Boosting Outcomes for Older Adults through Safe Transitions).
“Healthcare Reform and Optimizing Care Transitions to Reduce Readmissions” will be presented by Mark V. Williams, MD, FACP, FHM, principal investigator of Project BOOST; Jeffrey Greenwald, MD, SFHM; and Linda Magno, the director of the Medicare Demonstrations Group in the Office of Research, Development, and Information at the Centers for Medicare & Medicaid Services.
The presentation will bring the audience to the very crossroads of healthcare policy reform and quality improvement (QI) by illustrating the impact of readmissions on healthcare costs and patient safety, coupled with the innovative and individualized approaches that Project BOOST hospitalists are implementing.
Development of and pilot testing of Project BOOST was supported through grant funding from the John A. Hartford Foundation. Today, Project BOOST has been implemented in more than 60 sites and the program is now recruiting for its fall cohort.
For more information about HM11, visit www.hospitalmedicine2011.org.
For information about Project BOOST, visit www.hospitalmedicine.org/boost. TH
Brendon Shank is SHM’s assistant vice president of communications.
Since its inception, SHM’s annual meeting has grown every year, attracting more hospitalists, bringing influential leaders to presentations, and creating a welcome environment for some of the most innovative ideas in healthcare. That growth in influence—and influencers—will be evident at HM11 next month.
This year, HM11 will bring hospitalists closer than ever to the decision-makers. Featured presenters Robert Wachter, MD, MHM, professor, chief of the division of hospital medicine at the University of California at San Francisco, and former White House advisor Robert Kocher, MD, will be joined by Cecil B. Wilson, MD, president of the American Medical Association.
“The Society of Hospital Medicine is a dynamic, growing organization that is very responsive to the interests and needs of hospitalists,” Dr. Wilson told SHM. “So when the SHM leadership offered me the opportunity to speak at Hospital Medicine 2011, I was pleased and honored. … I am hopeful that the AMA and the SHM can continue to work together productively to advance the interests of physicians and our patients.”

In addition to hosting the country’s most influential figures in healthcare, HM11 will present some of its most cutting-edge ideas in improving care. The continued focus on reducing unplanned readmissions in hospitals across the country has turned to a search for solutions. A new session will put the spotlight on SHM’s own program, Project BOOST (Boosting Outcomes for Older Adults through Safe Transitions).
“Healthcare Reform and Optimizing Care Transitions to Reduce Readmissions” will be presented by Mark V. Williams, MD, FACP, FHM, principal investigator of Project BOOST; Jeffrey Greenwald, MD, SFHM; and Linda Magno, the director of the Medicare Demonstrations Group in the Office of Research, Development, and Information at the Centers for Medicare & Medicaid Services.
The presentation will bring the audience to the very crossroads of healthcare policy reform and quality improvement (QI) by illustrating the impact of readmissions on healthcare costs and patient safety, coupled with the innovative and individualized approaches that Project BOOST hospitalists are implementing.
Development of and pilot testing of Project BOOST was supported through grant funding from the John A. Hartford Foundation. Today, Project BOOST has been implemented in more than 60 sites and the program is now recruiting for its fall cohort.
For more information about HM11, visit www.hospitalmedicine2011.org.
For information about Project BOOST, visit www.hospitalmedicine.org/boost. TH
Brendon Shank is SHM’s assistant vice president of communications.
Since its inception, SHM’s annual meeting has grown every year, attracting more hospitalists, bringing influential leaders to presentations, and creating a welcome environment for some of the most innovative ideas in healthcare. That growth in influence—and influencers—will be evident at HM11 next month.
This year, HM11 will bring hospitalists closer than ever to the decision-makers. Featured presenters Robert Wachter, MD, MHM, professor, chief of the division of hospital medicine at the University of California at San Francisco, and former White House advisor Robert Kocher, MD, will be joined by Cecil B. Wilson, MD, president of the American Medical Association.
“The Society of Hospital Medicine is a dynamic, growing organization that is very responsive to the interests and needs of hospitalists,” Dr. Wilson told SHM. “So when the SHM leadership offered me the opportunity to speak at Hospital Medicine 2011, I was pleased and honored. … I am hopeful that the AMA and the SHM can continue to work together productively to advance the interests of physicians and our patients.”

In addition to hosting the country’s most influential figures in healthcare, HM11 will present some of its most cutting-edge ideas in improving care. The continued focus on reducing unplanned readmissions in hospitals across the country has turned to a search for solutions. A new session will put the spotlight on SHM’s own program, Project BOOST (Boosting Outcomes for Older Adults through Safe Transitions).
“Healthcare Reform and Optimizing Care Transitions to Reduce Readmissions” will be presented by Mark V. Williams, MD, FACP, FHM, principal investigator of Project BOOST; Jeffrey Greenwald, MD, SFHM; and Linda Magno, the director of the Medicare Demonstrations Group in the Office of Research, Development, and Information at the Centers for Medicare & Medicaid Services.
The presentation will bring the audience to the very crossroads of healthcare policy reform and quality improvement (QI) by illustrating the impact of readmissions on healthcare costs and patient safety, coupled with the innovative and individualized approaches that Project BOOST hospitalists are implementing.
Development of and pilot testing of Project BOOST was supported through grant funding from the John A. Hartford Foundation. Today, Project BOOST has been implemented in more than 60 sites and the program is now recruiting for its fall cohort.
For more information about HM11, visit www.hospitalmedicine2011.org.
For information about Project BOOST, visit www.hospitalmedicine.org/boost. TH
Brendon Shank is SHM’s assistant vice president of communications.
Q&A with Hospitalist Administrator Amit Prachand
Amit Prachand, MEng
Division Administrator, Hospital Medicine
Northwestern Memorial Hospital and Feinberg School of Medicine,
Northwestern University, Chicago
Question: What motivated you to join SHM’s Administrators Task Force (ATF)?
A: I wanted to be able to directly interface with the community of leaders in similar administrator roles in order to obtain a stronger perspective of the role, its rewards and challenges, and of the creative solutions different practices have implemented to address issues relevant to hospital medicine and the overall healthcare delivery model. I was also relatively new to hospital medicine practice management, and even healthcare, so I wanted to put myself in the best position to soak in as much as possible as well as help facilitate the sharing of ideas amongst my new group of peers.
Q: How is the Administrators Task Force moving HM forward?
A: One of our main thrusts in the task force is to help expand the administrative membership in SHM. As hospitalist programs mature and the environment in which hospital medicine is practiced evolves, it is imperative that we develop the community, the infrastructure, and the tools required to partner with our stakeholders—both internal and external—to help lead hospital medicine forward.
Q: Has your participation in the Administrators Task Force helped your group?
A: The ATF has helped develop direct lines of communication with peers. This helps when it come to issues for which we are finding the best solutions for; areas such as on-boarding of new physicians, negotiations with hospitals, coding and billing improvement, and meaningful performance reporting.
Q: How is the task force helping hospitals improve patient care?
A: By having a peer group on the administrative side, I believe we are now able to more readily share ideas that support the ideas around patient-care improvement that are being shared amongst the physician membership.
One of the key roles we play as an administrator is to help develop the systems and structures that help improve patient care. That may range from advocating for physician representation on certain hospital committees to facilitating a process/QI project that involves hospitalists and other members of the extended patient-care team, such as physicians from other medical specialties, nursing, pharmacists, case management, bed management, environmental services, and information technology.
Q: How is the task force helping hospitals improve healthcare overall?
A: We are continually improving the infrastructure for administrators to share ideas and solutions to address overall healthcare issues (payment reform, readmissions, compliance, cost). It is through this infrastructure that we can identify best implementation practices of ideas. The webinar series (www.hospitalmedicine.org/roundtables) that we’ve developed addresses many of the issues that healthcare in general is facing. This series has exceeded expectations for participation and interest.
Q: What do you like most about your job as an administrator?
A: It is never dull, always exciting. From the firefighting to the long-term planning, the role keeps me on my toes. I enjoy being in a position that is so tightly intertwined with so many critical functions and disciplines across the medical center in a profession—hospital medicine—that is continuing to lead advances in healthcare delivery.
—Brendon Shank
Amit Prachand, MEng
Division Administrator, Hospital Medicine
Northwestern Memorial Hospital and Feinberg School of Medicine,
Northwestern University, Chicago
Question: What motivated you to join SHM’s Administrators Task Force (ATF)?
A: I wanted to be able to directly interface with the community of leaders in similar administrator roles in order to obtain a stronger perspective of the role, its rewards and challenges, and of the creative solutions different practices have implemented to address issues relevant to hospital medicine and the overall healthcare delivery model. I was also relatively new to hospital medicine practice management, and even healthcare, so I wanted to put myself in the best position to soak in as much as possible as well as help facilitate the sharing of ideas amongst my new group of peers.
Q: How is the Administrators Task Force moving HM forward?
A: One of our main thrusts in the task force is to help expand the administrative membership in SHM. As hospitalist programs mature and the environment in which hospital medicine is practiced evolves, it is imperative that we develop the community, the infrastructure, and the tools required to partner with our stakeholders—both internal and external—to help lead hospital medicine forward.
Q: Has your participation in the Administrators Task Force helped your group?
A: The ATF has helped develop direct lines of communication with peers. This helps when it come to issues for which we are finding the best solutions for; areas such as on-boarding of new physicians, negotiations with hospitals, coding and billing improvement, and meaningful performance reporting.
Q: How is the task force helping hospitals improve patient care?
A: By having a peer group on the administrative side, I believe we are now able to more readily share ideas that support the ideas around patient-care improvement that are being shared amongst the physician membership.
One of the key roles we play as an administrator is to help develop the systems and structures that help improve patient care. That may range from advocating for physician representation on certain hospital committees to facilitating a process/QI project that involves hospitalists and other members of the extended patient-care team, such as physicians from other medical specialties, nursing, pharmacists, case management, bed management, environmental services, and information technology.
Q: How is the task force helping hospitals improve healthcare overall?
A: We are continually improving the infrastructure for administrators to share ideas and solutions to address overall healthcare issues (payment reform, readmissions, compliance, cost). It is through this infrastructure that we can identify best implementation practices of ideas. The webinar series (www.hospitalmedicine.org/roundtables) that we’ve developed addresses many of the issues that healthcare in general is facing. This series has exceeded expectations for participation and interest.
Q: What do you like most about your job as an administrator?
A: It is never dull, always exciting. From the firefighting to the long-term planning, the role keeps me on my toes. I enjoy being in a position that is so tightly intertwined with so many critical functions and disciplines across the medical center in a profession—hospital medicine—that is continuing to lead advances in healthcare delivery.
—Brendon Shank
Amit Prachand, MEng
Division Administrator, Hospital Medicine
Northwestern Memorial Hospital and Feinberg School of Medicine,
Northwestern University, Chicago
Question: What motivated you to join SHM’s Administrators Task Force (ATF)?
A: I wanted to be able to directly interface with the community of leaders in similar administrator roles in order to obtain a stronger perspective of the role, its rewards and challenges, and of the creative solutions different practices have implemented to address issues relevant to hospital medicine and the overall healthcare delivery model. I was also relatively new to hospital medicine practice management, and even healthcare, so I wanted to put myself in the best position to soak in as much as possible as well as help facilitate the sharing of ideas amongst my new group of peers.
Q: How is the Administrators Task Force moving HM forward?
A: One of our main thrusts in the task force is to help expand the administrative membership in SHM. As hospitalist programs mature and the environment in which hospital medicine is practiced evolves, it is imperative that we develop the community, the infrastructure, and the tools required to partner with our stakeholders—both internal and external—to help lead hospital medicine forward.
Q: Has your participation in the Administrators Task Force helped your group?
A: The ATF has helped develop direct lines of communication with peers. This helps when it come to issues for which we are finding the best solutions for; areas such as on-boarding of new physicians, negotiations with hospitals, coding and billing improvement, and meaningful performance reporting.
Q: How is the task force helping hospitals improve patient care?
A: By having a peer group on the administrative side, I believe we are now able to more readily share ideas that support the ideas around patient-care improvement that are being shared amongst the physician membership.
One of the key roles we play as an administrator is to help develop the systems and structures that help improve patient care. That may range from advocating for physician representation on certain hospital committees to facilitating a process/QI project that involves hospitalists and other members of the extended patient-care team, such as physicians from other medical specialties, nursing, pharmacists, case management, bed management, environmental services, and information technology.
Q: How is the task force helping hospitals improve healthcare overall?
A: We are continually improving the infrastructure for administrators to share ideas and solutions to address overall healthcare issues (payment reform, readmissions, compliance, cost). It is through this infrastructure that we can identify best implementation practices of ideas. The webinar series (www.hospitalmedicine.org/roundtables) that we’ve developed addresses many of the issues that healthcare in general is facing. This series has exceeded expectations for participation and interest.
Q: What do you like most about your job as an administrator?
A: It is never dull, always exciting. From the firefighting to the long-term planning, the role keeps me on my toes. I enjoy being in a position that is so tightly intertwined with so many critical functions and disciplines across the medical center in a profession—hospital medicine—that is continuing to lead advances in healthcare delivery.
—Brendon Shank
Q&A with Hospitalist Administrator Kristi Gylten
Kristi Gylten, MBA
Director, Hospitalist Service,
Rapid City (S.D.) Regional Hospital
Question: What motivated you to join the Administrators Task Force (ATF)?
Answer: I wanted to have the opportunity to meet and network with my peers, and to be a part of developing resources and a place “on the map” for hospitalist administrators. The Administrators Task Force is bringing awareness to the administrative and business side of hospital medicine through the eyes of the hospitalist administrators.
Q: Has your participation on the task force helped out your group?
A: My group has benefited through the access and utilization of the available tools and resources to evaluate my own program, including tools like dashboards, job descriptions, patient communication, and marketing materials. The ATF has increased my awareness of the resources available, clinical and operational, to hospitalist groups, including my own.
Q: How is the ATF helping hospitals improve healthcare overall?
A: I believe the task force has its pulse on how healthcare could ideally be provided in the future. And, to me, it is extremely exciting to be part of the team that will help design the future of inpatient medicine and, in part, the continuum of care.
As hospitalist administrators, you have a close and collaborative relationship with the inpatient providers. And I think that because of that relationship and the fact that they live and breathe inpatient medicine, you are able to engage your team in improving many aspects of healthcare.
Q: What do you like most about your job as an administrator?
A: I like the wide variety of opportunities and challenges the role presents: human resources, contracting, recruitment, marketing and public relations, customer satisfaction, quality, and financials. The list goes on. No one day is like the previous, and it’s never dull. And most of all, I enjoy the challenge of strategizing and planning for the future of providing healthcare.
—Brendon Shank
Kristi Gylten, MBA
Director, Hospitalist Service,
Rapid City (S.D.) Regional Hospital
Question: What motivated you to join the Administrators Task Force (ATF)?
Answer: I wanted to have the opportunity to meet and network with my peers, and to be a part of developing resources and a place “on the map” for hospitalist administrators. The Administrators Task Force is bringing awareness to the administrative and business side of hospital medicine through the eyes of the hospitalist administrators.
Q: Has your participation on the task force helped out your group?
A: My group has benefited through the access and utilization of the available tools and resources to evaluate my own program, including tools like dashboards, job descriptions, patient communication, and marketing materials. The ATF has increased my awareness of the resources available, clinical and operational, to hospitalist groups, including my own.
Q: How is the ATF helping hospitals improve healthcare overall?
A: I believe the task force has its pulse on how healthcare could ideally be provided in the future. And, to me, it is extremely exciting to be part of the team that will help design the future of inpatient medicine and, in part, the continuum of care.
As hospitalist administrators, you have a close and collaborative relationship with the inpatient providers. And I think that because of that relationship and the fact that they live and breathe inpatient medicine, you are able to engage your team in improving many aspects of healthcare.
Q: What do you like most about your job as an administrator?
A: I like the wide variety of opportunities and challenges the role presents: human resources, contracting, recruitment, marketing and public relations, customer satisfaction, quality, and financials. The list goes on. No one day is like the previous, and it’s never dull. And most of all, I enjoy the challenge of strategizing and planning for the future of providing healthcare.
—Brendon Shank
Kristi Gylten, MBA
Director, Hospitalist Service,
Rapid City (S.D.) Regional Hospital
Question: What motivated you to join the Administrators Task Force (ATF)?
Answer: I wanted to have the opportunity to meet and network with my peers, and to be a part of developing resources and a place “on the map” for hospitalist administrators. The Administrators Task Force is bringing awareness to the administrative and business side of hospital medicine through the eyes of the hospitalist administrators.
Q: Has your participation on the task force helped out your group?
A: My group has benefited through the access and utilization of the available tools and resources to evaluate my own program, including tools like dashboards, job descriptions, patient communication, and marketing materials. The ATF has increased my awareness of the resources available, clinical and operational, to hospitalist groups, including my own.
Q: How is the ATF helping hospitals improve healthcare overall?
A: I believe the task force has its pulse on how healthcare could ideally be provided in the future. And, to me, it is extremely exciting to be part of the team that will help design the future of inpatient medicine and, in part, the continuum of care.
As hospitalist administrators, you have a close and collaborative relationship with the inpatient providers. And I think that because of that relationship and the fact that they live and breathe inpatient medicine, you are able to engage your team in improving many aspects of healthcare.
Q: What do you like most about your job as an administrator?
A: I like the wide variety of opportunities and challenges the role presents: human resources, contracting, recruitment, marketing and public relations, customer satisfaction, quality, and financials. The list goes on. No one day is like the previous, and it’s never dull. And most of all, I enjoy the challenge of strategizing and planning for the future of providing healthcare.
—Brendon Shank