User login
MDS: What Do Hospitalists Need to Know?
Myelodysplastic syndromes (MDS) comprise a heterogeneous group of clonal hematopoietic stem cell neoplasms characterized by dysplasia, ineffective hematopoiesis resulting in peripheral blood (PB) cytopenias affecting one or more cell lines, and a variable risk of progression to acute myeloid leukemia (AML). The last 15 years have witnessed significant advances in our understanding of the complex pathogenesis, classification and prognostication, and therapeutic approaches to MDS. As more elderly patients are diagnosed with MDS, encounters with hospitalized MDS patients or patients in whom MDS should be considered in the differential diagnosis are common events for today's hospitalists. In this review, we discuss the epidemiology, diagnosis, pathogenesis, prognostication, and therapies for MDS, with an emphasis on practical aspects that would be useful for hospitalists caring for these patients.
EPIDEMIOLOGY OF MDS
Although MDS is one of the most common hematologic malignancies, MDS remains understudied epidemiologically.[1, 2] Our understanding of the epidemiology improved after the implementation of reporting requirements to cancer registries, especially the Surveillance, Epidemiology, and End Results (SEER) database in 2001.[1, 2, 3] Age‐adjusted incidence of MDS in the United States ranged between 3.3 to 4.6 per 100,000 persons per year in the period between 2001 and 2008.[1, 2, 4] The majority of MDS patients are elderly, and because MDS incidence increases with age, the number of patients diagnosed with MDS is expected to continue to rise with the aging population.[1, 2, 5] MDS is more common in men compared to women, and in Caucasians compared to African Americans.[1, 2] Different estimates put MDS prevalence in the United States somewhere between 60,000 and 170,000 persons.[2, 6]
DIAGNOSIS OF MDS
Many patients with MDS are asymptomatic at diagnosis and only come to medical attention due to abnormal blood counts done routinely or for other reasons. This contributes to MDS being underdiagnosed. When cytopenias are not severe enough to cause symptoms, it is also frequently overlooked in patients with mild anemia or other cytopenias.[7] Together, being asymptomatic and having relatively mild cytopenias are probably the most important factors that lead to under‐recognition of MDS among primary care physicians (PCPs).[7, 8, 9] There is a misconception that anemia is normal in the elderly, and when patients are not symptomatic that a workup is not needed.[6, 7] This is compounded by a lack of awareness of the importance of making a diagnosis in these patients and of currently available therapies for MDS.[7, 8, 9]
Anemia is not a normal consequence of aging and is always a pathologic state with an underlying etiology.[6, 7] Because a significant number of elderly patients with unexplained anemia could have MDS, patients with symptomatic or progressive anemia, especially if associated with other cytopenias, should be considered for further evaluation.[7, 9] Diagnosis is important given the recent availability of effective therapies for MDS that can improve anemia, decrease transfusion needs, improve life quality, and potentially increase survival. MDS is generally an indolent disease with a relative stability of blood counts in comparison to AML, so prior blood counts and the tempo of the process is an important consideration.[9, 10] The National Comprehensive Cancer Network clinical practice guidelines recommend exclusion of nutritional deficiencies (iron, vitamin B12, folate) and other causes of anemia (eg, gastrointestinal bleeding, renal insufficiency, and anemia of inflammation), assessment of reticulocyte count and serum erythropoietin level, and evaluation of a PB smear for evidence of dysplasia as important initial steps.[10, 11] Eventually the diagnosis of MDS requires a bone marrow (BM) evaluation to confirm the diagnosis and exclude other BM failure states by evaluating for BM cellularity, cell maturation, dysplasia (which should be present in at least 10% of any the myeloid lineages), percentage of blasts (20%), iron stores and sideroblasts, cytogenetics, MDS‐specific fluorescence in situ hybridization (FISH) panels, flow cytometry, and other special testing.[9, 10] Despite extensive testing, MDS can sometimes be very difficult to differentiate from other bone marrow failure states (eg, hypoplastic MDS from aplastic anemia) (Table 1).[10, 11] In the absence of significant morbidity related to MDS, the definitive diagnosis of MDS can be usually made on an outpatient basis. It is important to ensure adequate follow‐up with PCPs postdischarge and/or outpatient hematologist referral for patients with unexplained cytopenias.
|
| Idiopathic cytopenia of undetermined significance: no significant dysplasia or MDS‐associated karyotypic aberrations |
| Acute myeloid leukemia: BM blasts 20%, presence of core‐binding characteristic cytogenetic aberrations: t(8;21), t(15;17), inv(16) defines AML regardless of BM blast count; AML can be associated with hepatosplenomegaly or myeloid sarcomas |
| Chronic myeloid leukemia: presence of Philadelphia chromosome t(9;22) positive, basophilia, and splenomegaly |
| Myelofibrosis: significant BM fibrosis, splenomegaly, and leukoerythroblastic picture in PB (teardrop and nucleated RBCs, left‐shifted myeloid cells) |
| Chronic myelomonocytic leukemia: significant PB monocytosis |
| MDS/MPN overlap syndromes: dysplasia with myeloproliferative characteristics such as splenomegaly, thrombocytosis, or leukocytosis |
| Infections: for example, HIV and parvovirus B19 infections |
| Myelophthisis: infiltration of BM with other tumors (eg, melanoma) with resultant PB cytopenias |
| Nutritional disturbances: B12, folate, and copper deficiency, and zinc and arsenic excess can mimic MDS |
| Medications: drugs that interfere with DNA synthesis such as HIV medications, chemotherapeutic agents, cotrimoxazole, methotrexate, azathioprine, and G‐CSF |
| Immune disorders: for example, LGL leukemia, lupus, or rheumatoid arthritis |
| Other acquired or congenital hematological disorders: for example, paroxysmal nocturnal hemoglobinuria, congenital dyserythropoietic anemia, dyskeratosis congenita |
PATHOGENESIS AND ETIOLOGY OF MDS
Ineffective hematopoiesis due to excessive apoptosis of hematopoietic precursors is a prominent feature of MDS, which explains the apparent paradox of hypercellular BM and PB cytopenias. Although not fully understood, complex epigenetic, genetic, and immunologic mechanisms contribute to the pathogenesis of MDS and account for disease heterogeneity. Aberrant silencing of tumor‐suppressor and DNA repair genes mediated by hypermethylation of their promoters is believed to play an important part in the pathogenesis of MDS.[12] This theory is supported by the unique sensitivity of MDS to drugs that reverse DNA methylation. Genetic abnormalities not only contribute to the pathogenesis of MDS, but are also among the strongest prognostic indicators for MDS patients, and can also affect therapeutic decisions. Clonal karyotypic abnormalities are observed in 50% of patients with MDS using conventional karyotyping.[12, 13] The most common chromosomal aberrations in MDS include deletions of the long arm of chromosome 5 (del5q), monosomy Y, monosomy 7 (del7) or deletion of its long arm (del7q), trisomy 8, del20q, and complex karyotypes (3 chromosomal aberrations).[12, 13] These cytogenetic abnormalities correlate with the prognosis of MDS (eg, poor prognosis with complex karyotypes and chromosome 7 deletions vs better prognosis with isolated del5q).[12, 13]
Recently, FISH assays and genome‐wide screening techniques (eg, single nucleotide polymorphism arrays, array‐based comparative genomic hybridization, whole genome or exome sequencing) have enabled detection of an increasing number of genetic aberrations and recurrent somatic molecular abnormalities in a significant number of MDS patients (eg, abnormalities of ASXL1, IDH1/IDH2, DNMT3, EZH2, TET2, and SF3B1 genes).[12, 14] Most affected genes are involved in the epigenetic regulation of transcription (DNA methylation and demethylation, histone posttranslational modification) or mRNA splicing.[12, 13, 14]
Immunologic aberrations have also been proposed to contribute to pathogenesis of MDS. For example, in early‐stage MDS, an aberrant immune attack on myeloid progenitors resulting in increased apoptosis can contribute to BM failure.[15] This is supported by association of some forms of MDS with autoimmune diseases and observed responses in some patients to immunosuppressive therapies. The relative contribution of pathogenetic mechanisms varies between the different MDS subtypes. For example, haploinsufficiency of cell‐cycle regulatory and ribosomal protein genes located in the commonly deleted region of 5q play an important role in the pathogenesis of MDS with isolated del5q (5q syndrome).[16] Mutations in the RNA spliceosomal machinery gene SF3B have been shown to play a role in the pathogenesis of the MDS subtype refractory anemia with ringed sideroblasts (RARS), with those patients with RARS carrying this mutation having a more favorable prognosis than those with the wild‐type gene.[14] Several excellent recent reviews provide detailed discussion of the complex pathophysiology of MDS.[12, 13, 14, 17]
Approximately 10% of MDS patients have secondary MDS (MDS occurring after chemotherapy or radiation therapy administration for treatment of another malignancy).[2] Aside from advancing age, the causative factors for the other 90% of cases (primary MDS) are unknown in most patients, although environmental and occupational exposures (eg, smoking, painting, insecticides, pesticides, organic solvents), and genetic syndromes (eg, DNA repair defects such as Fanconi's anemia) are implicated in some patients.[2, 10] Recently, an epidemiologic study found an increased MDS risk with obesity.[18]
PROGNOSTICATION OF MDS
MDS is a form of cancer, and most affected patients eventually die from cytopenic complications or leukemic progression. MDS is not a single disease but rather encompasses a group of heterogeneous subtypes with significantly different natural histories and pace of progression. Therefore, accurate risk stratification of MDS is necessary not only to predict survival and risk of leukemic progression, but also to help choose the most appropriate therapeutic option for individual patients. Information about prognosis should also be utilized when making management decisions with patients for other comorbid conditions (eg, major surgery). Two morphologically based classification systems are commonly used for MDS: the French‐American‐British (FAB) system and the World Health Organization (WHO) classification (Table 2), which most recently has supplanted the FAB system as the primary pathologic classification system.[19, 20, 21] Several prognostic models have been developed around the morphologic classifications to better account for relevant clinical and cytogenetic modifiers of this disease. Although some of these models have been validated by different groups, each of these models has limitations. Although the predictions generated by these models are generally accurate for the different prognostic categories to which the patient is assigned, the extent to which the prediction applies to an individual MDS patient can vary significantly. In addition, comorbid conditions affect survival of MDS patients and are not included in the specific scoring systems. For example, congestive heart failure and chronic obstructive lung disease were associated with shortened survival in MDS patients.[18]
| MDS WHO Class | PB Findings | BM Findings |
|---|---|---|
| ||
| Refractory cytopenias with unilineage dysplasia: includes refractory anemia; refractory neutropenia; refractory thrombocytopenia | Unicytopenia or bicytopenia; PB blasts 1% | BM blasts 5%; unilineage dysplasia (10% of cells in any myeloid lineage); 15% of erythroid precursors are ringed sideroblasts |
| Refractory anemia with ring sideroblasts | Anemia; PB blasts 1% | BM blasts 5%; erythroid dysplasia only; 15% of erythroid precursors are ringed sideroblasts |
| Refractory cytopenia with multilineage dysplasia | Cytopenia(s); PB blasts 1%; no Auer rods; 1 106/L monocytes | BM blasts 5% ; dysplasia (10% of cells in at least 2 myeloid lineages); no Auer rods |
| Refractory anemia with excess blasts‐1 | Cytopenia(s); PB blasts 5%; no Auer rods; 1 106/L monocytes | BM blasts 5%9%; unilineage or multilineage dysplasia; no Auer rods |
| Refractory anemia with excess blasts‐2 | Cytopenia(s); PB blasts 5%19%; Auer rods; 1 106/L monocytes | BM blasts 10%19%; unilineage or multilineage dysplasia; Auer rods |
| Myelodysplastic syndromeunclassified | Cytopenias; PB blasts 1% | BM blasts 5%; unequivocal dysplasia in 10% of cells at least one myeloid cell lines when accompanied by a cytogenetic abnormality considered as presumptive evidence for a diagnosis of MDS |
| MDS associated with isolated del5q | Anemia; normal to elevated platelet count; PB blasts 1% | BM blasts 5%; normal to elevated megakaryocytes with hypolobated nuclei; isolated del5q karyotypic abnormality; no Auer rods |
The International Prognostic Scoring System (IPSS) is the most widely used prognostic tool for MDS (Table 3).[22] In this model, an aggregate score is calculated based on points assigned to the percentage of blasts in BM, the number of PB cell lines affected by cytopenias, and the karyotype. Based on this point score, the patient is assigned to 1 of 4 categories that portend significantly different outcomes: low, intermediate‐1 (INT‐1), intermediate‐2 (INT‐2), and high risk. The IPSS was developed from a database of mostly untreated MDS patients and does not account for other important prognostic parameters such as transfusion dependence, depth of cytopenias, and extent/severity of lineage dysplasia.[22] The WHO Prognostic Scoring System was proposed to overcome some of these shortcomings.[23, 24] Efforts to continue to improve the prognostic models further led to a large international collaboration that compiled a much larger database and resulted in the development of a revised IPSS (IPSS‐R).[25] New discoveries of novel prognostic epigenetic, genetic, and immunologic determinants will likely result in the ongoing evolution of the current prognostic systems to further improve their discriminatory power.[26]
| Calculation of Score Value Based on Prognostic Variables | |||||
|---|---|---|---|---|---|
| Score Value | |||||
| 0 | 0.5 | 1.0 | 1.5 | 2.0 | |
| |||||
| Prognostic variable | |||||
| Bone marrow blasts (%)a | 5 | 510 | 1120 | 2130 | |
| Karyotypeb | Good | Intermediate | Poor | ||
| Number of peripheral blood cell line affected by cytopeniasc | 0 or 1 | 2 or 3 | |||
| Median Survival and Risk of Progression to AML According to the IPSS Risk Category in Absence of Therapy | |||||
| Overall Score | Risk Category | Percentage in the IPSS Population | Median Survival (Years) | Median Time From Diagnosis at Which 25% of Patients Progress to AML (Years) | |
| 0 | Low | 33% | 5.7 | 9.4 | |
| 0.51.0 | INT‐1 | 38% | 3.5 | 3.3 | |
| 1.52.0 | INT‐2 | 22% | 1.1 | 1.1 | |
| >2.5 | High | 7% | 0.4 | 0.2 | |
MANAGEMENT OF MDS
Most patients with MDS were treated historically with supportive measures only. The approval of 3 agents for treatment of MDS including the DNA methyltransferase inhibitors (DNMTi) azacitidine and decitabine, as well as the immunomodulatory agent lenalidomide, in the last decade advanced the care of MDS patients significantly (Table 4). Nonetheless, the use of allogeneic hematopoietic stem cell transplantation (alloHSCT) remains the only known curative modality for patients with MDS and should always be considered as a possible therapeutic option.[27] Unfortunately, the majority of patients with MDS are not considered candidates for alloHSCT due to age, comorbidities, and lack of suitable donors.[27] Therefore, most patients with MDS are managed with noncurative treatment and supportive paradigms. Treatment goals generally depend on the risk stratification for the particular individual, age, functional status, comorbidities, and importantly, the patient's individual preference. For medical decision‐making purposes, MDS is traditionally divided into 2 major risk categories: low‐risk (LR) and high‐risk (HR) groups. LR‐MDS includes the IPSS risk categories of low or INT‐1, whereas HR‐MDS is usually defined by the IPSS risk categories of INT‐2 and high. Newer classification tools (eg, IPSS‐R) and better molecular markers are expected to impact such categories as well as treatment recommendations in the future.[26]
|
| Azacitidine (5‐azacytidine, Vidaza) and decitabine (5‐aza,2‐deoxycytidine, Dacogen) |
| Class |
| Hypomethylating agents, azanucleosides |
| Mechanism of action |
| Epigenetic modulation by inhibition of DNA methyltransferase enzymes and other mechanisms |
| Indication |
| First line therapy for HR‐MDS, second line therapy for LR‐MDS after failure of other therapies such as ESAs, lenalidomide, or immunosuppressive agents |
| Approved regimens for MDS |
| Azacitidine: 75 mg/m2/day IV or SC for 7 days Q 4 weeks |
| Decitabine: 15 mg/m2 IV infusion over 3 hours, Q 8 hours for 3 days, Q 6 weeks or 20 mg/m2 IV infusion over 1 hour daily for 5 days Q 4 weeks |
| Common side effects |
| Fatigue |
| Development of or worsening cytopenias (neutropenia, thrombocytopenia, and anemia) and their complications (eg, infections, bleeding) |
| Gastrointestinal disturbances (nausea, vomiting, or diarrhea) |
| Oral ulcers and rarely mucositis |
| Injection site reactions (redness, pain) |
| Lenalidomide (Revlimid) |
| Class |
| Immunomodulatory agent |
| Mechanism of action |
| Modulation of immune responses, gene expression, angiogenesis, cytokines and cell‐cycle regulatory phosphatases, and possibly other mechanisms |
| Indication |
| First line therapy for LR‐MDS with del5q (also used commonly off label for LR‐MDS without del5q as second line of therapy after ESAs) |
| Approved regimens for MDS |
| 10 mg orally once daily |
| Common side effects |
| Skin rash, dryness, and pruritus |
| Fatigue |
| Muscle cramps |
| Development of or worsening cytopenias (neutropenia, thrombocytopenia, and anemia) and their complications (eg, infections, bleeding) |
| Gastrointestinal disturbances (nausea, vomiting, or diarrhea) |
Despite recent advances, supportive care for all patients with MDS remains a very important aspect of management, either in combination with other therapies or as sole therapy for frail patients who cannot tolerate further interventions. Supportive therapy focuses on maintaining a high quality of life and includes careful blood count monitoring, use of growth factors, use of transfusions and antibiotics as needed, and use of iron chelation therapy in some patients. Some of the common situations in which hospitalists encounter patients with MDS are listed in Table 5.
|
| Complications of cytopenias |
| Bleeding: local management based on bleeding site, platelet transfusions, and other blood products (eg, red blood cells, fresh frozen plasma) as appropriate, antifibrinolytics |
| Infections and neutropenic fevers: Antibiotics, antifungals, use of colony granulocyte‐stimulating factors or granulocyte infusions advised only in cases of uncontrolled severe infections or sepsis |
| Severe or symptomatic anemia: red blood transfusions as appropriate based on patient's comorbidities, all disease‐modifying drugs (lenalidomide, azacitidine, decitabine) and ESAs are slow acting and can take weeks to months before improving anemia |
| Complications of therapies |
| Neutropenic fevers: as above plus holding therapy |
| Most other side effects (see Table 4) are well tolerated and are managed symptomatically without requiring hospitalization. If needed hospitalization for side effects: symptomatic management and holding the drug |
| Other medical or surgical condition in a patient with MDS |
| Therapy as per the underlying medical condition. For therapeutic decisions (eg, decision to undergo major surgery), prognostication tools such as the IPSS and newer models can be used to inform medical decision making in consultation with an experienced hematologist |
MANAGEMENT OF LR‐MDS
In addition to supportive care or enrollment in clinical trials, therapies for LR‐MDS include erythropoiesis‐stimulating agents, lenalidomide, and immunosuppressive therapy.
Erythropoiesis‐Stimulating Agents
Anemia in MDS is a multifactorial process that includes ineffective erythropoiesis and suboptimal serum erythropoietin responses.[10, 28, 29] There are no randomized studies to suggest that erythropoiesis‐stimulating agents (ESA) therapy prolongs survival in MDS patients. Nonetheless, ESAs improve anemia significantly in some patients and are widely used.[30, 31] Approximately 20% to 30% of unselected MDS patients and about 40% of LR‐MDS patients achieve clinically meaningful erythroid responses with ESA therapy with a median response duration of 2 years.[30, 31] It is important to correct coexisting nutritional deficiencies (eg, iron or folate deficiency) to optimize responses to ESA.[10] Granulocyte colony‐stimulating factor can be synergistic with ESAs especially in patients with RARS.[10] Patients with LR‐MDS who have low endogenous serum erythropoietin levels (200500 mU/mL) and lower red blood cell (RBC) transfusion requirements (2 U per month) are more likely to respond to ESA therapy.[32, 33] Compared to certain solid tumors, ESA therapy in MDS has not been associated with an increased risk of thromboembolic events.[34]
Lenalidomide
5q syndrome is a subtype of MDS characterized by refractory macrocytic anemia, normal or elevated platelet counts, low BM blast percentage, small hypolobated dysplastic megakaryocytes, an isolated interstitial deletion in 5q, and an indolent natural history.[17, 35] Lenalidomide, an oral derivative of thalidomide, induces high response rates in LR‐MDS patients with 5q deletions, including hematologic improvements, RBC transfusion independence (TI) (56%67%, median duration >104 weeks), cytogenetic responses (50%76%), and complete remissions.[35, 36] These findings resulted in approval of lenalidomide (Revlimid; Celgene Corp., Summit, NJ) for patients with IPSS low or INT‐1 MDS with transfusion‐dependent anemia and 5q deletions with or without additional cytogenetic abnormalities. In addition, lenalidomide has some activity against LR‐MDS without 5q deletions (TI, 26%, median duration 41 weeks) and some patients with HR‐MDS and 5q deletions (TI, 25.5%, median duration 26 weeks.[37, 38] Therefore, lenalidomide is a reasonable consideration in some patients with LR‐MDS without 5q deletions with primary or secondary resistance to ESA therapy.[10]
Immunosuppressive Therapy
Some patients with LR‐MDS respond to immunosuppressive therapy with antithymocyte globulin with or without cyclosporine. Characteristics that correlate with higher response rates: LR‐MDS, younger age (60 years), hypoplastic MDS, normal karyotype, human leukocyte antigen‐DR15 histocompatibility type, and presence of a paroxysmal nocturnal hemoglobinuria clone.[10, 39]
MANAGEMENT OF HR‐MDS
The goal of management for HR‐MDS is to modify the natural history of the disease and to prolong survival. In addition to a supportive care‐only approach or clinical trial referral, 3 standard therapeutic approaches are used for patients with HR‐MDS: alloHSCT, intensive chemotherapy, and DNMTi therapy. The use of intensive AML‐like chemotherapy for HR‐MDS is associated with high toxicity and very limited long‐term success. Despite recent innovations in the field of transplantation, only a minority of MDS patients undergo alloHSCT, as most patients with HR‐MDS are elderly and/or medically infirm. Even for the minority of patients who do undergo alloHSCT, relapse after alloHSCT remains a major challenge.
DNA Methyltransferase Inhibitor Therapy
5‐azacitidine (AZA), (Vidaza; Celgene Corp.) and decitabine (DAC) (Dacogen; Eisai, Inc.) are potent inhibitors of DNA methyltransferases, which are enzymes responsible for cytosine methylation.[38, 40] These so‐called differentiation agents appear to restore normal hematopoiesis for many MDS patients, and the approved regimens of DNMTi in MDS result in overall response rates in about 40% to 60% of patients. Unfortunately, complete remissions (CR) are rare (10%20%) and the duration of responses are also somewhat limited (median CR duration, 10 to 14 months).[41, 42, 43, 44] In randomized clinical trials, both AZA and DAC resulted in significant improvements in blood counts, reduction in transfusion needs, reduced infection rates, decreased risk of progression to AML, and improvements in patient‐reported quality‐of‐life measures.[41, 42, 43, 44] AZA, but not DAC, prolonged survival in HR‐MDS patients in a large randomized trial (median overall survival for the AZA group was 24.5 months compared to 15 months for a group of patients treated with 1 of 3 conventional care regimens).[41, 42, 43, 44] AZA and DAC have not been compared head to head in trials, but most experts recommend AZA for first‐line use in HR‐MDS based on its effect on survival.[10]
AZA and DAC have also been studied as treatments for patients with AML. These agents differ from traditional intensive chemotherapy, as both agents are commonly administered on an outpatient basis, and hematologic responses are generally expected after 4 to 6 cycles of treatment as compared to a single course of intensive cytarabine‐based induction chemotherapy used to treat AML.[45] Additionally, the impact on survival may not require the achievement of a CR based on the finding that MDS patients saw improved survival even in patients whose best responses were hematologic improvements.[46] However, therapy with DNMTi is not curative, and patients are maintained on treatment as long as they are responding and not experiencing major side effects. Still, all patients will eventually lose response to DNMTi.
CONCLUSIONS
MDS is a form of cancer that largely affects elderly patients and leads to a BM failure state and increased risk of leukemic transformation. MDS is underdiagnosed and is frequently overlooked in the differential diagnosis of anemia in the elderly. DNMTi, lenalidomide, and ESA therapy offer effective therapeutic options for many MDS patients, including some considered too old or frail for intensive medical interventions. The use of prognostic models help physicians and patients better understand the common course of patients with MDS and facilitate tailoring of risk‐adapted therapy. It is expected that our improved understanding of the genetic, epigenetic, and immunologic mechanisms that operate in MDS will help develop better classification tools and rationally design effective new therapies.
Acknowledgments
The authors thank Dr. Balazs Zsenits (Medical Director of the Rochester General Hospitalist Group, Rochester General Hospital, Rochester, NY) for his critical review of the article.
Disclosures: Dr. Steven Gore owned stock in Celgene until November 2011, received research support from Celgene and Novartis, and consulted for Celgene. Drs. B. Douglas Smith, Amer Zeidan, and Bishoy Faltas have no relevant disclosures.
- . Epidemiology of myelodysplastic syndromes. Am J Med. 2012;125:S2–S5.
- . Epidemiology, natural history, and practice patterns of patients with myelodysplastic syndromes in 2010. J Natl Compr Canc Netw. 2011;9:57–63.
- . Myelodysplastic syndromes: increasing disease awareness. Introduction. Am J Med. 2012;125:S1.
- , , , et al. Epidemiology of myelodysplastic syndromes and chronic myeloproliferative disorders in the United States, 2001–2004, using data from the NAACCR and SEER programs. Blood. 2008;112:45–52.
- , , , . Myelodysplastic syndromes: incidence and survival in the United States. Cancer. 2007;109:1536–1542.
- , , , , . Prevalence of anemia in persons 65 years and older in the United States: evidence for a high rate of unexplained anemia. Blood. 2004;104:2263–2268.
- . Myelodysplastic syndromes: increasing disease awareness. Discussion. Am J Med. 2012;125:S33–S34.
- . Why are myelodysplastic syndromes unrecognized and underdiagnosed? A primary care perspective. Am J Med. 2012;125:S15–S17.
- , . Clinical presentation, diagnosis, and prognosis of myelodysplastic syndromes. Am J Med. 2012;125:S6–S13.
- , , , et al. NCCN Clinical Practice Guidelines in Oncology: myelodysplastic syndromes. J Natl Compr Canc Netw. 2011;9:30–56.
- . Dysplasia has A differential diagnosis: distinguishing genuine myelodysplastic syndromes (MDS) from mimics, imitators, copycats and impostors. Curr Hematol Malig Rep. 2012;7:310–320.
- , . Interpreting new molecular genetics in myelodysplastic syndromes. Hematology Am Soc Hematol Educ Program. 2012;2012:56–64.
- , , , , . Updates in cytogenetics and molecular markers in MDS. Curr Hematol Malig Rep. 2011;6:126–135.
- , , , . Emerging roles of the spliceosomal machinery in myelodysplastic syndromes and other hematological disorders. Leukemia. 2012;26:2447–2454.
- , , , et al. Reduced natural killer (NK) function associated with high‐risk myelodysplastic syndrome (MDS) and reduced expression of activating NK receptors. Blood. 2007;109:4816–4824.
- , , , et al. Identification of RPS14 as a 5q− syndrome gene by RNA interference screen. Nature. 2008;451:335–339.
- , , . Unraveling the molecular pathophysiology of myelodysplastic syndromes. J Clin Oncol. 2011;29:504–515.
- , , , et al. Obesity, lifestyle factors, and risk of myelodysplastic syndromes in a large US cohort. Am J Epidemiol. 2009;169:1492–1499.
- , , , et al. Proposals for the classification of the myelodysplastic syndromes. Br J Haematol. 1982;51:189–199.
- , , , et al. World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues: report of the Clinical Advisory Committee Meeting–Airlie House, Virginia, November 1997. J Clin Oncol. 1999;17:3835–3849.
- , , , et al. WHO classification of MDS. In: World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues. Lyon, France: IARC Press; 2008.
- , , , et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89:2079–2088.
- , , , et al. Time‐dependent prognostic scoring system for predicting survival and leukemic evolution in myelodysplastic syndromes. J Clin Oncol. 2007;25:3503–3510.
- , , , et al. Impact of the degree of anemia on the outcome of patients with myelodysplastic syndrome and its integration into the WHO classification‐based Prognostic Scoring System (WPSS). Haematologica. 2011;96:1433–1440.
- , , , et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–2465.
- , , , . Prognostication in myelodysplastic syndromes: beyond the International Prognostic Scoring System (IPSS). Am J Med. 2013;126:e25.
- , . Myelodysplastic syndromes: who and when in the course of disease to transplant. Hematology Am Soc Hematol Educ Program. 2012;2012:49–55.
- , , , , , . “Low‐risk” myelodysplastic syndrome is associated with excessive apoptosis and an increased ratio of pro‐ versus anti‐apoptotic bcl‐2‐related proteins. Br J Haematol. 1998;103:1075–1082.
- , . Ineffective haemopoiesis and apoptosis in myelodysplastic syndromes. Br J Haematol. 1998;101:220–230.
- . Hematopoietic growth factors in myelodysplastic syndromes. Semin Oncol. 2011;38:635–647.
- , , , et al. Patient and physician characteristics associated with erythropoiesis‐stimulating agent use in patients with myelodysplastic syndromes. Haematologica. 2012;97:128–132.
- , , , et al. Predictive factors of response and survival in myelodysplastic syndrome treated with erythropoietin and G‐CSF: the GFM experience. Blood. 2008;111:574–582.
- , , , et al. Erythroid response to treatment with G‐CSF plus erythropoietin for the anaemia of patients with myelodysplastic syndromes: proposal for a predictive model. Br J Haematol. 1997;99:344–351.
- , , , et al. Erythropoiesis‐stimulating agents are not associated with increased risk of thrombosis in patients with myelodysplastic syndromes. Haematologica. 2012;97:15–20.
- , , , et al. Lenalidomide in the myelodysplastic syndrome with chromosome 5q deletion. N Engl J Med. 2006;355:1456–1465.
- , , , et al. A randomized phase 3 study of lenalidomide versus placebo in RBC transfusion‐dependent patients with low‐/‐ntermediate‐1‐risk myelodysplastic syndromes with del5q. Blood. 2011;118:3765–3776.
- , , , et al. Phase 2 study of lenalidomide in transfusion‐dependent, low‐risk, and intermediate‐1 risk myelodysplastic syndromes with karyotypes other than deletion 5q. Blood. 2008;111:86–93.
- , , , et al. Efficacy and safety of lenalidomide in intermediate‐2 or high‐risk myelodysplastic syndromes with 5q deletion: results of a phase 2 study. Blood. 2009;113:3947–3952.
- , , , , . Factors affecting response and survival in patients with myelodysplasia treated with immunosuppressive therapy. J Clin Oncol. 2008;26:2505–2511.
- , . DNA methyltransferase and histone deacetylase inhibitors in the treatment of myelodysplastic syndromes. Semin Hematol. 2008;45:23–30.
- , , , et al. Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher‐risk myelodysplastic syndromes: a randomised, open‐label, phase III study. Lancet Oncol. 2009;10:223–232.
- , , , et al. Randomized controlled trial of azacitidine in patients with the myelodysplastic syndrome: a study of the cancer and leukemia group B. J Clin Oncol. 2002;20:2429–2440.
- , , , et al. Decitabine improves patient outcomes in myelodysplastic syndromes: results of a phase III randomized study. Cancer. 2006;106:1794–1803.
- , , , et al. Low‐dose decitabine versus best supportive care in elderly patients with intermediate‐ or high‐risk myelodysplastic syndrome (MDS) ineligible for intensive chemotherapy: final results of the randomized phase III study of the European Organisation for Research and Treatment of Cancer Leukemia Group and the German MDS Study Group. J Clin Oncol. 2011;29:1987–1996.
- , , , et al. Further analysis of trials with azacitidine in patients with myelodysplastic syndrome: studies 8421, 8921, and 9221 by the Cancer and Leukemia Group B. J Clin Oncol. 2006;24:3895–3903.
- , , , et al. Prognostic factors for response and overall survival in 282 patients with higher‐risk myelodysplastic syndromes treated with azacitidine. Blood. 2011;117:403–411.
Myelodysplastic syndromes (MDS) comprise a heterogeneous group of clonal hematopoietic stem cell neoplasms characterized by dysplasia, ineffective hematopoiesis resulting in peripheral blood (PB) cytopenias affecting one or more cell lines, and a variable risk of progression to acute myeloid leukemia (AML). The last 15 years have witnessed significant advances in our understanding of the complex pathogenesis, classification and prognostication, and therapeutic approaches to MDS. As more elderly patients are diagnosed with MDS, encounters with hospitalized MDS patients or patients in whom MDS should be considered in the differential diagnosis are common events for today's hospitalists. In this review, we discuss the epidemiology, diagnosis, pathogenesis, prognostication, and therapies for MDS, with an emphasis on practical aspects that would be useful for hospitalists caring for these patients.
EPIDEMIOLOGY OF MDS
Although MDS is one of the most common hematologic malignancies, MDS remains understudied epidemiologically.[1, 2] Our understanding of the epidemiology improved after the implementation of reporting requirements to cancer registries, especially the Surveillance, Epidemiology, and End Results (SEER) database in 2001.[1, 2, 3] Age‐adjusted incidence of MDS in the United States ranged between 3.3 to 4.6 per 100,000 persons per year in the period between 2001 and 2008.[1, 2, 4] The majority of MDS patients are elderly, and because MDS incidence increases with age, the number of patients diagnosed with MDS is expected to continue to rise with the aging population.[1, 2, 5] MDS is more common in men compared to women, and in Caucasians compared to African Americans.[1, 2] Different estimates put MDS prevalence in the United States somewhere between 60,000 and 170,000 persons.[2, 6]
DIAGNOSIS OF MDS
Many patients with MDS are asymptomatic at diagnosis and only come to medical attention due to abnormal blood counts done routinely or for other reasons. This contributes to MDS being underdiagnosed. When cytopenias are not severe enough to cause symptoms, it is also frequently overlooked in patients with mild anemia or other cytopenias.[7] Together, being asymptomatic and having relatively mild cytopenias are probably the most important factors that lead to under‐recognition of MDS among primary care physicians (PCPs).[7, 8, 9] There is a misconception that anemia is normal in the elderly, and when patients are not symptomatic that a workup is not needed.[6, 7] This is compounded by a lack of awareness of the importance of making a diagnosis in these patients and of currently available therapies for MDS.[7, 8, 9]
Anemia is not a normal consequence of aging and is always a pathologic state with an underlying etiology.[6, 7] Because a significant number of elderly patients with unexplained anemia could have MDS, patients with symptomatic or progressive anemia, especially if associated with other cytopenias, should be considered for further evaluation.[7, 9] Diagnosis is important given the recent availability of effective therapies for MDS that can improve anemia, decrease transfusion needs, improve life quality, and potentially increase survival. MDS is generally an indolent disease with a relative stability of blood counts in comparison to AML, so prior blood counts and the tempo of the process is an important consideration.[9, 10] The National Comprehensive Cancer Network clinical practice guidelines recommend exclusion of nutritional deficiencies (iron, vitamin B12, folate) and other causes of anemia (eg, gastrointestinal bleeding, renal insufficiency, and anemia of inflammation), assessment of reticulocyte count and serum erythropoietin level, and evaluation of a PB smear for evidence of dysplasia as important initial steps.[10, 11] Eventually the diagnosis of MDS requires a bone marrow (BM) evaluation to confirm the diagnosis and exclude other BM failure states by evaluating for BM cellularity, cell maturation, dysplasia (which should be present in at least 10% of any the myeloid lineages), percentage of blasts (20%), iron stores and sideroblasts, cytogenetics, MDS‐specific fluorescence in situ hybridization (FISH) panels, flow cytometry, and other special testing.[9, 10] Despite extensive testing, MDS can sometimes be very difficult to differentiate from other bone marrow failure states (eg, hypoplastic MDS from aplastic anemia) (Table 1).[10, 11] In the absence of significant morbidity related to MDS, the definitive diagnosis of MDS can be usually made on an outpatient basis. It is important to ensure adequate follow‐up with PCPs postdischarge and/or outpatient hematologist referral for patients with unexplained cytopenias.
|
| Idiopathic cytopenia of undetermined significance: no significant dysplasia or MDS‐associated karyotypic aberrations |
| Acute myeloid leukemia: BM blasts 20%, presence of core‐binding characteristic cytogenetic aberrations: t(8;21), t(15;17), inv(16) defines AML regardless of BM blast count; AML can be associated with hepatosplenomegaly or myeloid sarcomas |
| Chronic myeloid leukemia: presence of Philadelphia chromosome t(9;22) positive, basophilia, and splenomegaly |
| Myelofibrosis: significant BM fibrosis, splenomegaly, and leukoerythroblastic picture in PB (teardrop and nucleated RBCs, left‐shifted myeloid cells) |
| Chronic myelomonocytic leukemia: significant PB monocytosis |
| MDS/MPN overlap syndromes: dysplasia with myeloproliferative characteristics such as splenomegaly, thrombocytosis, or leukocytosis |
| Infections: for example, HIV and parvovirus B19 infections |
| Myelophthisis: infiltration of BM with other tumors (eg, melanoma) with resultant PB cytopenias |
| Nutritional disturbances: B12, folate, and copper deficiency, and zinc and arsenic excess can mimic MDS |
| Medications: drugs that interfere with DNA synthesis such as HIV medications, chemotherapeutic agents, cotrimoxazole, methotrexate, azathioprine, and G‐CSF |
| Immune disorders: for example, LGL leukemia, lupus, or rheumatoid arthritis |
| Other acquired or congenital hematological disorders: for example, paroxysmal nocturnal hemoglobinuria, congenital dyserythropoietic anemia, dyskeratosis congenita |
PATHOGENESIS AND ETIOLOGY OF MDS
Ineffective hematopoiesis due to excessive apoptosis of hematopoietic precursors is a prominent feature of MDS, which explains the apparent paradox of hypercellular BM and PB cytopenias. Although not fully understood, complex epigenetic, genetic, and immunologic mechanisms contribute to the pathogenesis of MDS and account for disease heterogeneity. Aberrant silencing of tumor‐suppressor and DNA repair genes mediated by hypermethylation of their promoters is believed to play an important part in the pathogenesis of MDS.[12] This theory is supported by the unique sensitivity of MDS to drugs that reverse DNA methylation. Genetic abnormalities not only contribute to the pathogenesis of MDS, but are also among the strongest prognostic indicators for MDS patients, and can also affect therapeutic decisions. Clonal karyotypic abnormalities are observed in 50% of patients with MDS using conventional karyotyping.[12, 13] The most common chromosomal aberrations in MDS include deletions of the long arm of chromosome 5 (del5q), monosomy Y, monosomy 7 (del7) or deletion of its long arm (del7q), trisomy 8, del20q, and complex karyotypes (3 chromosomal aberrations).[12, 13] These cytogenetic abnormalities correlate with the prognosis of MDS (eg, poor prognosis with complex karyotypes and chromosome 7 deletions vs better prognosis with isolated del5q).[12, 13]
Recently, FISH assays and genome‐wide screening techniques (eg, single nucleotide polymorphism arrays, array‐based comparative genomic hybridization, whole genome or exome sequencing) have enabled detection of an increasing number of genetic aberrations and recurrent somatic molecular abnormalities in a significant number of MDS patients (eg, abnormalities of ASXL1, IDH1/IDH2, DNMT3, EZH2, TET2, and SF3B1 genes).[12, 14] Most affected genes are involved in the epigenetic regulation of transcription (DNA methylation and demethylation, histone posttranslational modification) or mRNA splicing.[12, 13, 14]
Immunologic aberrations have also been proposed to contribute to pathogenesis of MDS. For example, in early‐stage MDS, an aberrant immune attack on myeloid progenitors resulting in increased apoptosis can contribute to BM failure.[15] This is supported by association of some forms of MDS with autoimmune diseases and observed responses in some patients to immunosuppressive therapies. The relative contribution of pathogenetic mechanisms varies between the different MDS subtypes. For example, haploinsufficiency of cell‐cycle regulatory and ribosomal protein genes located in the commonly deleted region of 5q play an important role in the pathogenesis of MDS with isolated del5q (5q syndrome).[16] Mutations in the RNA spliceosomal machinery gene SF3B have been shown to play a role in the pathogenesis of the MDS subtype refractory anemia with ringed sideroblasts (RARS), with those patients with RARS carrying this mutation having a more favorable prognosis than those with the wild‐type gene.[14] Several excellent recent reviews provide detailed discussion of the complex pathophysiology of MDS.[12, 13, 14, 17]
Approximately 10% of MDS patients have secondary MDS (MDS occurring after chemotherapy or radiation therapy administration for treatment of another malignancy).[2] Aside from advancing age, the causative factors for the other 90% of cases (primary MDS) are unknown in most patients, although environmental and occupational exposures (eg, smoking, painting, insecticides, pesticides, organic solvents), and genetic syndromes (eg, DNA repair defects such as Fanconi's anemia) are implicated in some patients.[2, 10] Recently, an epidemiologic study found an increased MDS risk with obesity.[18]
PROGNOSTICATION OF MDS
MDS is a form of cancer, and most affected patients eventually die from cytopenic complications or leukemic progression. MDS is not a single disease but rather encompasses a group of heterogeneous subtypes with significantly different natural histories and pace of progression. Therefore, accurate risk stratification of MDS is necessary not only to predict survival and risk of leukemic progression, but also to help choose the most appropriate therapeutic option for individual patients. Information about prognosis should also be utilized when making management decisions with patients for other comorbid conditions (eg, major surgery). Two morphologically based classification systems are commonly used for MDS: the French‐American‐British (FAB) system and the World Health Organization (WHO) classification (Table 2), which most recently has supplanted the FAB system as the primary pathologic classification system.[19, 20, 21] Several prognostic models have been developed around the morphologic classifications to better account for relevant clinical and cytogenetic modifiers of this disease. Although some of these models have been validated by different groups, each of these models has limitations. Although the predictions generated by these models are generally accurate for the different prognostic categories to which the patient is assigned, the extent to which the prediction applies to an individual MDS patient can vary significantly. In addition, comorbid conditions affect survival of MDS patients and are not included in the specific scoring systems. For example, congestive heart failure and chronic obstructive lung disease were associated with shortened survival in MDS patients.[18]
| MDS WHO Class | PB Findings | BM Findings |
|---|---|---|
| ||
| Refractory cytopenias with unilineage dysplasia: includes refractory anemia; refractory neutropenia; refractory thrombocytopenia | Unicytopenia or bicytopenia; PB blasts 1% | BM blasts 5%; unilineage dysplasia (10% of cells in any myeloid lineage); 15% of erythroid precursors are ringed sideroblasts |
| Refractory anemia with ring sideroblasts | Anemia; PB blasts 1% | BM blasts 5%; erythroid dysplasia only; 15% of erythroid precursors are ringed sideroblasts |
| Refractory cytopenia with multilineage dysplasia | Cytopenia(s); PB blasts 1%; no Auer rods; 1 106/L monocytes | BM blasts 5% ; dysplasia (10% of cells in at least 2 myeloid lineages); no Auer rods |
| Refractory anemia with excess blasts‐1 | Cytopenia(s); PB blasts 5%; no Auer rods; 1 106/L monocytes | BM blasts 5%9%; unilineage or multilineage dysplasia; no Auer rods |
| Refractory anemia with excess blasts‐2 | Cytopenia(s); PB blasts 5%19%; Auer rods; 1 106/L monocytes | BM blasts 10%19%; unilineage or multilineage dysplasia; Auer rods |
| Myelodysplastic syndromeunclassified | Cytopenias; PB blasts 1% | BM blasts 5%; unequivocal dysplasia in 10% of cells at least one myeloid cell lines when accompanied by a cytogenetic abnormality considered as presumptive evidence for a diagnosis of MDS |
| MDS associated with isolated del5q | Anemia; normal to elevated platelet count; PB blasts 1% | BM blasts 5%; normal to elevated megakaryocytes with hypolobated nuclei; isolated del5q karyotypic abnormality; no Auer rods |
The International Prognostic Scoring System (IPSS) is the most widely used prognostic tool for MDS (Table 3).[22] In this model, an aggregate score is calculated based on points assigned to the percentage of blasts in BM, the number of PB cell lines affected by cytopenias, and the karyotype. Based on this point score, the patient is assigned to 1 of 4 categories that portend significantly different outcomes: low, intermediate‐1 (INT‐1), intermediate‐2 (INT‐2), and high risk. The IPSS was developed from a database of mostly untreated MDS patients and does not account for other important prognostic parameters such as transfusion dependence, depth of cytopenias, and extent/severity of lineage dysplasia.[22] The WHO Prognostic Scoring System was proposed to overcome some of these shortcomings.[23, 24] Efforts to continue to improve the prognostic models further led to a large international collaboration that compiled a much larger database and resulted in the development of a revised IPSS (IPSS‐R).[25] New discoveries of novel prognostic epigenetic, genetic, and immunologic determinants will likely result in the ongoing evolution of the current prognostic systems to further improve their discriminatory power.[26]
| Calculation of Score Value Based on Prognostic Variables | |||||
|---|---|---|---|---|---|
| Score Value | |||||
| 0 | 0.5 | 1.0 | 1.5 | 2.0 | |
| |||||
| Prognostic variable | |||||
| Bone marrow blasts (%)a | 5 | 510 | 1120 | 2130 | |
| Karyotypeb | Good | Intermediate | Poor | ||
| Number of peripheral blood cell line affected by cytopeniasc | 0 or 1 | 2 or 3 | |||
| Median Survival and Risk of Progression to AML According to the IPSS Risk Category in Absence of Therapy | |||||
| Overall Score | Risk Category | Percentage in the IPSS Population | Median Survival (Years) | Median Time From Diagnosis at Which 25% of Patients Progress to AML (Years) | |
| 0 | Low | 33% | 5.7 | 9.4 | |
| 0.51.0 | INT‐1 | 38% | 3.5 | 3.3 | |
| 1.52.0 | INT‐2 | 22% | 1.1 | 1.1 | |
| >2.5 | High | 7% | 0.4 | 0.2 | |
MANAGEMENT OF MDS
Most patients with MDS were treated historically with supportive measures only. The approval of 3 agents for treatment of MDS including the DNA methyltransferase inhibitors (DNMTi) azacitidine and decitabine, as well as the immunomodulatory agent lenalidomide, in the last decade advanced the care of MDS patients significantly (Table 4). Nonetheless, the use of allogeneic hematopoietic stem cell transplantation (alloHSCT) remains the only known curative modality for patients with MDS and should always be considered as a possible therapeutic option.[27] Unfortunately, the majority of patients with MDS are not considered candidates for alloHSCT due to age, comorbidities, and lack of suitable donors.[27] Therefore, most patients with MDS are managed with noncurative treatment and supportive paradigms. Treatment goals generally depend on the risk stratification for the particular individual, age, functional status, comorbidities, and importantly, the patient's individual preference. For medical decision‐making purposes, MDS is traditionally divided into 2 major risk categories: low‐risk (LR) and high‐risk (HR) groups. LR‐MDS includes the IPSS risk categories of low or INT‐1, whereas HR‐MDS is usually defined by the IPSS risk categories of INT‐2 and high. Newer classification tools (eg, IPSS‐R) and better molecular markers are expected to impact such categories as well as treatment recommendations in the future.[26]
|
| Azacitidine (5‐azacytidine, Vidaza) and decitabine (5‐aza,2‐deoxycytidine, Dacogen) |
| Class |
| Hypomethylating agents, azanucleosides |
| Mechanism of action |
| Epigenetic modulation by inhibition of DNA methyltransferase enzymes and other mechanisms |
| Indication |
| First line therapy for HR‐MDS, second line therapy for LR‐MDS after failure of other therapies such as ESAs, lenalidomide, or immunosuppressive agents |
| Approved regimens for MDS |
| Azacitidine: 75 mg/m2/day IV or SC for 7 days Q 4 weeks |
| Decitabine: 15 mg/m2 IV infusion over 3 hours, Q 8 hours for 3 days, Q 6 weeks or 20 mg/m2 IV infusion over 1 hour daily for 5 days Q 4 weeks |
| Common side effects |
| Fatigue |
| Development of or worsening cytopenias (neutropenia, thrombocytopenia, and anemia) and their complications (eg, infections, bleeding) |
| Gastrointestinal disturbances (nausea, vomiting, or diarrhea) |
| Oral ulcers and rarely mucositis |
| Injection site reactions (redness, pain) |
| Lenalidomide (Revlimid) |
| Class |
| Immunomodulatory agent |
| Mechanism of action |
| Modulation of immune responses, gene expression, angiogenesis, cytokines and cell‐cycle regulatory phosphatases, and possibly other mechanisms |
| Indication |
| First line therapy for LR‐MDS with del5q (also used commonly off label for LR‐MDS without del5q as second line of therapy after ESAs) |
| Approved regimens for MDS |
| 10 mg orally once daily |
| Common side effects |
| Skin rash, dryness, and pruritus |
| Fatigue |
| Muscle cramps |
| Development of or worsening cytopenias (neutropenia, thrombocytopenia, and anemia) and their complications (eg, infections, bleeding) |
| Gastrointestinal disturbances (nausea, vomiting, or diarrhea) |
Despite recent advances, supportive care for all patients with MDS remains a very important aspect of management, either in combination with other therapies or as sole therapy for frail patients who cannot tolerate further interventions. Supportive therapy focuses on maintaining a high quality of life and includes careful blood count monitoring, use of growth factors, use of transfusions and antibiotics as needed, and use of iron chelation therapy in some patients. Some of the common situations in which hospitalists encounter patients with MDS are listed in Table 5.
|
| Complications of cytopenias |
| Bleeding: local management based on bleeding site, platelet transfusions, and other blood products (eg, red blood cells, fresh frozen plasma) as appropriate, antifibrinolytics |
| Infections and neutropenic fevers: Antibiotics, antifungals, use of colony granulocyte‐stimulating factors or granulocyte infusions advised only in cases of uncontrolled severe infections or sepsis |
| Severe or symptomatic anemia: red blood transfusions as appropriate based on patient's comorbidities, all disease‐modifying drugs (lenalidomide, azacitidine, decitabine) and ESAs are slow acting and can take weeks to months before improving anemia |
| Complications of therapies |
| Neutropenic fevers: as above plus holding therapy |
| Most other side effects (see Table 4) are well tolerated and are managed symptomatically without requiring hospitalization. If needed hospitalization for side effects: symptomatic management and holding the drug |
| Other medical or surgical condition in a patient with MDS |
| Therapy as per the underlying medical condition. For therapeutic decisions (eg, decision to undergo major surgery), prognostication tools such as the IPSS and newer models can be used to inform medical decision making in consultation with an experienced hematologist |
MANAGEMENT OF LR‐MDS
In addition to supportive care or enrollment in clinical trials, therapies for LR‐MDS include erythropoiesis‐stimulating agents, lenalidomide, and immunosuppressive therapy.
Erythropoiesis‐Stimulating Agents
Anemia in MDS is a multifactorial process that includes ineffective erythropoiesis and suboptimal serum erythropoietin responses.[10, 28, 29] There are no randomized studies to suggest that erythropoiesis‐stimulating agents (ESA) therapy prolongs survival in MDS patients. Nonetheless, ESAs improve anemia significantly in some patients and are widely used.[30, 31] Approximately 20% to 30% of unselected MDS patients and about 40% of LR‐MDS patients achieve clinically meaningful erythroid responses with ESA therapy with a median response duration of 2 years.[30, 31] It is important to correct coexisting nutritional deficiencies (eg, iron or folate deficiency) to optimize responses to ESA.[10] Granulocyte colony‐stimulating factor can be synergistic with ESAs especially in patients with RARS.[10] Patients with LR‐MDS who have low endogenous serum erythropoietin levels (200500 mU/mL) and lower red blood cell (RBC) transfusion requirements (2 U per month) are more likely to respond to ESA therapy.[32, 33] Compared to certain solid tumors, ESA therapy in MDS has not been associated with an increased risk of thromboembolic events.[34]
Lenalidomide
5q syndrome is a subtype of MDS characterized by refractory macrocytic anemia, normal or elevated platelet counts, low BM blast percentage, small hypolobated dysplastic megakaryocytes, an isolated interstitial deletion in 5q, and an indolent natural history.[17, 35] Lenalidomide, an oral derivative of thalidomide, induces high response rates in LR‐MDS patients with 5q deletions, including hematologic improvements, RBC transfusion independence (TI) (56%67%, median duration >104 weeks), cytogenetic responses (50%76%), and complete remissions.[35, 36] These findings resulted in approval of lenalidomide (Revlimid; Celgene Corp., Summit, NJ) for patients with IPSS low or INT‐1 MDS with transfusion‐dependent anemia and 5q deletions with or without additional cytogenetic abnormalities. In addition, lenalidomide has some activity against LR‐MDS without 5q deletions (TI, 26%, median duration 41 weeks) and some patients with HR‐MDS and 5q deletions (TI, 25.5%, median duration 26 weeks.[37, 38] Therefore, lenalidomide is a reasonable consideration in some patients with LR‐MDS without 5q deletions with primary or secondary resistance to ESA therapy.[10]
Immunosuppressive Therapy
Some patients with LR‐MDS respond to immunosuppressive therapy with antithymocyte globulin with or without cyclosporine. Characteristics that correlate with higher response rates: LR‐MDS, younger age (60 years), hypoplastic MDS, normal karyotype, human leukocyte antigen‐DR15 histocompatibility type, and presence of a paroxysmal nocturnal hemoglobinuria clone.[10, 39]
MANAGEMENT OF HR‐MDS
The goal of management for HR‐MDS is to modify the natural history of the disease and to prolong survival. In addition to a supportive care‐only approach or clinical trial referral, 3 standard therapeutic approaches are used for patients with HR‐MDS: alloHSCT, intensive chemotherapy, and DNMTi therapy. The use of intensive AML‐like chemotherapy for HR‐MDS is associated with high toxicity and very limited long‐term success. Despite recent innovations in the field of transplantation, only a minority of MDS patients undergo alloHSCT, as most patients with HR‐MDS are elderly and/or medically infirm. Even for the minority of patients who do undergo alloHSCT, relapse after alloHSCT remains a major challenge.
DNA Methyltransferase Inhibitor Therapy
5‐azacitidine (AZA), (Vidaza; Celgene Corp.) and decitabine (DAC) (Dacogen; Eisai, Inc.) are potent inhibitors of DNA methyltransferases, which are enzymes responsible for cytosine methylation.[38, 40] These so‐called differentiation agents appear to restore normal hematopoiesis for many MDS patients, and the approved regimens of DNMTi in MDS result in overall response rates in about 40% to 60% of patients. Unfortunately, complete remissions (CR) are rare (10%20%) and the duration of responses are also somewhat limited (median CR duration, 10 to 14 months).[41, 42, 43, 44] In randomized clinical trials, both AZA and DAC resulted in significant improvements in blood counts, reduction in transfusion needs, reduced infection rates, decreased risk of progression to AML, and improvements in patient‐reported quality‐of‐life measures.[41, 42, 43, 44] AZA, but not DAC, prolonged survival in HR‐MDS patients in a large randomized trial (median overall survival for the AZA group was 24.5 months compared to 15 months for a group of patients treated with 1 of 3 conventional care regimens).[41, 42, 43, 44] AZA and DAC have not been compared head to head in trials, but most experts recommend AZA for first‐line use in HR‐MDS based on its effect on survival.[10]
AZA and DAC have also been studied as treatments for patients with AML. These agents differ from traditional intensive chemotherapy, as both agents are commonly administered on an outpatient basis, and hematologic responses are generally expected after 4 to 6 cycles of treatment as compared to a single course of intensive cytarabine‐based induction chemotherapy used to treat AML.[45] Additionally, the impact on survival may not require the achievement of a CR based on the finding that MDS patients saw improved survival even in patients whose best responses were hematologic improvements.[46] However, therapy with DNMTi is not curative, and patients are maintained on treatment as long as they are responding and not experiencing major side effects. Still, all patients will eventually lose response to DNMTi.
CONCLUSIONS
MDS is a form of cancer that largely affects elderly patients and leads to a BM failure state and increased risk of leukemic transformation. MDS is underdiagnosed and is frequently overlooked in the differential diagnosis of anemia in the elderly. DNMTi, lenalidomide, and ESA therapy offer effective therapeutic options for many MDS patients, including some considered too old or frail for intensive medical interventions. The use of prognostic models help physicians and patients better understand the common course of patients with MDS and facilitate tailoring of risk‐adapted therapy. It is expected that our improved understanding of the genetic, epigenetic, and immunologic mechanisms that operate in MDS will help develop better classification tools and rationally design effective new therapies.
Acknowledgments
The authors thank Dr. Balazs Zsenits (Medical Director of the Rochester General Hospitalist Group, Rochester General Hospital, Rochester, NY) for his critical review of the article.
Disclosures: Dr. Steven Gore owned stock in Celgene until November 2011, received research support from Celgene and Novartis, and consulted for Celgene. Drs. B. Douglas Smith, Amer Zeidan, and Bishoy Faltas have no relevant disclosures.
Myelodysplastic syndromes (MDS) comprise a heterogeneous group of clonal hematopoietic stem cell neoplasms characterized by dysplasia, ineffective hematopoiesis resulting in peripheral blood (PB) cytopenias affecting one or more cell lines, and a variable risk of progression to acute myeloid leukemia (AML). The last 15 years have witnessed significant advances in our understanding of the complex pathogenesis, classification and prognostication, and therapeutic approaches to MDS. As more elderly patients are diagnosed with MDS, encounters with hospitalized MDS patients or patients in whom MDS should be considered in the differential diagnosis are common events for today's hospitalists. In this review, we discuss the epidemiology, diagnosis, pathogenesis, prognostication, and therapies for MDS, with an emphasis on practical aspects that would be useful for hospitalists caring for these patients.
EPIDEMIOLOGY OF MDS
Although MDS is one of the most common hematologic malignancies, MDS remains understudied epidemiologically.[1, 2] Our understanding of the epidemiology improved after the implementation of reporting requirements to cancer registries, especially the Surveillance, Epidemiology, and End Results (SEER) database in 2001.[1, 2, 3] Age‐adjusted incidence of MDS in the United States ranged between 3.3 to 4.6 per 100,000 persons per year in the period between 2001 and 2008.[1, 2, 4] The majority of MDS patients are elderly, and because MDS incidence increases with age, the number of patients diagnosed with MDS is expected to continue to rise with the aging population.[1, 2, 5] MDS is more common in men compared to women, and in Caucasians compared to African Americans.[1, 2] Different estimates put MDS prevalence in the United States somewhere between 60,000 and 170,000 persons.[2, 6]
DIAGNOSIS OF MDS
Many patients with MDS are asymptomatic at diagnosis and only come to medical attention due to abnormal blood counts done routinely or for other reasons. This contributes to MDS being underdiagnosed. When cytopenias are not severe enough to cause symptoms, it is also frequently overlooked in patients with mild anemia or other cytopenias.[7] Together, being asymptomatic and having relatively mild cytopenias are probably the most important factors that lead to under‐recognition of MDS among primary care physicians (PCPs).[7, 8, 9] There is a misconception that anemia is normal in the elderly, and when patients are not symptomatic that a workup is not needed.[6, 7] This is compounded by a lack of awareness of the importance of making a diagnosis in these patients and of currently available therapies for MDS.[7, 8, 9]
Anemia is not a normal consequence of aging and is always a pathologic state with an underlying etiology.[6, 7] Because a significant number of elderly patients with unexplained anemia could have MDS, patients with symptomatic or progressive anemia, especially if associated with other cytopenias, should be considered for further evaluation.[7, 9] Diagnosis is important given the recent availability of effective therapies for MDS that can improve anemia, decrease transfusion needs, improve life quality, and potentially increase survival. MDS is generally an indolent disease with a relative stability of blood counts in comparison to AML, so prior blood counts and the tempo of the process is an important consideration.[9, 10] The National Comprehensive Cancer Network clinical practice guidelines recommend exclusion of nutritional deficiencies (iron, vitamin B12, folate) and other causes of anemia (eg, gastrointestinal bleeding, renal insufficiency, and anemia of inflammation), assessment of reticulocyte count and serum erythropoietin level, and evaluation of a PB smear for evidence of dysplasia as important initial steps.[10, 11] Eventually the diagnosis of MDS requires a bone marrow (BM) evaluation to confirm the diagnosis and exclude other BM failure states by evaluating for BM cellularity, cell maturation, dysplasia (which should be present in at least 10% of any the myeloid lineages), percentage of blasts (20%), iron stores and sideroblasts, cytogenetics, MDS‐specific fluorescence in situ hybridization (FISH) panels, flow cytometry, and other special testing.[9, 10] Despite extensive testing, MDS can sometimes be very difficult to differentiate from other bone marrow failure states (eg, hypoplastic MDS from aplastic anemia) (Table 1).[10, 11] In the absence of significant morbidity related to MDS, the definitive diagnosis of MDS can be usually made on an outpatient basis. It is important to ensure adequate follow‐up with PCPs postdischarge and/or outpatient hematologist referral for patients with unexplained cytopenias.
|
| Idiopathic cytopenia of undetermined significance: no significant dysplasia or MDS‐associated karyotypic aberrations |
| Acute myeloid leukemia: BM blasts 20%, presence of core‐binding characteristic cytogenetic aberrations: t(8;21), t(15;17), inv(16) defines AML regardless of BM blast count; AML can be associated with hepatosplenomegaly or myeloid sarcomas |
| Chronic myeloid leukemia: presence of Philadelphia chromosome t(9;22) positive, basophilia, and splenomegaly |
| Myelofibrosis: significant BM fibrosis, splenomegaly, and leukoerythroblastic picture in PB (teardrop and nucleated RBCs, left‐shifted myeloid cells) |
| Chronic myelomonocytic leukemia: significant PB monocytosis |
| MDS/MPN overlap syndromes: dysplasia with myeloproliferative characteristics such as splenomegaly, thrombocytosis, or leukocytosis |
| Infections: for example, HIV and parvovirus B19 infections |
| Myelophthisis: infiltration of BM with other tumors (eg, melanoma) with resultant PB cytopenias |
| Nutritional disturbances: B12, folate, and copper deficiency, and zinc and arsenic excess can mimic MDS |
| Medications: drugs that interfere with DNA synthesis such as HIV medications, chemotherapeutic agents, cotrimoxazole, methotrexate, azathioprine, and G‐CSF |
| Immune disorders: for example, LGL leukemia, lupus, or rheumatoid arthritis |
| Other acquired or congenital hematological disorders: for example, paroxysmal nocturnal hemoglobinuria, congenital dyserythropoietic anemia, dyskeratosis congenita |
PATHOGENESIS AND ETIOLOGY OF MDS
Ineffective hematopoiesis due to excessive apoptosis of hematopoietic precursors is a prominent feature of MDS, which explains the apparent paradox of hypercellular BM and PB cytopenias. Although not fully understood, complex epigenetic, genetic, and immunologic mechanisms contribute to the pathogenesis of MDS and account for disease heterogeneity. Aberrant silencing of tumor‐suppressor and DNA repair genes mediated by hypermethylation of their promoters is believed to play an important part in the pathogenesis of MDS.[12] This theory is supported by the unique sensitivity of MDS to drugs that reverse DNA methylation. Genetic abnormalities not only contribute to the pathogenesis of MDS, but are also among the strongest prognostic indicators for MDS patients, and can also affect therapeutic decisions. Clonal karyotypic abnormalities are observed in 50% of patients with MDS using conventional karyotyping.[12, 13] The most common chromosomal aberrations in MDS include deletions of the long arm of chromosome 5 (del5q), monosomy Y, monosomy 7 (del7) or deletion of its long arm (del7q), trisomy 8, del20q, and complex karyotypes (3 chromosomal aberrations).[12, 13] These cytogenetic abnormalities correlate with the prognosis of MDS (eg, poor prognosis with complex karyotypes and chromosome 7 deletions vs better prognosis with isolated del5q).[12, 13]
Recently, FISH assays and genome‐wide screening techniques (eg, single nucleotide polymorphism arrays, array‐based comparative genomic hybridization, whole genome or exome sequencing) have enabled detection of an increasing number of genetic aberrations and recurrent somatic molecular abnormalities in a significant number of MDS patients (eg, abnormalities of ASXL1, IDH1/IDH2, DNMT3, EZH2, TET2, and SF3B1 genes).[12, 14] Most affected genes are involved in the epigenetic regulation of transcription (DNA methylation and demethylation, histone posttranslational modification) or mRNA splicing.[12, 13, 14]
Immunologic aberrations have also been proposed to contribute to pathogenesis of MDS. For example, in early‐stage MDS, an aberrant immune attack on myeloid progenitors resulting in increased apoptosis can contribute to BM failure.[15] This is supported by association of some forms of MDS with autoimmune diseases and observed responses in some patients to immunosuppressive therapies. The relative contribution of pathogenetic mechanisms varies between the different MDS subtypes. For example, haploinsufficiency of cell‐cycle regulatory and ribosomal protein genes located in the commonly deleted region of 5q play an important role in the pathogenesis of MDS with isolated del5q (5q syndrome).[16] Mutations in the RNA spliceosomal machinery gene SF3B have been shown to play a role in the pathogenesis of the MDS subtype refractory anemia with ringed sideroblasts (RARS), with those patients with RARS carrying this mutation having a more favorable prognosis than those with the wild‐type gene.[14] Several excellent recent reviews provide detailed discussion of the complex pathophysiology of MDS.[12, 13, 14, 17]
Approximately 10% of MDS patients have secondary MDS (MDS occurring after chemotherapy or radiation therapy administration for treatment of another malignancy).[2] Aside from advancing age, the causative factors for the other 90% of cases (primary MDS) are unknown in most patients, although environmental and occupational exposures (eg, smoking, painting, insecticides, pesticides, organic solvents), and genetic syndromes (eg, DNA repair defects such as Fanconi's anemia) are implicated in some patients.[2, 10] Recently, an epidemiologic study found an increased MDS risk with obesity.[18]
PROGNOSTICATION OF MDS
MDS is a form of cancer, and most affected patients eventually die from cytopenic complications or leukemic progression. MDS is not a single disease but rather encompasses a group of heterogeneous subtypes with significantly different natural histories and pace of progression. Therefore, accurate risk stratification of MDS is necessary not only to predict survival and risk of leukemic progression, but also to help choose the most appropriate therapeutic option for individual patients. Information about prognosis should also be utilized when making management decisions with patients for other comorbid conditions (eg, major surgery). Two morphologically based classification systems are commonly used for MDS: the French‐American‐British (FAB) system and the World Health Organization (WHO) classification (Table 2), which most recently has supplanted the FAB system as the primary pathologic classification system.[19, 20, 21] Several prognostic models have been developed around the morphologic classifications to better account for relevant clinical and cytogenetic modifiers of this disease. Although some of these models have been validated by different groups, each of these models has limitations. Although the predictions generated by these models are generally accurate for the different prognostic categories to which the patient is assigned, the extent to which the prediction applies to an individual MDS patient can vary significantly. In addition, comorbid conditions affect survival of MDS patients and are not included in the specific scoring systems. For example, congestive heart failure and chronic obstructive lung disease were associated with shortened survival in MDS patients.[18]
| MDS WHO Class | PB Findings | BM Findings |
|---|---|---|
| ||
| Refractory cytopenias with unilineage dysplasia: includes refractory anemia; refractory neutropenia; refractory thrombocytopenia | Unicytopenia or bicytopenia; PB blasts 1% | BM blasts 5%; unilineage dysplasia (10% of cells in any myeloid lineage); 15% of erythroid precursors are ringed sideroblasts |
| Refractory anemia with ring sideroblasts | Anemia; PB blasts 1% | BM blasts 5%; erythroid dysplasia only; 15% of erythroid precursors are ringed sideroblasts |
| Refractory cytopenia with multilineage dysplasia | Cytopenia(s); PB blasts 1%; no Auer rods; 1 106/L monocytes | BM blasts 5% ; dysplasia (10% of cells in at least 2 myeloid lineages); no Auer rods |
| Refractory anemia with excess blasts‐1 | Cytopenia(s); PB blasts 5%; no Auer rods; 1 106/L monocytes | BM blasts 5%9%; unilineage or multilineage dysplasia; no Auer rods |
| Refractory anemia with excess blasts‐2 | Cytopenia(s); PB blasts 5%19%; Auer rods; 1 106/L monocytes | BM blasts 10%19%; unilineage or multilineage dysplasia; Auer rods |
| Myelodysplastic syndromeunclassified | Cytopenias; PB blasts 1% | BM blasts 5%; unequivocal dysplasia in 10% of cells at least one myeloid cell lines when accompanied by a cytogenetic abnormality considered as presumptive evidence for a diagnosis of MDS |
| MDS associated with isolated del5q | Anemia; normal to elevated platelet count; PB blasts 1% | BM blasts 5%; normal to elevated megakaryocytes with hypolobated nuclei; isolated del5q karyotypic abnormality; no Auer rods |
The International Prognostic Scoring System (IPSS) is the most widely used prognostic tool for MDS (Table 3).[22] In this model, an aggregate score is calculated based on points assigned to the percentage of blasts in BM, the number of PB cell lines affected by cytopenias, and the karyotype. Based on this point score, the patient is assigned to 1 of 4 categories that portend significantly different outcomes: low, intermediate‐1 (INT‐1), intermediate‐2 (INT‐2), and high risk. The IPSS was developed from a database of mostly untreated MDS patients and does not account for other important prognostic parameters such as transfusion dependence, depth of cytopenias, and extent/severity of lineage dysplasia.[22] The WHO Prognostic Scoring System was proposed to overcome some of these shortcomings.[23, 24] Efforts to continue to improve the prognostic models further led to a large international collaboration that compiled a much larger database and resulted in the development of a revised IPSS (IPSS‐R).[25] New discoveries of novel prognostic epigenetic, genetic, and immunologic determinants will likely result in the ongoing evolution of the current prognostic systems to further improve their discriminatory power.[26]
| Calculation of Score Value Based on Prognostic Variables | |||||
|---|---|---|---|---|---|
| Score Value | |||||
| 0 | 0.5 | 1.0 | 1.5 | 2.0 | |
| |||||
| Prognostic variable | |||||
| Bone marrow blasts (%)a | 5 | 510 | 1120 | 2130 | |
| Karyotypeb | Good | Intermediate | Poor | ||
| Number of peripheral blood cell line affected by cytopeniasc | 0 or 1 | 2 or 3 | |||
| Median Survival and Risk of Progression to AML According to the IPSS Risk Category in Absence of Therapy | |||||
| Overall Score | Risk Category | Percentage in the IPSS Population | Median Survival (Years) | Median Time From Diagnosis at Which 25% of Patients Progress to AML (Years) | |
| 0 | Low | 33% | 5.7 | 9.4 | |
| 0.51.0 | INT‐1 | 38% | 3.5 | 3.3 | |
| 1.52.0 | INT‐2 | 22% | 1.1 | 1.1 | |
| >2.5 | High | 7% | 0.4 | 0.2 | |
MANAGEMENT OF MDS
Most patients with MDS were treated historically with supportive measures only. The approval of 3 agents for treatment of MDS including the DNA methyltransferase inhibitors (DNMTi) azacitidine and decitabine, as well as the immunomodulatory agent lenalidomide, in the last decade advanced the care of MDS patients significantly (Table 4). Nonetheless, the use of allogeneic hematopoietic stem cell transplantation (alloHSCT) remains the only known curative modality for patients with MDS and should always be considered as a possible therapeutic option.[27] Unfortunately, the majority of patients with MDS are not considered candidates for alloHSCT due to age, comorbidities, and lack of suitable donors.[27] Therefore, most patients with MDS are managed with noncurative treatment and supportive paradigms. Treatment goals generally depend on the risk stratification for the particular individual, age, functional status, comorbidities, and importantly, the patient's individual preference. For medical decision‐making purposes, MDS is traditionally divided into 2 major risk categories: low‐risk (LR) and high‐risk (HR) groups. LR‐MDS includes the IPSS risk categories of low or INT‐1, whereas HR‐MDS is usually defined by the IPSS risk categories of INT‐2 and high. Newer classification tools (eg, IPSS‐R) and better molecular markers are expected to impact such categories as well as treatment recommendations in the future.[26]
|
| Azacitidine (5‐azacytidine, Vidaza) and decitabine (5‐aza,2‐deoxycytidine, Dacogen) |
| Class |
| Hypomethylating agents, azanucleosides |
| Mechanism of action |
| Epigenetic modulation by inhibition of DNA methyltransferase enzymes and other mechanisms |
| Indication |
| First line therapy for HR‐MDS, second line therapy for LR‐MDS after failure of other therapies such as ESAs, lenalidomide, or immunosuppressive agents |
| Approved regimens for MDS |
| Azacitidine: 75 mg/m2/day IV or SC for 7 days Q 4 weeks |
| Decitabine: 15 mg/m2 IV infusion over 3 hours, Q 8 hours for 3 days, Q 6 weeks or 20 mg/m2 IV infusion over 1 hour daily for 5 days Q 4 weeks |
| Common side effects |
| Fatigue |
| Development of or worsening cytopenias (neutropenia, thrombocytopenia, and anemia) and their complications (eg, infections, bleeding) |
| Gastrointestinal disturbances (nausea, vomiting, or diarrhea) |
| Oral ulcers and rarely mucositis |
| Injection site reactions (redness, pain) |
| Lenalidomide (Revlimid) |
| Class |
| Immunomodulatory agent |
| Mechanism of action |
| Modulation of immune responses, gene expression, angiogenesis, cytokines and cell‐cycle regulatory phosphatases, and possibly other mechanisms |
| Indication |
| First line therapy for LR‐MDS with del5q (also used commonly off label for LR‐MDS without del5q as second line of therapy after ESAs) |
| Approved regimens for MDS |
| 10 mg orally once daily |
| Common side effects |
| Skin rash, dryness, and pruritus |
| Fatigue |
| Muscle cramps |
| Development of or worsening cytopenias (neutropenia, thrombocytopenia, and anemia) and their complications (eg, infections, bleeding) |
| Gastrointestinal disturbances (nausea, vomiting, or diarrhea) |
Despite recent advances, supportive care for all patients with MDS remains a very important aspect of management, either in combination with other therapies or as sole therapy for frail patients who cannot tolerate further interventions. Supportive therapy focuses on maintaining a high quality of life and includes careful blood count monitoring, use of growth factors, use of transfusions and antibiotics as needed, and use of iron chelation therapy in some patients. Some of the common situations in which hospitalists encounter patients with MDS are listed in Table 5.
|
| Complications of cytopenias |
| Bleeding: local management based on bleeding site, platelet transfusions, and other blood products (eg, red blood cells, fresh frozen plasma) as appropriate, antifibrinolytics |
| Infections and neutropenic fevers: Antibiotics, antifungals, use of colony granulocyte‐stimulating factors or granulocyte infusions advised only in cases of uncontrolled severe infections or sepsis |
| Severe or symptomatic anemia: red blood transfusions as appropriate based on patient's comorbidities, all disease‐modifying drugs (lenalidomide, azacitidine, decitabine) and ESAs are slow acting and can take weeks to months before improving anemia |
| Complications of therapies |
| Neutropenic fevers: as above plus holding therapy |
| Most other side effects (see Table 4) are well tolerated and are managed symptomatically without requiring hospitalization. If needed hospitalization for side effects: symptomatic management and holding the drug |
| Other medical or surgical condition in a patient with MDS |
| Therapy as per the underlying medical condition. For therapeutic decisions (eg, decision to undergo major surgery), prognostication tools such as the IPSS and newer models can be used to inform medical decision making in consultation with an experienced hematologist |
MANAGEMENT OF LR‐MDS
In addition to supportive care or enrollment in clinical trials, therapies for LR‐MDS include erythropoiesis‐stimulating agents, lenalidomide, and immunosuppressive therapy.
Erythropoiesis‐Stimulating Agents
Anemia in MDS is a multifactorial process that includes ineffective erythropoiesis and suboptimal serum erythropoietin responses.[10, 28, 29] There are no randomized studies to suggest that erythropoiesis‐stimulating agents (ESA) therapy prolongs survival in MDS patients. Nonetheless, ESAs improve anemia significantly in some patients and are widely used.[30, 31] Approximately 20% to 30% of unselected MDS patients and about 40% of LR‐MDS patients achieve clinically meaningful erythroid responses with ESA therapy with a median response duration of 2 years.[30, 31] It is important to correct coexisting nutritional deficiencies (eg, iron or folate deficiency) to optimize responses to ESA.[10] Granulocyte colony‐stimulating factor can be synergistic with ESAs especially in patients with RARS.[10] Patients with LR‐MDS who have low endogenous serum erythropoietin levels (200500 mU/mL) and lower red blood cell (RBC) transfusion requirements (2 U per month) are more likely to respond to ESA therapy.[32, 33] Compared to certain solid tumors, ESA therapy in MDS has not been associated with an increased risk of thromboembolic events.[34]
Lenalidomide
5q syndrome is a subtype of MDS characterized by refractory macrocytic anemia, normal or elevated platelet counts, low BM blast percentage, small hypolobated dysplastic megakaryocytes, an isolated interstitial deletion in 5q, and an indolent natural history.[17, 35] Lenalidomide, an oral derivative of thalidomide, induces high response rates in LR‐MDS patients with 5q deletions, including hematologic improvements, RBC transfusion independence (TI) (56%67%, median duration >104 weeks), cytogenetic responses (50%76%), and complete remissions.[35, 36] These findings resulted in approval of lenalidomide (Revlimid; Celgene Corp., Summit, NJ) for patients with IPSS low or INT‐1 MDS with transfusion‐dependent anemia and 5q deletions with or without additional cytogenetic abnormalities. In addition, lenalidomide has some activity against LR‐MDS without 5q deletions (TI, 26%, median duration 41 weeks) and some patients with HR‐MDS and 5q deletions (TI, 25.5%, median duration 26 weeks.[37, 38] Therefore, lenalidomide is a reasonable consideration in some patients with LR‐MDS without 5q deletions with primary or secondary resistance to ESA therapy.[10]
Immunosuppressive Therapy
Some patients with LR‐MDS respond to immunosuppressive therapy with antithymocyte globulin with or without cyclosporine. Characteristics that correlate with higher response rates: LR‐MDS, younger age (60 years), hypoplastic MDS, normal karyotype, human leukocyte antigen‐DR15 histocompatibility type, and presence of a paroxysmal nocturnal hemoglobinuria clone.[10, 39]
MANAGEMENT OF HR‐MDS
The goal of management for HR‐MDS is to modify the natural history of the disease and to prolong survival. In addition to a supportive care‐only approach or clinical trial referral, 3 standard therapeutic approaches are used for patients with HR‐MDS: alloHSCT, intensive chemotherapy, and DNMTi therapy. The use of intensive AML‐like chemotherapy for HR‐MDS is associated with high toxicity and very limited long‐term success. Despite recent innovations in the field of transplantation, only a minority of MDS patients undergo alloHSCT, as most patients with HR‐MDS are elderly and/or medically infirm. Even for the minority of patients who do undergo alloHSCT, relapse after alloHSCT remains a major challenge.
DNA Methyltransferase Inhibitor Therapy
5‐azacitidine (AZA), (Vidaza; Celgene Corp.) and decitabine (DAC) (Dacogen; Eisai, Inc.) are potent inhibitors of DNA methyltransferases, which are enzymes responsible for cytosine methylation.[38, 40] These so‐called differentiation agents appear to restore normal hematopoiesis for many MDS patients, and the approved regimens of DNMTi in MDS result in overall response rates in about 40% to 60% of patients. Unfortunately, complete remissions (CR) are rare (10%20%) and the duration of responses are also somewhat limited (median CR duration, 10 to 14 months).[41, 42, 43, 44] In randomized clinical trials, both AZA and DAC resulted in significant improvements in blood counts, reduction in transfusion needs, reduced infection rates, decreased risk of progression to AML, and improvements in patient‐reported quality‐of‐life measures.[41, 42, 43, 44] AZA, but not DAC, prolonged survival in HR‐MDS patients in a large randomized trial (median overall survival for the AZA group was 24.5 months compared to 15 months for a group of patients treated with 1 of 3 conventional care regimens).[41, 42, 43, 44] AZA and DAC have not been compared head to head in trials, but most experts recommend AZA for first‐line use in HR‐MDS based on its effect on survival.[10]
AZA and DAC have also been studied as treatments for patients with AML. These agents differ from traditional intensive chemotherapy, as both agents are commonly administered on an outpatient basis, and hematologic responses are generally expected after 4 to 6 cycles of treatment as compared to a single course of intensive cytarabine‐based induction chemotherapy used to treat AML.[45] Additionally, the impact on survival may not require the achievement of a CR based on the finding that MDS patients saw improved survival even in patients whose best responses were hematologic improvements.[46] However, therapy with DNMTi is not curative, and patients are maintained on treatment as long as they are responding and not experiencing major side effects. Still, all patients will eventually lose response to DNMTi.
CONCLUSIONS
MDS is a form of cancer that largely affects elderly patients and leads to a BM failure state and increased risk of leukemic transformation. MDS is underdiagnosed and is frequently overlooked in the differential diagnosis of anemia in the elderly. DNMTi, lenalidomide, and ESA therapy offer effective therapeutic options for many MDS patients, including some considered too old or frail for intensive medical interventions. The use of prognostic models help physicians and patients better understand the common course of patients with MDS and facilitate tailoring of risk‐adapted therapy. It is expected that our improved understanding of the genetic, epigenetic, and immunologic mechanisms that operate in MDS will help develop better classification tools and rationally design effective new therapies.
Acknowledgments
The authors thank Dr. Balazs Zsenits (Medical Director of the Rochester General Hospitalist Group, Rochester General Hospital, Rochester, NY) for his critical review of the article.
Disclosures: Dr. Steven Gore owned stock in Celgene until November 2011, received research support from Celgene and Novartis, and consulted for Celgene. Drs. B. Douglas Smith, Amer Zeidan, and Bishoy Faltas have no relevant disclosures.
- . Epidemiology of myelodysplastic syndromes. Am J Med. 2012;125:S2–S5.
- . Epidemiology, natural history, and practice patterns of patients with myelodysplastic syndromes in 2010. J Natl Compr Canc Netw. 2011;9:57–63.
- . Myelodysplastic syndromes: increasing disease awareness. Introduction. Am J Med. 2012;125:S1.
- , , , et al. Epidemiology of myelodysplastic syndromes and chronic myeloproliferative disorders in the United States, 2001–2004, using data from the NAACCR and SEER programs. Blood. 2008;112:45–52.
- , , , . Myelodysplastic syndromes: incidence and survival in the United States. Cancer. 2007;109:1536–1542.
- , , , , . Prevalence of anemia in persons 65 years and older in the United States: evidence for a high rate of unexplained anemia. Blood. 2004;104:2263–2268.
- . Myelodysplastic syndromes: increasing disease awareness. Discussion. Am J Med. 2012;125:S33–S34.
- . Why are myelodysplastic syndromes unrecognized and underdiagnosed? A primary care perspective. Am J Med. 2012;125:S15–S17.
- , . Clinical presentation, diagnosis, and prognosis of myelodysplastic syndromes. Am J Med. 2012;125:S6–S13.
- , , , et al. NCCN Clinical Practice Guidelines in Oncology: myelodysplastic syndromes. J Natl Compr Canc Netw. 2011;9:30–56.
- . Dysplasia has A differential diagnosis: distinguishing genuine myelodysplastic syndromes (MDS) from mimics, imitators, copycats and impostors. Curr Hematol Malig Rep. 2012;7:310–320.
- , . Interpreting new molecular genetics in myelodysplastic syndromes. Hematology Am Soc Hematol Educ Program. 2012;2012:56–64.
- , , , , . Updates in cytogenetics and molecular markers in MDS. Curr Hematol Malig Rep. 2011;6:126–135.
- , , , . Emerging roles of the spliceosomal machinery in myelodysplastic syndromes and other hematological disorders. Leukemia. 2012;26:2447–2454.
- , , , et al. Reduced natural killer (NK) function associated with high‐risk myelodysplastic syndrome (MDS) and reduced expression of activating NK receptors. Blood. 2007;109:4816–4824.
- , , , et al. Identification of RPS14 as a 5q− syndrome gene by RNA interference screen. Nature. 2008;451:335–339.
- , , . Unraveling the molecular pathophysiology of myelodysplastic syndromes. J Clin Oncol. 2011;29:504–515.
- , , , et al. Obesity, lifestyle factors, and risk of myelodysplastic syndromes in a large US cohort. Am J Epidemiol. 2009;169:1492–1499.
- , , , et al. Proposals for the classification of the myelodysplastic syndromes. Br J Haematol. 1982;51:189–199.
- , , , et al. World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues: report of the Clinical Advisory Committee Meeting–Airlie House, Virginia, November 1997. J Clin Oncol. 1999;17:3835–3849.
- , , , et al. WHO classification of MDS. In: World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues. Lyon, France: IARC Press; 2008.
- , , , et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89:2079–2088.
- , , , et al. Time‐dependent prognostic scoring system for predicting survival and leukemic evolution in myelodysplastic syndromes. J Clin Oncol. 2007;25:3503–3510.
- , , , et al. Impact of the degree of anemia on the outcome of patients with myelodysplastic syndrome and its integration into the WHO classification‐based Prognostic Scoring System (WPSS). Haematologica. 2011;96:1433–1440.
- , , , et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–2465.
- , , , . Prognostication in myelodysplastic syndromes: beyond the International Prognostic Scoring System (IPSS). Am J Med. 2013;126:e25.
- , . Myelodysplastic syndromes: who and when in the course of disease to transplant. Hematology Am Soc Hematol Educ Program. 2012;2012:49–55.
- , , , , , . “Low‐risk” myelodysplastic syndrome is associated with excessive apoptosis and an increased ratio of pro‐ versus anti‐apoptotic bcl‐2‐related proteins. Br J Haematol. 1998;103:1075–1082.
- , . Ineffective haemopoiesis and apoptosis in myelodysplastic syndromes. Br J Haematol. 1998;101:220–230.
- . Hematopoietic growth factors in myelodysplastic syndromes. Semin Oncol. 2011;38:635–647.
- , , , et al. Patient and physician characteristics associated with erythropoiesis‐stimulating agent use in patients with myelodysplastic syndromes. Haematologica. 2012;97:128–132.
- , , , et al. Predictive factors of response and survival in myelodysplastic syndrome treated with erythropoietin and G‐CSF: the GFM experience. Blood. 2008;111:574–582.
- , , , et al. Erythroid response to treatment with G‐CSF plus erythropoietin for the anaemia of patients with myelodysplastic syndromes: proposal for a predictive model. Br J Haematol. 1997;99:344–351.
- , , , et al. Erythropoiesis‐stimulating agents are not associated with increased risk of thrombosis in patients with myelodysplastic syndromes. Haematologica. 2012;97:15–20.
- , , , et al. Lenalidomide in the myelodysplastic syndrome with chromosome 5q deletion. N Engl J Med. 2006;355:1456–1465.
- , , , et al. A randomized phase 3 study of lenalidomide versus placebo in RBC transfusion‐dependent patients with low‐/‐ntermediate‐1‐risk myelodysplastic syndromes with del5q. Blood. 2011;118:3765–3776.
- , , , et al. Phase 2 study of lenalidomide in transfusion‐dependent, low‐risk, and intermediate‐1 risk myelodysplastic syndromes with karyotypes other than deletion 5q. Blood. 2008;111:86–93.
- , , , et al. Efficacy and safety of lenalidomide in intermediate‐2 or high‐risk myelodysplastic syndromes with 5q deletion: results of a phase 2 study. Blood. 2009;113:3947–3952.
- , , , , . Factors affecting response and survival in patients with myelodysplasia treated with immunosuppressive therapy. J Clin Oncol. 2008;26:2505–2511.
- , . DNA methyltransferase and histone deacetylase inhibitors in the treatment of myelodysplastic syndromes. Semin Hematol. 2008;45:23–30.
- , , , et al. Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher‐risk myelodysplastic syndromes: a randomised, open‐label, phase III study. Lancet Oncol. 2009;10:223–232.
- , , , et al. Randomized controlled trial of azacitidine in patients with the myelodysplastic syndrome: a study of the cancer and leukemia group B. J Clin Oncol. 2002;20:2429–2440.
- , , , et al. Decitabine improves patient outcomes in myelodysplastic syndromes: results of a phase III randomized study. Cancer. 2006;106:1794–1803.
- , , , et al. Low‐dose decitabine versus best supportive care in elderly patients with intermediate‐ or high‐risk myelodysplastic syndrome (MDS) ineligible for intensive chemotherapy: final results of the randomized phase III study of the European Organisation for Research and Treatment of Cancer Leukemia Group and the German MDS Study Group. J Clin Oncol. 2011;29:1987–1996.
- , , , et al. Further analysis of trials with azacitidine in patients with myelodysplastic syndrome: studies 8421, 8921, and 9221 by the Cancer and Leukemia Group B. J Clin Oncol. 2006;24:3895–3903.
- , , , et al. Prognostic factors for response and overall survival in 282 patients with higher‐risk myelodysplastic syndromes treated with azacitidine. Blood. 2011;117:403–411.
- . Epidemiology of myelodysplastic syndromes. Am J Med. 2012;125:S2–S5.
- . Epidemiology, natural history, and practice patterns of patients with myelodysplastic syndromes in 2010. J Natl Compr Canc Netw. 2011;9:57–63.
- . Myelodysplastic syndromes: increasing disease awareness. Introduction. Am J Med. 2012;125:S1.
- , , , et al. Epidemiology of myelodysplastic syndromes and chronic myeloproliferative disorders in the United States, 2001–2004, using data from the NAACCR and SEER programs. Blood. 2008;112:45–52.
- , , , . Myelodysplastic syndromes: incidence and survival in the United States. Cancer. 2007;109:1536–1542.
- , , , , . Prevalence of anemia in persons 65 years and older in the United States: evidence for a high rate of unexplained anemia. Blood. 2004;104:2263–2268.
- . Myelodysplastic syndromes: increasing disease awareness. Discussion. Am J Med. 2012;125:S33–S34.
- . Why are myelodysplastic syndromes unrecognized and underdiagnosed? A primary care perspective. Am J Med. 2012;125:S15–S17.
- , . Clinical presentation, diagnosis, and prognosis of myelodysplastic syndromes. Am J Med. 2012;125:S6–S13.
- , , , et al. NCCN Clinical Practice Guidelines in Oncology: myelodysplastic syndromes. J Natl Compr Canc Netw. 2011;9:30–56.
- . Dysplasia has A differential diagnosis: distinguishing genuine myelodysplastic syndromes (MDS) from mimics, imitators, copycats and impostors. Curr Hematol Malig Rep. 2012;7:310–320.
- , . Interpreting new molecular genetics in myelodysplastic syndromes. Hematology Am Soc Hematol Educ Program. 2012;2012:56–64.
- , , , , . Updates in cytogenetics and molecular markers in MDS. Curr Hematol Malig Rep. 2011;6:126–135.
- , , , . Emerging roles of the spliceosomal machinery in myelodysplastic syndromes and other hematological disorders. Leukemia. 2012;26:2447–2454.
- , , , et al. Reduced natural killer (NK) function associated with high‐risk myelodysplastic syndrome (MDS) and reduced expression of activating NK receptors. Blood. 2007;109:4816–4824.
- , , , et al. Identification of RPS14 as a 5q− syndrome gene by RNA interference screen. Nature. 2008;451:335–339.
- , , . Unraveling the molecular pathophysiology of myelodysplastic syndromes. J Clin Oncol. 2011;29:504–515.
- , , , et al. Obesity, lifestyle factors, and risk of myelodysplastic syndromes in a large US cohort. Am J Epidemiol. 2009;169:1492–1499.
- , , , et al. Proposals for the classification of the myelodysplastic syndromes. Br J Haematol. 1982;51:189–199.
- , , , et al. World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues: report of the Clinical Advisory Committee Meeting–Airlie House, Virginia, November 1997. J Clin Oncol. 1999;17:3835–3849.
- , , , et al. WHO classification of MDS. In: World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues. Lyon, France: IARC Press; 2008.
- , , , et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89:2079–2088.
- , , , et al. Time‐dependent prognostic scoring system for predicting survival and leukemic evolution in myelodysplastic syndromes. J Clin Oncol. 2007;25:3503–3510.
- , , , et al. Impact of the degree of anemia on the outcome of patients with myelodysplastic syndrome and its integration into the WHO classification‐based Prognostic Scoring System (WPSS). Haematologica. 2011;96:1433–1440.
- , , , et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–2465.
- , , , . Prognostication in myelodysplastic syndromes: beyond the International Prognostic Scoring System (IPSS). Am J Med. 2013;126:e25.
- , . Myelodysplastic syndromes: who and when in the course of disease to transplant. Hematology Am Soc Hematol Educ Program. 2012;2012:49–55.
- , , , , , . “Low‐risk” myelodysplastic syndrome is associated with excessive apoptosis and an increased ratio of pro‐ versus anti‐apoptotic bcl‐2‐related proteins. Br J Haematol. 1998;103:1075–1082.
- , . Ineffective haemopoiesis and apoptosis in myelodysplastic syndromes. Br J Haematol. 1998;101:220–230.
- . Hematopoietic growth factors in myelodysplastic syndromes. Semin Oncol. 2011;38:635–647.
- , , , et al. Patient and physician characteristics associated with erythropoiesis‐stimulating agent use in patients with myelodysplastic syndromes. Haematologica. 2012;97:128–132.
- , , , et al. Predictive factors of response and survival in myelodysplastic syndrome treated with erythropoietin and G‐CSF: the GFM experience. Blood. 2008;111:574–582.
- , , , et al. Erythroid response to treatment with G‐CSF plus erythropoietin for the anaemia of patients with myelodysplastic syndromes: proposal for a predictive model. Br J Haematol. 1997;99:344–351.
- , , , et al. Erythropoiesis‐stimulating agents are not associated with increased risk of thrombosis in patients with myelodysplastic syndromes. Haematologica. 2012;97:15–20.
- , , , et al. Lenalidomide in the myelodysplastic syndrome with chromosome 5q deletion. N Engl J Med. 2006;355:1456–1465.
- , , , et al. A randomized phase 3 study of lenalidomide versus placebo in RBC transfusion‐dependent patients with low‐/‐ntermediate‐1‐risk myelodysplastic syndromes with del5q. Blood. 2011;118:3765–3776.
- , , , et al. Phase 2 study of lenalidomide in transfusion‐dependent, low‐risk, and intermediate‐1 risk myelodysplastic syndromes with karyotypes other than deletion 5q. Blood. 2008;111:86–93.
- , , , et al. Efficacy and safety of lenalidomide in intermediate‐2 or high‐risk myelodysplastic syndromes with 5q deletion: results of a phase 2 study. Blood. 2009;113:3947–3952.
- , , , , . Factors affecting response and survival in patients with myelodysplasia treated with immunosuppressive therapy. J Clin Oncol. 2008;26:2505–2511.
- , . DNA methyltransferase and histone deacetylase inhibitors in the treatment of myelodysplastic syndromes. Semin Hematol. 2008;45:23–30.
- , , , et al. Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher‐risk myelodysplastic syndromes: a randomised, open‐label, phase III study. Lancet Oncol. 2009;10:223–232.
- , , , et al. Randomized controlled trial of azacitidine in patients with the myelodysplastic syndrome: a study of the cancer and leukemia group B. J Clin Oncol. 2002;20:2429–2440.
- , , , et al. Decitabine improves patient outcomes in myelodysplastic syndromes: results of a phase III randomized study. Cancer. 2006;106:1794–1803.
- , , , et al. Low‐dose decitabine versus best supportive care in elderly patients with intermediate‐ or high‐risk myelodysplastic syndrome (MDS) ineligible for intensive chemotherapy: final results of the randomized phase III study of the European Organisation for Research and Treatment of Cancer Leukemia Group and the German MDS Study Group. J Clin Oncol. 2011;29:1987–1996.
- , , , et al. Further analysis of trials with azacitidine in patients with myelodysplastic syndrome: studies 8421, 8921, and 9221 by the Cancer and Leukemia Group B. J Clin Oncol. 2006;24:3895–3903.
- , , , et al. Prognostic factors for response and overall survival in 282 patients with higher‐risk myelodysplastic syndromes treated with azacitidine. Blood. 2011;117:403–411.
Dabigatran Etexilate
Vitamin K antagonists (VKAs) such as warfarin have been the backbone of oral anticoagulation in clinical practice since the middle of the last century. Despite their efficacy, VKAs have well‐recognized limitations that have led to their underutilization in patients who would otherwise be candidates for oral anticoagulation.14 These limitations include a narrow therapeutic window and significant intra‐ and interindividual variability in dose requirements as well as numerous drugdrug and drugfood interactions.59 Therefore, VKAs require close laboratory monitoring to prevent excessive or under‐anticoagulation, and maintaining therapeutic anticoagulation with VKAs remains a challenging task in many patients.2 It has been shown that 30%50% of international normalized ratio (INR) results fall outside of the targeted therapeutic range.10, 11 Consequently, it is not surprising that warfarin is a common cause of medication‐related emergency room visits.12 Despite many fruitless years of searching for better alternatives, VKAs have remained the mainstay of oral anticoagulation for more than 60 years.8
An ideal anticoagulant would be orally administered, effective, safe, exhibit a predictable pharmacokinetic profile and a low potential for drug or dietary interactions, and therefore would not require routine laboratory monitoring.2, 5, 13 Other desirable characteristics would include a rapid onset of action to decrease or eliminate the need for bridging therapy, and rapid reversibility with or without an antidote.8, 13 To date, no oral anticoagulant has been developed that possesses all of these desired characteristics. Dabigatran etexilate (Pradaxa, Boehringer Ingelheim Pharmaceuticals, Inc.) has recently become the first oral anticoagulant to be available for wide clinical use since the 1950s.14 In the following sections, we provide an overview of dabigatran etexilate, with a special focus on issues that are pertinent to hospitalists and the hospitalized patient.
PHARMACOLOGY OF DABIGATRAN ETEXILATE
Pharmacokinetics and Pharmacodynamics of Dabigatran Etexilate
A comparison of the pharmacokinetic (PK) and pharmacodynamic (PD) properties of dabigatran etexilate (dabigatran) and warfarin are presented in Table 1. Dabigatran etexilate (referred to from this point as dabigatran) is a prodrug of dabigatran, which blocks the terminal coagulation cascade by binding to the active site of thrombin and selectively inhibiting this critical serine protease in a dose‐dependent and reversible fashion.15 Thrombin plays a central role in blood coagulation by converting fibrinogen to fibrin, amplifying its own generation by feedback activation of factors V, VIII, and XI, and by activating platelets (Figure 1).16 Dabigatran is a direct thrombin inhibitor that acts independently of anti‐thrombin to inhibit both free and clot‐bound thrombin.17, 18 The bioavailability of dabigatran after oral intake is low (6%7%).1923 After absorption, the prodrug is rapidly converted by plasma and hepatic esterases to the active drug dabigatran, but it is not metabolized by the CYP‐450 system, therefore reducing the potential for drugdrug interactions.8, 2328 The long half‐life of dabigatran allows for once or twice daily dosing.21, 24 The PK profile of dabigatran is predictable, with minimal inter‐ and intraindividual variation.21, 22
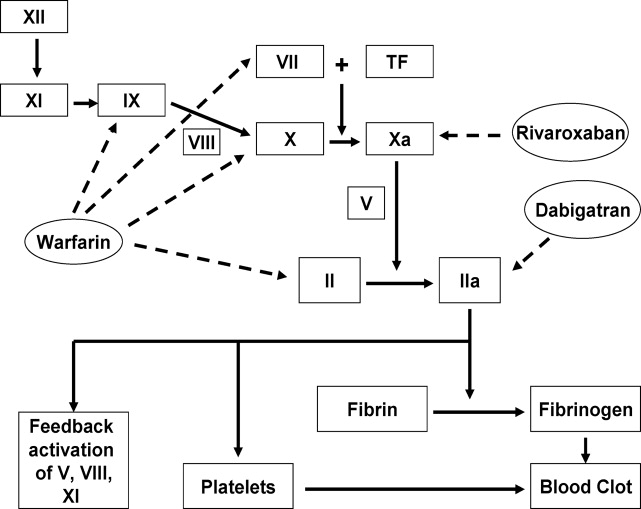
| Warfarin | Dabigatran | |
|---|---|---|
| Mechanism of action | Reduces functional levels of vitamin Kdependent factors II, VII, IX, and X by inhibiting vitamin K epoxide reductase | Binds to active site of thrombin (factor IIa) and reversibly inhibits free and clot‐bound thrombin |
| Prodrug | No | Yes |
| Bioavailability | >90%95% | 6%7% |
| Protein binding | 99% | 35% |
| Time to reach peak plasma levels | 7296 hr | 23 hr |
| Half‐life | 3644 hr | 1217 hr |
| Routine coagulation monitoring | Required, but frequency varies based on clinical situation | No requirement for routine monitoring |
| Schedule | INR‐adjusted, usually once daily | Fixed dose, once or twice daily |
| Metabolism | CYP‐450 hepatic microsomal enzymes, especially CYP2C9, CYP1A2, and CYP3A4 | Esterase‐catalyzed hydrolysis in plasma or liver after intestinal P‐gp transport |
| Clearance | Almost entirely hepatic | 80% unchanged renally (after an intravenous dose), 20% hepatic after conjugation |
| Drug interactions | Drugs that affect CYP‐450 hepatic microsomal enzymes and those that displace warfarin from plasma proteins | P‐gp inhibitors (CYP‐450 system not involved) |
| Antidote | Yes (vitamin K and plasma products) | No |
Dabigatran is packaged in capsules that are hygroscopic. Therefore, the capsules should be stored in the original container with the cap tightly closed. Exposure of dabigatran capsules to air for prolonged periods outside the original container can result in deterioration of the active compound and reduced efficacy.27, 28 Dabigatran capsules contain tartaric acid which is necessary to facilitate dissolution of the medication in the gastrointestinal tract for optimal absorption.2 Breaking the capsules or removing the drug from the capsule can result in increased exposure. Therefore, dabigatran capsules should be taken intact, and patients should be instructed that dabigatran capsules should not be broken, chewed, or opened before administration.28 Alternative anticoagulants should be used if patients cannot swallow the capsule intact for any reason (eg, intubated patients).
Dabigatran and Drug and Food Interactions
Dabigatran acts as a substrate of the transporter protein P‐glycoprotein (P‐gp), which is also involved in the transport of many other drugs.5, 16 P‐gp is an efflux pump that functions to prevent the absorption of drugs in the intestine or increase the renal excretion of drugs that are P‐gp substrates.25 Inhibitors of P‐gp increase the serum concentrations of P‐gp substrates, whereas P‐gp inducers reduce the concentrations of these medications.13 Examples of P‐gp inhibitors include clarithromycin, quinidine, and verapamil, whereas rifampin, pantoprazole, and St John's wort are known to induce P‐gp.5, 24, 26 As an illustration, the coadministration of dabigatran and amiodarone, a known P‐gp inhibitor, increases the area under the curve of drug plasmaconcentrationtime of dabigatran by 60% without significantly affecting levels of amiodarone.5, 27 Nevertheless, dagibatran's prescribing information in the United States advises that the P‐gp inhibitors ketoconazole, verapamil, amiodarone, quinidine, and clarithromycin do not require dose adjustments, although these results should not be extrapolated to other P‐gp inhibitors.28 In addition, the manufacturer recommends generally avoiding the concomitant use of the potent P‐gp inducer rifampin with dabigatran, whereas the European Medicines Agency advises caution in the coadministration of rifampin or St John's wort with dabigatran.27, 28
Not all P‐gp substrates result in clinically significant interactions with dabigatran (eg, digoxin, diclofenac, and atorvastatin).19, 29 The use of nonsteroidal anti‐inflammatory drugs and aspirin may increase the risk of bleeding in patients using dabigatran.5, 26, 27 It is not recommended to coadminister certain anti‐platelet agents (such as clopidogrel, prasugrel, or ticlopidine) with dabigatran.26, 30 Although the use of proton pump inhibitors such as pantoprazole leads to a 30% decrease in the area under the curve of dabigatran, coadministration of pantoprazole and other proton pump inhibitors with dabigatran in clinical trials did not affect bleeding risk or efficacy.27 Attention to potential drug interactions with dabigatran is important, because dabigatran is not usually monitored. Food interactions with dabigatran appear to be low, and therefore dabigatran can probably be taken with or without food, but caution is advised given the limited postmarketing experience with dabigatran.30 An excellent review of drug and dietary interactions of dabigatran has been published recently.5
Use of Dabigatran in Patients With Liver or Renal Impairment
Approximately 80% of dabigatran is excreted, largely unchanged, by the kidneys in healthy subjects.19 Patients with severe renal impairment (creatinine clearance [CrCL], 30 mL/min) were excluded from phase 3 trials that evaluated dabigatran.3135 A small study in patients with renal impairment showed a linear correlation between renal function and renal clearance of dabigatran, with proportional increases in the anticoagulant effects of dabigatran with decreasing renal function.36 For patients on hemodialysis, 62%68% of the dose was removed.36 The authors recommended avoidance of dabigatran in severe renal impairment, and a dose reduction was recommended for moderate renal impairment (CrCL, 3150 mL/min).13, 36 Despite exclusion of patients with CrCL of 30 mL/min from all phase 3 trials of dabigatran and the relative contraindication of the use of dabigatran in this patient population, the US Food and Drug Administration (FDA) approved a reduced dose of 75 mg twice daily for patients with CrCL of 1530 mL/min, but no dosing recommendations were made for patients with CrCL of 15 mL/min or for patients on dialysis.13, 28, 36 We believe that dabigatran should be used with great caution in patients with CrCl 1530 mL/min given the limited outcome data in these patients, and alternative anticoagulants should be strongly considered for these patients until more data are available.
Less than 20% of the dabigatran dose is conjugated in the liver and subsequently secreted in the biliary system.19, 23 Stangier et al. showed that moderate hepatic impairment does not affect the PK/PD or safety profile of dabigatran and concluded that dabigatran can be given to those patients without dose adjustment.37 On the other hand, severe hepatic impairment (Child‐Pugh class B or C cirrhosis) and an alanine aminotransferase level more than 2 to 3 times the upper limit of normal were used as exclusion criteria in most of the phase 3 trials that evaluated dabigatran.16, 24, 34, 35, 38 The hepatic toxicity noted with the first generation oral direct thrombin inhibitor, ximelagatran, has not been seen with dabigatran in clinical trials, although long‐term postmarketing data are lacking.32, 34, 35, 3840
The Effect of Dabigatran on Common Coagulation Laboratory Tests and Recommendations for Monitoring Dabigatran's Anticoagulant Effects
Despite the predictable PK profile of dabigatran, its effects on common coagulation assays remain incompletely defined.41 Most patients on dabigatran will have a prolonged activated partial thromboplastin time (aPTT) even at trough concentrations, but not in a linear predictable fashion.19, 20, 21, 36, 41 Dabigatran has few and unpredictable effects on prothrombin time (PT) and INR, and therapeutic concentrations of dabigatran usually result in only modest elevations of PT/INR.21, 42 Although thrombin time (TT) displays a good linear correlation with plasma concentrations of dabigatran, the reagents used to perform TT in most clinical laboratories are not standardized. Therefore, TT is better suited to detecting the presence of dabigatran rather than monitoring its anticoagulant effects.24, 42 Therefore, even a slightly prolonged aPTT or TT could reflect significant plasma dabigatran levels. The best assays for monitoring dabigatran are the ecarin clotting time (ECT), modified thrombelastographic evaluations of whole blood clot formation, and the Hemoclot Thrombin Inhibitor assay, but these tests are limited by lack of standardization and limited clinical availablity.24, 42, 43
EFFICACY OF DABIGATRAN
In this section, we provide a brief review of the major phase 3 trials that evaluated dabigatran for different indications (see references 13, 16, and 24 for recent detailed reviews of the clinical trials of dabigatran).
Dabigatran for Thromboprophylaxis in Patients with Atrial Fibrillation
The Randomized Evaluation of Long‐Term Anticoagulation Therapy (RE‐LY) trial was a prospective, noninferiority, phase 3 study of dabigatran that was the basis for its FDA approval in patients with nonvalvular AF.35, 44 In RE‐LY, 18,113 AF patients with another thromboembolic risk factor were randomized to receive fixed doses of dabigatran (110 mg or 150 mg twice daily) or adjusted‐dose warfarin.35 The median duration of follow‐up was 2 years and the primary outcome was stroke or systemic embolism. The primary outcome occurred in 1.69% per year in the warfarin group versus 1.53% per year in the group receiving 110 mg of dabigatran twice daily (relative risk with dabigatran, 0.91; 95% confidence interval [CI], 0.741.11; P 0.001 for noninferiority) and 1.11% per year in the group receiving 150 mg of dabigatran twice daily (relative risk, 0.66; 95% CI, 0.530.82; P 0.001 for superiority). The rate of major bleeding was 3.36% per year in the warfarin group versus 2.71% per year in the dabigatran 110 mg group (P = 0.003) and 3.11% per year in the dabigatran 150 mg group (P = 0.31). Intracranial bleeds were significantly less common in both dabigatran groups than with warfarin. Major gastrointestinal bleeding rate was significantly higher in the dabigatran group at the 150‐mg dose than in the warfarin group. The mortality rate was 4.13% per year in the warfarin group versus 3.75% per year with 110 mg of dabigatran (P = 0.13) and 3.64% per year with 150 mg of dabigatran (P = 0.051).35 The authors concluded that in patients with nonvalvular AF, dabigatran given at a dose of 110 mg twice daily was not inferior to warfarin, and was associated with lower rates of major hemorrhage than warfarin.35 Dabigatran given at a dose of 150 mg twice daily was associated with lower rates of stroke and systemic embolism than warfarin but had similar rates of major hemorrhage.35 These effects were maintained in patients with previous stroke or transient ischemic attack, and in these patients starting dabigatran with and without prior VKA treatment.45, 46
Dabigatran for Prevention of Venous Thromboembolism After Major Orthopedic Procedures
Without thromboprophylaxis, the incidence of venous thromboembolism (VTE) following major orthopedic surgery is 40%60%.47 Nevertheless, many patients do not receive appropriate thromboprophylaxis after orthopedic surgery, in part due to the limitations of VKAs and the inconvenience of low molecular weight heparin (LMWH) injections.48
RE‐NOVATE Trial
Oral dabigatran versus enoxaparin for thromboprophylaxis after primary total hip arthroplasty (RE‐NOVATE trail) was a prospective, noninferiority phase 3 trial in which 3494 patients undergoing total hip replacement (THR) were randomized in double‐blind fashion to 2835 days of dabigatran 220 mg or 150 mg once daily, starting with a half‐dose 14 hours after surgery, or subcutaneous (SC) enoxaparin 40 mg once daily, starting the evening before surgery.33 The primary efficacy outcome was the composite of total VTE (venographic or symptomatic) and death from all causes during treatment. The primary efficacy outcome occurred in 6.7% in the enoxaparin group versus 6.0% in the dabigatran 220 mg group (absolute difference [AD], 0.7%; 95% CI, 2.9% to 1.6%) and 8.6% in the 150 mg group (AD, 1.9%; 95% CI, 0.6% to 4.4%). There was no significant difference in major bleeding with either dose of dabigatran compared with enoxaparin (220 mg, P = 0.44; 150 mg, P = 0.60). It was concluded that oral dabigatran was not inferior to enoxaparin for prevention of VTE after THR surgery, with a similar safety profile.33
RE‐NOVATE II Trial
Oral dabigatran versus enoxaparin for thromboprophylaxis after primary total hip arthroplasty (RE‐NOVATE II trail) was a randomized, double‐blind, noninferiority phase 3 trial that compared dabigatran versus SC enoxaparin for extended thromboprophylaxis in patients undergoing THR.38 A total of 2055 patients were randomized to 2835 days of oral dabigatran, 220 mg once daily, starting with a half‐dose 14 hours after surgery, or SC enoxaparin 40 mg once daily, starting the evening before surgery. The primary efficacy outcome was the same as that in the RE‐NOVATE trial. The primary efficacy outcome occurred in 7.7% of the dabigatran group versus 8.8% of the enoxaparin group (risk difference, 1.1%; 95% CI, 3.8 to 1.6%; P 0.0001 for the prespecified noninferiority margin. Major VTE plus VTE‐related death occurred in 2.2% of the dabigatran group versus 4.2% of the enoxaparin group (risk difference, 1.9%; 95% CI, 3.6% to 0.2%; P = 0.03). Major bleeding occurred in 1.4% of the dabigatran group and 0.9% of the enoxaparin group (P = 0.40). It was concluded that extended prophylaxis with oral dabigatran 220 mg once daily was not inferior to SC enoxaparin 40 mg once daily for prevention of VTE after THR. The safety profiles were similar between the 2 arms.38
RE‐MODEL Trial
In the Oral dabigatran etexilate vs. subcutaneous enoxaparin for the prevention of venous thromblembloism after total knee replacement (RE‐MODEL trail) phase 3 trial, 2076 patients who underwent total knee replacement (TKR) were randomized to receive dabigatran 150 mg or 220 mg once daily starting with a half‐dose 14 hours after surgery, or SC enoxaparin 40 mg once daily starting the evening before surgery, for 610 days.32 Patients were followed‐up for 3 months. The primary efficacy outcome was a composite of total VTE (venographic or symptomatic) and mortality during treatment. The primary efficacy outcome occurred in 37.7% of the enoxaparin group versus 36.4% of the dabigatran 220 mg group (AD, 1.3%; 95% CI, 7.3 to 4.6) and 40.5% of the 150 mg group (AD, 2.8%; 95% CI, 3.1 to 8.7). The incidence of major bleeding did not differ between the groups (1.3% versus 1.5% and 1.3%, respectively). The conclusion was that dabigatran (220 mg or 150 mg) was not inferior to enoxaparin for prevention of VTE after TKR surgery and exhibited a similar safety profile.32
RE‐MOBILZE Trial
The oral thrombin inhibitor dabigatran etexilate vs the North American enoxaparin regimen for the prevention of venous thromboembolism after knee arthroplasty surgery (RE‐MOBILIZE trail) was a phase 3 trial that randomized 1896 patients after unilateral TKR to receive dabigatran 220 or 150 mg once daily versus enoxaparin 30 mg SC twice daily after surgery.40 Dosing stopped at contrast venography, 1215 days after surgery. Follow‐up was for 3 months. The primary outcome was a composite of total VTE events and all‐cause mortality during treatment. With respect to the primary outcome, dabigatran at 220 and 150 mg showed inferior efficacy to enoxaparin, with VTE rates of 31% (P = 0.02 vs enoxaparin), 34% (P 0.001 vs enoxaparin), and 25%, respectively. Major bleeding was similar. It was concluded that dabigatran was inferior to the twice‐daily North American enoxaparin regimen, probably because of the latter's more intense and prolonged dosing.40 It should be noted that the first dose of dabigatran in this study was given 612 hours after surgery, compared with 14 hours postoperatively in RE‐MODEL, which may have contributed to the inferior outcome.32, 40
Dabigatran for Treatment of Acute VTE
RE‐COVER was a large, randomized, noninferiority phase 3 trial that randomized 2564 patients with acute symptomatic proximal lower extremity deep vein thrombosis or pulmonary embolism to 6 months of dabigatran 150 mg twice daily or dose‐adjusted warfarin (INR 2/3).34 All patients initially received parenteral anticoagulation (LMWH or unfractionated heparin [UFH]) for a median of 9 days. Patients in the warfarin group spent 60% of the time in the therapeutic range. In the dabigatran arm, 2.4% had recurrent VTE versus 2.1% in the warfarin arm (P 0.001 for the prespecified noninferiority margin). Major bleeding occurred in 1.6% of patients in the dabigatran arm and 1.9% in the warfarin arm (hazards ratio, 0.82; 95% CI, 0.451.48). There was no difference in the other safety endpoints (acute coronary syndrome, abnormal liver function tests and deaths). Adverse events (especially gastrointestinal) leading to discontinuation of the study drug occurred in 9% of patients assigned to dabigatran and 6.8% of patients assigned to warfarin (P = 0.05). It was concluded that a fixed dose of dabigatran was not inferior to warfarin for treatment of VTE, with a similar safety profile.34 It is important to note that the first dose of dabigatran was given after a median of 9 days of parenteral anticoagulation therapy, so the findings of this study do not provide data regarding the use of dabigatran as initial monotherapy for acute VTE.34 The results of additional randomized trials evaluating the use of dabigatran for acute VTE treatment (RE‐COVER II) and secondary prevention of VTE (RE‐MEDY and RE‐SONATE) are expected soon.16
SAFETY OF DABIGATRAN
Aside from the bleeding risks discussed earlier, the most commonly reported side effect of dabigatran was dyspepsia. Dyspepsia occurred twice as frequently in patients taking dabigatran versus warfarin in the RE‐LY trial (11.5% vs 5.8%).35 One possible explanation for the higher incidence of dyspepsia is the tartaric acid component in dabigatran capsules.2 In the RE‐LY study, myocardial infarction occurred more commonly in the dabigatran arms (0.72% with 110 mg and 0.74% with 150 mg) than the warfarin arm (0.53%, P = 0.07 and 0.048, respectively).24, 35 It has been postulated that this observation could be related to a greater efficacy of warfarin for the prevention of myocardial infarction rather than an adverse effect of dabigatran.2 There was no increase in acute coronary syndrome rates noted with dabigatran in the other phase 3 trials.3234, 38, 40 No increased risk of elevated liver function test has been noted with dabigatran, but long‐term data are unavailable.32, 34, 35, 38
MANAGEMENT OF SPECIAL SITUATIONS THAT MAY ARISE IN THE USE OF DABIGATRAN
Switching From Warfarin to Dabigatran and Vice Versa
When converting patients from warfarin to dabigatran, it is recommended that dabigatran be started once the INR falls below the lower limit of the desired therapeutic range. Conversely, when switching from dabigatran to warfarin, the manufacturer recommends starting warfarin based on renal function (Table 2). It should be noted that because dabigatran can increase the INR, the INR will better reflect warfarin's effect after dabigatran has been stopped for at least 2 days.27, 28
| CrCL (mL/min) | Time of Warfarin Initiation |
|---|---|
| |
| 50 | 3 d before discontinuing dabigatran |
| 3150 | 2 d before discontinuing dabigatran |
| 1530 | 1 d before discontinuing dabigatran |
| 15 | No recommendations made |
Bridging from Dabigatran to Parenteral Anticoagulants and Vice Versa
For patients currently receiving a parenteral anticoagulant, the manufacturer recommends starting dabigatran 02 hours before the next administration time for parenteral anticoagulants (eg, LMWH) or at the time of discontinuation for continuously infused parenteral drugs (eg, intravenous UFH).28 For patients currently taking dabigatran who are transitioning to a parenteral anticoagulant, it is recommended to wait 12 hours (CrCl 30 mL/min) or 24 hours (CrCl 30 mL/min) after the last dose of dabigatran before initiating treatment with a parenteral anticoagulant.27, 28
Management of Dabigatran Before Elective and Urgent Invasive Procedures
Patients who undergo invasive procedures in the presence of therapeutic levels of dabigatran are at an increased risk of bleeding. The manufacturer recommends holding dabigatran for at least 24 hours before elective surgery depending on the degree of renal impairment and the risk of bleeding.28 Table 3 lists recommendations on the timing of discontinuation of dabigatran before a procedure. If emergent/urgent surgery is necessary for a patient who is on dabigatran, the risk of bleeding should be weighed against the urgency of the intervention.28, 42, 44 As mentioned earlier, the ECT or the Hemoclot Thrombin Inhibitor assay are the preferred tests for measurement of dabigatran effects, but they are not standardized or widely clinically available. Instead, prolongation of the TT (preferably) or the aPTT can be used to determine the presence of dabigatran.28, 42
| CrCL (mL/min) | Half‐Life (hr) | Suggested Timing of Discontinuation of Dabigatran Before Surgery | |
|---|---|---|---|
| Standard Risk of Bleeding | High Risk of Bleeding* | ||
| |||
| >80 | 13 (11‐22) | 24 hr | 24 d |
| 5180 | 15 (12‐34) | 24 hr | 24 d |
| 3150 | 18 (13‐23) | 48 hr | 4 d |
| 30 | 27 (22‐35) | 25 d | >5 d |
Overdose and Toxicity With Dabigatran
Accidental or intentional overdose, or accumulation of dabigatran due to renal impairment, may lead to hemorrhagic complications. Unlike warfarin and heparin, there is no antidote for dabigatran. There are no widely available, reliable laboratory tests to measure the anticoagulant activity of dabigatran, and evidence‐based guidelines to manage dabigatran toxicity do not exist. Therefore, in the event of dabigatran toxicity, treatment is largely supportive. Management of toxicity is dependent on whether the overdose/accumulation is accompanied by bleeding or not. For overdose, interventions include adequate diuresis and the use of activated charcoal to reduce the absorption of dabigatran (within 2 hours of ingestion).42 In the event of bleeding, proposed measures include application of mechanical pressure to the sites of bleeding and infusion of pro‐coagulant blood products such as activated prothrombin complex concentrates (eg, FEIBA VH, Baxter) or recombinant human activated factor VIIa (NovoSeven, Novo‐Nordisk) (reviewed in references 26 and 42). In life‐threatening situations, hemodialysis could be considered, because it can remove 60% of the drug within 23 hours.42 Hemoperfusion over a charcoal filter or large volume hemofiltration have also been suggested in extreme situations.27, 28, 36, 42 Acknowledging their limitations, the ECT, TT, or aPTT may be used to direct therapy.27, 42
Pregnancy and Dabigatran Therapy
Dabigatran is a class C drug during pregnancy, and there are no studies of dabigatran in pregnant women. Animal studies with dabigatran showed decreased fertility of pregnant rats; therefore, the risks and benefits of dabigatran therapy during pregnancy should be weighed carefully.27, 28, 44
CONCLUSIONS
Dabigatran is a novel, oral direct thrombin inhibitor that exhibits several advantages over warfarin. The predictable pharmacokinetic profile and minimal food and drug interactions of dabigatran allow for a fixed‐dosing regimen and obviate the need for routine laboratory monitoring. However, this apparent advantage is also a disadvantage. The lack of a reliable method to monitor dabigatran makes it more difficult to assess compliance, measure the impact of drug interactions, evaluate for toxicity, and determine bona fide therapeutic failure versus noncompliance in the event of breakthrough thromboembolism.28, 42 Other limitations of dabigatran include the lack of an antidote and the dependence on normal renal function for elimination, with the potential for drug accumulation and toxicity with renal impairment. The noninferiority design of the clinical trials that evaluated dabigatran, the absence of long‐term safety and efficacy data, and issues related to the cost effectiveness of dabigatran should be considered when prescribing this agent. More studies are needed to assess dabigatran in special patient populations (eg, the elderly, patients with renal and hepatic impairment, pediatric and pregnant patients) and to better understand dabigatrandrug interactions.
As more novel oral anticoagulant agents, such as factor Xa inhibitors, become available for clinical use, comparative studies will need to be performed to better define the role of each agent for specific indications. In the future, it might be possible to tailor the choice of the oral anticoagulant to the individual patient not only on the basis of the clinical indication but also the specific patient characteristics and possible drug interactions. For example, rivaroxaban (Xarelto) is an oral direct factor Xa that was recently approved in the United States for VTE thromboprophylaxis following orthopedic surgery and in patients with non‐valvular atrial fibrillation.2 Similar to dabigatran, rivaroxaban exhibits predictable PK and PD that allow fixed once or twice daily dosing and obviate the need for routine monitoring of its anticoagulant effects.2, 16 Unlike dabigatran, rivaroxaban is an active drug and not a prodrug, and has a significantly higher bioavailability than dabigatran (>80% vs 6%).16 In addition, the levels of rivaroxaban can be affected by drugs that interfere with both P‐gp and the hepatic CYP‐450 system, compared with dabigatran, which is affected only by drugs that affect P‐gp.8, 16
- ,,, et al.The use of antithrombotic therapies in the prevention and treatment of arterial and venous thrombosis: a survey of current knowledge and practice supporting the need for clinical education.Crit Pathw Cardiol.2010;9:41–48.
- .Warfarin versus new agents: interpreting the data.Hematology Am Soc Hematol Educ Program.2010;2010:221–228.
- ,,,,.Why do patients with atrial fibrillation not receive warfarin?Arch Intern Med.2000;160:41–46.
- ,,,,,.Warfarin use among ambulatory patients with nonvalvular atrial fibrillation: The anticoagulation and risk factors in atrial fibrillation (ATRIA) study.Ann Intern Med.1999;131:927–934.
- ,.Drug and dietary interactions of the new and emerging oral anticoagulants.Int J Clin Pract.2010;64:956–967.
- ,,, et al.The risk of bleeding complications in patients with cytochrome P450 CYP2C9*2 or CYP2C9*3 alleles on acenocoumarol or phenprocoumon.Thromb Haemost.2004;92:61–66.
- ,,, et al.Differentiating low‐molecular‐weight heparins based on chemical, biological, and pharmacologic properties: implications for the development of generic versions of low‐molecular‐weight heparins.Semin Thromb Hemost.2008;34:74–85.
- ,.Emerging anticoagulants.Expert Opin Emerg Drugs.2011;16:31–44.
- ,,, et al.Systematic overview of warfarin and its drug and food interactions.Arch Intern Med.2005;165:1095–1106.
- ,,,,,.Evaluation of the pattern of treatment, level of anticoagulation control, and outcome of treatment with warfarin in patients with non‐valvar atrial fibrillation: a record linkage study in a large british population.Heart.2005;91:472–477.
- ,,, et al.Comparison of outcomes among patients randomized to warfarin therapy according to anticoagulant control: results from SPORTIF III and V.Arch Intern Med.2007;167:239–245.
- ,,,.Medication use leading to emergency department visits for adverse drug events in older adults.Ann Intern Med.2007;147:755–765.
- .New oral anticoagulants: a practical guide for clinicians.J Thromb Thrombolysis.2010;29:182–191.
- ,,,.The quest for new anticoagulants: from clinical development to clinical practice [published ahead of print June 14, 2010].Cardiovasc Ther.2010. doi: 10.1111/j.1755–5922.2010.00160.x.
- ,,,,.In‐vitro profile and ex‐vivo anticoagulant activity of the direct thrombin inhibitor dabigatran and its orally active prodrug, dabigatran etexilate.Thromb Haemost.2007;98:155–162.
- ,,.Novel oral factor xa and thrombin inhibitors in the management of thromboembolism.Annu Rev Med.2011;62:41–57.
- ,,,,.Clot‐bound thrombin is protected from inhibition by heparin‐antithrombin III but is susceptible to inactivation by antithrombin III‐independent inhibitors.J Clin Invest.1990;86:385–391.
- ,,.Thrombin binds to soluble fibrin degradation products where it is protected from inhibition by heparin‐antithrombin but susceptible to inactivation by antithrombin‐independent inhibitors.Circulation.1998;97:544–552.
- .Clinical pharmacokinetics and pharmacodynamics of the oral direct thrombin inhibitor dabigatran etexilate.Clin Pharmacokinet.2008;47:285–295.
- ,.Pharmacology, pharmacokinetics, and pharmacodynamics of dabigatran etexilate, an oral direct thrombin inhibitor.Clin Appl Thromb Hemost.2009;15(suppl 1):9S–16S.
- ,,,,.The pharmacokinetics, pharmacodynamics and tolerability of dabigatran etexilate, a new oral direct thrombin inhibitor, in healthy male subjects.Br J Clin Pharmacol.2007;64:292–303.
- ,,,.Pharmacokinetics and pharmacodynamics of the direct oral thrombin inhibitor dabigatran in healthy elderly subjects.Clin Pharmacokinet.2008;47:47–59.
- ,,,,.The metabolism and disposition of the oral direct thrombin inhibitor, dabigatran, in humans.Drug Metab Dispos.2008;36:386–399.
- ,,.Dabigatran etexilate versus warfarin as the oral anticoagulant of choice? A review of clinical data.Pharmacol Ther.2011;129:185–194.
- .The role of P‐glycoprotein and organic anion‐transporting polypeptides in drug interactions.Drug Saf.2005;28:789–801.
- ,,.Novel oral anticoagulants: implications in the perioperative setting.Anesthesiology.2010;113:726–745.
- European Medicines Agency. Pradaxa (dabigatran etexilate) [product information]. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_‐_Product_Information/human/000829/WC 500041059.pdf. Accessed March 25,2011.
- Dabigatran medication guide. Available at: http://bidocs.boehringer‐ingelheim.com/BIWebAccess/ViewServlet.ser?docBase = renetnt9:59–68.
- ,,.Novel oral anticoagulants: the potential relegation of vitamin K antagonists in clinical practice.Int J Clin Pract.2010;64:835–838.
- .The RE‐LY study: Randomized Evaluation of Long‐term anticoagulant therapY: dabigatran vs. warfarin.Eur Heart J.2009;30:2554–2555.
- ,,, et al.Oral dabigatran etexilate vs. subcutaneous enoxaparin for the prevention of venous thromboembolism after total knee replacement: the RE‐MODEL randomized trial.J Thromb Haemost.2007;5:2178–2185.
- ,,, et al.Dabigatran etexilate versus enoxaparin for prevention of venous thromboembolism after total hip replacement: a randomised, double‐blind, non‐inferiority trial.Lancet.2007;370:949–956.
- ,,, et al.Dabigatran versus warfarin in the treatment of acute venous thromboembolism.N Engl J Med.2009;361:2342–2352.
- ,,, et al.Dabigatran versus warfarin in patients with atrial fibrillation.N Engl J Med.2009;361:1139–1151.
- ,,,.Influence of renal impairment on the pharmacokinetics and pharmacodynamics of oral dabigatran etexilate: an open‐label, parallel‐group, single‐centre study.Clin Pharmacokinet.2010;49:259–268.
- ,,,,.Pharmacokinetics and pharmacodynamics of dabigatran etexilate, an oral direct thrombin inhibitor, are not affected by moderate hepatic impairment.J Clin Pharmacol.2008;48:1411–1419.
- ,,, et al.Oral dabigatran versus enoxaparin for thromboprophylaxis after primary total hip arthroplasty (RE‐NOVATE II). A randomised, double‐blind, non‐inferiority trial.Thromb Haemost.2011;105:721–729.
- ,.Insights from the dabigatran versus warfarin trial in patients with venous thromboembolism (the RE‐COVER trial).Expert Opin Pharmacother.2010;11:1035–1037.
- RE‐MOBILIZE Writing Committee,,, et al.Oral thrombin inhibitor dabigatran etexilate vs north american enoxaparin regimen for prevention of venous thromboembolism after knee arthroplasty surgery.J Arthroplasty.2009;24:1–9.
- ,,, et al.Effects of the oral, direct thrombin inhibitor dabigatran on five common coagulation assays.Thromb Haemost.2011;105:371–378.
- ,,, et al.Dabigatran etexilate—a novel, reversible, oral direct thrombin inhibitor: interpretation of coagulation assays and reversal of anticoagulant activity.Thromb Haemost.2010;103:1116–1127.
- ,.A direct thrombin inhibitor studied by dynamic whole blood clot formation. haemostatic response to ex‐vivo addition of recombinant factor VIIa or activated prothrombin complex concentrate.Thromb Haemost.2006;96:446–453.
- US Food and Drug Administration. Dabigatran drug approval history. Available at: http://www.accessdata.fda.gov/drugsatfda_ docs/nda/2010/022512Orig1s000TOC.cfm. Accessed March 20,2011.
- ,,, et al.Dabigatran compared with warfarin in patients with atrial fibrillation and previous transient ischaemic attack or stroke: a subgroup analysis of the RE‐LY trial.Lancet Neurol.2010;9:1157–1163.
- ,,, et al.Dabigatran and warfarin in vitamin K antagonist‐naive and ‐experienced cohorts with atrial fibrillation.Circulation.2010;122:2246–2253.
- ,,, et al.Prevention of venous thromboembolism: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th edition).Chest.2008;133(6 suppl):381S–453S.
- ,,,.American Association of Orthopedic Surgeons and American College of Chest Physicians guidelines for venous thromboembolism prevention in hip and knee arthroplasty differ: what are the implications for clinicians and patients?Chest.2009;135:513–520.
Vitamin K antagonists (VKAs) such as warfarin have been the backbone of oral anticoagulation in clinical practice since the middle of the last century. Despite their efficacy, VKAs have well‐recognized limitations that have led to their underutilization in patients who would otherwise be candidates for oral anticoagulation.14 These limitations include a narrow therapeutic window and significant intra‐ and interindividual variability in dose requirements as well as numerous drugdrug and drugfood interactions.59 Therefore, VKAs require close laboratory monitoring to prevent excessive or under‐anticoagulation, and maintaining therapeutic anticoagulation with VKAs remains a challenging task in many patients.2 It has been shown that 30%50% of international normalized ratio (INR) results fall outside of the targeted therapeutic range.10, 11 Consequently, it is not surprising that warfarin is a common cause of medication‐related emergency room visits.12 Despite many fruitless years of searching for better alternatives, VKAs have remained the mainstay of oral anticoagulation for more than 60 years.8
An ideal anticoagulant would be orally administered, effective, safe, exhibit a predictable pharmacokinetic profile and a low potential for drug or dietary interactions, and therefore would not require routine laboratory monitoring.2, 5, 13 Other desirable characteristics would include a rapid onset of action to decrease or eliminate the need for bridging therapy, and rapid reversibility with or without an antidote.8, 13 To date, no oral anticoagulant has been developed that possesses all of these desired characteristics. Dabigatran etexilate (Pradaxa, Boehringer Ingelheim Pharmaceuticals, Inc.) has recently become the first oral anticoagulant to be available for wide clinical use since the 1950s.14 In the following sections, we provide an overview of dabigatran etexilate, with a special focus on issues that are pertinent to hospitalists and the hospitalized patient.
PHARMACOLOGY OF DABIGATRAN ETEXILATE
Pharmacokinetics and Pharmacodynamics of Dabigatran Etexilate
A comparison of the pharmacokinetic (PK) and pharmacodynamic (PD) properties of dabigatran etexilate (dabigatran) and warfarin are presented in Table 1. Dabigatran etexilate (referred to from this point as dabigatran) is a prodrug of dabigatran, which blocks the terminal coagulation cascade by binding to the active site of thrombin and selectively inhibiting this critical serine protease in a dose‐dependent and reversible fashion.15 Thrombin plays a central role in blood coagulation by converting fibrinogen to fibrin, amplifying its own generation by feedback activation of factors V, VIII, and XI, and by activating platelets (Figure 1).16 Dabigatran is a direct thrombin inhibitor that acts independently of anti‐thrombin to inhibit both free and clot‐bound thrombin.17, 18 The bioavailability of dabigatran after oral intake is low (6%7%).1923 After absorption, the prodrug is rapidly converted by plasma and hepatic esterases to the active drug dabigatran, but it is not metabolized by the CYP‐450 system, therefore reducing the potential for drugdrug interactions.8, 2328 The long half‐life of dabigatran allows for once or twice daily dosing.21, 24 The PK profile of dabigatran is predictable, with minimal inter‐ and intraindividual variation.21, 22
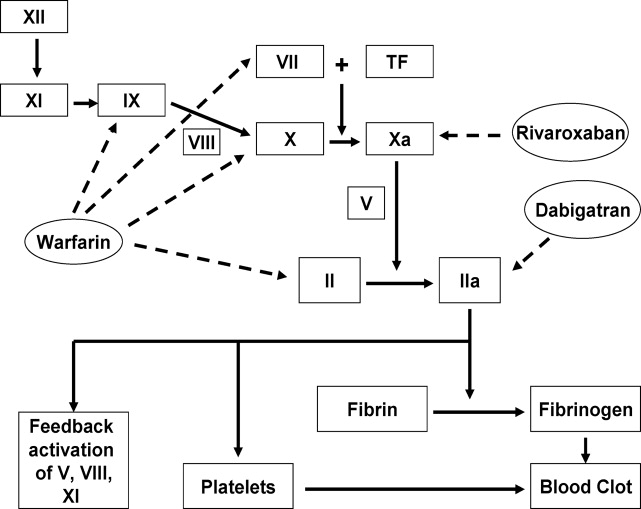
| Warfarin | Dabigatran | |
|---|---|---|
| Mechanism of action | Reduces functional levels of vitamin Kdependent factors II, VII, IX, and X by inhibiting vitamin K epoxide reductase | Binds to active site of thrombin (factor IIa) and reversibly inhibits free and clot‐bound thrombin |
| Prodrug | No | Yes |
| Bioavailability | >90%95% | 6%7% |
| Protein binding | 99% | 35% |
| Time to reach peak plasma levels | 7296 hr | 23 hr |
| Half‐life | 3644 hr | 1217 hr |
| Routine coagulation monitoring | Required, but frequency varies based on clinical situation | No requirement for routine monitoring |
| Schedule | INR‐adjusted, usually once daily | Fixed dose, once or twice daily |
| Metabolism | CYP‐450 hepatic microsomal enzymes, especially CYP2C9, CYP1A2, and CYP3A4 | Esterase‐catalyzed hydrolysis in plasma or liver after intestinal P‐gp transport |
| Clearance | Almost entirely hepatic | 80% unchanged renally (after an intravenous dose), 20% hepatic after conjugation |
| Drug interactions | Drugs that affect CYP‐450 hepatic microsomal enzymes and those that displace warfarin from plasma proteins | P‐gp inhibitors (CYP‐450 system not involved) |
| Antidote | Yes (vitamin K and plasma products) | No |
Dabigatran is packaged in capsules that are hygroscopic. Therefore, the capsules should be stored in the original container with the cap tightly closed. Exposure of dabigatran capsules to air for prolonged periods outside the original container can result in deterioration of the active compound and reduced efficacy.27, 28 Dabigatran capsules contain tartaric acid which is necessary to facilitate dissolution of the medication in the gastrointestinal tract for optimal absorption.2 Breaking the capsules or removing the drug from the capsule can result in increased exposure. Therefore, dabigatran capsules should be taken intact, and patients should be instructed that dabigatran capsules should not be broken, chewed, or opened before administration.28 Alternative anticoagulants should be used if patients cannot swallow the capsule intact for any reason (eg, intubated patients).
Dabigatran and Drug and Food Interactions
Dabigatran acts as a substrate of the transporter protein P‐glycoprotein (P‐gp), which is also involved in the transport of many other drugs.5, 16 P‐gp is an efflux pump that functions to prevent the absorption of drugs in the intestine or increase the renal excretion of drugs that are P‐gp substrates.25 Inhibitors of P‐gp increase the serum concentrations of P‐gp substrates, whereas P‐gp inducers reduce the concentrations of these medications.13 Examples of P‐gp inhibitors include clarithromycin, quinidine, and verapamil, whereas rifampin, pantoprazole, and St John's wort are known to induce P‐gp.5, 24, 26 As an illustration, the coadministration of dabigatran and amiodarone, a known P‐gp inhibitor, increases the area under the curve of drug plasmaconcentrationtime of dabigatran by 60% without significantly affecting levels of amiodarone.5, 27 Nevertheless, dagibatran's prescribing information in the United States advises that the P‐gp inhibitors ketoconazole, verapamil, amiodarone, quinidine, and clarithromycin do not require dose adjustments, although these results should not be extrapolated to other P‐gp inhibitors.28 In addition, the manufacturer recommends generally avoiding the concomitant use of the potent P‐gp inducer rifampin with dabigatran, whereas the European Medicines Agency advises caution in the coadministration of rifampin or St John's wort with dabigatran.27, 28
Not all P‐gp substrates result in clinically significant interactions with dabigatran (eg, digoxin, diclofenac, and atorvastatin).19, 29 The use of nonsteroidal anti‐inflammatory drugs and aspirin may increase the risk of bleeding in patients using dabigatran.5, 26, 27 It is not recommended to coadminister certain anti‐platelet agents (such as clopidogrel, prasugrel, or ticlopidine) with dabigatran.26, 30 Although the use of proton pump inhibitors such as pantoprazole leads to a 30% decrease in the area under the curve of dabigatran, coadministration of pantoprazole and other proton pump inhibitors with dabigatran in clinical trials did not affect bleeding risk or efficacy.27 Attention to potential drug interactions with dabigatran is important, because dabigatran is not usually monitored. Food interactions with dabigatran appear to be low, and therefore dabigatran can probably be taken with or without food, but caution is advised given the limited postmarketing experience with dabigatran.30 An excellent review of drug and dietary interactions of dabigatran has been published recently.5
Use of Dabigatran in Patients With Liver or Renal Impairment
Approximately 80% of dabigatran is excreted, largely unchanged, by the kidneys in healthy subjects.19 Patients with severe renal impairment (creatinine clearance [CrCL], 30 mL/min) were excluded from phase 3 trials that evaluated dabigatran.3135 A small study in patients with renal impairment showed a linear correlation between renal function and renal clearance of dabigatran, with proportional increases in the anticoagulant effects of dabigatran with decreasing renal function.36 For patients on hemodialysis, 62%68% of the dose was removed.36 The authors recommended avoidance of dabigatran in severe renal impairment, and a dose reduction was recommended for moderate renal impairment (CrCL, 3150 mL/min).13, 36 Despite exclusion of patients with CrCL of 30 mL/min from all phase 3 trials of dabigatran and the relative contraindication of the use of dabigatran in this patient population, the US Food and Drug Administration (FDA) approved a reduced dose of 75 mg twice daily for patients with CrCL of 1530 mL/min, but no dosing recommendations were made for patients with CrCL of 15 mL/min or for patients on dialysis.13, 28, 36 We believe that dabigatran should be used with great caution in patients with CrCl 1530 mL/min given the limited outcome data in these patients, and alternative anticoagulants should be strongly considered for these patients until more data are available.
Less than 20% of the dabigatran dose is conjugated in the liver and subsequently secreted in the biliary system.19, 23 Stangier et al. showed that moderate hepatic impairment does not affect the PK/PD or safety profile of dabigatran and concluded that dabigatran can be given to those patients without dose adjustment.37 On the other hand, severe hepatic impairment (Child‐Pugh class B or C cirrhosis) and an alanine aminotransferase level more than 2 to 3 times the upper limit of normal were used as exclusion criteria in most of the phase 3 trials that evaluated dabigatran.16, 24, 34, 35, 38 The hepatic toxicity noted with the first generation oral direct thrombin inhibitor, ximelagatran, has not been seen with dabigatran in clinical trials, although long‐term postmarketing data are lacking.32, 34, 35, 3840
The Effect of Dabigatran on Common Coagulation Laboratory Tests and Recommendations for Monitoring Dabigatran's Anticoagulant Effects
Despite the predictable PK profile of dabigatran, its effects on common coagulation assays remain incompletely defined.41 Most patients on dabigatran will have a prolonged activated partial thromboplastin time (aPTT) even at trough concentrations, but not in a linear predictable fashion.19, 20, 21, 36, 41 Dabigatran has few and unpredictable effects on prothrombin time (PT) and INR, and therapeutic concentrations of dabigatran usually result in only modest elevations of PT/INR.21, 42 Although thrombin time (TT) displays a good linear correlation with plasma concentrations of dabigatran, the reagents used to perform TT in most clinical laboratories are not standardized. Therefore, TT is better suited to detecting the presence of dabigatran rather than monitoring its anticoagulant effects.24, 42 Therefore, even a slightly prolonged aPTT or TT could reflect significant plasma dabigatran levels. The best assays for monitoring dabigatran are the ecarin clotting time (ECT), modified thrombelastographic evaluations of whole blood clot formation, and the Hemoclot Thrombin Inhibitor assay, but these tests are limited by lack of standardization and limited clinical availablity.24, 42, 43
EFFICACY OF DABIGATRAN
In this section, we provide a brief review of the major phase 3 trials that evaluated dabigatran for different indications (see references 13, 16, and 24 for recent detailed reviews of the clinical trials of dabigatran).
Dabigatran for Thromboprophylaxis in Patients with Atrial Fibrillation
The Randomized Evaluation of Long‐Term Anticoagulation Therapy (RE‐LY) trial was a prospective, noninferiority, phase 3 study of dabigatran that was the basis for its FDA approval in patients with nonvalvular AF.35, 44 In RE‐LY, 18,113 AF patients with another thromboembolic risk factor were randomized to receive fixed doses of dabigatran (110 mg or 150 mg twice daily) or adjusted‐dose warfarin.35 The median duration of follow‐up was 2 years and the primary outcome was stroke or systemic embolism. The primary outcome occurred in 1.69% per year in the warfarin group versus 1.53% per year in the group receiving 110 mg of dabigatran twice daily (relative risk with dabigatran, 0.91; 95% confidence interval [CI], 0.741.11; P 0.001 for noninferiority) and 1.11% per year in the group receiving 150 mg of dabigatran twice daily (relative risk, 0.66; 95% CI, 0.530.82; P 0.001 for superiority). The rate of major bleeding was 3.36% per year in the warfarin group versus 2.71% per year in the dabigatran 110 mg group (P = 0.003) and 3.11% per year in the dabigatran 150 mg group (P = 0.31). Intracranial bleeds were significantly less common in both dabigatran groups than with warfarin. Major gastrointestinal bleeding rate was significantly higher in the dabigatran group at the 150‐mg dose than in the warfarin group. The mortality rate was 4.13% per year in the warfarin group versus 3.75% per year with 110 mg of dabigatran (P = 0.13) and 3.64% per year with 150 mg of dabigatran (P = 0.051).35 The authors concluded that in patients with nonvalvular AF, dabigatran given at a dose of 110 mg twice daily was not inferior to warfarin, and was associated with lower rates of major hemorrhage than warfarin.35 Dabigatran given at a dose of 150 mg twice daily was associated with lower rates of stroke and systemic embolism than warfarin but had similar rates of major hemorrhage.35 These effects were maintained in patients with previous stroke or transient ischemic attack, and in these patients starting dabigatran with and without prior VKA treatment.45, 46
Dabigatran for Prevention of Venous Thromboembolism After Major Orthopedic Procedures
Without thromboprophylaxis, the incidence of venous thromboembolism (VTE) following major orthopedic surgery is 40%60%.47 Nevertheless, many patients do not receive appropriate thromboprophylaxis after orthopedic surgery, in part due to the limitations of VKAs and the inconvenience of low molecular weight heparin (LMWH) injections.48
RE‐NOVATE Trial
Oral dabigatran versus enoxaparin for thromboprophylaxis after primary total hip arthroplasty (RE‐NOVATE trail) was a prospective, noninferiority phase 3 trial in which 3494 patients undergoing total hip replacement (THR) were randomized in double‐blind fashion to 2835 days of dabigatran 220 mg or 150 mg once daily, starting with a half‐dose 14 hours after surgery, or subcutaneous (SC) enoxaparin 40 mg once daily, starting the evening before surgery.33 The primary efficacy outcome was the composite of total VTE (venographic or symptomatic) and death from all causes during treatment. The primary efficacy outcome occurred in 6.7% in the enoxaparin group versus 6.0% in the dabigatran 220 mg group (absolute difference [AD], 0.7%; 95% CI, 2.9% to 1.6%) and 8.6% in the 150 mg group (AD, 1.9%; 95% CI, 0.6% to 4.4%). There was no significant difference in major bleeding with either dose of dabigatran compared with enoxaparin (220 mg, P = 0.44; 150 mg, P = 0.60). It was concluded that oral dabigatran was not inferior to enoxaparin for prevention of VTE after THR surgery, with a similar safety profile.33
RE‐NOVATE II Trial
Oral dabigatran versus enoxaparin for thromboprophylaxis after primary total hip arthroplasty (RE‐NOVATE II trail) was a randomized, double‐blind, noninferiority phase 3 trial that compared dabigatran versus SC enoxaparin for extended thromboprophylaxis in patients undergoing THR.38 A total of 2055 patients were randomized to 2835 days of oral dabigatran, 220 mg once daily, starting with a half‐dose 14 hours after surgery, or SC enoxaparin 40 mg once daily, starting the evening before surgery. The primary efficacy outcome was the same as that in the RE‐NOVATE trial. The primary efficacy outcome occurred in 7.7% of the dabigatran group versus 8.8% of the enoxaparin group (risk difference, 1.1%; 95% CI, 3.8 to 1.6%; P 0.0001 for the prespecified noninferiority margin. Major VTE plus VTE‐related death occurred in 2.2% of the dabigatran group versus 4.2% of the enoxaparin group (risk difference, 1.9%; 95% CI, 3.6% to 0.2%; P = 0.03). Major bleeding occurred in 1.4% of the dabigatran group and 0.9% of the enoxaparin group (P = 0.40). It was concluded that extended prophylaxis with oral dabigatran 220 mg once daily was not inferior to SC enoxaparin 40 mg once daily for prevention of VTE after THR. The safety profiles were similar between the 2 arms.38
RE‐MODEL Trial
In the Oral dabigatran etexilate vs. subcutaneous enoxaparin for the prevention of venous thromblembloism after total knee replacement (RE‐MODEL trail) phase 3 trial, 2076 patients who underwent total knee replacement (TKR) were randomized to receive dabigatran 150 mg or 220 mg once daily starting with a half‐dose 14 hours after surgery, or SC enoxaparin 40 mg once daily starting the evening before surgery, for 610 days.32 Patients were followed‐up for 3 months. The primary efficacy outcome was a composite of total VTE (venographic or symptomatic) and mortality during treatment. The primary efficacy outcome occurred in 37.7% of the enoxaparin group versus 36.4% of the dabigatran 220 mg group (AD, 1.3%; 95% CI, 7.3 to 4.6) and 40.5% of the 150 mg group (AD, 2.8%; 95% CI, 3.1 to 8.7). The incidence of major bleeding did not differ between the groups (1.3% versus 1.5% and 1.3%, respectively). The conclusion was that dabigatran (220 mg or 150 mg) was not inferior to enoxaparin for prevention of VTE after TKR surgery and exhibited a similar safety profile.32
RE‐MOBILZE Trial
The oral thrombin inhibitor dabigatran etexilate vs the North American enoxaparin regimen for the prevention of venous thromboembolism after knee arthroplasty surgery (RE‐MOBILIZE trail) was a phase 3 trial that randomized 1896 patients after unilateral TKR to receive dabigatran 220 or 150 mg once daily versus enoxaparin 30 mg SC twice daily after surgery.40 Dosing stopped at contrast venography, 1215 days after surgery. Follow‐up was for 3 months. The primary outcome was a composite of total VTE events and all‐cause mortality during treatment. With respect to the primary outcome, dabigatran at 220 and 150 mg showed inferior efficacy to enoxaparin, with VTE rates of 31% (P = 0.02 vs enoxaparin), 34% (P 0.001 vs enoxaparin), and 25%, respectively. Major bleeding was similar. It was concluded that dabigatran was inferior to the twice‐daily North American enoxaparin regimen, probably because of the latter's more intense and prolonged dosing.40 It should be noted that the first dose of dabigatran in this study was given 612 hours after surgery, compared with 14 hours postoperatively in RE‐MODEL, which may have contributed to the inferior outcome.32, 40
Dabigatran for Treatment of Acute VTE
RE‐COVER was a large, randomized, noninferiority phase 3 trial that randomized 2564 patients with acute symptomatic proximal lower extremity deep vein thrombosis or pulmonary embolism to 6 months of dabigatran 150 mg twice daily or dose‐adjusted warfarin (INR 2/3).34 All patients initially received parenteral anticoagulation (LMWH or unfractionated heparin [UFH]) for a median of 9 days. Patients in the warfarin group spent 60% of the time in the therapeutic range. In the dabigatran arm, 2.4% had recurrent VTE versus 2.1% in the warfarin arm (P 0.001 for the prespecified noninferiority margin). Major bleeding occurred in 1.6% of patients in the dabigatran arm and 1.9% in the warfarin arm (hazards ratio, 0.82; 95% CI, 0.451.48). There was no difference in the other safety endpoints (acute coronary syndrome, abnormal liver function tests and deaths). Adverse events (especially gastrointestinal) leading to discontinuation of the study drug occurred in 9% of patients assigned to dabigatran and 6.8% of patients assigned to warfarin (P = 0.05). It was concluded that a fixed dose of dabigatran was not inferior to warfarin for treatment of VTE, with a similar safety profile.34 It is important to note that the first dose of dabigatran was given after a median of 9 days of parenteral anticoagulation therapy, so the findings of this study do not provide data regarding the use of dabigatran as initial monotherapy for acute VTE.34 The results of additional randomized trials evaluating the use of dabigatran for acute VTE treatment (RE‐COVER II) and secondary prevention of VTE (RE‐MEDY and RE‐SONATE) are expected soon.16
SAFETY OF DABIGATRAN
Aside from the bleeding risks discussed earlier, the most commonly reported side effect of dabigatran was dyspepsia. Dyspepsia occurred twice as frequently in patients taking dabigatran versus warfarin in the RE‐LY trial (11.5% vs 5.8%).35 One possible explanation for the higher incidence of dyspepsia is the tartaric acid component in dabigatran capsules.2 In the RE‐LY study, myocardial infarction occurred more commonly in the dabigatran arms (0.72% with 110 mg and 0.74% with 150 mg) than the warfarin arm (0.53%, P = 0.07 and 0.048, respectively).24, 35 It has been postulated that this observation could be related to a greater efficacy of warfarin for the prevention of myocardial infarction rather than an adverse effect of dabigatran.2 There was no increase in acute coronary syndrome rates noted with dabigatran in the other phase 3 trials.3234, 38, 40 No increased risk of elevated liver function test has been noted with dabigatran, but long‐term data are unavailable.32, 34, 35, 38
MANAGEMENT OF SPECIAL SITUATIONS THAT MAY ARISE IN THE USE OF DABIGATRAN
Switching From Warfarin to Dabigatran and Vice Versa
When converting patients from warfarin to dabigatran, it is recommended that dabigatran be started once the INR falls below the lower limit of the desired therapeutic range. Conversely, when switching from dabigatran to warfarin, the manufacturer recommends starting warfarin based on renal function (Table 2). It should be noted that because dabigatran can increase the INR, the INR will better reflect warfarin's effect after dabigatran has been stopped for at least 2 days.27, 28
| CrCL (mL/min) | Time of Warfarin Initiation |
|---|---|
| |
| 50 | 3 d before discontinuing dabigatran |
| 3150 | 2 d before discontinuing dabigatran |
| 1530 | 1 d before discontinuing dabigatran |
| 15 | No recommendations made |
Bridging from Dabigatran to Parenteral Anticoagulants and Vice Versa
For patients currently receiving a parenteral anticoagulant, the manufacturer recommends starting dabigatran 02 hours before the next administration time for parenteral anticoagulants (eg, LMWH) or at the time of discontinuation for continuously infused parenteral drugs (eg, intravenous UFH).28 For patients currently taking dabigatran who are transitioning to a parenteral anticoagulant, it is recommended to wait 12 hours (CrCl 30 mL/min) or 24 hours (CrCl 30 mL/min) after the last dose of dabigatran before initiating treatment with a parenteral anticoagulant.27, 28
Management of Dabigatran Before Elective and Urgent Invasive Procedures
Patients who undergo invasive procedures in the presence of therapeutic levels of dabigatran are at an increased risk of bleeding. The manufacturer recommends holding dabigatran for at least 24 hours before elective surgery depending on the degree of renal impairment and the risk of bleeding.28 Table 3 lists recommendations on the timing of discontinuation of dabigatran before a procedure. If emergent/urgent surgery is necessary for a patient who is on dabigatran, the risk of bleeding should be weighed against the urgency of the intervention.28, 42, 44 As mentioned earlier, the ECT or the Hemoclot Thrombin Inhibitor assay are the preferred tests for measurement of dabigatran effects, but they are not standardized or widely clinically available. Instead, prolongation of the TT (preferably) or the aPTT can be used to determine the presence of dabigatran.28, 42
| CrCL (mL/min) | Half‐Life (hr) | Suggested Timing of Discontinuation of Dabigatran Before Surgery | |
|---|---|---|---|
| Standard Risk of Bleeding | High Risk of Bleeding* | ||
| |||
| >80 | 13 (11‐22) | 24 hr | 24 d |
| 5180 | 15 (12‐34) | 24 hr | 24 d |
| 3150 | 18 (13‐23) | 48 hr | 4 d |
| 30 | 27 (22‐35) | 25 d | >5 d |
Overdose and Toxicity With Dabigatran
Accidental or intentional overdose, or accumulation of dabigatran due to renal impairment, may lead to hemorrhagic complications. Unlike warfarin and heparin, there is no antidote for dabigatran. There are no widely available, reliable laboratory tests to measure the anticoagulant activity of dabigatran, and evidence‐based guidelines to manage dabigatran toxicity do not exist. Therefore, in the event of dabigatran toxicity, treatment is largely supportive. Management of toxicity is dependent on whether the overdose/accumulation is accompanied by bleeding or not. For overdose, interventions include adequate diuresis and the use of activated charcoal to reduce the absorption of dabigatran (within 2 hours of ingestion).42 In the event of bleeding, proposed measures include application of mechanical pressure to the sites of bleeding and infusion of pro‐coagulant blood products such as activated prothrombin complex concentrates (eg, FEIBA VH, Baxter) or recombinant human activated factor VIIa (NovoSeven, Novo‐Nordisk) (reviewed in references 26 and 42). In life‐threatening situations, hemodialysis could be considered, because it can remove 60% of the drug within 23 hours.42 Hemoperfusion over a charcoal filter or large volume hemofiltration have also been suggested in extreme situations.27, 28, 36, 42 Acknowledging their limitations, the ECT, TT, or aPTT may be used to direct therapy.27, 42
Pregnancy and Dabigatran Therapy
Dabigatran is a class C drug during pregnancy, and there are no studies of dabigatran in pregnant women. Animal studies with dabigatran showed decreased fertility of pregnant rats; therefore, the risks and benefits of dabigatran therapy during pregnancy should be weighed carefully.27, 28, 44
CONCLUSIONS
Dabigatran is a novel, oral direct thrombin inhibitor that exhibits several advantages over warfarin. The predictable pharmacokinetic profile and minimal food and drug interactions of dabigatran allow for a fixed‐dosing regimen and obviate the need for routine laboratory monitoring. However, this apparent advantage is also a disadvantage. The lack of a reliable method to monitor dabigatran makes it more difficult to assess compliance, measure the impact of drug interactions, evaluate for toxicity, and determine bona fide therapeutic failure versus noncompliance in the event of breakthrough thromboembolism.28, 42 Other limitations of dabigatran include the lack of an antidote and the dependence on normal renal function for elimination, with the potential for drug accumulation and toxicity with renal impairment. The noninferiority design of the clinical trials that evaluated dabigatran, the absence of long‐term safety and efficacy data, and issues related to the cost effectiveness of dabigatran should be considered when prescribing this agent. More studies are needed to assess dabigatran in special patient populations (eg, the elderly, patients with renal and hepatic impairment, pediatric and pregnant patients) and to better understand dabigatrandrug interactions.
As more novel oral anticoagulant agents, such as factor Xa inhibitors, become available for clinical use, comparative studies will need to be performed to better define the role of each agent for specific indications. In the future, it might be possible to tailor the choice of the oral anticoagulant to the individual patient not only on the basis of the clinical indication but also the specific patient characteristics and possible drug interactions. For example, rivaroxaban (Xarelto) is an oral direct factor Xa that was recently approved in the United States for VTE thromboprophylaxis following orthopedic surgery and in patients with non‐valvular atrial fibrillation.2 Similar to dabigatran, rivaroxaban exhibits predictable PK and PD that allow fixed once or twice daily dosing and obviate the need for routine monitoring of its anticoagulant effects.2, 16 Unlike dabigatran, rivaroxaban is an active drug and not a prodrug, and has a significantly higher bioavailability than dabigatran (>80% vs 6%).16 In addition, the levels of rivaroxaban can be affected by drugs that interfere with both P‐gp and the hepatic CYP‐450 system, compared with dabigatran, which is affected only by drugs that affect P‐gp.8, 16
Vitamin K antagonists (VKAs) such as warfarin have been the backbone of oral anticoagulation in clinical practice since the middle of the last century. Despite their efficacy, VKAs have well‐recognized limitations that have led to their underutilization in patients who would otherwise be candidates for oral anticoagulation.14 These limitations include a narrow therapeutic window and significant intra‐ and interindividual variability in dose requirements as well as numerous drugdrug and drugfood interactions.59 Therefore, VKAs require close laboratory monitoring to prevent excessive or under‐anticoagulation, and maintaining therapeutic anticoagulation with VKAs remains a challenging task in many patients.2 It has been shown that 30%50% of international normalized ratio (INR) results fall outside of the targeted therapeutic range.10, 11 Consequently, it is not surprising that warfarin is a common cause of medication‐related emergency room visits.12 Despite many fruitless years of searching for better alternatives, VKAs have remained the mainstay of oral anticoagulation for more than 60 years.8
An ideal anticoagulant would be orally administered, effective, safe, exhibit a predictable pharmacokinetic profile and a low potential for drug or dietary interactions, and therefore would not require routine laboratory monitoring.2, 5, 13 Other desirable characteristics would include a rapid onset of action to decrease or eliminate the need for bridging therapy, and rapid reversibility with or without an antidote.8, 13 To date, no oral anticoagulant has been developed that possesses all of these desired characteristics. Dabigatran etexilate (Pradaxa, Boehringer Ingelheim Pharmaceuticals, Inc.) has recently become the first oral anticoagulant to be available for wide clinical use since the 1950s.14 In the following sections, we provide an overview of dabigatran etexilate, with a special focus on issues that are pertinent to hospitalists and the hospitalized patient.
PHARMACOLOGY OF DABIGATRAN ETEXILATE
Pharmacokinetics and Pharmacodynamics of Dabigatran Etexilate
A comparison of the pharmacokinetic (PK) and pharmacodynamic (PD) properties of dabigatran etexilate (dabigatran) and warfarin are presented in Table 1. Dabigatran etexilate (referred to from this point as dabigatran) is a prodrug of dabigatran, which blocks the terminal coagulation cascade by binding to the active site of thrombin and selectively inhibiting this critical serine protease in a dose‐dependent and reversible fashion.15 Thrombin plays a central role in blood coagulation by converting fibrinogen to fibrin, amplifying its own generation by feedback activation of factors V, VIII, and XI, and by activating platelets (Figure 1).16 Dabigatran is a direct thrombin inhibitor that acts independently of anti‐thrombin to inhibit both free and clot‐bound thrombin.17, 18 The bioavailability of dabigatran after oral intake is low (6%7%).1923 After absorption, the prodrug is rapidly converted by plasma and hepatic esterases to the active drug dabigatran, but it is not metabolized by the CYP‐450 system, therefore reducing the potential for drugdrug interactions.8, 2328 The long half‐life of dabigatran allows for once or twice daily dosing.21, 24 The PK profile of dabigatran is predictable, with minimal inter‐ and intraindividual variation.21, 22
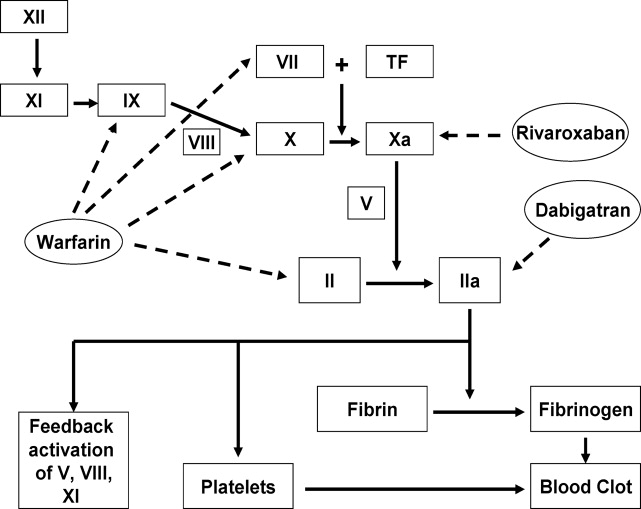
| Warfarin | Dabigatran | |
|---|---|---|
| Mechanism of action | Reduces functional levels of vitamin Kdependent factors II, VII, IX, and X by inhibiting vitamin K epoxide reductase | Binds to active site of thrombin (factor IIa) and reversibly inhibits free and clot‐bound thrombin |
| Prodrug | No | Yes |
| Bioavailability | >90%95% | 6%7% |
| Protein binding | 99% | 35% |
| Time to reach peak plasma levels | 7296 hr | 23 hr |
| Half‐life | 3644 hr | 1217 hr |
| Routine coagulation monitoring | Required, but frequency varies based on clinical situation | No requirement for routine monitoring |
| Schedule | INR‐adjusted, usually once daily | Fixed dose, once or twice daily |
| Metabolism | CYP‐450 hepatic microsomal enzymes, especially CYP2C9, CYP1A2, and CYP3A4 | Esterase‐catalyzed hydrolysis in plasma or liver after intestinal P‐gp transport |
| Clearance | Almost entirely hepatic | 80% unchanged renally (after an intravenous dose), 20% hepatic after conjugation |
| Drug interactions | Drugs that affect CYP‐450 hepatic microsomal enzymes and those that displace warfarin from plasma proteins | P‐gp inhibitors (CYP‐450 system not involved) |
| Antidote | Yes (vitamin K and plasma products) | No |
Dabigatran is packaged in capsules that are hygroscopic. Therefore, the capsules should be stored in the original container with the cap tightly closed. Exposure of dabigatran capsules to air for prolonged periods outside the original container can result in deterioration of the active compound and reduced efficacy.27, 28 Dabigatran capsules contain tartaric acid which is necessary to facilitate dissolution of the medication in the gastrointestinal tract for optimal absorption.2 Breaking the capsules or removing the drug from the capsule can result in increased exposure. Therefore, dabigatran capsules should be taken intact, and patients should be instructed that dabigatran capsules should not be broken, chewed, or opened before administration.28 Alternative anticoagulants should be used if patients cannot swallow the capsule intact for any reason (eg, intubated patients).
Dabigatran and Drug and Food Interactions
Dabigatran acts as a substrate of the transporter protein P‐glycoprotein (P‐gp), which is also involved in the transport of many other drugs.5, 16 P‐gp is an efflux pump that functions to prevent the absorption of drugs in the intestine or increase the renal excretion of drugs that are P‐gp substrates.25 Inhibitors of P‐gp increase the serum concentrations of P‐gp substrates, whereas P‐gp inducers reduce the concentrations of these medications.13 Examples of P‐gp inhibitors include clarithromycin, quinidine, and verapamil, whereas rifampin, pantoprazole, and St John's wort are known to induce P‐gp.5, 24, 26 As an illustration, the coadministration of dabigatran and amiodarone, a known P‐gp inhibitor, increases the area under the curve of drug plasmaconcentrationtime of dabigatran by 60% without significantly affecting levels of amiodarone.5, 27 Nevertheless, dagibatran's prescribing information in the United States advises that the P‐gp inhibitors ketoconazole, verapamil, amiodarone, quinidine, and clarithromycin do not require dose adjustments, although these results should not be extrapolated to other P‐gp inhibitors.28 In addition, the manufacturer recommends generally avoiding the concomitant use of the potent P‐gp inducer rifampin with dabigatran, whereas the European Medicines Agency advises caution in the coadministration of rifampin or St John's wort with dabigatran.27, 28
Not all P‐gp substrates result in clinically significant interactions with dabigatran (eg, digoxin, diclofenac, and atorvastatin).19, 29 The use of nonsteroidal anti‐inflammatory drugs and aspirin may increase the risk of bleeding in patients using dabigatran.5, 26, 27 It is not recommended to coadminister certain anti‐platelet agents (such as clopidogrel, prasugrel, or ticlopidine) with dabigatran.26, 30 Although the use of proton pump inhibitors such as pantoprazole leads to a 30% decrease in the area under the curve of dabigatran, coadministration of pantoprazole and other proton pump inhibitors with dabigatran in clinical trials did not affect bleeding risk or efficacy.27 Attention to potential drug interactions with dabigatran is important, because dabigatran is not usually monitored. Food interactions with dabigatran appear to be low, and therefore dabigatran can probably be taken with or without food, but caution is advised given the limited postmarketing experience with dabigatran.30 An excellent review of drug and dietary interactions of dabigatran has been published recently.5
Use of Dabigatran in Patients With Liver or Renal Impairment
Approximately 80% of dabigatran is excreted, largely unchanged, by the kidneys in healthy subjects.19 Patients with severe renal impairment (creatinine clearance [CrCL], 30 mL/min) were excluded from phase 3 trials that evaluated dabigatran.3135 A small study in patients with renal impairment showed a linear correlation between renal function and renal clearance of dabigatran, with proportional increases in the anticoagulant effects of dabigatran with decreasing renal function.36 For patients on hemodialysis, 62%68% of the dose was removed.36 The authors recommended avoidance of dabigatran in severe renal impairment, and a dose reduction was recommended for moderate renal impairment (CrCL, 3150 mL/min).13, 36 Despite exclusion of patients with CrCL of 30 mL/min from all phase 3 trials of dabigatran and the relative contraindication of the use of dabigatran in this patient population, the US Food and Drug Administration (FDA) approved a reduced dose of 75 mg twice daily for patients with CrCL of 1530 mL/min, but no dosing recommendations were made for patients with CrCL of 15 mL/min or for patients on dialysis.13, 28, 36 We believe that dabigatran should be used with great caution in patients with CrCl 1530 mL/min given the limited outcome data in these patients, and alternative anticoagulants should be strongly considered for these patients until more data are available.
Less than 20% of the dabigatran dose is conjugated in the liver and subsequently secreted in the biliary system.19, 23 Stangier et al. showed that moderate hepatic impairment does not affect the PK/PD or safety profile of dabigatran and concluded that dabigatran can be given to those patients without dose adjustment.37 On the other hand, severe hepatic impairment (Child‐Pugh class B or C cirrhosis) and an alanine aminotransferase level more than 2 to 3 times the upper limit of normal were used as exclusion criteria in most of the phase 3 trials that evaluated dabigatran.16, 24, 34, 35, 38 The hepatic toxicity noted with the first generation oral direct thrombin inhibitor, ximelagatran, has not been seen with dabigatran in clinical trials, although long‐term postmarketing data are lacking.32, 34, 35, 3840
The Effect of Dabigatran on Common Coagulation Laboratory Tests and Recommendations for Monitoring Dabigatran's Anticoagulant Effects
Despite the predictable PK profile of dabigatran, its effects on common coagulation assays remain incompletely defined.41 Most patients on dabigatran will have a prolonged activated partial thromboplastin time (aPTT) even at trough concentrations, but not in a linear predictable fashion.19, 20, 21, 36, 41 Dabigatran has few and unpredictable effects on prothrombin time (PT) and INR, and therapeutic concentrations of dabigatran usually result in only modest elevations of PT/INR.21, 42 Although thrombin time (TT) displays a good linear correlation with plasma concentrations of dabigatran, the reagents used to perform TT in most clinical laboratories are not standardized. Therefore, TT is better suited to detecting the presence of dabigatran rather than monitoring its anticoagulant effects.24, 42 Therefore, even a slightly prolonged aPTT or TT could reflect significant plasma dabigatran levels. The best assays for monitoring dabigatran are the ecarin clotting time (ECT), modified thrombelastographic evaluations of whole blood clot formation, and the Hemoclot Thrombin Inhibitor assay, but these tests are limited by lack of standardization and limited clinical availablity.24, 42, 43
EFFICACY OF DABIGATRAN
In this section, we provide a brief review of the major phase 3 trials that evaluated dabigatran for different indications (see references 13, 16, and 24 for recent detailed reviews of the clinical trials of dabigatran).
Dabigatran for Thromboprophylaxis in Patients with Atrial Fibrillation
The Randomized Evaluation of Long‐Term Anticoagulation Therapy (RE‐LY) trial was a prospective, noninferiority, phase 3 study of dabigatran that was the basis for its FDA approval in patients with nonvalvular AF.35, 44 In RE‐LY, 18,113 AF patients with another thromboembolic risk factor were randomized to receive fixed doses of dabigatran (110 mg or 150 mg twice daily) or adjusted‐dose warfarin.35 The median duration of follow‐up was 2 years and the primary outcome was stroke or systemic embolism. The primary outcome occurred in 1.69% per year in the warfarin group versus 1.53% per year in the group receiving 110 mg of dabigatran twice daily (relative risk with dabigatran, 0.91; 95% confidence interval [CI], 0.741.11; P 0.001 for noninferiority) and 1.11% per year in the group receiving 150 mg of dabigatran twice daily (relative risk, 0.66; 95% CI, 0.530.82; P 0.001 for superiority). The rate of major bleeding was 3.36% per year in the warfarin group versus 2.71% per year in the dabigatran 110 mg group (P = 0.003) and 3.11% per year in the dabigatran 150 mg group (P = 0.31). Intracranial bleeds were significantly less common in both dabigatran groups than with warfarin. Major gastrointestinal bleeding rate was significantly higher in the dabigatran group at the 150‐mg dose than in the warfarin group. The mortality rate was 4.13% per year in the warfarin group versus 3.75% per year with 110 mg of dabigatran (P = 0.13) and 3.64% per year with 150 mg of dabigatran (P = 0.051).35 The authors concluded that in patients with nonvalvular AF, dabigatran given at a dose of 110 mg twice daily was not inferior to warfarin, and was associated with lower rates of major hemorrhage than warfarin.35 Dabigatran given at a dose of 150 mg twice daily was associated with lower rates of stroke and systemic embolism than warfarin but had similar rates of major hemorrhage.35 These effects were maintained in patients with previous stroke or transient ischemic attack, and in these patients starting dabigatran with and without prior VKA treatment.45, 46
Dabigatran for Prevention of Venous Thromboembolism After Major Orthopedic Procedures
Without thromboprophylaxis, the incidence of venous thromboembolism (VTE) following major orthopedic surgery is 40%60%.47 Nevertheless, many patients do not receive appropriate thromboprophylaxis after orthopedic surgery, in part due to the limitations of VKAs and the inconvenience of low molecular weight heparin (LMWH) injections.48
RE‐NOVATE Trial
Oral dabigatran versus enoxaparin for thromboprophylaxis after primary total hip arthroplasty (RE‐NOVATE trail) was a prospective, noninferiority phase 3 trial in which 3494 patients undergoing total hip replacement (THR) were randomized in double‐blind fashion to 2835 days of dabigatran 220 mg or 150 mg once daily, starting with a half‐dose 14 hours after surgery, or subcutaneous (SC) enoxaparin 40 mg once daily, starting the evening before surgery.33 The primary efficacy outcome was the composite of total VTE (venographic or symptomatic) and death from all causes during treatment. The primary efficacy outcome occurred in 6.7% in the enoxaparin group versus 6.0% in the dabigatran 220 mg group (absolute difference [AD], 0.7%; 95% CI, 2.9% to 1.6%) and 8.6% in the 150 mg group (AD, 1.9%; 95% CI, 0.6% to 4.4%). There was no significant difference in major bleeding with either dose of dabigatran compared with enoxaparin (220 mg, P = 0.44; 150 mg, P = 0.60). It was concluded that oral dabigatran was not inferior to enoxaparin for prevention of VTE after THR surgery, with a similar safety profile.33
RE‐NOVATE II Trial
Oral dabigatran versus enoxaparin for thromboprophylaxis after primary total hip arthroplasty (RE‐NOVATE II trail) was a randomized, double‐blind, noninferiority phase 3 trial that compared dabigatran versus SC enoxaparin for extended thromboprophylaxis in patients undergoing THR.38 A total of 2055 patients were randomized to 2835 days of oral dabigatran, 220 mg once daily, starting with a half‐dose 14 hours after surgery, or SC enoxaparin 40 mg once daily, starting the evening before surgery. The primary efficacy outcome was the same as that in the RE‐NOVATE trial. The primary efficacy outcome occurred in 7.7% of the dabigatran group versus 8.8% of the enoxaparin group (risk difference, 1.1%; 95% CI, 3.8 to 1.6%; P 0.0001 for the prespecified noninferiority margin. Major VTE plus VTE‐related death occurred in 2.2% of the dabigatran group versus 4.2% of the enoxaparin group (risk difference, 1.9%; 95% CI, 3.6% to 0.2%; P = 0.03). Major bleeding occurred in 1.4% of the dabigatran group and 0.9% of the enoxaparin group (P = 0.40). It was concluded that extended prophylaxis with oral dabigatran 220 mg once daily was not inferior to SC enoxaparin 40 mg once daily for prevention of VTE after THR. The safety profiles were similar between the 2 arms.38
RE‐MODEL Trial
In the Oral dabigatran etexilate vs. subcutaneous enoxaparin for the prevention of venous thromblembloism after total knee replacement (RE‐MODEL trail) phase 3 trial, 2076 patients who underwent total knee replacement (TKR) were randomized to receive dabigatran 150 mg or 220 mg once daily starting with a half‐dose 14 hours after surgery, or SC enoxaparin 40 mg once daily starting the evening before surgery, for 610 days.32 Patients were followed‐up for 3 months. The primary efficacy outcome was a composite of total VTE (venographic or symptomatic) and mortality during treatment. The primary efficacy outcome occurred in 37.7% of the enoxaparin group versus 36.4% of the dabigatran 220 mg group (AD, 1.3%; 95% CI, 7.3 to 4.6) and 40.5% of the 150 mg group (AD, 2.8%; 95% CI, 3.1 to 8.7). The incidence of major bleeding did not differ between the groups (1.3% versus 1.5% and 1.3%, respectively). The conclusion was that dabigatran (220 mg or 150 mg) was not inferior to enoxaparin for prevention of VTE after TKR surgery and exhibited a similar safety profile.32
RE‐MOBILZE Trial
The oral thrombin inhibitor dabigatran etexilate vs the North American enoxaparin regimen for the prevention of venous thromboembolism after knee arthroplasty surgery (RE‐MOBILIZE trail) was a phase 3 trial that randomized 1896 patients after unilateral TKR to receive dabigatran 220 or 150 mg once daily versus enoxaparin 30 mg SC twice daily after surgery.40 Dosing stopped at contrast venography, 1215 days after surgery. Follow‐up was for 3 months. The primary outcome was a composite of total VTE events and all‐cause mortality during treatment. With respect to the primary outcome, dabigatran at 220 and 150 mg showed inferior efficacy to enoxaparin, with VTE rates of 31% (P = 0.02 vs enoxaparin), 34% (P 0.001 vs enoxaparin), and 25%, respectively. Major bleeding was similar. It was concluded that dabigatran was inferior to the twice‐daily North American enoxaparin regimen, probably because of the latter's more intense and prolonged dosing.40 It should be noted that the first dose of dabigatran in this study was given 612 hours after surgery, compared with 14 hours postoperatively in RE‐MODEL, which may have contributed to the inferior outcome.32, 40
Dabigatran for Treatment of Acute VTE
RE‐COVER was a large, randomized, noninferiority phase 3 trial that randomized 2564 patients with acute symptomatic proximal lower extremity deep vein thrombosis or pulmonary embolism to 6 months of dabigatran 150 mg twice daily or dose‐adjusted warfarin (INR 2/3).34 All patients initially received parenteral anticoagulation (LMWH or unfractionated heparin [UFH]) for a median of 9 days. Patients in the warfarin group spent 60% of the time in the therapeutic range. In the dabigatran arm, 2.4% had recurrent VTE versus 2.1% in the warfarin arm (P 0.001 for the prespecified noninferiority margin). Major bleeding occurred in 1.6% of patients in the dabigatran arm and 1.9% in the warfarin arm (hazards ratio, 0.82; 95% CI, 0.451.48). There was no difference in the other safety endpoints (acute coronary syndrome, abnormal liver function tests and deaths). Adverse events (especially gastrointestinal) leading to discontinuation of the study drug occurred in 9% of patients assigned to dabigatran and 6.8% of patients assigned to warfarin (P = 0.05). It was concluded that a fixed dose of dabigatran was not inferior to warfarin for treatment of VTE, with a similar safety profile.34 It is important to note that the first dose of dabigatran was given after a median of 9 days of parenteral anticoagulation therapy, so the findings of this study do not provide data regarding the use of dabigatran as initial monotherapy for acute VTE.34 The results of additional randomized trials evaluating the use of dabigatran for acute VTE treatment (RE‐COVER II) and secondary prevention of VTE (RE‐MEDY and RE‐SONATE) are expected soon.16
SAFETY OF DABIGATRAN
Aside from the bleeding risks discussed earlier, the most commonly reported side effect of dabigatran was dyspepsia. Dyspepsia occurred twice as frequently in patients taking dabigatran versus warfarin in the RE‐LY trial (11.5% vs 5.8%).35 One possible explanation for the higher incidence of dyspepsia is the tartaric acid component in dabigatran capsules.2 In the RE‐LY study, myocardial infarction occurred more commonly in the dabigatran arms (0.72% with 110 mg and 0.74% with 150 mg) than the warfarin arm (0.53%, P = 0.07 and 0.048, respectively).24, 35 It has been postulated that this observation could be related to a greater efficacy of warfarin for the prevention of myocardial infarction rather than an adverse effect of dabigatran.2 There was no increase in acute coronary syndrome rates noted with dabigatran in the other phase 3 trials.3234, 38, 40 No increased risk of elevated liver function test has been noted with dabigatran, but long‐term data are unavailable.32, 34, 35, 38
MANAGEMENT OF SPECIAL SITUATIONS THAT MAY ARISE IN THE USE OF DABIGATRAN
Switching From Warfarin to Dabigatran and Vice Versa
When converting patients from warfarin to dabigatran, it is recommended that dabigatran be started once the INR falls below the lower limit of the desired therapeutic range. Conversely, when switching from dabigatran to warfarin, the manufacturer recommends starting warfarin based on renal function (Table 2). It should be noted that because dabigatran can increase the INR, the INR will better reflect warfarin's effect after dabigatran has been stopped for at least 2 days.27, 28
| CrCL (mL/min) | Time of Warfarin Initiation |
|---|---|
| |
| 50 | 3 d before discontinuing dabigatran |
| 3150 | 2 d before discontinuing dabigatran |
| 1530 | 1 d before discontinuing dabigatran |
| 15 | No recommendations made |
Bridging from Dabigatran to Parenteral Anticoagulants and Vice Versa
For patients currently receiving a parenteral anticoagulant, the manufacturer recommends starting dabigatran 02 hours before the next administration time for parenteral anticoagulants (eg, LMWH) or at the time of discontinuation for continuously infused parenteral drugs (eg, intravenous UFH).28 For patients currently taking dabigatran who are transitioning to a parenteral anticoagulant, it is recommended to wait 12 hours (CrCl 30 mL/min) or 24 hours (CrCl 30 mL/min) after the last dose of dabigatran before initiating treatment with a parenteral anticoagulant.27, 28
Management of Dabigatran Before Elective and Urgent Invasive Procedures
Patients who undergo invasive procedures in the presence of therapeutic levels of dabigatran are at an increased risk of bleeding. The manufacturer recommends holding dabigatran for at least 24 hours before elective surgery depending on the degree of renal impairment and the risk of bleeding.28 Table 3 lists recommendations on the timing of discontinuation of dabigatran before a procedure. If emergent/urgent surgery is necessary for a patient who is on dabigatran, the risk of bleeding should be weighed against the urgency of the intervention.28, 42, 44 As mentioned earlier, the ECT or the Hemoclot Thrombin Inhibitor assay are the preferred tests for measurement of dabigatran effects, but they are not standardized or widely clinically available. Instead, prolongation of the TT (preferably) or the aPTT can be used to determine the presence of dabigatran.28, 42
| CrCL (mL/min) | Half‐Life (hr) | Suggested Timing of Discontinuation of Dabigatran Before Surgery | |
|---|---|---|---|
| Standard Risk of Bleeding | High Risk of Bleeding* | ||
| |||
| >80 | 13 (11‐22) | 24 hr | 24 d |
| 5180 | 15 (12‐34) | 24 hr | 24 d |
| 3150 | 18 (13‐23) | 48 hr | 4 d |
| 30 | 27 (22‐35) | 25 d | >5 d |
Overdose and Toxicity With Dabigatran
Accidental or intentional overdose, or accumulation of dabigatran due to renal impairment, may lead to hemorrhagic complications. Unlike warfarin and heparin, there is no antidote for dabigatran. There are no widely available, reliable laboratory tests to measure the anticoagulant activity of dabigatran, and evidence‐based guidelines to manage dabigatran toxicity do not exist. Therefore, in the event of dabigatran toxicity, treatment is largely supportive. Management of toxicity is dependent on whether the overdose/accumulation is accompanied by bleeding or not. For overdose, interventions include adequate diuresis and the use of activated charcoal to reduce the absorption of dabigatran (within 2 hours of ingestion).42 In the event of bleeding, proposed measures include application of mechanical pressure to the sites of bleeding and infusion of pro‐coagulant blood products such as activated prothrombin complex concentrates (eg, FEIBA VH, Baxter) or recombinant human activated factor VIIa (NovoSeven, Novo‐Nordisk) (reviewed in references 26 and 42). In life‐threatening situations, hemodialysis could be considered, because it can remove 60% of the drug within 23 hours.42 Hemoperfusion over a charcoal filter or large volume hemofiltration have also been suggested in extreme situations.27, 28, 36, 42 Acknowledging their limitations, the ECT, TT, or aPTT may be used to direct therapy.27, 42
Pregnancy and Dabigatran Therapy
Dabigatran is a class C drug during pregnancy, and there are no studies of dabigatran in pregnant women. Animal studies with dabigatran showed decreased fertility of pregnant rats; therefore, the risks and benefits of dabigatran therapy during pregnancy should be weighed carefully.27, 28, 44
CONCLUSIONS
Dabigatran is a novel, oral direct thrombin inhibitor that exhibits several advantages over warfarin. The predictable pharmacokinetic profile and minimal food and drug interactions of dabigatran allow for a fixed‐dosing regimen and obviate the need for routine laboratory monitoring. However, this apparent advantage is also a disadvantage. The lack of a reliable method to monitor dabigatran makes it more difficult to assess compliance, measure the impact of drug interactions, evaluate for toxicity, and determine bona fide therapeutic failure versus noncompliance in the event of breakthrough thromboembolism.28, 42 Other limitations of dabigatran include the lack of an antidote and the dependence on normal renal function for elimination, with the potential for drug accumulation and toxicity with renal impairment. The noninferiority design of the clinical trials that evaluated dabigatran, the absence of long‐term safety and efficacy data, and issues related to the cost effectiveness of dabigatran should be considered when prescribing this agent. More studies are needed to assess dabigatran in special patient populations (eg, the elderly, patients with renal and hepatic impairment, pediatric and pregnant patients) and to better understand dabigatrandrug interactions.
As more novel oral anticoagulant agents, such as factor Xa inhibitors, become available for clinical use, comparative studies will need to be performed to better define the role of each agent for specific indications. In the future, it might be possible to tailor the choice of the oral anticoagulant to the individual patient not only on the basis of the clinical indication but also the specific patient characteristics and possible drug interactions. For example, rivaroxaban (Xarelto) is an oral direct factor Xa that was recently approved in the United States for VTE thromboprophylaxis following orthopedic surgery and in patients with non‐valvular atrial fibrillation.2 Similar to dabigatran, rivaroxaban exhibits predictable PK and PD that allow fixed once or twice daily dosing and obviate the need for routine monitoring of its anticoagulant effects.2, 16 Unlike dabigatran, rivaroxaban is an active drug and not a prodrug, and has a significantly higher bioavailability than dabigatran (>80% vs 6%).16 In addition, the levels of rivaroxaban can be affected by drugs that interfere with both P‐gp and the hepatic CYP‐450 system, compared with dabigatran, which is affected only by drugs that affect P‐gp.8, 16
- ,,, et al.The use of antithrombotic therapies in the prevention and treatment of arterial and venous thrombosis: a survey of current knowledge and practice supporting the need for clinical education.Crit Pathw Cardiol.2010;9:41–48.
- .Warfarin versus new agents: interpreting the data.Hematology Am Soc Hematol Educ Program.2010;2010:221–228.
- ,,,,.Why do patients with atrial fibrillation not receive warfarin?Arch Intern Med.2000;160:41–46.
- ,,,,,.Warfarin use among ambulatory patients with nonvalvular atrial fibrillation: The anticoagulation and risk factors in atrial fibrillation (ATRIA) study.Ann Intern Med.1999;131:927–934.
- ,.Drug and dietary interactions of the new and emerging oral anticoagulants.Int J Clin Pract.2010;64:956–967.
- ,,, et al.The risk of bleeding complications in patients with cytochrome P450 CYP2C9*2 or CYP2C9*3 alleles on acenocoumarol or phenprocoumon.Thromb Haemost.2004;92:61–66.
- ,,, et al.Differentiating low‐molecular‐weight heparins based on chemical, biological, and pharmacologic properties: implications for the development of generic versions of low‐molecular‐weight heparins.Semin Thromb Hemost.2008;34:74–85.
- ,.Emerging anticoagulants.Expert Opin Emerg Drugs.2011;16:31–44.
- ,,, et al.Systematic overview of warfarin and its drug and food interactions.Arch Intern Med.2005;165:1095–1106.
- ,,,,,.Evaluation of the pattern of treatment, level of anticoagulation control, and outcome of treatment with warfarin in patients with non‐valvar atrial fibrillation: a record linkage study in a large british population.Heart.2005;91:472–477.
- ,,, et al.Comparison of outcomes among patients randomized to warfarin therapy according to anticoagulant control: results from SPORTIF III and V.Arch Intern Med.2007;167:239–245.
- ,,,.Medication use leading to emergency department visits for adverse drug events in older adults.Ann Intern Med.2007;147:755–765.
- .New oral anticoagulants: a practical guide for clinicians.J Thromb Thrombolysis.2010;29:182–191.
- ,,,.The quest for new anticoagulants: from clinical development to clinical practice [published ahead of print June 14, 2010].Cardiovasc Ther.2010. doi: 10.1111/j.1755–5922.2010.00160.x.
- ,,,,.In‐vitro profile and ex‐vivo anticoagulant activity of the direct thrombin inhibitor dabigatran and its orally active prodrug, dabigatran etexilate.Thromb Haemost.2007;98:155–162.
- ,,.Novel oral factor xa and thrombin inhibitors in the management of thromboembolism.Annu Rev Med.2011;62:41–57.
- ,,,,.Clot‐bound thrombin is protected from inhibition by heparin‐antithrombin III but is susceptible to inactivation by antithrombin III‐independent inhibitors.J Clin Invest.1990;86:385–391.
- ,,.Thrombin binds to soluble fibrin degradation products where it is protected from inhibition by heparin‐antithrombin but susceptible to inactivation by antithrombin‐independent inhibitors.Circulation.1998;97:544–552.
- .Clinical pharmacokinetics and pharmacodynamics of the oral direct thrombin inhibitor dabigatran etexilate.Clin Pharmacokinet.2008;47:285–295.
- ,.Pharmacology, pharmacokinetics, and pharmacodynamics of dabigatran etexilate, an oral direct thrombin inhibitor.Clin Appl Thromb Hemost.2009;15(suppl 1):9S–16S.
- ,,,,.The pharmacokinetics, pharmacodynamics and tolerability of dabigatran etexilate, a new oral direct thrombin inhibitor, in healthy male subjects.Br J Clin Pharmacol.2007;64:292–303.
- ,,,.Pharmacokinetics and pharmacodynamics of the direct oral thrombin inhibitor dabigatran in healthy elderly subjects.Clin Pharmacokinet.2008;47:47–59.
- ,,,,.The metabolism and disposition of the oral direct thrombin inhibitor, dabigatran, in humans.Drug Metab Dispos.2008;36:386–399.
- ,,.Dabigatran etexilate versus warfarin as the oral anticoagulant of choice? A review of clinical data.Pharmacol Ther.2011;129:185–194.
- .The role of P‐glycoprotein and organic anion‐transporting polypeptides in drug interactions.Drug Saf.2005;28:789–801.
- ,,.Novel oral anticoagulants: implications in the perioperative setting.Anesthesiology.2010;113:726–745.
- European Medicines Agency. Pradaxa (dabigatran etexilate) [product information]. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_‐_Product_Information/human/000829/WC 500041059.pdf. Accessed March 25,2011.
- Dabigatran medication guide. Available at: http://bidocs.boehringer‐ingelheim.com/BIWebAccess/ViewServlet.ser?docBase = renetnt9:59–68.
- ,,.Novel oral anticoagulants: the potential relegation of vitamin K antagonists in clinical practice.Int J Clin Pract.2010;64:835–838.
- .The RE‐LY study: Randomized Evaluation of Long‐term anticoagulant therapY: dabigatran vs. warfarin.Eur Heart J.2009;30:2554–2555.
- ,,, et al.Oral dabigatran etexilate vs. subcutaneous enoxaparin for the prevention of venous thromboembolism after total knee replacement: the RE‐MODEL randomized trial.J Thromb Haemost.2007;5:2178–2185.
- ,,, et al.Dabigatran etexilate versus enoxaparin for prevention of venous thromboembolism after total hip replacement: a randomised, double‐blind, non‐inferiority trial.Lancet.2007;370:949–956.
- ,,, et al.Dabigatran versus warfarin in the treatment of acute venous thromboembolism.N Engl J Med.2009;361:2342–2352.
- ,,, et al.Dabigatran versus warfarin in patients with atrial fibrillation.N Engl J Med.2009;361:1139–1151.
- ,,,.Influence of renal impairment on the pharmacokinetics and pharmacodynamics of oral dabigatran etexilate: an open‐label, parallel‐group, single‐centre study.Clin Pharmacokinet.2010;49:259–268.
- ,,,,.Pharmacokinetics and pharmacodynamics of dabigatran etexilate, an oral direct thrombin inhibitor, are not affected by moderate hepatic impairment.J Clin Pharmacol.2008;48:1411–1419.
- ,,, et al.Oral dabigatran versus enoxaparin for thromboprophylaxis after primary total hip arthroplasty (RE‐NOVATE II). A randomised, double‐blind, non‐inferiority trial.Thromb Haemost.2011;105:721–729.
- ,.Insights from the dabigatran versus warfarin trial in patients with venous thromboembolism (the RE‐COVER trial).Expert Opin Pharmacother.2010;11:1035–1037.
- RE‐MOBILIZE Writing Committee,,, et al.Oral thrombin inhibitor dabigatran etexilate vs north american enoxaparin regimen for prevention of venous thromboembolism after knee arthroplasty surgery.J Arthroplasty.2009;24:1–9.
- ,,, et al.Effects of the oral, direct thrombin inhibitor dabigatran on five common coagulation assays.Thromb Haemost.2011;105:371–378.
- ,,, et al.Dabigatran etexilate—a novel, reversible, oral direct thrombin inhibitor: interpretation of coagulation assays and reversal of anticoagulant activity.Thromb Haemost.2010;103:1116–1127.
- ,.A direct thrombin inhibitor studied by dynamic whole blood clot formation. haemostatic response to ex‐vivo addition of recombinant factor VIIa or activated prothrombin complex concentrate.Thromb Haemost.2006;96:446–453.
- US Food and Drug Administration. Dabigatran drug approval history. Available at: http://www.accessdata.fda.gov/drugsatfda_ docs/nda/2010/022512Orig1s000TOC.cfm. Accessed March 20,2011.
- ,,, et al.Dabigatran compared with warfarin in patients with atrial fibrillation and previous transient ischaemic attack or stroke: a subgroup analysis of the RE‐LY trial.Lancet Neurol.2010;9:1157–1163.
- ,,, et al.Dabigatran and warfarin in vitamin K antagonist‐naive and ‐experienced cohorts with atrial fibrillation.Circulation.2010;122:2246–2253.
- ,,, et al.Prevention of venous thromboembolism: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th edition).Chest.2008;133(6 suppl):381S–453S.
- ,,,.American Association of Orthopedic Surgeons and American College of Chest Physicians guidelines for venous thromboembolism prevention in hip and knee arthroplasty differ: what are the implications for clinicians and patients?Chest.2009;135:513–520.
- ,,, et al.The use of antithrombotic therapies in the prevention and treatment of arterial and venous thrombosis: a survey of current knowledge and practice supporting the need for clinical education.Crit Pathw Cardiol.2010;9:41–48.
- .Warfarin versus new agents: interpreting the data.Hematology Am Soc Hematol Educ Program.2010;2010:221–228.
- ,,,,.Why do patients with atrial fibrillation not receive warfarin?Arch Intern Med.2000;160:41–46.
- ,,,,,.Warfarin use among ambulatory patients with nonvalvular atrial fibrillation: The anticoagulation and risk factors in atrial fibrillation (ATRIA) study.Ann Intern Med.1999;131:927–934.
- ,.Drug and dietary interactions of the new and emerging oral anticoagulants.Int J Clin Pract.2010;64:956–967.
- ,,, et al.The risk of bleeding complications in patients with cytochrome P450 CYP2C9*2 or CYP2C9*3 alleles on acenocoumarol or phenprocoumon.Thromb Haemost.2004;92:61–66.
- ,,, et al.Differentiating low‐molecular‐weight heparins based on chemical, biological, and pharmacologic properties: implications for the development of generic versions of low‐molecular‐weight heparins.Semin Thromb Hemost.2008;34:74–85.
- ,.Emerging anticoagulants.Expert Opin Emerg Drugs.2011;16:31–44.
- ,,, et al.Systematic overview of warfarin and its drug and food interactions.Arch Intern Med.2005;165:1095–1106.
- ,,,,,.Evaluation of the pattern of treatment, level of anticoagulation control, and outcome of treatment with warfarin in patients with non‐valvar atrial fibrillation: a record linkage study in a large british population.Heart.2005;91:472–477.
- ,,, et al.Comparison of outcomes among patients randomized to warfarin therapy according to anticoagulant control: results from SPORTIF III and V.Arch Intern Med.2007;167:239–245.
- ,,,.Medication use leading to emergency department visits for adverse drug events in older adults.Ann Intern Med.2007;147:755–765.
- .New oral anticoagulants: a practical guide for clinicians.J Thromb Thrombolysis.2010;29:182–191.
- ,,,.The quest for new anticoagulants: from clinical development to clinical practice [published ahead of print June 14, 2010].Cardiovasc Ther.2010. doi: 10.1111/j.1755–5922.2010.00160.x.
- ,,,,.In‐vitro profile and ex‐vivo anticoagulant activity of the direct thrombin inhibitor dabigatran and its orally active prodrug, dabigatran etexilate.Thromb Haemost.2007;98:155–162.
- ,,.Novel oral factor xa and thrombin inhibitors in the management of thromboembolism.Annu Rev Med.2011;62:41–57.
- ,,,,.Clot‐bound thrombin is protected from inhibition by heparin‐antithrombin III but is susceptible to inactivation by antithrombin III‐independent inhibitors.J Clin Invest.1990;86:385–391.
- ,,.Thrombin binds to soluble fibrin degradation products where it is protected from inhibition by heparin‐antithrombin but susceptible to inactivation by antithrombin‐independent inhibitors.Circulation.1998;97:544–552.
- .Clinical pharmacokinetics and pharmacodynamics of the oral direct thrombin inhibitor dabigatran etexilate.Clin Pharmacokinet.2008;47:285–295.
- ,.Pharmacology, pharmacokinetics, and pharmacodynamics of dabigatran etexilate, an oral direct thrombin inhibitor.Clin Appl Thromb Hemost.2009;15(suppl 1):9S–16S.
- ,,,,.The pharmacokinetics, pharmacodynamics and tolerability of dabigatran etexilate, a new oral direct thrombin inhibitor, in healthy male subjects.Br J Clin Pharmacol.2007;64:292–303.
- ,,,.Pharmacokinetics and pharmacodynamics of the direct oral thrombin inhibitor dabigatran in healthy elderly subjects.Clin Pharmacokinet.2008;47:47–59.
- ,,,,.The metabolism and disposition of the oral direct thrombin inhibitor, dabigatran, in humans.Drug Metab Dispos.2008;36:386–399.
- ,,.Dabigatran etexilate versus warfarin as the oral anticoagulant of choice? A review of clinical data.Pharmacol Ther.2011;129:185–194.
- .The role of P‐glycoprotein and organic anion‐transporting polypeptides in drug interactions.Drug Saf.2005;28:789–801.
- ,,.Novel oral anticoagulants: implications in the perioperative setting.Anesthesiology.2010;113:726–745.
- European Medicines Agency. Pradaxa (dabigatran etexilate) [product information]. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_‐_Product_Information/human/000829/WC 500041059.pdf. Accessed March 25,2011.
- Dabigatran medication guide. Available at: http://bidocs.boehringer‐ingelheim.com/BIWebAccess/ViewServlet.ser?docBase = renetnt9:59–68.
- ,,.Novel oral anticoagulants: the potential relegation of vitamin K antagonists in clinical practice.Int J Clin Pract.2010;64:835–838.
- .The RE‐LY study: Randomized Evaluation of Long‐term anticoagulant therapY: dabigatran vs. warfarin.Eur Heart J.2009;30:2554–2555.
- ,,, et al.Oral dabigatran etexilate vs. subcutaneous enoxaparin for the prevention of venous thromboembolism after total knee replacement: the RE‐MODEL randomized trial.J Thromb Haemost.2007;5:2178–2185.
- ,,, et al.Dabigatran etexilate versus enoxaparin for prevention of venous thromboembolism after total hip replacement: a randomised, double‐blind, non‐inferiority trial.Lancet.2007;370:949–956.
- ,,, et al.Dabigatran versus warfarin in the treatment of acute venous thromboembolism.N Engl J Med.2009;361:2342–2352.
- ,,, et al.Dabigatran versus warfarin in patients with atrial fibrillation.N Engl J Med.2009;361:1139–1151.
- ,,,.Influence of renal impairment on the pharmacokinetics and pharmacodynamics of oral dabigatran etexilate: an open‐label, parallel‐group, single‐centre study.Clin Pharmacokinet.2010;49:259–268.
- ,,,,.Pharmacokinetics and pharmacodynamics of dabigatran etexilate, an oral direct thrombin inhibitor, are not affected by moderate hepatic impairment.J Clin Pharmacol.2008;48:1411–1419.
- ,,, et al.Oral dabigatran versus enoxaparin for thromboprophylaxis after primary total hip arthroplasty (RE‐NOVATE II). A randomised, double‐blind, non‐inferiority trial.Thromb Haemost.2011;105:721–729.
- ,.Insights from the dabigatran versus warfarin trial in patients with venous thromboembolism (the RE‐COVER trial).Expert Opin Pharmacother.2010;11:1035–1037.
- RE‐MOBILIZE Writing Committee,,, et al.Oral thrombin inhibitor dabigatran etexilate vs north american enoxaparin regimen for prevention of venous thromboembolism after knee arthroplasty surgery.J Arthroplasty.2009;24:1–9.
- ,,, et al.Effects of the oral, direct thrombin inhibitor dabigatran on five common coagulation assays.Thromb Haemost.2011;105:371–378.
- ,,, et al.Dabigatran etexilate—a novel, reversible, oral direct thrombin inhibitor: interpretation of coagulation assays and reversal of anticoagulant activity.Thromb Haemost.2010;103:1116–1127.
- ,.A direct thrombin inhibitor studied by dynamic whole blood clot formation. haemostatic response to ex‐vivo addition of recombinant factor VIIa or activated prothrombin complex concentrate.Thromb Haemost.2006;96:446–453.
- US Food and Drug Administration. Dabigatran drug approval history. Available at: http://www.accessdata.fda.gov/drugsatfda_ docs/nda/2010/022512Orig1s000TOC.cfm. Accessed March 20,2011.
- ,,, et al.Dabigatran compared with warfarin in patients with atrial fibrillation and previous transient ischaemic attack or stroke: a subgroup analysis of the RE‐LY trial.Lancet Neurol.2010;9:1157–1163.
- ,,, et al.Dabigatran and warfarin in vitamin K antagonist‐naive and ‐experienced cohorts with atrial fibrillation.Circulation.2010;122:2246–2253.
- ,,, et al.Prevention of venous thromboembolism: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th edition).Chest.2008;133(6 suppl):381S–453S.
- ,,,.American Association of Orthopedic Surgeons and American College of Chest Physicians guidelines for venous thromboembolism prevention in hip and knee arthroplasty differ: what are the implications for clinicians and patients?Chest.2009;135:513–520.