User login
Severe right hip pain
A 63-year-old woman with a 3-year history of osteoporosis presented to our clinic with a 2-week history of severe right hip pain. She had been taking a bisphosphonate—oral ibandronate sodium, 150 mg, once monthly—for about 6 years. The postmenopausal patient had a history of degenerative disc disease and lumbar back pain, but no known history of recent trauma or falls.
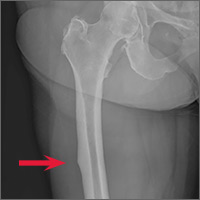
A clinical exam revealed full passive and active range of motion; however, she had pain with weight bearing. A full metabolic panel revealed no significant abnormalities. A leg length discrepancy was noted, so a bone length study was ordered. Anteroposterior x-rays of the bilateral lower extremities demonstrated a focal convexity along the lateral cortical junction of the proximal right femur (FIGURE).

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Bisphosphonate-associated proximal insufficiency fracture
Based on the patient’s clinical history and x-ray findings, we determined that the patient had sustained a bisphosphonate-associated proximal femoral insufficiency fracture. Insufficiency fractures arise from normal physiologic stress on abnormal bone. They commonly occur in conditions that impair normal bone physiology and remodeling, such as osteoporosis, renal insufficiency, rheumatoid arthritis, and diabetes.1
Could a bisphosphonate be to blame? Bisphosphonate therapy has been associated with significant benefits, including increased bone mineral density (BMD), decreased incidence of fracture, and improved mortality.2-4 But it’s been postulated that the global suppression of bone turnover caused by these drugs may also impair the bone remodeling process.5 Some case reports have suggested an association between chronic bisphosphonate use and atypical insufficiency fractures. These atypical femur fractures are characterized by their location (along the diaphysis in the region distal to the lesser trochanter), the patient’s history (there may be minimal to no trauma), and the potential for “beaking” (localized periosteal or endosteal thickening of the lateral cortex).6,7
Several large, population-based, case-control studies have found a temporal relationship between bisphosphonate therapy and a statistically significant increased risk of subtrochanteric fractures.8-10 These studies do note, however, that the absolute risk of insufficiency fracture is very low, and that the benefits of bisphosphonate therapy greatly outweigh the risks. A 2013 meta-analysis came to the same conclusion.11
Treatment options include PT, surgical intervention
When an insufficiency fracture is identified in a patient taking a bisphosphonate, the medication should be discontinued and a consultation with Endocrinology should be arranged. Nonsurgical management ranges from physical therapy to alternative medication regimens, such as teriparatide—a recombinant human parathyroid hormone used to restore bone quality. A variety of surgical stabilization options are also available.6
In contrast to typical subtrochanteric fractures, about half of patients with atypical insufficiency fractures demonstrate poor fracture healing that requires surgical intervention.12 Complete fractures almost always require surgery, while incomplete subtrochanteric femur fractures can usually be managed conservatively by altering pharmacologic prophylaxis (interval dosing or discontinuation of the bisphosphonate and initiation of an alternative therapy like teriparatide) in conjunction with routine radiologic surveillance. Internal fixation may be considered for cases of persistent pain or those that progress to an unstable fracture.13
Our patient declined surgical intervention. We switched her monthly ibandronate dosage to a periodic dosing schedule (6 months on, followed by 6 months off) and advised her to rest and take nonsteroidal anti-inflammatory drugs when needed. While consensus guidelines exist for the management of osteoporosis (see Osteoporosis: Assessing your patient’s risk), there is still debate over the optimal length of bisphosphonate therapy and the impact of drug holidays; a recent review in The BMJ discusses bisphosphonate use in detail.5
SIDEBAR
Osteoporosis: Assessing your patient's riskApproximately 9.9 million Americans have osteoporosis, and while the disease is more common in Caucasian females, patients with osteoporosis have the same elevated fracture risk regardless of their race.14 The US Preventive Services Task Force recommends bone mineral density (BMD) testing for all women ages 65 years and older (earlier if risk factor profile warrants).15
According to the World Health Organization (WHO), patients with BMD T-scores at the hip or lumbar spine that are ≤2.5 standard deviations below the mean BMD of a young-adult reference population are at highest risk for osteoporotic fractures.16 There are also free online risk assessment tools, like the WHO’s FRAX calculator (available at: http://www.shef.ac.uk/FRAX/tool.jsp?locationValue=9), which integrate clinical data to generate an evidence-based assessment of fracture risk.17
Follow-up x-rays 14 months later revealed that the insufficiency fracture had healed with a bony callus.
CORRESPONDENCE
Joseph S. McMonagle, MD, Eastern Virginia Medical School, Department of Radiology, P.O. Box 1980, Norfolk, VA; [email protected].
1. Sheehan SE, Shyu JY, Weaver MJ, et al. Proximal femoral fractures: what the orthopedic surgeon wants to know. Radiographics. 2015;35:1563-1584.
2. Wells G, Cranney A, Peterson J, et al. Risedronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008;(1):CD004523.
3. Wells GA, Cranney A, Peterson J, et al. Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008;(1):CD001155.
4. Wells GA, Cranney A, Peterson J, et al. Etidronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008;(1):CD003376.
5. Maraka S, Kennel KA. Bisphosphonates for the prevention and treatment of osteoporosis. BMJ. 2015;351:h3783.
6. Balach T, Baldwin PC, Intravia J. Atypical femur fractures associated with diphosphonate use. J Am Acad Orthop Surg. 2015;23:550-557.
7. Porrino JA Jr, Kohl CA, Taljanovic M, et al. Diagnosis of proximal femoral insufficiency fractures in patients receiving bisphosphonate therapy. AJR Am J Roentgenol. 2010;194:1061-1064.
8. Edwards BJ, Bunta AD, Lane J, et al. Bisphosphonates and nonhealing femoral fractures: analysis of the FDA Adverse Event Reporting System (FAERS) and international safety efforts: a systematic review from the Research on Adverse Drug Events And Reports (RADAR) project. J Bone Joint Surg Am. 2013;95:297-307.
9. Park-Wyllie LY, Mamdani MM, Juurlink DN, et al. Bisphosphonate use and the risk of subtrochanteric or femoral shaft fractures in older women. JAMA. 2011;305:783-789.
10. Schilcher J, Michaëlsson K, Aspenberg P. Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med. 2011;364:1728-1737.
11. Gedmintas L, Solomon DH, Kim SC. Bisphosphonates and risk of subtrochanteric, femoral shaft, and atypical femur fracture: a systematic review and meta-analysis. J Bone Miner Res. 2013;28:1729-1737.
12. Weil YA, Rivkin G, Safran O, et al. The outcome of surgically treated femur fractures associated with long-term bisphosphonate use. J Trauma. 2011;71:186-190.
13. Khan AA, Leslie WD, Lentle B, et al. Atypical femoral fractures: a teaching perspective. Can Assoc Radiol J. 2015;66:102-107.
14. Cosman F, de Beur SJ, LeBoff MS, et al; National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int. 2014;25:2359-2381.
15. US Preventive Services Task Force. Screening for osteoporosis: U.S. preventive services task force recommendation statement. Ann Intern Med. 2011;154:356-364.
16. World Health Organization (WHO). 1994. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: report of a WHO study group. WHO Technical Report Series, Report No. 843. WHO, Geneva, Switzerland.
17. Kanis JA, McCloskey EV, Johansson H, et al. Development and use of FRAX in osteoporosis. Osteoporos Int. 2010;21:S407-S413.
A 63-year-old woman with a 3-year history of osteoporosis presented to our clinic with a 2-week history of severe right hip pain. She had been taking a bisphosphonate—oral ibandronate sodium, 150 mg, once monthly—for about 6 years. The postmenopausal patient had a history of degenerative disc disease and lumbar back pain, but no known history of recent trauma or falls.
A clinical exam revealed full passive and active range of motion; however, she had pain with weight bearing. A full metabolic panel revealed no significant abnormalities. A leg length discrepancy was noted, so a bone length study was ordered. Anteroposterior x-rays of the bilateral lower extremities demonstrated a focal convexity along the lateral cortical junction of the proximal right femur (FIGURE).

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Bisphosphonate-associated proximal insufficiency fracture
Based on the patient’s clinical history and x-ray findings, we determined that the patient had sustained a bisphosphonate-associated proximal femoral insufficiency fracture. Insufficiency fractures arise from normal physiologic stress on abnormal bone. They commonly occur in conditions that impair normal bone physiology and remodeling, such as osteoporosis, renal insufficiency, rheumatoid arthritis, and diabetes.1
Could a bisphosphonate be to blame? Bisphosphonate therapy has been associated with significant benefits, including increased bone mineral density (BMD), decreased incidence of fracture, and improved mortality.2-4 But it’s been postulated that the global suppression of bone turnover caused by these drugs may also impair the bone remodeling process.5 Some case reports have suggested an association between chronic bisphosphonate use and atypical insufficiency fractures. These atypical femur fractures are characterized by their location (along the diaphysis in the region distal to the lesser trochanter), the patient’s history (there may be minimal to no trauma), and the potential for “beaking” (localized periosteal or endosteal thickening of the lateral cortex).6,7
Several large, population-based, case-control studies have found a temporal relationship between bisphosphonate therapy and a statistically significant increased risk of subtrochanteric fractures.8-10 These studies do note, however, that the absolute risk of insufficiency fracture is very low, and that the benefits of bisphosphonate therapy greatly outweigh the risks. A 2013 meta-analysis came to the same conclusion.11
Treatment options include PT, surgical intervention
When an insufficiency fracture is identified in a patient taking a bisphosphonate, the medication should be discontinued and a consultation with Endocrinology should be arranged. Nonsurgical management ranges from physical therapy to alternative medication regimens, such as teriparatide—a recombinant human parathyroid hormone used to restore bone quality. A variety of surgical stabilization options are also available.6
In contrast to typical subtrochanteric fractures, about half of patients with atypical insufficiency fractures demonstrate poor fracture healing that requires surgical intervention.12 Complete fractures almost always require surgery, while incomplete subtrochanteric femur fractures can usually be managed conservatively by altering pharmacologic prophylaxis (interval dosing or discontinuation of the bisphosphonate and initiation of an alternative therapy like teriparatide) in conjunction with routine radiologic surveillance. Internal fixation may be considered for cases of persistent pain or those that progress to an unstable fracture.13
Our patient declined surgical intervention. We switched her monthly ibandronate dosage to a periodic dosing schedule (6 months on, followed by 6 months off) and advised her to rest and take nonsteroidal anti-inflammatory drugs when needed. While consensus guidelines exist for the management of osteoporosis (see Osteoporosis: Assessing your patient’s risk), there is still debate over the optimal length of bisphosphonate therapy and the impact of drug holidays; a recent review in The BMJ discusses bisphosphonate use in detail.5
SIDEBAR
Osteoporosis: Assessing your patient's riskApproximately 9.9 million Americans have osteoporosis, and while the disease is more common in Caucasian females, patients with osteoporosis have the same elevated fracture risk regardless of their race.14 The US Preventive Services Task Force recommends bone mineral density (BMD) testing for all women ages 65 years and older (earlier if risk factor profile warrants).15
According to the World Health Organization (WHO), patients with BMD T-scores at the hip or lumbar spine that are ≤2.5 standard deviations below the mean BMD of a young-adult reference population are at highest risk for osteoporotic fractures.16 There are also free online risk assessment tools, like the WHO’s FRAX calculator (available at: http://www.shef.ac.uk/FRAX/tool.jsp?locationValue=9), which integrate clinical data to generate an evidence-based assessment of fracture risk.17
Follow-up x-rays 14 months later revealed that the insufficiency fracture had healed with a bony callus.
CORRESPONDENCE
Joseph S. McMonagle, MD, Eastern Virginia Medical School, Department of Radiology, P.O. Box 1980, Norfolk, VA; [email protected].
A 63-year-old woman with a 3-year history of osteoporosis presented to our clinic with a 2-week history of severe right hip pain. She had been taking a bisphosphonate—oral ibandronate sodium, 150 mg, once monthly—for about 6 years. The postmenopausal patient had a history of degenerative disc disease and lumbar back pain, but no known history of recent trauma or falls.
A clinical exam revealed full passive and active range of motion; however, she had pain with weight bearing. A full metabolic panel revealed no significant abnormalities. A leg length discrepancy was noted, so a bone length study was ordered. Anteroposterior x-rays of the bilateral lower extremities demonstrated a focal convexity along the lateral cortical junction of the proximal right femur (FIGURE).

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Bisphosphonate-associated proximal insufficiency fracture
Based on the patient’s clinical history and x-ray findings, we determined that the patient had sustained a bisphosphonate-associated proximal femoral insufficiency fracture. Insufficiency fractures arise from normal physiologic stress on abnormal bone. They commonly occur in conditions that impair normal bone physiology and remodeling, such as osteoporosis, renal insufficiency, rheumatoid arthritis, and diabetes.1
Could a bisphosphonate be to blame? Bisphosphonate therapy has been associated with significant benefits, including increased bone mineral density (BMD), decreased incidence of fracture, and improved mortality.2-4 But it’s been postulated that the global suppression of bone turnover caused by these drugs may also impair the bone remodeling process.5 Some case reports have suggested an association between chronic bisphosphonate use and atypical insufficiency fractures. These atypical femur fractures are characterized by their location (along the diaphysis in the region distal to the lesser trochanter), the patient’s history (there may be minimal to no trauma), and the potential for “beaking” (localized periosteal or endosteal thickening of the lateral cortex).6,7
Several large, population-based, case-control studies have found a temporal relationship between bisphosphonate therapy and a statistically significant increased risk of subtrochanteric fractures.8-10 These studies do note, however, that the absolute risk of insufficiency fracture is very low, and that the benefits of bisphosphonate therapy greatly outweigh the risks. A 2013 meta-analysis came to the same conclusion.11
Treatment options include PT, surgical intervention
When an insufficiency fracture is identified in a patient taking a bisphosphonate, the medication should be discontinued and a consultation with Endocrinology should be arranged. Nonsurgical management ranges from physical therapy to alternative medication regimens, such as teriparatide—a recombinant human parathyroid hormone used to restore bone quality. A variety of surgical stabilization options are also available.6
In contrast to typical subtrochanteric fractures, about half of patients with atypical insufficiency fractures demonstrate poor fracture healing that requires surgical intervention.12 Complete fractures almost always require surgery, while incomplete subtrochanteric femur fractures can usually be managed conservatively by altering pharmacologic prophylaxis (interval dosing or discontinuation of the bisphosphonate and initiation of an alternative therapy like teriparatide) in conjunction with routine radiologic surveillance. Internal fixation may be considered for cases of persistent pain or those that progress to an unstable fracture.13
Our patient declined surgical intervention. We switched her monthly ibandronate dosage to a periodic dosing schedule (6 months on, followed by 6 months off) and advised her to rest and take nonsteroidal anti-inflammatory drugs when needed. While consensus guidelines exist for the management of osteoporosis (see Osteoporosis: Assessing your patient’s risk), there is still debate over the optimal length of bisphosphonate therapy and the impact of drug holidays; a recent review in The BMJ discusses bisphosphonate use in detail.5
SIDEBAR
Osteoporosis: Assessing your patient's riskApproximately 9.9 million Americans have osteoporosis, and while the disease is more common in Caucasian females, patients with osteoporosis have the same elevated fracture risk regardless of their race.14 The US Preventive Services Task Force recommends bone mineral density (BMD) testing for all women ages 65 years and older (earlier if risk factor profile warrants).15
According to the World Health Organization (WHO), patients with BMD T-scores at the hip or lumbar spine that are ≤2.5 standard deviations below the mean BMD of a young-adult reference population are at highest risk for osteoporotic fractures.16 There are also free online risk assessment tools, like the WHO’s FRAX calculator (available at: http://www.shef.ac.uk/FRAX/tool.jsp?locationValue=9), which integrate clinical data to generate an evidence-based assessment of fracture risk.17
Follow-up x-rays 14 months later revealed that the insufficiency fracture had healed with a bony callus.
CORRESPONDENCE
Joseph S. McMonagle, MD, Eastern Virginia Medical School, Department of Radiology, P.O. Box 1980, Norfolk, VA; [email protected].
1. Sheehan SE, Shyu JY, Weaver MJ, et al. Proximal femoral fractures: what the orthopedic surgeon wants to know. Radiographics. 2015;35:1563-1584.
2. Wells G, Cranney A, Peterson J, et al. Risedronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008;(1):CD004523.
3. Wells GA, Cranney A, Peterson J, et al. Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008;(1):CD001155.
4. Wells GA, Cranney A, Peterson J, et al. Etidronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008;(1):CD003376.
5. Maraka S, Kennel KA. Bisphosphonates for the prevention and treatment of osteoporosis. BMJ. 2015;351:h3783.
6. Balach T, Baldwin PC, Intravia J. Atypical femur fractures associated with diphosphonate use. J Am Acad Orthop Surg. 2015;23:550-557.
7. Porrino JA Jr, Kohl CA, Taljanovic M, et al. Diagnosis of proximal femoral insufficiency fractures in patients receiving bisphosphonate therapy. AJR Am J Roentgenol. 2010;194:1061-1064.
8. Edwards BJ, Bunta AD, Lane J, et al. Bisphosphonates and nonhealing femoral fractures: analysis of the FDA Adverse Event Reporting System (FAERS) and international safety efforts: a systematic review from the Research on Adverse Drug Events And Reports (RADAR) project. J Bone Joint Surg Am. 2013;95:297-307.
9. Park-Wyllie LY, Mamdani MM, Juurlink DN, et al. Bisphosphonate use and the risk of subtrochanteric or femoral shaft fractures in older women. JAMA. 2011;305:783-789.
10. Schilcher J, Michaëlsson K, Aspenberg P. Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med. 2011;364:1728-1737.
11. Gedmintas L, Solomon DH, Kim SC. Bisphosphonates and risk of subtrochanteric, femoral shaft, and atypical femur fracture: a systematic review and meta-analysis. J Bone Miner Res. 2013;28:1729-1737.
12. Weil YA, Rivkin G, Safran O, et al. The outcome of surgically treated femur fractures associated with long-term bisphosphonate use. J Trauma. 2011;71:186-190.
13. Khan AA, Leslie WD, Lentle B, et al. Atypical femoral fractures: a teaching perspective. Can Assoc Radiol J. 2015;66:102-107.
14. Cosman F, de Beur SJ, LeBoff MS, et al; National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int. 2014;25:2359-2381.
15. US Preventive Services Task Force. Screening for osteoporosis: U.S. preventive services task force recommendation statement. Ann Intern Med. 2011;154:356-364.
16. World Health Organization (WHO). 1994. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: report of a WHO study group. WHO Technical Report Series, Report No. 843. WHO, Geneva, Switzerland.
17. Kanis JA, McCloskey EV, Johansson H, et al. Development and use of FRAX in osteoporosis. Osteoporos Int. 2010;21:S407-S413.
1. Sheehan SE, Shyu JY, Weaver MJ, et al. Proximal femoral fractures: what the orthopedic surgeon wants to know. Radiographics. 2015;35:1563-1584.
2. Wells G, Cranney A, Peterson J, et al. Risedronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008;(1):CD004523.
3. Wells GA, Cranney A, Peterson J, et al. Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008;(1):CD001155.
4. Wells GA, Cranney A, Peterson J, et al. Etidronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008;(1):CD003376.
5. Maraka S, Kennel KA. Bisphosphonates for the prevention and treatment of osteoporosis. BMJ. 2015;351:h3783.
6. Balach T, Baldwin PC, Intravia J. Atypical femur fractures associated with diphosphonate use. J Am Acad Orthop Surg. 2015;23:550-557.
7. Porrino JA Jr, Kohl CA, Taljanovic M, et al. Diagnosis of proximal femoral insufficiency fractures in patients receiving bisphosphonate therapy. AJR Am J Roentgenol. 2010;194:1061-1064.
8. Edwards BJ, Bunta AD, Lane J, et al. Bisphosphonates and nonhealing femoral fractures: analysis of the FDA Adverse Event Reporting System (FAERS) and international safety efforts: a systematic review from the Research on Adverse Drug Events And Reports (RADAR) project. J Bone Joint Surg Am. 2013;95:297-307.
9. Park-Wyllie LY, Mamdani MM, Juurlink DN, et al. Bisphosphonate use and the risk of subtrochanteric or femoral shaft fractures in older women. JAMA. 2011;305:783-789.
10. Schilcher J, Michaëlsson K, Aspenberg P. Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med. 2011;364:1728-1737.
11. Gedmintas L, Solomon DH, Kim SC. Bisphosphonates and risk of subtrochanteric, femoral shaft, and atypical femur fracture: a systematic review and meta-analysis. J Bone Miner Res. 2013;28:1729-1737.
12. Weil YA, Rivkin G, Safran O, et al. The outcome of surgically treated femur fractures associated with long-term bisphosphonate use. J Trauma. 2011;71:186-190.
13. Khan AA, Leslie WD, Lentle B, et al. Atypical femoral fractures: a teaching perspective. Can Assoc Radiol J. 2015;66:102-107.
14. Cosman F, de Beur SJ, LeBoff MS, et al; National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int. 2014;25:2359-2381.
15. US Preventive Services Task Force. Screening for osteoporosis: U.S. preventive services task force recommendation statement. Ann Intern Med. 2011;154:356-364.
16. World Health Organization (WHO). 1994. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: report of a WHO study group. WHO Technical Report Series, Report No. 843. WHO, Geneva, Switzerland.
17. Kanis JA, McCloskey EV, Johansson H, et al. Development and use of FRAX in osteoporosis. Osteoporos Int. 2010;21:S407-S413.