User login
Elevated serum alkaline phosphatase • generalized pruritus • Dx?
THE CASE
A 34-year-old woman was referred to the hepatology clinic for evaluation of an increased serum alkaline phosphatase (ALP) level. She was gravida 5 and in her 38th week of gestation. Her obstetric history was significant for 2 uncomplicated spontaneous term vaginal deliveries resulting in live births and 2 spontaneous abortions. The patient reported generalized pruritus for 2 months prior to the visit. She had no comorbidities and denied any other symptoms. She reported no family history of liver disease or complications during pregnancy in relatives. The patient did not smoke or drink, and had come to our hospital for her prenatal care visits.
The physical exam revealed normal vital signs, no jaundice, a gravid uterus, and acanthosis nigricans on the neck and axilla with scattered excoriations on the arms, legs, and abdomen. Her serum ALP level was 1093 U/L (normal: 50-136 U/L). Immediately before this pregnancy, her serum ALP had been normal at 95 U/L, but it had since been increasing with a peak value of 1134 U/L by 37 weeks’ gestation. Serum transaminase activities and albumin and bilirubin concentrations were normal, as was her prothrombin time. The rest of her lab tests were also normal, including her fasting serum bile acid concentration, which was 9 mcmol/L (normal: 4.5-19.2 mcmol/L).
THE DIAGNOSIS
Although cholestasis of pregnancy was considered, the patient’s markedly elevated serum ALP level suggested the presence of another cholestatic liver disease. Additional tests revealed an antimitochondrial antibody (AMA) titer of 1:320 (normal: <1:20) and immunoglobulin A, G, and M levels within normal limits. Accordingly, we diagnosed primary biliary cholangitis (PBC).
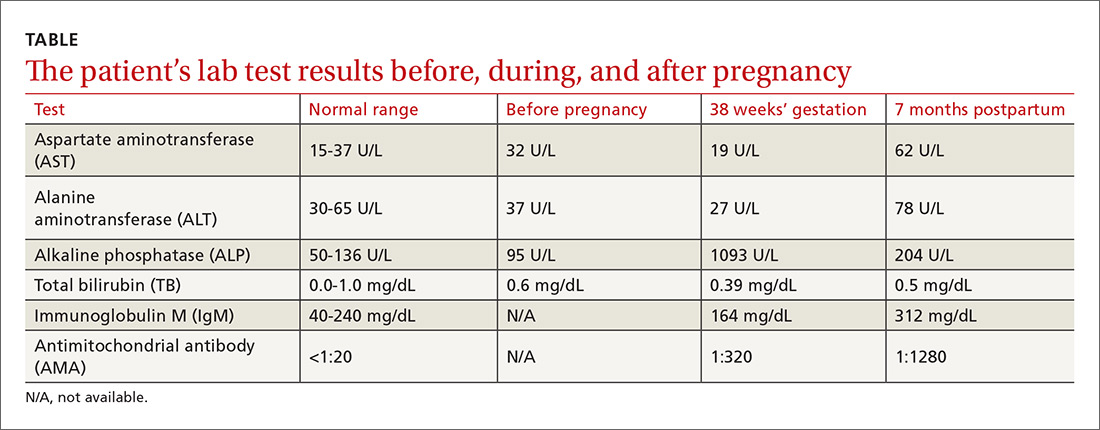
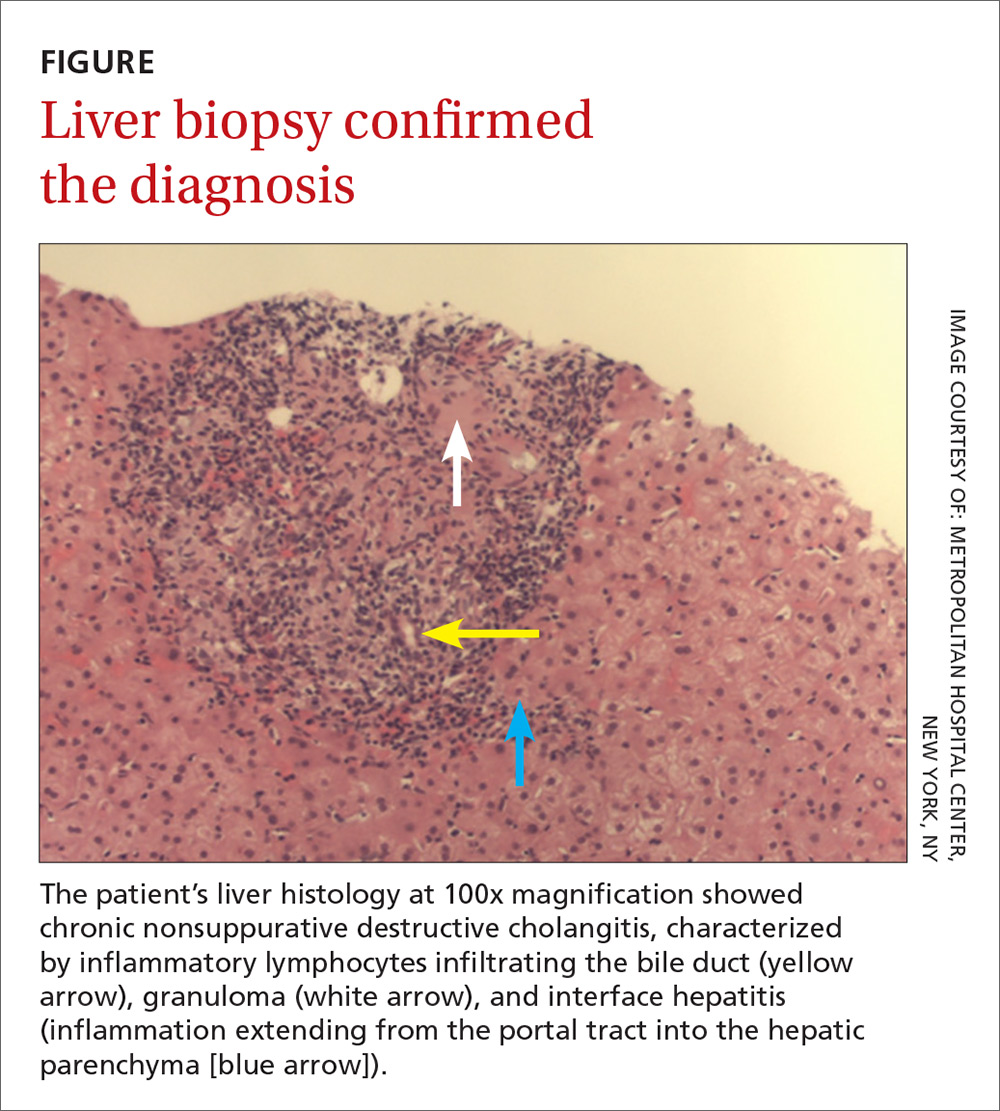
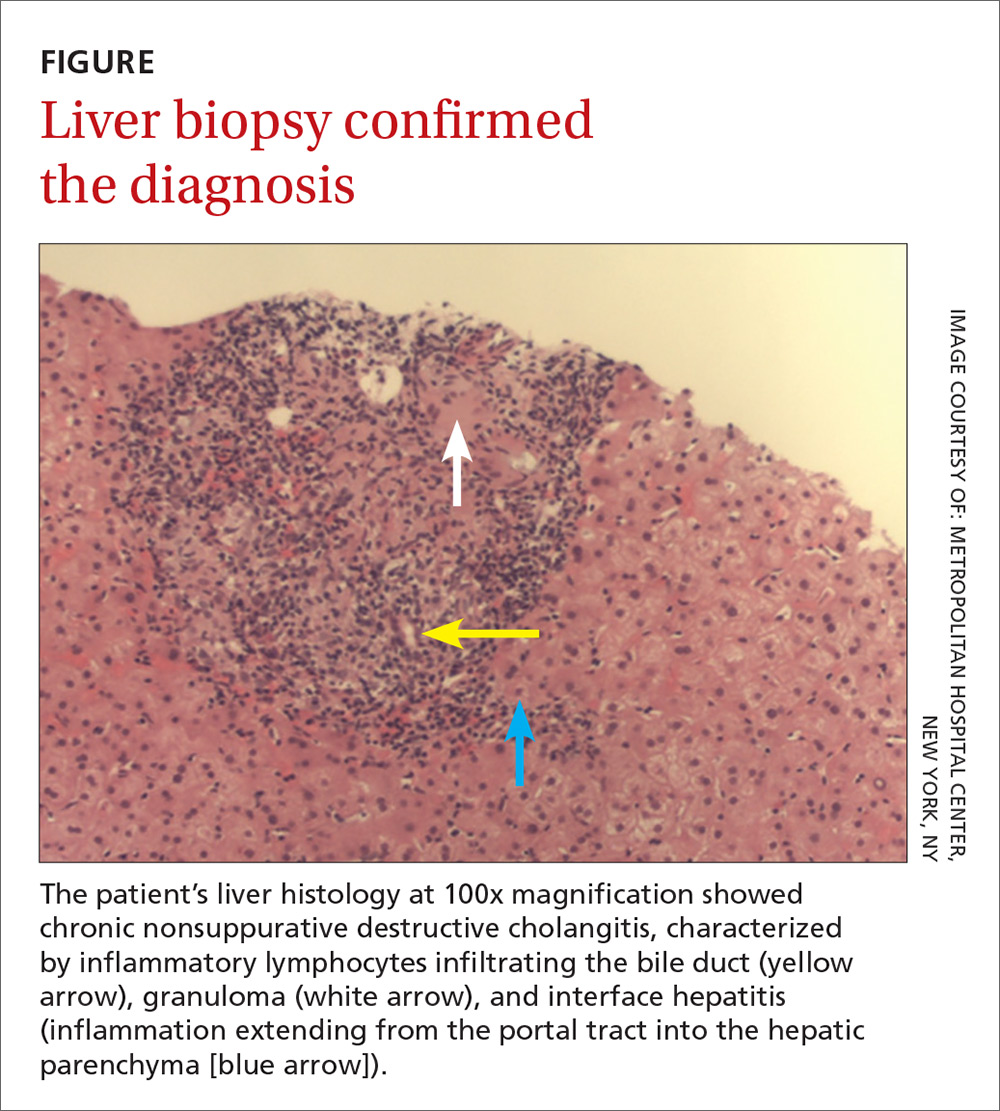
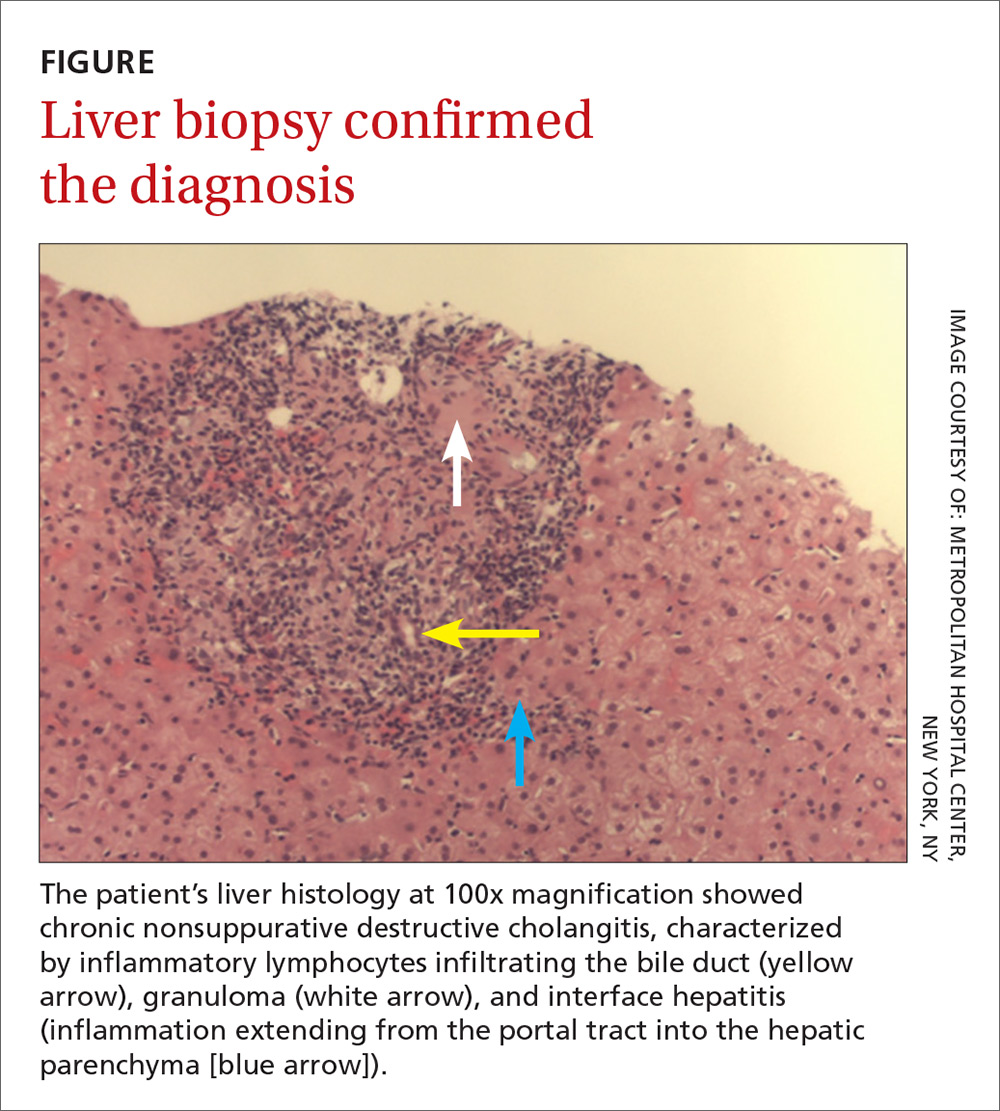
The patient delivered vaginally at another institution uneventfully and returned to the hepatology clinic 7 months postpartum. Repeat laboratory tests (TABLE) revealed increased AMA titer and immunoglobulin M levels from baseline (38 weeks’ gestation). The physical exam was notable for the absence of both jaundice and stigmata of chronic liver disease. A liver ultrasound was normal. The patient still reported pruritus, as well as a new symptom—fatigue. A liver biopsy was performed, and findings were consistent with PBC, stage 1 (FIGURE).
DISCUSSION
PBC, historically known as primary biliary cirrhosis, is a chronic, likely immune-mediated, cholestatic liver disease characterized by the progressive inflammatory destruction of intrahepatic bile ducts. The disease has a female to male predominance of 10:1, with age of diagnosis most often between 40 and 50 years, although about a quarter of female patients present during their reproductive years.1,2
PBC in pregnant women
During pregnancy, the profound physiologic changes and adaptations in the endocrine, metabolic, and immune systems that are necessary for normal fetal development can affect the maternal hepatobiliary system. In patients with prior autoimmune liver disease, the liver is known to adapt itself to these physiologic changes by entering a state of immune tolerance. This is induced by relative hypercortisolism, a shift from predominantly cell-mediated immunity to humoral immunity, and inhibition of T-cell activation. These changes can result in remission of autoimmune disease activity during pregnancy and postpartum flaring when these protective mechanisms are lost (although neither remission nor postpartum flaring occurred in this patient’s case).1-3
While a well-compensated state is associated with better fetal and maternal outcomes than a decompensated condition, cirrhosis is not a contraindication to pregnancy. Vaginal delivery is generally safe for patients with PBC, and studies have reported no childbirth complications or adverse maternal outcomes.1,3,4
The approved treatment for PBC, ursodeoxycholic acid (UDCA), was classified as a category B agent according to the Food and Drug Administration’s now defunct classification system for drugs used during pregnancy and lactation. It’s considered to be the treatment of choice for intrahepatic cholestasis of pregnancy, but there are no recommendations for its use in pregnant patients with PBC. Several studies have observed no significant teratogenic effect in babies whose mothers were treated with UDCA for PBC during pregnancy.1-4 Postpartum, 60% to 70% of PBC patients have been reported to exhibit biochemical disease activity,1,3 and in one case, a liver transplant was required due to liver failure.5
Look for AMA, elevated ALP
The diagnosis of the disease in this case was made by the detection of AMA, which has a specificity of 98% for PBC. However, isolated instances of the presence of AMA are not uncommon; they have been documented in up to 64% of healthy individuals.6 In addition, while one would expect to see a 2- to 4-fold rise in ALP levels during pregnancy (due to placental isoenzyme production),2,7 our patient’s serum ALP level was much higher, suggesting probable cholestatic liver disease such as PBC. The diagnosis in this case was confirmed by liver biopsy.
Our patient was started on UDCA 13 to 15 mg/kg/d. She remained clinically stable at subsequent follow-ups.
THE TAKEAWAY
Typically seen in middle-aged women, PBC can be detected by the presence of AMA and elevated ALP levels. Pregnant patients with chronic liver disease, including PBC, should be followed by a hepatologist and a high-risk obstetrician. They should be carefully monitored and frequently reassessed throughout the pregnancy, delivery, and postpartum period, even though studies have documented favorable outcomes for both mother and baby.1,3,4
1. Trivedi PJ, Kumagi T, Al-Harthy N, et al. Good maternal and fetal outcomes for pregnant women with primary biliary cirrhosis. Clin Gastroenterol Hepatol. 2014;12:1179-1185.
2. Marchioni Beery RM, Vaziri H, Forouhar F. Primary biliary cirrhosis and primary sclerosing cholangitis: a review featuring a women’s health perspective. J Clin Transl Hepatol. 2014;2:266-284.
3. Efe C, Kahramanoğlu-Aksoy E, Yilmaz B, et al. Pregnancy in women with primary biliary cirrhosis. Autoimmun Rev. 2014;13:931-935.
4. Floreani A, Infantolino C, Franceschet I, et al. Pregnancy and primary biliary cirrhosis: a case control study. Clin Rev Allergy Immunol. 2015;48:236-242.
5. Rabinovitz M, Appasamy R, Finkelstein S. Primary biliary cirrhosis diagnosed during pregnancy. Does it have a different outcome? Dig Dis Sci. 1995;40:571-574.
6. Carey EJ, Ali AH, Lindor KD. Primary biliary cirrhosis. Lancet. 2015;386:1565-1575.
7. The Johns Hopkins School of Medicine Department of Gynecology. Hurt KJ, Guile MW, Bienstock JL, et al, eds. The Johns Hopkins Manual of Gynecology and Obstetrics. 4th edition. Philadelphia, PA: Lippincott Williams and Wilkins; 2011.
THE CASE
A 34-year-old woman was referred to the hepatology clinic for evaluation of an increased serum alkaline phosphatase (ALP) level. She was gravida 5 and in her 38th week of gestation. Her obstetric history was significant for 2 uncomplicated spontaneous term vaginal deliveries resulting in live births and 2 spontaneous abortions. The patient reported generalized pruritus for 2 months prior to the visit. She had no comorbidities and denied any other symptoms. She reported no family history of liver disease or complications during pregnancy in relatives. The patient did not smoke or drink, and had come to our hospital for her prenatal care visits.
The physical exam revealed normal vital signs, no jaundice, a gravid uterus, and acanthosis nigricans on the neck and axilla with scattered excoriations on the arms, legs, and abdomen. Her serum ALP level was 1093 U/L (normal: 50-136 U/L). Immediately before this pregnancy, her serum ALP had been normal at 95 U/L, but it had since been increasing with a peak value of 1134 U/L by 37 weeks’ gestation. Serum transaminase activities and albumin and bilirubin concentrations were normal, as was her prothrombin time. The rest of her lab tests were also normal, including her fasting serum bile acid concentration, which was 9 mcmol/L (normal: 4.5-19.2 mcmol/L).
THE DIAGNOSIS
Although cholestasis of pregnancy was considered, the patient’s markedly elevated serum ALP level suggested the presence of another cholestatic liver disease. Additional tests revealed an antimitochondrial antibody (AMA) titer of 1:320 (normal: <1:20) and immunoglobulin A, G, and M levels within normal limits. Accordingly, we diagnosed primary biliary cholangitis (PBC).
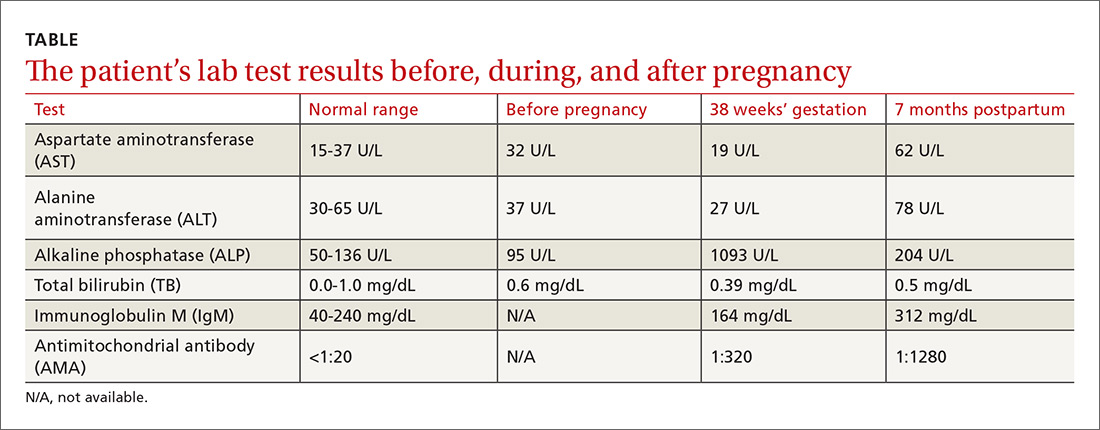
The patient delivered vaginally at another institution uneventfully and returned to the hepatology clinic 7 months postpartum. Repeat laboratory tests (TABLE) revealed increased AMA titer and immunoglobulin M levels from baseline (38 weeks’ gestation). The physical exam was notable for the absence of both jaundice and stigmata of chronic liver disease. A liver ultrasound was normal. The patient still reported pruritus, as well as a new symptom—fatigue. A liver biopsy was performed, and findings were consistent with PBC, stage 1 (FIGURE).
DISCUSSION
PBC, historically known as primary biliary cirrhosis, is a chronic, likely immune-mediated, cholestatic liver disease characterized by the progressive inflammatory destruction of intrahepatic bile ducts. The disease has a female to male predominance of 10:1, with age of diagnosis most often between 40 and 50 years, although about a quarter of female patients present during their reproductive years.1,2
PBC in pregnant women
During pregnancy, the profound physiologic changes and adaptations in the endocrine, metabolic, and immune systems that are necessary for normal fetal development can affect the maternal hepatobiliary system. In patients with prior autoimmune liver disease, the liver is known to adapt itself to these physiologic changes by entering a state of immune tolerance. This is induced by relative hypercortisolism, a shift from predominantly cell-mediated immunity to humoral immunity, and inhibition of T-cell activation. These changes can result in remission of autoimmune disease activity during pregnancy and postpartum flaring when these protective mechanisms are lost (although neither remission nor postpartum flaring occurred in this patient’s case).1-3
While a well-compensated state is associated with better fetal and maternal outcomes than a decompensated condition, cirrhosis is not a contraindication to pregnancy. Vaginal delivery is generally safe for patients with PBC, and studies have reported no childbirth complications or adverse maternal outcomes.1,3,4
The approved treatment for PBC, ursodeoxycholic acid (UDCA), was classified as a category B agent according to the Food and Drug Administration’s now defunct classification system for drugs used during pregnancy and lactation. It’s considered to be the treatment of choice for intrahepatic cholestasis of pregnancy, but there are no recommendations for its use in pregnant patients with PBC. Several studies have observed no significant teratogenic effect in babies whose mothers were treated with UDCA for PBC during pregnancy.1-4 Postpartum, 60% to 70% of PBC patients have been reported to exhibit biochemical disease activity,1,3 and in one case, a liver transplant was required due to liver failure.5
Look for AMA, elevated ALP
The diagnosis of the disease in this case was made by the detection of AMA, which has a specificity of 98% for PBC. However, isolated instances of the presence of AMA are not uncommon; they have been documented in up to 64% of healthy individuals.6 In addition, while one would expect to see a 2- to 4-fold rise in ALP levels during pregnancy (due to placental isoenzyme production),2,7 our patient’s serum ALP level was much higher, suggesting probable cholestatic liver disease such as PBC. The diagnosis in this case was confirmed by liver biopsy.
Our patient was started on UDCA 13 to 15 mg/kg/d. She remained clinically stable at subsequent follow-ups.
THE TAKEAWAY
Typically seen in middle-aged women, PBC can be detected by the presence of AMA and elevated ALP levels. Pregnant patients with chronic liver disease, including PBC, should be followed by a hepatologist and a high-risk obstetrician. They should be carefully monitored and frequently reassessed throughout the pregnancy, delivery, and postpartum period, even though studies have documented favorable outcomes for both mother and baby.1,3,4
THE CASE
A 34-year-old woman was referred to the hepatology clinic for evaluation of an increased serum alkaline phosphatase (ALP) level. She was gravida 5 and in her 38th week of gestation. Her obstetric history was significant for 2 uncomplicated spontaneous term vaginal deliveries resulting in live births and 2 spontaneous abortions. The patient reported generalized pruritus for 2 months prior to the visit. She had no comorbidities and denied any other symptoms. She reported no family history of liver disease or complications during pregnancy in relatives. The patient did not smoke or drink, and had come to our hospital for her prenatal care visits.
The physical exam revealed normal vital signs, no jaundice, a gravid uterus, and acanthosis nigricans on the neck and axilla with scattered excoriations on the arms, legs, and abdomen. Her serum ALP level was 1093 U/L (normal: 50-136 U/L). Immediately before this pregnancy, her serum ALP had been normal at 95 U/L, but it had since been increasing with a peak value of 1134 U/L by 37 weeks’ gestation. Serum transaminase activities and albumin and bilirubin concentrations were normal, as was her prothrombin time. The rest of her lab tests were also normal, including her fasting serum bile acid concentration, which was 9 mcmol/L (normal: 4.5-19.2 mcmol/L).
THE DIAGNOSIS
Although cholestasis of pregnancy was considered, the patient’s markedly elevated serum ALP level suggested the presence of another cholestatic liver disease. Additional tests revealed an antimitochondrial antibody (AMA) titer of 1:320 (normal: <1:20) and immunoglobulin A, G, and M levels within normal limits. Accordingly, we diagnosed primary biliary cholangitis (PBC).
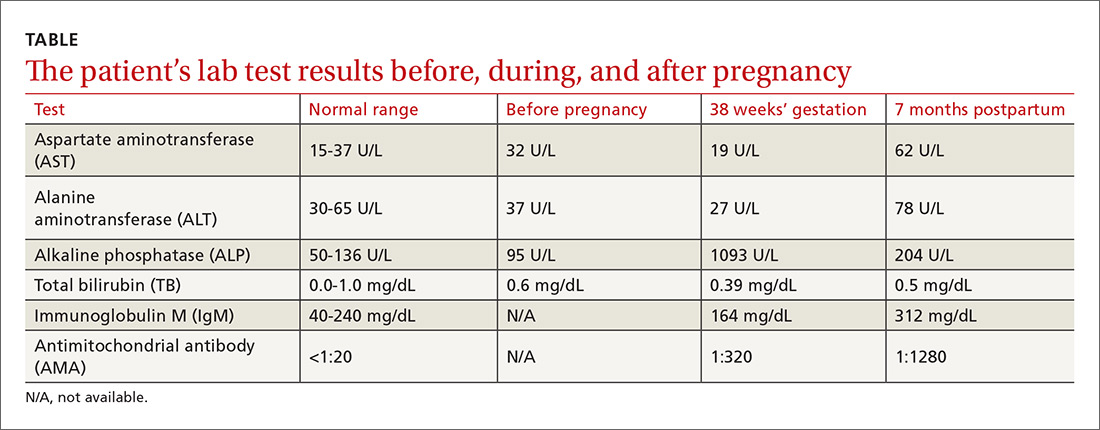
The patient delivered vaginally at another institution uneventfully and returned to the hepatology clinic 7 months postpartum. Repeat laboratory tests (TABLE) revealed increased AMA titer and immunoglobulin M levels from baseline (38 weeks’ gestation). The physical exam was notable for the absence of both jaundice and stigmata of chronic liver disease. A liver ultrasound was normal. The patient still reported pruritus, as well as a new symptom—fatigue. A liver biopsy was performed, and findings were consistent with PBC, stage 1 (FIGURE).
DISCUSSION
PBC, historically known as primary biliary cirrhosis, is a chronic, likely immune-mediated, cholestatic liver disease characterized by the progressive inflammatory destruction of intrahepatic bile ducts. The disease has a female to male predominance of 10:1, with age of diagnosis most often between 40 and 50 years, although about a quarter of female patients present during their reproductive years.1,2
PBC in pregnant women
During pregnancy, the profound physiologic changes and adaptations in the endocrine, metabolic, and immune systems that are necessary for normal fetal development can affect the maternal hepatobiliary system. In patients with prior autoimmune liver disease, the liver is known to adapt itself to these physiologic changes by entering a state of immune tolerance. This is induced by relative hypercortisolism, a shift from predominantly cell-mediated immunity to humoral immunity, and inhibition of T-cell activation. These changes can result in remission of autoimmune disease activity during pregnancy and postpartum flaring when these protective mechanisms are lost (although neither remission nor postpartum flaring occurred in this patient’s case).1-3
While a well-compensated state is associated with better fetal and maternal outcomes than a decompensated condition, cirrhosis is not a contraindication to pregnancy. Vaginal delivery is generally safe for patients with PBC, and studies have reported no childbirth complications or adverse maternal outcomes.1,3,4
The approved treatment for PBC, ursodeoxycholic acid (UDCA), was classified as a category B agent according to the Food and Drug Administration’s now defunct classification system for drugs used during pregnancy and lactation. It’s considered to be the treatment of choice for intrahepatic cholestasis of pregnancy, but there are no recommendations for its use in pregnant patients with PBC. Several studies have observed no significant teratogenic effect in babies whose mothers were treated with UDCA for PBC during pregnancy.1-4 Postpartum, 60% to 70% of PBC patients have been reported to exhibit biochemical disease activity,1,3 and in one case, a liver transplant was required due to liver failure.5
Look for AMA, elevated ALP
The diagnosis of the disease in this case was made by the detection of AMA, which has a specificity of 98% for PBC. However, isolated instances of the presence of AMA are not uncommon; they have been documented in up to 64% of healthy individuals.6 In addition, while one would expect to see a 2- to 4-fold rise in ALP levels during pregnancy (due to placental isoenzyme production),2,7 our patient’s serum ALP level was much higher, suggesting probable cholestatic liver disease such as PBC. The diagnosis in this case was confirmed by liver biopsy.
Our patient was started on UDCA 13 to 15 mg/kg/d. She remained clinically stable at subsequent follow-ups.
THE TAKEAWAY
Typically seen in middle-aged women, PBC can be detected by the presence of AMA and elevated ALP levels. Pregnant patients with chronic liver disease, including PBC, should be followed by a hepatologist and a high-risk obstetrician. They should be carefully monitored and frequently reassessed throughout the pregnancy, delivery, and postpartum period, even though studies have documented favorable outcomes for both mother and baby.1,3,4
1. Trivedi PJ, Kumagi T, Al-Harthy N, et al. Good maternal and fetal outcomes for pregnant women with primary biliary cirrhosis. Clin Gastroenterol Hepatol. 2014;12:1179-1185.
2. Marchioni Beery RM, Vaziri H, Forouhar F. Primary biliary cirrhosis and primary sclerosing cholangitis: a review featuring a women’s health perspective. J Clin Transl Hepatol. 2014;2:266-284.
3. Efe C, Kahramanoğlu-Aksoy E, Yilmaz B, et al. Pregnancy in women with primary biliary cirrhosis. Autoimmun Rev. 2014;13:931-935.
4. Floreani A, Infantolino C, Franceschet I, et al. Pregnancy and primary biliary cirrhosis: a case control study. Clin Rev Allergy Immunol. 2015;48:236-242.
5. Rabinovitz M, Appasamy R, Finkelstein S. Primary biliary cirrhosis diagnosed during pregnancy. Does it have a different outcome? Dig Dis Sci. 1995;40:571-574.
6. Carey EJ, Ali AH, Lindor KD. Primary biliary cirrhosis. Lancet. 2015;386:1565-1575.
7. The Johns Hopkins School of Medicine Department of Gynecology. Hurt KJ, Guile MW, Bienstock JL, et al, eds. The Johns Hopkins Manual of Gynecology and Obstetrics. 4th edition. Philadelphia, PA: Lippincott Williams and Wilkins; 2011.
1. Trivedi PJ, Kumagi T, Al-Harthy N, et al. Good maternal and fetal outcomes for pregnant women with primary biliary cirrhosis. Clin Gastroenterol Hepatol. 2014;12:1179-1185.
2. Marchioni Beery RM, Vaziri H, Forouhar F. Primary biliary cirrhosis and primary sclerosing cholangitis: a review featuring a women’s health perspective. J Clin Transl Hepatol. 2014;2:266-284.
3. Efe C, Kahramanoğlu-Aksoy E, Yilmaz B, et al. Pregnancy in women with primary biliary cirrhosis. Autoimmun Rev. 2014;13:931-935.
4. Floreani A, Infantolino C, Franceschet I, et al. Pregnancy and primary biliary cirrhosis: a case control study. Clin Rev Allergy Immunol. 2015;48:236-242.
5. Rabinovitz M, Appasamy R, Finkelstein S. Primary biliary cirrhosis diagnosed during pregnancy. Does it have a different outcome? Dig Dis Sci. 1995;40:571-574.
6. Carey EJ, Ali AH, Lindor KD. Primary biliary cirrhosis. Lancet. 2015;386:1565-1575.
7. The Johns Hopkins School of Medicine Department of Gynecology. Hurt KJ, Guile MW, Bienstock JL, et al, eds. The Johns Hopkins Manual of Gynecology and Obstetrics. 4th edition. Philadelphia, PA: Lippincott Williams and Wilkins; 2011.