User login
Official Newspaper of the American College of Surgeons
Lawmakers Participate in ACS Bleeding Control Training
Leaders of the American College of Surgeons (ACS) hosted a Stop the Bleed® training program on Capitol Hill October 12 for members of Congress and their staffs. The congressional event focused on how early intervention from a Stop the Bleed-trained individual can save the life of someone suffering from a bleeding injury. Participants came to learn more about the ACS’ efforts with Stop the Bleed and engage in the hands-on training in how to control bleeding. The training was led by ACS Fellows, including Lenworth M. Jacobs, Jr., MD, MPH, FACS; Leonard J. Weireter, Jr., MD, FACS; Mark L. Gestring, MD, FACS; John H. Armstrong, MD, FACS; Joseph V. Sakran, MD, MPH, MPA, FACS; and Jack Sava, MD, FACS. Congressional guests included Reps. Ami Bera, MD (D-CA); Phil Roe, MD (R-TN); Raul Ruiz, MD (D-CA); and Brad Wenstrup, DPM (R-OH), who provided opening remarks.
Members of Congress and their staff left the program with a better understanding of how to become life-saving immediate responders and the value of Stop the Bleed training. In addition to promoting Stop the Bleed training, the College also is advocating for widespread access to bleeding control education before federal and state lawmakers.
For more information about ACS trauma advocacy, contact Justin Rosen, Congressional Lobbyist, at [email protected] or 202-672-1528. For more information about the Stop the Bleed program, visit BleedingControl.org.
Leaders of the American College of Surgeons (ACS) hosted a Stop the Bleed® training program on Capitol Hill October 12 for members of Congress and their staffs. The congressional event focused on how early intervention from a Stop the Bleed-trained individual can save the life of someone suffering from a bleeding injury. Participants came to learn more about the ACS’ efforts with Stop the Bleed and engage in the hands-on training in how to control bleeding. The training was led by ACS Fellows, including Lenworth M. Jacobs, Jr., MD, MPH, FACS; Leonard J. Weireter, Jr., MD, FACS; Mark L. Gestring, MD, FACS; John H. Armstrong, MD, FACS; Joseph V. Sakran, MD, MPH, MPA, FACS; and Jack Sava, MD, FACS. Congressional guests included Reps. Ami Bera, MD (D-CA); Phil Roe, MD (R-TN); Raul Ruiz, MD (D-CA); and Brad Wenstrup, DPM (R-OH), who provided opening remarks.
Members of Congress and their staff left the program with a better understanding of how to become life-saving immediate responders and the value of Stop the Bleed training. In addition to promoting Stop the Bleed training, the College also is advocating for widespread access to bleeding control education before federal and state lawmakers.
For more information about ACS trauma advocacy, contact Justin Rosen, Congressional Lobbyist, at [email protected] or 202-672-1528. For more information about the Stop the Bleed program, visit BleedingControl.org.
Leaders of the American College of Surgeons (ACS) hosted a Stop the Bleed® training program on Capitol Hill October 12 for members of Congress and their staffs. The congressional event focused on how early intervention from a Stop the Bleed-trained individual can save the life of someone suffering from a bleeding injury. Participants came to learn more about the ACS’ efforts with Stop the Bleed and engage in the hands-on training in how to control bleeding. The training was led by ACS Fellows, including Lenworth M. Jacobs, Jr., MD, MPH, FACS; Leonard J. Weireter, Jr., MD, FACS; Mark L. Gestring, MD, FACS; John H. Armstrong, MD, FACS; Joseph V. Sakran, MD, MPH, MPA, FACS; and Jack Sava, MD, FACS. Congressional guests included Reps. Ami Bera, MD (D-CA); Phil Roe, MD (R-TN); Raul Ruiz, MD (D-CA); and Brad Wenstrup, DPM (R-OH), who provided opening remarks.
Members of Congress and their staff left the program with a better understanding of how to become life-saving immediate responders and the value of Stop the Bleed training. In addition to promoting Stop the Bleed training, the College also is advocating for widespread access to bleeding control education before federal and state lawmakers.
For more information about ACS trauma advocacy, contact Justin Rosen, Congressional Lobbyist, at [email protected] or 202-672-1528. For more information about the Stop the Bleed program, visit BleedingControl.org.
Read the November Bulletin : Should your health care system invest in an ambulatory surgical center
The November issue of the Bulletin of the American College of Surgeons is now available online at bulletin.facs.org. This month’s Bulletin includes the following features, columns, and new stories, among others:
Features
• Frank R. Lewis, Jr., MD, FACS: 15 years of visionary leadership at the American Board of Surgery
• A history of health information technology and the future of interoperability
Columns
• Looking forward: Health care reform
• What surgeons should know about...The New Medicare Card Project
• ACS NSQIP best practices case studies: Quality improvement in imaging strategies for pediatric appendicitis
News
• Barbara Lee Bass, MD, FACS, FRCS(Hon), installed as 98th ACS President
• Honorary Fellowship in the ACS awarded to 10 prominent surgeons
• Call for nominations for the ACS Board of Regents and ACS Officers-Elect
The Bulletin is available in a variety of digital formats to satisfy every reader’s preference, including an interactive version and a smartphone app. Go to the Bulletin website at bulletin.facs.org to connect to any of these versions or to read the articles directly online.
The November issue of the Bulletin of the American College of Surgeons is now available online at bulletin.facs.org. This month’s Bulletin includes the following features, columns, and new stories, among others:
Features
• Frank R. Lewis, Jr., MD, FACS: 15 years of visionary leadership at the American Board of Surgery
• A history of health information technology and the future of interoperability
Columns
• Looking forward: Health care reform
• What surgeons should know about...The New Medicare Card Project
• ACS NSQIP best practices case studies: Quality improvement in imaging strategies for pediatric appendicitis
News
• Barbara Lee Bass, MD, FACS, FRCS(Hon), installed as 98th ACS President
• Honorary Fellowship in the ACS awarded to 10 prominent surgeons
• Call for nominations for the ACS Board of Regents and ACS Officers-Elect
The Bulletin is available in a variety of digital formats to satisfy every reader’s preference, including an interactive version and a smartphone app. Go to the Bulletin website at bulletin.facs.org to connect to any of these versions or to read the articles directly online.
The November issue of the Bulletin of the American College of Surgeons is now available online at bulletin.facs.org. This month’s Bulletin includes the following features, columns, and new stories, among others:
Features
• Frank R. Lewis, Jr., MD, FACS: 15 years of visionary leadership at the American Board of Surgery
• A history of health information technology and the future of interoperability
Columns
• Looking forward: Health care reform
• What surgeons should know about...The New Medicare Card Project
• ACS NSQIP best practices case studies: Quality improvement in imaging strategies for pediatric appendicitis
News
• Barbara Lee Bass, MD, FACS, FRCS(Hon), installed as 98th ACS President
• Honorary Fellowship in the ACS awarded to 10 prominent surgeons
• Call for nominations for the ACS Board of Regents and ACS Officers-Elect
The Bulletin is available in a variety of digital formats to satisfy every reader’s preference, including an interactive version and a smartphone app. Go to the Bulletin website at bulletin.facs.org to connect to any of these versions or to read the articles directly online.
VIDEO: Liver transplant center competition tied to delisting patients
WASHINGTON – Low market competition among liver transplant centers may affect which patients are considered too sick to transplant, according to a study presented at the annual meeting of the American Association for the Study of Liver Diseases.
With 20% of patients dying while on the transplant wait list, including those who were delisted, understanding the distribution of organs among donor service areas (DSAs) is crucial to lowering mortality during the current organ shortage, according to presenter Yanik Babekov, MD, of Massachusetts General Hospital, Boston.
Investigators studied 3,131 patients who were delisted after being classified as “too sick” from 116 centers in 51 DSAs, between 2002 and 2012.
Researchers used the Herfindahl-Hirschman Index (HHI), which analyzes the market share of each participant to determine the overall level of competition. Measurements on the HHI range between 0 and 1, with 0 being the most competitive and 1 being the least.
Mean delisting Model for End-Stage Liver Disease (MELD) scores considered to be “too sick to transplant” were 26.1, and average HHI among DSAs was 0.46, according to investigators. They found that, for every 1% increase in HHI, the delisting MELD score increased by 0.06, according to a risk-adjustment analysis.
“In other words, more competitive DSAs delist patients for [being] ‘too sick’ at lower MELD scores,” Dr. Babekov explained in a video interview. “Interestingly, race, education, citizenship, and other DSA factors also impacted delisting MELD for ‘too sick.’ ”
While market competition may not be the only factor to explain the phenomenon of patients delisted for being ‘too sick,’ it is important to identify how having more transplant centers in DSAs can help more patients be added to, and stay on, these wait lists, according to investigators.
Dr. Babekov had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @eaztweets
WASHINGTON – Low market competition among liver transplant centers may affect which patients are considered too sick to transplant, according to a study presented at the annual meeting of the American Association for the Study of Liver Diseases.
With 20% of patients dying while on the transplant wait list, including those who were delisted, understanding the distribution of organs among donor service areas (DSAs) is crucial to lowering mortality during the current organ shortage, according to presenter Yanik Babekov, MD, of Massachusetts General Hospital, Boston.
Investigators studied 3,131 patients who were delisted after being classified as “too sick” from 116 centers in 51 DSAs, between 2002 and 2012.
Researchers used the Herfindahl-Hirschman Index (HHI), which analyzes the market share of each participant to determine the overall level of competition. Measurements on the HHI range between 0 and 1, with 0 being the most competitive and 1 being the least.
Mean delisting Model for End-Stage Liver Disease (MELD) scores considered to be “too sick to transplant” were 26.1, and average HHI among DSAs was 0.46, according to investigators. They found that, for every 1% increase in HHI, the delisting MELD score increased by 0.06, according to a risk-adjustment analysis.
“In other words, more competitive DSAs delist patients for [being] ‘too sick’ at lower MELD scores,” Dr. Babekov explained in a video interview. “Interestingly, race, education, citizenship, and other DSA factors also impacted delisting MELD for ‘too sick.’ ”
While market competition may not be the only factor to explain the phenomenon of patients delisted for being ‘too sick,’ it is important to identify how having more transplant centers in DSAs can help more patients be added to, and stay on, these wait lists, according to investigators.
Dr. Babekov had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @eaztweets
WASHINGTON – Low market competition among liver transplant centers may affect which patients are considered too sick to transplant, according to a study presented at the annual meeting of the American Association for the Study of Liver Diseases.
With 20% of patients dying while on the transplant wait list, including those who were delisted, understanding the distribution of organs among donor service areas (DSAs) is crucial to lowering mortality during the current organ shortage, according to presenter Yanik Babekov, MD, of Massachusetts General Hospital, Boston.
Investigators studied 3,131 patients who were delisted after being classified as “too sick” from 116 centers in 51 DSAs, between 2002 and 2012.
Researchers used the Herfindahl-Hirschman Index (HHI), which analyzes the market share of each participant to determine the overall level of competition. Measurements on the HHI range between 0 and 1, with 0 being the most competitive and 1 being the least.
Mean delisting Model for End-Stage Liver Disease (MELD) scores considered to be “too sick to transplant” were 26.1, and average HHI among DSAs was 0.46, according to investigators. They found that, for every 1% increase in HHI, the delisting MELD score increased by 0.06, according to a risk-adjustment analysis.
“In other words, more competitive DSAs delist patients for [being] ‘too sick’ at lower MELD scores,” Dr. Babekov explained in a video interview. “Interestingly, race, education, citizenship, and other DSA factors also impacted delisting MELD for ‘too sick.’ ”
While market competition may not be the only factor to explain the phenomenon of patients delisted for being ‘too sick,’ it is important to identify how having more transplant centers in DSAs can help more patients be added to, and stay on, these wait lists, according to investigators.
Dr. Babekov had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @eaztweets
AT THE LIVER MEETING 2017
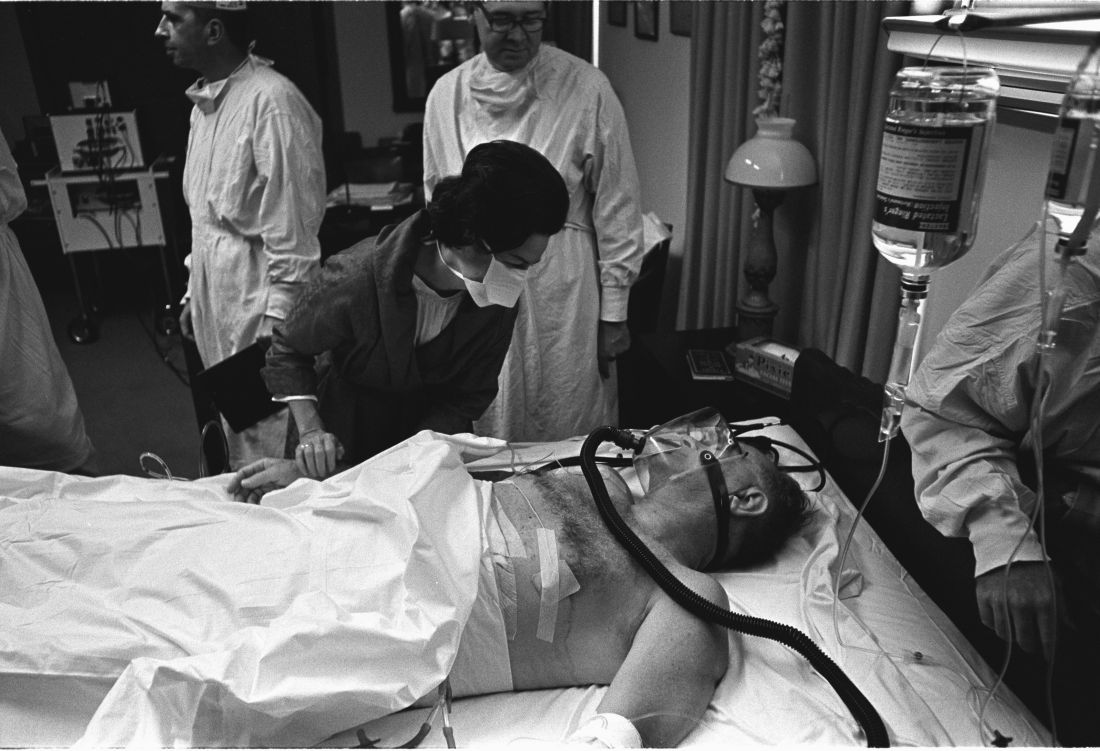
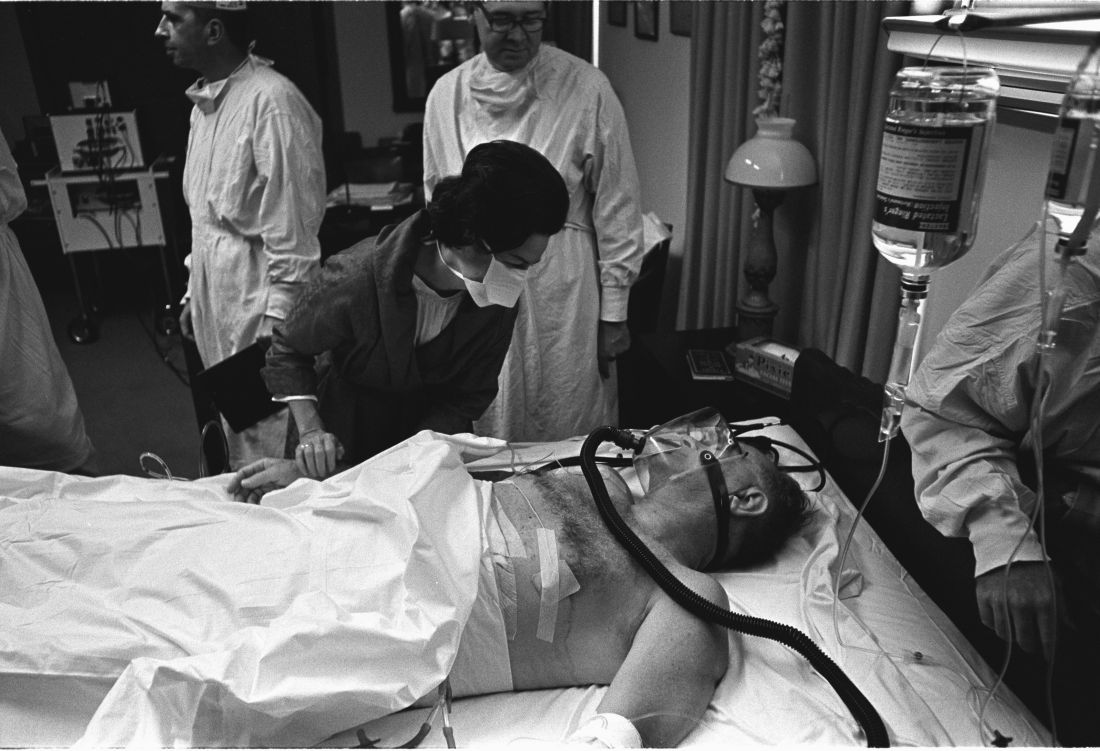
Surgeons paid a price for presidential procedures
SAN DIEGO – A surgical team was forced to perform a delicate oral procedure on a rocking yacht while making sure to preserve presidential whiskers. A domineering doctor ignored fellow physicians while a president spent months dying in agony. And, after helping to save the leader of the free world, the leader of the American College of Surgeons found himself viciously attacked by his own colleagues.
When a quartet of ill U.S. presidents developed major medical problems, an audience at the annual clinical congress of the American College of Surgeons learned, their treating physicians ended up with major headaches of their own.
President Grover Cleveland, for example, required his surgical team to remove an oral tumor in total secrecy in 1893, robbing him of a big chunk of his upper palate. “The president had a mustache, and the mustache had to be left alone, and there could be no scars,” said the Hospital for Special Surgery’s J. Patrick O’Leary, MD, FACS, who spoke in a session focused on the history of presidential medicine.
The only light came from a single incandescent bulb, and the procedure was performed at sea, on a yacht anchored off Long Island, N.Y.
“If you were presented with these parameters as a surgeon today, my guess is that you would have demurred on taking on this project,” Dr. O’Leary said. “It was a prescription for a disaster.”
President Cleveland survived for another 15 years. James Garfield, a fellow Civil War veteran, wasn’t so fortunate. In 1881, he was astonishingly unlucky, the unwitting victim of a fumbling physician who dominated his care after an assassin shot him in the chest.
That physician, Willard Bliss, MD, dismissed other doctors who knew the president well and isolated this gregarious man from friends and family. He also ignored emerging knowledge about germ control. And he fed Garfield a heavy diet that the digestively sensitive president probably couldn’t have tolerated in the best of times. The result: endless vomiting, the loss of almost 80 pounds, and an unsuccessful rectal feeding regimen.
Toward the end of the president’s gruesome summer-long decline, Dr. Bliss told all but two doctors to stay away, John B. Hanks, MD, of the University of Virginia, Charlottesville, said in his presentation. Then the president died of a wound that Dr. Hanks said would have been survivable with proper care even in the 1880s.
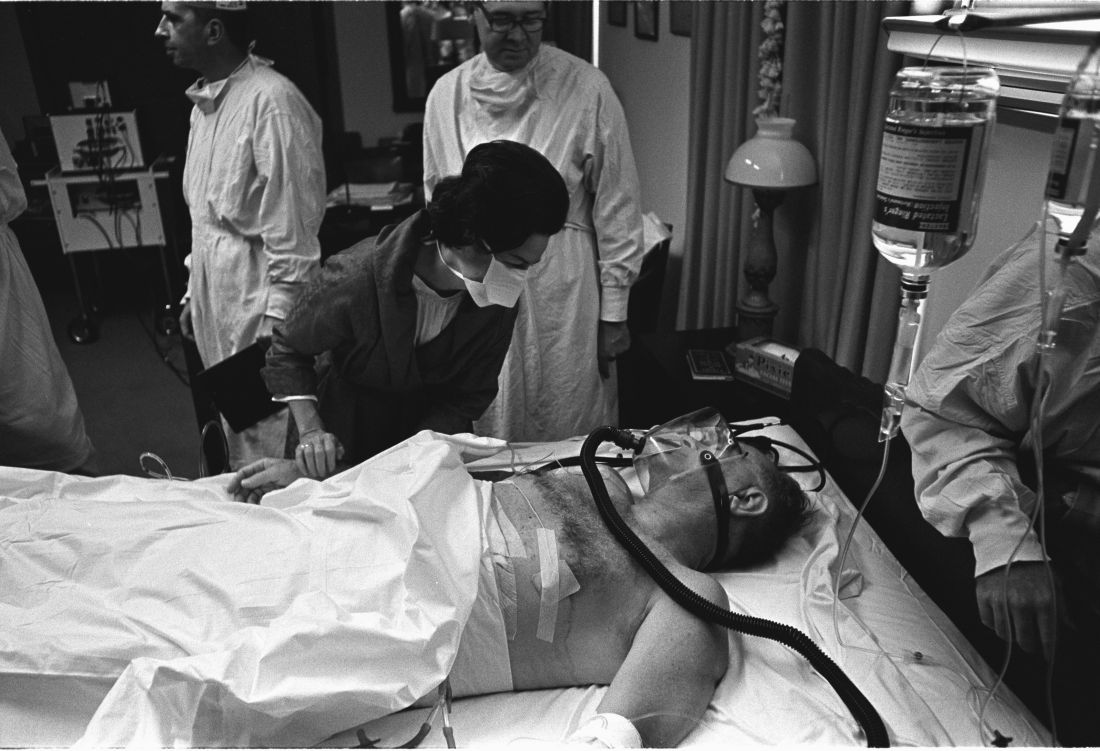
History has been unkind to Dr. Bliss, in part because his patient died. But another presidential physician faced bizarre post surgery scorn from his ACS colleagues, even though his patient lived, according to Justin Barr, MD, PhD, of Duke University, Durham, N.C.
In 1956, surgeon Isidor Ravdin, MD, of the University of Pennsylvania, Philadelphia, was called in when President Dwight D. Eisenhower needed surgery to eliminate a bowel obstruction.
A team of physicians agreed that the president needed surgery. “They felt they were dealing with an elderly, sick patient who’d been in shock during his illness and had recently suffered a myocardial infarction,” Dr. Barr said. “They unanimously decided to proceed with a bypass over resection.”
It’s clear today that the physicians made the correct choice, Dr. Barr said. But his colleagues attacked Dr. Ravdin, who later complained that criticisms multiplied in direct ratio to distance from the operating room.
At the time, Dr. Ravdin was chair of the ACS Board of Regents. The entire board accused him of violating college policies regarding “ghost surgery” (performing procedures without the patient’s knowledge) and “itinerant surgery” (traveling to perform a procedure and then leaving).
Dr. Ravdin acknowledged that he had performed itinerant surgery to some extent, but he denied the ghost surgery charge. In fact, he and the president became friends.
His colleagues also attacked him over his decision to not perform a resection procedure. “They were accusing him of not only being an unethical surgeon, but also an incompetent one,” said Dr. Barr, who calls the letters about the allegations “truly bewildering.”
Also bewildering: Lyndon B. Johnson’s choice to display his gallbladder surgery scar to the press in 1965, spawning one of the most infamous photos of his presidency.
Few surgeons see their handiwork so prominently displayed. Fortunately for them, the operating theater was in a naval hospital, not on a boat. And, as far as we know, no one fretted over the fate of a single facial hair.
SAN DIEGO – A surgical team was forced to perform a delicate oral procedure on a rocking yacht while making sure to preserve presidential whiskers. A domineering doctor ignored fellow physicians while a president spent months dying in agony. And, after helping to save the leader of the free world, the leader of the American College of Surgeons found himself viciously attacked by his own colleagues.
When a quartet of ill U.S. presidents developed major medical problems, an audience at the annual clinical congress of the American College of Surgeons learned, their treating physicians ended up with major headaches of their own.
President Grover Cleveland, for example, required his surgical team to remove an oral tumor in total secrecy in 1893, robbing him of a big chunk of his upper palate. “The president had a mustache, and the mustache had to be left alone, and there could be no scars,” said the Hospital for Special Surgery’s J. Patrick O’Leary, MD, FACS, who spoke in a session focused on the history of presidential medicine.
The only light came from a single incandescent bulb, and the procedure was performed at sea, on a yacht anchored off Long Island, N.Y.
“If you were presented with these parameters as a surgeon today, my guess is that you would have demurred on taking on this project,” Dr. O’Leary said. “It was a prescription for a disaster.”
President Cleveland survived for another 15 years. James Garfield, a fellow Civil War veteran, wasn’t so fortunate. In 1881, he was astonishingly unlucky, the unwitting victim of a fumbling physician who dominated his care after an assassin shot him in the chest.
That physician, Willard Bliss, MD, dismissed other doctors who knew the president well and isolated this gregarious man from friends and family. He also ignored emerging knowledge about germ control. And he fed Garfield a heavy diet that the digestively sensitive president probably couldn’t have tolerated in the best of times. The result: endless vomiting, the loss of almost 80 pounds, and an unsuccessful rectal feeding regimen.
Toward the end of the president’s gruesome summer-long decline, Dr. Bliss told all but two doctors to stay away, John B. Hanks, MD, of the University of Virginia, Charlottesville, said in his presentation. Then the president died of a wound that Dr. Hanks said would have been survivable with proper care even in the 1880s.
History has been unkind to Dr. Bliss, in part because his patient died. But another presidential physician faced bizarre post surgery scorn from his ACS colleagues, even though his patient lived, according to Justin Barr, MD, PhD, of Duke University, Durham, N.C.
In 1956, surgeon Isidor Ravdin, MD, of the University of Pennsylvania, Philadelphia, was called in when President Dwight D. Eisenhower needed surgery to eliminate a bowel obstruction.
A team of physicians agreed that the president needed surgery. “They felt they were dealing with an elderly, sick patient who’d been in shock during his illness and had recently suffered a myocardial infarction,” Dr. Barr said. “They unanimously decided to proceed with a bypass over resection.”
It’s clear today that the physicians made the correct choice, Dr. Barr said. But his colleagues attacked Dr. Ravdin, who later complained that criticisms multiplied in direct ratio to distance from the operating room.
At the time, Dr. Ravdin was chair of the ACS Board of Regents. The entire board accused him of violating college policies regarding “ghost surgery” (performing procedures without the patient’s knowledge) and “itinerant surgery” (traveling to perform a procedure and then leaving).
Dr. Ravdin acknowledged that he had performed itinerant surgery to some extent, but he denied the ghost surgery charge. In fact, he and the president became friends.
His colleagues also attacked him over his decision to not perform a resection procedure. “They were accusing him of not only being an unethical surgeon, but also an incompetent one,” said Dr. Barr, who calls the letters about the allegations “truly bewildering.”
Also bewildering: Lyndon B. Johnson’s choice to display his gallbladder surgery scar to the press in 1965, spawning one of the most infamous photos of his presidency.
Few surgeons see their handiwork so prominently displayed. Fortunately for them, the operating theater was in a naval hospital, not on a boat. And, as far as we know, no one fretted over the fate of a single facial hair.
SAN DIEGO – A surgical team was forced to perform a delicate oral procedure on a rocking yacht while making sure to preserve presidential whiskers. A domineering doctor ignored fellow physicians while a president spent months dying in agony. And, after helping to save the leader of the free world, the leader of the American College of Surgeons found himself viciously attacked by his own colleagues.
When a quartet of ill U.S. presidents developed major medical problems, an audience at the annual clinical congress of the American College of Surgeons learned, their treating physicians ended up with major headaches of their own.
President Grover Cleveland, for example, required his surgical team to remove an oral tumor in total secrecy in 1893, robbing him of a big chunk of his upper palate. “The president had a mustache, and the mustache had to be left alone, and there could be no scars,” said the Hospital for Special Surgery’s J. Patrick O’Leary, MD, FACS, who spoke in a session focused on the history of presidential medicine.
The only light came from a single incandescent bulb, and the procedure was performed at sea, on a yacht anchored off Long Island, N.Y.
“If you were presented with these parameters as a surgeon today, my guess is that you would have demurred on taking on this project,” Dr. O’Leary said. “It was a prescription for a disaster.”
President Cleveland survived for another 15 years. James Garfield, a fellow Civil War veteran, wasn’t so fortunate. In 1881, he was astonishingly unlucky, the unwitting victim of a fumbling physician who dominated his care after an assassin shot him in the chest.
That physician, Willard Bliss, MD, dismissed other doctors who knew the president well and isolated this gregarious man from friends and family. He also ignored emerging knowledge about germ control. And he fed Garfield a heavy diet that the digestively sensitive president probably couldn’t have tolerated in the best of times. The result: endless vomiting, the loss of almost 80 pounds, and an unsuccessful rectal feeding regimen.
Toward the end of the president’s gruesome summer-long decline, Dr. Bliss told all but two doctors to stay away, John B. Hanks, MD, of the University of Virginia, Charlottesville, said in his presentation. Then the president died of a wound that Dr. Hanks said would have been survivable with proper care even in the 1880s.
History has been unkind to Dr. Bliss, in part because his patient died. But another presidential physician faced bizarre post surgery scorn from his ACS colleagues, even though his patient lived, according to Justin Barr, MD, PhD, of Duke University, Durham, N.C.
In 1956, surgeon Isidor Ravdin, MD, of the University of Pennsylvania, Philadelphia, was called in when President Dwight D. Eisenhower needed surgery to eliminate a bowel obstruction.
A team of physicians agreed that the president needed surgery. “They felt they were dealing with an elderly, sick patient who’d been in shock during his illness and had recently suffered a myocardial infarction,” Dr. Barr said. “They unanimously decided to proceed with a bypass over resection.”
It’s clear today that the physicians made the correct choice, Dr. Barr said. But his colleagues attacked Dr. Ravdin, who later complained that criticisms multiplied in direct ratio to distance from the operating room.
At the time, Dr. Ravdin was chair of the ACS Board of Regents. The entire board accused him of violating college policies regarding “ghost surgery” (performing procedures without the patient’s knowledge) and “itinerant surgery” (traveling to perform a procedure and then leaving).
Dr. Ravdin acknowledged that he had performed itinerant surgery to some extent, but he denied the ghost surgery charge. In fact, he and the president became friends.
His colleagues also attacked him over his decision to not perform a resection procedure. “They were accusing him of not only being an unethical surgeon, but also an incompetent one,” said Dr. Barr, who calls the letters about the allegations “truly bewildering.”
Also bewildering: Lyndon B. Johnson’s choice to display his gallbladder surgery scar to the press in 1965, spawning one of the most infamous photos of his presidency.
Few surgeons see their handiwork so prominently displayed. Fortunately for them, the operating theater was in a naval hospital, not on a boat. And, as far as we know, no one fretted over the fate of a single facial hair.
AT THE ACS CLINICAL CONGRESS
Hypothyroidism carries higher surgical risk not captured by calculator
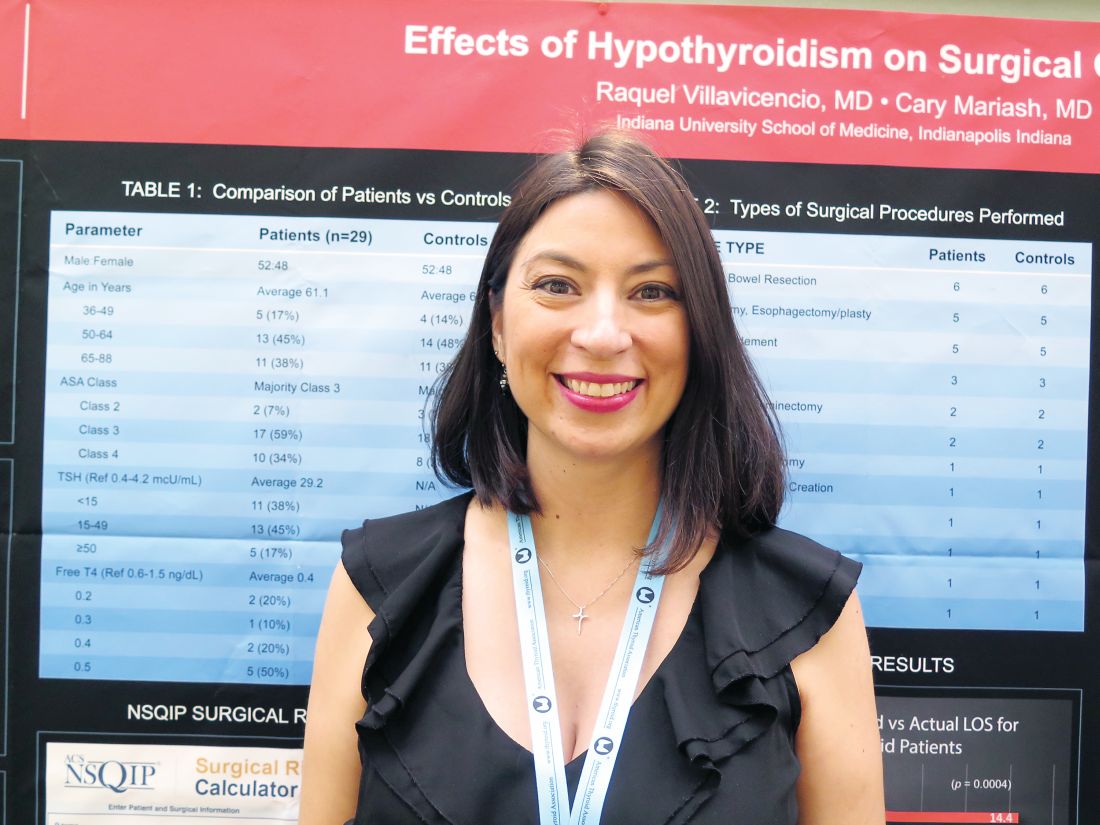
VICTORIA, B.C. – Even with contemporary anesthesia and surgical techniques, patients who are overtly hypothyroid at the time of major surgery have a rockier course, suggests a retrospective cohort study of 58 patients in a poster presentation at the annual meeting of the American Thyroid Association.
Actual length of stay for hypothyroid patients was twice that predicted by a commonly used risk calculator, whereas actual and predicted stays aligned well for euthyroid patients. The hypothyroid group had more cases of postoperative atrial fibrillation, ileus, reintubation, and death, although numbers were too small for statistical comparison.
“This will have an impact on how we look at patients, especially from a hospital standpoint and management. That’s quite a bit longer stay and quite a bit more cost. And the longer you stay, the more complications you have, too, so it could be riskier for the patient as well,” said first author Raquel Villavicencio, MD, a fellow at Indiana University at the time of the study, and now a clinical endocrinologist at Community Hospital in Indianapolis.
“Although we don’t consider hypothyroidism an absolute contraindication to surgery, especially if it’s necessary surgery, certainly anybody who is having elective surgery should have it postponed, in our opinion, until they are rendered euthyroid,” she said. “More studies are needed to look at this a little bit closer.”
Explaining the study’s rationale, Dr. Villavicencio noted, “This was a question that came up maybe three or four times a year, where we would get a hypothyroid patient and had to decide whether or not to clear them for surgery.”
Previous studies conducted at large institutions, the Mayo Clinic and Massachusetts General Hospital, had conflicting findings and were done about 30 years ago, she said. Anesthesia and surgical care have improved substantially since then, leading the investigators to hypothesize that hypothyroidism would not carry higher surgical risk today.
Dr. Villavicencio and her coinvestigator, Cary Mariash, MD, used their institutional database to identify 29 adult patients with a thyroid-stimulating hormone (TSH) level of greater than 10 mcU/mL alone or with a TSH level exceeding the upper limit of normal along with a free thyroxine (T4) level of less than 0.6 ng/dL who underwent surgery during 2010-2015. They matched each patient on age, sex, and surgical procedure with a control euthyroid patient.
The mean TSH level in the hypothyroid group was 29.2 mcU/mL. The majority of patients in each group – 59% of the hypothyroid group and 62% of the euthyroid group – had an American Surgical Association class of 3, denoting that this was a fairly sick population. The groups were generally similar on rates of comorbidity, except that the euthyroid patients had a slightly higher prevalence of obstructive sleep apnea.
In both groups, the majority of procedures were laparotomy and/or bowel resection; pharyngolaryngectomy and esophagectomy/esophagoplasty; and wound or bone debridement.
Main results showed that in the hypothyroid group, hospital length of stay predicted with the American College of Surgeons National Surgical Quality Improvement Program surgical risk calculator was 6.9 days, but actual length of stay was 14.4 days (P = .0004). In contrast, in the euthyroid group, predicted length of stay was a similar at 7.1 days, and actual length of stay was statistically indistinguishable at 9.2 days (P = .1).
“Hypothyroidism is not taken into account with this calculator,” Dr. Villavicencio noted, adding that she was unaware of any surgical calculators that do.
One patient in the hypothyroid group died, compared with none in the euthyroid group. In terms of postoperative cardiac complications, two patients in the hypothyroid group experienced atrial fibrillation, and there was one case of pulseless electrical–activity arrest in each group.
The groups did not differ on incidence of hypothermia, bradycardia, hyponatremia, time to extubation, and hypotension. However, mean arterial pressure tended to be lower in the hypothyroid group (51 mm Hg) than in the euthyroid group (56 mm Hg), and the former more often needed vasopressors. Furthermore, postoperative ileus and reintubation were more common in the hypothyroid group.
“I think that there are kind of a lot of little things that add up to explain [the longer stay],” said Dr. Villavicencio, who disclosed that she had no relevant conflicts of interest.
VICTORIA, B.C. – Even with contemporary anesthesia and surgical techniques, patients who are overtly hypothyroid at the time of major surgery have a rockier course, suggests a retrospective cohort study of 58 patients in a poster presentation at the annual meeting of the American Thyroid Association.
Actual length of stay for hypothyroid patients was twice that predicted by a commonly used risk calculator, whereas actual and predicted stays aligned well for euthyroid patients. The hypothyroid group had more cases of postoperative atrial fibrillation, ileus, reintubation, and death, although numbers were too small for statistical comparison.
“This will have an impact on how we look at patients, especially from a hospital standpoint and management. That’s quite a bit longer stay and quite a bit more cost. And the longer you stay, the more complications you have, too, so it could be riskier for the patient as well,” said first author Raquel Villavicencio, MD, a fellow at Indiana University at the time of the study, and now a clinical endocrinologist at Community Hospital in Indianapolis.
“Although we don’t consider hypothyroidism an absolute contraindication to surgery, especially if it’s necessary surgery, certainly anybody who is having elective surgery should have it postponed, in our opinion, until they are rendered euthyroid,” she said. “More studies are needed to look at this a little bit closer.”
Explaining the study’s rationale, Dr. Villavicencio noted, “This was a question that came up maybe three or four times a year, where we would get a hypothyroid patient and had to decide whether or not to clear them for surgery.”
Previous studies conducted at large institutions, the Mayo Clinic and Massachusetts General Hospital, had conflicting findings and were done about 30 years ago, she said. Anesthesia and surgical care have improved substantially since then, leading the investigators to hypothesize that hypothyroidism would not carry higher surgical risk today.
Dr. Villavicencio and her coinvestigator, Cary Mariash, MD, used their institutional database to identify 29 adult patients with a thyroid-stimulating hormone (TSH) level of greater than 10 mcU/mL alone or with a TSH level exceeding the upper limit of normal along with a free thyroxine (T4) level of less than 0.6 ng/dL who underwent surgery during 2010-2015. They matched each patient on age, sex, and surgical procedure with a control euthyroid patient.
The mean TSH level in the hypothyroid group was 29.2 mcU/mL. The majority of patients in each group – 59% of the hypothyroid group and 62% of the euthyroid group – had an American Surgical Association class of 3, denoting that this was a fairly sick population. The groups were generally similar on rates of comorbidity, except that the euthyroid patients had a slightly higher prevalence of obstructive sleep apnea.
In both groups, the majority of procedures were laparotomy and/or bowel resection; pharyngolaryngectomy and esophagectomy/esophagoplasty; and wound or bone debridement.
Main results showed that in the hypothyroid group, hospital length of stay predicted with the American College of Surgeons National Surgical Quality Improvement Program surgical risk calculator was 6.9 days, but actual length of stay was 14.4 days (P = .0004). In contrast, in the euthyroid group, predicted length of stay was a similar at 7.1 days, and actual length of stay was statistically indistinguishable at 9.2 days (P = .1).
“Hypothyroidism is not taken into account with this calculator,” Dr. Villavicencio noted, adding that she was unaware of any surgical calculators that do.
One patient in the hypothyroid group died, compared with none in the euthyroid group. In terms of postoperative cardiac complications, two patients in the hypothyroid group experienced atrial fibrillation, and there was one case of pulseless electrical–activity arrest in each group.
The groups did not differ on incidence of hypothermia, bradycardia, hyponatremia, time to extubation, and hypotension. However, mean arterial pressure tended to be lower in the hypothyroid group (51 mm Hg) than in the euthyroid group (56 mm Hg), and the former more often needed vasopressors. Furthermore, postoperative ileus and reintubation were more common in the hypothyroid group.
“I think that there are kind of a lot of little things that add up to explain [the longer stay],” said Dr. Villavicencio, who disclosed that she had no relevant conflicts of interest.
VICTORIA, B.C. – Even with contemporary anesthesia and surgical techniques, patients who are overtly hypothyroid at the time of major surgery have a rockier course, suggests a retrospective cohort study of 58 patients in a poster presentation at the annual meeting of the American Thyroid Association.
Actual length of stay for hypothyroid patients was twice that predicted by a commonly used risk calculator, whereas actual and predicted stays aligned well for euthyroid patients. The hypothyroid group had more cases of postoperative atrial fibrillation, ileus, reintubation, and death, although numbers were too small for statistical comparison.
“This will have an impact on how we look at patients, especially from a hospital standpoint and management. That’s quite a bit longer stay and quite a bit more cost. And the longer you stay, the more complications you have, too, so it could be riskier for the patient as well,” said first author Raquel Villavicencio, MD, a fellow at Indiana University at the time of the study, and now a clinical endocrinologist at Community Hospital in Indianapolis.
“Although we don’t consider hypothyroidism an absolute contraindication to surgery, especially if it’s necessary surgery, certainly anybody who is having elective surgery should have it postponed, in our opinion, until they are rendered euthyroid,” she said. “More studies are needed to look at this a little bit closer.”
Explaining the study’s rationale, Dr. Villavicencio noted, “This was a question that came up maybe three or four times a year, where we would get a hypothyroid patient and had to decide whether or not to clear them for surgery.”
Previous studies conducted at large institutions, the Mayo Clinic and Massachusetts General Hospital, had conflicting findings and were done about 30 years ago, she said. Anesthesia and surgical care have improved substantially since then, leading the investigators to hypothesize that hypothyroidism would not carry higher surgical risk today.
Dr. Villavicencio and her coinvestigator, Cary Mariash, MD, used their institutional database to identify 29 adult patients with a thyroid-stimulating hormone (TSH) level of greater than 10 mcU/mL alone or with a TSH level exceeding the upper limit of normal along with a free thyroxine (T4) level of less than 0.6 ng/dL who underwent surgery during 2010-2015. They matched each patient on age, sex, and surgical procedure with a control euthyroid patient.
The mean TSH level in the hypothyroid group was 29.2 mcU/mL. The majority of patients in each group – 59% of the hypothyroid group and 62% of the euthyroid group – had an American Surgical Association class of 3, denoting that this was a fairly sick population. The groups were generally similar on rates of comorbidity, except that the euthyroid patients had a slightly higher prevalence of obstructive sleep apnea.
In both groups, the majority of procedures were laparotomy and/or bowel resection; pharyngolaryngectomy and esophagectomy/esophagoplasty; and wound or bone debridement.
Main results showed that in the hypothyroid group, hospital length of stay predicted with the American College of Surgeons National Surgical Quality Improvement Program surgical risk calculator was 6.9 days, but actual length of stay was 14.4 days (P = .0004). In contrast, in the euthyroid group, predicted length of stay was a similar at 7.1 days, and actual length of stay was statistically indistinguishable at 9.2 days (P = .1).
“Hypothyroidism is not taken into account with this calculator,” Dr. Villavicencio noted, adding that she was unaware of any surgical calculators that do.
One patient in the hypothyroid group died, compared with none in the euthyroid group. In terms of postoperative cardiac complications, two patients in the hypothyroid group experienced atrial fibrillation, and there was one case of pulseless electrical–activity arrest in each group.
The groups did not differ on incidence of hypothermia, bradycardia, hyponatremia, time to extubation, and hypotension. However, mean arterial pressure tended to be lower in the hypothyroid group (51 mm Hg) than in the euthyroid group (56 mm Hg), and the former more often needed vasopressors. Furthermore, postoperative ileus and reintubation were more common in the hypothyroid group.
“I think that there are kind of a lot of little things that add up to explain [the longer stay],” said Dr. Villavicencio, who disclosed that she had no relevant conflicts of interest.
AT ATA 2017
Key clinical point:
Major finding: Actual length of stay was significantly longer than calculator-predicted length of stay among hypothyroid patients (14.4 vs. 6.9 days, P = .0004) but not among euthyroid patients (9.2 vs. 7.1 days; P = .1).
Data source: A retrospective cohort study of 29 hypothyroid patients and 29 matched euthyroid patients undergoing major surgery.
Disclosures: Dr. Villavicencio disclosed that she had no relevant conflicts of interest.
State regulations for tattoo facilities increased blood donor pools
SAN DIEGO – Tattoos are rapidly moving into mainstream America, and as more states regulate tattoo facilities, persons with tattoos can be blood donors without compromising patient safety, Mary Townsend of Blood Systems Inc. reported at the annual meeting of the American Association of Blood Banks.
“Two big states – Arizona and California – were added to the list of approved states, and we had a gain of 2,216 donors in California during a 3-month period and a gain of 4,035 donors in Arizona over 4 months,” Ms. Townsend said.
Both the AABB and the Food and Drug Administration require a 12-month deferral of donors after they have received tattoos using nonsterile needles or reusable ink. The FDA’s current 2015 guidance also states that tattooed donors can give plasma as soon as the inked area has healed if they reside in a state with applied inspections and licenses for tattoo facilities, and if a sterile needle and ink were used.
Blood Systems monitors state regulations to see if they require tattoo establishments to be licensed and require the use of sterile needles and non-reusable ink. To be considered an approved state, the regulations have to be statewide, covering all jurisdictions.
In the study, Ms. Townsend and her colleagues compared the rates of donors who were deferred before and after Arizona and California were added to the list of approved states, to determine the potential gain in donors with changes in state tattoo licensing regulations.
They analyzed blood centers in California and Arizona before and after implementation of state tattoo regulations, and also screened individuals who had received tattoos in those states with the question: “In the past 12 months have you had a tattoo?” and if the answer was ‘yes,’ if the tattoo was applied by a state regulated facility.
For California, they compared two periods – 3 months before regulations were implemented (February to April of 2015) and 3 months after (February to April of 2016) regulations were implemented. For Arizona, they selected a 4-month period (December 2015 to March 2016) and 4 months afterward (December 2016 to March 2017).
A higher proportion of donors who came to centers to donate blood admitted to having gotten a tattoo within the last 12 months in the postregulatory period in both states. The increase in donors occurred immediately following the addition of both states to the Acceptable States List. Accepted donors increased 13-fold in California and 3-fold in Arizona. The absolute number of accepted donors with tattoos rose from 13 to 567 in California and from 151 to 1,496 in Arizona, which represented an annual potential gain of 2,216 and 4,035 additional blood donations.
For blood donors who received a tattoo in a regulated state, blood donations were reviewed for the presence of infectious disease markers including HIV, hepatitis B, and hepatitis C. All donors who had received a tattoo in a regulated state tested negative for HIV, HBV, and HCV.
“Roughly one in three people (in the United States) have a tattoo and, of those, about 70% have more than one tattoo. The bottom line is that 45 million Americans have at least one tattoo,” she said. As state regulations adhere to guidelines regarding tattoos and blood donation, the pool of donors increases.
SAN DIEGO – Tattoos are rapidly moving into mainstream America, and as more states regulate tattoo facilities, persons with tattoos can be blood donors without compromising patient safety, Mary Townsend of Blood Systems Inc. reported at the annual meeting of the American Association of Blood Banks.
“Two big states – Arizona and California – were added to the list of approved states, and we had a gain of 2,216 donors in California during a 3-month period and a gain of 4,035 donors in Arizona over 4 months,” Ms. Townsend said.
Both the AABB and the Food and Drug Administration require a 12-month deferral of donors after they have received tattoos using nonsterile needles or reusable ink. The FDA’s current 2015 guidance also states that tattooed donors can give plasma as soon as the inked area has healed if they reside in a state with applied inspections and licenses for tattoo facilities, and if a sterile needle and ink were used.
Blood Systems monitors state regulations to see if they require tattoo establishments to be licensed and require the use of sterile needles and non-reusable ink. To be considered an approved state, the regulations have to be statewide, covering all jurisdictions.
In the study, Ms. Townsend and her colleagues compared the rates of donors who were deferred before and after Arizona and California were added to the list of approved states, to determine the potential gain in donors with changes in state tattoo licensing regulations.
They analyzed blood centers in California and Arizona before and after implementation of state tattoo regulations, and also screened individuals who had received tattoos in those states with the question: “In the past 12 months have you had a tattoo?” and if the answer was ‘yes,’ if the tattoo was applied by a state regulated facility.
For California, they compared two periods – 3 months before regulations were implemented (February to April of 2015) and 3 months after (February to April of 2016) regulations were implemented. For Arizona, they selected a 4-month period (December 2015 to March 2016) and 4 months afterward (December 2016 to March 2017).
A higher proportion of donors who came to centers to donate blood admitted to having gotten a tattoo within the last 12 months in the postregulatory period in both states. The increase in donors occurred immediately following the addition of both states to the Acceptable States List. Accepted donors increased 13-fold in California and 3-fold in Arizona. The absolute number of accepted donors with tattoos rose from 13 to 567 in California and from 151 to 1,496 in Arizona, which represented an annual potential gain of 2,216 and 4,035 additional blood donations.
For blood donors who received a tattoo in a regulated state, blood donations were reviewed for the presence of infectious disease markers including HIV, hepatitis B, and hepatitis C. All donors who had received a tattoo in a regulated state tested negative for HIV, HBV, and HCV.
“Roughly one in three people (in the United States) have a tattoo and, of those, about 70% have more than one tattoo. The bottom line is that 45 million Americans have at least one tattoo,” she said. As state regulations adhere to guidelines regarding tattoos and blood donation, the pool of donors increases.
SAN DIEGO – Tattoos are rapidly moving into mainstream America, and as more states regulate tattoo facilities, persons with tattoos can be blood donors without compromising patient safety, Mary Townsend of Blood Systems Inc. reported at the annual meeting of the American Association of Blood Banks.
“Two big states – Arizona and California – were added to the list of approved states, and we had a gain of 2,216 donors in California during a 3-month period and a gain of 4,035 donors in Arizona over 4 months,” Ms. Townsend said.
Both the AABB and the Food and Drug Administration require a 12-month deferral of donors after they have received tattoos using nonsterile needles or reusable ink. The FDA’s current 2015 guidance also states that tattooed donors can give plasma as soon as the inked area has healed if they reside in a state with applied inspections and licenses for tattoo facilities, and if a sterile needle and ink were used.
Blood Systems monitors state regulations to see if they require tattoo establishments to be licensed and require the use of sterile needles and non-reusable ink. To be considered an approved state, the regulations have to be statewide, covering all jurisdictions.
In the study, Ms. Townsend and her colleagues compared the rates of donors who were deferred before and after Arizona and California were added to the list of approved states, to determine the potential gain in donors with changes in state tattoo licensing regulations.
They analyzed blood centers in California and Arizona before and after implementation of state tattoo regulations, and also screened individuals who had received tattoos in those states with the question: “In the past 12 months have you had a tattoo?” and if the answer was ‘yes,’ if the tattoo was applied by a state regulated facility.
For California, they compared two periods – 3 months before regulations were implemented (February to April of 2015) and 3 months after (February to April of 2016) regulations were implemented. For Arizona, they selected a 4-month period (December 2015 to March 2016) and 4 months afterward (December 2016 to March 2017).
A higher proportion of donors who came to centers to donate blood admitted to having gotten a tattoo within the last 12 months in the postregulatory period in both states. The increase in donors occurred immediately following the addition of both states to the Acceptable States List. Accepted donors increased 13-fold in California and 3-fold in Arizona. The absolute number of accepted donors with tattoos rose from 13 to 567 in California and from 151 to 1,496 in Arizona, which represented an annual potential gain of 2,216 and 4,035 additional blood donations.
For blood donors who received a tattoo in a regulated state, blood donations were reviewed for the presence of infectious disease markers including HIV, hepatitis B, and hepatitis C. All donors who had received a tattoo in a regulated state tested negative for HIV, HBV, and HCV.
“Roughly one in three people (in the United States) have a tattoo and, of those, about 70% have more than one tattoo. The bottom line is that 45 million Americans have at least one tattoo,” she said. As state regulations adhere to guidelines regarding tattoos and blood donation, the pool of donors increases.
AT AABB 2017
Key clinical point:
Major finding: The absolute number of accepted donors with tattoos rose from 13 to 567 in California and from 151 to 1,496 in Arizona, which represented an annual potential gain of 2,216 and 4,035 additional blood donations.
Data source: An analysis of blood centers in California and Arizona before and after state tattoo regulations were implemented.
Disclosures: Dr. Townsend has no disclosures.
VIDEO: When surgery hurts the surgeon: Intervening to prevent ergonomic injuries
SAN DIEGO – Work-related musculoskeletal disorders are practically inevitable for surgeons, eventually occurring in more than 90%, no matter what type of surgery they practice.
At the annual clinical congress of the American College of Surgeons, this eyebrow-raising fact was presented with a sobering addendum: No one seems to be doing much about it.
“There are some ergonomic guidelines for surgeons out there, but most surgeons don’t know about them,” said Tatiana Catanzarite, MD, who has conducted research on this topic. When she began looking into the problem of work-related injuries among surgeons, she was surprised at the dearth of published research. It’s no wonder then, said Dr. Catanzarite and other panel members, that most surgeons learn proper work posture on the fly and may or may not be using the most efficient and mechanically sound instrumentation angles when performing surgery.
Dr. Catanzarite, a female pelvic medicine and reconstructive surgery fellow at the University of California, San Diego, has just published a literature review on surgeon ergonomics. But reading about how to stand, how to hold instruments, and even how to sit at a robotic surgical console is no match for having an observer on the ground guiding and reinforcing work posture, she said. Unfortunately, that’s an unrealistic expectation for most surgeons, so Dr. Catanzarite is borrowing video-gaming technology to address the situation, she said in an interview.
She has adapted a popular video game motion-capture system that uses an infrared laser projector and a computer sensor to capture video data in three dimensions. The sensing range of the depth sensor is adjustable, and the software is capable of automatically calibrating the sensor based on the physical environment, accommodating the presence of obstacles and using infrared and depth cameras to capture a subject’s 3-D movements. The system doesn’t require bulky wearable components, “making it an ideal technology for the live operating room setting,” Dr. Catanzarite said. “In order to effectively assess surgical ergonomics, a less intrusive approach is needed, which can deliver precise reports on the body movements of the surgeons, as well as capturing the temporal distribution of different postures and limb angles.”
Dr. Catanzarite is using the system to launch an ergonomics assessment tool she calls Ergo-Kinect. The system will record surgeons’ movements in real time, gathering data about how they stand, move, and operate their instruments.
“Three-D interactive visualizations allow us to rotate and investigate specific motor activities from the collected data,” she said. The technology enables them to capture the movements of the surgeon and assign an ergonomic score for each movement. “Eventually we may be able to develop a system that can warn surgeons in real time if they are performing an activity which may be harmful from an ergonomics standpoint,” Dr. Catanzarite said.
The research is in its earliest phase – Dr. Catanzarite has only scanned a few surgeons. But she will continue to accrue data in order to eventually construct a system that could help surgeons of the future avoid the painful, and sometimes debilitating, physical costs of their career.
Dr. Catanzarite reported having no financial disclosures.
[email protected]
On Twitter @alz_gal
SAN DIEGO – Work-related musculoskeletal disorders are practically inevitable for surgeons, eventually occurring in more than 90%, no matter what type of surgery they practice.
At the annual clinical congress of the American College of Surgeons, this eyebrow-raising fact was presented with a sobering addendum: No one seems to be doing much about it.
“There are some ergonomic guidelines for surgeons out there, but most surgeons don’t know about them,” said Tatiana Catanzarite, MD, who has conducted research on this topic. When she began looking into the problem of work-related injuries among surgeons, she was surprised at the dearth of published research. It’s no wonder then, said Dr. Catanzarite and other panel members, that most surgeons learn proper work posture on the fly and may or may not be using the most efficient and mechanically sound instrumentation angles when performing surgery.
Dr. Catanzarite, a female pelvic medicine and reconstructive surgery fellow at the University of California, San Diego, has just published a literature review on surgeon ergonomics. But reading about how to stand, how to hold instruments, and even how to sit at a robotic surgical console is no match for having an observer on the ground guiding and reinforcing work posture, she said. Unfortunately, that’s an unrealistic expectation for most surgeons, so Dr. Catanzarite is borrowing video-gaming technology to address the situation, she said in an interview.
She has adapted a popular video game motion-capture system that uses an infrared laser projector and a computer sensor to capture video data in three dimensions. The sensing range of the depth sensor is adjustable, and the software is capable of automatically calibrating the sensor based on the physical environment, accommodating the presence of obstacles and using infrared and depth cameras to capture a subject’s 3-D movements. The system doesn’t require bulky wearable components, “making it an ideal technology for the live operating room setting,” Dr. Catanzarite said. “In order to effectively assess surgical ergonomics, a less intrusive approach is needed, which can deliver precise reports on the body movements of the surgeons, as well as capturing the temporal distribution of different postures and limb angles.”
Dr. Catanzarite is using the system to launch an ergonomics assessment tool she calls Ergo-Kinect. The system will record surgeons’ movements in real time, gathering data about how they stand, move, and operate their instruments.
“Three-D interactive visualizations allow us to rotate and investigate specific motor activities from the collected data,” she said. The technology enables them to capture the movements of the surgeon and assign an ergonomic score for each movement. “Eventually we may be able to develop a system that can warn surgeons in real time if they are performing an activity which may be harmful from an ergonomics standpoint,” Dr. Catanzarite said.
The research is in its earliest phase – Dr. Catanzarite has only scanned a few surgeons. But she will continue to accrue data in order to eventually construct a system that could help surgeons of the future avoid the painful, and sometimes debilitating, physical costs of their career.
Dr. Catanzarite reported having no financial disclosures.
[email protected]
On Twitter @alz_gal
SAN DIEGO – Work-related musculoskeletal disorders are practically inevitable for surgeons, eventually occurring in more than 90%, no matter what type of surgery they practice.
At the annual clinical congress of the American College of Surgeons, this eyebrow-raising fact was presented with a sobering addendum: No one seems to be doing much about it.
“There are some ergonomic guidelines for surgeons out there, but most surgeons don’t know about them,” said Tatiana Catanzarite, MD, who has conducted research on this topic. When she began looking into the problem of work-related injuries among surgeons, she was surprised at the dearth of published research. It’s no wonder then, said Dr. Catanzarite and other panel members, that most surgeons learn proper work posture on the fly and may or may not be using the most efficient and mechanically sound instrumentation angles when performing surgery.
Dr. Catanzarite, a female pelvic medicine and reconstructive surgery fellow at the University of California, San Diego, has just published a literature review on surgeon ergonomics. But reading about how to stand, how to hold instruments, and even how to sit at a robotic surgical console is no match for having an observer on the ground guiding and reinforcing work posture, she said. Unfortunately, that’s an unrealistic expectation for most surgeons, so Dr. Catanzarite is borrowing video-gaming technology to address the situation, she said in an interview.
She has adapted a popular video game motion-capture system that uses an infrared laser projector and a computer sensor to capture video data in three dimensions. The sensing range of the depth sensor is adjustable, and the software is capable of automatically calibrating the sensor based on the physical environment, accommodating the presence of obstacles and using infrared and depth cameras to capture a subject’s 3-D movements. The system doesn’t require bulky wearable components, “making it an ideal technology for the live operating room setting,” Dr. Catanzarite said. “In order to effectively assess surgical ergonomics, a less intrusive approach is needed, which can deliver precise reports on the body movements of the surgeons, as well as capturing the temporal distribution of different postures and limb angles.”
Dr. Catanzarite is using the system to launch an ergonomics assessment tool she calls Ergo-Kinect. The system will record surgeons’ movements in real time, gathering data about how they stand, move, and operate their instruments.
“Three-D interactive visualizations allow us to rotate and investigate specific motor activities from the collected data,” she said. The technology enables them to capture the movements of the surgeon and assign an ergonomic score for each movement. “Eventually we may be able to develop a system that can warn surgeons in real time if they are performing an activity which may be harmful from an ergonomics standpoint,” Dr. Catanzarite said.
The research is in its earliest phase – Dr. Catanzarite has only scanned a few surgeons. But she will continue to accrue data in order to eventually construct a system that could help surgeons of the future avoid the painful, and sometimes debilitating, physical costs of their career.
Dr. Catanzarite reported having no financial disclosures.
[email protected]
On Twitter @alz_gal
AT THE ACS CLINICAL CONGRESS
Pre-injury statin use found to benefit survival following TBI
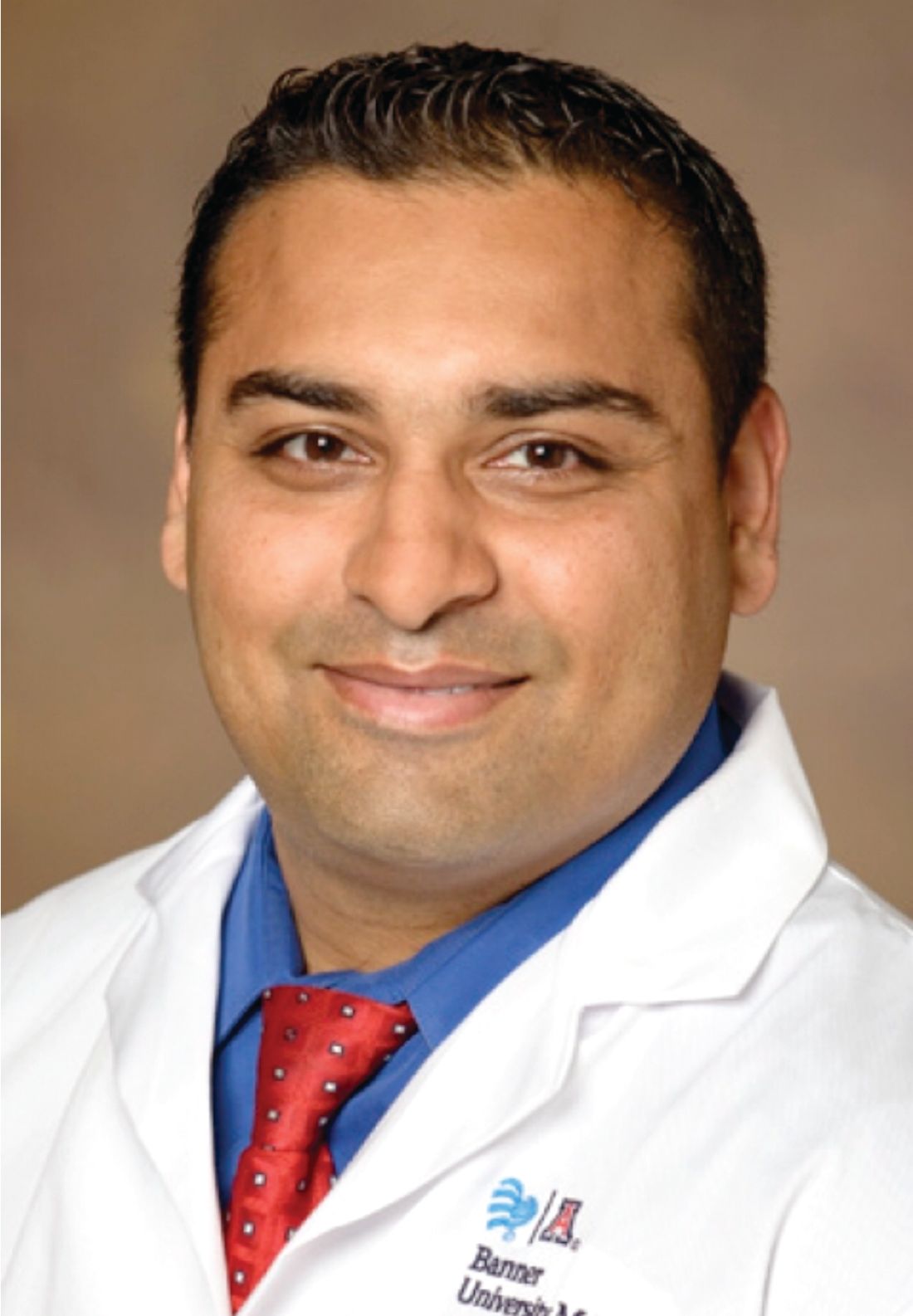
SAN DIEGO – Patients who were on statins prior to sustaining a traumatic brain injury doubled their survival rate over those who were not on the drugs in a retrospective analysis.
The study provides preliminary data that can help set a framework to conduct larger, randomized, controlled trials to further evaluate the role of statins, which have been shown in animal models to improve outcomes after traumatic brain injury (TBI).
In an effort to evaluate the effect of pre-injury statins on outcomes after TBI, Dr. Lokhandwala, a general surgery resident at the University of Arizona, Tucson, and his associates identified all patients aged 40 years and older from the Multiparameter Intelligent Monitoring in Intensive Care (MIMIC) III database with a diagnosis of TBI and ICU length of stay of greater than 24 hours. They divided patients into two groups: those who were on statins and those who were not. The primary outcome was in-hospital survival. Secondary outcomes measures were hospital length of stay and ICU length of stay.
Dr. Lokhandwala, who is also a commissioned officer with the U.S. Army Reserves, reported results from 918 patients with a TBI. Their mean age was 55 years, 76% were white, and 22% were on statins. The overall in-hospital survival rate was 78.6%, while the median Glasgow Coma Scale was 12. The median hospital length of stay and ICU length of stay were 9.1 and 7.2 days, respectively. The researchers observed that compared with patients who were not on statins, those on statin therapy had significantly higher rates of survival (88% vs. 68.4%; P less than .001). However, there was no difference in hospital or ICU length of stay between the two groups (P = .19 and P = .39, respectively). On regression analysis after controlling for confounding factors, statin use was found to be an independent predictor of survival (odds ratio, 1.8; 95% confidence interval, 1.5-2.2; P less than .001).
“Even though we isolated our patients to TBI, there could have been other causes of their mortality, like a pulmonary embolism or a myocardial infarction,” Dr. Lokhandwala said. “We need to conduct a randomized, controlled trial to follow these individuals and see what their actual mortality is and look at their psychosocial outcomes to see if there’s a long-term benefit to statins. Do these people have decreased incidence of PTSD or are they more functional? Is it easier for them to hold a job or develop social relationships? The impact of post-injury statin use could also be studied.”
He went on to note that many studies have shown that aggressive team-based rehabilitation can improve outcomes in TBI patients. “Would we be able to include statin use in such a program to see if statins further improve outcomes faster or are there individuals that don’t benefit as much?” Dr. Lokhandwala asked. “This study sets up a framework to show that there is a strong association, and take this further in a more structured trial to see if there is any potential for therapeutic use in TBI.”
Dr. Lokhandwala reported having no financial disclosures.
SAN DIEGO – Patients who were on statins prior to sustaining a traumatic brain injury doubled their survival rate over those who were not on the drugs in a retrospective analysis.
The study provides preliminary data that can help set a framework to conduct larger, randomized, controlled trials to further evaluate the role of statins, which have been shown in animal models to improve outcomes after traumatic brain injury (TBI).
In an effort to evaluate the effect of pre-injury statins on outcomes after TBI, Dr. Lokhandwala, a general surgery resident at the University of Arizona, Tucson, and his associates identified all patients aged 40 years and older from the Multiparameter Intelligent Monitoring in Intensive Care (MIMIC) III database with a diagnosis of TBI and ICU length of stay of greater than 24 hours. They divided patients into two groups: those who were on statins and those who were not. The primary outcome was in-hospital survival. Secondary outcomes measures were hospital length of stay and ICU length of stay.
Dr. Lokhandwala, who is also a commissioned officer with the U.S. Army Reserves, reported results from 918 patients with a TBI. Their mean age was 55 years, 76% were white, and 22% were on statins. The overall in-hospital survival rate was 78.6%, while the median Glasgow Coma Scale was 12. The median hospital length of stay and ICU length of stay were 9.1 and 7.2 days, respectively. The researchers observed that compared with patients who were not on statins, those on statin therapy had significantly higher rates of survival (88% vs. 68.4%; P less than .001). However, there was no difference in hospital or ICU length of stay between the two groups (P = .19 and P = .39, respectively). On regression analysis after controlling for confounding factors, statin use was found to be an independent predictor of survival (odds ratio, 1.8; 95% confidence interval, 1.5-2.2; P less than .001).
“Even though we isolated our patients to TBI, there could have been other causes of their mortality, like a pulmonary embolism or a myocardial infarction,” Dr. Lokhandwala said. “We need to conduct a randomized, controlled trial to follow these individuals and see what their actual mortality is and look at their psychosocial outcomes to see if there’s a long-term benefit to statins. Do these people have decreased incidence of PTSD or are they more functional? Is it easier for them to hold a job or develop social relationships? The impact of post-injury statin use could also be studied.”
He went on to note that many studies have shown that aggressive team-based rehabilitation can improve outcomes in TBI patients. “Would we be able to include statin use in such a program to see if statins further improve outcomes faster or are there individuals that don’t benefit as much?” Dr. Lokhandwala asked. “This study sets up a framework to show that there is a strong association, and take this further in a more structured trial to see if there is any potential for therapeutic use in TBI.”
Dr. Lokhandwala reported having no financial disclosures.
SAN DIEGO – Patients who were on statins prior to sustaining a traumatic brain injury doubled their survival rate over those who were not on the drugs in a retrospective analysis.
The study provides preliminary data that can help set a framework to conduct larger, randomized, controlled trials to further evaluate the role of statins, which have been shown in animal models to improve outcomes after traumatic brain injury (TBI).
In an effort to evaluate the effect of pre-injury statins on outcomes after TBI, Dr. Lokhandwala, a general surgery resident at the University of Arizona, Tucson, and his associates identified all patients aged 40 years and older from the Multiparameter Intelligent Monitoring in Intensive Care (MIMIC) III database with a diagnosis of TBI and ICU length of stay of greater than 24 hours. They divided patients into two groups: those who were on statins and those who were not. The primary outcome was in-hospital survival. Secondary outcomes measures were hospital length of stay and ICU length of stay.
Dr. Lokhandwala, who is also a commissioned officer with the U.S. Army Reserves, reported results from 918 patients with a TBI. Their mean age was 55 years, 76% were white, and 22% were on statins. The overall in-hospital survival rate was 78.6%, while the median Glasgow Coma Scale was 12. The median hospital length of stay and ICU length of stay were 9.1 and 7.2 days, respectively. The researchers observed that compared with patients who were not on statins, those on statin therapy had significantly higher rates of survival (88% vs. 68.4%; P less than .001). However, there was no difference in hospital or ICU length of stay between the two groups (P = .19 and P = .39, respectively). On regression analysis after controlling for confounding factors, statin use was found to be an independent predictor of survival (odds ratio, 1.8; 95% confidence interval, 1.5-2.2; P less than .001).
“Even though we isolated our patients to TBI, there could have been other causes of their mortality, like a pulmonary embolism or a myocardial infarction,” Dr. Lokhandwala said. “We need to conduct a randomized, controlled trial to follow these individuals and see what their actual mortality is and look at their psychosocial outcomes to see if there’s a long-term benefit to statins. Do these people have decreased incidence of PTSD or are they more functional? Is it easier for them to hold a job or develop social relationships? The impact of post-injury statin use could also be studied.”
He went on to note that many studies have shown that aggressive team-based rehabilitation can improve outcomes in TBI patients. “Would we be able to include statin use in such a program to see if statins further improve outcomes faster or are there individuals that don’t benefit as much?” Dr. Lokhandwala asked. “This study sets up a framework to show that there is a strong association, and take this further in a more structured trial to see if there is any potential for therapeutic use in TBI.”
Dr. Lokhandwala reported having no financial disclosures.
AT THE ACS CLINICAL CONGRESS
Key clinical point:
Major finding: After controlling for confounding factors, statin use was found to be an independent predictor of survival following traumatic brain injury (OR, 1.8; 95% CI, 1.5-2.2; P less than .001).
Study details: A retrospective analysis of 918 patients who sustained a TBI.
Disclosures: Dr. Lokhandwala reported having no financial disclosures.
Antibiotic exposure blunted metabolic improvement following vertical sleeve gastrectomy
SAN DIEGO – results from a mouse study demonstrated.
The finding raises the question of whether patients with suboptimal outcomes following vertical sleeve gastrectomy may benefit from microbial modulation.
According to Dr. Jahansouz of the University of Minnesota Microbiota Transplantation Program, mechanisms mediating metabolic improvement following bariatric surgery remain incompletely understood. “Outcomes are also somewhat variable: As many as 40%-75% of patients regain weight in the years following nadir of weight loss,” he said. “Human studies have shown an acute and sustained shift in the gut microbiota, and an altered bile acid profile. Bile acids increase following surgery.”
Meanwhile, mice deficient in Farnesoid X-receptor (FXR) and Takeda G protein–coupled Receptor 5 (TGR5) do not experience metabolic improvement following bariatric surgery; the composition of the microbiome can significantly impact the composition of bile acids.
“By altering the postsurgical composition of mice following bariatric surgery, we eliminate the metabolic benefits of surgery, possibly by altering bile acid profiles,” Dr. Jahansouz said.
For the trial, diet-induced obese mice were randomized to vertical sleeve gastrectomy (VSG) or sham surgery, with or without exposure to antibiotics that selectively suppress mainly gram-positive (fidaxomicin, streptomycin) or gram-negative (ceftriaxone) bacteria on postoperative days 1-4. The researchers characterized fecal microbiota before surgery and on postoperative days 7 and 28. Mice were metabolically characterized on postoperative days 30-32 and euthanized on postoperative day 35.
Mice in the VSG group experienced weight loss and shifts in the intestinal microbiota composition, compared with those in the sham surgery group.
“Antibiotic exposure resulted in sustained reductions in alpha (within sample) diversity of microbiota and shifts in its composition,” the researchers wrote in their abstract. “Different antimicrobial specificity of antibiotics led to functionally distinct physiologic effects. Specifically, fidaxomicin and streptomycin markedly altered hepatic bile acid signaling and lipid metabolism, while ceftriaxone resulted in greater reduction in the expression of key antimicrobial peptides.
“However, VSG mice exposed to antibiotics, regardless of their specificity, had significantly increased subcutaneous adiposity and impaired glucose homeostasis without changes in food intake, relative to control mice,” the investigators noted.
Dr. Jahansouz said that he was surprised by the fact that all three antibiotics tested, no matter their specificity in gut bacteria eliminated, resulted in significantly diminished weight loss and metabolic improvement following vertical sleeve gastrectomy in the mouse model. He acknowledged that translating the findings from mice to humans is a key limitation of the analysis.
“There are fundamental physiologic differences between mice and humans that need consideration in all murine models of metabolic disorders,” he said. “Therefore, it is critical that insights gained from these models are followed up in human studies.”
The study was funded by the American Diabetes Association and a Minnesota Discovery, Research and InnoVation Economy grant from the University of Minnesota. Dr. Jahansouz reported having no financial disclosures.
SAN DIEGO – results from a mouse study demonstrated.
The finding raises the question of whether patients with suboptimal outcomes following vertical sleeve gastrectomy may benefit from microbial modulation.
According to Dr. Jahansouz of the University of Minnesota Microbiota Transplantation Program, mechanisms mediating metabolic improvement following bariatric surgery remain incompletely understood. “Outcomes are also somewhat variable: As many as 40%-75% of patients regain weight in the years following nadir of weight loss,” he said. “Human studies have shown an acute and sustained shift in the gut microbiota, and an altered bile acid profile. Bile acids increase following surgery.”
Meanwhile, mice deficient in Farnesoid X-receptor (FXR) and Takeda G protein–coupled Receptor 5 (TGR5) do not experience metabolic improvement following bariatric surgery; the composition of the microbiome can significantly impact the composition of bile acids.
“By altering the postsurgical composition of mice following bariatric surgery, we eliminate the metabolic benefits of surgery, possibly by altering bile acid profiles,” Dr. Jahansouz said.
For the trial, diet-induced obese mice were randomized to vertical sleeve gastrectomy (VSG) or sham surgery, with or without exposure to antibiotics that selectively suppress mainly gram-positive (fidaxomicin, streptomycin) or gram-negative (ceftriaxone) bacteria on postoperative days 1-4. The researchers characterized fecal microbiota before surgery and on postoperative days 7 and 28. Mice were metabolically characterized on postoperative days 30-32 and euthanized on postoperative day 35.
Mice in the VSG group experienced weight loss and shifts in the intestinal microbiota composition, compared with those in the sham surgery group.
“Antibiotic exposure resulted in sustained reductions in alpha (within sample) diversity of microbiota and shifts in its composition,” the researchers wrote in their abstract. “Different antimicrobial specificity of antibiotics led to functionally distinct physiologic effects. Specifically, fidaxomicin and streptomycin markedly altered hepatic bile acid signaling and lipid metabolism, while ceftriaxone resulted in greater reduction in the expression of key antimicrobial peptides.
“However, VSG mice exposed to antibiotics, regardless of their specificity, had significantly increased subcutaneous adiposity and impaired glucose homeostasis without changes in food intake, relative to control mice,” the investigators noted.
Dr. Jahansouz said that he was surprised by the fact that all three antibiotics tested, no matter their specificity in gut bacteria eliminated, resulted in significantly diminished weight loss and metabolic improvement following vertical sleeve gastrectomy in the mouse model. He acknowledged that translating the findings from mice to humans is a key limitation of the analysis.
“There are fundamental physiologic differences between mice and humans that need consideration in all murine models of metabolic disorders,” he said. “Therefore, it is critical that insights gained from these models are followed up in human studies.”
The study was funded by the American Diabetes Association and a Minnesota Discovery, Research and InnoVation Economy grant from the University of Minnesota. Dr. Jahansouz reported having no financial disclosures.
SAN DIEGO – results from a mouse study demonstrated.
The finding raises the question of whether patients with suboptimal outcomes following vertical sleeve gastrectomy may benefit from microbial modulation.
According to Dr. Jahansouz of the University of Minnesota Microbiota Transplantation Program, mechanisms mediating metabolic improvement following bariatric surgery remain incompletely understood. “Outcomes are also somewhat variable: As many as 40%-75% of patients regain weight in the years following nadir of weight loss,” he said. “Human studies have shown an acute and sustained shift in the gut microbiota, and an altered bile acid profile. Bile acids increase following surgery.”
Meanwhile, mice deficient in Farnesoid X-receptor (FXR) and Takeda G protein–coupled Receptor 5 (TGR5) do not experience metabolic improvement following bariatric surgery; the composition of the microbiome can significantly impact the composition of bile acids.
“By altering the postsurgical composition of mice following bariatric surgery, we eliminate the metabolic benefits of surgery, possibly by altering bile acid profiles,” Dr. Jahansouz said.
For the trial, diet-induced obese mice were randomized to vertical sleeve gastrectomy (VSG) or sham surgery, with or without exposure to antibiotics that selectively suppress mainly gram-positive (fidaxomicin, streptomycin) or gram-negative (ceftriaxone) bacteria on postoperative days 1-4. The researchers characterized fecal microbiota before surgery and on postoperative days 7 and 28. Mice were metabolically characterized on postoperative days 30-32 and euthanized on postoperative day 35.
Mice in the VSG group experienced weight loss and shifts in the intestinal microbiota composition, compared with those in the sham surgery group.
“Antibiotic exposure resulted in sustained reductions in alpha (within sample) diversity of microbiota and shifts in its composition,” the researchers wrote in their abstract. “Different antimicrobial specificity of antibiotics led to functionally distinct physiologic effects. Specifically, fidaxomicin and streptomycin markedly altered hepatic bile acid signaling and lipid metabolism, while ceftriaxone resulted in greater reduction in the expression of key antimicrobial peptides.
“However, VSG mice exposed to antibiotics, regardless of their specificity, had significantly increased subcutaneous adiposity and impaired glucose homeostasis without changes in food intake, relative to control mice,” the investigators noted.
Dr. Jahansouz said that he was surprised by the fact that all three antibiotics tested, no matter their specificity in gut bacteria eliminated, resulted in significantly diminished weight loss and metabolic improvement following vertical sleeve gastrectomy in the mouse model. He acknowledged that translating the findings from mice to humans is a key limitation of the analysis.
“There are fundamental physiologic differences between mice and humans that need consideration in all murine models of metabolic disorders,” he said. “Therefore, it is critical that insights gained from these models are followed up in human studies.”
The study was funded by the American Diabetes Association and a Minnesota Discovery, Research and InnoVation Economy grant from the University of Minnesota. Dr. Jahansouz reported having no financial disclosures.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Postsurgical disruption of intestinal microbiota composition attenuates the metabolic efficacy of vertical sleeve gastrectomy.
Major finding: VSG mice exposed to antibiotics had significantly increased subcutaneous adiposity and impaired glucose homeostasis without changes in food intake, compared with control mice.
Study details: A study of diet-induced obese mice that were randomized to VSG or sham surgery, with or without exposure to antibiotics.
Disclosures: The study was funded by the American Diabetes Association and a Minnesota Discovery, Research and InnoVation Economy grant from the University of Minnesota. Dr. Jahansouz reported having no financial disclosures.
VIDEO: How to manage surgical pain in opioid addiction treatment
NEW ORLEANS – How do you manage surgical pain when someone is in treatment for opioid addiction? And how do you manage chronic pain?
It is possible to give patients opioids for post-op pain without increasing the risk of relapse, according to Margaret Chaplin, MD, a staff psychiatrist at Community Mental Health Affiliates in New Britain, Conn.
Dr. Chaplin generally uses buprenorphine and naloxone (Suboxone) for opioid use disorder, and she likes to keep her patients on it for surgery. That often means, however, talking with skeptical surgeons and anesthesiologists beforehand, and reminding them that buprenorphine itself has analgesic effects. Meanwhile, when her patients have chronic pain, sometimes they need help understanding that aspirin and acetaminophen help, even if they don’t give patients a warm, fuzzy feeling.
Dr. Chaplin shared those tips and more about pain management in opioid addiction in an interview at the American Psychiatric Association’s Institute on Psychiatric Services.
NEW ORLEANS – How do you manage surgical pain when someone is in treatment for opioid addiction? And how do you manage chronic pain?
It is possible to give patients opioids for post-op pain without increasing the risk of relapse, according to Margaret Chaplin, MD, a staff psychiatrist at Community Mental Health Affiliates in New Britain, Conn.
Dr. Chaplin generally uses buprenorphine and naloxone (Suboxone) for opioid use disorder, and she likes to keep her patients on it for surgery. That often means, however, talking with skeptical surgeons and anesthesiologists beforehand, and reminding them that buprenorphine itself has analgesic effects. Meanwhile, when her patients have chronic pain, sometimes they need help understanding that aspirin and acetaminophen help, even if they don’t give patients a warm, fuzzy feeling.
Dr. Chaplin shared those tips and more about pain management in opioid addiction in an interview at the American Psychiatric Association’s Institute on Psychiatric Services.
NEW ORLEANS – How do you manage surgical pain when someone is in treatment for opioid addiction? And how do you manage chronic pain?
It is possible to give patients opioids for post-op pain without increasing the risk of relapse, according to Margaret Chaplin, MD, a staff psychiatrist at Community Mental Health Affiliates in New Britain, Conn.
Dr. Chaplin generally uses buprenorphine and naloxone (Suboxone) for opioid use disorder, and she likes to keep her patients on it for surgery. That often means, however, talking with skeptical surgeons and anesthesiologists beforehand, and reminding them that buprenorphine itself has analgesic effects. Meanwhile, when her patients have chronic pain, sometimes they need help understanding that aspirin and acetaminophen help, even if they don’t give patients a warm, fuzzy feeling.
Dr. Chaplin shared those tips and more about pain management in opioid addiction in an interview at the American Psychiatric Association’s Institute on Psychiatric Services.
AT IPS 2017