User login
Official Newspaper of the American College of Surgeons
Obamacare enrollment numbers wanted: The Policy & Practice Podcast
Everyone wants to know. How many people have enrolled in health plans through the federal exchange? Health and Human Services Secretary Kathleen Sebelius says the first numbers will be out this week. But neither she, nor other HHS officials will divulge any further details.
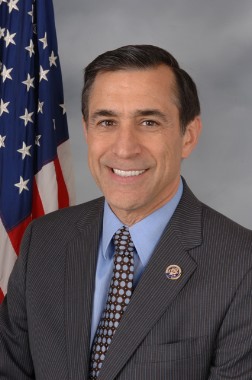
And Republicans want those details. House Oversight and Government Reform Committee Chairman Darrell Issa (R-Calif.) says he has confidential notes from inside HHS that show that only 6 people had enrolled by the second day of the exchange’s operation. He subpoenaed Secretary Sebelius, demanding more information on healthcare.gov’s problems, testing of the website, and the number of enrollees – all by Nov. 13.
House Ways and Means Committee Chairman Dave Camp (R-Mich.) also subpoenaed the Secretary, seeking much of the same information.
Meanwhile, the healthcare.gov website continues to suffer technical problems, which may be keeping people from signing up. Millions of Americans – at least 1 million in California alone – have received cancellation notices from their insurers. These are largely people who have policies in the individual market. HHS has said that those policies are generally expensive and don’t offer as many benefits as are required by the Affordable Care Act. But people are now being forced to look for new coverage at a time when it’s hard to shop on the federal exchange.
The situation led President Obama to apologize in an interview with NBC News. Even with that, some in Congress want to rewrite the ACA to let the individual policies continue. Sen. Mary Landrieu (D-La.) and Sen. Joe Manchin (D-W.Va.) introduced such a proposal, as did Sen. Ron Johnson (R-Wis.). Rep. Fred Upton (R-Mich.) has put forward the Keep Your Health Plan Act in the House, which may see a vote as early as this week.
For all that and more, have a listen to our podcast.
On Twitter @aliciaault
Everyone wants to know. How many people have enrolled in health plans through the federal exchange? Health and Human Services Secretary Kathleen Sebelius says the first numbers will be out this week. But neither she, nor other HHS officials will divulge any further details.
And Republicans want those details. House Oversight and Government Reform Committee Chairman Darrell Issa (R-Calif.) says he has confidential notes from inside HHS that show that only 6 people had enrolled by the second day of the exchange’s operation. He subpoenaed Secretary Sebelius, demanding more information on healthcare.gov’s problems, testing of the website, and the number of enrollees – all by Nov. 13.
House Ways and Means Committee Chairman Dave Camp (R-Mich.) also subpoenaed the Secretary, seeking much of the same information.
Meanwhile, the healthcare.gov website continues to suffer technical problems, which may be keeping people from signing up. Millions of Americans – at least 1 million in California alone – have received cancellation notices from their insurers. These are largely people who have policies in the individual market. HHS has said that those policies are generally expensive and don’t offer as many benefits as are required by the Affordable Care Act. But people are now being forced to look for new coverage at a time when it’s hard to shop on the federal exchange.
The situation led President Obama to apologize in an interview with NBC News. Even with that, some in Congress want to rewrite the ACA to let the individual policies continue. Sen. Mary Landrieu (D-La.) and Sen. Joe Manchin (D-W.Va.) introduced such a proposal, as did Sen. Ron Johnson (R-Wis.). Rep. Fred Upton (R-Mich.) has put forward the Keep Your Health Plan Act in the House, which may see a vote as early as this week.
For all that and more, have a listen to our podcast.
On Twitter @aliciaault
Everyone wants to know. How many people have enrolled in health plans through the federal exchange? Health and Human Services Secretary Kathleen Sebelius says the first numbers will be out this week. But neither she, nor other HHS officials will divulge any further details.
And Republicans want those details. House Oversight and Government Reform Committee Chairman Darrell Issa (R-Calif.) says he has confidential notes from inside HHS that show that only 6 people had enrolled by the second day of the exchange’s operation. He subpoenaed Secretary Sebelius, demanding more information on healthcare.gov’s problems, testing of the website, and the number of enrollees – all by Nov. 13.
House Ways and Means Committee Chairman Dave Camp (R-Mich.) also subpoenaed the Secretary, seeking much of the same information.
Meanwhile, the healthcare.gov website continues to suffer technical problems, which may be keeping people from signing up. Millions of Americans – at least 1 million in California alone – have received cancellation notices from their insurers. These are largely people who have policies in the individual market. HHS has said that those policies are generally expensive and don’t offer as many benefits as are required by the Affordable Care Act. But people are now being forced to look for new coverage at a time when it’s hard to shop on the federal exchange.
The situation led President Obama to apologize in an interview with NBC News. Even with that, some in Congress want to rewrite the ACA to let the individual policies continue. Sen. Mary Landrieu (D-La.) and Sen. Joe Manchin (D-W.Va.) introduced such a proposal, as did Sen. Ron Johnson (R-Wis.). Rep. Fred Upton (R-Mich.) has put forward the Keep Your Health Plan Act in the House, which may see a vote as early as this week.
For all that and more, have a listen to our podcast.
On Twitter @aliciaault
Inadequate neuromuscular blockade common during surgery
SAN FRANCISCO – Patients under general anesthesia may be getting insufficient neuromuscular blockade in 1%-45% of operations, depending on the definition, according to several studies presented in a joint session at the annual meeting of the American Society of Anesthesiologists.
Regardless of the exact definition, the findings suggest that the problem of insufficient blockade is considerably more common than expected, the anesthesiologists in attendance agreed.
A lack of clinical guidelines for neuromuscular blockade probably contributes to the problem, some speakers suggested. There is no established definition of insufficient neuromuscular blockade, which has been associated in prior studies with compromised surgical visualization, impaired ventilation leading to barotraumas, direct injury through unexpected movement, and other complications.
Investigators presented their results in posters and in a joint discussion session at the meeting. All studies were sponsored by Merck, which markets a neuromuscular blocking agent (rocuronium bromide, or Zemuron) and is seeking U.S. approval for a drug that rapidly reverses neuromuscular blockade (sugammadex, or Bridion).
One percent of 129,209 adults who underwent general anesthesia and received a nondepolarizing neuromuscular blockade agent in 2005-2013 experienced insufficient blockade in a way that interrupted surgery, either through undesired patient movement (0.3%) or an explicit request from the surgeon for additional muscle relaxation and administration of more neuromuscular blockade (0.7%), Dr. Timur Dubovoy and his associates reported.
They also found indirect evidence of insufficient neuromuscular blockade through two other criteria that were much more common, said Dr. Dubovoy of the University of Michigan, Ann Arbor. Anesthesiologists gave more neuromuscular blockade after documenting twitches on peripheral nerve stimulation (train-of-four monitoring) in 39% of patients, indicative of unintended recovery from neuromuscular blockade. Large or even "excessive" maintenance doses were given to 45% of patients, consistent with insufficient neuromuscular blockade, he said.
Those kinds of events typically don’t interrupt a procedure but can lead to residual neuromuscular blockade due to excessive dosing, potentially increasing complications and delaying recovery after anesthesia. The study looked only at the incidence of insufficient neuromuscular blockade, however, not outcomes.
"Current use of nondepolarizing neuromuscular blockade agents and subjective tactile train-of-four monitoring frequently exposes patients to inadequate neuromuscular blockade," Dr. Dubovoy said.
In a separate study, insufficient neuromuscular blockade affected 21%-28% of 48,315 adults undergoing abdominal, laparoscopic, and interventional neurovascular procedures at the Cleveland Clinic in 2005-2013, Dr. Brian D. Hesler and his associates reported.
"Our results suggest that insufficient block is relatively common, even in operations that are generally thought to require muscle relaxation," said Dr. Hesler of the Cleveland Clinic. "It is difficult to separate inadequate anesthesia from inadequate neuromuscular block, and both probably contributed in many cases."
He and his associates formed a panel of seven experienced anesthesiologists to identify anesthesiology actions that are indicative of episodes of insufficient neuromuscular block and searched for those criteria in patient records, with a three-person adjudication committee approving the search criteria through a random sample of at least 50 charts for each criterion.
Overall, 28% of operations had evidence of insufficient neuromuscular blockade, or 21% if the investigators excluded cases identified solely by electromyogram criteria.
In a separate analysis of the same cohort, Dr. Hesler and his associates searched for comments in the anesthetic records and found that insufficient blockade usually was identified more than 30 minutes before emergence, defined as the time when maintenance anesthesia was discontinued (106 cases), but 18% of the time it occurred 15-30 minutes before emergence (9 cases) or less than 15 minutes before emergence (14 cases).
The closer to the end of surgery, the more likely the anesthesiologist was to respond by deepening anesthesia instead of redosing the neuromuscular blocking agent, with other sedatives (opioids) used at a consistent rate in each time period.
A separate prospective, observational study of 448 patients undergoing elective laparoscopic or open abdominal surgical procedures at eight Canadian centers in 2011-2012 stratified residual neuromuscular blockade by train-of-four (TOF) ratios.
Lower TOF ratios at tracheal extubation and at arrival in the postanesthesia care unit (PACU) were associated with greater risk for complications and greater use of perioperative resources, Dr. Dolores McKeen and her associates reported.
Every 0.1-increment increase in the TOF ratio at tracheal extubation was associated with a 30% reduction in the odds of needing placement of an oral or nasal airway due to upper airway obstruction from the time of patient extubation to PACU discharge. Each 0.1-increment increase in the TOF ratio at tracheal extubation also was associated with 3% fewer bed visits by nurses, said Dr. McKeen of Dalhousie University, Halifax, N.S. Similar results were seen for TOF ratios upon arrival at the PACU.
This suggests that "more effective strategies to prevent and/or manage residual neuromuscular blockade are required to minimize the impact on the patient and health care provider," she said.
The incidence of postoperative residual neuromuscular blockade was 19% for patients with a TOF ratio less than 0.6 at tracheal extubation, 12% with a ratio of 0.6-0.7, 9% with a ratio of 0.7-0.8, 16% with a ratio of 0.8-0.9, and 44% with a ratio of 0.9 or greater. The incidence of residual blockade was 8% for patients with a TOF ratio less than 0.6 upon arrival to the PACU, 7% with a ratio of 0.6-0.7, 14% with a ratio of 0.7-0.8, 16% with a ratio of 0.8-0.9, and 56% with a ratio of 0.9 or greater.
In the United States, neostigmine, an acetylcholinesterase inhibitor, is the most common means of reversing neuromuscular blocking agents, according to Scott Devine, Ph.D., of Merck. Giving neostigmine too early can be ineffective, and giving it too late might induce skeletal muscle weakness.
He and his associates analyzed data from the Anesthesia Quality Institute’s National Anesthesia Clinical Outcomes Registry (NACOR) on 113,276 procedures utilizing rocuronium or vecuronium that were reversed with neostigmine in 2010-2012. The reversal agent was given a mean of 63 minutes after the last dose of a neuromuscular blocking agent, 7 minutes before surgical site closure, 14 minutes prior to emergence, and 29 minutes before the end of anesthesia time, though each administration time had a wide range, he reported.
A substantial number of patients would have spontaneously recovered from the effects of the neuromuscular blockers after 63 minutes, suggesting that neostigmine often may be given later than needed, he said. If neostigmine is given 7 minutes before surgical site closure, reversal of neuromuscular blockade could be well underway, resulting in increased muscle tension during surgical site closure, which could increase the risk of complications such as dehiscence or postsurgical hernias, he added.
The large variability in practice may be due to multiple factors and deserves further research, he said.
Merck, which markets a neuromuscular blockade agent, sponsored the studies and supplied at least one investigator for each study.
[email protected] On Twitter @sherryboschert
One part of what we anesthesiologists do, other than keeping patients asleep and pain free, is to have them in a condition so that surgeons can do their operations optimally. If patients are not relaxed, and if muscles are not relaxed, that makes the surgical conditions more difficult, which could potentially lead to longer duration of surgery, more complications, and things like that. So this topic is actually very important to surgeons.

|
|
In these studies, the neuromuscular blockade frequently seems to be insufficient, which is a little bit of a surprise. We hear from our surgery colleagues fairly often during surgery, "Give more muscle relaxants," because they have their hands in the field and they feel what’s going on. But anesthesiologists haven’t always agreed that it’s necessary to give more muscle relaxants, because we thought surgeons overestimated the conditions. It does seem that insufficient muscle relaxation is much more common than we had thought.
Many of these studies come from the Cleveland Clinic, so we’ve gone through their data in detail. We probably will be a little bit more liberal with muscle relaxation, which is difficult. If you overrelax patients, then it takes us longer to extubate them, which means we don’t get out of the OR before the surgeon comes to start the next case. So it’s a give and take.
That’s why to a certain extent it’s important that there are drugs available that promptly, within seconds, reverse our muscle relaxants. But they are not available in the United States yet. We are still waiting. Europe, South America – everybody is already using them.
It’s important for anesthesia and surgery to work together and see whether any of this actually does improve intermediate- or long-term outcomes of patients. That’s ultimately the goal.
Dr. Andrea Kurz is a professor and vice-chair of the Anesthesiology Institute at the Cleveland Clinic. She gave these remarks in an interview. Dr. Kurz reported having no financial disclosures.
One part of what we anesthesiologists do, other than keeping patients asleep and pain free, is to have them in a condition so that surgeons can do their operations optimally. If patients are not relaxed, and if muscles are not relaxed, that makes the surgical conditions more difficult, which could potentially lead to longer duration of surgery, more complications, and things like that. So this topic is actually very important to surgeons.

|
|
In these studies, the neuromuscular blockade frequently seems to be insufficient, which is a little bit of a surprise. We hear from our surgery colleagues fairly often during surgery, "Give more muscle relaxants," because they have their hands in the field and they feel what’s going on. But anesthesiologists haven’t always agreed that it’s necessary to give more muscle relaxants, because we thought surgeons overestimated the conditions. It does seem that insufficient muscle relaxation is much more common than we had thought.
Many of these studies come from the Cleveland Clinic, so we’ve gone through their data in detail. We probably will be a little bit more liberal with muscle relaxation, which is difficult. If you overrelax patients, then it takes us longer to extubate them, which means we don’t get out of the OR before the surgeon comes to start the next case. So it’s a give and take.
That’s why to a certain extent it’s important that there are drugs available that promptly, within seconds, reverse our muscle relaxants. But they are not available in the United States yet. We are still waiting. Europe, South America – everybody is already using them.
It’s important for anesthesia and surgery to work together and see whether any of this actually does improve intermediate- or long-term outcomes of patients. That’s ultimately the goal.
Dr. Andrea Kurz is a professor and vice-chair of the Anesthesiology Institute at the Cleveland Clinic. She gave these remarks in an interview. Dr. Kurz reported having no financial disclosures.
One part of what we anesthesiologists do, other than keeping patients asleep and pain free, is to have them in a condition so that surgeons can do their operations optimally. If patients are not relaxed, and if muscles are not relaxed, that makes the surgical conditions more difficult, which could potentially lead to longer duration of surgery, more complications, and things like that. So this topic is actually very important to surgeons.

|
|
In these studies, the neuromuscular blockade frequently seems to be insufficient, which is a little bit of a surprise. We hear from our surgery colleagues fairly often during surgery, "Give more muscle relaxants," because they have their hands in the field and they feel what’s going on. But anesthesiologists haven’t always agreed that it’s necessary to give more muscle relaxants, because we thought surgeons overestimated the conditions. It does seem that insufficient muscle relaxation is much more common than we had thought.
Many of these studies come from the Cleveland Clinic, so we’ve gone through their data in detail. We probably will be a little bit more liberal with muscle relaxation, which is difficult. If you overrelax patients, then it takes us longer to extubate them, which means we don’t get out of the OR before the surgeon comes to start the next case. So it’s a give and take.
That’s why to a certain extent it’s important that there are drugs available that promptly, within seconds, reverse our muscle relaxants. But they are not available in the United States yet. We are still waiting. Europe, South America – everybody is already using them.
It’s important for anesthesia and surgery to work together and see whether any of this actually does improve intermediate- or long-term outcomes of patients. That’s ultimately the goal.
Dr. Andrea Kurz is a professor and vice-chair of the Anesthesiology Institute at the Cleveland Clinic. She gave these remarks in an interview. Dr. Kurz reported having no financial disclosures.
SAN FRANCISCO – Patients under general anesthesia may be getting insufficient neuromuscular blockade in 1%-45% of operations, depending on the definition, according to several studies presented in a joint session at the annual meeting of the American Society of Anesthesiologists.
Regardless of the exact definition, the findings suggest that the problem of insufficient blockade is considerably more common than expected, the anesthesiologists in attendance agreed.
A lack of clinical guidelines for neuromuscular blockade probably contributes to the problem, some speakers suggested. There is no established definition of insufficient neuromuscular blockade, which has been associated in prior studies with compromised surgical visualization, impaired ventilation leading to barotraumas, direct injury through unexpected movement, and other complications.
Investigators presented their results in posters and in a joint discussion session at the meeting. All studies were sponsored by Merck, which markets a neuromuscular blocking agent (rocuronium bromide, or Zemuron) and is seeking U.S. approval for a drug that rapidly reverses neuromuscular blockade (sugammadex, or Bridion).
One percent of 129,209 adults who underwent general anesthesia and received a nondepolarizing neuromuscular blockade agent in 2005-2013 experienced insufficient blockade in a way that interrupted surgery, either through undesired patient movement (0.3%) or an explicit request from the surgeon for additional muscle relaxation and administration of more neuromuscular blockade (0.7%), Dr. Timur Dubovoy and his associates reported.
They also found indirect evidence of insufficient neuromuscular blockade through two other criteria that were much more common, said Dr. Dubovoy of the University of Michigan, Ann Arbor. Anesthesiologists gave more neuromuscular blockade after documenting twitches on peripheral nerve stimulation (train-of-four monitoring) in 39% of patients, indicative of unintended recovery from neuromuscular blockade. Large or even "excessive" maintenance doses were given to 45% of patients, consistent with insufficient neuromuscular blockade, he said.
Those kinds of events typically don’t interrupt a procedure but can lead to residual neuromuscular blockade due to excessive dosing, potentially increasing complications and delaying recovery after anesthesia. The study looked only at the incidence of insufficient neuromuscular blockade, however, not outcomes.
"Current use of nondepolarizing neuromuscular blockade agents and subjective tactile train-of-four monitoring frequently exposes patients to inadequate neuromuscular blockade," Dr. Dubovoy said.
In a separate study, insufficient neuromuscular blockade affected 21%-28% of 48,315 adults undergoing abdominal, laparoscopic, and interventional neurovascular procedures at the Cleveland Clinic in 2005-2013, Dr. Brian D. Hesler and his associates reported.
"Our results suggest that insufficient block is relatively common, even in operations that are generally thought to require muscle relaxation," said Dr. Hesler of the Cleveland Clinic. "It is difficult to separate inadequate anesthesia from inadequate neuromuscular block, and both probably contributed in many cases."
He and his associates formed a panel of seven experienced anesthesiologists to identify anesthesiology actions that are indicative of episodes of insufficient neuromuscular block and searched for those criteria in patient records, with a three-person adjudication committee approving the search criteria through a random sample of at least 50 charts for each criterion.
Overall, 28% of operations had evidence of insufficient neuromuscular blockade, or 21% if the investigators excluded cases identified solely by electromyogram criteria.
In a separate analysis of the same cohort, Dr. Hesler and his associates searched for comments in the anesthetic records and found that insufficient blockade usually was identified more than 30 minutes before emergence, defined as the time when maintenance anesthesia was discontinued (106 cases), but 18% of the time it occurred 15-30 minutes before emergence (9 cases) or less than 15 minutes before emergence (14 cases).
The closer to the end of surgery, the more likely the anesthesiologist was to respond by deepening anesthesia instead of redosing the neuromuscular blocking agent, with other sedatives (opioids) used at a consistent rate in each time period.
A separate prospective, observational study of 448 patients undergoing elective laparoscopic or open abdominal surgical procedures at eight Canadian centers in 2011-2012 stratified residual neuromuscular blockade by train-of-four (TOF) ratios.
Lower TOF ratios at tracheal extubation and at arrival in the postanesthesia care unit (PACU) were associated with greater risk for complications and greater use of perioperative resources, Dr. Dolores McKeen and her associates reported.
Every 0.1-increment increase in the TOF ratio at tracheal extubation was associated with a 30% reduction in the odds of needing placement of an oral or nasal airway due to upper airway obstruction from the time of patient extubation to PACU discharge. Each 0.1-increment increase in the TOF ratio at tracheal extubation also was associated with 3% fewer bed visits by nurses, said Dr. McKeen of Dalhousie University, Halifax, N.S. Similar results were seen for TOF ratios upon arrival at the PACU.
This suggests that "more effective strategies to prevent and/or manage residual neuromuscular blockade are required to minimize the impact on the patient and health care provider," she said.
The incidence of postoperative residual neuromuscular blockade was 19% for patients with a TOF ratio less than 0.6 at tracheal extubation, 12% with a ratio of 0.6-0.7, 9% with a ratio of 0.7-0.8, 16% with a ratio of 0.8-0.9, and 44% with a ratio of 0.9 or greater. The incidence of residual blockade was 8% for patients with a TOF ratio less than 0.6 upon arrival to the PACU, 7% with a ratio of 0.6-0.7, 14% with a ratio of 0.7-0.8, 16% with a ratio of 0.8-0.9, and 56% with a ratio of 0.9 or greater.
In the United States, neostigmine, an acetylcholinesterase inhibitor, is the most common means of reversing neuromuscular blocking agents, according to Scott Devine, Ph.D., of Merck. Giving neostigmine too early can be ineffective, and giving it too late might induce skeletal muscle weakness.
He and his associates analyzed data from the Anesthesia Quality Institute’s National Anesthesia Clinical Outcomes Registry (NACOR) on 113,276 procedures utilizing rocuronium or vecuronium that were reversed with neostigmine in 2010-2012. The reversal agent was given a mean of 63 minutes after the last dose of a neuromuscular blocking agent, 7 minutes before surgical site closure, 14 minutes prior to emergence, and 29 minutes before the end of anesthesia time, though each administration time had a wide range, he reported.
A substantial number of patients would have spontaneously recovered from the effects of the neuromuscular blockers after 63 minutes, suggesting that neostigmine often may be given later than needed, he said. If neostigmine is given 7 minutes before surgical site closure, reversal of neuromuscular blockade could be well underway, resulting in increased muscle tension during surgical site closure, which could increase the risk of complications such as dehiscence or postsurgical hernias, he added.
The large variability in practice may be due to multiple factors and deserves further research, he said.
Merck, which markets a neuromuscular blockade agent, sponsored the studies and supplied at least one investigator for each study.
[email protected] On Twitter @sherryboschert
SAN FRANCISCO – Patients under general anesthesia may be getting insufficient neuromuscular blockade in 1%-45% of operations, depending on the definition, according to several studies presented in a joint session at the annual meeting of the American Society of Anesthesiologists.
Regardless of the exact definition, the findings suggest that the problem of insufficient blockade is considerably more common than expected, the anesthesiologists in attendance agreed.
A lack of clinical guidelines for neuromuscular blockade probably contributes to the problem, some speakers suggested. There is no established definition of insufficient neuromuscular blockade, which has been associated in prior studies with compromised surgical visualization, impaired ventilation leading to barotraumas, direct injury through unexpected movement, and other complications.
Investigators presented their results in posters and in a joint discussion session at the meeting. All studies were sponsored by Merck, which markets a neuromuscular blocking agent (rocuronium bromide, or Zemuron) and is seeking U.S. approval for a drug that rapidly reverses neuromuscular blockade (sugammadex, or Bridion).
One percent of 129,209 adults who underwent general anesthesia and received a nondepolarizing neuromuscular blockade agent in 2005-2013 experienced insufficient blockade in a way that interrupted surgery, either through undesired patient movement (0.3%) or an explicit request from the surgeon for additional muscle relaxation and administration of more neuromuscular blockade (0.7%), Dr. Timur Dubovoy and his associates reported.
They also found indirect evidence of insufficient neuromuscular blockade through two other criteria that were much more common, said Dr. Dubovoy of the University of Michigan, Ann Arbor. Anesthesiologists gave more neuromuscular blockade after documenting twitches on peripheral nerve stimulation (train-of-four monitoring) in 39% of patients, indicative of unintended recovery from neuromuscular blockade. Large or even "excessive" maintenance doses were given to 45% of patients, consistent with insufficient neuromuscular blockade, he said.
Those kinds of events typically don’t interrupt a procedure but can lead to residual neuromuscular blockade due to excessive dosing, potentially increasing complications and delaying recovery after anesthesia. The study looked only at the incidence of insufficient neuromuscular blockade, however, not outcomes.
"Current use of nondepolarizing neuromuscular blockade agents and subjective tactile train-of-four monitoring frequently exposes patients to inadequate neuromuscular blockade," Dr. Dubovoy said.
In a separate study, insufficient neuromuscular blockade affected 21%-28% of 48,315 adults undergoing abdominal, laparoscopic, and interventional neurovascular procedures at the Cleveland Clinic in 2005-2013, Dr. Brian D. Hesler and his associates reported.
"Our results suggest that insufficient block is relatively common, even in operations that are generally thought to require muscle relaxation," said Dr. Hesler of the Cleveland Clinic. "It is difficult to separate inadequate anesthesia from inadequate neuromuscular block, and both probably contributed in many cases."
He and his associates formed a panel of seven experienced anesthesiologists to identify anesthesiology actions that are indicative of episodes of insufficient neuromuscular block and searched for those criteria in patient records, with a three-person adjudication committee approving the search criteria through a random sample of at least 50 charts for each criterion.
Overall, 28% of operations had evidence of insufficient neuromuscular blockade, or 21% if the investigators excluded cases identified solely by electromyogram criteria.
In a separate analysis of the same cohort, Dr. Hesler and his associates searched for comments in the anesthetic records and found that insufficient blockade usually was identified more than 30 minutes before emergence, defined as the time when maintenance anesthesia was discontinued (106 cases), but 18% of the time it occurred 15-30 minutes before emergence (9 cases) or less than 15 minutes before emergence (14 cases).
The closer to the end of surgery, the more likely the anesthesiologist was to respond by deepening anesthesia instead of redosing the neuromuscular blocking agent, with other sedatives (opioids) used at a consistent rate in each time period.
A separate prospective, observational study of 448 patients undergoing elective laparoscopic or open abdominal surgical procedures at eight Canadian centers in 2011-2012 stratified residual neuromuscular blockade by train-of-four (TOF) ratios.
Lower TOF ratios at tracheal extubation and at arrival in the postanesthesia care unit (PACU) were associated with greater risk for complications and greater use of perioperative resources, Dr. Dolores McKeen and her associates reported.
Every 0.1-increment increase in the TOF ratio at tracheal extubation was associated with a 30% reduction in the odds of needing placement of an oral or nasal airway due to upper airway obstruction from the time of patient extubation to PACU discharge. Each 0.1-increment increase in the TOF ratio at tracheal extubation also was associated with 3% fewer bed visits by nurses, said Dr. McKeen of Dalhousie University, Halifax, N.S. Similar results were seen for TOF ratios upon arrival at the PACU.
This suggests that "more effective strategies to prevent and/or manage residual neuromuscular blockade are required to minimize the impact on the patient and health care provider," she said.
The incidence of postoperative residual neuromuscular blockade was 19% for patients with a TOF ratio less than 0.6 at tracheal extubation, 12% with a ratio of 0.6-0.7, 9% with a ratio of 0.7-0.8, 16% with a ratio of 0.8-0.9, and 44% with a ratio of 0.9 or greater. The incidence of residual blockade was 8% for patients with a TOF ratio less than 0.6 upon arrival to the PACU, 7% with a ratio of 0.6-0.7, 14% with a ratio of 0.7-0.8, 16% with a ratio of 0.8-0.9, and 56% with a ratio of 0.9 or greater.
In the United States, neostigmine, an acetylcholinesterase inhibitor, is the most common means of reversing neuromuscular blocking agents, according to Scott Devine, Ph.D., of Merck. Giving neostigmine too early can be ineffective, and giving it too late might induce skeletal muscle weakness.
He and his associates analyzed data from the Anesthesia Quality Institute’s National Anesthesia Clinical Outcomes Registry (NACOR) on 113,276 procedures utilizing rocuronium or vecuronium that were reversed with neostigmine in 2010-2012. The reversal agent was given a mean of 63 minutes after the last dose of a neuromuscular blocking agent, 7 minutes before surgical site closure, 14 minutes prior to emergence, and 29 minutes before the end of anesthesia time, though each administration time had a wide range, he reported.
A substantial number of patients would have spontaneously recovered from the effects of the neuromuscular blockers after 63 minutes, suggesting that neostigmine often may be given later than needed, he said. If neostigmine is given 7 minutes before surgical site closure, reversal of neuromuscular blockade could be well underway, resulting in increased muscle tension during surgical site closure, which could increase the risk of complications such as dehiscence or postsurgical hernias, he added.
The large variability in practice may be due to multiple factors and deserves further research, he said.
Merck, which markets a neuromuscular blockade agent, sponsored the studies and supplied at least one investigator for each study.
[email protected] On Twitter @sherryboschert
AT THE ASA ANNUAL MEETING
Major finding: The incidence of inadequate neuromuscular blockade during surgery ranged from 1% to 45%, depending on the definition.
Data source: Multiple retrospective studies of adults undergoing surgery with general anesthesia who received neuromuscular blocking agents.
Disclosures: Merck, which markets a neuromuscular blockade reversal agent, sponsored the studies and supplied at least one investigator for each study.
Distribution of female pelvic medicine fellowships varied
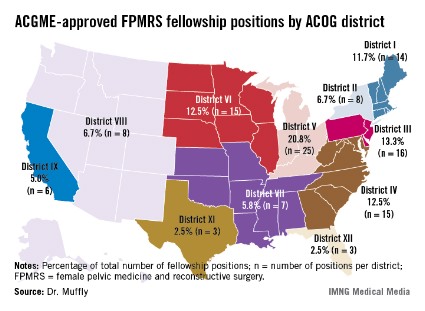
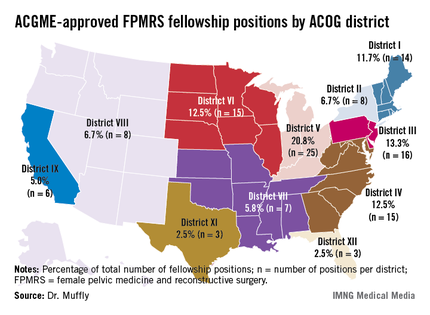
LAS VEGAS – The geographic distribution of female pelvic medicine and reconstructive surgery fellowships approved by the Accreditation Council for Graduate Medical Education varies widely in the United States, results from an analysis demonstrated.
Such variation "may limit the choices for residents wishing to pursue further training in female pelvic medicine and reconstructive surgery," Dr. Tyler Muffly said in an interview during a poster session at the annual meeting of the American Urogynecologic Society. "It also means that patients in some areas are going to have to travel further to get to a referral center."
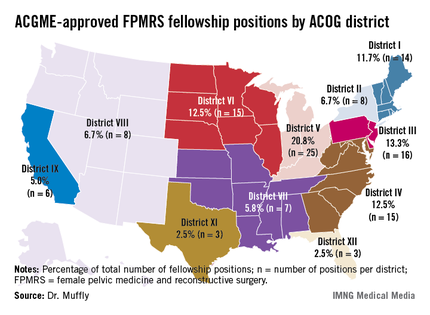
In an effort to determine the distribution of first-year female pelvic medicine and reconstructive surgery (FPMRS) fellowship positions according to population within states and within districts of the American Congress of Obstetrics and Gynecology, Dr. Muffly and his associates used data from the 2010 U.S. Census and from the number of 2012 female pelvic medicine and reconstructive surgery fellowship positions available through the match, which were obtained from the Accreditation Council for Graduate Medical Education (ACGME). They rounded off population data to the nearest 1,000 persons.
Dr. Muffly of the division of female pelvic medicine and reconstructive surgery (FPMRS) at the University of Colorado, Aurora, reported that there was a mean of 9.6 FPMRS fellowship positions per ACOG district and a mean of 2.3 FPMRS programs per ACOG district. More than two-thirds of fellowship programs were located east of the Mississippi River (67.5% vs. 32.5% west of that spot), with the greatest number clustered in ACOG District V, which consists of Michigan, Indiana, Ohio, and Kentucky (20.8%).
The researchers observed a significant difference between ACOG districts based on the number of FPMRS fellowship programs (P = .04) as well as a difference in total population between districts (P less than .0001). Specifically, Florida (ACOG District XII) had the highest proportion of women overall (P = .001) while California (ACOG District IX) had the highest proportion of postmenopausal women (P less than .001).
When Dr. Muffly and his associates analyzed the distribution of FPMRS fellowship positions within ACOG districts, a statistically significant difference was observed in the number of FPMRS fellowship positions per district (P = .03). For example, there were only 8 positions in ACOG District VIII (Arizona, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming), compared with 16 positions in ACOG District III (Delaware, New Jersey, and Pennsylvania).
"The findings suggest that future FPMRS fellowships might be started in the West or in high-density states like Florida or California where there are many postmenopausal women," Dr. Muffly concluded. "There are fellowships in all 11 ACOG districts. Physicians in the West or in the high plains states might have to look a little harder for a fellowship or a referral center for female pelvic medicine and reconstructive surgery."
Dr. Muffly said he had no relevant financial disclosures.
LAS VEGAS – The geographic distribution of female pelvic medicine and reconstructive surgery fellowships approved by the Accreditation Council for Graduate Medical Education varies widely in the United States, results from an analysis demonstrated.
Such variation "may limit the choices for residents wishing to pursue further training in female pelvic medicine and reconstructive surgery," Dr. Tyler Muffly said in an interview during a poster session at the annual meeting of the American Urogynecologic Society. "It also means that patients in some areas are going to have to travel further to get to a referral center."
In an effort to determine the distribution of first-year female pelvic medicine and reconstructive surgery (FPMRS) fellowship positions according to population within states and within districts of the American Congress of Obstetrics and Gynecology, Dr. Muffly and his associates used data from the 2010 U.S. Census and from the number of 2012 female pelvic medicine and reconstructive surgery fellowship positions available through the match, which were obtained from the Accreditation Council for Graduate Medical Education (ACGME). They rounded off population data to the nearest 1,000 persons.
Dr. Muffly of the division of female pelvic medicine and reconstructive surgery (FPMRS) at the University of Colorado, Aurora, reported that there was a mean of 9.6 FPMRS fellowship positions per ACOG district and a mean of 2.3 FPMRS programs per ACOG district. More than two-thirds of fellowship programs were located east of the Mississippi River (67.5% vs. 32.5% west of that spot), with the greatest number clustered in ACOG District V, which consists of Michigan, Indiana, Ohio, and Kentucky (20.8%).
The researchers observed a significant difference between ACOG districts based on the number of FPMRS fellowship programs (P = .04) as well as a difference in total population between districts (P less than .0001). Specifically, Florida (ACOG District XII) had the highest proportion of women overall (P = .001) while California (ACOG District IX) had the highest proportion of postmenopausal women (P less than .001).
When Dr. Muffly and his associates analyzed the distribution of FPMRS fellowship positions within ACOG districts, a statistically significant difference was observed in the number of FPMRS fellowship positions per district (P = .03). For example, there were only 8 positions in ACOG District VIII (Arizona, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming), compared with 16 positions in ACOG District III (Delaware, New Jersey, and Pennsylvania).
"The findings suggest that future FPMRS fellowships might be started in the West or in high-density states like Florida or California where there are many postmenopausal women," Dr. Muffly concluded. "There are fellowships in all 11 ACOG districts. Physicians in the West or in the high plains states might have to look a little harder for a fellowship or a referral center for female pelvic medicine and reconstructive surgery."
Dr. Muffly said he had no relevant financial disclosures.
LAS VEGAS – The geographic distribution of female pelvic medicine and reconstructive surgery fellowships approved by the Accreditation Council for Graduate Medical Education varies widely in the United States, results from an analysis demonstrated.
Such variation "may limit the choices for residents wishing to pursue further training in female pelvic medicine and reconstructive surgery," Dr. Tyler Muffly said in an interview during a poster session at the annual meeting of the American Urogynecologic Society. "It also means that patients in some areas are going to have to travel further to get to a referral center."
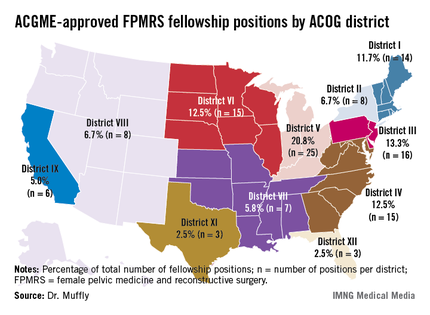
In an effort to determine the distribution of first-year female pelvic medicine and reconstructive surgery (FPMRS) fellowship positions according to population within states and within districts of the American Congress of Obstetrics and Gynecology, Dr. Muffly and his associates used data from the 2010 U.S. Census and from the number of 2012 female pelvic medicine and reconstructive surgery fellowship positions available through the match, which were obtained from the Accreditation Council for Graduate Medical Education (ACGME). They rounded off population data to the nearest 1,000 persons.
Dr. Muffly of the division of female pelvic medicine and reconstructive surgery (FPMRS) at the University of Colorado, Aurora, reported that there was a mean of 9.6 FPMRS fellowship positions per ACOG district and a mean of 2.3 FPMRS programs per ACOG district. More than two-thirds of fellowship programs were located east of the Mississippi River (67.5% vs. 32.5% west of that spot), with the greatest number clustered in ACOG District V, which consists of Michigan, Indiana, Ohio, and Kentucky (20.8%).
The researchers observed a significant difference between ACOG districts based on the number of FPMRS fellowship programs (P = .04) as well as a difference in total population between districts (P less than .0001). Specifically, Florida (ACOG District XII) had the highest proportion of women overall (P = .001) while California (ACOG District IX) had the highest proportion of postmenopausal women (P less than .001).
When Dr. Muffly and his associates analyzed the distribution of FPMRS fellowship positions within ACOG districts, a statistically significant difference was observed in the number of FPMRS fellowship positions per district (P = .03). For example, there were only 8 positions in ACOG District VIII (Arizona, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming), compared with 16 positions in ACOG District III (Delaware, New Jersey, and Pennsylvania).
"The findings suggest that future FPMRS fellowships might be started in the West or in high-density states like Florida or California where there are many postmenopausal women," Dr. Muffly concluded. "There are fellowships in all 11 ACOG districts. Physicians in the West or in the high plains states might have to look a little harder for a fellowship or a referral center for female pelvic medicine and reconstructive surgery."
Dr. Muffly said he had no relevant financial disclosures.
AT THE AUGS ANNUAL MEETING
Major finding: More than two-thirds of fellowship programs in female pelvic medicine and reconstructive surgery were located east of the Mississippi River (67.5% vs. 32.5% west of that spot), with the greatest number clustered in American Congress of Obstetrics and Gynecology District V, which consists of Michigan, Indiana, Ohio, and Kentucky (20.8%).
Data source: An analysis of data from the 2010 U.S. Census and from the number of 2012 female pelvic medicine and reconstructive surgery fellowship positions available through the match.
Disclosures: Dr. Muffly said he had no relevant financial disclosures.
Bracing lessened patellofemoral pain in OA
SAN DIEGO – Patients with osteoarthritis of the knee who wore a patellofemoral brace for 6 weeks experienced a significant reduction in pain and in bone marrow lesion volumes in the patellofemoral region, compared with those who did not wear the brace, a multicenter trial showed.
"There’s a pressing need for nonsurgical intervention for knee osteoarthritis," Dr. David T. Felson said in a press briefing at the annual meeting of the American College of Rheumatology.
"There are no currently approved structure-modifying treatments. This has been a focus of studies that have been testing modifying treatments on hyaline cartilage, which changes slowly, necessitating expensive, long-term, large trials. Even so, mechanopathology such as that caused by malalignment or meniscal tears may make it impossible to protect cartilage in existing OA," he noted.
Dr. Felson, director of the Research in Osteoarthritis in Manchester group at the University of Manchester (England) and professor of medicine at Boston University, went on to note that bone marrow lesions (BMLs) "have been well shown to predict later cartilage loss in that location and correlate with pain and its severity. Recently, we showed that BMLs fluctuate in volume in as little as 6 weeks. Further, one small trial has suggested that zoledronic acid may shrink BMLs and reduce knee pain. That leads us to suggest that BMLs may be a viable treatment target in OA."
The patellofemoral joint "is a major source of knee pain in OA, and there has been little study of the efficacy of PF braces," he continued. "In a body mechanics study, PF bracing has been shown to increase the contact area of the PF joint. It may thereby lower the contact stress and shrink BMLs."
He and his associates set out to determine whether bracing would improve pain and lessen the volume of BMLs in patients with knee OA. They enrolled 126 patients with a mean age of 55 years whose knee pain had been present daily for the previous 3 months. Half of the patients wore a soft neoprene PF brace for a mean of 7.3 hours per day, while the other half did not.
All study participants "had to have at least a score of 40 on a 0-100 mm visual analogue scale (VAS) for nominated aggravating activity likely to originate in the PF joint," Dr. Felson said. "They had to have pain with activities such as stair climbing, kneeling, prolonged sitting or squatting, [and] they also had to have a radiographic KL [Kellgren-Lawrence] score of grade 2 or 3 in the PF joint. That score had to be greater than the KL score for the tibiofemoral compartments. They also had to undergo a clinical exam by a trained physiotherapist to confirm PF joint tenderness."
The researchers performed contrast-enhanced knee MRIs at baseline and at 6 weeks. The primary symptom outcome measure was VAS pain during the patients’ nominated aggravating activity, while the primary structural outcome measure was BML volume in the PF joint as assessed on sagittal precontrast view.
At 6 weeks, Dr. Felson reported that patients in the no-brace group had a mean reduction in their VAS pain of 1.3, compared with a reduction of 18.2 in the braced group, a mean between-group difference of 16.9 that reached statistical significance (P less than .001).
As for PF BML volume, patients in the no-brace group showed a slight increase in volume (mean, 102.7 mm3), while the braced group showed a significant decrease in PF BML volume (mean, –554.9 mm3), for a mean between-group difference of 657.6 mm3 that reached statistical significance (P = .02). "That represents about a 25% decrease in volume," Dr. Felson said.
No differences were observed between the two groups in terms of tibiofemoral BML volume or in synovitis volume.
Dr. Felson acknowledged certain limitations of the study, including its 6-week design. "OA is a long-term chronic disease," he said. "We don’t know what relevance our findings have for longer-term structure changes of the knee."
The researchers stated that they had no relevant financial conflicts to disclose.
SAN DIEGO – Patients with osteoarthritis of the knee who wore a patellofemoral brace for 6 weeks experienced a significant reduction in pain and in bone marrow lesion volumes in the patellofemoral region, compared with those who did not wear the brace, a multicenter trial showed.
"There’s a pressing need for nonsurgical intervention for knee osteoarthritis," Dr. David T. Felson said in a press briefing at the annual meeting of the American College of Rheumatology.
"There are no currently approved structure-modifying treatments. This has been a focus of studies that have been testing modifying treatments on hyaline cartilage, which changes slowly, necessitating expensive, long-term, large trials. Even so, mechanopathology such as that caused by malalignment or meniscal tears may make it impossible to protect cartilage in existing OA," he noted.
Dr. Felson, director of the Research in Osteoarthritis in Manchester group at the University of Manchester (England) and professor of medicine at Boston University, went on to note that bone marrow lesions (BMLs) "have been well shown to predict later cartilage loss in that location and correlate with pain and its severity. Recently, we showed that BMLs fluctuate in volume in as little as 6 weeks. Further, one small trial has suggested that zoledronic acid may shrink BMLs and reduce knee pain. That leads us to suggest that BMLs may be a viable treatment target in OA."
The patellofemoral joint "is a major source of knee pain in OA, and there has been little study of the efficacy of PF braces," he continued. "In a body mechanics study, PF bracing has been shown to increase the contact area of the PF joint. It may thereby lower the contact stress and shrink BMLs."
He and his associates set out to determine whether bracing would improve pain and lessen the volume of BMLs in patients with knee OA. They enrolled 126 patients with a mean age of 55 years whose knee pain had been present daily for the previous 3 months. Half of the patients wore a soft neoprene PF brace for a mean of 7.3 hours per day, while the other half did not.
All study participants "had to have at least a score of 40 on a 0-100 mm visual analogue scale (VAS) for nominated aggravating activity likely to originate in the PF joint," Dr. Felson said. "They had to have pain with activities such as stair climbing, kneeling, prolonged sitting or squatting, [and] they also had to have a radiographic KL [Kellgren-Lawrence] score of grade 2 or 3 in the PF joint. That score had to be greater than the KL score for the tibiofemoral compartments. They also had to undergo a clinical exam by a trained physiotherapist to confirm PF joint tenderness."
The researchers performed contrast-enhanced knee MRIs at baseline and at 6 weeks. The primary symptom outcome measure was VAS pain during the patients’ nominated aggravating activity, while the primary structural outcome measure was BML volume in the PF joint as assessed on sagittal precontrast view.
At 6 weeks, Dr. Felson reported that patients in the no-brace group had a mean reduction in their VAS pain of 1.3, compared with a reduction of 18.2 in the braced group, a mean between-group difference of 16.9 that reached statistical significance (P less than .001).
As for PF BML volume, patients in the no-brace group showed a slight increase in volume (mean, 102.7 mm3), while the braced group showed a significant decrease in PF BML volume (mean, –554.9 mm3), for a mean between-group difference of 657.6 mm3 that reached statistical significance (P = .02). "That represents about a 25% decrease in volume," Dr. Felson said.
No differences were observed between the two groups in terms of tibiofemoral BML volume or in synovitis volume.
Dr. Felson acknowledged certain limitations of the study, including its 6-week design. "OA is a long-term chronic disease," he said. "We don’t know what relevance our findings have for longer-term structure changes of the knee."
The researchers stated that they had no relevant financial conflicts to disclose.
SAN DIEGO – Patients with osteoarthritis of the knee who wore a patellofemoral brace for 6 weeks experienced a significant reduction in pain and in bone marrow lesion volumes in the patellofemoral region, compared with those who did not wear the brace, a multicenter trial showed.
"There’s a pressing need for nonsurgical intervention for knee osteoarthritis," Dr. David T. Felson said in a press briefing at the annual meeting of the American College of Rheumatology.
"There are no currently approved structure-modifying treatments. This has been a focus of studies that have been testing modifying treatments on hyaline cartilage, which changes slowly, necessitating expensive, long-term, large trials. Even so, mechanopathology such as that caused by malalignment or meniscal tears may make it impossible to protect cartilage in existing OA," he noted.
Dr. Felson, director of the Research in Osteoarthritis in Manchester group at the University of Manchester (England) and professor of medicine at Boston University, went on to note that bone marrow lesions (BMLs) "have been well shown to predict later cartilage loss in that location and correlate with pain and its severity. Recently, we showed that BMLs fluctuate in volume in as little as 6 weeks. Further, one small trial has suggested that zoledronic acid may shrink BMLs and reduce knee pain. That leads us to suggest that BMLs may be a viable treatment target in OA."
The patellofemoral joint "is a major source of knee pain in OA, and there has been little study of the efficacy of PF braces," he continued. "In a body mechanics study, PF bracing has been shown to increase the contact area of the PF joint. It may thereby lower the contact stress and shrink BMLs."
He and his associates set out to determine whether bracing would improve pain and lessen the volume of BMLs in patients with knee OA. They enrolled 126 patients with a mean age of 55 years whose knee pain had been present daily for the previous 3 months. Half of the patients wore a soft neoprene PF brace for a mean of 7.3 hours per day, while the other half did not.
All study participants "had to have at least a score of 40 on a 0-100 mm visual analogue scale (VAS) for nominated aggravating activity likely to originate in the PF joint," Dr. Felson said. "They had to have pain with activities such as stair climbing, kneeling, prolonged sitting or squatting, [and] they also had to have a radiographic KL [Kellgren-Lawrence] score of grade 2 or 3 in the PF joint. That score had to be greater than the KL score for the tibiofemoral compartments. They also had to undergo a clinical exam by a trained physiotherapist to confirm PF joint tenderness."
The researchers performed contrast-enhanced knee MRIs at baseline and at 6 weeks. The primary symptom outcome measure was VAS pain during the patients’ nominated aggravating activity, while the primary structural outcome measure was BML volume in the PF joint as assessed on sagittal precontrast view.
At 6 weeks, Dr. Felson reported that patients in the no-brace group had a mean reduction in their VAS pain of 1.3, compared with a reduction of 18.2 in the braced group, a mean between-group difference of 16.9 that reached statistical significance (P less than .001).
As for PF BML volume, patients in the no-brace group showed a slight increase in volume (mean, 102.7 mm3), while the braced group showed a significant decrease in PF BML volume (mean, –554.9 mm3), for a mean between-group difference of 657.6 mm3 that reached statistical significance (P = .02). "That represents about a 25% decrease in volume," Dr. Felson said.
No differences were observed between the two groups in terms of tibiofemoral BML volume or in synovitis volume.
Dr. Felson acknowledged certain limitations of the study, including its 6-week design. "OA is a long-term chronic disease," he said. "We don’t know what relevance our findings have for longer-term structure changes of the knee."
The researchers stated that they had no relevant financial conflicts to disclose.
AT THE ACR ANNUAL MEETING
Major finding: Patients who wore a patellofemoral brace over the course of 6 weeks had a significant reduction in patellofemoral pain as measured by a visual analogue scale compared with those who did not wear a brace (reductions of 18.2 and 1.3, respectively; P less than .001).
Data source: 126 patients with a mean age of 55 years who had knee pain present daily for the previous 3 months. Half of the patients wore a soft neoprene PF brace for a mean of 7.3 hours per day, while the other half did not.
Disclosures: The researchers had no relevant financial conflicts to disclose.
What's coming through the door? Prepping for new ACA patients
Millions of Americans can now purchase health insurance through the federal and state exchanges. But while interest is high, no one knows for sure just how many people will end up enrolling in a plan.
And the bigger question for physicians is how many patients will show up in their offices early next year when coverage starts.
The answer may depend on where you live, according to Paul B. Ginsburg, Ph.D., an economist and president of the Center for Studying Health System Change.
Multiple factors dictate demand
States with the highest number of uninsured residents are likely to have the most people entering the insurance market, Dr. Ginsburg said. But the expansion of Medicaid is also a factor.
As originally enacted, much of the increased insurance coverage under the Affordable Care Act was to come from the expansion of Medicaid. That changed when the Supreme Court gave states the choice of whether or not to expand eligibility for their programs; so far 25 states are actively moving forward with expansion.
Texas has one of the highest rates of uninsurance in the nation, but is not expanding its Medicaid program. Arkansas, Arizona, and New Mexico – all with high rates of uninsurance – are.
The exchanges will allow some patients in the system – who are currently without coverage – to gain insurance, said Dr. Reid B. Blackwelder, president of the American Academy of Family Physicians (AAFP). This should provide some relief for struggling physicians, he said.
In a survey of members, the AAFP found that family physicians provide free or reduced rate visits for uninsured or underinsured patients an average of 10 times a week.
"A lot of the folks that will get insurance are already in the system," Dr. Blackwelder said. "They are already being cared for, but cost the system money. This will actually help."
Tough for solo practices
So who will be coming through the front door? Experts say it will be both the sick and the healthy.
The ACA’s preventive care benefits make it easier for healthy patients to come in for mammograms and colonoscopies, said Jennifer Caudle, D.O., of Washington Township, N.J. But she predicted that physicians will also see patients who have been out of the health care system for years and have uncontrolled chronic illnesses.
That’s what Dr. Richard Dupee saw when Massachusetts enacted its health reform law in 2006.
"Some pretty serious train wrecks came in here," said Dr. Dupee, a solo primary care physician in Wellesley and president of the Massachusetts chapter of the American Geriatrics Society. Overall, he added, Massachusetts is seeing better outcomes for conditions such as diabetes. But the downside is that physicians still don’t get paid adequately to provide intensive visits.
"There’s no such thing as the 1-hour doctor visit anymore because no one will pay for it," he said.
At his office, which operates as a patient-centered medical home, they work to get complex patients to come in for a series of visits and have them seen initially by either a nurse practitioner or a physician assistant.
Dr. Dupee recommended that physicians who believe they will see an influx of new, potentially sicker patients consider restructuring the way they provide care.
"If you’re a single doc, you can’t do it," he said.
Redesigning care
Dr. Blackwelder suggested that practices will need to look at different ways to meet patients’ needs.
For example, a patient may come to the office with a list of 10 or so questions that he or she would like addressed in a single visit. If the physician has an online patient portal that links to the electronic health record, the patient could winnow that list by viewing lab results and requesting medical refills outside of the office visit structure.
"What we can do, if we’re being effective, is perhaps handle six or seven of those 10 things differently so that when [patients] come in, we now don’t feel as pressured and we can focus on whatever is most important," he said. "We get more bang for our buck during that time."
Using existing staff effectively also will be important, according to Dr. Douglas Curran of Athens, Tex.
Dr. Curran, who is part of a 14-physician group, has no plans to make significant investments in staff or technology. "We’ve got enough flexibility," he said. "We think we can accommodate a lot of these patients."
Instead, he’s talking to insurers to figure out which health plans will be available in his area and he’s talking to patients to find out who is signing up for insurance.
Dr. Curran said that he is not expecting to see thousands of new patients show up on Jan. 1. Instead, he predicted that there would be a gradual drift in much the same way as when a new employer enters the community and people gain coverage and begin seeking care.
Doubts about the ACA rollout
Not all physicians are positive about the health care law rollout. A new survey conducted by the Medical Group Management Association (MGMA) found that many medical practices have concerns about low payment rates and administrative burdens. And they are still weighing their options when it comes to participation in the new insurance products being sold on the exchanges.
The survey, which included responses from more than 1,000 medical practice executives and administrators, found that about 56% had an unfavorable view of the impact that the ACA’s insurance exchanges will have on their practices. About 28% were neutral and 16% had a favorable view.
Less than a third of the practices responding said they planned to participate in the new exchange plans, while 14% said they would not. Most respondents were still evaluating whether to participate.
Conservative groups such as the Heritage Foundation have seized on the results as proof that the ACA rollout is doomed to fail because doctors won’t show up.
But Anders M. Gilberg, senior vice president of government affairs for MGMA, said the findings reflect the uncertainty that practices are facing, since many are still awaiting complete information from health plans about the size of their networks and the payment rates.
"You can’t make business changes if you don’t know what you’re dealing with," he said.
The 30% of survey respondents who said they plan to participate have probably received fairly complete information about the fee schedule that made them comfortable enough to sign a contract, Mr. Gilberg said.
He urged physicians who have not yet heard from area insurers to be proactive.
Reach out to any plans with which they already contract. Find out if they will be offering plans on the exchange and if they have an "all product" clause that requires physicians to be part of all their plans. Be vigilant about any addendums that the plans send that may require participation in the new products. This is a critical time to read all the fine print from insurers, he said.
On Twitter @MaryEllenNY
Be prepared to change and adapt, or follow the dinosaur.
Forewarned is forearmed.
Dr. Paul A. Selecky, FCCP, is with the Pulmonary Department, Sleep Disorders Center and Palliative Medicine Service at Hoag Memorial Hospital in
Newport Beach, Calif.
Be prepared to change and adapt, or follow the dinosaur.
Forewarned is forearmed.
Dr. Paul A. Selecky, FCCP, is with the Pulmonary Department, Sleep Disorders Center and Palliative Medicine Service at Hoag Memorial Hospital in
Newport Beach, Calif.
Be prepared to change and adapt, or follow the dinosaur.
Forewarned is forearmed.
Dr. Paul A. Selecky, FCCP, is with the Pulmonary Department, Sleep Disorders Center and Palliative Medicine Service at Hoag Memorial Hospital in
Newport Beach, Calif.
Millions of Americans can now purchase health insurance through the federal and state exchanges. But while interest is high, no one knows for sure just how many people will end up enrolling in a plan.
And the bigger question for physicians is how many patients will show up in their offices early next year when coverage starts.
The answer may depend on where you live, according to Paul B. Ginsburg, Ph.D., an economist and president of the Center for Studying Health System Change.
Multiple factors dictate demand
States with the highest number of uninsured residents are likely to have the most people entering the insurance market, Dr. Ginsburg said. But the expansion of Medicaid is also a factor.
As originally enacted, much of the increased insurance coverage under the Affordable Care Act was to come from the expansion of Medicaid. That changed when the Supreme Court gave states the choice of whether or not to expand eligibility for their programs; so far 25 states are actively moving forward with expansion.
Texas has one of the highest rates of uninsurance in the nation, but is not expanding its Medicaid program. Arkansas, Arizona, and New Mexico – all with high rates of uninsurance – are.
The exchanges will allow some patients in the system – who are currently without coverage – to gain insurance, said Dr. Reid B. Blackwelder, president of the American Academy of Family Physicians (AAFP). This should provide some relief for struggling physicians, he said.
In a survey of members, the AAFP found that family physicians provide free or reduced rate visits for uninsured or underinsured patients an average of 10 times a week.
"A lot of the folks that will get insurance are already in the system," Dr. Blackwelder said. "They are already being cared for, but cost the system money. This will actually help."
Tough for solo practices
So who will be coming through the front door? Experts say it will be both the sick and the healthy.
The ACA’s preventive care benefits make it easier for healthy patients to come in for mammograms and colonoscopies, said Jennifer Caudle, D.O., of Washington Township, N.J. But she predicted that physicians will also see patients who have been out of the health care system for years and have uncontrolled chronic illnesses.
That’s what Dr. Richard Dupee saw when Massachusetts enacted its health reform law in 2006.
"Some pretty serious train wrecks came in here," said Dr. Dupee, a solo primary care physician in Wellesley and president of the Massachusetts chapter of the American Geriatrics Society. Overall, he added, Massachusetts is seeing better outcomes for conditions such as diabetes. But the downside is that physicians still don’t get paid adequately to provide intensive visits.
"There’s no such thing as the 1-hour doctor visit anymore because no one will pay for it," he said.
At his office, which operates as a patient-centered medical home, they work to get complex patients to come in for a series of visits and have them seen initially by either a nurse practitioner or a physician assistant.
Dr. Dupee recommended that physicians who believe they will see an influx of new, potentially sicker patients consider restructuring the way they provide care.
"If you’re a single doc, you can’t do it," he said.
Redesigning care
Dr. Blackwelder suggested that practices will need to look at different ways to meet patients’ needs.
For example, a patient may come to the office with a list of 10 or so questions that he or she would like addressed in a single visit. If the physician has an online patient portal that links to the electronic health record, the patient could winnow that list by viewing lab results and requesting medical refills outside of the office visit structure.
"What we can do, if we’re being effective, is perhaps handle six or seven of those 10 things differently so that when [patients] come in, we now don’t feel as pressured and we can focus on whatever is most important," he said. "We get more bang for our buck during that time."
Using existing staff effectively also will be important, according to Dr. Douglas Curran of Athens, Tex.
Dr. Curran, who is part of a 14-physician group, has no plans to make significant investments in staff or technology. "We’ve got enough flexibility," he said. "We think we can accommodate a lot of these patients."
Instead, he’s talking to insurers to figure out which health plans will be available in his area and he’s talking to patients to find out who is signing up for insurance.
Dr. Curran said that he is not expecting to see thousands of new patients show up on Jan. 1. Instead, he predicted that there would be a gradual drift in much the same way as when a new employer enters the community and people gain coverage and begin seeking care.
Doubts about the ACA rollout
Not all physicians are positive about the health care law rollout. A new survey conducted by the Medical Group Management Association (MGMA) found that many medical practices have concerns about low payment rates and administrative burdens. And they are still weighing their options when it comes to participation in the new insurance products being sold on the exchanges.
The survey, which included responses from more than 1,000 medical practice executives and administrators, found that about 56% had an unfavorable view of the impact that the ACA’s insurance exchanges will have on their practices. About 28% were neutral and 16% had a favorable view.
Less than a third of the practices responding said they planned to participate in the new exchange plans, while 14% said they would not. Most respondents were still evaluating whether to participate.
Conservative groups such as the Heritage Foundation have seized on the results as proof that the ACA rollout is doomed to fail because doctors won’t show up.
But Anders M. Gilberg, senior vice president of government affairs for MGMA, said the findings reflect the uncertainty that practices are facing, since many are still awaiting complete information from health plans about the size of their networks and the payment rates.
"You can’t make business changes if you don’t know what you’re dealing with," he said.
The 30% of survey respondents who said they plan to participate have probably received fairly complete information about the fee schedule that made them comfortable enough to sign a contract, Mr. Gilberg said.
He urged physicians who have not yet heard from area insurers to be proactive.
Reach out to any plans with which they already contract. Find out if they will be offering plans on the exchange and if they have an "all product" clause that requires physicians to be part of all their plans. Be vigilant about any addendums that the plans send that may require participation in the new products. This is a critical time to read all the fine print from insurers, he said.
On Twitter @MaryEllenNY
Millions of Americans can now purchase health insurance through the federal and state exchanges. But while interest is high, no one knows for sure just how many people will end up enrolling in a plan.
And the bigger question for physicians is how many patients will show up in their offices early next year when coverage starts.
The answer may depend on where you live, according to Paul B. Ginsburg, Ph.D., an economist and president of the Center for Studying Health System Change.
Multiple factors dictate demand
States with the highest number of uninsured residents are likely to have the most people entering the insurance market, Dr. Ginsburg said. But the expansion of Medicaid is also a factor.
As originally enacted, much of the increased insurance coverage under the Affordable Care Act was to come from the expansion of Medicaid. That changed when the Supreme Court gave states the choice of whether or not to expand eligibility for their programs; so far 25 states are actively moving forward with expansion.
Texas has one of the highest rates of uninsurance in the nation, but is not expanding its Medicaid program. Arkansas, Arizona, and New Mexico – all with high rates of uninsurance – are.
The exchanges will allow some patients in the system – who are currently without coverage – to gain insurance, said Dr. Reid B. Blackwelder, president of the American Academy of Family Physicians (AAFP). This should provide some relief for struggling physicians, he said.
In a survey of members, the AAFP found that family physicians provide free or reduced rate visits for uninsured or underinsured patients an average of 10 times a week.
"A lot of the folks that will get insurance are already in the system," Dr. Blackwelder said. "They are already being cared for, but cost the system money. This will actually help."
Tough for solo practices
So who will be coming through the front door? Experts say it will be both the sick and the healthy.
The ACA’s preventive care benefits make it easier for healthy patients to come in for mammograms and colonoscopies, said Jennifer Caudle, D.O., of Washington Township, N.J. But she predicted that physicians will also see patients who have been out of the health care system for years and have uncontrolled chronic illnesses.
That’s what Dr. Richard Dupee saw when Massachusetts enacted its health reform law in 2006.
"Some pretty serious train wrecks came in here," said Dr. Dupee, a solo primary care physician in Wellesley and president of the Massachusetts chapter of the American Geriatrics Society. Overall, he added, Massachusetts is seeing better outcomes for conditions such as diabetes. But the downside is that physicians still don’t get paid adequately to provide intensive visits.
"There’s no such thing as the 1-hour doctor visit anymore because no one will pay for it," he said.
At his office, which operates as a patient-centered medical home, they work to get complex patients to come in for a series of visits and have them seen initially by either a nurse practitioner or a physician assistant.
Dr. Dupee recommended that physicians who believe they will see an influx of new, potentially sicker patients consider restructuring the way they provide care.
"If you’re a single doc, you can’t do it," he said.
Redesigning care
Dr. Blackwelder suggested that practices will need to look at different ways to meet patients’ needs.
For example, a patient may come to the office with a list of 10 or so questions that he or she would like addressed in a single visit. If the physician has an online patient portal that links to the electronic health record, the patient could winnow that list by viewing lab results and requesting medical refills outside of the office visit structure.
"What we can do, if we’re being effective, is perhaps handle six or seven of those 10 things differently so that when [patients] come in, we now don’t feel as pressured and we can focus on whatever is most important," he said. "We get more bang for our buck during that time."
Using existing staff effectively also will be important, according to Dr. Douglas Curran of Athens, Tex.
Dr. Curran, who is part of a 14-physician group, has no plans to make significant investments in staff or technology. "We’ve got enough flexibility," he said. "We think we can accommodate a lot of these patients."
Instead, he’s talking to insurers to figure out which health plans will be available in his area and he’s talking to patients to find out who is signing up for insurance.
Dr. Curran said that he is not expecting to see thousands of new patients show up on Jan. 1. Instead, he predicted that there would be a gradual drift in much the same way as when a new employer enters the community and people gain coverage and begin seeking care.
Doubts about the ACA rollout
Not all physicians are positive about the health care law rollout. A new survey conducted by the Medical Group Management Association (MGMA) found that many medical practices have concerns about low payment rates and administrative burdens. And they are still weighing their options when it comes to participation in the new insurance products being sold on the exchanges.
The survey, which included responses from more than 1,000 medical practice executives and administrators, found that about 56% had an unfavorable view of the impact that the ACA’s insurance exchanges will have on their practices. About 28% were neutral and 16% had a favorable view.
Less than a third of the practices responding said they planned to participate in the new exchange plans, while 14% said they would not. Most respondents were still evaluating whether to participate.
Conservative groups such as the Heritage Foundation have seized on the results as proof that the ACA rollout is doomed to fail because doctors won’t show up.
But Anders M. Gilberg, senior vice president of government affairs for MGMA, said the findings reflect the uncertainty that practices are facing, since many are still awaiting complete information from health plans about the size of their networks and the payment rates.
"You can’t make business changes if you don’t know what you’re dealing with," he said.
The 30% of survey respondents who said they plan to participate have probably received fairly complete information about the fee schedule that made them comfortable enough to sign a contract, Mr. Gilberg said.
He urged physicians who have not yet heard from area insurers to be proactive.
Reach out to any plans with which they already contract. Find out if they will be offering plans on the exchange and if they have an "all product" clause that requires physicians to be part of all their plans. Be vigilant about any addendums that the plans send that may require participation in the new products. This is a critical time to read all the fine print from insurers, he said.
On Twitter @MaryEllenNY
Gastric bypass associated with greatest improvement in cardiac risk factors
WASHINGTON – One year out from surgery, gastric bypass, gastric sleeve, and gastric banding all showed considerable reductions in cardiac risk factors, but gastric bypass showed the greatest risk reduction of all three, as well as greater improvement in body mass index, according to a study presented at this year’s annual clinical congress of the American College of Surgeons.
Baseline and 1-year postoperative data were collected on 1,398 consecutive bariatric surgery patients by Christopher S. Crowe and his colleagues at Stanford (Calif.) University. The investigators sought to evaluate each type of surgery’s effect on biochemical cardiovascular risk factors. The follow-up rate at 12 months was 77%.
The values measured were hemoglobin A1c, fasting insulin, high-density lipoprotein (HDL), low-density lipoprotein (LDL), total cholesterol, triglycerides, high-sensitivity C-reactive protein (CRP), homocysteine, and lipoprotein (a).
Across the three groups, bypass patients tended to be younger by 1-2 years (mean age of this group was 44.3 years), and they had a higher baseline body mass index on average.
Excess weight loss after 1 year averaged 75% in the bypass patients, 55% in the patients with a sleeve, and 40% in those with a band.
When analyzing laboratory values for each group, the investigators found that fasting insulin levels were notably improved in all three groups; but at an improvement rate of 67.0%, the bypass patients had more than double the improvement of the gastric-band patients, while the gastric-sleeve patients showed a 63.7% improvement rate.
The CRP levels also improved dramatically in the bypass patients (67.1%), especially when compared with the band (21.2%) and sleeve (26.3%) groups. In addition, the ratio between triglycerides and HDL, a strong predictor of cardiovascular events, was differentially most improved in the bypass patients (38.5%), although improvement was also seen in both band (20.6%) and sleeve (35.2%) groups.
The investigators also sought to correlate each bariatric procedure’s resultant weight loss to improvement in specific cardiac risk factors. Only bypass was found to have a correlate between weight loss and total cholesterol and LDL reduction.
The triglyceride/HDL ratio improved with weight loss in both the bypass and band surgical groups. However, patients over age 50 and with a BMI greater than 50 kg/m2 had the least improvement in this ratio.
Reduction in CRP level was not found to be related to weight loss for any of the procedures, although CRP did improve substantially after all three operations, primarily in bypass patients. In response to a question from an audience member, Mr. Crowe, a medical student, said this was probably because of changes in patient lifestyle, diet, and medications, as well as smoking cessation, postoperatively.
"When someone comes in for a bariatric procedure, they’re not just receiving the surgery, they are changing a lot about their life," said Mr. Crowe. "Those changes could, in effect, decrease the CRP levels after surgery, without it being weight loss–dependent."
Mr. Crowe reported no relevant disclosures. His coinvestigators reported serving as consultants to Ethicon and Covidien.
WASHINGTON – One year out from surgery, gastric bypass, gastric sleeve, and gastric banding all showed considerable reductions in cardiac risk factors, but gastric bypass showed the greatest risk reduction of all three, as well as greater improvement in body mass index, according to a study presented at this year’s annual clinical congress of the American College of Surgeons.
Baseline and 1-year postoperative data were collected on 1,398 consecutive bariatric surgery patients by Christopher S. Crowe and his colleagues at Stanford (Calif.) University. The investigators sought to evaluate each type of surgery’s effect on biochemical cardiovascular risk factors. The follow-up rate at 12 months was 77%.
The values measured were hemoglobin A1c, fasting insulin, high-density lipoprotein (HDL), low-density lipoprotein (LDL), total cholesterol, triglycerides, high-sensitivity C-reactive protein (CRP), homocysteine, and lipoprotein (a).
Across the three groups, bypass patients tended to be younger by 1-2 years (mean age of this group was 44.3 years), and they had a higher baseline body mass index on average.
Excess weight loss after 1 year averaged 75% in the bypass patients, 55% in the patients with a sleeve, and 40% in those with a band.
When analyzing laboratory values for each group, the investigators found that fasting insulin levels were notably improved in all three groups; but at an improvement rate of 67.0%, the bypass patients had more than double the improvement of the gastric-band patients, while the gastric-sleeve patients showed a 63.7% improvement rate.
The CRP levels also improved dramatically in the bypass patients (67.1%), especially when compared with the band (21.2%) and sleeve (26.3%) groups. In addition, the ratio between triglycerides and HDL, a strong predictor of cardiovascular events, was differentially most improved in the bypass patients (38.5%), although improvement was also seen in both band (20.6%) and sleeve (35.2%) groups.
The investigators also sought to correlate each bariatric procedure’s resultant weight loss to improvement in specific cardiac risk factors. Only bypass was found to have a correlate between weight loss and total cholesterol and LDL reduction.
The triglyceride/HDL ratio improved with weight loss in both the bypass and band surgical groups. However, patients over age 50 and with a BMI greater than 50 kg/m2 had the least improvement in this ratio.
Reduction in CRP level was not found to be related to weight loss for any of the procedures, although CRP did improve substantially after all three operations, primarily in bypass patients. In response to a question from an audience member, Mr. Crowe, a medical student, said this was probably because of changes in patient lifestyle, diet, and medications, as well as smoking cessation, postoperatively.
"When someone comes in for a bariatric procedure, they’re not just receiving the surgery, they are changing a lot about their life," said Mr. Crowe. "Those changes could, in effect, decrease the CRP levels after surgery, without it being weight loss–dependent."
Mr. Crowe reported no relevant disclosures. His coinvestigators reported serving as consultants to Ethicon and Covidien.
WASHINGTON – One year out from surgery, gastric bypass, gastric sleeve, and gastric banding all showed considerable reductions in cardiac risk factors, but gastric bypass showed the greatest risk reduction of all three, as well as greater improvement in body mass index, according to a study presented at this year’s annual clinical congress of the American College of Surgeons.
Baseline and 1-year postoperative data were collected on 1,398 consecutive bariatric surgery patients by Christopher S. Crowe and his colleagues at Stanford (Calif.) University. The investigators sought to evaluate each type of surgery’s effect on biochemical cardiovascular risk factors. The follow-up rate at 12 months was 77%.
The values measured were hemoglobin A1c, fasting insulin, high-density lipoprotein (HDL), low-density lipoprotein (LDL), total cholesterol, triglycerides, high-sensitivity C-reactive protein (CRP), homocysteine, and lipoprotein (a).
Across the three groups, bypass patients tended to be younger by 1-2 years (mean age of this group was 44.3 years), and they had a higher baseline body mass index on average.
Excess weight loss after 1 year averaged 75% in the bypass patients, 55% in the patients with a sleeve, and 40% in those with a band.
When analyzing laboratory values for each group, the investigators found that fasting insulin levels were notably improved in all three groups; but at an improvement rate of 67.0%, the bypass patients had more than double the improvement of the gastric-band patients, while the gastric-sleeve patients showed a 63.7% improvement rate.
The CRP levels also improved dramatically in the bypass patients (67.1%), especially when compared with the band (21.2%) and sleeve (26.3%) groups. In addition, the ratio between triglycerides and HDL, a strong predictor of cardiovascular events, was differentially most improved in the bypass patients (38.5%), although improvement was also seen in both band (20.6%) and sleeve (35.2%) groups.
The investigators also sought to correlate each bariatric procedure’s resultant weight loss to improvement in specific cardiac risk factors. Only bypass was found to have a correlate between weight loss and total cholesterol and LDL reduction.
The triglyceride/HDL ratio improved with weight loss in both the bypass and band surgical groups. However, patients over age 50 and with a BMI greater than 50 kg/m2 had the least improvement in this ratio.
Reduction in CRP level was not found to be related to weight loss for any of the procedures, although CRP did improve substantially after all three operations, primarily in bypass patients. In response to a question from an audience member, Mr. Crowe, a medical student, said this was probably because of changes in patient lifestyle, diet, and medications, as well as smoking cessation, postoperatively.
"When someone comes in for a bariatric procedure, they’re not just receiving the surgery, they are changing a lot about their life," said Mr. Crowe. "Those changes could, in effect, decrease the CRP levels after surgery, without it being weight loss–dependent."
Mr. Crowe reported no relevant disclosures. His coinvestigators reported serving as consultants to Ethicon and Covidien.
AT THE ACS CLINICAL CONGRESS
Major finding: Gastric bypass showed greater improvement in all cardiovascular risk factors 1 year postoperatively.
Data source: Prospective analysis of 1,398 consecutive bariatric procedures (gastric bypass, sleeve gastrectomy, gastric banding) at baseline and 1 year postoperatively.
Disclosures: Mr. Crowe reported no relevant disclosures. His coinvestigators reported serving as consultants to Ethicon and Covidien.
Knee replacement delayed by hyaluronic acid injections
SAN DIEGO – Viscosupplementation using hyaluronic acid injections delayed total knee replacement for patients with knee osteoarthritis by up to a median 2.6 years in a retrospective observational study.
The study, involving analysis of a large commercial health insurance claims database (Truven MarketScan), included all 16,529 patients with knee osteoarthritis (OA) who made their first visit to a specialist for the condition in 2008-2011 and who eventually went on to total knee replacement surgery.
Among this group were 4,178 knee OA patients who underwent one or more courses of treatment with any of the Food and Drug Administration–approved injectable hyaluronic acid products. A total of 3,647 of these patients were successfully matched to controls with knee OA who had total knee replacement surgery without any prior hyaluronic acid injections, Dr. Roy D. Altman explained at the annual meeting of the American College of Rheumatology.
The matching process relied upon propensity scores based on age, sex, physician specialty, diagnosis at the first specialist visit, and year. Therein lays a significant study limitation: These variables provide only limited ability to adjust for any differences in baseline knee OA severity that might have existed between patients who did or didn’t receive hyaluronic acid injections. Nor can an observational study establish causality, observed Dr. Altman, professor emeritus of medicine at the University of California, Los Angeles.
That being said, the study demonstrated a strong dose-dependent relationship between viscosupplementation and time from first specialist visit to knee replacement surgery, he noted.
Seventy-nine percent of patients who got hyaluronic acid injections received a single course consisting of either one injection or a series of injections, depending upon the specific product. Those patients experienced a median 233-day increase in the time to surgery, compared with matched controls who didn’t get hyaluronic acid injections.
Moreover, the 16% of viscosupplementation recipients who underwent a second round of treatment further delayed their median time from first specialist visit to total knee replacement by an additional 7 months. And that pattern continued in the relatively small numbers of patients who underwent three or more courses of viscosupplementation: Each round of hyaluronic acid injections brought a roughly 7-month further delay in time to surgery, out to a total of 2.6 years.
The study was sponsored by Johnson & Johnson. Dr. Altman reported having no financial conflicts.
SAN DIEGO – Viscosupplementation using hyaluronic acid injections delayed total knee replacement for patients with knee osteoarthritis by up to a median 2.6 years in a retrospective observational study.
The study, involving analysis of a large commercial health insurance claims database (Truven MarketScan), included all 16,529 patients with knee osteoarthritis (OA) who made their first visit to a specialist for the condition in 2008-2011 and who eventually went on to total knee replacement surgery.
Among this group were 4,178 knee OA patients who underwent one or more courses of treatment with any of the Food and Drug Administration–approved injectable hyaluronic acid products. A total of 3,647 of these patients were successfully matched to controls with knee OA who had total knee replacement surgery without any prior hyaluronic acid injections, Dr. Roy D. Altman explained at the annual meeting of the American College of Rheumatology.
The matching process relied upon propensity scores based on age, sex, physician specialty, diagnosis at the first specialist visit, and year. Therein lays a significant study limitation: These variables provide only limited ability to adjust for any differences in baseline knee OA severity that might have existed between patients who did or didn’t receive hyaluronic acid injections. Nor can an observational study establish causality, observed Dr. Altman, professor emeritus of medicine at the University of California, Los Angeles.
That being said, the study demonstrated a strong dose-dependent relationship between viscosupplementation and time from first specialist visit to knee replacement surgery, he noted.
Seventy-nine percent of patients who got hyaluronic acid injections received a single course consisting of either one injection or a series of injections, depending upon the specific product. Those patients experienced a median 233-day increase in the time to surgery, compared with matched controls who didn’t get hyaluronic acid injections.
Moreover, the 16% of viscosupplementation recipients who underwent a second round of treatment further delayed their median time from first specialist visit to total knee replacement by an additional 7 months. And that pattern continued in the relatively small numbers of patients who underwent three or more courses of viscosupplementation: Each round of hyaluronic acid injections brought a roughly 7-month further delay in time to surgery, out to a total of 2.6 years.
The study was sponsored by Johnson & Johnson. Dr. Altman reported having no financial conflicts.
SAN DIEGO – Viscosupplementation using hyaluronic acid injections delayed total knee replacement for patients with knee osteoarthritis by up to a median 2.6 years in a retrospective observational study.
The study, involving analysis of a large commercial health insurance claims database (Truven MarketScan), included all 16,529 patients with knee osteoarthritis (OA) who made their first visit to a specialist for the condition in 2008-2011 and who eventually went on to total knee replacement surgery.
Among this group were 4,178 knee OA patients who underwent one or more courses of treatment with any of the Food and Drug Administration–approved injectable hyaluronic acid products. A total of 3,647 of these patients were successfully matched to controls with knee OA who had total knee replacement surgery without any prior hyaluronic acid injections, Dr. Roy D. Altman explained at the annual meeting of the American College of Rheumatology.
The matching process relied upon propensity scores based on age, sex, physician specialty, diagnosis at the first specialist visit, and year. Therein lays a significant study limitation: These variables provide only limited ability to adjust for any differences in baseline knee OA severity that might have existed between patients who did or didn’t receive hyaluronic acid injections. Nor can an observational study establish causality, observed Dr. Altman, professor emeritus of medicine at the University of California, Los Angeles.
That being said, the study demonstrated a strong dose-dependent relationship between viscosupplementation and time from first specialist visit to knee replacement surgery, he noted.
Seventy-nine percent of patients who got hyaluronic acid injections received a single course consisting of either one injection or a series of injections, depending upon the specific product. Those patients experienced a median 233-day increase in the time to surgery, compared with matched controls who didn’t get hyaluronic acid injections.
Moreover, the 16% of viscosupplementation recipients who underwent a second round of treatment further delayed their median time from first specialist visit to total knee replacement by an additional 7 months. And that pattern continued in the relatively small numbers of patients who underwent three or more courses of viscosupplementation: Each round of hyaluronic acid injections brought a roughly 7-month further delay in time to surgery, out to a total of 2.6 years.
The study was sponsored by Johnson & Johnson. Dr. Altman reported having no financial conflicts.
AT THE ACR ANNUAL MEETING
Major finding: Patients with knee osteoarthritis who eventually underwent total knee replacement had their surgery delayed by a median 233 days if they received one course of viscosupplementation using hyaluronic acid injections. For those who received more than one round of injections, each additional course brought a further average 7-month delay in time to surgery out to 2.6 years.
Data source: Retrospective observational study involving a large commercial health insurance claims database matched 3,647 patients with knee osteoarthritis who underwent total knee replacement after receiving one or more courses of hyaluronic acid injections to an equal number who didn’t get hyaluronic acid injections prior to surgery.
Disclosures: The study was sponsored by Johnson & Johnson. The presenter reported having no financial conflicts.
Younger adults with brain metastases survive longer with radiosurgery alone
ATLANTA – Younger adults with one to three brain metastases survive longer when they are treated with stereotactic radiosurgery alone rather than whole-brain radiation therapy or a combination of both modalities, researchers reported at the annual meeting of the American Society for Radiation Oncology.
Among patients aged 35-50 years, stereotactic radiosurgery (SRS) alone was associated with hazard ratios (HR) for death ranging from 0.46 to 0.64, compared with an age-matched cohort treated with a combination of SRS and whole-brain radiation therapy (WBRT), based on a meta-analysis of data on 389 individual patients in three randomized clinical trials.
For local control, however, the data show a benefit for combined SRS and WBRT. For control of distant brain metastases, the data indicate a benefit for the combined therapies, but only among patients aged 55 years and older, reported Dr. Arjun Sahgal, associate professor of radiation oncology at the University of Toronto.
"Our overall survival results favoring radiosurgery alone in younger patients may be explained by the lack of benefit of whole-brain radiation with respect to distant brain control in this cohort, while still exposing them to the harms of whole-brain radiation with respect to memory function and quality of life," he said.
Dr. Sahgal and his colleagues had previously published an aggregate meta-analysis showing that WBRT and SRS improved distant and local brain control but without overall survival benefit compared with SRS alone.
The current study looked at the raw, individual patient data from the three randomized controlled trials included in the original aggregate analysis. The trials included a 2006 study of 132 patients with an endpoint of brain tumor recurrence, a 2009 trial looking at the effect of SRS/WBRT on neurocognitive function in 58 patients, and a 2011 study examining the effect of adjuvant SRS on World Health Organization performance status scores.
The overall median time to local failure in the trials was 6.6 months for SRS alone, compared with 7.7 months for SRS/WBRT. Time to distant failure was also shorter with SRS alone, at a median of 4.7 vs. 7.7 months, respectively. Median time to death, however, was longer with SRS, at 10 vs. 8.2 months.
In a multivariate model for overall survival, the HR was 0.46 for patients at age 35 years, 0.52 at age 40, 0.58 at age 45, and 0.64 at age 50; all hazard ratios had significant confidence intervals. For patients aged 55 years and older, however, the HR for overall survival was not significant.
Patients with only one metastasis had a significantly lower risk of dying, compared with those who had two or three metastases (HR, 0.72).
The risk of local failure was significantly greater with SRS alone for patients aged 45-70.
The risk of new distant metastases was significant with SRS alone for patients aged 55 years and older, and was significantly lower for patients with one metastasis (HR, 0.63) vs. two or more metastases.
Salvage therapy was performed in 28% of patients who underwent SRS alone and 12% of those who received the combined therapies. Distant brain failures occurred in 54% of those in the SRS alone group, compared with 34% of those in the SRS/WBRT group.
Patients who underwent salvage therapy had significantly greater survival rates than those who did not, and this effect did not vary significantly by age, Dr. Sahgal reported.
The authors did not report specific funding sources. Dr. Sahgal reported having no relevant financial disclosures.
ATLANTA – Younger adults with one to three brain metastases survive longer when they are treated with stereotactic radiosurgery alone rather than whole-brain radiation therapy or a combination of both modalities, researchers reported at the annual meeting of the American Society for Radiation Oncology.
Among patients aged 35-50 years, stereotactic radiosurgery (SRS) alone was associated with hazard ratios (HR) for death ranging from 0.46 to 0.64, compared with an age-matched cohort treated with a combination of SRS and whole-brain radiation therapy (WBRT), based on a meta-analysis of data on 389 individual patients in three randomized clinical trials.
For local control, however, the data show a benefit for combined SRS and WBRT. For control of distant brain metastases, the data indicate a benefit for the combined therapies, but only among patients aged 55 years and older, reported Dr. Arjun Sahgal, associate professor of radiation oncology at the University of Toronto.
"Our overall survival results favoring radiosurgery alone in younger patients may be explained by the lack of benefit of whole-brain radiation with respect to distant brain control in this cohort, while still exposing them to the harms of whole-brain radiation with respect to memory function and quality of life," he said.
Dr. Sahgal and his colleagues had previously published an aggregate meta-analysis showing that WBRT and SRS improved distant and local brain control but without overall survival benefit compared with SRS alone.
The current study looked at the raw, individual patient data from the three randomized controlled trials included in the original aggregate analysis. The trials included a 2006 study of 132 patients with an endpoint of brain tumor recurrence, a 2009 trial looking at the effect of SRS/WBRT on neurocognitive function in 58 patients, and a 2011 study examining the effect of adjuvant SRS on World Health Organization performance status scores.
The overall median time to local failure in the trials was 6.6 months for SRS alone, compared with 7.7 months for SRS/WBRT. Time to distant failure was also shorter with SRS alone, at a median of 4.7 vs. 7.7 months, respectively. Median time to death, however, was longer with SRS, at 10 vs. 8.2 months.
In a multivariate model for overall survival, the HR was 0.46 for patients at age 35 years, 0.52 at age 40, 0.58 at age 45, and 0.64 at age 50; all hazard ratios had significant confidence intervals. For patients aged 55 years and older, however, the HR for overall survival was not significant.
Patients with only one metastasis had a significantly lower risk of dying, compared with those who had two or three metastases (HR, 0.72).
The risk of local failure was significantly greater with SRS alone for patients aged 45-70.
The risk of new distant metastases was significant with SRS alone for patients aged 55 years and older, and was significantly lower for patients with one metastasis (HR, 0.63) vs. two or more metastases.
Salvage therapy was performed in 28% of patients who underwent SRS alone and 12% of those who received the combined therapies. Distant brain failures occurred in 54% of those in the SRS alone group, compared with 34% of those in the SRS/WBRT group.
Patients who underwent salvage therapy had significantly greater survival rates than those who did not, and this effect did not vary significantly by age, Dr. Sahgal reported.
The authors did not report specific funding sources. Dr. Sahgal reported having no relevant financial disclosures.
ATLANTA – Younger adults with one to three brain metastases survive longer when they are treated with stereotactic radiosurgery alone rather than whole-brain radiation therapy or a combination of both modalities, researchers reported at the annual meeting of the American Society for Radiation Oncology.
Among patients aged 35-50 years, stereotactic radiosurgery (SRS) alone was associated with hazard ratios (HR) for death ranging from 0.46 to 0.64, compared with an age-matched cohort treated with a combination of SRS and whole-brain radiation therapy (WBRT), based on a meta-analysis of data on 389 individual patients in three randomized clinical trials.
For local control, however, the data show a benefit for combined SRS and WBRT. For control of distant brain metastases, the data indicate a benefit for the combined therapies, but only among patients aged 55 years and older, reported Dr. Arjun Sahgal, associate professor of radiation oncology at the University of Toronto.
"Our overall survival results favoring radiosurgery alone in younger patients may be explained by the lack of benefit of whole-brain radiation with respect to distant brain control in this cohort, while still exposing them to the harms of whole-brain radiation with respect to memory function and quality of life," he said.
Dr. Sahgal and his colleagues had previously published an aggregate meta-analysis showing that WBRT and SRS improved distant and local brain control but without overall survival benefit compared with SRS alone.
The current study looked at the raw, individual patient data from the three randomized controlled trials included in the original aggregate analysis. The trials included a 2006 study of 132 patients with an endpoint of brain tumor recurrence, a 2009 trial looking at the effect of SRS/WBRT on neurocognitive function in 58 patients, and a 2011 study examining the effect of adjuvant SRS on World Health Organization performance status scores.
The overall median time to local failure in the trials was 6.6 months for SRS alone, compared with 7.7 months for SRS/WBRT. Time to distant failure was also shorter with SRS alone, at a median of 4.7 vs. 7.7 months, respectively. Median time to death, however, was longer with SRS, at 10 vs. 8.2 months.
In a multivariate model for overall survival, the HR was 0.46 for patients at age 35 years, 0.52 at age 40, 0.58 at age 45, and 0.64 at age 50; all hazard ratios had significant confidence intervals. For patients aged 55 years and older, however, the HR for overall survival was not significant.
Patients with only one metastasis had a significantly lower risk of dying, compared with those who had two or three metastases (HR, 0.72).
The risk of local failure was significantly greater with SRS alone for patients aged 45-70.
The risk of new distant metastases was significant with SRS alone for patients aged 55 years and older, and was significantly lower for patients with one metastasis (HR, 0.63) vs. two or more metastases.
Salvage therapy was performed in 28% of patients who underwent SRS alone and 12% of those who received the combined therapies. Distant brain failures occurred in 54% of those in the SRS alone group, compared with 34% of those in the SRS/WBRT group.
Patients who underwent salvage therapy had significantly greater survival rates than those who did not, and this effect did not vary significantly by age, Dr. Sahgal reported.
The authors did not report specific funding sources. Dr. Sahgal reported having no relevant financial disclosures.
AT THE ASTRO ANNUAL MEETING
Major finding: Stereotactic radiosurgery was associated with significantly longer overall survival among patients age 50 years and younger (hazard ratios from 0.46 to 0.64).
Data source: Meta-analysis of individual patient data from three randomized controlled clinical trials enrolling a total of 389 patients.
Disclosures: The authors did not report specific funding sources. Dr. Sahgal reported having no relevant financial disclosures.
One in five women undergoes urogynecologic surgery
LAS VEGAS – Among women with private health insurance in this country, the lifetime risk of surgery for either stress urinary incontinence or pelvic organ prolapse stands at 20.2%, results from a large analysis demonstrated.
"This means that one out of every five women in the United States will undergo a urogynecologic procedure by the age of 80," Dr. Jennifer M. Wu said at the annual meeting of the American Urogynecologic Society. "This high rate highlights the public health burden of pelvic floor disorders, exposes the need for improved prevention strategies, and underscores the importance of effective long-term surgical interventions."
A commonly referenced statistic is that the lifetime risk of surgery for either stress urinary incontinence (SUI) or pelvic organ prolapse (POP) is 11%, but this was based on a study of 395 patients who underwent surgery in 1995 in the Northwest (Obstet. Gynecol. 1997;89:501-6).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Since 1995, several factors may have increased this risk. These include "the integration of midurethral slings and vaginal mesh prolapse procedures, regional differences in surgery rates, and the greater number of elderly women," explained Dr. Wu of the department of obstetrics and gynecology and the Center for Women’s Health Research at the University of North Carolina at Chapel Hill. "Thus, the objective of our study was to estimate the cumulative risk of SUI or POP surgery over a woman’s lifetime until the age of 80."
The researchers used the Market Scan Commercial Claims and Encounters database with the Medicare Supplemental, which contains de-identified inpatient and outpatient claims data from about 100 employer-based insurance plans in the United States. They included women aged 18 years and older and identified any SUI or POP surgery performed between 2007 and 2011 based on CPT codes. This resulted in a study population of 51.8 million women. Of these, 311,070 underwent surgery for either SUI or POP.
To estimate age-specific incidence rates for each age between 18 and 80 years, Dr. Wu and her associates multiplied age-specific prevalence rates by the proportion of cases that were incident. To estimate the proportion of all procedures that were repeat surgeries, they evaluated women who had a SUI or POP surgery in 2011 and "looked back" 5 years to identify prior surgeries. Finally, they used Monte Carlo simulations to determine the cumulative lifetime risk of either incontinence or prolapse surgery with 95% confidence intervals.
Dr. Wu reported that the cumulative lifetime risk of either SUI or POP surgery was 20.2% (95% CI, 19.2%-21.1%). The cumulative lifetime risk of SUI was 14.5% (95% CI, 13.4%-15.5%), and the risk of POP surgery was 13.7% (95% CI, 12.6%-14.8%). The cumulative lifetime risk for SUI or POP surgery increased with age in a stepwise fashion, from 11.4% by age 60 years to 15.9% by age 70 and 20.2% by age 80, she noted.
To place the risk of any primary surgery for SUI or POP in perspective, Dr. Wu drew a comparison with the lifetime risk estimates for colon cancer (4.8%), lung cancer (6.3%), breast cancer (14.8%), and any type of cancer (41.3%). "Granted, incontinence and prolapse are not life-threatening conditions, but this 20% risk highlights how common surgeries are for pelvic floor disorders, despite the fact that they’re widely underrecognized," she noted.
She acknowledged certain limitations of the study, including the fact that she and her associates were unable to review actual medical records to confirm the rate of prior surgeries. "In addition, we assumed a closed cohort and no competing risks such that all women live until the age of 80," she said. "Also, these results reflect women with private insurance and may not be generalizable to those who are uninsured or underinsured."
Dr. Wu disclosed that she is a consultant for Procter & Gamble.
Dr. David M. Jaspan comments: Direct to consumer advertising has enabled more women to feel comfortable discussing incontinence with their health care providers, which is great. Industry had inundated general ob.gyn. offices with the opportunity to attend short courses to learn "mesh procedures," which may not have been great. Therefore, I am not surprised that the numbers of women with private insurance undergoing urogynecologic surgery are so high.
These advanced procedures should be undertaken by those surgeons with sufficient training and experience to properly counsel women about the risk and benefit of a native tissue repair, compared with a graft placement. In addition, surgeons should have a volume of experience and training that qualifies them to provide this detailed counseling and should perform an appropriate preoperative evaluation to determine the absolute need for a procedure. More procedures may have brought more risk to women.
I applaud the American College of Obstetricians and Gynecologists for the 2011 ACOG Committee Opinion #513, which says, "Surgeons performing complex pelvic floor reconstructive surgery should have adequate experience and training in native tissue repairs as well as repairs using mesh augmentation specific to each device, should have a thorough understanding of pelvic anatomy, and should be able to counsel patients regarding the risk/benefit ratio on the use of mesh compared with native tissue repairs" (Obstet. Gynecol. 2011;118:1459-64).
In its 2011 Safety Communication, the Food and Drug Administration said that transvaginal placement of surgical mesh for POP is of "continuing serious concern." In the document, the FDA restated its 2008 recommendation that health care providers "inform patients about the potential for serious complications and the effect on quality of life, including pain during sexual intercourse, scarring, and narrowing of the vaginal wall in POP repair using surgical mesh; and provide a copy of the patient labeling from the surgical mesh manufacturer if available."
The FDA also made several new recommendations for health care providers in its report:
- Surgeons should recognize that, in most cases, POP can be treated successfully without mesh, thus avoiding the risk of mesh-related complications.
- Surgeons should choose mesh surgery only after weighing the risks and benefits of surgery with mesh versus all surgical and nonsurgical alternatives.
- Removal of mesh may involve multiple surgical procedures and significantly impair the patient's quality of life. Complete removal of mesh may not be possible and may not result in complete resolution of complications, including pain.
Patient counseling needs to include discussion of alternative native tissue repair and the fact that synthetic mesh is permanent, according to ACOG. Other issues to discuss include that vaginal bleeding, pain, and dyspareunia may be related to vaginal mesh; Patients reporting such symptoms should undergo a thorough vaginal exam, including an exam under anesthesia if necessary.
Dr. David M. Jaspan is chairman of ob.gyn. for the Einstein Health Care Network in Philadelphia. He was asked to comment on Dr. Wu's study. Dr. Jaspan said that he had no financial disclosures.
Remember to ask about pelvic floor issues
Dr. Meadow Maze Good comments: This is a well done and important study that highlights the magnitude of pelvic floor disorders in women. Previous studies indicate that women delay or do not seek care for pelvic floor disorders and incorrectly think that these problems are a normal result of aging.
These data presented at the American Urogynecologic Society meeting by Dr. Wu and her colleagues reinforce the need for increased public awareness and education regarding pelvic floor disorders as well as available treatment options, including nonsurgical and surgical options. Additionally, this study points out that the physicians treating women of all ages including the primary care provider (family practice physicians and obstetrician/gynecologists) should query women about possible pelvic floor symptoms, including incontinence, prolapse, and sexual function.
It is especially important for the ob.gyn. to ask their patient about these symptoms if there is planning underway for a hysterectomy for other causes. This is an exciting time for the newly board-certifiable field of female pelvic medicine and reconstructive surgery. As the aging population of women with prolapse and incontinence increases, fellowship programs are graduating physicians knowledgeable in this specific field who are dedicated to taking care of women with these treatable conditions.
Meadow Maze Good, D.O., is a fellow in female pelvic medicine and reconstructive surgery at the University of Texas Southwestern Medical Center, Dallas. Dr. Good, who is also the chair of the Junior Fellow Congress Advisory Council of the American Congress of Obstetricians and Gynecologists, was asked to comment on Dr. Wu's study. She said she had no relevant financial disclosures.
Dr. David M. Jaspan comments: Direct to consumer advertising has enabled more women to feel comfortable discussing incontinence with their health care providers, which is great. Industry had inundated general ob.gyn. offices with the opportunity to attend short courses to learn "mesh procedures," which may not have been great. Therefore, I am not surprised that the numbers of women with private insurance undergoing urogynecologic surgery are so high.
These advanced procedures should be undertaken by those surgeons with sufficient training and experience to properly counsel women about the risk and benefit of a native tissue repair, compared with a graft placement. In addition, surgeons should have a volume of experience and training that qualifies them to provide this detailed counseling and should perform an appropriate preoperative evaluation to determine the absolute need for a procedure. More procedures may have brought more risk to women.
I applaud the American College of Obstetricians and Gynecologists for the 2011 ACOG Committee Opinion #513, which says, "Surgeons performing complex pelvic floor reconstructive surgery should have adequate experience and training in native tissue repairs as well as repairs using mesh augmentation specific to each device, should have a thorough understanding of pelvic anatomy, and should be able to counsel patients regarding the risk/benefit ratio on the use of mesh compared with native tissue repairs" (Obstet. Gynecol. 2011;118:1459-64).
In its 2011 Safety Communication, the Food and Drug Administration said that transvaginal placement of surgical mesh for POP is of "continuing serious concern." In the document, the FDA restated its 2008 recommendation that health care providers "inform patients about the potential for serious complications and the effect on quality of life, including pain during sexual intercourse, scarring, and narrowing of the vaginal wall in POP repair using surgical mesh; and provide a copy of the patient labeling from the surgical mesh manufacturer if available."
The FDA also made several new recommendations for health care providers in its report:
- Surgeons should recognize that, in most cases, POP can be treated successfully without mesh, thus avoiding the risk of mesh-related complications.
- Surgeons should choose mesh surgery only after weighing the risks and benefits of surgery with mesh versus all surgical and nonsurgical alternatives.
- Removal of mesh may involve multiple surgical procedures and significantly impair the patient's quality of life. Complete removal of mesh may not be possible and may not result in complete resolution of complications, including pain.
Patient counseling needs to include discussion of alternative native tissue repair and the fact that synthetic mesh is permanent, according to ACOG. Other issues to discuss include that vaginal bleeding, pain, and dyspareunia may be related to vaginal mesh; Patients reporting such symptoms should undergo a thorough vaginal exam, including an exam under anesthesia if necessary.
Dr. David M. Jaspan is chairman of ob.gyn. for the Einstein Health Care Network in Philadelphia. He was asked to comment on Dr. Wu's study. Dr. Jaspan said that he had no financial disclosures.
Remember to ask about pelvic floor issues
Dr. Meadow Maze Good comments: This is a well done and important study that highlights the magnitude of pelvic floor disorders in women. Previous studies indicate that women delay or do not seek care for pelvic floor disorders and incorrectly think that these problems are a normal result of aging.
These data presented at the American Urogynecologic Society meeting by Dr. Wu and her colleagues reinforce the need for increased public awareness and education regarding pelvic floor disorders as well as available treatment options, including nonsurgical and surgical options. Additionally, this study points out that the physicians treating women of all ages including the primary care provider (family practice physicians and obstetrician/gynecologists) should query women about possible pelvic floor symptoms, including incontinence, prolapse, and sexual function.
It is especially important for the ob.gyn. to ask their patient about these symptoms if there is planning underway for a hysterectomy for other causes. This is an exciting time for the newly board-certifiable field of female pelvic medicine and reconstructive surgery. As the aging population of women with prolapse and incontinence increases, fellowship programs are graduating physicians knowledgeable in this specific field who are dedicated to taking care of women with these treatable conditions.
Meadow Maze Good, D.O., is a fellow in female pelvic medicine and reconstructive surgery at the University of Texas Southwestern Medical Center, Dallas. Dr. Good, who is also the chair of the Junior Fellow Congress Advisory Council of the American Congress of Obstetricians and Gynecologists, was asked to comment on Dr. Wu's study. She said she had no relevant financial disclosures.
Dr. David M. Jaspan comments: Direct to consumer advertising has enabled more women to feel comfortable discussing incontinence with their health care providers, which is great. Industry had inundated general ob.gyn. offices with the opportunity to attend short courses to learn "mesh procedures," which may not have been great. Therefore, I am not surprised that the numbers of women with private insurance undergoing urogynecologic surgery are so high.
These advanced procedures should be undertaken by those surgeons with sufficient training and experience to properly counsel women about the risk and benefit of a native tissue repair, compared with a graft placement. In addition, surgeons should have a volume of experience and training that qualifies them to provide this detailed counseling and should perform an appropriate preoperative evaluation to determine the absolute need for a procedure. More procedures may have brought more risk to women.
I applaud the American College of Obstetricians and Gynecologists for the 2011 ACOG Committee Opinion #513, which says, "Surgeons performing complex pelvic floor reconstructive surgery should have adequate experience and training in native tissue repairs as well as repairs using mesh augmentation specific to each device, should have a thorough understanding of pelvic anatomy, and should be able to counsel patients regarding the risk/benefit ratio on the use of mesh compared with native tissue repairs" (Obstet. Gynecol. 2011;118:1459-64).
In its 2011 Safety Communication, the Food and Drug Administration said that transvaginal placement of surgical mesh for POP is of "continuing serious concern." In the document, the FDA restated its 2008 recommendation that health care providers "inform patients about the potential for serious complications and the effect on quality of life, including pain during sexual intercourse, scarring, and narrowing of the vaginal wall in POP repair using surgical mesh; and provide a copy of the patient labeling from the surgical mesh manufacturer if available."
The FDA also made several new recommendations for health care providers in its report:
- Surgeons should recognize that, in most cases, POP can be treated successfully without mesh, thus avoiding the risk of mesh-related complications.
- Surgeons should choose mesh surgery only after weighing the risks and benefits of surgery with mesh versus all surgical and nonsurgical alternatives.
- Removal of mesh may involve multiple surgical procedures and significantly impair the patient's quality of life. Complete removal of mesh may not be possible and may not result in complete resolution of complications, including pain.
Patient counseling needs to include discussion of alternative native tissue repair and the fact that synthetic mesh is permanent, according to ACOG. Other issues to discuss include that vaginal bleeding, pain, and dyspareunia may be related to vaginal mesh; Patients reporting such symptoms should undergo a thorough vaginal exam, including an exam under anesthesia if necessary.
Dr. David M. Jaspan is chairman of ob.gyn. for the Einstein Health Care Network in Philadelphia. He was asked to comment on Dr. Wu's study. Dr. Jaspan said that he had no financial disclosures.
Remember to ask about pelvic floor issues
Dr. Meadow Maze Good comments: This is a well done and important study that highlights the magnitude of pelvic floor disorders in women. Previous studies indicate that women delay or do not seek care for pelvic floor disorders and incorrectly think that these problems are a normal result of aging.
These data presented at the American Urogynecologic Society meeting by Dr. Wu and her colleagues reinforce the need for increased public awareness and education regarding pelvic floor disorders as well as available treatment options, including nonsurgical and surgical options. Additionally, this study points out that the physicians treating women of all ages including the primary care provider (family practice physicians and obstetrician/gynecologists) should query women about possible pelvic floor symptoms, including incontinence, prolapse, and sexual function.
It is especially important for the ob.gyn. to ask their patient about these symptoms if there is planning underway for a hysterectomy for other causes. This is an exciting time for the newly board-certifiable field of female pelvic medicine and reconstructive surgery. As the aging population of women with prolapse and incontinence increases, fellowship programs are graduating physicians knowledgeable in this specific field who are dedicated to taking care of women with these treatable conditions.
Meadow Maze Good, D.O., is a fellow in female pelvic medicine and reconstructive surgery at the University of Texas Southwestern Medical Center, Dallas. Dr. Good, who is also the chair of the Junior Fellow Congress Advisory Council of the American Congress of Obstetricians and Gynecologists, was asked to comment on Dr. Wu's study. She said she had no relevant financial disclosures.
LAS VEGAS – Among women with private health insurance in this country, the lifetime risk of surgery for either stress urinary incontinence or pelvic organ prolapse stands at 20.2%, results from a large analysis demonstrated.
"This means that one out of every five women in the United States will undergo a urogynecologic procedure by the age of 80," Dr. Jennifer M. Wu said at the annual meeting of the American Urogynecologic Society. "This high rate highlights the public health burden of pelvic floor disorders, exposes the need for improved prevention strategies, and underscores the importance of effective long-term surgical interventions."
A commonly referenced statistic is that the lifetime risk of surgery for either stress urinary incontinence (SUI) or pelvic organ prolapse (POP) is 11%, but this was based on a study of 395 patients who underwent surgery in 1995 in the Northwest (Obstet. Gynecol. 1997;89:501-6).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Since 1995, several factors may have increased this risk. These include "the integration of midurethral slings and vaginal mesh prolapse procedures, regional differences in surgery rates, and the greater number of elderly women," explained Dr. Wu of the department of obstetrics and gynecology and the Center for Women’s Health Research at the University of North Carolina at Chapel Hill. "Thus, the objective of our study was to estimate the cumulative risk of SUI or POP surgery over a woman’s lifetime until the age of 80."
The researchers used the Market Scan Commercial Claims and Encounters database with the Medicare Supplemental, which contains de-identified inpatient and outpatient claims data from about 100 employer-based insurance plans in the United States. They included women aged 18 years and older and identified any SUI or POP surgery performed between 2007 and 2011 based on CPT codes. This resulted in a study population of 51.8 million women. Of these, 311,070 underwent surgery for either SUI or POP.
To estimate age-specific incidence rates for each age between 18 and 80 years, Dr. Wu and her associates multiplied age-specific prevalence rates by the proportion of cases that were incident. To estimate the proportion of all procedures that were repeat surgeries, they evaluated women who had a SUI or POP surgery in 2011 and "looked back" 5 years to identify prior surgeries. Finally, they used Monte Carlo simulations to determine the cumulative lifetime risk of either incontinence or prolapse surgery with 95% confidence intervals.
Dr. Wu reported that the cumulative lifetime risk of either SUI or POP surgery was 20.2% (95% CI, 19.2%-21.1%). The cumulative lifetime risk of SUI was 14.5% (95% CI, 13.4%-15.5%), and the risk of POP surgery was 13.7% (95% CI, 12.6%-14.8%). The cumulative lifetime risk for SUI or POP surgery increased with age in a stepwise fashion, from 11.4% by age 60 years to 15.9% by age 70 and 20.2% by age 80, she noted.
To place the risk of any primary surgery for SUI or POP in perspective, Dr. Wu drew a comparison with the lifetime risk estimates for colon cancer (4.8%), lung cancer (6.3%), breast cancer (14.8%), and any type of cancer (41.3%). "Granted, incontinence and prolapse are not life-threatening conditions, but this 20% risk highlights how common surgeries are for pelvic floor disorders, despite the fact that they’re widely underrecognized," she noted.
She acknowledged certain limitations of the study, including the fact that she and her associates were unable to review actual medical records to confirm the rate of prior surgeries. "In addition, we assumed a closed cohort and no competing risks such that all women live until the age of 80," she said. "Also, these results reflect women with private insurance and may not be generalizable to those who are uninsured or underinsured."
Dr. Wu disclosed that she is a consultant for Procter & Gamble.
LAS VEGAS – Among women with private health insurance in this country, the lifetime risk of surgery for either stress urinary incontinence or pelvic organ prolapse stands at 20.2%, results from a large analysis demonstrated.
"This means that one out of every five women in the United States will undergo a urogynecologic procedure by the age of 80," Dr. Jennifer M. Wu said at the annual meeting of the American Urogynecologic Society. "This high rate highlights the public health burden of pelvic floor disorders, exposes the need for improved prevention strategies, and underscores the importance of effective long-term surgical interventions."
A commonly referenced statistic is that the lifetime risk of surgery for either stress urinary incontinence (SUI) or pelvic organ prolapse (POP) is 11%, but this was based on a study of 395 patients who underwent surgery in 1995 in the Northwest (Obstet. Gynecol. 1997;89:501-6).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Since 1995, several factors may have increased this risk. These include "the integration of midurethral slings and vaginal mesh prolapse procedures, regional differences in surgery rates, and the greater number of elderly women," explained Dr. Wu of the department of obstetrics and gynecology and the Center for Women’s Health Research at the University of North Carolina at Chapel Hill. "Thus, the objective of our study was to estimate the cumulative risk of SUI or POP surgery over a woman’s lifetime until the age of 80."
The researchers used the Market Scan Commercial Claims and Encounters database with the Medicare Supplemental, which contains de-identified inpatient and outpatient claims data from about 100 employer-based insurance plans in the United States. They included women aged 18 years and older and identified any SUI or POP surgery performed between 2007 and 2011 based on CPT codes. This resulted in a study population of 51.8 million women. Of these, 311,070 underwent surgery for either SUI or POP.
To estimate age-specific incidence rates for each age between 18 and 80 years, Dr. Wu and her associates multiplied age-specific prevalence rates by the proportion of cases that were incident. To estimate the proportion of all procedures that were repeat surgeries, they evaluated women who had a SUI or POP surgery in 2011 and "looked back" 5 years to identify prior surgeries. Finally, they used Monte Carlo simulations to determine the cumulative lifetime risk of either incontinence or prolapse surgery with 95% confidence intervals.
Dr. Wu reported that the cumulative lifetime risk of either SUI or POP surgery was 20.2% (95% CI, 19.2%-21.1%). The cumulative lifetime risk of SUI was 14.5% (95% CI, 13.4%-15.5%), and the risk of POP surgery was 13.7% (95% CI, 12.6%-14.8%). The cumulative lifetime risk for SUI or POP surgery increased with age in a stepwise fashion, from 11.4% by age 60 years to 15.9% by age 70 and 20.2% by age 80, she noted.
To place the risk of any primary surgery for SUI or POP in perspective, Dr. Wu drew a comparison with the lifetime risk estimates for colon cancer (4.8%), lung cancer (6.3%), breast cancer (14.8%), and any type of cancer (41.3%). "Granted, incontinence and prolapse are not life-threatening conditions, but this 20% risk highlights how common surgeries are for pelvic floor disorders, despite the fact that they’re widely underrecognized," she noted.
She acknowledged certain limitations of the study, including the fact that she and her associates were unable to review actual medical records to confirm the rate of prior surgeries. "In addition, we assumed a closed cohort and no competing risks such that all women live until the age of 80," she said. "Also, these results reflect women with private insurance and may not be generalizable to those who are uninsured or underinsured."
Dr. Wu disclosed that she is a consultant for Procter & Gamble.
AT THE AUGS ANNUAL MEETING
Major finding: The cumulative lifetime risk of surgery for either stress urinary incontinence (SUI) or pelvic organ prolapse (POP) was 20.2% (95%CI 19.2%, 21.1%).
Data source: Claims data from 311,070 women in the United States who underwent any SUI or POP surgery between 2007 and 2011.
Disclosures: Dr. Wu disclosed that she is a consultant for Procter & Gamble.
Left liver grafts may benefit from hepatic vein/IVC anastomosis
WASHINGTON – A novel anastomosis technique may help avoid small-for-size syndrome in adult living donor liver transplantation, according to Dr. Mitsuhisa Takatsuki.
Reconstructing the hepatic vein by cross-clamping with the inferior vena cava creates improved outflow from the graft. This can avert the potential failure of a left liver graft, which, because of its smaller size, is more prone to the syndrome than is a right liver graft, said Dr. Takatsuki of Nagasaki (Japan) University.
A left liver graft is the first choice for living donor transplant in Japan because this graft is less likely to experience congestion than is a right lobe graft. Donors with a left graft are also less likely to have serious postoperative complications or to die. However, the graft volume of the left liver is less than that of the right, making it susceptible to the problems of a high portal inflow. Dr. Takatsuki’s novel securing of the hepatic vein to the inferior vena cava increases liver outflow and, hopefully, prevents graft congestion, he said at the annual clinical congress of the American College of Surgeons.
The conventional hepatic vein reconstruction side clamps the middle and left hepatic veins. This common trunk is then joined to the graft hepatic vein. Dr. Takatsuki’s technique takes advantage of the inferior vena cava to increase graft outflow, he noted.
He closes the right hepatic vein with a vascular stapler. He then opens the common trunk of the middle and left hepatic veins and creates a wide cavotomy in the inferior vena cava. "This wide orifice of hepatic vein is anastomosed to the graft hepatic vein. The size of the hepatic vein orifice is easily adjustable to suit the size of the graft hepatic vein," Dr. Takatsuki said.
He reported the results of a study of 47 adult living donor transplants. Of these 47 patients, 21 had the side clamp hepatic vein reconstruction and 26, the new technique of cross-clamping the inferior vena cava.
The patients were a mean of 56 years old and evenly split between men and women. The mean Model for End-Stage Liver Disease(MELD) score was 15.5. Surgery lasted a mean of 915 minutes in the side clamp group and 746 minutes in the cross-clamp group – a significant difference. Blood loss was also significantly less in the cross-clamp group (3,800 g vs.5,450 g).
By postoperative day 7, there were no significant between-group differences in total bilirubin or prothrombin time. There was significantly less ascites in the cross-clamp group.
Dr. Takatsuki saw the same results in a subgroup of 17 patients (7 in the side clamp group and 10 in the cross-clamp group) in whom the graft weight/recipient standard liver volume was less than 30%.
Among these patients – who were at the highest risk for graft failure because of the weight/volume differential – those with the cross-clamped anastomosis had significantly higher graft survival (90% vs. 71%) at 1 year.
Dr. Takatsuki said he had no relevant financial disclosures.
WASHINGTON – A novel anastomosis technique may help avoid small-for-size syndrome in adult living donor liver transplantation, according to Dr. Mitsuhisa Takatsuki.
Reconstructing the hepatic vein by cross-clamping with the inferior vena cava creates improved outflow from the graft. This can avert the potential failure of a left liver graft, which, because of its smaller size, is more prone to the syndrome than is a right liver graft, said Dr. Takatsuki of Nagasaki (Japan) University.
A left liver graft is the first choice for living donor transplant in Japan because this graft is less likely to experience congestion than is a right lobe graft. Donors with a left graft are also less likely to have serious postoperative complications or to die. However, the graft volume of the left liver is less than that of the right, making it susceptible to the problems of a high portal inflow. Dr. Takatsuki’s novel securing of the hepatic vein to the inferior vena cava increases liver outflow and, hopefully, prevents graft congestion, he said at the annual clinical congress of the American College of Surgeons.
The conventional hepatic vein reconstruction side clamps the middle and left hepatic veins. This common trunk is then joined to the graft hepatic vein. Dr. Takatsuki’s technique takes advantage of the inferior vena cava to increase graft outflow, he noted.
He closes the right hepatic vein with a vascular stapler. He then opens the common trunk of the middle and left hepatic veins and creates a wide cavotomy in the inferior vena cava. "This wide orifice of hepatic vein is anastomosed to the graft hepatic vein. The size of the hepatic vein orifice is easily adjustable to suit the size of the graft hepatic vein," Dr. Takatsuki said.
He reported the results of a study of 47 adult living donor transplants. Of these 47 patients, 21 had the side clamp hepatic vein reconstruction and 26, the new technique of cross-clamping the inferior vena cava.
The patients were a mean of 56 years old and evenly split between men and women. The mean Model for End-Stage Liver Disease(MELD) score was 15.5. Surgery lasted a mean of 915 minutes in the side clamp group and 746 minutes in the cross-clamp group – a significant difference. Blood loss was also significantly less in the cross-clamp group (3,800 g vs.5,450 g).
By postoperative day 7, there were no significant between-group differences in total bilirubin or prothrombin time. There was significantly less ascites in the cross-clamp group.
Dr. Takatsuki saw the same results in a subgroup of 17 patients (7 in the side clamp group and 10 in the cross-clamp group) in whom the graft weight/recipient standard liver volume was less than 30%.
Among these patients – who were at the highest risk for graft failure because of the weight/volume differential – those with the cross-clamped anastomosis had significantly higher graft survival (90% vs. 71%) at 1 year.
Dr. Takatsuki said he had no relevant financial disclosures.
WASHINGTON – A novel anastomosis technique may help avoid small-for-size syndrome in adult living donor liver transplantation, according to Dr. Mitsuhisa Takatsuki.
Reconstructing the hepatic vein by cross-clamping with the inferior vena cava creates improved outflow from the graft. This can avert the potential failure of a left liver graft, which, because of its smaller size, is more prone to the syndrome than is a right liver graft, said Dr. Takatsuki of Nagasaki (Japan) University.
A left liver graft is the first choice for living donor transplant in Japan because this graft is less likely to experience congestion than is a right lobe graft. Donors with a left graft are also less likely to have serious postoperative complications or to die. However, the graft volume of the left liver is less than that of the right, making it susceptible to the problems of a high portal inflow. Dr. Takatsuki’s novel securing of the hepatic vein to the inferior vena cava increases liver outflow and, hopefully, prevents graft congestion, he said at the annual clinical congress of the American College of Surgeons.
The conventional hepatic vein reconstruction side clamps the middle and left hepatic veins. This common trunk is then joined to the graft hepatic vein. Dr. Takatsuki’s technique takes advantage of the inferior vena cava to increase graft outflow, he noted.
He closes the right hepatic vein with a vascular stapler. He then opens the common trunk of the middle and left hepatic veins and creates a wide cavotomy in the inferior vena cava. "This wide orifice of hepatic vein is anastomosed to the graft hepatic vein. The size of the hepatic vein orifice is easily adjustable to suit the size of the graft hepatic vein," Dr. Takatsuki said.
He reported the results of a study of 47 adult living donor transplants. Of these 47 patients, 21 had the side clamp hepatic vein reconstruction and 26, the new technique of cross-clamping the inferior vena cava.
The patients were a mean of 56 years old and evenly split between men and women. The mean Model for End-Stage Liver Disease(MELD) score was 15.5. Surgery lasted a mean of 915 minutes in the side clamp group and 746 minutes in the cross-clamp group – a significant difference. Blood loss was also significantly less in the cross-clamp group (3,800 g vs.5,450 g).
By postoperative day 7, there were no significant between-group differences in total bilirubin or prothrombin time. There was significantly less ascites in the cross-clamp group.
Dr. Takatsuki saw the same results in a subgroup of 17 patients (7 in the side clamp group and 10 in the cross-clamp group) in whom the graft weight/recipient standard liver volume was less than 30%.
Among these patients – who were at the highest risk for graft failure because of the weight/volume differential – those with the cross-clamped anastomosis had significantly higher graft survival (90% vs. 71%) at 1 year.
Dr. Takatsuki said he had no relevant financial disclosures.
AT THE ACS Clincal Congress
Major finding: One-year liver graft survival was significantly better in patients with a hepatic vein/inferior vena cava anastomosis than in those who had the traditional hepatic vein side clamp (90% vs. 71%).
Data source: A randomized study involving 47 patients who received a living donor left liver transplant.
Disclosures: Dr. Takatsuki said he had no relevant financial disclosures.