User login
MOC update: GI societies and ABIM explore new recertification pathway
AGA is committed to making recertification less burdensome for GIs. After a productive meeting between the GI societies and ABIM, we’re hopeful a new, more flexible pathway is on the horizon.
We heard you
The four major physician organizations in gastroenterology and hepatology — AGA, AASLD, ACG and ASGE — share a fundamental commitment to an efficient, clinically relevant and impactful process for the demonstration of ongoing learning and maintenance of specialty board certification for gastroenterologists and hepatologists.
Inspired by our shared objective to create an alternative to the current ABIM 10-year exam and upcoming two-year check-in, the four societies have collaborated to explore alternatives that are less onerous, more relevant, less costly and less time consuming. We look forward to working to achieve this objective for all of GI and hepatology.
Finding a path forward on MOC for GI & hepatology
On Oct. 4, the four societies met with the leadership of ABIM in Philadelphia, Pennsylvania, and presented concepts focusing on a flexible model that can provide a path forward, allowing members of our specialties and subspecialties to focus on knowledge that is relevant to their practice and choose the path that best fits their personal needs.
The GI societies and ABIM agreed to work together to explore the development of a third option for MOC.
Guided by core principles
In working together to develop an alternative to MOC, the four GI societies are guided by these core principles embraced by our organizations several years ago:
• MOC needs to be simpler, less intrusive and less expensive.
• We continue to support alternatives to the high-stakes, every-10-year recertification exam.
• We do not support single source or time-limited assessments, as they do not represent the current realities of medicine in the digital age.
• We support the concept that, for the many diplomates who specialize within certain areas of gastroenterology and hepatology, MOC should not include high-stakes assessments of areas in which the diplomate may not practice.
• We support the principles of lifelong learning, as evidenced by ongoing CME activities, rather than lifelong testing.
AGA is committed to making recertification less burdensome for GIs. After a productive meeting between the GI societies and ABIM, we’re hopeful a new, more flexible pathway is on the horizon.
We heard you
The four major physician organizations in gastroenterology and hepatology — AGA, AASLD, ACG and ASGE — share a fundamental commitment to an efficient, clinically relevant and impactful process for the demonstration of ongoing learning and maintenance of specialty board certification for gastroenterologists and hepatologists.
Inspired by our shared objective to create an alternative to the current ABIM 10-year exam and upcoming two-year check-in, the four societies have collaborated to explore alternatives that are less onerous, more relevant, less costly and less time consuming. We look forward to working to achieve this objective for all of GI and hepatology.
Finding a path forward on MOC for GI & hepatology
On Oct. 4, the four societies met with the leadership of ABIM in Philadelphia, Pennsylvania, and presented concepts focusing on a flexible model that can provide a path forward, allowing members of our specialties and subspecialties to focus on knowledge that is relevant to their practice and choose the path that best fits their personal needs.
The GI societies and ABIM agreed to work together to explore the development of a third option for MOC.
Guided by core principles
In working together to develop an alternative to MOC, the four GI societies are guided by these core principles embraced by our organizations several years ago:
• MOC needs to be simpler, less intrusive and less expensive.
• We continue to support alternatives to the high-stakes, every-10-year recertification exam.
• We do not support single source or time-limited assessments, as they do not represent the current realities of medicine in the digital age.
• We support the concept that, for the many diplomates who specialize within certain areas of gastroenterology and hepatology, MOC should not include high-stakes assessments of areas in which the diplomate may not practice.
• We support the principles of lifelong learning, as evidenced by ongoing CME activities, rather than lifelong testing.
AGA is committed to making recertification less burdensome for GIs. After a productive meeting between the GI societies and ABIM, we’re hopeful a new, more flexible pathway is on the horizon.
We heard you
The four major physician organizations in gastroenterology and hepatology — AGA, AASLD, ACG and ASGE — share a fundamental commitment to an efficient, clinically relevant and impactful process for the demonstration of ongoing learning and maintenance of specialty board certification for gastroenterologists and hepatologists.
Inspired by our shared objective to create an alternative to the current ABIM 10-year exam and upcoming two-year check-in, the four societies have collaborated to explore alternatives that are less onerous, more relevant, less costly and less time consuming. We look forward to working to achieve this objective for all of GI and hepatology.
Finding a path forward on MOC for GI & hepatology
On Oct. 4, the four societies met with the leadership of ABIM in Philadelphia, Pennsylvania, and presented concepts focusing on a flexible model that can provide a path forward, allowing members of our specialties and subspecialties to focus on knowledge that is relevant to their practice and choose the path that best fits their personal needs.
The GI societies and ABIM agreed to work together to explore the development of a third option for MOC.
Guided by core principles
In working together to develop an alternative to MOC, the four GI societies are guided by these core principles embraced by our organizations several years ago:
• MOC needs to be simpler, less intrusive and less expensive.
• We continue to support alternatives to the high-stakes, every-10-year recertification exam.
• We do not support single source or time-limited assessments, as they do not represent the current realities of medicine in the digital age.
• We support the concept that, for the many diplomates who specialize within certain areas of gastroenterology and hepatology, MOC should not include high-stakes assessments of areas in which the diplomate may not practice.
• We support the principles of lifelong learning, as evidenced by ongoing CME activities, rather than lifelong testing.
DDW® 2019 abstract submission site is now open
Digestive Disease Week® (DDW) will be accepting abstracts for DDW 2019 from now through Dec. 1, 2018.
Since 1969, Digestive Disease Week has been the most important venue for sharing research and breakthroughs in digestive disease. What better way to commemorate DDW’s legacy than to make sure your research is included to help promote basic, clinical, and translational research on a global scale?
For DDW 2019, AGA is planning a program filled with cutting-edge advances in the field. To help you match your abstract(s) to the best descriptor for submission to AGA, the AGA Institute Council released an expanded descriptor document, gastro.org/Descriptors, to indicate what the abstract review committee is looking for in submitted abstracts.
Mark your calendar with the important abstract submission dates below and visit the DDW website for more information on submitting your research.
Important dates
Dec. 1, 2018, at 9 p.m. ET: Abstract submission site closes. No abstract edits, author additions or changes to author information will be accepted after this deadline.
Dec. 14, 2018, at 3 p.m. ET: Co-author disclosures due.
Feb. 12, 2019: Acceptance notifications sent by email to presenting authors.
Take advantage of this opportunity to make sure your research is included.
Digestive Disease Week® (DDW) will be accepting abstracts for DDW 2019 from now through Dec. 1, 2018.
Since 1969, Digestive Disease Week has been the most important venue for sharing research and breakthroughs in digestive disease. What better way to commemorate DDW’s legacy than to make sure your research is included to help promote basic, clinical, and translational research on a global scale?
For DDW 2019, AGA is planning a program filled with cutting-edge advances in the field. To help you match your abstract(s) to the best descriptor for submission to AGA, the AGA Institute Council released an expanded descriptor document, gastro.org/Descriptors, to indicate what the abstract review committee is looking for in submitted abstracts.
Mark your calendar with the important abstract submission dates below and visit the DDW website for more information on submitting your research.
Important dates
Dec. 1, 2018, at 9 p.m. ET: Abstract submission site closes. No abstract edits, author additions or changes to author information will be accepted after this deadline.
Dec. 14, 2018, at 3 p.m. ET: Co-author disclosures due.
Feb. 12, 2019: Acceptance notifications sent by email to presenting authors.
Take advantage of this opportunity to make sure your research is included.
Digestive Disease Week® (DDW) will be accepting abstracts for DDW 2019 from now through Dec. 1, 2018.
Since 1969, Digestive Disease Week has been the most important venue for sharing research and breakthroughs in digestive disease. What better way to commemorate DDW’s legacy than to make sure your research is included to help promote basic, clinical, and translational research on a global scale?
For DDW 2019, AGA is planning a program filled with cutting-edge advances in the field. To help you match your abstract(s) to the best descriptor for submission to AGA, the AGA Institute Council released an expanded descriptor document, gastro.org/Descriptors, to indicate what the abstract review committee is looking for in submitted abstracts.
Mark your calendar with the important abstract submission dates below and visit the DDW website for more information on submitting your research.
Important dates
Dec. 1, 2018, at 9 p.m. ET: Abstract submission site closes. No abstract edits, author additions or changes to author information will be accepted after this deadline.
Dec. 14, 2018, at 3 p.m. ET: Co-author disclosures due.
Feb. 12, 2019: Acceptance notifications sent by email to presenting authors.
Take advantage of this opportunity to make sure your research is included.
AGA’s Future Leaders Program receives stellar reviews
Future Leaders alumni and past mentors took to the AGA Community recently to share their experiences with the award-winning program. Now in its third year, the program continues to have an impact on the careers of its participants and AGA.
Here’s what they had to say
“The Future Leaders Program provided robust leadership training, valuable mentorship, and invaluable networking with AGA leaders and other AGA members.” – Bryson Katona, MD, MS, PhD, editor of The New Gastroenterologist, University of Pennsylvania
“Through the Future Leaders Program I gained leadership skills, problem-solving skills, and even new research collaborations.” – Jennifer Weiss MD, MS, AGAF, University of Wisconsin School of Medicine and Public Health
“The program not only introduced Future Leaders Program members to the AGA inner circle and provided a deep insight into AGA governance, but also placed participants into meaningful, actionable projects that had the potential to generate real benefits for the AGA itself.” – David Levinthal, MD, PhD, University of Pittsburgh Medical Center
“I think I learned as much from the two outstanding faculty whom I mentored, Jennifer Weiss and Art Beyder, as they did from me!” – Kim Barrett, PhD, AGAF, University of California, San Diego (Mentor)
The program is designed for GIs who aspire to further develop their leadership skills with an eye toward serving in a key leadership position both within the field and AGA. Participation from experienced GIs is also critical to the program’s success. They are needed to serve as mentors and help develop the next generation of leaders. This is the opportunity to help drive AGA’s strategic plan and advance in the field.
Members can access the full discussion: A Fantastic Opportunity: AGA Future Leaders Program in community.gastro.org. Stay tuned to see the list of members selected for the 2019 AGA Future Leaders Program.
Future Leaders alumni and past mentors took to the AGA Community recently to share their experiences with the award-winning program. Now in its third year, the program continues to have an impact on the careers of its participants and AGA.
Here’s what they had to say
“The Future Leaders Program provided robust leadership training, valuable mentorship, and invaluable networking with AGA leaders and other AGA members.” – Bryson Katona, MD, MS, PhD, editor of The New Gastroenterologist, University of Pennsylvania
“Through the Future Leaders Program I gained leadership skills, problem-solving skills, and even new research collaborations.” – Jennifer Weiss MD, MS, AGAF, University of Wisconsin School of Medicine and Public Health
“The program not only introduced Future Leaders Program members to the AGA inner circle and provided a deep insight into AGA governance, but also placed participants into meaningful, actionable projects that had the potential to generate real benefits for the AGA itself.” – David Levinthal, MD, PhD, University of Pittsburgh Medical Center
“I think I learned as much from the two outstanding faculty whom I mentored, Jennifer Weiss and Art Beyder, as they did from me!” – Kim Barrett, PhD, AGAF, University of California, San Diego (Mentor)
The program is designed for GIs who aspire to further develop their leadership skills with an eye toward serving in a key leadership position both within the field and AGA. Participation from experienced GIs is also critical to the program’s success. They are needed to serve as mentors and help develop the next generation of leaders. This is the opportunity to help drive AGA’s strategic plan and advance in the field.
Members can access the full discussion: A Fantastic Opportunity: AGA Future Leaders Program in community.gastro.org. Stay tuned to see the list of members selected for the 2019 AGA Future Leaders Program.
Future Leaders alumni and past mentors took to the AGA Community recently to share their experiences with the award-winning program. Now in its third year, the program continues to have an impact on the careers of its participants and AGA.
Here’s what they had to say
“The Future Leaders Program provided robust leadership training, valuable mentorship, and invaluable networking with AGA leaders and other AGA members.” – Bryson Katona, MD, MS, PhD, editor of The New Gastroenterologist, University of Pennsylvania
“Through the Future Leaders Program I gained leadership skills, problem-solving skills, and even new research collaborations.” – Jennifer Weiss MD, MS, AGAF, University of Wisconsin School of Medicine and Public Health
“The program not only introduced Future Leaders Program members to the AGA inner circle and provided a deep insight into AGA governance, but also placed participants into meaningful, actionable projects that had the potential to generate real benefits for the AGA itself.” – David Levinthal, MD, PhD, University of Pittsburgh Medical Center
“I think I learned as much from the two outstanding faculty whom I mentored, Jennifer Weiss and Art Beyder, as they did from me!” – Kim Barrett, PhD, AGAF, University of California, San Diego (Mentor)
The program is designed for GIs who aspire to further develop their leadership skills with an eye toward serving in a key leadership position both within the field and AGA. Participation from experienced GIs is also critical to the program’s success. They are needed to serve as mentors and help develop the next generation of leaders. This is the opportunity to help drive AGA’s strategic plan and advance in the field.
Members can access the full discussion: A Fantastic Opportunity: AGA Future Leaders Program in community.gastro.org. Stay tuned to see the list of members selected for the 2019 AGA Future Leaders Program.
Residents: Apply for Research Award
The SVS Research and Education Committee encourages eligible members to apply for the prestigious Resident Research Award. The recipient will showcase his or her work at the 2019 Vascular Annual Meeting in June as well as receive a $5,000 award. This award is designed to provide special recognition of original scientific work that has yet to be published in manuscript form. It’s an excellent opportunity for surgical trainees in vascular research laboratories to be recognized and rewarded for their research efforts. The application deadline is Jan. 16, 2019, and the annual meeting will take place June 12 to 15 in National Harbor, Md., outside of Washington, D.C.
The SVS Research and Education Committee encourages eligible members to apply for the prestigious Resident Research Award. The recipient will showcase his or her work at the 2019 Vascular Annual Meeting in June as well as receive a $5,000 award. This award is designed to provide special recognition of original scientific work that has yet to be published in manuscript form. It’s an excellent opportunity for surgical trainees in vascular research laboratories to be recognized and rewarded for their research efforts. The application deadline is Jan. 16, 2019, and the annual meeting will take place June 12 to 15 in National Harbor, Md., outside of Washington, D.C.
The SVS Research and Education Committee encourages eligible members to apply for the prestigious Resident Research Award. The recipient will showcase his or her work at the 2019 Vascular Annual Meeting in June as well as receive a $5,000 award. This award is designed to provide special recognition of original scientific work that has yet to be published in manuscript form. It’s an excellent opportunity for surgical trainees in vascular research laboratories to be recognized and rewarded for their research efforts. The application deadline is Jan. 16, 2019, and the annual meeting will take place June 12 to 15 in National Harbor, Md., outside of Washington, D.C.
VAM Abstract Site Now Open
The abstract submission site for the 2019 Vascular Annual Meeting is now open. Submissions may be considered for the following programs: Scientific Session, Vascular and Endovascular Surgical Society (VESS), International Forum, International Fast Talk, Poster Competition and Interactive Poster. In addition to the International Forum and International Fast Talk, the international community has added two further opportunities to showcase research: The International Young Surgeon Competition and the International Poster Competition. This year the submission site is mobile friendly! Get more information on submission and policy guidelines here.
The abstract submission site for the 2019 Vascular Annual Meeting is now open. Submissions may be considered for the following programs: Scientific Session, Vascular and Endovascular Surgical Society (VESS), International Forum, International Fast Talk, Poster Competition and Interactive Poster. In addition to the International Forum and International Fast Talk, the international community has added two further opportunities to showcase research: The International Young Surgeon Competition and the International Poster Competition. This year the submission site is mobile friendly! Get more information on submission and policy guidelines here.
The abstract submission site for the 2019 Vascular Annual Meeting is now open. Submissions may be considered for the following programs: Scientific Session, Vascular and Endovascular Surgical Society (VESS), International Forum, International Fast Talk, Poster Competition and Interactive Poster. In addition to the International Forum and International Fast Talk, the international community has added two further opportunities to showcase research: The International Young Surgeon Competition and the International Poster Competition. This year the submission site is mobile friendly! Get more information on submission and policy guidelines here.
Dr. Mary Edwards Walker Inspiring Women in Surgery Award presented to Dr. Lee
The American College of Surgeons (ACS) presented the Dr. Mary Edwards Walker Inspiring Women in Surgery Award to Yeu-Tsu Margaret Lee, MD, FACS, at the Convocation at Clinical Congress 2018 in Boston, MA. This award was established by the ACS Women in Surgery Committee (WiSC) and is presented annually at the Clinical Congress to recognize an individual’s significant contributions to the advancement of women in surgery.
Dr. Lee is from Honolulu, HI, and was born in Xian, China, in 1936. During her childhood, four of her siblings died from illness, motivating Dr. Lee to become a physician. Her family was forced to flee to Taiwan after the Chinese Civil War, and she immigrated to the U.S. in 1955, graduated from Harvard Medical School, Boston, in 1961, and has worked as a general surgeon and a surgical oncologist for more than 50 years. In the early 1980s, she was a tenured associate professor of surgery, University of Southern California (USC), Los Angeles, and head physician, Los Angeles County-USC Medical Center, but chose to pursue a different path.
In 1983, Dr. Lee moved to Hawaii, worked at Tripler Army Medical Center, Honolulu, as chief, surgical oncology section of general surgical services, and joined the U.S. Army Corps. She was deployed to Iraq during Operation Desert Storm and treated many U.S. soldiers as well as Iraqi prisoners of war. She served on a team of surgeons that performed more than 125 operations in a 400-bed hospital in northern Saudi Arabia. Dr. Lee received several accolades in the military, including an “A” Proficiency Designator from the Army Medical Department and a Certificate of Achievement. After retiring from the Army as a colonel, she became professor of surgery, University of Hawaii at Manoa, Honolulu, where she was the only woman surgeon for most of her career.
Dr. Lee has participated in medical missions to Ghana, Honduras, Cambodia, Laos, the Philippines, and other underserved countries. She has made many international trips to promote friendship and medical exchanges. Notably, in 1995, she was the leader of a Women Surgeons Delegation to Russia and Romania. The trip was a Citizen Ambassador Program sponsored by People to People International, which was established by President Dwight D. Eisenhower. From 2000 to 2017, Dr. Lee taught surgery for a month, four times a year, at the Tzu-Chi University School of Medicine, Hualien, Taiwan.
Dr. Lee was one of 21 women surgeons in attendance at a networking breakfast at the 1981 Clinical Congress—led by ACS Past-President Patricia Numann, MD, FACS—which proved to be the genesis of the Association of Women Surgeons (AWS). She has been a supporter of the association, in time and talent, since its inception, and her presence at the AWS meetings, her academic career at teaching hospitals, and her research publications provide women surgeons and medical students from around the world an example of what women can achieve in the field.
Because her home is in Hawaii, midway between the East and West, she hopes to function as a “bridge,” contributing to global understanding and promoting communication, collaboration, and goodwill, and continues to work in the areas of medical education, international health, and world peace.
Committed to improving the care of the surgical patient, Dr. Lee is an outstanding leader and role model for surgeons everywhere. Her contributions to academic medicine in surgery, in the military, and in surgical volunteerism worldwide have made a lasting impression on the surgical profession. Her passion, endless energy, and dedication to the ACS and to women in surgery are without equal.
The American College of Surgeons (ACS) presented the Dr. Mary Edwards Walker Inspiring Women in Surgery Award to Yeu-Tsu Margaret Lee, MD, FACS, at the Convocation at Clinical Congress 2018 in Boston, MA. This award was established by the ACS Women in Surgery Committee (WiSC) and is presented annually at the Clinical Congress to recognize an individual’s significant contributions to the advancement of women in surgery.
Dr. Lee is from Honolulu, HI, and was born in Xian, China, in 1936. During her childhood, four of her siblings died from illness, motivating Dr. Lee to become a physician. Her family was forced to flee to Taiwan after the Chinese Civil War, and she immigrated to the U.S. in 1955, graduated from Harvard Medical School, Boston, in 1961, and has worked as a general surgeon and a surgical oncologist for more than 50 years. In the early 1980s, she was a tenured associate professor of surgery, University of Southern California (USC), Los Angeles, and head physician, Los Angeles County-USC Medical Center, but chose to pursue a different path.
In 1983, Dr. Lee moved to Hawaii, worked at Tripler Army Medical Center, Honolulu, as chief, surgical oncology section of general surgical services, and joined the U.S. Army Corps. She was deployed to Iraq during Operation Desert Storm and treated many U.S. soldiers as well as Iraqi prisoners of war. She served on a team of surgeons that performed more than 125 operations in a 400-bed hospital in northern Saudi Arabia. Dr. Lee received several accolades in the military, including an “A” Proficiency Designator from the Army Medical Department and a Certificate of Achievement. After retiring from the Army as a colonel, she became professor of surgery, University of Hawaii at Manoa, Honolulu, where she was the only woman surgeon for most of her career.
Dr. Lee has participated in medical missions to Ghana, Honduras, Cambodia, Laos, the Philippines, and other underserved countries. She has made many international trips to promote friendship and medical exchanges. Notably, in 1995, she was the leader of a Women Surgeons Delegation to Russia and Romania. The trip was a Citizen Ambassador Program sponsored by People to People International, which was established by President Dwight D. Eisenhower. From 2000 to 2017, Dr. Lee taught surgery for a month, four times a year, at the Tzu-Chi University School of Medicine, Hualien, Taiwan.
Dr. Lee was one of 21 women surgeons in attendance at a networking breakfast at the 1981 Clinical Congress—led by ACS Past-President Patricia Numann, MD, FACS—which proved to be the genesis of the Association of Women Surgeons (AWS). She has been a supporter of the association, in time and talent, since its inception, and her presence at the AWS meetings, her academic career at teaching hospitals, and her research publications provide women surgeons and medical students from around the world an example of what women can achieve in the field.
Because her home is in Hawaii, midway between the East and West, she hopes to function as a “bridge,” contributing to global understanding and promoting communication, collaboration, and goodwill, and continues to work in the areas of medical education, international health, and world peace.
Committed to improving the care of the surgical patient, Dr. Lee is an outstanding leader and role model for surgeons everywhere. Her contributions to academic medicine in surgery, in the military, and in surgical volunteerism worldwide have made a lasting impression on the surgical profession. Her passion, endless energy, and dedication to the ACS and to women in surgery are without equal.
The American College of Surgeons (ACS) presented the Dr. Mary Edwards Walker Inspiring Women in Surgery Award to Yeu-Tsu Margaret Lee, MD, FACS, at the Convocation at Clinical Congress 2018 in Boston, MA. This award was established by the ACS Women in Surgery Committee (WiSC) and is presented annually at the Clinical Congress to recognize an individual’s significant contributions to the advancement of women in surgery.
Dr. Lee is from Honolulu, HI, and was born in Xian, China, in 1936. During her childhood, four of her siblings died from illness, motivating Dr. Lee to become a physician. Her family was forced to flee to Taiwan after the Chinese Civil War, and she immigrated to the U.S. in 1955, graduated from Harvard Medical School, Boston, in 1961, and has worked as a general surgeon and a surgical oncologist for more than 50 years. In the early 1980s, she was a tenured associate professor of surgery, University of Southern California (USC), Los Angeles, and head physician, Los Angeles County-USC Medical Center, but chose to pursue a different path.
In 1983, Dr. Lee moved to Hawaii, worked at Tripler Army Medical Center, Honolulu, as chief, surgical oncology section of general surgical services, and joined the U.S. Army Corps. She was deployed to Iraq during Operation Desert Storm and treated many U.S. soldiers as well as Iraqi prisoners of war. She served on a team of surgeons that performed more than 125 operations in a 400-bed hospital in northern Saudi Arabia. Dr. Lee received several accolades in the military, including an “A” Proficiency Designator from the Army Medical Department and a Certificate of Achievement. After retiring from the Army as a colonel, she became professor of surgery, University of Hawaii at Manoa, Honolulu, where she was the only woman surgeon for most of her career.
Dr. Lee has participated in medical missions to Ghana, Honduras, Cambodia, Laos, the Philippines, and other underserved countries. She has made many international trips to promote friendship and medical exchanges. Notably, in 1995, she was the leader of a Women Surgeons Delegation to Russia and Romania. The trip was a Citizen Ambassador Program sponsored by People to People International, which was established by President Dwight D. Eisenhower. From 2000 to 2017, Dr. Lee taught surgery for a month, four times a year, at the Tzu-Chi University School of Medicine, Hualien, Taiwan.
Dr. Lee was one of 21 women surgeons in attendance at a networking breakfast at the 1981 Clinical Congress—led by ACS Past-President Patricia Numann, MD, FACS—which proved to be the genesis of the Association of Women Surgeons (AWS). She has been a supporter of the association, in time and talent, since its inception, and her presence at the AWS meetings, her academic career at teaching hospitals, and her research publications provide women surgeons and medical students from around the world an example of what women can achieve in the field.
Because her home is in Hawaii, midway between the East and West, she hopes to function as a “bridge,” contributing to global understanding and promoting communication, collaboration, and goodwill, and continues to work in the areas of medical education, international health, and world peace.
Committed to improving the care of the surgical patient, Dr. Lee is an outstanding leader and role model for surgeons everywhere. Her contributions to academic medicine in surgery, in the military, and in surgical volunteerism worldwide have made a lasting impression on the surgical profession. Her passion, endless energy, and dedication to the ACS and to women in surgery are without equal.
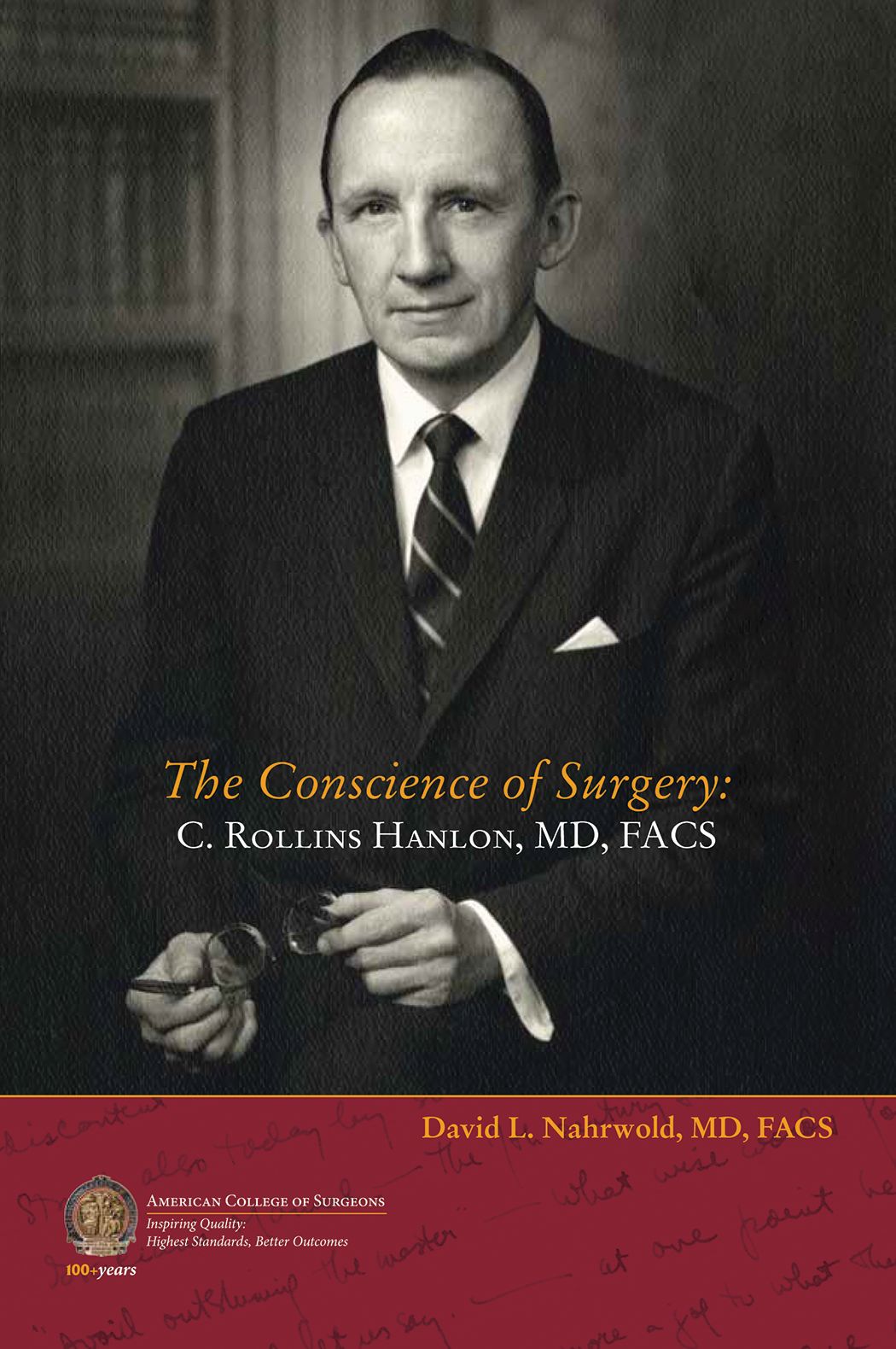
Biography of C. Rollins Hanlon, MD, FACS, Past-Director of the ACS, now available
The American College of Surgeons (ACS) recently published a new biography of C. Rollins Hanlon, MD, FACS, ACS Past-Director, a seminal figure in the history of surgery and the College, titled The Conscience of Surgery: C. Rollins Hanlon, MD, FACS. Written by David L. Nahrwold, MD, FACS, this account examines the life of the erudite, principled cardiothoracic surgeon and innovator, who co-developed the Blalock-Hanlon operation with Alfred P. Blalock, MD, FACS.
The book covers every aspect of Dr. Hanlon’s life—from his boyhood in Baltimore, MD, to his quest to be the best clinician and surgeon-scientist, to his views on the government’s increasing influence on the delivery of surgical care, and to his undying love of the written word. For many surgeons, Dr. Hanlon was the embodiment of what it means to be a Fellow of the ACS.
“I got to know [Dr. Hanlon] as a person and a professional during my stint as the Interim Director of the ACS in 1999 when he was ‘retired’ and serving as Executive Consultant,” Dr. Nahrwold writes in the book’s preface. “He insisted that the mission of the College was to advance the ethical and competent practice of surgery and not to improve the financial well-being of surgeons.”
Throughout his career, Dr. Hanlon’s mentors, colleagues, and students included many eminent surgeons at Johns Hopkins Medical School, Baltimore, MD; Cincinnati General Hospital, OH; and the University of California, San Francisco. He trained under Dean DeWitt Lewis, Walter E. Dandy, Howard C. Naffziger, Warfield “Monty” Firor, and Mont Reid (all MD, FACS). He worked alongside William P. Longmire, MD, FACS; Dr. Blalock; and Mark C. Ravitch, MD, FACS; and his residents and interns at St. Louis University, MO, included Vallee Willman, Theodore Cooper, Theodore Dubuque, and William Stoneman (all MD, FACS), among others.
Dr. Hanlon served in the U.S. Navy in World War II, and followed with a distinguished career at Johns Hopkins and at St. Louis University, where, as chair of surgery, he developed the institution’s cardiac research capabilities, which helped to pioneer early open-heart and heart transplant procedures.
Dr. Hanlon became a Fellow of the College in 1953 and served as the ACS Director for 17 years (1969–1986), making him the longest-serving Director to date. Additionally, he served on the Board of Regents and as the ACS President (1985–1986). After retirement, he stayed on as ACS Executive Consultant, offering his sage advice to his successors, including Paul A. Ebert, MD, FACS; Samuel Wells, MD, FACS; Dr. Nahrwold; Thomas R. Russell, MD, FACS; and David B. Hoyt, MD, FACS. Through these positions, Dr. Hanlon had a profound effect on the direction and philosophy of the College, including in philanthropic endeavors and the establishment of the ACS Archives. He received the first ACS Lifetime Achievement Award in 2010.
“Hanlon’s integrity, faith, hard work, and service to others led him to become a role model for physicians and laypersons alike. These attributes also drove his brilliant career as an innovative surgeon, leadership in academic and organized medicine, and reputation as a humanist and ethicist,” Dr. Narhwold concludes in the preface. “Before he died I knew that I must write his biography to expose his principled life, his goodness, and his devotion to surgery and to surgeons, especially young surgeons, with the hope that they and others will find his life worthy of study and emulation.”
Dr. Nahrwold is Emeritus Professor of Surgery at Northwestern University Feinberg School of Medicine, Chicago, IL, where he was the Loyal and Edith Davis Professor and Chairman, department of surgery, and surgeon-in-chief, Northwestern Memorial Hospital. He is a recipient of the College’s highest honor—the Distinguished Service Award.
Dr. Nahrwold is author of A Mirror Reflecting Surgery, Surgeons, and their College: The Bulletin of the American College of Surgeons, and co-author, with Peter J. Kernahan, MD, PhD, FACS, of A Century of Surgeons and Surgery: The American College of Surgeons 1913–2012.
The Conscience of Surgery: C. Rollins Hanlon, MD, FACS, is available for $15.95 on the ACS E-Store at web4.facs.org/eBusiness/ProductCatalog/Product.aspx?ID=1060 and on amazon.com.
The American College of Surgeons (ACS) recently published a new biography of C. Rollins Hanlon, MD, FACS, ACS Past-Director, a seminal figure in the history of surgery and the College, titled The Conscience of Surgery: C. Rollins Hanlon, MD, FACS. Written by David L. Nahrwold, MD, FACS, this account examines the life of the erudite, principled cardiothoracic surgeon and innovator, who co-developed the Blalock-Hanlon operation with Alfred P. Blalock, MD, FACS.
The book covers every aspect of Dr. Hanlon’s life—from his boyhood in Baltimore, MD, to his quest to be the best clinician and surgeon-scientist, to his views on the government’s increasing influence on the delivery of surgical care, and to his undying love of the written word. For many surgeons, Dr. Hanlon was the embodiment of what it means to be a Fellow of the ACS.
“I got to know [Dr. Hanlon] as a person and a professional during my stint as the Interim Director of the ACS in 1999 when he was ‘retired’ and serving as Executive Consultant,” Dr. Nahrwold writes in the book’s preface. “He insisted that the mission of the College was to advance the ethical and competent practice of surgery and not to improve the financial well-being of surgeons.”
Throughout his career, Dr. Hanlon’s mentors, colleagues, and students included many eminent surgeons at Johns Hopkins Medical School, Baltimore, MD; Cincinnati General Hospital, OH; and the University of California, San Francisco. He trained under Dean DeWitt Lewis, Walter E. Dandy, Howard C. Naffziger, Warfield “Monty” Firor, and Mont Reid (all MD, FACS). He worked alongside William P. Longmire, MD, FACS; Dr. Blalock; and Mark C. Ravitch, MD, FACS; and his residents and interns at St. Louis University, MO, included Vallee Willman, Theodore Cooper, Theodore Dubuque, and William Stoneman (all MD, FACS), among others.
Dr. Hanlon served in the U.S. Navy in World War II, and followed with a distinguished career at Johns Hopkins and at St. Louis University, where, as chair of surgery, he developed the institution’s cardiac research capabilities, which helped to pioneer early open-heart and heart transplant procedures.
Dr. Hanlon became a Fellow of the College in 1953 and served as the ACS Director for 17 years (1969–1986), making him the longest-serving Director to date. Additionally, he served on the Board of Regents and as the ACS President (1985–1986). After retirement, he stayed on as ACS Executive Consultant, offering his sage advice to his successors, including Paul A. Ebert, MD, FACS; Samuel Wells, MD, FACS; Dr. Nahrwold; Thomas R. Russell, MD, FACS; and David B. Hoyt, MD, FACS. Through these positions, Dr. Hanlon had a profound effect on the direction and philosophy of the College, including in philanthropic endeavors and the establishment of the ACS Archives. He received the first ACS Lifetime Achievement Award in 2010.
“Hanlon’s integrity, faith, hard work, and service to others led him to become a role model for physicians and laypersons alike. These attributes also drove his brilliant career as an innovative surgeon, leadership in academic and organized medicine, and reputation as a humanist and ethicist,” Dr. Narhwold concludes in the preface. “Before he died I knew that I must write his biography to expose his principled life, his goodness, and his devotion to surgery and to surgeons, especially young surgeons, with the hope that they and others will find his life worthy of study and emulation.”
Dr. Nahrwold is Emeritus Professor of Surgery at Northwestern University Feinberg School of Medicine, Chicago, IL, where he was the Loyal and Edith Davis Professor and Chairman, department of surgery, and surgeon-in-chief, Northwestern Memorial Hospital. He is a recipient of the College’s highest honor—the Distinguished Service Award.
Dr. Nahrwold is author of A Mirror Reflecting Surgery, Surgeons, and their College: The Bulletin of the American College of Surgeons, and co-author, with Peter J. Kernahan, MD, PhD, FACS, of A Century of Surgeons and Surgery: The American College of Surgeons 1913–2012.
The Conscience of Surgery: C. Rollins Hanlon, MD, FACS, is available for $15.95 on the ACS E-Store at web4.facs.org/eBusiness/ProductCatalog/Product.aspx?ID=1060 and on amazon.com.
The American College of Surgeons (ACS) recently published a new biography of C. Rollins Hanlon, MD, FACS, ACS Past-Director, a seminal figure in the history of surgery and the College, titled The Conscience of Surgery: C. Rollins Hanlon, MD, FACS. Written by David L. Nahrwold, MD, FACS, this account examines the life of the erudite, principled cardiothoracic surgeon and innovator, who co-developed the Blalock-Hanlon operation with Alfred P. Blalock, MD, FACS.
The book covers every aspect of Dr. Hanlon’s life—from his boyhood in Baltimore, MD, to his quest to be the best clinician and surgeon-scientist, to his views on the government’s increasing influence on the delivery of surgical care, and to his undying love of the written word. For many surgeons, Dr. Hanlon was the embodiment of what it means to be a Fellow of the ACS.
“I got to know [Dr. Hanlon] as a person and a professional during my stint as the Interim Director of the ACS in 1999 when he was ‘retired’ and serving as Executive Consultant,” Dr. Nahrwold writes in the book’s preface. “He insisted that the mission of the College was to advance the ethical and competent practice of surgery and not to improve the financial well-being of surgeons.”
Throughout his career, Dr. Hanlon’s mentors, colleagues, and students included many eminent surgeons at Johns Hopkins Medical School, Baltimore, MD; Cincinnati General Hospital, OH; and the University of California, San Francisco. He trained under Dean DeWitt Lewis, Walter E. Dandy, Howard C. Naffziger, Warfield “Monty” Firor, and Mont Reid (all MD, FACS). He worked alongside William P. Longmire, MD, FACS; Dr. Blalock; and Mark C. Ravitch, MD, FACS; and his residents and interns at St. Louis University, MO, included Vallee Willman, Theodore Cooper, Theodore Dubuque, and William Stoneman (all MD, FACS), among others.
Dr. Hanlon served in the U.S. Navy in World War II, and followed with a distinguished career at Johns Hopkins and at St. Louis University, where, as chair of surgery, he developed the institution’s cardiac research capabilities, which helped to pioneer early open-heart and heart transplant procedures.
Dr. Hanlon became a Fellow of the College in 1953 and served as the ACS Director for 17 years (1969–1986), making him the longest-serving Director to date. Additionally, he served on the Board of Regents and as the ACS President (1985–1986). After retirement, he stayed on as ACS Executive Consultant, offering his sage advice to his successors, including Paul A. Ebert, MD, FACS; Samuel Wells, MD, FACS; Dr. Nahrwold; Thomas R. Russell, MD, FACS; and David B. Hoyt, MD, FACS. Through these positions, Dr. Hanlon had a profound effect on the direction and philosophy of the College, including in philanthropic endeavors and the establishment of the ACS Archives. He received the first ACS Lifetime Achievement Award in 2010.
“Hanlon’s integrity, faith, hard work, and service to others led him to become a role model for physicians and laypersons alike. These attributes also drove his brilliant career as an innovative surgeon, leadership in academic and organized medicine, and reputation as a humanist and ethicist,” Dr. Narhwold concludes in the preface. “Before he died I knew that I must write his biography to expose his principled life, his goodness, and his devotion to surgery and to surgeons, especially young surgeons, with the hope that they and others will find his life worthy of study and emulation.”
Dr. Nahrwold is Emeritus Professor of Surgery at Northwestern University Feinberg School of Medicine, Chicago, IL, where he was the Loyal and Edith Davis Professor and Chairman, department of surgery, and surgeon-in-chief, Northwestern Memorial Hospital. He is a recipient of the College’s highest honor—the Distinguished Service Award.
Dr. Nahrwold is author of A Mirror Reflecting Surgery, Surgeons, and their College: The Bulletin of the American College of Surgeons, and co-author, with Peter J. Kernahan, MD, PhD, FACS, of A Century of Surgeons and Surgery: The American College of Surgeons 1913–2012.
The Conscience of Surgery: C. Rollins Hanlon, MD, FACS, is available for $15.95 on the ACS E-Store at web4.facs.org/eBusiness/ProductCatalog/Product.aspx?ID=1060 and on amazon.com.
Heidi Nelson, MD, FACS, named Medical Director of ACS Cancer Programs
The American College of Surgeons (ACS) recently announced that Heidi Nelson, MD, FACS, a colorectal surgeon from Rochester, MN, will be joining the ACS Division of Research and Optimal Patient Care (DROPC) as Medical Director, Cancer Programs, succeeding David P. Winchester, MD, FACS, as he transitions from the position he has served in for more than 30 years. Dr. Nelson comes to the ACS from her position as chair, and vice-chair for research, department of surgery, Mayo Clinic, as well as professor of surgery, Mayo Clinic College of Medicine and Science, Rochester. She has master’s faculty privileges in clinical and translation science at the Mayo Clinic Graduate School of Biomedical Sciences and the Mayo Clinic College of Medicine and Science.
Dr. Nelson received a bachelor’s degree from Western Washington University, Bellingham, and her medical degree from the University of Washington School of Medicine, Seattle. She completed an internship and residency in general surgery at Oregon Health & Science University, Portland, where she also served as an American Cancer Society Fellow. She then went to the Mayo Clinic College of Medicine and Science, where she was a colon and rectal surgery fellow and completed a research fellowship. Dr. Nelson returned to the University of Washington, where she was a Leo Hirsch Traveling Fellow.
Dr. Nelson has received numerous awards and held membership in many professional organizations, including the American Society of Colon and Rectal Surgeons (ASCRS), the Mayo Clinic Board of Governors, the Society of Surgical Oncology, and the Association of Women Surgeons, among others.
Research activities
As the Fred C. Andersen Professor for the Mayo Foundation and a consultant for Mayo Clinic’s division of colon and rectal surgery, Dr. Nelson is internationally renowned for her research in the field of colon and rectal cancer. The goal of her research activities has been to improve the duration and quality of life for these patients. These efforts have helped to reduce the impact of surgery on patients with early-stage disease through the safe introduction of laparoscopic and minimally invasive surgical approaches. Her work also has helped to reduce the cancer burden in patients with locally advanced and recurrent rectal cancer through studies examining the role of complex operations and intraoperative radiation therapy. Dr. Nelson’s work has been funded by the National Institutes of Health, the American Cancer Society, the ASCRS, and many other organizations. In addition to her clinical activities, she has led the Center for Individualized Medicine Microbiome Program at the Mayo Clinic, where she conducts, presents, and publishes research on the human microbiome and its connection to health and disease.
Leadership
Dr. Nelson brings a wealth of experience from leading others and establishing results-oriented teams. She has mentored trainees and investigators and has served as an editor and publisher for high-impact journals. She also has been extensively involved with the ACS throughout her career—Dr. Nelson became an ACS Fellow in 1993 and has served as former Director, ACS Clinical Research Program; former co-chair, ACS Oncology Group; and as a member, Commission on Cancer Executive Committee.
Dr. Nelson started working with the ACS in September on an initial part-time basis, overlapping with Dr. Winchester to ensure a smooth transition and continuity of leadership.
“The American College of Surgeons is excited about Dr. Nelson joining our Executive Leadership Team. Her research acumen and leadership in the cancer care community are well known and widely respected. Her addition to our team will benefit our members, our relationships with cancer care organizations, and the patients whom we serve,” said ACS Executive Director David B. Hoyt, MD, FACS.
The American College of Surgeons (ACS) recently announced that Heidi Nelson, MD, FACS, a colorectal surgeon from Rochester, MN, will be joining the ACS Division of Research and Optimal Patient Care (DROPC) as Medical Director, Cancer Programs, succeeding David P. Winchester, MD, FACS, as he transitions from the position he has served in for more than 30 years. Dr. Nelson comes to the ACS from her position as chair, and vice-chair for research, department of surgery, Mayo Clinic, as well as professor of surgery, Mayo Clinic College of Medicine and Science, Rochester. She has master’s faculty privileges in clinical and translation science at the Mayo Clinic Graduate School of Biomedical Sciences and the Mayo Clinic College of Medicine and Science.
Dr. Nelson received a bachelor’s degree from Western Washington University, Bellingham, and her medical degree from the University of Washington School of Medicine, Seattle. She completed an internship and residency in general surgery at Oregon Health & Science University, Portland, where she also served as an American Cancer Society Fellow. She then went to the Mayo Clinic College of Medicine and Science, where she was a colon and rectal surgery fellow and completed a research fellowship. Dr. Nelson returned to the University of Washington, where she was a Leo Hirsch Traveling Fellow.
Dr. Nelson has received numerous awards and held membership in many professional organizations, including the American Society of Colon and Rectal Surgeons (ASCRS), the Mayo Clinic Board of Governors, the Society of Surgical Oncology, and the Association of Women Surgeons, among others.
Research activities
As the Fred C. Andersen Professor for the Mayo Foundation and a consultant for Mayo Clinic’s division of colon and rectal surgery, Dr. Nelson is internationally renowned for her research in the field of colon and rectal cancer. The goal of her research activities has been to improve the duration and quality of life for these patients. These efforts have helped to reduce the impact of surgery on patients with early-stage disease through the safe introduction of laparoscopic and minimally invasive surgical approaches. Her work also has helped to reduce the cancer burden in patients with locally advanced and recurrent rectal cancer through studies examining the role of complex operations and intraoperative radiation therapy. Dr. Nelson’s work has been funded by the National Institutes of Health, the American Cancer Society, the ASCRS, and many other organizations. In addition to her clinical activities, she has led the Center for Individualized Medicine Microbiome Program at the Mayo Clinic, where she conducts, presents, and publishes research on the human microbiome and its connection to health and disease.
Leadership
Dr. Nelson brings a wealth of experience from leading others and establishing results-oriented teams. She has mentored trainees and investigators and has served as an editor and publisher for high-impact journals. She also has been extensively involved with the ACS throughout her career—Dr. Nelson became an ACS Fellow in 1993 and has served as former Director, ACS Clinical Research Program; former co-chair, ACS Oncology Group; and as a member, Commission on Cancer Executive Committee.
Dr. Nelson started working with the ACS in September on an initial part-time basis, overlapping with Dr. Winchester to ensure a smooth transition and continuity of leadership.
“The American College of Surgeons is excited about Dr. Nelson joining our Executive Leadership Team. Her research acumen and leadership in the cancer care community are well known and widely respected. Her addition to our team will benefit our members, our relationships with cancer care organizations, and the patients whom we serve,” said ACS Executive Director David B. Hoyt, MD, FACS.
The American College of Surgeons (ACS) recently announced that Heidi Nelson, MD, FACS, a colorectal surgeon from Rochester, MN, will be joining the ACS Division of Research and Optimal Patient Care (DROPC) as Medical Director, Cancer Programs, succeeding David P. Winchester, MD, FACS, as he transitions from the position he has served in for more than 30 years. Dr. Nelson comes to the ACS from her position as chair, and vice-chair for research, department of surgery, Mayo Clinic, as well as professor of surgery, Mayo Clinic College of Medicine and Science, Rochester. She has master’s faculty privileges in clinical and translation science at the Mayo Clinic Graduate School of Biomedical Sciences and the Mayo Clinic College of Medicine and Science.
Dr. Nelson received a bachelor’s degree from Western Washington University, Bellingham, and her medical degree from the University of Washington School of Medicine, Seattle. She completed an internship and residency in general surgery at Oregon Health & Science University, Portland, where she also served as an American Cancer Society Fellow. She then went to the Mayo Clinic College of Medicine and Science, where she was a colon and rectal surgery fellow and completed a research fellowship. Dr. Nelson returned to the University of Washington, where she was a Leo Hirsch Traveling Fellow.
Dr. Nelson has received numerous awards and held membership in many professional organizations, including the American Society of Colon and Rectal Surgeons (ASCRS), the Mayo Clinic Board of Governors, the Society of Surgical Oncology, and the Association of Women Surgeons, among others.
Research activities
As the Fred C. Andersen Professor for the Mayo Foundation and a consultant for Mayo Clinic’s division of colon and rectal surgery, Dr. Nelson is internationally renowned for her research in the field of colon and rectal cancer. The goal of her research activities has been to improve the duration and quality of life for these patients. These efforts have helped to reduce the impact of surgery on patients with early-stage disease through the safe introduction of laparoscopic and minimally invasive surgical approaches. Her work also has helped to reduce the cancer burden in patients with locally advanced and recurrent rectal cancer through studies examining the role of complex operations and intraoperative radiation therapy. Dr. Nelson’s work has been funded by the National Institutes of Health, the American Cancer Society, the ASCRS, and many other organizations. In addition to her clinical activities, she has led the Center for Individualized Medicine Microbiome Program at the Mayo Clinic, where she conducts, presents, and publishes research on the human microbiome and its connection to health and disease.
Leadership
Dr. Nelson brings a wealth of experience from leading others and establishing results-oriented teams. She has mentored trainees and investigators and has served as an editor and publisher for high-impact journals. She also has been extensively involved with the ACS throughout her career—Dr. Nelson became an ACS Fellow in 1993 and has served as former Director, ACS Clinical Research Program; former co-chair, ACS Oncology Group; and as a member, Commission on Cancer Executive Committee.
Dr. Nelson started working with the ACS in September on an initial part-time basis, overlapping with Dr. Winchester to ensure a smooth transition and continuity of leadership.
“The American College of Surgeons is excited about Dr. Nelson joining our Executive Leadership Team. Her research acumen and leadership in the cancer care community are well known and widely respected. Her addition to our team will benefit our members, our relationships with cancer care organizations, and the patients whom we serve,” said ACS Executive Director David B. Hoyt, MD, FACS.
Ronald V. Maier, MD, FACS, FRCSEd(Hon), FCSHK(Hon) installed as 2018–2019
Ronald. V. Maier, MD, FACS, FRCSEd(Hon), FCSHK(Hon), the Jane and Donald D. Trunkey Endowed Chair in Trauma Surgery; vice-chairman, department of surgery; and professor of surgery, University of Washington School of Medicine, Seattle, was installed as the 99th President of the American College of Surgeons (ACS) at Convocation, October 21, at Clinical Congress 2018 in Boston, MA.
Dr. Maier is highly esteemed for his contributions to trauma surgery, surgical research, and surgical education. In addition to his positions at the University of Washington, he is director, Northwest Regional Trauma Center; and surgeon-in-chief and co-director, surgical intensive care unit (SICU), Harborview Medical Center, Seattle. He also is associate medical staff, University of Washington Medical Center and Seattle Cancer Care Alliance. A Fellow of the College since 1984, Dr. Maier served as First Vice-President of the ACS (2015−2016) and has played an active role on several key committees, most notably the Committee on Trauma (COT).
Mark C. Weissler, MD, FACS, Past-Chair of the ACS Board of Regents (2014−2015) was installed as the First Vice-President. An otolaryngologist-head and neck surgeon, Dr. Weissler is the Joseph P. Riddle Distinguished Professor, department of otolaryngology–head and neck surgery, and chief, division of head and neck surgery, University of North Carolina (UNC) School of Medicine, Chapel Hill. An ACS Fellow since 1989, Dr. Weissler is a former ACS Regent, serving as Vice-Chair of the Board of Regents for two years (2012–2014) and Chair for one year (2014−2015). He has served on the ACS Board of Governors and in other leadership capacities for the College, including the Committee on Ethics, Central Judiciary Committee, Advisory Council for Otolaryngology−Head and Neck Surgery; and President, North Carolina Chapter of the ACS.
The Second Vice-President is Phillip R. Caropreso, MD, FACS, a general surgeon from Keokuk, IA. A committed rural surgeon, Dr. Caropreso has practiced in Mason City, IA; Keokuk, IA; and Carthage, IL. Academic positions have included serving on the teaching faculty, family practice residency, North Iowa Medical Center, Mason City; adjunct clinical professor of surgery, University of Iowa, Iowa City; and director, general surgery rotation, North Iowa Medical Center. A Fellow of the ACS since 1979, Dr. Caropreso has been active at the local and national level. He was Chair, Iowa State COT; President of the Iowa Chapter; and ACS Governor, serving on the Board of Governors Committee on Surgical Practices.
Read more about Dr. Maier, Dr. Weissler, and Dr. Caropreso in the November Bulletin at www.bulletin.facs.org.
Ronald. V. Maier, MD, FACS, FRCSEd(Hon), FCSHK(Hon), the Jane and Donald D. Trunkey Endowed Chair in Trauma Surgery; vice-chairman, department of surgery; and professor of surgery, University of Washington School of Medicine, Seattle, was installed as the 99th President of the American College of Surgeons (ACS) at Convocation, October 21, at Clinical Congress 2018 in Boston, MA.
Dr. Maier is highly esteemed for his contributions to trauma surgery, surgical research, and surgical education. In addition to his positions at the University of Washington, he is director, Northwest Regional Trauma Center; and surgeon-in-chief and co-director, surgical intensive care unit (SICU), Harborview Medical Center, Seattle. He also is associate medical staff, University of Washington Medical Center and Seattle Cancer Care Alliance. A Fellow of the College since 1984, Dr. Maier served as First Vice-President of the ACS (2015−2016) and has played an active role on several key committees, most notably the Committee on Trauma (COT).
Mark C. Weissler, MD, FACS, Past-Chair of the ACS Board of Regents (2014−2015) was installed as the First Vice-President. An otolaryngologist-head and neck surgeon, Dr. Weissler is the Joseph P. Riddle Distinguished Professor, department of otolaryngology–head and neck surgery, and chief, division of head and neck surgery, University of North Carolina (UNC) School of Medicine, Chapel Hill. An ACS Fellow since 1989, Dr. Weissler is a former ACS Regent, serving as Vice-Chair of the Board of Regents for two years (2012–2014) and Chair for one year (2014−2015). He has served on the ACS Board of Governors and in other leadership capacities for the College, including the Committee on Ethics, Central Judiciary Committee, Advisory Council for Otolaryngology−Head and Neck Surgery; and President, North Carolina Chapter of the ACS.
The Second Vice-President is Phillip R. Caropreso, MD, FACS, a general surgeon from Keokuk, IA. A committed rural surgeon, Dr. Caropreso has practiced in Mason City, IA; Keokuk, IA; and Carthage, IL. Academic positions have included serving on the teaching faculty, family practice residency, North Iowa Medical Center, Mason City; adjunct clinical professor of surgery, University of Iowa, Iowa City; and director, general surgery rotation, North Iowa Medical Center. A Fellow of the ACS since 1979, Dr. Caropreso has been active at the local and national level. He was Chair, Iowa State COT; President of the Iowa Chapter; and ACS Governor, serving on the Board of Governors Committee on Surgical Practices.
Read more about Dr. Maier, Dr. Weissler, and Dr. Caropreso in the November Bulletin at www.bulletin.facs.org.
Ronald. V. Maier, MD, FACS, FRCSEd(Hon), FCSHK(Hon), the Jane and Donald D. Trunkey Endowed Chair in Trauma Surgery; vice-chairman, department of surgery; and professor of surgery, University of Washington School of Medicine, Seattle, was installed as the 99th President of the American College of Surgeons (ACS) at Convocation, October 21, at Clinical Congress 2018 in Boston, MA.
Dr. Maier is highly esteemed for his contributions to trauma surgery, surgical research, and surgical education. In addition to his positions at the University of Washington, he is director, Northwest Regional Trauma Center; and surgeon-in-chief and co-director, surgical intensive care unit (SICU), Harborview Medical Center, Seattle. He also is associate medical staff, University of Washington Medical Center and Seattle Cancer Care Alliance. A Fellow of the College since 1984, Dr. Maier served as First Vice-President of the ACS (2015−2016) and has played an active role on several key committees, most notably the Committee on Trauma (COT).
Mark C. Weissler, MD, FACS, Past-Chair of the ACS Board of Regents (2014−2015) was installed as the First Vice-President. An otolaryngologist-head and neck surgeon, Dr. Weissler is the Joseph P. Riddle Distinguished Professor, department of otolaryngology–head and neck surgery, and chief, division of head and neck surgery, University of North Carolina (UNC) School of Medicine, Chapel Hill. An ACS Fellow since 1989, Dr. Weissler is a former ACS Regent, serving as Vice-Chair of the Board of Regents for two years (2012–2014) and Chair for one year (2014−2015). He has served on the ACS Board of Governors and in other leadership capacities for the College, including the Committee on Ethics, Central Judiciary Committee, Advisory Council for Otolaryngology−Head and Neck Surgery; and President, North Carolina Chapter of the ACS.
The Second Vice-President is Phillip R. Caropreso, MD, FACS, a general surgeon from Keokuk, IA. A committed rural surgeon, Dr. Caropreso has practiced in Mason City, IA; Keokuk, IA; and Carthage, IL. Academic positions have included serving on the teaching faculty, family practice residency, North Iowa Medical Center, Mason City; adjunct clinical professor of surgery, University of Iowa, Iowa City; and director, general surgery rotation, North Iowa Medical Center. A Fellow of the ACS since 1979, Dr. Caropreso has been active at the local and national level. He was Chair, Iowa State COT; President of the Iowa Chapter; and ACS Governor, serving on the Board of Governors Committee on Surgical Practices.
Read more about Dr. Maier, Dr. Weissler, and Dr. Caropreso in the November Bulletin at www.bulletin.facs.org.
VRIC Registration and Abtract Submission Site Now Open
Both registration and the abstract submission site for the 2019 Vascular Research Initiatives Conference are now open. This one-day meeting encourages interactive participation of all attendees and emphasizes emerging vascular science. To maximize researchers' and participants' travel dollars and time, VRIC will be held on May 13, 2019, in Boston, the day before the American Heart Association’s Vascular Discovery Scientific Sessions
Both registration and the abstract submission site for the 2019 Vascular Research Initiatives Conference are now open. This one-day meeting encourages interactive participation of all attendees and emphasizes emerging vascular science. To maximize researchers' and participants' travel dollars and time, VRIC will be held on May 13, 2019, in Boston, the day before the American Heart Association’s Vascular Discovery Scientific Sessions
Both registration and the abstract submission site for the 2019 Vascular Research Initiatives Conference are now open. This one-day meeting encourages interactive participation of all attendees and emphasizes emerging vascular science. To maximize researchers' and participants' travel dollars and time, VRIC will be held on May 13, 2019, in Boston, the day before the American Heart Association’s Vascular Discovery Scientific Sessions