User login
Environmental scan: Drivers of change in technology
Emerging technology has long been a driver of change in health care, and the pace of technological change has accelerated dramatically in the past decade. Physicians are being challenged to incorporate blockchain technology, virtual health care, artificial intelligence, gamification of learning, and the rapidly developing Internet of Things into their work and into their interactions with patients.
Blockchain in health care
Blockchain is a log of activity that is time stamped, tamper proof, and shared across a network of computers. Each transaction that goes into the log of activity is enclosed in a block and linked together in chronological order to form a chain, now called blockchain.
The potential applications of this emerging technology in health-care delivery are almost limitless.1 Shared, secure, and linked data that can be accessed by all can give rise to the automation of complex problems, community-generated solutions to problems that empower patients, and an increase in trust, transparency, and incentive alignment. Currently, insurance claims, prescriptions, and payments mostly reside in sequestered computer systems, but a blockchain of the transactions among them would open up a wealth of learning and efficiency possibilities.2 Hospitals, medical centers, insurance companies, clinical trials, and large practices can collaborate to create a blockchain of transactions in which all members can view access, share, and analyze the data.
Burton Lesnick, MD, FCCP, has given the topic of technology change and the practice of medicine some thought. He is a member of the CHEST Board of Regents and the former founding medical director of The Children’s Care Network, a pediatric accountable care organization of 1,800 providers in metro Atlanta area. Dr. Lesnick notes that blockchain is still in its early phases, partly because it is expensive in terms of computing power and electricity to adequately maintain a distributed ledger.
“I would see it being used in the next decade for high-value public registries, especially where the authenticity of data is critical. For instance, in Europe, we are already seeing a lot of effort to prevent counterfeit drugs from entering the pharmacy chain. We may soon see blockchain being used to track expensive drugs in our health-care system, thus ensuring chain of possession and preventing fraud,” he said.
Virtual care
Some traditional face-to-face encounters between doctor and patient will be replaced by virtual care of different types. Telemedicine is growing, thanks in part to advocacy from Medicare and Medicaid, although the lack of federal guidance on coverage and reimbursement could be a barrier.3 mHealth, the delivery of care via mobile devices, is being utilized for preventive services, appointment confirmation, and follow-up information, but the future of this technology will probably expand into transmission of data from patients and health devices, as well as health alerts.

According to a report by the World Health Organization, an increasing proportion of the population is accessing health information and services through mobile phones.4 According to the Physicians Practice 2018 Mobile Health Survey, a majority of practices that participated in the study stated they use mobile health in their practice on a weekly basis.5 Those still not using mHealth cite concerns over HIPAA compliance. Dr. Lesnick offers some cautionary perspectives.
“Many of us can already download data from medical devices such as CPAP machines and home ventilators. A prominent pharmaceutical company has recently gained FDA approval for an inhaler that date and time stamps when and how the inhaler has been used. Wearable health devices, such as fitness monitors and watches that can alert users about life-threatening arrhythmias are wonderful. But the potential for physicians being overwhelmed by the incoming data flow is concerning. This is especially true when physicians are already reporting high levels of burnout associated with frustration using electronic medical record systems. We can only hope that algorithms will be developed to sift the precious stones from the digital effluent.”
Despite the security concerns, health-care providers, along with the Centers for Medicare & Medicaid Services and the insurance industry, are planning to address the projected shortages in the health-care workforce with virtual care.3
Dr. Lesnick added, “Doctors need to be engaged at the level of their health-care systems and national organizations. Providers are needed to provide context and balance to ensure that new technology utilizes appropriate scope of practice, optimizes care, and reduces costs, while reducing burdens on caregivers.”
Artificial intelligence and the Internet of Things
Artificial intelligence (AI) in health care is the use of complex algorithms and software to approximate human analysis of complicated medical data. The applications in medicine are potentially limitless given the rapid accumulation of data related to health care.
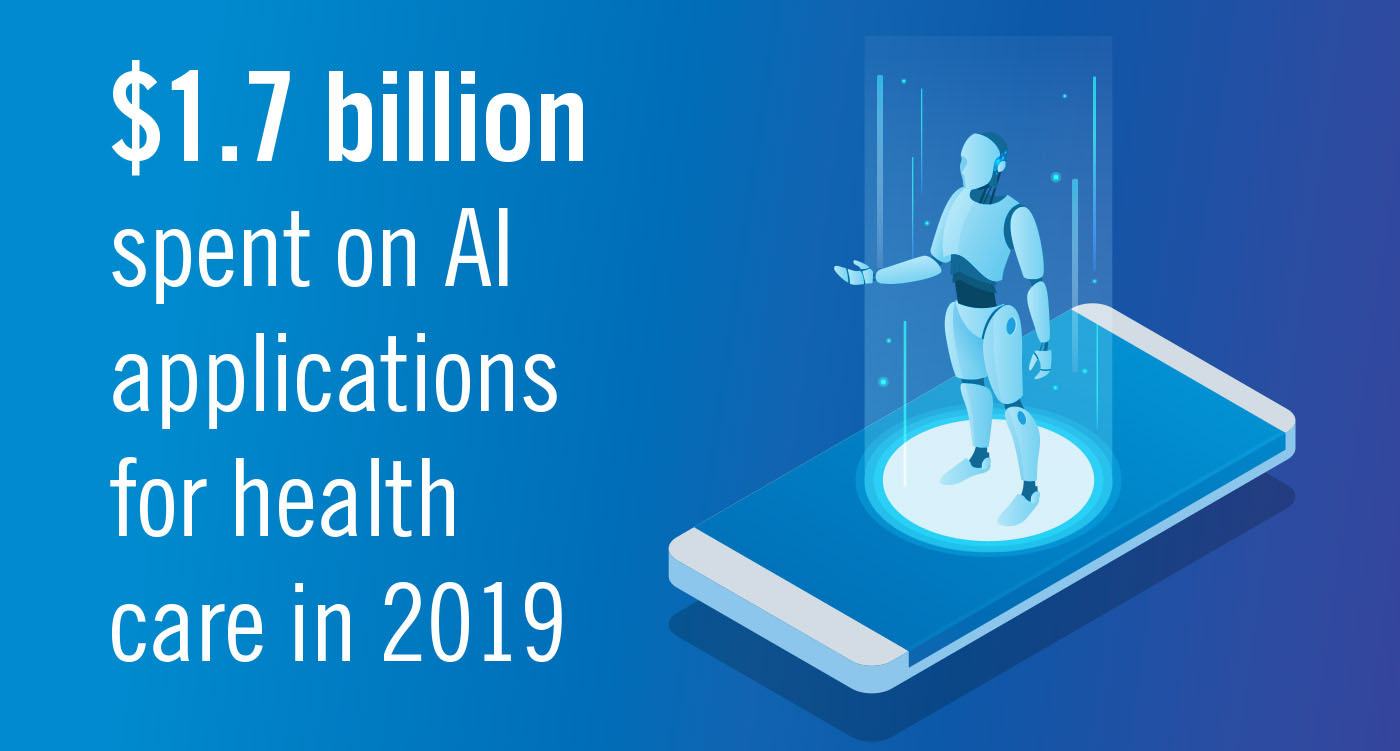
According to Forbes, AI for health-care IT application will cross $1.7 billion by 2019.2 By operationalizing AI platforms across select health-care workflows, organizations could see significant productivity gains during the next few years. Forbes also predicts more AI solutions will be used in imaging diagnostics, drug discovery, and risk-analytics applications.2
At the Icahn School of Medicine at Mount Sinai, New York, researchers use an in-house AI system known as Deep Patient, to predict risk factors for 78 different diseases. Doctors use the system to aid in diagnoses.9 AI is being used to diagnose patient wounds via smartphones, remotely monitor the elderly, and help health systems to digitally verify a patient’s insurance information.
Dr. Lesnick observed that chess computers started beating grand masters more than 20 years ago. However, the best chess players, in combination with a computer, can still reliably beat a computer alone. We need organizations like CHEST to help us become more adept at using technology. AI is a powerful tool but just another instrument to be employed in care of patients.
Big data and AI will combine to create a new ways of practicing medicine in the coming years, but what this trend will mean to individual clinicians remains to seen.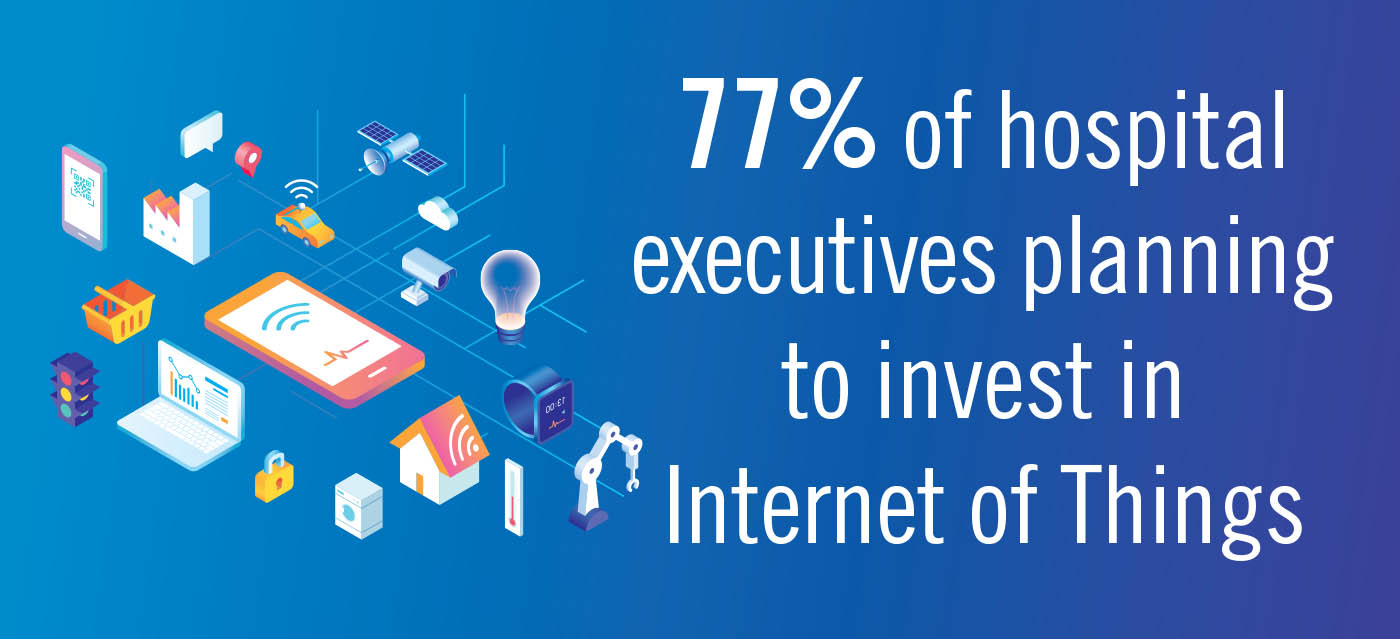
An area of rapid development is the Internet of Things, the extension of internet connectivity into everyday objects and devices designed to monitor and send information. Health-care devices now incorporate AI, real-time analytics, machine learning, physiologic sensors, and embedded systems.10 Physicians will increasingly have access to real-time data on individual patients. For physicians, managing, storing, and analyzing data from the personalized health-care devices of their patients will be a major challenge as the Internet of Things continues to expand into health care.
Dr. Lesnick noted, “In my collaboration with Georgia Tech [in Atlanta], one area I’m really excited about is process mining. Instead of sorting individual data points for statistical correlation, process mining looks at groups of actions and decisions. We’ve applied this to our local emergency room. I’m hoping we can find the most efficient processes and hardwire them in order sets. If we can eventually apply process mining to the health-care system as a whole, we might start to see gains in efficiencies.”
Gamification
Gamification is the term used to describe any tool or platform that applies game mechanics to nongame initiatives in order to encourage and increase engagement. Elements of gamification often include the use of badges, reward points, prizes, social interaction, and leaderboards. Gamification is frequently used by sales teams, marketers, employee training and performance management, onboarding, learning management, and health and wellness.11
The rise in smartphone ownership and wearable technology will likely increase the adoption of gamification technologies to manage health-related concerns and issues. Patient education via gamification is a potentially powerful tool to enhance engagement around disease management. Maintenance of certification and CME are also growth areas for gamification.
Cybersecurity and data breaches
The rapid development of mobile devices and the Internet of Things, in addition to the transmission of health data on a massive scale, will mean more health data will be stolen for a variety of illegal purposes. Hacking and unauthorized access are now common occurrences. Privacy breaches, potential HIPAA violations, and financial damage to patients and institutions are all areas of concern that accompany technological changes.12

Dr. Lesnick stressed that all health-care professionals must be accountable for safeguarding patient information and using the latest security software. “Physicians can be advocates for their patients by cautioning them about the risks of placing their private medical information into public spaces, such as social media. Patients should also know that they may be waiving their privacy rights when they utilize commercial entities that collect and store DNA analyses for purposes of ancestry tracking or medical screening,” he concluded.
References
1. Dhillon V et al. “Blockchain in healthcare: Innovations that empower patients, connect professionals and improve care.” (New York: CRC Press, 2019).
2. Das R. Top 8 healthcare predictions for 2019. Forbes. 2018 Nov 13.
3. 2019 Predictions. Teladoc Health. 2019. http://go.teladochealth.com/predictions/3/.
4. Director-General. “mHealth: Use of appropriate digital technologies for public health.” World Health Organization. 2018 Mar 26.
5. Physicians Practice Staff. 2018 Mobile Health Survey Results. Physicians Practice. 2018 Feb 20.
6. Trend 1: Citizen AI. Accenture. 2018 May 24.
7. Siwicki B. Zocdoc appointment booking app now verifies insurance with AI. Healthcare IT News. 2017 Oct 25
8. Schepke J. What’s your healthcare gamification strategy? Becker’s Healthcare. 2018 May 31.
9. November 2018 healthcare data breach report. HIPAA Journal. 2018 Dec 20.
10. Siwicki, B. Zocdoc appointment booking app now verifies insurance with AI. HeathcareITNews. 2017 Oct 25.
11. Schepke, J. What’s your healthcare gamification strategy? Becker’s Health IT & CIO Report. 2018. May 31.
12. November 2018 healthcare data breach report. HIPAA Journal. 2018 Dec 20.
Note: Background research performed by Avenue M Group.
Emerging technology has long been a driver of change in health care, and the pace of technological change has accelerated dramatically in the past decade. Physicians are being challenged to incorporate blockchain technology, virtual health care, artificial intelligence, gamification of learning, and the rapidly developing Internet of Things into their work and into their interactions with patients.
Blockchain in health care
Blockchain is a log of activity that is time stamped, tamper proof, and shared across a network of computers. Each transaction that goes into the log of activity is enclosed in a block and linked together in chronological order to form a chain, now called blockchain.
The potential applications of this emerging technology in health-care delivery are almost limitless.1 Shared, secure, and linked data that can be accessed by all can give rise to the automation of complex problems, community-generated solutions to problems that empower patients, and an increase in trust, transparency, and incentive alignment. Currently, insurance claims, prescriptions, and payments mostly reside in sequestered computer systems, but a blockchain of the transactions among them would open up a wealth of learning and efficiency possibilities.2 Hospitals, medical centers, insurance companies, clinical trials, and large practices can collaborate to create a blockchain of transactions in which all members can view access, share, and analyze the data.
Burton Lesnick, MD, FCCP, has given the topic of technology change and the practice of medicine some thought. He is a member of the CHEST Board of Regents and the former founding medical director of The Children’s Care Network, a pediatric accountable care organization of 1,800 providers in metro Atlanta area. Dr. Lesnick notes that blockchain is still in its early phases, partly because it is expensive in terms of computing power and electricity to adequately maintain a distributed ledger.
“I would see it being used in the next decade for high-value public registries, especially where the authenticity of data is critical. For instance, in Europe, we are already seeing a lot of effort to prevent counterfeit drugs from entering the pharmacy chain. We may soon see blockchain being used to track expensive drugs in our health-care system, thus ensuring chain of possession and preventing fraud,” he said.
Virtual care
Some traditional face-to-face encounters between doctor and patient will be replaced by virtual care of different types. Telemedicine is growing, thanks in part to advocacy from Medicare and Medicaid, although the lack of federal guidance on coverage and reimbursement could be a barrier.3 mHealth, the delivery of care via mobile devices, is being utilized for preventive services, appointment confirmation, and follow-up information, but the future of this technology will probably expand into transmission of data from patients and health devices, as well as health alerts.

According to a report by the World Health Organization, an increasing proportion of the population is accessing health information and services through mobile phones.4 According to the Physicians Practice 2018 Mobile Health Survey, a majority of practices that participated in the study stated they use mobile health in their practice on a weekly basis.5 Those still not using mHealth cite concerns over HIPAA compliance. Dr. Lesnick offers some cautionary perspectives.
“Many of us can already download data from medical devices such as CPAP machines and home ventilators. A prominent pharmaceutical company has recently gained FDA approval for an inhaler that date and time stamps when and how the inhaler has been used. Wearable health devices, such as fitness monitors and watches that can alert users about life-threatening arrhythmias are wonderful. But the potential for physicians being overwhelmed by the incoming data flow is concerning. This is especially true when physicians are already reporting high levels of burnout associated with frustration using electronic medical record systems. We can only hope that algorithms will be developed to sift the precious stones from the digital effluent.”
Despite the security concerns, health-care providers, along with the Centers for Medicare & Medicaid Services and the insurance industry, are planning to address the projected shortages in the health-care workforce with virtual care.3
Dr. Lesnick added, “Doctors need to be engaged at the level of their health-care systems and national organizations. Providers are needed to provide context and balance to ensure that new technology utilizes appropriate scope of practice, optimizes care, and reduces costs, while reducing burdens on caregivers.”
Artificial intelligence and the Internet of Things
Artificial intelligence (AI) in health care is the use of complex algorithms and software to approximate human analysis of complicated medical data. The applications in medicine are potentially limitless given the rapid accumulation of data related to health care.
According to Forbes, AI for health-care IT application will cross $1.7 billion by 2019.2 By operationalizing AI platforms across select health-care workflows, organizations could see significant productivity gains during the next few years. Forbes also predicts more AI solutions will be used in imaging diagnostics, drug discovery, and risk-analytics applications.2
At the Icahn School of Medicine at Mount Sinai, New York, researchers use an in-house AI system known as Deep Patient, to predict risk factors for 78 different diseases. Doctors use the system to aid in diagnoses.9 AI is being used to diagnose patient wounds via smartphones, remotely monitor the elderly, and help health systems to digitally verify a patient’s insurance information.
Dr. Lesnick observed that chess computers started beating grand masters more than 20 years ago. However, the best chess players, in combination with a computer, can still reliably beat a computer alone. We need organizations like CHEST to help us become more adept at using technology. AI is a powerful tool but just another instrument to be employed in care of patients.
Big data and AI will combine to create a new ways of practicing medicine in the coming years, but what this trend will mean to individual clinicians remains to seen.
An area of rapid development is the Internet of Things, the extension of internet connectivity into everyday objects and devices designed to monitor and send information. Health-care devices now incorporate AI, real-time analytics, machine learning, physiologic sensors, and embedded systems.10 Physicians will increasingly have access to real-time data on individual patients. For physicians, managing, storing, and analyzing data from the personalized health-care devices of their patients will be a major challenge as the Internet of Things continues to expand into health care.
Dr. Lesnick noted, “In my collaboration with Georgia Tech [in Atlanta], one area I’m really excited about is process mining. Instead of sorting individual data points for statistical correlation, process mining looks at groups of actions and decisions. We’ve applied this to our local emergency room. I’m hoping we can find the most efficient processes and hardwire them in order sets. If we can eventually apply process mining to the health-care system as a whole, we might start to see gains in efficiencies.”
Gamification
Gamification is the term used to describe any tool or platform that applies game mechanics to nongame initiatives in order to encourage and increase engagement. Elements of gamification often include the use of badges, reward points, prizes, social interaction, and leaderboards. Gamification is frequently used by sales teams, marketers, employee training and performance management, onboarding, learning management, and health and wellness.11
The rise in smartphone ownership and wearable technology will likely increase the adoption of gamification technologies to manage health-related concerns and issues. Patient education via gamification is a potentially powerful tool to enhance engagement around disease management. Maintenance of certification and CME are also growth areas for gamification.
Cybersecurity and data breaches
The rapid development of mobile devices and the Internet of Things, in addition to the transmission of health data on a massive scale, will mean more health data will be stolen for a variety of illegal purposes. Hacking and unauthorized access are now common occurrences. Privacy breaches, potential HIPAA violations, and financial damage to patients and institutions are all areas of concern that accompany technological changes.12

Dr. Lesnick stressed that all health-care professionals must be accountable for safeguarding patient information and using the latest security software. “Physicians can be advocates for their patients by cautioning them about the risks of placing their private medical information into public spaces, such as social media. Patients should also know that they may be waiving their privacy rights when they utilize commercial entities that collect and store DNA analyses for purposes of ancestry tracking or medical screening,” he concluded.
References
1. Dhillon V et al. “Blockchain in healthcare: Innovations that empower patients, connect professionals and improve care.” (New York: CRC Press, 2019).
2. Das R. Top 8 healthcare predictions for 2019. Forbes. 2018 Nov 13.
3. 2019 Predictions. Teladoc Health. 2019. http://go.teladochealth.com/predictions/3/.
4. Director-General. “mHealth: Use of appropriate digital technologies for public health.” World Health Organization. 2018 Mar 26.
5. Physicians Practice Staff. 2018 Mobile Health Survey Results. Physicians Practice. 2018 Feb 20.
6. Trend 1: Citizen AI. Accenture. 2018 May 24.
7. Siwicki B. Zocdoc appointment booking app now verifies insurance with AI. Healthcare IT News. 2017 Oct 25
8. Schepke J. What’s your healthcare gamification strategy? Becker’s Healthcare. 2018 May 31.
9. November 2018 healthcare data breach report. HIPAA Journal. 2018 Dec 20.
10. Siwicki, B. Zocdoc appointment booking app now verifies insurance with AI. HeathcareITNews. 2017 Oct 25.
11. Schepke, J. What’s your healthcare gamification strategy? Becker’s Health IT & CIO Report. 2018. May 31.
12. November 2018 healthcare data breach report. HIPAA Journal. 2018 Dec 20.
Note: Background research performed by Avenue M Group.
Emerging technology has long been a driver of change in health care, and the pace of technological change has accelerated dramatically in the past decade. Physicians are being challenged to incorporate blockchain technology, virtual health care, artificial intelligence, gamification of learning, and the rapidly developing Internet of Things into their work and into their interactions with patients.
Blockchain in health care
Blockchain is a log of activity that is time stamped, tamper proof, and shared across a network of computers. Each transaction that goes into the log of activity is enclosed in a block and linked together in chronological order to form a chain, now called blockchain.
The potential applications of this emerging technology in health-care delivery are almost limitless.1 Shared, secure, and linked data that can be accessed by all can give rise to the automation of complex problems, community-generated solutions to problems that empower patients, and an increase in trust, transparency, and incentive alignment. Currently, insurance claims, prescriptions, and payments mostly reside in sequestered computer systems, but a blockchain of the transactions among them would open up a wealth of learning and efficiency possibilities.2 Hospitals, medical centers, insurance companies, clinical trials, and large practices can collaborate to create a blockchain of transactions in which all members can view access, share, and analyze the data.
Burton Lesnick, MD, FCCP, has given the topic of technology change and the practice of medicine some thought. He is a member of the CHEST Board of Regents and the former founding medical director of The Children’s Care Network, a pediatric accountable care organization of 1,800 providers in metro Atlanta area. Dr. Lesnick notes that blockchain is still in its early phases, partly because it is expensive in terms of computing power and electricity to adequately maintain a distributed ledger.
“I would see it being used in the next decade for high-value public registries, especially where the authenticity of data is critical. For instance, in Europe, we are already seeing a lot of effort to prevent counterfeit drugs from entering the pharmacy chain. We may soon see blockchain being used to track expensive drugs in our health-care system, thus ensuring chain of possession and preventing fraud,” he said.
Virtual care
Some traditional face-to-face encounters between doctor and patient will be replaced by virtual care of different types. Telemedicine is growing, thanks in part to advocacy from Medicare and Medicaid, although the lack of federal guidance on coverage and reimbursement could be a barrier.3 mHealth, the delivery of care via mobile devices, is being utilized for preventive services, appointment confirmation, and follow-up information, but the future of this technology will probably expand into transmission of data from patients and health devices, as well as health alerts.

According to a report by the World Health Organization, an increasing proportion of the population is accessing health information and services through mobile phones.4 According to the Physicians Practice 2018 Mobile Health Survey, a majority of practices that participated in the study stated they use mobile health in their practice on a weekly basis.5 Those still not using mHealth cite concerns over HIPAA compliance. Dr. Lesnick offers some cautionary perspectives.
“Many of us can already download data from medical devices such as CPAP machines and home ventilators. A prominent pharmaceutical company has recently gained FDA approval for an inhaler that date and time stamps when and how the inhaler has been used. Wearable health devices, such as fitness monitors and watches that can alert users about life-threatening arrhythmias are wonderful. But the potential for physicians being overwhelmed by the incoming data flow is concerning. This is especially true when physicians are already reporting high levels of burnout associated with frustration using electronic medical record systems. We can only hope that algorithms will be developed to sift the precious stones from the digital effluent.”
Despite the security concerns, health-care providers, along with the Centers for Medicare & Medicaid Services and the insurance industry, are planning to address the projected shortages in the health-care workforce with virtual care.3
Dr. Lesnick added, “Doctors need to be engaged at the level of their health-care systems and national organizations. Providers are needed to provide context and balance to ensure that new technology utilizes appropriate scope of practice, optimizes care, and reduces costs, while reducing burdens on caregivers.”
Artificial intelligence and the Internet of Things
Artificial intelligence (AI) in health care is the use of complex algorithms and software to approximate human analysis of complicated medical data. The applications in medicine are potentially limitless given the rapid accumulation of data related to health care.
According to Forbes, AI for health-care IT application will cross $1.7 billion by 2019.2 By operationalizing AI platforms across select health-care workflows, organizations could see significant productivity gains during the next few years. Forbes also predicts more AI solutions will be used in imaging diagnostics, drug discovery, and risk-analytics applications.2
At the Icahn School of Medicine at Mount Sinai, New York, researchers use an in-house AI system known as Deep Patient, to predict risk factors for 78 different diseases. Doctors use the system to aid in diagnoses.9 AI is being used to diagnose patient wounds via smartphones, remotely monitor the elderly, and help health systems to digitally verify a patient’s insurance information.
Dr. Lesnick observed that chess computers started beating grand masters more than 20 years ago. However, the best chess players, in combination with a computer, can still reliably beat a computer alone. We need organizations like CHEST to help us become more adept at using technology. AI is a powerful tool but just another instrument to be employed in care of patients.
Big data and AI will combine to create a new ways of practicing medicine in the coming years, but what this trend will mean to individual clinicians remains to seen.
An area of rapid development is the Internet of Things, the extension of internet connectivity into everyday objects and devices designed to monitor and send information. Health-care devices now incorporate AI, real-time analytics, machine learning, physiologic sensors, and embedded systems.10 Physicians will increasingly have access to real-time data on individual patients. For physicians, managing, storing, and analyzing data from the personalized health-care devices of their patients will be a major challenge as the Internet of Things continues to expand into health care.
Dr. Lesnick noted, “In my collaboration with Georgia Tech [in Atlanta], one area I’m really excited about is process mining. Instead of sorting individual data points for statistical correlation, process mining looks at groups of actions and decisions. We’ve applied this to our local emergency room. I’m hoping we can find the most efficient processes and hardwire them in order sets. If we can eventually apply process mining to the health-care system as a whole, we might start to see gains in efficiencies.”
Gamification
Gamification is the term used to describe any tool or platform that applies game mechanics to nongame initiatives in order to encourage and increase engagement. Elements of gamification often include the use of badges, reward points, prizes, social interaction, and leaderboards. Gamification is frequently used by sales teams, marketers, employee training and performance management, onboarding, learning management, and health and wellness.11
The rise in smartphone ownership and wearable technology will likely increase the adoption of gamification technologies to manage health-related concerns and issues. Patient education via gamification is a potentially powerful tool to enhance engagement around disease management. Maintenance of certification and CME are also growth areas for gamification.
Cybersecurity and data breaches
The rapid development of mobile devices and the Internet of Things, in addition to the transmission of health data on a massive scale, will mean more health data will be stolen for a variety of illegal purposes. Hacking and unauthorized access are now common occurrences. Privacy breaches, potential HIPAA violations, and financial damage to patients and institutions are all areas of concern that accompany technological changes.12

Dr. Lesnick stressed that all health-care professionals must be accountable for safeguarding patient information and using the latest security software. “Physicians can be advocates for their patients by cautioning them about the risks of placing their private medical information into public spaces, such as social media. Patients should also know that they may be waiving their privacy rights when they utilize commercial entities that collect and store DNA analyses for purposes of ancestry tracking or medical screening,” he concluded.
References
1. Dhillon V et al. “Blockchain in healthcare: Innovations that empower patients, connect professionals and improve care.” (New York: CRC Press, 2019).
2. Das R. Top 8 healthcare predictions for 2019. Forbes. 2018 Nov 13.
3. 2019 Predictions. Teladoc Health. 2019. http://go.teladochealth.com/predictions/3/.
4. Director-General. “mHealth: Use of appropriate digital technologies for public health.” World Health Organization. 2018 Mar 26.
5. Physicians Practice Staff. 2018 Mobile Health Survey Results. Physicians Practice. 2018 Feb 20.
6. Trend 1: Citizen AI. Accenture. 2018 May 24.
7. Siwicki B. Zocdoc appointment booking app now verifies insurance with AI. Healthcare IT News. 2017 Oct 25
8. Schepke J. What’s your healthcare gamification strategy? Becker’s Healthcare. 2018 May 31.
9. November 2018 healthcare data breach report. HIPAA Journal. 2018 Dec 20.
10. Siwicki, B. Zocdoc appointment booking app now verifies insurance with AI. HeathcareITNews. 2017 Oct 25.
11. Schepke, J. What’s your healthcare gamification strategy? Becker’s Health IT & CIO Report. 2018. May 31.
12. November 2018 healthcare data breach report. HIPAA Journal. 2018 Dec 20.
Note: Background research performed by Avenue M Group.
Dr. Mark Rosen - My mentor, my friend
By now, most of you know that the CHEST family lost one of our dearest members and leaders in early July, Past President Mark Rosen. This loss has been felt deeply by many, not only because he was taken so suddenly, but because of who Mark was and what he meant to us. We did not get the chance to say goodbye. We shared Mark’s official obituary last month in CHEST Physician. This month, we thought it important to share something more personal.
When I think of Mark, so many words come to mind: master educator, astute and caring clinician, researcher, mentor, leader. So many qualities come to mind: generous, kind, honest, brilliant, and funny. Mark loved CHEST. He gave so much to the organization and was happy to do so. He was one of the Past Presidents who contributed even more after his presidency than during or before. Mark left an enormous footprint on our educational programs, including the annual meeting, Pulmonary Board Review, and SEEK. He was instrumental in building our international educational programs and a key player in assisting our Chinese colleagues in establishing pulmonary fellowships in their country.
When I think of my own journey with Mark, I think back to the first time I saw him. I was a senior fellow taking the Pulmonary Board Review course in Chicago. I don’t remember much from that course – except for Mark’s presentations. They included everything you needed to know, in a very logical outline. More importantly, he had a presence on stage that was larger than life. He made you laugh throughout the entire talk! Mark’s humor was self-deprecating, and he made you feel like you had been best friends forever---even if he’d never met you. From that first encounter, he became a giant in chest medicine to me. It wasn’t too many years later that, as a junior volunteer leader in the organization, I was able to finally meet Mark. He could not have been more welcoming or humble, and he instantly took on the role of mentor. I was so lucky; not only did that mentorship grow, but so did our friendship. I quickly got to the point that I looked forward to the times I would travel for CHEST events, because I knew I would see Mark. I did establish one rule, however, when we started teaching together. I refused to follow Mark in the agenda, as there was no way I could ever live up to his presentation style and humor. I didn’t want to be a let down to the crowd!
Much of what I and others have accomplished with CHEST and in pulmonary medicine is directly related to the wonderful mentors we have had in the organization, and Mark was certainly one of the most prominent. He introduced me to so many additional friends and mentors. And, Mark did this for hundreds of trainees and junior faculty throughout his career. If I were to guess, I would say that this is the thing that made him most proud. Yes, he was an established international expert in several areas of pulmonary medicine; he held several prominent positions in academic medicine and at CHEST. But, what made him most happy was seeing his trainees and mentees succeed – you would have thought we were one of his kids (whom he was also very proud of and loved dearly). Mark was THE example of an outstanding mentor.
The memory I will carry forever of Mark, however, is when he got on stage and was the Master of Ceremonies for the CHEST Challenge Championship. He was in his element as an educator, interacting with the next generation of chest medicine physicians. He spent the entire time making the contestants, and the audience, laugh. People came to the final round to see Mark, even if they had no dog in the fight. I will always fondly recall that way he would look over at me and the other judges if he wasn’t sure about a team’s answer and then have an immediate witty comeback. Many of my CHEST friends have said that Mark was the Jerry Seinfeld of CHEST. I’ve never watched a single episode of Seinfeld, but if this description is true, I plan to!
Mark kept his sense of humor until the very end, telling me in his final days that he chose to focus on “humor markers,” rather than “tumor markers” – he said that always worked out better for him! Mark, we all miss you friend. We can’t wait to share a Chopin Martini with a twist of lemon when we see you on the other side. Thank you for all you did for your family, your patients, your trainees, your colleagues, and CHEST.
By now, most of you know that the CHEST family lost one of our dearest members and leaders in early July, Past President Mark Rosen. This loss has been felt deeply by many, not only because he was taken so suddenly, but because of who Mark was and what he meant to us. We did not get the chance to say goodbye. We shared Mark’s official obituary last month in CHEST Physician. This month, we thought it important to share something more personal.
When I think of Mark, so many words come to mind: master educator, astute and caring clinician, researcher, mentor, leader. So many qualities come to mind: generous, kind, honest, brilliant, and funny. Mark loved CHEST. He gave so much to the organization and was happy to do so. He was one of the Past Presidents who contributed even more after his presidency than during or before. Mark left an enormous footprint on our educational programs, including the annual meeting, Pulmonary Board Review, and SEEK. He was instrumental in building our international educational programs and a key player in assisting our Chinese colleagues in establishing pulmonary fellowships in their country.
When I think of my own journey with Mark, I think back to the first time I saw him. I was a senior fellow taking the Pulmonary Board Review course in Chicago. I don’t remember much from that course – except for Mark’s presentations. They included everything you needed to know, in a very logical outline. More importantly, he had a presence on stage that was larger than life. He made you laugh throughout the entire talk! Mark’s humor was self-deprecating, and he made you feel like you had been best friends forever---even if he’d never met you. From that first encounter, he became a giant in chest medicine to me. It wasn’t too many years later that, as a junior volunteer leader in the organization, I was able to finally meet Mark. He could not have been more welcoming or humble, and he instantly took on the role of mentor. I was so lucky; not only did that mentorship grow, but so did our friendship. I quickly got to the point that I looked forward to the times I would travel for CHEST events, because I knew I would see Mark. I did establish one rule, however, when we started teaching together. I refused to follow Mark in the agenda, as there was no way I could ever live up to his presentation style and humor. I didn’t want to be a let down to the crowd!
Much of what I and others have accomplished with CHEST and in pulmonary medicine is directly related to the wonderful mentors we have had in the organization, and Mark was certainly one of the most prominent. He introduced me to so many additional friends and mentors. And, Mark did this for hundreds of trainees and junior faculty throughout his career. If I were to guess, I would say that this is the thing that made him most proud. Yes, he was an established international expert in several areas of pulmonary medicine; he held several prominent positions in academic medicine and at CHEST. But, what made him most happy was seeing his trainees and mentees succeed – you would have thought we were one of his kids (whom he was also very proud of and loved dearly). Mark was THE example of an outstanding mentor.
The memory I will carry forever of Mark, however, is when he got on stage and was the Master of Ceremonies for the CHEST Challenge Championship. He was in his element as an educator, interacting with the next generation of chest medicine physicians. He spent the entire time making the contestants, and the audience, laugh. People came to the final round to see Mark, even if they had no dog in the fight. I will always fondly recall that way he would look over at me and the other judges if he wasn’t sure about a team’s answer and then have an immediate witty comeback. Many of my CHEST friends have said that Mark was the Jerry Seinfeld of CHEST. I’ve never watched a single episode of Seinfeld, but if this description is true, I plan to!
Mark kept his sense of humor until the very end, telling me in his final days that he chose to focus on “humor markers,” rather than “tumor markers” – he said that always worked out better for him! Mark, we all miss you friend. We can’t wait to share a Chopin Martini with a twist of lemon when we see you on the other side. Thank you for all you did for your family, your patients, your trainees, your colleagues, and CHEST.
By now, most of you know that the CHEST family lost one of our dearest members and leaders in early July, Past President Mark Rosen. This loss has been felt deeply by many, not only because he was taken so suddenly, but because of who Mark was and what he meant to us. We did not get the chance to say goodbye. We shared Mark’s official obituary last month in CHEST Physician. This month, we thought it important to share something more personal.
When I think of Mark, so many words come to mind: master educator, astute and caring clinician, researcher, mentor, leader. So many qualities come to mind: generous, kind, honest, brilliant, and funny. Mark loved CHEST. He gave so much to the organization and was happy to do so. He was one of the Past Presidents who contributed even more after his presidency than during or before. Mark left an enormous footprint on our educational programs, including the annual meeting, Pulmonary Board Review, and SEEK. He was instrumental in building our international educational programs and a key player in assisting our Chinese colleagues in establishing pulmonary fellowships in their country.
When I think of my own journey with Mark, I think back to the first time I saw him. I was a senior fellow taking the Pulmonary Board Review course in Chicago. I don’t remember much from that course – except for Mark’s presentations. They included everything you needed to know, in a very logical outline. More importantly, he had a presence on stage that was larger than life. He made you laugh throughout the entire talk! Mark’s humor was self-deprecating, and he made you feel like you had been best friends forever---even if he’d never met you. From that first encounter, he became a giant in chest medicine to me. It wasn’t too many years later that, as a junior volunteer leader in the organization, I was able to finally meet Mark. He could not have been more welcoming or humble, and he instantly took on the role of mentor. I was so lucky; not only did that mentorship grow, but so did our friendship. I quickly got to the point that I looked forward to the times I would travel for CHEST events, because I knew I would see Mark. I did establish one rule, however, when we started teaching together. I refused to follow Mark in the agenda, as there was no way I could ever live up to his presentation style and humor. I didn’t want to be a let down to the crowd!
Much of what I and others have accomplished with CHEST and in pulmonary medicine is directly related to the wonderful mentors we have had in the organization, and Mark was certainly one of the most prominent. He introduced me to so many additional friends and mentors. And, Mark did this for hundreds of trainees and junior faculty throughout his career. If I were to guess, I would say that this is the thing that made him most proud. Yes, he was an established international expert in several areas of pulmonary medicine; he held several prominent positions in academic medicine and at CHEST. But, what made him most happy was seeing his trainees and mentees succeed – you would have thought we were one of his kids (whom he was also very proud of and loved dearly). Mark was THE example of an outstanding mentor.
The memory I will carry forever of Mark, however, is when he got on stage and was the Master of Ceremonies for the CHEST Challenge Championship. He was in his element as an educator, interacting with the next generation of chest medicine physicians. He spent the entire time making the contestants, and the audience, laugh. People came to the final round to see Mark, even if they had no dog in the fight. I will always fondly recall that way he would look over at me and the other judges if he wasn’t sure about a team’s answer and then have an immediate witty comeback. Many of my CHEST friends have said that Mark was the Jerry Seinfeld of CHEST. I’ve never watched a single episode of Seinfeld, but if this description is true, I plan to!
Mark kept his sense of humor until the very end, telling me in his final days that he chose to focus on “humor markers,” rather than “tumor markers” – he said that always worked out better for him! Mark, we all miss you friend. We can’t wait to share a Chopin Martini with a twist of lemon when we see you on the other side. Thank you for all you did for your family, your patients, your trainees, your colleagues, and CHEST.
CHEST Foundation 2019
As we put summer in our rear-view mirror and look ahead to the switch of seasons and the vivid colors of fall and prepare to indulge and learn at CHEST 2019, it is evident change is in the air. Fall is a time of change and learning about the many opportunities the CHEST 2019 meeting offers our members, and it is also the launch of all that is changing and new for you to be a part of the CHEST Foundation.
At CHEST 2019 this year, the CHEST Foundation will be holding their 3rd Annual Women & Pulmonary Luncheon on Monday, October 21. This annual luncheon has brought over 350 attendees together to not only collaborate on patient care while focusing on gender differences but also to discuss better ways to advocate for career advancements for women pulmonologists. A new change for this year is the addition of a networking hour following the luncheon, creating an open environment to discuss empowerment, education, and resources.
The CHEST Foundation continues to help young clinicians come to the CHEST Annual Meeting. As of today, more than $250,000 has been awarded by the Foundation in travel grants and complimentary registrations to more than 125 early career clinicians. YOU can have an impact and make a change for an individual by supporting travel grants this year.
The Foundation’s most noteworthy change, and one we hope all of our membership and donors will be a part of, is the launch of our new endowment in 2019/2020. The Erin Popovich Endowment will enable access to resources for patients and families, empower patients to take charge, find support groups, seek second opinions, and more, and will support research to advance patient care and improve treatment options and outcomes. This endowment will change and improve quality of life for patients and families affected by interstitial lung disease, and we encourage you to join us at the Donor Lounge to learn more.
As you embrace the changing of the season and prepare your highlights for CHEST 2019 in NOLA, we invite you to come and discover all the changes and impact the CHEST Foundation is making and why you are so important in all we do!
As we put summer in our rear-view mirror and look ahead to the switch of seasons and the vivid colors of fall and prepare to indulge and learn at CHEST 2019, it is evident change is in the air. Fall is a time of change and learning about the many opportunities the CHEST 2019 meeting offers our members, and it is also the launch of all that is changing and new for you to be a part of the CHEST Foundation.
At CHEST 2019 this year, the CHEST Foundation will be holding their 3rd Annual Women & Pulmonary Luncheon on Monday, October 21. This annual luncheon has brought over 350 attendees together to not only collaborate on patient care while focusing on gender differences but also to discuss better ways to advocate for career advancements for women pulmonologists. A new change for this year is the addition of a networking hour following the luncheon, creating an open environment to discuss empowerment, education, and resources.
The CHEST Foundation continues to help young clinicians come to the CHEST Annual Meeting. As of today, more than $250,000 has been awarded by the Foundation in travel grants and complimentary registrations to more than 125 early career clinicians. YOU can have an impact and make a change for an individual by supporting travel grants this year.
The Foundation’s most noteworthy change, and one we hope all of our membership and donors will be a part of, is the launch of our new endowment in 2019/2020. The Erin Popovich Endowment will enable access to resources for patients and families, empower patients to take charge, find support groups, seek second opinions, and more, and will support research to advance patient care and improve treatment options and outcomes. This endowment will change and improve quality of life for patients and families affected by interstitial lung disease, and we encourage you to join us at the Donor Lounge to learn more.
As you embrace the changing of the season and prepare your highlights for CHEST 2019 in NOLA, we invite you to come and discover all the changes and impact the CHEST Foundation is making and why you are so important in all we do!
As we put summer in our rear-view mirror and look ahead to the switch of seasons and the vivid colors of fall and prepare to indulge and learn at CHEST 2019, it is evident change is in the air. Fall is a time of change and learning about the many opportunities the CHEST 2019 meeting offers our members, and it is also the launch of all that is changing and new for you to be a part of the CHEST Foundation.
At CHEST 2019 this year, the CHEST Foundation will be holding their 3rd Annual Women & Pulmonary Luncheon on Monday, October 21. This annual luncheon has brought over 350 attendees together to not only collaborate on patient care while focusing on gender differences but also to discuss better ways to advocate for career advancements for women pulmonologists. A new change for this year is the addition of a networking hour following the luncheon, creating an open environment to discuss empowerment, education, and resources.
The CHEST Foundation continues to help young clinicians come to the CHEST Annual Meeting. As of today, more than $250,000 has been awarded by the Foundation in travel grants and complimentary registrations to more than 125 early career clinicians. YOU can have an impact and make a change for an individual by supporting travel grants this year.
The Foundation’s most noteworthy change, and one we hope all of our membership and donors will be a part of, is the launch of our new endowment in 2019/2020. The Erin Popovich Endowment will enable access to resources for patients and families, empower patients to take charge, find support groups, seek second opinions, and more, and will support research to advance patient care and improve treatment options and outcomes. This endowment will change and improve quality of life for patients and families affected by interstitial lung disease, and we encourage you to join us at the Donor Lounge to learn more.
As you embrace the changing of the season and prepare your highlights for CHEST 2019 in NOLA, we invite you to come and discover all the changes and impact the CHEST Foundation is making and why you are so important in all we do!
CHEST 2019 introduces self-study bundles for additional CME/MOC
This year, in conjunction with CHEST Annual Meeting, CHEST is piloting self-study bundles that will allow attendees to earn additional Continuing Medical Education/Continuing Education credits and American Board of Internal Medicine Maintenance of Certification points, apart from the total credits available for the overall meeting. Attendees will receive complimentary access to the eight self-study bundles, in which they will read articles and answer questions related to the articles, in the following areas:
• Pulmonary Hypertension
• Critical Care
• Sleep
• COPD
• Asthma
• Lung Cancer
• Interstitial Lung Disease
• Transplant
This value-added addition will offer the opportunity to earn three credits CME/CE and the corresponding number of ABIM MOC points for each bundle; if someone completes all eight bundles, they can earn up to 24 credits.
The deadline for completion of and claiming CME/CE for the self-study bundles is the same as the claiming deadline for the CHEST Annual Meeting, February 29, 2020.
This year, in conjunction with CHEST Annual Meeting, CHEST is piloting self-study bundles that will allow attendees to earn additional Continuing Medical Education/Continuing Education credits and American Board of Internal Medicine Maintenance of Certification points, apart from the total credits available for the overall meeting. Attendees will receive complimentary access to the eight self-study bundles, in which they will read articles and answer questions related to the articles, in the following areas:
• Pulmonary Hypertension
• Critical Care
• Sleep
• COPD
• Asthma
• Lung Cancer
• Interstitial Lung Disease
• Transplant
This value-added addition will offer the opportunity to earn three credits CME/CE and the corresponding number of ABIM MOC points for each bundle; if someone completes all eight bundles, they can earn up to 24 credits.
The deadline for completion of and claiming CME/CE for the self-study bundles is the same as the claiming deadline for the CHEST Annual Meeting, February 29, 2020.
This year, in conjunction with CHEST Annual Meeting, CHEST is piloting self-study bundles that will allow attendees to earn additional Continuing Medical Education/Continuing Education credits and American Board of Internal Medicine Maintenance of Certification points, apart from the total credits available for the overall meeting. Attendees will receive complimentary access to the eight self-study bundles, in which they will read articles and answer questions related to the articles, in the following areas:
• Pulmonary Hypertension
• Critical Care
• Sleep
• COPD
• Asthma
• Lung Cancer
• Interstitial Lung Disease
• Transplant
This value-added addition will offer the opportunity to earn three credits CME/CE and the corresponding number of ABIM MOC points for each bundle; if someone completes all eight bundles, they can earn up to 24 credits.
The deadline for completion of and claiming CME/CE for the self-study bundles is the same as the claiming deadline for the CHEST Annual Meeting, February 29, 2020.
This month in the journal CHEST®
Editor’s picks
COMMENTARY
Rare Lung Disease Research: National Heart, Lung, and Blood Institute’s Commitment to Partnership and Progress.
By L. J. Vuga, et al
ORIGINAL RESEARCH
Validation of Predictive Metabolic Syndrome Biomarkers of World Trade Center Lung Injury: A 16-Year Longitudinal Study
By S. Kwon, et al.
Association of Short Sleep Duration and Atrial Fibrillation
By M. W. Genuardi, et al.
Determinants of Depressive Symptoms at 1 Year Following ICU Discharge in Survivors of 7 or More Days of Mechanical Ventilation: Results From the RECOVER Program, a Secondary Analysis of a Prospective Multicenter Cohort Study
By M. Hamilton, et al.
TOPICS IN PRACTICE MANAGEMENT
Clinician Strategies to Improve the Care of Patients Using Supplemental Oxygen
By S. S. Jacobs
Editor’s picks
Editor’s picks
COMMENTARY
Rare Lung Disease Research: National Heart, Lung, and Blood Institute’s Commitment to Partnership and Progress.
By L. J. Vuga, et al
ORIGINAL RESEARCH
Validation of Predictive Metabolic Syndrome Biomarkers of World Trade Center Lung Injury: A 16-Year Longitudinal Study
By S. Kwon, et al.
Association of Short Sleep Duration and Atrial Fibrillation
By M. W. Genuardi, et al.
Determinants of Depressive Symptoms at 1 Year Following ICU Discharge in Survivors of 7 or More Days of Mechanical Ventilation: Results From the RECOVER Program, a Secondary Analysis of a Prospective Multicenter Cohort Study
By M. Hamilton, et al.
TOPICS IN PRACTICE MANAGEMENT
Clinician Strategies to Improve the Care of Patients Using Supplemental Oxygen
By S. S. Jacobs
COMMENTARY
Rare Lung Disease Research: National Heart, Lung, and Blood Institute’s Commitment to Partnership and Progress.
By L. J. Vuga, et al
ORIGINAL RESEARCH
Validation of Predictive Metabolic Syndrome Biomarkers of World Trade Center Lung Injury: A 16-Year Longitudinal Study
By S. Kwon, et al.
Association of Short Sleep Duration and Atrial Fibrillation
By M. W. Genuardi, et al.
Determinants of Depressive Symptoms at 1 Year Following ICU Discharge in Survivors of 7 or More Days of Mechanical Ventilation: Results From the RECOVER Program, a Secondary Analysis of a Prospective Multicenter Cohort Study
By M. Hamilton, et al.
TOPICS IN PRACTICE MANAGEMENT
Clinician Strategies to Improve the Care of Patients Using Supplemental Oxygen
By S. S. Jacobs
CHEST Annual Meeting 2019 introduces Wellness Zone with tips and tricks to manage stress
Working as a clinician doesn’t always allow for extra time to focus on the wellness of your body and mind. After taking care of patients all day, it’s important to find the time to also take care of yourself.
This year’s CHEST’s Annual Meeting is introducing a new interactive experience that aims to provide physicians with the necessary tools to decompress from the stressors of work. Visit the CHEST Wellness Zone at CHEST Annual Meeting 2019 to learn easy methods to handle stress and relax after a long day at work.
CHEST 2019 attendees will learn tips and tricks geared toward improving health, and consultants will provide attendees with personalized methods to maintain a healthy lifestyle in the workplace and at home. For those who have yet to register for the annual meeting, this new initiative might change your mind.
At the Wellness Zone, you can relax while getting your feet massaged at one of the four massage machine stations. Clinicians are always on the go, and this station will help to relieve the pressures of being on your feet all day at work.
Essential oils will also be on display for you to smell. Experts will show you the best oil combinations to use in and out of the office.
With a daily strenuous workload, clinicians often forget about their own health, which can lead to poor posture. The Wellness Zone is equipped with consultants who will examine your posture to provide you with feedback to improve your stance. You will walk away after an evaluation with before and after pictures from your consult and a full posture analysis report.
Do you want to try meditation? There is a space dedicated to guiding you through a first-time practice equipped with headphones. You can visit this area to learn about guided meditation apps that make it easy to follow along when meditating at work and home.
The Wellness Zone will feature a variety of 15- to 30-minute sessions focused on providing you with the resources to create a new wellness routine after the annual meeting’s conclusion.
Geared toward improving both one’s physical and mental health, these sessions will dive deeper into maintaining a healthy lifestyle while at work and home. You will walk away from the Wellness Zone with new habits that you are encouraged to incorporate into your daily life to keep your stress levels down to avoid burnout.
The Wellness Zone will be located in the lobby/foyer space inside the New Orleans Ernest N. Morial Convention Center and will be open all day October 20-23, except for during the Opening Sessions. Attendees can visit the Wellness Zone at any time with no appointment necessary.
Visit chestmeeting.chestnet.org for a list of sessions that are offered in the Wellness Zone, including Creating Well-Being in the Workplace and more. Plan your visit now to enjoy all the benefits CHEST 2019 has to offer.
Working as a clinician doesn’t always allow for extra time to focus on the wellness of your body and mind. After taking care of patients all day, it’s important to find the time to also take care of yourself.
This year’s CHEST’s Annual Meeting is introducing a new interactive experience that aims to provide physicians with the necessary tools to decompress from the stressors of work. Visit the CHEST Wellness Zone at CHEST Annual Meeting 2019 to learn easy methods to handle stress and relax after a long day at work.
CHEST 2019 attendees will learn tips and tricks geared toward improving health, and consultants will provide attendees with personalized methods to maintain a healthy lifestyle in the workplace and at home. For those who have yet to register for the annual meeting, this new initiative might change your mind.
At the Wellness Zone, you can relax while getting your feet massaged at one of the four massage machine stations. Clinicians are always on the go, and this station will help to relieve the pressures of being on your feet all day at work.
Essential oils will also be on display for you to smell. Experts will show you the best oil combinations to use in and out of the office.
With a daily strenuous workload, clinicians often forget about their own health, which can lead to poor posture. The Wellness Zone is equipped with consultants who will examine your posture to provide you with feedback to improve your stance. You will walk away after an evaluation with before and after pictures from your consult and a full posture analysis report.
Do you want to try meditation? There is a space dedicated to guiding you through a first-time practice equipped with headphones. You can visit this area to learn about guided meditation apps that make it easy to follow along when meditating at work and home.
The Wellness Zone will feature a variety of 15- to 30-minute sessions focused on providing you with the resources to create a new wellness routine after the annual meeting’s conclusion.
Geared toward improving both one’s physical and mental health, these sessions will dive deeper into maintaining a healthy lifestyle while at work and home. You will walk away from the Wellness Zone with new habits that you are encouraged to incorporate into your daily life to keep your stress levels down to avoid burnout.
The Wellness Zone will be located in the lobby/foyer space inside the New Orleans Ernest N. Morial Convention Center and will be open all day October 20-23, except for during the Opening Sessions. Attendees can visit the Wellness Zone at any time with no appointment necessary.
Visit chestmeeting.chestnet.org for a list of sessions that are offered in the Wellness Zone, including Creating Well-Being in the Workplace and more. Plan your visit now to enjoy all the benefits CHEST 2019 has to offer.
Working as a clinician doesn’t always allow for extra time to focus on the wellness of your body and mind. After taking care of patients all day, it’s important to find the time to also take care of yourself.
This year’s CHEST’s Annual Meeting is introducing a new interactive experience that aims to provide physicians with the necessary tools to decompress from the stressors of work. Visit the CHEST Wellness Zone at CHEST Annual Meeting 2019 to learn easy methods to handle stress and relax after a long day at work.
CHEST 2019 attendees will learn tips and tricks geared toward improving health, and consultants will provide attendees with personalized methods to maintain a healthy lifestyle in the workplace and at home. For those who have yet to register for the annual meeting, this new initiative might change your mind.
At the Wellness Zone, you can relax while getting your feet massaged at one of the four massage machine stations. Clinicians are always on the go, and this station will help to relieve the pressures of being on your feet all day at work.
Essential oils will also be on display for you to smell. Experts will show you the best oil combinations to use in and out of the office.
With a daily strenuous workload, clinicians often forget about their own health, which can lead to poor posture. The Wellness Zone is equipped with consultants who will examine your posture to provide you with feedback to improve your stance. You will walk away after an evaluation with before and after pictures from your consult and a full posture analysis report.
Do you want to try meditation? There is a space dedicated to guiding you through a first-time practice equipped with headphones. You can visit this area to learn about guided meditation apps that make it easy to follow along when meditating at work and home.
The Wellness Zone will feature a variety of 15- to 30-minute sessions focused on providing you with the resources to create a new wellness routine after the annual meeting’s conclusion.
Geared toward improving both one’s physical and mental health, these sessions will dive deeper into maintaining a healthy lifestyle while at work and home. You will walk away from the Wellness Zone with new habits that you are encouraged to incorporate into your daily life to keep your stress levels down to avoid burnout.
The Wellness Zone will be located in the lobby/foyer space inside the New Orleans Ernest N. Morial Convention Center and will be open all day October 20-23, except for during the Opening Sessions. Attendees can visit the Wellness Zone at any time with no appointment necessary.
Visit chestmeeting.chestnet.org for a list of sessions that are offered in the Wellness Zone, including Creating Well-Being in the Workplace and more. Plan your visit now to enjoy all the benefits CHEST 2019 has to offer.
Latent TB testing. High flow nasal cannula. Statins in OSA
Occupational and Environmental Health
New guidelines for latent TB testing in health-care personnel
Latent infection with Mycobacterium tuberculosis (TB) infection is of public health concern because of the lifetime risk of reactivation, a risk highest in the first 2 years after TB infection. Treatment of latent TB infection (LTBI) reduces the risk of reactivation by as much as 90%, and, thus, screening for LTBI in high-risk populations can identify patients eligible for treatment (Horsburgh & Rubin. N Engl J Med. 2011;364[15]:1441). The Centers for Disease Control and Prevention (CDC) previously recommended annual testing for LTBI in health-care personnel (HCP) as a high-risk group for developing LTBI (Jensen et al. MMWR Recomm Rep. 2005;54[No. RR-17]).
The annual national TB rate in the United States has decreased by 73% since 1991 (Stewart et al. MMWR Morb Mortal Wkly Rep. 2018;67[11]:317), and surveillance data show that TB incidence among HCPs does not differ significantly from the general population. The CDC thus formed the National Tuberculosis Controllers Association (NTCA)-CDC work group to revisit the recommendations for LTBI screening in HCPs. A systematic evidence review of all studies of LTBI testing in HCPs since 2005 was performed. Analysis of data from identified studies showed that less than 5% of HCPs converted from baseline negative to positive on routine annual screening.
Based on this, the CDC updated their recommendations from the 2005 guidelines: (1) Serial annual LTBI testing is no longer routinely recommended for all HCPs but may be considered for select HCPs (eg, pulmonologists, infectious disease specialists, respiratory therapists); (2) Treatment is encouraged for all HCPs with positive LTBI testing, unless medically contraindicated; (3) The recommendations for baseline LTBI and postexposure testing in all HCPs remain unchanged (Sosa et al. MMWR Morb Mortal Wkly Rep. 2019;68[19]:439).
Sujith Cherian, MD, FCCP
Steering Committee Member
Amy Ahasic, MD, MPH, FCCP
Chair
Respiratory Care
Aerosol drug delivery via high-flow nasal cannula
As a noninvasive, easy-to-use oxygen device, high-flow nasal cannula (HFNC) meets patients’ inspiratory demands, increases functional residual capacity, and decreases the need for intubation (Rochwerg, et al. Intensive Care Med. 2019;45[5]:563).
Using HFNC for aerosol drug delivery is an innovative approach (Ari, et al. Pediatr Pulmonol. 2011;46[8]:795) and the seven most important things about aerosol delivery via HFNC are listed below for clinicians:
1. Aerosols can be delivered via HFNC in the treatment of patients with respiratory distress through all age groups.
2. Delivery efficiency of mesh nebulizers is greater than jet nebulizers during HFNC. Unlike jet nebulizers, they do not interfere with FiO2 and the function of HFNC by adding extra gas flow to the system.
3. Placing mesh nebulizers before the humidifier improves aerosol delivery via HFNC.
4. Higher inspiratory flow rates with HFNC decreases aerosol delivery due to increased turbulence and impactive loss of aerosols during therapy.
5. While aerosol deposition is greater with the larger prong sizes, its size should not block more than 50% of the cross-sectional area of each nostril to allow gas leakage around the cannula.
6. Although oxygen is commonly used with HFNC, administering aerosolized medications with heliox during HFNC improves lung deposition more than oxygen.
7. Training patients on the closed mouth technique and nasal breathing during therapy may improve aerosol drug delivery via HFNC.
HFNC is a promising tool in aerosol therapy, and developing clinical guidelines on aerosol delivery via HFNC is needed to improve its effectiveness in drug delivery.
Arzu Ari, PhD, RRT
Steering Committee Member
Jessica Overgoner, RRT
NetWork Member
Sleep Medicine
Statins in OSA
Obstructive sleep apnea is linked with cardiovascular disease (CVD) (Wolk R, et al. Circulation. 2003;108[1]:9), and the primary treatment of OSA, ie, continuous positive airway pressure (CPAP), may reverse the adverse CVD sequelae associated with OSA. However, recent randomized controlled trials, including SAVE and RICCADSA, fail to show significant reductions in CVD events with CPAP therapy (McEvoy RD, et al. J Thorac Dis. 2010;2[3]:138; Peker Y, et al. Am J Respir Crit Care Med. 2016;194[5]:613). Although numerous reasons are postulated for these unexpected trial findings, one potential explanation is that individuals in these trials were already on CVD protective drugs. One such drug category is statins. Statins are prescribed for their lipid lowering effects; however, they have pleiotropic properties including reduction in vascular inflammation and oxidative stress. Statins also enhance endothelial function and improve blood pressure. In animal studies, statins prevented the adverse effects of chronic intermittent hypoxemia on systolic blood pressure, endothelial function, and carotid artery compliance. Human studies confirm some of the aforementioned animal study findings. In a study of patients with OSA, statin therapy preserved the anti-inflammatory cell surface proteins that are typically reduced in these patients (Emin M, et al. Sci Transl Med. 2016;8[320]:320ra1). In a randomized controlled trial of patients with OSA, statin therapy significantly improved systolic blood pressure but did not improve reactive hyperemia index, which is a marker of endothelial dysfunction (Joyeux-Faure M, et al. Mediators Inflamm. 2014 Aug 25. doi: 10.1155/2014/423120).
Therefore, the jury is still out regarding the independent impact of statin therapy on CVD risk reduction in patients with OSA. Yet, there is select evidence suggesting there may be a role for statins in patients with OSA to mitigate the CVD risk associated with OSA. It remains unknown whether statins work synergistically with CPAP to further reduce CVD risk.
Neomi Shah, MD
Steering Committee Member
Occupational and Environmental Health
New guidelines for latent TB testing in health-care personnel
Latent infection with Mycobacterium tuberculosis (TB) infection is of public health concern because of the lifetime risk of reactivation, a risk highest in the first 2 years after TB infection. Treatment of latent TB infection (LTBI) reduces the risk of reactivation by as much as 90%, and, thus, screening for LTBI in high-risk populations can identify patients eligible for treatment (Horsburgh & Rubin. N Engl J Med. 2011;364[15]:1441). The Centers for Disease Control and Prevention (CDC) previously recommended annual testing for LTBI in health-care personnel (HCP) as a high-risk group for developing LTBI (Jensen et al. MMWR Recomm Rep. 2005;54[No. RR-17]).
The annual national TB rate in the United States has decreased by 73% since 1991 (Stewart et al. MMWR Morb Mortal Wkly Rep. 2018;67[11]:317), and surveillance data show that TB incidence among HCPs does not differ significantly from the general population. The CDC thus formed the National Tuberculosis Controllers Association (NTCA)-CDC work group to revisit the recommendations for LTBI screening in HCPs. A systematic evidence review of all studies of LTBI testing in HCPs since 2005 was performed. Analysis of data from identified studies showed that less than 5% of HCPs converted from baseline negative to positive on routine annual screening.
Based on this, the CDC updated their recommendations from the 2005 guidelines: (1) Serial annual LTBI testing is no longer routinely recommended for all HCPs but may be considered for select HCPs (eg, pulmonologists, infectious disease specialists, respiratory therapists); (2) Treatment is encouraged for all HCPs with positive LTBI testing, unless medically contraindicated; (3) The recommendations for baseline LTBI and postexposure testing in all HCPs remain unchanged (Sosa et al. MMWR Morb Mortal Wkly Rep. 2019;68[19]:439).
Sujith Cherian, MD, FCCP
Steering Committee Member
Amy Ahasic, MD, MPH, FCCP
Chair
Respiratory Care
Aerosol drug delivery via high-flow nasal cannula
As a noninvasive, easy-to-use oxygen device, high-flow nasal cannula (HFNC) meets patients’ inspiratory demands, increases functional residual capacity, and decreases the need for intubation (Rochwerg, et al. Intensive Care Med. 2019;45[5]:563).
Using HFNC for aerosol drug delivery is an innovative approach (Ari, et al. Pediatr Pulmonol. 2011;46[8]:795) and the seven most important things about aerosol delivery via HFNC are listed below for clinicians:
1. Aerosols can be delivered via HFNC in the treatment of patients with respiratory distress through all age groups.
2. Delivery efficiency of mesh nebulizers is greater than jet nebulizers during HFNC. Unlike jet nebulizers, they do not interfere with FiO2 and the function of HFNC by adding extra gas flow to the system.
3. Placing mesh nebulizers before the humidifier improves aerosol delivery via HFNC.
4. Higher inspiratory flow rates with HFNC decreases aerosol delivery due to increased turbulence and impactive loss of aerosols during therapy.
5. While aerosol deposition is greater with the larger prong sizes, its size should not block more than 50% of the cross-sectional area of each nostril to allow gas leakage around the cannula.
6. Although oxygen is commonly used with HFNC, administering aerosolized medications with heliox during HFNC improves lung deposition more than oxygen.
7. Training patients on the closed mouth technique and nasal breathing during therapy may improve aerosol drug delivery via HFNC.
HFNC is a promising tool in aerosol therapy, and developing clinical guidelines on aerosol delivery via HFNC is needed to improve its effectiveness in drug delivery.
Arzu Ari, PhD, RRT
Steering Committee Member
Jessica Overgoner, RRT
NetWork Member
Sleep Medicine
Statins in OSA
Obstructive sleep apnea is linked with cardiovascular disease (CVD) (Wolk R, et al. Circulation. 2003;108[1]:9), and the primary treatment of OSA, ie, continuous positive airway pressure (CPAP), may reverse the adverse CVD sequelae associated with OSA. However, recent randomized controlled trials, including SAVE and RICCADSA, fail to show significant reductions in CVD events with CPAP therapy (McEvoy RD, et al. J Thorac Dis. 2010;2[3]:138; Peker Y, et al. Am J Respir Crit Care Med. 2016;194[5]:613). Although numerous reasons are postulated for these unexpected trial findings, one potential explanation is that individuals in these trials were already on CVD protective drugs. One such drug category is statins. Statins are prescribed for their lipid lowering effects; however, they have pleiotropic properties including reduction in vascular inflammation and oxidative stress. Statins also enhance endothelial function and improve blood pressure. In animal studies, statins prevented the adverse effects of chronic intermittent hypoxemia on systolic blood pressure, endothelial function, and carotid artery compliance. Human studies confirm some of the aforementioned animal study findings. In a study of patients with OSA, statin therapy preserved the anti-inflammatory cell surface proteins that are typically reduced in these patients (Emin M, et al. Sci Transl Med. 2016;8[320]:320ra1). In a randomized controlled trial of patients with OSA, statin therapy significantly improved systolic blood pressure but did not improve reactive hyperemia index, which is a marker of endothelial dysfunction (Joyeux-Faure M, et al. Mediators Inflamm. 2014 Aug 25. doi: 10.1155/2014/423120).
Therefore, the jury is still out regarding the independent impact of statin therapy on CVD risk reduction in patients with OSA. Yet, there is select evidence suggesting there may be a role for statins in patients with OSA to mitigate the CVD risk associated with OSA. It remains unknown whether statins work synergistically with CPAP to further reduce CVD risk.
Neomi Shah, MD
Steering Committee Member
Occupational and Environmental Health
New guidelines for latent TB testing in health-care personnel
Latent infection with Mycobacterium tuberculosis (TB) infection is of public health concern because of the lifetime risk of reactivation, a risk highest in the first 2 years after TB infection. Treatment of latent TB infection (LTBI) reduces the risk of reactivation by as much as 90%, and, thus, screening for LTBI in high-risk populations can identify patients eligible for treatment (Horsburgh & Rubin. N Engl J Med. 2011;364[15]:1441). The Centers for Disease Control and Prevention (CDC) previously recommended annual testing for LTBI in health-care personnel (HCP) as a high-risk group for developing LTBI (Jensen et al. MMWR Recomm Rep. 2005;54[No. RR-17]).
The annual national TB rate in the United States has decreased by 73% since 1991 (Stewart et al. MMWR Morb Mortal Wkly Rep. 2018;67[11]:317), and surveillance data show that TB incidence among HCPs does not differ significantly from the general population. The CDC thus formed the National Tuberculosis Controllers Association (NTCA)-CDC work group to revisit the recommendations for LTBI screening in HCPs. A systematic evidence review of all studies of LTBI testing in HCPs since 2005 was performed. Analysis of data from identified studies showed that less than 5% of HCPs converted from baseline negative to positive on routine annual screening.
Based on this, the CDC updated their recommendations from the 2005 guidelines: (1) Serial annual LTBI testing is no longer routinely recommended for all HCPs but may be considered for select HCPs (eg, pulmonologists, infectious disease specialists, respiratory therapists); (2) Treatment is encouraged for all HCPs with positive LTBI testing, unless medically contraindicated; (3) The recommendations for baseline LTBI and postexposure testing in all HCPs remain unchanged (Sosa et al. MMWR Morb Mortal Wkly Rep. 2019;68[19]:439).
Sujith Cherian, MD, FCCP
Steering Committee Member
Amy Ahasic, MD, MPH, FCCP
Chair
Respiratory Care
Aerosol drug delivery via high-flow nasal cannula
As a noninvasive, easy-to-use oxygen device, high-flow nasal cannula (HFNC) meets patients’ inspiratory demands, increases functional residual capacity, and decreases the need for intubation (Rochwerg, et al. Intensive Care Med. 2019;45[5]:563).
Using HFNC for aerosol drug delivery is an innovative approach (Ari, et al. Pediatr Pulmonol. 2011;46[8]:795) and the seven most important things about aerosol delivery via HFNC are listed below for clinicians:
1. Aerosols can be delivered via HFNC in the treatment of patients with respiratory distress through all age groups.
2. Delivery efficiency of mesh nebulizers is greater than jet nebulizers during HFNC. Unlike jet nebulizers, they do not interfere with FiO2 and the function of HFNC by adding extra gas flow to the system.
3. Placing mesh nebulizers before the humidifier improves aerosol delivery via HFNC.
4. Higher inspiratory flow rates with HFNC decreases aerosol delivery due to increased turbulence and impactive loss of aerosols during therapy.
5. While aerosol deposition is greater with the larger prong sizes, its size should not block more than 50% of the cross-sectional area of each nostril to allow gas leakage around the cannula.
6. Although oxygen is commonly used with HFNC, administering aerosolized medications with heliox during HFNC improves lung deposition more than oxygen.
7. Training patients on the closed mouth technique and nasal breathing during therapy may improve aerosol drug delivery via HFNC.
HFNC is a promising tool in aerosol therapy, and developing clinical guidelines on aerosol delivery via HFNC is needed to improve its effectiveness in drug delivery.
Arzu Ari, PhD, RRT
Steering Committee Member
Jessica Overgoner, RRT
NetWork Member
Sleep Medicine
Statins in OSA
Obstructive sleep apnea is linked with cardiovascular disease (CVD) (Wolk R, et al. Circulation. 2003;108[1]:9), and the primary treatment of OSA, ie, continuous positive airway pressure (CPAP), may reverse the adverse CVD sequelae associated with OSA. However, recent randomized controlled trials, including SAVE and RICCADSA, fail to show significant reductions in CVD events with CPAP therapy (McEvoy RD, et al. J Thorac Dis. 2010;2[3]:138; Peker Y, et al. Am J Respir Crit Care Med. 2016;194[5]:613). Although numerous reasons are postulated for these unexpected trial findings, one potential explanation is that individuals in these trials were already on CVD protective drugs. One such drug category is statins. Statins are prescribed for their lipid lowering effects; however, they have pleiotropic properties including reduction in vascular inflammation and oxidative stress. Statins also enhance endothelial function and improve blood pressure. In animal studies, statins prevented the adverse effects of chronic intermittent hypoxemia on systolic blood pressure, endothelial function, and carotid artery compliance. Human studies confirm some of the aforementioned animal study findings. In a study of patients with OSA, statin therapy preserved the anti-inflammatory cell surface proteins that are typically reduced in these patients (Emin M, et al. Sci Transl Med. 2016;8[320]:320ra1). In a randomized controlled trial of patients with OSA, statin therapy significantly improved systolic blood pressure but did not improve reactive hyperemia index, which is a marker of endothelial dysfunction (Joyeux-Faure M, et al. Mediators Inflamm. 2014 Aug 25. doi: 10.1155/2014/423120).
Therefore, the jury is still out regarding the independent impact of statin therapy on CVD risk reduction in patients with OSA. Yet, there is select evidence suggesting there may be a role for statins in patients with OSA to mitigate the CVD risk associated with OSA. It remains unknown whether statins work synergistically with CPAP to further reduce CVD risk.
Neomi Shah, MD
Steering Committee Member
Getting to know our incoming CHEST President
Stephanie M. Levine, MD, FCCP, is an expert in lung transplantation, and pulmonary and critical care issues in pregnancy and women’s lung health. She is a Professor of Medicine in the Division of Pulmonary Diseases and Critical Care Medicine at the University of Texas Health Science Center in San Antonio, Texas; the Program Director of the Pulmonary and Critical Care Fellowship at the University of Texas Health Science Center; and the Co-Director of the Medical Intensive Care Unit at the University Hospital. She is also a staff physician at the Audie Murphy Veteran Administration Hospital.
Dr. Levine has been Editor for both CHEST SEEK Critical Care Medicine and Pulmonary Medicine editions. In 2009 she received the CHEST Presidential Citation Award; in 2010, the CHEST Distinguished Service Award; and in 2017, the Master Clinician Educator Award. She has also been recognized as a Distinguished CHEST Educator in 2017, 2018, and 2019.
Dr. Levine has been active in CHEST international activities with CHEST World Congress meetings, the 2017 Basel Joint CHEST/SPG Congress in collaboration with the Swiss Lung Association, and with the pulmonary/critical care subspecialty training programs being developed in China. She was President and Chair of the CHEST Foundation from 2010-2014 and is currently on the CHEST Board of Regents.
We asked Dr. Levine for some thoughts on her upcoming CHEST presidency.
What would you like to accomplish as President of CHEST?
Every 5 years, the Board of Regents sets forth a new 5-year strategic plan, which is re-evaluated annually. We try to make sure all our decisions and actions align with this strategic plan. As President, I will promote the vision and mission of CHEST while guiding our organization to succeed in our 2018-2022 strategic plan. What will this include? This will include developing new innovative, evidenced-based, education and educational products in the areas of pulmonary, critical care, and sleep medicine; producing evidence-based guidelines; and expanding our educational expertise both nationally and globally. I am committed to actively engage and retain our fellows-in-training (being a longstanding program director), and to mentor our future leaders. I will reach out to engage and educate advanced practice providers, who are an integral part of our patient care teams. We will grow the CHEST Foundation in the areas of patient education and access, clinical research funding, and community service. On the global front, we will continue with our new global strategy of holding congresses based on the annual meeting content and smaller board review format regional conferences in different parts of the world seeking education in pulmonary, critical care, and sleep medicine. Our next meeting is in Bologna, Italy, in June of 2020. I will build on our collaborative inter-societal relationships with our related societies. Some of the specific areas I plan to focus on are defining the true value of CHEST membership, engaging all members of the health-care team, and revisiting the structure and function of our NetWorks to ensure the maximum opportunities for leadership and engagement.
What do you consider to be the greatest strength of CHEST, and how will you build upon this during your Presidency?
Our greatest strengths are the education we deliver; the people at all levels who deliver, learn from, and support the delivery of this core component of our vision and mission; and the culture in which this all takes place. These people include leaders, volunteers, faculty, members and all clinicians on the health-care team, and our top-notch staff (our EVP/CEO, Executive and Operations Team and staff at all levels). To build upon this, we need to strive for continued educational innovation and relevance and creative delivery of our educational products.
What are some challenges facing CHEST, and how will you address these challenges?
Ironically, maintaining our greatest strengths in the setting of a changing health-care environment can also be one of the greatest challenges. We must continue to make our education vibrant, relevant, and experiential. To do this, we need to ensure innovative, year-round education, whether at the annual meeting or through our e-learning platforms, simulation activities, SEEK, state-of the-art guidelines, board review courses, and courses and meetings at CHEST Global Headquarters in Glenview, Illinois, or at a global destination. We also need to stay relevant from the point of view of the value of membership and engagement. We must be cognizant of what members and others who engage with CHEST are looking for and ensure that we are meeting those ongoing expectations. Also, the need to identify, attract, develop, and retain talented and diverse members, volunteers, faculty, and future leaders and staff is imperative. As a program director, I am particularly interested in the retention of our fellows-in-training.
And finally, what is your charge to the members and new Fellows (FCCPs) of CHEST?
Get involved and stay involved. There are so many opportunities to do this! Attend the CHEST Annual Meeting. Join a NetWork. Submit articles to the journal CHEST or abstracts and case reports to the meeting. Participate in a Board Review Course or one of our e-learning opportunities. Come to a live course at headquarters or at a global destination. Participate in a simulation experience. Network at a meeting or a course. Engage with the CHEST Foundation. Connect with us on social media. Sign up to be a moderator and/or grader at the CHEST Annual Meeting. Become an FCCP. Apply for leadership openings, and if you don’t get it the first time, try again! You will be impressed with all that CHEST has to offer!!
Stephanie M. Levine, MD, FCCP, is an expert in lung transplantation, and pulmonary and critical care issues in pregnancy and women’s lung health. She is a Professor of Medicine in the Division of Pulmonary Diseases and Critical Care Medicine at the University of Texas Health Science Center in San Antonio, Texas; the Program Director of the Pulmonary and Critical Care Fellowship at the University of Texas Health Science Center; and the Co-Director of the Medical Intensive Care Unit at the University Hospital. She is also a staff physician at the Audie Murphy Veteran Administration Hospital.
Dr. Levine has been Editor for both CHEST SEEK Critical Care Medicine and Pulmonary Medicine editions. In 2009 she received the CHEST Presidential Citation Award; in 2010, the CHEST Distinguished Service Award; and in 2017, the Master Clinician Educator Award. She has also been recognized as a Distinguished CHEST Educator in 2017, 2018, and 2019.
Dr. Levine has been active in CHEST international activities with CHEST World Congress meetings, the 2017 Basel Joint CHEST/SPG Congress in collaboration with the Swiss Lung Association, and with the pulmonary/critical care subspecialty training programs being developed in China. She was President and Chair of the CHEST Foundation from 2010-2014 and is currently on the CHEST Board of Regents.
We asked Dr. Levine for some thoughts on her upcoming CHEST presidency.
What would you like to accomplish as President of CHEST?
Every 5 years, the Board of Regents sets forth a new 5-year strategic plan, which is re-evaluated annually. We try to make sure all our decisions and actions align with this strategic plan. As President, I will promote the vision and mission of CHEST while guiding our organization to succeed in our 2018-2022 strategic plan. What will this include? This will include developing new innovative, evidenced-based, education and educational products in the areas of pulmonary, critical care, and sleep medicine; producing evidence-based guidelines; and expanding our educational expertise both nationally and globally. I am committed to actively engage and retain our fellows-in-training (being a longstanding program director), and to mentor our future leaders. I will reach out to engage and educate advanced practice providers, who are an integral part of our patient care teams. We will grow the CHEST Foundation in the areas of patient education and access, clinical research funding, and community service. On the global front, we will continue with our new global strategy of holding congresses based on the annual meeting content and smaller board review format regional conferences in different parts of the world seeking education in pulmonary, critical care, and sleep medicine. Our next meeting is in Bologna, Italy, in June of 2020. I will build on our collaborative inter-societal relationships with our related societies. Some of the specific areas I plan to focus on are defining the true value of CHEST membership, engaging all members of the health-care team, and revisiting the structure and function of our NetWorks to ensure the maximum opportunities for leadership and engagement.
What do you consider to be the greatest strength of CHEST, and how will you build upon this during your Presidency?
Our greatest strengths are the education we deliver; the people at all levels who deliver, learn from, and support the delivery of this core component of our vision and mission; and the culture in which this all takes place. These people include leaders, volunteers, faculty, members and all clinicians on the health-care team, and our top-notch staff (our EVP/CEO, Executive and Operations Team and staff at all levels). To build upon this, we need to strive for continued educational innovation and relevance and creative delivery of our educational products.
What are some challenges facing CHEST, and how will you address these challenges?
Ironically, maintaining our greatest strengths in the setting of a changing health-care environment can also be one of the greatest challenges. We must continue to make our education vibrant, relevant, and experiential. To do this, we need to ensure innovative, year-round education, whether at the annual meeting or through our e-learning platforms, simulation activities, SEEK, state-of the-art guidelines, board review courses, and courses and meetings at CHEST Global Headquarters in Glenview, Illinois, or at a global destination. We also need to stay relevant from the point of view of the value of membership and engagement. We must be cognizant of what members and others who engage with CHEST are looking for and ensure that we are meeting those ongoing expectations. Also, the need to identify, attract, develop, and retain talented and diverse members, volunteers, faculty, and future leaders and staff is imperative. As a program director, I am particularly interested in the retention of our fellows-in-training.
And finally, what is your charge to the members and new Fellows (FCCPs) of CHEST?
Get involved and stay involved. There are so many opportunities to do this! Attend the CHEST Annual Meeting. Join a NetWork. Submit articles to the journal CHEST or abstracts and case reports to the meeting. Participate in a Board Review Course or one of our e-learning opportunities. Come to a live course at headquarters or at a global destination. Participate in a simulation experience. Network at a meeting or a course. Engage with the CHEST Foundation. Connect with us on social media. Sign up to be a moderator and/or grader at the CHEST Annual Meeting. Become an FCCP. Apply for leadership openings, and if you don’t get it the first time, try again! You will be impressed with all that CHEST has to offer!!
Stephanie M. Levine, MD, FCCP, is an expert in lung transplantation, and pulmonary and critical care issues in pregnancy and women’s lung health. She is a Professor of Medicine in the Division of Pulmonary Diseases and Critical Care Medicine at the University of Texas Health Science Center in San Antonio, Texas; the Program Director of the Pulmonary and Critical Care Fellowship at the University of Texas Health Science Center; and the Co-Director of the Medical Intensive Care Unit at the University Hospital. She is also a staff physician at the Audie Murphy Veteran Administration Hospital.
Dr. Levine has been Editor for both CHEST SEEK Critical Care Medicine and Pulmonary Medicine editions. In 2009 she received the CHEST Presidential Citation Award; in 2010, the CHEST Distinguished Service Award; and in 2017, the Master Clinician Educator Award. She has also been recognized as a Distinguished CHEST Educator in 2017, 2018, and 2019.
Dr. Levine has been active in CHEST international activities with CHEST World Congress meetings, the 2017 Basel Joint CHEST/SPG Congress in collaboration with the Swiss Lung Association, and with the pulmonary/critical care subspecialty training programs being developed in China. She was President and Chair of the CHEST Foundation from 2010-2014 and is currently on the CHEST Board of Regents.
We asked Dr. Levine for some thoughts on her upcoming CHEST presidency.
What would you like to accomplish as President of CHEST?
Every 5 years, the Board of Regents sets forth a new 5-year strategic plan, which is re-evaluated annually. We try to make sure all our decisions and actions align with this strategic plan. As President, I will promote the vision and mission of CHEST while guiding our organization to succeed in our 2018-2022 strategic plan. What will this include? This will include developing new innovative, evidenced-based, education and educational products in the areas of pulmonary, critical care, and sleep medicine; producing evidence-based guidelines; and expanding our educational expertise both nationally and globally. I am committed to actively engage and retain our fellows-in-training (being a longstanding program director), and to mentor our future leaders. I will reach out to engage and educate advanced practice providers, who are an integral part of our patient care teams. We will grow the CHEST Foundation in the areas of patient education and access, clinical research funding, and community service. On the global front, we will continue with our new global strategy of holding congresses based on the annual meeting content and smaller board review format regional conferences in different parts of the world seeking education in pulmonary, critical care, and sleep medicine. Our next meeting is in Bologna, Italy, in June of 2020. I will build on our collaborative inter-societal relationships with our related societies. Some of the specific areas I plan to focus on are defining the true value of CHEST membership, engaging all members of the health-care team, and revisiting the structure and function of our NetWorks to ensure the maximum opportunities for leadership and engagement.
What do you consider to be the greatest strength of CHEST, and how will you build upon this during your Presidency?
Our greatest strengths are the education we deliver; the people at all levels who deliver, learn from, and support the delivery of this core component of our vision and mission; and the culture in which this all takes place. These people include leaders, volunteers, faculty, members and all clinicians on the health-care team, and our top-notch staff (our EVP/CEO, Executive and Operations Team and staff at all levels). To build upon this, we need to strive for continued educational innovation and relevance and creative delivery of our educational products.
What are some challenges facing CHEST, and how will you address these challenges?
Ironically, maintaining our greatest strengths in the setting of a changing health-care environment can also be one of the greatest challenges. We must continue to make our education vibrant, relevant, and experiential. To do this, we need to ensure innovative, year-round education, whether at the annual meeting or through our e-learning platforms, simulation activities, SEEK, state-of the-art guidelines, board review courses, and courses and meetings at CHEST Global Headquarters in Glenview, Illinois, or at a global destination. We also need to stay relevant from the point of view of the value of membership and engagement. We must be cognizant of what members and others who engage with CHEST are looking for and ensure that we are meeting those ongoing expectations. Also, the need to identify, attract, develop, and retain talented and diverse members, volunteers, faculty, and future leaders and staff is imperative. As a program director, I am particularly interested in the retention of our fellows-in-training.
And finally, what is your charge to the members and new Fellows (FCCPs) of CHEST?
Get involved and stay involved. There are so many opportunities to do this! Attend the CHEST Annual Meeting. Join a NetWork. Submit articles to the journal CHEST or abstracts and case reports to the meeting. Participate in a Board Review Course or one of our e-learning opportunities. Come to a live course at headquarters or at a global destination. Participate in a simulation experience. Network at a meeting or a course. Engage with the CHEST Foundation. Connect with us on social media. Sign up to be a moderator and/or grader at the CHEST Annual Meeting. Become an FCCP. Apply for leadership openings, and if you don’t get it the first time, try again! You will be impressed with all that CHEST has to offer!!
Broad cross section of clinical topics highlights NAMDRC 2020 Conference
NAMDRC will host its Annual Educational Conference at the Scottsdale Resort at McCormick Ranch in Scottsdale, Arizona, March 12-14, 2020, and features a wide cross section of clinical, management, and health policy issues.
The NAMDRC Educational Conference is unlike other medical conferences you have attended. Conference sessions begin early each day and conclude by 12:30 so attendees, spouses, and guests can enjoy the venue, this year in Scottsdale, Arizona. All registrants and their guests enjoy numerous complimentary meals, and speakers and corporate partners invariably linger with the attendees during receptions for those more casual opportunities for conversations and less formal Q&A.
The Program Committee has announced its plans to focus the first day of the 3-day event on lung cancer, severe asthma, and pulmonary hypertension. Speakers include Maxwell Smith, MD from the Mayo Clinic, Arizona; James Herman, MD, Co-Director of the Lung Cancer Program at UPMC, and Colleen Channick, MD, FCCP, Director of Interventional Pulmonary at UCLA Medical Center to address timely updates on lung cancer diagnosis and treatment. The morning sessions also include a presentation on severe asthma by Monica Kraft, MD, FCCP, University of Arizona; and Richard Channick, MD, Geffen School of Medicine, UCLA, examining pulmonary hypertension with a concentration on current approaches to diagnosis and treatment.
On Friday, March 13, the focus shifts from the clinical to the changing landscape in the delivery of medicine, with a concentrated focus on innovation and new tools available to guide physicians in treatment of their patients. Claibe Yarbrough, MD, National Program Director of Pulmonary, Critical Care and Sleep at the VA, University of Texas, will examine the growth of telemedicine in the ICU. Steve Peters, MD, FCCP, a past President of NAMDRC and a current Board member, will look at artificial intelligence and the future of medicine. Dr. Peters will also present a practice management update in partnership with Alan Plummer, MD, FCCP, as he addresses coding changes in the practice of pulmonary, critical care, and sleep medicine effective 2020-21.
Shifting back to a clinical focus, the Walter J. O’Donohue memorial lecture will be given by Gerald Criner, MD, FCCP, Temple University, to examine endobronchial valve therapy for emphysema. Rounding out the presentations will be luncheon speaker Susan Tanski, MD, looking at electronic nicotine delivery systems.
On Saturday, the topics turn to sleep and mechanical ventilation. Insomnia is the subject matter for Jennifer Martin, MD, Geffen School of Medicine at UCLA; Sairam Parthasarathy, MD, at the University of Arizona, will address sleep and noninvasive mechanical ventilation. And, in a corollary presentation, home mechanical ventilation is the topic for John Hansen-Flaschen, MD, FCCP, Hospital of the University of Pennsylvania.
The final morning rounds out with controversies in septic shock, Rodrigo Cartin-Ceba, MD, at the Mayo Clinic in Scottsdale, and palliative care in the ICU, Mark Edwin, also from the Mayo Clinic.
For more information about membership in NAMDRC and conference information, visit its website at www.namdrc.org.
NAMDRC will host its Annual Educational Conference at the Scottsdale Resort at McCormick Ranch in Scottsdale, Arizona, March 12-14, 2020, and features a wide cross section of clinical, management, and health policy issues.
The NAMDRC Educational Conference is unlike other medical conferences you have attended. Conference sessions begin early each day and conclude by 12:30 so attendees, spouses, and guests can enjoy the venue, this year in Scottsdale, Arizona. All registrants and their guests enjoy numerous complimentary meals, and speakers and corporate partners invariably linger with the attendees during receptions for those more casual opportunities for conversations and less formal Q&A.
The Program Committee has announced its plans to focus the first day of the 3-day event on lung cancer, severe asthma, and pulmonary hypertension. Speakers include Maxwell Smith, MD from the Mayo Clinic, Arizona; James Herman, MD, Co-Director of the Lung Cancer Program at UPMC, and Colleen Channick, MD, FCCP, Director of Interventional Pulmonary at UCLA Medical Center to address timely updates on lung cancer diagnosis and treatment. The morning sessions also include a presentation on severe asthma by Monica Kraft, MD, FCCP, University of Arizona; and Richard Channick, MD, Geffen School of Medicine, UCLA, examining pulmonary hypertension with a concentration on current approaches to diagnosis and treatment.
On Friday, March 13, the focus shifts from the clinical to the changing landscape in the delivery of medicine, with a concentrated focus on innovation and new tools available to guide physicians in treatment of their patients. Claibe Yarbrough, MD, National Program Director of Pulmonary, Critical Care and Sleep at the VA, University of Texas, will examine the growth of telemedicine in the ICU. Steve Peters, MD, FCCP, a past President of NAMDRC and a current Board member, will look at artificial intelligence and the future of medicine. Dr. Peters will also present a practice management update in partnership with Alan Plummer, MD, FCCP, as he addresses coding changes in the practice of pulmonary, critical care, and sleep medicine effective 2020-21.
Shifting back to a clinical focus, the Walter J. O’Donohue memorial lecture will be given by Gerald Criner, MD, FCCP, Temple University, to examine endobronchial valve therapy for emphysema. Rounding out the presentations will be luncheon speaker Susan Tanski, MD, looking at electronic nicotine delivery systems.
On Saturday, the topics turn to sleep and mechanical ventilation. Insomnia is the subject matter for Jennifer Martin, MD, Geffen School of Medicine at UCLA; Sairam Parthasarathy, MD, at the University of Arizona, will address sleep and noninvasive mechanical ventilation. And, in a corollary presentation, home mechanical ventilation is the topic for John Hansen-Flaschen, MD, FCCP, Hospital of the University of Pennsylvania.
The final morning rounds out with controversies in septic shock, Rodrigo Cartin-Ceba, MD, at the Mayo Clinic in Scottsdale, and palliative care in the ICU, Mark Edwin, also from the Mayo Clinic.
For more information about membership in NAMDRC and conference information, visit its website at www.namdrc.org.
NAMDRC will host its Annual Educational Conference at the Scottsdale Resort at McCormick Ranch in Scottsdale, Arizona, March 12-14, 2020, and features a wide cross section of clinical, management, and health policy issues.
The NAMDRC Educational Conference is unlike other medical conferences you have attended. Conference sessions begin early each day and conclude by 12:30 so attendees, spouses, and guests can enjoy the venue, this year in Scottsdale, Arizona. All registrants and their guests enjoy numerous complimentary meals, and speakers and corporate partners invariably linger with the attendees during receptions for those more casual opportunities for conversations and less formal Q&A.
The Program Committee has announced its plans to focus the first day of the 3-day event on lung cancer, severe asthma, and pulmonary hypertension. Speakers include Maxwell Smith, MD from the Mayo Clinic, Arizona; James Herman, MD, Co-Director of the Lung Cancer Program at UPMC, and Colleen Channick, MD, FCCP, Director of Interventional Pulmonary at UCLA Medical Center to address timely updates on lung cancer diagnosis and treatment. The morning sessions also include a presentation on severe asthma by Monica Kraft, MD, FCCP, University of Arizona; and Richard Channick, MD, Geffen School of Medicine, UCLA, examining pulmonary hypertension with a concentration on current approaches to diagnosis and treatment.
On Friday, March 13, the focus shifts from the clinical to the changing landscape in the delivery of medicine, with a concentrated focus on innovation and new tools available to guide physicians in treatment of their patients. Claibe Yarbrough, MD, National Program Director of Pulmonary, Critical Care and Sleep at the VA, University of Texas, will examine the growth of telemedicine in the ICU. Steve Peters, MD, FCCP, a past President of NAMDRC and a current Board member, will look at artificial intelligence and the future of medicine. Dr. Peters will also present a practice management update in partnership with Alan Plummer, MD, FCCP, as he addresses coding changes in the practice of pulmonary, critical care, and sleep medicine effective 2020-21.
Shifting back to a clinical focus, the Walter J. O’Donohue memorial lecture will be given by Gerald Criner, MD, FCCP, Temple University, to examine endobronchial valve therapy for emphysema. Rounding out the presentations will be luncheon speaker Susan Tanski, MD, looking at electronic nicotine delivery systems.
On Saturday, the topics turn to sleep and mechanical ventilation. Insomnia is the subject matter for Jennifer Martin, MD, Geffen School of Medicine at UCLA; Sairam Parthasarathy, MD, at the University of Arizona, will address sleep and noninvasive mechanical ventilation. And, in a corollary presentation, home mechanical ventilation is the topic for John Hansen-Flaschen, MD, FCCP, Hospital of the University of Pennsylvania.
The final morning rounds out with controversies in septic shock, Rodrigo Cartin-Ceba, MD, at the Mayo Clinic in Scottsdale, and palliative care in the ICU, Mark Edwin, also from the Mayo Clinic.
For more information about membership in NAMDRC and conference information, visit its website at www.namdrc.org.
17 fellows advancing GI and patient care
These fellows showcased their commitment to advancing our field through their quality improvement projects presented at DDW® 2019.
Each year during Digestive Disease Week®, AGA hosts a session titled “Advancing Clinical Practice: GI Fellow-Directed Quality-Improvement Projects.” During the 2019 session, 17 quality improvement initiatives were presented — you can review these abstracts in the July issue of Gastroenterology in the “AGA Section,” www.gastrojournal.org/issue/S0016-5085(19)X0009-8. Kudos to the promising fellows featured below, who all served as lead authors for their QI projects.
Manasi Agrawal, MD
Lenox Hill Hospital, New York City
@ManasiAgrawalMD
Jessica Breton, MD
Children’s Hospital of Philadelphia
Adam Faye, MD
Columbia University Medical Center, New York City
@AdamFaye4
Shelly Gurwara, MD
Wake Forest Baptist Health Medical Center, Winston-Salem, N.C.
Afrin Kamal, MD
Stanford University, Calif.
Ani Kardashian, MD
University of California, Los Angeles
@AniKardashianMD
Sonali Palchaudhuri, MD
University of Pennsylvania, Philadelphia
@sopalchaudhuri
Nasim Parsa, MD
University of Missouri Health System, Columbia
Sahil Patel, MD
Drexel University, Philadelphia
@sahilr
Vikram Raghu, MD
Children’s Hospital of Pittsburgh, Pennsylvania
Amit Shah, MD
Children’s Hospital of Philadelphia
Lin Shen, MD
Brigham and Women’s Hospital, Boston
@LinShenMD
Charles Snyder, MD
Icahn School of Medicine at Mount Sinai, New York City
Brian Sullivan, MD
Duke University, Durham, N.C.
Ashley Vachon, MD
University of Colorado Anschutz Medical Campus, Aurora
Ted Walker, MD
Washington University/Barnes Jewish Hospital, St. Louis, Mo.
Xiao Jing Wang, MD
Mayo Clinic, Rochester, Minn.
@IrisWangMD
These fellows showcased their commitment to advancing our field through their quality improvement projects presented at DDW® 2019.
Each year during Digestive Disease Week®, AGA hosts a session titled “Advancing Clinical Practice: GI Fellow-Directed Quality-Improvement Projects.” During the 2019 session, 17 quality improvement initiatives were presented — you can review these abstracts in the July issue of Gastroenterology in the “AGA Section,” www.gastrojournal.org/issue/S0016-5085(19)X0009-8. Kudos to the promising fellows featured below, who all served as lead authors for their QI projects.
Manasi Agrawal, MD
Lenox Hill Hospital, New York City
@ManasiAgrawalMD
Jessica Breton, MD
Children’s Hospital of Philadelphia
Adam Faye, MD
Columbia University Medical Center, New York City
@AdamFaye4
Shelly Gurwara, MD
Wake Forest Baptist Health Medical Center, Winston-Salem, N.C.
Afrin Kamal, MD
Stanford University, Calif.
Ani Kardashian, MD
University of California, Los Angeles
@AniKardashianMD
Sonali Palchaudhuri, MD
University of Pennsylvania, Philadelphia
@sopalchaudhuri
Nasim Parsa, MD
University of Missouri Health System, Columbia
Sahil Patel, MD
Drexel University, Philadelphia
@sahilr
Vikram Raghu, MD
Children’s Hospital of Pittsburgh, Pennsylvania
Amit Shah, MD
Children’s Hospital of Philadelphia
Lin Shen, MD
Brigham and Women’s Hospital, Boston
@LinShenMD
Charles Snyder, MD
Icahn School of Medicine at Mount Sinai, New York City
Brian Sullivan, MD
Duke University, Durham, N.C.
Ashley Vachon, MD
University of Colorado Anschutz Medical Campus, Aurora
Ted Walker, MD
Washington University/Barnes Jewish Hospital, St. Louis, Mo.
Xiao Jing Wang, MD
Mayo Clinic, Rochester, Minn.
@IrisWangMD
These fellows showcased their commitment to advancing our field through their quality improvement projects presented at DDW® 2019.
Each year during Digestive Disease Week®, AGA hosts a session titled “Advancing Clinical Practice: GI Fellow-Directed Quality-Improvement Projects.” During the 2019 session, 17 quality improvement initiatives were presented — you can review these abstracts in the July issue of Gastroenterology in the “AGA Section,” www.gastrojournal.org/issue/S0016-5085(19)X0009-8. Kudos to the promising fellows featured below, who all served as lead authors for their QI projects.
Manasi Agrawal, MD
Lenox Hill Hospital, New York City
@ManasiAgrawalMD
Jessica Breton, MD
Children’s Hospital of Philadelphia
Adam Faye, MD
Columbia University Medical Center, New York City
@AdamFaye4
Shelly Gurwara, MD
Wake Forest Baptist Health Medical Center, Winston-Salem, N.C.
Afrin Kamal, MD
Stanford University, Calif.
Ani Kardashian, MD
University of California, Los Angeles
@AniKardashianMD
Sonali Palchaudhuri, MD
University of Pennsylvania, Philadelphia
@sopalchaudhuri
Nasim Parsa, MD
University of Missouri Health System, Columbia
Sahil Patel, MD
Drexel University, Philadelphia
@sahilr
Vikram Raghu, MD
Children’s Hospital of Pittsburgh, Pennsylvania
Amit Shah, MD
Children’s Hospital of Philadelphia
Lin Shen, MD
Brigham and Women’s Hospital, Boston
@LinShenMD
Charles Snyder, MD
Icahn School of Medicine at Mount Sinai, New York City
Brian Sullivan, MD
Duke University, Durham, N.C.
Ashley Vachon, MD
University of Colorado Anschutz Medical Campus, Aurora
Ted Walker, MD
Washington University/Barnes Jewish Hospital, St. Louis, Mo.
Xiao Jing Wang, MD
Mayo Clinic, Rochester, Minn.
@IrisWangMD