User login
This month in the journal CHEST®
Editor’s picks
ORIGINAL RESEARCH
The Saint Georges Respiratory Questionnaire definition of chronic bronchitis may be a better predictor of COPD exacerbations compared to the classic definition. By Dr. V. Kim, et al.
Confocal laser endomicroscopy (CLE) as a guidance tool for pleural biopsies in malignant pleural mesothelioma. By Dr. L. Wijmans, et al.
Association of Angiotensin Modulators With the Course of Idiopathic Pulmonary Fibrosis. By Dr. M. Kreuter, et al.
Age-Stratified National Trends in Pulmonary Embolism Admissions. By Dr. E. D. Pauley, et al.
COMMENTARY
Solving the Opioid Crisis: Respiratory Depression by Opioids as Critical Endpoint.By Dr. G. Montandon and Dr. A. S. Slutsky.
Editor’s picks
Editor’s picks
ORIGINAL RESEARCH
The Saint Georges Respiratory Questionnaire definition of chronic bronchitis may be a better predictor of COPD exacerbations compared to the classic definition. By Dr. V. Kim, et al.
Confocal laser endomicroscopy (CLE) as a guidance tool for pleural biopsies in malignant pleural mesothelioma. By Dr. L. Wijmans, et al.
Association of Angiotensin Modulators With the Course of Idiopathic Pulmonary Fibrosis. By Dr. M. Kreuter, et al.
Age-Stratified National Trends in Pulmonary Embolism Admissions. By Dr. E. D. Pauley, et al.
COMMENTARY
Solving the Opioid Crisis: Respiratory Depression by Opioids as Critical Endpoint.By Dr. G. Montandon and Dr. A. S. Slutsky.
ORIGINAL RESEARCH
The Saint Georges Respiratory Questionnaire definition of chronic bronchitis may be a better predictor of COPD exacerbations compared to the classic definition. By Dr. V. Kim, et al.
Confocal laser endomicroscopy (CLE) as a guidance tool for pleural biopsies in malignant pleural mesothelioma. By Dr. L. Wijmans, et al.
Association of Angiotensin Modulators With the Course of Idiopathic Pulmonary Fibrosis. By Dr. M. Kreuter, et al.
Age-Stratified National Trends in Pulmonary Embolism Admissions. By Dr. E. D. Pauley, et al.
COMMENTARY
Solving the Opioid Crisis: Respiratory Depression by Opioids as Critical Endpoint.By Dr. G. Montandon and Dr. A. S. Slutsky.
E-cigarette-associated respiratory diseases: Ask your patients about vaping substances via e-cigarettes
E-cigarettes arrived in the U.S. market between 2005 and 2007. Vaping via e-cigarettes involves inhaling substances such as nicotine, flavorings, chemicals, and, sometimes, marijuana and/or other substances deep into the lungs. While the use of these devices is prevalent, the long-term effects are not known. We, as clinicians, need to specifically ask our patients about their use of substances via e-cigarettes because of alarming cases of severe, life-threatening respiratory illnesses recently being reported throughout the United States in young, otherwise healthy, individuals.
As of September 11, 2019, over 380 cases have been reported to the Centers for Disease Control and Prevention (CDC), where young, healthy people from 33 states and one US territory were hospitalized with severe respiratory disease. There have been at least six confirmed deaths and approximately one-third of those who survived required aggressive support with intubation and mechanical ventilation. The number of reported cases is rapidly rising (from 215 possible cases on August 27, 2019). The common theme in these cases is that every patient reported using an e-cigarette product within 90 days of the onset of symptoms, and most within the prior 2 weeks. By definition, other etiologies of respiratory failure, such as infections, collagen vascular, immunologic diseases, and malignancies were excluded.
Between 90% and 98% of patients presented to the hospital with respiratory symptoms, such as shortness of breath, cough, hemoptysis, and/or chest pain. The most common reported e-cigarette product exposure among these case patients is tetrahydrocannabinol, THC (in approximately 80% to 85%); however, some used only nicotine-based products (15% to 20%). In addition, approximately 45% to 50% reported using THC and nicotine-based products. One concerning fact that requires special attention is that some affected patients initially presented with nonrespiratory complaints, such as GI symptoms of nausea, vomiting, and/or diarrhea; constitutional symptoms such as fever (up to 104oF), fatigue, and/or weight loss; and neurologic symptoms such as headaches and even seizures. Many of these symptoms preceded the respiratory symptoms by up to 2 weeks. Therefore, a few of these patients initially presented without significant respiratory symptoms and with normal chest radiographs – but progressed over days to weeks to acute hypoxemic respiratory failure.
Up to 75% of the affected patients who ultimately required hospitalization for e-cigarette-associated respiratory disease initially presented to a primary care clinic or ED and were sent home due to nonspecific signs and symptoms, which mimic common viral illnesses. Therefore, it is critical for all health-care professionals to have a high clinical suspicion for e-cigarette-associated respiratory disease, particularly while more data are being gathered. When suspected, the CDC recommends asking patients about specific substances inhaled, the manufacturer, where the products/cartridges were obtained, type of device(s) used, and method used (ie, aerosolization, dabbing, dripping, etc).
The most common types of imaging and pathologic patterns attributed to e-cigarette use reported to date include lipoid pneumonia, diffuse alveolar damage, acute
respiratory distress syndrome (ARDS), diffuse alveolar hemorrhage (DAH), acute eosinophilic pneumonia, hypersensitivity pneumonitis, and organizing pneumonia. The most common patterns on imaging include basilar-predominant consolidation and ground-glass opacities with areas of subpleural sparing. In addition, approximately 10% to 15% of the reported cases had a spontaneous pneumothorax, pneumomediastinum, and/or associated pleural effusions. Bronchoscopy specimens, such as bronchoalveolar lavage (BAL) and transbronchial biopsies (TBBx), were often but not always obtained. In patients who underwent bronchoscopy; many were found to have lipid-laden alveolar macrophages. These findings were discovered by staining fresh (ie, those not placed in fixative) specimens from BAL and/or TBBx for lipids with oil red O or another stain to specifically detect fat within the samples. Other etiologies of these radiographic/pathologic patterns and conditions should be excluded, as listed above.
The clinical course varies widely among these reported cases of vaping and e-cigarette-associated respiratory diseases. A minority of the reported patients spontaneously improved, and others required significant supportive care – from supplemental oxygen to complete support with ECMO. Some were treated with systemic corticosteroids with a wide range of responses and with various dosages: from prednisone of 0.5 to 1 mg/kg up to pulse-dose steroids with 1 g methylprednisolone for 3 days with a slow taper.
The information and data reported about these e-cigarette-associated respiratory diseases are clearly evolving quickly and vary from center to center and state to state. All suspected cases should be reported to your state health department. Similar to other inhalational injuries, it is critical to monitor these patients following recovery from the acute illness to help determine the long-term pulmonary effects and clinical courses of these individuals. Offering assistance and treatment for addiction is also important in these patients to help reduce their chances of recurrent respiratory problems from ongoing exposure to these substances in e-cigarettes. The bottom line is that cases of e-cigarette-associated respiratory diseases are increasing rapidly throughout the United States. Therefore, we should all be vigilant about asking our patients about their use of these substances and providing clear and strong messages for each of our patients to avoid vaping any substances through e-cigarettes.
Dr. Adams is Professor of Medicine, Pulmonary/Critical Care Division, Distinguished Teaching Professor, UT Health San Antonio; Staff Physician, South Texas Veterans Health Care System, San Antonio, Texas
References
Centers for Disease Control and Prevention. Severe pulmonary disease associated with using e-cigarette products. Health Alert Network. August 30, 2019. CDCHAN-00421. .
https://emergency.cdc.gov/han/han00421.asp
Centers for Disease Control and Prevention. Outbreak of lung illness associated with using e-cigarette products. Investigation Notice. September 6, 2019. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html.
Henry TS et al. Imaging of vaping-associated lung disease. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMc1911995. [Epub ahead of print].
Layden JE et al. Pulmonary illness related to e-cigarette use in Illinois and Wisconsin – preliminary report. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMoa1911614. [Epub ahead of print].
Maddock SD et al. Pulmonary lipid-laden macrophages and vaping. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMc1912038. [Epub ahead of print].
E-cigarettes arrived in the U.S. market between 2005 and 2007. Vaping via e-cigarettes involves inhaling substances such as nicotine, flavorings, chemicals, and, sometimes, marijuana and/or other substances deep into the lungs. While the use of these devices is prevalent, the long-term effects are not known. We, as clinicians, need to specifically ask our patients about their use of substances via e-cigarettes because of alarming cases of severe, life-threatening respiratory illnesses recently being reported throughout the United States in young, otherwise healthy, individuals.
As of September 11, 2019, over 380 cases have been reported to the Centers for Disease Control and Prevention (CDC), where young, healthy people from 33 states and one US territory were hospitalized with severe respiratory disease. There have been at least six confirmed deaths and approximately one-third of those who survived required aggressive support with intubation and mechanical ventilation. The number of reported cases is rapidly rising (from 215 possible cases on August 27, 2019). The common theme in these cases is that every patient reported using an e-cigarette product within 90 days of the onset of symptoms, and most within the prior 2 weeks. By definition, other etiologies of respiratory failure, such as infections, collagen vascular, immunologic diseases, and malignancies were excluded.
Between 90% and 98% of patients presented to the hospital with respiratory symptoms, such as shortness of breath, cough, hemoptysis, and/or chest pain. The most common reported e-cigarette product exposure among these case patients is tetrahydrocannabinol, THC (in approximately 80% to 85%); however, some used only nicotine-based products (15% to 20%). In addition, approximately 45% to 50% reported using THC and nicotine-based products. One concerning fact that requires special attention is that some affected patients initially presented with nonrespiratory complaints, such as GI symptoms of nausea, vomiting, and/or diarrhea; constitutional symptoms such as fever (up to 104oF), fatigue, and/or weight loss; and neurologic symptoms such as headaches and even seizures. Many of these symptoms preceded the respiratory symptoms by up to 2 weeks. Therefore, a few of these patients initially presented without significant respiratory symptoms and with normal chest radiographs – but progressed over days to weeks to acute hypoxemic respiratory failure.
Up to 75% of the affected patients who ultimately required hospitalization for e-cigarette-associated respiratory disease initially presented to a primary care clinic or ED and were sent home due to nonspecific signs and symptoms, which mimic common viral illnesses. Therefore, it is critical for all health-care professionals to have a high clinical suspicion for e-cigarette-associated respiratory disease, particularly while more data are being gathered. When suspected, the CDC recommends asking patients about specific substances inhaled, the manufacturer, where the products/cartridges were obtained, type of device(s) used, and method used (ie, aerosolization, dabbing, dripping, etc).
The most common types of imaging and pathologic patterns attributed to e-cigarette use reported to date include lipoid pneumonia, diffuse alveolar damage, acute
respiratory distress syndrome (ARDS), diffuse alveolar hemorrhage (DAH), acute eosinophilic pneumonia, hypersensitivity pneumonitis, and organizing pneumonia. The most common patterns on imaging include basilar-predominant consolidation and ground-glass opacities with areas of subpleural sparing. In addition, approximately 10% to 15% of the reported cases had a spontaneous pneumothorax, pneumomediastinum, and/or associated pleural effusions. Bronchoscopy specimens, such as bronchoalveolar lavage (BAL) and transbronchial biopsies (TBBx), were often but not always obtained. In patients who underwent bronchoscopy; many were found to have lipid-laden alveolar macrophages. These findings were discovered by staining fresh (ie, those not placed in fixative) specimens from BAL and/or TBBx for lipids with oil red O or another stain to specifically detect fat within the samples. Other etiologies of these radiographic/pathologic patterns and conditions should be excluded, as listed above.
The clinical course varies widely among these reported cases of vaping and e-cigarette-associated respiratory diseases. A minority of the reported patients spontaneously improved, and others required significant supportive care – from supplemental oxygen to complete support with ECMO. Some were treated with systemic corticosteroids with a wide range of responses and with various dosages: from prednisone of 0.5 to 1 mg/kg up to pulse-dose steroids with 1 g methylprednisolone for 3 days with a slow taper.
The information and data reported about these e-cigarette-associated respiratory diseases are clearly evolving quickly and vary from center to center and state to state. All suspected cases should be reported to your state health department. Similar to other inhalational injuries, it is critical to monitor these patients following recovery from the acute illness to help determine the long-term pulmonary effects and clinical courses of these individuals. Offering assistance and treatment for addiction is also important in these patients to help reduce their chances of recurrent respiratory problems from ongoing exposure to these substances in e-cigarettes. The bottom line is that cases of e-cigarette-associated respiratory diseases are increasing rapidly throughout the United States. Therefore, we should all be vigilant about asking our patients about their use of these substances and providing clear and strong messages for each of our patients to avoid vaping any substances through e-cigarettes.
Dr. Adams is Professor of Medicine, Pulmonary/Critical Care Division, Distinguished Teaching Professor, UT Health San Antonio; Staff Physician, South Texas Veterans Health Care System, San Antonio, Texas
References
Centers for Disease Control and Prevention. Severe pulmonary disease associated with using e-cigarette products. Health Alert Network. August 30, 2019. CDCHAN-00421. .
https://emergency.cdc.gov/han/han00421.asp
Centers for Disease Control and Prevention. Outbreak of lung illness associated with using e-cigarette products. Investigation Notice. September 6, 2019. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html.
Henry TS et al. Imaging of vaping-associated lung disease. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMc1911995. [Epub ahead of print].
Layden JE et al. Pulmonary illness related to e-cigarette use in Illinois and Wisconsin – preliminary report. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMoa1911614. [Epub ahead of print].
Maddock SD et al. Pulmonary lipid-laden macrophages and vaping. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMc1912038. [Epub ahead of print].
E-cigarettes arrived in the U.S. market between 2005 and 2007. Vaping via e-cigarettes involves inhaling substances such as nicotine, flavorings, chemicals, and, sometimes, marijuana and/or other substances deep into the lungs. While the use of these devices is prevalent, the long-term effects are not known. We, as clinicians, need to specifically ask our patients about their use of substances via e-cigarettes because of alarming cases of severe, life-threatening respiratory illnesses recently being reported throughout the United States in young, otherwise healthy, individuals.
As of September 11, 2019, over 380 cases have been reported to the Centers for Disease Control and Prevention (CDC), where young, healthy people from 33 states and one US territory were hospitalized with severe respiratory disease. There have been at least six confirmed deaths and approximately one-third of those who survived required aggressive support with intubation and mechanical ventilation. The number of reported cases is rapidly rising (from 215 possible cases on August 27, 2019). The common theme in these cases is that every patient reported using an e-cigarette product within 90 days of the onset of symptoms, and most within the prior 2 weeks. By definition, other etiologies of respiratory failure, such as infections, collagen vascular, immunologic diseases, and malignancies were excluded.
Between 90% and 98% of patients presented to the hospital with respiratory symptoms, such as shortness of breath, cough, hemoptysis, and/or chest pain. The most common reported e-cigarette product exposure among these case patients is tetrahydrocannabinol, THC (in approximately 80% to 85%); however, some used only nicotine-based products (15% to 20%). In addition, approximately 45% to 50% reported using THC and nicotine-based products. One concerning fact that requires special attention is that some affected patients initially presented with nonrespiratory complaints, such as GI symptoms of nausea, vomiting, and/or diarrhea; constitutional symptoms such as fever (up to 104oF), fatigue, and/or weight loss; and neurologic symptoms such as headaches and even seizures. Many of these symptoms preceded the respiratory symptoms by up to 2 weeks. Therefore, a few of these patients initially presented without significant respiratory symptoms and with normal chest radiographs – but progressed over days to weeks to acute hypoxemic respiratory failure.
Up to 75% of the affected patients who ultimately required hospitalization for e-cigarette-associated respiratory disease initially presented to a primary care clinic or ED and were sent home due to nonspecific signs and symptoms, which mimic common viral illnesses. Therefore, it is critical for all health-care professionals to have a high clinical suspicion for e-cigarette-associated respiratory disease, particularly while more data are being gathered. When suspected, the CDC recommends asking patients about specific substances inhaled, the manufacturer, where the products/cartridges were obtained, type of device(s) used, and method used (ie, aerosolization, dabbing, dripping, etc).
The most common types of imaging and pathologic patterns attributed to e-cigarette use reported to date include lipoid pneumonia, diffuse alveolar damage, acute
respiratory distress syndrome (ARDS), diffuse alveolar hemorrhage (DAH), acute eosinophilic pneumonia, hypersensitivity pneumonitis, and organizing pneumonia. The most common patterns on imaging include basilar-predominant consolidation and ground-glass opacities with areas of subpleural sparing. In addition, approximately 10% to 15% of the reported cases had a spontaneous pneumothorax, pneumomediastinum, and/or associated pleural effusions. Bronchoscopy specimens, such as bronchoalveolar lavage (BAL) and transbronchial biopsies (TBBx), were often but not always obtained. In patients who underwent bronchoscopy; many were found to have lipid-laden alveolar macrophages. These findings were discovered by staining fresh (ie, those not placed in fixative) specimens from BAL and/or TBBx for lipids with oil red O or another stain to specifically detect fat within the samples. Other etiologies of these radiographic/pathologic patterns and conditions should be excluded, as listed above.
The clinical course varies widely among these reported cases of vaping and e-cigarette-associated respiratory diseases. A minority of the reported patients spontaneously improved, and others required significant supportive care – from supplemental oxygen to complete support with ECMO. Some were treated with systemic corticosteroids with a wide range of responses and with various dosages: from prednisone of 0.5 to 1 mg/kg up to pulse-dose steroids with 1 g methylprednisolone for 3 days with a slow taper.
The information and data reported about these e-cigarette-associated respiratory diseases are clearly evolving quickly and vary from center to center and state to state. All suspected cases should be reported to your state health department. Similar to other inhalational injuries, it is critical to monitor these patients following recovery from the acute illness to help determine the long-term pulmonary effects and clinical courses of these individuals. Offering assistance and treatment for addiction is also important in these patients to help reduce their chances of recurrent respiratory problems from ongoing exposure to these substances in e-cigarettes. The bottom line is that cases of e-cigarette-associated respiratory diseases are increasing rapidly throughout the United States. Therefore, we should all be vigilant about asking our patients about their use of these substances and providing clear and strong messages for each of our patients to avoid vaping any substances through e-cigarettes.
Dr. Adams is Professor of Medicine, Pulmonary/Critical Care Division, Distinguished Teaching Professor, UT Health San Antonio; Staff Physician, South Texas Veterans Health Care System, San Antonio, Texas
References
Centers for Disease Control and Prevention. Severe pulmonary disease associated with using e-cigarette products. Health Alert Network. August 30, 2019. CDCHAN-00421. .
https://emergency.cdc.gov/han/han00421.asp
Centers for Disease Control and Prevention. Outbreak of lung illness associated with using e-cigarette products. Investigation Notice. September 6, 2019. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html.
Henry TS et al. Imaging of vaping-associated lung disease. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMc1911995. [Epub ahead of print].
Layden JE et al. Pulmonary illness related to e-cigarette use in Illinois and Wisconsin – preliminary report. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMoa1911614. [Epub ahead of print].
Maddock SD et al. Pulmonary lipid-laden macrophages and vaping. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMc1912038. [Epub ahead of print].
Coding changes coming soon
There may be some positive changes coming to evaluation and management (E/M) services effective January 1, 2021. In the proposed calendar year 2020 Physician Fee Schedule (CY 2020 PFS), the Centers for Medicare & Medicaid Services (CMS) suggested a number of coding, payment, and documentation changes for office/outpatient E/M visits, Current Procedural Terminology (CPT®) codes 99201-99215. A summary of these changes include:
• Separate payment for the five levels of office/outpatient E/M visit CPT codes, as revised by the CPT Editorial Panel effective January 1, 2021. This would include deletion of CPT code 99201 (Level 1 new patient office/outpatient E/M visit) and adoption of the revised CPT code descriptors for CPT codes 99202-99215;
• Elimination of the use of history and/or physical exam to select among code levels;
• Choice of time or medical decision making to decide the level of office/outpatient E/M visit (using the revised CPT interpretive guidelines for medical decision making);
• Payment for prolonged office/outpatient E/M visits using the revised CPT code for such services, including separate payment for new CPT code 99XXX and deletion of Healthcare Common Procedure Coding System (HCPCS) code GPRO1 (extended office/outpatient E/M visit) that was previously finalized for 2021;
• Revise the descriptor for HCPCS code GPC1X and delete HCPCS code GCG0X; and
• Increase in value for HCPCS code GPC1X and allowing it to be reported with all office/outpatient E/M visit levels.
These changes were recommended by CMS to improve payment accuracy, reduce the administrative burden, and better reflect the current practice of medicine. These changes are predicted to result in a simplification of physician documentation and a redistribution of payments favoring providers who deliver primary care or care to more complex patients.
In CY 2019 PFS, CMS proposed to pay a single (blended) rate for office/outpatient visits 2-4, but due to comments from stakeholders, including specialty societies, CMS proposed to accept alternate recommendations by AMA/CPT. These recommendations include using medical decision making or time to determine the level of a visit, rather than the schema that was based on history and physical exam and outlined in the 1995/1997 guidelines. This resulted in elimination of CPT code 99201 and changes to the descriptors of 99202-99215. These codes were resurveyed by the Relative Value Update Committee (RUC) resulting in new values and times. (See Table 1).
One can see that there has been an incremental increase in time and value for most codes. When selecting a code based upon time, there is a range that is defined for each code,and additional information about the codes, including the descriptors and ranges, can be found on the AMA website https://www.ama-assn.org/cpt-evaluation-and-management.
For CPT codes 99205 and 99215 (level 5 codes), an add-on code has also been proposed that would account for additional time spent above the new levels defined in the codes. The descriptor for CPT 99XXX (the final numbers have not yet been assigned) reads Prolonged office or other outpatient evaluation and management service(s) (beyond the total time of the primary procedure which has been selected using total time), requiring total time with or without direct patient contact beyond the usual service, on the date of the primary service; each 15 minutes (List separately in addition to codes 99205, 99215 for office or other outpatient Evaluation and Management services). 99XXX is similar to CPT add-on code 99292 in that it may be used multiple times for a single encounter. This is illustrated in Table 2.
However, 99XXX is only used with level 5 codes. It will replace HCPCS code GPRO1, which had been finalized in the CY 2019 PFS. The proposed code will have a value of 0.61 RVU.
Finally, there is a proposal to revise the descriptor for HCPCS code GPC1X and eliminate HCPCS code GCG0X. The new descriptor for GPC1X Visit complexity inherent to evaluation and management associated with medical care services that serve as the continuing focal point for all needed health care services and/or with medical care services that are part of ongoing care related to a patient’s single, serious, or complex chronic condition. (Add-on code, list separately in addition to office/outpatient evaluation and management visit, new or established) is being updated to simplify the coding and, with the elimination of GCG0X, to remove the perception that the code is primary care or specialty specific. The value of GPC1X is also being increased to 0.33 RVU.
It must be made clear that these changes are proposals only, and CMS is still reviewing stakeholder and public comments. Any actual changes will not be codified until publication of the CY2020 PFS later this year. Additional information regarding the proposed rule can be found by accessing https://federalregister.gov/d/2019-16041.
There may be some positive changes coming to evaluation and management (E/M) services effective January 1, 2021. In the proposed calendar year 2020 Physician Fee Schedule (CY 2020 PFS), the Centers for Medicare & Medicaid Services (CMS) suggested a number of coding, payment, and documentation changes for office/outpatient E/M visits, Current Procedural Terminology (CPT®) codes 99201-99215. A summary of these changes include:
• Separate payment for the five levels of office/outpatient E/M visit CPT codes, as revised by the CPT Editorial Panel effective January 1, 2021. This would include deletion of CPT code 99201 (Level 1 new patient office/outpatient E/M visit) and adoption of the revised CPT code descriptors for CPT codes 99202-99215;
• Elimination of the use of history and/or physical exam to select among code levels;
• Choice of time or medical decision making to decide the level of office/outpatient E/M visit (using the revised CPT interpretive guidelines for medical decision making);
• Payment for prolonged office/outpatient E/M visits using the revised CPT code for such services, including separate payment for new CPT code 99XXX and deletion of Healthcare Common Procedure Coding System (HCPCS) code GPRO1 (extended office/outpatient E/M visit) that was previously finalized for 2021;
• Revise the descriptor for HCPCS code GPC1X and delete HCPCS code GCG0X; and
• Increase in value for HCPCS code GPC1X and allowing it to be reported with all office/outpatient E/M visit levels.
These changes were recommended by CMS to improve payment accuracy, reduce the administrative burden, and better reflect the current practice of medicine. These changes are predicted to result in a simplification of physician documentation and a redistribution of payments favoring providers who deliver primary care or care to more complex patients.
In CY 2019 PFS, CMS proposed to pay a single (blended) rate for office/outpatient visits 2-4, but due to comments from stakeholders, including specialty societies, CMS proposed to accept alternate recommendations by AMA/CPT. These recommendations include using medical decision making or time to determine the level of a visit, rather than the schema that was based on history and physical exam and outlined in the 1995/1997 guidelines. This resulted in elimination of CPT code 99201 and changes to the descriptors of 99202-99215. These codes were resurveyed by the Relative Value Update Committee (RUC) resulting in new values and times. (See Table 1).
One can see that there has been an incremental increase in time and value for most codes. When selecting a code based upon time, there is a range that is defined for each code,and additional information about the codes, including the descriptors and ranges, can be found on the AMA website https://www.ama-assn.org/cpt-evaluation-and-management.
For CPT codes 99205 and 99215 (level 5 codes), an add-on code has also been proposed that would account for additional time spent above the new levels defined in the codes. The descriptor for CPT 99XXX (the final numbers have not yet been assigned) reads Prolonged office or other outpatient evaluation and management service(s) (beyond the total time of the primary procedure which has been selected using total time), requiring total time with or without direct patient contact beyond the usual service, on the date of the primary service; each 15 minutes (List separately in addition to codes 99205, 99215 for office or other outpatient Evaluation and Management services). 99XXX is similar to CPT add-on code 99292 in that it may be used multiple times for a single encounter. This is illustrated in Table 2.
However, 99XXX is only used with level 5 codes. It will replace HCPCS code GPRO1, which had been finalized in the CY 2019 PFS. The proposed code will have a value of 0.61 RVU.
Finally, there is a proposal to revise the descriptor for HCPCS code GPC1X and eliminate HCPCS code GCG0X. The new descriptor for GPC1X Visit complexity inherent to evaluation and management associated with medical care services that serve as the continuing focal point for all needed health care services and/or with medical care services that are part of ongoing care related to a patient’s single, serious, or complex chronic condition. (Add-on code, list separately in addition to office/outpatient evaluation and management visit, new or established) is being updated to simplify the coding and, with the elimination of GCG0X, to remove the perception that the code is primary care or specialty specific. The value of GPC1X is also being increased to 0.33 RVU.
It must be made clear that these changes are proposals only, and CMS is still reviewing stakeholder and public comments. Any actual changes will not be codified until publication of the CY2020 PFS later this year. Additional information regarding the proposed rule can be found by accessing https://federalregister.gov/d/2019-16041.
There may be some positive changes coming to evaluation and management (E/M) services effective January 1, 2021. In the proposed calendar year 2020 Physician Fee Schedule (CY 2020 PFS), the Centers for Medicare & Medicaid Services (CMS) suggested a number of coding, payment, and documentation changes for office/outpatient E/M visits, Current Procedural Terminology (CPT®) codes 99201-99215. A summary of these changes include:
• Separate payment for the five levels of office/outpatient E/M visit CPT codes, as revised by the CPT Editorial Panel effective January 1, 2021. This would include deletion of CPT code 99201 (Level 1 new patient office/outpatient E/M visit) and adoption of the revised CPT code descriptors for CPT codes 99202-99215;
• Elimination of the use of history and/or physical exam to select among code levels;
• Choice of time or medical decision making to decide the level of office/outpatient E/M visit (using the revised CPT interpretive guidelines for medical decision making);
• Payment for prolonged office/outpatient E/M visits using the revised CPT code for such services, including separate payment for new CPT code 99XXX and deletion of Healthcare Common Procedure Coding System (HCPCS) code GPRO1 (extended office/outpatient E/M visit) that was previously finalized for 2021;
• Revise the descriptor for HCPCS code GPC1X and delete HCPCS code GCG0X; and
• Increase in value for HCPCS code GPC1X and allowing it to be reported with all office/outpatient E/M visit levels.
These changes were recommended by CMS to improve payment accuracy, reduce the administrative burden, and better reflect the current practice of medicine. These changes are predicted to result in a simplification of physician documentation and a redistribution of payments favoring providers who deliver primary care or care to more complex patients.
In CY 2019 PFS, CMS proposed to pay a single (blended) rate for office/outpatient visits 2-4, but due to comments from stakeholders, including specialty societies, CMS proposed to accept alternate recommendations by AMA/CPT. These recommendations include using medical decision making or time to determine the level of a visit, rather than the schema that was based on history and physical exam and outlined in the 1995/1997 guidelines. This resulted in elimination of CPT code 99201 and changes to the descriptors of 99202-99215. These codes were resurveyed by the Relative Value Update Committee (RUC) resulting in new values and times. (See Table 1).
One can see that there has been an incremental increase in time and value for most codes. When selecting a code based upon time, there is a range that is defined for each code,and additional information about the codes, including the descriptors and ranges, can be found on the AMA website https://www.ama-assn.org/cpt-evaluation-and-management.
For CPT codes 99205 and 99215 (level 5 codes), an add-on code has also been proposed that would account for additional time spent above the new levels defined in the codes. The descriptor for CPT 99XXX (the final numbers have not yet been assigned) reads Prolonged office or other outpatient evaluation and management service(s) (beyond the total time of the primary procedure which has been selected using total time), requiring total time with or without direct patient contact beyond the usual service, on the date of the primary service; each 15 minutes (List separately in addition to codes 99205, 99215 for office or other outpatient Evaluation and Management services). 99XXX is similar to CPT add-on code 99292 in that it may be used multiple times for a single encounter. This is illustrated in Table 2.
However, 99XXX is only used with level 5 codes. It will replace HCPCS code GPRO1, which had been finalized in the CY 2019 PFS. The proposed code will have a value of 0.61 RVU.
Finally, there is a proposal to revise the descriptor for HCPCS code GPC1X and eliminate HCPCS code GCG0X. The new descriptor for GPC1X Visit complexity inherent to evaluation and management associated with medical care services that serve as the continuing focal point for all needed health care services and/or with medical care services that are part of ongoing care related to a patient’s single, serious, or complex chronic condition. (Add-on code, list separately in addition to office/outpatient evaluation and management visit, new or established) is being updated to simplify the coding and, with the elimination of GCG0X, to remove the perception that the code is primary care or specialty specific. The value of GPC1X is also being increased to 0.33 RVU.
It must be made clear that these changes are proposals only, and CMS is still reviewing stakeholder and public comments. Any actual changes will not be codified until publication of the CY2020 PFS later this year. Additional information regarding the proposed rule can be found by accessing https://federalregister.gov/d/2019-16041.
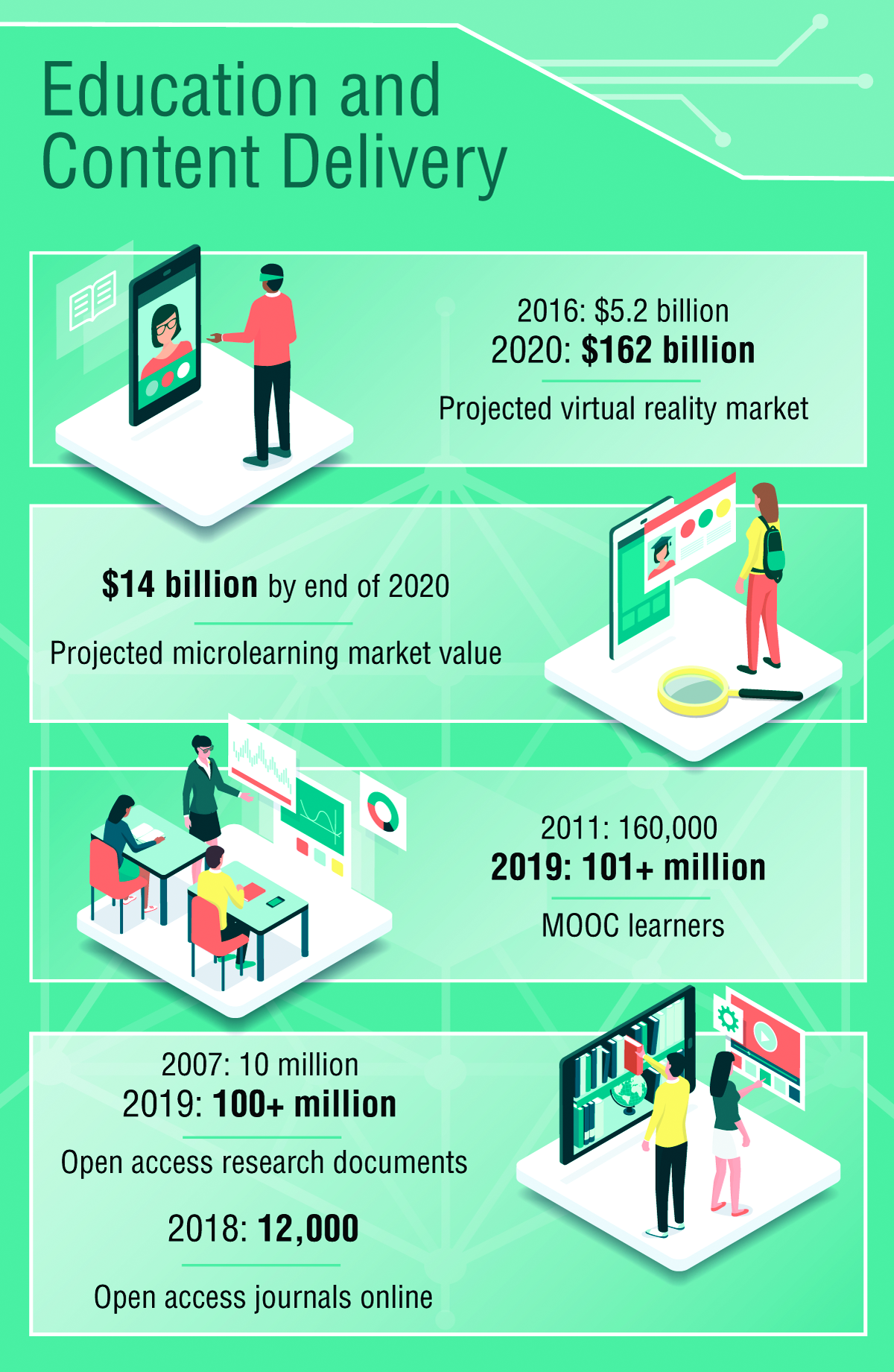
Environmental Scan: Drivers of change in education, content delivery, and career advancement
Keeping up to date and maintaining currency on developments in medicine are a routine part of medical practice, but the means by which this is accomplished are changing rapidly. Training, maintenance of certification, continuing education, mentoring, and career development will all be transformed in the coming years because of new technology and changing needs of physicians. Traditional learning channels such as print media and in-person courses will give way to options that emphasize ease of access, collaboration with fellow learners, and digitally optimized content.
Education and content delivery
The primary distribution channels for keeping medical professionals current in their specialty will continue to shift away from print publications and expand to digital outlets including podcasts, video, and online access to content.1 Individuals seeking to keep up professionally will increasingly turn to resources that can be found quickly and easily, for example, through voice search. Content that has been optimized to appear quickly and with a clear layout adapted to a wide variety of devices will most likely be consumed at a higher rate than resources from well-established organizations that have not transformed their continuing education content. There is already a growing demand for video and audiocasts accessible via mobile device.2
John D. Buckley, MD, FCCP, professor of medicine and vice chair for education at Indiana University, Indianapolis, sees the transformation of content delivery as a net plus for physicians, with a couple of caveats. He noted, “Whether it is conducting an in-depth literature search, reading/streaming a review lecture, or simply confirming a medical fact, quick access can enhance patient care and advance learning in a manner that meets an individual’s learning style. One potential downside is the risk of unreliable information, so accessing trustworthy sources is essential. Another potential downside is that, while accessing the answer to a very specific question can be done very easily, this might compromise additional learning of related material that used to occur when you had to read an entire book chapter to answer your question. Not only did you answer your question, you learned a lot of other relevant information along the way.”
Online learning is now a vast industry and has been harnessed by millions to further professional learning opportunities. Massive Open Online Courses (MOOCs) are free online courses available for anyone to enroll.3 MOOCs have been established at Harvard, MIT, Microsoft, and other top universities and institutions in subjects like computer science, data science, business, and more. MOOCs are being replicated in conventional universities and are projected to be a model for adult learning in the coming decade.4
Another trend is the growing interest in microlearning, defined as short educational activities that deal with relatively small learning units utilized at the point where the learner will actually need the information.5
Dr. Buckley sees potential in microlearning for continuing medical education. “It is unlikely that microlearning would be eligible for CME currently unless there were a mechanism for aggregating multiple events into a substantive unit of credit. But the ACCME [Accreditation Council for Continuing Medical Education] has been very adaptive to various forms of learning, so aggregate microlearning for CME credit may be possible in the future.” He added that the benefits of rapid and reliable access of specific information from a trusted source are significant, and the opportunities for microlearning for chest physicians are almost limitless. “Whether searching for the most updated review of a medical topic, or checking to see if your ICU patient’s sedating medication can cause serotonin syndrome, microlearning is already playing a large role in physician education, just less formal that what’s been used historically,” he said.
Institutions for which professional development learning modules are an important revenue stream will increasingly be challenged to compete with open-access courses of varying quality.
A key trend identified in 2018 is accelerating higher-education technology adoption and a growing focus on measured outcomes and learning.5 Individuals are interested in personalized learning plans and adaptive learning systems that can provide real-time assessments and immediate feedback. It is expected that learning modules and curricula will be most successful if they are easily accessed, attractively presented, and incorporate immediate feedback on learning progress. Driving technology adoption in higher education in the next 3-5 years will be the proliferation of open educational resources and the rise of new forms of interdisciplinary studies. As the environment for providing and accessing content shifts from pay-to-access to open-access, organizations will need to identify a new value proposition if they wish to grow or maintain related revenue streams.6
The implications of these changes in demand are profound for creators of continuing education content for medical professionals. Major investment will be needed in new, possibly costly platforms that deliver high-quality content with accessibility and interactive elements to meet the demands of professionals, the younger generation in particular.7 The market will continue to develop new technology to serve continuing education needs and preferences of users, thus fueling competition among stakeholders. With the proliferation of free and low-cost online and virtual programs, continuing education providers may experience a negative impact on an important revenue stream if they don’t identify a competitive advantage that meets the needs of tomorrow’s workforce. However, educational programs and courses that use artificial intelligence, virtual reality, and augmented reality to enhance the learning experience are likely to experience higher levels of use in the coming years.8
Workforce diversity and mentoring
A global economy requires organizations to seek a diverse workforce. Diversity can also lead to higher levels of profitability and employee satisfaction. As such, it will be essential for organizations to increase opportunities for individuals from diverse backgrounds to join the workforce. Creating a diverse workforce will mean removing barriers of time and location to skill building through online learning opportunities and facilitation of interdisciplinary career paths.
A critical piece of the emerging model of career development will be mentoring. Many professionals in today’s workforce view mentoring as an opportunity to gain immediate skills and knowledge quickly and effectively. Mentoring has evolved from pairing young professionals with seasoned veterans to creating relationships that match individuals with others who have the skills and knowledge they desire to learn about – regardless of age and experience. Institutions striving to develop a diverse workforce will need many individuals to serve as both mentors and mentees. When searching for solutions to work-related challenges, individuals will increasingly turn to knowledge management and collaboration systems (virtual mentoring) that provide them with the opportunity to match their needs in an efficient and effective manner.
Dr. Buckley values peer-to-peer mentoring as a means of accessing and sharing niche expertise among colleagues, but he acknowledges the difficulties in incorporating it into everyday practice. “The biggest obstacles are probably time and access. More and more learners and mentors are recognizing the tremendous value of effective mentorship, so convincing people is less of an issue than finding time,” he said.
Mentorship will continue to play a central role in the advancement of one’s career, yet women and minorities find it increasingly difficult to match with a mentor within the workplace. These candidates are likely to seek external opportunities. Individuals will evaluate the experience, opportunities for career advancement and the level of diversity and inclusion when seeking and accepting a new job.
Dr. Buckley sees both progress and remaining challenges in reducing barriers to underrepresented groups in medical institutions. “There continues to be a need for ongoing training to help individuals and institutions recognize and eliminate their barriers and biases, both conscious and subconscious, that interfere with achieving diversity and inclusion. Another important limitation is the pipeline of underrepresented groups that are pursuing careers in medicine. We need to do more empowerment, encouragement, and recruitment of underrepresented groups at a very early stage in their education if we ever expect to achieve our goals.”
Future challenges
The transformations described above will require a large investment by physicians aiming to maintain professional currency, by creators of continuing education content, and by employers seeking a diversified workforce. All these stakeholders have an interest in the future direction of continuing education and professional training. The development of new platforms for delivery of content that is easily accessible, formatted for a wide variety of devices, and built with real-time feedback functions will require a significant commitment of resources.
References
1. IDC Trackers. “Worldwide semiannual augmented and virtual reality spending guide.” Accessed Sept. 3, 2019.
2. ASAE. “Foresight Works: User’s Guide.” ASAE Foundation, 2018.
3. Online Course Report. “The State of MOOC 2016: A year of massive landscape change for massive open online courses.” Accessed Sept. 3, 2019.
4. Bill & Melinda Gates Foundation. “Postsecondary Success: Data and Information.” Accessed Sept. 4, 2019.
5. QYReports. “The Microlearning Market Report, 2018.” Accessed Sept. 4, 2019.
6. Adams S et al. “NMC Horizon Report: 2018 Higher Education Edition.” Louisville, CO: EDUCAUSE, 2018.
7. An M. “Content trends: Preferences emerge along generational fault lines.” Hubspot: Nov. 6, 2017; updated Dec 14, 2018.
8. Grajek S and Grama J. “Higher education’s 2018 trend watch and top 10 strategic technologies.” EDUCAUSE Review, Jan 29, 2018.
Note: Background research performed by Avenue M Group.
CHEST Inspiration is a collection of programmatic initiatives developed by the American College of Chest Physicians leadership and aimed at stimulating and encouraging innovation within the association. One of the components of CHEST Inspiration is the Environmental Scan, a series of articles focusing on the internal and external environmental factors that bear on success currently and in the future. See “Envisioning the Future: The CHEST Environmental Scan,” CHEST Physician, June 2019, p. 44, for an introduction to the series.
Keeping up to date and maintaining currency on developments in medicine are a routine part of medical practice, but the means by which this is accomplished are changing rapidly. Training, maintenance of certification, continuing education, mentoring, and career development will all be transformed in the coming years because of new technology and changing needs of physicians. Traditional learning channels such as print media and in-person courses will give way to options that emphasize ease of access, collaboration with fellow learners, and digitally optimized content.
Education and content delivery
The primary distribution channels for keeping medical professionals current in their specialty will continue to shift away from print publications and expand to digital outlets including podcasts, video, and online access to content.1 Individuals seeking to keep up professionally will increasingly turn to resources that can be found quickly and easily, for example, through voice search. Content that has been optimized to appear quickly and with a clear layout adapted to a wide variety of devices will most likely be consumed at a higher rate than resources from well-established organizations that have not transformed their continuing education content. There is already a growing demand for video and audiocasts accessible via mobile device.2
John D. Buckley, MD, FCCP, professor of medicine and vice chair for education at Indiana University, Indianapolis, sees the transformation of content delivery as a net plus for physicians, with a couple of caveats. He noted, “Whether it is conducting an in-depth literature search, reading/streaming a review lecture, or simply confirming a medical fact, quick access can enhance patient care and advance learning in a manner that meets an individual’s learning style. One potential downside is the risk of unreliable information, so accessing trustworthy sources is essential. Another potential downside is that, while accessing the answer to a very specific question can be done very easily, this might compromise additional learning of related material that used to occur when you had to read an entire book chapter to answer your question. Not only did you answer your question, you learned a lot of other relevant information along the way.”
Online learning is now a vast industry and has been harnessed by millions to further professional learning opportunities. Massive Open Online Courses (MOOCs) are free online courses available for anyone to enroll.3 MOOCs have been established at Harvard, MIT, Microsoft, and other top universities and institutions in subjects like computer science, data science, business, and more. MOOCs are being replicated in conventional universities and are projected to be a model for adult learning in the coming decade.4
Another trend is the growing interest in microlearning, defined as short educational activities that deal with relatively small learning units utilized at the point where the learner will actually need the information.5
Dr. Buckley sees potential in microlearning for continuing medical education. “It is unlikely that microlearning would be eligible for CME currently unless there were a mechanism for aggregating multiple events into a substantive unit of credit. But the ACCME [Accreditation Council for Continuing Medical Education] has been very adaptive to various forms of learning, so aggregate microlearning for CME credit may be possible in the future.” He added that the benefits of rapid and reliable access of specific information from a trusted source are significant, and the opportunities for microlearning for chest physicians are almost limitless. “Whether searching for the most updated review of a medical topic, or checking to see if your ICU patient’s sedating medication can cause serotonin syndrome, microlearning is already playing a large role in physician education, just less formal that what’s been used historically,” he said.
Institutions for which professional development learning modules are an important revenue stream will increasingly be challenged to compete with open-access courses of varying quality.
A key trend identified in 2018 is accelerating higher-education technology adoption and a growing focus on measured outcomes and learning.5 Individuals are interested in personalized learning plans and adaptive learning systems that can provide real-time assessments and immediate feedback. It is expected that learning modules and curricula will be most successful if they are easily accessed, attractively presented, and incorporate immediate feedback on learning progress. Driving technology adoption in higher education in the next 3-5 years will be the proliferation of open educational resources and the rise of new forms of interdisciplinary studies. As the environment for providing and accessing content shifts from pay-to-access to open-access, organizations will need to identify a new value proposition if they wish to grow or maintain related revenue streams.6
The implications of these changes in demand are profound for creators of continuing education content for medical professionals. Major investment will be needed in new, possibly costly platforms that deliver high-quality content with accessibility and interactive elements to meet the demands of professionals, the younger generation in particular.7 The market will continue to develop new technology to serve continuing education needs and preferences of users, thus fueling competition among stakeholders. With the proliferation of free and low-cost online and virtual programs, continuing education providers may experience a negative impact on an important revenue stream if they don’t identify a competitive advantage that meets the needs of tomorrow’s workforce. However, educational programs and courses that use artificial intelligence, virtual reality, and augmented reality to enhance the learning experience are likely to experience higher levels of use in the coming years.8
Workforce diversity and mentoring
A global economy requires organizations to seek a diverse workforce. Diversity can also lead to higher levels of profitability and employee satisfaction. As such, it will be essential for organizations to increase opportunities for individuals from diverse backgrounds to join the workforce. Creating a diverse workforce will mean removing barriers of time and location to skill building through online learning opportunities and facilitation of interdisciplinary career paths.
A critical piece of the emerging model of career development will be mentoring. Many professionals in today’s workforce view mentoring as an opportunity to gain immediate skills and knowledge quickly and effectively. Mentoring has evolved from pairing young professionals with seasoned veterans to creating relationships that match individuals with others who have the skills and knowledge they desire to learn about – regardless of age and experience. Institutions striving to develop a diverse workforce will need many individuals to serve as both mentors and mentees. When searching for solutions to work-related challenges, individuals will increasingly turn to knowledge management and collaboration systems (virtual mentoring) that provide them with the opportunity to match their needs in an efficient and effective manner.
Dr. Buckley values peer-to-peer mentoring as a means of accessing and sharing niche expertise among colleagues, but he acknowledges the difficulties in incorporating it into everyday practice. “The biggest obstacles are probably time and access. More and more learners and mentors are recognizing the tremendous value of effective mentorship, so convincing people is less of an issue than finding time,” he said.
Mentorship will continue to play a central role in the advancement of one’s career, yet women and minorities find it increasingly difficult to match with a mentor within the workplace. These candidates are likely to seek external opportunities. Individuals will evaluate the experience, opportunities for career advancement and the level of diversity and inclusion when seeking and accepting a new job.
Dr. Buckley sees both progress and remaining challenges in reducing barriers to underrepresented groups in medical institutions. “There continues to be a need for ongoing training to help individuals and institutions recognize and eliminate their barriers and biases, both conscious and subconscious, that interfere with achieving diversity and inclusion. Another important limitation is the pipeline of underrepresented groups that are pursuing careers in medicine. We need to do more empowerment, encouragement, and recruitment of underrepresented groups at a very early stage in their education if we ever expect to achieve our goals.”
Future challenges
The transformations described above will require a large investment by physicians aiming to maintain professional currency, by creators of continuing education content, and by employers seeking a diversified workforce. All these stakeholders have an interest in the future direction of continuing education and professional training. The development of new platforms for delivery of content that is easily accessible, formatted for a wide variety of devices, and built with real-time feedback functions will require a significant commitment of resources.
References
1. IDC Trackers. “Worldwide semiannual augmented and virtual reality spending guide.” Accessed Sept. 3, 2019.
2. ASAE. “Foresight Works: User’s Guide.” ASAE Foundation, 2018.
3. Online Course Report. “The State of MOOC 2016: A year of massive landscape change for massive open online courses.” Accessed Sept. 3, 2019.
4. Bill & Melinda Gates Foundation. “Postsecondary Success: Data and Information.” Accessed Sept. 4, 2019.
5. QYReports. “The Microlearning Market Report, 2018.” Accessed Sept. 4, 2019.
6. Adams S et al. “NMC Horizon Report: 2018 Higher Education Edition.” Louisville, CO: EDUCAUSE, 2018.
7. An M. “Content trends: Preferences emerge along generational fault lines.” Hubspot: Nov. 6, 2017; updated Dec 14, 2018.
8. Grajek S and Grama J. “Higher education’s 2018 trend watch and top 10 strategic technologies.” EDUCAUSE Review, Jan 29, 2018.
Note: Background research performed by Avenue M Group.
CHEST Inspiration is a collection of programmatic initiatives developed by the American College of Chest Physicians leadership and aimed at stimulating and encouraging innovation within the association. One of the components of CHEST Inspiration is the Environmental Scan, a series of articles focusing on the internal and external environmental factors that bear on success currently and in the future. See “Envisioning the Future: The CHEST Environmental Scan,” CHEST Physician, June 2019, p. 44, for an introduction to the series.
Keeping up to date and maintaining currency on developments in medicine are a routine part of medical practice, but the means by which this is accomplished are changing rapidly. Training, maintenance of certification, continuing education, mentoring, and career development will all be transformed in the coming years because of new technology and changing needs of physicians. Traditional learning channels such as print media and in-person courses will give way to options that emphasize ease of access, collaboration with fellow learners, and digitally optimized content.
Education and content delivery
The primary distribution channels for keeping medical professionals current in their specialty will continue to shift away from print publications and expand to digital outlets including podcasts, video, and online access to content.1 Individuals seeking to keep up professionally will increasingly turn to resources that can be found quickly and easily, for example, through voice search. Content that has been optimized to appear quickly and with a clear layout adapted to a wide variety of devices will most likely be consumed at a higher rate than resources from well-established organizations that have not transformed their continuing education content. There is already a growing demand for video and audiocasts accessible via mobile device.2
John D. Buckley, MD, FCCP, professor of medicine and vice chair for education at Indiana University, Indianapolis, sees the transformation of content delivery as a net plus for physicians, with a couple of caveats. He noted, “Whether it is conducting an in-depth literature search, reading/streaming a review lecture, or simply confirming a medical fact, quick access can enhance patient care and advance learning in a manner that meets an individual’s learning style. One potential downside is the risk of unreliable information, so accessing trustworthy sources is essential. Another potential downside is that, while accessing the answer to a very specific question can be done very easily, this might compromise additional learning of related material that used to occur when you had to read an entire book chapter to answer your question. Not only did you answer your question, you learned a lot of other relevant information along the way.”
Online learning is now a vast industry and has been harnessed by millions to further professional learning opportunities. Massive Open Online Courses (MOOCs) are free online courses available for anyone to enroll.3 MOOCs have been established at Harvard, MIT, Microsoft, and other top universities and institutions in subjects like computer science, data science, business, and more. MOOCs are being replicated in conventional universities and are projected to be a model for adult learning in the coming decade.4
Another trend is the growing interest in microlearning, defined as short educational activities that deal with relatively small learning units utilized at the point where the learner will actually need the information.5
Dr. Buckley sees potential in microlearning for continuing medical education. “It is unlikely that microlearning would be eligible for CME currently unless there were a mechanism for aggregating multiple events into a substantive unit of credit. But the ACCME [Accreditation Council for Continuing Medical Education] has been very adaptive to various forms of learning, so aggregate microlearning for CME credit may be possible in the future.” He added that the benefits of rapid and reliable access of specific information from a trusted source are significant, and the opportunities for microlearning for chest physicians are almost limitless. “Whether searching for the most updated review of a medical topic, or checking to see if your ICU patient’s sedating medication can cause serotonin syndrome, microlearning is already playing a large role in physician education, just less formal that what’s been used historically,” he said.
Institutions for which professional development learning modules are an important revenue stream will increasingly be challenged to compete with open-access courses of varying quality.
A key trend identified in 2018 is accelerating higher-education technology adoption and a growing focus on measured outcomes and learning.5 Individuals are interested in personalized learning plans and adaptive learning systems that can provide real-time assessments and immediate feedback. It is expected that learning modules and curricula will be most successful if they are easily accessed, attractively presented, and incorporate immediate feedback on learning progress. Driving technology adoption in higher education in the next 3-5 years will be the proliferation of open educational resources and the rise of new forms of interdisciplinary studies. As the environment for providing and accessing content shifts from pay-to-access to open-access, organizations will need to identify a new value proposition if they wish to grow or maintain related revenue streams.6
The implications of these changes in demand are profound for creators of continuing education content for medical professionals. Major investment will be needed in new, possibly costly platforms that deliver high-quality content with accessibility and interactive elements to meet the demands of professionals, the younger generation in particular.7 The market will continue to develop new technology to serve continuing education needs and preferences of users, thus fueling competition among stakeholders. With the proliferation of free and low-cost online and virtual programs, continuing education providers may experience a negative impact on an important revenue stream if they don’t identify a competitive advantage that meets the needs of tomorrow’s workforce. However, educational programs and courses that use artificial intelligence, virtual reality, and augmented reality to enhance the learning experience are likely to experience higher levels of use in the coming years.8
Workforce diversity and mentoring
A global economy requires organizations to seek a diverse workforce. Diversity can also lead to higher levels of profitability and employee satisfaction. As such, it will be essential for organizations to increase opportunities for individuals from diverse backgrounds to join the workforce. Creating a diverse workforce will mean removing barriers of time and location to skill building through online learning opportunities and facilitation of interdisciplinary career paths.
A critical piece of the emerging model of career development will be mentoring. Many professionals in today’s workforce view mentoring as an opportunity to gain immediate skills and knowledge quickly and effectively. Mentoring has evolved from pairing young professionals with seasoned veterans to creating relationships that match individuals with others who have the skills and knowledge they desire to learn about – regardless of age and experience. Institutions striving to develop a diverse workforce will need many individuals to serve as both mentors and mentees. When searching for solutions to work-related challenges, individuals will increasingly turn to knowledge management and collaboration systems (virtual mentoring) that provide them with the opportunity to match their needs in an efficient and effective manner.
Dr. Buckley values peer-to-peer mentoring as a means of accessing and sharing niche expertise among colleagues, but he acknowledges the difficulties in incorporating it into everyday practice. “The biggest obstacles are probably time and access. More and more learners and mentors are recognizing the tremendous value of effective mentorship, so convincing people is less of an issue than finding time,” he said.
Mentorship will continue to play a central role in the advancement of one’s career, yet women and minorities find it increasingly difficult to match with a mentor within the workplace. These candidates are likely to seek external opportunities. Individuals will evaluate the experience, opportunities for career advancement and the level of diversity and inclusion when seeking and accepting a new job.
Dr. Buckley sees both progress and remaining challenges in reducing barriers to underrepresented groups in medical institutions. “There continues to be a need for ongoing training to help individuals and institutions recognize and eliminate their barriers and biases, both conscious and subconscious, that interfere with achieving diversity and inclusion. Another important limitation is the pipeline of underrepresented groups that are pursuing careers in medicine. We need to do more empowerment, encouragement, and recruitment of underrepresented groups at a very early stage in their education if we ever expect to achieve our goals.”
Future challenges
The transformations described above will require a large investment by physicians aiming to maintain professional currency, by creators of continuing education content, and by employers seeking a diversified workforce. All these stakeholders have an interest in the future direction of continuing education and professional training. The development of new platforms for delivery of content that is easily accessible, formatted for a wide variety of devices, and built with real-time feedback functions will require a significant commitment of resources.
References
1. IDC Trackers. “Worldwide semiannual augmented and virtual reality spending guide.” Accessed Sept. 3, 2019.
2. ASAE. “Foresight Works: User’s Guide.” ASAE Foundation, 2018.
3. Online Course Report. “The State of MOOC 2016: A year of massive landscape change for massive open online courses.” Accessed Sept. 3, 2019.
4. Bill & Melinda Gates Foundation. “Postsecondary Success: Data and Information.” Accessed Sept. 4, 2019.
5. QYReports. “The Microlearning Market Report, 2018.” Accessed Sept. 4, 2019.
6. Adams S et al. “NMC Horizon Report: 2018 Higher Education Edition.” Louisville, CO: EDUCAUSE, 2018.
7. An M. “Content trends: Preferences emerge along generational fault lines.” Hubspot: Nov. 6, 2017; updated Dec 14, 2018.
8. Grajek S and Grama J. “Higher education’s 2018 trend watch and top 10 strategic technologies.” EDUCAUSE Review, Jan 29, 2018.
Note: Background research performed by Avenue M Group.
CHEST Inspiration is a collection of programmatic initiatives developed by the American College of Chest Physicians leadership and aimed at stimulating and encouraging innovation within the association. One of the components of CHEST Inspiration is the Environmental Scan, a series of articles focusing on the internal and external environmental factors that bear on success currently and in the future. See “Envisioning the Future: The CHEST Environmental Scan,” CHEST Physician, June 2019, p. 44, for an introduction to the series.
Prepare for VAM 2020
Mark your calendars: the 2020 Vascular Annual Meeting will take place June 17-20 at the Toronto Convention Center in Toronto, Ontario, Canada. All U.S. residents entering Canada will be required to travel with a valid passport. Your passport expiration date may not be within six months of your travel dates. For additional information (including passport requirements for international travelers), please visit the Canada Border Services Agency’s website. Read all future VAM details here.
Mark your calendars: the 2020 Vascular Annual Meeting will take place June 17-20 at the Toronto Convention Center in Toronto, Ontario, Canada. All U.S. residents entering Canada will be required to travel with a valid passport. Your passport expiration date may not be within six months of your travel dates. For additional information (including passport requirements for international travelers), please visit the Canada Border Services Agency’s website. Read all future VAM details here.
Mark your calendars: the 2020 Vascular Annual Meeting will take place June 17-20 at the Toronto Convention Center in Toronto, Ontario, Canada. All U.S. residents entering Canada will be required to travel with a valid passport. Your passport expiration date may not be within six months of your travel dates. For additional information (including passport requirements for international travelers), please visit the Canada Border Services Agency’s website. Read all future VAM details here.
Utilize SVS Patient Resources
Our website contains many resources that SVS members can use for help with managing a practice, continuing education, patient education materials and much more. The patient resource pages on the site cover a variety of vascular conditions, tests and treatments. Most recently, we’ve added a page for Transcarotid Artery Revascularization (TCAR). This, and most of our pages, can give patients and/or their loved ones a better understanding of their vascular condition, as well as how it’s being tested and treated. Take a look at our pages and share with your patients today.
Our website contains many resources that SVS members can use for help with managing a practice, continuing education, patient education materials and much more. The patient resource pages on the site cover a variety of vascular conditions, tests and treatments. Most recently, we’ve added a page for Transcarotid Artery Revascularization (TCAR). This, and most of our pages, can give patients and/or their loved ones a better understanding of their vascular condition, as well as how it’s being tested and treated. Take a look at our pages and share with your patients today.
Our website contains many resources that SVS members can use for help with managing a practice, continuing education, patient education materials and much more. The patient resource pages on the site cover a variety of vascular conditions, tests and treatments. Most recently, we’ve added a page for Transcarotid Artery Revascularization (TCAR). This, and most of our pages, can give patients and/or their loved ones a better understanding of their vascular condition, as well as how it’s being tested and treated. Take a look at our pages and share with your patients today.
Food as therapy and toxin
I return to write the Editor’s comments after missing last month because I joined over 700,000 Americans who, this year, will undergo knee replacement surgery.
This month, we feature a couple articles from the 2019 James W. Freston Conference (an annual AGA event that highlights cutting-edge science). Jim was the 89th AGA President (1995) and this conference is a fitting legacy. This year’s topic was “Food at the intersection of gut health and disease.” As usual, the Freston Conference attracted international experts and interested clinicians who want to understand how current research will alter our clinical care in the near future.
Our front-page articles are fascinating. One highlights new advances in the management of celiac disease. Although the only current treatment that reverses intestinal immunological damage is adoption of a gluten-free diet, there is demand for alternative treatments including medical therapies targeting specific steps in the celiac damage pathway. While none are ready for wide-spread adoption, research will continue. Patient self-management with gluten detection-devices were also discussed.
Advances in the genetics of Crohn’s disease are being published at an accelerating rate. This month we highlight an article about how gene expression analysis can predict response to a Crohn’s flare. Evidence-based therapy for inflammatory bowel disease is complex, so clinicians need to stay current. Each year, the premier IBD educational venue is co-produced by the AGA and the Crohn’s & Colitis Foundation. The 2020 Crohn’s and Colitis Congress will be held in Austin, Texas January 23-25. Learn more at: https://www.crohnscolitiscongress.org.
Finally, I want to highlight an article about the risk of venous thromboembolism (VTE) during and after an IBD flare. This risk is underappreciated by many treating physicians but it is real and can be life-threatening. Gastroenterologists must be knowledgeable about current guidelines for VTE in IBD patients (see Gastroenterology 2014;146:835-48).
John I. Allen, MD, MBA, AGAF
Editor in Chief
I return to write the Editor’s comments after missing last month because I joined over 700,000 Americans who, this year, will undergo knee replacement surgery.
This month, we feature a couple articles from the 2019 James W. Freston Conference (an annual AGA event that highlights cutting-edge science). Jim was the 89th AGA President (1995) and this conference is a fitting legacy. This year’s topic was “Food at the intersection of gut health and disease.” As usual, the Freston Conference attracted international experts and interested clinicians who want to understand how current research will alter our clinical care in the near future.
Our front-page articles are fascinating. One highlights new advances in the management of celiac disease. Although the only current treatment that reverses intestinal immunological damage is adoption of a gluten-free diet, there is demand for alternative treatments including medical therapies targeting specific steps in the celiac damage pathway. While none are ready for wide-spread adoption, research will continue. Patient self-management with gluten detection-devices were also discussed.
Advances in the genetics of Crohn’s disease are being published at an accelerating rate. This month we highlight an article about how gene expression analysis can predict response to a Crohn’s flare. Evidence-based therapy for inflammatory bowel disease is complex, so clinicians need to stay current. Each year, the premier IBD educational venue is co-produced by the AGA and the Crohn’s & Colitis Foundation. The 2020 Crohn’s and Colitis Congress will be held in Austin, Texas January 23-25. Learn more at: https://www.crohnscolitiscongress.org.
Finally, I want to highlight an article about the risk of venous thromboembolism (VTE) during and after an IBD flare. This risk is underappreciated by many treating physicians but it is real and can be life-threatening. Gastroenterologists must be knowledgeable about current guidelines for VTE in IBD patients (see Gastroenterology 2014;146:835-48).
John I. Allen, MD, MBA, AGAF
Editor in Chief
I return to write the Editor’s comments after missing last month because I joined over 700,000 Americans who, this year, will undergo knee replacement surgery.
This month, we feature a couple articles from the 2019 James W. Freston Conference (an annual AGA event that highlights cutting-edge science). Jim was the 89th AGA President (1995) and this conference is a fitting legacy. This year’s topic was “Food at the intersection of gut health and disease.” As usual, the Freston Conference attracted international experts and interested clinicians who want to understand how current research will alter our clinical care in the near future.
Our front-page articles are fascinating. One highlights new advances in the management of celiac disease. Although the only current treatment that reverses intestinal immunological damage is adoption of a gluten-free diet, there is demand for alternative treatments including medical therapies targeting specific steps in the celiac damage pathway. While none are ready for wide-spread adoption, research will continue. Patient self-management with gluten detection-devices were also discussed.
Advances in the genetics of Crohn’s disease are being published at an accelerating rate. This month we highlight an article about how gene expression analysis can predict response to a Crohn’s flare. Evidence-based therapy for inflammatory bowel disease is complex, so clinicians need to stay current. Each year, the premier IBD educational venue is co-produced by the AGA and the Crohn’s & Colitis Foundation. The 2020 Crohn’s and Colitis Congress will be held in Austin, Texas January 23-25. Learn more at: https://www.crohnscolitiscongress.org.
Finally, I want to highlight an article about the risk of venous thromboembolism (VTE) during and after an IBD flare. This risk is underappreciated by many treating physicians but it is real and can be life-threatening. Gastroenterologists must be knowledgeable about current guidelines for VTE in IBD patients (see Gastroenterology 2014;146:835-48).
John I. Allen, MD, MBA, AGAF
Editor in Chief
Tell your patients these four things about prebiotics
Explaining prebiotics:
- • Prebiotics serve as food for specific microbes in the gut but their health benefits are likely due to broader changes in the function of communities of microbes.
- • Prebiotics can lead to a durable change in overall function of a gut microbial community with potential for long-term health benefit while probiotics are live microorganisms that when administered in adequate amounts can confer a health benefit even in the short term.
- • Prebiotics ferment to short-chain fatty acids known to positively influence human metabolism and immunity. Commercial prebiotics may be beneficial in some individuals but intolerable in others.
- • Further research is needed to determine the specificity of prebiotics in terms of their biological effects. Other dietary fibers/proteins may have similar health benefits that have not yet been determined.
These tips are from “Prebiotics 101,” the first of a four-part CME series in AGA University, agau.gastro.org, titled, “The Microbiome and Digestive Health: A Look at Prebiotics.” Part two, “Diet vs. Prebiotics” is also available.
Looking for more information on prebiotics?
AGA has educational materials for patients on probiotics (also available in Spanish) at gastro.org/patient.
Explaining prebiotics:
- • Prebiotics serve as food for specific microbes in the gut but their health benefits are likely due to broader changes in the function of communities of microbes.
- • Prebiotics can lead to a durable change in overall function of a gut microbial community with potential for long-term health benefit while probiotics are live microorganisms that when administered in adequate amounts can confer a health benefit even in the short term.
- • Prebiotics ferment to short-chain fatty acids known to positively influence human metabolism and immunity. Commercial prebiotics may be beneficial in some individuals but intolerable in others.
- • Further research is needed to determine the specificity of prebiotics in terms of their biological effects. Other dietary fibers/proteins may have similar health benefits that have not yet been determined.
These tips are from “Prebiotics 101,” the first of a four-part CME series in AGA University, agau.gastro.org, titled, “The Microbiome and Digestive Health: A Look at Prebiotics.” Part two, “Diet vs. Prebiotics” is also available.
Looking for more information on prebiotics?
AGA has educational materials for patients on probiotics (also available in Spanish) at gastro.org/patient.
Explaining prebiotics:
- • Prebiotics serve as food for specific microbes in the gut but their health benefits are likely due to broader changes in the function of communities of microbes.
- • Prebiotics can lead to a durable change in overall function of a gut microbial community with potential for long-term health benefit while probiotics are live microorganisms that when administered in adequate amounts can confer a health benefit even in the short term.
- • Prebiotics ferment to short-chain fatty acids known to positively influence human metabolism and immunity. Commercial prebiotics may be beneficial in some individuals but intolerable in others.
- • Further research is needed to determine the specificity of prebiotics in terms of their biological effects. Other dietary fibers/proteins may have similar health benefits that have not yet been determined.
These tips are from “Prebiotics 101,” the first of a four-part CME series in AGA University, agau.gastro.org, titled, “The Microbiome and Digestive Health: A Look at Prebiotics.” Part two, “Diet vs. Prebiotics” is also available.
Looking for more information on prebiotics?
AGA has educational materials for patients on probiotics (also available in Spanish) at gastro.org/patient.
AGA urges Medicare to fix CRC screening coinsurance issue
AGA and our sister societies met with Medicare staff in Washington, DC, to voice our opposition to its proposal that would require physicians to inform patients about potential colorectal cancer (CRC) screening costs. Under the proposal, physicians who plan to perform a CRC screening for a Medicare beneficiary must tell the beneficiary in advance that they may have to pay coinsurance under the Medicare program if the screening finds polyps that are removed as part of the screening procedure and document the conversation in the beneficiary’s medical record starting Jan. 1, 2020.
Under the Affordable Care Act, Medicare beneficiaries do not need to pay for screenings that receive an A or B from the U.S. Preventive Services Task Force (USPSTF), such as screening colonoscopy. However, because of Medicare’s interpretation of the coding rules, when a polyp is found and removed during a screening colonoscopy, it is considered a diagnostic procedure and the patient is required to pay the coinsurance. Medicare’s new proposal does not solve the underlying problem — fixing the coinsurance issue for Medicare beneficiaries; instead, it shifts responsibility to notify Medicare beneficiaries to the physician.
The gastroenterology community, together with patient advocates, has been asking CMS since 2011 to use its authority to fix the Medicare screening colonoscopy coinsurance problem. It was never the intention of Congress for polypectomy resulting from the initial screening to be excluded from the screening benefit. The Obama administration provided guidance for commercial plans on this screening benefit and stated that plans should not impose coinsurance since “removal of polyp is integral to the screening” and thus most private insurers recognize the benefit of waiving the coinsurance.
In our meeting with Medicare, we told them that beneficiaries should not be penalized because of the agency’s misinterpretation of Congress’ legislation. We also urged Medicare not to add to physician burden, to take responsibility for notifying patients of its own coverage and payment policies, and to focus on ways to help patients avoid unfair financial penalties resulting from its misinterpretation of Congress’s mandate for free CRC screening.
Medicare needs to hear from you today. Sign our letter on gastro.org/advocacy to let your voice be heard.
AGA and our sister societies met with Medicare staff in Washington, DC, to voice our opposition to its proposal that would require physicians to inform patients about potential colorectal cancer (CRC) screening costs. Under the proposal, physicians who plan to perform a CRC screening for a Medicare beneficiary must tell the beneficiary in advance that they may have to pay coinsurance under the Medicare program if the screening finds polyps that are removed as part of the screening procedure and document the conversation in the beneficiary’s medical record starting Jan. 1, 2020.
Under the Affordable Care Act, Medicare beneficiaries do not need to pay for screenings that receive an A or B from the U.S. Preventive Services Task Force (USPSTF), such as screening colonoscopy. However, because of Medicare’s interpretation of the coding rules, when a polyp is found and removed during a screening colonoscopy, it is considered a diagnostic procedure and the patient is required to pay the coinsurance. Medicare’s new proposal does not solve the underlying problem — fixing the coinsurance issue for Medicare beneficiaries; instead, it shifts responsibility to notify Medicare beneficiaries to the physician.
The gastroenterology community, together with patient advocates, has been asking CMS since 2011 to use its authority to fix the Medicare screening colonoscopy coinsurance problem. It was never the intention of Congress for polypectomy resulting from the initial screening to be excluded from the screening benefit. The Obama administration provided guidance for commercial plans on this screening benefit and stated that plans should not impose coinsurance since “removal of polyp is integral to the screening” and thus most private insurers recognize the benefit of waiving the coinsurance.
In our meeting with Medicare, we told them that beneficiaries should not be penalized because of the agency’s misinterpretation of Congress’ legislation. We also urged Medicare not to add to physician burden, to take responsibility for notifying patients of its own coverage and payment policies, and to focus on ways to help patients avoid unfair financial penalties resulting from its misinterpretation of Congress’s mandate for free CRC screening.
Medicare needs to hear from you today. Sign our letter on gastro.org/advocacy to let your voice be heard.
AGA and our sister societies met with Medicare staff in Washington, DC, to voice our opposition to its proposal that would require physicians to inform patients about potential colorectal cancer (CRC) screening costs. Under the proposal, physicians who plan to perform a CRC screening for a Medicare beneficiary must tell the beneficiary in advance that they may have to pay coinsurance under the Medicare program if the screening finds polyps that are removed as part of the screening procedure and document the conversation in the beneficiary’s medical record starting Jan. 1, 2020.
Under the Affordable Care Act, Medicare beneficiaries do not need to pay for screenings that receive an A or B from the U.S. Preventive Services Task Force (USPSTF), such as screening colonoscopy. However, because of Medicare’s interpretation of the coding rules, when a polyp is found and removed during a screening colonoscopy, it is considered a diagnostic procedure and the patient is required to pay the coinsurance. Medicare’s new proposal does not solve the underlying problem — fixing the coinsurance issue for Medicare beneficiaries; instead, it shifts responsibility to notify Medicare beneficiaries to the physician.
The gastroenterology community, together with patient advocates, has been asking CMS since 2011 to use its authority to fix the Medicare screening colonoscopy coinsurance problem. It was never the intention of Congress for polypectomy resulting from the initial screening to be excluded from the screening benefit. The Obama administration provided guidance for commercial plans on this screening benefit and stated that plans should not impose coinsurance since “removal of polyp is integral to the screening” and thus most private insurers recognize the benefit of waiving the coinsurance.
In our meeting with Medicare, we told them that beneficiaries should not be penalized because of the agency’s misinterpretation of Congress’ legislation. We also urged Medicare not to add to physician burden, to take responsibility for notifying patients of its own coverage and payment policies, and to focus on ways to help patients avoid unfair financial penalties resulting from its misinterpretation of Congress’s mandate for free CRC screening.
Medicare needs to hear from you today. Sign our letter on gastro.org/advocacy to let your voice be heard.
Include the AGA Research Foundation in your estate plan
Gifts to charitable organizations, such as the AGA Research Foundation, in your future plans ensure your support for our mission continues even after your lifetime. Review these goals to turn financial aspiration into charitable action to achieve your philanthropic vision.
Goal: Take care of those you love
Use your will or living trust to clearly communicate your intentions for how you would like to provide for your loved ones and favorite causes, including the AGA Research Foundation. You can feel secure knowing you will maintain control of your assets until after your lifetime and that your gifts are revocable so you can change your mind at any time.
Goal: Eliminate capital gains tax on stocks
When you donate appreciated securities – that is, stocks you’ve owned for more than 1 year that are now worth more than you originally paid for them – you can benefit yourself and the AGA Research Foundation. You can reduce or even eliminate federal capital gains taxes on the stock transfer, and you may be entitled to a federal income tax charitable deduction.
Tip: There are a number of ways to give appreciated securities, such as outright giving or funding a charitable gift annuity or a charitable remainder trust.
Goal: Conserve today’s finances
Save critical funds now by naming the AGA Research Foundation as the beneficiary of all or a percentage (1%-100%) of your IRA. Leaving all or part of your IRA to charity after your lifetime dramatically lowers future taxes for your beneficiaries. Naming a charity, like the AGA Research Foundation, as a beneficiary can eliminate federal income taxes that could consume a substantial portion of your account.
Want to learn more about including a gift to the AGA Research Foundation in your future plans? Visit our website at https://gastro.planmylegacy.org or contact Harmony Excellent at 301-272-1602 or [email protected].
Gifts to charitable organizations, such as the AGA Research Foundation, in your future plans ensure your support for our mission continues even after your lifetime. Review these goals to turn financial aspiration into charitable action to achieve your philanthropic vision.
Goal: Take care of those you love
Use your will or living trust to clearly communicate your intentions for how you would like to provide for your loved ones and favorite causes, including the AGA Research Foundation. You can feel secure knowing you will maintain control of your assets until after your lifetime and that your gifts are revocable so you can change your mind at any time.
Goal: Eliminate capital gains tax on stocks
When you donate appreciated securities – that is, stocks you’ve owned for more than 1 year that are now worth more than you originally paid for them – you can benefit yourself and the AGA Research Foundation. You can reduce or even eliminate federal capital gains taxes on the stock transfer, and you may be entitled to a federal income tax charitable deduction.
Tip: There are a number of ways to give appreciated securities, such as outright giving or funding a charitable gift annuity or a charitable remainder trust.
Goal: Conserve today’s finances
Save critical funds now by naming the AGA Research Foundation as the beneficiary of all or a percentage (1%-100%) of your IRA. Leaving all or part of your IRA to charity after your lifetime dramatically lowers future taxes for your beneficiaries. Naming a charity, like the AGA Research Foundation, as a beneficiary can eliminate federal income taxes that could consume a substantial portion of your account.
Want to learn more about including a gift to the AGA Research Foundation in your future plans? Visit our website at https://gastro.planmylegacy.org or contact Harmony Excellent at 301-272-1602 or [email protected].
Gifts to charitable organizations, such as the AGA Research Foundation, in your future plans ensure your support for our mission continues even after your lifetime. Review these goals to turn financial aspiration into charitable action to achieve your philanthropic vision.
Goal: Take care of those you love
Use your will or living trust to clearly communicate your intentions for how you would like to provide for your loved ones and favorite causes, including the AGA Research Foundation. You can feel secure knowing you will maintain control of your assets until after your lifetime and that your gifts are revocable so you can change your mind at any time.
Goal: Eliminate capital gains tax on stocks
When you donate appreciated securities – that is, stocks you’ve owned for more than 1 year that are now worth more than you originally paid for them – you can benefit yourself and the AGA Research Foundation. You can reduce or even eliminate federal capital gains taxes on the stock transfer, and you may be entitled to a federal income tax charitable deduction.
Tip: There are a number of ways to give appreciated securities, such as outright giving or funding a charitable gift annuity or a charitable remainder trust.
Goal: Conserve today’s finances
Save critical funds now by naming the AGA Research Foundation as the beneficiary of all or a percentage (1%-100%) of your IRA. Leaving all or part of your IRA to charity after your lifetime dramatically lowers future taxes for your beneficiaries. Naming a charity, like the AGA Research Foundation, as a beneficiary can eliminate federal income taxes that could consume a substantial portion of your account.
Want to learn more about including a gift to the AGA Research Foundation in your future plans? Visit our website at https://gastro.planmylegacy.org or contact Harmony Excellent at 301-272-1602 or [email protected].