User login
AGA says stay the course, despite the Delta variant
As COVID-19 cases rise in the United States due to the Delta variant, there is renewed concern about infection and transmission of SARS-CoV-2 during endoscopy. In May 2021, AGA released updated recommendations on preprocedure testing post vaccination in the setting of ongoing population-wide vaccination programs for the prevention of COVID-19–related morbidity. In vaccinated individuals, breakthrough infections occurred very infrequently. Weighing the evidence demonstrating extremely low rates of rates of infection and transmission with vaccination and PPE, and considering the downsides of routine testing (burden, cost, false test results, increased disparities), AGA made a conditional recommendation against routine preprocedure testing for elective cases. The highly contagious Delta variant has now emerged as the predominant SARS-CoV2 virus in the U.S. and some data suggests that it may cause more severe illness than previous strains. While more breakthrough infections may develop in fully vaccinated individuals, the greatest risk of infection, transmission and hospitalizations is among those who are unvaccinated.
- AGA suggests against reinstituting routine preprocedure testing prior to elective endoscopy. The downsides (delays in patient care, burden, inaccurate results) outweigh potential benefits. Infection and transmission of SARS-CoV-2 from asymptomatic individuals is rare especially among vaccinated health care workers using personal protective equipment (PPE), even with the emergence of the Delta variant.
- If PPE is available, AGA recommends using N95 for upper endoscopy and suggests using N95 or surgical masks for lower endoscopy (acknowledging that upper endoscopy is more aerosolizing than lower endoscopy) and continuation of elective and nonelective endoscopy.
- Based on local prevalence rates, PPE, and test availability, in intermediate- and high-prevalence settings, preprocedure testing may be used to inform PPE decisions (N95 versus surgical mask). Additional benefits to testing are small and include deferring elective endoscopy in individuals testing positive and reducing anxiety among staff and patients.
As COVID-19 cases rise in the United States due to the Delta variant, there is renewed concern about infection and transmission of SARS-CoV-2 during endoscopy. In May 2021, AGA released updated recommendations on preprocedure testing post vaccination in the setting of ongoing population-wide vaccination programs for the prevention of COVID-19–related morbidity. In vaccinated individuals, breakthrough infections occurred very infrequently. Weighing the evidence demonstrating extremely low rates of rates of infection and transmission with vaccination and PPE, and considering the downsides of routine testing (burden, cost, false test results, increased disparities), AGA made a conditional recommendation against routine preprocedure testing for elective cases. The highly contagious Delta variant has now emerged as the predominant SARS-CoV2 virus in the U.S. and some data suggests that it may cause more severe illness than previous strains. While more breakthrough infections may develop in fully vaccinated individuals, the greatest risk of infection, transmission and hospitalizations is among those who are unvaccinated.
- AGA suggests against reinstituting routine preprocedure testing prior to elective endoscopy. The downsides (delays in patient care, burden, inaccurate results) outweigh potential benefits. Infection and transmission of SARS-CoV-2 from asymptomatic individuals is rare especially among vaccinated health care workers using personal protective equipment (PPE), even with the emergence of the Delta variant.
- If PPE is available, AGA recommends using N95 for upper endoscopy and suggests using N95 or surgical masks for lower endoscopy (acknowledging that upper endoscopy is more aerosolizing than lower endoscopy) and continuation of elective and nonelective endoscopy.
- Based on local prevalence rates, PPE, and test availability, in intermediate- and high-prevalence settings, preprocedure testing may be used to inform PPE decisions (N95 versus surgical mask). Additional benefits to testing are small and include deferring elective endoscopy in individuals testing positive and reducing anxiety among staff and patients.
As COVID-19 cases rise in the United States due to the Delta variant, there is renewed concern about infection and transmission of SARS-CoV-2 during endoscopy. In May 2021, AGA released updated recommendations on preprocedure testing post vaccination in the setting of ongoing population-wide vaccination programs for the prevention of COVID-19–related morbidity. In vaccinated individuals, breakthrough infections occurred very infrequently. Weighing the evidence demonstrating extremely low rates of rates of infection and transmission with vaccination and PPE, and considering the downsides of routine testing (burden, cost, false test results, increased disparities), AGA made a conditional recommendation against routine preprocedure testing for elective cases. The highly contagious Delta variant has now emerged as the predominant SARS-CoV2 virus in the U.S. and some data suggests that it may cause more severe illness than previous strains. While more breakthrough infections may develop in fully vaccinated individuals, the greatest risk of infection, transmission and hospitalizations is among those who are unvaccinated.
- AGA suggests against reinstituting routine preprocedure testing prior to elective endoscopy. The downsides (delays in patient care, burden, inaccurate results) outweigh potential benefits. Infection and transmission of SARS-CoV-2 from asymptomatic individuals is rare especially among vaccinated health care workers using personal protective equipment (PPE), even with the emergence of the Delta variant.
- If PPE is available, AGA recommends using N95 for upper endoscopy and suggests using N95 or surgical masks for lower endoscopy (acknowledging that upper endoscopy is more aerosolizing than lower endoscopy) and continuation of elective and nonelective endoscopy.
- Based on local prevalence rates, PPE, and test availability, in intermediate- and high-prevalence settings, preprocedure testing may be used to inform PPE decisions (N95 versus surgical mask). Additional benefits to testing are small and include deferring elective endoscopy in individuals testing positive and reducing anxiety among staff and patients.
AGA leaders met with federal regulators
AGA President John Inadomi, MD, and former AGA President David Lieberman, MD, along with American Cancer Society Cancer Action Network and Fight CRC, met with Assistant Secretary of Labor, Ali Khawar, and representatives from the U.S. Department of Health & Human Services and U.S. Department of Treasury to request they direct private health plans to cover colonoscopy after a positive noninvasive colorectal cancer (CRC) screening test.
The meeting was in response to an appeal sent to the three agencies, which provided guidance to health plans to ensure that workers have the benefits that have been agreed upon by their employers. As part of the Affordable Care Act, plans are mandated to cover colorectal cancer screening without cost sharing.
In May 2021, when the United States Preventive Services Task Force (USPFTF) lowered the recommended CRC screening age to 45, it also stated that “positive results on stool-based screening tests require follow-up with colonoscopy for the screening benefits to be achieved.”
To ensure that privately insured Americans receive proper CRC screening, AGA, ACS, and Fight CRC are pushing the government to provide written guidance to private plans clarifying that follow-up colonoscopies conducted after a positive noninvasive screening test are part of the colorectal cancer screening process and, therefore, patients should not face out-of-pocket costs when completing colorectal cancer screening.
Colorectal cancer remains the second leading killer in cancer in the United States despite the availability of preventive screening options. In 2018, just 68.8% of those eligible were screened for colorectal cancer. The challenge of getting people screened was exacerbated in 2020 when it is estimated that colorectal cancer screening declined by 86% during the first few months of the COVID-19 pandemic.
AGA President John Inadomi, MD, and former AGA President David Lieberman, MD, along with American Cancer Society Cancer Action Network and Fight CRC, met with Assistant Secretary of Labor, Ali Khawar, and representatives from the U.S. Department of Health & Human Services and U.S. Department of Treasury to request they direct private health plans to cover colonoscopy after a positive noninvasive colorectal cancer (CRC) screening test.
The meeting was in response to an appeal sent to the three agencies, which provided guidance to health plans to ensure that workers have the benefits that have been agreed upon by their employers. As part of the Affordable Care Act, plans are mandated to cover colorectal cancer screening without cost sharing.
In May 2021, when the United States Preventive Services Task Force (USPFTF) lowered the recommended CRC screening age to 45, it also stated that “positive results on stool-based screening tests require follow-up with colonoscopy for the screening benefits to be achieved.”
To ensure that privately insured Americans receive proper CRC screening, AGA, ACS, and Fight CRC are pushing the government to provide written guidance to private plans clarifying that follow-up colonoscopies conducted after a positive noninvasive screening test are part of the colorectal cancer screening process and, therefore, patients should not face out-of-pocket costs when completing colorectal cancer screening.
Colorectal cancer remains the second leading killer in cancer in the United States despite the availability of preventive screening options. In 2018, just 68.8% of those eligible were screened for colorectal cancer. The challenge of getting people screened was exacerbated in 2020 when it is estimated that colorectal cancer screening declined by 86% during the first few months of the COVID-19 pandemic.
AGA President John Inadomi, MD, and former AGA President David Lieberman, MD, along with American Cancer Society Cancer Action Network and Fight CRC, met with Assistant Secretary of Labor, Ali Khawar, and representatives from the U.S. Department of Health & Human Services and U.S. Department of Treasury to request they direct private health plans to cover colonoscopy after a positive noninvasive colorectal cancer (CRC) screening test.
The meeting was in response to an appeal sent to the three agencies, which provided guidance to health plans to ensure that workers have the benefits that have been agreed upon by their employers. As part of the Affordable Care Act, plans are mandated to cover colorectal cancer screening without cost sharing.
In May 2021, when the United States Preventive Services Task Force (USPFTF) lowered the recommended CRC screening age to 45, it also stated that “positive results on stool-based screening tests require follow-up with colonoscopy for the screening benefits to be achieved.”
To ensure that privately insured Americans receive proper CRC screening, AGA, ACS, and Fight CRC are pushing the government to provide written guidance to private plans clarifying that follow-up colonoscopies conducted after a positive noninvasive screening test are part of the colorectal cancer screening process and, therefore, patients should not face out-of-pocket costs when completing colorectal cancer screening.
Colorectal cancer remains the second leading killer in cancer in the United States despite the availability of preventive screening options. In 2018, just 68.8% of those eligible were screened for colorectal cancer. The challenge of getting people screened was exacerbated in 2020 when it is estimated that colorectal cancer screening declined by 86% during the first few months of the COVID-19 pandemic.
Is the end near for surgical and transbronchial biopsies? Challenges in the pediatric workforce; Cascade testing in PAH; and more ...
Interventional chest/diagnostic procedures
Endobronchial optical coherence tomography and interstitial lung diseases: Is the end near for surgical and transbronchial lung biopsies?
The early diagnosis of interstitial lung diseases (ILD) is paramount to initiating appropriate treatment and preventing irreversible pulmonary damage. Specific ILD subtypes may be diagnosed based on clinical evaluation, high resolution chest CT (HRCT) patterns, and serologic testing, but many patients require invasive procedures for histopathologic evaluation of lung tissue. Current modalities for obtaining tissue include transbronchial lung cryobiopsy (TBLC) and surgical lung biopsy (SLB), both of which carry a risk of potential complications (Troy LK, et al. Lancet Respir Med. 2020;8:171-81; Hutchinson JP, et al. Am J Respir Crit Care Med. 2016;193[10]:1161-7).
Recently, genomic classifiers applied to transbronchial biopsies have been proposed to facilitate the diagnosis of usual interstitial pneumonia (UIP), but the limited information provided still does not obviate the need for tissue diagnosis when needed (Raghu G, et al. Lancet Respir Med. 2019;7[6]:487-96). It is in this context that endobronchial optical coherence tomography (EB-OCT) was proposed as a real-time, in vivo, optical biopsy method for ILD.
EB-OCT uses near infrared light to generate large volumes of in-vivo three-dimensional tissue imaging with microscopic resolution (Goorsenberg A, et al. Respiration. 2020;99:190-205; Nandy S, et al. Am J Respir Crit Care Med. 2021;article in press). The OCT catheter is advanced through the bronchoscope working channel and can be used during outpatient procedures under conscious sedation. Available data suggests that minimal training is necessary, both for proceduralists and interpreting pathologists, but this will need to be confirmed in larger studies and various practice settings. Early studies suggest that OCT can identify microscopic honeycombing and other abnormalities even before they are evident on HRCT scans (Goorsenberg A, et al. Respiration. 2020;99:190-205). Newer research comparing ILD diagnosis from EB-OCT cross-sectional images with that obtained from SLB specimens revealed EB-OCT can distinguish UIP from non-UIP ILD with high sensitivity and specificity (Nandy S, et al. Am J Respir Crit Care Med. 2021;article in press). Could this mean the end of SLB and TBLC for the diagnosis of ILD? While the ability to diagnose ILD subtypes with high reliability and low risk of complications is certainly promising, studies remain admittedly small and the technique itself is only available to highly select individuals and specialized ILD centers. Let’s not pack up the cryoprobe just yet.
Audra J. Schwalk, MD, MBA: Steering Committee Member
Fabien Maldonado, MD, FCCP: Steering Committee Member
Pediatric chest medicine
Challenges in the pediatric pulmonary workforce
The future of the pediatric workforce has been the source of extensive discussion within the pediatric community and resulted in a considerable body of medical literature (Vinci RJ. Pediatrics. 2021;147[6]:e2020013292). In pediatric pulmonology, there is growing concern that current trends will lead to a workforce shortage resulting in patients having difficulty accessing subspecialty care (Harris C, et al. Pediatric Pulmonol. 2019;54[4]:444-50). The etiology of this shortage is multifactorial. Duration of fellowship training and subsequent financial implications are reported potential barriers to pursuing a fellowship (Nelson BA, et al. Pediatric Pulmonol. 2020;1-7). Discrepancies between pediatric and adult compensation may be another barrier. Insightful recruitment strategies based on the results of a recent study included maximizing resident interaction with pulmonary faculty, early identification and support of interested trainees, and consideration of flexible training models (Nelson BA, et al. ATS Sch. 2020;1:372-83). Lifestyle has also been a factor that contributes to a trainee’s decision to go into pediatric pulmonology (Freed GL, et al. Pediatrics. 2009;123(suppl 1):S31‐S37).
As our field addresses the critical need to recruit more trainees in light of the unfilled fellowship positions and the increasing average age of members of the field, we should not underestimate the prevalence of systemic racism and bias in medicine (Chiel L, et al. ATS Sch. 2020;1[4]:337-39) nor gender discrimination. Instead, we should seize the opportunity to understand and knock down barriers that trainees who are underrepresented in medicine face in pursuing pediatric subspecialty careers and build upon the excellent recent body of literature in this field to help recruit, support , and grow a robust, diverse workforce to provide the best pediatric care to all.
Anne C. Coates, MD – Steering Committee Member
Pulmonary vascular disease
Cascade testing in PAH: Is there a role?
Pediatric guidelines for pulmonary arterial hypertension (PAH) recommends genetic screening as a part of the evaluation for the newly diagnosed, with expansion to first-degree relatives as indicated. Currently, this is not mandated, and implementation is variable. In adults, genetic screening is not routinely offered, and family screening is rare. This reflects a lack of definitive guidelines (Abman SH, et al. Circulation. 2015:24;132[21]:2037-99). However, it is intuitive that if carriers are not identified by screening, they will come to attention after pulmonary vascular disease burden causes symptoms and affects outcomes.
Cascade testing is a screening methodology that is used in heritable cancers (George RM, et al. Genet Couns. 2015;24[3]:388-99). In cascade testing, identification of an index case prompts screening of at-risk family members. If these relatives are positive for mutations, the cycle is repeated (cascaded) to their immediate relatives, allowing for targeted screening. This approach is especially effective in genetic mutations that are inherited in an autosomal dominant fashion, such as in BMPR2 gene mutation. Cascade testing is an effective way to capture relatives who would otherwise be overlooked.
Unfortunately, in the United States, the cost of genetic testing is a significant obstacle to universal implementation. A new diagnosis of heritable pulmonary arterial hypertension (HPAH) is often followed by a multigene panel with costs exceeding $1000 and may prompt subsequent targeted testing resulting in additional expense (Chung WK, et al. Can J Cardiol. 2015;31[4]:544-47). Furthermore, a positive mutation detected on screening is not definitively associated with disease due to variable penetrance (Morrell NW, et al. Eur Respir J. 2019;53[1]:1801899]. As such, mass screening strategies are not recommended. The recent DELPHI-2 study [Montani D, et al. Eur Respir J. 2021;58[1]:2004229) have demonstrated that genetic screening is impactful in families with HPAH. A genetic screening algorithm should be considered, and cascade testing could be a cost-effective targeted approach.
Sandeep Sahay, MD, MSc, FCCP: Steering Committee Member
Jean M. Elwing, MD, FCCP: Chair
Pulmonary physiology, function, and rehabilitation network
Physiological benefits of awake proning: Its role and relevance in the COVID-19 pandemic
The advent of the COVID-19 pandemic has put a significant strain on the health care systems and critical care services across several countries, including the United States. Amidst this, several concerted efforts to reduce the need for mechanical ventilation has resulted in the emergence of awake proning as a strategy to improve oxygenation, which has been instituted in critical care units, in-patient settings, as well as in EDs. Although the evidence on this strategy has been vastly limited to case series and observational studies, several societies have incorporated awake proning as an initial management strategy in hypoxemic respiratory failure within their clinical guidelines (Chalmers JD, et al. Eur Respir J. 2021;57:2100048; Koeckerling D, et al. Thorax. 2020;75:833-4) and consensus statements (Nasa P, et al. Crit Care. 2021;25:106).
Physiological benefits of awake proning include improvement in ventilation-perfusion matching secondary to relative increase in ventilation in dorsal nondependent areas in the setting of higher density of perfusion within these units, thus reducing shunt and, hence, improving oxygenation. Other physiological mechanisms include homogenization of transpulmonary pressures, reduction of ventilator-induced lung injury (VILI) or patient self-inflicted lung injury (P-SILI), and possibly lung injury from pendelluft (Telias I, et al. JAMA. 2020;323[22]:2265-67).
A recent meta-trial involving randomized controlled trials done across six countries compared prone positioning with standard care in patients with hypoxemic respiratory failure (defined as SpO2/ FiO2 < 315 and on high flow oxygen therapy) showed a reduced incidence of treatment failure and need for intubation without any signal of harm; although no mortality benefit was reported (Ehrmann S, et al. Lancet Respir Med. 2021 Aug 20;S2213-2600(21)00356-8). The number needed to treat to prevent one intubation was 14. While promising and reinforcing the safety of this relatively easy maneuver, several questions remain—which patients would benefit the most? Can it be applied within general wards safely? Does institution of awake proning delay intubation rates with consequent worse outcomes? Several ongoing (NCT 04402879) and completed studies (NCT 04383613 and NCT 04350723) may shed light on these important questions (Weatherald J, et al. Lancet Respir Med. 2021 Aug 20;S2213-2600[21]00368-4).
Sujith Cherian, MD, FCCP: Steering Committee Member
Interventional chest/diagnostic procedures
Endobronchial optical coherence tomography and interstitial lung diseases: Is the end near for surgical and transbronchial lung biopsies?
The early diagnosis of interstitial lung diseases (ILD) is paramount to initiating appropriate treatment and preventing irreversible pulmonary damage. Specific ILD subtypes may be diagnosed based on clinical evaluation, high resolution chest CT (HRCT) patterns, and serologic testing, but many patients require invasive procedures for histopathologic evaluation of lung tissue. Current modalities for obtaining tissue include transbronchial lung cryobiopsy (TBLC) and surgical lung biopsy (SLB), both of which carry a risk of potential complications (Troy LK, et al. Lancet Respir Med. 2020;8:171-81; Hutchinson JP, et al. Am J Respir Crit Care Med. 2016;193[10]:1161-7).
Recently, genomic classifiers applied to transbronchial biopsies have been proposed to facilitate the diagnosis of usual interstitial pneumonia (UIP), but the limited information provided still does not obviate the need for tissue diagnosis when needed (Raghu G, et al. Lancet Respir Med. 2019;7[6]:487-96). It is in this context that endobronchial optical coherence tomography (EB-OCT) was proposed as a real-time, in vivo, optical biopsy method for ILD.
EB-OCT uses near infrared light to generate large volumes of in-vivo three-dimensional tissue imaging with microscopic resolution (Goorsenberg A, et al. Respiration. 2020;99:190-205; Nandy S, et al. Am J Respir Crit Care Med. 2021;article in press). The OCT catheter is advanced through the bronchoscope working channel and can be used during outpatient procedures under conscious sedation. Available data suggests that minimal training is necessary, both for proceduralists and interpreting pathologists, but this will need to be confirmed in larger studies and various practice settings. Early studies suggest that OCT can identify microscopic honeycombing and other abnormalities even before they are evident on HRCT scans (Goorsenberg A, et al. Respiration. 2020;99:190-205). Newer research comparing ILD diagnosis from EB-OCT cross-sectional images with that obtained from SLB specimens revealed EB-OCT can distinguish UIP from non-UIP ILD with high sensitivity and specificity (Nandy S, et al. Am J Respir Crit Care Med. 2021;article in press). Could this mean the end of SLB and TBLC for the diagnosis of ILD? While the ability to diagnose ILD subtypes with high reliability and low risk of complications is certainly promising, studies remain admittedly small and the technique itself is only available to highly select individuals and specialized ILD centers. Let’s not pack up the cryoprobe just yet.
Audra J. Schwalk, MD, MBA: Steering Committee Member
Fabien Maldonado, MD, FCCP: Steering Committee Member
Pediatric chest medicine
Challenges in the pediatric pulmonary workforce
The future of the pediatric workforce has been the source of extensive discussion within the pediatric community and resulted in a considerable body of medical literature (Vinci RJ. Pediatrics. 2021;147[6]:e2020013292). In pediatric pulmonology, there is growing concern that current trends will lead to a workforce shortage resulting in patients having difficulty accessing subspecialty care (Harris C, et al. Pediatric Pulmonol. 2019;54[4]:444-50). The etiology of this shortage is multifactorial. Duration of fellowship training and subsequent financial implications are reported potential barriers to pursuing a fellowship (Nelson BA, et al. Pediatric Pulmonol. 2020;1-7). Discrepancies between pediatric and adult compensation may be another barrier. Insightful recruitment strategies based on the results of a recent study included maximizing resident interaction with pulmonary faculty, early identification and support of interested trainees, and consideration of flexible training models (Nelson BA, et al. ATS Sch. 2020;1:372-83). Lifestyle has also been a factor that contributes to a trainee’s decision to go into pediatric pulmonology (Freed GL, et al. Pediatrics. 2009;123(suppl 1):S31‐S37).
As our field addresses the critical need to recruit more trainees in light of the unfilled fellowship positions and the increasing average age of members of the field, we should not underestimate the prevalence of systemic racism and bias in medicine (Chiel L, et al. ATS Sch. 2020;1[4]:337-39) nor gender discrimination. Instead, we should seize the opportunity to understand and knock down barriers that trainees who are underrepresented in medicine face in pursuing pediatric subspecialty careers and build upon the excellent recent body of literature in this field to help recruit, support , and grow a robust, diverse workforce to provide the best pediatric care to all.
Anne C. Coates, MD – Steering Committee Member
Pulmonary vascular disease
Cascade testing in PAH: Is there a role?
Pediatric guidelines for pulmonary arterial hypertension (PAH) recommends genetic screening as a part of the evaluation for the newly diagnosed, with expansion to first-degree relatives as indicated. Currently, this is not mandated, and implementation is variable. In adults, genetic screening is not routinely offered, and family screening is rare. This reflects a lack of definitive guidelines (Abman SH, et al. Circulation. 2015:24;132[21]:2037-99). However, it is intuitive that if carriers are not identified by screening, they will come to attention after pulmonary vascular disease burden causes symptoms and affects outcomes.
Cascade testing is a screening methodology that is used in heritable cancers (George RM, et al. Genet Couns. 2015;24[3]:388-99). In cascade testing, identification of an index case prompts screening of at-risk family members. If these relatives are positive for mutations, the cycle is repeated (cascaded) to their immediate relatives, allowing for targeted screening. This approach is especially effective in genetic mutations that are inherited in an autosomal dominant fashion, such as in BMPR2 gene mutation. Cascade testing is an effective way to capture relatives who would otherwise be overlooked.
Unfortunately, in the United States, the cost of genetic testing is a significant obstacle to universal implementation. A new diagnosis of heritable pulmonary arterial hypertension (HPAH) is often followed by a multigene panel with costs exceeding $1000 and may prompt subsequent targeted testing resulting in additional expense (Chung WK, et al. Can J Cardiol. 2015;31[4]:544-47). Furthermore, a positive mutation detected on screening is not definitively associated with disease due to variable penetrance (Morrell NW, et al. Eur Respir J. 2019;53[1]:1801899]. As such, mass screening strategies are not recommended. The recent DELPHI-2 study [Montani D, et al. Eur Respir J. 2021;58[1]:2004229) have demonstrated that genetic screening is impactful in families with HPAH. A genetic screening algorithm should be considered, and cascade testing could be a cost-effective targeted approach.
Sandeep Sahay, MD, MSc, FCCP: Steering Committee Member
Jean M. Elwing, MD, FCCP: Chair
Pulmonary physiology, function, and rehabilitation network
Physiological benefits of awake proning: Its role and relevance in the COVID-19 pandemic
The advent of the COVID-19 pandemic has put a significant strain on the health care systems and critical care services across several countries, including the United States. Amidst this, several concerted efforts to reduce the need for mechanical ventilation has resulted in the emergence of awake proning as a strategy to improve oxygenation, which has been instituted in critical care units, in-patient settings, as well as in EDs. Although the evidence on this strategy has been vastly limited to case series and observational studies, several societies have incorporated awake proning as an initial management strategy in hypoxemic respiratory failure within their clinical guidelines (Chalmers JD, et al. Eur Respir J. 2021;57:2100048; Koeckerling D, et al. Thorax. 2020;75:833-4) and consensus statements (Nasa P, et al. Crit Care. 2021;25:106).
Physiological benefits of awake proning include improvement in ventilation-perfusion matching secondary to relative increase in ventilation in dorsal nondependent areas in the setting of higher density of perfusion within these units, thus reducing shunt and, hence, improving oxygenation. Other physiological mechanisms include homogenization of transpulmonary pressures, reduction of ventilator-induced lung injury (VILI) or patient self-inflicted lung injury (P-SILI), and possibly lung injury from pendelluft (Telias I, et al. JAMA. 2020;323[22]:2265-67).
A recent meta-trial involving randomized controlled trials done across six countries compared prone positioning with standard care in patients with hypoxemic respiratory failure (defined as SpO2/ FiO2 < 315 and on high flow oxygen therapy) showed a reduced incidence of treatment failure and need for intubation without any signal of harm; although no mortality benefit was reported (Ehrmann S, et al. Lancet Respir Med. 2021 Aug 20;S2213-2600(21)00356-8). The number needed to treat to prevent one intubation was 14. While promising and reinforcing the safety of this relatively easy maneuver, several questions remain—which patients would benefit the most? Can it be applied within general wards safely? Does institution of awake proning delay intubation rates with consequent worse outcomes? Several ongoing (NCT 04402879) and completed studies (NCT 04383613 and NCT 04350723) may shed light on these important questions (Weatherald J, et al. Lancet Respir Med. 2021 Aug 20;S2213-2600[21]00368-4).
Sujith Cherian, MD, FCCP: Steering Committee Member
Interventional chest/diagnostic procedures
Endobronchial optical coherence tomography and interstitial lung diseases: Is the end near for surgical and transbronchial lung biopsies?
The early diagnosis of interstitial lung diseases (ILD) is paramount to initiating appropriate treatment and preventing irreversible pulmonary damage. Specific ILD subtypes may be diagnosed based on clinical evaluation, high resolution chest CT (HRCT) patterns, and serologic testing, but many patients require invasive procedures for histopathologic evaluation of lung tissue. Current modalities for obtaining tissue include transbronchial lung cryobiopsy (TBLC) and surgical lung biopsy (SLB), both of which carry a risk of potential complications (Troy LK, et al. Lancet Respir Med. 2020;8:171-81; Hutchinson JP, et al. Am J Respir Crit Care Med. 2016;193[10]:1161-7).
Recently, genomic classifiers applied to transbronchial biopsies have been proposed to facilitate the diagnosis of usual interstitial pneumonia (UIP), but the limited information provided still does not obviate the need for tissue diagnosis when needed (Raghu G, et al. Lancet Respir Med. 2019;7[6]:487-96). It is in this context that endobronchial optical coherence tomography (EB-OCT) was proposed as a real-time, in vivo, optical biopsy method for ILD.
EB-OCT uses near infrared light to generate large volumes of in-vivo three-dimensional tissue imaging with microscopic resolution (Goorsenberg A, et al. Respiration. 2020;99:190-205; Nandy S, et al. Am J Respir Crit Care Med. 2021;article in press). The OCT catheter is advanced through the bronchoscope working channel and can be used during outpatient procedures under conscious sedation. Available data suggests that minimal training is necessary, both for proceduralists and interpreting pathologists, but this will need to be confirmed in larger studies and various practice settings. Early studies suggest that OCT can identify microscopic honeycombing and other abnormalities even before they are evident on HRCT scans (Goorsenberg A, et al. Respiration. 2020;99:190-205). Newer research comparing ILD diagnosis from EB-OCT cross-sectional images with that obtained from SLB specimens revealed EB-OCT can distinguish UIP from non-UIP ILD with high sensitivity and specificity (Nandy S, et al. Am J Respir Crit Care Med. 2021;article in press). Could this mean the end of SLB and TBLC for the diagnosis of ILD? While the ability to diagnose ILD subtypes with high reliability and low risk of complications is certainly promising, studies remain admittedly small and the technique itself is only available to highly select individuals and specialized ILD centers. Let’s not pack up the cryoprobe just yet.
Audra J. Schwalk, MD, MBA: Steering Committee Member
Fabien Maldonado, MD, FCCP: Steering Committee Member
Pediatric chest medicine
Challenges in the pediatric pulmonary workforce
The future of the pediatric workforce has been the source of extensive discussion within the pediatric community and resulted in a considerable body of medical literature (Vinci RJ. Pediatrics. 2021;147[6]:e2020013292). In pediatric pulmonology, there is growing concern that current trends will lead to a workforce shortage resulting in patients having difficulty accessing subspecialty care (Harris C, et al. Pediatric Pulmonol. 2019;54[4]:444-50). The etiology of this shortage is multifactorial. Duration of fellowship training and subsequent financial implications are reported potential barriers to pursuing a fellowship (Nelson BA, et al. Pediatric Pulmonol. 2020;1-7). Discrepancies between pediatric and adult compensation may be another barrier. Insightful recruitment strategies based on the results of a recent study included maximizing resident interaction with pulmonary faculty, early identification and support of interested trainees, and consideration of flexible training models (Nelson BA, et al. ATS Sch. 2020;1:372-83). Lifestyle has also been a factor that contributes to a trainee’s decision to go into pediatric pulmonology (Freed GL, et al. Pediatrics. 2009;123(suppl 1):S31‐S37).
As our field addresses the critical need to recruit more trainees in light of the unfilled fellowship positions and the increasing average age of members of the field, we should not underestimate the prevalence of systemic racism and bias in medicine (Chiel L, et al. ATS Sch. 2020;1[4]:337-39) nor gender discrimination. Instead, we should seize the opportunity to understand and knock down barriers that trainees who are underrepresented in medicine face in pursuing pediatric subspecialty careers and build upon the excellent recent body of literature in this field to help recruit, support , and grow a robust, diverse workforce to provide the best pediatric care to all.
Anne C. Coates, MD – Steering Committee Member
Pulmonary vascular disease
Cascade testing in PAH: Is there a role?
Pediatric guidelines for pulmonary arterial hypertension (PAH) recommends genetic screening as a part of the evaluation for the newly diagnosed, with expansion to first-degree relatives as indicated. Currently, this is not mandated, and implementation is variable. In adults, genetic screening is not routinely offered, and family screening is rare. This reflects a lack of definitive guidelines (Abman SH, et al. Circulation. 2015:24;132[21]:2037-99). However, it is intuitive that if carriers are not identified by screening, they will come to attention after pulmonary vascular disease burden causes symptoms and affects outcomes.
Cascade testing is a screening methodology that is used in heritable cancers (George RM, et al. Genet Couns. 2015;24[3]:388-99). In cascade testing, identification of an index case prompts screening of at-risk family members. If these relatives are positive for mutations, the cycle is repeated (cascaded) to their immediate relatives, allowing for targeted screening. This approach is especially effective in genetic mutations that are inherited in an autosomal dominant fashion, such as in BMPR2 gene mutation. Cascade testing is an effective way to capture relatives who would otherwise be overlooked.
Unfortunately, in the United States, the cost of genetic testing is a significant obstacle to universal implementation. A new diagnosis of heritable pulmonary arterial hypertension (HPAH) is often followed by a multigene panel with costs exceeding $1000 and may prompt subsequent targeted testing resulting in additional expense (Chung WK, et al. Can J Cardiol. 2015;31[4]:544-47). Furthermore, a positive mutation detected on screening is not definitively associated with disease due to variable penetrance (Morrell NW, et al. Eur Respir J. 2019;53[1]:1801899]. As such, mass screening strategies are not recommended. The recent DELPHI-2 study [Montani D, et al. Eur Respir J. 2021;58[1]:2004229) have demonstrated that genetic screening is impactful in families with HPAH. A genetic screening algorithm should be considered, and cascade testing could be a cost-effective targeted approach.
Sandeep Sahay, MD, MSc, FCCP: Steering Committee Member
Jean M. Elwing, MD, FCCP: Chair
Pulmonary physiology, function, and rehabilitation network
Physiological benefits of awake proning: Its role and relevance in the COVID-19 pandemic
The advent of the COVID-19 pandemic has put a significant strain on the health care systems and critical care services across several countries, including the United States. Amidst this, several concerted efforts to reduce the need for mechanical ventilation has resulted in the emergence of awake proning as a strategy to improve oxygenation, which has been instituted in critical care units, in-patient settings, as well as in EDs. Although the evidence on this strategy has been vastly limited to case series and observational studies, several societies have incorporated awake proning as an initial management strategy in hypoxemic respiratory failure within their clinical guidelines (Chalmers JD, et al. Eur Respir J. 2021;57:2100048; Koeckerling D, et al. Thorax. 2020;75:833-4) and consensus statements (Nasa P, et al. Crit Care. 2021;25:106).
Physiological benefits of awake proning include improvement in ventilation-perfusion matching secondary to relative increase in ventilation in dorsal nondependent areas in the setting of higher density of perfusion within these units, thus reducing shunt and, hence, improving oxygenation. Other physiological mechanisms include homogenization of transpulmonary pressures, reduction of ventilator-induced lung injury (VILI) or patient self-inflicted lung injury (P-SILI), and possibly lung injury from pendelluft (Telias I, et al. JAMA. 2020;323[22]:2265-67).
A recent meta-trial involving randomized controlled trials done across six countries compared prone positioning with standard care in patients with hypoxemic respiratory failure (defined as SpO2/ FiO2 < 315 and on high flow oxygen therapy) showed a reduced incidence of treatment failure and need for intubation without any signal of harm; although no mortality benefit was reported (Ehrmann S, et al. Lancet Respir Med. 2021 Aug 20;S2213-2600(21)00356-8). The number needed to treat to prevent one intubation was 14. While promising and reinforcing the safety of this relatively easy maneuver, several questions remain—which patients would benefit the most? Can it be applied within general wards safely? Does institution of awake proning delay intubation rates with consequent worse outcomes? Several ongoing (NCT 04402879) and completed studies (NCT 04383613 and NCT 04350723) may shed light on these important questions (Weatherald J, et al. Lancet Respir Med. 2021 Aug 20;S2213-2600[21]00368-4).
Sujith Cherian, MD, FCCP: Steering Committee Member
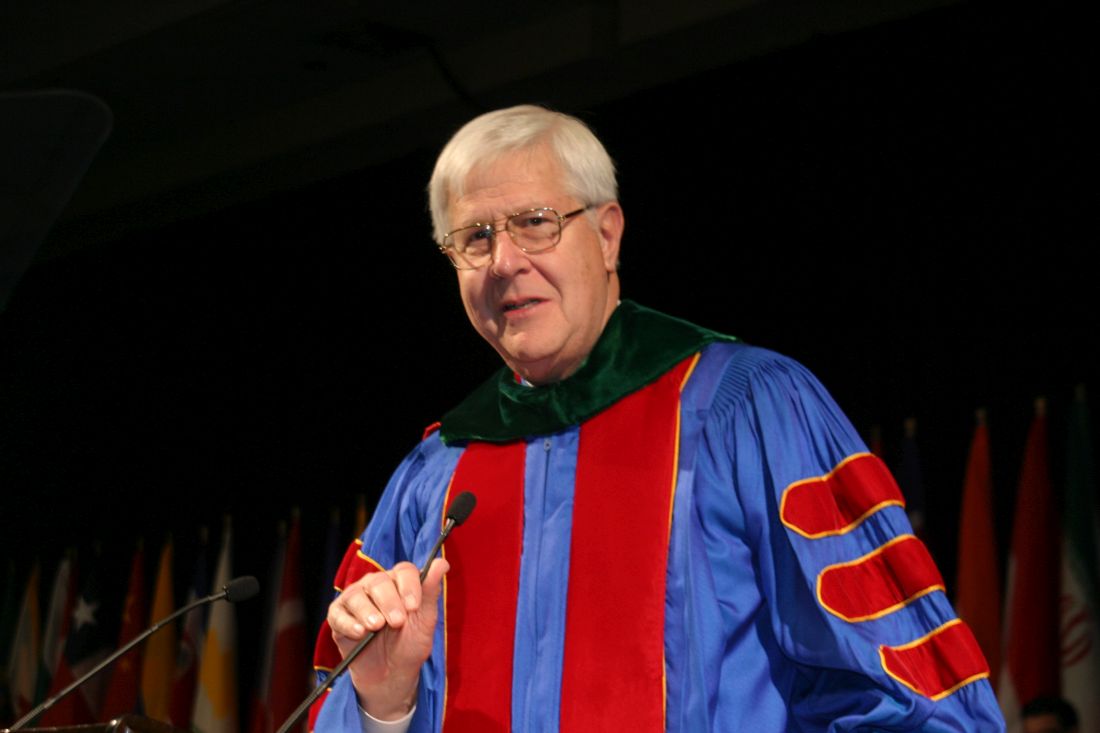
Thoughts on becoming CHEST President
I am honored to have the privilege of serving as the 84th President of the American College of Chest Physicians. When I attended my first CHEST meeting, I sat in the opening plenary session with thousands of other members, never imagining that I would have the opportunity to lead the organization just two decades later. And while I don’t recall many sessions from that meeting, I vividly remember the way it made an emotional impact. I never felt like one of a drove of nameless learners; both faculty and staff made it a collegial experience, much like attending pulmonary grand rounds at my own institution. Speakers would stay after their presentations to answer questions from even the most junior members. Leadership made themselves available over coffee or in the hallways between sessions. And that experience was the first of a great many memorable interactions I have had with CHEST.
CHEST has meant a great deal to me personally; it served as my first professional home away from home. I had the opportunity to grow in a number of different areas through my service to CHEST, in ways that I would not have been able to do easily at my own institution. I’ve worked with incredible staff and volunteers in my service on a number of our committees, including the Council of NetWorks, the Training and Transitions Committee, the Education Committee, and the Program Committee, to name a few. While I’ve had a chance to learn what role each of these component parts of the College serves during my tenure on those committees, it wasn’t until far more recently that I better understood the role of the President. Before I get into what I’d like to achieve during my year as President, I’d like to briefly review what that role entails.
Contrary to popular belief, the President does not set the organizational goals for CHEST; those are set by the Board of Regents. While I will have the privilege of running the Board meetings, it is the seventeen incredibly talented folks who serve as voting members of the Board that set the College’s direction. Once the organizational goals are set, it is our committees that take charge of designing and implementing plans to work toward those goals. Concomitantly, Dr. Robert Musacchio (CHEST chief executive officer and executive vice president) meets with his own executive leadership team to design a structure that lets the CHEST staff work, both on their own and in tandem with our members, to achieve these goals. One of the President’s main roles, as I see it, is to serve as a liaison. When the Board makes decisions that affect the membership, it will be my job to communicate changes and why they are being made. When our members have challenges that the College might be able to help solve, it is my role to work with the Board and the CEO to see what we can do about them. And when there is need to interface with other organizations, the President (or their designee) can speak on behalf of the College in those interactions.
In the context of those duties, what are the things that I would like to accomplish during my tenure as CHEST president? First, I want to spend more time with our committees and you, our members. CHEST is a member-focused organization; I believe that this is the main thing that sets our professional society apart from its sister societies. I have always found CHEST to be very collegial and welcoming. But I am aware that some of our members haven’t always found it accessible. And I get that; our structure is complex. That’s the reason I provided a description of my role, and the reason that I intend to spend time making CHEST more accessible to all of you. We’ve already developed dedicated social media channels for a number of our NetWorks in order to make you all more aware of their activities. In the coming year, I’ll provide regular updates to membership about ongoing CHEST activities. I’ll work to provide more member awareness of what role each of our committees plays in forwarding the College’s goals. And I’ll provide you with more information about the type of qualifications that each committee seeks in its nominees, in an effort to encourage you to run for a leadership position that best suits your interests and skill set.
While improving our members’ understanding of the inner workings at CHEST will help each of you better see how the College can meet your needs, my hope is that this increase in organizational accessibility will motivate each of you to engage more actively with us. This is my second goal as President. For some of you, that engagement may take the form of joining our Twitter chats; for others, it could mean attending one of our live learning courses in Chicago for the first time. But I hope that some of you will consider submitting session proposals to our annual meeting for the first time, or running for an available leadership position within the College when nominations open in the Spring.
As our organization grows (now almost twenty thousand members strong!), I want to provide a second home for all our members, spanning the range from medical students to full professors, from lifelong academic physicians to those just starting out in community practices, from busy clinicians to physician scientists, and including all members of the healthcare team. Although the makeup of our volunteer leadership is becoming more representative of the full breadth of our membership, we are not fully there yet. Until we get to that intended target, I would like to ask each of you to reach out to me with any thoughts about how CHEST can better meet your professional needs. Creating greater access to leadership to let each of your opinions be heard is my third goal as President of CHEST. I’ll provide more details about how I’m hoping to achieve this in the coming months.
The world has been a crazy place over the last eighteen months, filled with challenges that we could never have foreseen even a year prior. Our members have been on the front lines of the pandemic; in addition to the professional stresses related to caring for innumerable critically ill patients, many of us have suffered personal losses. Although none of us knows what 2022 holds, I look forward to a brighter future, knowing that regardless of what the coming year brings, we will face it together.
I am honored to have the privilege of serving as the 84th President of the American College of Chest Physicians. When I attended my first CHEST meeting, I sat in the opening plenary session with thousands of other members, never imagining that I would have the opportunity to lead the organization just two decades later. And while I don’t recall many sessions from that meeting, I vividly remember the way it made an emotional impact. I never felt like one of a drove of nameless learners; both faculty and staff made it a collegial experience, much like attending pulmonary grand rounds at my own institution. Speakers would stay after their presentations to answer questions from even the most junior members. Leadership made themselves available over coffee or in the hallways between sessions. And that experience was the first of a great many memorable interactions I have had with CHEST.
CHEST has meant a great deal to me personally; it served as my first professional home away from home. I had the opportunity to grow in a number of different areas through my service to CHEST, in ways that I would not have been able to do easily at my own institution. I’ve worked with incredible staff and volunteers in my service on a number of our committees, including the Council of NetWorks, the Training and Transitions Committee, the Education Committee, and the Program Committee, to name a few. While I’ve had a chance to learn what role each of these component parts of the College serves during my tenure on those committees, it wasn’t until far more recently that I better understood the role of the President. Before I get into what I’d like to achieve during my year as President, I’d like to briefly review what that role entails.
Contrary to popular belief, the President does not set the organizational goals for CHEST; those are set by the Board of Regents. While I will have the privilege of running the Board meetings, it is the seventeen incredibly talented folks who serve as voting members of the Board that set the College’s direction. Once the organizational goals are set, it is our committees that take charge of designing and implementing plans to work toward those goals. Concomitantly, Dr. Robert Musacchio (CHEST chief executive officer and executive vice president) meets with his own executive leadership team to design a structure that lets the CHEST staff work, both on their own and in tandem with our members, to achieve these goals. One of the President’s main roles, as I see it, is to serve as a liaison. When the Board makes decisions that affect the membership, it will be my job to communicate changes and why they are being made. When our members have challenges that the College might be able to help solve, it is my role to work with the Board and the CEO to see what we can do about them. And when there is need to interface with other organizations, the President (or their designee) can speak on behalf of the College in those interactions.
In the context of those duties, what are the things that I would like to accomplish during my tenure as CHEST president? First, I want to spend more time with our committees and you, our members. CHEST is a member-focused organization; I believe that this is the main thing that sets our professional society apart from its sister societies. I have always found CHEST to be very collegial and welcoming. But I am aware that some of our members haven’t always found it accessible. And I get that; our structure is complex. That’s the reason I provided a description of my role, and the reason that I intend to spend time making CHEST more accessible to all of you. We’ve already developed dedicated social media channels for a number of our NetWorks in order to make you all more aware of their activities. In the coming year, I’ll provide regular updates to membership about ongoing CHEST activities. I’ll work to provide more member awareness of what role each of our committees plays in forwarding the College’s goals. And I’ll provide you with more information about the type of qualifications that each committee seeks in its nominees, in an effort to encourage you to run for a leadership position that best suits your interests and skill set.
While improving our members’ understanding of the inner workings at CHEST will help each of you better see how the College can meet your needs, my hope is that this increase in organizational accessibility will motivate each of you to engage more actively with us. This is my second goal as President. For some of you, that engagement may take the form of joining our Twitter chats; for others, it could mean attending one of our live learning courses in Chicago for the first time. But I hope that some of you will consider submitting session proposals to our annual meeting for the first time, or running for an available leadership position within the College when nominations open in the Spring.
As our organization grows (now almost twenty thousand members strong!), I want to provide a second home for all our members, spanning the range from medical students to full professors, from lifelong academic physicians to those just starting out in community practices, from busy clinicians to physician scientists, and including all members of the healthcare team. Although the makeup of our volunteer leadership is becoming more representative of the full breadth of our membership, we are not fully there yet. Until we get to that intended target, I would like to ask each of you to reach out to me with any thoughts about how CHEST can better meet your professional needs. Creating greater access to leadership to let each of your opinions be heard is my third goal as President of CHEST. I’ll provide more details about how I’m hoping to achieve this in the coming months.
The world has been a crazy place over the last eighteen months, filled with challenges that we could never have foreseen even a year prior. Our members have been on the front lines of the pandemic; in addition to the professional stresses related to caring for innumerable critically ill patients, many of us have suffered personal losses. Although none of us knows what 2022 holds, I look forward to a brighter future, knowing that regardless of what the coming year brings, we will face it together.
I am honored to have the privilege of serving as the 84th President of the American College of Chest Physicians. When I attended my first CHEST meeting, I sat in the opening plenary session with thousands of other members, never imagining that I would have the opportunity to lead the organization just two decades later. And while I don’t recall many sessions from that meeting, I vividly remember the way it made an emotional impact. I never felt like one of a drove of nameless learners; both faculty and staff made it a collegial experience, much like attending pulmonary grand rounds at my own institution. Speakers would stay after their presentations to answer questions from even the most junior members. Leadership made themselves available over coffee or in the hallways between sessions. And that experience was the first of a great many memorable interactions I have had with CHEST.
CHEST has meant a great deal to me personally; it served as my first professional home away from home. I had the opportunity to grow in a number of different areas through my service to CHEST, in ways that I would not have been able to do easily at my own institution. I’ve worked with incredible staff and volunteers in my service on a number of our committees, including the Council of NetWorks, the Training and Transitions Committee, the Education Committee, and the Program Committee, to name a few. While I’ve had a chance to learn what role each of these component parts of the College serves during my tenure on those committees, it wasn’t until far more recently that I better understood the role of the President. Before I get into what I’d like to achieve during my year as President, I’d like to briefly review what that role entails.
Contrary to popular belief, the President does not set the organizational goals for CHEST; those are set by the Board of Regents. While I will have the privilege of running the Board meetings, it is the seventeen incredibly talented folks who serve as voting members of the Board that set the College’s direction. Once the organizational goals are set, it is our committees that take charge of designing and implementing plans to work toward those goals. Concomitantly, Dr. Robert Musacchio (CHEST chief executive officer and executive vice president) meets with his own executive leadership team to design a structure that lets the CHEST staff work, both on their own and in tandem with our members, to achieve these goals. One of the President’s main roles, as I see it, is to serve as a liaison. When the Board makes decisions that affect the membership, it will be my job to communicate changes and why they are being made. When our members have challenges that the College might be able to help solve, it is my role to work with the Board and the CEO to see what we can do about them. And when there is need to interface with other organizations, the President (or their designee) can speak on behalf of the College in those interactions.
In the context of those duties, what are the things that I would like to accomplish during my tenure as CHEST president? First, I want to spend more time with our committees and you, our members. CHEST is a member-focused organization; I believe that this is the main thing that sets our professional society apart from its sister societies. I have always found CHEST to be very collegial and welcoming. But I am aware that some of our members haven’t always found it accessible. And I get that; our structure is complex. That’s the reason I provided a description of my role, and the reason that I intend to spend time making CHEST more accessible to all of you. We’ve already developed dedicated social media channels for a number of our NetWorks in order to make you all more aware of their activities. In the coming year, I’ll provide regular updates to membership about ongoing CHEST activities. I’ll work to provide more member awareness of what role each of our committees plays in forwarding the College’s goals. And I’ll provide you with more information about the type of qualifications that each committee seeks in its nominees, in an effort to encourage you to run for a leadership position that best suits your interests and skill set.
While improving our members’ understanding of the inner workings at CHEST will help each of you better see how the College can meet your needs, my hope is that this increase in organizational accessibility will motivate each of you to engage more actively with us. This is my second goal as President. For some of you, that engagement may take the form of joining our Twitter chats; for others, it could mean attending one of our live learning courses in Chicago for the first time. But I hope that some of you will consider submitting session proposals to our annual meeting for the first time, or running for an available leadership position within the College when nominations open in the Spring.
As our organization grows (now almost twenty thousand members strong!), I want to provide a second home for all our members, spanning the range from medical students to full professors, from lifelong academic physicians to those just starting out in community practices, from busy clinicians to physician scientists, and including all members of the healthcare team. Although the makeup of our volunteer leadership is becoming more representative of the full breadth of our membership, we are not fully there yet. Until we get to that intended target, I would like to ask each of you to reach out to me with any thoughts about how CHEST can better meet your professional needs. Creating greater access to leadership to let each of your opinions be heard is my third goal as President of CHEST. I’ll provide more details about how I’m hoping to achieve this in the coming months.
The world has been a crazy place over the last eighteen months, filled with challenges that we could never have foreseen even a year prior. Our members have been on the front lines of the pandemic; in addition to the professional stresses related to caring for innumerable critically ill patients, many of us have suffered personal losses. Although none of us knows what 2022 holds, I look forward to a brighter future, knowing that regardless of what the coming year brings, we will face it together.
This month in the journal CHEST®
Editor’s picks
How I do it: Transitioning asthma care from adolescents to adults: Severe Asthma Series. By Dr. A. Nanzer.
Outpatient management of patients with COVID-19: Multicenter prospective validation of the HOME-CoV Rule to safely discharge patients. By Dr. D. Douillet, et al.
Emphysema progression and lung function decline among angiotensin converting enzyme inhibitors (ACEi) and angiotensin-receptor blockade (ARB) users in the COPDGene Cohort. By Dr. V. Tejwani, et al.
Sarcoidosis: An occupational disease? By Dr. C.L. Oliver, et al.
Pulmonary thrombosis and thromboembolism in COVID-19. By Dr. H. Poor.
How I do it: Mediastinal staging for lung cancer. By Dr. F. Farjah, et al.
Editor’s picks
Editor’s picks
How I do it: Transitioning asthma care from adolescents to adults: Severe Asthma Series. By Dr. A. Nanzer.
Outpatient management of patients with COVID-19: Multicenter prospective validation of the HOME-CoV Rule to safely discharge patients. By Dr. D. Douillet, et al.
Emphysema progression and lung function decline among angiotensin converting enzyme inhibitors (ACEi) and angiotensin-receptor blockade (ARB) users in the COPDGene Cohort. By Dr. V. Tejwani, et al.
Sarcoidosis: An occupational disease? By Dr. C.L. Oliver, et al.
Pulmonary thrombosis and thromboembolism in COVID-19. By Dr. H. Poor.
How I do it: Mediastinal staging for lung cancer. By Dr. F. Farjah, et al.
How I do it: Transitioning asthma care from adolescents to adults: Severe Asthma Series. By Dr. A. Nanzer.
Outpatient management of patients with COVID-19: Multicenter prospective validation of the HOME-CoV Rule to safely discharge patients. By Dr. D. Douillet, et al.
Emphysema progression and lung function decline among angiotensin converting enzyme inhibitors (ACEi) and angiotensin-receptor blockade (ARB) users in the COPDGene Cohort. By Dr. V. Tejwani, et al.
Sarcoidosis: An occupational disease? By Dr. C.L. Oliver, et al.
Pulmonary thrombosis and thromboembolism in COVID-19. By Dr. H. Poor.
How I do it: Mediastinal staging for lung cancer. By Dr. F. Farjah, et al.
AGA Career Compass app
We’ve launched a new app designed to help AGA trainees and early career members navigate each step along their GI career path. Once users get started by setting up their professional profile, AGA Career Compass offers curated resources on topics like career planning, clinical education, and leadership skills.
The Connections Corner section hosts experienced mentors and matches them with users based on profile compatibility and shared topics of interest, such as grant writing, setting up a lab, navigating career options in academic medicine, managing burnout, and more. Download the app today to branch out from your institution or practice and receive personalized career guidance.
Now available in Apple and Google Play stores.
We’ve launched a new app designed to help AGA trainees and early career members navigate each step along their GI career path. Once users get started by setting up their professional profile, AGA Career Compass offers curated resources on topics like career planning, clinical education, and leadership skills.
The Connections Corner section hosts experienced mentors and matches them with users based on profile compatibility and shared topics of interest, such as grant writing, setting up a lab, navigating career options in academic medicine, managing burnout, and more. Download the app today to branch out from your institution or practice and receive personalized career guidance.
Now available in Apple and Google Play stores.
We’ve launched a new app designed to help AGA trainees and early career members navigate each step along their GI career path. Once users get started by setting up their professional profile, AGA Career Compass offers curated resources on topics like career planning, clinical education, and leadership skills.
The Connections Corner section hosts experienced mentors and matches them with users based on profile compatibility and shared topics of interest, such as grant writing, setting up a lab, navigating career options in academic medicine, managing burnout, and more. Download the app today to branch out from your institution or practice and receive personalized career guidance.
Now available in Apple and Google Play stores.
Top cases
Physicians with difficult patient scenarios regularly bring their questions to the AGA Community to seek advice from colleagues about therapy and disease management options, best practices, and diagnoses. Here’s a preview of a recent popular clinical discussion:
Junaid Beig, MBBS, FRACP wrote the following in “Subtherapeutic Azathioprine metabolites despite being adherent to medication”:
“I have an Ulcerative patient (Pancolitis) on Mesalazine and Azathioprine 150mg since 2018. His levels are subtherapeutic (6TGN 159 and 6MMP 70) despite being adherent to medication. He drinks 2 liters of wine per week.
“Questions: Is there any way we can find if he has high TPMT activity (Level is normal 6.1)? Does alcohol have an impact on TPMT activity? Does he warrant alternative treatment?”
See how AGA members responded and join the discussion: https://community.gastro.org/posts/25109.
Physicians with difficult patient scenarios regularly bring their questions to the AGA Community to seek advice from colleagues about therapy and disease management options, best practices, and diagnoses. Here’s a preview of a recent popular clinical discussion:
Junaid Beig, MBBS, FRACP wrote the following in “Subtherapeutic Azathioprine metabolites despite being adherent to medication”:
“I have an Ulcerative patient (Pancolitis) on Mesalazine and Azathioprine 150mg since 2018. His levels are subtherapeutic (6TGN 159 and 6MMP 70) despite being adherent to medication. He drinks 2 liters of wine per week.
“Questions: Is there any way we can find if he has high TPMT activity (Level is normal 6.1)? Does alcohol have an impact on TPMT activity? Does he warrant alternative treatment?”
See how AGA members responded and join the discussion: https://community.gastro.org/posts/25109.
Physicians with difficult patient scenarios regularly bring their questions to the AGA Community to seek advice from colleagues about therapy and disease management options, best practices, and diagnoses. Here’s a preview of a recent popular clinical discussion:
Junaid Beig, MBBS, FRACP wrote the following in “Subtherapeutic Azathioprine metabolites despite being adherent to medication”:
“I have an Ulcerative patient (Pancolitis) on Mesalazine and Azathioprine 150mg since 2018. His levels are subtherapeutic (6TGN 159 and 6MMP 70) despite being adherent to medication. He drinks 2 liters of wine per week.
“Questions: Is there any way we can find if he has high TPMT activity (Level is normal 6.1)? Does alcohol have an impact on TPMT activity? Does he warrant alternative treatment?”
See how AGA members responded and join the discussion: https://community.gastro.org/posts/25109.
Remember the past, be wary of the future
A Perspective on the intended Philip Morris International acquisition of Vectura
On July 9, Philip Morris International Inc. (PMI) issued a statement of intent to purchase Vectura Group plc (Vectura), a provider of inhaled drug delivery solutions. According to the statement, the acquisition contributes to the PMI goal to move “beyond nicotine” by leveraging Vectura’s expertise in inhalation and aerosolization into adjacent areas.
Given PMI’s strong ties to tobacco, the acquisition raises concerns across the medical field. D. Robert McCaffree, MD, Master FCCP, shares his thoughts on the prospective acquisition in the following guest feature.
August 2021: D. Robert McCaffree, MD, Master FCCP
In 2018, Dr. Neeraj Desai and I published an editorial in the journal CHEST®. The title was, in part, “Is Big Tobacco Still Trying to Deceive the Public? ... ”1 Before I give an opinion about the answer, I should give some background on events eliciting the editorial.
In 1999, the U.S. Department of Justice (DOJ) sued major tobacco companies (Philip Morris, USA; Altria; RJ Reynolds; and Lorillard) for being in violation of the Racketeer Influenced Corrupt Organization Act (RICO) in that they colluded for decades to mislead the public about the risks of smoking and risks of secondhand smoke, downplayed the addictiveness of nicotine, manipulated nicotine levels, marketed cigarettes as “low tar” or “light” when they knew these were no less hazardous than full-flavored cigarettes, purposefully targeted youth, and failed to produce a safer cigarette.
In 2006, Judge Gladys Kessler of the D.C. District Court issued a1 700-page opinion finding the defendants had violated RICO. In her words,
• “[This case] is about an industry, and in particular these defendants, that survives, and profits, from selling a highly addictive product which causes diseases that lead to ... [an] immeasurable amount of human suffering ... they have consistently, repeatedly and with enormous skill and sophistication, denied these facts to the public, the Government, and to the public health community.”
“Defendants have marketed and sold their lethal products with zeal, with deception, with a single-minded focus on their financial success, and without regard for the human tragedy ... exacted.”
• “Over the course of more than 50 years, defendants lied, misrepresented, and deceived the American public, including ... the young people they avidly sought as ‘replacement’ smokers.”
• “The evidence in this case clearly establishes that defendants have not ceased engaging in unlawful activity ... ”
Since, under RICO, the government could not recover monetary damages but only require corrective actions going forward, the court ordered them to publish “corrective statements” (five different ones in total) in major publications and on television during prime time over the course of several months, as well as at the point of sale. (They are still appealing the point-of-sale display.)
Of course, the defendants appealed, but those appeals were largely thwarted until the (almost) final order in 2017, which then led to our editorial in 2018.
While this is a rather long introduction, I thought it necessary to depict the long-standing nature and behavioral patterns of deception, distortion, and destructive behavior of this industry – all designed to maintain their incredible profits - before trying to answer the question posed in our editorial.
Since all of the above, is there evidence the industry’s behaviors have changed? On the negative side, there is a recent study published on the Tobacco Free Kids website documenting the past and continued marketing to women and girls, with all the adverse consequences to women’s health.2 The industry continues to produce and market cigarettes to everyone, including youths and focused markets such as Blacks and LGBTQ populations. However, they are quite aware that the future of combustible tobacco, the major source of their incredible profits, is threatened.
Currently, most of the profits from Philip Morris International (PMI), as well as the other major players, come from combustible products. But, the CEO of PMI has stated that he thinks combustible tobacco products will be gone in 10 to 15 years and PMI will be selling only smoke-free products by 2025. So, to preserve similar profits as their combustible products diminish, they have made major investments in vaping products, such as Juul, and development of other noncombustible tobacco products. But these are still addictive, and any reduction in health consequences is still being evaluated. A prime example of trying to change their image is Philip Morris’ Beyond Nicotine campaign. However, currently all the companies continue to produce combustible products in large amounts, both locally and internationally.
One way of assessing the vision of any company is to see where it is putting its money. Currently, all major tobacco companies are investing in marijuana companies. For example, Philip Morris has invested $2.4 billion into Cosmos, a Canadian marijuana company.
They also recently purchased Vectura, Fertin, and Kraft Foods. I know, it’s hard to see where Kraft Foods fits in here, but Vectura, an inhalational device manufacturer, and Fertin, which makes nicotine gum, as well as vehicles such as powders, pouches that dissolve in the mouth, and lozenges, certainly do fit in.
My take on these recent acquisitions is that tobacco companies realize combustibles are dying. However, they continue to develop and market nicotine in noncombustible forms. They are likely looking to move into marijuana, at least as an investment. It’s not a huge leap to consider the possibility that the purchase of Vectura will help develop delivery systems for nicotine, marijuana, and possibly medications. It’s unclear whether PMI intends to get further into inhaled pharmaceuticals.
Bottom line is that, as pulmonary physicians, we need to be aware of all developments in inhaled substances and delivery methods. On the upside, everything the industry is currently doing is apparently more transparent than they have been in the past. They are not yet, however, ceasing production and marketing of cigarettes.
It’s also important that we remind ourselves of their past actions because, personally, that past still bothers me, and I’m not quite ready to trust them. When it comes to “Big Tobacco,” it is appropriate that we always keep in mind the immortal words, often repeated in various forms, of Edgar Allen Poe, master teller of horror stories, “Believe nothing you hear and only half that you see.”3
References
1. McCaffree DR and Desai NR. Is big tobacco still trying to deceive the public? This is no time to rest on our laurels. Chest. 2018 May;153(5):1085-6. doi: 10.1016/j.chest.2018.01.012.
2. A lifetime of damage: How Big Tobacco’s predatory marketing practices harms the health of women and girls. Tobacco-Free Kids. May 2021.
3. Quote Investigator. 2017 Jun 23. “The system of Dr. Tarr and Prof. Fether,” from Graham’s Magazine, November 1845.
A Perspective on the intended Philip Morris International acquisition of Vectura
A Perspective on the intended Philip Morris International acquisition of Vectura
On July 9, Philip Morris International Inc. (PMI) issued a statement of intent to purchase Vectura Group plc (Vectura), a provider of inhaled drug delivery solutions. According to the statement, the acquisition contributes to the PMI goal to move “beyond nicotine” by leveraging Vectura’s expertise in inhalation and aerosolization into adjacent areas.
Given PMI’s strong ties to tobacco, the acquisition raises concerns across the medical field. D. Robert McCaffree, MD, Master FCCP, shares his thoughts on the prospective acquisition in the following guest feature.
August 2021: D. Robert McCaffree, MD, Master FCCP
In 2018, Dr. Neeraj Desai and I published an editorial in the journal CHEST®. The title was, in part, “Is Big Tobacco Still Trying to Deceive the Public? ... ”1 Before I give an opinion about the answer, I should give some background on events eliciting the editorial.
In 1999, the U.S. Department of Justice (DOJ) sued major tobacco companies (Philip Morris, USA; Altria; RJ Reynolds; and Lorillard) for being in violation of the Racketeer Influenced Corrupt Organization Act (RICO) in that they colluded for decades to mislead the public about the risks of smoking and risks of secondhand smoke, downplayed the addictiveness of nicotine, manipulated nicotine levels, marketed cigarettes as “low tar” or “light” when they knew these were no less hazardous than full-flavored cigarettes, purposefully targeted youth, and failed to produce a safer cigarette.
In 2006, Judge Gladys Kessler of the D.C. District Court issued a1 700-page opinion finding the defendants had violated RICO. In her words,
• “[This case] is about an industry, and in particular these defendants, that survives, and profits, from selling a highly addictive product which causes diseases that lead to ... [an] immeasurable amount of human suffering ... they have consistently, repeatedly and with enormous skill and sophistication, denied these facts to the public, the Government, and to the public health community.”
“Defendants have marketed and sold their lethal products with zeal, with deception, with a single-minded focus on their financial success, and without regard for the human tragedy ... exacted.”
• “Over the course of more than 50 years, defendants lied, misrepresented, and deceived the American public, including ... the young people they avidly sought as ‘replacement’ smokers.”
• “The evidence in this case clearly establishes that defendants have not ceased engaging in unlawful activity ... ”
Since, under RICO, the government could not recover monetary damages but only require corrective actions going forward, the court ordered them to publish “corrective statements” (five different ones in total) in major publications and on television during prime time over the course of several months, as well as at the point of sale. (They are still appealing the point-of-sale display.)
Of course, the defendants appealed, but those appeals were largely thwarted until the (almost) final order in 2017, which then led to our editorial in 2018.
While this is a rather long introduction, I thought it necessary to depict the long-standing nature and behavioral patterns of deception, distortion, and destructive behavior of this industry – all designed to maintain their incredible profits - before trying to answer the question posed in our editorial.
Since all of the above, is there evidence the industry’s behaviors have changed? On the negative side, there is a recent study published on the Tobacco Free Kids website documenting the past and continued marketing to women and girls, with all the adverse consequences to women’s health.2 The industry continues to produce and market cigarettes to everyone, including youths and focused markets such as Blacks and LGBTQ populations. However, they are quite aware that the future of combustible tobacco, the major source of their incredible profits, is threatened.
Currently, most of the profits from Philip Morris International (PMI), as well as the other major players, come from combustible products. But, the CEO of PMI has stated that he thinks combustible tobacco products will be gone in 10 to 15 years and PMI will be selling only smoke-free products by 2025. So, to preserve similar profits as their combustible products diminish, they have made major investments in vaping products, such as Juul, and development of other noncombustible tobacco products. But these are still addictive, and any reduction in health consequences is still being evaluated. A prime example of trying to change their image is Philip Morris’ Beyond Nicotine campaign. However, currently all the companies continue to produce combustible products in large amounts, both locally and internationally.
One way of assessing the vision of any company is to see where it is putting its money. Currently, all major tobacco companies are investing in marijuana companies. For example, Philip Morris has invested $2.4 billion into Cosmos, a Canadian marijuana company.
They also recently purchased Vectura, Fertin, and Kraft Foods. I know, it’s hard to see where Kraft Foods fits in here, but Vectura, an inhalational device manufacturer, and Fertin, which makes nicotine gum, as well as vehicles such as powders, pouches that dissolve in the mouth, and lozenges, certainly do fit in.
My take on these recent acquisitions is that tobacco companies realize combustibles are dying. However, they continue to develop and market nicotine in noncombustible forms. They are likely looking to move into marijuana, at least as an investment. It’s not a huge leap to consider the possibility that the purchase of Vectura will help develop delivery systems for nicotine, marijuana, and possibly medications. It’s unclear whether PMI intends to get further into inhaled pharmaceuticals.
Bottom line is that, as pulmonary physicians, we need to be aware of all developments in inhaled substances and delivery methods. On the upside, everything the industry is currently doing is apparently more transparent than they have been in the past. They are not yet, however, ceasing production and marketing of cigarettes.
It’s also important that we remind ourselves of their past actions because, personally, that past still bothers me, and I’m not quite ready to trust them. When it comes to “Big Tobacco,” it is appropriate that we always keep in mind the immortal words, often repeated in various forms, of Edgar Allen Poe, master teller of horror stories, “Believe nothing you hear and only half that you see.”3
References
1. McCaffree DR and Desai NR. Is big tobacco still trying to deceive the public? This is no time to rest on our laurels. Chest. 2018 May;153(5):1085-6. doi: 10.1016/j.chest.2018.01.012.
2. A lifetime of damage: How Big Tobacco’s predatory marketing practices harms the health of women and girls. Tobacco-Free Kids. May 2021.
3. Quote Investigator. 2017 Jun 23. “The system of Dr. Tarr and Prof. Fether,” from Graham’s Magazine, November 1845.
On July 9, Philip Morris International Inc. (PMI) issued a statement of intent to purchase Vectura Group plc (Vectura), a provider of inhaled drug delivery solutions. According to the statement, the acquisition contributes to the PMI goal to move “beyond nicotine” by leveraging Vectura’s expertise in inhalation and aerosolization into adjacent areas.
Given PMI’s strong ties to tobacco, the acquisition raises concerns across the medical field. D. Robert McCaffree, MD, Master FCCP, shares his thoughts on the prospective acquisition in the following guest feature.
August 2021: D. Robert McCaffree, MD, Master FCCP
In 2018, Dr. Neeraj Desai and I published an editorial in the journal CHEST®. The title was, in part, “Is Big Tobacco Still Trying to Deceive the Public? ... ”1 Before I give an opinion about the answer, I should give some background on events eliciting the editorial.
In 1999, the U.S. Department of Justice (DOJ) sued major tobacco companies (Philip Morris, USA; Altria; RJ Reynolds; and Lorillard) for being in violation of the Racketeer Influenced Corrupt Organization Act (RICO) in that they colluded for decades to mislead the public about the risks of smoking and risks of secondhand smoke, downplayed the addictiveness of nicotine, manipulated nicotine levels, marketed cigarettes as “low tar” or “light” when they knew these were no less hazardous than full-flavored cigarettes, purposefully targeted youth, and failed to produce a safer cigarette.
In 2006, Judge Gladys Kessler of the D.C. District Court issued a1 700-page opinion finding the defendants had violated RICO. In her words,
• “[This case] is about an industry, and in particular these defendants, that survives, and profits, from selling a highly addictive product which causes diseases that lead to ... [an] immeasurable amount of human suffering ... they have consistently, repeatedly and with enormous skill and sophistication, denied these facts to the public, the Government, and to the public health community.”
“Defendants have marketed and sold their lethal products with zeal, with deception, with a single-minded focus on their financial success, and without regard for the human tragedy ... exacted.”
• “Over the course of more than 50 years, defendants lied, misrepresented, and deceived the American public, including ... the young people they avidly sought as ‘replacement’ smokers.”
• “The evidence in this case clearly establishes that defendants have not ceased engaging in unlawful activity ... ”
Since, under RICO, the government could not recover monetary damages but only require corrective actions going forward, the court ordered them to publish “corrective statements” (five different ones in total) in major publications and on television during prime time over the course of several months, as well as at the point of sale. (They are still appealing the point-of-sale display.)
Of course, the defendants appealed, but those appeals were largely thwarted until the (almost) final order in 2017, which then led to our editorial in 2018.
While this is a rather long introduction, I thought it necessary to depict the long-standing nature and behavioral patterns of deception, distortion, and destructive behavior of this industry – all designed to maintain their incredible profits - before trying to answer the question posed in our editorial.
Since all of the above, is there evidence the industry’s behaviors have changed? On the negative side, there is a recent study published on the Tobacco Free Kids website documenting the past and continued marketing to women and girls, with all the adverse consequences to women’s health.2 The industry continues to produce and market cigarettes to everyone, including youths and focused markets such as Blacks and LGBTQ populations. However, they are quite aware that the future of combustible tobacco, the major source of their incredible profits, is threatened.
Currently, most of the profits from Philip Morris International (PMI), as well as the other major players, come from combustible products. But, the CEO of PMI has stated that he thinks combustible tobacco products will be gone in 10 to 15 years and PMI will be selling only smoke-free products by 2025. So, to preserve similar profits as their combustible products diminish, they have made major investments in vaping products, such as Juul, and development of other noncombustible tobacco products. But these are still addictive, and any reduction in health consequences is still being evaluated. A prime example of trying to change their image is Philip Morris’ Beyond Nicotine campaign. However, currently all the companies continue to produce combustible products in large amounts, both locally and internationally.
One way of assessing the vision of any company is to see where it is putting its money. Currently, all major tobacco companies are investing in marijuana companies. For example, Philip Morris has invested $2.4 billion into Cosmos, a Canadian marijuana company.
They also recently purchased Vectura, Fertin, and Kraft Foods. I know, it’s hard to see where Kraft Foods fits in here, but Vectura, an inhalational device manufacturer, and Fertin, which makes nicotine gum, as well as vehicles such as powders, pouches that dissolve in the mouth, and lozenges, certainly do fit in.
My take on these recent acquisitions is that tobacco companies realize combustibles are dying. However, they continue to develop and market nicotine in noncombustible forms. They are likely looking to move into marijuana, at least as an investment. It’s not a huge leap to consider the possibility that the purchase of Vectura will help develop delivery systems for nicotine, marijuana, and possibly medications. It’s unclear whether PMI intends to get further into inhaled pharmaceuticals.
Bottom line is that, as pulmonary physicians, we need to be aware of all developments in inhaled substances and delivery methods. On the upside, everything the industry is currently doing is apparently more transparent than they have been in the past. They are not yet, however, ceasing production and marketing of cigarettes.
It’s also important that we remind ourselves of their past actions because, personally, that past still bothers me, and I’m not quite ready to trust them. When it comes to “Big Tobacco,” it is appropriate that we always keep in mind the immortal words, often repeated in various forms, of Edgar Allen Poe, master teller of horror stories, “Believe nothing you hear and only half that you see.”3
References
1. McCaffree DR and Desai NR. Is big tobacco still trying to deceive the public? This is no time to rest on our laurels. Chest. 2018 May;153(5):1085-6. doi: 10.1016/j.chest.2018.01.012.
2. A lifetime of damage: How Big Tobacco’s predatory marketing practices harms the health of women and girls. Tobacco-Free Kids. May 2021.
3. Quote Investigator. 2017 Jun 23. “The system of Dr. Tarr and Prof. Fether,” from Graham’s Magazine, November 1845.
In memoriam
Paul D. Stein, MD, Master FCCP
Past President (1992-1993) of the American College of Chest Physicians (CHEST), Dr. Paul D. Stein, Master FCCP, died on July 15, 2021, in Boynton Beach, Florida. His long career in cardiovascular research included monumental studies in pulmonary embolism, pulmonary hypertension, and valvular heart disease.
Dr. Stein was regarded as a world expert on pulmonary embolism. His contributions to medicine include hundreds of published articles, five books, and countless lectures that have given the world its current understanding of heart and pulmonary diseases. Throughout his almost 50 years as a member of CHEST, as Past President, and as a Master Fellow, Dr. Stein served the College graciously in these and many other leadership roles. We extend heartfelt condolences to the Stein family.
Editor’s Note: In 2016, Dr. Stein provided CHEST Physician with a wonderful update on his current activities. You can find it in the November 2016 issue on page 54.
Paul D. Stein, MD, Master FCCP
Past President (1992-1993) of the American College of Chest Physicians (CHEST), Dr. Paul D. Stein, Master FCCP, died on July 15, 2021, in Boynton Beach, Florida. His long career in cardiovascular research included monumental studies in pulmonary embolism, pulmonary hypertension, and valvular heart disease.
Dr. Stein was regarded as a world expert on pulmonary embolism. His contributions to medicine include hundreds of published articles, five books, and countless lectures that have given the world its current understanding of heart and pulmonary diseases. Throughout his almost 50 years as a member of CHEST, as Past President, and as a Master Fellow, Dr. Stein served the College graciously in these and many other leadership roles. We extend heartfelt condolences to the Stein family.
Editor’s Note: In 2016, Dr. Stein provided CHEST Physician with a wonderful update on his current activities. You can find it in the November 2016 issue on page 54.
Paul D. Stein, MD, Master FCCP
Past President (1992-1993) of the American College of Chest Physicians (CHEST), Dr. Paul D. Stein, Master FCCP, died on July 15, 2021, in Boynton Beach, Florida. His long career in cardiovascular research included monumental studies in pulmonary embolism, pulmonary hypertension, and valvular heart disease.
Dr. Stein was regarded as a world expert on pulmonary embolism. His contributions to medicine include hundreds of published articles, five books, and countless lectures that have given the world its current understanding of heart and pulmonary diseases. Throughout his almost 50 years as a member of CHEST, as Past President, and as a Master Fellow, Dr. Stein served the College graciously in these and many other leadership roles. We extend heartfelt condolences to the Stein family.
Editor’s Note: In 2016, Dr. Stein provided CHEST Physician with a wonderful update on his current activities. You can find it in the November 2016 issue on page 54.
2021 AMA Meeting of the AMA House of Delegates – Updates
The American Medical Association (AMA) conducted its June 2021 AMA Special Meeting of the AMA House of Delegates from June 11-16 virtually. Delegates from more than 170 societies (state societies, specialties, subspecialties, and uniformed services), comprised of nearly 700 physicians, residents, and medical students, gathered for the June 2021 AMA Special Meeting of the AMA House of Delegates (HOD) to consider a wide array of proposals.
CHEST is an active member, and through the HOD and Specialty and Service Society Caucus, CHEST has partnered with AMA and its sister societies to work with each other on important regulatory issues. Chest/Allergy Section Council (participants at this meeting were from the AAAAI, AAOA, AASM, ACAAI, ATS, CHEST, and SCCM) met before the proceedings of the House to discuss pending business. The meeting was hosted by the current CHEST/Allergy council chair Dr. Wesley Vander Ark (AMA Delegate AAOA) and Jami Lucas, CEO AAOA.
Brief updates on the Resolutions
Continuity of care of patients discharged from hospital settings (Adapted as a new policy)
The policy focuses on key issues around the continuity of care of patients. It includes protections of continuity of care for medical services and medications that are prescribed during patient hospitalizations, including when there are formulary or treatment coverage changes that have the potential to disrupt therapy following discharge.
Licensure and telehealth
The policy urges AMA to continue to support state efforts to expand physician licensure recognition across state lines in accordance with the standards and safeguards Coverage and Payment for Telemedicine. (New HOD Policy)
AMA to conduct or commission a study on the effect that telemedicine services have had on health insurance premiums, focusing on the differences between states that had telehealth payment parity provisions in effect prior to the pandemic vs those that did not, and report back at the 2021 Interim Meeting of the AMA House of Delegates. (Directive to Take Action). CHEST has taken an active role in supporting this resolution through advocating for telemedicine services and reimbursement, as well as leading the CHEST Clinician Matching Network that pairs volunteer doctors with hospitals based on their need throughout the country.
Vaccines (Adopted as a new policy)
The policy urges AMA to advocate for the prohibition of the use of patient/customer information collected by retail pharmacies for COVID-19 vaccination scheduling and/or the vaccine administration process for the purpose of commercial marketing or future patient recruiting purposes, especially any targeting based on medical history condition. AMA opposes the sale of medical history data and contact information accumulated through the scheduling or provision of government-funded vaccinations to third parties for use in marketing or advertising.
Additionally, as it relates to vaccines, CHEST has joined a joint society statement supporting a vaccine mandate for all health care workers.
Optimizing match outcomes (Directive to Take Action)
The policy urges AMA to encourage the Association of American Medical Colleges, American Association of Colleges of Osteopathic Medicine, National Resident Matching Program, and other key stakeholders to jointly create a no-fee, easily accessible clearinghouse of reliable and valid advice and tools for residency program applicants seeking cost-effective methods for applying to and successfully matching into residency.
Ensuring adequate health care resources to address the long COVID crisis and call for increased funding and research for post-viral syndromes
The policy directs AMA to support the development of an ICD-10 code or family of codes to recognize Post-Acute Sequelae of SARS-CoV-2 infection (“PASC” or “Long COVID”) and other novel post-viral syndromes as distinct diagnoses. (New HOD Policy). Further, the policy directs AMA to advocate for legislation to provide funding for research, prevention, control, and treatment of post-viral syndromes and long-term sequelae associated with viral infections, such as COVID-19 and AMA provide physicians and medical students with accurate and current information on post-viral syndromes and long-term sequelae associated with viral infections, such as COVID-19; and further that AMA collaborate with other medical and educational entities to promote education among patients about post-viral syndromes and long-term sequelae associated with viral infections, such as COVID-19, to minimize the harm and disability current and future patients face. (Directive to Take Action)
Medical misinformation in the age of social media (Directive to Take Action)
AMA encourage social media organizations to further strengthen their content moderation policies related to medical misinformation, including, but not limited to, enhanced content monitoring, augmentation of recommendation engines focused on false information, and stronger integration of verified health information. AMA should encourage social media organizations to recognize the spread of medical misinformation over dissemination networks and collaborate with relevant stakeholders, and work with public health agencies to establish relationships with journalists and news agencies to enhance the public reach in disseminating accurate medical information.
Promoting equity in global vaccine distribution
AMA call for the cooperation of all governments and international agencies to share data, research, and resources for the production and distribution of medicines, vaccines, and personal protective equipment (Directive to Take Action); and be it further, AMA promote and support efforts to supply COVID vaccines to 21health care agencies in other parts of the world to be administered to individuals who can’t afford them. (Directive to Take Action). AMA urge the US government to provide all possible assistance, including surplus vaccines and vaccines that have not had emergency use authorization, to the citizens of India and other countries in a similar situation in this humanitarian crisis (New HOD Policy).
CHEST has taken an active role in promoting equity in health care and vaccine distribution in partnership with the American Lung Association and the American Thoracic Society, including establishing a research grant program focused on this topic.
Addressing inflammatory and untruthful online ratings (Directive to Take Action)
AMA take action that would urge online review organizations to create internal mechanisms ensuring due process to physicians before the publication of negative reviews.
This is just a small sampling of the activities and more information, including reports from the various Councils, are available on the AMA website.
CHEST members interested in the AMA policy-making process may observe any AMA-HOD meeting or participate in the AMA’s democratic processes. Attendees will also be able to increase their knowledge and skills at no cost. They will also be able to connect with more than 1,500 peers and other meeting attendees from across the country. CHEST members with the time (there are two 5-day meetings each year) and interest are invited to apply to be an official CHEST delegate to the AMA. Contact Suzanne Sletto at [email protected] for details.
Delegates and alternate delegates to the House of Delegates (HOD) play a critical role in the democratic policy-making process that is the foundation of the AMA. Their role is multi-dimensional and includes:
- Advocacy for patients within the HOD to improve the health of the public and the health care system;
- Representation of the perspectives of their sponsoring organization to the HOD;
- Representation of their physician and medical student constituents in the decision-making process of the HOD;
- Representation of the AMA and its House of Delegates to member and nonmember physicians, medical associations, and others; and
- Solicitation of input from and provision of feedback to constituents.
Also, HOD delegates and alternate delegates are expected to foster a positive and useful two-way relationship between grassroots physicians and the CHEST leadership.
Dr. Desai is with the Chicago Chest Center and AMITA Health Suburban Lung Associates; and the Division of Pulmonary, Critical Care, Sleep and Allergy, University of Illinois at Chicago.
The American Medical Association (AMA) conducted its June 2021 AMA Special Meeting of the AMA House of Delegates from June 11-16 virtually. Delegates from more than 170 societies (state societies, specialties, subspecialties, and uniformed services), comprised of nearly 700 physicians, residents, and medical students, gathered for the June 2021 AMA Special Meeting of the AMA House of Delegates (HOD) to consider a wide array of proposals.
CHEST is an active member, and through the HOD and Specialty and Service Society Caucus, CHEST has partnered with AMA and its sister societies to work with each other on important regulatory issues. Chest/Allergy Section Council (participants at this meeting were from the AAAAI, AAOA, AASM, ACAAI, ATS, CHEST, and SCCM) met before the proceedings of the House to discuss pending business. The meeting was hosted by the current CHEST/Allergy council chair Dr. Wesley Vander Ark (AMA Delegate AAOA) and Jami Lucas, CEO AAOA.
Brief updates on the Resolutions
Continuity of care of patients discharged from hospital settings (Adapted as a new policy)
The policy focuses on key issues around the continuity of care of patients. It includes protections of continuity of care for medical services and medications that are prescribed during patient hospitalizations, including when there are formulary or treatment coverage changes that have the potential to disrupt therapy following discharge.
Licensure and telehealth
The policy urges AMA to continue to support state efforts to expand physician licensure recognition across state lines in accordance with the standards and safeguards Coverage and Payment for Telemedicine. (New HOD Policy)
AMA to conduct or commission a study on the effect that telemedicine services have had on health insurance premiums, focusing on the differences between states that had telehealth payment parity provisions in effect prior to the pandemic vs those that did not, and report back at the 2021 Interim Meeting of the AMA House of Delegates. (Directive to Take Action). CHEST has taken an active role in supporting this resolution through advocating for telemedicine services and reimbursement, as well as leading the CHEST Clinician Matching Network that pairs volunteer doctors with hospitals based on their need throughout the country.
Vaccines (Adopted as a new policy)
The policy urges AMA to advocate for the prohibition of the use of patient/customer information collected by retail pharmacies for COVID-19 vaccination scheduling and/or the vaccine administration process for the purpose of commercial marketing or future patient recruiting purposes, especially any targeting based on medical history condition. AMA opposes the sale of medical history data and contact information accumulated through the scheduling or provision of government-funded vaccinations to third parties for use in marketing or advertising.
Additionally, as it relates to vaccines, CHEST has joined a joint society statement supporting a vaccine mandate for all health care workers.
Optimizing match outcomes (Directive to Take Action)
The policy urges AMA to encourage the Association of American Medical Colleges, American Association of Colleges of Osteopathic Medicine, National Resident Matching Program, and other key stakeholders to jointly create a no-fee, easily accessible clearinghouse of reliable and valid advice and tools for residency program applicants seeking cost-effective methods for applying to and successfully matching into residency.
Ensuring adequate health care resources to address the long COVID crisis and call for increased funding and research for post-viral syndromes
The policy directs AMA to support the development of an ICD-10 code or family of codes to recognize Post-Acute Sequelae of SARS-CoV-2 infection (“PASC” or “Long COVID”) and other novel post-viral syndromes as distinct diagnoses. (New HOD Policy). Further, the policy directs AMA to advocate for legislation to provide funding for research, prevention, control, and treatment of post-viral syndromes and long-term sequelae associated with viral infections, such as COVID-19 and AMA provide physicians and medical students with accurate and current information on post-viral syndromes and long-term sequelae associated with viral infections, such as COVID-19; and further that AMA collaborate with other medical and educational entities to promote education among patients about post-viral syndromes and long-term sequelae associated with viral infections, such as COVID-19, to minimize the harm and disability current and future patients face. (Directive to Take Action)
Medical misinformation in the age of social media (Directive to Take Action)
AMA encourage social media organizations to further strengthen their content moderation policies related to medical misinformation, including, but not limited to, enhanced content monitoring, augmentation of recommendation engines focused on false information, and stronger integration of verified health information. AMA should encourage social media organizations to recognize the spread of medical misinformation over dissemination networks and collaborate with relevant stakeholders, and work with public health agencies to establish relationships with journalists and news agencies to enhance the public reach in disseminating accurate medical information.
Promoting equity in global vaccine distribution
AMA call for the cooperation of all governments and international agencies to share data, research, and resources for the production and distribution of medicines, vaccines, and personal protective equipment (Directive to Take Action); and be it further, AMA promote and support efforts to supply COVID vaccines to 21health care agencies in other parts of the world to be administered to individuals who can’t afford them. (Directive to Take Action). AMA urge the US government to provide all possible assistance, including surplus vaccines and vaccines that have not had emergency use authorization, to the citizens of India and other countries in a similar situation in this humanitarian crisis (New HOD Policy).
CHEST has taken an active role in promoting equity in health care and vaccine distribution in partnership with the American Lung Association and the American Thoracic Society, including establishing a research grant program focused on this topic.
Addressing inflammatory and untruthful online ratings (Directive to Take Action)
AMA take action that would urge online review organizations to create internal mechanisms ensuring due process to physicians before the publication of negative reviews.
This is just a small sampling of the activities and more information, including reports from the various Councils, are available on the AMA website.
CHEST members interested in the AMA policy-making process may observe any AMA-HOD meeting or participate in the AMA’s democratic processes. Attendees will also be able to increase their knowledge and skills at no cost. They will also be able to connect with more than 1,500 peers and other meeting attendees from across the country. CHEST members with the time (there are two 5-day meetings each year) and interest are invited to apply to be an official CHEST delegate to the AMA. Contact Suzanne Sletto at [email protected] for details.
Delegates and alternate delegates to the House of Delegates (HOD) play a critical role in the democratic policy-making process that is the foundation of the AMA. Their role is multi-dimensional and includes:
- Advocacy for patients within the HOD to improve the health of the public and the health care system;
- Representation of the perspectives of their sponsoring organization to the HOD;
- Representation of their physician and medical student constituents in the decision-making process of the HOD;
- Representation of the AMA and its House of Delegates to member and nonmember physicians, medical associations, and others; and
- Solicitation of input from and provision of feedback to constituents.
Also, HOD delegates and alternate delegates are expected to foster a positive and useful two-way relationship between grassroots physicians and the CHEST leadership.
Dr. Desai is with the Chicago Chest Center and AMITA Health Suburban Lung Associates; and the Division of Pulmonary, Critical Care, Sleep and Allergy, University of Illinois at Chicago.
The American Medical Association (AMA) conducted its June 2021 AMA Special Meeting of the AMA House of Delegates from June 11-16 virtually. Delegates from more than 170 societies (state societies, specialties, subspecialties, and uniformed services), comprised of nearly 700 physicians, residents, and medical students, gathered for the June 2021 AMA Special Meeting of the AMA House of Delegates (HOD) to consider a wide array of proposals.
CHEST is an active member, and through the HOD and Specialty and Service Society Caucus, CHEST has partnered with AMA and its sister societies to work with each other on important regulatory issues. Chest/Allergy Section Council (participants at this meeting were from the AAAAI, AAOA, AASM, ACAAI, ATS, CHEST, and SCCM) met before the proceedings of the House to discuss pending business. The meeting was hosted by the current CHEST/Allergy council chair Dr. Wesley Vander Ark (AMA Delegate AAOA) and Jami Lucas, CEO AAOA.
Brief updates on the Resolutions
Continuity of care of patients discharged from hospital settings (Adapted as a new policy)
The policy focuses on key issues around the continuity of care of patients. It includes protections of continuity of care for medical services and medications that are prescribed during patient hospitalizations, including when there are formulary or treatment coverage changes that have the potential to disrupt therapy following discharge.
Licensure and telehealth
The policy urges AMA to continue to support state efforts to expand physician licensure recognition across state lines in accordance with the standards and safeguards Coverage and Payment for Telemedicine. (New HOD Policy)
AMA to conduct or commission a study on the effect that telemedicine services have had on health insurance premiums, focusing on the differences between states that had telehealth payment parity provisions in effect prior to the pandemic vs those that did not, and report back at the 2021 Interim Meeting of the AMA House of Delegates. (Directive to Take Action). CHEST has taken an active role in supporting this resolution through advocating for telemedicine services and reimbursement, as well as leading the CHEST Clinician Matching Network that pairs volunteer doctors with hospitals based on their need throughout the country.
Vaccines (Adopted as a new policy)
The policy urges AMA to advocate for the prohibition of the use of patient/customer information collected by retail pharmacies for COVID-19 vaccination scheduling and/or the vaccine administration process for the purpose of commercial marketing or future patient recruiting purposes, especially any targeting based on medical history condition. AMA opposes the sale of medical history data and contact information accumulated through the scheduling or provision of government-funded vaccinations to third parties for use in marketing or advertising.
Additionally, as it relates to vaccines, CHEST has joined a joint society statement supporting a vaccine mandate for all health care workers.
Optimizing match outcomes (Directive to Take Action)
The policy urges AMA to encourage the Association of American Medical Colleges, American Association of Colleges of Osteopathic Medicine, National Resident Matching Program, and other key stakeholders to jointly create a no-fee, easily accessible clearinghouse of reliable and valid advice and tools for residency program applicants seeking cost-effective methods for applying to and successfully matching into residency.
Ensuring adequate health care resources to address the long COVID crisis and call for increased funding and research for post-viral syndromes
The policy directs AMA to support the development of an ICD-10 code or family of codes to recognize Post-Acute Sequelae of SARS-CoV-2 infection (“PASC” or “Long COVID”) and other novel post-viral syndromes as distinct diagnoses. (New HOD Policy). Further, the policy directs AMA to advocate for legislation to provide funding for research, prevention, control, and treatment of post-viral syndromes and long-term sequelae associated with viral infections, such as COVID-19 and AMA provide physicians and medical students with accurate and current information on post-viral syndromes and long-term sequelae associated with viral infections, such as COVID-19; and further that AMA collaborate with other medical and educational entities to promote education among patients about post-viral syndromes and long-term sequelae associated with viral infections, such as COVID-19, to minimize the harm and disability current and future patients face. (Directive to Take Action)
Medical misinformation in the age of social media (Directive to Take Action)
AMA encourage social media organizations to further strengthen their content moderation policies related to medical misinformation, including, but not limited to, enhanced content monitoring, augmentation of recommendation engines focused on false information, and stronger integration of verified health information. AMA should encourage social media organizations to recognize the spread of medical misinformation over dissemination networks and collaborate with relevant stakeholders, and work with public health agencies to establish relationships with journalists and news agencies to enhance the public reach in disseminating accurate medical information.
Promoting equity in global vaccine distribution
AMA call for the cooperation of all governments and international agencies to share data, research, and resources for the production and distribution of medicines, vaccines, and personal protective equipment (Directive to Take Action); and be it further, AMA promote and support efforts to supply COVID vaccines to 21health care agencies in other parts of the world to be administered to individuals who can’t afford them. (Directive to Take Action). AMA urge the US government to provide all possible assistance, including surplus vaccines and vaccines that have not had emergency use authorization, to the citizens of India and other countries in a similar situation in this humanitarian crisis (New HOD Policy).
CHEST has taken an active role in promoting equity in health care and vaccine distribution in partnership with the American Lung Association and the American Thoracic Society, including establishing a research grant program focused on this topic.
Addressing inflammatory and untruthful online ratings (Directive to Take Action)
AMA take action that would urge online review organizations to create internal mechanisms ensuring due process to physicians before the publication of negative reviews.
This is just a small sampling of the activities and more information, including reports from the various Councils, are available on the AMA website.
CHEST members interested in the AMA policy-making process may observe any AMA-HOD meeting or participate in the AMA’s democratic processes. Attendees will also be able to increase their knowledge and skills at no cost. They will also be able to connect with more than 1,500 peers and other meeting attendees from across the country. CHEST members with the time (there are two 5-day meetings each year) and interest are invited to apply to be an official CHEST delegate to the AMA. Contact Suzanne Sletto at [email protected] for details.
Delegates and alternate delegates to the House of Delegates (HOD) play a critical role in the democratic policy-making process that is the foundation of the AMA. Their role is multi-dimensional and includes:
- Advocacy for patients within the HOD to improve the health of the public and the health care system;
- Representation of the perspectives of their sponsoring organization to the HOD;
- Representation of their physician and medical student constituents in the decision-making process of the HOD;
- Representation of the AMA and its House of Delegates to member and nonmember physicians, medical associations, and others; and
- Solicitation of input from and provision of feedback to constituents.
Also, HOD delegates and alternate delegates are expected to foster a positive and useful two-way relationship between grassroots physicians and the CHEST leadership.
Dr. Desai is with the Chicago Chest Center and AMITA Health Suburban Lung Associates; and the Division of Pulmonary, Critical Care, Sleep and Allergy, University of Illinois at Chicago.