User login
New Regents, B/G Executive Committee Members Elected
Two new members of the American College of Surgeons (ACS) Board of Regents (B/R) were elected at the October 19 Annual Business Meeting of Members: Anthony Atala, MD, FACS, and Fabrizio Michelassi, MD, FACS. Dr. Atala is director, Wake Forest Institute for Regenerative Medicine, and W. Boyce Professor and Chair, department of urology, Wake Forest University, Winston Salem, NC. Dr. Michelassi is the Lewis Atterbury Stimson Professor and Chair, Weill Cornell Medical Center, and surgeon-in-chief, New York-Presbyterian/Weill Cornell Medical Center, NY, and Immediate Past-Chair of the Board of Governors (B/G).
The 2016-2017 Chair of the B/R is Michael J. Zinner, MD, FACS, an ACS Regent since 2010 and founding chief executive officer and executive medical director, Miami Cancer Institute, Baptist Health South Florida, Coral Gables. The Vice-Chair is Leigh A. Neumayer, MD, MS, FACS, a Regent since 2009 and professor and chair, department of surgery, University of Arizona, and Margaret and Fenton Maynard Endowed Chair in Breast Cancer Research, University of Arizona College of Medicine, Tucson.
Replacing Dr. Michelassi as Chair of the B/G Executive Committee is Diana L. Farmer, MD, FACS, a pediatric surgeon, Pearl Stamps Stewart Professor of Surgery, and chair, department of surgery, University of California Davis Health System, Sacramento. Steven C. Stain, MD, FACS, a general surgeon and Henry and Sally Schaffer Chair and Professor, department of surgery, Albany Medical Center, NY, has been elected Vice-Chair; and Susan K. Mosier, MD, MBA, FACS, an ophthalmologist, Secretary, Kansas Department of Health and Environment, and State Health Officer for Kansas, Topeka, has been elected Secretary.
In addition, S. Rob Todd, MD, FACS, FCCM, was elected to serve an initial one-year term on the Executive Committee of the B/G. Dr. Todd is professor and chief, section of acute care surgery, department of surgery, and program director, surgical critical care residency, Baylor College of Medicine; and chief, general surgery, and director, Ginni and Richard Mithoff Trauma Center, Ben Taub Hospital, Houston, TX. Elected to an initial two-year term on the B/G Executive Committee was Nicole S. Gibran, MD, FACS, David and Nancy Auth-Washington Research Foundation Endowed Chair for Restorative Burn Surgery, professor, department of surgery, director, UW Medicine Regional Burn Center at Harborview Medical Center, and adjunct professor, department of medicine, division of dermatology, University of Washington, Seattle.
Two new members of the American College of Surgeons (ACS) Board of Regents (B/R) were elected at the October 19 Annual Business Meeting of Members: Anthony Atala, MD, FACS, and Fabrizio Michelassi, MD, FACS. Dr. Atala is director, Wake Forest Institute for Regenerative Medicine, and W. Boyce Professor and Chair, department of urology, Wake Forest University, Winston Salem, NC. Dr. Michelassi is the Lewis Atterbury Stimson Professor and Chair, Weill Cornell Medical Center, and surgeon-in-chief, New York-Presbyterian/Weill Cornell Medical Center, NY, and Immediate Past-Chair of the Board of Governors (B/G).
The 2016-2017 Chair of the B/R is Michael J. Zinner, MD, FACS, an ACS Regent since 2010 and founding chief executive officer and executive medical director, Miami Cancer Institute, Baptist Health South Florida, Coral Gables. The Vice-Chair is Leigh A. Neumayer, MD, MS, FACS, a Regent since 2009 and professor and chair, department of surgery, University of Arizona, and Margaret and Fenton Maynard Endowed Chair in Breast Cancer Research, University of Arizona College of Medicine, Tucson.
Replacing Dr. Michelassi as Chair of the B/G Executive Committee is Diana L. Farmer, MD, FACS, a pediatric surgeon, Pearl Stamps Stewart Professor of Surgery, and chair, department of surgery, University of California Davis Health System, Sacramento. Steven C. Stain, MD, FACS, a general surgeon and Henry and Sally Schaffer Chair and Professor, department of surgery, Albany Medical Center, NY, has been elected Vice-Chair; and Susan K. Mosier, MD, MBA, FACS, an ophthalmologist, Secretary, Kansas Department of Health and Environment, and State Health Officer for Kansas, Topeka, has been elected Secretary.
In addition, S. Rob Todd, MD, FACS, FCCM, was elected to serve an initial one-year term on the Executive Committee of the B/G. Dr. Todd is professor and chief, section of acute care surgery, department of surgery, and program director, surgical critical care residency, Baylor College of Medicine; and chief, general surgery, and director, Ginni and Richard Mithoff Trauma Center, Ben Taub Hospital, Houston, TX. Elected to an initial two-year term on the B/G Executive Committee was Nicole S. Gibran, MD, FACS, David and Nancy Auth-Washington Research Foundation Endowed Chair for Restorative Burn Surgery, professor, department of surgery, director, UW Medicine Regional Burn Center at Harborview Medical Center, and adjunct professor, department of medicine, division of dermatology, University of Washington, Seattle.
Two new members of the American College of Surgeons (ACS) Board of Regents (B/R) were elected at the October 19 Annual Business Meeting of Members: Anthony Atala, MD, FACS, and Fabrizio Michelassi, MD, FACS. Dr. Atala is director, Wake Forest Institute for Regenerative Medicine, and W. Boyce Professor and Chair, department of urology, Wake Forest University, Winston Salem, NC. Dr. Michelassi is the Lewis Atterbury Stimson Professor and Chair, Weill Cornell Medical Center, and surgeon-in-chief, New York-Presbyterian/Weill Cornell Medical Center, NY, and Immediate Past-Chair of the Board of Governors (B/G).
The 2016-2017 Chair of the B/R is Michael J. Zinner, MD, FACS, an ACS Regent since 2010 and founding chief executive officer and executive medical director, Miami Cancer Institute, Baptist Health South Florida, Coral Gables. The Vice-Chair is Leigh A. Neumayer, MD, MS, FACS, a Regent since 2009 and professor and chair, department of surgery, University of Arizona, and Margaret and Fenton Maynard Endowed Chair in Breast Cancer Research, University of Arizona College of Medicine, Tucson.
Replacing Dr. Michelassi as Chair of the B/G Executive Committee is Diana L. Farmer, MD, FACS, a pediatric surgeon, Pearl Stamps Stewart Professor of Surgery, and chair, department of surgery, University of California Davis Health System, Sacramento. Steven C. Stain, MD, FACS, a general surgeon and Henry and Sally Schaffer Chair and Professor, department of surgery, Albany Medical Center, NY, has been elected Vice-Chair; and Susan K. Mosier, MD, MBA, FACS, an ophthalmologist, Secretary, Kansas Department of Health and Environment, and State Health Officer for Kansas, Topeka, has been elected Secretary.
In addition, S. Rob Todd, MD, FACS, FCCM, was elected to serve an initial one-year term on the Executive Committee of the B/G. Dr. Todd is professor and chief, section of acute care surgery, department of surgery, and program director, surgical critical care residency, Baylor College of Medicine; and chief, general surgery, and director, Ginni and Richard Mithoff Trauma Center, Ben Taub Hospital, Houston, TX. Elected to an initial two-year term on the B/G Executive Committee was Nicole S. Gibran, MD, FACS, David and Nancy Auth-Washington Research Foundation Endowed Chair for Restorative Burn Surgery, professor, department of surgery, director, UW Medicine Regional Burn Center at Harborview Medical Center, and adjunct professor, department of medicine, division of dermatology, University of Washington, Seattle.
SVS Foundation Video Highlights Importance of Contributions
A new video highlights the many pioneering innovations of some of our SVS pioneers. Research was and is key. Your tax-deductible contributions to the SVS Foundation supports vascular research -- and the breakthroughs of tomorrow.
A new video highlights the many pioneering innovations of some of our SVS pioneers. Research was and is key. Your tax-deductible contributions to the SVS Foundation supports vascular research -- and the breakthroughs of tomorrow.
A new video highlights the many pioneering innovations of some of our SVS pioneers. Research was and is key. Your tax-deductible contributions to the SVS Foundation supports vascular research -- and the breakthroughs of tomorrow.
Let your Voice Be Heard; Please Donate to SVS PAC
With the election of a new President and new members of Congress, many changes are coming to health care in the United States – vascular surgeons need our voices heard in Washington. Your participation in the SVS Political Action Committee will ensure that the priorities of vascular surgery and the needs of our patients are understood by Congressional leaders and members.
This is the only PAC that is totally focused on the interests of vascular surgery, particularly our reimbursement and our patients. To continue influencing current and future events, please consider donating to the SVS PAC. You will be recognized for your contribution in the 2016 PAC Annual Report.
With the election of a new President and new members of Congress, many changes are coming to health care in the United States – vascular surgeons need our voices heard in Washington. Your participation in the SVS Political Action Committee will ensure that the priorities of vascular surgery and the needs of our patients are understood by Congressional leaders and members.
This is the only PAC that is totally focused on the interests of vascular surgery, particularly our reimbursement and our patients. To continue influencing current and future events, please consider donating to the SVS PAC. You will be recognized for your contribution in the 2016 PAC Annual Report.
With the election of a new President and new members of Congress, many changes are coming to health care in the United States – vascular surgeons need our voices heard in Washington. Your participation in the SVS Political Action Committee will ensure that the priorities of vascular surgery and the needs of our patients are understood by Congressional leaders and members.
This is the only PAC that is totally focused on the interests of vascular surgery, particularly our reimbursement and our patients. To continue influencing current and future events, please consider donating to the SVS PAC. You will be recognized for your contribution in the 2016 PAC Annual Report.
AGA Patient INFO Center now offers gMed instructions
The Patient INFO Center, AGA’s digital library of patient education, continues to grow and expand. As new topics and educational resources are added, there are also opportunities to enhance the experience of using the library to better connect with patients.
In addition to electronic health record systems Athena, Cerner, and EPIC, you can now integrate AGA’s patient education materials into gMed. Based on member feedback and popular demand, AGA created instructions with gMed consultants and tested them with members to ensure accuracy and ease of use.
Check out the newly added gMed instructions and everything else the Patient INFO Center has to offer.
Have thoughts on the Patient INFO Center? Email [email protected].
The Patient INFO Center, AGA’s digital library of patient education, continues to grow and expand. As new topics and educational resources are added, there are also opportunities to enhance the experience of using the library to better connect with patients.
In addition to electronic health record systems Athena, Cerner, and EPIC, you can now integrate AGA’s patient education materials into gMed. Based on member feedback and popular demand, AGA created instructions with gMed consultants and tested them with members to ensure accuracy and ease of use.
Check out the newly added gMed instructions and everything else the Patient INFO Center has to offer.
Have thoughts on the Patient INFO Center? Email [email protected].
The Patient INFO Center, AGA’s digital library of patient education, continues to grow and expand. As new topics and educational resources are added, there are also opportunities to enhance the experience of using the library to better connect with patients.
In addition to electronic health record systems Athena, Cerner, and EPIC, you can now integrate AGA’s patient education materials into gMed. Based on member feedback and popular demand, AGA created instructions with gMed consultants and tested them with members to ensure accuracy and ease of use.
Check out the newly added gMed instructions and everything else the Patient INFO Center has to offer.
Have thoughts on the Patient INFO Center? Email [email protected].
Five tips to prepare for MACRA
As we start off 2017, you’re probably thinking about how to plan for the implementation of MACRA (Medicare Access and CHIP Reauthorization Act of 2015), which begins Jan. 1. While the process might seem overwhelming, AGA is here to provide five steps that you can take to prepare yourself and your practice.
1. Meet 2016 Physician Quality Reporting System (PQRS) reporting requirements.
2. Review your practice’s Quality and Resource Use Reports (QRURs) for 2015 and the first part of 2016. The QRUR will help you understand how you are currently being rated on cost and quality.
3. Watch your mail for a CMS letter alerting you if you’ll be considered a low-volume provider for 2017 under the Merit-based Incentive Program (MIPs) and exempt from MACRA in 2017.
4. Check Medicare Physician Compare, which will allow patients to compare providers in ways they haven’t been able to before. Brainstorm ways to improve patient communication and discover whether outside resources may need to be added to help patients stay healthy ... and happy.
5. Visit www.gastro.org/MACRA for prerecorded webinars and other AGA resources designed to help make MACRA implementation as seamless as possible.
To learn more about MACRA, visit www.gastro.org/MACRA.
As we start off 2017, you’re probably thinking about how to plan for the implementation of MACRA (Medicare Access and CHIP Reauthorization Act of 2015), which begins Jan. 1. While the process might seem overwhelming, AGA is here to provide five steps that you can take to prepare yourself and your practice.
1. Meet 2016 Physician Quality Reporting System (PQRS) reporting requirements.
2. Review your practice’s Quality and Resource Use Reports (QRURs) for 2015 and the first part of 2016. The QRUR will help you understand how you are currently being rated on cost and quality.
3. Watch your mail for a CMS letter alerting you if you’ll be considered a low-volume provider for 2017 under the Merit-based Incentive Program (MIPs) and exempt from MACRA in 2017.
4. Check Medicare Physician Compare, which will allow patients to compare providers in ways they haven’t been able to before. Brainstorm ways to improve patient communication and discover whether outside resources may need to be added to help patients stay healthy ... and happy.
5. Visit www.gastro.org/MACRA for prerecorded webinars and other AGA resources designed to help make MACRA implementation as seamless as possible.
To learn more about MACRA, visit www.gastro.org/MACRA.
As we start off 2017, you’re probably thinking about how to plan for the implementation of MACRA (Medicare Access and CHIP Reauthorization Act of 2015), which begins Jan. 1. While the process might seem overwhelming, AGA is here to provide five steps that you can take to prepare yourself and your practice.
1. Meet 2016 Physician Quality Reporting System (PQRS) reporting requirements.
2. Review your practice’s Quality and Resource Use Reports (QRURs) for 2015 and the first part of 2016. The QRUR will help you understand how you are currently being rated on cost and quality.
3. Watch your mail for a CMS letter alerting you if you’ll be considered a low-volume provider for 2017 under the Merit-based Incentive Program (MIPs) and exempt from MACRA in 2017.
4. Check Medicare Physician Compare, which will allow patients to compare providers in ways they haven’t been able to before. Brainstorm ways to improve patient communication and discover whether outside resources may need to be added to help patients stay healthy ... and happy.
5. Visit www.gastro.org/MACRA for prerecorded webinars and other AGA resources designed to help make MACRA implementation as seamless as possible.
To learn more about MACRA, visit www.gastro.org/MACRA.
Apply for These 2017 Research Grants Before They Close
Round out 2016 by preparing for a 2017 AGA Research Foundation grant. Eight grants are currently open for both established and young investigators, but all will close in January 2017. Make sure you’re prepared to submit your application before the deadline.
Complete information about these and other research awards is available on gastro.org. All recipients will be acknowledged at the Research Recognition Celebration at Digestive Disease Week® 2017 (www.ddw.org) in Chicago, IL.
Jan 6. 2017
- The AGA-Elsevier Gut Microbiome Pilot Research Award will provide $25,000 to support pilot research projects pertaining to the gut microbiome.
- The AGA-Elsevier Pilot Research Award is a 1-year grant providing young investigators, instructors, research associates, or equivalents $25,000 to support pilot research projects in gastroenterology- or hepatology-related areas.
- The AGA-Medtronic Research & Development Pilot Award in Technology grants $31,000 for 1 year to investigators to support the research and development of novel devices or technologies that will potentially impact the diagnosis or treatment of digestive disease.
Jan. 13, 2017
- The AGA-Rome Foundation Functional GI and Motility Disorders Pilot Research Award offers $50,000 for 1 year to early-stage investigators, established investigators, postdoctoral research fellows and combined research and clinical fellows to support pilot research projects pertaining to functional GI and motility disorders.
- The AGA Microbiome Junior Investigator Research Award is a 2-year award of $60,000 for junior investigators engaged in basic, translational, clinical, or health services research related to the gut microbiome.
- The AGA-Pfizer Pilot Research Award in Inflammatory Bowel Disease is a 1-year, $30,000 award offered to established and young investigators to support pilot research projects related to IBD.
Jan. 20, 2017
- The AGA-June & Donald O. Castell, MD, Esophageal Clinical Research Award is a 1-year, $25,000 grant that provides research or salary support for junior faculty involved in clinical research in esophageal diseases.
- The AGA-Caroline Craig Augustyn & Damian Augustyn Award in Digestive Cancer is a 1-year, $40,000 award designed to support a young investigator, instructor, research associate or equivalent who currently holds a federal or nonfederal career development award devoted to conducting research related to digestive cancer.
Round out 2016 by preparing for a 2017 AGA Research Foundation grant. Eight grants are currently open for both established and young investigators, but all will close in January 2017. Make sure you’re prepared to submit your application before the deadline.
Complete information about these and other research awards is available on gastro.org. All recipients will be acknowledged at the Research Recognition Celebration at Digestive Disease Week® 2017 (www.ddw.org) in Chicago, IL.
Jan 6. 2017
- The AGA-Elsevier Gut Microbiome Pilot Research Award will provide $25,000 to support pilot research projects pertaining to the gut microbiome.
- The AGA-Elsevier Pilot Research Award is a 1-year grant providing young investigators, instructors, research associates, or equivalents $25,000 to support pilot research projects in gastroenterology- or hepatology-related areas.
- The AGA-Medtronic Research & Development Pilot Award in Technology grants $31,000 for 1 year to investigators to support the research and development of novel devices or technologies that will potentially impact the diagnosis or treatment of digestive disease.
Jan. 13, 2017
- The AGA-Rome Foundation Functional GI and Motility Disorders Pilot Research Award offers $50,000 for 1 year to early-stage investigators, established investigators, postdoctoral research fellows and combined research and clinical fellows to support pilot research projects pertaining to functional GI and motility disorders.
- The AGA Microbiome Junior Investigator Research Award is a 2-year award of $60,000 for junior investigators engaged in basic, translational, clinical, or health services research related to the gut microbiome.
- The AGA-Pfizer Pilot Research Award in Inflammatory Bowel Disease is a 1-year, $30,000 award offered to established and young investigators to support pilot research projects related to IBD.
Jan. 20, 2017
- The AGA-June & Donald O. Castell, MD, Esophageal Clinical Research Award is a 1-year, $25,000 grant that provides research or salary support for junior faculty involved in clinical research in esophageal diseases.
- The AGA-Caroline Craig Augustyn & Damian Augustyn Award in Digestive Cancer is a 1-year, $40,000 award designed to support a young investigator, instructor, research associate or equivalent who currently holds a federal or nonfederal career development award devoted to conducting research related to digestive cancer.
Round out 2016 by preparing for a 2017 AGA Research Foundation grant. Eight grants are currently open for both established and young investigators, but all will close in January 2017. Make sure you’re prepared to submit your application before the deadline.
Complete information about these and other research awards is available on gastro.org. All recipients will be acknowledged at the Research Recognition Celebration at Digestive Disease Week® 2017 (www.ddw.org) in Chicago, IL.
Jan 6. 2017
- The AGA-Elsevier Gut Microbiome Pilot Research Award will provide $25,000 to support pilot research projects pertaining to the gut microbiome.
- The AGA-Elsevier Pilot Research Award is a 1-year grant providing young investigators, instructors, research associates, or equivalents $25,000 to support pilot research projects in gastroenterology- or hepatology-related areas.
- The AGA-Medtronic Research & Development Pilot Award in Technology grants $31,000 for 1 year to investigators to support the research and development of novel devices or technologies that will potentially impact the diagnosis or treatment of digestive disease.
Jan. 13, 2017
- The AGA-Rome Foundation Functional GI and Motility Disorders Pilot Research Award offers $50,000 for 1 year to early-stage investigators, established investigators, postdoctoral research fellows and combined research and clinical fellows to support pilot research projects pertaining to functional GI and motility disorders.
- The AGA Microbiome Junior Investigator Research Award is a 2-year award of $60,000 for junior investigators engaged in basic, translational, clinical, or health services research related to the gut microbiome.
- The AGA-Pfizer Pilot Research Award in Inflammatory Bowel Disease is a 1-year, $30,000 award offered to established and young investigators to support pilot research projects related to IBD.
Jan. 20, 2017
- The AGA-June & Donald O. Castell, MD, Esophageal Clinical Research Award is a 1-year, $25,000 grant that provides research or salary support for junior faculty involved in clinical research in esophageal diseases.
- The AGA-Caroline Craig Augustyn & Damian Augustyn Award in Digestive Cancer is a 1-year, $40,000 award designed to support a young investigator, instructor, research associate or equivalent who currently holds a federal or nonfederal career development award devoted to conducting research related to digestive cancer.
Memorial and honorary gifts: A special tribute
Did you know you can honor a family member, friend, or colleague whose life has been touched by GI research or celebrate a special occasion such as a birthday while supporting the work of our mission through a gift to the AGA Research Foundation? Your gift will honor a loved one or yourself and support the AGA Research Awards Program, while giving you a tax benefit:
- Giving now or later. Any charitable gift can be made in honor or memory of someone.
- A gift today. An outright gift will help fund the AGA Research Awards Program. Your gift will assist in furthering basic digestive disease research, which can ultimately advance research into all digestive diseases. The financial benefits include an income tax deduction and possible elimination of capital gains tax. A cash gift of $25,000 or more qualifies for membership in the AGA Legacy Society, which recognizes the foundation’s most generous individual donors.
- A gift through your will or living trust. You can include a bequest in your will or living trust stating that a specific asset, certain dollar amount, or more commonly a percentage of your estate will pass to the AGA Research Foundation at your death in honor of your loved one. A gift of $50,000 or more in your will qualifies for membership in the AGA Legacy Society.
- Named DDW Sessions. A named DDW session is established with a minimum gift of $125,000 over the course of 5 years or through an irrevocable planned gift. Gifts of cash, appreciated securities, life insurance, or property are gift vehicles that may be used to establish a named session. Donors will be eligible for naming recognition of a DDW AGA Institute Council session for 10 years. A gift at that level will qualifies for membership in the AGA Legacy Society.
Your next step
An honorary gift is a wonderful way to acknowledge someone’s vision for the future. To learn more about ways to recognize your honoree, visit our website at www.gastro.org/contribute or contact Harmony Excellent at 301-272-1602 or [email protected].
Did you know you can honor a family member, friend, or colleague whose life has been touched by GI research or celebrate a special occasion such as a birthday while supporting the work of our mission through a gift to the AGA Research Foundation? Your gift will honor a loved one or yourself and support the AGA Research Awards Program, while giving you a tax benefit:
- Giving now or later. Any charitable gift can be made in honor or memory of someone.
- A gift today. An outright gift will help fund the AGA Research Awards Program. Your gift will assist in furthering basic digestive disease research, which can ultimately advance research into all digestive diseases. The financial benefits include an income tax deduction and possible elimination of capital gains tax. A cash gift of $25,000 or more qualifies for membership in the AGA Legacy Society, which recognizes the foundation’s most generous individual donors.
- A gift through your will or living trust. You can include a bequest in your will or living trust stating that a specific asset, certain dollar amount, or more commonly a percentage of your estate will pass to the AGA Research Foundation at your death in honor of your loved one. A gift of $50,000 or more in your will qualifies for membership in the AGA Legacy Society.
- Named DDW Sessions. A named DDW session is established with a minimum gift of $125,000 over the course of 5 years or through an irrevocable planned gift. Gifts of cash, appreciated securities, life insurance, or property are gift vehicles that may be used to establish a named session. Donors will be eligible for naming recognition of a DDW AGA Institute Council session for 10 years. A gift at that level will qualifies for membership in the AGA Legacy Society.
Your next step
An honorary gift is a wonderful way to acknowledge someone’s vision for the future. To learn more about ways to recognize your honoree, visit our website at www.gastro.org/contribute or contact Harmony Excellent at 301-272-1602 or [email protected].
Did you know you can honor a family member, friend, or colleague whose life has been touched by GI research or celebrate a special occasion such as a birthday while supporting the work of our mission through a gift to the AGA Research Foundation? Your gift will honor a loved one or yourself and support the AGA Research Awards Program, while giving you a tax benefit:
- Giving now or later. Any charitable gift can be made in honor or memory of someone.
- A gift today. An outright gift will help fund the AGA Research Awards Program. Your gift will assist in furthering basic digestive disease research, which can ultimately advance research into all digestive diseases. The financial benefits include an income tax deduction and possible elimination of capital gains tax. A cash gift of $25,000 or more qualifies for membership in the AGA Legacy Society, which recognizes the foundation’s most generous individual donors.
- A gift through your will or living trust. You can include a bequest in your will or living trust stating that a specific asset, certain dollar amount, or more commonly a percentage of your estate will pass to the AGA Research Foundation at your death in honor of your loved one. A gift of $50,000 or more in your will qualifies for membership in the AGA Legacy Society.
- Named DDW Sessions. A named DDW session is established with a minimum gift of $125,000 over the course of 5 years or through an irrevocable planned gift. Gifts of cash, appreciated securities, life insurance, or property are gift vehicles that may be used to establish a named session. Donors will be eligible for naming recognition of a DDW AGA Institute Council session for 10 years. A gift at that level will qualifies for membership in the AGA Legacy Society.
Your next step
An honorary gift is a wonderful way to acknowledge someone’s vision for the future. To learn more about ways to recognize your honoree, visit our website at www.gastro.org/contribute or contact Harmony Excellent at 301-272-1602 or [email protected].
My journey into pulmonary-critical care medicine
Growing up was not easy. Camden, an inner city in southern New Jersey, is known for its abject poverty, constant violence, and drug trafficking and has been notoriously labeled as one of the “most dangerous cities in the US.” It is a daunting place for many, but home for me. My story is one of a single mother high school dropout with eight children, who worked tirelessly to provide my siblings and me with more advantageous circumstances than she had.
They say “home is where the heart is.” I guess this old statement holds true in my case when I think of why I choose to return to Camden for my residency training at Cooper Hospital. Driving to work in Camden is always a memorable event for me. With every corner and bend in the city, I get a short trip down memory lane. I remember fondly walking to the corner store to buy candy with quarters that my sisters and I dredged up from our couch cushions.
Sundays were my favorite days growing up. We all woke up very early with the singular purpose of getting ready for church. As a child, I loved the attention we all gave each other, especially on Sundays. My siblings and I squabbled and played pranks on each other all morning to my mother’s displeasure, but, somehow, we always made it to church on time, dressed in our Sunday best. After church, our home was filled with hours of laughter, good food, and games only children knew how to play. Our house was always a second home to other kids from our block and friends of my mother who stopped by to try her famous chicken dishes. The days always had the feel of a fun holiday, like Halloween, or Christmas without the lights. It is important that people don’t see Camden as a stereotype, as it has more to offer than murder stories, stray cats, and drug dealing. I am a product of this city.
Embarking on pulmonary-critical care medicine is my next chapter. I see the scourge of pulmonary disease in my internal medicine clinic and am looking forward to arming myself with the knowledge to ease my patients’ burdens. Furthermore, I relish the opportunity to learn how to organize a chaos-filled room into an efficient, harmonized resuscitation situation. The process encourages teamwork, mindfulness, and empathy while being a scientist for the sickest patients in the hospital. These are all fundamental qualities I’ve strived to develop over my maturation as an internal medicine resident and traits I’ve also gained through my various life experiences. I am certain that no other field of medicine would better position me to serve in the broadest sense as a clinician, and I am sure that my life experiences will complement my scientific skill set.
It is said that a journey of a thousand miles begins with a single step. Who knew that someday, I would be able to help repay Camden for nurturing me as a child. I am ready for my new challenges and to embark on this new, pulmonary-critical care medicine chapter in my life.
Dr. Lee is an internal medicine resident at Cooper University Hospital at Cooper Medical School of Rowan University, Camden, NJ.
Editor’s Note
Dr. Lee’s thoughtful piece about why she chose to go into pulmonary–critical care medicine is both inspiring and insightful. She deserves commendation for her willingness to share her story, and I am humbled by her words.
Nitin Puri, MD, FCCP, is the editor of the Pulmonary Perspectives section of CHEST Physician.
Growing up was not easy. Camden, an inner city in southern New Jersey, is known for its abject poverty, constant violence, and drug trafficking and has been notoriously labeled as one of the “most dangerous cities in the US.” It is a daunting place for many, but home for me. My story is one of a single mother high school dropout with eight children, who worked tirelessly to provide my siblings and me with more advantageous circumstances than she had.
They say “home is where the heart is.” I guess this old statement holds true in my case when I think of why I choose to return to Camden for my residency training at Cooper Hospital. Driving to work in Camden is always a memorable event for me. With every corner and bend in the city, I get a short trip down memory lane. I remember fondly walking to the corner store to buy candy with quarters that my sisters and I dredged up from our couch cushions.
Sundays were my favorite days growing up. We all woke up very early with the singular purpose of getting ready for church. As a child, I loved the attention we all gave each other, especially on Sundays. My siblings and I squabbled and played pranks on each other all morning to my mother’s displeasure, but, somehow, we always made it to church on time, dressed in our Sunday best. After church, our home was filled with hours of laughter, good food, and games only children knew how to play. Our house was always a second home to other kids from our block and friends of my mother who stopped by to try her famous chicken dishes. The days always had the feel of a fun holiday, like Halloween, or Christmas without the lights. It is important that people don’t see Camden as a stereotype, as it has more to offer than murder stories, stray cats, and drug dealing. I am a product of this city.
Embarking on pulmonary-critical care medicine is my next chapter. I see the scourge of pulmonary disease in my internal medicine clinic and am looking forward to arming myself with the knowledge to ease my patients’ burdens. Furthermore, I relish the opportunity to learn how to organize a chaos-filled room into an efficient, harmonized resuscitation situation. The process encourages teamwork, mindfulness, and empathy while being a scientist for the sickest patients in the hospital. These are all fundamental qualities I’ve strived to develop over my maturation as an internal medicine resident and traits I’ve also gained through my various life experiences. I am certain that no other field of medicine would better position me to serve in the broadest sense as a clinician, and I am sure that my life experiences will complement my scientific skill set.
It is said that a journey of a thousand miles begins with a single step. Who knew that someday, I would be able to help repay Camden for nurturing me as a child. I am ready for my new challenges and to embark on this new, pulmonary-critical care medicine chapter in my life.
Dr. Lee is an internal medicine resident at Cooper University Hospital at Cooper Medical School of Rowan University, Camden, NJ.
Editor’s Note
Dr. Lee’s thoughtful piece about why she chose to go into pulmonary–critical care medicine is both inspiring and insightful. She deserves commendation for her willingness to share her story, and I am humbled by her words.
Nitin Puri, MD, FCCP, is the editor of the Pulmonary Perspectives section of CHEST Physician.
Growing up was not easy. Camden, an inner city in southern New Jersey, is known for its abject poverty, constant violence, and drug trafficking and has been notoriously labeled as one of the “most dangerous cities in the US.” It is a daunting place for many, but home for me. My story is one of a single mother high school dropout with eight children, who worked tirelessly to provide my siblings and me with more advantageous circumstances than she had.
They say “home is where the heart is.” I guess this old statement holds true in my case when I think of why I choose to return to Camden for my residency training at Cooper Hospital. Driving to work in Camden is always a memorable event for me. With every corner and bend in the city, I get a short trip down memory lane. I remember fondly walking to the corner store to buy candy with quarters that my sisters and I dredged up from our couch cushions.
Sundays were my favorite days growing up. We all woke up very early with the singular purpose of getting ready for church. As a child, I loved the attention we all gave each other, especially on Sundays. My siblings and I squabbled and played pranks on each other all morning to my mother’s displeasure, but, somehow, we always made it to church on time, dressed in our Sunday best. After church, our home was filled with hours of laughter, good food, and games only children knew how to play. Our house was always a second home to other kids from our block and friends of my mother who stopped by to try her famous chicken dishes. The days always had the feel of a fun holiday, like Halloween, or Christmas without the lights. It is important that people don’t see Camden as a stereotype, as it has more to offer than murder stories, stray cats, and drug dealing. I am a product of this city.
Embarking on pulmonary-critical care medicine is my next chapter. I see the scourge of pulmonary disease in my internal medicine clinic and am looking forward to arming myself with the knowledge to ease my patients’ burdens. Furthermore, I relish the opportunity to learn how to organize a chaos-filled room into an efficient, harmonized resuscitation situation. The process encourages teamwork, mindfulness, and empathy while being a scientist for the sickest patients in the hospital. These are all fundamental qualities I’ve strived to develop over my maturation as an internal medicine resident and traits I’ve also gained through my various life experiences. I am certain that no other field of medicine would better position me to serve in the broadest sense as a clinician, and I am sure that my life experiences will complement my scientific skill set.
It is said that a journey of a thousand miles begins with a single step. Who knew that someday, I would be able to help repay Camden for nurturing me as a child. I am ready for my new challenges and to embark on this new, pulmonary-critical care medicine chapter in my life.
Dr. Lee is an internal medicine resident at Cooper University Hospital at Cooper Medical School of Rowan University, Camden, NJ.
Editor’s Note
Dr. Lee’s thoughtful piece about why she chose to go into pulmonary–critical care medicine is both inspiring and insightful. She deserves commendation for her willingness to share her story, and I am humbled by her words.
Nitin Puri, MD, FCCP, is the editor of the Pulmonary Perspectives section of CHEST Physician.
This Month in CHEST: Editor’s Picks
Oral Macrolide Therapy Following Short-term Combination Antibiotic Treatment of Mycobacterium massiliense Lung Disease. By Dr. Won-Jung Koh, et al.
Impact of Acute Changes in CPAP Flow Route in Sleep Apnea Treatment. By Dr. R. G. Andrade, et al.
Endobronchial Ultrasound: Clinical Uses and Professional Reimbursements. By Dr. T. R. Gildea and Dr. K. Nicolacakis.
Chronic Cough Due to Gastroesophageal Reflux in Adults: CHEST Guideline and Expert Panel Report. By Dr. P. J. Kahrilas, et al., on behalf of the CHEST Expert Cough Panel.
Oral Macrolide Therapy Following Short-term Combination Antibiotic Treatment of Mycobacterium massiliense Lung Disease. By Dr. Won-Jung Koh, et al.
Impact of Acute Changes in CPAP Flow Route in Sleep Apnea Treatment. By Dr. R. G. Andrade, et al.
Endobronchial Ultrasound: Clinical Uses and Professional Reimbursements. By Dr. T. R. Gildea and Dr. K. Nicolacakis.
Chronic Cough Due to Gastroesophageal Reflux in Adults: CHEST Guideline and Expert Panel Report. By Dr. P. J. Kahrilas, et al., on behalf of the CHEST Expert Cough Panel.
Oral Macrolide Therapy Following Short-term Combination Antibiotic Treatment of Mycobacterium massiliense Lung Disease. By Dr. Won-Jung Koh, et al.
Impact of Acute Changes in CPAP Flow Route in Sleep Apnea Treatment. By Dr. R. G. Andrade, et al.
Endobronchial Ultrasound: Clinical Uses and Professional Reimbursements. By Dr. T. R. Gildea and Dr. K. Nicolacakis.
Chronic Cough Due to Gastroesophageal Reflux in Adults: CHEST Guideline and Expert Panel Report. By Dr. P. J. Kahrilas, et al., on behalf of the CHEST Expert Cough Panel.
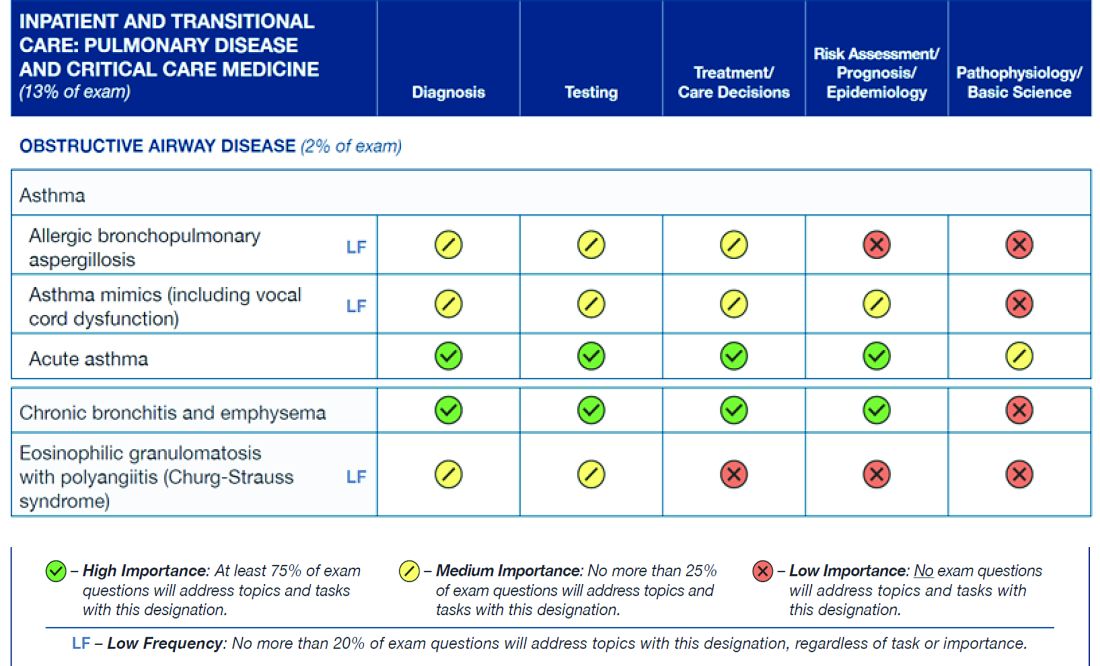
ABIM Pulmonary Medicine Board urges participation in survey
The American Board of Internal Medicine (ABIM) has emailed diplomates a survey regarding the blueprint for the Maintenance of Certification (MOC) pulmonary exam.
This survey relates to the content of the exam, as opposed to a prior survey that asked diplomates for their opinion about new proposals for 2- and 5-year cycles for the exam.
Participating in the survey gives diplomates a voice in determining the content of the MOC exam for pulmonary medicine. If enough individuals participate in the survey and the data support changing the distribution of exam content, it is very likely that ABIM will make improvements to the MOC exam.
The figure below illustrates the information provided by diplomates that ABIM used to help them decide the exam content for the Hospital Medicine exam.
Diplomates can find the survey when they log into their respective homepages on the ABIM website at www.abim.org. The survey does not need to be completed in one sitting, but rather can be done one section at a time. It takes approximately 15 minutes to finish each section.
A link to the survey is located in the My Reminders tab.
This is a great opportunity for individuals to make their voices heard.
The American Board of Internal Medicine (ABIM) has emailed diplomates a survey regarding the blueprint for the Maintenance of Certification (MOC) pulmonary exam.
This survey relates to the content of the exam, as opposed to a prior survey that asked diplomates for their opinion about new proposals for 2- and 5-year cycles for the exam.
Participating in the survey gives diplomates a voice in determining the content of the MOC exam for pulmonary medicine. If enough individuals participate in the survey and the data support changing the distribution of exam content, it is very likely that ABIM will make improvements to the MOC exam.
The figure below illustrates the information provided by diplomates that ABIM used to help them decide the exam content for the Hospital Medicine exam.
Diplomates can find the survey when they log into their respective homepages on the ABIM website at www.abim.org. The survey does not need to be completed in one sitting, but rather can be done one section at a time. It takes approximately 15 minutes to finish each section.
A link to the survey is located in the My Reminders tab.
This is a great opportunity for individuals to make their voices heard.
The American Board of Internal Medicine (ABIM) has emailed diplomates a survey regarding the blueprint for the Maintenance of Certification (MOC) pulmonary exam.
This survey relates to the content of the exam, as opposed to a prior survey that asked diplomates for their opinion about new proposals for 2- and 5-year cycles for the exam.
Participating in the survey gives diplomates a voice in determining the content of the MOC exam for pulmonary medicine. If enough individuals participate in the survey and the data support changing the distribution of exam content, it is very likely that ABIM will make improvements to the MOC exam.
The figure below illustrates the information provided by diplomates that ABIM used to help them decide the exam content for the Hospital Medicine exam.
Diplomates can find the survey when they log into their respective homepages on the ABIM website at www.abim.org. The survey does not need to be completed in one sitting, but rather can be done one section at a time. It takes approximately 15 minutes to finish each section.
A link to the survey is located in the My Reminders tab.
This is a great opportunity for individuals to make their voices heard.