User login
First 2018 Membership Application Deadline is March 1
To improve access, efficiency and service to existing and future SVS members, the Society is now reviewing and approving membership applications quarterly, instead of yearly. The first deadline for 2018 is March 1.
Learn more at vsweb.org/JoinSVS and apply today.
To improve access, efficiency and service to existing and future SVS members, the Society is now reviewing and approving membership applications quarterly, instead of yearly. The first deadline for 2018 is March 1.
Learn more at vsweb.org/JoinSVS and apply today.
To improve access, efficiency and service to existing and future SVS members, the Society is now reviewing and approving membership applications quarterly, instead of yearly. The first deadline for 2018 is March 1.
Learn more at vsweb.org/JoinSVS and apply today.
Community-Practice Surgeons! Apply for YOUR Grant
There’s only a month left to apply for the new SVS Foundation grant program for our community practice members and designed at improving community health.
Applications are due March 1 for the new Community Awareness and Prevention Project Grant, intended to help members in community practice environments conduct projects that address wellness and disease prevention and emphasize patient education, public awareness or risk assessment.
Awardees will receive up to $10,000 for an innovative, community-based initiative. Priority will go to projects that will benefit under-served areas or that include community partnerships.
Learn more vsweb.org/CommunityGrants.
The new program complements the Foundation’s expanded mission, which includes not only basic research but also increased public awareness about vascular disease and treatments and efforts to improve patient vascular care.
There’s only a month left to apply for the new SVS Foundation grant program for our community practice members and designed at improving community health.
Applications are due March 1 for the new Community Awareness and Prevention Project Grant, intended to help members in community practice environments conduct projects that address wellness and disease prevention and emphasize patient education, public awareness or risk assessment.
Awardees will receive up to $10,000 for an innovative, community-based initiative. Priority will go to projects that will benefit under-served areas or that include community partnerships.
Learn more vsweb.org/CommunityGrants.
The new program complements the Foundation’s expanded mission, which includes not only basic research but also increased public awareness about vascular disease and treatments and efforts to improve patient vascular care.
There’s only a month left to apply for the new SVS Foundation grant program for our community practice members and designed at improving community health.
Applications are due March 1 for the new Community Awareness and Prevention Project Grant, intended to help members in community practice environments conduct projects that address wellness and disease prevention and emphasize patient education, public awareness or risk assessment.
Awardees will receive up to $10,000 for an innovative, community-based initiative. Priority will go to projects that will benefit under-served areas or that include community partnerships.
Learn more vsweb.org/CommunityGrants.
The new program complements the Foundation’s expanded mission, which includes not only basic research but also increased public awareness about vascular disease and treatments and efforts to improve patient vascular care.
Applications due Feb. 1 for VAM Scholarships, Research Fellowship
SVS members, please encourage medical or pre-med students interested in vascular surgery to apply for scholarships to attend the 2018 Vascular Annual Meeting. Scholarship applications are due by Feb. 1.
The awards are the General Surgery Resident/Medical Student Travel Scholarship and the Diversity Medical Student Travel Scholarship. Recipients become part of the hugely popular scholarship program, designed to let residents and students explore their interest in vascular surgery.
VAM will be held June 20 to 23, 2018, in Boston, with scientific sessions on June 21-23 and exhibits open June 21-22.)
The SVS Foundation seeks applicants for its Student Research Fellowship awards, designed to stimulate laboratory and clinical vascular research by undergraduate college students and medical students attending universities in the United States and Canada. Urge students you know with an interest in research to apply today.
SVS members, please encourage medical or pre-med students interested in vascular surgery to apply for scholarships to attend the 2018 Vascular Annual Meeting. Scholarship applications are due by Feb. 1.
The awards are the General Surgery Resident/Medical Student Travel Scholarship and the Diversity Medical Student Travel Scholarship. Recipients become part of the hugely popular scholarship program, designed to let residents and students explore their interest in vascular surgery.
VAM will be held June 20 to 23, 2018, in Boston, with scientific sessions on June 21-23 and exhibits open June 21-22.)
The SVS Foundation seeks applicants for its Student Research Fellowship awards, designed to stimulate laboratory and clinical vascular research by undergraduate college students and medical students attending universities in the United States and Canada. Urge students you know with an interest in research to apply today.
SVS members, please encourage medical or pre-med students interested in vascular surgery to apply for scholarships to attend the 2018 Vascular Annual Meeting. Scholarship applications are due by Feb. 1.
The awards are the General Surgery Resident/Medical Student Travel Scholarship and the Diversity Medical Student Travel Scholarship. Recipients become part of the hugely popular scholarship program, designed to let residents and students explore their interest in vascular surgery.
VAM will be held June 20 to 23, 2018, in Boston, with scientific sessions on June 21-23 and exhibits open June 21-22.)
The SVS Foundation seeks applicants for its Student Research Fellowship awards, designed to stimulate laboratory and clinical vascular research by undergraduate college students and medical students attending universities in the United States and Canada. Urge students you know with an interest in research to apply today.
Support GI Research through the AGA Research Foundation
The way we diagnose and treat patients is thanks to years of research. Decades of research and discoveries by dedicated investigators have revolutionized the care of many digestive disease patients. As the charitable arm of the American Gastroenterological Association (AGA), the AGA Research Foundation contributes to this tradition of discovery.
Federal research funding is at risk. Promising early-stage investigators find it increasingly difficult to secure funding and many leave the field because they are unable to sustain a research career. The foundation provides a key source of funding at a critical juncture in a young investigator’s career.
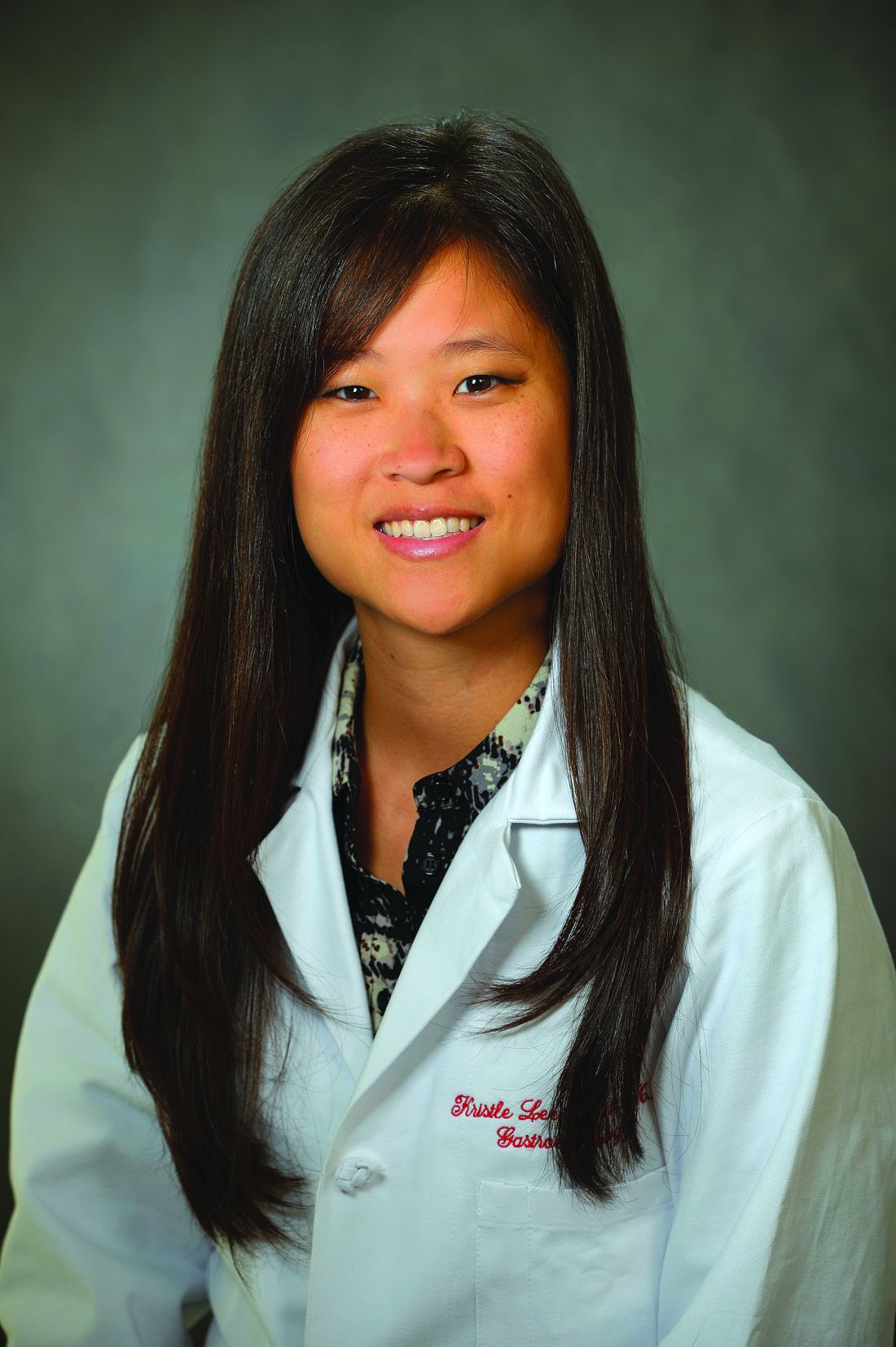
“As a clinical researcher, funding for investigation is critical in scientific breakthroughs to promote more efficient and robust patient care. My project will provide novel insights into the role of distensibility in the treatment of patients with esophageal eosinophilia, potentially resulting in more efficient treatment selection and disease management.”
By joining others in donating to the AGA Research Foundation, you can help fill the funding gap and protect the next generation of investigators.
Your tax-deductible donation will make a critical difference in retaining talented GI scientists, like Dr. Kristle Lynch, whose research will impact the future care of patients.
Donate on the foundation’s website at www.gastro.org/donateonline or by mail to 4930 Del Ray Avenue, Bethesda, MD 20814.
The way we diagnose and treat patients is thanks to years of research. Decades of research and discoveries by dedicated investigators have revolutionized the care of many digestive disease patients. As the charitable arm of the American Gastroenterological Association (AGA), the AGA Research Foundation contributes to this tradition of discovery.
Federal research funding is at risk. Promising early-stage investigators find it increasingly difficult to secure funding and many leave the field because they are unable to sustain a research career. The foundation provides a key source of funding at a critical juncture in a young investigator’s career.
“As a clinical researcher, funding for investigation is critical in scientific breakthroughs to promote more efficient and robust patient care. My project will provide novel insights into the role of distensibility in the treatment of patients with esophageal eosinophilia, potentially resulting in more efficient treatment selection and disease management.”
By joining others in donating to the AGA Research Foundation, you can help fill the funding gap and protect the next generation of investigators.
Your tax-deductible donation will make a critical difference in retaining talented GI scientists, like Dr. Kristle Lynch, whose research will impact the future care of patients.
Donate on the foundation’s website at www.gastro.org/donateonline or by mail to 4930 Del Ray Avenue, Bethesda, MD 20814.
The way we diagnose and treat patients is thanks to years of research. Decades of research and discoveries by dedicated investigators have revolutionized the care of many digestive disease patients. As the charitable arm of the American Gastroenterological Association (AGA), the AGA Research Foundation contributes to this tradition of discovery.
Federal research funding is at risk. Promising early-stage investigators find it increasingly difficult to secure funding and many leave the field because they are unable to sustain a research career. The foundation provides a key source of funding at a critical juncture in a young investigator’s career.
“As a clinical researcher, funding for investigation is critical in scientific breakthroughs to promote more efficient and robust patient care. My project will provide novel insights into the role of distensibility in the treatment of patients with esophageal eosinophilia, potentially resulting in more efficient treatment selection and disease management.”
By joining others in donating to the AGA Research Foundation, you can help fill the funding gap and protect the next generation of investigators.
Your tax-deductible donation will make a critical difference in retaining talented GI scientists, like Dr. Kristle Lynch, whose research will impact the future care of patients.
Donate on the foundation’s website at www.gastro.org/donateonline or by mail to 4930 Del Ray Avenue, Bethesda, MD 20814.
Tough patient cases from 2017
AGA’s member-only online networking platform, the AGA Community, was the hub for clinical case scenarios in 2017. About 100 deidentified patient cases were submitted to the forum, generating over 475 private and public responses from your peers.
Here is a summary of the three cases that sparked the most discussion among AGA members. You can view all discussions in the forum at community.gastro.org/discussions.
#3 “Esophageal hyperkeratosis” (February 2017)
Patient scenario: Patient was having dysphagia. EGD showed circumferential thickening of esophageal lining in the lower half of the esophagus causing partial obstruction; lumen diameter was 7 mm (scope was able to pass with mild resistance). Human papillomavirus (HPV) stain was negative. Multiple biopsies were negative for malignancy, so the practice did not recommend esophagectomy and believed the symptoms were consistent with hyperkeratosis of esophagus. Endoscopic cryotherapy was being considered.
Question: Has anyone come across a case like this?
#2 Thickened stomach (May 2017)
Patient scenario: A 74-year-old male presented early satiety, anemia, and dyspepsia. EGD showed diffuse moderate erythema of the stomach sparing the antrum, and two small superficial duodenal ulcers. Biopsies showed mild chronic inflammation, duodenitis, and negative for H. pylori. The patient was started on a proton pump inhibitor (PPI).
One month later, patient reported early satiety, a 40-pound weight loss over last few months, nausea and vomiting, with minimal improvement while using the PPI. A CT scan of the abdomen and pelvis showed diffuse thickening of the stomach, but was otherwise unremarkable.
One month after that, a repeated EGD showed moderate erythema with enlarged gastric folds, cobblestone of mucosa, again all sparing the antrum. The colonoscopy results were unremarkable. Gastric biopsies showed mild chronic inflammation. Endoscopic ultrasound showed a thickened gastric wall to 14 mm (normal 5 mm) and fine needle aspiration showed normal gastric foveolar epithelium. The patient received a PEG-J tube to maintain nutrition, and then had a laparoscopic assisted full thickness gastric biopsy, which showed benign hypertrophic gastric smooth muscle tissue.
Serum protein electrophoresis and urine protein electrophoresis test results were normal, with total IgG and IgA normal, total IgM low at 31 (normal 60-265), albumin low, other proteins normal, and immunofixation negative. Prealbumin was low at 5 (normal 15-45). Albumin initially normal and over a couple of days low at 2.6 (normal 3.4-5.0). Total protein initially normal and over a couple of days was low at 6.3 (normal 6.8-8.8). Gastrin level was insignificant on the PPI, in the 400s. Zollinger Ellison gastrin not impressive, and the patient is HIV negative.
Question: With a negative biopsy and other test results, Menetrier’s, malignancy, sarcoidosis, eosinophilic gastroenteritis, and amyloidosis can be ruled out. What could the diagnosis be?
#1 IBD and prior hep B (July 2017)
Patient scenario: A 53-year-old male diagnosed with ulcerative colitis (UC) at outside hospital after presenting with abdominal pain, perforation of sigmoid colon. He underwent total colectomy with ileostomy, which showed he has remnant rectum, and the path of colon showed UC with sigmoid stricture. There is no malignancy or dysplasia, and the terminal ileum included in the resection was normal. He had complicated post-op course with enterocutaneous fistula.
He underwent takedown of ileostomy, small bowel resection and ileostomy revision. Path showed segmental small bowel showing viable mucosa with acute serositis and serial adhesions. Ileal mucosa was normal. Rectum has inflammation, and he has symptoms of mucus, urgency, and blood. He had rectal burning and did not tolerate CANASA® suppository. He did not seem to improve with hydrocortisone suppository either.
In trying to decipher next treatment step, hepatitis panel was done, which showed positive hepatitis B core antibody (IgM). Hepatitis B viral load was undetectable. Hepatitis B surface antibody test (HBsAb) quantitative was 6 (not quite the range for immunity of greater than 10). Hepatitis B “e” antigen (HBeAg) negative and hepatitis B “e” antibody (HBeAb) positive. This patient’s hep B core total was positive and hep B surface antigen was negative.
Question: How would you treat this patient? Would you use Imuran?
Share your difficult patient case for the GI community to help you solve at community.gastro.org/quickpost.
AGA’s member-only online networking platform, the AGA Community, was the hub for clinical case scenarios in 2017. About 100 deidentified patient cases were submitted to the forum, generating over 475 private and public responses from your peers.
Here is a summary of the three cases that sparked the most discussion among AGA members. You can view all discussions in the forum at community.gastro.org/discussions.
#3 “Esophageal hyperkeratosis” (February 2017)
Patient scenario: Patient was having dysphagia. EGD showed circumferential thickening of esophageal lining in the lower half of the esophagus causing partial obstruction; lumen diameter was 7 mm (scope was able to pass with mild resistance). Human papillomavirus (HPV) stain was negative. Multiple biopsies were negative for malignancy, so the practice did not recommend esophagectomy and believed the symptoms were consistent with hyperkeratosis of esophagus. Endoscopic cryotherapy was being considered.
Question: Has anyone come across a case like this?
#2 Thickened stomach (May 2017)
Patient scenario: A 74-year-old male presented early satiety, anemia, and dyspepsia. EGD showed diffuse moderate erythema of the stomach sparing the antrum, and two small superficial duodenal ulcers. Biopsies showed mild chronic inflammation, duodenitis, and negative for H. pylori. The patient was started on a proton pump inhibitor (PPI).
One month later, patient reported early satiety, a 40-pound weight loss over last few months, nausea and vomiting, with minimal improvement while using the PPI. A CT scan of the abdomen and pelvis showed diffuse thickening of the stomach, but was otherwise unremarkable.
One month after that, a repeated EGD showed moderate erythema with enlarged gastric folds, cobblestone of mucosa, again all sparing the antrum. The colonoscopy results were unremarkable. Gastric biopsies showed mild chronic inflammation. Endoscopic ultrasound showed a thickened gastric wall to 14 mm (normal 5 mm) and fine needle aspiration showed normal gastric foveolar epithelium. The patient received a PEG-J tube to maintain nutrition, and then had a laparoscopic assisted full thickness gastric biopsy, which showed benign hypertrophic gastric smooth muscle tissue.
Serum protein electrophoresis and urine protein electrophoresis test results were normal, with total IgG and IgA normal, total IgM low at 31 (normal 60-265), albumin low, other proteins normal, and immunofixation negative. Prealbumin was low at 5 (normal 15-45). Albumin initially normal and over a couple of days low at 2.6 (normal 3.4-5.0). Total protein initially normal and over a couple of days was low at 6.3 (normal 6.8-8.8). Gastrin level was insignificant on the PPI, in the 400s. Zollinger Ellison gastrin not impressive, and the patient is HIV negative.
Question: With a negative biopsy and other test results, Menetrier’s, malignancy, sarcoidosis, eosinophilic gastroenteritis, and amyloidosis can be ruled out. What could the diagnosis be?
#1 IBD and prior hep B (July 2017)
Patient scenario: A 53-year-old male diagnosed with ulcerative colitis (UC) at outside hospital after presenting with abdominal pain, perforation of sigmoid colon. He underwent total colectomy with ileostomy, which showed he has remnant rectum, and the path of colon showed UC with sigmoid stricture. There is no malignancy or dysplasia, and the terminal ileum included in the resection was normal. He had complicated post-op course with enterocutaneous fistula.
He underwent takedown of ileostomy, small bowel resection and ileostomy revision. Path showed segmental small bowel showing viable mucosa with acute serositis and serial adhesions. Ileal mucosa was normal. Rectum has inflammation, and he has symptoms of mucus, urgency, and blood. He had rectal burning and did not tolerate CANASA® suppository. He did not seem to improve with hydrocortisone suppository either.
In trying to decipher next treatment step, hepatitis panel was done, which showed positive hepatitis B core antibody (IgM). Hepatitis B viral load was undetectable. Hepatitis B surface antibody test (HBsAb) quantitative was 6 (not quite the range for immunity of greater than 10). Hepatitis B “e” antigen (HBeAg) negative and hepatitis B “e” antibody (HBeAb) positive. This patient’s hep B core total was positive and hep B surface antigen was negative.
Question: How would you treat this patient? Would you use Imuran?
Share your difficult patient case for the GI community to help you solve at community.gastro.org/quickpost.
AGA’s member-only online networking platform, the AGA Community, was the hub for clinical case scenarios in 2017. About 100 deidentified patient cases were submitted to the forum, generating over 475 private and public responses from your peers.
Here is a summary of the three cases that sparked the most discussion among AGA members. You can view all discussions in the forum at community.gastro.org/discussions.
#3 “Esophageal hyperkeratosis” (February 2017)
Patient scenario: Patient was having dysphagia. EGD showed circumferential thickening of esophageal lining in the lower half of the esophagus causing partial obstruction; lumen diameter was 7 mm (scope was able to pass with mild resistance). Human papillomavirus (HPV) stain was negative. Multiple biopsies were negative for malignancy, so the practice did not recommend esophagectomy and believed the symptoms were consistent with hyperkeratosis of esophagus. Endoscopic cryotherapy was being considered.
Question: Has anyone come across a case like this?
#2 Thickened stomach (May 2017)
Patient scenario: A 74-year-old male presented early satiety, anemia, and dyspepsia. EGD showed diffuse moderate erythema of the stomach sparing the antrum, and two small superficial duodenal ulcers. Biopsies showed mild chronic inflammation, duodenitis, and negative for H. pylori. The patient was started on a proton pump inhibitor (PPI).
One month later, patient reported early satiety, a 40-pound weight loss over last few months, nausea and vomiting, with minimal improvement while using the PPI. A CT scan of the abdomen and pelvis showed diffuse thickening of the stomach, but was otherwise unremarkable.
One month after that, a repeated EGD showed moderate erythema with enlarged gastric folds, cobblestone of mucosa, again all sparing the antrum. The colonoscopy results were unremarkable. Gastric biopsies showed mild chronic inflammation. Endoscopic ultrasound showed a thickened gastric wall to 14 mm (normal 5 mm) and fine needle aspiration showed normal gastric foveolar epithelium. The patient received a PEG-J tube to maintain nutrition, and then had a laparoscopic assisted full thickness gastric biopsy, which showed benign hypertrophic gastric smooth muscle tissue.
Serum protein electrophoresis and urine protein electrophoresis test results were normal, with total IgG and IgA normal, total IgM low at 31 (normal 60-265), albumin low, other proteins normal, and immunofixation negative. Prealbumin was low at 5 (normal 15-45). Albumin initially normal and over a couple of days low at 2.6 (normal 3.4-5.0). Total protein initially normal and over a couple of days was low at 6.3 (normal 6.8-8.8). Gastrin level was insignificant on the PPI, in the 400s. Zollinger Ellison gastrin not impressive, and the patient is HIV negative.
Question: With a negative biopsy and other test results, Menetrier’s, malignancy, sarcoidosis, eosinophilic gastroenteritis, and amyloidosis can be ruled out. What could the diagnosis be?
#1 IBD and prior hep B (July 2017)
Patient scenario: A 53-year-old male diagnosed with ulcerative colitis (UC) at outside hospital after presenting with abdominal pain, perforation of sigmoid colon. He underwent total colectomy with ileostomy, which showed he has remnant rectum, and the path of colon showed UC with sigmoid stricture. There is no malignancy or dysplasia, and the terminal ileum included in the resection was normal. He had complicated post-op course with enterocutaneous fistula.
He underwent takedown of ileostomy, small bowel resection and ileostomy revision. Path showed segmental small bowel showing viable mucosa with acute serositis and serial adhesions. Ileal mucosa was normal. Rectum has inflammation, and he has symptoms of mucus, urgency, and blood. He had rectal burning and did not tolerate CANASA® suppository. He did not seem to improve with hydrocortisone suppository either.
In trying to decipher next treatment step, hepatitis panel was done, which showed positive hepatitis B core antibody (IgM). Hepatitis B viral load was undetectable. Hepatitis B surface antibody test (HBsAb) quantitative was 6 (not quite the range for immunity of greater than 10). Hepatitis B “e” antigen (HBeAg) negative and hepatitis B “e” antibody (HBeAb) positive. This patient’s hep B core total was positive and hep B surface antigen was negative.
Question: How would you treat this patient? Would you use Imuran?
Share your difficult patient case for the GI community to help you solve at community.gastro.org/quickpost.
Insurance barriers should not hinder step therapy treatment for IBD
As part of Crohn’s and Colitis Awareness Week 2017 (Dec. 1-7), AGA participated in a congressional briefing sponsored by Takeda and the California Life Sciences Association highlighting advances in inflammatory bowel disease (IBD) therapies, as well as the barriers that patients face in receiving proper treatment for managing their disease.
Physician perspective
Michael Weinstein, MD, representing AGA and the Digestive Health Physicians Association, discussed how treatment options have changed considerably since he began practicing in the 1980s when the only treatment options were immunosuppressive drugs or high-dose steroids that led to dangerous side effects. He highlighted the burden that physicians face with prior authorization practices, especially step therapy in which a patient is required to fail several therapies before being granted coverage to the preferred, physician-prescribed therapy. These insurance protocols can have dire effects on patient care and can be very disruptive to patients who may be so ill that they cannot work or go to school. Dr. Weinstein stated that the burden step therapy places on his practice requires him to have a full-time employee just to navigate the various insurance policies. Many small practices do not have the resources to handle these burdens. Read more from Dr. Weinstein in his op-ed from The Hill.
Patient perspective
Members of Congress and congressional staff heard compelling testimony from Kate Detwiler, an IBD patient who spoke of her family history of IBD, her experience with the disease, and how disruptive it has been to find the best provider and treatments to manage her disease. She and Dr. Weinstein both stressed the financial burdens that the disease puts on families and how limiting it can be to patients who are starting out in their careers or school.
Legislator perspective
Rep. Brad Weinstrup, R-OH, and Rep. Raul Ruiz, D-CA, addressed the briefing as the lead sponsors of HR 2077, the Restoring Patient’s Voice Act, which would provide patients and providers with a clear, equitable, and transparent appeals process when subject to step therapy protocols. Both Rep. Wenstrup and Rep. Ruiz are physicians and have seen the real-life consequences of these policies and their impact on patient care. Both representatives stressed that this is a bipartisan, commonsense solution to ensuring that patients have access to the care that they need when they need it.
AGA continues to advocate for support and passage of HR 2077 and thanks those members who have contacted their members of Congress to request their support. If you haven’t already, please call on your legislator to support this legislation. We will continue to work to garner additional support for the bill in this Congress.
As part of Crohn’s and Colitis Awareness Week 2017 (Dec. 1-7), AGA participated in a congressional briefing sponsored by Takeda and the California Life Sciences Association highlighting advances in inflammatory bowel disease (IBD) therapies, as well as the barriers that patients face in receiving proper treatment for managing their disease.
Physician perspective
Michael Weinstein, MD, representing AGA and the Digestive Health Physicians Association, discussed how treatment options have changed considerably since he began practicing in the 1980s when the only treatment options were immunosuppressive drugs or high-dose steroids that led to dangerous side effects. He highlighted the burden that physicians face with prior authorization practices, especially step therapy in which a patient is required to fail several therapies before being granted coverage to the preferred, physician-prescribed therapy. These insurance protocols can have dire effects on patient care and can be very disruptive to patients who may be so ill that they cannot work or go to school. Dr. Weinstein stated that the burden step therapy places on his practice requires him to have a full-time employee just to navigate the various insurance policies. Many small practices do not have the resources to handle these burdens. Read more from Dr. Weinstein in his op-ed from The Hill.
Patient perspective
Members of Congress and congressional staff heard compelling testimony from Kate Detwiler, an IBD patient who spoke of her family history of IBD, her experience with the disease, and how disruptive it has been to find the best provider and treatments to manage her disease. She and Dr. Weinstein both stressed the financial burdens that the disease puts on families and how limiting it can be to patients who are starting out in their careers or school.
Legislator perspective
Rep. Brad Weinstrup, R-OH, and Rep. Raul Ruiz, D-CA, addressed the briefing as the lead sponsors of HR 2077, the Restoring Patient’s Voice Act, which would provide patients and providers with a clear, equitable, and transparent appeals process when subject to step therapy protocols. Both Rep. Wenstrup and Rep. Ruiz are physicians and have seen the real-life consequences of these policies and their impact on patient care. Both representatives stressed that this is a bipartisan, commonsense solution to ensuring that patients have access to the care that they need when they need it.
AGA continues to advocate for support and passage of HR 2077 and thanks those members who have contacted their members of Congress to request their support. If you haven’t already, please call on your legislator to support this legislation. We will continue to work to garner additional support for the bill in this Congress.
As part of Crohn’s and Colitis Awareness Week 2017 (Dec. 1-7), AGA participated in a congressional briefing sponsored by Takeda and the California Life Sciences Association highlighting advances in inflammatory bowel disease (IBD) therapies, as well as the barriers that patients face in receiving proper treatment for managing their disease.
Physician perspective
Michael Weinstein, MD, representing AGA and the Digestive Health Physicians Association, discussed how treatment options have changed considerably since he began practicing in the 1980s when the only treatment options were immunosuppressive drugs or high-dose steroids that led to dangerous side effects. He highlighted the burden that physicians face with prior authorization practices, especially step therapy in which a patient is required to fail several therapies before being granted coverage to the preferred, physician-prescribed therapy. These insurance protocols can have dire effects on patient care and can be very disruptive to patients who may be so ill that they cannot work or go to school. Dr. Weinstein stated that the burden step therapy places on his practice requires him to have a full-time employee just to navigate the various insurance policies. Many small practices do not have the resources to handle these burdens. Read more from Dr. Weinstein in his op-ed from The Hill.
Patient perspective
Members of Congress and congressional staff heard compelling testimony from Kate Detwiler, an IBD patient who spoke of her family history of IBD, her experience with the disease, and how disruptive it has been to find the best provider and treatments to manage her disease. She and Dr. Weinstein both stressed the financial burdens that the disease puts on families and how limiting it can be to patients who are starting out in their careers or school.
Legislator perspective
Rep. Brad Weinstrup, R-OH, and Rep. Raul Ruiz, D-CA, addressed the briefing as the lead sponsors of HR 2077, the Restoring Patient’s Voice Act, which would provide patients and providers with a clear, equitable, and transparent appeals process when subject to step therapy protocols. Both Rep. Wenstrup and Rep. Ruiz are physicians and have seen the real-life consequences of these policies and their impact on patient care. Both representatives stressed that this is a bipartisan, commonsense solution to ensuring that patients have access to the care that they need when they need it.
AGA continues to advocate for support and passage of HR 2077 and thanks those members who have contacted their members of Congress to request their support. If you haven’t already, please call on your legislator to support this legislation. We will continue to work to garner additional support for the bill in this Congress.
Registration open for DDW® 2018 and 2018 AGA Postgraduate Course
Digestive Disease Week® (DDW), taking place in Washington, D.C., June 2-5, is the gold standard digestive disease meeting. Attend to learn monumental developments in science and medicine, meet leaders in the field, network with colleagues, and attain practical takeaways that you can implement in your career. Visit www.ddw.org to register, for general meeting information, details about the host city, and much more.
On the DDW website, you can also register for the AGA Postgraduate Course taking place during DDW, June 2-3. The 2018 AGA Postgraduate Course will provide a comprehensive look at the latest medical, surgical, and technological advances over the past 12 months that aim to keep you up to date in a field that is rapidly changing. Each presenter will turn abstract ideas into concrete action items that you can immediately implement in your practice. At the end of the course, the take-home points will be compiled and distributed with the eSyllabus.
Digestive Disease Week® (DDW), taking place in Washington, D.C., June 2-5, is the gold standard digestive disease meeting. Attend to learn monumental developments in science and medicine, meet leaders in the field, network with colleagues, and attain practical takeaways that you can implement in your career. Visit www.ddw.org to register, for general meeting information, details about the host city, and much more.
On the DDW website, you can also register for the AGA Postgraduate Course taking place during DDW, June 2-3. The 2018 AGA Postgraduate Course will provide a comprehensive look at the latest medical, surgical, and technological advances over the past 12 months that aim to keep you up to date in a field that is rapidly changing. Each presenter will turn abstract ideas into concrete action items that you can immediately implement in your practice. At the end of the course, the take-home points will be compiled and distributed with the eSyllabus.
Digestive Disease Week® (DDW), taking place in Washington, D.C., June 2-5, is the gold standard digestive disease meeting. Attend to learn monumental developments in science and medicine, meet leaders in the field, network with colleagues, and attain practical takeaways that you can implement in your career. Visit www.ddw.org to register, for general meeting information, details about the host city, and much more.
On the DDW website, you can also register for the AGA Postgraduate Course taking place during DDW, June 2-3. The 2018 AGA Postgraduate Course will provide a comprehensive look at the latest medical, surgical, and technological advances over the past 12 months that aim to keep you up to date in a field that is rapidly changing. Each presenter will turn abstract ideas into concrete action items that you can immediately implement in your practice. At the end of the course, the take-home points will be compiled and distributed with the eSyllabus.
Calendar
For more information about upcoming events and award deadlines, please visit http://www.gastro.org/education and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Feb. 22, 2018; March 22, 2018
Reimbursement, Coding and Compliance for Gastroenterology
Improve the efficiency and performance of your practice by staying current on the latest reimbursement, coding, and compliance changes.
2/22 (Edison, NJ); 3/22 (St. Charles, MO)
AGA Regional Practice Skills Workshop – Ohio
During this free workshop, senior and junior GI leaders will guide you through various practice options and address topics rarely discussed during fellowship, such as employment models, partnerships, hospital politics, billing and coding, compliance, contracts and more. Find out more at http://www.gastro.org/in-person/aga-regional-practice-skills-workshop-ohio.
Columbus, OH
March 12, 2018; March 14, 2018
Advancing Collaborative Approaches in IBD Treatment Decision-Making
This is a unique opportunity for payers and providers to gather in the same room to discuss inflammatory bowel disease therapy selection, disease monitoring, treatment criteria, and access.
3/12 (Pittsburgh); 3/14 (Chicago)
March 21-23, 2018
2018 AGA Tech Summit: Connecting Stakeholders in GI Innovation
Join leaders in the physician, investor, regulatory, and medtech communities as they examine the issues surrounding the development and delivery of new GI medical technologies.
Boston, MA
April 11, 2018
AGA Regional Practice Skills Workshop – Pennsylvania
During this free workshop, senior and junior GI leaders will guide you through various practice options and address topics rarely discussed during fellowship, such as employment models, partnerships, hospital politics, billing and coding, compliance, contracts, and more. Find out more at http://www.gastro.org/in-person/regional-practice-skills-workshop-philadelphia.
Philadelphia
May 10-11, 2018
HIV and Hepatitis Management: THE NEW YORK COURSE
This advanced CME activity will provide participants with state-of-the-art information and practical guidance on progress in managing HIV, hepatitis B, and hepatitis C and will enable practitioners to deliver the highest-quality care in all practice settings.
New York City
Jun. 2-5, 2018
DIGESTIVE DISEASE WEEK® (DDW) 2018 – WASHINGTON, DC
AGA Trainee and Early-Career GI Sessions
Join your colleagues at special sessions to meet the unique needs of physicians who are new to the field. Participants will learn about all aspects of starting a career in clinical practice or research, have the opportunity to network with mentors and peers, and review board material.
• June 2, 8:15 a.m.-5:30 p.m.; June 3, 8:30 a.m.-12:35 p.m.
AGA Postgraduate Course: From Abstract to Reality
Attend this multi-topic course to get practical, applicable information to push your practice to the next level. The 2018 course will provide a comprehensive look at the latest medical, surgical, and technological advances over the past 12 months that aim to keep you up to date in a rapidly changing field. Each presenter will turn abstract ideas into concrete action items that you can implement in your practice immediately. AGA member trainees and early-career GIs receive discounted pricing for this course.
• June 3, 4-5:30 p.m.
Difficult Conversations: Navigating People, Negotiations, Promotions, and Complications
During this session, attendees will obtain effective negotiation techniques and learn how to navigate difficult situations in clinical and research environments.
• June 4, 4-5:30 p.m.
Advancing Clinical Practice: Gastroenterology Fellow–Directed Quality-Improvement Projects
This trainee-focused session will showcase selected abstracts from GI fellows based on quality improvement with a state-of-the-art lecture. Attendees will be provided with information that defines practical approaches to quality improvement from start to finish. A limited supply of coffee and tea will be provided during the session.
• June 5, 1:30-5:30 p.m.
Board Review Course
This session, designed around content from DDSEP® 8, serves as a primer for third-year fellows preparing for the board exam as well as a review course for others wanting to test their knowledge. Session attendees will receive a $50 coupon to use at the AGA Store at DDW to purchase DDSEP 8.
• TBD
AGA Early-Career Networking Hour
Date, time, and location to be announced soon.
June 4-8, 2018
Exosomes/Microvesicles: Heterogeneity, Biogenesis, Function, and Therapeutic Developments (E2)
Deepen your understanding of the structural and functional complexity of extracellular vesicles, their biogenesis and function in health and disease, cargo enrichment, potential as ideal biomarkers, and breakthroughs in their use as therapeutic targets/agents.
Breckenridge, CO
AWARDS APPLICATION DEADLINES
AGA Fellow Abstract Award
This travel award provides $500 and one $1,000 prize to recipients who are MD and/or PhD postdoctoral fellows presenting posters/oral sessions at DDW.
Application Deadline: Feb. 16, 2018
AGA-Moti L. & Kamla Rustgi International Travel Awards
This travel award provides $750 to recipients who are young basic, translational, or clinical investigators residing outside North America to support travel and related expenses to attend DDW.
Application Deadline: Feb. 16, 2018
AGA Student Abstract Award
This travel award provides $500 and one $1,000 prize to recipients who are high school, undergraduate, graduate, medical students, or residents (residents up to year 3 postgraduates) presenting posters/oral sessions at DDW.
Application Deadline: Feb. 16, 2018
For more information about upcoming events and award deadlines, please visit http://www.gastro.org/education and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Feb. 22, 2018; March 22, 2018
Reimbursement, Coding and Compliance for Gastroenterology
Improve the efficiency and performance of your practice by staying current on the latest reimbursement, coding, and compliance changes.
2/22 (Edison, NJ); 3/22 (St. Charles, MO)
AGA Regional Practice Skills Workshop – Ohio
During this free workshop, senior and junior GI leaders will guide you through various practice options and address topics rarely discussed during fellowship, such as employment models, partnerships, hospital politics, billing and coding, compliance, contracts and more. Find out more at http://www.gastro.org/in-person/aga-regional-practice-skills-workshop-ohio.
Columbus, OH
March 12, 2018; March 14, 2018
Advancing Collaborative Approaches in IBD Treatment Decision-Making
This is a unique opportunity for payers and providers to gather in the same room to discuss inflammatory bowel disease therapy selection, disease monitoring, treatment criteria, and access.
3/12 (Pittsburgh); 3/14 (Chicago)
March 21-23, 2018
2018 AGA Tech Summit: Connecting Stakeholders in GI Innovation
Join leaders in the physician, investor, regulatory, and medtech communities as they examine the issues surrounding the development and delivery of new GI medical technologies.
Boston, MA
April 11, 2018
AGA Regional Practice Skills Workshop – Pennsylvania
During this free workshop, senior and junior GI leaders will guide you through various practice options and address topics rarely discussed during fellowship, such as employment models, partnerships, hospital politics, billing and coding, compliance, contracts, and more. Find out more at http://www.gastro.org/in-person/regional-practice-skills-workshop-philadelphia.
Philadelphia
May 10-11, 2018
HIV and Hepatitis Management: THE NEW YORK COURSE
This advanced CME activity will provide participants with state-of-the-art information and practical guidance on progress in managing HIV, hepatitis B, and hepatitis C and will enable practitioners to deliver the highest-quality care in all practice settings.
New York City
Jun. 2-5, 2018
DIGESTIVE DISEASE WEEK® (DDW) 2018 – WASHINGTON, DC
AGA Trainee and Early-Career GI Sessions
Join your colleagues at special sessions to meet the unique needs of physicians who are new to the field. Participants will learn about all aspects of starting a career in clinical practice or research, have the opportunity to network with mentors and peers, and review board material.
• June 2, 8:15 a.m.-5:30 p.m.; June 3, 8:30 a.m.-12:35 p.m.
AGA Postgraduate Course: From Abstract to Reality
Attend this multi-topic course to get practical, applicable information to push your practice to the next level. The 2018 course will provide a comprehensive look at the latest medical, surgical, and technological advances over the past 12 months that aim to keep you up to date in a rapidly changing field. Each presenter will turn abstract ideas into concrete action items that you can implement in your practice immediately. AGA member trainees and early-career GIs receive discounted pricing for this course.
• June 3, 4-5:30 p.m.
Difficult Conversations: Navigating People, Negotiations, Promotions, and Complications
During this session, attendees will obtain effective negotiation techniques and learn how to navigate difficult situations in clinical and research environments.
• June 4, 4-5:30 p.m.
Advancing Clinical Practice: Gastroenterology Fellow–Directed Quality-Improvement Projects
This trainee-focused session will showcase selected abstracts from GI fellows based on quality improvement with a state-of-the-art lecture. Attendees will be provided with information that defines practical approaches to quality improvement from start to finish. A limited supply of coffee and tea will be provided during the session.
• June 5, 1:30-5:30 p.m.
Board Review Course
This session, designed around content from DDSEP® 8, serves as a primer for third-year fellows preparing for the board exam as well as a review course for others wanting to test their knowledge. Session attendees will receive a $50 coupon to use at the AGA Store at DDW to purchase DDSEP 8.
• TBD
AGA Early-Career Networking Hour
Date, time, and location to be announced soon.
June 4-8, 2018
Exosomes/Microvesicles: Heterogeneity, Biogenesis, Function, and Therapeutic Developments (E2)
Deepen your understanding of the structural and functional complexity of extracellular vesicles, their biogenesis and function in health and disease, cargo enrichment, potential as ideal biomarkers, and breakthroughs in their use as therapeutic targets/agents.
Breckenridge, CO
AWARDS APPLICATION DEADLINES
AGA Fellow Abstract Award
This travel award provides $500 and one $1,000 prize to recipients who are MD and/or PhD postdoctoral fellows presenting posters/oral sessions at DDW.
Application Deadline: Feb. 16, 2018
AGA-Moti L. & Kamla Rustgi International Travel Awards
This travel award provides $750 to recipients who are young basic, translational, or clinical investigators residing outside North America to support travel and related expenses to attend DDW.
Application Deadline: Feb. 16, 2018
AGA Student Abstract Award
This travel award provides $500 and one $1,000 prize to recipients who are high school, undergraduate, graduate, medical students, or residents (residents up to year 3 postgraduates) presenting posters/oral sessions at DDW.
Application Deadline: Feb. 16, 2018
For more information about upcoming events and award deadlines, please visit http://www.gastro.org/education and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Feb. 22, 2018; March 22, 2018
Reimbursement, Coding and Compliance for Gastroenterology
Improve the efficiency and performance of your practice by staying current on the latest reimbursement, coding, and compliance changes.
2/22 (Edison, NJ); 3/22 (St. Charles, MO)
AGA Regional Practice Skills Workshop – Ohio
During this free workshop, senior and junior GI leaders will guide you through various practice options and address topics rarely discussed during fellowship, such as employment models, partnerships, hospital politics, billing and coding, compliance, contracts and more. Find out more at http://www.gastro.org/in-person/aga-regional-practice-skills-workshop-ohio.
Columbus, OH
March 12, 2018; March 14, 2018
Advancing Collaborative Approaches in IBD Treatment Decision-Making
This is a unique opportunity for payers and providers to gather in the same room to discuss inflammatory bowel disease therapy selection, disease monitoring, treatment criteria, and access.
3/12 (Pittsburgh); 3/14 (Chicago)
March 21-23, 2018
2018 AGA Tech Summit: Connecting Stakeholders in GI Innovation
Join leaders in the physician, investor, regulatory, and medtech communities as they examine the issues surrounding the development and delivery of new GI medical technologies.
Boston, MA
April 11, 2018
AGA Regional Practice Skills Workshop – Pennsylvania
During this free workshop, senior and junior GI leaders will guide you through various practice options and address topics rarely discussed during fellowship, such as employment models, partnerships, hospital politics, billing and coding, compliance, contracts, and more. Find out more at http://www.gastro.org/in-person/regional-practice-skills-workshop-philadelphia.
Philadelphia
May 10-11, 2018
HIV and Hepatitis Management: THE NEW YORK COURSE
This advanced CME activity will provide participants with state-of-the-art information and practical guidance on progress in managing HIV, hepatitis B, and hepatitis C and will enable practitioners to deliver the highest-quality care in all practice settings.
New York City
Jun. 2-5, 2018
DIGESTIVE DISEASE WEEK® (DDW) 2018 – WASHINGTON, DC
AGA Trainee and Early-Career GI Sessions
Join your colleagues at special sessions to meet the unique needs of physicians who are new to the field. Participants will learn about all aspects of starting a career in clinical practice or research, have the opportunity to network with mentors and peers, and review board material.
• June 2, 8:15 a.m.-5:30 p.m.; June 3, 8:30 a.m.-12:35 p.m.
AGA Postgraduate Course: From Abstract to Reality
Attend this multi-topic course to get practical, applicable information to push your practice to the next level. The 2018 course will provide a comprehensive look at the latest medical, surgical, and technological advances over the past 12 months that aim to keep you up to date in a rapidly changing field. Each presenter will turn abstract ideas into concrete action items that you can implement in your practice immediately. AGA member trainees and early-career GIs receive discounted pricing for this course.
• June 3, 4-5:30 p.m.
Difficult Conversations: Navigating People, Negotiations, Promotions, and Complications
During this session, attendees will obtain effective negotiation techniques and learn how to navigate difficult situations in clinical and research environments.
• June 4, 4-5:30 p.m.
Advancing Clinical Practice: Gastroenterology Fellow–Directed Quality-Improvement Projects
This trainee-focused session will showcase selected abstracts from GI fellows based on quality improvement with a state-of-the-art lecture. Attendees will be provided with information that defines practical approaches to quality improvement from start to finish. A limited supply of coffee and tea will be provided during the session.
• June 5, 1:30-5:30 p.m.
Board Review Course
This session, designed around content from DDSEP® 8, serves as a primer for third-year fellows preparing for the board exam as well as a review course for others wanting to test their knowledge. Session attendees will receive a $50 coupon to use at the AGA Store at DDW to purchase DDSEP 8.
• TBD
AGA Early-Career Networking Hour
Date, time, and location to be announced soon.
June 4-8, 2018
Exosomes/Microvesicles: Heterogeneity, Biogenesis, Function, and Therapeutic Developments (E2)
Deepen your understanding of the structural and functional complexity of extracellular vesicles, their biogenesis and function in health and disease, cargo enrichment, potential as ideal biomarkers, and breakthroughs in their use as therapeutic targets/agents.
Breckenridge, CO
AWARDS APPLICATION DEADLINES
AGA Fellow Abstract Award
This travel award provides $500 and one $1,000 prize to recipients who are MD and/or PhD postdoctoral fellows presenting posters/oral sessions at DDW.
Application Deadline: Feb. 16, 2018
AGA-Moti L. & Kamla Rustgi International Travel Awards
This travel award provides $750 to recipients who are young basic, translational, or clinical investigators residing outside North America to support travel and related expenses to attend DDW.
Application Deadline: Feb. 16, 2018
AGA Student Abstract Award
This travel award provides $500 and one $1,000 prize to recipients who are high school, undergraduate, graduate, medical students, or residents (residents up to year 3 postgraduates) presenting posters/oral sessions at DDW.
Application Deadline: Feb. 16, 2018
Register Today for May 9 VRIC
Registration is now open for the Vascular Research Initiatives Conference, to be held May 9 at the Hilton San Francisco Union Square. The one-day meeting emphasizes emerging vascular science and is held the day before the American Heart Association's Arteriosclerosis, Thrombosis and Vascular Biology Scientific Sessions.
VRIC registration fees are $275 for members; $300, nonmembers; and $150 for residents, students, candidates and nonmember residents and students.
Registration is now open for the Vascular Research Initiatives Conference, to be held May 9 at the Hilton San Francisco Union Square. The one-day meeting emphasizes emerging vascular science and is held the day before the American Heart Association's Arteriosclerosis, Thrombosis and Vascular Biology Scientific Sessions.
VRIC registration fees are $275 for members; $300, nonmembers; and $150 for residents, students, candidates and nonmember residents and students.
Registration is now open for the Vascular Research Initiatives Conference, to be held May 9 at the Hilton San Francisco Union Square. The one-day meeting emphasizes emerging vascular science and is held the day before the American Heart Association's Arteriosclerosis, Thrombosis and Vascular Biology Scientific Sessions.
VRIC registration fees are $275 for members; $300, nonmembers; and $150 for residents, students, candidates and nonmember residents and students.
First 2018 Membership Application Deadline is March 1
To improve access, efficiency and service to existing and future SVS members, the Society is now reviewing and approving membership applications quarterly, instead of yearly. The first deadline for 2018 is March 1.
Learn more at vsweb.org/JoinSVS and apply today.
The SVS is also the management home for the Society for Vascular Nursing. SVN welcomes nurses and nurse practitioners in the vascular setting at many levels and ranges of expertise. For more information, visit svnnet.org.
To improve access, efficiency and service to existing and future SVS members, the Society is now reviewing and approving membership applications quarterly, instead of yearly. The first deadline for 2018 is March 1.
Learn more at vsweb.org/JoinSVS and apply today.
The SVS is also the management home for the Society for Vascular Nursing. SVN welcomes nurses and nurse practitioners in the vascular setting at many levels and ranges of expertise. For more information, visit svnnet.org.
To improve access, efficiency and service to existing and future SVS members, the Society is now reviewing and approving membership applications quarterly, instead of yearly. The first deadline for 2018 is March 1.
Learn more at vsweb.org/JoinSVS and apply today.
The SVS is also the management home for the Society for Vascular Nursing. SVN welcomes nurses and nurse practitioners in the vascular setting at many levels and ranges of expertise. For more information, visit svnnet.org.