User login
Baby, that bill is high: Private equity ‘gambit’ squeezes excessive ER charges from routine births
Elizabeth Huffner thinks it is obvious: A full-term, healthy pregnancy results in a birth.
“When your due date has come and gone, you’re expecting a baby any minute,” Ms. Huffner said. So she was surprised to discover she was an “unknown accident” – at least from a billing standpoint – when she went to the hospital during labor. Her bill included a charge for something she said she didn’t know she’d ever entered: an obstetrics ED.
That’s where a doctor briefly checked her cervix, timed her contractions, and monitored the fetal heartbeat before telling her to go home and come back later. The area is separated from the rest of the labor-and-delivery department by a curtain. The hospital got about $1,300 for that visit – $530 of it from Ms. Huffner’s pocket.
In recent years, hospitals of every stripe have opened obstetrics EDs, or OBEDs. They come with a requirement that patients with pregnancy or postpartum medical concerns be seen quickly by a qualified provider, which can be important in a real emergency. But it also means healthy patients like Ms. Huffner get bills for emergency care they didn’t know they got.
“It should be a cautionary tale to every woman,” said Ms. Huffner, of Rockford, Ill.
Three of the four major companies that set up and staff OBEDs are affiliated with private equity firms, which are known for making a profit on quick-turnaround investments. Private equity has been around for a long time in other medical specialties, and researchers are now tracking its move into women’s health care, including obstetrics. These private equity–associated practices come with a promise of increased patient satisfaction and better care, which can help the hospital avoid malpractice costs from bad outcomes.
But private equity also is trying to boost revenue. Robert Wachter, MD, chair of the department of medicine at the University of California, San Francisco, calls the private equity encroachment into medicine “worrisome.”
“Hospitals will do what they can do to maximize income as long as they’re not breaking the rules,” Dr. Wachter said. “And it sounds like that’s sort of what they’re doing with this ER gambit.”
Surprising bills
KHN reviewed the bills of a dozen patients in five states who said they were hit with surprise emergency charges for being triaged in an OBED while in labor. That included a woman in Grand Junction, Colo., who said she felt “gaslit” when she had to pay $300 in emergency charges for the care she received in the small room where they confirmed she was in full-term labor. And in Kansas, a family said they were paying $400 for the same services, also rendered in a “very tiny” room – even though HCA Healthcare, the national for-profit chain that runs the hospital, told KHN that emergency charges are supposed to be waived if the patient is admitted for delivery.
Few of the patients KHN interviewed could recall being told that they were accessing emergency services, nor did they recall entering a space that looked like an ED or was marked as one. Insurance denied the charges in some cases. But in others families were left to pay hundreds of dollars for their share of the tab – adding to already large hospital bills. Several patients reported noticing big jumps in cost for their most recent births, compared with those of previous children, even though they did not notice any changes to the facilities where they delivered.
Three physicians in Colorado told KHN that the hospitals where they work made minimal changes when the institutions opened OBEDs: The facilities were the same triage rooms as before, just with a different sign outside – and different billing practices.
“When I see somebody for a really minor thing, like, someone who comes in at 38 weeks, thinks she’s in labor, but she’s not in labor, gets discharged home – I feel really bad,” said Vanessa Gilliland, MD, who until recently worked as a hospitalist in OBEDs at two hospitals near Denver. “I hope she doesn’t get some $500 bill for just coming in for that.”
The bills generated by encounters with OBEDs can be baffling to patients.
Clara Love and Jonathan Guerra-Rodríguez, MD, an ICU nurse and an internist, respectively, found a charge for the highest level of emergency care in the bill for their son’s birth. It took months of back and forth – and the looming threat of collections – before the hospital explained that the charge was for treatment in an obstetrics ED, the triage area where a nurse examined Ms. Love before she was admitted in full-term labor. “I don’t like using hyperbole, but as a provider I have never seen anything like this,” Dr. Guerra-Rodríguez said.
Patients with medical backgrounds may be more likely than other people to notice these unusual charges, which can be hidden in long or opaque billing documents. A physician assistant in North Carolina and an ICU nurse in Texas also were shocked by the OBED charges they faced.
Figuring out where OBEDs even are can be difficult.
Health departments in California, Colorado, Massachusetts, and New York said they do not track hospitals that open OBEDs because they are considered an extension of a hospital’s main ED. Neither do professional groups like the American Hospital Association, the American College of Obstetricians and Gynecologists, and the Joint Commission, which accredits health care programs across the country.
Some hospitals state clearly on their websites that they have an OBED. A few hospitals state that visiting their OBED will incur emergency room charges. Other hospitals with OBEDs don’t mention their existence at all.
Origins of the OBED concept
Three of the main companies that set up and staff OBEDs – the OB Hospitalist Group, or OBHG; TeamHealth; and Envision Healthcare – are affiliated with private equity firms. The fourth, Pediatrix Medical Group, formerly known as Mednax, is publicly traded. All are for-profit companies.
Several are clear about the revenue benefits of opening OBEDs. TeamHealth – one of the country’s dominant ER staffing companies – is owned by private equity firm Blackstone and has faced criticism from lawmakers for high ER bills. In a document aimed at hospital administrators, TeamHealth says OBEDs are good for “boosting hospital revenues” with “little to no structural investment for the hospital.” It markets OBED success stories to potential customers, highlighting hospitals in California and South Florida where OBEDs reportedly improved patient care – and “produced additional revenue through OBED services.” OBHG, which staffs close to 200 OBEDs in 33 states, markets a scoring tool designed to help hospitals maximize charges from OBEDs and has marketed its services to about 3,000 hospitals.
Staffing companies and hospitals, contacted by KHN, said that OBEDs help deliver better care and that private equity involvement doesn’t impede that care.
Data from Colorado offers a window into how hospitals may be shifting the way they bill for triaging healthy labor. In an analysis for KHN, the Center for Improving Value in Health Care found that the share of uncomplicated vaginal deliveries that had an ED charge embedded in their bills more than doubled in Colorado from 2016 to 2020. It is still a small segment of births, however, rising from 1.4% to 3.3%.
Major staffing companies are set up to charge for every single little thing, said Wayne Farley, MD. He would know: He used to have a leadership role in one of those major staffing companies, the private equity-backed Envision, after it bought his previous employer. Now he’s a practicing ob.gyn. hospitalist at four OBEDs and a consultant who helps hospitals start OBEDs.
“I’ve actually thought about creating a business where I review billings for these patients and help them fight claims,” said Dr. Farley, who thinks a high-level emergency charge makes sense only if the patient had serious complications or required a high level of care.
Proponents of OBEDs say converting a triage room into an obstetrics ED can help pay for a hospital to hire 24/7 hospitalists. In labor and delivery, that means obstetric specialists are available purely to respond to patients who come to the hospital, rather than juggling those cases with clinic visits. Supporters of OBEDs say there’s evidence that having hospitalists on hand is safer for patients and can reduce unnecessary cesarean sections.
“That’s no excuse,” said Lawrence Casalino, MD, a physician and health policy researcher at Weill Cornell Medicine, New York. “To have people get an emergency room charge when they don’t even know they’re in an emergency room – I mean, that doesn’t meet the laugh test.”
But Christopher Swain, MD, who founded the OB Hospitalist Group and is credited with inventing the OBED concept, said that having round-the-clock hospitalists on staff is essential for giving pregnant patients good care and that starting an OBED can help pay for those hospitalists.
Dr. Swain said he started the nation’s first OBED in 2006 in Kissimmee, Fla. He said that, at early-adopter hospitals, OBEDs helped pay to have a doctor available on the labor-and-delivery floor 24/7 and that hospitals subsequently saw better outcomes and lower malpractice rates.
“We feel like we fixed something,” Dr. Swain said. “I feel like we really helped to move the bar to improve the quality of care and to provide better outcomes.”
Dr. Swain is no longer affiliated with OBHG, which has been in private equity hands since at least 2013. The company has recently gone so far as to present OBEDs as part of the solution to the country’s maternal mortality problem. Hospitals such as an Ascension St. Joseph’s hospital in Milwaukee have echoed that statement in their reasons for opening an OBED.
But Dr. Wachter – who coined the term “hospitalist” and who generally believes the presence of hospitalists leads to better care – thinks that reasoning is questionable, especially because hospitals find ways to pay for hospitalists in other specialties without engineering new facility fees.
“I’m always a little skeptical of the justification,” Dr. Wachter said. “They will always have a rationale for why income maximization is a reasonable and moral strategy.”
Private equity’s footprint in women’s health care
Dr. Farley estimates that he has helped set up OBEDs – including Colorado’s first in 2013 – in at least 30 hospitals. He’s aware of hospitals that claim they have OBEDs when the only change they’ve made is to have an ob.gyn. on site round the clock.
“You can’t just hang out a shingle and say: ‘We have an OBED.’ It’s an investment on the part of the hospital,” he said. That means having, among other things, a separate entrance from the rest of the labor-and-delivery department, clear signage inside and outside the hospital, and a separate waiting room. Some hospitals he has worked with have invested millions of dollars in upgrading facilities for their OBED.
Private equity firms often promise more efficient management, plus investment in technology and facilities that could improve patient care or satisfaction. In some parts of health care, that could really help, said Ambar La Forgia, PhD, who researches health care management at the University of California, Berkeley, and is studying private equity investment in fertility care. But Dr. La Forgia said that in much of health care, gauging whether such firms are truly maintaining or improving the quality of care is difficult.
“Private equity is about being able to extract some sort of value very quickly,” Dr. La Forgia said. “And in health care, when prices are so opaque and there’s so much lack of transparency, a lot of those impacts on the prices are eventually going to fall on the patient.”
It’s changing circumstances for doctors, too. Michelle Barhaghi, MD, a Colorado obstetrician, said OBEDs may make sense in busy, urban hospitals with lots of patients who did not get prenatal care. But now they’re cropping up everywhere. “From a doctor standpoint, none of us want these jobs because now we’re like a resident again, where we have to see every single patient that walks through that door,” said Dr. Barhaghi, rather than triaging many cases on the phone with a nurse.
Still, private equity is continuing its advance into women’s health care.
Indeed, Dr. Barhaghi said private equity came knocking on her door earlier this year: Women’s Care Enterprises, backed by private equity company BC Partners, wanted to know whether she would consider selling her practice. She said “no.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Elizabeth Huffner thinks it is obvious: A full-term, healthy pregnancy results in a birth.
“When your due date has come and gone, you’re expecting a baby any minute,” Ms. Huffner said. So she was surprised to discover she was an “unknown accident” – at least from a billing standpoint – when she went to the hospital during labor. Her bill included a charge for something she said she didn’t know she’d ever entered: an obstetrics ED.
That’s where a doctor briefly checked her cervix, timed her contractions, and monitored the fetal heartbeat before telling her to go home and come back later. The area is separated from the rest of the labor-and-delivery department by a curtain. The hospital got about $1,300 for that visit – $530 of it from Ms. Huffner’s pocket.
In recent years, hospitals of every stripe have opened obstetrics EDs, or OBEDs. They come with a requirement that patients with pregnancy or postpartum medical concerns be seen quickly by a qualified provider, which can be important in a real emergency. But it also means healthy patients like Ms. Huffner get bills for emergency care they didn’t know they got.
“It should be a cautionary tale to every woman,” said Ms. Huffner, of Rockford, Ill.
Three of the four major companies that set up and staff OBEDs are affiliated with private equity firms, which are known for making a profit on quick-turnaround investments. Private equity has been around for a long time in other medical specialties, and researchers are now tracking its move into women’s health care, including obstetrics. These private equity–associated practices come with a promise of increased patient satisfaction and better care, which can help the hospital avoid malpractice costs from bad outcomes.
But private equity also is trying to boost revenue. Robert Wachter, MD, chair of the department of medicine at the University of California, San Francisco, calls the private equity encroachment into medicine “worrisome.”
“Hospitals will do what they can do to maximize income as long as they’re not breaking the rules,” Dr. Wachter said. “And it sounds like that’s sort of what they’re doing with this ER gambit.”
Surprising bills
KHN reviewed the bills of a dozen patients in five states who said they were hit with surprise emergency charges for being triaged in an OBED while in labor. That included a woman in Grand Junction, Colo., who said she felt “gaslit” when she had to pay $300 in emergency charges for the care she received in the small room where they confirmed she was in full-term labor. And in Kansas, a family said they were paying $400 for the same services, also rendered in a “very tiny” room – even though HCA Healthcare, the national for-profit chain that runs the hospital, told KHN that emergency charges are supposed to be waived if the patient is admitted for delivery.
Few of the patients KHN interviewed could recall being told that they were accessing emergency services, nor did they recall entering a space that looked like an ED or was marked as one. Insurance denied the charges in some cases. But in others families were left to pay hundreds of dollars for their share of the tab – adding to already large hospital bills. Several patients reported noticing big jumps in cost for their most recent births, compared with those of previous children, even though they did not notice any changes to the facilities where they delivered.
Three physicians in Colorado told KHN that the hospitals where they work made minimal changes when the institutions opened OBEDs: The facilities were the same triage rooms as before, just with a different sign outside – and different billing practices.
“When I see somebody for a really minor thing, like, someone who comes in at 38 weeks, thinks she’s in labor, but she’s not in labor, gets discharged home – I feel really bad,” said Vanessa Gilliland, MD, who until recently worked as a hospitalist in OBEDs at two hospitals near Denver. “I hope she doesn’t get some $500 bill for just coming in for that.”
The bills generated by encounters with OBEDs can be baffling to patients.
Clara Love and Jonathan Guerra-Rodríguez, MD, an ICU nurse and an internist, respectively, found a charge for the highest level of emergency care in the bill for their son’s birth. It took months of back and forth – and the looming threat of collections – before the hospital explained that the charge was for treatment in an obstetrics ED, the triage area where a nurse examined Ms. Love before she was admitted in full-term labor. “I don’t like using hyperbole, but as a provider I have never seen anything like this,” Dr. Guerra-Rodríguez said.
Patients with medical backgrounds may be more likely than other people to notice these unusual charges, which can be hidden in long or opaque billing documents. A physician assistant in North Carolina and an ICU nurse in Texas also were shocked by the OBED charges they faced.
Figuring out where OBEDs even are can be difficult.
Health departments in California, Colorado, Massachusetts, and New York said they do not track hospitals that open OBEDs because they are considered an extension of a hospital’s main ED. Neither do professional groups like the American Hospital Association, the American College of Obstetricians and Gynecologists, and the Joint Commission, which accredits health care programs across the country.
Some hospitals state clearly on their websites that they have an OBED. A few hospitals state that visiting their OBED will incur emergency room charges. Other hospitals with OBEDs don’t mention their existence at all.
Origins of the OBED concept
Three of the main companies that set up and staff OBEDs – the OB Hospitalist Group, or OBHG; TeamHealth; and Envision Healthcare – are affiliated with private equity firms. The fourth, Pediatrix Medical Group, formerly known as Mednax, is publicly traded. All are for-profit companies.
Several are clear about the revenue benefits of opening OBEDs. TeamHealth – one of the country’s dominant ER staffing companies – is owned by private equity firm Blackstone and has faced criticism from lawmakers for high ER bills. In a document aimed at hospital administrators, TeamHealth says OBEDs are good for “boosting hospital revenues” with “little to no structural investment for the hospital.” It markets OBED success stories to potential customers, highlighting hospitals in California and South Florida where OBEDs reportedly improved patient care – and “produced additional revenue through OBED services.” OBHG, which staffs close to 200 OBEDs in 33 states, markets a scoring tool designed to help hospitals maximize charges from OBEDs and has marketed its services to about 3,000 hospitals.
Staffing companies and hospitals, contacted by KHN, said that OBEDs help deliver better care and that private equity involvement doesn’t impede that care.
Data from Colorado offers a window into how hospitals may be shifting the way they bill for triaging healthy labor. In an analysis for KHN, the Center for Improving Value in Health Care found that the share of uncomplicated vaginal deliveries that had an ED charge embedded in their bills more than doubled in Colorado from 2016 to 2020. It is still a small segment of births, however, rising from 1.4% to 3.3%.
Major staffing companies are set up to charge for every single little thing, said Wayne Farley, MD. He would know: He used to have a leadership role in one of those major staffing companies, the private equity-backed Envision, after it bought his previous employer. Now he’s a practicing ob.gyn. hospitalist at four OBEDs and a consultant who helps hospitals start OBEDs.
“I’ve actually thought about creating a business where I review billings for these patients and help them fight claims,” said Dr. Farley, who thinks a high-level emergency charge makes sense only if the patient had serious complications or required a high level of care.
Proponents of OBEDs say converting a triage room into an obstetrics ED can help pay for a hospital to hire 24/7 hospitalists. In labor and delivery, that means obstetric specialists are available purely to respond to patients who come to the hospital, rather than juggling those cases with clinic visits. Supporters of OBEDs say there’s evidence that having hospitalists on hand is safer for patients and can reduce unnecessary cesarean sections.
“That’s no excuse,” said Lawrence Casalino, MD, a physician and health policy researcher at Weill Cornell Medicine, New York. “To have people get an emergency room charge when they don’t even know they’re in an emergency room – I mean, that doesn’t meet the laugh test.”
But Christopher Swain, MD, who founded the OB Hospitalist Group and is credited with inventing the OBED concept, said that having round-the-clock hospitalists on staff is essential for giving pregnant patients good care and that starting an OBED can help pay for those hospitalists.
Dr. Swain said he started the nation’s first OBED in 2006 in Kissimmee, Fla. He said that, at early-adopter hospitals, OBEDs helped pay to have a doctor available on the labor-and-delivery floor 24/7 and that hospitals subsequently saw better outcomes and lower malpractice rates.
“We feel like we fixed something,” Dr. Swain said. “I feel like we really helped to move the bar to improve the quality of care and to provide better outcomes.”
Dr. Swain is no longer affiliated with OBHG, which has been in private equity hands since at least 2013. The company has recently gone so far as to present OBEDs as part of the solution to the country’s maternal mortality problem. Hospitals such as an Ascension St. Joseph’s hospital in Milwaukee have echoed that statement in their reasons for opening an OBED.
But Dr. Wachter – who coined the term “hospitalist” and who generally believes the presence of hospitalists leads to better care – thinks that reasoning is questionable, especially because hospitals find ways to pay for hospitalists in other specialties without engineering new facility fees.
“I’m always a little skeptical of the justification,” Dr. Wachter said. “They will always have a rationale for why income maximization is a reasonable and moral strategy.”
Private equity’s footprint in women’s health care
Dr. Farley estimates that he has helped set up OBEDs – including Colorado’s first in 2013 – in at least 30 hospitals. He’s aware of hospitals that claim they have OBEDs when the only change they’ve made is to have an ob.gyn. on site round the clock.
“You can’t just hang out a shingle and say: ‘We have an OBED.’ It’s an investment on the part of the hospital,” he said. That means having, among other things, a separate entrance from the rest of the labor-and-delivery department, clear signage inside and outside the hospital, and a separate waiting room. Some hospitals he has worked with have invested millions of dollars in upgrading facilities for their OBED.
Private equity firms often promise more efficient management, plus investment in technology and facilities that could improve patient care or satisfaction. In some parts of health care, that could really help, said Ambar La Forgia, PhD, who researches health care management at the University of California, Berkeley, and is studying private equity investment in fertility care. But Dr. La Forgia said that in much of health care, gauging whether such firms are truly maintaining or improving the quality of care is difficult.
“Private equity is about being able to extract some sort of value very quickly,” Dr. La Forgia said. “And in health care, when prices are so opaque and there’s so much lack of transparency, a lot of those impacts on the prices are eventually going to fall on the patient.”
It’s changing circumstances for doctors, too. Michelle Barhaghi, MD, a Colorado obstetrician, said OBEDs may make sense in busy, urban hospitals with lots of patients who did not get prenatal care. But now they’re cropping up everywhere. “From a doctor standpoint, none of us want these jobs because now we’re like a resident again, where we have to see every single patient that walks through that door,” said Dr. Barhaghi, rather than triaging many cases on the phone with a nurse.
Still, private equity is continuing its advance into women’s health care.
Indeed, Dr. Barhaghi said private equity came knocking on her door earlier this year: Women’s Care Enterprises, backed by private equity company BC Partners, wanted to know whether she would consider selling her practice. She said “no.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Elizabeth Huffner thinks it is obvious: A full-term, healthy pregnancy results in a birth.
“When your due date has come and gone, you’re expecting a baby any minute,” Ms. Huffner said. So she was surprised to discover she was an “unknown accident” – at least from a billing standpoint – when she went to the hospital during labor. Her bill included a charge for something she said she didn’t know she’d ever entered: an obstetrics ED.
That’s where a doctor briefly checked her cervix, timed her contractions, and monitored the fetal heartbeat before telling her to go home and come back later. The area is separated from the rest of the labor-and-delivery department by a curtain. The hospital got about $1,300 for that visit – $530 of it from Ms. Huffner’s pocket.
In recent years, hospitals of every stripe have opened obstetrics EDs, or OBEDs. They come with a requirement that patients with pregnancy or postpartum medical concerns be seen quickly by a qualified provider, which can be important in a real emergency. But it also means healthy patients like Ms. Huffner get bills for emergency care they didn’t know they got.
“It should be a cautionary tale to every woman,” said Ms. Huffner, of Rockford, Ill.
Three of the four major companies that set up and staff OBEDs are affiliated with private equity firms, which are known for making a profit on quick-turnaround investments. Private equity has been around for a long time in other medical specialties, and researchers are now tracking its move into women’s health care, including obstetrics. These private equity–associated practices come with a promise of increased patient satisfaction and better care, which can help the hospital avoid malpractice costs from bad outcomes.
But private equity also is trying to boost revenue. Robert Wachter, MD, chair of the department of medicine at the University of California, San Francisco, calls the private equity encroachment into medicine “worrisome.”
“Hospitals will do what they can do to maximize income as long as they’re not breaking the rules,” Dr. Wachter said. “And it sounds like that’s sort of what they’re doing with this ER gambit.”
Surprising bills
KHN reviewed the bills of a dozen patients in five states who said they were hit with surprise emergency charges for being triaged in an OBED while in labor. That included a woman in Grand Junction, Colo., who said she felt “gaslit” when she had to pay $300 in emergency charges for the care she received in the small room where they confirmed she was in full-term labor. And in Kansas, a family said they were paying $400 for the same services, also rendered in a “very tiny” room – even though HCA Healthcare, the national for-profit chain that runs the hospital, told KHN that emergency charges are supposed to be waived if the patient is admitted for delivery.
Few of the patients KHN interviewed could recall being told that they were accessing emergency services, nor did they recall entering a space that looked like an ED or was marked as one. Insurance denied the charges in some cases. But in others families were left to pay hundreds of dollars for their share of the tab – adding to already large hospital bills. Several patients reported noticing big jumps in cost for their most recent births, compared with those of previous children, even though they did not notice any changes to the facilities where they delivered.
Three physicians in Colorado told KHN that the hospitals where they work made minimal changes when the institutions opened OBEDs: The facilities were the same triage rooms as before, just with a different sign outside – and different billing practices.
“When I see somebody for a really minor thing, like, someone who comes in at 38 weeks, thinks she’s in labor, but she’s not in labor, gets discharged home – I feel really bad,” said Vanessa Gilliland, MD, who until recently worked as a hospitalist in OBEDs at two hospitals near Denver. “I hope she doesn’t get some $500 bill for just coming in for that.”
The bills generated by encounters with OBEDs can be baffling to patients.
Clara Love and Jonathan Guerra-Rodríguez, MD, an ICU nurse and an internist, respectively, found a charge for the highest level of emergency care in the bill for their son’s birth. It took months of back and forth – and the looming threat of collections – before the hospital explained that the charge was for treatment in an obstetrics ED, the triage area where a nurse examined Ms. Love before she was admitted in full-term labor. “I don’t like using hyperbole, but as a provider I have never seen anything like this,” Dr. Guerra-Rodríguez said.
Patients with medical backgrounds may be more likely than other people to notice these unusual charges, which can be hidden in long or opaque billing documents. A physician assistant in North Carolina and an ICU nurse in Texas also were shocked by the OBED charges they faced.
Figuring out where OBEDs even are can be difficult.
Health departments in California, Colorado, Massachusetts, and New York said they do not track hospitals that open OBEDs because they are considered an extension of a hospital’s main ED. Neither do professional groups like the American Hospital Association, the American College of Obstetricians and Gynecologists, and the Joint Commission, which accredits health care programs across the country.
Some hospitals state clearly on their websites that they have an OBED. A few hospitals state that visiting their OBED will incur emergency room charges. Other hospitals with OBEDs don’t mention their existence at all.
Origins of the OBED concept
Three of the main companies that set up and staff OBEDs – the OB Hospitalist Group, or OBHG; TeamHealth; and Envision Healthcare – are affiliated with private equity firms. The fourth, Pediatrix Medical Group, formerly known as Mednax, is publicly traded. All are for-profit companies.
Several are clear about the revenue benefits of opening OBEDs. TeamHealth – one of the country’s dominant ER staffing companies – is owned by private equity firm Blackstone and has faced criticism from lawmakers for high ER bills. In a document aimed at hospital administrators, TeamHealth says OBEDs are good for “boosting hospital revenues” with “little to no structural investment for the hospital.” It markets OBED success stories to potential customers, highlighting hospitals in California and South Florida where OBEDs reportedly improved patient care – and “produced additional revenue through OBED services.” OBHG, which staffs close to 200 OBEDs in 33 states, markets a scoring tool designed to help hospitals maximize charges from OBEDs and has marketed its services to about 3,000 hospitals.
Staffing companies and hospitals, contacted by KHN, said that OBEDs help deliver better care and that private equity involvement doesn’t impede that care.
Data from Colorado offers a window into how hospitals may be shifting the way they bill for triaging healthy labor. In an analysis for KHN, the Center for Improving Value in Health Care found that the share of uncomplicated vaginal deliveries that had an ED charge embedded in their bills more than doubled in Colorado from 2016 to 2020. It is still a small segment of births, however, rising from 1.4% to 3.3%.
Major staffing companies are set up to charge for every single little thing, said Wayne Farley, MD. He would know: He used to have a leadership role in one of those major staffing companies, the private equity-backed Envision, after it bought his previous employer. Now he’s a practicing ob.gyn. hospitalist at four OBEDs and a consultant who helps hospitals start OBEDs.
“I’ve actually thought about creating a business where I review billings for these patients and help them fight claims,” said Dr. Farley, who thinks a high-level emergency charge makes sense only if the patient had serious complications or required a high level of care.
Proponents of OBEDs say converting a triage room into an obstetrics ED can help pay for a hospital to hire 24/7 hospitalists. In labor and delivery, that means obstetric specialists are available purely to respond to patients who come to the hospital, rather than juggling those cases with clinic visits. Supporters of OBEDs say there’s evidence that having hospitalists on hand is safer for patients and can reduce unnecessary cesarean sections.
“That’s no excuse,” said Lawrence Casalino, MD, a physician and health policy researcher at Weill Cornell Medicine, New York. “To have people get an emergency room charge when they don’t even know they’re in an emergency room – I mean, that doesn’t meet the laugh test.”
But Christopher Swain, MD, who founded the OB Hospitalist Group and is credited with inventing the OBED concept, said that having round-the-clock hospitalists on staff is essential for giving pregnant patients good care and that starting an OBED can help pay for those hospitalists.
Dr. Swain said he started the nation’s first OBED in 2006 in Kissimmee, Fla. He said that, at early-adopter hospitals, OBEDs helped pay to have a doctor available on the labor-and-delivery floor 24/7 and that hospitals subsequently saw better outcomes and lower malpractice rates.
“We feel like we fixed something,” Dr. Swain said. “I feel like we really helped to move the bar to improve the quality of care and to provide better outcomes.”
Dr. Swain is no longer affiliated with OBHG, which has been in private equity hands since at least 2013. The company has recently gone so far as to present OBEDs as part of the solution to the country’s maternal mortality problem. Hospitals such as an Ascension St. Joseph’s hospital in Milwaukee have echoed that statement in their reasons for opening an OBED.
But Dr. Wachter – who coined the term “hospitalist” and who generally believes the presence of hospitalists leads to better care – thinks that reasoning is questionable, especially because hospitals find ways to pay for hospitalists in other specialties without engineering new facility fees.
“I’m always a little skeptical of the justification,” Dr. Wachter said. “They will always have a rationale for why income maximization is a reasonable and moral strategy.”
Private equity’s footprint in women’s health care
Dr. Farley estimates that he has helped set up OBEDs – including Colorado’s first in 2013 – in at least 30 hospitals. He’s aware of hospitals that claim they have OBEDs when the only change they’ve made is to have an ob.gyn. on site round the clock.
“You can’t just hang out a shingle and say: ‘We have an OBED.’ It’s an investment on the part of the hospital,” he said. That means having, among other things, a separate entrance from the rest of the labor-and-delivery department, clear signage inside and outside the hospital, and a separate waiting room. Some hospitals he has worked with have invested millions of dollars in upgrading facilities for their OBED.
Private equity firms often promise more efficient management, plus investment in technology and facilities that could improve patient care or satisfaction. In some parts of health care, that could really help, said Ambar La Forgia, PhD, who researches health care management at the University of California, Berkeley, and is studying private equity investment in fertility care. But Dr. La Forgia said that in much of health care, gauging whether such firms are truly maintaining or improving the quality of care is difficult.
“Private equity is about being able to extract some sort of value very quickly,” Dr. La Forgia said. “And in health care, when prices are so opaque and there’s so much lack of transparency, a lot of those impacts on the prices are eventually going to fall on the patient.”
It’s changing circumstances for doctors, too. Michelle Barhaghi, MD, a Colorado obstetrician, said OBEDs may make sense in busy, urban hospitals with lots of patients who did not get prenatal care. But now they’re cropping up everywhere. “From a doctor standpoint, none of us want these jobs because now we’re like a resident again, where we have to see every single patient that walks through that door,” said Dr. Barhaghi, rather than triaging many cases on the phone with a nurse.
Still, private equity is continuing its advance into women’s health care.
Indeed, Dr. Barhaghi said private equity came knocking on her door earlier this year: Women’s Care Enterprises, backed by private equity company BC Partners, wanted to know whether she would consider selling her practice. She said “no.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
How do patients with chronic urticaria fare during pregnancy?
In addition, the rates of preterm births and medical problems of newborns in patients with CU are similar to those of the normal population and not linked to treatment used during pregnancy.
Those are the key findings from an analysis of new data from PREG-CU, an international, multicenter study of the Urticaria Centers of Reference and Excellence (UCARE) network. Results from the first PREG-CU analysis published in 2021 found that CU improved in about half of patients with CU during pregnancy. “However, two in five patients reported acute exacerbations of CU especially at the beginning and end of pregnancy,” investigators led by Emek Kocatürk, MD, of the department of dermatology and UCARE at Koç University School of Medicine, Istanbul, wrote in the new study, recently published in the Journal of the European Academy of Dermatology and Venereology.
“In addition, 1 in 10 pregnant CU patients required urticaria emergency care and 1 of 6 had angioedema during pregnancy,” they said. Risk factors for worsening CU during pregnancy, they added, were “mild disease and no angioedema before pregnancy, not taking treatment before pregnancy, chronic inducible urticaria, CU worsening during a previous pregnancy, stress as a driver of exacerbations, and treatment during pregnancy.”
Analysis involved 288 pregnant women
To optimize treatment of CU during pregnancy and to better understand how treatment affects pregnancy outcomes, the researchers analyzed 288 pregnancies in 288 women with CU from 13 countries and 21 centers worldwide. Their mean age at pregnancy was 32.1 years, and their mean duration of CU was 84.9 months. Prior to pregnancy, 35.7% of patients rated the severity of their CU symptoms as mild, 34.2% rated it as moderate, and 29.7% rated it as severe.
The researchers found that during pregnancy, 60% of patients used urticaria medication, including standard-dose second-generation H1-antihistamines (35.1%), first-generation H1-antihistamines (7.6%), high-dose second-generation H1-antihistamines (5.6%), and omalizumab (5.6%). The preterm birth rate was 10.2%, which was similar between patients who did and did not receive treatment during pregnancy (11.6% vs. 8.7%, respectively; P = .59).
On multivariate logistic regression, two predictors for preterm birth emerged: giving birth to twins (a 13.3-fold increased risk; P = .016) and emergency referrals for CU (a 4.3-fold increased risk; P =.016). The cesarean delivery rate was 51.3%, and more than 90% of newborns were healthy at birth. There was no link between any patient or disease characteristics or treatments and medical problems at birth.
In other findings, 78.8% of women with CU breastfed their babies. Of the 58 patients who did not breastfeed, 20.7% indicated severe urticaria/angioedema and/or taking medications as the main reason for not breastfeeding.
“Most CU patients use treatment during pregnancy and such treatments, especially second generation H1 antihistamines, seem to be safe during pregnancy regardless of the trimester,” the researchers concluded. “Outcomes of pregnancy in patients with CU were similar compared to the general population and not linked to treatment used during pregnancy. Notably, emergency referral for CU was an independent risk factor for preterm birth,” and the high cesarean delivery rate was “probably linked to comorbidities associated with the disease,” they added. “Overall, these findings suggest that patients should continue their treatments using an individualized dose to provide optimal symptom control.”
International guidelines
The authors noted that international guidelines for the management of urticaria published in 2022 suggest that modern second-generation H1-antihistamines should be used for pregnant patients, preferably loratadine with a possible extrapolation to desloratadine, cetirizine, or levocetirizine.
“Similarly, in this population, we found that cetirizine and loratadine were the most commonly used antihistamines, followed by levocetirizine and fexofenadine,” Dr. Kocatürk and colleagues wrote.
“Guidelines also suggest that the use of first-generation H1-antihistamines should be avoided given their sedative effects; but if these are to be given, it would be wise to know that use of first-generation H1-antihistamines immediately before parturition could cause respiratory depression and other adverse effects in the neonate,” they added, noting that chlorpheniramine and diphenhydramine are the first-generation H1-antihistamines with the greatest evidence of safety in pregnancy.
They acknowledged certain limitations of the analysis, including its retrospective design and the fact that there were no data on low birth weight, small for gestational age, or miscarriage rates. In addition, disease activity or severity during pregnancy and after birth were not monitored.
Asked to comment on these results, Raj Chovatiya, MD, PhD, who directs the center for eczema and itch in the department of dermatology at Northwestern University, Chicago, noted that despite a higher prevalence of CU among females compared with males, very little is known about how the condition is managed during pregnancy. “This retrospective study shows that most patients continue to utilize CU treatment during pregnancy (primarily second-generation antihistamines), with similar birth outcomes as the general population,” he said. “Interestingly, cesarean rates were higher among mothers with CU, and emergency CU referral was a risk factor for preterm birth. While additional prospective studies are needed, these results suggest that CU patients should be carefully managed, particularly during pregnancy, when treatment should be optimized.”
Dr. Kocatürk reported having received personal fees from Novartis, Ibrahim Etem-Menarini, and Sanofi, outside the submitted work. Many coauthors reported having numerous financial disclosures. Dr. Chovatiya disclosed that he is a consultant to, a speaker for, and/or a member of the advisory board for AbbVie, Arcutis, Arena, Incyte, Pfizer, Regeneron, and Sanofi Genzyme.
In addition, the rates of preterm births and medical problems of newborns in patients with CU are similar to those of the normal population and not linked to treatment used during pregnancy.
Those are the key findings from an analysis of new data from PREG-CU, an international, multicenter study of the Urticaria Centers of Reference and Excellence (UCARE) network. Results from the first PREG-CU analysis published in 2021 found that CU improved in about half of patients with CU during pregnancy. “However, two in five patients reported acute exacerbations of CU especially at the beginning and end of pregnancy,” investigators led by Emek Kocatürk, MD, of the department of dermatology and UCARE at Koç University School of Medicine, Istanbul, wrote in the new study, recently published in the Journal of the European Academy of Dermatology and Venereology.
“In addition, 1 in 10 pregnant CU patients required urticaria emergency care and 1 of 6 had angioedema during pregnancy,” they said. Risk factors for worsening CU during pregnancy, they added, were “mild disease and no angioedema before pregnancy, not taking treatment before pregnancy, chronic inducible urticaria, CU worsening during a previous pregnancy, stress as a driver of exacerbations, and treatment during pregnancy.”
Analysis involved 288 pregnant women
To optimize treatment of CU during pregnancy and to better understand how treatment affects pregnancy outcomes, the researchers analyzed 288 pregnancies in 288 women with CU from 13 countries and 21 centers worldwide. Their mean age at pregnancy was 32.1 years, and their mean duration of CU was 84.9 months. Prior to pregnancy, 35.7% of patients rated the severity of their CU symptoms as mild, 34.2% rated it as moderate, and 29.7% rated it as severe.
The researchers found that during pregnancy, 60% of patients used urticaria medication, including standard-dose second-generation H1-antihistamines (35.1%), first-generation H1-antihistamines (7.6%), high-dose second-generation H1-antihistamines (5.6%), and omalizumab (5.6%). The preterm birth rate was 10.2%, which was similar between patients who did and did not receive treatment during pregnancy (11.6% vs. 8.7%, respectively; P = .59).
On multivariate logistic regression, two predictors for preterm birth emerged: giving birth to twins (a 13.3-fold increased risk; P = .016) and emergency referrals for CU (a 4.3-fold increased risk; P =.016). The cesarean delivery rate was 51.3%, and more than 90% of newborns were healthy at birth. There was no link between any patient or disease characteristics or treatments and medical problems at birth.
In other findings, 78.8% of women with CU breastfed their babies. Of the 58 patients who did not breastfeed, 20.7% indicated severe urticaria/angioedema and/or taking medications as the main reason for not breastfeeding.
“Most CU patients use treatment during pregnancy and such treatments, especially second generation H1 antihistamines, seem to be safe during pregnancy regardless of the trimester,” the researchers concluded. “Outcomes of pregnancy in patients with CU were similar compared to the general population and not linked to treatment used during pregnancy. Notably, emergency referral for CU was an independent risk factor for preterm birth,” and the high cesarean delivery rate was “probably linked to comorbidities associated with the disease,” they added. “Overall, these findings suggest that patients should continue their treatments using an individualized dose to provide optimal symptom control.”
International guidelines
The authors noted that international guidelines for the management of urticaria published in 2022 suggest that modern second-generation H1-antihistamines should be used for pregnant patients, preferably loratadine with a possible extrapolation to desloratadine, cetirizine, or levocetirizine.
“Similarly, in this population, we found that cetirizine and loratadine were the most commonly used antihistamines, followed by levocetirizine and fexofenadine,” Dr. Kocatürk and colleagues wrote.
“Guidelines also suggest that the use of first-generation H1-antihistamines should be avoided given their sedative effects; but if these are to be given, it would be wise to know that use of first-generation H1-antihistamines immediately before parturition could cause respiratory depression and other adverse effects in the neonate,” they added, noting that chlorpheniramine and diphenhydramine are the first-generation H1-antihistamines with the greatest evidence of safety in pregnancy.
They acknowledged certain limitations of the analysis, including its retrospective design and the fact that there were no data on low birth weight, small for gestational age, or miscarriage rates. In addition, disease activity or severity during pregnancy and after birth were not monitored.
Asked to comment on these results, Raj Chovatiya, MD, PhD, who directs the center for eczema and itch in the department of dermatology at Northwestern University, Chicago, noted that despite a higher prevalence of CU among females compared with males, very little is known about how the condition is managed during pregnancy. “This retrospective study shows that most patients continue to utilize CU treatment during pregnancy (primarily second-generation antihistamines), with similar birth outcomes as the general population,” he said. “Interestingly, cesarean rates were higher among mothers with CU, and emergency CU referral was a risk factor for preterm birth. While additional prospective studies are needed, these results suggest that CU patients should be carefully managed, particularly during pregnancy, when treatment should be optimized.”
Dr. Kocatürk reported having received personal fees from Novartis, Ibrahim Etem-Menarini, and Sanofi, outside the submitted work. Many coauthors reported having numerous financial disclosures. Dr. Chovatiya disclosed that he is a consultant to, a speaker for, and/or a member of the advisory board for AbbVie, Arcutis, Arena, Incyte, Pfizer, Regeneron, and Sanofi Genzyme.
In addition, the rates of preterm births and medical problems of newborns in patients with CU are similar to those of the normal population and not linked to treatment used during pregnancy.
Those are the key findings from an analysis of new data from PREG-CU, an international, multicenter study of the Urticaria Centers of Reference and Excellence (UCARE) network. Results from the first PREG-CU analysis published in 2021 found that CU improved in about half of patients with CU during pregnancy. “However, two in five patients reported acute exacerbations of CU especially at the beginning and end of pregnancy,” investigators led by Emek Kocatürk, MD, of the department of dermatology and UCARE at Koç University School of Medicine, Istanbul, wrote in the new study, recently published in the Journal of the European Academy of Dermatology and Venereology.
“In addition, 1 in 10 pregnant CU patients required urticaria emergency care and 1 of 6 had angioedema during pregnancy,” they said. Risk factors for worsening CU during pregnancy, they added, were “mild disease and no angioedema before pregnancy, not taking treatment before pregnancy, chronic inducible urticaria, CU worsening during a previous pregnancy, stress as a driver of exacerbations, and treatment during pregnancy.”
Analysis involved 288 pregnant women
To optimize treatment of CU during pregnancy and to better understand how treatment affects pregnancy outcomes, the researchers analyzed 288 pregnancies in 288 women with CU from 13 countries and 21 centers worldwide. Their mean age at pregnancy was 32.1 years, and their mean duration of CU was 84.9 months. Prior to pregnancy, 35.7% of patients rated the severity of their CU symptoms as mild, 34.2% rated it as moderate, and 29.7% rated it as severe.
The researchers found that during pregnancy, 60% of patients used urticaria medication, including standard-dose second-generation H1-antihistamines (35.1%), first-generation H1-antihistamines (7.6%), high-dose second-generation H1-antihistamines (5.6%), and omalizumab (5.6%). The preterm birth rate was 10.2%, which was similar between patients who did and did not receive treatment during pregnancy (11.6% vs. 8.7%, respectively; P = .59).
On multivariate logistic regression, two predictors for preterm birth emerged: giving birth to twins (a 13.3-fold increased risk; P = .016) and emergency referrals for CU (a 4.3-fold increased risk; P =.016). The cesarean delivery rate was 51.3%, and more than 90% of newborns were healthy at birth. There was no link between any patient or disease characteristics or treatments and medical problems at birth.
In other findings, 78.8% of women with CU breastfed their babies. Of the 58 patients who did not breastfeed, 20.7% indicated severe urticaria/angioedema and/or taking medications as the main reason for not breastfeeding.
“Most CU patients use treatment during pregnancy and such treatments, especially second generation H1 antihistamines, seem to be safe during pregnancy regardless of the trimester,” the researchers concluded. “Outcomes of pregnancy in patients with CU were similar compared to the general population and not linked to treatment used during pregnancy. Notably, emergency referral for CU was an independent risk factor for preterm birth,” and the high cesarean delivery rate was “probably linked to comorbidities associated with the disease,” they added. “Overall, these findings suggest that patients should continue their treatments using an individualized dose to provide optimal symptom control.”
International guidelines
The authors noted that international guidelines for the management of urticaria published in 2022 suggest that modern second-generation H1-antihistamines should be used for pregnant patients, preferably loratadine with a possible extrapolation to desloratadine, cetirizine, or levocetirizine.
“Similarly, in this population, we found that cetirizine and loratadine were the most commonly used antihistamines, followed by levocetirizine and fexofenadine,” Dr. Kocatürk and colleagues wrote.
“Guidelines also suggest that the use of first-generation H1-antihistamines should be avoided given their sedative effects; but if these are to be given, it would be wise to know that use of first-generation H1-antihistamines immediately before parturition could cause respiratory depression and other adverse effects in the neonate,” they added, noting that chlorpheniramine and diphenhydramine are the first-generation H1-antihistamines with the greatest evidence of safety in pregnancy.
They acknowledged certain limitations of the analysis, including its retrospective design and the fact that there were no data on low birth weight, small for gestational age, or miscarriage rates. In addition, disease activity or severity during pregnancy and after birth were not monitored.
Asked to comment on these results, Raj Chovatiya, MD, PhD, who directs the center for eczema and itch in the department of dermatology at Northwestern University, Chicago, noted that despite a higher prevalence of CU among females compared with males, very little is known about how the condition is managed during pregnancy. “This retrospective study shows that most patients continue to utilize CU treatment during pregnancy (primarily second-generation antihistamines), with similar birth outcomes as the general population,” he said. “Interestingly, cesarean rates were higher among mothers with CU, and emergency CU referral was a risk factor for preterm birth. While additional prospective studies are needed, these results suggest that CU patients should be carefully managed, particularly during pregnancy, when treatment should be optimized.”
Dr. Kocatürk reported having received personal fees from Novartis, Ibrahim Etem-Menarini, and Sanofi, outside the submitted work. Many coauthors reported having numerous financial disclosures. Dr. Chovatiya disclosed that he is a consultant to, a speaker for, and/or a member of the advisory board for AbbVie, Arcutis, Arena, Incyte, Pfizer, Regeneron, and Sanofi Genzyme.
FROM JEADV
Viral threats to the fetus and mother: Parvovirus and varicella
We review 2 important viral infections in this article. One, parvovirus, poses a major threat to the fetus. The second, varicella, poses less risk to the fetus but significantly greater risk to the mother. We focus on the epidemiology, clinical presentation, diagnosis, and management of each infection.
Parvovirus infection and its risks to the fetus
CASE #1 Pregnant teacher exposed to fifth disease
A 28-year-old primigravid woman at 16 weeks’ gestation works as an elementary school teacher. Over the past 3 weeks, she has been exposed to 4 children who had fifth disease. She now requests evaluation because she has malaise, arthralgias, myalgias, fever of 38.2°C, and a fine lacelike erythematous rash on her trunk, arms, and cheeks.
- What is the most likely diagnosis?
- What diagnostic tests are indicated?
- Is her fetus at risk?
Epidemiology of parvovirus
Parvovirus B19 is a small, single-stranded DNA virus. It is highly contagious and is transmitted primarily by respiratory droplets. Transmission also can occur via infected blood, for example, through a blood transfusion. The incubation period is 10 to 20 days. Among adults, the individuals at greatest risk for infection are those who have close contact with young children, such as parents, day-care workers, and elementary school teachers. With sustained exposure in the household or classroom, the risk of seroconversion approaches 50%.1 Approximately 50% to 60% of reproductive-aged women have evidence of prior infection, and immunity is usually lifelong.
Clinical manifestations
The classic presentation of parvovirus infection is erythema infectiosum, also called fifth disease. This condition is characterized by a “slapped cheek” facial rash, malaise, myalgias, arthralgias, and low-grade fever. A fine lacelike rash often develops over the torso. In adults, the characteristic rash may be absent, and the most common presentation is a flu-like illness with joint pains.1,2 In children and in adults with an underlying hemoglobinopathy, parvovirus can cause transient aplastic crisis, and patients present with signs of a severe anemia, such as dyspnea, pallor, and fatigue.
Although parvovirus infection usually poses no serious risk in otherwise healthy children and adults, it can cause major fetal injury when the pregnant woman is infected early in pregnancy. The principal manifestation of fetal infection is hydrops. Hydrops primarily results when the virus crosses the placenta and attaches to the P antigen on the surface of red cell progenitors in the fetal marrow, causing an aplastic anemia with resultant high-output congestive heart failure. The virus also may directly injure the fetal myocardium, thus exacerbating heart failure. Other manifestations of congenital parvovirus include thrombocytopenia and hepatitis.3
The severity of fetal injury is inversely proportional to the gestational age at the time of maternal infection. When primary maternal infection occurs in the first trimester, the frequency of fetal hydrops is 5% to 10%. If infection develops in weeks 13 to 20, the risk of hydrops decreases to 5% or less. If infection develops beyond week 20, the incidence of fetal hydrops is 1% or lower.2
Continue to: Diagnostic steps...
Diagnostic steps
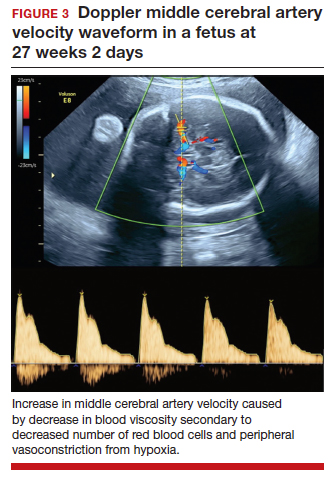
Appropriate diagnostic evaluation for a pregnant woman with exposure to parvovirus or clinical manifestations suggestive of parvovirus infection is outlined in FIGURE 1.
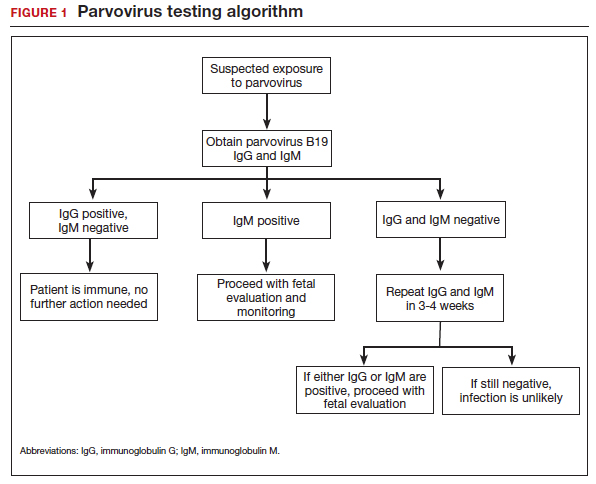
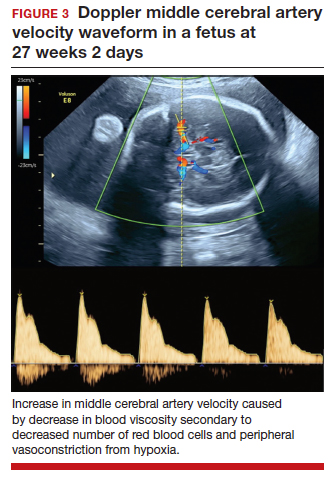
If infection is confirmed, serial ultrasound monitoring should be performed on a weekly to biweekly basis for 8 to 12 weeks, as delineated in FIGURE 2. Extended surveillance is necessary because the incubation period in the fetus is longer than that in the mother.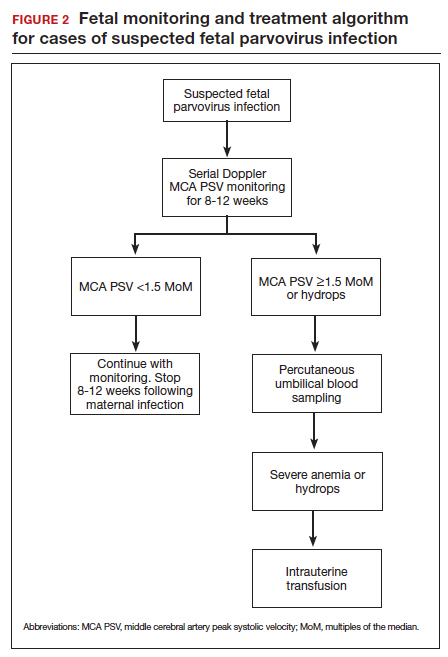
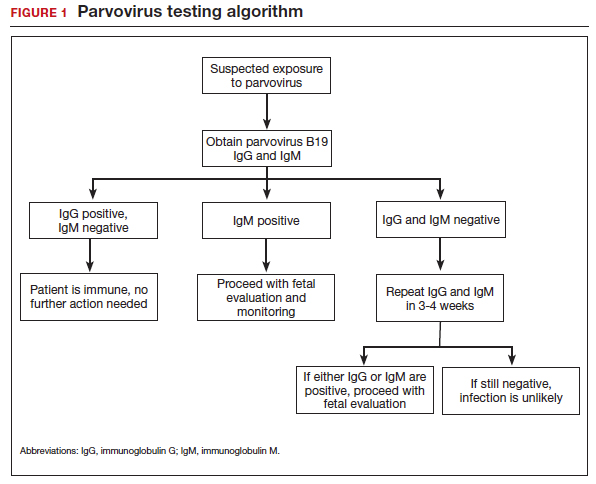
As the fetus develops anemia, peripheral tissues become hypoxic, leading to reflex peripheral vasoconstriction and increased cardiac output. At the same time, reduction in the number of fetal red blood cells decreases blood viscosity. The combination of these changes results in an increase in blood flow to the fetal brain, which can be detected by measuring the peak systolic velocity of flow in the middle cerebral artery (MCA PSV) with Doppler ultrasound imaging (FIGURE 3). The increase in MCA PSV parallels the decrease in fetal hematocrit and precedes the development of hydrops. In fact, signs of fetal hydrops do not usually develop until the fetal hematocrit falls to 15 to 20 vol%.
Management may necessitate intrauterine transfusion
Although some cases of fetal hydrops may resolve spontaneously, most authors agree that intrauterine transfusion is essential. In most instances, only a single intrauterine transfusion is necessary. In some fetuses, however, the infection is so prolonged and the anemia so severe that 2 to 3 transfusions may be required.
Infants who survive the intrauterine transfusion usually have an excellent long-term prognosis. However, isolated case reports have documented neurologic morbidity and prolonged transfusion-dependent anemia.4 In light of these reports, we recommend that a third trimester ultrasound exam be performed to assess fetal growth and evaluate the anatomy of the fetal brain. For the fetus with abnormal intracranial findings on ultrasonography, fetal magnetic resonance imaging is indicated.5
CASE #1 Diagnosis is probable parvovirus
The most likely diagnosis in this case is erythema infectiosum. This diagnosis can be confirmed by identifying positive immunogloblulin M (IgM) antibody and by detecting parvovirus in the maternal serum by polymerase chain reaction. Given the gestational age of 16 weeks, the risk of serious fetal injury should be less than 5%. Nevertheless, serial ultrasound examinations should be performed to assess for signs of fetal anemia.
Varicella exposure in pregnancy
CASE #2 Pregnant woman exposed to chickenpox has symptoms
Two weeks ago, a 32-year-old woman (G3P2002) at 24 weeks’ gestation was exposed to a neighbor’s child who had chickenpox. The patient has no history of natural infection or vaccination. She now has a fever of 38.6°C, malaise, headache, and a diffuse pruritic vesicular rash on her trunk and extremities. She also is experiencing a dry cough and mild dyspnea.
- What diagnostic tests are indicated?
- What treatment is indicated?
- What risk does this condition pose to the fetus?
Epidemiology of varicella
Varicella (chickenpox) is caused by the DNA varicella-zoster virus, an organism that is a member of the herpesvirus family. The disease occurs predominantly in children, and the infection is transmitted by respiratory droplets and by direct contact. Its incubation period is short (10–14 days), and it is highly contagious. More than 90% of susceptible close contacts will become infected after exposure to the index case. Like other herpesviruses, the varicella virus can establish a latent infection and then become manifest years later as herpes zoster (shingles).5,6
Continue to: Clinical manifestations...
Clinical manifestations
Patients with varicella usually have prodromal symptoms and signs that include malaise, fatigue, arthralgias, myalgias, and a low-grade fever. Varicella’s pathognomonic manifestation is a pruritic, macular rash that starts on the face and trunk and then spreads centripetally to the extremities. The lesions typically appear in “crops” and evolve through several distinct phases: macule, papule, vesicle, pustule, ulcer, and crust.5
In children, varicella is manifest almost entirely by mucocutaneous lesions. In adults, however, 2 serious and potentially life-threatening complications can occur. Approximately 1% of infected adults develop encephalitis and about 20% develop viral pneumonia, often accompanied by a severe superimposed bacterial pneumonia.5
When maternal infection develops in the first half of pregnancy, approximately 2% of fetuses will have evidence of congenital infection, usually manifested by circular, constricting scars on the extremities. These lesions typically occur in a dermatomal distribution. Spontaneous abortion and fetal death in utero also have been reported, but fortunately they are quite rare. When maternal infection occurs beyond 20 weeks of gestation, fetal injury is very uncommon.7
Interestingly, when maternal infection occurs at the time of delivery or shortly thereafter (from 5 days before until 2 days after delivery), neonatal varicella may develop. This infection may take 3 forms: disseminated mucocutaneous lesions, a deep-seated visceral infection, or severe pneumonia. In the era before the ready availability of antiviral agents, the case fatality rate from neonatal varicella was approximately 30%.5
Diagnosis is clinical
The diagnosis of varicella usually is established on the basis of clinical examination. It can be confirmed by identification of anti–varicella-zoster IgM.
Management includes assessing immunity
If a patient is seen for a preconception appointment, ask her whether she has ever had varicella or been vaccinated for this disease. If she is uncertain, a varicella-zoster immunoglobulin G (IgG) titer should be ordered. If the IgG titer is negative, denoting susceptibility to infection, the patient should be vaccinated before she tries to conceive (see below).8
If a patient has not had a preconception appointment and now presents for her first prenatal appointment, she should be asked about immunity to varicella. If she is uncertain, a varicella-zoster IgG assay should be obtained. Approximately 75% of patients who are uncertain about immunity will, in fact, be immune. Those who are not immune should be counseled to avoid exposure to individuals who may have varicella, and they should be targeted for vaccination immediately postpartum.5,9
If a susceptible pregnant patient has been exposed to an individual with varicella, she should receive 1 of 2 regimens within 72 to 96 hours to minimize the risk of maternal infection.5,9,10 One option is intramuscular varicella-zoster immune globulin (VariZIG), 125 U/10 kg body weight, with a maximum dose of 625 U (5 vials). The distributor of this agent is FFF Enterprises in Temucula, California (telephone: 800-843-7477). A company representative will assess the patient’s eligibility and deliver the drug within 24 hours if the patient is considered eligible. An alternative prophylactic regimen is oral acyclovir, 800 mg 5 times daily for 7 days, or oral valacyclovir, 1,000 mg 3 times daily for 7 days.
If, despite prophylaxis, the pregnant woman becomes infected, she should immediately be treated with 1 of the oral antiviral regimens described above. If she has evidence of encephalitis, pneumonia, or severe disseminated mucocutaneous infection, or if she is immunosuppressed, she should be hospitalized and treated with intravenous acyclovir, 10 mg/kg infused over 1 hour every 8 hours for 10 days.
Ultrasonography is the most valuable test to identify fetal infection. Key findings that suggest congenital varicella are fetal growth restriction, microcephaly, ventriculomegaly, echogenic foci in the liver, and limb abnormalities. There is no proven therapy for congenital varicella.
When a patient has varicella at the time of delivery, she should be isolated from her infant until all lesions have crusted over. In addition, the neonate should be treated with either VariZIG or an antiviral agent.5,9
Prevention with varicella vaccine
The varicella vaccine (Varivax) is a live-virus vaccine that is highly immunogenic. The vaccine is now part of the routine childhood immunization sequence. Children ages 1 to 12 years require only a single dose of the vaccine. Individuals older than 12 years of age require 2 doses, administered 4 to 6 weeks apart. The vaccine should not be administered during pregnancy. It also should not be administered to individuals who are severely immunocompromised, are receiving high-dose systemic steroids, have untreated tuberculosis, or have an allergy to neomycin, which is a component of the vaccine. The vaccine does not pose a risk to the breastfeeding infant.11
CASE #2 Hospitalization is recommended for this patient
The patient in this case developed acute varicella pneumonia as a result of her exposure to the neighbor’s child. The diagnosis can be confirmed by demonstrating a positive varicella-zoster IgM and by obtaining a chest x-ray that identifies the diffuse patchy infiltrates characteristic of viral pneumonia. Because this is such a potentially serious illness, the patient should be hospitalized and treated with intravenous acyclovir or valacyclovir. Antibiotics such as ceftriaxone and azithromycin may be indicated to treat superimposed bacterial pneumonia. Given the later gestational age, the fetus is at low risk for serious injury. ●
- Valeur-Jensen AK, Pedersen CB, Westergaard T, et al. Risk factors for parvovirus B19 infection in pregnancy. JAMA. 1999;281:1099-1105.
- Harger JH, Adler SP, Koch WC, et al. Prospective evaluation of 618 pregnant women exposed to parvovirus B19: risks and symptoms. Obstet Gynecol. 1998;91:413-420.
- Melamed N, Whittle W, Kelly EN, et al. Fetal thrombocytopenia in pregnancies with fetal human parvovirus-B19 infection. Am J Obstet Gynecol. 2015;212:793.e1-8.
- Nagel HTC, de Haan TR, Vandenbussche FPH, et al. Long-term outcome after fetal transfusion for hydrops associated with parvovirus B19 infection. Obstet Gynecol. 2007;109:42-47.
- Duff P. Maternal and fetal infections. In: Resnik R, Lockwood CJ, Moore TR, et al (eds). Creasy & Resnik’s Maternal-Fetal Medicine: Principles and Practice. 8th ed. Elsevier; 2019:911-912.
- Cohen JI. Herpes zoster. N Engl J Med. 2013;369:255-263.
- Enders G, Miller E, Cradock-Watson J, et al. Consequences of varicella and herpes zoster in pregnancy: prospective study of 1739 cases. Lancet. 1994;343:1548-1551.
- Duff P. Varicella in pregnancy: five priorities for clinicians. Infect Dis Obstet Gynecol. 1994;1:163-165.
- Marin M, Guris D, Chaves SS, et al; Advisory Committee on Immunization Practices, Centers for Disease Control and Prevention. Prevention of varicella. MMWR Recommend Rep. 2007;56(RR-4):1-40.
- Swamy GK, Dotters-Katz SK. Safety and varicella outcomes after varicella zoster immune globulin administration in pregnancy. Am J Obstet Gynecol. 2019;221:655-656.
- Duff P. Varicella vaccine. Infect Dis Obstet Gynecol. 1996;4:63-65.
We review 2 important viral infections in this article. One, parvovirus, poses a major threat to the fetus. The second, varicella, poses less risk to the fetus but significantly greater risk to the mother. We focus on the epidemiology, clinical presentation, diagnosis, and management of each infection.
Parvovirus infection and its risks to the fetus
CASE #1 Pregnant teacher exposed to fifth disease
A 28-year-old primigravid woman at 16 weeks’ gestation works as an elementary school teacher. Over the past 3 weeks, she has been exposed to 4 children who had fifth disease. She now requests evaluation because she has malaise, arthralgias, myalgias, fever of 38.2°C, and a fine lacelike erythematous rash on her trunk, arms, and cheeks.
- What is the most likely diagnosis?
- What diagnostic tests are indicated?
- Is her fetus at risk?
Epidemiology of parvovirus
Parvovirus B19 is a small, single-stranded DNA virus. It is highly contagious and is transmitted primarily by respiratory droplets. Transmission also can occur via infected blood, for example, through a blood transfusion. The incubation period is 10 to 20 days. Among adults, the individuals at greatest risk for infection are those who have close contact with young children, such as parents, day-care workers, and elementary school teachers. With sustained exposure in the household or classroom, the risk of seroconversion approaches 50%.1 Approximately 50% to 60% of reproductive-aged women have evidence of prior infection, and immunity is usually lifelong.
Clinical manifestations
The classic presentation of parvovirus infection is erythema infectiosum, also called fifth disease. This condition is characterized by a “slapped cheek” facial rash, malaise, myalgias, arthralgias, and low-grade fever. A fine lacelike rash often develops over the torso. In adults, the characteristic rash may be absent, and the most common presentation is a flu-like illness with joint pains.1,2 In children and in adults with an underlying hemoglobinopathy, parvovirus can cause transient aplastic crisis, and patients present with signs of a severe anemia, such as dyspnea, pallor, and fatigue.
Although parvovirus infection usually poses no serious risk in otherwise healthy children and adults, it can cause major fetal injury when the pregnant woman is infected early in pregnancy. The principal manifestation of fetal infection is hydrops. Hydrops primarily results when the virus crosses the placenta and attaches to the P antigen on the surface of red cell progenitors in the fetal marrow, causing an aplastic anemia with resultant high-output congestive heart failure. The virus also may directly injure the fetal myocardium, thus exacerbating heart failure. Other manifestations of congenital parvovirus include thrombocytopenia and hepatitis.3
The severity of fetal injury is inversely proportional to the gestational age at the time of maternal infection. When primary maternal infection occurs in the first trimester, the frequency of fetal hydrops is 5% to 10%. If infection develops in weeks 13 to 20, the risk of hydrops decreases to 5% or less. If infection develops beyond week 20, the incidence of fetal hydrops is 1% or lower.2
Continue to: Diagnostic steps...
Diagnostic steps
Appropriate diagnostic evaluation for a pregnant woman with exposure to parvovirus or clinical manifestations suggestive of parvovirus infection is outlined in FIGURE 1.
If infection is confirmed, serial ultrasound monitoring should be performed on a weekly to biweekly basis for 8 to 12 weeks, as delineated in FIGURE 2. Extended surveillance is necessary because the incubation period in the fetus is longer than that in the mother.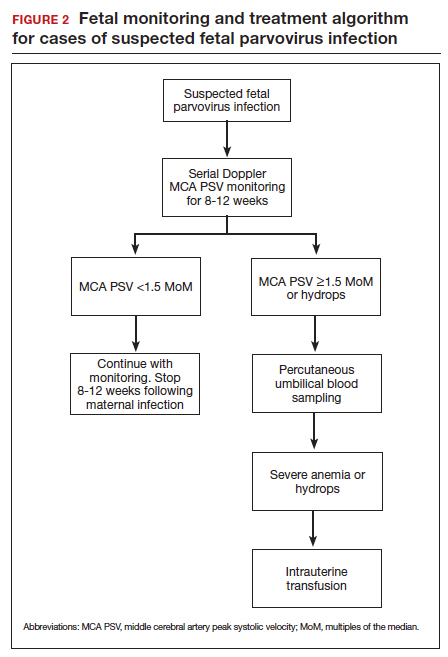
As the fetus develops anemia, peripheral tissues become hypoxic, leading to reflex peripheral vasoconstriction and increased cardiac output. At the same time, reduction in the number of fetal red blood cells decreases blood viscosity. The combination of these changes results in an increase in blood flow to the fetal brain, which can be detected by measuring the peak systolic velocity of flow in the middle cerebral artery (MCA PSV) with Doppler ultrasound imaging (FIGURE 3). The increase in MCA PSV parallels the decrease in fetal hematocrit and precedes the development of hydrops. In fact, signs of fetal hydrops do not usually develop until the fetal hematocrit falls to 15 to 20 vol%.
Management may necessitate intrauterine transfusion
Although some cases of fetal hydrops may resolve spontaneously, most authors agree that intrauterine transfusion is essential. In most instances, only a single intrauterine transfusion is necessary. In some fetuses, however, the infection is so prolonged and the anemia so severe that 2 to 3 transfusions may be required.
Infants who survive the intrauterine transfusion usually have an excellent long-term prognosis. However, isolated case reports have documented neurologic morbidity and prolonged transfusion-dependent anemia.4 In light of these reports, we recommend that a third trimester ultrasound exam be performed to assess fetal growth and evaluate the anatomy of the fetal brain. For the fetus with abnormal intracranial findings on ultrasonography, fetal magnetic resonance imaging is indicated.5
CASE #1 Diagnosis is probable parvovirus
The most likely diagnosis in this case is erythema infectiosum. This diagnosis can be confirmed by identifying positive immunogloblulin M (IgM) antibody and by detecting parvovirus in the maternal serum by polymerase chain reaction. Given the gestational age of 16 weeks, the risk of serious fetal injury should be less than 5%. Nevertheless, serial ultrasound examinations should be performed to assess for signs of fetal anemia.
Varicella exposure in pregnancy
CASE #2 Pregnant woman exposed to chickenpox has symptoms
Two weeks ago, a 32-year-old woman (G3P2002) at 24 weeks’ gestation was exposed to a neighbor’s child who had chickenpox. The patient has no history of natural infection or vaccination. She now has a fever of 38.6°C, malaise, headache, and a diffuse pruritic vesicular rash on her trunk and extremities. She also is experiencing a dry cough and mild dyspnea.
- What diagnostic tests are indicated?
- What treatment is indicated?
- What risk does this condition pose to the fetus?
Epidemiology of varicella
Varicella (chickenpox) is caused by the DNA varicella-zoster virus, an organism that is a member of the herpesvirus family. The disease occurs predominantly in children, and the infection is transmitted by respiratory droplets and by direct contact. Its incubation period is short (10–14 days), and it is highly contagious. More than 90% of susceptible close contacts will become infected after exposure to the index case. Like other herpesviruses, the varicella virus can establish a latent infection and then become manifest years later as herpes zoster (shingles).5,6
Continue to: Clinical manifestations...
Clinical manifestations
Patients with varicella usually have prodromal symptoms and signs that include malaise, fatigue, arthralgias, myalgias, and a low-grade fever. Varicella’s pathognomonic manifestation is a pruritic, macular rash that starts on the face and trunk and then spreads centripetally to the extremities. The lesions typically appear in “crops” and evolve through several distinct phases: macule, papule, vesicle, pustule, ulcer, and crust.5
In children, varicella is manifest almost entirely by mucocutaneous lesions. In adults, however, 2 serious and potentially life-threatening complications can occur. Approximately 1% of infected adults develop encephalitis and about 20% develop viral pneumonia, often accompanied by a severe superimposed bacterial pneumonia.5
When maternal infection develops in the first half of pregnancy, approximately 2% of fetuses will have evidence of congenital infection, usually manifested by circular, constricting scars on the extremities. These lesions typically occur in a dermatomal distribution. Spontaneous abortion and fetal death in utero also have been reported, but fortunately they are quite rare. When maternal infection occurs beyond 20 weeks of gestation, fetal injury is very uncommon.7
Interestingly, when maternal infection occurs at the time of delivery or shortly thereafter (from 5 days before until 2 days after delivery), neonatal varicella may develop. This infection may take 3 forms: disseminated mucocutaneous lesions, a deep-seated visceral infection, or severe pneumonia. In the era before the ready availability of antiviral agents, the case fatality rate from neonatal varicella was approximately 30%.5
Diagnosis is clinical
The diagnosis of varicella usually is established on the basis of clinical examination. It can be confirmed by identification of anti–varicella-zoster IgM.
Management includes assessing immunity
If a patient is seen for a preconception appointment, ask her whether she has ever had varicella or been vaccinated for this disease. If she is uncertain, a varicella-zoster immunoglobulin G (IgG) titer should be ordered. If the IgG titer is negative, denoting susceptibility to infection, the patient should be vaccinated before she tries to conceive (see below).8
If a patient has not had a preconception appointment and now presents for her first prenatal appointment, she should be asked about immunity to varicella. If she is uncertain, a varicella-zoster IgG assay should be obtained. Approximately 75% of patients who are uncertain about immunity will, in fact, be immune. Those who are not immune should be counseled to avoid exposure to individuals who may have varicella, and they should be targeted for vaccination immediately postpartum.5,9
If a susceptible pregnant patient has been exposed to an individual with varicella, she should receive 1 of 2 regimens within 72 to 96 hours to minimize the risk of maternal infection.5,9,10 One option is intramuscular varicella-zoster immune globulin (VariZIG), 125 U/10 kg body weight, with a maximum dose of 625 U (5 vials). The distributor of this agent is FFF Enterprises in Temucula, California (telephone: 800-843-7477). A company representative will assess the patient’s eligibility and deliver the drug within 24 hours if the patient is considered eligible. An alternative prophylactic regimen is oral acyclovir, 800 mg 5 times daily for 7 days, or oral valacyclovir, 1,000 mg 3 times daily for 7 days.
If, despite prophylaxis, the pregnant woman becomes infected, she should immediately be treated with 1 of the oral antiviral regimens described above. If she has evidence of encephalitis, pneumonia, or severe disseminated mucocutaneous infection, or if she is immunosuppressed, she should be hospitalized and treated with intravenous acyclovir, 10 mg/kg infused over 1 hour every 8 hours for 10 days.
Ultrasonography is the most valuable test to identify fetal infection. Key findings that suggest congenital varicella are fetal growth restriction, microcephaly, ventriculomegaly, echogenic foci in the liver, and limb abnormalities. There is no proven therapy for congenital varicella.
When a patient has varicella at the time of delivery, she should be isolated from her infant until all lesions have crusted over. In addition, the neonate should be treated with either VariZIG or an antiviral agent.5,9
Prevention with varicella vaccine
The varicella vaccine (Varivax) is a live-virus vaccine that is highly immunogenic. The vaccine is now part of the routine childhood immunization sequence. Children ages 1 to 12 years require only a single dose of the vaccine. Individuals older than 12 years of age require 2 doses, administered 4 to 6 weeks apart. The vaccine should not be administered during pregnancy. It also should not be administered to individuals who are severely immunocompromised, are receiving high-dose systemic steroids, have untreated tuberculosis, or have an allergy to neomycin, which is a component of the vaccine. The vaccine does not pose a risk to the breastfeeding infant.11
CASE #2 Hospitalization is recommended for this patient
The patient in this case developed acute varicella pneumonia as a result of her exposure to the neighbor’s child. The diagnosis can be confirmed by demonstrating a positive varicella-zoster IgM and by obtaining a chest x-ray that identifies the diffuse patchy infiltrates characteristic of viral pneumonia. Because this is such a potentially serious illness, the patient should be hospitalized and treated with intravenous acyclovir or valacyclovir. Antibiotics such as ceftriaxone and azithromycin may be indicated to treat superimposed bacterial pneumonia. Given the later gestational age, the fetus is at low risk for serious injury. ●
We review 2 important viral infections in this article. One, parvovirus, poses a major threat to the fetus. The second, varicella, poses less risk to the fetus but significantly greater risk to the mother. We focus on the epidemiology, clinical presentation, diagnosis, and management of each infection.
Parvovirus infection and its risks to the fetus
CASE #1 Pregnant teacher exposed to fifth disease
A 28-year-old primigravid woman at 16 weeks’ gestation works as an elementary school teacher. Over the past 3 weeks, she has been exposed to 4 children who had fifth disease. She now requests evaluation because she has malaise, arthralgias, myalgias, fever of 38.2°C, and a fine lacelike erythematous rash on her trunk, arms, and cheeks.
- What is the most likely diagnosis?
- What diagnostic tests are indicated?
- Is her fetus at risk?
Epidemiology of parvovirus
Parvovirus B19 is a small, single-stranded DNA virus. It is highly contagious and is transmitted primarily by respiratory droplets. Transmission also can occur via infected blood, for example, through a blood transfusion. The incubation period is 10 to 20 days. Among adults, the individuals at greatest risk for infection are those who have close contact with young children, such as parents, day-care workers, and elementary school teachers. With sustained exposure in the household or classroom, the risk of seroconversion approaches 50%.1 Approximately 50% to 60% of reproductive-aged women have evidence of prior infection, and immunity is usually lifelong.
Clinical manifestations
The classic presentation of parvovirus infection is erythema infectiosum, also called fifth disease. This condition is characterized by a “slapped cheek” facial rash, malaise, myalgias, arthralgias, and low-grade fever. A fine lacelike rash often develops over the torso. In adults, the characteristic rash may be absent, and the most common presentation is a flu-like illness with joint pains.1,2 In children and in adults with an underlying hemoglobinopathy, parvovirus can cause transient aplastic crisis, and patients present with signs of a severe anemia, such as dyspnea, pallor, and fatigue.
Although parvovirus infection usually poses no serious risk in otherwise healthy children and adults, it can cause major fetal injury when the pregnant woman is infected early in pregnancy. The principal manifestation of fetal infection is hydrops. Hydrops primarily results when the virus crosses the placenta and attaches to the P antigen on the surface of red cell progenitors in the fetal marrow, causing an aplastic anemia with resultant high-output congestive heart failure. The virus also may directly injure the fetal myocardium, thus exacerbating heart failure. Other manifestations of congenital parvovirus include thrombocytopenia and hepatitis.3
The severity of fetal injury is inversely proportional to the gestational age at the time of maternal infection. When primary maternal infection occurs in the first trimester, the frequency of fetal hydrops is 5% to 10%. If infection develops in weeks 13 to 20, the risk of hydrops decreases to 5% or less. If infection develops beyond week 20, the incidence of fetal hydrops is 1% or lower.2
Continue to: Diagnostic steps...
Diagnostic steps
Appropriate diagnostic evaluation for a pregnant woman with exposure to parvovirus or clinical manifestations suggestive of parvovirus infection is outlined in FIGURE 1.
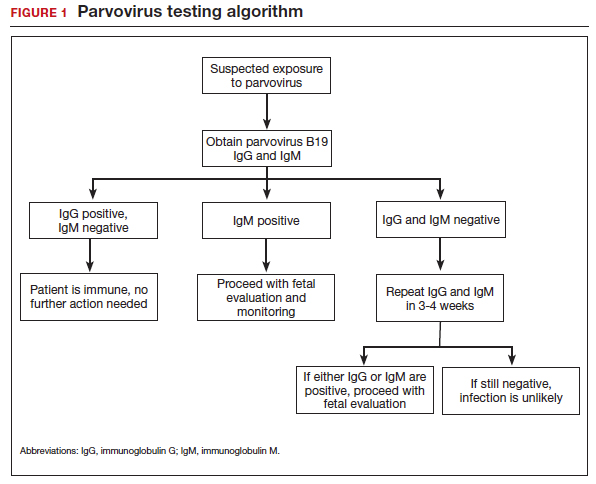
If infection is confirmed, serial ultrasound monitoring should be performed on a weekly to biweekly basis for 8 to 12 weeks, as delineated in FIGURE 2. Extended surveillance is necessary because the incubation period in the fetus is longer than that in the mother.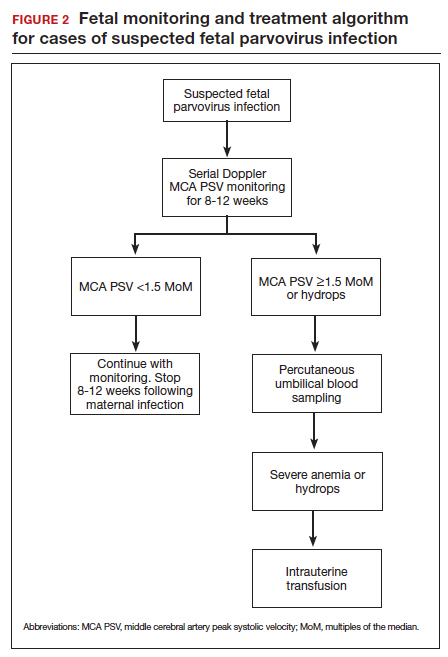
As the fetus develops anemia, peripheral tissues become hypoxic, leading to reflex peripheral vasoconstriction and increased cardiac output. At the same time, reduction in the number of fetal red blood cells decreases blood viscosity. The combination of these changes results in an increase in blood flow to the fetal brain, which can be detected by measuring the peak systolic velocity of flow in the middle cerebral artery (MCA PSV) with Doppler ultrasound imaging (FIGURE 3). The increase in MCA PSV parallels the decrease in fetal hematocrit and precedes the development of hydrops. In fact, signs of fetal hydrops do not usually develop until the fetal hematocrit falls to 15 to 20 vol%.
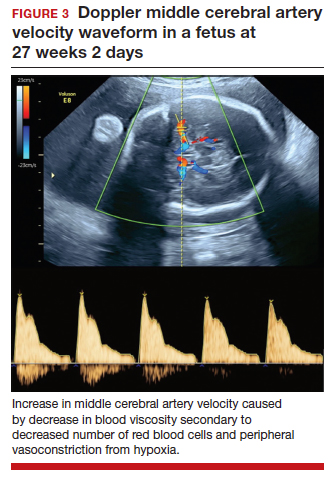
Management may necessitate intrauterine transfusion
Although some cases of fetal hydrops may resolve spontaneously, most authors agree that intrauterine transfusion is essential. In most instances, only a single intrauterine transfusion is necessary. In some fetuses, however, the infection is so prolonged and the anemia so severe that 2 to 3 transfusions may be required.
Infants who survive the intrauterine transfusion usually have an excellent long-term prognosis. However, isolated case reports have documented neurologic morbidity and prolonged transfusion-dependent anemia.4 In light of these reports, we recommend that a third trimester ultrasound exam be performed to assess fetal growth and evaluate the anatomy of the fetal brain. For the fetus with abnormal intracranial findings on ultrasonography, fetal magnetic resonance imaging is indicated.5
CASE #1 Diagnosis is probable parvovirus
The most likely diagnosis in this case is erythema infectiosum. This diagnosis can be confirmed by identifying positive immunogloblulin M (IgM) antibody and by detecting parvovirus in the maternal serum by polymerase chain reaction. Given the gestational age of 16 weeks, the risk of serious fetal injury should be less than 5%. Nevertheless, serial ultrasound examinations should be performed to assess for signs of fetal anemia.
Varicella exposure in pregnancy
CASE #2 Pregnant woman exposed to chickenpox has symptoms
Two weeks ago, a 32-year-old woman (G3P2002) at 24 weeks’ gestation was exposed to a neighbor’s child who had chickenpox. The patient has no history of natural infection or vaccination. She now has a fever of 38.6°C, malaise, headache, and a diffuse pruritic vesicular rash on her trunk and extremities. She also is experiencing a dry cough and mild dyspnea.
- What diagnostic tests are indicated?
- What treatment is indicated?
- What risk does this condition pose to the fetus?
Epidemiology of varicella
Varicella (chickenpox) is caused by the DNA varicella-zoster virus, an organism that is a member of the herpesvirus family. The disease occurs predominantly in children, and the infection is transmitted by respiratory droplets and by direct contact. Its incubation period is short (10–14 days), and it is highly contagious. More than 90% of susceptible close contacts will become infected after exposure to the index case. Like other herpesviruses, the varicella virus can establish a latent infection and then become manifest years later as herpes zoster (shingles).5,6
Continue to: Clinical manifestations...
Clinical manifestations
Patients with varicella usually have prodromal symptoms and signs that include malaise, fatigue, arthralgias, myalgias, and a low-grade fever. Varicella’s pathognomonic manifestation is a pruritic, macular rash that starts on the face and trunk and then spreads centripetally to the extremities. The lesions typically appear in “crops” and evolve through several distinct phases: macule, papule, vesicle, pustule, ulcer, and crust.5
In children, varicella is manifest almost entirely by mucocutaneous lesions. In adults, however, 2 serious and potentially life-threatening complications can occur. Approximately 1% of infected adults develop encephalitis and about 20% develop viral pneumonia, often accompanied by a severe superimposed bacterial pneumonia.5
When maternal infection develops in the first half of pregnancy, approximately 2% of fetuses will have evidence of congenital infection, usually manifested by circular, constricting scars on the extremities. These lesions typically occur in a dermatomal distribution. Spontaneous abortion and fetal death in utero also have been reported, but fortunately they are quite rare. When maternal infection occurs beyond 20 weeks of gestation, fetal injury is very uncommon.7
Interestingly, when maternal infection occurs at the time of delivery or shortly thereafter (from 5 days before until 2 days after delivery), neonatal varicella may develop. This infection may take 3 forms: disseminated mucocutaneous lesions, a deep-seated visceral infection, or severe pneumonia. In the era before the ready availability of antiviral agents, the case fatality rate from neonatal varicella was approximately 30%.5
Diagnosis is clinical
The diagnosis of varicella usually is established on the basis of clinical examination. It can be confirmed by identification of anti–varicella-zoster IgM.
Management includes assessing immunity
If a patient is seen for a preconception appointment, ask her whether she has ever had varicella or been vaccinated for this disease. If she is uncertain, a varicella-zoster immunoglobulin G (IgG) titer should be ordered. If the IgG titer is negative, denoting susceptibility to infection, the patient should be vaccinated before she tries to conceive (see below).8
If a patient has not had a preconception appointment and now presents for her first prenatal appointment, she should be asked about immunity to varicella. If she is uncertain, a varicella-zoster IgG assay should be obtained. Approximately 75% of patients who are uncertain about immunity will, in fact, be immune. Those who are not immune should be counseled to avoid exposure to individuals who may have varicella, and they should be targeted for vaccination immediately postpartum.5,9
If a susceptible pregnant patient has been exposed to an individual with varicella, she should receive 1 of 2 regimens within 72 to 96 hours to minimize the risk of maternal infection.5,9,10 One option is intramuscular varicella-zoster immune globulin (VariZIG), 125 U/10 kg body weight, with a maximum dose of 625 U (5 vials). The distributor of this agent is FFF Enterprises in Temucula, California (telephone: 800-843-7477). A company representative will assess the patient’s eligibility and deliver the drug within 24 hours if the patient is considered eligible. An alternative prophylactic regimen is oral acyclovir, 800 mg 5 times daily for 7 days, or oral valacyclovir, 1,000 mg 3 times daily for 7 days.
If, despite prophylaxis, the pregnant woman becomes infected, she should immediately be treated with 1 of the oral antiviral regimens described above. If she has evidence of encephalitis, pneumonia, or severe disseminated mucocutaneous infection, or if she is immunosuppressed, she should be hospitalized and treated with intravenous acyclovir, 10 mg/kg infused over 1 hour every 8 hours for 10 days.
Ultrasonography is the most valuable test to identify fetal infection. Key findings that suggest congenital varicella are fetal growth restriction, microcephaly, ventriculomegaly, echogenic foci in the liver, and limb abnormalities. There is no proven therapy for congenital varicella.
When a patient has varicella at the time of delivery, she should be isolated from her infant until all lesions have crusted over. In addition, the neonate should be treated with either VariZIG or an antiviral agent.5,9
Prevention with varicella vaccine
The varicella vaccine (Varivax) is a live-virus vaccine that is highly immunogenic. The vaccine is now part of the routine childhood immunization sequence. Children ages 1 to 12 years require only a single dose of the vaccine. Individuals older than 12 years of age require 2 doses, administered 4 to 6 weeks apart. The vaccine should not be administered during pregnancy. It also should not be administered to individuals who are severely immunocompromised, are receiving high-dose systemic steroids, have untreated tuberculosis, or have an allergy to neomycin, which is a component of the vaccine. The vaccine does not pose a risk to the breastfeeding infant.11
CASE #2 Hospitalization is recommended for this patient
The patient in this case developed acute varicella pneumonia as a result of her exposure to the neighbor’s child. The diagnosis can be confirmed by demonstrating a positive varicella-zoster IgM and by obtaining a chest x-ray that identifies the diffuse patchy infiltrates characteristic of viral pneumonia. Because this is such a potentially serious illness, the patient should be hospitalized and treated with intravenous acyclovir or valacyclovir. Antibiotics such as ceftriaxone and azithromycin may be indicated to treat superimposed bacterial pneumonia. Given the later gestational age, the fetus is at low risk for serious injury. ●
- Valeur-Jensen AK, Pedersen CB, Westergaard T, et al. Risk factors for parvovirus B19 infection in pregnancy. JAMA. 1999;281:1099-1105.
- Harger JH, Adler SP, Koch WC, et al. Prospective evaluation of 618 pregnant women exposed to parvovirus B19: risks and symptoms. Obstet Gynecol. 1998;91:413-420.
- Melamed N, Whittle W, Kelly EN, et al. Fetal thrombocytopenia in pregnancies with fetal human parvovirus-B19 infection. Am J Obstet Gynecol. 2015;212:793.e1-8.
- Nagel HTC, de Haan TR, Vandenbussche FPH, et al. Long-term outcome after fetal transfusion for hydrops associated with parvovirus B19 infection. Obstet Gynecol. 2007;109:42-47.
- Duff P. Maternal and fetal infections. In: Resnik R, Lockwood CJ, Moore TR, et al (eds). Creasy & Resnik’s Maternal-Fetal Medicine: Principles and Practice. 8th ed. Elsevier; 2019:911-912.
- Cohen JI. Herpes zoster. N Engl J Med. 2013;369:255-263.
- Enders G, Miller E, Cradock-Watson J, et al. Consequences of varicella and herpes zoster in pregnancy: prospective study of 1739 cases. Lancet. 1994;343:1548-1551.
- Duff P. Varicella in pregnancy: five priorities for clinicians. Infect Dis Obstet Gynecol. 1994;1:163-165.
- Marin M, Guris D, Chaves SS, et al; Advisory Committee on Immunization Practices, Centers for Disease Control and Prevention. Prevention of varicella. MMWR Recommend Rep. 2007;56(RR-4):1-40.
- Swamy GK, Dotters-Katz SK. Safety and varicella outcomes after varicella zoster immune globulin administration in pregnancy. Am J Obstet Gynecol. 2019;221:655-656.
- Duff P. Varicella vaccine. Infect Dis Obstet Gynecol. 1996;4:63-65.
- Valeur-Jensen AK, Pedersen CB, Westergaard T, et al. Risk factors for parvovirus B19 infection in pregnancy. JAMA. 1999;281:1099-1105.
- Harger JH, Adler SP, Koch WC, et al. Prospective evaluation of 618 pregnant women exposed to parvovirus B19: risks and symptoms. Obstet Gynecol. 1998;91:413-420.
- Melamed N, Whittle W, Kelly EN, et al. Fetal thrombocytopenia in pregnancies with fetal human parvovirus-B19 infection. Am J Obstet Gynecol. 2015;212:793.e1-8.
- Nagel HTC, de Haan TR, Vandenbussche FPH, et al. Long-term outcome after fetal transfusion for hydrops associated with parvovirus B19 infection. Obstet Gynecol. 2007;109:42-47.
- Duff P. Maternal and fetal infections. In: Resnik R, Lockwood CJ, Moore TR, et al (eds). Creasy & Resnik’s Maternal-Fetal Medicine: Principles and Practice. 8th ed. Elsevier; 2019:911-912.
- Cohen JI. Herpes zoster. N Engl J Med. 2013;369:255-263.
- Enders G, Miller E, Cradock-Watson J, et al. Consequences of varicella and herpes zoster in pregnancy: prospective study of 1739 cases. Lancet. 1994;343:1548-1551.
- Duff P. Varicella in pregnancy: five priorities for clinicians. Infect Dis Obstet Gynecol. 1994;1:163-165.
- Marin M, Guris D, Chaves SS, et al; Advisory Committee on Immunization Practices, Centers for Disease Control and Prevention. Prevention of varicella. MMWR Recommend Rep. 2007;56(RR-4):1-40.
- Swamy GK, Dotters-Katz SK. Safety and varicella outcomes after varicella zoster immune globulin administration in pregnancy. Am J Obstet Gynecol. 2019;221:655-656.
- Duff P. Varicella vaccine. Infect Dis Obstet Gynecol. 1996;4:63-65.
FDA: Newborns protected by whooping cough vaccine
The Food and Drug Administration has approved a whooping cough vaccine that protects newborns under 2 months of age.
The vaccine, manufactured by GlaxoSmithKline, was previously approved among pregnant people for their own protection.
“Infants younger than 2 months of age are too young to be protected by the childhood pertussis vaccine series,” Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said in a press release. “This is the first vaccine approved specifically for use during pregnancy to prevent a disease in young infants whose mothers are vaccinated during pregnancy.”
Pertussis is a highly contagious respiratory tract infection caused by the bacterium Bordetella pertussis. Most cases that result in hospitalizations and death are among infants within 2 months of birth.
The FDA said its decision was based on data from observational studies, which included 108 cases of pertussis in infants younger than 2 months old. According to data evaluated by the agency, the vaccine was 78% effective in preventing whooping cough.
Boostrix is administered as a single 0.5-mL dose.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved a whooping cough vaccine that protects newborns under 2 months of age.
The vaccine, manufactured by GlaxoSmithKline, was previously approved among pregnant people for their own protection.
“Infants younger than 2 months of age are too young to be protected by the childhood pertussis vaccine series,” Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said in a press release. “This is the first vaccine approved specifically for use during pregnancy to prevent a disease in young infants whose mothers are vaccinated during pregnancy.”
Pertussis is a highly contagious respiratory tract infection caused by the bacterium Bordetella pertussis. Most cases that result in hospitalizations and death are among infants within 2 months of birth.
The FDA said its decision was based on data from observational studies, which included 108 cases of pertussis in infants younger than 2 months old. According to data evaluated by the agency, the vaccine was 78% effective in preventing whooping cough.
Boostrix is administered as a single 0.5-mL dose.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved a whooping cough vaccine that protects newborns under 2 months of age.
The vaccine, manufactured by GlaxoSmithKline, was previously approved among pregnant people for their own protection.
“Infants younger than 2 months of age are too young to be protected by the childhood pertussis vaccine series,” Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said in a press release. “This is the first vaccine approved specifically for use during pregnancy to prevent a disease in young infants whose mothers are vaccinated during pregnancy.”
Pertussis is a highly contagious respiratory tract infection caused by the bacterium Bordetella pertussis. Most cases that result in hospitalizations and death are among infants within 2 months of birth.
The FDA said its decision was based on data from observational studies, which included 108 cases of pertussis in infants younger than 2 months old. According to data evaluated by the agency, the vaccine was 78% effective in preventing whooping cough.
Boostrix is administered as a single 0.5-mL dose.
A version of this article first appeared on Medscape.com.
HPV infection in pregnancy higher among women living with HIV
Pregnant women living with HIV were more likely to be infected with human papillomavirus (HPV) than were pregnant women without HIV, a recent systematic review and meta-analysis reports.
“High prevalence of HPV was documented in pregnant WLWH [women living with HIV], exceeding the prevalence among pregnant women without HIV,” Elisabeth McClymont, PhD, of the University of British Columbia, Vancouver, and colleagues wrote in the Journal of Acquired Immune Deficiency Syndrome.
Their results contribute to two major global public health goals: eliminating cervical cancer and improving the health outcomes of newborn babies.
“Our findings of a high prevalence of HPV infection during pregnancy in WLWH, particularly of highly oncogenic HPV types, emphasize the need for HPV screening and vaccination in WLWH,” they added. “WLWH are a key population for both HPV and adverse pregnancy outcome prevention.”
Emerging evidence suggests that being infected with HPV during pregnancy may be linked with adverse pregnancy outcomes. Although women living with HIV have higher rates of HPV infection and adverse pregnancy outcomes, no prior reviews have reported on HPV infection during pregnancy in women living with HIV, the authors explained.
A study of studies
Dr. McClymont and colleagues searched the standard medical research databases through Jan. 18, 2022, for pooled and type-specific HPV prevalence and associated pregnancy outcomes among pregnant women living with HIV, including available within-study comparators of women without HIV.
They performed subgroup analyses according to polymerase chain reaction primers used to detect HPV type and according to region (Africa, Asia and Europe, the Americas).
Their analysis of 10 studies describing HPV prevalence in 1,594 pregnant women living with HIV found:
- The pooled HPV prevalence in pregnant women living with HIV was 75.5% (95% confidence interval, 50.2%-90.4%) but ranged from 23% to 98% between individual studies.
- Among the five studies that also analyzed HPV prevalence in pregnant women without HIV, the pooled prevalence was 48.1% (95% CI, 27.1%-69.8%).
- Pregnant women living with HIV had 54% higher odds of being HPV positive than did pregnant women without HIV.
- HPV-16 was the most common HPV type detected in pregnant women living with HIV, followed by HPV-52; other common types included HPV-18 and HPV-58.
- One study provided data on pregnancy outcomes in women living with HIV but did not correlate pregnancy outcomes with HPV status.
Experts urge HPV, cervical cancer screening for women living with HIV
“HPV is a common virus that can lead to cervical dysplasia and cervical cancer,” cautioned Clara Paik, MD, professor and clinic medical director of obstetrics and gynecology at UC Davis Health, Sacramento.
“HPV can also be associated with adverse pregnancy outcomes, including preterm birth and premature membrane rupture,” she said in an interview. “It is important to know the prevalence of HPV infection in pregnant women living with HIV in order to assess if this specific population is at higher risk for adverse pregnancy outcomes.”
Dr. Paik, who was not involved in the study, would like these results to lead to better HPV screening in pregnant women living with HIV.
“The study’s strengths include the large number of women studied when all the research studies were pooled,” she said. “A weakness is that, if individual studies had limitations, a systematic review based on weaker studies may not necessarily yield results that are conclusive.”
Linda Eckert, MD, professor of obstetrics and gynecology at the University of Washington, Seattle, said that the study highlights the importance of including cervical cancer screening in antepartum care, especially in areas of high HIV prevalence.
“Women living with HIV have a sixfold increased rate of developing cervical cancer compared to women without HIV,” she added, citing a 2020 analysis in The Lancet Global Health that estimated global cervical cancer risk among women living with HIV.
“This [new] study allows us to definitively say that pregnant women living with HIV have higher rates of HPV than do pregnant women without HIV,” noted Dr. Eckert, who was not involved in either study. “And HPV type 16 – the HPV type most associated with developing cervical cancer – was the most common high-risk HPV type found in these patients.”
HPV vaccination recommended
The World Health Organization’s call to eliminate cervical cancer has generated interest and funding for cervical cancer screening of women with HIV, Dr. Eckert said. “WHO recommends that women living with HIV who are 25 years of age and above be screened for cervical cancer annually.”
The authors urged that women living with HIV not only be screened for HPV but that they also be vaccinated against HPV.
“We know that HPV vaccination is unprecedented in its ability to prevent HPV infections when it is received prior to acquiring HPV infection,” Dr. Eckert said, “but currently data showing that HPV vaccination would treat HPV16 in pregnant women already infected with HPV16 are lacking.
“This study points to the need for a trial to investigate HPV vaccination in pregnant women living with HIV who have the high-risk HPV types,” she suggested.
Dr. Eckert contributed to the American College of Obstetricians and Gynecologists’ 2020 Human Papillomavirus Vaccination Committee Opinion. One study coauthor reported financial relationships with Merck. Dr. McClymont, the other coauthors, as well as Dr. Paik and Dr. Eckert reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pregnant women living with HIV were more likely to be infected with human papillomavirus (HPV) than were pregnant women without HIV, a recent systematic review and meta-analysis reports.
“High prevalence of HPV was documented in pregnant WLWH [women living with HIV], exceeding the prevalence among pregnant women without HIV,” Elisabeth McClymont, PhD, of the University of British Columbia, Vancouver, and colleagues wrote in the Journal of Acquired Immune Deficiency Syndrome.
Their results contribute to two major global public health goals: eliminating cervical cancer and improving the health outcomes of newborn babies.
“Our findings of a high prevalence of HPV infection during pregnancy in WLWH, particularly of highly oncogenic HPV types, emphasize the need for HPV screening and vaccination in WLWH,” they added. “WLWH are a key population for both HPV and adverse pregnancy outcome prevention.”
Emerging evidence suggests that being infected with HPV during pregnancy may be linked with adverse pregnancy outcomes. Although women living with HIV have higher rates of HPV infection and adverse pregnancy outcomes, no prior reviews have reported on HPV infection during pregnancy in women living with HIV, the authors explained.
A study of studies
Dr. McClymont and colleagues searched the standard medical research databases through Jan. 18, 2022, for pooled and type-specific HPV prevalence and associated pregnancy outcomes among pregnant women living with HIV, including available within-study comparators of women without HIV.
They performed subgroup analyses according to polymerase chain reaction primers used to detect HPV type and according to region (Africa, Asia and Europe, the Americas).
Their analysis of 10 studies describing HPV prevalence in 1,594 pregnant women living with HIV found:
- The pooled HPV prevalence in pregnant women living with HIV was 75.5% (95% confidence interval, 50.2%-90.4%) but ranged from 23% to 98% between individual studies.
- Among the five studies that also analyzed HPV prevalence in pregnant women without HIV, the pooled prevalence was 48.1% (95% CI, 27.1%-69.8%).
- Pregnant women living with HIV had 54% higher odds of being HPV positive than did pregnant women without HIV.
- HPV-16 was the most common HPV type detected in pregnant women living with HIV, followed by HPV-52; other common types included HPV-18 and HPV-58.
- One study provided data on pregnancy outcomes in women living with HIV but did not correlate pregnancy outcomes with HPV status.
Experts urge HPV, cervical cancer screening for women living with HIV
“HPV is a common virus that can lead to cervical dysplasia and cervical cancer,” cautioned Clara Paik, MD, professor and clinic medical director of obstetrics and gynecology at UC Davis Health, Sacramento.
“HPV can also be associated with adverse pregnancy outcomes, including preterm birth and premature membrane rupture,” she said in an interview. “It is important to know the prevalence of HPV infection in pregnant women living with HIV in order to assess if this specific population is at higher risk for adverse pregnancy outcomes.”
Dr. Paik, who was not involved in the study, would like these results to lead to better HPV screening in pregnant women living with HIV.
“The study’s strengths include the large number of women studied when all the research studies were pooled,” she said. “A weakness is that, if individual studies had limitations, a systematic review based on weaker studies may not necessarily yield results that are conclusive.”
Linda Eckert, MD, professor of obstetrics and gynecology at the University of Washington, Seattle, said that the study highlights the importance of including cervical cancer screening in antepartum care, especially in areas of high HIV prevalence.
“Women living with HIV have a sixfold increased rate of developing cervical cancer compared to women without HIV,” she added, citing a 2020 analysis in The Lancet Global Health that estimated global cervical cancer risk among women living with HIV.
“This [new] study allows us to definitively say that pregnant women living with HIV have higher rates of HPV than do pregnant women without HIV,” noted Dr. Eckert, who was not involved in either study. “And HPV type 16 – the HPV type most associated with developing cervical cancer – was the most common high-risk HPV type found in these patients.”
HPV vaccination recommended
The World Health Organization’s call to eliminate cervical cancer has generated interest and funding for cervical cancer screening of women with HIV, Dr. Eckert said. “WHO recommends that women living with HIV who are 25 years of age and above be screened for cervical cancer annually.”
The authors urged that women living with HIV not only be screened for HPV but that they also be vaccinated against HPV.
“We know that HPV vaccination is unprecedented in its ability to prevent HPV infections when it is received prior to acquiring HPV infection,” Dr. Eckert said, “but currently data showing that HPV vaccination would treat HPV16 in pregnant women already infected with HPV16 are lacking.
“This study points to the need for a trial to investigate HPV vaccination in pregnant women living with HIV who have the high-risk HPV types,” she suggested.
Dr. Eckert contributed to the American College of Obstetricians and Gynecologists’ 2020 Human Papillomavirus Vaccination Committee Opinion. One study coauthor reported financial relationships with Merck. Dr. McClymont, the other coauthors, as well as Dr. Paik and Dr. Eckert reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pregnant women living with HIV were more likely to be infected with human papillomavirus (HPV) than were pregnant women without HIV, a recent systematic review and meta-analysis reports.
“High prevalence of HPV was documented in pregnant WLWH [women living with HIV], exceeding the prevalence among pregnant women without HIV,” Elisabeth McClymont, PhD, of the University of British Columbia, Vancouver, and colleagues wrote in the Journal of Acquired Immune Deficiency Syndrome.
Their results contribute to two major global public health goals: eliminating cervical cancer and improving the health outcomes of newborn babies.
“Our findings of a high prevalence of HPV infection during pregnancy in WLWH, particularly of highly oncogenic HPV types, emphasize the need for HPV screening and vaccination in WLWH,” they added. “WLWH are a key population for both HPV and adverse pregnancy outcome prevention.”
Emerging evidence suggests that being infected with HPV during pregnancy may be linked with adverse pregnancy outcomes. Although women living with HIV have higher rates of HPV infection and adverse pregnancy outcomes, no prior reviews have reported on HPV infection during pregnancy in women living with HIV, the authors explained.
A study of studies
Dr. McClymont and colleagues searched the standard medical research databases through Jan. 18, 2022, for pooled and type-specific HPV prevalence and associated pregnancy outcomes among pregnant women living with HIV, including available within-study comparators of women without HIV.
They performed subgroup analyses according to polymerase chain reaction primers used to detect HPV type and according to region (Africa, Asia and Europe, the Americas).
Their analysis of 10 studies describing HPV prevalence in 1,594 pregnant women living with HIV found:
- The pooled HPV prevalence in pregnant women living with HIV was 75.5% (95% confidence interval, 50.2%-90.4%) but ranged from 23% to 98% between individual studies.
- Among the five studies that also analyzed HPV prevalence in pregnant women without HIV, the pooled prevalence was 48.1% (95% CI, 27.1%-69.8%).
- Pregnant women living with HIV had 54% higher odds of being HPV positive than did pregnant women without HIV.
- HPV-16 was the most common HPV type detected in pregnant women living with HIV, followed by HPV-52; other common types included HPV-18 and HPV-58.
- One study provided data on pregnancy outcomes in women living with HIV but did not correlate pregnancy outcomes with HPV status.
Experts urge HPV, cervical cancer screening for women living with HIV
“HPV is a common virus that can lead to cervical dysplasia and cervical cancer,” cautioned Clara Paik, MD, professor and clinic medical director of obstetrics and gynecology at UC Davis Health, Sacramento.
“HPV can also be associated with adverse pregnancy outcomes, including preterm birth and premature membrane rupture,” she said in an interview. “It is important to know the prevalence of HPV infection in pregnant women living with HIV in order to assess if this specific population is at higher risk for adverse pregnancy outcomes.”
Dr. Paik, who was not involved in the study, would like these results to lead to better HPV screening in pregnant women living with HIV.
“The study’s strengths include the large number of women studied when all the research studies were pooled,” she said. “A weakness is that, if individual studies had limitations, a systematic review based on weaker studies may not necessarily yield results that are conclusive.”
Linda Eckert, MD, professor of obstetrics and gynecology at the University of Washington, Seattle, said that the study highlights the importance of including cervical cancer screening in antepartum care, especially in areas of high HIV prevalence.
“Women living with HIV have a sixfold increased rate of developing cervical cancer compared to women without HIV,” she added, citing a 2020 analysis in The Lancet Global Health that estimated global cervical cancer risk among women living with HIV.
“This [new] study allows us to definitively say that pregnant women living with HIV have higher rates of HPV than do pregnant women without HIV,” noted Dr. Eckert, who was not involved in either study. “And HPV type 16 – the HPV type most associated with developing cervical cancer – was the most common high-risk HPV type found in these patients.”
HPV vaccination recommended
The World Health Organization’s call to eliminate cervical cancer has generated interest and funding for cervical cancer screening of women with HIV, Dr. Eckert said. “WHO recommends that women living with HIV who are 25 years of age and above be screened for cervical cancer annually.”
The authors urged that women living with HIV not only be screened for HPV but that they also be vaccinated against HPV.
“We know that HPV vaccination is unprecedented in its ability to prevent HPV infections when it is received prior to acquiring HPV infection,” Dr. Eckert said, “but currently data showing that HPV vaccination would treat HPV16 in pregnant women already infected with HPV16 are lacking.
“This study points to the need for a trial to investigate HPV vaccination in pregnant women living with HIV who have the high-risk HPV types,” she suggested.
Dr. Eckert contributed to the American College of Obstetricians and Gynecologists’ 2020 Human Papillomavirus Vaccination Committee Opinion. One study coauthor reported financial relationships with Merck. Dr. McClymont, the other coauthors, as well as Dr. Paik and Dr. Eckert reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF ACQUIRED IMMUNE DEFICIENCY SYNDROME.
Nifedipine during labor controls BP in severe preeclampsia
Women with preeclampsia with severe features benefit from treatment with oral nifedipine during labor and delivery, results of a randomized controlled trial suggest.
The study showed that intrapartum administration of extended-release oral nifedipine was safe and reduced the need for acute intravenous or immediate-release oral hypertensive therapy. There was a trend toward fewer cesarean deliveries and less need for neonatal intensive care.
The results suggest that providers “consider initiating long-acting nifedipine every 24 hours for individuals with preeclampsia with severe features who are undergoing induction of labor,” Erin M. Cleary, MD, with the Ohio State University, Columbus, told this news organization.
“There is no need to wait until patients require one or more doses of acute [antihypertensive] therapy before starting long-acting nifedipine, as long as they otherwise meet criteria for preeclampsia with severe features,” Dr. Cleary said.
The study was published online in Hypertension.
Clear benefits for mom and baby
Preeclampsia complicates up to 8% of pregnancies and often leads to significant maternal and perinatal morbidity.
“We know that bringing down very high blood pressure to a safer range will help prevent maternal and fetal complications. However, besides rapid-acting, intravenous medicines for severe hypertension during pregnancy, optimal management for hypertension during the labor and delivery process has not been studied,” Dr. Cleary explains in a news release.
In a randomized, triple-blind, placebo-controlled study, the researchers assessed whether treatment with long-acting nifedipine could prevent severe hypertension in women with a singleton or twin gestation and preeclampsia with severe features, as defined according to American College of Obstetrics and Gynecology criteria.
During induction of labor between 22 and 41 weeks’ gestation, 55 women were assigned to 30-mg oral extended-release nifedipine, and 55 received matching placebo, administered every 24 hours until delivery.
The primary outcome was receipt of one or more doses of acute hypertension therapy for blood pressure of at least 160/110 mm Hg that was sustained for 10 minutes or longer.
The primary outcome occurred in significantly fewer women in the nifedipine group than in the placebo group (34% vs. 55%; relative risk, 0.62; 95% CI, 0.39-0.97; number needed to treat, 4.7).
Fewer women in the nifedipine group than in the placebo group required cesarean delivery, although this difference did not meet statistical significance (21% vs. 35%; RR, 0.60; 95% CI, 0.31-1.15).
There was no between-group difference in the rate of hypotensive episodes, including symptomatic hypotension requiring phenylephrine for pressure support following neuraxial anesthesia (9.4% vs. 8.2%; RR, 1.15; 95% CI, 0.33-4.06).
After delivery, there was no difference in the rate of persistently severe blood pressure that required acute therapy and maintenance therapy at time of discharge home.
Birth weight and rates of births of neonates who were small for gestational age were similar in the two groups. There was a trend for decreased rates of neonatal intensive care unit admission among infants born to mothers who received nifedipine (29% vs. 47%; RR, 0.62; 95% CI, 0.37-1.02).
The neonatal composite outcome was also similar between the nifedipine group and the placebo group (36% vs. 41%; RR, 0.83; 95% CI, 0.51-1.37). The composite outcome included Apgar score of less than 7 at 5 minutes, hyperbilirubinemia requiring phototherapy, hypoglycemia requiring intravenous therapy, or supplemental oxygen therapy beyond the first 24 hours of life.
“Our findings support the growing trend in more active management of hypertension in pregnancy with daily maintenance medications,” Dr. Cleary and colleagues note in their article.
“Even in the absence of preeclampsia, emerging research suggests pregnant individuals may benefit from initiating and titrating antihypertensive therapy at goals similar to the nonobstetric population,” they add.
Potentially practice changing
Reached for comment, Vesna Garovic, MD, PhD, with Mayo Clinic, Rochester, Minn., said that this is an “important initial paper to start a very important conversation about blood pressure treatment goals in preeclampsia.”
Dr. Garovic noted that for chronic hypertension in pregnancy, the blood pressure treatment goal is now less than or equal to 140/90 mm Hg.
“However, this does not apply to preeclampsia, where quite high blood pressures, such 160/110 mm Hg or higher, are still allowed before treatment is considered,” Dr. Garovic said.
“This study shows that as soon as you reach that level, treatment with oral nifedipine should be initiated and that timely initiation of oral nifedipine may optimize blood pressure control and decrease the need for intravenous therapy subsequently, and that has good effects on the mother without adversely affecting the baby,” Dr. Garovic said.
“This is potentially practice changing,” Dr. Garovic added. “But the elephant in the room is the question of why we are waiting for blood pressure to reach such dangerous levels before initiating treatment, and whether initiating treatment at a blood pressure of 140/90 or higher may prevent blood pressure reaching these high levels and women developing complications that are the consequence of severe hypertension.”
The study was funded by the Ohio State University’s Department of Obstetrics and Gynecology. Dr. Cleary and Dr. Garovic have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Women with preeclampsia with severe features benefit from treatment with oral nifedipine during labor and delivery, results of a randomized controlled trial suggest.
The study showed that intrapartum administration of extended-release oral nifedipine was safe and reduced the need for acute intravenous or immediate-release oral hypertensive therapy. There was a trend toward fewer cesarean deliveries and less need for neonatal intensive care.
The results suggest that providers “consider initiating long-acting nifedipine every 24 hours for individuals with preeclampsia with severe features who are undergoing induction of labor,” Erin M. Cleary, MD, with the Ohio State University, Columbus, told this news organization.
“There is no need to wait until patients require one or more doses of acute [antihypertensive] therapy before starting long-acting nifedipine, as long as they otherwise meet criteria for preeclampsia with severe features,” Dr. Cleary said.
The study was published online in Hypertension.
Clear benefits for mom and baby
Preeclampsia complicates up to 8% of pregnancies and often leads to significant maternal and perinatal morbidity.
“We know that bringing down very high blood pressure to a safer range will help prevent maternal and fetal complications. However, besides rapid-acting, intravenous medicines for severe hypertension during pregnancy, optimal management for hypertension during the labor and delivery process has not been studied,” Dr. Cleary explains in a news release.
In a randomized, triple-blind, placebo-controlled study, the researchers assessed whether treatment with long-acting nifedipine could prevent severe hypertension in women with a singleton or twin gestation and preeclampsia with severe features, as defined according to American College of Obstetrics and Gynecology criteria.
During induction of labor between 22 and 41 weeks’ gestation, 55 women were assigned to 30-mg oral extended-release nifedipine, and 55 received matching placebo, administered every 24 hours until delivery.
The primary outcome was receipt of one or more doses of acute hypertension therapy for blood pressure of at least 160/110 mm Hg that was sustained for 10 minutes or longer.
The primary outcome occurred in significantly fewer women in the nifedipine group than in the placebo group (34% vs. 55%; relative risk, 0.62; 95% CI, 0.39-0.97; number needed to treat, 4.7).
Fewer women in the nifedipine group than in the placebo group required cesarean delivery, although this difference did not meet statistical significance (21% vs. 35%; RR, 0.60; 95% CI, 0.31-1.15).
There was no between-group difference in the rate of hypotensive episodes, including symptomatic hypotension requiring phenylephrine for pressure support following neuraxial anesthesia (9.4% vs. 8.2%; RR, 1.15; 95% CI, 0.33-4.06).
After delivery, there was no difference in the rate of persistently severe blood pressure that required acute therapy and maintenance therapy at time of discharge home.
Birth weight and rates of births of neonates who were small for gestational age were similar in the two groups. There was a trend for decreased rates of neonatal intensive care unit admission among infants born to mothers who received nifedipine (29% vs. 47%; RR, 0.62; 95% CI, 0.37-1.02).
The neonatal composite outcome was also similar between the nifedipine group and the placebo group (36% vs. 41%; RR, 0.83; 95% CI, 0.51-1.37). The composite outcome included Apgar score of less than 7 at 5 minutes, hyperbilirubinemia requiring phototherapy, hypoglycemia requiring intravenous therapy, or supplemental oxygen therapy beyond the first 24 hours of life.
“Our findings support the growing trend in more active management of hypertension in pregnancy with daily maintenance medications,” Dr. Cleary and colleagues note in their article.
“Even in the absence of preeclampsia, emerging research suggests pregnant individuals may benefit from initiating and titrating antihypertensive therapy at goals similar to the nonobstetric population,” they add.
Potentially practice changing
Reached for comment, Vesna Garovic, MD, PhD, with Mayo Clinic, Rochester, Minn., said that this is an “important initial paper to start a very important conversation about blood pressure treatment goals in preeclampsia.”
Dr. Garovic noted that for chronic hypertension in pregnancy, the blood pressure treatment goal is now less than or equal to 140/90 mm Hg.
“However, this does not apply to preeclampsia, where quite high blood pressures, such 160/110 mm Hg or higher, are still allowed before treatment is considered,” Dr. Garovic said.
“This study shows that as soon as you reach that level, treatment with oral nifedipine should be initiated and that timely initiation of oral nifedipine may optimize blood pressure control and decrease the need for intravenous therapy subsequently, and that has good effects on the mother without adversely affecting the baby,” Dr. Garovic said.
“This is potentially practice changing,” Dr. Garovic added. “But the elephant in the room is the question of why we are waiting for blood pressure to reach such dangerous levels before initiating treatment, and whether initiating treatment at a blood pressure of 140/90 or higher may prevent blood pressure reaching these high levels and women developing complications that are the consequence of severe hypertension.”
The study was funded by the Ohio State University’s Department of Obstetrics and Gynecology. Dr. Cleary and Dr. Garovic have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Women with preeclampsia with severe features benefit from treatment with oral nifedipine during labor and delivery, results of a randomized controlled trial suggest.
The study showed that intrapartum administration of extended-release oral nifedipine was safe and reduced the need for acute intravenous or immediate-release oral hypertensive therapy. There was a trend toward fewer cesarean deliveries and less need for neonatal intensive care.
The results suggest that providers “consider initiating long-acting nifedipine every 24 hours for individuals with preeclampsia with severe features who are undergoing induction of labor,” Erin M. Cleary, MD, with the Ohio State University, Columbus, told this news organization.
“There is no need to wait until patients require one or more doses of acute [antihypertensive] therapy before starting long-acting nifedipine, as long as they otherwise meet criteria for preeclampsia with severe features,” Dr. Cleary said.
The study was published online in Hypertension.
Clear benefits for mom and baby
Preeclampsia complicates up to 8% of pregnancies and often leads to significant maternal and perinatal morbidity.
“We know that bringing down very high blood pressure to a safer range will help prevent maternal and fetal complications. However, besides rapid-acting, intravenous medicines for severe hypertension during pregnancy, optimal management for hypertension during the labor and delivery process has not been studied,” Dr. Cleary explains in a news release.
In a randomized, triple-blind, placebo-controlled study, the researchers assessed whether treatment with long-acting nifedipine could prevent severe hypertension in women with a singleton or twin gestation and preeclampsia with severe features, as defined according to American College of Obstetrics and Gynecology criteria.
During induction of labor between 22 and 41 weeks’ gestation, 55 women were assigned to 30-mg oral extended-release nifedipine, and 55 received matching placebo, administered every 24 hours until delivery.
The primary outcome was receipt of one or more doses of acute hypertension therapy for blood pressure of at least 160/110 mm Hg that was sustained for 10 minutes or longer.
The primary outcome occurred in significantly fewer women in the nifedipine group than in the placebo group (34% vs. 55%; relative risk, 0.62; 95% CI, 0.39-0.97; number needed to treat, 4.7).
Fewer women in the nifedipine group than in the placebo group required cesarean delivery, although this difference did not meet statistical significance (21% vs. 35%; RR, 0.60; 95% CI, 0.31-1.15).
There was no between-group difference in the rate of hypotensive episodes, including symptomatic hypotension requiring phenylephrine for pressure support following neuraxial anesthesia (9.4% vs. 8.2%; RR, 1.15; 95% CI, 0.33-4.06).
After delivery, there was no difference in the rate of persistently severe blood pressure that required acute therapy and maintenance therapy at time of discharge home.
Birth weight and rates of births of neonates who were small for gestational age were similar in the two groups. There was a trend for decreased rates of neonatal intensive care unit admission among infants born to mothers who received nifedipine (29% vs. 47%; RR, 0.62; 95% CI, 0.37-1.02).
The neonatal composite outcome was also similar between the nifedipine group and the placebo group (36% vs. 41%; RR, 0.83; 95% CI, 0.51-1.37). The composite outcome included Apgar score of less than 7 at 5 minutes, hyperbilirubinemia requiring phototherapy, hypoglycemia requiring intravenous therapy, or supplemental oxygen therapy beyond the first 24 hours of life.
“Our findings support the growing trend in more active management of hypertension in pregnancy with daily maintenance medications,” Dr. Cleary and colleagues note in their article.
“Even in the absence of preeclampsia, emerging research suggests pregnant individuals may benefit from initiating and titrating antihypertensive therapy at goals similar to the nonobstetric population,” they add.
Potentially practice changing
Reached for comment, Vesna Garovic, MD, PhD, with Mayo Clinic, Rochester, Minn., said that this is an “important initial paper to start a very important conversation about blood pressure treatment goals in preeclampsia.”
Dr. Garovic noted that for chronic hypertension in pregnancy, the blood pressure treatment goal is now less than or equal to 140/90 mm Hg.
“However, this does not apply to preeclampsia, where quite high blood pressures, such 160/110 mm Hg or higher, are still allowed before treatment is considered,” Dr. Garovic said.
“This study shows that as soon as you reach that level, treatment with oral nifedipine should be initiated and that timely initiation of oral nifedipine may optimize blood pressure control and decrease the need for intravenous therapy subsequently, and that has good effects on the mother without adversely affecting the baby,” Dr. Garovic said.
“This is potentially practice changing,” Dr. Garovic added. “But the elephant in the room is the question of why we are waiting for blood pressure to reach such dangerous levels before initiating treatment, and whether initiating treatment at a blood pressure of 140/90 or higher may prevent blood pressure reaching these high levels and women developing complications that are the consequence of severe hypertension.”
The study was funded by the Ohio State University’s Department of Obstetrics and Gynecology. Dr. Cleary and Dr. Garovic have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HYPERTENSION
Ultra-processed food intake by moms linked with childhood obesity
A mother’s consumption of ultra-processed foods appears to be related to an increased risk of overweight or obesity in her children, according to new research.
Among the 19,958 mother-child pairs studied, 12.4% of children developed obesity or overweight in the full analytic study group, and the offspring of those mothers who ate the most ultra-processed foods had a 26% higher risk of obesity/overweight (12.1 servings/day), compared with those with the lowest consumption (3.4 servings/day), report Andrew T. Chan, MD, MPH, professor of medicine at Harvard Medical School, Boston, and colleagues.
This study demonstrates the possible advantages of restricting ultra-processed food consumption among women and mothers who are in their reproductive years to potentially lower the risk of childhood obesity, the investigators note.
“These data support the importance of refining dietary recommendations and the development of programs to improve nutrition for women of reproductive age to promote offspring health,” they write in their article, published in BMJ.
“As a medical and public health community, we have to understand that the period of time in which a woman is carrying a child or ... the time when she is raising her children represents a unique opportunity to potentially intervene to affect both the health of the mother and also the health of the children,” Dr. Chan said in an interview.
It is important to address these trends both on an individual clinician level and on a societal level, noted Dr. Chan.
“This is a good opportunity to counsel patients about the potential linkage between their consumption of ultra-processed food for not just themselves but also their kids, and I think that added counseling and awareness may motivate individuals to think about their diets in a more favorable way,” he added.
But ultra-processed foods are affordable and convenient, and many communities are not able to easily access fresh and healthy foods, so “it is incumbent upon [clinicians] to make it a priority and to break down those social and economic barriers, which make it difficult to have healthy and less processed food,” Dr. Chan elaborated.
Assessment of maternal junk food intake during peri-pregnancy and childhood
Modern Western diets frequently include ultra-processed foods – such as packaged baked goods and snacks, fizzy drinks, and sugary cereals – which are linked to adult weight increase. The relationship between parental consumption of highly processed meals and offspring weight is, however, unclear across generations, the researchers note.
Hence, they set out to determine whether eating ultra-processed foods during peri-pregnancy and while raising children increased the risk of being overweight or having obesity among children and teens.
The study team assessed 14,553 mothers and their 19,958 children from the Growing Up Today Study (GUTS I and II) and Nurses’ Health Study II (NHS II) in the United States. Males accounted for 45% of the children in the study, and the children’s ages ranged from 7 to 17 years.
The NHS II is a continuing investigation following the lifestyle and health choices of over 100,000 female registered nurses in the United States in 1989, while the GUTS I involved about 17,000 children of the nurses in the NHS II. Participants in GUTS I filled out an initial lifestyle and health survey and were evaluated annually between 1997 and 2001 and every 2 years thereafter.
Roughly 11,000 children from the NHS II were included in the GUTS II. The children were further evaluated in 2006, 2008, and 2011, as well as every 2 years thereafter.
Participants were followed until the children reached 18 years of age or experienced obesity and overweight onset. A subcohort consisted of 2,925 mother-child pairs with data on peri-pregnancy eating patterns.
Maternal intake of ultra-processed foods while raising children was linked with obesity or overweight in children. Moreover, compared with the lowest consumption cohort (3.4 servings/day), there was a 26% greater risk for the greatest maternal ultra-processed food intake cohort (12.1 servings/day) after adjusting for child’s sedentary time, ultra-processed food intake, physical activity, and established maternal risk factors.
Even though rates were elevated, ultra-processed food intake during pregnancy was not significantly linked to a higher risk of obesity or overweight in children (P for trend = .07).
Sex, birth weight, age, gestational age, or maternal body weight had no effect on these correlations either.
The study’s limitations include the fact that some of the children in the pairs were lost during follow-up; there may have been data misreporting, as the weight and diet measures were provided via self-reported questionnaires; and potential residual confounding given the observational study design, the researchers note.
Other limitations include that the mothers involved in the study came from similar socioeconomic backgrounds, had similar personal and familial educational statuses, and were primarily White, which limits the generalizability of these data to other ethnic groups, the authors add.
“Further studies are warranted to investigate specific biological mechanisms and socioeconomic determinants underlying the observed associations between maternal ultra-processed food intake and offspring overweight and obesity,” the researchers conclude.
A version of this article first appeared on Medscape.com.
A mother’s consumption of ultra-processed foods appears to be related to an increased risk of overweight or obesity in her children, according to new research.
Among the 19,958 mother-child pairs studied, 12.4% of children developed obesity or overweight in the full analytic study group, and the offspring of those mothers who ate the most ultra-processed foods had a 26% higher risk of obesity/overweight (12.1 servings/day), compared with those with the lowest consumption (3.4 servings/day), report Andrew T. Chan, MD, MPH, professor of medicine at Harvard Medical School, Boston, and colleagues.
This study demonstrates the possible advantages of restricting ultra-processed food consumption among women and mothers who are in their reproductive years to potentially lower the risk of childhood obesity, the investigators note.
“These data support the importance of refining dietary recommendations and the development of programs to improve nutrition for women of reproductive age to promote offspring health,” they write in their article, published in BMJ.
“As a medical and public health community, we have to understand that the period of time in which a woman is carrying a child or ... the time when she is raising her children represents a unique opportunity to potentially intervene to affect both the health of the mother and also the health of the children,” Dr. Chan said in an interview.
It is important to address these trends both on an individual clinician level and on a societal level, noted Dr. Chan.
“This is a good opportunity to counsel patients about the potential linkage between their consumption of ultra-processed food for not just themselves but also their kids, and I think that added counseling and awareness may motivate individuals to think about their diets in a more favorable way,” he added.
But ultra-processed foods are affordable and convenient, and many communities are not able to easily access fresh and healthy foods, so “it is incumbent upon [clinicians] to make it a priority and to break down those social and economic barriers, which make it difficult to have healthy and less processed food,” Dr. Chan elaborated.
Assessment of maternal junk food intake during peri-pregnancy and childhood
Modern Western diets frequently include ultra-processed foods – such as packaged baked goods and snacks, fizzy drinks, and sugary cereals – which are linked to adult weight increase. The relationship between parental consumption of highly processed meals and offspring weight is, however, unclear across generations, the researchers note.
Hence, they set out to determine whether eating ultra-processed foods during peri-pregnancy and while raising children increased the risk of being overweight or having obesity among children and teens.
The study team assessed 14,553 mothers and their 19,958 children from the Growing Up Today Study (GUTS I and II) and Nurses’ Health Study II (NHS II) in the United States. Males accounted for 45% of the children in the study, and the children’s ages ranged from 7 to 17 years.
The NHS II is a continuing investigation following the lifestyle and health choices of over 100,000 female registered nurses in the United States in 1989, while the GUTS I involved about 17,000 children of the nurses in the NHS II. Participants in GUTS I filled out an initial lifestyle and health survey and were evaluated annually between 1997 and 2001 and every 2 years thereafter.
Roughly 11,000 children from the NHS II were included in the GUTS II. The children were further evaluated in 2006, 2008, and 2011, as well as every 2 years thereafter.
Participants were followed until the children reached 18 years of age or experienced obesity and overweight onset. A subcohort consisted of 2,925 mother-child pairs with data on peri-pregnancy eating patterns.
Maternal intake of ultra-processed foods while raising children was linked with obesity or overweight in children. Moreover, compared with the lowest consumption cohort (3.4 servings/day), there was a 26% greater risk for the greatest maternal ultra-processed food intake cohort (12.1 servings/day) after adjusting for child’s sedentary time, ultra-processed food intake, physical activity, and established maternal risk factors.
Even though rates were elevated, ultra-processed food intake during pregnancy was not significantly linked to a higher risk of obesity or overweight in children (P for trend = .07).
Sex, birth weight, age, gestational age, or maternal body weight had no effect on these correlations either.
The study’s limitations include the fact that some of the children in the pairs were lost during follow-up; there may have been data misreporting, as the weight and diet measures were provided via self-reported questionnaires; and potential residual confounding given the observational study design, the researchers note.
Other limitations include that the mothers involved in the study came from similar socioeconomic backgrounds, had similar personal and familial educational statuses, and were primarily White, which limits the generalizability of these data to other ethnic groups, the authors add.
“Further studies are warranted to investigate specific biological mechanisms and socioeconomic determinants underlying the observed associations between maternal ultra-processed food intake and offspring overweight and obesity,” the researchers conclude.
A version of this article first appeared on Medscape.com.
A mother’s consumption of ultra-processed foods appears to be related to an increased risk of overweight or obesity in her children, according to new research.
Among the 19,958 mother-child pairs studied, 12.4% of children developed obesity or overweight in the full analytic study group, and the offspring of those mothers who ate the most ultra-processed foods had a 26% higher risk of obesity/overweight (12.1 servings/day), compared with those with the lowest consumption (3.4 servings/day), report Andrew T. Chan, MD, MPH, professor of medicine at Harvard Medical School, Boston, and colleagues.
This study demonstrates the possible advantages of restricting ultra-processed food consumption among women and mothers who are in their reproductive years to potentially lower the risk of childhood obesity, the investigators note.
“These data support the importance of refining dietary recommendations and the development of programs to improve nutrition for women of reproductive age to promote offspring health,” they write in their article, published in BMJ.
“As a medical and public health community, we have to understand that the period of time in which a woman is carrying a child or ... the time when she is raising her children represents a unique opportunity to potentially intervene to affect both the health of the mother and also the health of the children,” Dr. Chan said in an interview.
It is important to address these trends both on an individual clinician level and on a societal level, noted Dr. Chan.
“This is a good opportunity to counsel patients about the potential linkage between their consumption of ultra-processed food for not just themselves but also their kids, and I think that added counseling and awareness may motivate individuals to think about their diets in a more favorable way,” he added.
But ultra-processed foods are affordable and convenient, and many communities are not able to easily access fresh and healthy foods, so “it is incumbent upon [clinicians] to make it a priority and to break down those social and economic barriers, which make it difficult to have healthy and less processed food,” Dr. Chan elaborated.
Assessment of maternal junk food intake during peri-pregnancy and childhood
Modern Western diets frequently include ultra-processed foods – such as packaged baked goods and snacks, fizzy drinks, and sugary cereals – which are linked to adult weight increase. The relationship between parental consumption of highly processed meals and offspring weight is, however, unclear across generations, the researchers note.
Hence, they set out to determine whether eating ultra-processed foods during peri-pregnancy and while raising children increased the risk of being overweight or having obesity among children and teens.
The study team assessed 14,553 mothers and their 19,958 children from the Growing Up Today Study (GUTS I and II) and Nurses’ Health Study II (NHS II) in the United States. Males accounted for 45% of the children in the study, and the children’s ages ranged from 7 to 17 years.
The NHS II is a continuing investigation following the lifestyle and health choices of over 100,000 female registered nurses in the United States in 1989, while the GUTS I involved about 17,000 children of the nurses in the NHS II. Participants in GUTS I filled out an initial lifestyle and health survey and were evaluated annually between 1997 and 2001 and every 2 years thereafter.
Roughly 11,000 children from the NHS II were included in the GUTS II. The children were further evaluated in 2006, 2008, and 2011, as well as every 2 years thereafter.
Participants were followed until the children reached 18 years of age or experienced obesity and overweight onset. A subcohort consisted of 2,925 mother-child pairs with data on peri-pregnancy eating patterns.
Maternal intake of ultra-processed foods while raising children was linked with obesity or overweight in children. Moreover, compared with the lowest consumption cohort (3.4 servings/day), there was a 26% greater risk for the greatest maternal ultra-processed food intake cohort (12.1 servings/day) after adjusting for child’s sedentary time, ultra-processed food intake, physical activity, and established maternal risk factors.
Even though rates were elevated, ultra-processed food intake during pregnancy was not significantly linked to a higher risk of obesity or overweight in children (P for trend = .07).
Sex, birth weight, age, gestational age, or maternal body weight had no effect on these correlations either.
The study’s limitations include the fact that some of the children in the pairs were lost during follow-up; there may have been data misreporting, as the weight and diet measures were provided via self-reported questionnaires; and potential residual confounding given the observational study design, the researchers note.
Other limitations include that the mothers involved in the study came from similar socioeconomic backgrounds, had similar personal and familial educational statuses, and were primarily White, which limits the generalizability of these data to other ethnic groups, the authors add.
“Further studies are warranted to investigate specific biological mechanisms and socioeconomic determinants underlying the observed associations between maternal ultra-processed food intake and offspring overweight and obesity,” the researchers conclude.
A version of this article first appeared on Medscape.com.
What role does the uterine microbiome play in fertility?
Until the second half of the 20th century, it was believed that the uterine cavity was sterile. Since then, technological advances have provided insight into the nature of the microbiome throughout the female reproductive tract. The role of these microorganisms on the fertility of women of reproductive age has been the subject of research. Is there an “optimal microbiome” for fertility? Can changing the microbiome of the uterine cavity affect fertility? There is still no definitive scientific response to these questions.
Several studies describe the healthy state of the uterine microbiota in women of reproductive age, with most of these studies reporting dominance of Lactobacillus species. However, by contrast, some studies did not observe Lactobacillus predominance inside the uterine cavity in cases of healthy uterine microbiomes. The presence of other microorganisms, such as Gardnerella vaginalis, was associated with reduced success in patients attempting in vitro fertilization (IVF) treatment, such as, for example, embryo implantation failure and miscarriage.
It is also possible that a physiologic endometrial microbiome could be considered healthy despite a minor presence of pathogenic bacteria. Importantly, responses from the host also modulate many aspects of human conception. These shifts correlate with parameters such as age, hormonal changes, ethnicity, sexual activity, and intrauterine devices.
Carlos Simón, MD, PhD, is a gynecologist and obstetrician and professor at the University of Valencia in Valencia, Spain; Harvard University, Cambridge, Mass.; and Baylor College of Medicine, Houston. He was in São Paulo at the time of the XXVI Brazilian Congress of Assisted Reproduction and agreed to be interviewed by Medscape Portuguese Edition. Dr. Simón, who is Spanish and is an international reference in uterine microbiome studies, created an endometrial receptivity analysis (ERA).
“What we know is that the human uterus has its own microbiome. Thanks to next-generation sequencing (NGS), we can detect microbial DNA. We’re talking about a microbiome that, if changed, affects [embryo] implantation. We have identified that Lactobacilli are the good [microorganisms], but if there are Streptococci, Gardnerella, or other bacteria, the implantation [of the embryo] is affected.”
In 2018, Dr. Simón’s team published a pilot study assessing the microbiome of 30 patients during fertilization treatment. It was observed that, when there is a change in the microbiome, the implantation rate drops to half and the miscarriage rate doubles.
Following this study, also in 2018, the team published a multicenter, prospective, observational study. A 16S ribosomal RNA (16S rRNA) gene sequencing technique was used to analyze endometrial fluid and biopsy samples before embryo transfer in a cohort of 342 infertile patients asymptomatic for infection. Participants underwent fertilization procedures in 13 centers on three continents.
A dysbiotic endometrial microbiota profile composed of Atopobium, Bifidobacterium, Chryseobacterium, Gardnerella, Haemophilus, Klebsiella, Neisseria, Staphylococcus, and Streptococcus was associated with unsuccessful outcomes. In contrast, Lactobacillus was consistently enriched in patients with live birth outcomes. The authors concluded that endometrial microbiota composition before embryo transfer is a useful biomarker to predict reproductive outcome.
“You see a microbial signature in patients who become pregnant, another in those who do not become pregnant, and yet another in those who miscarry,” Dr. Simón summarized. “By knowing this signature, the microbiome can be analyzed and treated so that it is stabilized before the embryo is transferred.”
What should be done?
Endometrial microbiome profiles do not use microbial cultures. They are obtained by NGS of the endometrial sample. This is because the 16S rRNA gene, which can be found in bacteria, presents hypervariable regions that serve as markers to identify the bacteria present.
If a microbiome is found to be somewhat unhealthy, it is theoretically possible to change its composition, increasing the chances of successful assisted reproduction. The administration of antibiotics and vaginal probiotics are two treatment approaches.
According to Dr. Simón, treatment is specific to the bacterium (metronidazole, and, if that fails, rifampicin for Gardnerella, amoxicillin and clavulanic acid for Streptococci). Once the pathogenic bacterium has been treated, the probiotics can be administered. “If all is well, we can then go ahead with the procedure,” he explained.
Dr. Simón pointed out that, with respect to treatment, knowledge is still limited and primarily based on case reports. “You look for issues in the microbiome when the patient experiences reproductive failure and there are no other causes,” he emphasized. “Microbiology plays a role in reproduction, affecting the human uterus. It’s good to know about it to improve reproductive outcomes. When there are repeated [embryo] implantation failures, we suggest an endometrial biopsy to identify the implantation window and determine whether the uterine microbiome is healthy or not. And if there are any abnormalities in the microbiome, they can be treated.”
There are still many open questions, such as how long the “good microbiome” lasts after antibiotic therapy. “We suggest checking the microbiome after [antibiotic] treatment and before implanting the embryo,” said Dr. Simón.
Although there is no consensus on how the endometrial microbiota relate to reproductive outcomes, the analysis and change in microbiome are already being offered in clinical practice as a way to increase the chances of conception. Márcia Riboldi, PhD, a genetics specialist serving as Country Manager for Igenomix Brasil and Argentina, the company that offers the analyses, provides an idea of the market for such analyses in Brazil. “We perform approximately 500 analyses per month,” she said, adding that most patients have a history of [embryo] implantation failure or miscarriage.
Matheus Roque, MD, PhD, an IVF specialist, shared two IVF case reports from the Mater Prime Human Reproduction Clinic in the southern region of the city of São Paulo. He emphasized that the decision to perform a microbiome analysis was made only after repeated implantation failure.
“With the outcomes the doctors started to see, the paradigm started to shift,” said Dr. Riboldi. “Why wait for the patient to have [an embryo] transfer failure? Let’s study the endometrium, check the ideal moment for the transfer, see whether it’s receptive or not, if there’s any disease and if there are Lactobacilli,” she proposed. “We need medical training and awareness, and we need to use them appropriately. We have the tests. Doctors need to learn about them and know when and how to use them.” The microbiome analysis costs approximately BRL 2,000, plus expenses for the medical procedure.
Is it too early?
Caio Parente Barbosa, MD, PhD, is an obstetrician/gynecologist specializing in human reproduction, as well as the director general and founder of the Fertile Idea Institute for Reproductive Health. He shared a few of his experiences in an interview with this news organization. “I would say it is still too early to confirm that [the microbiome analysis] produces effective outcomes.”
Dr. Barbosa, who is also provost of graduate studies, research, and innovation of the ABC School of Medicine, Santo André, Brazil, emphasized there is still little global experience with these analyses. “There are doubts worldwide regarding whether these analyses produce effective outcomes. Scientific studies are entirely controversial.”
He stated that some professionals recommend the microbiome analysis for “patients who don’t know what else to do,” but also recognized that there is already a demand for patients who don’t fit this category, who research the analyses on social networks and YouTube. “But it is the smallest of demands. Patients are not as worried about this yet.”
Dr. Barbosa recognized that the idea of an increasingly tailored treatment plan is inevitable. He believes that the study and treatment of the microbiome will become more critical in the future, but he thinks it still “does not offer any value.”
Dr. Barbosa emphasized that the financial side of things must also be considered. “If we add all these tests when investigating a patient’s issues, the treatment becomes ridiculously expensive.” He pointed out that health care professionals need to be careful to perform minimal testing. “We have already added some tests, such as the karyotype test, to the minimal testing for all patients.”
Dr. Simón responded to this criticism, stating: “The cost of repeating cycles is always greater than that of being thorough and knowing what’s going on. Nothing is certain, but if my daughter or wife needed it, I would like to have as much information as possible to make this decision.”
Dr. Barbosa and Dr. Simón reported no relevant financial relationships. Dr. Riboldi is Country Manager for Igenomix Brasil and Argentina, the company that offers the analyses.
This article was translated from the Medscape Portuguese edition and appeared on Medscape.com.
Until the second half of the 20th century, it was believed that the uterine cavity was sterile. Since then, technological advances have provided insight into the nature of the microbiome throughout the female reproductive tract. The role of these microorganisms on the fertility of women of reproductive age has been the subject of research. Is there an “optimal microbiome” for fertility? Can changing the microbiome of the uterine cavity affect fertility? There is still no definitive scientific response to these questions.
Several studies describe the healthy state of the uterine microbiota in women of reproductive age, with most of these studies reporting dominance of Lactobacillus species. However, by contrast, some studies did not observe Lactobacillus predominance inside the uterine cavity in cases of healthy uterine microbiomes. The presence of other microorganisms, such as Gardnerella vaginalis, was associated with reduced success in patients attempting in vitro fertilization (IVF) treatment, such as, for example, embryo implantation failure and miscarriage.
It is also possible that a physiologic endometrial microbiome could be considered healthy despite a minor presence of pathogenic bacteria. Importantly, responses from the host also modulate many aspects of human conception. These shifts correlate with parameters such as age, hormonal changes, ethnicity, sexual activity, and intrauterine devices.
Carlos Simón, MD, PhD, is a gynecologist and obstetrician and professor at the University of Valencia in Valencia, Spain; Harvard University, Cambridge, Mass.; and Baylor College of Medicine, Houston. He was in São Paulo at the time of the XXVI Brazilian Congress of Assisted Reproduction and agreed to be interviewed by Medscape Portuguese Edition. Dr. Simón, who is Spanish and is an international reference in uterine microbiome studies, created an endometrial receptivity analysis (ERA).
“What we know is that the human uterus has its own microbiome. Thanks to next-generation sequencing (NGS), we can detect microbial DNA. We’re talking about a microbiome that, if changed, affects [embryo] implantation. We have identified that Lactobacilli are the good [microorganisms], but if there are Streptococci, Gardnerella, or other bacteria, the implantation [of the embryo] is affected.”
In 2018, Dr. Simón’s team published a pilot study assessing the microbiome of 30 patients during fertilization treatment. It was observed that, when there is a change in the microbiome, the implantation rate drops to half and the miscarriage rate doubles.
Following this study, also in 2018, the team published a multicenter, prospective, observational study. A 16S ribosomal RNA (16S rRNA) gene sequencing technique was used to analyze endometrial fluid and biopsy samples before embryo transfer in a cohort of 342 infertile patients asymptomatic for infection. Participants underwent fertilization procedures in 13 centers on three continents.
A dysbiotic endometrial microbiota profile composed of Atopobium, Bifidobacterium, Chryseobacterium, Gardnerella, Haemophilus, Klebsiella, Neisseria, Staphylococcus, and Streptococcus was associated with unsuccessful outcomes. In contrast, Lactobacillus was consistently enriched in patients with live birth outcomes. The authors concluded that endometrial microbiota composition before embryo transfer is a useful biomarker to predict reproductive outcome.
“You see a microbial signature in patients who become pregnant, another in those who do not become pregnant, and yet another in those who miscarry,” Dr. Simón summarized. “By knowing this signature, the microbiome can be analyzed and treated so that it is stabilized before the embryo is transferred.”
What should be done?
Endometrial microbiome profiles do not use microbial cultures. They are obtained by NGS of the endometrial sample. This is because the 16S rRNA gene, which can be found in bacteria, presents hypervariable regions that serve as markers to identify the bacteria present.
If a microbiome is found to be somewhat unhealthy, it is theoretically possible to change its composition, increasing the chances of successful assisted reproduction. The administration of antibiotics and vaginal probiotics are two treatment approaches.
According to Dr. Simón, treatment is specific to the bacterium (metronidazole, and, if that fails, rifampicin for Gardnerella, amoxicillin and clavulanic acid for Streptococci). Once the pathogenic bacterium has been treated, the probiotics can be administered. “If all is well, we can then go ahead with the procedure,” he explained.
Dr. Simón pointed out that, with respect to treatment, knowledge is still limited and primarily based on case reports. “You look for issues in the microbiome when the patient experiences reproductive failure and there are no other causes,” he emphasized. “Microbiology plays a role in reproduction, affecting the human uterus. It’s good to know about it to improve reproductive outcomes. When there are repeated [embryo] implantation failures, we suggest an endometrial biopsy to identify the implantation window and determine whether the uterine microbiome is healthy or not. And if there are any abnormalities in the microbiome, they can be treated.”
There are still many open questions, such as how long the “good microbiome” lasts after antibiotic therapy. “We suggest checking the microbiome after [antibiotic] treatment and before implanting the embryo,” said Dr. Simón.
Although there is no consensus on how the endometrial microbiota relate to reproductive outcomes, the analysis and change in microbiome are already being offered in clinical practice as a way to increase the chances of conception. Márcia Riboldi, PhD, a genetics specialist serving as Country Manager for Igenomix Brasil and Argentina, the company that offers the analyses, provides an idea of the market for such analyses in Brazil. “We perform approximately 500 analyses per month,” she said, adding that most patients have a history of [embryo] implantation failure or miscarriage.
Matheus Roque, MD, PhD, an IVF specialist, shared two IVF case reports from the Mater Prime Human Reproduction Clinic in the southern region of the city of São Paulo. He emphasized that the decision to perform a microbiome analysis was made only after repeated implantation failure.
“With the outcomes the doctors started to see, the paradigm started to shift,” said Dr. Riboldi. “Why wait for the patient to have [an embryo] transfer failure? Let’s study the endometrium, check the ideal moment for the transfer, see whether it’s receptive or not, if there’s any disease and if there are Lactobacilli,” she proposed. “We need medical training and awareness, and we need to use them appropriately. We have the tests. Doctors need to learn about them and know when and how to use them.” The microbiome analysis costs approximately BRL 2,000, plus expenses for the medical procedure.
Is it too early?
Caio Parente Barbosa, MD, PhD, is an obstetrician/gynecologist specializing in human reproduction, as well as the director general and founder of the Fertile Idea Institute for Reproductive Health. He shared a few of his experiences in an interview with this news organization. “I would say it is still too early to confirm that [the microbiome analysis] produces effective outcomes.”
Dr. Barbosa, who is also provost of graduate studies, research, and innovation of the ABC School of Medicine, Santo André, Brazil, emphasized there is still little global experience with these analyses. “There are doubts worldwide regarding whether these analyses produce effective outcomes. Scientific studies are entirely controversial.”
He stated that some professionals recommend the microbiome analysis for “patients who don’t know what else to do,” but also recognized that there is already a demand for patients who don’t fit this category, who research the analyses on social networks and YouTube. “But it is the smallest of demands. Patients are not as worried about this yet.”
Dr. Barbosa recognized that the idea of an increasingly tailored treatment plan is inevitable. He believes that the study and treatment of the microbiome will become more critical in the future, but he thinks it still “does not offer any value.”
Dr. Barbosa emphasized that the financial side of things must also be considered. “If we add all these tests when investigating a patient’s issues, the treatment becomes ridiculously expensive.” He pointed out that health care professionals need to be careful to perform minimal testing. “We have already added some tests, such as the karyotype test, to the minimal testing for all patients.”
Dr. Simón responded to this criticism, stating: “The cost of repeating cycles is always greater than that of being thorough and knowing what’s going on. Nothing is certain, but if my daughter or wife needed it, I would like to have as much information as possible to make this decision.”
Dr. Barbosa and Dr. Simón reported no relevant financial relationships. Dr. Riboldi is Country Manager for Igenomix Brasil and Argentina, the company that offers the analyses.
This article was translated from the Medscape Portuguese edition and appeared on Medscape.com.
Until the second half of the 20th century, it was believed that the uterine cavity was sterile. Since then, technological advances have provided insight into the nature of the microbiome throughout the female reproductive tract. The role of these microorganisms on the fertility of women of reproductive age has been the subject of research. Is there an “optimal microbiome” for fertility? Can changing the microbiome of the uterine cavity affect fertility? There is still no definitive scientific response to these questions.
Several studies describe the healthy state of the uterine microbiota in women of reproductive age, with most of these studies reporting dominance of Lactobacillus species. However, by contrast, some studies did not observe Lactobacillus predominance inside the uterine cavity in cases of healthy uterine microbiomes. The presence of other microorganisms, such as Gardnerella vaginalis, was associated with reduced success in patients attempting in vitro fertilization (IVF) treatment, such as, for example, embryo implantation failure and miscarriage.
It is also possible that a physiologic endometrial microbiome could be considered healthy despite a minor presence of pathogenic bacteria. Importantly, responses from the host also modulate many aspects of human conception. These shifts correlate with parameters such as age, hormonal changes, ethnicity, sexual activity, and intrauterine devices.
Carlos Simón, MD, PhD, is a gynecologist and obstetrician and professor at the University of Valencia in Valencia, Spain; Harvard University, Cambridge, Mass.; and Baylor College of Medicine, Houston. He was in São Paulo at the time of the XXVI Brazilian Congress of Assisted Reproduction and agreed to be interviewed by Medscape Portuguese Edition. Dr. Simón, who is Spanish and is an international reference in uterine microbiome studies, created an endometrial receptivity analysis (ERA).
“What we know is that the human uterus has its own microbiome. Thanks to next-generation sequencing (NGS), we can detect microbial DNA. We’re talking about a microbiome that, if changed, affects [embryo] implantation. We have identified that Lactobacilli are the good [microorganisms], but if there are Streptococci, Gardnerella, or other bacteria, the implantation [of the embryo] is affected.”
In 2018, Dr. Simón’s team published a pilot study assessing the microbiome of 30 patients during fertilization treatment. It was observed that, when there is a change in the microbiome, the implantation rate drops to half and the miscarriage rate doubles.
Following this study, also in 2018, the team published a multicenter, prospective, observational study. A 16S ribosomal RNA (16S rRNA) gene sequencing technique was used to analyze endometrial fluid and biopsy samples before embryo transfer in a cohort of 342 infertile patients asymptomatic for infection. Participants underwent fertilization procedures in 13 centers on three continents.
A dysbiotic endometrial microbiota profile composed of Atopobium, Bifidobacterium, Chryseobacterium, Gardnerella, Haemophilus, Klebsiella, Neisseria, Staphylococcus, and Streptococcus was associated with unsuccessful outcomes. In contrast, Lactobacillus was consistently enriched in patients with live birth outcomes. The authors concluded that endometrial microbiota composition before embryo transfer is a useful biomarker to predict reproductive outcome.
“You see a microbial signature in patients who become pregnant, another in those who do not become pregnant, and yet another in those who miscarry,” Dr. Simón summarized. “By knowing this signature, the microbiome can be analyzed and treated so that it is stabilized before the embryo is transferred.”
What should be done?
Endometrial microbiome profiles do not use microbial cultures. They are obtained by NGS of the endometrial sample. This is because the 16S rRNA gene, which can be found in bacteria, presents hypervariable regions that serve as markers to identify the bacteria present.
If a microbiome is found to be somewhat unhealthy, it is theoretically possible to change its composition, increasing the chances of successful assisted reproduction. The administration of antibiotics and vaginal probiotics are two treatment approaches.
According to Dr. Simón, treatment is specific to the bacterium (metronidazole, and, if that fails, rifampicin for Gardnerella, amoxicillin and clavulanic acid for Streptococci). Once the pathogenic bacterium has been treated, the probiotics can be administered. “If all is well, we can then go ahead with the procedure,” he explained.
Dr. Simón pointed out that, with respect to treatment, knowledge is still limited and primarily based on case reports. “You look for issues in the microbiome when the patient experiences reproductive failure and there are no other causes,” he emphasized. “Microbiology plays a role in reproduction, affecting the human uterus. It’s good to know about it to improve reproductive outcomes. When there are repeated [embryo] implantation failures, we suggest an endometrial biopsy to identify the implantation window and determine whether the uterine microbiome is healthy or not. And if there are any abnormalities in the microbiome, they can be treated.”
There are still many open questions, such as how long the “good microbiome” lasts after antibiotic therapy. “We suggest checking the microbiome after [antibiotic] treatment and before implanting the embryo,” said Dr. Simón.
Although there is no consensus on how the endometrial microbiota relate to reproductive outcomes, the analysis and change in microbiome are already being offered in clinical practice as a way to increase the chances of conception. Márcia Riboldi, PhD, a genetics specialist serving as Country Manager for Igenomix Brasil and Argentina, the company that offers the analyses, provides an idea of the market for such analyses in Brazil. “We perform approximately 500 analyses per month,” she said, adding that most patients have a history of [embryo] implantation failure or miscarriage.
Matheus Roque, MD, PhD, an IVF specialist, shared two IVF case reports from the Mater Prime Human Reproduction Clinic in the southern region of the city of São Paulo. He emphasized that the decision to perform a microbiome analysis was made only after repeated implantation failure.
“With the outcomes the doctors started to see, the paradigm started to shift,” said Dr. Riboldi. “Why wait for the patient to have [an embryo] transfer failure? Let’s study the endometrium, check the ideal moment for the transfer, see whether it’s receptive or not, if there’s any disease and if there are Lactobacilli,” she proposed. “We need medical training and awareness, and we need to use them appropriately. We have the tests. Doctors need to learn about them and know when and how to use them.” The microbiome analysis costs approximately BRL 2,000, plus expenses for the medical procedure.
Is it too early?
Caio Parente Barbosa, MD, PhD, is an obstetrician/gynecologist specializing in human reproduction, as well as the director general and founder of the Fertile Idea Institute for Reproductive Health. He shared a few of his experiences in an interview with this news organization. “I would say it is still too early to confirm that [the microbiome analysis] produces effective outcomes.”
Dr. Barbosa, who is also provost of graduate studies, research, and innovation of the ABC School of Medicine, Santo André, Brazil, emphasized there is still little global experience with these analyses. “There are doubts worldwide regarding whether these analyses produce effective outcomes. Scientific studies are entirely controversial.”
He stated that some professionals recommend the microbiome analysis for “patients who don’t know what else to do,” but also recognized that there is already a demand for patients who don’t fit this category, who research the analyses on social networks and YouTube. “But it is the smallest of demands. Patients are not as worried about this yet.”
Dr. Barbosa recognized that the idea of an increasingly tailored treatment plan is inevitable. He believes that the study and treatment of the microbiome will become more critical in the future, but he thinks it still “does not offer any value.”
Dr. Barbosa emphasized that the financial side of things must also be considered. “If we add all these tests when investigating a patient’s issues, the treatment becomes ridiculously expensive.” He pointed out that health care professionals need to be careful to perform minimal testing. “We have already added some tests, such as the karyotype test, to the minimal testing for all patients.”
Dr. Simón responded to this criticism, stating: “The cost of repeating cycles is always greater than that of being thorough and knowing what’s going on. Nothing is certain, but if my daughter or wife needed it, I would like to have as much information as possible to make this decision.”
Dr. Barbosa and Dr. Simón reported no relevant financial relationships. Dr. Riboldi is Country Manager for Igenomix Brasil and Argentina, the company that offers the analyses.
This article was translated from the Medscape Portuguese edition and appeared on Medscape.com.
Mouse embryo experiment could teach us about miscarriages
Miscarriages are a devastating, if natural, occurrence. Nearly 1 million pregnant people in the United States experience a miscarriage every year, according to the National Advocates for Pregnant Women. New research could lend insight into the causes of some types of early pregnancy loss and maybe one day help prevent miscarriages.
In the bioengineering breakthrough, scientists created a mouse embryo in a lab without using sperm or eggs. The experimental embryo, called a model, was grown out of stem cells and developed further than any earlier experiments, with a beating heart and the foundation of a brain within a yolk sac, according to the researchers.
The experiment, while conducted with mouse stem cells, could help explain why some human pregnancies fail. Miscarriages occur in up to 15% of pregnancies confirmed by doctors, according to some studies, and also for many pregnant people before they even knew of the pregnancy. This experiment gives researchers a glimpse of a critical developmental stage for the first time.
“We are building mouse embryo models, but they have exactly the same principle as real human embryos,” says lead researcher Magdalena Zernicka-Goetz, PhD, professor in mammalian development and stem cell biology at Cambridge (England) University. “That’s why they tell us about real pregnancy.”
With the new mouse models, the researchers can study implantation, the stage when embryos embed themselves in the mother’s body – a stage that’s often difficult for embryos to survive. The same process happens in mouse embryos, which develop very similarly to human embryos at this early stage of life.
Six years ago, researchers from the University of Cambridge and the California Institute of Technology set out to create models that would allow them to study fetal development in three-dimensional form but without the need for human embryos.
“We are trying to understand the major principles of time and space that have to be fulfilled” to form a successful pregnancy, Dr. Zernicka-Goetz explains. “If those principles are not fulfilled, the pregnancies are terminated, even before women know they’re pregnant.”
There are limits on using human embryos for research, and previous experiments have tended to replicate only one aspect of development. That led to two-dimensional experiments: flat cells on the bottom of a petri dish that lack the structural organization of real tissue.
The new models are three-dimensional with beating hearts and the yolk sacs in which embryos feed and grow. The models even progressed to forming the beginning of a brain – a research first.
The scientists used the foundational cellular “building blocks” called stem cells and managed to get the cells to communicate along a timeline that mimicked natural development, simulating those developmental stages, says Dr. Zernicka-Goetz. Those “building blocks” are actually three types of stem cells: pluripotent stem cells that build body tissue, and two other types of stem cells that build the placenta and the amniotic sac.
Completing the experiment required the right quantity of each stem cell type. The researchers also needed to understand how those cells exchange information before they can begin to grow. The researchers were able to “decipher the code” of how the cells talk to each other, Dr. Zernicka-Goetz says.
Initially, the three types of stem cells combine, almost like a soup, but when the timing is right, they have to recognize each other and sort themselves. Next, each stem cell type must start building a different structure necessary for fetal development. Dr. Zernicka-Goetz thinks of this construction as the architecture of human tissue.
With the new technique, researchers can continue investigating the implantation stage and beyond. And they did – tweaking the experiment to create a genetically flawed embryo on purpose.
Dr. Zernicka-Goetz and her team eliminated a certain gene known to regulate how cells establish their own identities. Doing so resulted in the same brain development flaws as in human embryos, providing “a proof of concept” that the experimental models can be used to study other genetic mysteries, she says.
Scientists are still in the dark about what some genes do, as well as the point when they become critical to brain development.
“Many genes have very early roles in specifying, for example, the position of the head and also how our brain will function,” Dr. Zernicka-Goetz says. “We can now use this model system to assess the function of those genes.”
A version of this article first appeared on WebMD.com.
Miscarriages are a devastating, if natural, occurrence. Nearly 1 million pregnant people in the United States experience a miscarriage every year, according to the National Advocates for Pregnant Women. New research could lend insight into the causes of some types of early pregnancy loss and maybe one day help prevent miscarriages.
In the bioengineering breakthrough, scientists created a mouse embryo in a lab without using sperm or eggs. The experimental embryo, called a model, was grown out of stem cells and developed further than any earlier experiments, with a beating heart and the foundation of a brain within a yolk sac, according to the researchers.
The experiment, while conducted with mouse stem cells, could help explain why some human pregnancies fail. Miscarriages occur in up to 15% of pregnancies confirmed by doctors, according to some studies, and also for many pregnant people before they even knew of the pregnancy. This experiment gives researchers a glimpse of a critical developmental stage for the first time.
“We are building mouse embryo models, but they have exactly the same principle as real human embryos,” says lead researcher Magdalena Zernicka-Goetz, PhD, professor in mammalian development and stem cell biology at Cambridge (England) University. “That’s why they tell us about real pregnancy.”
With the new mouse models, the researchers can study implantation, the stage when embryos embed themselves in the mother’s body – a stage that’s often difficult for embryos to survive. The same process happens in mouse embryos, which develop very similarly to human embryos at this early stage of life.
Six years ago, researchers from the University of Cambridge and the California Institute of Technology set out to create models that would allow them to study fetal development in three-dimensional form but without the need for human embryos.
“We are trying to understand the major principles of time and space that have to be fulfilled” to form a successful pregnancy, Dr. Zernicka-Goetz explains. “If those principles are not fulfilled, the pregnancies are terminated, even before women know they’re pregnant.”
There are limits on using human embryos for research, and previous experiments have tended to replicate only one aspect of development. That led to two-dimensional experiments: flat cells on the bottom of a petri dish that lack the structural organization of real tissue.
The new models are three-dimensional with beating hearts and the yolk sacs in which embryos feed and grow. The models even progressed to forming the beginning of a brain – a research first.
The scientists used the foundational cellular “building blocks” called stem cells and managed to get the cells to communicate along a timeline that mimicked natural development, simulating those developmental stages, says Dr. Zernicka-Goetz. Those “building blocks” are actually three types of stem cells: pluripotent stem cells that build body tissue, and two other types of stem cells that build the placenta and the amniotic sac.
Completing the experiment required the right quantity of each stem cell type. The researchers also needed to understand how those cells exchange information before they can begin to grow. The researchers were able to “decipher the code” of how the cells talk to each other, Dr. Zernicka-Goetz says.
Initially, the three types of stem cells combine, almost like a soup, but when the timing is right, they have to recognize each other and sort themselves. Next, each stem cell type must start building a different structure necessary for fetal development. Dr. Zernicka-Goetz thinks of this construction as the architecture of human tissue.
With the new technique, researchers can continue investigating the implantation stage and beyond. And they did – tweaking the experiment to create a genetically flawed embryo on purpose.
Dr. Zernicka-Goetz and her team eliminated a certain gene known to regulate how cells establish their own identities. Doing so resulted in the same brain development flaws as in human embryos, providing “a proof of concept” that the experimental models can be used to study other genetic mysteries, she says.
Scientists are still in the dark about what some genes do, as well as the point when they become critical to brain development.
“Many genes have very early roles in specifying, for example, the position of the head and also how our brain will function,” Dr. Zernicka-Goetz says. “We can now use this model system to assess the function of those genes.”
A version of this article first appeared on WebMD.com.
Miscarriages are a devastating, if natural, occurrence. Nearly 1 million pregnant people in the United States experience a miscarriage every year, according to the National Advocates for Pregnant Women. New research could lend insight into the causes of some types of early pregnancy loss and maybe one day help prevent miscarriages.
In the bioengineering breakthrough, scientists created a mouse embryo in a lab without using sperm or eggs. The experimental embryo, called a model, was grown out of stem cells and developed further than any earlier experiments, with a beating heart and the foundation of a brain within a yolk sac, according to the researchers.
The experiment, while conducted with mouse stem cells, could help explain why some human pregnancies fail. Miscarriages occur in up to 15% of pregnancies confirmed by doctors, according to some studies, and also for many pregnant people before they even knew of the pregnancy. This experiment gives researchers a glimpse of a critical developmental stage for the first time.
“We are building mouse embryo models, but they have exactly the same principle as real human embryos,” says lead researcher Magdalena Zernicka-Goetz, PhD, professor in mammalian development and stem cell biology at Cambridge (England) University. “That’s why they tell us about real pregnancy.”
With the new mouse models, the researchers can study implantation, the stage when embryos embed themselves in the mother’s body – a stage that’s often difficult for embryos to survive. The same process happens in mouse embryos, which develop very similarly to human embryos at this early stage of life.
Six years ago, researchers from the University of Cambridge and the California Institute of Technology set out to create models that would allow them to study fetal development in three-dimensional form but without the need for human embryos.
“We are trying to understand the major principles of time and space that have to be fulfilled” to form a successful pregnancy, Dr. Zernicka-Goetz explains. “If those principles are not fulfilled, the pregnancies are terminated, even before women know they’re pregnant.”
There are limits on using human embryos for research, and previous experiments have tended to replicate only one aspect of development. That led to two-dimensional experiments: flat cells on the bottom of a petri dish that lack the structural organization of real tissue.
The new models are three-dimensional with beating hearts and the yolk sacs in which embryos feed and grow. The models even progressed to forming the beginning of a brain – a research first.
The scientists used the foundational cellular “building blocks” called stem cells and managed to get the cells to communicate along a timeline that mimicked natural development, simulating those developmental stages, says Dr. Zernicka-Goetz. Those “building blocks” are actually three types of stem cells: pluripotent stem cells that build body tissue, and two other types of stem cells that build the placenta and the amniotic sac.
Completing the experiment required the right quantity of each stem cell type. The researchers also needed to understand how those cells exchange information before they can begin to grow. The researchers were able to “decipher the code” of how the cells talk to each other, Dr. Zernicka-Goetz says.
Initially, the three types of stem cells combine, almost like a soup, but when the timing is right, they have to recognize each other and sort themselves. Next, each stem cell type must start building a different structure necessary for fetal development. Dr. Zernicka-Goetz thinks of this construction as the architecture of human tissue.
With the new technique, researchers can continue investigating the implantation stage and beyond. And they did – tweaking the experiment to create a genetically flawed embryo on purpose.
Dr. Zernicka-Goetz and her team eliminated a certain gene known to regulate how cells establish their own identities. Doing so resulted in the same brain development flaws as in human embryos, providing “a proof of concept” that the experimental models can be used to study other genetic mysteries, she says.
Scientists are still in the dark about what some genes do, as well as the point when they become critical to brain development.
“Many genes have very early roles in specifying, for example, the position of the head and also how our brain will function,” Dr. Zernicka-Goetz says. “We can now use this model system to assess the function of those genes.”
A version of this article first appeared on WebMD.com.
Rates of gestational diabetes in the United States, 2020