User login
Folic acid and multivitamin supplements associated with reduced autism risk
Taking folic acid and/or multivitamin supplements preceding and during pregnancy is associated with a lower risk of offspring developing autism spectrum disorder (ASD), an observational epidemiologic study published Jan. 3 showed.
The findings could have important public health implications, reported Stephen Z. Levine, PhD, and his associates.
The investigators found that 572 children, or 1.3%, received an ASD diagnosis. Dr. Levine and his associates found that children whose mothers took folic acid and multivitamin supplements during pregnancy had a lower risk of developing ASD (relative risk, 0.27; 95% confidence interval, 0.22-0.33; P less than .001), compared with those whose mothers took no supplements. Similarly, there was reduced risk among those whose mothers took only folic acid during pregnancy (RR, 0.32; CI, 0.26-0.41; P less than .001) or only multivitamins (RR, 0.35; CI, 0.28-0.44; P less than .001). Likewise, lower risks were seen among offspring whose mothers took supplements before pregnancy: Compared with no supplements, the RR was 0.39 for folic acid and/or multivitamins (CI, 0.30-0.50; P less than .001), 0.56 for just folic acid (95%CI, 0.42-0.74; P = .001), and 0.36 for just multivitamins (95%CI, 0.24-0.52; P less than .001). Similar associations were found among male and female offspring.
“This finding may reflect noncompliance, higher rates of vitamin deficiency, or poor diet among persons with psychiatric conditions,” wrote Dr. Levine, of the department of community mental health at the University of Haifa, Israel, and his associates in JAMA Psychiatry.
Another important finding is that maternal exposure to folic acid and multivitamin supplements 2 years before pregnancy is tied to a lower ASD risk.
The investigators acknowledged that the study was limited by their inability to determine possible confounding factors, such as the vehicle of vitamin dispensations, use of over-the-counter supplements, false-positive classifications from noncompliance, and absence of information on gestational age. In addition, they said, “causality cannot be inferred from observational studies such as this one.” In light of those limitations, investigators said, additional studies replicating these findings are needed.
The study was funded by several entities, including the National Institutes of Health, the Fredrik and Ingrid Thuring Foundation, and the Swedish Society of Medicine. Dr. Levine reported receiving support from Shire Pharmaceuticals, and coauthor Arad Kodesh, MD, is an employee of Meuhedet Health Services. No other relevant financial disclosures were reported.
SOURCE: Levine SZ et al. JAMA Psychiatry. 2018 Jan 3. doi: 10.1001/jamapsychiatry.2017.4050.
Taking folic acid and/or multivitamin supplements preceding and during pregnancy is associated with a lower risk of offspring developing autism spectrum disorder (ASD), an observational epidemiologic study published Jan. 3 showed.
The findings could have important public health implications, reported Stephen Z. Levine, PhD, and his associates.
The investigators found that 572 children, or 1.3%, received an ASD diagnosis. Dr. Levine and his associates found that children whose mothers took folic acid and multivitamin supplements during pregnancy had a lower risk of developing ASD (relative risk, 0.27; 95% confidence interval, 0.22-0.33; P less than .001), compared with those whose mothers took no supplements. Similarly, there was reduced risk among those whose mothers took only folic acid during pregnancy (RR, 0.32; CI, 0.26-0.41; P less than .001) or only multivitamins (RR, 0.35; CI, 0.28-0.44; P less than .001). Likewise, lower risks were seen among offspring whose mothers took supplements before pregnancy: Compared with no supplements, the RR was 0.39 for folic acid and/or multivitamins (CI, 0.30-0.50; P less than .001), 0.56 for just folic acid (95%CI, 0.42-0.74; P = .001), and 0.36 for just multivitamins (95%CI, 0.24-0.52; P less than .001). Similar associations were found among male and female offspring.
“This finding may reflect noncompliance, higher rates of vitamin deficiency, or poor diet among persons with psychiatric conditions,” wrote Dr. Levine, of the department of community mental health at the University of Haifa, Israel, and his associates in JAMA Psychiatry.
Another important finding is that maternal exposure to folic acid and multivitamin supplements 2 years before pregnancy is tied to a lower ASD risk.
The investigators acknowledged that the study was limited by their inability to determine possible confounding factors, such as the vehicle of vitamin dispensations, use of over-the-counter supplements, false-positive classifications from noncompliance, and absence of information on gestational age. In addition, they said, “causality cannot be inferred from observational studies such as this one.” In light of those limitations, investigators said, additional studies replicating these findings are needed.
The study was funded by several entities, including the National Institutes of Health, the Fredrik and Ingrid Thuring Foundation, and the Swedish Society of Medicine. Dr. Levine reported receiving support from Shire Pharmaceuticals, and coauthor Arad Kodesh, MD, is an employee of Meuhedet Health Services. No other relevant financial disclosures were reported.
SOURCE: Levine SZ et al. JAMA Psychiatry. 2018 Jan 3. doi: 10.1001/jamapsychiatry.2017.4050.
Taking folic acid and/or multivitamin supplements preceding and during pregnancy is associated with a lower risk of offspring developing autism spectrum disorder (ASD), an observational epidemiologic study published Jan. 3 showed.
The findings could have important public health implications, reported Stephen Z. Levine, PhD, and his associates.
The investigators found that 572 children, or 1.3%, received an ASD diagnosis. Dr. Levine and his associates found that children whose mothers took folic acid and multivitamin supplements during pregnancy had a lower risk of developing ASD (relative risk, 0.27; 95% confidence interval, 0.22-0.33; P less than .001), compared with those whose mothers took no supplements. Similarly, there was reduced risk among those whose mothers took only folic acid during pregnancy (RR, 0.32; CI, 0.26-0.41; P less than .001) or only multivitamins (RR, 0.35; CI, 0.28-0.44; P less than .001). Likewise, lower risks were seen among offspring whose mothers took supplements before pregnancy: Compared with no supplements, the RR was 0.39 for folic acid and/or multivitamins (CI, 0.30-0.50; P less than .001), 0.56 for just folic acid (95%CI, 0.42-0.74; P = .001), and 0.36 for just multivitamins (95%CI, 0.24-0.52; P less than .001). Similar associations were found among male and female offspring.
“This finding may reflect noncompliance, higher rates of vitamin deficiency, or poor diet among persons with psychiatric conditions,” wrote Dr. Levine, of the department of community mental health at the University of Haifa, Israel, and his associates in JAMA Psychiatry.
Another important finding is that maternal exposure to folic acid and multivitamin supplements 2 years before pregnancy is tied to a lower ASD risk.
The investigators acknowledged that the study was limited by their inability to determine possible confounding factors, such as the vehicle of vitamin dispensations, use of over-the-counter supplements, false-positive classifications from noncompliance, and absence of information on gestational age. In addition, they said, “causality cannot be inferred from observational studies such as this one.” In light of those limitations, investigators said, additional studies replicating these findings are needed.
The study was funded by several entities, including the National Institutes of Health, the Fredrik and Ingrid Thuring Foundation, and the Swedish Society of Medicine. Dr. Levine reported receiving support from Shire Pharmaceuticals, and coauthor Arad Kodesh, MD, is an employee of Meuhedet Health Services. No other relevant financial disclosures were reported.
SOURCE: Levine SZ et al. JAMA Psychiatry. 2018 Jan 3. doi: 10.1001/jamapsychiatry.2017.4050.
Key clinical point: Taking folic acid and multivitamin supplements before and during pregnancy can reduce risk of autism in children.
Major finding: Children whose mothers took folic acid and/or multivitamin supplements during pregnancy had a decreased risk of developing ASD, compared with those whose mothers did not (relative risk, 0.27; 95% confidence interval, 0.22-0.33; P less than .001).
Study details: Observational epidemiologic study of 45,300 Israeli children born between January 2003 and December 2007 and followed until January 2015.
Disclosures: The study was funded by several entities, including the National Institutes of Health, the Fredrik and Ingrid Thuring Foundation, and the Swedish Society of Medicine. Dr. Levine reported receiving support from Shire Pharmaceuticals, and coauthor Arad Kodesh, MD, is an employee of Meuhedet Health Services. No other relevant financial disclosures were reported.
Source: Levine SZ et al. JAMA Psychiatry. 2018 Jan 3. doi: 10.1001/jamapsychiatry.2017.4050.
2018 Update on obstetrics
The past year brought new information and guidance from the American College of Obstetricians and Gynecologists (ACOG) on many relevant obstetric topics, making it difficult to choose just a few for this Update. Opioid use in pregnancy was an obvious choice given the national media attention and the potential opportunity for intervention in pregnancy for both the mother and the fetus/newborn. Postpartum hemorrhage, an “oldie but goodie,” was chosen for several reasons: It got a new definition, a new focus on multidisciplinary care, and an exciting novel tool for the treatment toolbox. Finally, given the rapidly changing technology, new screening recommendations, and the complexity of counseling, carrier screening was chosen as a genetic hot topic for this year.
Opioids, obstetrics, and opportunities
Reddy UM, Davis JM, Ren Z, Greene MF; Opioid Use in Pregnancy, Neonatal Abstinence Syndrome, and Childhood Outcomes Workshop Invited Speakers. Opioid use in pregnancy, neonatal abstinence syndrome, and childhood outcomes: Executive summary of a joint workshop. Obstet Gynecol. 2017;130(1):10-28.
ACOG Committee on Obstetric Practice. ACOG committee opinion No. 711: Opioid use and opioid use disorder in pregnancy. Obstet Gynecol. 2017;130(2):e81-e94.
The term "opioid epidemic" is omnipresent in both the lay media and the medical literature. In the past decade, the United States has had a huge increase in the number of opioid prescriptions, the rate of admissions and deaths due to prescription opioid misuse and abuse, and an increased rate of heroin use attributed to prior prescription opioid use.
Obstetrics is unique in that opioid use and abuse disorders affect 2 patients simultaneously (the mother and fetus), and the treatment options are somewhat at odds in that they need to balance a stable maternal status and intrauterine environment with the risk of neonatal abstinence syndrome (NAS). Additionally, pregnancy is an opportunity for a woman with opioid use disorder to have access to medical care (possibly for the first time) leading to the diagnosis and treatment of her disease. As the clinicians on the front line, obstetricians therefore require education and guidance on best practice for management of opioid use in pregnancy.
In 2017, Reddy and colleagues, as part of a joint workshop on opioid use in pregnancy, and a committee opinion from ACOG provided the following recommendations.
Screening
Universally screen for substance use, starting at the first prenatal visit; this is recommended over risk factor-based screening.
Use a validated screening tool. A tool such as a questionnaire is recommended as the first-line screening test (for example, the 4Ps screen, the National Institute on Drug Abuse Quick Screen, and the CRAFFT Screening Interview).
Do not universally screen urine and hair for drugs. This type of screening has many limitations, such as the limited number of substances tested, false-positive results, and inaccurate determination of the frequency or timing of drug use. Information regarding the consequences of the test must be provided, and patient consent must be obtained prior to performing the test.
Treatment
Use medication-assisted treatment with buprenorphine or methadone, which is preferred to medically supervised withdrawal. Medication-assisted treatment prevents withdrawal symptoms and cravings, decreases the risk of relapse, improves compliance with prenatal care and addiction treatment programs, and leads to better obstetric outcomes (higher birth weight, lower rate of preterm birth, lower perinatal mortality).
Know that buprenorphine has several advantages over methadone, including the convenience of an outpatient prescription, a lower risk of overdose, and improved neonatal outcomes (higher birth weight, lower doses of morphine to treat NAS, shorter treatment duration).
Prioritize methadone as the preferred option for pregnant women who are already receiving methadone treatment (changing to buprenorphine may precipitate withdrawal), those with a long-standing history of or multi-substance abuse, and those who have failed other treatment programs.
Prenatal care
Screen for comorbid conditions such as sexually transmitted infections, other medications or substance use, social conditions, and mental health disorders.
Perform ultrasonography serially to monitor fetal growth because of the increased risk of fetal growth restriction.
Consult with anesthesiology for pain control recommendations for labor and delivery and with neonatalogy/pediatrics for NAS counseling.
Intrapartum/postpartum care
Recognize heightened pain. Women with opioid use disorder have increased sensitivity to painful stimuli.
Continue the maintenance dose of methadone or buprenorphine throughout hospitalization, with short-acting opioids added for a brief period for postoperative pain.
Prioritize regional anesthesia for pain control in labor or for cesarean delivery.
Consider alternative therapies such as regional blocks, nonopioid medications (nonsteroidal anti-inflammatory drugs, acetaminophen), or relaxation/mindfulness training.
Avoid mixed antagonist and agonist narcotics (butorphanol, nalbuphine, pentazocine) as they may cause acute withdrawal.
Encourage breastfeeding to decrease the severity of NAS and maternal stress and increase maternal-child bonding and maternal confidence.
Offer contraceptive counseling and services immediately postpartum in the hospital, with strong consideration for long-acting reversible contraception.
Opioid prescribing practices
Opioids are prescribed in excess post–cesarean delivery. Several recent studies have demonstrated that most women are prescribed opioids post–cesarean delivery in excess of the amount they use (median 30–40 tablets prescribed, median 20 tablets used).1,2 The leftover opioid medication usually is not discarded and therefore is at risk for diversion or misuse. A small subset of patients will use all the opioids prescribed and feel as though they have not received enough medication.
Prescribe post–cesarean delivery opioids more appropriately by considering individual inpatient opioid requirements or a shared decision-making model.3
Prioritize acetaminophen and ibuprofen during breastfeeding. In a recent editorial in OBG Management, Robert L. Barbieri, MD, recommended that whenever possible, acetaminophen and ibuprofen should be the first-line treatment for breastfeeding women, and narcotics that are metabolized by CYP2D6 should be avoided to reduce the risk to the newborn.4
Universal screening for substance use should be performed in all pregnant women, and clinicians should offer medication-assisted treatment in conjunction with prenatal care and other supportive services as the standard therapy for opioid use disorder. More selective, patient-specific opioid prescribing practices should be applied in the obstetric population.
Read about new strategies for postpartum hemorrhage.
Postpartum hemorrhage: New definitions and new strategies for stemming the flow
ACOG Committee on Practice Bulletins—Obstetrics. ACOG practice bulletin No. 183: Postpartum hemorrhage. Obstet Gynecol. 2017;130(4):e168-e186.
From the very first sentence of the new ACOG practice bulletin, postpartum hemorrhage (PPH) is redefined as "cumulative blood loss greater than or equal to 1,000 mL or blood loss accompanied by signs or symptoms of hypovolemia within 24 hours after the birth process (includes intrapartum loss) regardless of route of delivery." Although this does not seem to be a huge change from the traditional teaching of a 500-mL blood loss at vaginal delivery and a 1,000-mL loss at cesarean delivery, it reflects a shift in focus from simply responding to a certain amount of bleeding to using a multidisciplinary action plan for treating this leading cause of maternal mortality worldwide.
Focus on developing a PPH action plan
As part of the shift toward a multidisciplinary action plan for PPH, all obstetric team members should be aware of the following:
- For most postpartum women, by the time they begin to show signs of hemodynamic compromise, the amount of blood loss approaches 25% of their total blood volume (1,500 mL). Lactic acidosis, systemic inflammation, and a consumptive coagulopathy result.
- Risk stratification prior to delivery, recognition and identification of the source of bleeding, and aggressive early resuscitation to prevent hypovolemia are paramount. Experience gleaned from trauma massive transfusion protocols suggests that judicious transfusion of packed red blood cells, fresh frozen plasma, and platelets in a 1:1:1 ratio is appropriate for obstetric patients. Additionally, patients with low fibrinogen levels should be treated with cryoprecipitate.
- The use of fixed transfusion ratios and standardized protocols for recognition and management of PPH has been demonstrated to increase earlier intervention and resolution of hemorrhage at an earlier stage, although the maternal outcomes results have been mixed.
- Multidisciplinary team drills and simulation exercises also should be considered to help solidify training of an institution's teams responsible for PPH response.
Novel management option: Tranexamic acid
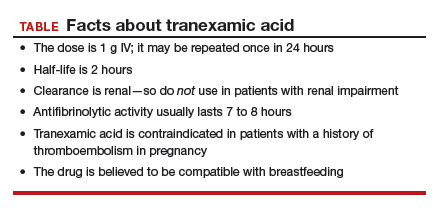
In addition to these strategies, there is a new recommendation for managing refractory PPH: tranexamic acid, which works by binding to lysine receptors on plasminogen and plasmin, inhibiting plasmin-mediated fibrin degradation.5 Previously, tranexamic acid was known to be effective in trauma, heart surgery, and in patients with thrombophilias. Pacheco and colleagues recently demonstrated reduced mortality from obstetric bleeding if tranexamic acid was given within 3 hours of delivery, without increased thrombotic complications.5 ACOG recommends its use if initial medical therapy fails, while the World Health Organization strongly recommends that tranexamic acid be part of a standard PPH package for all cases of PPH (TABLE).6
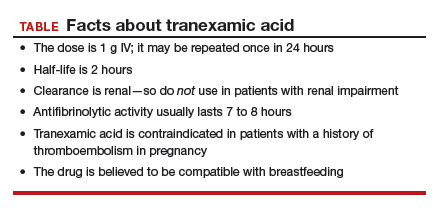
Postpartum hemorrhage requires early, aggressive, and multidisciplinary coordination to ensure that 1) patients at risk for hemorrhage are identified for preventive measures; 2) existing hemorrhage is recognized and quickly treated, first with noninvasive methods and then with more definitive surgical treatments; and 3) blood product replacement follows an evidence-based standardized protocol. Tranexamic acid is recommended as an adjunct treatment for PPH (of any cause) and should be used within 3 hours of delivery.
Read about new ACOG guidance on prepregnancy and prenatal screening.
Carrier screening—choose something
ACOG Committee on Genetics. Committee opinion No. 690: Carrier screening in the age of genomic medicine. Obstet Gynecol. 2017;129(3):e35-e40.
ACOG Committee on Genetics. Committee opinion No. 691: Carrier screening for genetic conditions. Obstet Gynecol. 2017;129(3):e41-e55.
Ideally, carrier screening should be offered prior to pregnancy to fully inform couples of their reproductive risks and options for pregnancy. If not performed in the preconception period, carrier screening should be offered to all pregnant women. If a patient chooses screening and screens positive for a particular disorder, her reproductive partner should then be offered screening so that the risk of having an affected child can be determined.
New ACOG guidance on prepregnancy and prenatal screening
Carrier screening recommendations have evolved as the technology available has expanded. All 3 of the following strategies now are considered "acceptable" according to 2 recently published ACOG committee opinions.
Traditional ethnic-specific carrier screening, previously ACOG's sole recommendation, involves offering specific genetic screening to patients from populations with a high prevalence for certain conditions. One such example is Tay-Sachs disease screening in Ashkenazi Jewish patients.
Panethnic screening, which takes into account mixed or uncertain backgrounds, involves screening for a certain panel of disorders and is available to all patients regardless of their background (for example, cystic fibrosis screening offered to all pregnant patients).
Expanded carrier screening is when a large number of disorders can be screened for simultaneously for a lower cost than previous testing strategies. Expanded carrier screening panels vary in number and which conditions are tested by the laboratory. An ideal expanded carrier screening panel has been debated in the literature but not agreed on.7
ObGyns and practices therefore are encouraged to develop a standard counseling and screening protocol to offer to all their patients while being flexible to make available any patient-requested screening that is outside their protocol. Pretest and posttest counseling, including a thorough family history, is essential (as with any genetic testing) and should include residual risk after testing, potential need for specific familial mutation testing instead of general carrier screening, and issues with consanguinity.
Three essential screens
Regardless of the screening strategy chosen from the above options, 3 screening tests should be offered to all pregnant women or couples considering pregnancy (either individually or in the context of an expanded screening panel):
- Cystic fibrosis. At the least, a panel of the 23 most common mutations should be used. More expanded panels, which include hundreds of mutations, increase detection in non-Caucasian populations and for milder forms of the disease or infertility-related mutations.
- Hemoglobinopathies (sickle cell, α- and β-thalassemia). Complete blood count and red blood indices are recommended for all, with hemoglobin electrophoresis recommended for patients of African, Middle Eastern, Mediterranean, or West Indian descent or if mean corpuscular volume is low.
- Spinal muscular atrophy (SMA). The most recent addition to ACOG's recommendations for general carrier screening due to the relatively high carrier frequency (1-in-40 to 1-in-60) and the severity of the disease, SMA causes degeneration of the spinal cord neurons, skeletal muscular atrophy, and overall weakness. Screening is via polymerase chain reaction for SMN1 copy number: 2 copies are normal, and 1 copy indicates a carrier of the SMN1 deletion. About 3% to 4% of patients will screen negative but still will be "carriers" due to having 2 copies of the SMN1 gene on 1 chromosome and no copies on the other chromosome.
All pregnant patients or patients considering pregnancy should be offered carrier screening as standard reproductive care, including screening for cystic fibrosis, hemoglobinopathies, and spinal muscular atrophy. Ethnic, panethnic, or expanded carrier screening (and patient-requested specific screening) all are acceptable options, and a standard screening and counseling protocol should be determined by the ObGyn or practice.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130(1):29–35.
- Osmundson SS, Schornack LA, Grasch JL, Zuckerwise LC, Young JL, Richardson MD. Postdischarge opioid use after cesarean delivery. Obstet Gynecol. 2017;130(1):36–41.
- Prabhu M, McQuaid-Hanson E, Hopp S, et al. A shared decision-making intervention to guide opioid prescribing after cesarean delivery. Obstet Gynecol. 2017;130(1):42–46.
- Barbieri RL. Stop using codeine, oxycodone, hydrocodone, tramadol, and aspirin in women who are breastfeeding. OBG Manag. 2017;29(10):8–12.
- Pacheco LD, Hankins GD, Saad AF, Costantine MM, Chiossi G, Saade GR. Tranexamic acid for the management of obstetric hemorrhage. Obstet Gynecol. 2017;130(4);765–769.
- WHO recommendation on tranexamic acid for the treatment of postpartum haemorrhage. Geneva, Switzerland: World Health Organization; 2017.
- Stevens B, Krstic N, Jones M, Murphy L, Hoskovec J. Finding middle ground in constructing a clinically useful expanded carrier screening panel. Obstet Gynecol. 2017;130(2):279–284.
The past year brought new information and guidance from the American College of Obstetricians and Gynecologists (ACOG) on many relevant obstetric topics, making it difficult to choose just a few for this Update. Opioid use in pregnancy was an obvious choice given the national media attention and the potential opportunity for intervention in pregnancy for both the mother and the fetus/newborn. Postpartum hemorrhage, an “oldie but goodie,” was chosen for several reasons: It got a new definition, a new focus on multidisciplinary care, and an exciting novel tool for the treatment toolbox. Finally, given the rapidly changing technology, new screening recommendations, and the complexity of counseling, carrier screening was chosen as a genetic hot topic for this year.
Opioids, obstetrics, and opportunities
Reddy UM, Davis JM, Ren Z, Greene MF; Opioid Use in Pregnancy, Neonatal Abstinence Syndrome, and Childhood Outcomes Workshop Invited Speakers. Opioid use in pregnancy, neonatal abstinence syndrome, and childhood outcomes: Executive summary of a joint workshop. Obstet Gynecol. 2017;130(1):10-28.
ACOG Committee on Obstetric Practice. ACOG committee opinion No. 711: Opioid use and opioid use disorder in pregnancy. Obstet Gynecol. 2017;130(2):e81-e94.
The term "opioid epidemic" is omnipresent in both the lay media and the medical literature. In the past decade, the United States has had a huge increase in the number of opioid prescriptions, the rate of admissions and deaths due to prescription opioid misuse and abuse, and an increased rate of heroin use attributed to prior prescription opioid use.
Obstetrics is unique in that opioid use and abuse disorders affect 2 patients simultaneously (the mother and fetus), and the treatment options are somewhat at odds in that they need to balance a stable maternal status and intrauterine environment with the risk of neonatal abstinence syndrome (NAS). Additionally, pregnancy is an opportunity for a woman with opioid use disorder to have access to medical care (possibly for the first time) leading to the diagnosis and treatment of her disease. As the clinicians on the front line, obstetricians therefore require education and guidance on best practice for management of opioid use in pregnancy.
In 2017, Reddy and colleagues, as part of a joint workshop on opioid use in pregnancy, and a committee opinion from ACOG provided the following recommendations.
Screening
Universally screen for substance use, starting at the first prenatal visit; this is recommended over risk factor-based screening.
Use a validated screening tool. A tool such as a questionnaire is recommended as the first-line screening test (for example, the 4Ps screen, the National Institute on Drug Abuse Quick Screen, and the CRAFFT Screening Interview).
Do not universally screen urine and hair for drugs. This type of screening has many limitations, such as the limited number of substances tested, false-positive results, and inaccurate determination of the frequency or timing of drug use. Information regarding the consequences of the test must be provided, and patient consent must be obtained prior to performing the test.
Treatment
Use medication-assisted treatment with buprenorphine or methadone, which is preferred to medically supervised withdrawal. Medication-assisted treatment prevents withdrawal symptoms and cravings, decreases the risk of relapse, improves compliance with prenatal care and addiction treatment programs, and leads to better obstetric outcomes (higher birth weight, lower rate of preterm birth, lower perinatal mortality).
Know that buprenorphine has several advantages over methadone, including the convenience of an outpatient prescription, a lower risk of overdose, and improved neonatal outcomes (higher birth weight, lower doses of morphine to treat NAS, shorter treatment duration).
Prioritize methadone as the preferred option for pregnant women who are already receiving methadone treatment (changing to buprenorphine may precipitate withdrawal), those with a long-standing history of or multi-substance abuse, and those who have failed other treatment programs.
Prenatal care
Screen for comorbid conditions such as sexually transmitted infections, other medications or substance use, social conditions, and mental health disorders.
Perform ultrasonography serially to monitor fetal growth because of the increased risk of fetal growth restriction.
Consult with anesthesiology for pain control recommendations for labor and delivery and with neonatalogy/pediatrics for NAS counseling.
Intrapartum/postpartum care
Recognize heightened pain. Women with opioid use disorder have increased sensitivity to painful stimuli.
Continue the maintenance dose of methadone or buprenorphine throughout hospitalization, with short-acting opioids added for a brief period for postoperative pain.
Prioritize regional anesthesia for pain control in labor or for cesarean delivery.
Consider alternative therapies such as regional blocks, nonopioid medications (nonsteroidal anti-inflammatory drugs, acetaminophen), or relaxation/mindfulness training.
Avoid mixed antagonist and agonist narcotics (butorphanol, nalbuphine, pentazocine) as they may cause acute withdrawal.
Encourage breastfeeding to decrease the severity of NAS and maternal stress and increase maternal-child bonding and maternal confidence.
Offer contraceptive counseling and services immediately postpartum in the hospital, with strong consideration for long-acting reversible contraception.
Opioid prescribing practices
Opioids are prescribed in excess post–cesarean delivery. Several recent studies have demonstrated that most women are prescribed opioids post–cesarean delivery in excess of the amount they use (median 30–40 tablets prescribed, median 20 tablets used).1,2 The leftover opioid medication usually is not discarded and therefore is at risk for diversion or misuse. A small subset of patients will use all the opioids prescribed and feel as though they have not received enough medication.
Prescribe post–cesarean delivery opioids more appropriately by considering individual inpatient opioid requirements or a shared decision-making model.3
Prioritize acetaminophen and ibuprofen during breastfeeding. In a recent editorial in OBG Management, Robert L. Barbieri, MD, recommended that whenever possible, acetaminophen and ibuprofen should be the first-line treatment for breastfeeding women, and narcotics that are metabolized by CYP2D6 should be avoided to reduce the risk to the newborn.4
Universal screening for substance use should be performed in all pregnant women, and clinicians should offer medication-assisted treatment in conjunction with prenatal care and other supportive services as the standard therapy for opioid use disorder. More selective, patient-specific opioid prescribing practices should be applied in the obstetric population.
Read about new strategies for postpartum hemorrhage.
Postpartum hemorrhage: New definitions and new strategies for stemming the flow
ACOG Committee on Practice Bulletins—Obstetrics. ACOG practice bulletin No. 183: Postpartum hemorrhage. Obstet Gynecol. 2017;130(4):e168-e186.
From the very first sentence of the new ACOG practice bulletin, postpartum hemorrhage (PPH) is redefined as "cumulative blood loss greater than or equal to 1,000 mL or blood loss accompanied by signs or symptoms of hypovolemia within 24 hours after the birth process (includes intrapartum loss) regardless of route of delivery." Although this does not seem to be a huge change from the traditional teaching of a 500-mL blood loss at vaginal delivery and a 1,000-mL loss at cesarean delivery, it reflects a shift in focus from simply responding to a certain amount of bleeding to using a multidisciplinary action plan for treating this leading cause of maternal mortality worldwide.
Focus on developing a PPH action plan
As part of the shift toward a multidisciplinary action plan for PPH, all obstetric team members should be aware of the following:
- For most postpartum women, by the time they begin to show signs of hemodynamic compromise, the amount of blood loss approaches 25% of their total blood volume (1,500 mL). Lactic acidosis, systemic inflammation, and a consumptive coagulopathy result.
- Risk stratification prior to delivery, recognition and identification of the source of bleeding, and aggressive early resuscitation to prevent hypovolemia are paramount. Experience gleaned from trauma massive transfusion protocols suggests that judicious transfusion of packed red blood cells, fresh frozen plasma, and platelets in a 1:1:1 ratio is appropriate for obstetric patients. Additionally, patients with low fibrinogen levels should be treated with cryoprecipitate.
- The use of fixed transfusion ratios and standardized protocols for recognition and management of PPH has been demonstrated to increase earlier intervention and resolution of hemorrhage at an earlier stage, although the maternal outcomes results have been mixed.
- Multidisciplinary team drills and simulation exercises also should be considered to help solidify training of an institution's teams responsible for PPH response.
Novel management option: Tranexamic acid
In addition to these strategies, there is a new recommendation for managing refractory PPH: tranexamic acid, which works by binding to lysine receptors on plasminogen and plasmin, inhibiting plasmin-mediated fibrin degradation.5 Previously, tranexamic acid was known to be effective in trauma, heart surgery, and in patients with thrombophilias. Pacheco and colleagues recently demonstrated reduced mortality from obstetric bleeding if tranexamic acid was given within 3 hours of delivery, without increased thrombotic complications.5 ACOG recommends its use if initial medical therapy fails, while the World Health Organization strongly recommends that tranexamic acid be part of a standard PPH package for all cases of PPH (TABLE).6
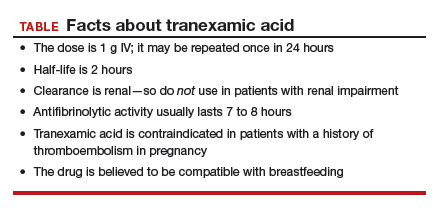
Postpartum hemorrhage requires early, aggressive, and multidisciplinary coordination to ensure that 1) patients at risk for hemorrhage are identified for preventive measures; 2) existing hemorrhage is recognized and quickly treated, first with noninvasive methods and then with more definitive surgical treatments; and 3) blood product replacement follows an evidence-based standardized protocol. Tranexamic acid is recommended as an adjunct treatment for PPH (of any cause) and should be used within 3 hours of delivery.
Read about new ACOG guidance on prepregnancy and prenatal screening.
Carrier screening—choose something
ACOG Committee on Genetics. Committee opinion No. 690: Carrier screening in the age of genomic medicine. Obstet Gynecol. 2017;129(3):e35-e40.
ACOG Committee on Genetics. Committee opinion No. 691: Carrier screening for genetic conditions. Obstet Gynecol. 2017;129(3):e41-e55.
Ideally, carrier screening should be offered prior to pregnancy to fully inform couples of their reproductive risks and options for pregnancy. If not performed in the preconception period, carrier screening should be offered to all pregnant women. If a patient chooses screening and screens positive for a particular disorder, her reproductive partner should then be offered screening so that the risk of having an affected child can be determined.
New ACOG guidance on prepregnancy and prenatal screening
Carrier screening recommendations have evolved as the technology available has expanded. All 3 of the following strategies now are considered "acceptable" according to 2 recently published ACOG committee opinions.
Traditional ethnic-specific carrier screening, previously ACOG's sole recommendation, involves offering specific genetic screening to patients from populations with a high prevalence for certain conditions. One such example is Tay-Sachs disease screening in Ashkenazi Jewish patients.
Panethnic screening, which takes into account mixed or uncertain backgrounds, involves screening for a certain panel of disorders and is available to all patients regardless of their background (for example, cystic fibrosis screening offered to all pregnant patients).
Expanded carrier screening is when a large number of disorders can be screened for simultaneously for a lower cost than previous testing strategies. Expanded carrier screening panels vary in number and which conditions are tested by the laboratory. An ideal expanded carrier screening panel has been debated in the literature but not agreed on.7
ObGyns and practices therefore are encouraged to develop a standard counseling and screening protocol to offer to all their patients while being flexible to make available any patient-requested screening that is outside their protocol. Pretest and posttest counseling, including a thorough family history, is essential (as with any genetic testing) and should include residual risk after testing, potential need for specific familial mutation testing instead of general carrier screening, and issues with consanguinity.
Three essential screens
Regardless of the screening strategy chosen from the above options, 3 screening tests should be offered to all pregnant women or couples considering pregnancy (either individually or in the context of an expanded screening panel):
- Cystic fibrosis. At the least, a panel of the 23 most common mutations should be used. More expanded panels, which include hundreds of mutations, increase detection in non-Caucasian populations and for milder forms of the disease or infertility-related mutations.
- Hemoglobinopathies (sickle cell, α- and β-thalassemia). Complete blood count and red blood indices are recommended for all, with hemoglobin electrophoresis recommended for patients of African, Middle Eastern, Mediterranean, or West Indian descent or if mean corpuscular volume is low.
- Spinal muscular atrophy (SMA). The most recent addition to ACOG's recommendations for general carrier screening due to the relatively high carrier frequency (1-in-40 to 1-in-60) and the severity of the disease, SMA causes degeneration of the spinal cord neurons, skeletal muscular atrophy, and overall weakness. Screening is via polymerase chain reaction for SMN1 copy number: 2 copies are normal, and 1 copy indicates a carrier of the SMN1 deletion. About 3% to 4% of patients will screen negative but still will be "carriers" due to having 2 copies of the SMN1 gene on 1 chromosome and no copies on the other chromosome.
All pregnant patients or patients considering pregnancy should be offered carrier screening as standard reproductive care, including screening for cystic fibrosis, hemoglobinopathies, and spinal muscular atrophy. Ethnic, panethnic, or expanded carrier screening (and patient-requested specific screening) all are acceptable options, and a standard screening and counseling protocol should be determined by the ObGyn or practice.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The past year brought new information and guidance from the American College of Obstetricians and Gynecologists (ACOG) on many relevant obstetric topics, making it difficult to choose just a few for this Update. Opioid use in pregnancy was an obvious choice given the national media attention and the potential opportunity for intervention in pregnancy for both the mother and the fetus/newborn. Postpartum hemorrhage, an “oldie but goodie,” was chosen for several reasons: It got a new definition, a new focus on multidisciplinary care, and an exciting novel tool for the treatment toolbox. Finally, given the rapidly changing technology, new screening recommendations, and the complexity of counseling, carrier screening was chosen as a genetic hot topic for this year.
Opioids, obstetrics, and opportunities
Reddy UM, Davis JM, Ren Z, Greene MF; Opioid Use in Pregnancy, Neonatal Abstinence Syndrome, and Childhood Outcomes Workshop Invited Speakers. Opioid use in pregnancy, neonatal abstinence syndrome, and childhood outcomes: Executive summary of a joint workshop. Obstet Gynecol. 2017;130(1):10-28.
ACOG Committee on Obstetric Practice. ACOG committee opinion No. 711: Opioid use and opioid use disorder in pregnancy. Obstet Gynecol. 2017;130(2):e81-e94.
The term "opioid epidemic" is omnipresent in both the lay media and the medical literature. In the past decade, the United States has had a huge increase in the number of opioid prescriptions, the rate of admissions and deaths due to prescription opioid misuse and abuse, and an increased rate of heroin use attributed to prior prescription opioid use.
Obstetrics is unique in that opioid use and abuse disorders affect 2 patients simultaneously (the mother and fetus), and the treatment options are somewhat at odds in that they need to balance a stable maternal status and intrauterine environment with the risk of neonatal abstinence syndrome (NAS). Additionally, pregnancy is an opportunity for a woman with opioid use disorder to have access to medical care (possibly for the first time) leading to the diagnosis and treatment of her disease. As the clinicians on the front line, obstetricians therefore require education and guidance on best practice for management of opioid use in pregnancy.
In 2017, Reddy and colleagues, as part of a joint workshop on opioid use in pregnancy, and a committee opinion from ACOG provided the following recommendations.
Screening
Universally screen for substance use, starting at the first prenatal visit; this is recommended over risk factor-based screening.
Use a validated screening tool. A tool such as a questionnaire is recommended as the first-line screening test (for example, the 4Ps screen, the National Institute on Drug Abuse Quick Screen, and the CRAFFT Screening Interview).
Do not universally screen urine and hair for drugs. This type of screening has many limitations, such as the limited number of substances tested, false-positive results, and inaccurate determination of the frequency or timing of drug use. Information regarding the consequences of the test must be provided, and patient consent must be obtained prior to performing the test.
Treatment
Use medication-assisted treatment with buprenorphine or methadone, which is preferred to medically supervised withdrawal. Medication-assisted treatment prevents withdrawal symptoms and cravings, decreases the risk of relapse, improves compliance with prenatal care and addiction treatment programs, and leads to better obstetric outcomes (higher birth weight, lower rate of preterm birth, lower perinatal mortality).
Know that buprenorphine has several advantages over methadone, including the convenience of an outpatient prescription, a lower risk of overdose, and improved neonatal outcomes (higher birth weight, lower doses of morphine to treat NAS, shorter treatment duration).
Prioritize methadone as the preferred option for pregnant women who are already receiving methadone treatment (changing to buprenorphine may precipitate withdrawal), those with a long-standing history of or multi-substance abuse, and those who have failed other treatment programs.
Prenatal care
Screen for comorbid conditions such as sexually transmitted infections, other medications or substance use, social conditions, and mental health disorders.
Perform ultrasonography serially to monitor fetal growth because of the increased risk of fetal growth restriction.
Consult with anesthesiology for pain control recommendations for labor and delivery and with neonatalogy/pediatrics for NAS counseling.
Intrapartum/postpartum care
Recognize heightened pain. Women with opioid use disorder have increased sensitivity to painful stimuli.
Continue the maintenance dose of methadone or buprenorphine throughout hospitalization, with short-acting opioids added for a brief period for postoperative pain.
Prioritize regional anesthesia for pain control in labor or for cesarean delivery.
Consider alternative therapies such as regional blocks, nonopioid medications (nonsteroidal anti-inflammatory drugs, acetaminophen), or relaxation/mindfulness training.
Avoid mixed antagonist and agonist narcotics (butorphanol, nalbuphine, pentazocine) as they may cause acute withdrawal.
Encourage breastfeeding to decrease the severity of NAS and maternal stress and increase maternal-child bonding and maternal confidence.
Offer contraceptive counseling and services immediately postpartum in the hospital, with strong consideration for long-acting reversible contraception.
Opioid prescribing practices
Opioids are prescribed in excess post–cesarean delivery. Several recent studies have demonstrated that most women are prescribed opioids post–cesarean delivery in excess of the amount they use (median 30–40 tablets prescribed, median 20 tablets used).1,2 The leftover opioid medication usually is not discarded and therefore is at risk for diversion or misuse. A small subset of patients will use all the opioids prescribed and feel as though they have not received enough medication.
Prescribe post–cesarean delivery opioids more appropriately by considering individual inpatient opioid requirements or a shared decision-making model.3
Prioritize acetaminophen and ibuprofen during breastfeeding. In a recent editorial in OBG Management, Robert L. Barbieri, MD, recommended that whenever possible, acetaminophen and ibuprofen should be the first-line treatment for breastfeeding women, and narcotics that are metabolized by CYP2D6 should be avoided to reduce the risk to the newborn.4
Universal screening for substance use should be performed in all pregnant women, and clinicians should offer medication-assisted treatment in conjunction with prenatal care and other supportive services as the standard therapy for opioid use disorder. More selective, patient-specific opioid prescribing practices should be applied in the obstetric population.
Read about new strategies for postpartum hemorrhage.
Postpartum hemorrhage: New definitions and new strategies for stemming the flow
ACOG Committee on Practice Bulletins—Obstetrics. ACOG practice bulletin No. 183: Postpartum hemorrhage. Obstet Gynecol. 2017;130(4):e168-e186.
From the very first sentence of the new ACOG practice bulletin, postpartum hemorrhage (PPH) is redefined as "cumulative blood loss greater than or equal to 1,000 mL or blood loss accompanied by signs or symptoms of hypovolemia within 24 hours after the birth process (includes intrapartum loss) regardless of route of delivery." Although this does not seem to be a huge change from the traditional teaching of a 500-mL blood loss at vaginal delivery and a 1,000-mL loss at cesarean delivery, it reflects a shift in focus from simply responding to a certain amount of bleeding to using a multidisciplinary action plan for treating this leading cause of maternal mortality worldwide.
Focus on developing a PPH action plan
As part of the shift toward a multidisciplinary action plan for PPH, all obstetric team members should be aware of the following:
- For most postpartum women, by the time they begin to show signs of hemodynamic compromise, the amount of blood loss approaches 25% of their total blood volume (1,500 mL). Lactic acidosis, systemic inflammation, and a consumptive coagulopathy result.
- Risk stratification prior to delivery, recognition and identification of the source of bleeding, and aggressive early resuscitation to prevent hypovolemia are paramount. Experience gleaned from trauma massive transfusion protocols suggests that judicious transfusion of packed red blood cells, fresh frozen plasma, and platelets in a 1:1:1 ratio is appropriate for obstetric patients. Additionally, patients with low fibrinogen levels should be treated with cryoprecipitate.
- The use of fixed transfusion ratios and standardized protocols for recognition and management of PPH has been demonstrated to increase earlier intervention and resolution of hemorrhage at an earlier stage, although the maternal outcomes results have been mixed.
- Multidisciplinary team drills and simulation exercises also should be considered to help solidify training of an institution's teams responsible for PPH response.
Novel management option: Tranexamic acid
In addition to these strategies, there is a new recommendation for managing refractory PPH: tranexamic acid, which works by binding to lysine receptors on plasminogen and plasmin, inhibiting plasmin-mediated fibrin degradation.5 Previously, tranexamic acid was known to be effective in trauma, heart surgery, and in patients with thrombophilias. Pacheco and colleagues recently demonstrated reduced mortality from obstetric bleeding if tranexamic acid was given within 3 hours of delivery, without increased thrombotic complications.5 ACOG recommends its use if initial medical therapy fails, while the World Health Organization strongly recommends that tranexamic acid be part of a standard PPH package for all cases of PPH (TABLE).6
Postpartum hemorrhage requires early, aggressive, and multidisciplinary coordination to ensure that 1) patients at risk for hemorrhage are identified for preventive measures; 2) existing hemorrhage is recognized and quickly treated, first with noninvasive methods and then with more definitive surgical treatments; and 3) blood product replacement follows an evidence-based standardized protocol. Tranexamic acid is recommended as an adjunct treatment for PPH (of any cause) and should be used within 3 hours of delivery.
Read about new ACOG guidance on prepregnancy and prenatal screening.
Carrier screening—choose something
ACOG Committee on Genetics. Committee opinion No. 690: Carrier screening in the age of genomic medicine. Obstet Gynecol. 2017;129(3):e35-e40.
ACOG Committee on Genetics. Committee opinion No. 691: Carrier screening for genetic conditions. Obstet Gynecol. 2017;129(3):e41-e55.
Ideally, carrier screening should be offered prior to pregnancy to fully inform couples of their reproductive risks and options for pregnancy. If not performed in the preconception period, carrier screening should be offered to all pregnant women. If a patient chooses screening and screens positive for a particular disorder, her reproductive partner should then be offered screening so that the risk of having an affected child can be determined.
New ACOG guidance on prepregnancy and prenatal screening
Carrier screening recommendations have evolved as the technology available has expanded. All 3 of the following strategies now are considered "acceptable" according to 2 recently published ACOG committee opinions.
Traditional ethnic-specific carrier screening, previously ACOG's sole recommendation, involves offering specific genetic screening to patients from populations with a high prevalence for certain conditions. One such example is Tay-Sachs disease screening in Ashkenazi Jewish patients.
Panethnic screening, which takes into account mixed or uncertain backgrounds, involves screening for a certain panel of disorders and is available to all patients regardless of their background (for example, cystic fibrosis screening offered to all pregnant patients).
Expanded carrier screening is when a large number of disorders can be screened for simultaneously for a lower cost than previous testing strategies. Expanded carrier screening panels vary in number and which conditions are tested by the laboratory. An ideal expanded carrier screening panel has been debated in the literature but not agreed on.7
ObGyns and practices therefore are encouraged to develop a standard counseling and screening protocol to offer to all their patients while being flexible to make available any patient-requested screening that is outside their protocol. Pretest and posttest counseling, including a thorough family history, is essential (as with any genetic testing) and should include residual risk after testing, potential need for specific familial mutation testing instead of general carrier screening, and issues with consanguinity.
Three essential screens
Regardless of the screening strategy chosen from the above options, 3 screening tests should be offered to all pregnant women or couples considering pregnancy (either individually or in the context of an expanded screening panel):
- Cystic fibrosis. At the least, a panel of the 23 most common mutations should be used. More expanded panels, which include hundreds of mutations, increase detection in non-Caucasian populations and for milder forms of the disease or infertility-related mutations.
- Hemoglobinopathies (sickle cell, α- and β-thalassemia). Complete blood count and red blood indices are recommended for all, with hemoglobin electrophoresis recommended for patients of African, Middle Eastern, Mediterranean, or West Indian descent or if mean corpuscular volume is low.
- Spinal muscular atrophy (SMA). The most recent addition to ACOG's recommendations for general carrier screening due to the relatively high carrier frequency (1-in-40 to 1-in-60) and the severity of the disease, SMA causes degeneration of the spinal cord neurons, skeletal muscular atrophy, and overall weakness. Screening is via polymerase chain reaction for SMN1 copy number: 2 copies are normal, and 1 copy indicates a carrier of the SMN1 deletion. About 3% to 4% of patients will screen negative but still will be "carriers" due to having 2 copies of the SMN1 gene on 1 chromosome and no copies on the other chromosome.
All pregnant patients or patients considering pregnancy should be offered carrier screening as standard reproductive care, including screening for cystic fibrosis, hemoglobinopathies, and spinal muscular atrophy. Ethnic, panethnic, or expanded carrier screening (and patient-requested specific screening) all are acceptable options, and a standard screening and counseling protocol should be determined by the ObGyn or practice.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130(1):29–35.
- Osmundson SS, Schornack LA, Grasch JL, Zuckerwise LC, Young JL, Richardson MD. Postdischarge opioid use after cesarean delivery. Obstet Gynecol. 2017;130(1):36–41.
- Prabhu M, McQuaid-Hanson E, Hopp S, et al. A shared decision-making intervention to guide opioid prescribing after cesarean delivery. Obstet Gynecol. 2017;130(1):42–46.
- Barbieri RL. Stop using codeine, oxycodone, hydrocodone, tramadol, and aspirin in women who are breastfeeding. OBG Manag. 2017;29(10):8–12.
- Pacheco LD, Hankins GD, Saad AF, Costantine MM, Chiossi G, Saade GR. Tranexamic acid for the management of obstetric hemorrhage. Obstet Gynecol. 2017;130(4);765–769.
- WHO recommendation on tranexamic acid for the treatment of postpartum haemorrhage. Geneva, Switzerland: World Health Organization; 2017.
- Stevens B, Krstic N, Jones M, Murphy L, Hoskovec J. Finding middle ground in constructing a clinically useful expanded carrier screening panel. Obstet Gynecol. 2017;130(2):279–284.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130(1):29–35.
- Osmundson SS, Schornack LA, Grasch JL, Zuckerwise LC, Young JL, Richardson MD. Postdischarge opioid use after cesarean delivery. Obstet Gynecol. 2017;130(1):36–41.
- Prabhu M, McQuaid-Hanson E, Hopp S, et al. A shared decision-making intervention to guide opioid prescribing after cesarean delivery. Obstet Gynecol. 2017;130(1):42–46.
- Barbieri RL. Stop using codeine, oxycodone, hydrocodone, tramadol, and aspirin in women who are breastfeeding. OBG Manag. 2017;29(10):8–12.
- Pacheco LD, Hankins GD, Saad AF, Costantine MM, Chiossi G, Saade GR. Tranexamic acid for the management of obstetric hemorrhage. Obstet Gynecol. 2017;130(4);765–769.
- WHO recommendation on tranexamic acid for the treatment of postpartum haemorrhage. Geneva, Switzerland: World Health Organization; 2017.
- Stevens B, Krstic N, Jones M, Murphy L, Hoskovec J. Finding middle ground in constructing a clinically useful expanded carrier screening panel. Obstet Gynecol. 2017;130(2):279–284.
8 common questions about newborn circumcision
In the United States, circumcision is the fourth most common surgical procedure—behind cataract removal, cesarean delivery, and joint replacement.1 This operation, which dates to ancient times, is chosen for medical, personal, or religious reasons. It is performed on 77% of males born in the United States and on 42% of those born elsewhere who are living in this country.2 Whether it is performed depends not only on the parents’ race, ethnic background, and religion but also on region: US circumcision rates range from 74% in the Midwest to 30% in the West, and in between are the Northeast (67%) and the South (61%).3
Circumcision is not without controversy. Some claim that it is unnecessary cosmetic surgery, that it is genital mutilation, that the patient cannot choose it or object to it, or that it decreases sexual satisfaction.
In this article, I review 8 common questions about circumcision and provide data-based answers to them.
1. Should a newborn be circumcised?
For many years, the medical benefits of circumcision were scientifically ambiguous. With no clear answers, some thought that parents should base their decision for or against circumcision not on any potential medical benefit but rather on their family or religious tradition, or on a social standard, that is, what the majority of families in their community do.
Over the past 20 years, a growing body of evidence has demonstrated real medical benefits of circumcision. In 2012, the American Academy of Pediatrics (AAP), which previously had been neutral on the subject, issued a task force report concluding that the health benefits of circumcision outweigh its risks and justify access to the procedure.3,4 However, the report stopped short of recommending circumcision.
Opponents have expressed several concerns about circumcision. First, they say, it is painful and unnecessary, and performing it when life has just begun takes the decision away from the adult-to-be, who may want to be uncircumcised as an adult but will have no recourse. Second, they say circumcision will diminish the adult’s sexual pleasure. However, there is no proof this occurs, and it is unclear how the claim could be adequately verified.5
Health benefits of circumcision3
- Prevention of phimosis and balanoposthitis (inflammation of glans and foreskin), penile retraction disorders, and penile cancer
- Fewer infant urinary tract infections
- Decreased spread of human papillomavirus–related disease, including cervical cancer and its precursors, to sexual partners
- Lower risk of acquiring, harboring, and spreading human immunodeficiency virus infection, herpes virus infection, and other sexually transmitted diseases
- Easier genital hygiene
- No need for circumcision later in life, when the procedure is more involved
2. What is the best analgesia for circumcision?
Although in decades past circumcision was often performed without any analgesia, in the United States analgesia is now standard of care. The AAP Task Force on Circumcision formalized this standard in a 2012 policy statement.4 For newborn circumcision, analgesia can be given in the form of analgesic cream, penile ring block, or dorsal nerve block.
Analgesic EMLA cream (a mixture of local anesthetics such as lidocaine 2.5%/prilocaine 2.5%) is easy to use but is minimally effective in relieving circumcision pain,6 although some investigators have reported it is efficacious compared with placebo.7 When used, the analgesic cream is applied 30 to 60 minutes before circumcision.
Both penile ring block and dorsal nerve block with 1% lidocaine are easy to administer and are very effective.8,9 They are best used with buffered lidocaine, which partially relieves the burning that occurs with injection. With both methods, the smaller the needle used (preferably 30 gauge), the better.
These 2 block methods have different injection sites. For the ring block, small amounts of lidocaine (1 to 1.5 mL) are given in a series of injections around the entire circumference of the base of the penis. The dorsal block targets the 2 dorsal nerves located at 10 o’clock and 2 o’clock at the base of the penis. Epinephrine, given its vasoconstrictive properties and the potential for necrosis, should never be used with local analgesia for penile infiltration.
Analgesia can be supplemented with comfort measures, such as a pacifier, sugar water, gentle rubbing on the forehead, and soothing speech.10
Related article:
Circumcision impedes viral disease. Will opposition fade?
3. What conditions are required for safe circumcision?
As circumcision is not medically required and need not occur in the days immediately after birth, it should be performed only when conditions are optimal:
- A pediatrician or other practitioner must first examine the newborn.
- The newborn must be full-term, healthy, and stable.
- The best time to circumcise a baby born prematurely is right before discharge from the intensive care nursery.
- The penis must be of normal size and without anatomical defect—no micropenis, hypospadias, or penoscrotal webbing.
- The lower abdominal fat pad must not be so large that it will cause the shaft’s skin to cover the exposed penile head.
- If there is a family history of a bleeding disorder, the newborn must be evaluated for the disorder before the circumcision.
- The newborn must have received his vitamin K shot.
4. What is the best circumcision method?
Circumcision can be performed with the Gomco circumcision clamp, the Mogen circumcision clamp, or the PlastiBell circumcision device. Each device works well, provides excellent results, and has its pluses and minuses. Practitioners should use the device with which they are most familiar and comfortable, which likely will be the device they used in training.
In the United States, the Gomco clamp is perhaps the most commonly used device. It provides good cosmetic results, and its metal “bell” protects the entire head of the penis. Of the 3 methods, however, it is the most difficult—the partially cut foreskin must be threaded between the bell and the clamp frame before the clamp is tightened. In many cases, too, there is bleeding at the penile frenulum.
The Mogen clamp, another commonly used device, also is used in traditional Jewish circumcisions. Of the 3 methods, it is the quickest, produces the best hemostasis, and is associated with the least discomfort.10 To those unfamiliar with the method, there may seem to be a potential for amputation of the head of the penis, but actually there virtually is no risk, as an indentation on the penile side of the clamp protects the penile head.
The PlastiBell device is very easy to use but must stay on until the foreskin becomes necrotic and the bell and foreskin fall off on their own—a process that takes 7 to 10 days. Many parents dislike this method because its final result is not immediate and they have to contend with a medical implement during their newborn’s first week home.
Electrocautery is not recommended. Some clinicians, especially urologists, use electrocautery as the cutting mechanism for circumcision. A review of the literature, however, reveals that electrocautery has not been studied head-to-head against traditional techniques, and that various significant complications—transected penile head, severe burns, meatal stenosis—have been reported.11,12 It is certainly not a mainstream procedure for neonatal circumcision.
Evaluate penile anatomy for abnormalities
Before performing any circumcision, the head of the penis should be examined to rule out hypospadias or other penile abnormalities. This is because the foreskin is utilized in certain penile repair procedures. The pediatrician should perform an initial examination of the penis at the formal newborn physical within 24 hours of delivery. The clinician performing the circumcision should re-examine the penis just before the procedure is begun—by pushing back the foreskin as much as possible—as well as during the procedure, once the foreskin is lifted off the penile head but before the foreskin is excised.
Read about how to ensure the best outcome of circumcision.
5. When is the best time to perform a circumcision?
The medical literature provides no firm answer to this question. The younger the baby, the easier it is to perform a circumcision as a simple procedure with local anesthesia. The older the baby, the larger the penis and the more aware the baby will be of his surroundings. Both these factors will make the procedure more difficult.
Most clinicians would be reluctant to perform a circumcision in the office or clinic after the baby is 6 to 8 weeks old. If a family desires their son to be circumcised after that time—or a medical condition precludes earlier circumcision—the procedure is best performed by a pediatric urologist in the operating room.
Related article:
Circumcision accident: $1.3M verdict
6. What are the potential complications of circumcision?
The rate of circumcision complications is very low: 0.2%.13 That being said, the 3 most common types of complications are postoperative bleeding, infection, and damage to the penis.
Far and away the most common complication is postoperative bleeding , usually at the frenulum of the head of the penis (the 6 o’clock position). In most cases, the bleeding is light to moderate. It is controlled with direct pressure applied for several minutes, the use of processed gelatin (Gelfoam) or cellulose (Surgicel), sparing use of silver nitrate, or placement of a polyglycolic acid (Vicryl) 5-0 suture.
Infection, an unusual occurrence, is seen within 24 to 72 hours after circumcision. It is marked by swelling, redness, and a foul-smelling mucus discharge. This discharge must be differentiated from dried fibrin, which is commonly seen on the head of the penis in the days after circumcision but has no odor or association with erythema, fever, or infant fussiness. True infection should be treated, in collaboration with the child’s pediatrician, with a staphylococcal-sensitive penicillin (such as dicloxacillin).
More serious is damage to the penis, which ranges from accidental dilation of the meatus to partial amputation of the penile glans. Any such injury should immediately prompt a consultation with a pediatric urologist.
More of a nuisance than a complication is the sliding of the penile shaft’s skin up and over the glans. This is a relatively frequent occurrence after normal, successful circumcisions. Parents of an affected newborn should be instructed to gently slide the skin back until the head of the penis is completely exposed again. After several days, the skin will adhere to its proper position on the shaft.
- Just before the procedure, have a face-to-face discussion with the parents. Confirm that they want the circumcision done, explain exactly what it entails, and let them know they will receive complete aftercare instructions.
- Make sure one of the parents signs the consent form.
- Circumcise the right baby! Check the identification bracelet and confirm that the newborn’s hospital and chart numbers match.
- Prevent excessive hip movement by securing the baby's legs. The usual solution is a specially designed plastic restraint board with Velcro straps for the legs.
- Examine the infant’s penile anatomy prior to the procedure to make certain it is normal.
- For pain relief, administer enough analgesia, as either dorsal nerve block or penile ring block (the best methods). Before injection, draw the plunger of the syringe back to make certain that the needle is not in a blood vessel.
- During the procedure, make sure the entire membranous layer of foreskin covering the head of the penis is separated from the glans.
- Watch the penis for several minutes after the circumcision to make sure there is no bleeding.
7. What is a Jewish ritual circumcision?
For their newborn’s circumcision, Jewish parents may choose a bris ceremony, formally called a brit milah, in fulfillment of religious tradition. The ceremony involves a brief religious service, circumcision with the traditional Mogen clamp, a special blessing, and an official religious naming rite. The bris traditionally is performed by a mohel, a rabbi or other religious official trained in circumcision. Many parents have the bris done by a mohel who is a medical doctor. In the United States, the availability of both types of mohels varies.
8. Who should perform circumcisions—obstetricians or pediatricians?
The answer to this question depends on where you practice. In some communities or hospitals, the obstetrician performs newborn circumcision, while in other places the pediatrician does. In addition, depending on local circumstances or the specific population involved, circumcisions may be performed by a pediatric urologist, nurse practitioner, or even out of hospital by a trained religiously affiliated practitioner.
Obstetricians began doing circumcisions for 2 reasons. First, obstetricians are surgically trained whereas pediatricians are not. It was therefore thought to be more appropriate for obstetricians to do this minor surgical procedure. Second, circumcisions used to be done right in the delivery room shortly after delivery. It was thought that the crying induced by performing the circumcision helped clear the baby’s lungs and invigorated sluggish babies. Now, however, in-hospital circumcisions are usually done in the days following delivery, after the baby has had the opportunity to undergo his first physical examination to make sure that all is well and that the penile anatomy is normal.
Clinician experience, proper protocol contribute to a safe procedure
In the United States, a large percentage of male infants are circumcised. Although circumcision has known medical benefits, the procedure generally is performed for family, religious, or cultural reasons. Circumcision is a safe and straightforward procedure but has its risks and potential complications. As with most surgeries, the best outcomes are achieved by practitioners who are well trained, who perform the procedure under supervision until their experience is sufficient, and who follow correct protocol during the entire operation.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Dallas ME. The 10 most common surgeries in the US. Healthgrades website. https://www.healthgrades.com/explore/the-10-most-common-surgeries-in-the-us. Reviewed August 15, 2017. Accessed October 2, 2017.
- Laumann EO, Masi CM, Zuckerman EW. Circumcision in the United States: prevalence, prophylactic effects, and sexual practice. JAMA. 1997;277(13):1052–1057.
- American Academy of Pediatrics Task Force on Circumcision. Male circumcision. Pediatrics. 2012;130(3):e756–e785.
- American Academy of Pediatrics Task Force on Circumcision. Circumcision policy statement. Pediatrics. 2012;130(3):585–586.
- Morris BJ, Krieger JN. Does male circumcision affect sexual function, sensitivity, or satisfaction? A systematic review. J Sex Med. 2013;10(11):2644–2657.
- Howard FM, Howard CR, Fortune K, Generelli P, Zolnoun D, tenHoopen C. A randomized, placebo-controlled comparison of EMLA and dorsal penile nerve block for pain relief during neonatal circumcision. Prim Care Update Ob Gyns. 1998;5(4):196.
- Taddio A, Stevens B, Craig K, et al. Efficacy and safety of lidocaine-prilocaine cream for pain during circumcision. N Engl J Med. 1997;336(17):1197–1201.
- Lander J, Brady-Fryer B, Metcalfe JB, Nazarali S, Muttitt S. Comparison of ring block, dorsal penile nerve block, and topical anesthesia for neonatal circumcision: a randomized controlled trial. JAMA. 1997;278(24):2157–2162.
- Hardwick-Smith S, Mastrobattista JM, Wallace PA, Ritchey ML. Ring block for neonatal circumcision. Obstet Gynecol. 1998;91(6):930–934.
- Kaufman GE, Cimo S, Miller LW, Blass EM. An evaluation of the effects of sucrose on neonatal pain with 2 commonly used circumcision methods. Am J Obstet Gynecol. 2002;186(3):564–568.
- Tucker SC, Cerqueiro J, Sterne GD, Bracka A. Circumcision: a refined technique and 5 year review. Ann R Coll Surg Engl. 2001;83(2):121–125.
- Fraser ID, Tjoe J. Circumcision using bipolar scissors can be a safe and simple operation. Ann R Coll Surg Engl. 2000;82(3):190–191.
- Wiswell TE, Geschke DW. Risks from circumcision during the first month of life compared with those for uncircumcised boys. Pediatrics. 1989;83(6):1011–1015.
In the United States, circumcision is the fourth most common surgical procedure—behind cataract removal, cesarean delivery, and joint replacement.1 This operation, which dates to ancient times, is chosen for medical, personal, or religious reasons. It is performed on 77% of males born in the United States and on 42% of those born elsewhere who are living in this country.2 Whether it is performed depends not only on the parents’ race, ethnic background, and religion but also on region: US circumcision rates range from 74% in the Midwest to 30% in the West, and in between are the Northeast (67%) and the South (61%).3
Circumcision is not without controversy. Some claim that it is unnecessary cosmetic surgery, that it is genital mutilation, that the patient cannot choose it or object to it, or that it decreases sexual satisfaction.
In this article, I review 8 common questions about circumcision and provide data-based answers to them.
1. Should a newborn be circumcised?
For many years, the medical benefits of circumcision were scientifically ambiguous. With no clear answers, some thought that parents should base their decision for or against circumcision not on any potential medical benefit but rather on their family or religious tradition, or on a social standard, that is, what the majority of families in their community do.
Over the past 20 years, a growing body of evidence has demonstrated real medical benefits of circumcision. In 2012, the American Academy of Pediatrics (AAP), which previously had been neutral on the subject, issued a task force report concluding that the health benefits of circumcision outweigh its risks and justify access to the procedure.3,4 However, the report stopped short of recommending circumcision.
Opponents have expressed several concerns about circumcision. First, they say, it is painful and unnecessary, and performing it when life has just begun takes the decision away from the adult-to-be, who may want to be uncircumcised as an adult but will have no recourse. Second, they say circumcision will diminish the adult’s sexual pleasure. However, there is no proof this occurs, and it is unclear how the claim could be adequately verified.5
Health benefits of circumcision3
- Prevention of phimosis and balanoposthitis (inflammation of glans and foreskin), penile retraction disorders, and penile cancer
- Fewer infant urinary tract infections
- Decreased spread of human papillomavirus–related disease, including cervical cancer and its precursors, to sexual partners
- Lower risk of acquiring, harboring, and spreading human immunodeficiency virus infection, herpes virus infection, and other sexually transmitted diseases
- Easier genital hygiene
- No need for circumcision later in life, when the procedure is more involved
2. What is the best analgesia for circumcision?
Although in decades past circumcision was often performed without any analgesia, in the United States analgesia is now standard of care. The AAP Task Force on Circumcision formalized this standard in a 2012 policy statement.4 For newborn circumcision, analgesia can be given in the form of analgesic cream, penile ring block, or dorsal nerve block.
Analgesic EMLA cream (a mixture of local anesthetics such as lidocaine 2.5%/prilocaine 2.5%) is easy to use but is minimally effective in relieving circumcision pain,6 although some investigators have reported it is efficacious compared with placebo.7 When used, the analgesic cream is applied 30 to 60 minutes before circumcision.
Both penile ring block and dorsal nerve block with 1% lidocaine are easy to administer and are very effective.8,9 They are best used with buffered lidocaine, which partially relieves the burning that occurs with injection. With both methods, the smaller the needle used (preferably 30 gauge), the better.
These 2 block methods have different injection sites. For the ring block, small amounts of lidocaine (1 to 1.5 mL) are given in a series of injections around the entire circumference of the base of the penis. The dorsal block targets the 2 dorsal nerves located at 10 o’clock and 2 o’clock at the base of the penis. Epinephrine, given its vasoconstrictive properties and the potential for necrosis, should never be used with local analgesia for penile infiltration.
Analgesia can be supplemented with comfort measures, such as a pacifier, sugar water, gentle rubbing on the forehead, and soothing speech.10
Related article:
Circumcision impedes viral disease. Will opposition fade?
3. What conditions are required for safe circumcision?
As circumcision is not medically required and need not occur in the days immediately after birth, it should be performed only when conditions are optimal:
- A pediatrician or other practitioner must first examine the newborn.
- The newborn must be full-term, healthy, and stable.
- The best time to circumcise a baby born prematurely is right before discharge from the intensive care nursery.
- The penis must be of normal size and without anatomical defect—no micropenis, hypospadias, or penoscrotal webbing.
- The lower abdominal fat pad must not be so large that it will cause the shaft’s skin to cover the exposed penile head.
- If there is a family history of a bleeding disorder, the newborn must be evaluated for the disorder before the circumcision.
- The newborn must have received his vitamin K shot.
4. What is the best circumcision method?
Circumcision can be performed with the Gomco circumcision clamp, the Mogen circumcision clamp, or the PlastiBell circumcision device. Each device works well, provides excellent results, and has its pluses and minuses. Practitioners should use the device with which they are most familiar and comfortable, which likely will be the device they used in training.
In the United States, the Gomco clamp is perhaps the most commonly used device. It provides good cosmetic results, and its metal “bell” protects the entire head of the penis. Of the 3 methods, however, it is the most difficult—the partially cut foreskin must be threaded between the bell and the clamp frame before the clamp is tightened. In many cases, too, there is bleeding at the penile frenulum.
The Mogen clamp, another commonly used device, also is used in traditional Jewish circumcisions. Of the 3 methods, it is the quickest, produces the best hemostasis, and is associated with the least discomfort.10 To those unfamiliar with the method, there may seem to be a potential for amputation of the head of the penis, but actually there virtually is no risk, as an indentation on the penile side of the clamp protects the penile head.
The PlastiBell device is very easy to use but must stay on until the foreskin becomes necrotic and the bell and foreskin fall off on their own—a process that takes 7 to 10 days. Many parents dislike this method because its final result is not immediate and they have to contend with a medical implement during their newborn’s first week home.
Electrocautery is not recommended. Some clinicians, especially urologists, use electrocautery as the cutting mechanism for circumcision. A review of the literature, however, reveals that electrocautery has not been studied head-to-head against traditional techniques, and that various significant complications—transected penile head, severe burns, meatal stenosis—have been reported.11,12 It is certainly not a mainstream procedure for neonatal circumcision.
Evaluate penile anatomy for abnormalities
Before performing any circumcision, the head of the penis should be examined to rule out hypospadias or other penile abnormalities. This is because the foreskin is utilized in certain penile repair procedures. The pediatrician should perform an initial examination of the penis at the formal newborn physical within 24 hours of delivery. The clinician performing the circumcision should re-examine the penis just before the procedure is begun—by pushing back the foreskin as much as possible—as well as during the procedure, once the foreskin is lifted off the penile head but before the foreskin is excised.
Read about how to ensure the best outcome of circumcision.
5. When is the best time to perform a circumcision?
The medical literature provides no firm answer to this question. The younger the baby, the easier it is to perform a circumcision as a simple procedure with local anesthesia. The older the baby, the larger the penis and the more aware the baby will be of his surroundings. Both these factors will make the procedure more difficult.
Most clinicians would be reluctant to perform a circumcision in the office or clinic after the baby is 6 to 8 weeks old. If a family desires their son to be circumcised after that time—or a medical condition precludes earlier circumcision—the procedure is best performed by a pediatric urologist in the operating room.
Related article:
Circumcision accident: $1.3M verdict
6. What are the potential complications of circumcision?
The rate of circumcision complications is very low: 0.2%.13 That being said, the 3 most common types of complications are postoperative bleeding, infection, and damage to the penis.
Far and away the most common complication is postoperative bleeding , usually at the frenulum of the head of the penis (the 6 o’clock position). In most cases, the bleeding is light to moderate. It is controlled with direct pressure applied for several minutes, the use of processed gelatin (Gelfoam) or cellulose (Surgicel), sparing use of silver nitrate, or placement of a polyglycolic acid (Vicryl) 5-0 suture.
Infection, an unusual occurrence, is seen within 24 to 72 hours after circumcision. It is marked by swelling, redness, and a foul-smelling mucus discharge. This discharge must be differentiated from dried fibrin, which is commonly seen on the head of the penis in the days after circumcision but has no odor or association with erythema, fever, or infant fussiness. True infection should be treated, in collaboration with the child’s pediatrician, with a staphylococcal-sensitive penicillin (such as dicloxacillin).
More serious is damage to the penis, which ranges from accidental dilation of the meatus to partial amputation of the penile glans. Any such injury should immediately prompt a consultation with a pediatric urologist.
More of a nuisance than a complication is the sliding of the penile shaft’s skin up and over the glans. This is a relatively frequent occurrence after normal, successful circumcisions. Parents of an affected newborn should be instructed to gently slide the skin back until the head of the penis is completely exposed again. After several days, the skin will adhere to its proper position on the shaft.
- Just before the procedure, have a face-to-face discussion with the parents. Confirm that they want the circumcision done, explain exactly what it entails, and let them know they will receive complete aftercare instructions.
- Make sure one of the parents signs the consent form.
- Circumcise the right baby! Check the identification bracelet and confirm that the newborn’s hospital and chart numbers match.
- Prevent excessive hip movement by securing the baby's legs. The usual solution is a specially designed plastic restraint board with Velcro straps for the legs.
- Examine the infant’s penile anatomy prior to the procedure to make certain it is normal.
- For pain relief, administer enough analgesia, as either dorsal nerve block or penile ring block (the best methods). Before injection, draw the plunger of the syringe back to make certain that the needle is not in a blood vessel.
- During the procedure, make sure the entire membranous layer of foreskin covering the head of the penis is separated from the glans.
- Watch the penis for several minutes after the circumcision to make sure there is no bleeding.
7. What is a Jewish ritual circumcision?
For their newborn’s circumcision, Jewish parents may choose a bris ceremony, formally called a brit milah, in fulfillment of religious tradition. The ceremony involves a brief religious service, circumcision with the traditional Mogen clamp, a special blessing, and an official religious naming rite. The bris traditionally is performed by a mohel, a rabbi or other religious official trained in circumcision. Many parents have the bris done by a mohel who is a medical doctor. In the United States, the availability of both types of mohels varies.
8. Who should perform circumcisions—obstetricians or pediatricians?
The answer to this question depends on where you practice. In some communities or hospitals, the obstetrician performs newborn circumcision, while in other places the pediatrician does. In addition, depending on local circumstances or the specific population involved, circumcisions may be performed by a pediatric urologist, nurse practitioner, or even out of hospital by a trained religiously affiliated practitioner.
Obstetricians began doing circumcisions for 2 reasons. First, obstetricians are surgically trained whereas pediatricians are not. It was therefore thought to be more appropriate for obstetricians to do this minor surgical procedure. Second, circumcisions used to be done right in the delivery room shortly after delivery. It was thought that the crying induced by performing the circumcision helped clear the baby’s lungs and invigorated sluggish babies. Now, however, in-hospital circumcisions are usually done in the days following delivery, after the baby has had the opportunity to undergo his first physical examination to make sure that all is well and that the penile anatomy is normal.
Clinician experience, proper protocol contribute to a safe procedure
In the United States, a large percentage of male infants are circumcised. Although circumcision has known medical benefits, the procedure generally is performed for family, religious, or cultural reasons. Circumcision is a safe and straightforward procedure but has its risks and potential complications. As with most surgeries, the best outcomes are achieved by practitioners who are well trained, who perform the procedure under supervision until their experience is sufficient, and who follow correct protocol during the entire operation.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In the United States, circumcision is the fourth most common surgical procedure—behind cataract removal, cesarean delivery, and joint replacement.1 This operation, which dates to ancient times, is chosen for medical, personal, or religious reasons. It is performed on 77% of males born in the United States and on 42% of those born elsewhere who are living in this country.2 Whether it is performed depends not only on the parents’ race, ethnic background, and religion but also on region: US circumcision rates range from 74% in the Midwest to 30% in the West, and in between are the Northeast (67%) and the South (61%).3
Circumcision is not without controversy. Some claim that it is unnecessary cosmetic surgery, that it is genital mutilation, that the patient cannot choose it or object to it, or that it decreases sexual satisfaction.
In this article, I review 8 common questions about circumcision and provide data-based answers to them.
1. Should a newborn be circumcised?
For many years, the medical benefits of circumcision were scientifically ambiguous. With no clear answers, some thought that parents should base their decision for or against circumcision not on any potential medical benefit but rather on their family or religious tradition, or on a social standard, that is, what the majority of families in their community do.
Over the past 20 years, a growing body of evidence has demonstrated real medical benefits of circumcision. In 2012, the American Academy of Pediatrics (AAP), which previously had been neutral on the subject, issued a task force report concluding that the health benefits of circumcision outweigh its risks and justify access to the procedure.3,4 However, the report stopped short of recommending circumcision.
Opponents have expressed several concerns about circumcision. First, they say, it is painful and unnecessary, and performing it when life has just begun takes the decision away from the adult-to-be, who may want to be uncircumcised as an adult but will have no recourse. Second, they say circumcision will diminish the adult’s sexual pleasure. However, there is no proof this occurs, and it is unclear how the claim could be adequately verified.5
Health benefits of circumcision3
- Prevention of phimosis and balanoposthitis (inflammation of glans and foreskin), penile retraction disorders, and penile cancer
- Fewer infant urinary tract infections
- Decreased spread of human papillomavirus–related disease, including cervical cancer and its precursors, to sexual partners
- Lower risk of acquiring, harboring, and spreading human immunodeficiency virus infection, herpes virus infection, and other sexually transmitted diseases
- Easier genital hygiene
- No need for circumcision later in life, when the procedure is more involved
2. What is the best analgesia for circumcision?
Although in decades past circumcision was often performed without any analgesia, in the United States analgesia is now standard of care. The AAP Task Force on Circumcision formalized this standard in a 2012 policy statement.4 For newborn circumcision, analgesia can be given in the form of analgesic cream, penile ring block, or dorsal nerve block.
Analgesic EMLA cream (a mixture of local anesthetics such as lidocaine 2.5%/prilocaine 2.5%) is easy to use but is minimally effective in relieving circumcision pain,6 although some investigators have reported it is efficacious compared with placebo.7 When used, the analgesic cream is applied 30 to 60 minutes before circumcision.
Both penile ring block and dorsal nerve block with 1% lidocaine are easy to administer and are very effective.8,9 They are best used with buffered lidocaine, which partially relieves the burning that occurs with injection. With both methods, the smaller the needle used (preferably 30 gauge), the better.
These 2 block methods have different injection sites. For the ring block, small amounts of lidocaine (1 to 1.5 mL) are given in a series of injections around the entire circumference of the base of the penis. The dorsal block targets the 2 dorsal nerves located at 10 o’clock and 2 o’clock at the base of the penis. Epinephrine, given its vasoconstrictive properties and the potential for necrosis, should never be used with local analgesia for penile infiltration.
Analgesia can be supplemented with comfort measures, such as a pacifier, sugar water, gentle rubbing on the forehead, and soothing speech.10
Related article:
Circumcision impedes viral disease. Will opposition fade?
3. What conditions are required for safe circumcision?
As circumcision is not medically required and need not occur in the days immediately after birth, it should be performed only when conditions are optimal:
- A pediatrician or other practitioner must first examine the newborn.
- The newborn must be full-term, healthy, and stable.
- The best time to circumcise a baby born prematurely is right before discharge from the intensive care nursery.
- The penis must be of normal size and without anatomical defect—no micropenis, hypospadias, or penoscrotal webbing.
- The lower abdominal fat pad must not be so large that it will cause the shaft’s skin to cover the exposed penile head.
- If there is a family history of a bleeding disorder, the newborn must be evaluated for the disorder before the circumcision.
- The newborn must have received his vitamin K shot.
4. What is the best circumcision method?
Circumcision can be performed with the Gomco circumcision clamp, the Mogen circumcision clamp, or the PlastiBell circumcision device. Each device works well, provides excellent results, and has its pluses and minuses. Practitioners should use the device with which they are most familiar and comfortable, which likely will be the device they used in training.
In the United States, the Gomco clamp is perhaps the most commonly used device. It provides good cosmetic results, and its metal “bell” protects the entire head of the penis. Of the 3 methods, however, it is the most difficult—the partially cut foreskin must be threaded between the bell and the clamp frame before the clamp is tightened. In many cases, too, there is bleeding at the penile frenulum.
The Mogen clamp, another commonly used device, also is used in traditional Jewish circumcisions. Of the 3 methods, it is the quickest, produces the best hemostasis, and is associated with the least discomfort.10 To those unfamiliar with the method, there may seem to be a potential for amputation of the head of the penis, but actually there virtually is no risk, as an indentation on the penile side of the clamp protects the penile head.
The PlastiBell device is very easy to use but must stay on until the foreskin becomes necrotic and the bell and foreskin fall off on their own—a process that takes 7 to 10 days. Many parents dislike this method because its final result is not immediate and they have to contend with a medical implement during their newborn’s first week home.
Electrocautery is not recommended. Some clinicians, especially urologists, use electrocautery as the cutting mechanism for circumcision. A review of the literature, however, reveals that electrocautery has not been studied head-to-head against traditional techniques, and that various significant complications—transected penile head, severe burns, meatal stenosis—have been reported.11,12 It is certainly not a mainstream procedure for neonatal circumcision.
Evaluate penile anatomy for abnormalities
Before performing any circumcision, the head of the penis should be examined to rule out hypospadias or other penile abnormalities. This is because the foreskin is utilized in certain penile repair procedures. The pediatrician should perform an initial examination of the penis at the formal newborn physical within 24 hours of delivery. The clinician performing the circumcision should re-examine the penis just before the procedure is begun—by pushing back the foreskin as much as possible—as well as during the procedure, once the foreskin is lifted off the penile head but before the foreskin is excised.
Read about how to ensure the best outcome of circumcision.
5. When is the best time to perform a circumcision?
The medical literature provides no firm answer to this question. The younger the baby, the easier it is to perform a circumcision as a simple procedure with local anesthesia. The older the baby, the larger the penis and the more aware the baby will be of his surroundings. Both these factors will make the procedure more difficult.
Most clinicians would be reluctant to perform a circumcision in the office or clinic after the baby is 6 to 8 weeks old. If a family desires their son to be circumcised after that time—or a medical condition precludes earlier circumcision—the procedure is best performed by a pediatric urologist in the operating room.
Related article:
Circumcision accident: $1.3M verdict
6. What are the potential complications of circumcision?
The rate of circumcision complications is very low: 0.2%.13 That being said, the 3 most common types of complications are postoperative bleeding, infection, and damage to the penis.
Far and away the most common complication is postoperative bleeding , usually at the frenulum of the head of the penis (the 6 o’clock position). In most cases, the bleeding is light to moderate. It is controlled with direct pressure applied for several minutes, the use of processed gelatin (Gelfoam) or cellulose (Surgicel), sparing use of silver nitrate, or placement of a polyglycolic acid (Vicryl) 5-0 suture.
Infection, an unusual occurrence, is seen within 24 to 72 hours after circumcision. It is marked by swelling, redness, and a foul-smelling mucus discharge. This discharge must be differentiated from dried fibrin, which is commonly seen on the head of the penis in the days after circumcision but has no odor or association with erythema, fever, or infant fussiness. True infection should be treated, in collaboration with the child’s pediatrician, with a staphylococcal-sensitive penicillin (such as dicloxacillin).
More serious is damage to the penis, which ranges from accidental dilation of the meatus to partial amputation of the penile glans. Any such injury should immediately prompt a consultation with a pediatric urologist.
More of a nuisance than a complication is the sliding of the penile shaft’s skin up and over the glans. This is a relatively frequent occurrence after normal, successful circumcisions. Parents of an affected newborn should be instructed to gently slide the skin back until the head of the penis is completely exposed again. After several days, the skin will adhere to its proper position on the shaft.
- Just before the procedure, have a face-to-face discussion with the parents. Confirm that they want the circumcision done, explain exactly what it entails, and let them know they will receive complete aftercare instructions.
- Make sure one of the parents signs the consent form.
- Circumcise the right baby! Check the identification bracelet and confirm that the newborn’s hospital and chart numbers match.
- Prevent excessive hip movement by securing the baby's legs. The usual solution is a specially designed plastic restraint board with Velcro straps for the legs.
- Examine the infant’s penile anatomy prior to the procedure to make certain it is normal.
- For pain relief, administer enough analgesia, as either dorsal nerve block or penile ring block (the best methods). Before injection, draw the plunger of the syringe back to make certain that the needle is not in a blood vessel.
- During the procedure, make sure the entire membranous layer of foreskin covering the head of the penis is separated from the glans.
- Watch the penis for several minutes after the circumcision to make sure there is no bleeding.
7. What is a Jewish ritual circumcision?
For their newborn’s circumcision, Jewish parents may choose a bris ceremony, formally called a brit milah, in fulfillment of religious tradition. The ceremony involves a brief religious service, circumcision with the traditional Mogen clamp, a special blessing, and an official religious naming rite. The bris traditionally is performed by a mohel, a rabbi or other religious official trained in circumcision. Many parents have the bris done by a mohel who is a medical doctor. In the United States, the availability of both types of mohels varies.
8. Who should perform circumcisions—obstetricians or pediatricians?
The answer to this question depends on where you practice. In some communities or hospitals, the obstetrician performs newborn circumcision, while in other places the pediatrician does. In addition, depending on local circumstances or the specific population involved, circumcisions may be performed by a pediatric urologist, nurse practitioner, or even out of hospital by a trained religiously affiliated practitioner.
Obstetricians began doing circumcisions for 2 reasons. First, obstetricians are surgically trained whereas pediatricians are not. It was therefore thought to be more appropriate for obstetricians to do this minor surgical procedure. Second, circumcisions used to be done right in the delivery room shortly after delivery. It was thought that the crying induced by performing the circumcision helped clear the baby’s lungs and invigorated sluggish babies. Now, however, in-hospital circumcisions are usually done in the days following delivery, after the baby has had the opportunity to undergo his first physical examination to make sure that all is well and that the penile anatomy is normal.
Clinician experience, proper protocol contribute to a safe procedure
In the United States, a large percentage of male infants are circumcised. Although circumcision has known medical benefits, the procedure generally is performed for family, religious, or cultural reasons. Circumcision is a safe and straightforward procedure but has its risks and potential complications. As with most surgeries, the best outcomes are achieved by practitioners who are well trained, who perform the procedure under supervision until their experience is sufficient, and who follow correct protocol during the entire operation.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Dallas ME. The 10 most common surgeries in the US. Healthgrades website. https://www.healthgrades.com/explore/the-10-most-common-surgeries-in-the-us. Reviewed August 15, 2017. Accessed October 2, 2017.
- Laumann EO, Masi CM, Zuckerman EW. Circumcision in the United States: prevalence, prophylactic effects, and sexual practice. JAMA. 1997;277(13):1052–1057.
- American Academy of Pediatrics Task Force on Circumcision. Male circumcision. Pediatrics. 2012;130(3):e756–e785.
- American Academy of Pediatrics Task Force on Circumcision. Circumcision policy statement. Pediatrics. 2012;130(3):585–586.
- Morris BJ, Krieger JN. Does male circumcision affect sexual function, sensitivity, or satisfaction? A systematic review. J Sex Med. 2013;10(11):2644–2657.
- Howard FM, Howard CR, Fortune K, Generelli P, Zolnoun D, tenHoopen C. A randomized, placebo-controlled comparison of EMLA and dorsal penile nerve block for pain relief during neonatal circumcision. Prim Care Update Ob Gyns. 1998;5(4):196.
- Taddio A, Stevens B, Craig K, et al. Efficacy and safety of lidocaine-prilocaine cream for pain during circumcision. N Engl J Med. 1997;336(17):1197–1201.
- Lander J, Brady-Fryer B, Metcalfe JB, Nazarali S, Muttitt S. Comparison of ring block, dorsal penile nerve block, and topical anesthesia for neonatal circumcision: a randomized controlled trial. JAMA. 1997;278(24):2157–2162.
- Hardwick-Smith S, Mastrobattista JM, Wallace PA, Ritchey ML. Ring block for neonatal circumcision. Obstet Gynecol. 1998;91(6):930–934.
- Kaufman GE, Cimo S, Miller LW, Blass EM. An evaluation of the effects of sucrose on neonatal pain with 2 commonly used circumcision methods. Am J Obstet Gynecol. 2002;186(3):564–568.
- Tucker SC, Cerqueiro J, Sterne GD, Bracka A. Circumcision: a refined technique and 5 year review. Ann R Coll Surg Engl. 2001;83(2):121–125.
- Fraser ID, Tjoe J. Circumcision using bipolar scissors can be a safe and simple operation. Ann R Coll Surg Engl. 2000;82(3):190–191.
- Wiswell TE, Geschke DW. Risks from circumcision during the first month of life compared with those for uncircumcised boys. Pediatrics. 1989;83(6):1011–1015.
- Dallas ME. The 10 most common surgeries in the US. Healthgrades website. https://www.healthgrades.com/explore/the-10-most-common-surgeries-in-the-us. Reviewed August 15, 2017. Accessed October 2, 2017.
- Laumann EO, Masi CM, Zuckerman EW. Circumcision in the United States: prevalence, prophylactic effects, and sexual practice. JAMA. 1997;277(13):1052–1057.
- American Academy of Pediatrics Task Force on Circumcision. Male circumcision. Pediatrics. 2012;130(3):e756–e785.
- American Academy of Pediatrics Task Force on Circumcision. Circumcision policy statement. Pediatrics. 2012;130(3):585–586.
- Morris BJ, Krieger JN. Does male circumcision affect sexual function, sensitivity, or satisfaction? A systematic review. J Sex Med. 2013;10(11):2644–2657.
- Howard FM, Howard CR, Fortune K, Generelli P, Zolnoun D, tenHoopen C. A randomized, placebo-controlled comparison of EMLA and dorsal penile nerve block for pain relief during neonatal circumcision. Prim Care Update Ob Gyns. 1998;5(4):196.
- Taddio A, Stevens B, Craig K, et al. Efficacy and safety of lidocaine-prilocaine cream for pain during circumcision. N Engl J Med. 1997;336(17):1197–1201.
- Lander J, Brady-Fryer B, Metcalfe JB, Nazarali S, Muttitt S. Comparison of ring block, dorsal penile nerve block, and topical anesthesia for neonatal circumcision: a randomized controlled trial. JAMA. 1997;278(24):2157–2162.
- Hardwick-Smith S, Mastrobattista JM, Wallace PA, Ritchey ML. Ring block for neonatal circumcision. Obstet Gynecol. 1998;91(6):930–934.
- Kaufman GE, Cimo S, Miller LW, Blass EM. An evaluation of the effects of sucrose on neonatal pain with 2 commonly used circumcision methods. Am J Obstet Gynecol. 2002;186(3):564–568.
- Tucker SC, Cerqueiro J, Sterne GD, Bracka A. Circumcision: a refined technique and 5 year review. Ann R Coll Surg Engl. 2001;83(2):121–125.
- Fraser ID, Tjoe J. Circumcision using bipolar scissors can be a safe and simple operation. Ann R Coll Surg Engl. 2000;82(3):190–191.
- Wiswell TE, Geschke DW. Risks from circumcision during the first month of life compared with those for uncircumcised boys. Pediatrics. 1989;83(6):1011–1015.
Questions value of ACOG/SMFM guidelines
FOR THE MANAGEMENT OF LABOR, PATIENCE IS A VIRTUE
ROBERT L. BARBIERI, MD (EDITORIAL; AUGUST 2017)
Questions value of ACOG/SMFM guidelines
The labor management guidelines recommended by the American College of Obstetricians and Gynecologists (ACOG) and the Society of Maternal-Fetal Medicine (SMFM) are terrible. Now retired, I trained in 1959–1963. In my career as an obstetrician, my primary cesarean delivery rate was 10% or less, and part of that was external pressure from people who did not know how to deliver a baby. Persistent occiput posterior position is a problem of inadequate flexion of the head, often due to ineffective contractions earlier. In such a situation, “pit” early! Rotate the head if you must, and teach residents how, please. The guidelines do not discuss the exhausted mother who goes home after a long labor or hours of pushing. I have interviewed new obstetricians in my community as early as 1980 who did not know what deep transverse arrest was. There, I am done voicing my disgust with obstetrics as it is practiced today.
James Honig, MD
Merritt Island, Florida
Managing difficult labor scenarios
I concur with Dr. Barbieri’s views on labor management that watchful waiting and giving the patient adequate time to progress naturally is the key to increase the chances of vaginal delivery. After all, labor is a physiologic process and should progress naturally. Having said that, I would like to know Dr. Barbieri’s views on handling certain circumstances in which patients these days land in the labor room, including 1) postdatedpregnancy with reduced fetal movements and not in labor; 2) full-term/postterm pregnancy with free-floating head and poor Bishop score; 3) full-term pregnancy with niggling pains for more than 1 week; and many such conditions that place you in the dilemma of whether to induce, knowing that chances of failure are high.
Manju Hotchandani, MD
New Delhi, India
Midwives always use patience to guide labor
As a Certified Nurse-Midwife since 1985 (now retired), “patience” in managing labor has always been my guide, as it has been for my midwifery colleagues. This is another example of ACOG finally acknowledging the truths we women have always known, without crediting the wisdom of midwives over the centuries. Lamaze International’s 6 Healthy Birth Practices also must have been their guide. “Evolving concepts of normal labor progress,” as though this was new information, would be humorous if it were not so frustrating!
Marsha Kelly, CNM
Charlotte, North Carolina
Dr. Barbieri responds
The readers of OBG
Every clinician involved in the birth process is deeply committed to a safe delivery for both mother and baby. Clinicians guide the birth process based on the unique characteristics and needs of each woman. Dr. Honig advocates for the active management of the labor process, while Ms. Kelly advocates for less intervention. Both approaches to labor management may be optimal depending on the unique clinical needs of each woman. Dr. Hotchandani inquires about managing common obstetric presentations. In my practice, induction is recommended for all women postterm who report consistently reduced fetal movement with the goal of reducing the risk of sudden intrauterine fetal demise. For healthy women at term with painful contractions and reassuring fetal status, but no cervical change, we support and counsel the patient and offer therapeutic rest with morphine. For women at term with a floating head and poor Bishop score, we would not intervene, until 41 weeks’ gestation when we would initiate gentle cervical ripening with mechanical or pharmacologic treatment.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
FOR THE MANAGEMENT OF LABOR, PATIENCE IS A VIRTUE
ROBERT L. BARBIERI, MD (EDITORIAL; AUGUST 2017)
Questions value of ACOG/SMFM guidelines
The labor management guidelines recommended by the American College of Obstetricians and Gynecologists (ACOG) and the Society of Maternal-Fetal Medicine (SMFM) are terrible. Now retired, I trained in 1959–1963. In my career as an obstetrician, my primary cesarean delivery rate was 10% or less, and part of that was external pressure from people who did not know how to deliver a baby. Persistent occiput posterior position is a problem of inadequate flexion of the head, often due to ineffective contractions earlier. In such a situation, “pit” early! Rotate the head if you must, and teach residents how, please. The guidelines do not discuss the exhausted mother who goes home after a long labor or hours of pushing. I have interviewed new obstetricians in my community as early as 1980 who did not know what deep transverse arrest was. There, I am done voicing my disgust with obstetrics as it is practiced today.
James Honig, MD
Merritt Island, Florida
Managing difficult labor scenarios
I concur with Dr. Barbieri’s views on labor management that watchful waiting and giving the patient adequate time to progress naturally is the key to increase the chances of vaginal delivery. After all, labor is a physiologic process and should progress naturally. Having said that, I would like to know Dr. Barbieri’s views on handling certain circumstances in which patients these days land in the labor room, including 1) postdatedpregnancy with reduced fetal movements and not in labor; 2) full-term/postterm pregnancy with free-floating head and poor Bishop score; 3) full-term pregnancy with niggling pains for more than 1 week; and many such conditions that place you in the dilemma of whether to induce, knowing that chances of failure are high.
Manju Hotchandani, MD
New Delhi, India
Midwives always use patience to guide labor
As a Certified Nurse-Midwife since 1985 (now retired), “patience” in managing labor has always been my guide, as it has been for my midwifery colleagues. This is another example of ACOG finally acknowledging the truths we women have always known, without crediting the wisdom of midwives over the centuries. Lamaze International’s 6 Healthy Birth Practices also must have been their guide. “Evolving concepts of normal labor progress,” as though this was new information, would be humorous if it were not so frustrating!
Marsha Kelly, CNM
Charlotte, North Carolina
Dr. Barbieri responds
The readers of OBG
Every clinician involved in the birth process is deeply committed to a safe delivery for both mother and baby. Clinicians guide the birth process based on the unique characteristics and needs of each woman. Dr. Honig advocates for the active management of the labor process, while Ms. Kelly advocates for less intervention. Both approaches to labor management may be optimal depending on the unique clinical needs of each woman. Dr. Hotchandani inquires about managing common obstetric presentations. In my practice, induction is recommended for all women postterm who report consistently reduced fetal movement with the goal of reducing the risk of sudden intrauterine fetal demise. For healthy women at term with painful contractions and reassuring fetal status, but no cervical change, we support and counsel the patient and offer therapeutic rest with morphine. For women at term with a floating head and poor Bishop score, we would not intervene, until 41 weeks’ gestation when we would initiate gentle cervical ripening with mechanical or pharmacologic treatment.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
FOR THE MANAGEMENT OF LABOR, PATIENCE IS A VIRTUE
ROBERT L. BARBIERI, MD (EDITORIAL; AUGUST 2017)
Questions value of ACOG/SMFM guidelines
The labor management guidelines recommended by the American College of Obstetricians and Gynecologists (ACOG) and the Society of Maternal-Fetal Medicine (SMFM) are terrible. Now retired, I trained in 1959–1963. In my career as an obstetrician, my primary cesarean delivery rate was 10% or less, and part of that was external pressure from people who did not know how to deliver a baby. Persistent occiput posterior position is a problem of inadequate flexion of the head, often due to ineffective contractions earlier. In such a situation, “pit” early! Rotate the head if you must, and teach residents how, please. The guidelines do not discuss the exhausted mother who goes home after a long labor or hours of pushing. I have interviewed new obstetricians in my community as early as 1980 who did not know what deep transverse arrest was. There, I am done voicing my disgust with obstetrics as it is practiced today.
James Honig, MD
Merritt Island, Florida
Managing difficult labor scenarios
I concur with Dr. Barbieri’s views on labor management that watchful waiting and giving the patient adequate time to progress naturally is the key to increase the chances of vaginal delivery. After all, labor is a physiologic process and should progress naturally. Having said that, I would like to know Dr. Barbieri’s views on handling certain circumstances in which patients these days land in the labor room, including 1) postdatedpregnancy with reduced fetal movements and not in labor; 2) full-term/postterm pregnancy with free-floating head and poor Bishop score; 3) full-term pregnancy with niggling pains for more than 1 week; and many such conditions that place you in the dilemma of whether to induce, knowing that chances of failure are high.
Manju Hotchandani, MD
New Delhi, India
Midwives always use patience to guide labor
As a Certified Nurse-Midwife since 1985 (now retired), “patience” in managing labor has always been my guide, as it has been for my midwifery colleagues. This is another example of ACOG finally acknowledging the truths we women have always known, without crediting the wisdom of midwives over the centuries. Lamaze International’s 6 Healthy Birth Practices also must have been their guide. “Evolving concepts of normal labor progress,” as though this was new information, would be humorous if it were not so frustrating!
Marsha Kelly, CNM
Charlotte, North Carolina
Dr. Barbieri responds
The readers of OBG
Every clinician involved in the birth process is deeply committed to a safe delivery for both mother and baby. Clinicians guide the birth process based on the unique characteristics and needs of each woman. Dr. Honig advocates for the active management of the labor process, while Ms. Kelly advocates for less intervention. Both approaches to labor management may be optimal depending on the unique clinical needs of each woman. Dr. Hotchandani inquires about managing common obstetric presentations. In my practice, induction is recommended for all women postterm who report consistently reduced fetal movement with the goal of reducing the risk of sudden intrauterine fetal demise. For healthy women at term with painful contractions and reassuring fetal status, but no cervical change, we support and counsel the patient and offer therapeutic rest with morphine. For women at term with a floating head and poor Bishop score, we would not intervene, until 41 weeks’ gestation when we would initiate gentle cervical ripening with mechanical or pharmacologic treatment.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Brachial plexus injury: permanent disability
Brachial plexus injury: permanent disability
After concerning test results, a woman went to the hospital for induction of labor. During vaginal delivery, a shoulder dystocia was encountered. The baby was born within 60 seconds using the McRoberts maneuver and suprapubic pressure. The ObGyn charted mild shoulder dystocia.
The child has decreased mobility of his left arm. MRI studies and surgical findings confirmed brachial plexus rupture and avulsion at C5-C7. Despite nerve grafting, the child has a significant disability to his left arm and shoulder.
PARENT'S CLAIM: The ObGyn negligently applied excessive lateral traction, improperly used lateral traction as a maneuver, and instructed the mother to continuously push.
PHYSICIAN'S DEFENSE: Shoulder dystocia was properly diagnosed and resolved using standard maneuvers. Traction and pushing are needed during shoulder dystocia management to determine whether the maneuvers are successful. Brachial plexus injuries can occur because of the normal forces of labor and delivery.
VERDICT: An Illinois defense verdict was returned.
Mother claims PTSD after twin's stillbirth
Expecting twins, a 23-year-old woman at 33.5 weeks' gestation reported pain. The ObGyn noted that her cervix was 4-cm dilated, 1 twin was in breech position, and that labor had begun. He recommended that the patient go to the hospital for cesarean delivery but told her that she could go home, shower, and gather her belongings first. When the mother arrived at the hospital 2.5 hours later, the fetal heart-rate (FHR) monitor indicated that one twin's heart was not active. An emergency cesarean delivery was performed. One twin was safely born, but the other died.
PARENT'S CLAIM: The ObGyn failed to properly address the onset of labor. The twin died because of compression of the umbilical cord. If the mother had gone directly to the hospital, FHR abnormalities would have been apparent and timely intervention could have been taken.
The stillbirth caused the onset of severe emotional distress in the mother leading to posttraumatic stress disorder (PTSD). She had extensive counseling. Her psychologist reported that the patient also suffered from complex grief disorder.
PHYSICIAN'S DEFENSE: The ObGyn's actions did not cause the injury. The twins' hearts were monitored at the last prenatal examination and were normal. It was appropriate for the ObGyn to allow the patient to return home before going to the hospital; the situation was urgent but not emergent. The stillbirth resulted from chorioamnionitis, a microscopic condition that is difficult to detect. A pathologist confirmed the diagnosis after examining the placenta.
The extent of the patient's grief was contested. An expert psychiatrist reported that complex grief disorder is not a recognized medical condition, and that, upon his examination, the patient did not exhibit PTSD symptoms.
VERDICT: A New York defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Brachial plexus injury: permanent disability
After concerning test results, a woman went to the hospital for induction of labor. During vaginal delivery, a shoulder dystocia was encountered. The baby was born within 60 seconds using the McRoberts maneuver and suprapubic pressure. The ObGyn charted mild shoulder dystocia.
The child has decreased mobility of his left arm. MRI studies and surgical findings confirmed brachial plexus rupture and avulsion at C5-C7. Despite nerve grafting, the child has a significant disability to his left arm and shoulder.
PARENT'S CLAIM: The ObGyn negligently applied excessive lateral traction, improperly used lateral traction as a maneuver, and instructed the mother to continuously push.
PHYSICIAN'S DEFENSE: Shoulder dystocia was properly diagnosed and resolved using standard maneuvers. Traction and pushing are needed during shoulder dystocia management to determine whether the maneuvers are successful. Brachial plexus injuries can occur because of the normal forces of labor and delivery.
VERDICT: An Illinois defense verdict was returned.
Mother claims PTSD after twin's stillbirth
Expecting twins, a 23-year-old woman at 33.5 weeks' gestation reported pain. The ObGyn noted that her cervix was 4-cm dilated, 1 twin was in breech position, and that labor had begun. He recommended that the patient go to the hospital for cesarean delivery but told her that she could go home, shower, and gather her belongings first. When the mother arrived at the hospital 2.5 hours later, the fetal heart-rate (FHR) monitor indicated that one twin's heart was not active. An emergency cesarean delivery was performed. One twin was safely born, but the other died.
PARENT'S CLAIM: The ObGyn failed to properly address the onset of labor. The twin died because of compression of the umbilical cord. If the mother had gone directly to the hospital, FHR abnormalities would have been apparent and timely intervention could have been taken.
The stillbirth caused the onset of severe emotional distress in the mother leading to posttraumatic stress disorder (PTSD). She had extensive counseling. Her psychologist reported that the patient also suffered from complex grief disorder.
PHYSICIAN'S DEFENSE: The ObGyn's actions did not cause the injury. The twins' hearts were monitored at the last prenatal examination and were normal. It was appropriate for the ObGyn to allow the patient to return home before going to the hospital; the situation was urgent but not emergent. The stillbirth resulted from chorioamnionitis, a microscopic condition that is difficult to detect. A pathologist confirmed the diagnosis after examining the placenta.
The extent of the patient's grief was contested. An expert psychiatrist reported that complex grief disorder is not a recognized medical condition, and that, upon his examination, the patient did not exhibit PTSD symptoms.
VERDICT: A New York defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Brachial plexus injury: permanent disability
After concerning test results, a woman went to the hospital for induction of labor. During vaginal delivery, a shoulder dystocia was encountered. The baby was born within 60 seconds using the McRoberts maneuver and suprapubic pressure. The ObGyn charted mild shoulder dystocia.
The child has decreased mobility of his left arm. MRI studies and surgical findings confirmed brachial plexus rupture and avulsion at C5-C7. Despite nerve grafting, the child has a significant disability to his left arm and shoulder.
PARENT'S CLAIM: The ObGyn negligently applied excessive lateral traction, improperly used lateral traction as a maneuver, and instructed the mother to continuously push.
PHYSICIAN'S DEFENSE: Shoulder dystocia was properly diagnosed and resolved using standard maneuvers. Traction and pushing are needed during shoulder dystocia management to determine whether the maneuvers are successful. Brachial plexus injuries can occur because of the normal forces of labor and delivery.
VERDICT: An Illinois defense verdict was returned.
Mother claims PTSD after twin's stillbirth
Expecting twins, a 23-year-old woman at 33.5 weeks' gestation reported pain. The ObGyn noted that her cervix was 4-cm dilated, 1 twin was in breech position, and that labor had begun. He recommended that the patient go to the hospital for cesarean delivery but told her that she could go home, shower, and gather her belongings first. When the mother arrived at the hospital 2.5 hours later, the fetal heart-rate (FHR) monitor indicated that one twin's heart was not active. An emergency cesarean delivery was performed. One twin was safely born, but the other died.
PARENT'S CLAIM: The ObGyn failed to properly address the onset of labor. The twin died because of compression of the umbilical cord. If the mother had gone directly to the hospital, FHR abnormalities would have been apparent and timely intervention could have been taken.
The stillbirth caused the onset of severe emotional distress in the mother leading to posttraumatic stress disorder (PTSD). She had extensive counseling. Her psychologist reported that the patient also suffered from complex grief disorder.
PHYSICIAN'S DEFENSE: The ObGyn's actions did not cause the injury. The twins' hearts were monitored at the last prenatal examination and were normal. It was appropriate for the ObGyn to allow the patient to return home before going to the hospital; the situation was urgent but not emergent. The stillbirth resulted from chorioamnionitis, a microscopic condition that is difficult to detect. A pathologist confirmed the diagnosis after examining the placenta.
The extent of the patient's grief was contested. An expert psychiatrist reported that complex grief disorder is not a recognized medical condition, and that, upon his examination, the patient did not exhibit PTSD symptoms.
VERDICT: A New York defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Product Update: MyoSure MANUAL; Rivanna's Accuro 3D; PeriGen; Instavit
HYSTEROSCOPY TISSUE REMOVAL DEVICE

Hologic, Inc, has introduced the MyoSure® MANUAL Tissue Removal Device for resecting and removing tissue during in-office hysteroscopic intrauterine procedures. When used with the MyoSure hysteroscope, the MyoSure MANUAL device has a fully integrated vacuum that does not require external suction and can be operated using a 1-L saline bag. The clear tissue trap allows for visual co
This new Hologic product joins the MyoSure suite of gynecologic surgical products that includes the MyoSure, MyoSure REACH, MyoSure XL, and MyoSure LITE devices.
FOR MORE INFORMATION, VISIT: http://myosure.com/
SPINAL NAVIGATION TECHNOLOGY FOR EPIDURAL ANESTHESIA
The Accuro® 3D image-guided spinal navigation technology by Rivanna Medical® is a handheld, lightweight, untethered ultrasound-based system designed to help apply spinal and epidural anesthesia. Ultrasonography is the imaging modality of choice for epidurals in expectant mothers who must avoid the radiation involved in other imaging procedures, according to Rivanna Medical.
In a recent trial, Accuro identified the appropriate epidural injection sites along the lower spine and calculated the depth to the epidural space. Actual epidural depth was confirmed by measuring needle penetration during successful epidural delivery by anesthesia providers. Accuro predicted this depth within an average of 0.61 cm, reports Rivanna Medical. In addition, Accuro identified the appropriate spinal interspace for needle insertion in 94% of patients and enabled 87% success in first-attempt epidural administration.
FOR MORE INFORMATION, VISIT: https://rivannamedical.com/
SOFTWARE AND HUB HELP IDENTIFY CRITICALLY ILL L&D PATIENTS
PeriGen, Inc, a software-solutions company, has launched PeriWatch™ HUB™, new perinatal software and a dashboard for labor and delivery (L&D) units.
PeriGen says that its PeriWatch modules provide state-of-the-art L&D documentation and fetal surveillance coupled with analytics and an electronic critical-condition dashboard for hospital maternity units.
HUB is an intelligent perinatal dashboard designed to facilitate the timely recognition of maternity patients who develop critical illness. Using PeriGen’s proprietary algorithms, it prioritizes patients based on physician-chosen threshold settings for vital signs, labor progress, and fetal heart rate patterns, and consolidates that data into an easy-to-read interactive dashboard.
FOR MORE INFORMATION, VISIT: http://perigen.com/
ORAL SPRAY VITAMINS: ALTERNATIVE TO PILLS

Instavit® Spray Vitamins offer an alternative to patients who have difficulty swallowing pills. Instavit says that its oral vitamins, sprayed directly into the mouth, are sugar-free, tasty, gluten-free, and contain zero calories. The sprays are manufactured to the highest standard in cGMP, FDA approved facilities in the United States. Each Instavit spray provides an exact and measured amount of liquid, allowing for correct dosing and also permitting individualization of intake. A 14-oz spray bottle contains about 28 doses.
The Instavit line includes: “Prenatal Care,” “Vitamin B12,” “Instant Energy,” “Vitamin D,” “Daily Health,” “Sweet Dreams,” “Immune Strength,” “Clearer Thinking,” and “Instavit for Kids.” Instavit products are available in retail stores in North America.
FOR MORE INFORMATION, VISIT: http://www.instavit.com/
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
HYSTEROSCOPY TISSUE REMOVAL DEVICE

Hologic, Inc, has introduced the MyoSure® MANUAL Tissue Removal Device for resecting and removing tissue during in-office hysteroscopic intrauterine procedures. When used with the MyoSure hysteroscope, the MyoSure MANUAL device has a fully integrated vacuum that does not require external suction and can be operated using a 1-L saline bag. The clear tissue trap allows for visual co
This new Hologic product joins the MyoSure suite of gynecologic surgical products that includes the MyoSure, MyoSure REACH, MyoSure XL, and MyoSure LITE devices.
FOR MORE INFORMATION, VISIT: http://myosure.com/
SPINAL NAVIGATION TECHNOLOGY FOR EPIDURAL ANESTHESIA
The Accuro® 3D image-guided spinal navigation technology by Rivanna Medical® is a handheld, lightweight, untethered ultrasound-based system designed to help apply spinal and epidural anesthesia. Ultrasonography is the imaging modality of choice for epidurals in expectant mothers who must avoid the radiation involved in other imaging procedures, according to Rivanna Medical.
In a recent trial, Accuro identified the appropriate epidural injection sites along the lower spine and calculated the depth to the epidural space. Actual epidural depth was confirmed by measuring needle penetration during successful epidural delivery by anesthesia providers. Accuro predicted this depth within an average of 0.61 cm, reports Rivanna Medical. In addition, Accuro identified the appropriate spinal interspace for needle insertion in 94% of patients and enabled 87% success in first-attempt epidural administration.
FOR MORE INFORMATION, VISIT: https://rivannamedical.com/
SOFTWARE AND HUB HELP IDENTIFY CRITICALLY ILL L&D PATIENTS
PeriGen, Inc, a software-solutions company, has launched PeriWatch™ HUB™, new perinatal software and a dashboard for labor and delivery (L&D) units.
PeriGen says that its PeriWatch modules provide state-of-the-art L&D documentation and fetal surveillance coupled with analytics and an electronic critical-condition dashboard for hospital maternity units.
HUB is an intelligent perinatal dashboard designed to facilitate the timely recognition of maternity patients who develop critical illness. Using PeriGen’s proprietary algorithms, it prioritizes patients based on physician-chosen threshold settings for vital signs, labor progress, and fetal heart rate patterns, and consolidates that data into an easy-to-read interactive dashboard.
FOR MORE INFORMATION, VISIT: http://perigen.com/
ORAL SPRAY VITAMINS: ALTERNATIVE TO PILLS

Instavit® Spray Vitamins offer an alternative to patients who have difficulty swallowing pills. Instavit says that its oral vitamins, sprayed directly into the mouth, are sugar-free, tasty, gluten-free, and contain zero calories. The sprays are manufactured to the highest standard in cGMP, FDA approved facilities in the United States. Each Instavit spray provides an exact and measured amount of liquid, allowing for correct dosing and also permitting individualization of intake. A 14-oz spray bottle contains about 28 doses.
The Instavit line includes: “Prenatal Care,” “Vitamin B12,” “Instant Energy,” “Vitamin D,” “Daily Health,” “Sweet Dreams,” “Immune Strength,” “Clearer Thinking,” and “Instavit for Kids.” Instavit products are available in retail stores in North America.
FOR MORE INFORMATION, VISIT: http://www.instavit.com/
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
HYSTEROSCOPY TISSUE REMOVAL DEVICE

Hologic, Inc, has introduced the MyoSure® MANUAL Tissue Removal Device for resecting and removing tissue during in-office hysteroscopic intrauterine procedures. When used with the MyoSure hysteroscope, the MyoSure MANUAL device has a fully integrated vacuum that does not require external suction and can be operated using a 1-L saline bag. The clear tissue trap allows for visual co
This new Hologic product joins the MyoSure suite of gynecologic surgical products that includes the MyoSure, MyoSure REACH, MyoSure XL, and MyoSure LITE devices.
FOR MORE INFORMATION, VISIT: http://myosure.com/
SPINAL NAVIGATION TECHNOLOGY FOR EPIDURAL ANESTHESIA
The Accuro® 3D image-guided spinal navigation technology by Rivanna Medical® is a handheld, lightweight, untethered ultrasound-based system designed to help apply spinal and epidural anesthesia. Ultrasonography is the imaging modality of choice for epidurals in expectant mothers who must avoid the radiation involved in other imaging procedures, according to Rivanna Medical.
In a recent trial, Accuro identified the appropriate epidural injection sites along the lower spine and calculated the depth to the epidural space. Actual epidural depth was confirmed by measuring needle penetration during successful epidural delivery by anesthesia providers. Accuro predicted this depth within an average of 0.61 cm, reports Rivanna Medical. In addition, Accuro identified the appropriate spinal interspace for needle insertion in 94% of patients and enabled 87% success in first-attempt epidural administration.
FOR MORE INFORMATION, VISIT: https://rivannamedical.com/
SOFTWARE AND HUB HELP IDENTIFY CRITICALLY ILL L&D PATIENTS
PeriGen, Inc, a software-solutions company, has launched PeriWatch™ HUB™, new perinatal software and a dashboard for labor and delivery (L&D) units.
PeriGen says that its PeriWatch modules provide state-of-the-art L&D documentation and fetal surveillance coupled with analytics and an electronic critical-condition dashboard for hospital maternity units.
HUB is an intelligent perinatal dashboard designed to facilitate the timely recognition of maternity patients who develop critical illness. Using PeriGen’s proprietary algorithms, it prioritizes patients based on physician-chosen threshold settings for vital signs, labor progress, and fetal heart rate patterns, and consolidates that data into an easy-to-read interactive dashboard.
FOR MORE INFORMATION, VISIT: http://perigen.com/
ORAL SPRAY VITAMINS: ALTERNATIVE TO PILLS

Instavit® Spray Vitamins offer an alternative to patients who have difficulty swallowing pills. Instavit says that its oral vitamins, sprayed directly into the mouth, are sugar-free, tasty, gluten-free, and contain zero calories. The sprays are manufactured to the highest standard in cGMP, FDA approved facilities in the United States. Each Instavit spray provides an exact and measured amount of liquid, allowing for correct dosing and also permitting individualization of intake. A 14-oz spray bottle contains about 28 doses.
The Instavit line includes: “Prenatal Care,” “Vitamin B12,” “Instant Energy,” “Vitamin D,” “Daily Health,” “Sweet Dreams,” “Immune Strength,” “Clearer Thinking,” and “Instavit for Kids.” Instavit products are available in retail stores in North America.
FOR MORE INFORMATION, VISIT: http://www.instavit.com/
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Unplanned cesareans more common with excess gestational weight gain
MONTREAL – The risk for unplanned cesarean delivery is increased when maternal gestational weight gain exceeds the recommended amount – as it does in almost half of pregnancies in the United States.
In a new analysis of data from the Infant Feeding Practices Study II (IFPS II), women with excessive gestational weight gain (GWG) were found to have an adjusted odds ratio of 1.61 for unplanned cesarean delivery, compared with women with adequate GWG (95% confidence interval, 1.11-2.33; P = .013).
Maternal obesity is known to be a risk factor for cesarean delivery, at least in part because excess adipose tissue may interfere with the normal ability of the cervix to thin and dilate with contractions, said Mr. Francescon, a medical student at Ohio University Heritage College of Osteopathic Medicine, Athens. Labor can be prolonged, and it’s often difficult to monitor fetal activity with external activity, he said.
To see whether unplanned cesarean deliveries were associated with excess GWG, Mr. Francescon and his collaborators included data from 2,107 of the 3,033 respondents to the IFPS II, excluding those with missing data and those with planned cesarean deliveries.
Weight gain was grouped into three categories – adequate, inadequate, and excessive – according to guidelines set by the Institute of Medicine. The odds of an unplanned cesarean delivery were adjusted by using multivariable analysis that took into account ethnicity, education, poverty status, parity, and previous obstetric history. The statistical analysis also accounted for the presence of gestational diabetes and the type of birth attendant.
A total of 1,038 women (49.3%) had excessive GWG according to the IOM guidelines, and 287 women (13.6%) overall had an unplanned cesarean delivery. After adjusting for the potentially confounding variables, only excessive weight gain was significantly associated with the risk for unplanned cesarean delivery; those with inadequate weight gain had an odds ratio of 1.03 (95% CI, 0.63-1.69; not significant).
, but rather were attended by a nonobstetrician physician or a midwife, said Mr. Francescon. After excluding patients who planned to have cesarean deliveries, 257 of 1,385 (15.6%) of patients seeing obstetricians had unplanned cesarean deliveries; this figure was 9% for nonobstetrician physicians and 4.1% for midwives/nurse midwives.
“This finding suggests that psychosocial factors, such as the bond formed between caregiver and patient, could also potentially influence birthing patterns,” wrote Mr. Francescon and his collaborators.
“Our study findings are supported by previous studies that found increased likelihood of cesarean delivery among women with excessive GWG,” said the investigators.
The study had a large sample size, used well-tested survey instruments, and could include many variables in statistical analysis, all strengths, wrote Mr. Francescon and his coauthors. However, there remained the potential for volunteer bias and recall bias. In addition, weight gain carries social stigma, which could have influence the self-reported results.
“Gestational weight gain is a modifiable risk factor for unplanned cesarean delivery,” Mr. Francescon said. He and his collaborators propose that a comprehensive plan of dietary and lifestyle modifications beginning pre-conception, together with enhanced patient and provider awareness of the risk of unplanned cesarean deliveries with excess gestational weight gain, could help reduce the number of unplanned cesarean deliveries.
The data for the study were provided by the Centers for Disease Control and Prevention. Mr. Francescon reported no conflicts of interest.
SOURCE: Francescon J. NAPCRG 2017 Abstract P495.
MONTREAL – The risk for unplanned cesarean delivery is increased when maternal gestational weight gain exceeds the recommended amount – as it does in almost half of pregnancies in the United States.
In a new analysis of data from the Infant Feeding Practices Study II (IFPS II), women with excessive gestational weight gain (GWG) were found to have an adjusted odds ratio of 1.61 for unplanned cesarean delivery, compared with women with adequate GWG (95% confidence interval, 1.11-2.33; P = .013).
Maternal obesity is known to be a risk factor for cesarean delivery, at least in part because excess adipose tissue may interfere with the normal ability of the cervix to thin and dilate with contractions, said Mr. Francescon, a medical student at Ohio University Heritage College of Osteopathic Medicine, Athens. Labor can be prolonged, and it’s often difficult to monitor fetal activity with external activity, he said.
To see whether unplanned cesarean deliveries were associated with excess GWG, Mr. Francescon and his collaborators included data from 2,107 of the 3,033 respondents to the IFPS II, excluding those with missing data and those with planned cesarean deliveries.
Weight gain was grouped into three categories – adequate, inadequate, and excessive – according to guidelines set by the Institute of Medicine. The odds of an unplanned cesarean delivery were adjusted by using multivariable analysis that took into account ethnicity, education, poverty status, parity, and previous obstetric history. The statistical analysis also accounted for the presence of gestational diabetes and the type of birth attendant.
A total of 1,038 women (49.3%) had excessive GWG according to the IOM guidelines, and 287 women (13.6%) overall had an unplanned cesarean delivery. After adjusting for the potentially confounding variables, only excessive weight gain was significantly associated with the risk for unplanned cesarean delivery; those with inadequate weight gain had an odds ratio of 1.03 (95% CI, 0.63-1.69; not significant).
, but rather were attended by a nonobstetrician physician or a midwife, said Mr. Francescon. After excluding patients who planned to have cesarean deliveries, 257 of 1,385 (15.6%) of patients seeing obstetricians had unplanned cesarean deliveries; this figure was 9% for nonobstetrician physicians and 4.1% for midwives/nurse midwives.
“This finding suggests that psychosocial factors, such as the bond formed between caregiver and patient, could also potentially influence birthing patterns,” wrote Mr. Francescon and his collaborators.
“Our study findings are supported by previous studies that found increased likelihood of cesarean delivery among women with excessive GWG,” said the investigators.
The study had a large sample size, used well-tested survey instruments, and could include many variables in statistical analysis, all strengths, wrote Mr. Francescon and his coauthors. However, there remained the potential for volunteer bias and recall bias. In addition, weight gain carries social stigma, which could have influence the self-reported results.
“Gestational weight gain is a modifiable risk factor for unplanned cesarean delivery,” Mr. Francescon said. He and his collaborators propose that a comprehensive plan of dietary and lifestyle modifications beginning pre-conception, together with enhanced patient and provider awareness of the risk of unplanned cesarean deliveries with excess gestational weight gain, could help reduce the number of unplanned cesarean deliveries.
The data for the study were provided by the Centers for Disease Control and Prevention. Mr. Francescon reported no conflicts of interest.
SOURCE: Francescon J. NAPCRG 2017 Abstract P495.
MONTREAL – The risk for unplanned cesarean delivery is increased when maternal gestational weight gain exceeds the recommended amount – as it does in almost half of pregnancies in the United States.
In a new analysis of data from the Infant Feeding Practices Study II (IFPS II), women with excessive gestational weight gain (GWG) were found to have an adjusted odds ratio of 1.61 for unplanned cesarean delivery, compared with women with adequate GWG (95% confidence interval, 1.11-2.33; P = .013).
Maternal obesity is known to be a risk factor for cesarean delivery, at least in part because excess adipose tissue may interfere with the normal ability of the cervix to thin and dilate with contractions, said Mr. Francescon, a medical student at Ohio University Heritage College of Osteopathic Medicine, Athens. Labor can be prolonged, and it’s often difficult to monitor fetal activity with external activity, he said.
To see whether unplanned cesarean deliveries were associated with excess GWG, Mr. Francescon and his collaborators included data from 2,107 of the 3,033 respondents to the IFPS II, excluding those with missing data and those with planned cesarean deliveries.
Weight gain was grouped into three categories – adequate, inadequate, and excessive – according to guidelines set by the Institute of Medicine. The odds of an unplanned cesarean delivery were adjusted by using multivariable analysis that took into account ethnicity, education, poverty status, parity, and previous obstetric history. The statistical analysis also accounted for the presence of gestational diabetes and the type of birth attendant.
A total of 1,038 women (49.3%) had excessive GWG according to the IOM guidelines, and 287 women (13.6%) overall had an unplanned cesarean delivery. After adjusting for the potentially confounding variables, only excessive weight gain was significantly associated with the risk for unplanned cesarean delivery; those with inadequate weight gain had an odds ratio of 1.03 (95% CI, 0.63-1.69; not significant).
, but rather were attended by a nonobstetrician physician or a midwife, said Mr. Francescon. After excluding patients who planned to have cesarean deliveries, 257 of 1,385 (15.6%) of patients seeing obstetricians had unplanned cesarean deliveries; this figure was 9% for nonobstetrician physicians and 4.1% for midwives/nurse midwives.
“This finding suggests that psychosocial factors, such as the bond formed between caregiver and patient, could also potentially influence birthing patterns,” wrote Mr. Francescon and his collaborators.
“Our study findings are supported by previous studies that found increased likelihood of cesarean delivery among women with excessive GWG,” said the investigators.
The study had a large sample size, used well-tested survey instruments, and could include many variables in statistical analysis, all strengths, wrote Mr. Francescon and his coauthors. However, there remained the potential for volunteer bias and recall bias. In addition, weight gain carries social stigma, which could have influence the self-reported results.
“Gestational weight gain is a modifiable risk factor for unplanned cesarean delivery,” Mr. Francescon said. He and his collaborators propose that a comprehensive plan of dietary and lifestyle modifications beginning pre-conception, together with enhanced patient and provider awareness of the risk of unplanned cesarean deliveries with excess gestational weight gain, could help reduce the number of unplanned cesarean deliveries.
The data for the study were provided by the Centers for Disease Control and Prevention. Mr. Francescon reported no conflicts of interest.
SOURCE: Francescon J. NAPCRG 2017 Abstract P495.
REPORTING FROM NAPCRG 2017
Key clinical point: The risk for an unplanned cesarean delivery rose with excess gestational weight gain.
Major finding: The adjusted odds ratio for unplanned cesarean was 1.61 for those with excess GWG (P = .013).
Study details: Retrospective analysis of 2,107 responses to the Infant Feeding Practices Study II (IFPSII).
Disclosures: Study data were provided by the Centers for Disease Control and Prevention. Mr. Francescon reported no conflicts of interest.
Source: Francescon J. NAPCRG 2017 Abstract P495.
Leflunomide use in pregnancy shows little impact on newborns
Leflunomide, prescribed in Canada to treat active rheumatoid arthritis, was previously classified as a category X pregnancy medication because it is embryotoxic and teratogenic in rats and rabbits in doses similar to those used in humans, wrote Anick Bérard, MD, of CHU Sainte Justine, Montreal, and her colleagues, in a study published in Annals of the Rheumatic Diseases.
However, data on the impact of leflunomide on a developing human embryo are limited, so the researchers analyzed the Quebec Pregnancy Cohort, an ongoing study of all pregnancies in Quebec, Canada, between Jan. 1, 1998, and Dec. 31, 2015.
The findings are consistent with those from previous studies and suggest that continued caution is warranted for women of childbearing age who are taking or considering leflunomide, the researchers concluded.
They also examined the potential impact of several categories of other antirheumatic drugs to account for indication bias: other conventional disease-modifying antirheumatic drugs, biologic agents, nonsteroidal anti-inflammatory drugs, oral corticosteroids, and gold salts. Oral corticosteroid use in the first trimester was associated with an increased risk of major congenital malformations (aOR 1.31; 95% CI, 1.06-1.61), and the risk of prematurity also was significant with their use in the second or third trimester (aOR 1.32; 95% CI, 1.09 to 1.60). The risk of major congenital malformations was significantly higher with the use of NSAIDs in the first trimester (aOR 1.15; 95% CI, 1.03-1.29). Any use of disease-modifying antirheumatic drugs overall between the first day of gestation and the index date increased the odds for spontaneous abortion (aOR, 1.54; 95% CI, 1.06-2.22).
Cholestyramine may lower the blood level of the active metabolite of leflunomide to a safe level, the researchers noted, but the study population showed no evidence of cholestyramine or charcoal use for leflunomide washout, and any cholestyramine exposures during pregnancy were not concurrent with leflunomide exposure. “In three first-trimester leflunomide-exposed pregnancies, cholestyramine was introduced in monotherapy in the third trimester,” they wrote.
The results were limited by the small number of women exposed to leflunomide, despite the population-based study being the largest of its kind published to date, the researchers said.
The study was supported in part by the Fonds de la Recherche du Québec-Santé and by Sanofi. Two authors are employees of Sanofi.
SOURCE: Bérard A et al., Ann Rheum Dis. 2017 Dec 8. doi: 10.1136/annrheumdis-2017-212078
Leflunomide, prescribed in Canada to treat active rheumatoid arthritis, was previously classified as a category X pregnancy medication because it is embryotoxic and teratogenic in rats and rabbits in doses similar to those used in humans, wrote Anick Bérard, MD, of CHU Sainte Justine, Montreal, and her colleagues, in a study published in Annals of the Rheumatic Diseases.
However, data on the impact of leflunomide on a developing human embryo are limited, so the researchers analyzed the Quebec Pregnancy Cohort, an ongoing study of all pregnancies in Quebec, Canada, between Jan. 1, 1998, and Dec. 31, 2015.
The findings are consistent with those from previous studies and suggest that continued caution is warranted for women of childbearing age who are taking or considering leflunomide, the researchers concluded.
They also examined the potential impact of several categories of other antirheumatic drugs to account for indication bias: other conventional disease-modifying antirheumatic drugs, biologic agents, nonsteroidal anti-inflammatory drugs, oral corticosteroids, and gold salts. Oral corticosteroid use in the first trimester was associated with an increased risk of major congenital malformations (aOR 1.31; 95% CI, 1.06-1.61), and the risk of prematurity also was significant with their use in the second or third trimester (aOR 1.32; 95% CI, 1.09 to 1.60). The risk of major congenital malformations was significantly higher with the use of NSAIDs in the first trimester (aOR 1.15; 95% CI, 1.03-1.29). Any use of disease-modifying antirheumatic drugs overall between the first day of gestation and the index date increased the odds for spontaneous abortion (aOR, 1.54; 95% CI, 1.06-2.22).
Cholestyramine may lower the blood level of the active metabolite of leflunomide to a safe level, the researchers noted, but the study population showed no evidence of cholestyramine or charcoal use for leflunomide washout, and any cholestyramine exposures during pregnancy were not concurrent with leflunomide exposure. “In three first-trimester leflunomide-exposed pregnancies, cholestyramine was introduced in monotherapy in the third trimester,” they wrote.
The results were limited by the small number of women exposed to leflunomide, despite the population-based study being the largest of its kind published to date, the researchers said.
The study was supported in part by the Fonds de la Recherche du Québec-Santé and by Sanofi. Two authors are employees of Sanofi.
SOURCE: Bérard A et al., Ann Rheum Dis. 2017 Dec 8. doi: 10.1136/annrheumdis-2017-212078
Leflunomide, prescribed in Canada to treat active rheumatoid arthritis, was previously classified as a category X pregnancy medication because it is embryotoxic and teratogenic in rats and rabbits in doses similar to those used in humans, wrote Anick Bérard, MD, of CHU Sainte Justine, Montreal, and her colleagues, in a study published in Annals of the Rheumatic Diseases.
However, data on the impact of leflunomide on a developing human embryo are limited, so the researchers analyzed the Quebec Pregnancy Cohort, an ongoing study of all pregnancies in Quebec, Canada, between Jan. 1, 1998, and Dec. 31, 2015.
The findings are consistent with those from previous studies and suggest that continued caution is warranted for women of childbearing age who are taking or considering leflunomide, the researchers concluded.
They also examined the potential impact of several categories of other antirheumatic drugs to account for indication bias: other conventional disease-modifying antirheumatic drugs, biologic agents, nonsteroidal anti-inflammatory drugs, oral corticosteroids, and gold salts. Oral corticosteroid use in the first trimester was associated with an increased risk of major congenital malformations (aOR 1.31; 95% CI, 1.06-1.61), and the risk of prematurity also was significant with their use in the second or third trimester (aOR 1.32; 95% CI, 1.09 to 1.60). The risk of major congenital malformations was significantly higher with the use of NSAIDs in the first trimester (aOR 1.15; 95% CI, 1.03-1.29). Any use of disease-modifying antirheumatic drugs overall between the first day of gestation and the index date increased the odds for spontaneous abortion (aOR, 1.54; 95% CI, 1.06-2.22).
Cholestyramine may lower the blood level of the active metabolite of leflunomide to a safe level, the researchers noted, but the study population showed no evidence of cholestyramine or charcoal use for leflunomide washout, and any cholestyramine exposures during pregnancy were not concurrent with leflunomide exposure. “In three first-trimester leflunomide-exposed pregnancies, cholestyramine was introduced in monotherapy in the third trimester,” they wrote.
The results were limited by the small number of women exposed to leflunomide, despite the population-based study being the largest of its kind published to date, the researchers said.
The study was supported in part by the Fonds de la Recherche du Québec-Santé and by Sanofi. Two authors are employees of Sanofi.
SOURCE: Bérard A et al., Ann Rheum Dis. 2017 Dec 8. doi: 10.1136/annrheumdis-2017-212078
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point: Exposure to leflunomide during pregnancy was not associated with significantly increased risk of major congenital malformations, low birth weight, premature birth, or spontaneous abortions.
Major finding: No significant association was seen between leflunomide use in the first trimester and an increased risk of major congenital malformations based on five cases (adjusted odds ratio, 0.97).
Data source: A population-based cohort study of 289,688 pregnancies in Canada between 1998 and 2015.
Disclosures: The study was supported in part by the Fonds de la Recherche du Québec-Santé and by Sanofi. Two authors are employees of Sanofi.
Source: Bérard A et al., Ann Rheum Dis. 2017 Dec 8. doi: 10.1136/annrheumdis-2017-212078
Maternal mortality is set to be a top issue for 2018
Addressing issues around maternal mortality is going to be the top focus for the American Congress of Obstetricians and Gynecologists in 2018.
“It is will be the priority of my presidency here at ACOG,” President-elect Lisa Hollier, MD, said in an interview. Her term as president begins at the end of April 2018.
Rates of maternal mortality – defined as rates of death within 365 days of pregnancy – have become an increasingly prominent issue in the United States. Many states have created dedicated committees to examine the causes of increasing mortality and look for solutions. California, in particular, has had some success in reducing these rates.
To address the maternal mortality issue, ACOG is working on passing legislation through Congress that would give the federal government a role in funding these state-level committees.
“The main crux of the bill is to provide authorization for state maternal mortality, for funds to support state maternal mortality review committees,” said Rachel Tetlow, the director of federal affairs at ACOG. “We know that while a majority of states do have committees, there are still some who are struggling to stand them up and others that are struggling to fund them at full capacity. This legislation looks to support those state efforts to ensure that states really are able to move forward with reviewing maternal deaths and in some cases near misses in their states and recommend local state-based solutions.”
Another hot button issue that could affect maternal mortality is access to abortion.
“It is going to be interesting to see how those numbers shift as abortion providers are no longer available,” said Constance J. Bohon, MD, an ob.gyn. in Washington, D.C., and the ACOG state legislative chair from the District of Columbia. “For example, there is a concern that in states such as Texas, the maternal mortality rates may rise because of a lack of abortion providers.”
Attacks on abortion rights at both the state and federal level are expected in the coming year as well, Dr. Bohon said. She also expressed concerns over initiatives moving through some state houses that would hold doctors criminally liable for performing an abortion.
“What we have seen in the past is that these [abortion] bills come up really quickly without a whole lot of warning, so it’s difficult to say the specific legislation that we will see,” Ms. Tetlow said. “I am fairly confident that we will see at least one more vote in the House of Representatives and potentially one in the Senate ... before the 2018 elections.”
Maternal mortality could be symptomatic of another key issue in women’s health – an overall lack of access to adequate health care.
“One big issue is going to be how we get obstetrical care to women in communities where there is limited access,” she said. “We have got to figure out how to get all women, especially women in underserved areas who could be high risk into pregnancy care early on.”
Beyond that, ACOG is expecting that the women’s health services that have been in the cross hairs recently will continue to be so in 2018.
“2017 has been a year of just challenges and challenges and challenges for practicing ob.gyns. and patients, and we are expecting pretty much the same in 2018,” said Lucia DiVenere, a government and political affairs officer at ACOG.
Cuts to Medicaid, which House Speaker Paul Ryan (R-Wisc.) has identified as a key legislative priority for 2018, could create some significant issues for patients’ access to services.
“Roughly about 50% of deliveries are paid for by Medicaid,” Dr. Bohon said, noting that, for some states, that number can reach as high as 64%. “If those women don’t have access to care, it will be a disaster.”
The American Academy of Family Physicians will also be looking to maintain coverage of women’s health services in the Affordable Care Act.
“I think that our focus in 2018 is going to be around women’s continued access to comprehensive reproductive health care,” said AAFP President Michael Munger, MD. “Not only ensuring they have access to their breast, uterine, and cervical cancer screenings, prenatal maternity and postnatal care, but also preventive services.”
Dr. Munger singled out the Trump administration’s 2017 regulations allowing employers to opt out of providing contraception coverage for moral or religious reasons. “I think that is going to be a continued focus moving forward.”
“Three-quarters of women of childbearing age are in the workforce,” said Kandice Kapinos, PhD, of the Rand Corporation. “The studies on maternity leave show really positive effects of maternity leave on a wide range of child and maternal health outcomes.”
Not having an adequate amount of maternity leave can affect a woman’s ability to breastfeed her newborn, Dr. Kapinos added. “Breastfeeding can be difficult when you return to work,” she said. “Paid maternity leave would result in increases in breastfeeding. That has pretty big implications for health for women and children, which translates into pretty big cost savings.”
[email protected]
Addressing issues around maternal mortality is going to be the top focus for the American Congress of Obstetricians and Gynecologists in 2018.
“It is will be the priority of my presidency here at ACOG,” President-elect Lisa Hollier, MD, said in an interview. Her term as president begins at the end of April 2018.
Rates of maternal mortality – defined as rates of death within 365 days of pregnancy – have become an increasingly prominent issue in the United States. Many states have created dedicated committees to examine the causes of increasing mortality and look for solutions. California, in particular, has had some success in reducing these rates.
To address the maternal mortality issue, ACOG is working on passing legislation through Congress that would give the federal government a role in funding these state-level committees.
“The main crux of the bill is to provide authorization for state maternal mortality, for funds to support state maternal mortality review committees,” said Rachel Tetlow, the director of federal affairs at ACOG. “We know that while a majority of states do have committees, there are still some who are struggling to stand them up and others that are struggling to fund them at full capacity. This legislation looks to support those state efforts to ensure that states really are able to move forward with reviewing maternal deaths and in some cases near misses in their states and recommend local state-based solutions.”
Another hot button issue that could affect maternal mortality is access to abortion.
“It is going to be interesting to see how those numbers shift as abortion providers are no longer available,” said Constance J. Bohon, MD, an ob.gyn. in Washington, D.C., and the ACOG state legislative chair from the District of Columbia. “For example, there is a concern that in states such as Texas, the maternal mortality rates may rise because of a lack of abortion providers.”
Attacks on abortion rights at both the state and federal level are expected in the coming year as well, Dr. Bohon said. She also expressed concerns over initiatives moving through some state houses that would hold doctors criminally liable for performing an abortion.
“What we have seen in the past is that these [abortion] bills come up really quickly without a whole lot of warning, so it’s difficult to say the specific legislation that we will see,” Ms. Tetlow said. “I am fairly confident that we will see at least one more vote in the House of Representatives and potentially one in the Senate ... before the 2018 elections.”
Maternal mortality could be symptomatic of another key issue in women’s health – an overall lack of access to adequate health care.
“One big issue is going to be how we get obstetrical care to women in communities where there is limited access,” she said. “We have got to figure out how to get all women, especially women in underserved areas who could be high risk into pregnancy care early on.”
Beyond that, ACOG is expecting that the women’s health services that have been in the cross hairs recently will continue to be so in 2018.
“2017 has been a year of just challenges and challenges and challenges for practicing ob.gyns. and patients, and we are expecting pretty much the same in 2018,” said Lucia DiVenere, a government and political affairs officer at ACOG.
Cuts to Medicaid, which House Speaker Paul Ryan (R-Wisc.) has identified as a key legislative priority for 2018, could create some significant issues for patients’ access to services.
“Roughly about 50% of deliveries are paid for by Medicaid,” Dr. Bohon said, noting that, for some states, that number can reach as high as 64%. “If those women don’t have access to care, it will be a disaster.”
The American Academy of Family Physicians will also be looking to maintain coverage of women’s health services in the Affordable Care Act.
“I think that our focus in 2018 is going to be around women’s continued access to comprehensive reproductive health care,” said AAFP President Michael Munger, MD. “Not only ensuring they have access to their breast, uterine, and cervical cancer screenings, prenatal maternity and postnatal care, but also preventive services.”
Dr. Munger singled out the Trump administration’s 2017 regulations allowing employers to opt out of providing contraception coverage for moral or religious reasons. “I think that is going to be a continued focus moving forward.”
“Three-quarters of women of childbearing age are in the workforce,” said Kandice Kapinos, PhD, of the Rand Corporation. “The studies on maternity leave show really positive effects of maternity leave on a wide range of child and maternal health outcomes.”
Not having an adequate amount of maternity leave can affect a woman’s ability to breastfeed her newborn, Dr. Kapinos added. “Breastfeeding can be difficult when you return to work,” she said. “Paid maternity leave would result in increases in breastfeeding. That has pretty big implications for health for women and children, which translates into pretty big cost savings.”
[email protected]
Addressing issues around maternal mortality is going to be the top focus for the American Congress of Obstetricians and Gynecologists in 2018.
“It is will be the priority of my presidency here at ACOG,” President-elect Lisa Hollier, MD, said in an interview. Her term as president begins at the end of April 2018.
Rates of maternal mortality – defined as rates of death within 365 days of pregnancy – have become an increasingly prominent issue in the United States. Many states have created dedicated committees to examine the causes of increasing mortality and look for solutions. California, in particular, has had some success in reducing these rates.
To address the maternal mortality issue, ACOG is working on passing legislation through Congress that would give the federal government a role in funding these state-level committees.
“The main crux of the bill is to provide authorization for state maternal mortality, for funds to support state maternal mortality review committees,” said Rachel Tetlow, the director of federal affairs at ACOG. “We know that while a majority of states do have committees, there are still some who are struggling to stand them up and others that are struggling to fund them at full capacity. This legislation looks to support those state efforts to ensure that states really are able to move forward with reviewing maternal deaths and in some cases near misses in their states and recommend local state-based solutions.”
Another hot button issue that could affect maternal mortality is access to abortion.
“It is going to be interesting to see how those numbers shift as abortion providers are no longer available,” said Constance J. Bohon, MD, an ob.gyn. in Washington, D.C., and the ACOG state legislative chair from the District of Columbia. “For example, there is a concern that in states such as Texas, the maternal mortality rates may rise because of a lack of abortion providers.”
Attacks on abortion rights at both the state and federal level are expected in the coming year as well, Dr. Bohon said. She also expressed concerns over initiatives moving through some state houses that would hold doctors criminally liable for performing an abortion.
“What we have seen in the past is that these [abortion] bills come up really quickly without a whole lot of warning, so it’s difficult to say the specific legislation that we will see,” Ms. Tetlow said. “I am fairly confident that we will see at least one more vote in the House of Representatives and potentially one in the Senate ... before the 2018 elections.”
Maternal mortality could be symptomatic of another key issue in women’s health – an overall lack of access to adequate health care.
“One big issue is going to be how we get obstetrical care to women in communities where there is limited access,” she said. “We have got to figure out how to get all women, especially women in underserved areas who could be high risk into pregnancy care early on.”
Beyond that, ACOG is expecting that the women’s health services that have been in the cross hairs recently will continue to be so in 2018.
“2017 has been a year of just challenges and challenges and challenges for practicing ob.gyns. and patients, and we are expecting pretty much the same in 2018,” said Lucia DiVenere, a government and political affairs officer at ACOG.
Cuts to Medicaid, which House Speaker Paul Ryan (R-Wisc.) has identified as a key legislative priority for 2018, could create some significant issues for patients’ access to services.
“Roughly about 50% of deliveries are paid for by Medicaid,” Dr. Bohon said, noting that, for some states, that number can reach as high as 64%. “If those women don’t have access to care, it will be a disaster.”
The American Academy of Family Physicians will also be looking to maintain coverage of women’s health services in the Affordable Care Act.
“I think that our focus in 2018 is going to be around women’s continued access to comprehensive reproductive health care,” said AAFP President Michael Munger, MD. “Not only ensuring they have access to their breast, uterine, and cervical cancer screenings, prenatal maternity and postnatal care, but also preventive services.”
Dr. Munger singled out the Trump administration’s 2017 regulations allowing employers to opt out of providing contraception coverage for moral or religious reasons. “I think that is going to be a continued focus moving forward.”
“Three-quarters of women of childbearing age are in the workforce,” said Kandice Kapinos, PhD, of the Rand Corporation. “The studies on maternity leave show really positive effects of maternity leave on a wide range of child and maternal health outcomes.”
Not having an adequate amount of maternity leave can affect a woman’s ability to breastfeed her newborn, Dr. Kapinos added. “Breastfeeding can be difficult when you return to work,” she said. “Paid maternity leave would result in increases in breastfeeding. That has pretty big implications for health for women and children, which translates into pretty big cost savings.”
[email protected]
Studies looking at pravastatin for preeclampsia prevention
In the United States, preeclampsia affects 3%-5% of all pregnancies and 10%-20% of pregnancies complicated by diabetes. Up to 20% of maternal deaths in the United States – and a much larger percentage of maternal deaths worldwide – occur in women with the condition, as do numerous maternal and fetal comorbidities. These include severe hypertension, pulmonary edema, stroke, and kidney and liver injury in the mother, and stillbirth, placental abruption, growth restriction, and premature delivery of the fetus.
Longer-term complications for the offspring include chronic lung disease, hearing and vision disorders, cerebral palsy and other neurodevelopmental disorders, and – as shown by more recent research – poor cardiovascular and metabolic outcomes.
Preeclampsia predisposes the mother to at least a twofold increased risk of future heart disease, compared with a woman who does not have the condition. In addition, women with preeclampsia who deliver at term are approximately two times more likely to die prematurely from heart disease than women without a history of preeclampsia, and those who deliver before 34 weeks’ gestation have been shown to have a ninefold greater risk of premature death. The American Heart Association, in fact, now includes preeclampsia in its list of heart disease risk factors.
Much attention now is focused on statins (inhibitors of HMG-CoA reductase), which have been used for more than 30 years for the primary and secondary prevention of heart disease. The properties and mechanisms of this class of drugs – and the similarities in the pathophysiology of cardiovascular disease and preeclampsia – make statins a plausible candidate for preeclampsia prevention. Thus far, data from preclinical work and subsequent pilot studies have been encouraging.
The commonalities
Preeclampsia is unique to pregnancy, but its pathophysiology and risk factors largely overlap with those of adult atherosclerotic cardiovascular disease. The exact pathophysiology of preeclampsia is unknown, but it is generally agreed that angiogenic imbalance and endothelial dysfunction play key roles, as do associated inflammation and oxidative stress.
Women with preeclampsia have been shown, for instance, to have had increased levels of antiangiogenic factors (soluble FMS-like tyrosine kinase 1 and soluble endoglin) and decreased levels of angiogenic factors (vascular endothelial growth factor and placental growth factor) prior to developing the condition clinically. Risk factors common to both preeclampsia and heart disease include chronic hypertension, dyslipidemia, diabetes or insulin resistance, obesity, and a family history of the condition.
Statins, meanwhile, have been shown to prevent or reverse angiogenic imbalance by promoting the release of vascular endothelial growth factor and placental growth factor and by suppressing the production of soluble FMS-like tyrosine kinase 1 and soluble endoglin. The drugs also improve vascular relaxation and exhibit anti-inflammatory and antioxidative effects, thereby broadly improving endovascular health. In the cardiovascular arena, notably, men and women who have elevated inflammatory markers even without hypercholesterolemia have been shown to have improved cardiovascular outcomes with statin treatment.
In various mouse models of preeclampsia studied in the past decade, pravastatin, a hydrophilic statin, has had beneficial effects. Mice with the angiogenic imbalance characteristic of preeclampsia that received this statin have shown a reversal of the imbalance, as well as reduced blood pressure, increased levels of nitric oxide synthase production, decreased oxidative stress, improved vascular reactivity, decreased kidney damage and proteinuria, and other positive effects. These effects occurred without detrimental outcomes to the mice or any increase in the rates of anomalies or resorption in offspring (Clin Obstet Gynecol. 2017 Mar;60:161-8).
Moreover, in addition to ameliorating the preeclampsia phenotype, pravastatin use in these animal models has improved pregnancy outcomes and reduced rates of pregnancy losses.
Safety issues
So, can we use statins in pregnancy? When statins were originally marketed in the 1980s, they were labeled pregnancy category X, which means 1) that there is evidence of fetal abnormalities or risk and 2) that these risks clearly outweigh potential benefits.
This designation for statins was based largely on the second half of the definition (no benefit to outweigh any risk). In addition, there were theoretical concerns about the inhibition of cholesterol synthesis during embryologic development and about a small case series of the original lipophilic statins suggesting an increased risk of malformations. While pregnancy category X does not exist anymore, statins are still labeled as contraindicated in pregnancy.
Pravastatin is one of the safest statins to consider in pregnancy for several reasons: It is one of the most hydrophilic statins and is a substrate of the placental efflux transporters, such as P-glycoprotein; both of those properties limit its ability to cross the placenta. It also has a short-elimination half-life, is cleared through both hepatic and renal routes, and is among the most hepatoselective statins available (one of the weakest inhibitors of HMG-CoA reductase). Indeed, in vitro placental transfer studies suggest that pravastatin transfer is limited and slow and that clearance is significantly higher in the fetal-to-maternal direction than in the maternal-to-fetal direction.
Animal studies have demonstrated that pravastatin is not teratogenic and has no effect on placental weight, pup birth weight, and pup adult weight. Moreover, at least six published cohort studies of women with first-trimester exposure to statins (women who had been prescribed the drugs before becoming pregnant and who received the drugs in the first trimester before realizing they were pregnant) showed no patterns or increased rates of congenital anomalies, compared with women without exposure to known teratogens. Additionally, these cohorts did not show any associations with miscarriage or fetal growth restriction (Obstet Gynecol. 2013 Feb;121:349-53).
A more recent cohort study of close to 900,000 women – of which 1,152 women used a statin (pravastatin or other statins) during their first trimester – similarly found no significant increases in any type of congenital malformation, compared with other completed pregnancies in the larger cohort. Notably, the analysis of this cohort was done using propensity score–based methods to control for potential confounders, including prepregnancy conditions that prompted use of a statin (BMJ. 2015;350:h1035).
A drawback to this body of research is that, with the exception of the BMJ study, the cohorts have been generally small; furthermore, in keeping with current recommendations, most of the statin-exposed patients discontinued use of the drugs upon confirmation of their pregnancies, thereby leaving the effects of long-term use unknown.
A promising pilot
Daily pravastatin use in pregnancy, starting in the second trimester, got its first major test of safety and pharmacokinetics in a pilot randomized, controlled trial undertaken by the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s (NICHD’s) Obstetric-Fetal Pharmacology Research Units Network. Women with singleton pregnancies and a history of severe preeclampsia requiring delivery prior to 34 weeks’ gestation were randomized between 12 and 16 weeks’ gestation to receive pravastatin or placebo until delivery.
This pilot is the first of three cohorts of women who were or will be randomized in separate pilot trials to escalating doses of pravastatin: 10 mg, 20 mg, and 40 mg (the last of which is the usual dose for lipid lowering in adults). Results of the first cohort, in which 20 patients were randomized to 10 mg pravastatin or placebo, were reported in 2016, and those from the second cohort will be reported soon. The third pilot is currently enrolling women.
In this first pilot we found no differences in rates of congenital anomalies or other identifiable maternal or fetal/neonatal safety risks, no differences in adverse events, and no maternal, fetal, or neonatal deaths. There were also no reports of myopathy/rhabdomyolysis or liver injury; the most common adverse events were heartburn (reported by four patients in the pravastatin group and three in the placebo group) and musculoskeletal pain (reported by four patients and one patient, respectively).
Although not statistically significant, a 10-mg dose of pravastatin was associated with favorable outcomes. None of the women receiving pravastatin developed preeclampsia, while four in the placebo group developed the disorder (with three of these four having severe preeclampsia).
Women in the pravastatin group also were less likely to have an indicated preterm delivery (one vs. five in the placebo group), and their neonates were less likely to be admitted to intermediate nurseries or the neonatal ICU. In addition, their angiogenic profiles were improved (higher placental growth factor and lower FMS-like tyrosine kinase 1 and soluble endoglin).
Importantly, while pravastatin reduced maternal cholesterol concentrations, there were no differences in birth weight or umbilical cord cholesterol concentrations (total cholesterol or LDL) between the two groups (Am J Obstet Gynecol. 2016;214[6]:720.e1-17).
That cholesterol concentrations were not reduced in fetuses exposed to pravastatin is reassuring and aligns with findings from other studies showing that fetal cholesterol concentrations are largely independent from maternal cholesterol concentrations or diet. For instance, we know from studies of Smith-Lemli-Opitz syndrome, a multiple congenital anomaly/intellectual disability syndrome caused by a defect in cholesterol synthesis, that there is not any significant interaction between cholesterol concentrations of the mother and fetus. Only about 10% of the fetal absolute cholesterol requirement comes from the mother, research has demonstrated.
The future
Infant follow-up in the NICHD study is planned, and a large, randomized clinical trial powered to look at the efficacy of pravastatin for preventing preeclampsia in high-risk women has been approved by the NICHD. Once funded, the study is expected to enroll approximately 1,700 pregnant women who have a history of severe preeclampsia and delivery before 36 weeks’ gestation and who are between 10 and 16 weeks’ gestation.
With continued research, we face the question of whether pravastatin may potentiate the benefit of aspirin in pregnant women. In cardiovascular medicine, there is evidence for additive or synergistic effects of the combined use of aspirin and statins.
Interestingly, a recent prospective cohort study of women with antiphospholipid syndrome and poor outcomes in prior pregnancies showed dramatic improvement in both maternal and fetal/neonatal outcomes when pravastatin was administered after the onset of preeclampsia or intrauterine growth restriction. All 21 women in the cohort were treated with low-dose aspirin and low-molecular-weight heparin; after the development of preeclampsia or intrauterine growth restriction, 10 patients were maintained on aspirin and LMWH, and 11 were started on 20 mg daily pravastatin along with the aspirin and LMWH (J Clin Invest. 2016 Aug;126[8]:2933-40; and J Clin Invest. 2016 Aug;126[8]:2792-4).
Those who received the statin had improved uterine artery Doppler velocimetry, lower systemic blood pressure, and delivered infants with higher birth weights and at a more advanced gestational age (median, 36 weeks’ vs. 26.5 weeks’ gestation). The study did not randomly allocate the women and did not include a placebo arm. Still, it is another impressive proof-of-concept study.
Dr. Costantine is an associate professor of obstetrics and gynecology at the University of Texas Medical Branch in Galveston. He reported that he has no financial disclosures.
In the United States, preeclampsia affects 3%-5% of all pregnancies and 10%-20% of pregnancies complicated by diabetes. Up to 20% of maternal deaths in the United States – and a much larger percentage of maternal deaths worldwide – occur in women with the condition, as do numerous maternal and fetal comorbidities. These include severe hypertension, pulmonary edema, stroke, and kidney and liver injury in the mother, and stillbirth, placental abruption, growth restriction, and premature delivery of the fetus.
Longer-term complications for the offspring include chronic lung disease, hearing and vision disorders, cerebral palsy and other neurodevelopmental disorders, and – as shown by more recent research – poor cardiovascular and metabolic outcomes.
Preeclampsia predisposes the mother to at least a twofold increased risk of future heart disease, compared with a woman who does not have the condition. In addition, women with preeclampsia who deliver at term are approximately two times more likely to die prematurely from heart disease than women without a history of preeclampsia, and those who deliver before 34 weeks’ gestation have been shown to have a ninefold greater risk of premature death. The American Heart Association, in fact, now includes preeclampsia in its list of heart disease risk factors.
Much attention now is focused on statins (inhibitors of HMG-CoA reductase), which have been used for more than 30 years for the primary and secondary prevention of heart disease. The properties and mechanisms of this class of drugs – and the similarities in the pathophysiology of cardiovascular disease and preeclampsia – make statins a plausible candidate for preeclampsia prevention. Thus far, data from preclinical work and subsequent pilot studies have been encouraging.
The commonalities
Preeclampsia is unique to pregnancy, but its pathophysiology and risk factors largely overlap with those of adult atherosclerotic cardiovascular disease. The exact pathophysiology of preeclampsia is unknown, but it is generally agreed that angiogenic imbalance and endothelial dysfunction play key roles, as do associated inflammation and oxidative stress.
Women with preeclampsia have been shown, for instance, to have had increased levels of antiangiogenic factors (soluble FMS-like tyrosine kinase 1 and soluble endoglin) and decreased levels of angiogenic factors (vascular endothelial growth factor and placental growth factor) prior to developing the condition clinically. Risk factors common to both preeclampsia and heart disease include chronic hypertension, dyslipidemia, diabetes or insulin resistance, obesity, and a family history of the condition.
Statins, meanwhile, have been shown to prevent or reverse angiogenic imbalance by promoting the release of vascular endothelial growth factor and placental growth factor and by suppressing the production of soluble FMS-like tyrosine kinase 1 and soluble endoglin. The drugs also improve vascular relaxation and exhibit anti-inflammatory and antioxidative effects, thereby broadly improving endovascular health. In the cardiovascular arena, notably, men and women who have elevated inflammatory markers even without hypercholesterolemia have been shown to have improved cardiovascular outcomes with statin treatment.
In various mouse models of preeclampsia studied in the past decade, pravastatin, a hydrophilic statin, has had beneficial effects. Mice with the angiogenic imbalance characteristic of preeclampsia that received this statin have shown a reversal of the imbalance, as well as reduced blood pressure, increased levels of nitric oxide synthase production, decreased oxidative stress, improved vascular reactivity, decreased kidney damage and proteinuria, and other positive effects. These effects occurred without detrimental outcomes to the mice or any increase in the rates of anomalies or resorption in offspring (Clin Obstet Gynecol. 2017 Mar;60:161-8).
Moreover, in addition to ameliorating the preeclampsia phenotype, pravastatin use in these animal models has improved pregnancy outcomes and reduced rates of pregnancy losses.
Safety issues
So, can we use statins in pregnancy? When statins were originally marketed in the 1980s, they were labeled pregnancy category X, which means 1) that there is evidence of fetal abnormalities or risk and 2) that these risks clearly outweigh potential benefits.
This designation for statins was based largely on the second half of the definition (no benefit to outweigh any risk). In addition, there were theoretical concerns about the inhibition of cholesterol synthesis during embryologic development and about a small case series of the original lipophilic statins suggesting an increased risk of malformations. While pregnancy category X does not exist anymore, statins are still labeled as contraindicated in pregnancy.
Pravastatin is one of the safest statins to consider in pregnancy for several reasons: It is one of the most hydrophilic statins and is a substrate of the placental efflux transporters, such as P-glycoprotein; both of those properties limit its ability to cross the placenta. It also has a short-elimination half-life, is cleared through both hepatic and renal routes, and is among the most hepatoselective statins available (one of the weakest inhibitors of HMG-CoA reductase). Indeed, in vitro placental transfer studies suggest that pravastatin transfer is limited and slow and that clearance is significantly higher in the fetal-to-maternal direction than in the maternal-to-fetal direction.
Animal studies have demonstrated that pravastatin is not teratogenic and has no effect on placental weight, pup birth weight, and pup adult weight. Moreover, at least six published cohort studies of women with first-trimester exposure to statins (women who had been prescribed the drugs before becoming pregnant and who received the drugs in the first trimester before realizing they were pregnant) showed no patterns or increased rates of congenital anomalies, compared with women without exposure to known teratogens. Additionally, these cohorts did not show any associations with miscarriage or fetal growth restriction (Obstet Gynecol. 2013 Feb;121:349-53).
A more recent cohort study of close to 900,000 women – of which 1,152 women used a statin (pravastatin or other statins) during their first trimester – similarly found no significant increases in any type of congenital malformation, compared with other completed pregnancies in the larger cohort. Notably, the analysis of this cohort was done using propensity score–based methods to control for potential confounders, including prepregnancy conditions that prompted use of a statin (BMJ. 2015;350:h1035).
A drawback to this body of research is that, with the exception of the BMJ study, the cohorts have been generally small; furthermore, in keeping with current recommendations, most of the statin-exposed patients discontinued use of the drugs upon confirmation of their pregnancies, thereby leaving the effects of long-term use unknown.
A promising pilot
Daily pravastatin use in pregnancy, starting in the second trimester, got its first major test of safety and pharmacokinetics in a pilot randomized, controlled trial undertaken by the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s (NICHD’s) Obstetric-Fetal Pharmacology Research Units Network. Women with singleton pregnancies and a history of severe preeclampsia requiring delivery prior to 34 weeks’ gestation were randomized between 12 and 16 weeks’ gestation to receive pravastatin or placebo until delivery.
This pilot is the first of three cohorts of women who were or will be randomized in separate pilot trials to escalating doses of pravastatin: 10 mg, 20 mg, and 40 mg (the last of which is the usual dose for lipid lowering in adults). Results of the first cohort, in which 20 patients were randomized to 10 mg pravastatin or placebo, were reported in 2016, and those from the second cohort will be reported soon. The third pilot is currently enrolling women.
In this first pilot we found no differences in rates of congenital anomalies or other identifiable maternal or fetal/neonatal safety risks, no differences in adverse events, and no maternal, fetal, or neonatal deaths. There were also no reports of myopathy/rhabdomyolysis or liver injury; the most common adverse events were heartburn (reported by four patients in the pravastatin group and three in the placebo group) and musculoskeletal pain (reported by four patients and one patient, respectively).
Although not statistically significant, a 10-mg dose of pravastatin was associated with favorable outcomes. None of the women receiving pravastatin developed preeclampsia, while four in the placebo group developed the disorder (with three of these four having severe preeclampsia).
Women in the pravastatin group also were less likely to have an indicated preterm delivery (one vs. five in the placebo group), and their neonates were less likely to be admitted to intermediate nurseries or the neonatal ICU. In addition, their angiogenic profiles were improved (higher placental growth factor and lower FMS-like tyrosine kinase 1 and soluble endoglin).
Importantly, while pravastatin reduced maternal cholesterol concentrations, there were no differences in birth weight or umbilical cord cholesterol concentrations (total cholesterol or LDL) between the two groups (Am J Obstet Gynecol. 2016;214[6]:720.e1-17).
That cholesterol concentrations were not reduced in fetuses exposed to pravastatin is reassuring and aligns with findings from other studies showing that fetal cholesterol concentrations are largely independent from maternal cholesterol concentrations or diet. For instance, we know from studies of Smith-Lemli-Opitz syndrome, a multiple congenital anomaly/intellectual disability syndrome caused by a defect in cholesterol synthesis, that there is not any significant interaction between cholesterol concentrations of the mother and fetus. Only about 10% of the fetal absolute cholesterol requirement comes from the mother, research has demonstrated.
The future
Infant follow-up in the NICHD study is planned, and a large, randomized clinical trial powered to look at the efficacy of pravastatin for preventing preeclampsia in high-risk women has been approved by the NICHD. Once funded, the study is expected to enroll approximately 1,700 pregnant women who have a history of severe preeclampsia and delivery before 36 weeks’ gestation and who are between 10 and 16 weeks’ gestation.
With continued research, we face the question of whether pravastatin may potentiate the benefit of aspirin in pregnant women. In cardiovascular medicine, there is evidence for additive or synergistic effects of the combined use of aspirin and statins.
Interestingly, a recent prospective cohort study of women with antiphospholipid syndrome and poor outcomes in prior pregnancies showed dramatic improvement in both maternal and fetal/neonatal outcomes when pravastatin was administered after the onset of preeclampsia or intrauterine growth restriction. All 21 women in the cohort were treated with low-dose aspirin and low-molecular-weight heparin; after the development of preeclampsia or intrauterine growth restriction, 10 patients were maintained on aspirin and LMWH, and 11 were started on 20 mg daily pravastatin along with the aspirin and LMWH (J Clin Invest. 2016 Aug;126[8]:2933-40; and J Clin Invest. 2016 Aug;126[8]:2792-4).
Those who received the statin had improved uterine artery Doppler velocimetry, lower systemic blood pressure, and delivered infants with higher birth weights and at a more advanced gestational age (median, 36 weeks’ vs. 26.5 weeks’ gestation). The study did not randomly allocate the women and did not include a placebo arm. Still, it is another impressive proof-of-concept study.
Dr. Costantine is an associate professor of obstetrics and gynecology at the University of Texas Medical Branch in Galveston. He reported that he has no financial disclosures.
In the United States, preeclampsia affects 3%-5% of all pregnancies and 10%-20% of pregnancies complicated by diabetes. Up to 20% of maternal deaths in the United States – and a much larger percentage of maternal deaths worldwide – occur in women with the condition, as do numerous maternal and fetal comorbidities. These include severe hypertension, pulmonary edema, stroke, and kidney and liver injury in the mother, and stillbirth, placental abruption, growth restriction, and premature delivery of the fetus.
Longer-term complications for the offspring include chronic lung disease, hearing and vision disorders, cerebral palsy and other neurodevelopmental disorders, and – as shown by more recent research – poor cardiovascular and metabolic outcomes.
Preeclampsia predisposes the mother to at least a twofold increased risk of future heart disease, compared with a woman who does not have the condition. In addition, women with preeclampsia who deliver at term are approximately two times more likely to die prematurely from heart disease than women without a history of preeclampsia, and those who deliver before 34 weeks’ gestation have been shown to have a ninefold greater risk of premature death. The American Heart Association, in fact, now includes preeclampsia in its list of heart disease risk factors.
Much attention now is focused on statins (inhibitors of HMG-CoA reductase), which have been used for more than 30 years for the primary and secondary prevention of heart disease. The properties and mechanisms of this class of drugs – and the similarities in the pathophysiology of cardiovascular disease and preeclampsia – make statins a plausible candidate for preeclampsia prevention. Thus far, data from preclinical work and subsequent pilot studies have been encouraging.
The commonalities
Preeclampsia is unique to pregnancy, but its pathophysiology and risk factors largely overlap with those of adult atherosclerotic cardiovascular disease. The exact pathophysiology of preeclampsia is unknown, but it is generally agreed that angiogenic imbalance and endothelial dysfunction play key roles, as do associated inflammation and oxidative stress.
Women with preeclampsia have been shown, for instance, to have had increased levels of antiangiogenic factors (soluble FMS-like tyrosine kinase 1 and soluble endoglin) and decreased levels of angiogenic factors (vascular endothelial growth factor and placental growth factor) prior to developing the condition clinically. Risk factors common to both preeclampsia and heart disease include chronic hypertension, dyslipidemia, diabetes or insulin resistance, obesity, and a family history of the condition.
Statins, meanwhile, have been shown to prevent or reverse angiogenic imbalance by promoting the release of vascular endothelial growth factor and placental growth factor and by suppressing the production of soluble FMS-like tyrosine kinase 1 and soluble endoglin. The drugs also improve vascular relaxation and exhibit anti-inflammatory and antioxidative effects, thereby broadly improving endovascular health. In the cardiovascular arena, notably, men and women who have elevated inflammatory markers even without hypercholesterolemia have been shown to have improved cardiovascular outcomes with statin treatment.
In various mouse models of preeclampsia studied in the past decade, pravastatin, a hydrophilic statin, has had beneficial effects. Mice with the angiogenic imbalance characteristic of preeclampsia that received this statin have shown a reversal of the imbalance, as well as reduced blood pressure, increased levels of nitric oxide synthase production, decreased oxidative stress, improved vascular reactivity, decreased kidney damage and proteinuria, and other positive effects. These effects occurred without detrimental outcomes to the mice or any increase in the rates of anomalies or resorption in offspring (Clin Obstet Gynecol. 2017 Mar;60:161-8).
Moreover, in addition to ameliorating the preeclampsia phenotype, pravastatin use in these animal models has improved pregnancy outcomes and reduced rates of pregnancy losses.
Safety issues
So, can we use statins in pregnancy? When statins were originally marketed in the 1980s, they were labeled pregnancy category X, which means 1) that there is evidence of fetal abnormalities or risk and 2) that these risks clearly outweigh potential benefits.
This designation for statins was based largely on the second half of the definition (no benefit to outweigh any risk). In addition, there were theoretical concerns about the inhibition of cholesterol synthesis during embryologic development and about a small case series of the original lipophilic statins suggesting an increased risk of malformations. While pregnancy category X does not exist anymore, statins are still labeled as contraindicated in pregnancy.
Pravastatin is one of the safest statins to consider in pregnancy for several reasons: It is one of the most hydrophilic statins and is a substrate of the placental efflux transporters, such as P-glycoprotein; both of those properties limit its ability to cross the placenta. It also has a short-elimination half-life, is cleared through both hepatic and renal routes, and is among the most hepatoselective statins available (one of the weakest inhibitors of HMG-CoA reductase). Indeed, in vitro placental transfer studies suggest that pravastatin transfer is limited and slow and that clearance is significantly higher in the fetal-to-maternal direction than in the maternal-to-fetal direction.
Animal studies have demonstrated that pravastatin is not teratogenic and has no effect on placental weight, pup birth weight, and pup adult weight. Moreover, at least six published cohort studies of women with first-trimester exposure to statins (women who had been prescribed the drugs before becoming pregnant and who received the drugs in the first trimester before realizing they were pregnant) showed no patterns or increased rates of congenital anomalies, compared with women without exposure to known teratogens. Additionally, these cohorts did not show any associations with miscarriage or fetal growth restriction (Obstet Gynecol. 2013 Feb;121:349-53).
A more recent cohort study of close to 900,000 women – of which 1,152 women used a statin (pravastatin or other statins) during their first trimester – similarly found no significant increases in any type of congenital malformation, compared with other completed pregnancies in the larger cohort. Notably, the analysis of this cohort was done using propensity score–based methods to control for potential confounders, including prepregnancy conditions that prompted use of a statin (BMJ. 2015;350:h1035).
A drawback to this body of research is that, with the exception of the BMJ study, the cohorts have been generally small; furthermore, in keeping with current recommendations, most of the statin-exposed patients discontinued use of the drugs upon confirmation of their pregnancies, thereby leaving the effects of long-term use unknown.
A promising pilot
Daily pravastatin use in pregnancy, starting in the second trimester, got its first major test of safety and pharmacokinetics in a pilot randomized, controlled trial undertaken by the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s (NICHD’s) Obstetric-Fetal Pharmacology Research Units Network. Women with singleton pregnancies and a history of severe preeclampsia requiring delivery prior to 34 weeks’ gestation were randomized between 12 and 16 weeks’ gestation to receive pravastatin or placebo until delivery.
This pilot is the first of three cohorts of women who were or will be randomized in separate pilot trials to escalating doses of pravastatin: 10 mg, 20 mg, and 40 mg (the last of which is the usual dose for lipid lowering in adults). Results of the first cohort, in which 20 patients were randomized to 10 mg pravastatin or placebo, were reported in 2016, and those from the second cohort will be reported soon. The third pilot is currently enrolling women.
In this first pilot we found no differences in rates of congenital anomalies or other identifiable maternal or fetal/neonatal safety risks, no differences in adverse events, and no maternal, fetal, or neonatal deaths. There were also no reports of myopathy/rhabdomyolysis or liver injury; the most common adverse events were heartburn (reported by four patients in the pravastatin group and three in the placebo group) and musculoskeletal pain (reported by four patients and one patient, respectively).
Although not statistically significant, a 10-mg dose of pravastatin was associated with favorable outcomes. None of the women receiving pravastatin developed preeclampsia, while four in the placebo group developed the disorder (with three of these four having severe preeclampsia).
Women in the pravastatin group also were less likely to have an indicated preterm delivery (one vs. five in the placebo group), and their neonates were less likely to be admitted to intermediate nurseries or the neonatal ICU. In addition, their angiogenic profiles were improved (higher placental growth factor and lower FMS-like tyrosine kinase 1 and soluble endoglin).
Importantly, while pravastatin reduced maternal cholesterol concentrations, there were no differences in birth weight or umbilical cord cholesterol concentrations (total cholesterol or LDL) between the two groups (Am J Obstet Gynecol. 2016;214[6]:720.e1-17).
That cholesterol concentrations were not reduced in fetuses exposed to pravastatin is reassuring and aligns with findings from other studies showing that fetal cholesterol concentrations are largely independent from maternal cholesterol concentrations or diet. For instance, we know from studies of Smith-Lemli-Opitz syndrome, a multiple congenital anomaly/intellectual disability syndrome caused by a defect in cholesterol synthesis, that there is not any significant interaction between cholesterol concentrations of the mother and fetus. Only about 10% of the fetal absolute cholesterol requirement comes from the mother, research has demonstrated.
The future
Infant follow-up in the NICHD study is planned, and a large, randomized clinical trial powered to look at the efficacy of pravastatin for preventing preeclampsia in high-risk women has been approved by the NICHD. Once funded, the study is expected to enroll approximately 1,700 pregnant women who have a history of severe preeclampsia and delivery before 36 weeks’ gestation and who are between 10 and 16 weeks’ gestation.
With continued research, we face the question of whether pravastatin may potentiate the benefit of aspirin in pregnant women. In cardiovascular medicine, there is evidence for additive or synergistic effects of the combined use of aspirin and statins.
Interestingly, a recent prospective cohort study of women with antiphospholipid syndrome and poor outcomes in prior pregnancies showed dramatic improvement in both maternal and fetal/neonatal outcomes when pravastatin was administered after the onset of preeclampsia or intrauterine growth restriction. All 21 women in the cohort were treated with low-dose aspirin and low-molecular-weight heparin; after the development of preeclampsia or intrauterine growth restriction, 10 patients were maintained on aspirin and LMWH, and 11 were started on 20 mg daily pravastatin along with the aspirin and LMWH (J Clin Invest. 2016 Aug;126[8]:2933-40; and J Clin Invest. 2016 Aug;126[8]:2792-4).
Those who received the statin had improved uterine artery Doppler velocimetry, lower systemic blood pressure, and delivered infants with higher birth weights and at a more advanced gestational age (median, 36 weeks’ vs. 26.5 weeks’ gestation). The study did not randomly allocate the women and did not include a placebo arm. Still, it is another impressive proof-of-concept study.
Dr. Costantine is an associate professor of obstetrics and gynecology at the University of Texas Medical Branch in Galveston. He reported that he has no financial disclosures.