User login
Neuropsychiatric outcomes similar for hospitalized COVID-19 patients and non–COVID-19 patients
Hospitalized COVID-19 survivors showed greater cognitive impairment 6 months later, compared with patients hospitalized for other causes, but the overall disease burden was similar, based on data from 85 adults with COVID-19.
Previous studies have shown that cognitive and neuropsychiatric symptoms can occur from 2-6 months after COVID-19 recovery, and such symptoms are known to be associated with hospitalization for other severe medical conditions, Vardan Nersesjan, MD, of Copenhagen University Hospital, and colleagues wrote.
However, it remains unknown if COVID-19 is associated with a unique pattern of cognitive and mental impairment compared with other similarly severe medical conditions, they said.
In a study published in JAMA Psychiatry (2022 Mar 23. doi: 10.1001/jamapsychiatry.2022.0284), the researchers identified 85 adult COVID-19 survivors and 61 controls with non-COVID medical conditions who were treated and released between July 2020 and July 2021. The COVID-19 patients and controls were matched for age, sex, and ICU status. Cognitive impairment was assessed using the Mini-International Neuropsychiatric Interview, the Montreal Cognitive Assessment (MoCA), neurologic examination, and a semistructured interview to determine subjective symptoms.
The primary outcomes were the total scores on the MoCA and any new-onset psychiatric diagnoses. Secondary outcomes included specific psychiatric diagnoses such as depression, neurologic examination findings, and self-reported neuropsychiatric and cognitive symptoms. The mean age of the COVID-19 patients was 56.8 years, and 42% were women.
At 6 months’ follow-up, cognitive status was significantly lower in COVID-19 survivors, compared with controls, based on total geometric mean MoCA scores (26.7 vs. 27.5, P = .01). However, cognitive status improved significantly from 19.2 at hospital discharge to 26.1 at 6 months in 15 of the COVID-19 patients (P = .004), the researchers noted.
New-onset psychiatric diagnoses occurred in 16 COVID-19 patients and 12 of the controls (19% vs. 20%); this difference was not significant.
Secondary outcomes were not significantly different at 6 months between the groups, with the exception of anosmia, which was significantly more common in the COVID-19 patients; however, the significance disappeared in adjusted analysis, the researchers said.
The study findings were limited by several factors including the inability to prove causality because of the case-control feature and by the inability to detect small differences in neuropsychiatric outcomes, the researchers noted.
However, the results were strengthened by the use of a prospectively matched control group with similar disease severity admitted to the same hospital in the same time frame. Although the overall burden of neuropsychiatric and neurologic symptoms and diagnoses appeared similar in COVID-19 patients and those with other medical conditions, more research in larger populations is needed to determine smaller differences in neuropsychiatric profiles, the researchers noted.
Study fills research gap
The study is important at this time because, although prolonged neuropsychiatric and cognitive symptoms have been reported after COVID-19, the field lacked prospective case-control studies with well-matched controls to investigate whether these outcomes differed from those seen in other critical illnesses that had also required hospitalization, corresponding author Michael E. Benros, MD, of the Mental Health Center, Copenhagen, said in an interview.
“I was surprised that there was a significant worse cognitive functioning among COVID-19 patients 6 months after symptom onset also when compared to this well-matched control group that had been hospitalized for non–COVID-19 illness, although the absolute difference between the groups in cognition score were small,” said Dr. Benros. “Another notable finding is the large improvement in cognitive functioning from discharge to follow-up,” he added on behalf of himself and fellow corresponding author Daniel Kondziella, MD.
The study results show that cognitive function affected by COVID-19 and critical illness as observed at discharge showed a substantial improvement at 6 months after symptom onset, said Dr. Benros. “However, the cognitive function was significantly worse among severely ill COVID-19 patients 6 months after symptom onset when compared to a matched control group of individuals hospitalized for non–COVID-19 illness, although this difference in cognitive function was rather small in absolute numbers, and smaller than what had been suggested by other studies that lacked control groups. Strikingly, neuropsychiatric disorders were similar across the two groups, which was also the case when looking at neuropsychiatric symptoms.
“Larger prospective case-control studies of neuropsychiatric and cognitive functioning after COVID-19, compared with matched controls are still needed to detect smaller differences, and more detailed cognitive domains, and with longer follow-up time, which we are currently conducting,” Dr. Benros said.
Controlled studies will help planning
“Lingering neuropsychiatric complications are common after COVID-19, but only controlled studies can tell us whether these complications are specific to COVID-19, rather than a general effect of having been medically ill,” Alasdair G. Rooney, MRCPsych MD PhD, of the University of Edinburgh, said in an interview. “The answer matters ultimately because COVID-19 is a new disease; societies and health care services need to be able to plan for its specific consequences.”
The health status of the control group is important as well. “Most previous studies had compared COVID-19 survivors against healthy controls or patients from a historical database. This new study compared COVID-19 survivors against those hospitalized for other medical causes over the same period,” Dr. Rooney said. “This is a more stringent test of whether COVID-19 has specific neurocognitive and neuropsychiatric consequences.
“The study found that new-onset neuropsychiatric diagnoses and symptoms were no more likely to occur after COVID-19 than after similarly severe medical illnesses,” Dr. Rooney said. “This negative finding runs counter to some earlier studies and may surprise some.” The findings need to be replicated in larger samples, but the current study shows the importance of prospectively recruiting active controls.
“In a subgroup analysis, some patients showed good improvement in cognitive scores between discharge and follow-up. While unsurprising, this is encouraging and suggests that the early postdischarge months are an important time for neurocognitive recovery,” Dr. Rooney noted.
“The findings suggest that COVID-19 may impair attention more selectively than other medical causes of hospitalization. COVID-19 survivors may also be at higher risk of significant overall cognitive impairment than survivors of similarly severe medical illnesses, after a similar duration,” said Dr. Rooney. “If the results are replicated by other prospective studies, they would suggest that there is something about COVID-19 that causes clinically significant neurocognitive difficulties in a minority of survivors.
“Larger well-controlled studies are required, with longer follow-up and more detailed neurocognitive testing,” as the duration of impairment and scope for further recovery are not known, Dr. Rooney added. Also unknown is whether COVID-19 affects attention permanently, or whether recovery is simply slower after COVID-19 compared to other medical illnesses.
“Knowing who is at the greatest risk of severe cognitive impairment after COVID-19 is important and likely to allow tailoring of more effective shielding strategies,” said Dr. Rooney. “This study was conducted before the widespread availability of vaccines for COVID-19. Long-term neuropsychiatric outcomes in vaccinated patients remain largely unknown. Arguably, these are now more important to understand, as future COVID-19 waves will occur mainly among vaccinated individuals.”
The study was supported by the Lundbeck Foundation and the Novo Nordisk Foundation. Lead author Dr. Nersesjan had no financial conflicts to disclose. Dr. Benros reported grants from Lundbeck Foundation and Novo Nordisk Foundation during the conduct of the study. Dr. Rooney had no financial conflicts to disclose.
This article was updated 3/25/22.
Hospitalized COVID-19 survivors showed greater cognitive impairment 6 months later, compared with patients hospitalized for other causes, but the overall disease burden was similar, based on data from 85 adults with COVID-19.
Previous studies have shown that cognitive and neuropsychiatric symptoms can occur from 2-6 months after COVID-19 recovery, and such symptoms are known to be associated with hospitalization for other severe medical conditions, Vardan Nersesjan, MD, of Copenhagen University Hospital, and colleagues wrote.
However, it remains unknown if COVID-19 is associated with a unique pattern of cognitive and mental impairment compared with other similarly severe medical conditions, they said.
In a study published in JAMA Psychiatry (2022 Mar 23. doi: 10.1001/jamapsychiatry.2022.0284), the researchers identified 85 adult COVID-19 survivors and 61 controls with non-COVID medical conditions who were treated and released between July 2020 and July 2021. The COVID-19 patients and controls were matched for age, sex, and ICU status. Cognitive impairment was assessed using the Mini-International Neuropsychiatric Interview, the Montreal Cognitive Assessment (MoCA), neurologic examination, and a semistructured interview to determine subjective symptoms.
The primary outcomes were the total scores on the MoCA and any new-onset psychiatric diagnoses. Secondary outcomes included specific psychiatric diagnoses such as depression, neurologic examination findings, and self-reported neuropsychiatric and cognitive symptoms. The mean age of the COVID-19 patients was 56.8 years, and 42% were women.
At 6 months’ follow-up, cognitive status was significantly lower in COVID-19 survivors, compared with controls, based on total geometric mean MoCA scores (26.7 vs. 27.5, P = .01). However, cognitive status improved significantly from 19.2 at hospital discharge to 26.1 at 6 months in 15 of the COVID-19 patients (P = .004), the researchers noted.
New-onset psychiatric diagnoses occurred in 16 COVID-19 patients and 12 of the controls (19% vs. 20%); this difference was not significant.
Secondary outcomes were not significantly different at 6 months between the groups, with the exception of anosmia, which was significantly more common in the COVID-19 patients; however, the significance disappeared in adjusted analysis, the researchers said.
The study findings were limited by several factors including the inability to prove causality because of the case-control feature and by the inability to detect small differences in neuropsychiatric outcomes, the researchers noted.
However, the results were strengthened by the use of a prospectively matched control group with similar disease severity admitted to the same hospital in the same time frame. Although the overall burden of neuropsychiatric and neurologic symptoms and diagnoses appeared similar in COVID-19 patients and those with other medical conditions, more research in larger populations is needed to determine smaller differences in neuropsychiatric profiles, the researchers noted.
Study fills research gap
The study is important at this time because, although prolonged neuropsychiatric and cognitive symptoms have been reported after COVID-19, the field lacked prospective case-control studies with well-matched controls to investigate whether these outcomes differed from those seen in other critical illnesses that had also required hospitalization, corresponding author Michael E. Benros, MD, of the Mental Health Center, Copenhagen, said in an interview.
“I was surprised that there was a significant worse cognitive functioning among COVID-19 patients 6 months after symptom onset also when compared to this well-matched control group that had been hospitalized for non–COVID-19 illness, although the absolute difference between the groups in cognition score were small,” said Dr. Benros. “Another notable finding is the large improvement in cognitive functioning from discharge to follow-up,” he added on behalf of himself and fellow corresponding author Daniel Kondziella, MD.
The study results show that cognitive function affected by COVID-19 and critical illness as observed at discharge showed a substantial improvement at 6 months after symptom onset, said Dr. Benros. “However, the cognitive function was significantly worse among severely ill COVID-19 patients 6 months after symptom onset when compared to a matched control group of individuals hospitalized for non–COVID-19 illness, although this difference in cognitive function was rather small in absolute numbers, and smaller than what had been suggested by other studies that lacked control groups. Strikingly, neuropsychiatric disorders were similar across the two groups, which was also the case when looking at neuropsychiatric symptoms.
“Larger prospective case-control studies of neuropsychiatric and cognitive functioning after COVID-19, compared with matched controls are still needed to detect smaller differences, and more detailed cognitive domains, and with longer follow-up time, which we are currently conducting,” Dr. Benros said.
Controlled studies will help planning
“Lingering neuropsychiatric complications are common after COVID-19, but only controlled studies can tell us whether these complications are specific to COVID-19, rather than a general effect of having been medically ill,” Alasdair G. Rooney, MRCPsych MD PhD, of the University of Edinburgh, said in an interview. “The answer matters ultimately because COVID-19 is a new disease; societies and health care services need to be able to plan for its specific consequences.”
The health status of the control group is important as well. “Most previous studies had compared COVID-19 survivors against healthy controls or patients from a historical database. This new study compared COVID-19 survivors against those hospitalized for other medical causes over the same period,” Dr. Rooney said. “This is a more stringent test of whether COVID-19 has specific neurocognitive and neuropsychiatric consequences.
“The study found that new-onset neuropsychiatric diagnoses and symptoms were no more likely to occur after COVID-19 than after similarly severe medical illnesses,” Dr. Rooney said. “This negative finding runs counter to some earlier studies and may surprise some.” The findings need to be replicated in larger samples, but the current study shows the importance of prospectively recruiting active controls.
“In a subgroup analysis, some patients showed good improvement in cognitive scores between discharge and follow-up. While unsurprising, this is encouraging and suggests that the early postdischarge months are an important time for neurocognitive recovery,” Dr. Rooney noted.
“The findings suggest that COVID-19 may impair attention more selectively than other medical causes of hospitalization. COVID-19 survivors may also be at higher risk of significant overall cognitive impairment than survivors of similarly severe medical illnesses, after a similar duration,” said Dr. Rooney. “If the results are replicated by other prospective studies, they would suggest that there is something about COVID-19 that causes clinically significant neurocognitive difficulties in a minority of survivors.
“Larger well-controlled studies are required, with longer follow-up and more detailed neurocognitive testing,” as the duration of impairment and scope for further recovery are not known, Dr. Rooney added. Also unknown is whether COVID-19 affects attention permanently, or whether recovery is simply slower after COVID-19 compared to other medical illnesses.
“Knowing who is at the greatest risk of severe cognitive impairment after COVID-19 is important and likely to allow tailoring of more effective shielding strategies,” said Dr. Rooney. “This study was conducted before the widespread availability of vaccines for COVID-19. Long-term neuropsychiatric outcomes in vaccinated patients remain largely unknown. Arguably, these are now more important to understand, as future COVID-19 waves will occur mainly among vaccinated individuals.”
The study was supported by the Lundbeck Foundation and the Novo Nordisk Foundation. Lead author Dr. Nersesjan had no financial conflicts to disclose. Dr. Benros reported grants from Lundbeck Foundation and Novo Nordisk Foundation during the conduct of the study. Dr. Rooney had no financial conflicts to disclose.
This article was updated 3/25/22.
Hospitalized COVID-19 survivors showed greater cognitive impairment 6 months later, compared with patients hospitalized for other causes, but the overall disease burden was similar, based on data from 85 adults with COVID-19.
Previous studies have shown that cognitive and neuropsychiatric symptoms can occur from 2-6 months after COVID-19 recovery, and such symptoms are known to be associated with hospitalization for other severe medical conditions, Vardan Nersesjan, MD, of Copenhagen University Hospital, and colleagues wrote.
However, it remains unknown if COVID-19 is associated with a unique pattern of cognitive and mental impairment compared with other similarly severe medical conditions, they said.
In a study published in JAMA Psychiatry (2022 Mar 23. doi: 10.1001/jamapsychiatry.2022.0284), the researchers identified 85 adult COVID-19 survivors and 61 controls with non-COVID medical conditions who were treated and released between July 2020 and July 2021. The COVID-19 patients and controls were matched for age, sex, and ICU status. Cognitive impairment was assessed using the Mini-International Neuropsychiatric Interview, the Montreal Cognitive Assessment (MoCA), neurologic examination, and a semistructured interview to determine subjective symptoms.
The primary outcomes were the total scores on the MoCA and any new-onset psychiatric diagnoses. Secondary outcomes included specific psychiatric diagnoses such as depression, neurologic examination findings, and self-reported neuropsychiatric and cognitive symptoms. The mean age of the COVID-19 patients was 56.8 years, and 42% were women.
At 6 months’ follow-up, cognitive status was significantly lower in COVID-19 survivors, compared with controls, based on total geometric mean MoCA scores (26.7 vs. 27.5, P = .01). However, cognitive status improved significantly from 19.2 at hospital discharge to 26.1 at 6 months in 15 of the COVID-19 patients (P = .004), the researchers noted.
New-onset psychiatric diagnoses occurred in 16 COVID-19 patients and 12 of the controls (19% vs. 20%); this difference was not significant.
Secondary outcomes were not significantly different at 6 months between the groups, with the exception of anosmia, which was significantly more common in the COVID-19 patients; however, the significance disappeared in adjusted analysis, the researchers said.
The study findings were limited by several factors including the inability to prove causality because of the case-control feature and by the inability to detect small differences in neuropsychiatric outcomes, the researchers noted.
However, the results were strengthened by the use of a prospectively matched control group with similar disease severity admitted to the same hospital in the same time frame. Although the overall burden of neuropsychiatric and neurologic symptoms and diagnoses appeared similar in COVID-19 patients and those with other medical conditions, more research in larger populations is needed to determine smaller differences in neuropsychiatric profiles, the researchers noted.
Study fills research gap
The study is important at this time because, although prolonged neuropsychiatric and cognitive symptoms have been reported after COVID-19, the field lacked prospective case-control studies with well-matched controls to investigate whether these outcomes differed from those seen in other critical illnesses that had also required hospitalization, corresponding author Michael E. Benros, MD, of the Mental Health Center, Copenhagen, said in an interview.
“I was surprised that there was a significant worse cognitive functioning among COVID-19 patients 6 months after symptom onset also when compared to this well-matched control group that had been hospitalized for non–COVID-19 illness, although the absolute difference between the groups in cognition score were small,” said Dr. Benros. “Another notable finding is the large improvement in cognitive functioning from discharge to follow-up,” he added on behalf of himself and fellow corresponding author Daniel Kondziella, MD.
The study results show that cognitive function affected by COVID-19 and critical illness as observed at discharge showed a substantial improvement at 6 months after symptom onset, said Dr. Benros. “However, the cognitive function was significantly worse among severely ill COVID-19 patients 6 months after symptom onset when compared to a matched control group of individuals hospitalized for non–COVID-19 illness, although this difference in cognitive function was rather small in absolute numbers, and smaller than what had been suggested by other studies that lacked control groups. Strikingly, neuropsychiatric disorders were similar across the two groups, which was also the case when looking at neuropsychiatric symptoms.
“Larger prospective case-control studies of neuropsychiatric and cognitive functioning after COVID-19, compared with matched controls are still needed to detect smaller differences, and more detailed cognitive domains, and with longer follow-up time, which we are currently conducting,” Dr. Benros said.
Controlled studies will help planning
“Lingering neuropsychiatric complications are common after COVID-19, but only controlled studies can tell us whether these complications are specific to COVID-19, rather than a general effect of having been medically ill,” Alasdair G. Rooney, MRCPsych MD PhD, of the University of Edinburgh, said in an interview. “The answer matters ultimately because COVID-19 is a new disease; societies and health care services need to be able to plan for its specific consequences.”
The health status of the control group is important as well. “Most previous studies had compared COVID-19 survivors against healthy controls or patients from a historical database. This new study compared COVID-19 survivors against those hospitalized for other medical causes over the same period,” Dr. Rooney said. “This is a more stringent test of whether COVID-19 has specific neurocognitive and neuropsychiatric consequences.
“The study found that new-onset neuropsychiatric diagnoses and symptoms were no more likely to occur after COVID-19 than after similarly severe medical illnesses,” Dr. Rooney said. “This negative finding runs counter to some earlier studies and may surprise some.” The findings need to be replicated in larger samples, but the current study shows the importance of prospectively recruiting active controls.
“In a subgroup analysis, some patients showed good improvement in cognitive scores between discharge and follow-up. While unsurprising, this is encouraging and suggests that the early postdischarge months are an important time for neurocognitive recovery,” Dr. Rooney noted.
“The findings suggest that COVID-19 may impair attention more selectively than other medical causes of hospitalization. COVID-19 survivors may also be at higher risk of significant overall cognitive impairment than survivors of similarly severe medical illnesses, after a similar duration,” said Dr. Rooney. “If the results are replicated by other prospective studies, they would suggest that there is something about COVID-19 that causes clinically significant neurocognitive difficulties in a minority of survivors.
“Larger well-controlled studies are required, with longer follow-up and more detailed neurocognitive testing,” as the duration of impairment and scope for further recovery are not known, Dr. Rooney added. Also unknown is whether COVID-19 affects attention permanently, or whether recovery is simply slower after COVID-19 compared to other medical illnesses.
“Knowing who is at the greatest risk of severe cognitive impairment after COVID-19 is important and likely to allow tailoring of more effective shielding strategies,” said Dr. Rooney. “This study was conducted before the widespread availability of vaccines for COVID-19. Long-term neuropsychiatric outcomes in vaccinated patients remain largely unknown. Arguably, these are now more important to understand, as future COVID-19 waves will occur mainly among vaccinated individuals.”
The study was supported by the Lundbeck Foundation and the Novo Nordisk Foundation. Lead author Dr. Nersesjan had no financial conflicts to disclose. Dr. Benros reported grants from Lundbeck Foundation and Novo Nordisk Foundation during the conduct of the study. Dr. Rooney had no financial conflicts to disclose.
This article was updated 3/25/22.
FROM JAMA PSYCHIATRY
Aducanumab and ARIA: Does the FDA’s prescribing label put patients at risk?
Specifically, the drug’s label calls for three MRI brain scans before, and during, the titration period. The problem is the trial data used for the drug’s approval by the U.S. Food and Drug Administration included five MRIs to screen for ARIA.
“We recommend proceeding as per the clinical trials,” said Meghan Riddle, MD, associate director, Memory and Aging program, Butler Hospital, and assistant professor of psychiatry and human behavior, Brown University, Providence, R.I.
Dr. Riddle shared her team’s clinical experience with aducanumab, as well as information on four ARIA cases from their clinic, during a presentation at the American Association for Geriatric Psychiatry (AAGP) 2022 Annual Meeting.
Significant safety risk?
As previously reported by this news organization, the FDA granted accelerated approval of aducanumab for AD last year.
ARIA is the most common risk associated with aducanumab and has two types: ARIA-E (with edema) and ARIA-H (with hemosiderin). These can co-occur, particularly in areas of high amyloid burden, Dr. Riddle noted during her presentation.
ARIA is often detected incidentally via MRI. Patients are usually asymptomatic, but when they do have symptoms, headache, dizziness, and vision changes are the most common complaints. However, these are generally mild, said Dr. Riddle.
Nevertheless, in some cases, there can be severe sequelae, including severe edema or bleeding and seizures, she added.
A major risk factor for ARIA is apolipoprotein 4 (APOE ε4) status. Carriers are twice as likely to develop ARIA as non-carriers.
“If you’re heterozygote for APOE ε4, you have about a 40% chance of developing ARIA, and if you’re homozygote, you have about a 66% chance of developing ARIA,” Dr. Riddle said.
Given the high rate of ARIA in APOE ε4 carriers, the team from Butler Hospital recommends APOE testing prior to treatment with aducanumab.
The risk for developing ARIA is highest within the year of dose titration, Dr. Riddle noted. The current FDA label recommends obtaining a recent brain MRI, within 1 year, and then scans before the 7th and 12th infusions. However, the protocol during the clinical trials of aducanumab included MRI at baseline and prior to the 5th, 7th, 9th, and 12th infusions.
Dr. Riddle’s group has opted to continue the research protocol with new patients. “There’s concern that the decreased MRI monitoring based on the current FDA label may pose a significant safety risk, particularly among those who we know are already at a higher risk of developing ARIA,” she said.
Dr. Riddle also shared how her team selects aducanumab candidates. They need to have mild cognitive impairment (MCI), a mini-mental state examination (MMSE) score of 24 to 30, and a recent MRI to review for eligibility and APOE testing.
The most common reason for treatment exclusion is advanced disease and comorbidity, such as stroke.
Once approved for treatment, patients receive monthly infusions titrated over 6 months – 1 mg/kg for 2 months, 3 mg/kg for 2 months, 6 mg/kg for 2 months, then 10 mg/kg.
Patients are monitored to ensure safety and tolerability and regular review of MRI findings. In addition, patients and their families receive ongoing education about the drug.
Dr. Riddle and her team permanently discontinue the aducanumab if patients develop microhemorrhage, more than one area of superficial siderosis, more than 10 microhemorrhages, more than two episodes of ARIA, or severe symptoms of ARIA.
Four cases
Of the 11 patients who were candidates for aducanumab treatment, four developed ARIA. All are APOE ε4 carriers, with two homozygotes and two heterozygotes. All had severe radiographic ARIA-E, with one developing ARIA-H.
“Importantly, they were all initially asymptomatic and the ARIA was just picked up on their regular surveillance MRI,” said Dr. Riddle. She added that the drug was discontinued in all four cases.
Three of the ARIA cases were detected prior to the 5th scan, which is “concerning,” said Dr. Riddle. “Based on the current FDA label of safety monitoring, they don’t recommend doing that MRI. So [clinicians] would have dosed through that ARIA, which could put someone at much greater risk of developing severe symptoms.”
In addition, 14 patients at the center are receiving treatment with aducanumab. However, at this point they have not yet received their first MRI screen.
Dr. Riddle noted that when patients are told they are not candidates for treatment, or when treatment is discontinued, they are upset. However, she added, there is also a substantial level of understanding.
“We have a very layered discussion that includes the simple fact that we still aren’t sure if this is going to provide any clinical benefit, that this decision [to approve the drug] was accelerated, and that data are still being gathered,” Dr. Riddle added.
Dr. Riddle noted that the risk of ARIA is highest during the dose titration period: “There’s a signal that once you get to the 10 mg/kg dose, that plateaus.”
None of the patients at her center have reached that 12-month treatment mark. “The current plan is to do the MRI at 12 months then to give serial MRIs but less frequently, and whether that’s at 6 months or annually is yet to be determined.”
“We’re kind of writing these protocols as information evolves,” Dr. Riddle said.
The Memory and Aging Program receives grants from NIH-ADNI, Alzheimer’s Association, Fain Family Foundation, Joukowsky Family Foundation, Winter Family, Rhode Island Foundation, Goodman Family Foundation, and Global Alzheimer Platform Foundation; and clinical trials include: Lilly, Biogen, Genentech, Avid, Roche, Eisai, and Novartis. Dr. Riddle has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Specifically, the drug’s label calls for three MRI brain scans before, and during, the titration period. The problem is the trial data used for the drug’s approval by the U.S. Food and Drug Administration included five MRIs to screen for ARIA.
“We recommend proceeding as per the clinical trials,” said Meghan Riddle, MD, associate director, Memory and Aging program, Butler Hospital, and assistant professor of psychiatry and human behavior, Brown University, Providence, R.I.
Dr. Riddle shared her team’s clinical experience with aducanumab, as well as information on four ARIA cases from their clinic, during a presentation at the American Association for Geriatric Psychiatry (AAGP) 2022 Annual Meeting.
Significant safety risk?
As previously reported by this news organization, the FDA granted accelerated approval of aducanumab for AD last year.
ARIA is the most common risk associated with aducanumab and has two types: ARIA-E (with edema) and ARIA-H (with hemosiderin). These can co-occur, particularly in areas of high amyloid burden, Dr. Riddle noted during her presentation.
ARIA is often detected incidentally via MRI. Patients are usually asymptomatic, but when they do have symptoms, headache, dizziness, and vision changes are the most common complaints. However, these are generally mild, said Dr. Riddle.
Nevertheless, in some cases, there can be severe sequelae, including severe edema or bleeding and seizures, she added.
A major risk factor for ARIA is apolipoprotein 4 (APOE ε4) status. Carriers are twice as likely to develop ARIA as non-carriers.
“If you’re heterozygote for APOE ε4, you have about a 40% chance of developing ARIA, and if you’re homozygote, you have about a 66% chance of developing ARIA,” Dr. Riddle said.
Given the high rate of ARIA in APOE ε4 carriers, the team from Butler Hospital recommends APOE testing prior to treatment with aducanumab.
The risk for developing ARIA is highest within the year of dose titration, Dr. Riddle noted. The current FDA label recommends obtaining a recent brain MRI, within 1 year, and then scans before the 7th and 12th infusions. However, the protocol during the clinical trials of aducanumab included MRI at baseline and prior to the 5th, 7th, 9th, and 12th infusions.
Dr. Riddle’s group has opted to continue the research protocol with new patients. “There’s concern that the decreased MRI monitoring based on the current FDA label may pose a significant safety risk, particularly among those who we know are already at a higher risk of developing ARIA,” she said.
Dr. Riddle also shared how her team selects aducanumab candidates. They need to have mild cognitive impairment (MCI), a mini-mental state examination (MMSE) score of 24 to 30, and a recent MRI to review for eligibility and APOE testing.
The most common reason for treatment exclusion is advanced disease and comorbidity, such as stroke.
Once approved for treatment, patients receive monthly infusions titrated over 6 months – 1 mg/kg for 2 months, 3 mg/kg for 2 months, 6 mg/kg for 2 months, then 10 mg/kg.
Patients are monitored to ensure safety and tolerability and regular review of MRI findings. In addition, patients and their families receive ongoing education about the drug.
Dr. Riddle and her team permanently discontinue the aducanumab if patients develop microhemorrhage, more than one area of superficial siderosis, more than 10 microhemorrhages, more than two episodes of ARIA, or severe symptoms of ARIA.
Four cases
Of the 11 patients who were candidates for aducanumab treatment, four developed ARIA. All are APOE ε4 carriers, with two homozygotes and two heterozygotes. All had severe radiographic ARIA-E, with one developing ARIA-H.
“Importantly, they were all initially asymptomatic and the ARIA was just picked up on their regular surveillance MRI,” said Dr. Riddle. She added that the drug was discontinued in all four cases.
Three of the ARIA cases were detected prior to the 5th scan, which is “concerning,” said Dr. Riddle. “Based on the current FDA label of safety monitoring, they don’t recommend doing that MRI. So [clinicians] would have dosed through that ARIA, which could put someone at much greater risk of developing severe symptoms.”
In addition, 14 patients at the center are receiving treatment with aducanumab. However, at this point they have not yet received their first MRI screen.
Dr. Riddle noted that when patients are told they are not candidates for treatment, or when treatment is discontinued, they are upset. However, she added, there is also a substantial level of understanding.
“We have a very layered discussion that includes the simple fact that we still aren’t sure if this is going to provide any clinical benefit, that this decision [to approve the drug] was accelerated, and that data are still being gathered,” Dr. Riddle added.
Dr. Riddle noted that the risk of ARIA is highest during the dose titration period: “There’s a signal that once you get to the 10 mg/kg dose, that plateaus.”
None of the patients at her center have reached that 12-month treatment mark. “The current plan is to do the MRI at 12 months then to give serial MRIs but less frequently, and whether that’s at 6 months or annually is yet to be determined.”
“We’re kind of writing these protocols as information evolves,” Dr. Riddle said.
The Memory and Aging Program receives grants from NIH-ADNI, Alzheimer’s Association, Fain Family Foundation, Joukowsky Family Foundation, Winter Family, Rhode Island Foundation, Goodman Family Foundation, and Global Alzheimer Platform Foundation; and clinical trials include: Lilly, Biogen, Genentech, Avid, Roche, Eisai, and Novartis. Dr. Riddle has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Specifically, the drug’s label calls for three MRI brain scans before, and during, the titration period. The problem is the trial data used for the drug’s approval by the U.S. Food and Drug Administration included five MRIs to screen for ARIA.
“We recommend proceeding as per the clinical trials,” said Meghan Riddle, MD, associate director, Memory and Aging program, Butler Hospital, and assistant professor of psychiatry and human behavior, Brown University, Providence, R.I.
Dr. Riddle shared her team’s clinical experience with aducanumab, as well as information on four ARIA cases from their clinic, during a presentation at the American Association for Geriatric Psychiatry (AAGP) 2022 Annual Meeting.
Significant safety risk?
As previously reported by this news organization, the FDA granted accelerated approval of aducanumab for AD last year.
ARIA is the most common risk associated with aducanumab and has two types: ARIA-E (with edema) and ARIA-H (with hemosiderin). These can co-occur, particularly in areas of high amyloid burden, Dr. Riddle noted during her presentation.
ARIA is often detected incidentally via MRI. Patients are usually asymptomatic, but when they do have symptoms, headache, dizziness, and vision changes are the most common complaints. However, these are generally mild, said Dr. Riddle.
Nevertheless, in some cases, there can be severe sequelae, including severe edema or bleeding and seizures, she added.
A major risk factor for ARIA is apolipoprotein 4 (APOE ε4) status. Carriers are twice as likely to develop ARIA as non-carriers.
“If you’re heterozygote for APOE ε4, you have about a 40% chance of developing ARIA, and if you’re homozygote, you have about a 66% chance of developing ARIA,” Dr. Riddle said.
Given the high rate of ARIA in APOE ε4 carriers, the team from Butler Hospital recommends APOE testing prior to treatment with aducanumab.
The risk for developing ARIA is highest within the year of dose titration, Dr. Riddle noted. The current FDA label recommends obtaining a recent brain MRI, within 1 year, and then scans before the 7th and 12th infusions. However, the protocol during the clinical trials of aducanumab included MRI at baseline and prior to the 5th, 7th, 9th, and 12th infusions.
Dr. Riddle’s group has opted to continue the research protocol with new patients. “There’s concern that the decreased MRI monitoring based on the current FDA label may pose a significant safety risk, particularly among those who we know are already at a higher risk of developing ARIA,” she said.
Dr. Riddle also shared how her team selects aducanumab candidates. They need to have mild cognitive impairment (MCI), a mini-mental state examination (MMSE) score of 24 to 30, and a recent MRI to review for eligibility and APOE testing.
The most common reason for treatment exclusion is advanced disease and comorbidity, such as stroke.
Once approved for treatment, patients receive monthly infusions titrated over 6 months – 1 mg/kg for 2 months, 3 mg/kg for 2 months, 6 mg/kg for 2 months, then 10 mg/kg.
Patients are monitored to ensure safety and tolerability and regular review of MRI findings. In addition, patients and their families receive ongoing education about the drug.
Dr. Riddle and her team permanently discontinue the aducanumab if patients develop microhemorrhage, more than one area of superficial siderosis, more than 10 microhemorrhages, more than two episodes of ARIA, or severe symptoms of ARIA.
Four cases
Of the 11 patients who were candidates for aducanumab treatment, four developed ARIA. All are APOE ε4 carriers, with two homozygotes and two heterozygotes. All had severe radiographic ARIA-E, with one developing ARIA-H.
“Importantly, they were all initially asymptomatic and the ARIA was just picked up on their regular surveillance MRI,” said Dr. Riddle. She added that the drug was discontinued in all four cases.
Three of the ARIA cases were detected prior to the 5th scan, which is “concerning,” said Dr. Riddle. “Based on the current FDA label of safety monitoring, they don’t recommend doing that MRI. So [clinicians] would have dosed through that ARIA, which could put someone at much greater risk of developing severe symptoms.”
In addition, 14 patients at the center are receiving treatment with aducanumab. However, at this point they have not yet received their first MRI screen.
Dr. Riddle noted that when patients are told they are not candidates for treatment, or when treatment is discontinued, they are upset. However, she added, there is also a substantial level of understanding.
“We have a very layered discussion that includes the simple fact that we still aren’t sure if this is going to provide any clinical benefit, that this decision [to approve the drug] was accelerated, and that data are still being gathered,” Dr. Riddle added.
Dr. Riddle noted that the risk of ARIA is highest during the dose titration period: “There’s a signal that once you get to the 10 mg/kg dose, that plateaus.”
None of the patients at her center have reached that 12-month treatment mark. “The current plan is to do the MRI at 12 months then to give serial MRIs but less frequently, and whether that’s at 6 months or annually is yet to be determined.”
“We’re kind of writing these protocols as information evolves,” Dr. Riddle said.
The Memory and Aging Program receives grants from NIH-ADNI, Alzheimer’s Association, Fain Family Foundation, Joukowsky Family Foundation, Winter Family, Rhode Island Foundation, Goodman Family Foundation, and Global Alzheimer Platform Foundation; and clinical trials include: Lilly, Biogen, Genentech, Avid, Roche, Eisai, and Novartis. Dr. Riddle has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAGP 2022
Schizophrenia risk lower for people with access to green space
The investigators, led by Martin Rotenberg, MD, of Centre for Addiction and Mental Health and the University of Toronto, found individuals living in areas with the lowest levels of green space were 24% more likely to develop schizophrenia.
This study contributes to a growing body of evidence showing the importance of exposure to green space to mental health.
“These findings contribute to a growing evidence base that environmental factors may play a role in the etiology of schizophrenia,” the researchers write.
The study was published online Feb. 4 in the Canadian Journal of Psychiatry.
Underlying mechanism unknown
For the study, researchers used a retrospective population-based cohort of 649,020 individuals between ages 14 and 40 years from different neighborhoods in Toronto.
Green space was calculated using geospatial data of all public parks and green spaces in the city; data were drawn from the Urban Health Equity Assessment and Response Tool.
Over a 10-year period, 4,841 participants were diagnosed with schizophrenia.
Those who lived in neighborhoods with the least amount of green space were significantly more likely to develop schizophrenia than those who lived in areas with the most green space, even after adjusting for age, sex, and neighborhood-level marginalization (adjusted incidence rate ratio, 1.24; 95% confidence interval, 1.06-1.45).
Overall, schizophrenia risk was also elevated in men vs. women (adjusted IRR, 1.59; 95% CI, 1.50-1.68). Those living in areas with moderate amounts of green space did not have an increased schizophrenia risk.
“We found that residing in an area with the lowest amount of green space was associated with an increased risk of developing schizophrenia, independent of other sociodemographic and socioenvironmental factors,” the researchers note. “The underlying mechanism at play is unknown and requires further study.”
One possibility, they added, is that exposure to green space may reduce the risk of air pollution, which other studies have suggested may be associated with increased schizophrenia risk.
The new study builds on a 2018 report from Denmark that showed a 52% increased risk of psychotic disorders in adulthood among people who spent their childhood in neighborhoods with little green space.
Important, longitudinal data
Commenting on the findings, John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, said the study provides important longitudinal data.
“The 10-year duration of the study and large sample size make the results very compelling and help confirm what has been thought about green space and risk of schizophrenia,” Dr. Torous said.
“Often, we think of green space at a very macro level,” he added. “This study is important because it shows us that green space matters on a block-by-block level just as much.”
The study was unfunded. The authors and Dr. Torous have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The investigators, led by Martin Rotenberg, MD, of Centre for Addiction and Mental Health and the University of Toronto, found individuals living in areas with the lowest levels of green space were 24% more likely to develop schizophrenia.
This study contributes to a growing body of evidence showing the importance of exposure to green space to mental health.
“These findings contribute to a growing evidence base that environmental factors may play a role in the etiology of schizophrenia,” the researchers write.
The study was published online Feb. 4 in the Canadian Journal of Psychiatry.
Underlying mechanism unknown
For the study, researchers used a retrospective population-based cohort of 649,020 individuals between ages 14 and 40 years from different neighborhoods in Toronto.
Green space was calculated using geospatial data of all public parks and green spaces in the city; data were drawn from the Urban Health Equity Assessment and Response Tool.
Over a 10-year period, 4,841 participants were diagnosed with schizophrenia.
Those who lived in neighborhoods with the least amount of green space were significantly more likely to develop schizophrenia than those who lived in areas with the most green space, even after adjusting for age, sex, and neighborhood-level marginalization (adjusted incidence rate ratio, 1.24; 95% confidence interval, 1.06-1.45).
Overall, schizophrenia risk was also elevated in men vs. women (adjusted IRR, 1.59; 95% CI, 1.50-1.68). Those living in areas with moderate amounts of green space did not have an increased schizophrenia risk.
“We found that residing in an area with the lowest amount of green space was associated with an increased risk of developing schizophrenia, independent of other sociodemographic and socioenvironmental factors,” the researchers note. “The underlying mechanism at play is unknown and requires further study.”
One possibility, they added, is that exposure to green space may reduce the risk of air pollution, which other studies have suggested may be associated with increased schizophrenia risk.
The new study builds on a 2018 report from Denmark that showed a 52% increased risk of psychotic disorders in adulthood among people who spent their childhood in neighborhoods with little green space.
Important, longitudinal data
Commenting on the findings, John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, said the study provides important longitudinal data.
“The 10-year duration of the study and large sample size make the results very compelling and help confirm what has been thought about green space and risk of schizophrenia,” Dr. Torous said.
“Often, we think of green space at a very macro level,” he added. “This study is important because it shows us that green space matters on a block-by-block level just as much.”
The study was unfunded. The authors and Dr. Torous have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The investigators, led by Martin Rotenberg, MD, of Centre for Addiction and Mental Health and the University of Toronto, found individuals living in areas with the lowest levels of green space were 24% more likely to develop schizophrenia.
This study contributes to a growing body of evidence showing the importance of exposure to green space to mental health.
“These findings contribute to a growing evidence base that environmental factors may play a role in the etiology of schizophrenia,” the researchers write.
The study was published online Feb. 4 in the Canadian Journal of Psychiatry.
Underlying mechanism unknown
For the study, researchers used a retrospective population-based cohort of 649,020 individuals between ages 14 and 40 years from different neighborhoods in Toronto.
Green space was calculated using geospatial data of all public parks and green spaces in the city; data were drawn from the Urban Health Equity Assessment and Response Tool.
Over a 10-year period, 4,841 participants were diagnosed with schizophrenia.
Those who lived in neighborhoods with the least amount of green space were significantly more likely to develop schizophrenia than those who lived in areas with the most green space, even after adjusting for age, sex, and neighborhood-level marginalization (adjusted incidence rate ratio, 1.24; 95% confidence interval, 1.06-1.45).
Overall, schizophrenia risk was also elevated in men vs. women (adjusted IRR, 1.59; 95% CI, 1.50-1.68). Those living in areas with moderate amounts of green space did not have an increased schizophrenia risk.
“We found that residing in an area with the lowest amount of green space was associated with an increased risk of developing schizophrenia, independent of other sociodemographic and socioenvironmental factors,” the researchers note. “The underlying mechanism at play is unknown and requires further study.”
One possibility, they added, is that exposure to green space may reduce the risk of air pollution, which other studies have suggested may be associated with increased schizophrenia risk.
The new study builds on a 2018 report from Denmark that showed a 52% increased risk of psychotic disorders in adulthood among people who spent their childhood in neighborhoods with little green space.
Important, longitudinal data
Commenting on the findings, John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, said the study provides important longitudinal data.
“The 10-year duration of the study and large sample size make the results very compelling and help confirm what has been thought about green space and risk of schizophrenia,” Dr. Torous said.
“Often, we think of green space at a very macro level,” he added. “This study is important because it shows us that green space matters on a block-by-block level just as much.”
The study was unfunded. The authors and Dr. Torous have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CANADIAN JOURNAL OF PSYCHIATRY
Executive-function deficits a new treatment target for PTSD?
DENVER –
“To our knowledge, this study is the first to show that executive-function deficits maintain PTSD symptoms following trauma exposure,” investigators noted in research presented at the Anxiety and Depression Association of America (ADAA) Anxiety & Depression conference.
The results are important in “developing precision medicine–based approaches for alleviating [posttraumatic stress] symptoms, and improving well-established PTSD treatments for those with relative deficits in executive function,” study investigator Joseph R. Bardeen, PhD, associate professor at Auburn (Ala.) University, told meeting attendees.
The findings were published in the Journal of Anxiety Disorders.
Cognitive impairment
In earlier research, deficits in EF were associated with an increased vulnerability for PTSD symptoms. However, less is known about the role of these deficits, which can impair higher-level cognitive ability, in sustaining PTSD symptoms.
To investigate, the authors conducted a longitudinal study that included 98 participants aged 18-65 years who had been identified via phone screening as experiencing clinically significant PTSD symptoms.
Participants completed self-report measures for PTSD symptoms, as well as measures for EF deficits at baseline and 6-month (n = 92) and 12-month (n = 91) follow-up sessions.
A path analysis showed a significant relationship between baseline PTSD symptoms and EF deficits at 6 months (P < .001). Baseline PTSD symptoms were associated with 12-month PTSD symptoms (P < .04).
EF deficits at 6 months were also associated with 12-month PTSD symptoms (P = .02).
Importantly, no associations were observed between baseline or 6-month PTSD symptoms and EF deficits at 12 months. However, EF deficits at 6 months drove the relationship between PTSD symptoms at baseline and at 1 year (indirect effect = .061).
“What this suggests is that executive-function deficits are a mechanism that maintains patients’ symptoms over the course of 1 year,” Dr. Bardeen said.
“And you don’t see the reverse,” he added. “You don’t see that PTSD symptoms at [6 months] mediate the relationship between [baseline] and 6 month executive-function deficits.”
Surprising finding
The findings suggest deficits in executive functioning have a stronger role in maintaining PTSD symptoms than these symptoms have in maintaining EF deficits, Dr. Bardeen told this news organization.
“I had originally hypothesized a bidirectional relationship in which PTSD symptoms influenced future executive-function deficits and executive-function deficits influenced future PTSD symptoms,” he said.
“So, it was a surprise that, when accounting for both variables in the same model, executive-function deficits predicted future PTSD symptoms, but PTSD symptoms did not significantly predict future EF deficits,” he added.
Dr. Bardeen noted this suggests that EF deficits “may be a particularly important maintenance factor.”
In addition, he recommended the use of neuropsychological assessments prior to treatment to identify individuals with EF deficits and distinguish those deficits from PTSD symptoms.
“There is certainly overlap between executive-function deficits and PTSD symptoms,” Dr. Bardeen said. “For example, several of the symptoms of PTSD, such as concentration difficulties, may be indicators of executive-function deficits.”
He noted assessments such as the Delis Kaplan Executive Function System, and Clinician Administered PTSD Scale for DSM-5, when used as part of a larger assessment battery, can help differentiate between the EF deficits and PTSD.
“This would take several hours to administer, but in cases in which serious cognitive impairment is suspected, a comprehensive assessment is the way to go,” Dr. Bardeen said.
The standard approaches of prolonged exposure therapy and cognitive processing therapy can be effective in patients without EF deficits, while some modifications may benefit those with these deficits, he added.
“For example, it’s important to provide a more directive and structured environment in which the practitioner repeats key points frequently, uses concrete language, simplifies worksheets, and provides written summaries and reminder cards,” he said.
Further findings
In additional research presented at the meeting, Elsa Mattson, a PhD student from Case Western Reserve University, Cleveland, and colleagues reported findings further distinguishing the role of EF in PTSD.
In that study of 149 patients with chronic PTSD, those with low performing working memory, but not high working memory, had higher pre- as well as posttreatment PTSD symptom severity and depressive symptoms.
“Clinicians should consider that impairments in executive function may play a role in reduced treatment response, potentially impairing a client’s ability to learn new information in treatment,” the investigators wrote.
“Understanding how executive function processes change over the course of treatment, particularly in relation to processing the trauma memories, is an important next step,” they added.
The first study was supported by a grant from the National Institute of Mental Health. The investigators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
DENVER –
“To our knowledge, this study is the first to show that executive-function deficits maintain PTSD symptoms following trauma exposure,” investigators noted in research presented at the Anxiety and Depression Association of America (ADAA) Anxiety & Depression conference.
The results are important in “developing precision medicine–based approaches for alleviating [posttraumatic stress] symptoms, and improving well-established PTSD treatments for those with relative deficits in executive function,” study investigator Joseph R. Bardeen, PhD, associate professor at Auburn (Ala.) University, told meeting attendees.
The findings were published in the Journal of Anxiety Disorders.
Cognitive impairment
In earlier research, deficits in EF were associated with an increased vulnerability for PTSD symptoms. However, less is known about the role of these deficits, which can impair higher-level cognitive ability, in sustaining PTSD symptoms.
To investigate, the authors conducted a longitudinal study that included 98 participants aged 18-65 years who had been identified via phone screening as experiencing clinically significant PTSD symptoms.
Participants completed self-report measures for PTSD symptoms, as well as measures for EF deficits at baseline and 6-month (n = 92) and 12-month (n = 91) follow-up sessions.
A path analysis showed a significant relationship between baseline PTSD symptoms and EF deficits at 6 months (P < .001). Baseline PTSD symptoms were associated with 12-month PTSD symptoms (P < .04).
EF deficits at 6 months were also associated with 12-month PTSD symptoms (P = .02).
Importantly, no associations were observed between baseline or 6-month PTSD symptoms and EF deficits at 12 months. However, EF deficits at 6 months drove the relationship between PTSD symptoms at baseline and at 1 year (indirect effect = .061).
“What this suggests is that executive-function deficits are a mechanism that maintains patients’ symptoms over the course of 1 year,” Dr. Bardeen said.
“And you don’t see the reverse,” he added. “You don’t see that PTSD symptoms at [6 months] mediate the relationship between [baseline] and 6 month executive-function deficits.”
Surprising finding
The findings suggest deficits in executive functioning have a stronger role in maintaining PTSD symptoms than these symptoms have in maintaining EF deficits, Dr. Bardeen told this news organization.
“I had originally hypothesized a bidirectional relationship in which PTSD symptoms influenced future executive-function deficits and executive-function deficits influenced future PTSD symptoms,” he said.
“So, it was a surprise that, when accounting for both variables in the same model, executive-function deficits predicted future PTSD symptoms, but PTSD symptoms did not significantly predict future EF deficits,” he added.
Dr. Bardeen noted this suggests that EF deficits “may be a particularly important maintenance factor.”
In addition, he recommended the use of neuropsychological assessments prior to treatment to identify individuals with EF deficits and distinguish those deficits from PTSD symptoms.
“There is certainly overlap between executive-function deficits and PTSD symptoms,” Dr. Bardeen said. “For example, several of the symptoms of PTSD, such as concentration difficulties, may be indicators of executive-function deficits.”
He noted assessments such as the Delis Kaplan Executive Function System, and Clinician Administered PTSD Scale for DSM-5, when used as part of a larger assessment battery, can help differentiate between the EF deficits and PTSD.
“This would take several hours to administer, but in cases in which serious cognitive impairment is suspected, a comprehensive assessment is the way to go,” Dr. Bardeen said.
The standard approaches of prolonged exposure therapy and cognitive processing therapy can be effective in patients without EF deficits, while some modifications may benefit those with these deficits, he added.
“For example, it’s important to provide a more directive and structured environment in which the practitioner repeats key points frequently, uses concrete language, simplifies worksheets, and provides written summaries and reminder cards,” he said.
Further findings
In additional research presented at the meeting, Elsa Mattson, a PhD student from Case Western Reserve University, Cleveland, and colleagues reported findings further distinguishing the role of EF in PTSD.
In that study of 149 patients with chronic PTSD, those with low performing working memory, but not high working memory, had higher pre- as well as posttreatment PTSD symptom severity and depressive symptoms.
“Clinicians should consider that impairments in executive function may play a role in reduced treatment response, potentially impairing a client’s ability to learn new information in treatment,” the investigators wrote.
“Understanding how executive function processes change over the course of treatment, particularly in relation to processing the trauma memories, is an important next step,” they added.
The first study was supported by a grant from the National Institute of Mental Health. The investigators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
DENVER –
“To our knowledge, this study is the first to show that executive-function deficits maintain PTSD symptoms following trauma exposure,” investigators noted in research presented at the Anxiety and Depression Association of America (ADAA) Anxiety & Depression conference.
The results are important in “developing precision medicine–based approaches for alleviating [posttraumatic stress] symptoms, and improving well-established PTSD treatments for those with relative deficits in executive function,” study investigator Joseph R. Bardeen, PhD, associate professor at Auburn (Ala.) University, told meeting attendees.
The findings were published in the Journal of Anxiety Disorders.
Cognitive impairment
In earlier research, deficits in EF were associated with an increased vulnerability for PTSD symptoms. However, less is known about the role of these deficits, which can impair higher-level cognitive ability, in sustaining PTSD symptoms.
To investigate, the authors conducted a longitudinal study that included 98 participants aged 18-65 years who had been identified via phone screening as experiencing clinically significant PTSD symptoms.
Participants completed self-report measures for PTSD symptoms, as well as measures for EF deficits at baseline and 6-month (n = 92) and 12-month (n = 91) follow-up sessions.
A path analysis showed a significant relationship between baseline PTSD symptoms and EF deficits at 6 months (P < .001). Baseline PTSD symptoms were associated with 12-month PTSD symptoms (P < .04).
EF deficits at 6 months were also associated with 12-month PTSD symptoms (P = .02).
Importantly, no associations were observed between baseline or 6-month PTSD symptoms and EF deficits at 12 months. However, EF deficits at 6 months drove the relationship between PTSD symptoms at baseline and at 1 year (indirect effect = .061).
“What this suggests is that executive-function deficits are a mechanism that maintains patients’ symptoms over the course of 1 year,” Dr. Bardeen said.
“And you don’t see the reverse,” he added. “You don’t see that PTSD symptoms at [6 months] mediate the relationship between [baseline] and 6 month executive-function deficits.”
Surprising finding
The findings suggest deficits in executive functioning have a stronger role in maintaining PTSD symptoms than these symptoms have in maintaining EF deficits, Dr. Bardeen told this news organization.
“I had originally hypothesized a bidirectional relationship in which PTSD symptoms influenced future executive-function deficits and executive-function deficits influenced future PTSD symptoms,” he said.
“So, it was a surprise that, when accounting for both variables in the same model, executive-function deficits predicted future PTSD symptoms, but PTSD symptoms did not significantly predict future EF deficits,” he added.
Dr. Bardeen noted this suggests that EF deficits “may be a particularly important maintenance factor.”
In addition, he recommended the use of neuropsychological assessments prior to treatment to identify individuals with EF deficits and distinguish those deficits from PTSD symptoms.
“There is certainly overlap between executive-function deficits and PTSD symptoms,” Dr. Bardeen said. “For example, several of the symptoms of PTSD, such as concentration difficulties, may be indicators of executive-function deficits.”
He noted assessments such as the Delis Kaplan Executive Function System, and Clinician Administered PTSD Scale for DSM-5, when used as part of a larger assessment battery, can help differentiate between the EF deficits and PTSD.
“This would take several hours to administer, but in cases in which serious cognitive impairment is suspected, a comprehensive assessment is the way to go,” Dr. Bardeen said.
The standard approaches of prolonged exposure therapy and cognitive processing therapy can be effective in patients without EF deficits, while some modifications may benefit those with these deficits, he added.
“For example, it’s important to provide a more directive and structured environment in which the practitioner repeats key points frequently, uses concrete language, simplifies worksheets, and provides written summaries and reminder cards,” he said.
Further findings
In additional research presented at the meeting, Elsa Mattson, a PhD student from Case Western Reserve University, Cleveland, and colleagues reported findings further distinguishing the role of EF in PTSD.
In that study of 149 patients with chronic PTSD, those with low performing working memory, but not high working memory, had higher pre- as well as posttreatment PTSD symptom severity and depressive symptoms.
“Clinicians should consider that impairments in executive function may play a role in reduced treatment response, potentially impairing a client’s ability to learn new information in treatment,” the investigators wrote.
“Understanding how executive function processes change over the course of treatment, particularly in relation to processing the trauma memories, is an important next step,” they added.
The first study was supported by a grant from the National Institute of Mental Health. The investigators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
REPORTING FROM ADAA 2022
Jury is out on universal screening for eating disorders
Eating disorders (binge eating disorder, bulimia nervosa, and anorexia nervosa) can cause “serious harms to physical and psychosocial health and take a tremendous toll on individuals and families,” task force member Lori Pbert, PhD, told this news organization.
“Screening for eating disorders has the potential to improve health by leading to early detection and effective treatment,” said Dr. Pbert, with the department of population and quantitative health sciences, University of Massachusetts, Worcester.
However, a “deep dive” into the available literature failed to turn up adequate evidence to recommend for or against routine screening for eating disorders for children and adolescents aged 10 years and older and for adults who have no signs or symptoms of an eating disorder or concerns about their eating and who have not previously been diagnosed with an eating disorder, Dr. Pbert said.
The task force, therefore, issued an “I” statement (insufficient evidence), meaning it cannot at this time recommend for or against screening for eating disorders.
An “I” statement is “fundamentally a call for more research,” Dr. Pbert noted.
Adolescents and adults who have signs and symptoms of an eating disorder – which include rapid weight loss; weight gain or pronounced deviation from growth trajectory; pubertal delay; bradycardia; oligomenorrhea; and amenorrhea – are not included in this recommendation.
The USPSTF recommendation statement and accompanying evidence report were published online March 15 in JAMA.
Clinical judgment key
In the absence of evidence, clinicians should use their judgment when determining whether or not to screen an individual patient for an eating disorder, Dr. Pbert advised.
One thing to consider is whether the patient is in a group at higher risk for eating disorders, such as athletes, females, young adults aged 18-29, and transgender individuals.
Another is whether the patient reports engaging in unhealthy weight control behaviors, such as fasting or skipping meals, Dr. Pbert said.
Importantly, any patient who has signs or symptoms of an eating disorder or is expressing concerns about their eating should be assessed and referred for appropriate care, Dr. Pbert said.
“The good news is that eating disorders can be treated,” she said.
Several organizations currently recommend screening in the context of monitoring changes in weight and other vital signs or signs and symptoms to determine whether a patient might have an eating disorder.
Dr. Pbert said it’s important to recognize that the USPSTF statement “doesn’t really conflict” with the recommendations of other organizations. “We all agree that patients who present with signs or symptoms of an eating disorder should be assessed further.”
Evidence gaps
The authors of an invited commentary in JAMA) say the task force has identified several “notable deficiencies” in the available data on screening for eating disorders.
“Directing attention to rigorous research to close this evidence gap will be important to find optimal approaches to identify patients with these complex disorders and improve their health outcomes,” write Evelyn Attia, MD, with Weill Cornell Medicine in New York, and Angela Guarda, MD, with Johns Hopkins University, Baltimore.
This “I” statement, they say, “highlights the need to prioritize research aimed at closing the evidence gap identified by USPSTF in a timely manner and underscores the need for new studies that address screening for eating disorders, treatment trials that enroll screen-detected populations from primary care settings, and screening in specific populations.
“Research on screening in primary care also should be paired with development and assessment of early brief intervention strategies for those individuals who screen positive, especially adolescents,” Dr. Attia and Dr. Guarda say.
Members of the USPSTF have disclosed no relevant financial relationships. Dr. Attia has received research support from the National Institute of Mental Health and the Hilda & Preston David Foundation; royalties from UpToDate; and has served as a clinical advisor to Equip Health. Dr. Guarda has received support from the Stephen and Jean Robinson Fund and research funding from the Klarman Family Foundation.
A version of this article first appeared on Medscape.com.
Eating disorders (binge eating disorder, bulimia nervosa, and anorexia nervosa) can cause “serious harms to physical and psychosocial health and take a tremendous toll on individuals and families,” task force member Lori Pbert, PhD, told this news organization.
“Screening for eating disorders has the potential to improve health by leading to early detection and effective treatment,” said Dr. Pbert, with the department of population and quantitative health sciences, University of Massachusetts, Worcester.
However, a “deep dive” into the available literature failed to turn up adequate evidence to recommend for or against routine screening for eating disorders for children and adolescents aged 10 years and older and for adults who have no signs or symptoms of an eating disorder or concerns about their eating and who have not previously been diagnosed with an eating disorder, Dr. Pbert said.
The task force, therefore, issued an “I” statement (insufficient evidence), meaning it cannot at this time recommend for or against screening for eating disorders.
An “I” statement is “fundamentally a call for more research,” Dr. Pbert noted.
Adolescents and adults who have signs and symptoms of an eating disorder – which include rapid weight loss; weight gain or pronounced deviation from growth trajectory; pubertal delay; bradycardia; oligomenorrhea; and amenorrhea – are not included in this recommendation.
The USPSTF recommendation statement and accompanying evidence report were published online March 15 in JAMA.
Clinical judgment key
In the absence of evidence, clinicians should use their judgment when determining whether or not to screen an individual patient for an eating disorder, Dr. Pbert advised.
One thing to consider is whether the patient is in a group at higher risk for eating disorders, such as athletes, females, young adults aged 18-29, and transgender individuals.
Another is whether the patient reports engaging in unhealthy weight control behaviors, such as fasting or skipping meals, Dr. Pbert said.
Importantly, any patient who has signs or symptoms of an eating disorder or is expressing concerns about their eating should be assessed and referred for appropriate care, Dr. Pbert said.
“The good news is that eating disorders can be treated,” she said.
Several organizations currently recommend screening in the context of monitoring changes in weight and other vital signs or signs and symptoms to determine whether a patient might have an eating disorder.
Dr. Pbert said it’s important to recognize that the USPSTF statement “doesn’t really conflict” with the recommendations of other organizations. “We all agree that patients who present with signs or symptoms of an eating disorder should be assessed further.”
Evidence gaps
The authors of an invited commentary in JAMA) say the task force has identified several “notable deficiencies” in the available data on screening for eating disorders.
“Directing attention to rigorous research to close this evidence gap will be important to find optimal approaches to identify patients with these complex disorders and improve their health outcomes,” write Evelyn Attia, MD, with Weill Cornell Medicine in New York, and Angela Guarda, MD, with Johns Hopkins University, Baltimore.
This “I” statement, they say, “highlights the need to prioritize research aimed at closing the evidence gap identified by USPSTF in a timely manner and underscores the need for new studies that address screening for eating disorders, treatment trials that enroll screen-detected populations from primary care settings, and screening in specific populations.
“Research on screening in primary care also should be paired with development and assessment of early brief intervention strategies for those individuals who screen positive, especially adolescents,” Dr. Attia and Dr. Guarda say.
Members of the USPSTF have disclosed no relevant financial relationships. Dr. Attia has received research support from the National Institute of Mental Health and the Hilda & Preston David Foundation; royalties from UpToDate; and has served as a clinical advisor to Equip Health. Dr. Guarda has received support from the Stephen and Jean Robinson Fund and research funding from the Klarman Family Foundation.
A version of this article first appeared on Medscape.com.
Eating disorders (binge eating disorder, bulimia nervosa, and anorexia nervosa) can cause “serious harms to physical and psychosocial health and take a tremendous toll on individuals and families,” task force member Lori Pbert, PhD, told this news organization.
“Screening for eating disorders has the potential to improve health by leading to early detection and effective treatment,” said Dr. Pbert, with the department of population and quantitative health sciences, University of Massachusetts, Worcester.
However, a “deep dive” into the available literature failed to turn up adequate evidence to recommend for or against routine screening for eating disorders for children and adolescents aged 10 years and older and for adults who have no signs or symptoms of an eating disorder or concerns about their eating and who have not previously been diagnosed with an eating disorder, Dr. Pbert said.
The task force, therefore, issued an “I” statement (insufficient evidence), meaning it cannot at this time recommend for or against screening for eating disorders.
An “I” statement is “fundamentally a call for more research,” Dr. Pbert noted.
Adolescents and adults who have signs and symptoms of an eating disorder – which include rapid weight loss; weight gain or pronounced deviation from growth trajectory; pubertal delay; bradycardia; oligomenorrhea; and amenorrhea – are not included in this recommendation.
The USPSTF recommendation statement and accompanying evidence report were published online March 15 in JAMA.
Clinical judgment key
In the absence of evidence, clinicians should use their judgment when determining whether or not to screen an individual patient for an eating disorder, Dr. Pbert advised.
One thing to consider is whether the patient is in a group at higher risk for eating disorders, such as athletes, females, young adults aged 18-29, and transgender individuals.
Another is whether the patient reports engaging in unhealthy weight control behaviors, such as fasting or skipping meals, Dr. Pbert said.
Importantly, any patient who has signs or symptoms of an eating disorder or is expressing concerns about their eating should be assessed and referred for appropriate care, Dr. Pbert said.
“The good news is that eating disorders can be treated,” she said.
Several organizations currently recommend screening in the context of monitoring changes in weight and other vital signs or signs and symptoms to determine whether a patient might have an eating disorder.
Dr. Pbert said it’s important to recognize that the USPSTF statement “doesn’t really conflict” with the recommendations of other organizations. “We all agree that patients who present with signs or symptoms of an eating disorder should be assessed further.”
Evidence gaps
The authors of an invited commentary in JAMA) say the task force has identified several “notable deficiencies” in the available data on screening for eating disorders.
“Directing attention to rigorous research to close this evidence gap will be important to find optimal approaches to identify patients with these complex disorders and improve their health outcomes,” write Evelyn Attia, MD, with Weill Cornell Medicine in New York, and Angela Guarda, MD, with Johns Hopkins University, Baltimore.
This “I” statement, they say, “highlights the need to prioritize research aimed at closing the evidence gap identified by USPSTF in a timely manner and underscores the need for new studies that address screening for eating disorders, treatment trials that enroll screen-detected populations from primary care settings, and screening in specific populations.
“Research on screening in primary care also should be paired with development and assessment of early brief intervention strategies for those individuals who screen positive, especially adolescents,” Dr. Attia and Dr. Guarda say.
Members of the USPSTF have disclosed no relevant financial relationships. Dr. Attia has received research support from the National Institute of Mental Health and the Hilda & Preston David Foundation; royalties from UpToDate; and has served as a clinical advisor to Equip Health. Dr. Guarda has received support from the Stephen and Jean Robinson Fund and research funding from the Klarman Family Foundation.
A version of this article first appeared on Medscape.com.
Common eye disorder in children tied to mental illness
Misaligned eyes in children are associated with an increased prevalence of mental illness, results of a large study suggest.
“Psychiatrists who have a patient with depression or anxiety and notice that patient also has strabismus might think about the link between those two conditions and refer that patient,” study investigator Stacy L. Pineles, MD, professor, department of ophthalmology, University of California, Los Angeles, told this news organization.
The study was published online March 10 in JAMA Ophthalmology.
A common condition
Strabismus, a condition in which the eyes don’t line up or are “crossed,” is one of the most common eye diseases in children, with some estimates suggesting it affects more than 1.5 million American youth.
Patients with strabismus have problems making eye contact and are affected socially and functionally, said Dr. Pineles. They’re often met with a negative bias, as shown by children’s responses to pictures of faces with and without strabismus, she said.
There is a signal from previous research suggesting that strabismus is linked to a higher risk of mental illness. However, most of these studies were small and had relatively homogenous populations, said Dr. Pineles.
The new study includes over 12 million children (mean age, 8.0 years) from a private health insurance claims database that represents diverse races and ethnicities as well as geographic regions across the United States.
The sample included 352,636 children with strabismus and 11,652,553 children with no diagnosed eye disease who served as controls. Most participants were White (51.6%), came from a family with an annual household income of $40,000 or more (51.0%), had point-of-service insurance (68.7%), and had at least one comorbid condition (64.5%).
The study evaluated five mental illness diagnoses. These included anxiety disorder, depressive disorder, substance use or addictive disorder, bipolar disorder, and schizophrenia.
Overall, children with strabismus had a higher prevalence of all these illnesses, with the exception of substance use disorder.
After adjusting for age, sex, race and ethnicity, census region, education level of caregiver, family net worth, and presence of at least one comorbid condition, the odds ratios among those with versus without strabismus were: 2.01 (95% confidence interval, 1.99-2.04; P < .001) for anxiety disorder, 1.83 (95% CI, 1.76-1.90; P < .001) for schizophrenia, 1.64 (95% CI, 1.59-1.70; P < .001) for bipolar disorder, and 1.61 (95% CI, 1.59-1.63; P < .001) for depressive disorder.
Substance use disorder had a negative unadjusted association with strabismus, but after adjustment for confounders, the association was not significant (OR, 0.99; 95% CI, 0.97-1.02; P = .48).
Dr. Pineles noted that the study participants, who were all under age 19, may be too young to have substance use disorders.
The results for substance use disorders provided something of an “internal control” and reaffirmed results for the other four conditions, said Dr. Pineles.
“When you do research on such a large database, you’re very likely to find significant associations; the dataset is so large that even very small differences become statistically significant. It was interesting that not everything gave us a positive association.”
Researchers divided the strabismus group into those with esotropia, where the eyes turn inward (52.2%), exotropia, where they turn outward (46.3%), and hypertropia, where one eye wanders upward (12.5%). Investigators found that all three conditions were associated with increased risk of anxiety disorder, depressive disorder, bipolar disorders, and schizophrenia.
Investigators note that rates in the current study were lower than in previous studies, which showed that children with congenital esotropia were 2.6 times more likely to receive a mental health diagnosis, and children with intermittent exotropia were 2.7 times more likely to receive a mental health diagnosis.
“It is probable that our study found a lower risk than these studies, because our study was cross-sectional and claims based, whereas these studies observed the children to early adulthood and were based on medical records,” the investigators note.
It’s impossible to determine from this study how strabismus is connected to mental illness. However, Dr. Pineles believes depression and anxiety might be tied to strabismus via teasing, which affects self-esteem, although genetics could also play a role. For conditions such as schizophrenia, a shared genetic link with strabismus might be more likely, she added.
“Schizophrenia is a pretty severe diagnosis, so just being teased or having poor self-esteem is probably not enough” to develop schizophrenia.
Based on her clinical experience, Dr. Pineles said that realigning the eyes of patients with milder forms of depression or anxiety “definitely anecdotally helps these patients a lot.”
Dr. Pineles and colleagues have another paper in press that examines mental illnesses and other serious eye disorders in children and shows similar findings, she said.
Implications for insurance coverage?
In an accompanying editorial, experts, led by S. Grace Prakalapakorn, MD, department of ophthalmology and pediatrics, Duke University Medical Center, Durham, N.C., noted the exclusion of children covered under government insurance or without insurance is an important study limitation, largely because socioeconomic status is a risk factor for poor mental health.
The editorialists point to studies showing that surgical correction of ocular misalignments may be associated with reduced anxiety and depression. However, health insurance coverage for such surgical correction “may not be available owing to a misconception that these conditions are ‘cosmetic’.”
Evidence of the broader association of strabismus with physical and mental health “may play an important role in shifting policy to promote insurance coverage for timely strabismus care,” they write.
As many mental health disorders begin in childhood or adolescence, “it is paramount to identify, address, and, if possible, prevent mental health disorders at a young age, because failure to intervene in a timely fashion can have lifelong health consequences,” say Dr. Prakalapakorn and colleagues.
With mental health conditions and disorders increasing worldwide, compounded by the stressors of the COVID-19 pandemic, additional studies are needed to explore the causal relationships between ocular and psychiatric phenomena, their treatment, and outcomes, they add.
The study was supported by a grant from the National Eye Institute and an unrestricted grant from Research to Prevent Blindness. Dr. Pineles has reported no relevant conflicts of interest. Commentary author Manpreet K. Singh, MD, has reported receiving research support from Stanford’s Maternal Child Health Research Institute and Stanford’s Department of Psychiatry and Behavioral Sciences, the National Institute of Mental Health, the National Institute on Aging, the Patient-Centered Outcomes Research Institute, Johnson & Johnson, Allergan, and the Brain and Behavior Research Foundation; serving on the advisory board for Sunovion and Skyland Trail; serving as a consultant for Johnson & Johnson; previously serving as a consultant for X, the moonshot factory, Alphabet, and Limbix Health; receiving honoraria from the American Academy of Child and Adolescent Psychiatry; and receiving royalties from American Psychiatric Association Publishing and Thrive Global. Commentary author Nathan Congdon, MD, has reported receiving personal fees from Belkin Vision outside the submitted work.
A version of this article first appeared on Medscape.com.
Misaligned eyes in children are associated with an increased prevalence of mental illness, results of a large study suggest.
“Psychiatrists who have a patient with depression or anxiety and notice that patient also has strabismus might think about the link between those two conditions and refer that patient,” study investigator Stacy L. Pineles, MD, professor, department of ophthalmology, University of California, Los Angeles, told this news organization.
The study was published online March 10 in JAMA Ophthalmology.
A common condition
Strabismus, a condition in which the eyes don’t line up or are “crossed,” is one of the most common eye diseases in children, with some estimates suggesting it affects more than 1.5 million American youth.
Patients with strabismus have problems making eye contact and are affected socially and functionally, said Dr. Pineles. They’re often met with a negative bias, as shown by children’s responses to pictures of faces with and without strabismus, she said.
There is a signal from previous research suggesting that strabismus is linked to a higher risk of mental illness. However, most of these studies were small and had relatively homogenous populations, said Dr. Pineles.
The new study includes over 12 million children (mean age, 8.0 years) from a private health insurance claims database that represents diverse races and ethnicities as well as geographic regions across the United States.
The sample included 352,636 children with strabismus and 11,652,553 children with no diagnosed eye disease who served as controls. Most participants were White (51.6%), came from a family with an annual household income of $40,000 or more (51.0%), had point-of-service insurance (68.7%), and had at least one comorbid condition (64.5%).
The study evaluated five mental illness diagnoses. These included anxiety disorder, depressive disorder, substance use or addictive disorder, bipolar disorder, and schizophrenia.
Overall, children with strabismus had a higher prevalence of all these illnesses, with the exception of substance use disorder.
After adjusting for age, sex, race and ethnicity, census region, education level of caregiver, family net worth, and presence of at least one comorbid condition, the odds ratios among those with versus without strabismus were: 2.01 (95% confidence interval, 1.99-2.04; P < .001) for anxiety disorder, 1.83 (95% CI, 1.76-1.90; P < .001) for schizophrenia, 1.64 (95% CI, 1.59-1.70; P < .001) for bipolar disorder, and 1.61 (95% CI, 1.59-1.63; P < .001) for depressive disorder.
Substance use disorder had a negative unadjusted association with strabismus, but after adjustment for confounders, the association was not significant (OR, 0.99; 95% CI, 0.97-1.02; P = .48).
Dr. Pineles noted that the study participants, who were all under age 19, may be too young to have substance use disorders.
The results for substance use disorders provided something of an “internal control” and reaffirmed results for the other four conditions, said Dr. Pineles.
“When you do research on such a large database, you’re very likely to find significant associations; the dataset is so large that even very small differences become statistically significant. It was interesting that not everything gave us a positive association.”
Researchers divided the strabismus group into those with esotropia, where the eyes turn inward (52.2%), exotropia, where they turn outward (46.3%), and hypertropia, where one eye wanders upward (12.5%). Investigators found that all three conditions were associated with increased risk of anxiety disorder, depressive disorder, bipolar disorders, and schizophrenia.
Investigators note that rates in the current study were lower than in previous studies, which showed that children with congenital esotropia were 2.6 times more likely to receive a mental health diagnosis, and children with intermittent exotropia were 2.7 times more likely to receive a mental health diagnosis.
“It is probable that our study found a lower risk than these studies, because our study was cross-sectional and claims based, whereas these studies observed the children to early adulthood and were based on medical records,” the investigators note.
It’s impossible to determine from this study how strabismus is connected to mental illness. However, Dr. Pineles believes depression and anxiety might be tied to strabismus via teasing, which affects self-esteem, although genetics could also play a role. For conditions such as schizophrenia, a shared genetic link with strabismus might be more likely, she added.
“Schizophrenia is a pretty severe diagnosis, so just being teased or having poor self-esteem is probably not enough” to develop schizophrenia.
Based on her clinical experience, Dr. Pineles said that realigning the eyes of patients with milder forms of depression or anxiety “definitely anecdotally helps these patients a lot.”
Dr. Pineles and colleagues have another paper in press that examines mental illnesses and other serious eye disorders in children and shows similar findings, she said.
Implications for insurance coverage?
In an accompanying editorial, experts, led by S. Grace Prakalapakorn, MD, department of ophthalmology and pediatrics, Duke University Medical Center, Durham, N.C., noted the exclusion of children covered under government insurance or without insurance is an important study limitation, largely because socioeconomic status is a risk factor for poor mental health.
The editorialists point to studies showing that surgical correction of ocular misalignments may be associated with reduced anxiety and depression. However, health insurance coverage for such surgical correction “may not be available owing to a misconception that these conditions are ‘cosmetic’.”
Evidence of the broader association of strabismus with physical and mental health “may play an important role in shifting policy to promote insurance coverage for timely strabismus care,” they write.
As many mental health disorders begin in childhood or adolescence, “it is paramount to identify, address, and, if possible, prevent mental health disorders at a young age, because failure to intervene in a timely fashion can have lifelong health consequences,” say Dr. Prakalapakorn and colleagues.
With mental health conditions and disorders increasing worldwide, compounded by the stressors of the COVID-19 pandemic, additional studies are needed to explore the causal relationships between ocular and psychiatric phenomena, their treatment, and outcomes, they add.
The study was supported by a grant from the National Eye Institute and an unrestricted grant from Research to Prevent Blindness. Dr. Pineles has reported no relevant conflicts of interest. Commentary author Manpreet K. Singh, MD, has reported receiving research support from Stanford’s Maternal Child Health Research Institute and Stanford’s Department of Psychiatry and Behavioral Sciences, the National Institute of Mental Health, the National Institute on Aging, the Patient-Centered Outcomes Research Institute, Johnson & Johnson, Allergan, and the Brain and Behavior Research Foundation; serving on the advisory board for Sunovion and Skyland Trail; serving as a consultant for Johnson & Johnson; previously serving as a consultant for X, the moonshot factory, Alphabet, and Limbix Health; receiving honoraria from the American Academy of Child and Adolescent Psychiatry; and receiving royalties from American Psychiatric Association Publishing and Thrive Global. Commentary author Nathan Congdon, MD, has reported receiving personal fees from Belkin Vision outside the submitted work.
A version of this article first appeared on Medscape.com.
Misaligned eyes in children are associated with an increased prevalence of mental illness, results of a large study suggest.
“Psychiatrists who have a patient with depression or anxiety and notice that patient also has strabismus might think about the link between those two conditions and refer that patient,” study investigator Stacy L. Pineles, MD, professor, department of ophthalmology, University of California, Los Angeles, told this news organization.
The study was published online March 10 in JAMA Ophthalmology.
A common condition
Strabismus, a condition in which the eyes don’t line up or are “crossed,” is one of the most common eye diseases in children, with some estimates suggesting it affects more than 1.5 million American youth.
Patients with strabismus have problems making eye contact and are affected socially and functionally, said Dr. Pineles. They’re often met with a negative bias, as shown by children’s responses to pictures of faces with and without strabismus, she said.
There is a signal from previous research suggesting that strabismus is linked to a higher risk of mental illness. However, most of these studies were small and had relatively homogenous populations, said Dr. Pineles.
The new study includes over 12 million children (mean age, 8.0 years) from a private health insurance claims database that represents diverse races and ethnicities as well as geographic regions across the United States.
The sample included 352,636 children with strabismus and 11,652,553 children with no diagnosed eye disease who served as controls. Most participants were White (51.6%), came from a family with an annual household income of $40,000 or more (51.0%), had point-of-service insurance (68.7%), and had at least one comorbid condition (64.5%).
The study evaluated five mental illness diagnoses. These included anxiety disorder, depressive disorder, substance use or addictive disorder, bipolar disorder, and schizophrenia.
Overall, children with strabismus had a higher prevalence of all these illnesses, with the exception of substance use disorder.
After adjusting for age, sex, race and ethnicity, census region, education level of caregiver, family net worth, and presence of at least one comorbid condition, the odds ratios among those with versus without strabismus were: 2.01 (95% confidence interval, 1.99-2.04; P < .001) for anxiety disorder, 1.83 (95% CI, 1.76-1.90; P < .001) for schizophrenia, 1.64 (95% CI, 1.59-1.70; P < .001) for bipolar disorder, and 1.61 (95% CI, 1.59-1.63; P < .001) for depressive disorder.
Substance use disorder had a negative unadjusted association with strabismus, but after adjustment for confounders, the association was not significant (OR, 0.99; 95% CI, 0.97-1.02; P = .48).
Dr. Pineles noted that the study participants, who were all under age 19, may be too young to have substance use disorders.
The results for substance use disorders provided something of an “internal control” and reaffirmed results for the other four conditions, said Dr. Pineles.
“When you do research on such a large database, you’re very likely to find significant associations; the dataset is so large that even very small differences become statistically significant. It was interesting that not everything gave us a positive association.”
Researchers divided the strabismus group into those with esotropia, where the eyes turn inward (52.2%), exotropia, where they turn outward (46.3%), and hypertropia, where one eye wanders upward (12.5%). Investigators found that all three conditions were associated with increased risk of anxiety disorder, depressive disorder, bipolar disorders, and schizophrenia.
Investigators note that rates in the current study were lower than in previous studies, which showed that children with congenital esotropia were 2.6 times more likely to receive a mental health diagnosis, and children with intermittent exotropia were 2.7 times more likely to receive a mental health diagnosis.
“It is probable that our study found a lower risk than these studies, because our study was cross-sectional and claims based, whereas these studies observed the children to early adulthood and were based on medical records,” the investigators note.
It’s impossible to determine from this study how strabismus is connected to mental illness. However, Dr. Pineles believes depression and anxiety might be tied to strabismus via teasing, which affects self-esteem, although genetics could also play a role. For conditions such as schizophrenia, a shared genetic link with strabismus might be more likely, she added.
“Schizophrenia is a pretty severe diagnosis, so just being teased or having poor self-esteem is probably not enough” to develop schizophrenia.
Based on her clinical experience, Dr. Pineles said that realigning the eyes of patients with milder forms of depression or anxiety “definitely anecdotally helps these patients a lot.”
Dr. Pineles and colleagues have another paper in press that examines mental illnesses and other serious eye disorders in children and shows similar findings, she said.
Implications for insurance coverage?
In an accompanying editorial, experts, led by S. Grace Prakalapakorn, MD, department of ophthalmology and pediatrics, Duke University Medical Center, Durham, N.C., noted the exclusion of children covered under government insurance or without insurance is an important study limitation, largely because socioeconomic status is a risk factor for poor mental health.
The editorialists point to studies showing that surgical correction of ocular misalignments may be associated with reduced anxiety and depression. However, health insurance coverage for such surgical correction “may not be available owing to a misconception that these conditions are ‘cosmetic’.”
Evidence of the broader association of strabismus with physical and mental health “may play an important role in shifting policy to promote insurance coverage for timely strabismus care,” they write.
As many mental health disorders begin in childhood or adolescence, “it is paramount to identify, address, and, if possible, prevent mental health disorders at a young age, because failure to intervene in a timely fashion can have lifelong health consequences,” say Dr. Prakalapakorn and colleagues.
With mental health conditions and disorders increasing worldwide, compounded by the stressors of the COVID-19 pandemic, additional studies are needed to explore the causal relationships between ocular and psychiatric phenomena, their treatment, and outcomes, they add.
The study was supported by a grant from the National Eye Institute and an unrestricted grant from Research to Prevent Blindness. Dr. Pineles has reported no relevant conflicts of interest. Commentary author Manpreet K. Singh, MD, has reported receiving research support from Stanford’s Maternal Child Health Research Institute and Stanford’s Department of Psychiatry and Behavioral Sciences, the National Institute of Mental Health, the National Institute on Aging, the Patient-Centered Outcomes Research Institute, Johnson & Johnson, Allergan, and the Brain and Behavior Research Foundation; serving on the advisory board for Sunovion and Skyland Trail; serving as a consultant for Johnson & Johnson; previously serving as a consultant for X, the moonshot factory, Alphabet, and Limbix Health; receiving honoraria from the American Academy of Child and Adolescent Psychiatry; and receiving royalties from American Psychiatric Association Publishing and Thrive Global. Commentary author Nathan Congdon, MD, has reported receiving personal fees from Belkin Vision outside the submitted work.
A version of this article first appeared on Medscape.com.
‘Alarming’ worldwide decline in mental health
The Mental Health Million project of Sapien Labs issued its second report, published online March 15, encompassing 34 countries and over 220,000 Internet-enabled adults. It found a continued decline in mental health in all age groups and genders, with English-speaking countries having the lowest mental well-being.
The decline was significantly correlated with the stringency of COVID-19 lockdown measures in each country and was directionally correlated to the cases and deaths per million.
The youngest age group (18-24 years) reported the poorest mental well-being, with better mental health scores rising in every successively older age group.
“Some of our findings, especially regarding mental health in young adults, are alarming,” Tara Thiagarajan, PhD, Sapien Labs founder and chief scientist, told this news organization.
“Our data, which are continually updated in real time, are freely available for nonprofit, noncommercial use and research, and we hope that researchers will get involved in an interdisciplinary way that spans sociology, economics, psychiatry, and other fields,” she said.
Pioneering research
Dr. Thiagarajan and her team pioneered the Mental Health Million project, an ongoing research initiative utilizing a “free and anonymous assessment tool,” the Mental Health Quotient (MHQ), which “encompasses a comprehensive view of our emotional, social, and cognitive function and capability.”
The MHQ consists of 47 “elements of mental well-being,” with scores ranging from –100 to +200. (Negative scores indicate poorer mental well-being.) The MHQ categorizes respondents as “clinical, at-risk, enduring, managing, succeeding, and thriving” and computes scores on the basis of six broad dimensions of mental health: core cognition, complex cognition, mood and outlook, drive and motivation, social self, and mind-body connection.
As reported by this news organization, Sapien Lab’s first Mental Health State of the World report (n = 49,000 adults) was conducted in eight English-speaking countries in 2020. Participants were compared to a smaller sample of people from the same countries polled in 2019.
In this year’s report, “we expanded quite substantially,” Dr. Thiagarajan said. The project added Spanish, French, and Arabic and recruited participants from 34 countries on six continents (n = 223,087) via advertising on Google and Facebook.
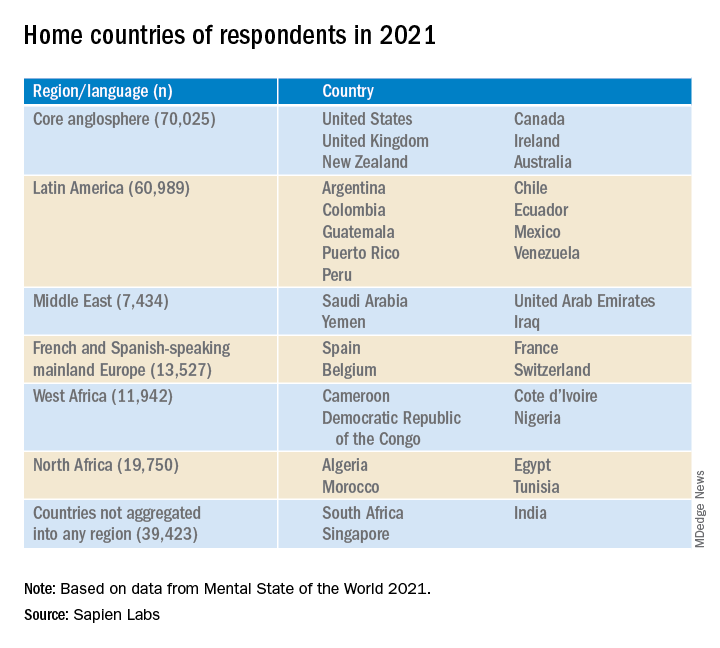
Economic prosperity not protective
Across the eight English-speaking countries, there was a decline in mental well-being of 3% from 2020 to 2021, which was smaller than the 8% decline from 2019 to 2020. The percentage of people who were “distressed or struggling” increased from 26% to 30% in 2021.
“Now that a lot of pandemic issue seems to be easing up, I hope we’ll see mental well-being coming back up, but at least it’s a smaller decline than we saw between 2019 and 2020,” said Dr. Thiagarajan.
The decline across countries from 2019 to 2021 was significantly correlated with the stringency of governmental COVID-19-related measures (based on the Oxford COVID-19 Government Response Tracker, 2022; r = .54) and directionally correlated to the cases and deaths per million.
In total, 30% of respondents in English-speaking countries had mental well-being scores in the “distressed” or “struggling” range – higher than the Middle Eastern countries, North Africa, Latin America, and Europe (23%, 23%, 24%, and 18%, respectively).
Only 36% of participants in the English-speaking countries, the Middle East, and North Africa reported “thriving or succeeding,” vs. 45% and 46% in Latin America and Europe, respectively. Venezuela topped the list with an average MHQ of 91, while the United Kingdom and South Africa had the lowest scores, at 46 each.
Mental well-being was slightly higher in males than in females but was dramatically lower in nonbinary/third-gender respondents. In fact, those identifying as nonbinary/third gender had the lowest mental well-being of any group.
Across all countries and languages, higher education was associated with better mental well-being. Employment was also associated with superior mental well-being, compared with being unemployed – particularly in core English-speaking countries.
However, “country indicators of economic prosperity were negatively correlated with mental well-being, particularly for young adults and males, belying the commonly held belief that national economic prosperity translates into greater mental well-being,” said Dr. Thiagarajan.
‘Stark’ contrast
The most dramatic finding was the difference in mental well-being between younger and older adults, which was two- to threefold larger than differences in other dimensions (for example, age, gender, employment). Even the maximum difference between countries overall (15%) was still smaller than the generational gap within any region.
While only 7% (6%- 9%) of participants aged ≥65 years were “distressed and struggling” with their mental well-being to a “clinical” extent, 44% (38%-50%) of those aged 18-24 years reported mental well-being scores in the “distressed or struggling” range – representing a “growing gap between generations that, while present prior to the COVID-19 pandemic, has since been exacerbated,” the authors state.
With every successive decrement in age group, mental well-being “plummeted,” Dr. Thiagarajan said. She noted that research conducted prior to 2010 in several regions of the world showed that young adults typically had the highest well-being. “Our findings stand in stark contrast to these previous patterns.”
The relationship between lockdown stringency and poorer mental health could play a role. “The impact of social isolation may be most strongly felt in younger people,” she said.
Internet a culprit?
“Within almost every region, scores for cognition and drive and motivation were highest while mood and outlook and social self were the lowest,” the authors report.
The aggregate percentage of respondents who reported being “distressed or struggling” in the various MHQ dimensions is shown in the following table.
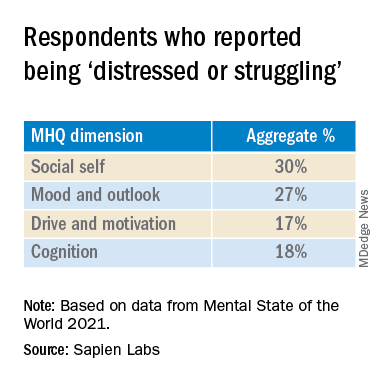
In particular, English-speaking countries scored lowest on the social self scale.
The sense of social self is “how you see yourself with respect to others, how you relate to others and the ability to form strong, stable relationships and maintain them with other people,” said Dr. Thiagarajan.
Internet use might account for the “massive” difference between the youngest and the oldest generations, she suggested. “Following 2010, mobile phone penetration picked up and rose rapidly. ... Mobile phones took over the world.”
Time spent on the Internet – an estimated 7-10 hours per day – “eats into the time people in older generations used in building the social self. Kids who grow up on the Internet are losing thousands of hours in social interactions, which is challenging their ability to form relationships, how they see themselves, and how they fit into the social fabric,” Dr. Thiagarajan added
Sedentary time
Commenting for this news organization, Bernardo Ng, MD, a member of the American Psychiatric Association’s Council on International Psychiatry and Global Health and medical director of Sun Valley Research Center, Imperial, Calif., called the report “interesting, with an impressive sample size” and an “impressive geographic distribution.”
Dr. Ng, who was not involved in the report, said, “I did not think the impact of Internet use on mental health was as dramatic before looking at this report.
“On the other hand, I have personally been interested in the impact of sedentarism in mental health – not only emotionally but also biologically. Sedentarism, which is directly related to screen use time, produces inflammation that worsens brain function.”
Also commenting, Ken Duckworth, MD, chief medical officer of the National Alliance of Mental Illness, called the survey “extremely well timed and creative, although it looked only at Internet-enabled populations, so one cannot make too many overall pronouncements, because a lot of people don’t have access to the Internet.”
The data regarding young people are particularly powerful. “The idea that young people are having a decrease in their experience of mental health across the world is something I haven’t seen before.”
Dr. Duckworth suggested the reason might “have to do with the impact of the COVID lockdown on normal development that young people go through, while older people don’t struggle with these developmental challenges in the same way.”
A version of this article first appeared on Medscape.com.
The Mental Health Million project of Sapien Labs issued its second report, published online March 15, encompassing 34 countries and over 220,000 Internet-enabled adults. It found a continued decline in mental health in all age groups and genders, with English-speaking countries having the lowest mental well-being.
The decline was significantly correlated with the stringency of COVID-19 lockdown measures in each country and was directionally correlated to the cases and deaths per million.
The youngest age group (18-24 years) reported the poorest mental well-being, with better mental health scores rising in every successively older age group.
“Some of our findings, especially regarding mental health in young adults, are alarming,” Tara Thiagarajan, PhD, Sapien Labs founder and chief scientist, told this news organization.
“Our data, which are continually updated in real time, are freely available for nonprofit, noncommercial use and research, and we hope that researchers will get involved in an interdisciplinary way that spans sociology, economics, psychiatry, and other fields,” she said.
Pioneering research
Dr. Thiagarajan and her team pioneered the Mental Health Million project, an ongoing research initiative utilizing a “free and anonymous assessment tool,” the Mental Health Quotient (MHQ), which “encompasses a comprehensive view of our emotional, social, and cognitive function and capability.”
The MHQ consists of 47 “elements of mental well-being,” with scores ranging from –100 to +200. (Negative scores indicate poorer mental well-being.) The MHQ categorizes respondents as “clinical, at-risk, enduring, managing, succeeding, and thriving” and computes scores on the basis of six broad dimensions of mental health: core cognition, complex cognition, mood and outlook, drive and motivation, social self, and mind-body connection.
As reported by this news organization, Sapien Lab’s first Mental Health State of the World report (n = 49,000 adults) was conducted in eight English-speaking countries in 2020. Participants were compared to a smaller sample of people from the same countries polled in 2019.
In this year’s report, “we expanded quite substantially,” Dr. Thiagarajan said. The project added Spanish, French, and Arabic and recruited participants from 34 countries on six continents (n = 223,087) via advertising on Google and Facebook.
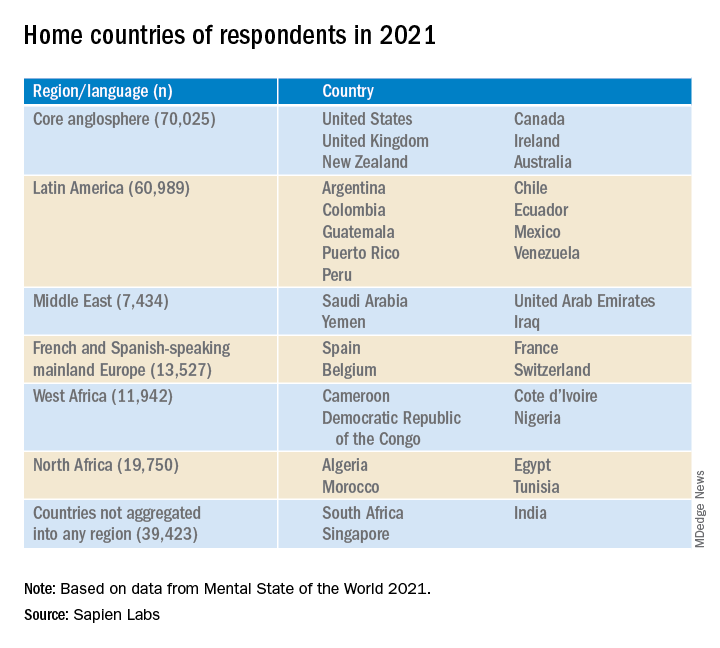
Economic prosperity not protective
Across the eight English-speaking countries, there was a decline in mental well-being of 3% from 2020 to 2021, which was smaller than the 8% decline from 2019 to 2020. The percentage of people who were “distressed or struggling” increased from 26% to 30% in 2021.
“Now that a lot of pandemic issue seems to be easing up, I hope we’ll see mental well-being coming back up, but at least it’s a smaller decline than we saw between 2019 and 2020,” said Dr. Thiagarajan.
The decline across countries from 2019 to 2021 was significantly correlated with the stringency of governmental COVID-19-related measures (based on the Oxford COVID-19 Government Response Tracker, 2022; r = .54) and directionally correlated to the cases and deaths per million.
In total, 30% of respondents in English-speaking countries had mental well-being scores in the “distressed” or “struggling” range – higher than the Middle Eastern countries, North Africa, Latin America, and Europe (23%, 23%, 24%, and 18%, respectively).
Only 36% of participants in the English-speaking countries, the Middle East, and North Africa reported “thriving or succeeding,” vs. 45% and 46% in Latin America and Europe, respectively. Venezuela topped the list with an average MHQ of 91, while the United Kingdom and South Africa had the lowest scores, at 46 each.
Mental well-being was slightly higher in males than in females but was dramatically lower in nonbinary/third-gender respondents. In fact, those identifying as nonbinary/third gender had the lowest mental well-being of any group.
Across all countries and languages, higher education was associated with better mental well-being. Employment was also associated with superior mental well-being, compared with being unemployed – particularly in core English-speaking countries.
However, “country indicators of economic prosperity were negatively correlated with mental well-being, particularly for young adults and males, belying the commonly held belief that national economic prosperity translates into greater mental well-being,” said Dr. Thiagarajan.
‘Stark’ contrast
The most dramatic finding was the difference in mental well-being between younger and older adults, which was two- to threefold larger than differences in other dimensions (for example, age, gender, employment). Even the maximum difference between countries overall (15%) was still smaller than the generational gap within any region.
While only 7% (6%- 9%) of participants aged ≥65 years were “distressed and struggling” with their mental well-being to a “clinical” extent, 44% (38%-50%) of those aged 18-24 years reported mental well-being scores in the “distressed or struggling” range – representing a “growing gap between generations that, while present prior to the COVID-19 pandemic, has since been exacerbated,” the authors state.
With every successive decrement in age group, mental well-being “plummeted,” Dr. Thiagarajan said. She noted that research conducted prior to 2010 in several regions of the world showed that young adults typically had the highest well-being. “Our findings stand in stark contrast to these previous patterns.”
The relationship between lockdown stringency and poorer mental health could play a role. “The impact of social isolation may be most strongly felt in younger people,” she said.
Internet a culprit?
“Within almost every region, scores for cognition and drive and motivation were highest while mood and outlook and social self were the lowest,” the authors report.
The aggregate percentage of respondents who reported being “distressed or struggling” in the various MHQ dimensions is shown in the following table.
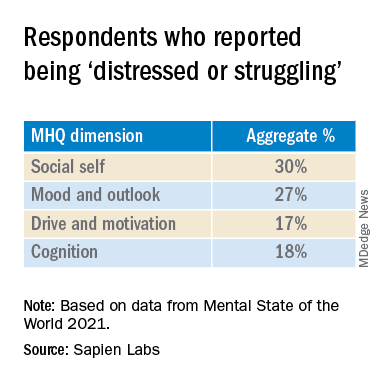
In particular, English-speaking countries scored lowest on the social self scale.
The sense of social self is “how you see yourself with respect to others, how you relate to others and the ability to form strong, stable relationships and maintain them with other people,” said Dr. Thiagarajan.
Internet use might account for the “massive” difference between the youngest and the oldest generations, she suggested. “Following 2010, mobile phone penetration picked up and rose rapidly. ... Mobile phones took over the world.”
Time spent on the Internet – an estimated 7-10 hours per day – “eats into the time people in older generations used in building the social self. Kids who grow up on the Internet are losing thousands of hours in social interactions, which is challenging their ability to form relationships, how they see themselves, and how they fit into the social fabric,” Dr. Thiagarajan added
Sedentary time
Commenting for this news organization, Bernardo Ng, MD, a member of the American Psychiatric Association’s Council on International Psychiatry and Global Health and medical director of Sun Valley Research Center, Imperial, Calif., called the report “interesting, with an impressive sample size” and an “impressive geographic distribution.”
Dr. Ng, who was not involved in the report, said, “I did not think the impact of Internet use on mental health was as dramatic before looking at this report.
“On the other hand, I have personally been interested in the impact of sedentarism in mental health – not only emotionally but also biologically. Sedentarism, which is directly related to screen use time, produces inflammation that worsens brain function.”
Also commenting, Ken Duckworth, MD, chief medical officer of the National Alliance of Mental Illness, called the survey “extremely well timed and creative, although it looked only at Internet-enabled populations, so one cannot make too many overall pronouncements, because a lot of people don’t have access to the Internet.”
The data regarding young people are particularly powerful. “The idea that young people are having a decrease in their experience of mental health across the world is something I haven’t seen before.”
Dr. Duckworth suggested the reason might “have to do with the impact of the COVID lockdown on normal development that young people go through, while older people don’t struggle with these developmental challenges in the same way.”
A version of this article first appeared on Medscape.com.
The Mental Health Million project of Sapien Labs issued its second report, published online March 15, encompassing 34 countries and over 220,000 Internet-enabled adults. It found a continued decline in mental health in all age groups and genders, with English-speaking countries having the lowest mental well-being.
The decline was significantly correlated with the stringency of COVID-19 lockdown measures in each country and was directionally correlated to the cases and deaths per million.
The youngest age group (18-24 years) reported the poorest mental well-being, with better mental health scores rising in every successively older age group.
“Some of our findings, especially regarding mental health in young adults, are alarming,” Tara Thiagarajan, PhD, Sapien Labs founder and chief scientist, told this news organization.
“Our data, which are continually updated in real time, are freely available for nonprofit, noncommercial use and research, and we hope that researchers will get involved in an interdisciplinary way that spans sociology, economics, psychiatry, and other fields,” she said.
Pioneering research
Dr. Thiagarajan and her team pioneered the Mental Health Million project, an ongoing research initiative utilizing a “free and anonymous assessment tool,” the Mental Health Quotient (MHQ), which “encompasses a comprehensive view of our emotional, social, and cognitive function and capability.”
The MHQ consists of 47 “elements of mental well-being,” with scores ranging from –100 to +200. (Negative scores indicate poorer mental well-being.) The MHQ categorizes respondents as “clinical, at-risk, enduring, managing, succeeding, and thriving” and computes scores on the basis of six broad dimensions of mental health: core cognition, complex cognition, mood and outlook, drive and motivation, social self, and mind-body connection.
As reported by this news organization, Sapien Lab’s first Mental Health State of the World report (n = 49,000 adults) was conducted in eight English-speaking countries in 2020. Participants were compared to a smaller sample of people from the same countries polled in 2019.
In this year’s report, “we expanded quite substantially,” Dr. Thiagarajan said. The project added Spanish, French, and Arabic and recruited participants from 34 countries on six continents (n = 223,087) via advertising on Google and Facebook.
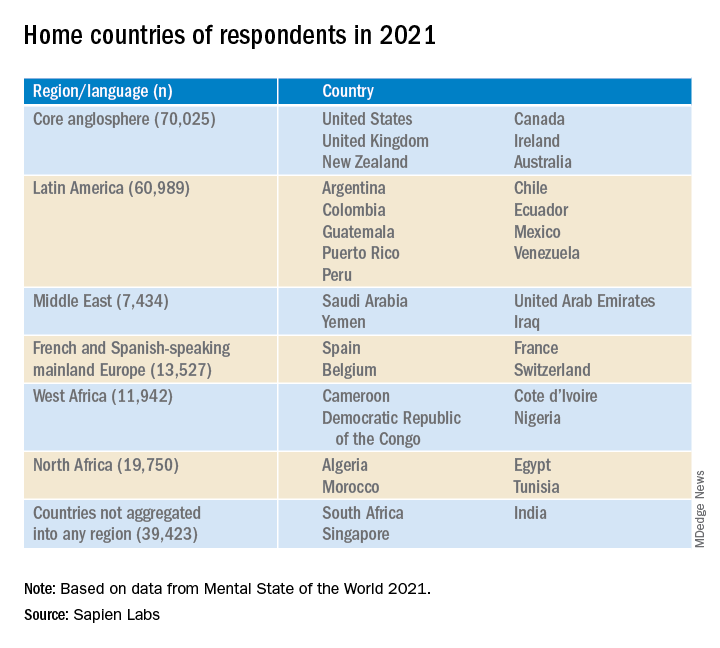
Economic prosperity not protective
Across the eight English-speaking countries, there was a decline in mental well-being of 3% from 2020 to 2021, which was smaller than the 8% decline from 2019 to 2020. The percentage of people who were “distressed or struggling” increased from 26% to 30% in 2021.
“Now that a lot of pandemic issue seems to be easing up, I hope we’ll see mental well-being coming back up, but at least it’s a smaller decline than we saw between 2019 and 2020,” said Dr. Thiagarajan.
The decline across countries from 2019 to 2021 was significantly correlated with the stringency of governmental COVID-19-related measures (based on the Oxford COVID-19 Government Response Tracker, 2022; r = .54) and directionally correlated to the cases and deaths per million.
In total, 30% of respondents in English-speaking countries had mental well-being scores in the “distressed” or “struggling” range – higher than the Middle Eastern countries, North Africa, Latin America, and Europe (23%, 23%, 24%, and 18%, respectively).
Only 36% of participants in the English-speaking countries, the Middle East, and North Africa reported “thriving or succeeding,” vs. 45% and 46% in Latin America and Europe, respectively. Venezuela topped the list with an average MHQ of 91, while the United Kingdom and South Africa had the lowest scores, at 46 each.
Mental well-being was slightly higher in males than in females but was dramatically lower in nonbinary/third-gender respondents. In fact, those identifying as nonbinary/third gender had the lowest mental well-being of any group.
Across all countries and languages, higher education was associated with better mental well-being. Employment was also associated with superior mental well-being, compared with being unemployed – particularly in core English-speaking countries.
However, “country indicators of economic prosperity were negatively correlated with mental well-being, particularly for young adults and males, belying the commonly held belief that national economic prosperity translates into greater mental well-being,” said Dr. Thiagarajan.
‘Stark’ contrast
The most dramatic finding was the difference in mental well-being between younger and older adults, which was two- to threefold larger than differences in other dimensions (for example, age, gender, employment). Even the maximum difference between countries overall (15%) was still smaller than the generational gap within any region.
While only 7% (6%- 9%) of participants aged ≥65 years were “distressed and struggling” with their mental well-being to a “clinical” extent, 44% (38%-50%) of those aged 18-24 years reported mental well-being scores in the “distressed or struggling” range – representing a “growing gap between generations that, while present prior to the COVID-19 pandemic, has since been exacerbated,” the authors state.
With every successive decrement in age group, mental well-being “plummeted,” Dr. Thiagarajan said. She noted that research conducted prior to 2010 in several regions of the world showed that young adults typically had the highest well-being. “Our findings stand in stark contrast to these previous patterns.”
The relationship between lockdown stringency and poorer mental health could play a role. “The impact of social isolation may be most strongly felt in younger people,” she said.
Internet a culprit?
“Within almost every region, scores for cognition and drive and motivation were highest while mood and outlook and social self were the lowest,” the authors report.
The aggregate percentage of respondents who reported being “distressed or struggling” in the various MHQ dimensions is shown in the following table.
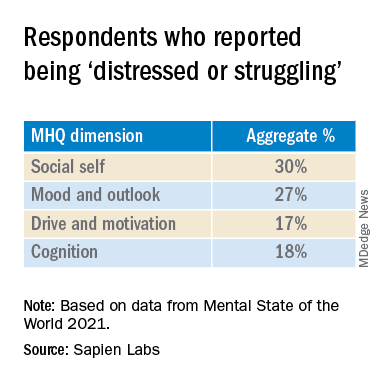
In particular, English-speaking countries scored lowest on the social self scale.
The sense of social self is “how you see yourself with respect to others, how you relate to others and the ability to form strong, stable relationships and maintain them with other people,” said Dr. Thiagarajan.
Internet use might account for the “massive” difference between the youngest and the oldest generations, she suggested. “Following 2010, mobile phone penetration picked up and rose rapidly. ... Mobile phones took over the world.”
Time spent on the Internet – an estimated 7-10 hours per day – “eats into the time people in older generations used in building the social self. Kids who grow up on the Internet are losing thousands of hours in social interactions, which is challenging their ability to form relationships, how they see themselves, and how they fit into the social fabric,” Dr. Thiagarajan added
Sedentary time
Commenting for this news organization, Bernardo Ng, MD, a member of the American Psychiatric Association’s Council on International Psychiatry and Global Health and medical director of Sun Valley Research Center, Imperial, Calif., called the report “interesting, with an impressive sample size” and an “impressive geographic distribution.”
Dr. Ng, who was not involved in the report, said, “I did not think the impact of Internet use on mental health was as dramatic before looking at this report.
“On the other hand, I have personally been interested in the impact of sedentarism in mental health – not only emotionally but also biologically. Sedentarism, which is directly related to screen use time, produces inflammation that worsens brain function.”
Also commenting, Ken Duckworth, MD, chief medical officer of the National Alliance of Mental Illness, called the survey “extremely well timed and creative, although it looked only at Internet-enabled populations, so one cannot make too many overall pronouncements, because a lot of people don’t have access to the Internet.”
The data regarding young people are particularly powerful. “The idea that young people are having a decrease in their experience of mental health across the world is something I haven’t seen before.”
Dr. Duckworth suggested the reason might “have to do with the impact of the COVID lockdown on normal development that young people go through, while older people don’t struggle with these developmental challenges in the same way.”
A version of this article first appeared on Medscape.com.
Standard of care in suicide prevention in pediatrics: A review of the Blueprint for Youth Suicide Prevention
In March, an unprecedented collaboration between the American Academy of Pediatrics (AAP), American Foundation for Suicide Prevention (AFSP), and National Institute of Mental Health (NIMH) resulted in the development of the Blueprint for Youth Suicide Prevention. The blueprint comprises a consensus summary of expert recommendations, educational resources, and specific and practical strategies for pediatricians and other health care providers to support youth at risk for suicide in pediatric primary care settings. It is ambitious and far-reaching in scope and speaks to the growing understanding that suicide care pathways offer a clear ray of hope toward a shared “zero suicide” goal.
Following the declaration of a national emergency for child and adolescent mental health, the blueprint represents a resource to help us move forward during this national emergency. It offers practically focused suggestions at the clinic site and individual level, in addition to community and school levels, to tackle the deeply concerning and alarming increasing rate of emergency department visits by 30% in the last 2 pandemic years for youth suicide attempts. A reflexive visit for an emergency mental health evaluation in an emergency department after a disclosure of suicidal ideation isn’t always the next best step in a pathway to care, nor a sustainable community solution with the dearth of mental health and crisis resources nationally.
With this new tool, let’s proceed through a case of how one would approach a patient in the office setting with a concerning disclosure.
Case
Emily is a 12-year-old girl who presents for a routine well-check in your practice. Her mother shared with you before your examination that she has wondered if Emily may need more support. Since the pandemic, Emily had increasingly spent time using social media and watching television. When you meet with Emily on her own, she says, “I know that life is getting back to normal, and I am supposed to be excited for that, but now I have some anxiety about doing what I used to do. I’ve had some thoughts that it would be better to sleep forever and not wake up ...”
Case discussion
The blueprint recommends universal screening for suicide in all youths aged 12 and over. Not all children, like Emily, will be as open about their inner thoughts. The blueprint provides a link to the ASQ, which comprises questions to ascertain suicide risk and takes 20 seconds to complete with a patient. It is recommended as a first-line screening tool by the NIMH: Suicide Risk Screening Tool. This tool can guide one’s clinical thinking beyond the question of whether or not a child feels “suicidal” after a disclosure such as Emily’s. The blueprint also provides a tip sheet on how to frame these screenings to ensure their thoroughness and interpersonal effectiveness.
Case continued
You go through the ASQ with Emily and she revealed that she has had thoughts about suicide but not currently and without further plans. According to the ASQ, this screening falls into the category of a “non-acute positive screen (potential risk identified),” and now the patient requires a brief suicide safety assessment to determine if an emergency mental health evaluation is needed.
Case discussion
An initial screen (ASQ) should be followed by a Brief Suicide Safety Assessment (BSSA). Two common ones are the ASQ-BSSA (created by the same group that created the ASQ) or the C-SSRS (Columbia suicide severity rating scale).
The blueprint suggests adding this level of depth to one’s investigation in a pediatrics office for a divulged concern with suicidal ideation and following the algorithm to ensure safety.
The complete screening process is also described, in detail, in this instructional video: Suicide Risk Screening Training: How to Manage Patients at Risk for Suicide.
Case continued
Following the ASQ-BSSA, you determine that a referral to more immediate mental health resources would be most helpful and discuss your concerns with Emily and her family. You connect her via a “warm handoff” to a therapist in the office available from the newly adopted primary care mental health integration model. Emily completes further screening for anxiety and depressive disorders and begins a course of cognitive-behavioral therapy. You feel reassured that the therapist can connect with the consulting psychiatrist in the model who can offer a comprehensive psychiatric evaluation if needed. A referral to the emergency department to complete this screening has been avoided. You also plan for a “caring contact” from the office in a day to check in on Emily and her family and, before they go, provide them with crisis services and resources.
The blueprint represents a thoughtful means to know when emergency department visits are necessary and when other forms of support such as robust safety planning, a connection to other nonemergency services, and “caring contacts” from the office within 24-48 hours are actually of more benefit. “Caring contacts,” in particular, have been lauded as having a significant impact in modifying the course of a patient with suicidal ideation. Data show that differences such as follow-up phone calls by any staff member or even postcards from the clinic over 6-12 months can affect suicide risk.
Beyond outlining suicide care pathways, the blueprint also shares clinical algorithms from the National Network of Child Psychiatry Access Programs (NNCPAP). These algorithms help clinicians assess common issues in pediatrics and reserve referrals to psychiatry and escalations of care to the emergency department for certain high-risk circumstances.
The blueprint seeks to provide a “one-stop-shop” for accessible and usable resources in the clinic workflow for suicide prevention. It is inspiring to see our professional organizations pursuing practical and practice-based solutions to our children’s mental health crisis in unison.
Dr. Pawlowski is a child and adolescent consulting psychiatrist. She is a division chief at the University of Vermont Medical Center where she focuses on primary care mental health integration within primary care pediatrics, internal medicine, and family medicine. Email her at [email protected].
In March, an unprecedented collaboration between the American Academy of Pediatrics (AAP), American Foundation for Suicide Prevention (AFSP), and National Institute of Mental Health (NIMH) resulted in the development of the Blueprint for Youth Suicide Prevention. The blueprint comprises a consensus summary of expert recommendations, educational resources, and specific and practical strategies for pediatricians and other health care providers to support youth at risk for suicide in pediatric primary care settings. It is ambitious and far-reaching in scope and speaks to the growing understanding that suicide care pathways offer a clear ray of hope toward a shared “zero suicide” goal.
Following the declaration of a national emergency for child and adolescent mental health, the blueprint represents a resource to help us move forward during this national emergency. It offers practically focused suggestions at the clinic site and individual level, in addition to community and school levels, to tackle the deeply concerning and alarming increasing rate of emergency department visits by 30% in the last 2 pandemic years for youth suicide attempts. A reflexive visit for an emergency mental health evaluation in an emergency department after a disclosure of suicidal ideation isn’t always the next best step in a pathway to care, nor a sustainable community solution with the dearth of mental health and crisis resources nationally.
With this new tool, let’s proceed through a case of how one would approach a patient in the office setting with a concerning disclosure.
Case
Emily is a 12-year-old girl who presents for a routine well-check in your practice. Her mother shared with you before your examination that she has wondered if Emily may need more support. Since the pandemic, Emily had increasingly spent time using social media and watching television. When you meet with Emily on her own, she says, “I know that life is getting back to normal, and I am supposed to be excited for that, but now I have some anxiety about doing what I used to do. I’ve had some thoughts that it would be better to sleep forever and not wake up ...”
Case discussion
The blueprint recommends universal screening for suicide in all youths aged 12 and over. Not all children, like Emily, will be as open about their inner thoughts. The blueprint provides a link to the ASQ, which comprises questions to ascertain suicide risk and takes 20 seconds to complete with a patient. It is recommended as a first-line screening tool by the NIMH: Suicide Risk Screening Tool. This tool can guide one’s clinical thinking beyond the question of whether or not a child feels “suicidal” after a disclosure such as Emily’s. The blueprint also provides a tip sheet on how to frame these screenings to ensure their thoroughness and interpersonal effectiveness.
Case continued
You go through the ASQ with Emily and she revealed that she has had thoughts about suicide but not currently and without further plans. According to the ASQ, this screening falls into the category of a “non-acute positive screen (potential risk identified),” and now the patient requires a brief suicide safety assessment to determine if an emergency mental health evaluation is needed.
Case discussion
An initial screen (ASQ) should be followed by a Brief Suicide Safety Assessment (BSSA). Two common ones are the ASQ-BSSA (created by the same group that created the ASQ) or the C-SSRS (Columbia suicide severity rating scale).
The blueprint suggests adding this level of depth to one’s investigation in a pediatrics office for a divulged concern with suicidal ideation and following the algorithm to ensure safety.
The complete screening process is also described, in detail, in this instructional video: Suicide Risk Screening Training: How to Manage Patients at Risk for Suicide.
Case continued
Following the ASQ-BSSA, you determine that a referral to more immediate mental health resources would be most helpful and discuss your concerns with Emily and her family. You connect her via a “warm handoff” to a therapist in the office available from the newly adopted primary care mental health integration model. Emily completes further screening for anxiety and depressive disorders and begins a course of cognitive-behavioral therapy. You feel reassured that the therapist can connect with the consulting psychiatrist in the model who can offer a comprehensive psychiatric evaluation if needed. A referral to the emergency department to complete this screening has been avoided. You also plan for a “caring contact” from the office in a day to check in on Emily and her family and, before they go, provide them with crisis services and resources.
The blueprint represents a thoughtful means to know when emergency department visits are necessary and when other forms of support such as robust safety planning, a connection to other nonemergency services, and “caring contacts” from the office within 24-48 hours are actually of more benefit. “Caring contacts,” in particular, have been lauded as having a significant impact in modifying the course of a patient with suicidal ideation. Data show that differences such as follow-up phone calls by any staff member or even postcards from the clinic over 6-12 months can affect suicide risk.
Beyond outlining suicide care pathways, the blueprint also shares clinical algorithms from the National Network of Child Psychiatry Access Programs (NNCPAP). These algorithms help clinicians assess common issues in pediatrics and reserve referrals to psychiatry and escalations of care to the emergency department for certain high-risk circumstances.
The blueprint seeks to provide a “one-stop-shop” for accessible and usable resources in the clinic workflow for suicide prevention. It is inspiring to see our professional organizations pursuing practical and practice-based solutions to our children’s mental health crisis in unison.
Dr. Pawlowski is a child and adolescent consulting psychiatrist. She is a division chief at the University of Vermont Medical Center where she focuses on primary care mental health integration within primary care pediatrics, internal medicine, and family medicine. Email her at [email protected].
In March, an unprecedented collaboration between the American Academy of Pediatrics (AAP), American Foundation for Suicide Prevention (AFSP), and National Institute of Mental Health (NIMH) resulted in the development of the Blueprint for Youth Suicide Prevention. The blueprint comprises a consensus summary of expert recommendations, educational resources, and specific and practical strategies for pediatricians and other health care providers to support youth at risk for suicide in pediatric primary care settings. It is ambitious and far-reaching in scope and speaks to the growing understanding that suicide care pathways offer a clear ray of hope toward a shared “zero suicide” goal.
Following the declaration of a national emergency for child and adolescent mental health, the blueprint represents a resource to help us move forward during this national emergency. It offers practically focused suggestions at the clinic site and individual level, in addition to community and school levels, to tackle the deeply concerning and alarming increasing rate of emergency department visits by 30% in the last 2 pandemic years for youth suicide attempts. A reflexive visit for an emergency mental health evaluation in an emergency department after a disclosure of suicidal ideation isn’t always the next best step in a pathway to care, nor a sustainable community solution with the dearth of mental health and crisis resources nationally.
With this new tool, let’s proceed through a case of how one would approach a patient in the office setting with a concerning disclosure.
Case
Emily is a 12-year-old girl who presents for a routine well-check in your practice. Her mother shared with you before your examination that she has wondered if Emily may need more support. Since the pandemic, Emily had increasingly spent time using social media and watching television. When you meet with Emily on her own, she says, “I know that life is getting back to normal, and I am supposed to be excited for that, but now I have some anxiety about doing what I used to do. I’ve had some thoughts that it would be better to sleep forever and not wake up ...”
Case discussion
The blueprint recommends universal screening for suicide in all youths aged 12 and over. Not all children, like Emily, will be as open about their inner thoughts. The blueprint provides a link to the ASQ, which comprises questions to ascertain suicide risk and takes 20 seconds to complete with a patient. It is recommended as a first-line screening tool by the NIMH: Suicide Risk Screening Tool. This tool can guide one’s clinical thinking beyond the question of whether or not a child feels “suicidal” after a disclosure such as Emily’s. The blueprint also provides a tip sheet on how to frame these screenings to ensure their thoroughness and interpersonal effectiveness.
Case continued
You go through the ASQ with Emily and she revealed that she has had thoughts about suicide but not currently and without further plans. According to the ASQ, this screening falls into the category of a “non-acute positive screen (potential risk identified),” and now the patient requires a brief suicide safety assessment to determine if an emergency mental health evaluation is needed.
Case discussion
An initial screen (ASQ) should be followed by a Brief Suicide Safety Assessment (BSSA). Two common ones are the ASQ-BSSA (created by the same group that created the ASQ) or the C-SSRS (Columbia suicide severity rating scale).
The blueprint suggests adding this level of depth to one’s investigation in a pediatrics office for a divulged concern with suicidal ideation and following the algorithm to ensure safety.
The complete screening process is also described, in detail, in this instructional video: Suicide Risk Screening Training: How to Manage Patients at Risk for Suicide.
Case continued
Following the ASQ-BSSA, you determine that a referral to more immediate mental health resources would be most helpful and discuss your concerns with Emily and her family. You connect her via a “warm handoff” to a therapist in the office available from the newly adopted primary care mental health integration model. Emily completes further screening for anxiety and depressive disorders and begins a course of cognitive-behavioral therapy. You feel reassured that the therapist can connect with the consulting psychiatrist in the model who can offer a comprehensive psychiatric evaluation if needed. A referral to the emergency department to complete this screening has been avoided. You also plan for a “caring contact” from the office in a day to check in on Emily and her family and, before they go, provide them with crisis services and resources.
The blueprint represents a thoughtful means to know when emergency department visits are necessary and when other forms of support such as robust safety planning, a connection to other nonemergency services, and “caring contacts” from the office within 24-48 hours are actually of more benefit. “Caring contacts,” in particular, have been lauded as having a significant impact in modifying the course of a patient with suicidal ideation. Data show that differences such as follow-up phone calls by any staff member or even postcards from the clinic over 6-12 months can affect suicide risk.
Beyond outlining suicide care pathways, the blueprint also shares clinical algorithms from the National Network of Child Psychiatry Access Programs (NNCPAP). These algorithms help clinicians assess common issues in pediatrics and reserve referrals to psychiatry and escalations of care to the emergency department for certain high-risk circumstances.
The blueprint seeks to provide a “one-stop-shop” for accessible and usable resources in the clinic workflow for suicide prevention. It is inspiring to see our professional organizations pursuing practical and practice-based solutions to our children’s mental health crisis in unison.
Dr. Pawlowski is a child and adolescent consulting psychiatrist. She is a division chief at the University of Vermont Medical Center where she focuses on primary care mental health integration within primary care pediatrics, internal medicine, and family medicine. Email her at [email protected].
Diagnosing adolescent ADHD
Pediatricians are increasingly expert in the assessment and treatment of attention-deficit/hyperactivity disorder. But what do you do when adolescents present to your office saying they think they have ADHD? While ADHD is a common and treatable disorder of youth, it is important to take special care when assessing an adolescent. Difficulties with attention and concentration are common symptoms for many different challenges of adolescence, and for ADHD to be the underlying cause, those symptoms must have started prior to adolescence (according to DSM-5, prior to the age of 12). When your adolescent patients or their parents come to your office complaining of inattention, it is important to consider the full range of possible explanations.
Sleep
We have written in this column previously about the challenges that adolescents face in getting adequate sleep consistently. Teenagers, on average, need more than 9 hours of sleep nightly and American teenagers get fewer than 6. This mismatch is because of physiologic shifts that move their natural sleep onset time significantly later, while school still starts early. It’s often compounded by other demands on their time, including homework, extracurricular activities, and the gravitational pull of social connections. Independent teenagers make their own decisions about how to manage their time and may feel sleep is optional, or manage their fatigue with naps and caffeine, both of which will further compromise the quality and efficiency of sleep.
Chronic sleep deprivation will present with difficulties with focus, attention, memory, and cognitive performance. Treatment of this problem with stimulants is likely to make the underlying poor sleep habits even worse. When your patient presents complaining of difficulty concentrating and worsening school performance, be sure to start with a thorough sleep history, and always provide guidance about the body’s need for sleep and healthy sleep habits.
Anxiety
Anxiety disorders are the most common psychiatric illnesses of youth, with estimates of as many as 30% of children and adolescents experiencing one. The true prevalence of ADHD is estimated to be about 4% of the population. Whether social phobia, generalized anxiety disorder, or even posttraumatic stress disorder, anxiety disorders interfere with attention as ruminative worry tends to distract those experiencing it. It can also affect attention and focus indirectly by interfering with restful sleep. Anxiety disorders can be difficult to identify, as the sufferers typically internalize their symptoms. But inquire about specific worries (such as speaking in front of others, meeting new people, or an illness or accident striking themselves or a loved one) and how much time they take up. Explore if worries fill their thoughts during quiet or downtime, and explore more about their worries. You may use a screening instrument such as the Pediatric Symptom Checklist or the SCARED, both of which will indicate a likely problem with anxiety. While it is possible to have comorbid ADHD with an anxiety disorder, the anxiety disorder will likely worsen with stimulants and should be treated first. These are usually curable illnesses and you may find that remission of anxiety symptoms resolves the attentional problems.
Depression
Mood disorders are less common than anxiety disorders in youth, but far more prevalent than ADHD. And depression is usually marked by serious difficulty concentrating across settings (including for things that were previously very interesting). A sullen teenager who is deeply self-critical about school performance would benefit from exploration of associated changes in mood, interests, energy, appetite, sleep, and for feelings of worthlessness, guilt, and suicidal thoughts. The PHQ9A is a simple, free screening instrument that is reasonable to use with every sick visit (and well-check) with your adolescent patients, given the risks of undetected and untreated depression. If your patient presents complaining of poor school performance, always screen for depression. As with anxiety disorders, comorbid ADHD is possible, but it is always recommended to treat the mood disorder first and then to assess for residual ADHD symptoms once the mood disorder is in remission.
Substance abuse
Adolescence is a time of exploration, and drug and alcohol use is common. While attentional impairment will happen with intoxication, occasional or rare use should not lead to consistent impairment in school. But when parents are more worried than their children about a significant change in school performance, it is important to screen for substance abuse. A child with a secret substance use disorder will often present with behavioral changes and deteriorating school performance and might deny any drug or alcohol use to parents. Indeed, stimulants have some street value and some patients may be seeking a stimulant prescription to sell or trade for other drugs. Regular marijuana use may present with only deteriorating school performance and no irritability or other noticeable behavioral changes. Marijuana is seen as safe and even healthy by many teenagers (and even many parents), and some youth may be using it recreationally or to manage difficulties with sleep, anxiety, or mood symptoms.
But there is compelling evidence that marijuana use causes cognitive impairment, including difficulty with sustaining attention, short-term memory, and processing speed, for as long as 24 hours after use. If a teenager is using marijuana daily after school, it is certainly going to interfere, in a dose-dependent manner, with attention and cognitive function. Sustained heavy use can lead to permanent cognitive deficits. It can also trigger or worsen anxiety or mood symptoms (contrary to much popular opinion).
Gathering a thorough substance use history is essential when assessing a teenager for difficulties with focus or attention, especially when these are accompanied by change in behavior and school performance. Remember, it is critical to interview these children without their parents present to invite them to be forthcoming with you.
History
While true ADHD should have been present throughout childhood, it is possible that the symptoms have become noticeable only in adolescence. For patients with very high intelligence and lower levels of impulsivity and hyperactivity, they might easily have “flown under the radar” during their elementary and even middle school years. Their difficulties with attention and focus might become apparent only when the volume and difficulty of schoolwork both are great enough that their intelligence is not enough to get good grades. That is, their problems with executive function, prioritizing, shifting sets, and completing tasks in a timely way make it impossible to keep up good grades when the work gets harder.
Your history should reveal a long history of dreaminess or distractibility, a tendency to lose and forget things, and the other symptoms of inattention. Did they often seem to not be listening when they were younger? Forget to hand in homework? Leave chores unfinished? Leave messes behind everywhere they went? These will not be definitive, but they do reassure that symptoms may have been present for a long time, even if school performance was considered fine until the workload got too large. If such problems were not present before puberty, consider whether a subtle learning disability could be impairing them as they face more challenging academic subjects.
If you have ruled out anxiety, mood, and substance use concerns, and helped them to address a sleep deficit, then you can proceed. It is worthwhile to get Vanderbilt Assessments as you would for a younger child. If they meet criteria, discuss the risks and benefits of medication, executive skills coaching, and environmental adjustments (extra time for tests, a less stimulating environment) that can help them explore academic challenges without the discouragement that ADHD can bring.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Pediatricians are increasingly expert in the assessment and treatment of attention-deficit/hyperactivity disorder. But what do you do when adolescents present to your office saying they think they have ADHD? While ADHD is a common and treatable disorder of youth, it is important to take special care when assessing an adolescent. Difficulties with attention and concentration are common symptoms for many different challenges of adolescence, and for ADHD to be the underlying cause, those symptoms must have started prior to adolescence (according to DSM-5, prior to the age of 12). When your adolescent patients or their parents come to your office complaining of inattention, it is important to consider the full range of possible explanations.
Sleep
We have written in this column previously about the challenges that adolescents face in getting adequate sleep consistently. Teenagers, on average, need more than 9 hours of sleep nightly and American teenagers get fewer than 6. This mismatch is because of physiologic shifts that move their natural sleep onset time significantly later, while school still starts early. It’s often compounded by other demands on their time, including homework, extracurricular activities, and the gravitational pull of social connections. Independent teenagers make their own decisions about how to manage their time and may feel sleep is optional, or manage their fatigue with naps and caffeine, both of which will further compromise the quality and efficiency of sleep.
Chronic sleep deprivation will present with difficulties with focus, attention, memory, and cognitive performance. Treatment of this problem with stimulants is likely to make the underlying poor sleep habits even worse. When your patient presents complaining of difficulty concentrating and worsening school performance, be sure to start with a thorough sleep history, and always provide guidance about the body’s need for sleep and healthy sleep habits.
Anxiety
Anxiety disorders are the most common psychiatric illnesses of youth, with estimates of as many as 30% of children and adolescents experiencing one. The true prevalence of ADHD is estimated to be about 4% of the population. Whether social phobia, generalized anxiety disorder, or even posttraumatic stress disorder, anxiety disorders interfere with attention as ruminative worry tends to distract those experiencing it. It can also affect attention and focus indirectly by interfering with restful sleep. Anxiety disorders can be difficult to identify, as the sufferers typically internalize their symptoms. But inquire about specific worries (such as speaking in front of others, meeting new people, or an illness or accident striking themselves or a loved one) and how much time they take up. Explore if worries fill their thoughts during quiet or downtime, and explore more about their worries. You may use a screening instrument such as the Pediatric Symptom Checklist or the SCARED, both of which will indicate a likely problem with anxiety. While it is possible to have comorbid ADHD with an anxiety disorder, the anxiety disorder will likely worsen with stimulants and should be treated first. These are usually curable illnesses and you may find that remission of anxiety symptoms resolves the attentional problems.
Depression
Mood disorders are less common than anxiety disorders in youth, but far more prevalent than ADHD. And depression is usually marked by serious difficulty concentrating across settings (including for things that were previously very interesting). A sullen teenager who is deeply self-critical about school performance would benefit from exploration of associated changes in mood, interests, energy, appetite, sleep, and for feelings of worthlessness, guilt, and suicidal thoughts. The PHQ9A is a simple, free screening instrument that is reasonable to use with every sick visit (and well-check) with your adolescent patients, given the risks of undetected and untreated depression. If your patient presents complaining of poor school performance, always screen for depression. As with anxiety disorders, comorbid ADHD is possible, but it is always recommended to treat the mood disorder first and then to assess for residual ADHD symptoms once the mood disorder is in remission.
Substance abuse
Adolescence is a time of exploration, and drug and alcohol use is common. While attentional impairment will happen with intoxication, occasional or rare use should not lead to consistent impairment in school. But when parents are more worried than their children about a significant change in school performance, it is important to screen for substance abuse. A child with a secret substance use disorder will often present with behavioral changes and deteriorating school performance and might deny any drug or alcohol use to parents. Indeed, stimulants have some street value and some patients may be seeking a stimulant prescription to sell or trade for other drugs. Regular marijuana use may present with only deteriorating school performance and no irritability or other noticeable behavioral changes. Marijuana is seen as safe and even healthy by many teenagers (and even many parents), and some youth may be using it recreationally or to manage difficulties with sleep, anxiety, or mood symptoms.
But there is compelling evidence that marijuana use causes cognitive impairment, including difficulty with sustaining attention, short-term memory, and processing speed, for as long as 24 hours after use. If a teenager is using marijuana daily after school, it is certainly going to interfere, in a dose-dependent manner, with attention and cognitive function. Sustained heavy use can lead to permanent cognitive deficits. It can also trigger or worsen anxiety or mood symptoms (contrary to much popular opinion).
Gathering a thorough substance use history is essential when assessing a teenager for difficulties with focus or attention, especially when these are accompanied by change in behavior and school performance. Remember, it is critical to interview these children without their parents present to invite them to be forthcoming with you.
History
While true ADHD should have been present throughout childhood, it is possible that the symptoms have become noticeable only in adolescence. For patients with very high intelligence and lower levels of impulsivity and hyperactivity, they might easily have “flown under the radar” during their elementary and even middle school years. Their difficulties with attention and focus might become apparent only when the volume and difficulty of schoolwork both are great enough that their intelligence is not enough to get good grades. That is, their problems with executive function, prioritizing, shifting sets, and completing tasks in a timely way make it impossible to keep up good grades when the work gets harder.
Your history should reveal a long history of dreaminess or distractibility, a tendency to lose and forget things, and the other symptoms of inattention. Did they often seem to not be listening when they were younger? Forget to hand in homework? Leave chores unfinished? Leave messes behind everywhere they went? These will not be definitive, but they do reassure that symptoms may have been present for a long time, even if school performance was considered fine until the workload got too large. If such problems were not present before puberty, consider whether a subtle learning disability could be impairing them as they face more challenging academic subjects.
If you have ruled out anxiety, mood, and substance use concerns, and helped them to address a sleep deficit, then you can proceed. It is worthwhile to get Vanderbilt Assessments as you would for a younger child. If they meet criteria, discuss the risks and benefits of medication, executive skills coaching, and environmental adjustments (extra time for tests, a less stimulating environment) that can help them explore academic challenges without the discouragement that ADHD can bring.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Pediatricians are increasingly expert in the assessment and treatment of attention-deficit/hyperactivity disorder. But what do you do when adolescents present to your office saying they think they have ADHD? While ADHD is a common and treatable disorder of youth, it is important to take special care when assessing an adolescent. Difficulties with attention and concentration are common symptoms for many different challenges of adolescence, and for ADHD to be the underlying cause, those symptoms must have started prior to adolescence (according to DSM-5, prior to the age of 12). When your adolescent patients or their parents come to your office complaining of inattention, it is important to consider the full range of possible explanations.
Sleep
We have written in this column previously about the challenges that adolescents face in getting adequate sleep consistently. Teenagers, on average, need more than 9 hours of sleep nightly and American teenagers get fewer than 6. This mismatch is because of physiologic shifts that move their natural sleep onset time significantly later, while school still starts early. It’s often compounded by other demands on their time, including homework, extracurricular activities, and the gravitational pull of social connections. Independent teenagers make their own decisions about how to manage their time and may feel sleep is optional, or manage their fatigue with naps and caffeine, both of which will further compromise the quality and efficiency of sleep.
Chronic sleep deprivation will present with difficulties with focus, attention, memory, and cognitive performance. Treatment of this problem with stimulants is likely to make the underlying poor sleep habits even worse. When your patient presents complaining of difficulty concentrating and worsening school performance, be sure to start with a thorough sleep history, and always provide guidance about the body’s need for sleep and healthy sleep habits.
Anxiety
Anxiety disorders are the most common psychiatric illnesses of youth, with estimates of as many as 30% of children and adolescents experiencing one. The true prevalence of ADHD is estimated to be about 4% of the population. Whether social phobia, generalized anxiety disorder, or even posttraumatic stress disorder, anxiety disorders interfere with attention as ruminative worry tends to distract those experiencing it. It can also affect attention and focus indirectly by interfering with restful sleep. Anxiety disorders can be difficult to identify, as the sufferers typically internalize their symptoms. But inquire about specific worries (such as speaking in front of others, meeting new people, or an illness or accident striking themselves or a loved one) and how much time they take up. Explore if worries fill their thoughts during quiet or downtime, and explore more about their worries. You may use a screening instrument such as the Pediatric Symptom Checklist or the SCARED, both of which will indicate a likely problem with anxiety. While it is possible to have comorbid ADHD with an anxiety disorder, the anxiety disorder will likely worsen with stimulants and should be treated first. These are usually curable illnesses and you may find that remission of anxiety symptoms resolves the attentional problems.
Depression
Mood disorders are less common than anxiety disorders in youth, but far more prevalent than ADHD. And depression is usually marked by serious difficulty concentrating across settings (including for things that were previously very interesting). A sullen teenager who is deeply self-critical about school performance would benefit from exploration of associated changes in mood, interests, energy, appetite, sleep, and for feelings of worthlessness, guilt, and suicidal thoughts. The PHQ9A is a simple, free screening instrument that is reasonable to use with every sick visit (and well-check) with your adolescent patients, given the risks of undetected and untreated depression. If your patient presents complaining of poor school performance, always screen for depression. As with anxiety disorders, comorbid ADHD is possible, but it is always recommended to treat the mood disorder first and then to assess for residual ADHD symptoms once the mood disorder is in remission.
Substance abuse
Adolescence is a time of exploration, and drug and alcohol use is common. While attentional impairment will happen with intoxication, occasional or rare use should not lead to consistent impairment in school. But when parents are more worried than their children about a significant change in school performance, it is important to screen for substance abuse. A child with a secret substance use disorder will often present with behavioral changes and deteriorating school performance and might deny any drug or alcohol use to parents. Indeed, stimulants have some street value and some patients may be seeking a stimulant prescription to sell or trade for other drugs. Regular marijuana use may present with only deteriorating school performance and no irritability or other noticeable behavioral changes. Marijuana is seen as safe and even healthy by many teenagers (and even many parents), and some youth may be using it recreationally or to manage difficulties with sleep, anxiety, or mood symptoms.
But there is compelling evidence that marijuana use causes cognitive impairment, including difficulty with sustaining attention, short-term memory, and processing speed, for as long as 24 hours after use. If a teenager is using marijuana daily after school, it is certainly going to interfere, in a dose-dependent manner, with attention and cognitive function. Sustained heavy use can lead to permanent cognitive deficits. It can also trigger or worsen anxiety or mood symptoms (contrary to much popular opinion).
Gathering a thorough substance use history is essential when assessing a teenager for difficulties with focus or attention, especially when these are accompanied by change in behavior and school performance. Remember, it is critical to interview these children without their parents present to invite them to be forthcoming with you.
History
While true ADHD should have been present throughout childhood, it is possible that the symptoms have become noticeable only in adolescence. For patients with very high intelligence and lower levels of impulsivity and hyperactivity, they might easily have “flown under the radar” during their elementary and even middle school years. Their difficulties with attention and focus might become apparent only when the volume and difficulty of schoolwork both are great enough that their intelligence is not enough to get good grades. That is, their problems with executive function, prioritizing, shifting sets, and completing tasks in a timely way make it impossible to keep up good grades when the work gets harder.
Your history should reveal a long history of dreaminess or distractibility, a tendency to lose and forget things, and the other symptoms of inattention. Did they often seem to not be listening when they were younger? Forget to hand in homework? Leave chores unfinished? Leave messes behind everywhere they went? These will not be definitive, but they do reassure that symptoms may have been present for a long time, even if school performance was considered fine until the workload got too large. If such problems were not present before puberty, consider whether a subtle learning disability could be impairing them as they face more challenging academic subjects.
If you have ruled out anxiety, mood, and substance use concerns, and helped them to address a sleep deficit, then you can proceed. It is worthwhile to get Vanderbilt Assessments as you would for a younger child. If they meet criteria, discuss the risks and benefits of medication, executive skills coaching, and environmental adjustments (extra time for tests, a less stimulating environment) that can help them explore academic challenges without the discouragement that ADHD can bring.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Pollution levels linked to physical and mental health problems
Other analyses of data have found environmental air pollution from sources such as car exhaust and factory output can trigger an inflammatory response in the body. What’s new about a study published in RMD Open is that it explored an association between long-term exposure to pollution and risk of autoimmune diseases, wrote Giovanni Adami, MD, of the University of Verona (Italy) and colleagues.
“Environmental air pollution, according to the World Health Organization, is a major risk to health and 99% of the population worldwide is living in places where recommendations for air quality are not met,” said Dr. Adami in an interview. The limited data on the precise role of air pollution on rheumatic diseases in particular prompted the study, he said.
To explore the potential link between air pollution exposure and autoimmune disease, the researchers reviewed medical information from 81,363 adults via a national medical database in Italy; the data were submitted between June 2016 and November 2020.
The average age of the study population was 65 years, and 92% were women; 22% had at least one coexisting health condition. Each study participant was linked to local environmental monitoring via their residential postcode.
The researchers obtained details about concentrations of particulate matter in the environment from the Italian Institute of Environmental Protection that included 617 monitoring stations in 110 Italian provinces. They focused on concentrations of 10 and 2.5 (PM10 and PM2.5).
Exposure thresholds of 30 mcg/m3 for PM10 and 20 mcg/m3 for PM2.5 are generally considered harmful to health, they noted. On average, the long-term exposure was 16 mcg/m3 for PM2.5 and 25 mcg/m3 for PM10 between 2013 and 2019.
Overall, 9,723 individuals (12%) were diagnosed with an autoimmune disease between 2016 and 2020.
Exposure to PM10 was associated with a 7% higher risk of diagnosis with any autoimmune disease for every 10 mcg/m3 increase in concentration, but no association appeared between PM2.5 exposure and increased risk of autoimmune diseases.
However, in an adjusted model, chronic exposure to PM10 above 30 mcg/m3 and to PM2.5 above 20 mcg/m3 were associated with a 12% and 13% higher risk, respectively, of any autoimmune disease.
Chronic exposure to high levels of PM10 was specifically associated with a higher risk of rheumatoid arthritis, but no other autoimmune diseases. Chronic exposure to high levels of PM2.5 was associated with a higher risk of rheumatoid arthritis, connective tissue diseases, and inflammatory bowel diseases.
In their discussion, the researchers noted that the smaller diameter of PM2.5 molecules fluctuate less in response to rain and other weather, compared with PM10 molecules, which might make them a more accurate predictor of exposure to chronic air pollution.
The study findings were limited by several factors including the observational design, which prohibits the establishment of cause, and a lack of data on the start of symptoms and dates of diagnoses for autoimmune diseases, the researchers noted. Other limitations include the high percentage of older women in the study, which may limit generalizability, and the inability to account for additional personal exposure to pollutants outside of the environmental exposure, they said.
However, the results were strengthened by the large sample size and wide geographic distribution with variable pollution exposure, they said.
“Unfortunately, we were not surprised at all,” by the findings, Dr. Adami said in an interview.
“The biological rationale underpinning our findings is strong. Nevertheless, the magnitude of the effect was overwhelming. In addition, we saw an effect even at threshold of exposure that is widely considered as safe,” Dr. Adami noted.
Clinicians have been taught to consider cigarette smoking or other lifestyle behaviors as major risk factors for the development of several autoimmune diseases, said Dr. Adami. “In the future, we probably should include air pollution exposure as a risk factor as well. Interestingly, there is also accumulating evidence linking acute exposure to environmental air pollution with flares of chronic arthritis,” he said.
“Our study could have direct societal and political consequences,” and might help direct policy makers’ decisions on addressing strategies aimed to reduce fossil emissions, he said. As for additional research, “we certainly need multination studies to confirm our results on a larger scale,” Dr. Adami emphasized. “In addition, it is time to take action and start designing interventions aimed to reduce acute and chronic exposure to air pollution in patients suffering from RMDs.”
Consider the big picture of air quality
The Italian study is especially timely “given our evolving and emerging understanding of environmental risk factors for acute and chronic diseases, which we must first understand before we can address,” said Eileen Barrett, MD, of the University of New Mexico, Albuquerque, in an interview.
“I am largely surprised about the findings, as most physicians aren’t studying ambient air quality and risk for autoimmune disease,” said Dr. Barrett. “More often we think of air quality when we think of risk for respiratory diseases than autoimmune diseases, per se,” she said.
“There are several take-home messages from this study,” said Dr. Barrett. “The first is that we need more research to understand the consequences of air pollutants on health. Second, this study reminds us to think broadly about how air quality and our environment can affect health. And third, all clinicians should be committed to promoting science that can improve public health and reduce death and disability,” she emphasized.
The findings do not specifically reflect associations between pollution and other conditions such as chronic obstructive pulmonary disease and asthma although previous studies have shown an association between asthma and COPD exacerbations and air pollution, Dr. Barrett said.
“Further research will be needed to confirm the associations reported in this study,” Dr. Barrett said.
More research in other countries, including research related to other autoimmune diseases, and with other datasets on population and community level risks from poor air quality, would be helpful, and that information could be used to advise smart public policy, Dr. Barrett added.
Air pollution’s mental health impact
Air pollution’s effects extend beyond physical to the psychological, a new study of depression in teenagers showed. This study was published in Developmental Psychology.
Previous research on the environmental factors associated with depressive symptoms in teens has focused mainly on individual and family level contributors; the impact of the physical environment has not been well studied, the investigators, Erika M. Manczak, PhD, of the University of Denver and colleagues, wrote.
In their paper, the authors found a significant impact of neighborhood ozone exposure on the trajectory of depressive symptoms in teens over a 4-year period.
“Given that inhaling pollution activates biological pathways implicated in the development of depression, including immune, cardiovascular, and neurodevelopmental processes, exposure to ambient air pollution may influence the development and/or trajectory of depressive symptoms in youth,” they said.
The researchers recruited 213 adolescents in the San Francisco Bay area through local advertisements. The participants were aged 9-13 years at baseline, with an average age of 11 years. A total of 121 were female, 47% were white, 8.5% were African American, 12.3% were Asian, 10.4% were nonwhite Latin, and 21.7% were biracial or another ethnicity. The participants self-reported depressive symptoms and other psychopathology symptoms up to three times during the study period. Ozone exposure was calculated based on home addresses.
After controlling for other personal, family, and neighborhood variables, the researchers found that higher levels of ozone exposure were significantly associated with increased depressive symptoms over time, and the slope of trajectory of depressive symptoms became steeper as the ozone levels increased (P less than .001). Ozone did not significantly predict the trajectory of any other psychopathology symptoms.
“The results of this study provide preliminary support for the possibility that ozone is an overlooked contributor to the development or course of youth depressive symptoms,” the researchers wrote in their discussion.
“Interestingly, the association between ozone and symptom trajectories as measured by Anxious/Depressed subscale of the [Youth Self-Report] was not as strong as it was for the [Children’s Depression Inventory-Short Version] or Withdrawn/Depressed scales, suggesting that associations are more robust for behavioral withdrawal symptoms of depression than for other types of symptoms,” they noted.
The study findings were limited by the use of self-reports and by the inability of the study design to show causality, the researchers said. Other limitations include the use of average assessments of ozone that are less precise, lack of assessment of biological pathways for risk, lack of formal psychiatric diagnoses, and the small geographic region included in the study, they said.
However, the results provide preliminary evidence that ozone exposure is a potential contributing factor to depressive symptoms in youth, and serve as a jumping-off point for future research, they noted. Future studies should address changes in systemic inflammation, neurodevelopment, or stress reactivity, as well as concurrent psychosocial or biological factors, and temporal associations between air pollution and mental health symptoms, they concluded.
Environmental factors drive inflammatory responses
Peter L. Loper Jr., MD, considers the findings of the Developmental Psychology study to be unsurprising but important – because air pollution is simply getting worse.
“As the study authors cite, there is sufficient data correlating ozone to negative physical health outcomes in youth, but a paucity of data exploring the impact of poor air quality on mental health outcomes in this demographic,” noted Dr. Loper, of the University of South Carolina, Columbia, in an interview.
“As discussed by the study researchers, any environmental exposure that increases immune-mediated inflammation can result in negative health outcomes. In fact, there is already data to suggest that similar cytokines, or immune cell signalers, that get released by our immune system due to environmental exposures and that contribute to asthma, may also be implicated in depression and other mental health problems,” he noted.
“Just like downstream symptom indicators of physical illnesses such as asthma are secondary to immune-mediated pulmonary inflammation, downstream symptom indicators of mental illness, such as depression, are secondary to immune-mediated neuroinflammation,” Dr. Loper emphasized. “The most well-characterized upstream phenomenon perpetuating the downstream symptom indicators of depression involve neuroinflammatory states due to psychosocial and relational factors such as chronic stress, poor relationships, or substance use. However, any environmental factor that triggers an immune response and inflammation can promote neuroinflammation that manifests as symptoms of mental illness.”
The message for teens with depression and their families is that “we are a product of our environment,” Dr. Loper said. “When our environments are proinflammatory, or cause our immune system to become overactive, then we will develop illness; however, the most potent mediator of inflammation in the brain, and the downstream symptoms of depression, is our relationships with those we love most,” he said.
Dr. Loper suggested research aimed at identifying other sources of immune-mediated inflammation caused by physical environments and better understanding how environmental phenomenon like ozone may compound previously established risk factors for mental illness could be useful.
The RMD Open study received no outside funding, and its authors had no financial conflicts.
The Developmental Psychology study was supported by the National Institute of Mental Health and the Stanford University Precision Health and Integrated Diagnostics Center. The researchers for that report, and Dr. Loper and Dr. Barrett had no conflicts to disclose.
Other analyses of data have found environmental air pollution from sources such as car exhaust and factory output can trigger an inflammatory response in the body. What’s new about a study published in RMD Open is that it explored an association between long-term exposure to pollution and risk of autoimmune diseases, wrote Giovanni Adami, MD, of the University of Verona (Italy) and colleagues.
“Environmental air pollution, according to the World Health Organization, is a major risk to health and 99% of the population worldwide is living in places where recommendations for air quality are not met,” said Dr. Adami in an interview. The limited data on the precise role of air pollution on rheumatic diseases in particular prompted the study, he said.
To explore the potential link between air pollution exposure and autoimmune disease, the researchers reviewed medical information from 81,363 adults via a national medical database in Italy; the data were submitted between June 2016 and November 2020.
The average age of the study population was 65 years, and 92% were women; 22% had at least one coexisting health condition. Each study participant was linked to local environmental monitoring via their residential postcode.
The researchers obtained details about concentrations of particulate matter in the environment from the Italian Institute of Environmental Protection that included 617 monitoring stations in 110 Italian provinces. They focused on concentrations of 10 and 2.5 (PM10 and PM2.5).
Exposure thresholds of 30 mcg/m3 for PM10 and 20 mcg/m3 for PM2.5 are generally considered harmful to health, they noted. On average, the long-term exposure was 16 mcg/m3 for PM2.5 and 25 mcg/m3 for PM10 between 2013 and 2019.
Overall, 9,723 individuals (12%) were diagnosed with an autoimmune disease between 2016 and 2020.
Exposure to PM10 was associated with a 7% higher risk of diagnosis with any autoimmune disease for every 10 mcg/m3 increase in concentration, but no association appeared between PM2.5 exposure and increased risk of autoimmune diseases.
However, in an adjusted model, chronic exposure to PM10 above 30 mcg/m3 and to PM2.5 above 20 mcg/m3 were associated with a 12% and 13% higher risk, respectively, of any autoimmune disease.
Chronic exposure to high levels of PM10 was specifically associated with a higher risk of rheumatoid arthritis, but no other autoimmune diseases. Chronic exposure to high levels of PM2.5 was associated with a higher risk of rheumatoid arthritis, connective tissue diseases, and inflammatory bowel diseases.
In their discussion, the researchers noted that the smaller diameter of PM2.5 molecules fluctuate less in response to rain and other weather, compared with PM10 molecules, which might make them a more accurate predictor of exposure to chronic air pollution.
The study findings were limited by several factors including the observational design, which prohibits the establishment of cause, and a lack of data on the start of symptoms and dates of diagnoses for autoimmune diseases, the researchers noted. Other limitations include the high percentage of older women in the study, which may limit generalizability, and the inability to account for additional personal exposure to pollutants outside of the environmental exposure, they said.
However, the results were strengthened by the large sample size and wide geographic distribution with variable pollution exposure, they said.
“Unfortunately, we were not surprised at all,” by the findings, Dr. Adami said in an interview.
“The biological rationale underpinning our findings is strong. Nevertheless, the magnitude of the effect was overwhelming. In addition, we saw an effect even at threshold of exposure that is widely considered as safe,” Dr. Adami noted.
Clinicians have been taught to consider cigarette smoking or other lifestyle behaviors as major risk factors for the development of several autoimmune diseases, said Dr. Adami. “In the future, we probably should include air pollution exposure as a risk factor as well. Interestingly, there is also accumulating evidence linking acute exposure to environmental air pollution with flares of chronic arthritis,” he said.
“Our study could have direct societal and political consequences,” and might help direct policy makers’ decisions on addressing strategies aimed to reduce fossil emissions, he said. As for additional research, “we certainly need multination studies to confirm our results on a larger scale,” Dr. Adami emphasized. “In addition, it is time to take action and start designing interventions aimed to reduce acute and chronic exposure to air pollution in patients suffering from RMDs.”
Consider the big picture of air quality
The Italian study is especially timely “given our evolving and emerging understanding of environmental risk factors for acute and chronic diseases, which we must first understand before we can address,” said Eileen Barrett, MD, of the University of New Mexico, Albuquerque, in an interview.
“I am largely surprised about the findings, as most physicians aren’t studying ambient air quality and risk for autoimmune disease,” said Dr. Barrett. “More often we think of air quality when we think of risk for respiratory diseases than autoimmune diseases, per se,” she said.
“There are several take-home messages from this study,” said Dr. Barrett. “The first is that we need more research to understand the consequences of air pollutants on health. Second, this study reminds us to think broadly about how air quality and our environment can affect health. And third, all clinicians should be committed to promoting science that can improve public health and reduce death and disability,” she emphasized.
The findings do not specifically reflect associations between pollution and other conditions such as chronic obstructive pulmonary disease and asthma although previous studies have shown an association between asthma and COPD exacerbations and air pollution, Dr. Barrett said.
“Further research will be needed to confirm the associations reported in this study,” Dr. Barrett said.
More research in other countries, including research related to other autoimmune diseases, and with other datasets on population and community level risks from poor air quality, would be helpful, and that information could be used to advise smart public policy, Dr. Barrett added.
Air pollution’s mental health impact
Air pollution’s effects extend beyond physical to the psychological, a new study of depression in teenagers showed. This study was published in Developmental Psychology.
Previous research on the environmental factors associated with depressive symptoms in teens has focused mainly on individual and family level contributors; the impact of the physical environment has not been well studied, the investigators, Erika M. Manczak, PhD, of the University of Denver and colleagues, wrote.
In their paper, the authors found a significant impact of neighborhood ozone exposure on the trajectory of depressive symptoms in teens over a 4-year period.
“Given that inhaling pollution activates biological pathways implicated in the development of depression, including immune, cardiovascular, and neurodevelopmental processes, exposure to ambient air pollution may influence the development and/or trajectory of depressive symptoms in youth,” they said.
The researchers recruited 213 adolescents in the San Francisco Bay area through local advertisements. The participants were aged 9-13 years at baseline, with an average age of 11 years. A total of 121 were female, 47% were white, 8.5% were African American, 12.3% were Asian, 10.4% were nonwhite Latin, and 21.7% were biracial or another ethnicity. The participants self-reported depressive symptoms and other psychopathology symptoms up to three times during the study period. Ozone exposure was calculated based on home addresses.
After controlling for other personal, family, and neighborhood variables, the researchers found that higher levels of ozone exposure were significantly associated with increased depressive symptoms over time, and the slope of trajectory of depressive symptoms became steeper as the ozone levels increased (P less than .001). Ozone did not significantly predict the trajectory of any other psychopathology symptoms.
“The results of this study provide preliminary support for the possibility that ozone is an overlooked contributor to the development or course of youth depressive symptoms,” the researchers wrote in their discussion.
“Interestingly, the association between ozone and symptom trajectories as measured by Anxious/Depressed subscale of the [Youth Self-Report] was not as strong as it was for the [Children’s Depression Inventory-Short Version] or Withdrawn/Depressed scales, suggesting that associations are more robust for behavioral withdrawal symptoms of depression than for other types of symptoms,” they noted.
The study findings were limited by the use of self-reports and by the inability of the study design to show causality, the researchers said. Other limitations include the use of average assessments of ozone that are less precise, lack of assessment of biological pathways for risk, lack of formal psychiatric diagnoses, and the small geographic region included in the study, they said.
However, the results provide preliminary evidence that ozone exposure is a potential contributing factor to depressive symptoms in youth, and serve as a jumping-off point for future research, they noted. Future studies should address changes in systemic inflammation, neurodevelopment, or stress reactivity, as well as concurrent psychosocial or biological factors, and temporal associations between air pollution and mental health symptoms, they concluded.
Environmental factors drive inflammatory responses
Peter L. Loper Jr., MD, considers the findings of the Developmental Psychology study to be unsurprising but important – because air pollution is simply getting worse.
“As the study authors cite, there is sufficient data correlating ozone to negative physical health outcomes in youth, but a paucity of data exploring the impact of poor air quality on mental health outcomes in this demographic,” noted Dr. Loper, of the University of South Carolina, Columbia, in an interview.
“As discussed by the study researchers, any environmental exposure that increases immune-mediated inflammation can result in negative health outcomes. In fact, there is already data to suggest that similar cytokines, or immune cell signalers, that get released by our immune system due to environmental exposures and that contribute to asthma, may also be implicated in depression and other mental health problems,” he noted.
“Just like downstream symptom indicators of physical illnesses such as asthma are secondary to immune-mediated pulmonary inflammation, downstream symptom indicators of mental illness, such as depression, are secondary to immune-mediated neuroinflammation,” Dr. Loper emphasized. “The most well-characterized upstream phenomenon perpetuating the downstream symptom indicators of depression involve neuroinflammatory states due to psychosocial and relational factors such as chronic stress, poor relationships, or substance use. However, any environmental factor that triggers an immune response and inflammation can promote neuroinflammation that manifests as symptoms of mental illness.”
The message for teens with depression and their families is that “we are a product of our environment,” Dr. Loper said. “When our environments are proinflammatory, or cause our immune system to become overactive, then we will develop illness; however, the most potent mediator of inflammation in the brain, and the downstream symptoms of depression, is our relationships with those we love most,” he said.
Dr. Loper suggested research aimed at identifying other sources of immune-mediated inflammation caused by physical environments and better understanding how environmental phenomenon like ozone may compound previously established risk factors for mental illness could be useful.
The RMD Open study received no outside funding, and its authors had no financial conflicts.
The Developmental Psychology study was supported by the National Institute of Mental Health and the Stanford University Precision Health and Integrated Diagnostics Center. The researchers for that report, and Dr. Loper and Dr. Barrett had no conflicts to disclose.
Other analyses of data have found environmental air pollution from sources such as car exhaust and factory output can trigger an inflammatory response in the body. What’s new about a study published in RMD Open is that it explored an association between long-term exposure to pollution and risk of autoimmune diseases, wrote Giovanni Adami, MD, of the University of Verona (Italy) and colleagues.
“Environmental air pollution, according to the World Health Organization, is a major risk to health and 99% of the population worldwide is living in places where recommendations for air quality are not met,” said Dr. Adami in an interview. The limited data on the precise role of air pollution on rheumatic diseases in particular prompted the study, he said.
To explore the potential link between air pollution exposure and autoimmune disease, the researchers reviewed medical information from 81,363 adults via a national medical database in Italy; the data were submitted between June 2016 and November 2020.
The average age of the study population was 65 years, and 92% were women; 22% had at least one coexisting health condition. Each study participant was linked to local environmental monitoring via their residential postcode.
The researchers obtained details about concentrations of particulate matter in the environment from the Italian Institute of Environmental Protection that included 617 monitoring stations in 110 Italian provinces. They focused on concentrations of 10 and 2.5 (PM10 and PM2.5).
Exposure thresholds of 30 mcg/m3 for PM10 and 20 mcg/m3 for PM2.5 are generally considered harmful to health, they noted. On average, the long-term exposure was 16 mcg/m3 for PM2.5 and 25 mcg/m3 for PM10 between 2013 and 2019.
Overall, 9,723 individuals (12%) were diagnosed with an autoimmune disease between 2016 and 2020.
Exposure to PM10 was associated with a 7% higher risk of diagnosis with any autoimmune disease for every 10 mcg/m3 increase in concentration, but no association appeared between PM2.5 exposure and increased risk of autoimmune diseases.
However, in an adjusted model, chronic exposure to PM10 above 30 mcg/m3 and to PM2.5 above 20 mcg/m3 were associated with a 12% and 13% higher risk, respectively, of any autoimmune disease.
Chronic exposure to high levels of PM10 was specifically associated with a higher risk of rheumatoid arthritis, but no other autoimmune diseases. Chronic exposure to high levels of PM2.5 was associated with a higher risk of rheumatoid arthritis, connective tissue diseases, and inflammatory bowel diseases.
In their discussion, the researchers noted that the smaller diameter of PM2.5 molecules fluctuate less in response to rain and other weather, compared with PM10 molecules, which might make them a more accurate predictor of exposure to chronic air pollution.
The study findings were limited by several factors including the observational design, which prohibits the establishment of cause, and a lack of data on the start of symptoms and dates of diagnoses for autoimmune diseases, the researchers noted. Other limitations include the high percentage of older women in the study, which may limit generalizability, and the inability to account for additional personal exposure to pollutants outside of the environmental exposure, they said.
However, the results were strengthened by the large sample size and wide geographic distribution with variable pollution exposure, they said.
“Unfortunately, we were not surprised at all,” by the findings, Dr. Adami said in an interview.
“The biological rationale underpinning our findings is strong. Nevertheless, the magnitude of the effect was overwhelming. In addition, we saw an effect even at threshold of exposure that is widely considered as safe,” Dr. Adami noted.
Clinicians have been taught to consider cigarette smoking or other lifestyle behaviors as major risk factors for the development of several autoimmune diseases, said Dr. Adami. “In the future, we probably should include air pollution exposure as a risk factor as well. Interestingly, there is also accumulating evidence linking acute exposure to environmental air pollution with flares of chronic arthritis,” he said.
“Our study could have direct societal and political consequences,” and might help direct policy makers’ decisions on addressing strategies aimed to reduce fossil emissions, he said. As for additional research, “we certainly need multination studies to confirm our results on a larger scale,” Dr. Adami emphasized. “In addition, it is time to take action and start designing interventions aimed to reduce acute and chronic exposure to air pollution in patients suffering from RMDs.”
Consider the big picture of air quality
The Italian study is especially timely “given our evolving and emerging understanding of environmental risk factors for acute and chronic diseases, which we must first understand before we can address,” said Eileen Barrett, MD, of the University of New Mexico, Albuquerque, in an interview.
“I am largely surprised about the findings, as most physicians aren’t studying ambient air quality and risk for autoimmune disease,” said Dr. Barrett. “More often we think of air quality when we think of risk for respiratory diseases than autoimmune diseases, per se,” she said.
“There are several take-home messages from this study,” said Dr. Barrett. “The first is that we need more research to understand the consequences of air pollutants on health. Second, this study reminds us to think broadly about how air quality and our environment can affect health. And third, all clinicians should be committed to promoting science that can improve public health and reduce death and disability,” she emphasized.
The findings do not specifically reflect associations between pollution and other conditions such as chronic obstructive pulmonary disease and asthma although previous studies have shown an association between asthma and COPD exacerbations and air pollution, Dr. Barrett said.
“Further research will be needed to confirm the associations reported in this study,” Dr. Barrett said.
More research in other countries, including research related to other autoimmune diseases, and with other datasets on population and community level risks from poor air quality, would be helpful, and that information could be used to advise smart public policy, Dr. Barrett added.
Air pollution’s mental health impact
Air pollution’s effects extend beyond physical to the psychological, a new study of depression in teenagers showed. This study was published in Developmental Psychology.
Previous research on the environmental factors associated with depressive symptoms in teens has focused mainly on individual and family level contributors; the impact of the physical environment has not been well studied, the investigators, Erika M. Manczak, PhD, of the University of Denver and colleagues, wrote.
In their paper, the authors found a significant impact of neighborhood ozone exposure on the trajectory of depressive symptoms in teens over a 4-year period.
“Given that inhaling pollution activates biological pathways implicated in the development of depression, including immune, cardiovascular, and neurodevelopmental processes, exposure to ambient air pollution may influence the development and/or trajectory of depressive symptoms in youth,” they said.
The researchers recruited 213 adolescents in the San Francisco Bay area through local advertisements. The participants were aged 9-13 years at baseline, with an average age of 11 years. A total of 121 were female, 47% were white, 8.5% were African American, 12.3% were Asian, 10.4% were nonwhite Latin, and 21.7% were biracial or another ethnicity. The participants self-reported depressive symptoms and other psychopathology symptoms up to three times during the study period. Ozone exposure was calculated based on home addresses.
After controlling for other personal, family, and neighborhood variables, the researchers found that higher levels of ozone exposure were significantly associated with increased depressive symptoms over time, and the slope of trajectory of depressive symptoms became steeper as the ozone levels increased (P less than .001). Ozone did not significantly predict the trajectory of any other psychopathology symptoms.
“The results of this study provide preliminary support for the possibility that ozone is an overlooked contributor to the development or course of youth depressive symptoms,” the researchers wrote in their discussion.
“Interestingly, the association between ozone and symptom trajectories as measured by Anxious/Depressed subscale of the [Youth Self-Report] was not as strong as it was for the [Children’s Depression Inventory-Short Version] or Withdrawn/Depressed scales, suggesting that associations are more robust for behavioral withdrawal symptoms of depression than for other types of symptoms,” they noted.
The study findings were limited by the use of self-reports and by the inability of the study design to show causality, the researchers said. Other limitations include the use of average assessments of ozone that are less precise, lack of assessment of biological pathways for risk, lack of formal psychiatric diagnoses, and the small geographic region included in the study, they said.
However, the results provide preliminary evidence that ozone exposure is a potential contributing factor to depressive symptoms in youth, and serve as a jumping-off point for future research, they noted. Future studies should address changes in systemic inflammation, neurodevelopment, or stress reactivity, as well as concurrent psychosocial or biological factors, and temporal associations between air pollution and mental health symptoms, they concluded.
Environmental factors drive inflammatory responses
Peter L. Loper Jr., MD, considers the findings of the Developmental Psychology study to be unsurprising but important – because air pollution is simply getting worse.
“As the study authors cite, there is sufficient data correlating ozone to negative physical health outcomes in youth, but a paucity of data exploring the impact of poor air quality on mental health outcomes in this demographic,” noted Dr. Loper, of the University of South Carolina, Columbia, in an interview.
“As discussed by the study researchers, any environmental exposure that increases immune-mediated inflammation can result in negative health outcomes. In fact, there is already data to suggest that similar cytokines, or immune cell signalers, that get released by our immune system due to environmental exposures and that contribute to asthma, may also be implicated in depression and other mental health problems,” he noted.
“Just like downstream symptom indicators of physical illnesses such as asthma are secondary to immune-mediated pulmonary inflammation, downstream symptom indicators of mental illness, such as depression, are secondary to immune-mediated neuroinflammation,” Dr. Loper emphasized. “The most well-characterized upstream phenomenon perpetuating the downstream symptom indicators of depression involve neuroinflammatory states due to psychosocial and relational factors such as chronic stress, poor relationships, or substance use. However, any environmental factor that triggers an immune response and inflammation can promote neuroinflammation that manifests as symptoms of mental illness.”
The message for teens with depression and their families is that “we are a product of our environment,” Dr. Loper said. “When our environments are proinflammatory, or cause our immune system to become overactive, then we will develop illness; however, the most potent mediator of inflammation in the brain, and the downstream symptoms of depression, is our relationships with those we love most,” he said.
Dr. Loper suggested research aimed at identifying other sources of immune-mediated inflammation caused by physical environments and better understanding how environmental phenomenon like ozone may compound previously established risk factors for mental illness could be useful.
The RMD Open study received no outside funding, and its authors had no financial conflicts.
The Developmental Psychology study was supported by the National Institute of Mental Health and the Stanford University Precision Health and Integrated Diagnostics Center. The researchers for that report, and Dr. Loper and Dr. Barrett had no conflicts to disclose.
FROM RMD OPEN