User login
NCCN guidelines highlight ‘complicated’ treatment for pediatric lymphomas
The National Comprehensive Cancer Network (NCCN) has released its first set of guidelines for managing pediatric aggressive mature B-cell lymphomas.
The guidelines highlight the complexities of treating pediatric Burkitt lymphoma (BL) and diffuse large B-cell lymphoma (DLBCL), as recommendations include a range of multiagent regimens for different patient groups at various time points.
“The treatment of this disease is relatively complicated,” said Kimberly J. Davies, MD, a pediatric hematologist/oncologist at Dana-Farber Cancer Institute in Boston and chair of the guidelines panel. “The chemotherapy regimens have a lot of drugs, a lot of nuances to how they’re supposed to be given. These guidelines delineate that treatment and help the provider … make sure they are delivering the treatment a patient needs.”
The guidelines recommend different regimens according to a patient’s risk group, but the same treatment approach should be used for patients with BL and those with DLBCL.
“The biggest difference between pediatric and adult patients is that pediatric patients are more uniformly treated, regardless of what type of aggressive B-cell lymphoma they have,” said Matthew Barth, MD, a pediatric hematologist/oncologist at Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., and vice chair of the NCCN guidelines panel.
“Adults with diffuse large B-cell lymphoma and Burkitt lymphoma are generally treated with different chemotherapy regimens, but, in pediatrics, we use the same treatment regimens for both diffuse large B-cell lymphoma and Burkitt lymphoma,” he added.
As an example, the new guidelines recommend that pediatric patients with low-risk BL/DLBCL receive the POG9219 regimen (N Engl J Med. 1997 Oct 30;337[18]:1259-66) or FAB/LMB96 regimen A (Br J Haematol. 2008 Jun;141[6]:840-7) as induction, or they should be enrolled in a clinical trial.
On the other hand, induction for high-risk pediatric BL/DLBCL patients should consist of rituximab and a chemotherapy regimen used in the COG ANHL1131 trial. The recommendation to incorporate rituximab in high-risk pediatric patients is based on results from that trial (J Clin Oncol. 2016 May 20. doi: 10.1200/JCO.2016.34.15_suppl.10507).
“Until recent clinical trial data was available, we weren’t really sure how to incorporate rituximab into the treatment of pediatric patients with mature B-cell lymphomas,” Dr. Barth said. “We now have evidence that rituximab is clearly beneficial for patients who are in higher-risk groups.”
Dr. Barth and Dr. Davies both noted that pediatric BL and DLBCL have high cure rates. Long-term survival rates range from about 80% to more than 90%, according to the American Cancer Society. However, the patients who do relapse or progress can be difficult to treat.
“We have quite good cure rates at this point in time, which is a great success, but that means that a very small population of patients don’t respond to initial therapy, and … it’s hard to know what the best treatment for those patients is,” Dr. Davies said.
She noted that studies are underway to determine if immunotherapies, including chimeric antigen receptor T-cell therapy, might improve outcomes in patients with relapsed or refractory disease.
For now, the NCCN guidelines recommend clinical trial enrollment for relapsed/refractory patients. Alternatively, these patients can receive additional chemotherapy, and responders can proceed to transplant. Patients who don’t achieve at least a partial response may go on to a clinical trial or receive best supportive care.
Dr. Davies and Dr. Barth reported having no conflicts of interest.
The National Comprehensive Cancer Network (NCCN) has released its first set of guidelines for managing pediatric aggressive mature B-cell lymphomas.
The guidelines highlight the complexities of treating pediatric Burkitt lymphoma (BL) and diffuse large B-cell lymphoma (DLBCL), as recommendations include a range of multiagent regimens for different patient groups at various time points.
“The treatment of this disease is relatively complicated,” said Kimberly J. Davies, MD, a pediatric hematologist/oncologist at Dana-Farber Cancer Institute in Boston and chair of the guidelines panel. “The chemotherapy regimens have a lot of drugs, a lot of nuances to how they’re supposed to be given. These guidelines delineate that treatment and help the provider … make sure they are delivering the treatment a patient needs.”
The guidelines recommend different regimens according to a patient’s risk group, but the same treatment approach should be used for patients with BL and those with DLBCL.
“The biggest difference between pediatric and adult patients is that pediatric patients are more uniformly treated, regardless of what type of aggressive B-cell lymphoma they have,” said Matthew Barth, MD, a pediatric hematologist/oncologist at Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., and vice chair of the NCCN guidelines panel.
“Adults with diffuse large B-cell lymphoma and Burkitt lymphoma are generally treated with different chemotherapy regimens, but, in pediatrics, we use the same treatment regimens for both diffuse large B-cell lymphoma and Burkitt lymphoma,” he added.
As an example, the new guidelines recommend that pediatric patients with low-risk BL/DLBCL receive the POG9219 regimen (N Engl J Med. 1997 Oct 30;337[18]:1259-66) or FAB/LMB96 regimen A (Br J Haematol. 2008 Jun;141[6]:840-7) as induction, or they should be enrolled in a clinical trial.
On the other hand, induction for high-risk pediatric BL/DLBCL patients should consist of rituximab and a chemotherapy regimen used in the COG ANHL1131 trial. The recommendation to incorporate rituximab in high-risk pediatric patients is based on results from that trial (J Clin Oncol. 2016 May 20. doi: 10.1200/JCO.2016.34.15_suppl.10507).
“Until recent clinical trial data was available, we weren’t really sure how to incorporate rituximab into the treatment of pediatric patients with mature B-cell lymphomas,” Dr. Barth said. “We now have evidence that rituximab is clearly beneficial for patients who are in higher-risk groups.”
Dr. Barth and Dr. Davies both noted that pediatric BL and DLBCL have high cure rates. Long-term survival rates range from about 80% to more than 90%, according to the American Cancer Society. However, the patients who do relapse or progress can be difficult to treat.
“We have quite good cure rates at this point in time, which is a great success, but that means that a very small population of patients don’t respond to initial therapy, and … it’s hard to know what the best treatment for those patients is,” Dr. Davies said.
She noted that studies are underway to determine if immunotherapies, including chimeric antigen receptor T-cell therapy, might improve outcomes in patients with relapsed or refractory disease.
For now, the NCCN guidelines recommend clinical trial enrollment for relapsed/refractory patients. Alternatively, these patients can receive additional chemotherapy, and responders can proceed to transplant. Patients who don’t achieve at least a partial response may go on to a clinical trial or receive best supportive care.
Dr. Davies and Dr. Barth reported having no conflicts of interest.
The National Comprehensive Cancer Network (NCCN) has released its first set of guidelines for managing pediatric aggressive mature B-cell lymphomas.
The guidelines highlight the complexities of treating pediatric Burkitt lymphoma (BL) and diffuse large B-cell lymphoma (DLBCL), as recommendations include a range of multiagent regimens for different patient groups at various time points.
“The treatment of this disease is relatively complicated,” said Kimberly J. Davies, MD, a pediatric hematologist/oncologist at Dana-Farber Cancer Institute in Boston and chair of the guidelines panel. “The chemotherapy regimens have a lot of drugs, a lot of nuances to how they’re supposed to be given. These guidelines delineate that treatment and help the provider … make sure they are delivering the treatment a patient needs.”
The guidelines recommend different regimens according to a patient’s risk group, but the same treatment approach should be used for patients with BL and those with DLBCL.
“The biggest difference between pediatric and adult patients is that pediatric patients are more uniformly treated, regardless of what type of aggressive B-cell lymphoma they have,” said Matthew Barth, MD, a pediatric hematologist/oncologist at Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., and vice chair of the NCCN guidelines panel.
“Adults with diffuse large B-cell lymphoma and Burkitt lymphoma are generally treated with different chemotherapy regimens, but, in pediatrics, we use the same treatment regimens for both diffuse large B-cell lymphoma and Burkitt lymphoma,” he added.
As an example, the new guidelines recommend that pediatric patients with low-risk BL/DLBCL receive the POG9219 regimen (N Engl J Med. 1997 Oct 30;337[18]:1259-66) or FAB/LMB96 regimen A (Br J Haematol. 2008 Jun;141[6]:840-7) as induction, or they should be enrolled in a clinical trial.
On the other hand, induction for high-risk pediatric BL/DLBCL patients should consist of rituximab and a chemotherapy regimen used in the COG ANHL1131 trial. The recommendation to incorporate rituximab in high-risk pediatric patients is based on results from that trial (J Clin Oncol. 2016 May 20. doi: 10.1200/JCO.2016.34.15_suppl.10507).
“Until recent clinical trial data was available, we weren’t really sure how to incorporate rituximab into the treatment of pediatric patients with mature B-cell lymphomas,” Dr. Barth said. “We now have evidence that rituximab is clearly beneficial for patients who are in higher-risk groups.”
Dr. Barth and Dr. Davies both noted that pediatric BL and DLBCL have high cure rates. Long-term survival rates range from about 80% to more than 90%, according to the American Cancer Society. However, the patients who do relapse or progress can be difficult to treat.
“We have quite good cure rates at this point in time, which is a great success, but that means that a very small population of patients don’t respond to initial therapy, and … it’s hard to know what the best treatment for those patients is,” Dr. Davies said.
She noted that studies are underway to determine if immunotherapies, including chimeric antigen receptor T-cell therapy, might improve outcomes in patients with relapsed or refractory disease.
For now, the NCCN guidelines recommend clinical trial enrollment for relapsed/refractory patients. Alternatively, these patients can receive additional chemotherapy, and responders can proceed to transplant. Patients who don’t achieve at least a partial response may go on to a clinical trial or receive best supportive care.
Dr. Davies and Dr. Barth reported having no conflicts of interest.
CAR T cells produce complete responses in T-cell malignancies
ORLANDO – Anti-CD5 chimeric antigen receptor (CAR) T cells can produce complete responses (CRs) in patients with relapsed or refractory T-cell malignancies, according to findings from a phase 1 trial.
Three of 11 patients achieved a CR after CAR T-cell therapy, and one patient achieved a mixed response that deepened to a CR after transplant. Three responders, all of whom had T-cell lymphoma, were still alive and in CR at last follow-up.
There were no cases of severe cytokine release syndrome (CRS) or severe neurotoxicity, no serious infectious complications, and no nonhematologic grade 4 adverse events in this trial.
LaQuisa C. Hill, MD, of Baylor College of Medicine, Houston, presented these results at the annual meeting of the American Society of Hematology.
“While CD19 CAR T cells have revolutionized the treatment of relapsed/refractory B-cell malignancies, development of CAR T-cell platforms targeting T-cell-driven malignancies have been hindered by three main factors: CAR T-cell fratricide due to shared expression of target antigens leading to impaired expansion, ablation of normal T cells continuing to cause profound immunodeficiency, and the potential of transduced tumor cells providing a means of tumor escape,” Dr. Hill said.
Researchers have theorized that anti-CD5 CAR T cells can overcome these obstacles. In preclinical studies, anti-CD5 CAR T cells eliminated malignant blasts in vitro and in vivo and resulted in “limited and transient” fratricide (Blood. 2015 Aug 20;126[8]:983-92).
With this in mind, Dr. Hill and her colleagues tested CD5.28z CAR T cells in a phase 1 trial (NCT03081910). Eleven patients have been treated thus far – five with T-cell acute lymphoblastic leukemia (T-ALL), three with peripheral T-cell lymphoma (PTCL), two with angioimmunoblastic T-cell lymphoma (AITL), and one with Sézary syndrome.
The patients’ median age at baseline was 62 years (range, 21-71 years), and 63% were men. They had received a median of 5 prior therapies (range, 3-18). Two patients had relapsed after allogeneic hematopoietic stem cell transplant (HSCT), three had relapsed after autologous HSCT, and five were primary refractory.
Patients underwent lymphodepletion with fludarabine and cyclophosphamide, then received CAR T cells at doses of 1 x 107 or 5 x 107.
Response
Three lymphoma patients – two with AITL and one with PTCL – were still alive and in CR at last follow-up. The PTCL patient achieved a CR after CAR T-cell therapy and declined a subsequent HSCT. The patient has not received additional therapy and has retained the CR for 7 months.
One AITL patient achieved a CR and declined transplant as well. He relapsed after 7 months but received subsequent therapy and achieved another CR. The other AITL patient had a mixed response to CAR T-cell therapy but proceeded to allogeneic HSCT and achieved a CR that has lasted 9 months.
The remaining three lymphoma patients – two with PTCL and one with Sézary syndrome – progressed and died.
One T-ALL patient achieved a CR lasting 6 weeks, but the patient died while undergoing transplant workup. Two T-ALL patients did not respond to treatment and died. The remaining two patients progressed, and one of them died. The other patient who progressed is still alive and in CR after receiving subsequent therapy.
Factors associated with response
Dr. Hill said a shortened manufacturing process may be associated with enhanced response, as all responders received CAR T cells produced via a shorter manufacturing process. The shortened process involves freezing cells on day 4-5 post transduction, as opposed to day 7.
“While the numbers are too small to make any definitive conclusions, this seems to correlate with less terminal differentiation, which might improve potency,” Dr. Hill said. “However, additional analyses are ongoing.”
Dr. Hill also pointed out that CAR T-cell expansion was observed in all patients, with higher peak levels observed at the higher dose. In addition, CAR T-cell persistence was durable at both dose levels.
“We have been able to detect the CAR transgene at all follow-up time points, out to 9 months for some patients,” Dr. Hill said. “While limited persistence may play a role in nonresponders, it does not appear to be the only factor.”
Safety
“Surprisingly, no selective ablation of normal T cells has been observed,” Dr. Hill said. “As CAR T cells dwindled [after infusion], we were able to see recovery of normal T cells, all of which expressed normal levels of CD5. This was observed in all patients on study, except for one patient who had prolonged pancytopenia.”
Cytopenias were the most common grade 3/4 adverse events, including neutropenia (n = 8), anemia (n = 7), and thrombocytopenia (n = 5). Other grade 3/4 events included elevated aspartate aminotransferase (n = 2), hypoalbuminemia (n = 1), hyponatremia (n = 1), hypophosphatemia (n = 1), and elevated alanine aminotransferase (n = 1). There were no grade 5 adverse events.
Two patients developed grade 1 CRS, and two had grade 2 CRS. Both patients with grade 2 CRS were treated with tocilizumab, and their symptoms resolved.
One patient developed grade 2 immune effector cell-associated neurotoxicity syndrome, but this resolved with supportive care.
One patient had a central line–associated bloodstream infection (coagulase-negative staphylococci), and one had cytomegalovirus and BK virus reactivation. There were no fungal infections.
“We have demonstrated that CD5 CAR T cells can be manufactured from heavily pretreated patients with T-cell malignancies, and therapy is well tolerated,” Dr. Hill said. “We have seen strong and promising activity in T-cell lymphoma, which we hope to be able to translate to T-ALL as well.”
Dr. Hill said she and her colleagues hope to improve upon these results with a higher dose level of CD5 CAR T cells (1 x 108), which the team plans to start testing soon. The researchers may also investigate other target antigens, such as CD7, as well as the use of donor-derived CAR T cells for patients who have relapsed after allogeneic HSCT.
Dr. Hill said she has no relevant disclosures. Baylor College of Medicine is sponsoring this trial.
SOURCE: Hill L et al. ASH 2019. Abstract 199.
ORLANDO – Anti-CD5 chimeric antigen receptor (CAR) T cells can produce complete responses (CRs) in patients with relapsed or refractory T-cell malignancies, according to findings from a phase 1 trial.
Three of 11 patients achieved a CR after CAR T-cell therapy, and one patient achieved a mixed response that deepened to a CR after transplant. Three responders, all of whom had T-cell lymphoma, were still alive and in CR at last follow-up.
There were no cases of severe cytokine release syndrome (CRS) or severe neurotoxicity, no serious infectious complications, and no nonhematologic grade 4 adverse events in this trial.
LaQuisa C. Hill, MD, of Baylor College of Medicine, Houston, presented these results at the annual meeting of the American Society of Hematology.
“While CD19 CAR T cells have revolutionized the treatment of relapsed/refractory B-cell malignancies, development of CAR T-cell platforms targeting T-cell-driven malignancies have been hindered by three main factors: CAR T-cell fratricide due to shared expression of target antigens leading to impaired expansion, ablation of normal T cells continuing to cause profound immunodeficiency, and the potential of transduced tumor cells providing a means of tumor escape,” Dr. Hill said.
Researchers have theorized that anti-CD5 CAR T cells can overcome these obstacles. In preclinical studies, anti-CD5 CAR T cells eliminated malignant blasts in vitro and in vivo and resulted in “limited and transient” fratricide (Blood. 2015 Aug 20;126[8]:983-92).
With this in mind, Dr. Hill and her colleagues tested CD5.28z CAR T cells in a phase 1 trial (NCT03081910). Eleven patients have been treated thus far – five with T-cell acute lymphoblastic leukemia (T-ALL), three with peripheral T-cell lymphoma (PTCL), two with angioimmunoblastic T-cell lymphoma (AITL), and one with Sézary syndrome.
The patients’ median age at baseline was 62 years (range, 21-71 years), and 63% were men. They had received a median of 5 prior therapies (range, 3-18). Two patients had relapsed after allogeneic hematopoietic stem cell transplant (HSCT), three had relapsed after autologous HSCT, and five were primary refractory.
Patients underwent lymphodepletion with fludarabine and cyclophosphamide, then received CAR T cells at doses of 1 x 107 or 5 x 107.
Response
Three lymphoma patients – two with AITL and one with PTCL – were still alive and in CR at last follow-up. The PTCL patient achieved a CR after CAR T-cell therapy and declined a subsequent HSCT. The patient has not received additional therapy and has retained the CR for 7 months.
One AITL patient achieved a CR and declined transplant as well. He relapsed after 7 months but received subsequent therapy and achieved another CR. The other AITL patient had a mixed response to CAR T-cell therapy but proceeded to allogeneic HSCT and achieved a CR that has lasted 9 months.
The remaining three lymphoma patients – two with PTCL and one with Sézary syndrome – progressed and died.
One T-ALL patient achieved a CR lasting 6 weeks, but the patient died while undergoing transplant workup. Two T-ALL patients did not respond to treatment and died. The remaining two patients progressed, and one of them died. The other patient who progressed is still alive and in CR after receiving subsequent therapy.
Factors associated with response
Dr. Hill said a shortened manufacturing process may be associated with enhanced response, as all responders received CAR T cells produced via a shorter manufacturing process. The shortened process involves freezing cells on day 4-5 post transduction, as opposed to day 7.
“While the numbers are too small to make any definitive conclusions, this seems to correlate with less terminal differentiation, which might improve potency,” Dr. Hill said. “However, additional analyses are ongoing.”
Dr. Hill also pointed out that CAR T-cell expansion was observed in all patients, with higher peak levels observed at the higher dose. In addition, CAR T-cell persistence was durable at both dose levels.
“We have been able to detect the CAR transgene at all follow-up time points, out to 9 months for some patients,” Dr. Hill said. “While limited persistence may play a role in nonresponders, it does not appear to be the only factor.”
Safety
“Surprisingly, no selective ablation of normal T cells has been observed,” Dr. Hill said. “As CAR T cells dwindled [after infusion], we were able to see recovery of normal T cells, all of which expressed normal levels of CD5. This was observed in all patients on study, except for one patient who had prolonged pancytopenia.”
Cytopenias were the most common grade 3/4 adverse events, including neutropenia (n = 8), anemia (n = 7), and thrombocytopenia (n = 5). Other grade 3/4 events included elevated aspartate aminotransferase (n = 2), hypoalbuminemia (n = 1), hyponatremia (n = 1), hypophosphatemia (n = 1), and elevated alanine aminotransferase (n = 1). There were no grade 5 adverse events.
Two patients developed grade 1 CRS, and two had grade 2 CRS. Both patients with grade 2 CRS were treated with tocilizumab, and their symptoms resolved.
One patient developed grade 2 immune effector cell-associated neurotoxicity syndrome, but this resolved with supportive care.
One patient had a central line–associated bloodstream infection (coagulase-negative staphylococci), and one had cytomegalovirus and BK virus reactivation. There were no fungal infections.
“We have demonstrated that CD5 CAR T cells can be manufactured from heavily pretreated patients with T-cell malignancies, and therapy is well tolerated,” Dr. Hill said. “We have seen strong and promising activity in T-cell lymphoma, which we hope to be able to translate to T-ALL as well.”
Dr. Hill said she and her colleagues hope to improve upon these results with a higher dose level of CD5 CAR T cells (1 x 108), which the team plans to start testing soon. The researchers may also investigate other target antigens, such as CD7, as well as the use of donor-derived CAR T cells for patients who have relapsed after allogeneic HSCT.
Dr. Hill said she has no relevant disclosures. Baylor College of Medicine is sponsoring this trial.
SOURCE: Hill L et al. ASH 2019. Abstract 199.
ORLANDO – Anti-CD5 chimeric antigen receptor (CAR) T cells can produce complete responses (CRs) in patients with relapsed or refractory T-cell malignancies, according to findings from a phase 1 trial.
Three of 11 patients achieved a CR after CAR T-cell therapy, and one patient achieved a mixed response that deepened to a CR after transplant. Three responders, all of whom had T-cell lymphoma, were still alive and in CR at last follow-up.
There were no cases of severe cytokine release syndrome (CRS) or severe neurotoxicity, no serious infectious complications, and no nonhematologic grade 4 adverse events in this trial.
LaQuisa C. Hill, MD, of Baylor College of Medicine, Houston, presented these results at the annual meeting of the American Society of Hematology.
“While CD19 CAR T cells have revolutionized the treatment of relapsed/refractory B-cell malignancies, development of CAR T-cell platforms targeting T-cell-driven malignancies have been hindered by three main factors: CAR T-cell fratricide due to shared expression of target antigens leading to impaired expansion, ablation of normal T cells continuing to cause profound immunodeficiency, and the potential of transduced tumor cells providing a means of tumor escape,” Dr. Hill said.
Researchers have theorized that anti-CD5 CAR T cells can overcome these obstacles. In preclinical studies, anti-CD5 CAR T cells eliminated malignant blasts in vitro and in vivo and resulted in “limited and transient” fratricide (Blood. 2015 Aug 20;126[8]:983-92).
With this in mind, Dr. Hill and her colleagues tested CD5.28z CAR T cells in a phase 1 trial (NCT03081910). Eleven patients have been treated thus far – five with T-cell acute lymphoblastic leukemia (T-ALL), three with peripheral T-cell lymphoma (PTCL), two with angioimmunoblastic T-cell lymphoma (AITL), and one with Sézary syndrome.
The patients’ median age at baseline was 62 years (range, 21-71 years), and 63% were men. They had received a median of 5 prior therapies (range, 3-18). Two patients had relapsed after allogeneic hematopoietic stem cell transplant (HSCT), three had relapsed after autologous HSCT, and five were primary refractory.
Patients underwent lymphodepletion with fludarabine and cyclophosphamide, then received CAR T cells at doses of 1 x 107 or 5 x 107.
Response
Three lymphoma patients – two with AITL and one with PTCL – were still alive and in CR at last follow-up. The PTCL patient achieved a CR after CAR T-cell therapy and declined a subsequent HSCT. The patient has not received additional therapy and has retained the CR for 7 months.
One AITL patient achieved a CR and declined transplant as well. He relapsed after 7 months but received subsequent therapy and achieved another CR. The other AITL patient had a mixed response to CAR T-cell therapy but proceeded to allogeneic HSCT and achieved a CR that has lasted 9 months.
The remaining three lymphoma patients – two with PTCL and one with Sézary syndrome – progressed and died.
One T-ALL patient achieved a CR lasting 6 weeks, but the patient died while undergoing transplant workup. Two T-ALL patients did not respond to treatment and died. The remaining two patients progressed, and one of them died. The other patient who progressed is still alive and in CR after receiving subsequent therapy.
Factors associated with response
Dr. Hill said a shortened manufacturing process may be associated with enhanced response, as all responders received CAR T cells produced via a shorter manufacturing process. The shortened process involves freezing cells on day 4-5 post transduction, as opposed to day 7.
“While the numbers are too small to make any definitive conclusions, this seems to correlate with less terminal differentiation, which might improve potency,” Dr. Hill said. “However, additional analyses are ongoing.”
Dr. Hill also pointed out that CAR T-cell expansion was observed in all patients, with higher peak levels observed at the higher dose. In addition, CAR T-cell persistence was durable at both dose levels.
“We have been able to detect the CAR transgene at all follow-up time points, out to 9 months for some patients,” Dr. Hill said. “While limited persistence may play a role in nonresponders, it does not appear to be the only factor.”
Safety
“Surprisingly, no selective ablation of normal T cells has been observed,” Dr. Hill said. “As CAR T cells dwindled [after infusion], we were able to see recovery of normal T cells, all of which expressed normal levels of CD5. This was observed in all patients on study, except for one patient who had prolonged pancytopenia.”
Cytopenias were the most common grade 3/4 adverse events, including neutropenia (n = 8), anemia (n = 7), and thrombocytopenia (n = 5). Other grade 3/4 events included elevated aspartate aminotransferase (n = 2), hypoalbuminemia (n = 1), hyponatremia (n = 1), hypophosphatemia (n = 1), and elevated alanine aminotransferase (n = 1). There were no grade 5 adverse events.
Two patients developed grade 1 CRS, and two had grade 2 CRS. Both patients with grade 2 CRS were treated with tocilizumab, and their symptoms resolved.
One patient developed grade 2 immune effector cell-associated neurotoxicity syndrome, but this resolved with supportive care.
One patient had a central line–associated bloodstream infection (coagulase-negative staphylococci), and one had cytomegalovirus and BK virus reactivation. There were no fungal infections.
“We have demonstrated that CD5 CAR T cells can be manufactured from heavily pretreated patients with T-cell malignancies, and therapy is well tolerated,” Dr. Hill said. “We have seen strong and promising activity in T-cell lymphoma, which we hope to be able to translate to T-ALL as well.”
Dr. Hill said she and her colleagues hope to improve upon these results with a higher dose level of CD5 CAR T cells (1 x 108), which the team plans to start testing soon. The researchers may also investigate other target antigens, such as CD7, as well as the use of donor-derived CAR T cells for patients who have relapsed after allogeneic HSCT.
Dr. Hill said she has no relevant disclosures. Baylor College of Medicine is sponsoring this trial.
SOURCE: Hill L et al. ASH 2019. Abstract 199.
REPORTING FROM ASH 2019
Inhibitor appears to strengthen anti-BCMA CAR T cells in myeloma patients
ORLANDO – A gamma secretase inhibitor could enhance the efficacy of B-cell maturation antigen (BCMA)-directed chimeric antigen receptor (CAR) T cells in patients with relapsed or refractory multiple myeloma, a phase 1 trial suggests.
The inhibitor, JSMD194, increased BCMA expression in all 10 patients studied. All patients responded to anti-BCMA CAR T-cell therapy, including three patients who had previously failed BCMA-directed therapy.
Nine patients remain alive and in response at a median follow-up of 20 weeks, with two patients being followed for more than a year. One patient experienced dose-limiting toxicity and died, which prompted a change to the study’s eligibility criteria.
Andrew J. Cowan, MD, of the University of Washington and Fred Hutchinson Cancer Research Center in Seattle, presented these results at the annual meeting of the American Society of Hematology.
Dr. Cowan and colleagues previously showed that treatment with a gamma secretase inhibitor increased BCMA expression on tumor cells and improved the efficacy of BCMA-targeted CAR T cells in a mouse model of multiple myeloma. The team also showed that a gamma secretase inhibitor could “markedly” increase the percentage of BCMA-positive tumor cells in myeloma patients (Blood. 2019 Nov 7;134[19]:1585-97).
To expand upon these findings, the researchers began a phase 1 trial of BCMA-directed CAR T cells and the oral gamma secretase inhibitor JSMD194 in patients with relapsed/refractory multiple myeloma.
Ten patients have been treated, five men and five women. The patients’ median age at baseline was 66 years (range, 44-74 years). They received a median of 10 prior therapies (range, 4-23). Nine patients had received at least one autologous stem cell transplant, and one patient had two. One patient underwent allogeneic transplant (as well as autologous transplant).
Three patients had received prior BCMA-directed therapy. Two patients had received BCMA-directed CAR T cells. One of them did not respond, and the other responded but relapsed. The third patient received a BCMA-targeted bispecific T-cell engager and did not respond.
Study treatment
Patients had BCMA expression measured at baseline, then underwent apheresis for CAR T-cell production.
Patients received JSMD194 at 25 mg on days 1, 3, and 5. Then, they received cyclophosphamide at 300 mg and fludarabine at 25 mg for 3 days.
Next, patients received a single CAR T-cell infusion at a dose of 50 x 106 (n = 5), 150 x 106 (n = 3), or 300 x 106 (n = 2). They also received JSMD194 at 25 mg three times a week for 3 weeks.
Safety
“Nearly all patients had a serious adverse event, which was typically admission to the hospital for neutropenic fever,” Dr. Cowan said.
One patient experienced dose-limiting toxicity and died at day 33. The patient had a disseminating fungal infection, grade 4 cytokine release syndrome (CRS), and neurotoxicity. The patient’s death prompted the researchers to include performance status in the study’s eligibility criteria.
All patients developed CRS. Only the aforementioned patient had grade 4 CRS, and three patients had grade 3 CRS. Six patients experienced neurotoxicity. There were no cases of tumor lysis syndrome.
Efficacy
“All patients experienced an increase of cells expressing BCMA,” Dr. Cowan said. “While there was significant variability in BCMA expression at baseline, all cells expressed BCMA after three doses of the gamma secretase inhibitor.”
The median BCMA expression after JSMD194 treatment was 99% (range, 96%-100%), and there was a median 20-fold (range, 8- to 157-fold) increase in BCMA surface density.
The overall response rate was 100%. Two patients achieved a stringent complete response (CR), one achieved a CR, five patients had a very good partial response, and two had a partial response.
The patient with a CR received the 50 x 106 dose of CAR T cells, and the patients with stringent CRs received the 150 x 106 and 300 x 106 doses.
Of the three patients who previously received BCMA-directed therapy, two achieved a very good partial response, and one had a partial response.
Nine of the 10 patients are still alive and in response, with a median follow-up of 20 weeks. The longest follow-up is 444 days.
“To date, all patients have evidence of durable responses,” Dr. Cowan said. “Moreover, all patients had dramatic reductions in involved serum free light chain ... and serum monoclonal proteins.”
Dr. Cowan noted that longer follow-up is needed to assess CAR T-cell persistence and the durability of response.
This trial is sponsored by the Fred Hutchinson Cancer Research Center in collaboration with the National Cancer Institute. Two researchers involved in this work are employees of Juno Therapeutics. Dr. Cowan reported relationships with Juno Therapeutics, Janssen, Celgene, AbbVie, Cellectar, and Sanofi.
SOURCE: Cowan AJ et al. ASH 2019. Abstract 204.
ORLANDO – A gamma secretase inhibitor could enhance the efficacy of B-cell maturation antigen (BCMA)-directed chimeric antigen receptor (CAR) T cells in patients with relapsed or refractory multiple myeloma, a phase 1 trial suggests.
The inhibitor, JSMD194, increased BCMA expression in all 10 patients studied. All patients responded to anti-BCMA CAR T-cell therapy, including three patients who had previously failed BCMA-directed therapy.
Nine patients remain alive and in response at a median follow-up of 20 weeks, with two patients being followed for more than a year. One patient experienced dose-limiting toxicity and died, which prompted a change to the study’s eligibility criteria.
Andrew J. Cowan, MD, of the University of Washington and Fred Hutchinson Cancer Research Center in Seattle, presented these results at the annual meeting of the American Society of Hematology.
Dr. Cowan and colleagues previously showed that treatment with a gamma secretase inhibitor increased BCMA expression on tumor cells and improved the efficacy of BCMA-targeted CAR T cells in a mouse model of multiple myeloma. The team also showed that a gamma secretase inhibitor could “markedly” increase the percentage of BCMA-positive tumor cells in myeloma patients (Blood. 2019 Nov 7;134[19]:1585-97).
To expand upon these findings, the researchers began a phase 1 trial of BCMA-directed CAR T cells and the oral gamma secretase inhibitor JSMD194 in patients with relapsed/refractory multiple myeloma.
Ten patients have been treated, five men and five women. The patients’ median age at baseline was 66 years (range, 44-74 years). They received a median of 10 prior therapies (range, 4-23). Nine patients had received at least one autologous stem cell transplant, and one patient had two. One patient underwent allogeneic transplant (as well as autologous transplant).
Three patients had received prior BCMA-directed therapy. Two patients had received BCMA-directed CAR T cells. One of them did not respond, and the other responded but relapsed. The third patient received a BCMA-targeted bispecific T-cell engager and did not respond.
Study treatment
Patients had BCMA expression measured at baseline, then underwent apheresis for CAR T-cell production.
Patients received JSMD194 at 25 mg on days 1, 3, and 5. Then, they received cyclophosphamide at 300 mg and fludarabine at 25 mg for 3 days.
Next, patients received a single CAR T-cell infusion at a dose of 50 x 106 (n = 5), 150 x 106 (n = 3), or 300 x 106 (n = 2). They also received JSMD194 at 25 mg three times a week for 3 weeks.
Safety
“Nearly all patients had a serious adverse event, which was typically admission to the hospital for neutropenic fever,” Dr. Cowan said.
One patient experienced dose-limiting toxicity and died at day 33. The patient had a disseminating fungal infection, grade 4 cytokine release syndrome (CRS), and neurotoxicity. The patient’s death prompted the researchers to include performance status in the study’s eligibility criteria.
All patients developed CRS. Only the aforementioned patient had grade 4 CRS, and three patients had grade 3 CRS. Six patients experienced neurotoxicity. There were no cases of tumor lysis syndrome.
Efficacy
“All patients experienced an increase of cells expressing BCMA,” Dr. Cowan said. “While there was significant variability in BCMA expression at baseline, all cells expressed BCMA after three doses of the gamma secretase inhibitor.”
The median BCMA expression after JSMD194 treatment was 99% (range, 96%-100%), and there was a median 20-fold (range, 8- to 157-fold) increase in BCMA surface density.
The overall response rate was 100%. Two patients achieved a stringent complete response (CR), one achieved a CR, five patients had a very good partial response, and two had a partial response.
The patient with a CR received the 50 x 106 dose of CAR T cells, and the patients with stringent CRs received the 150 x 106 and 300 x 106 doses.
Of the three patients who previously received BCMA-directed therapy, two achieved a very good partial response, and one had a partial response.
Nine of the 10 patients are still alive and in response, with a median follow-up of 20 weeks. The longest follow-up is 444 days.
“To date, all patients have evidence of durable responses,” Dr. Cowan said. “Moreover, all patients had dramatic reductions in involved serum free light chain ... and serum monoclonal proteins.”
Dr. Cowan noted that longer follow-up is needed to assess CAR T-cell persistence and the durability of response.
This trial is sponsored by the Fred Hutchinson Cancer Research Center in collaboration with the National Cancer Institute. Two researchers involved in this work are employees of Juno Therapeutics. Dr. Cowan reported relationships with Juno Therapeutics, Janssen, Celgene, AbbVie, Cellectar, and Sanofi.
SOURCE: Cowan AJ et al. ASH 2019. Abstract 204.
ORLANDO – A gamma secretase inhibitor could enhance the efficacy of B-cell maturation antigen (BCMA)-directed chimeric antigen receptor (CAR) T cells in patients with relapsed or refractory multiple myeloma, a phase 1 trial suggests.
The inhibitor, JSMD194, increased BCMA expression in all 10 patients studied. All patients responded to anti-BCMA CAR T-cell therapy, including three patients who had previously failed BCMA-directed therapy.
Nine patients remain alive and in response at a median follow-up of 20 weeks, with two patients being followed for more than a year. One patient experienced dose-limiting toxicity and died, which prompted a change to the study’s eligibility criteria.
Andrew J. Cowan, MD, of the University of Washington and Fred Hutchinson Cancer Research Center in Seattle, presented these results at the annual meeting of the American Society of Hematology.
Dr. Cowan and colleagues previously showed that treatment with a gamma secretase inhibitor increased BCMA expression on tumor cells and improved the efficacy of BCMA-targeted CAR T cells in a mouse model of multiple myeloma. The team also showed that a gamma secretase inhibitor could “markedly” increase the percentage of BCMA-positive tumor cells in myeloma patients (Blood. 2019 Nov 7;134[19]:1585-97).
To expand upon these findings, the researchers began a phase 1 trial of BCMA-directed CAR T cells and the oral gamma secretase inhibitor JSMD194 in patients with relapsed/refractory multiple myeloma.
Ten patients have been treated, five men and five women. The patients’ median age at baseline was 66 years (range, 44-74 years). They received a median of 10 prior therapies (range, 4-23). Nine patients had received at least one autologous stem cell transplant, and one patient had two. One patient underwent allogeneic transplant (as well as autologous transplant).
Three patients had received prior BCMA-directed therapy. Two patients had received BCMA-directed CAR T cells. One of them did not respond, and the other responded but relapsed. The third patient received a BCMA-targeted bispecific T-cell engager and did not respond.
Study treatment
Patients had BCMA expression measured at baseline, then underwent apheresis for CAR T-cell production.
Patients received JSMD194 at 25 mg on days 1, 3, and 5. Then, they received cyclophosphamide at 300 mg and fludarabine at 25 mg for 3 days.
Next, patients received a single CAR T-cell infusion at a dose of 50 x 106 (n = 5), 150 x 106 (n = 3), or 300 x 106 (n = 2). They also received JSMD194 at 25 mg three times a week for 3 weeks.
Safety
“Nearly all patients had a serious adverse event, which was typically admission to the hospital for neutropenic fever,” Dr. Cowan said.
One patient experienced dose-limiting toxicity and died at day 33. The patient had a disseminating fungal infection, grade 4 cytokine release syndrome (CRS), and neurotoxicity. The patient’s death prompted the researchers to include performance status in the study’s eligibility criteria.
All patients developed CRS. Only the aforementioned patient had grade 4 CRS, and three patients had grade 3 CRS. Six patients experienced neurotoxicity. There were no cases of tumor lysis syndrome.
Efficacy
“All patients experienced an increase of cells expressing BCMA,” Dr. Cowan said. “While there was significant variability in BCMA expression at baseline, all cells expressed BCMA after three doses of the gamma secretase inhibitor.”
The median BCMA expression after JSMD194 treatment was 99% (range, 96%-100%), and there was a median 20-fold (range, 8- to 157-fold) increase in BCMA surface density.
The overall response rate was 100%. Two patients achieved a stringent complete response (CR), one achieved a CR, five patients had a very good partial response, and two had a partial response.
The patient with a CR received the 50 x 106 dose of CAR T cells, and the patients with stringent CRs received the 150 x 106 and 300 x 106 doses.
Of the three patients who previously received BCMA-directed therapy, two achieved a very good partial response, and one had a partial response.
Nine of the 10 patients are still alive and in response, with a median follow-up of 20 weeks. The longest follow-up is 444 days.
“To date, all patients have evidence of durable responses,” Dr. Cowan said. “Moreover, all patients had dramatic reductions in involved serum free light chain ... and serum monoclonal proteins.”
Dr. Cowan noted that longer follow-up is needed to assess CAR T-cell persistence and the durability of response.
This trial is sponsored by the Fred Hutchinson Cancer Research Center in collaboration with the National Cancer Institute. Two researchers involved in this work are employees of Juno Therapeutics. Dr. Cowan reported relationships with Juno Therapeutics, Janssen, Celgene, AbbVie, Cellectar, and Sanofi.
SOURCE: Cowan AJ et al. ASH 2019. Abstract 204.
REPORTING FROM ASH 2019
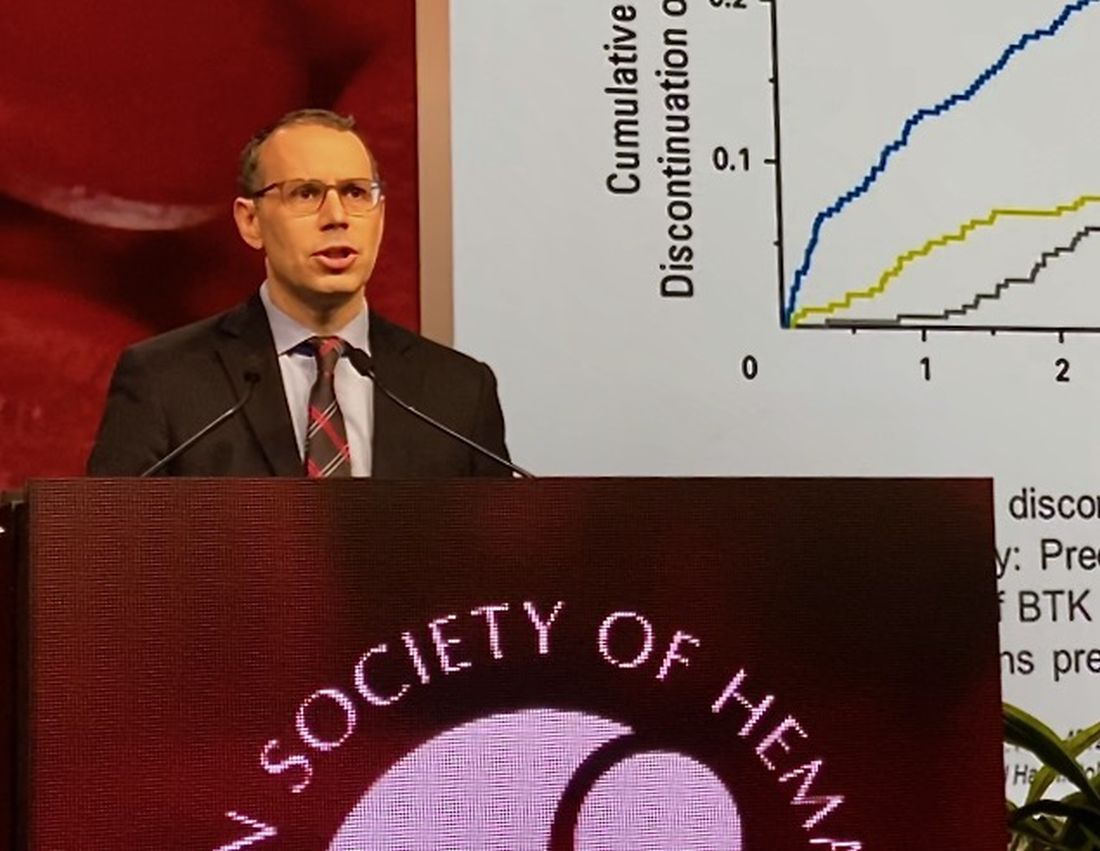
LOXO-305: Next-gen BTK inhibitor safe and effective in B-cell malignancies
ORLANDO – A phase 1 trial of the next-generation Bruton tyrosine kinase (BTK) inhibitor LOXO-305 has demonstrated safety and provided evidence of its efficacy in heavily pretreated patients with B-cell malignancies, including some with acquired resistance to other BTK inhibitors and venetoclax, according to an investigator.
The antitumor activity of this highly selective investigational oral BTK inhibitor was significant in patients with chronic lymphocytic leukemia (CLL) and mantle cell lymphoma (MCL), with a rapid onset of action and resolution of lymphocytosis “consistent with effective BTK target inhibition,” said Anthony R. Mato, MD, of the Center for CLL at Memorial Sloan Kettering Cancer Center in New York.
Responses were also seen in patients with BTK C481 mutations, the primary cause of progressive CLL after BTK inhibitor use, Dr. Mato said at the annual meeting of the American Society of Hematology.
The safety and tolerability profile of LOXO-305 is “consistent with highly selective drug design,” with no evidence of off-target effects, he said. “Collectively, these data demonstrate that BTK remains a highly actionable target despite progression on covalent BTK inhibitors.”
While BTK inhibitors have transformed treatment of B-cell malignancies, resistance remains a major problem, said Dr. Mato, citing 5-year ibrutinib discontinuation rates of 41% in the front line setting and 53.7% in the relapsed/refractory setting.
Key reasons for discontinuation are intolerance, events such as atrial fibrillation and major bleeding, progression of disease, and the appearance of BTK C481 mutations, which prevent covalent BTK inhibitors from achieving effective target inhibition, he said. In contrast, LOXO-305 is designed to non-covalently bind to BTK, regardless of C481 status.
Dr. Mato described results of the phase 1 BRUIN trial, in which 28 adult patients with CLL or B-cell non-Hodgkin lymphomas received once daily oral LOXO-305 at doses ranging from 25 mg to 200 mg. All patients had received at least two lines of prior therapy and had active disease in need of treatment.
For 13 evaluable CLL patients, the overall response rate was 77% (10 patients), Dr. Mato reported. Overall response rates for MCL and other B-cell malignancies were 50%, or three out of six MCL patients and two of four patients with Waldenström macroglobulinemia, diffuse large B-cell lymphoma, or marginal zone lymphoma.
Though only a small subset of CLL patients have had multiple response assessments, the available data suggest that responses “deepen over time” with continued LOXO-305 treatment, Dr. Mato said.
With the median follow-up of 2.7 months, 24 of 28 patients remain on therapy, including all responders. “Some of the responses appear to be quite durable,” Dr. Mato said.
There have been no dose-limiting toxicities, the maximum tolerated dose has not been reached, and there have been no notable adverse events characteristic of covalent BTK inhibitors – namely atrial fibrillation or major bleeding – despite frequent monitoring, according to Dr. Mato.
There were two grade 3 events (leukocytosis and neutropenia), but the remaining treatment-emergent adverse events have been grade 1-2. “Having managed many of these patients, I can tell you that these adverse events were quite manageable,” Dr. Mato told attendees.
BRUIN is a global trial that continues to enroll patients at 18 sites in 3 countries, with a plan in 2020 to incorporate “rational combinations” of agents, according to the investigator.
Dr. Mato reported disclosures related to Gilead, Pharmacyclics, AstraZeneca, AbbVie, Sunesis, Johnson & Johnson, TG Therapeutics, LOXO, DTRM Biopharma, Genentech, Janssen, Acerta, Pharmacyclics, and Celgene.
SOURCE: Mato AR et al. ASH 2019, Abstract 501.
ORLANDO – A phase 1 trial of the next-generation Bruton tyrosine kinase (BTK) inhibitor LOXO-305 has demonstrated safety and provided evidence of its efficacy in heavily pretreated patients with B-cell malignancies, including some with acquired resistance to other BTK inhibitors and venetoclax, according to an investigator.
The antitumor activity of this highly selective investigational oral BTK inhibitor was significant in patients with chronic lymphocytic leukemia (CLL) and mantle cell lymphoma (MCL), with a rapid onset of action and resolution of lymphocytosis “consistent with effective BTK target inhibition,” said Anthony R. Mato, MD, of the Center for CLL at Memorial Sloan Kettering Cancer Center in New York.
Responses were also seen in patients with BTK C481 mutations, the primary cause of progressive CLL after BTK inhibitor use, Dr. Mato said at the annual meeting of the American Society of Hematology.
The safety and tolerability profile of LOXO-305 is “consistent with highly selective drug design,” with no evidence of off-target effects, he said. “Collectively, these data demonstrate that BTK remains a highly actionable target despite progression on covalent BTK inhibitors.”
While BTK inhibitors have transformed treatment of B-cell malignancies, resistance remains a major problem, said Dr. Mato, citing 5-year ibrutinib discontinuation rates of 41% in the front line setting and 53.7% in the relapsed/refractory setting.
Key reasons for discontinuation are intolerance, events such as atrial fibrillation and major bleeding, progression of disease, and the appearance of BTK C481 mutations, which prevent covalent BTK inhibitors from achieving effective target inhibition, he said. In contrast, LOXO-305 is designed to non-covalently bind to BTK, regardless of C481 status.
Dr. Mato described results of the phase 1 BRUIN trial, in which 28 adult patients with CLL or B-cell non-Hodgkin lymphomas received once daily oral LOXO-305 at doses ranging from 25 mg to 200 mg. All patients had received at least two lines of prior therapy and had active disease in need of treatment.
For 13 evaluable CLL patients, the overall response rate was 77% (10 patients), Dr. Mato reported. Overall response rates for MCL and other B-cell malignancies were 50%, or three out of six MCL patients and two of four patients with Waldenström macroglobulinemia, diffuse large B-cell lymphoma, or marginal zone lymphoma.
Though only a small subset of CLL patients have had multiple response assessments, the available data suggest that responses “deepen over time” with continued LOXO-305 treatment, Dr. Mato said.
With the median follow-up of 2.7 months, 24 of 28 patients remain on therapy, including all responders. “Some of the responses appear to be quite durable,” Dr. Mato said.
There have been no dose-limiting toxicities, the maximum tolerated dose has not been reached, and there have been no notable adverse events characteristic of covalent BTK inhibitors – namely atrial fibrillation or major bleeding – despite frequent monitoring, according to Dr. Mato.
There were two grade 3 events (leukocytosis and neutropenia), but the remaining treatment-emergent adverse events have been grade 1-2. “Having managed many of these patients, I can tell you that these adverse events were quite manageable,” Dr. Mato told attendees.
BRUIN is a global trial that continues to enroll patients at 18 sites in 3 countries, with a plan in 2020 to incorporate “rational combinations” of agents, according to the investigator.
Dr. Mato reported disclosures related to Gilead, Pharmacyclics, AstraZeneca, AbbVie, Sunesis, Johnson & Johnson, TG Therapeutics, LOXO, DTRM Biopharma, Genentech, Janssen, Acerta, Pharmacyclics, and Celgene.
SOURCE: Mato AR et al. ASH 2019, Abstract 501.
ORLANDO – A phase 1 trial of the next-generation Bruton tyrosine kinase (BTK) inhibitor LOXO-305 has demonstrated safety and provided evidence of its efficacy in heavily pretreated patients with B-cell malignancies, including some with acquired resistance to other BTK inhibitors and venetoclax, according to an investigator.
The antitumor activity of this highly selective investigational oral BTK inhibitor was significant in patients with chronic lymphocytic leukemia (CLL) and mantle cell lymphoma (MCL), with a rapid onset of action and resolution of lymphocytosis “consistent with effective BTK target inhibition,” said Anthony R. Mato, MD, of the Center for CLL at Memorial Sloan Kettering Cancer Center in New York.
Responses were also seen in patients with BTK C481 mutations, the primary cause of progressive CLL after BTK inhibitor use, Dr. Mato said at the annual meeting of the American Society of Hematology.
The safety and tolerability profile of LOXO-305 is “consistent with highly selective drug design,” with no evidence of off-target effects, he said. “Collectively, these data demonstrate that BTK remains a highly actionable target despite progression on covalent BTK inhibitors.”
While BTK inhibitors have transformed treatment of B-cell malignancies, resistance remains a major problem, said Dr. Mato, citing 5-year ibrutinib discontinuation rates of 41% in the front line setting and 53.7% in the relapsed/refractory setting.
Key reasons for discontinuation are intolerance, events such as atrial fibrillation and major bleeding, progression of disease, and the appearance of BTK C481 mutations, which prevent covalent BTK inhibitors from achieving effective target inhibition, he said. In contrast, LOXO-305 is designed to non-covalently bind to BTK, regardless of C481 status.
Dr. Mato described results of the phase 1 BRUIN trial, in which 28 adult patients with CLL or B-cell non-Hodgkin lymphomas received once daily oral LOXO-305 at doses ranging from 25 mg to 200 mg. All patients had received at least two lines of prior therapy and had active disease in need of treatment.
For 13 evaluable CLL patients, the overall response rate was 77% (10 patients), Dr. Mato reported. Overall response rates for MCL and other B-cell malignancies were 50%, or three out of six MCL patients and two of four patients with Waldenström macroglobulinemia, diffuse large B-cell lymphoma, or marginal zone lymphoma.
Though only a small subset of CLL patients have had multiple response assessments, the available data suggest that responses “deepen over time” with continued LOXO-305 treatment, Dr. Mato said.
With the median follow-up of 2.7 months, 24 of 28 patients remain on therapy, including all responders. “Some of the responses appear to be quite durable,” Dr. Mato said.
There have been no dose-limiting toxicities, the maximum tolerated dose has not been reached, and there have been no notable adverse events characteristic of covalent BTK inhibitors – namely atrial fibrillation or major bleeding – despite frequent monitoring, according to Dr. Mato.
There were two grade 3 events (leukocytosis and neutropenia), but the remaining treatment-emergent adverse events have been grade 1-2. “Having managed many of these patients, I can tell you that these adverse events were quite manageable,” Dr. Mato told attendees.
BRUIN is a global trial that continues to enroll patients at 18 sites in 3 countries, with a plan in 2020 to incorporate “rational combinations” of agents, according to the investigator.
Dr. Mato reported disclosures related to Gilead, Pharmacyclics, AstraZeneca, AbbVie, Sunesis, Johnson & Johnson, TG Therapeutics, LOXO, DTRM Biopharma, Genentech, Janssen, Acerta, Pharmacyclics, and Celgene.
SOURCE: Mato AR et al. ASH 2019, Abstract 501.
REPORTING FROM ASH 2019
Survival data reported from largest CAR T trial in B-cell lymphoma
ORLANDO – Updated results from the TRANSCEND NHL trial include survival data with lisocabtagene maraleucel (liso-cel), an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, in patients with relapsed/refractory B-cell lymphomas.
The median progression-free survival (PFS) was 6.8 months, and the median overall survival was 21.1 months. PFS results were best among complete responders and among patients with primary mediastinal large B-cell lymphoma or transformed follicular lymphoma.
Jeremy S. Abramson, MD, of Massachusetts General Hospital in Boston, presented these results at the annual meeting of the American Society of Hematology.
“TRANSCEND NHL is the largest clinical study to date of CD19-directed CAR T cells in patients with relapsed/refractory aggressive B-cell lymphoma,” Dr. Abramson said.
The phase 1 trial (NCT02631044) includes 269 patients who received liso-cel. They were diagnosed with transformed follicular lymphoma (22%) or other indolent lymphoma (7%), high-grade B-cell lymphoma (13%), primary mediastinal large B-cell lymphoma (6%), grade 3B follicular lymphoma (1%), or diffuse large B-cell lymphoma not otherwise specified (51%).
At baseline, patients had received a median of three prior systemic therapies (range, one to eight). Some patients had received autologous (33%) or allogeneic (3%) transplant. Many patients were chemotherapy refractory (67%) or had never achieved a complete response to prior therapy (44%).
More than half of patients (59%) received bridging therapy during liso-cel manufacturing. All patients received lymphodepletion with fludarabine and cyclophosphamide, followed by liso-cel at 50 x 106 CAR T cells, 100 x 106 CAR T cells, or 150 x 106 CAR T cells.
Response and survival
The median follow-up was 12.0 months. The overall response rate was 73%, and the complete response rate was 53%.
“Remissions were rapid, with a median of 1 month from CAR T-cell infusion, and durable, with a median duration of response that has not been reached and 55% of patients remaining in response at 1 year,” Dr. Abramson said.
The median PFS was 6.8 months overall, not reached for patients who achieved a complete response, 2.8 months for patients with a partial response, and 1.1 months for patients with stable disease or progressive disease.
The median PFS was not reached for patients with primary mediastinal large B-cell lymphoma or transformed follicular lymphoma, 5.0 months for high-grade B-cell lymphoma, 3.0 months for diffuse large B-cell lymphoma not otherwise specified, and 2.9 months in transformed indolent non-Hodgkin lymphoma.
The median overall survival was 21.1 months overall, not reached for patients who achieved a complete response, 9.0 months for patients who had a partial response, and 5.1 months for patients with stable disease or progressive disease.
Safety
Common treatment-emergent adverse events were neutropenia (63%), anemia (48%), fatigue (44%), nausea (33%), thrombocytopenia (31%), headache (30%), decreased appetite (28%), and diarrhea (26%).
Cytokine release syndrome (CRS) occurred in 42% of patients, and neurologic events occurred in 30%. Grade 3-4 CRS occurred in 2% of patients, and grade 3-4 neurologic events occurred in 10%. There were no cases of grade 5 CRS or neurologic events.
The median time to CRS onset was 5 days, and the median time to onset of neurologic events was 9 days. The median time to resolution of CRS and neurologic events was 5 days and 11 days, respectively.
“The low incidence of severe CRS and neurologic events and their late time of onset support using this product in a large range of patients and in the outpatient setting,” Dr. Abramson said.
There were seven grade 5 treatment-related adverse events, including diffuse alveolar damage, pulmonary hemorrhage, multiple organ dysfunction syndrome, cardiomyopathy, fludarabine leukoencephalopathy, septic shock, and progressive multifocal leukoencephalopathy.
This trial is sponsored by Bristol-Myers Squibb. Dr. Abramson reported relationships with Juno Therapeutics and Celgene, now owned by Bristol-Myers Squibb, and a range of other companies.
SOURCE: Abramson JS et al. ASH 2019, Abstract 241.
ORLANDO – Updated results from the TRANSCEND NHL trial include survival data with lisocabtagene maraleucel (liso-cel), an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, in patients with relapsed/refractory B-cell lymphomas.
The median progression-free survival (PFS) was 6.8 months, and the median overall survival was 21.1 months. PFS results were best among complete responders and among patients with primary mediastinal large B-cell lymphoma or transformed follicular lymphoma.
Jeremy S. Abramson, MD, of Massachusetts General Hospital in Boston, presented these results at the annual meeting of the American Society of Hematology.
“TRANSCEND NHL is the largest clinical study to date of CD19-directed CAR T cells in patients with relapsed/refractory aggressive B-cell lymphoma,” Dr. Abramson said.
The phase 1 trial (NCT02631044) includes 269 patients who received liso-cel. They were diagnosed with transformed follicular lymphoma (22%) or other indolent lymphoma (7%), high-grade B-cell lymphoma (13%), primary mediastinal large B-cell lymphoma (6%), grade 3B follicular lymphoma (1%), or diffuse large B-cell lymphoma not otherwise specified (51%).
At baseline, patients had received a median of three prior systemic therapies (range, one to eight). Some patients had received autologous (33%) or allogeneic (3%) transplant. Many patients were chemotherapy refractory (67%) or had never achieved a complete response to prior therapy (44%).
More than half of patients (59%) received bridging therapy during liso-cel manufacturing. All patients received lymphodepletion with fludarabine and cyclophosphamide, followed by liso-cel at 50 x 106 CAR T cells, 100 x 106 CAR T cells, or 150 x 106 CAR T cells.
Response and survival
The median follow-up was 12.0 months. The overall response rate was 73%, and the complete response rate was 53%.
“Remissions were rapid, with a median of 1 month from CAR T-cell infusion, and durable, with a median duration of response that has not been reached and 55% of patients remaining in response at 1 year,” Dr. Abramson said.
The median PFS was 6.8 months overall, not reached for patients who achieved a complete response, 2.8 months for patients with a partial response, and 1.1 months for patients with stable disease or progressive disease.
The median PFS was not reached for patients with primary mediastinal large B-cell lymphoma or transformed follicular lymphoma, 5.0 months for high-grade B-cell lymphoma, 3.0 months for diffuse large B-cell lymphoma not otherwise specified, and 2.9 months in transformed indolent non-Hodgkin lymphoma.
The median overall survival was 21.1 months overall, not reached for patients who achieved a complete response, 9.0 months for patients who had a partial response, and 5.1 months for patients with stable disease or progressive disease.
Safety
Common treatment-emergent adverse events were neutropenia (63%), anemia (48%), fatigue (44%), nausea (33%), thrombocytopenia (31%), headache (30%), decreased appetite (28%), and diarrhea (26%).
Cytokine release syndrome (CRS) occurred in 42% of patients, and neurologic events occurred in 30%. Grade 3-4 CRS occurred in 2% of patients, and grade 3-4 neurologic events occurred in 10%. There were no cases of grade 5 CRS or neurologic events.
The median time to CRS onset was 5 days, and the median time to onset of neurologic events was 9 days. The median time to resolution of CRS and neurologic events was 5 days and 11 days, respectively.
“The low incidence of severe CRS and neurologic events and their late time of onset support using this product in a large range of patients and in the outpatient setting,” Dr. Abramson said.
There were seven grade 5 treatment-related adverse events, including diffuse alveolar damage, pulmonary hemorrhage, multiple organ dysfunction syndrome, cardiomyopathy, fludarabine leukoencephalopathy, septic shock, and progressive multifocal leukoencephalopathy.
This trial is sponsored by Bristol-Myers Squibb. Dr. Abramson reported relationships with Juno Therapeutics and Celgene, now owned by Bristol-Myers Squibb, and a range of other companies.
SOURCE: Abramson JS et al. ASH 2019, Abstract 241.
ORLANDO – Updated results from the TRANSCEND NHL trial include survival data with lisocabtagene maraleucel (liso-cel), an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, in patients with relapsed/refractory B-cell lymphomas.
The median progression-free survival (PFS) was 6.8 months, and the median overall survival was 21.1 months. PFS results were best among complete responders and among patients with primary mediastinal large B-cell lymphoma or transformed follicular lymphoma.
Jeremy S. Abramson, MD, of Massachusetts General Hospital in Boston, presented these results at the annual meeting of the American Society of Hematology.
“TRANSCEND NHL is the largest clinical study to date of CD19-directed CAR T cells in patients with relapsed/refractory aggressive B-cell lymphoma,” Dr. Abramson said.
The phase 1 trial (NCT02631044) includes 269 patients who received liso-cel. They were diagnosed with transformed follicular lymphoma (22%) or other indolent lymphoma (7%), high-grade B-cell lymphoma (13%), primary mediastinal large B-cell lymphoma (6%), grade 3B follicular lymphoma (1%), or diffuse large B-cell lymphoma not otherwise specified (51%).
At baseline, patients had received a median of three prior systemic therapies (range, one to eight). Some patients had received autologous (33%) or allogeneic (3%) transplant. Many patients were chemotherapy refractory (67%) or had never achieved a complete response to prior therapy (44%).
More than half of patients (59%) received bridging therapy during liso-cel manufacturing. All patients received lymphodepletion with fludarabine and cyclophosphamide, followed by liso-cel at 50 x 106 CAR T cells, 100 x 106 CAR T cells, or 150 x 106 CAR T cells.
Response and survival
The median follow-up was 12.0 months. The overall response rate was 73%, and the complete response rate was 53%.
“Remissions were rapid, with a median of 1 month from CAR T-cell infusion, and durable, with a median duration of response that has not been reached and 55% of patients remaining in response at 1 year,” Dr. Abramson said.
The median PFS was 6.8 months overall, not reached for patients who achieved a complete response, 2.8 months for patients with a partial response, and 1.1 months for patients with stable disease or progressive disease.
The median PFS was not reached for patients with primary mediastinal large B-cell lymphoma or transformed follicular lymphoma, 5.0 months for high-grade B-cell lymphoma, 3.0 months for diffuse large B-cell lymphoma not otherwise specified, and 2.9 months in transformed indolent non-Hodgkin lymphoma.
The median overall survival was 21.1 months overall, not reached for patients who achieved a complete response, 9.0 months for patients who had a partial response, and 5.1 months for patients with stable disease or progressive disease.
Safety
Common treatment-emergent adverse events were neutropenia (63%), anemia (48%), fatigue (44%), nausea (33%), thrombocytopenia (31%), headache (30%), decreased appetite (28%), and diarrhea (26%).
Cytokine release syndrome (CRS) occurred in 42% of patients, and neurologic events occurred in 30%. Grade 3-4 CRS occurred in 2% of patients, and grade 3-4 neurologic events occurred in 10%. There were no cases of grade 5 CRS or neurologic events.
The median time to CRS onset was 5 days, and the median time to onset of neurologic events was 9 days. The median time to resolution of CRS and neurologic events was 5 days and 11 days, respectively.
“The low incidence of severe CRS and neurologic events and their late time of onset support using this product in a large range of patients and in the outpatient setting,” Dr. Abramson said.
There were seven grade 5 treatment-related adverse events, including diffuse alveolar damage, pulmonary hemorrhage, multiple organ dysfunction syndrome, cardiomyopathy, fludarabine leukoencephalopathy, septic shock, and progressive multifocal leukoencephalopathy.
This trial is sponsored by Bristol-Myers Squibb. Dr. Abramson reported relationships with Juno Therapeutics and Celgene, now owned by Bristol-Myers Squibb, and a range of other companies.
SOURCE: Abramson JS et al. ASH 2019, Abstract 241.
REPORTING FROM ASH 2019
D-RVd for frontline myeloma looks robust in GRIFFIN trial update
ORLANDO – While the benefit of daratumumab added to lenalidomide, bortezomib, and dexamethasone (D-RVd) continues to improve with longer follow-up of the GRIFFIN trial, even early adopters may want to wait for additional data before declaring the combination a first-line standard for transplant-eligible multiple myeloma, according to an investigator on the trial.
D-RVd has significantly improved both response rates and depth of response, compared with RVd alone, Peter M. Voorhees, MD, of Levine Cancer Institute, Atrium Health, Charlotte, N.C., reported at the annual meeting of the American Society of Hematology.
Additionally, rates of response and minimal residual disease (MRD) negativity with D-RVd have increased with longer follow-up beyond posttransplant consolidation, in the ongoing randomized phase 2 trial, Dr. Voorhees said.
“Those of you that are early adopters have good ammunition based on this result, but I would argue that we do need to confirm that the increased MRD-negative rate that we’re seeing translates into a sustained improvement in MRD negativity,” said Dr. Voorhees while presenting the updated results.
Most importantly, it needs to be confirmed that improved depth of response with D-RVd translates into an improvement in progression-free survival, not only in GRIFFIN, he said, but in PERSEUS, a large, randomized European phase 3 trial of subcutaneous daratumumab plus RVd versus RVd alone.
In the GRIFFIN trial, a total of 207 patients with transplant-eligible newly diagnosed multiple myeloma were randomized to intravenous daratumumab plus RVd versus RVd alone, with a primary endpoint of stringent complete response (sCR) by the end of consolidation.
Primary findings, presented in September at the 17th International Myeloma Workshop (IMW) meeting in Boston, indicated an sCR of 42.4% for D-RVd versus 32.0% for RVd at a median follow-up of 13.5 months, a difference that Dr. Voorhees said was statistically significant as defined by the protocol (1-sided P = .068), with an odds ratio of 1.57 (95% confidence interval, 0.87-2.82) in favor of the D-RVd arm.
With longer follow-up data, which Dr. Voorhees reported at ASH, the responses have “deepened over time” in both arms of the study, though he said the daratumumab arm continues to perform better. The sCR with 22.1 months of follow-up was 62.6% for D-RVd versus 45.4% for RVd.
The rates of MRD negativity at this clinical cutoff were 51.0% versus 20.4% for the D-RVd and RVd arms, respectively (P less than .0001), while the 24-month PFS rates were 95.8% for D-RVd and 89.8% for RVd. “Suffice it to say that both groups of patients are doing incredibly well at 2 years,” Dr. Voorhees said.
Rates of grade 3 and 4 neutropenia and thrombocytopenia were higher in the D-RVd arm, and there were more infections, though this was largely driven by an increased incidence of grade 1 or 2 upper respiratory tract infections, according to Dr. Voorhees.
Daratumumab did not impact time to engraftment, with a median CD34+ cell yield of 8.2 x 106 cells/kg for D-RVd and 9.4 x 106 cells/kg for RVd, a difference that Dr. Voorhees said was “not of clinical significance.”
Dr. Voorhees reported disclosures related to Takeda, Oncopeptides, Novartis, GSK, Janssen, Celgene, BMS, Adaptive Biotechnologies, Amgen, and TeneBio.
SOURCE: Voorhees PM et al. ASH 2019, Abstract 691.
ORLANDO – While the benefit of daratumumab added to lenalidomide, bortezomib, and dexamethasone (D-RVd) continues to improve with longer follow-up of the GRIFFIN trial, even early adopters may want to wait for additional data before declaring the combination a first-line standard for transplant-eligible multiple myeloma, according to an investigator on the trial.
D-RVd has significantly improved both response rates and depth of response, compared with RVd alone, Peter M. Voorhees, MD, of Levine Cancer Institute, Atrium Health, Charlotte, N.C., reported at the annual meeting of the American Society of Hematology.
Additionally, rates of response and minimal residual disease (MRD) negativity with D-RVd have increased with longer follow-up beyond posttransplant consolidation, in the ongoing randomized phase 2 trial, Dr. Voorhees said.
“Those of you that are early adopters have good ammunition based on this result, but I would argue that we do need to confirm that the increased MRD-negative rate that we’re seeing translates into a sustained improvement in MRD negativity,” said Dr. Voorhees while presenting the updated results.
Most importantly, it needs to be confirmed that improved depth of response with D-RVd translates into an improvement in progression-free survival, not only in GRIFFIN, he said, but in PERSEUS, a large, randomized European phase 3 trial of subcutaneous daratumumab plus RVd versus RVd alone.
In the GRIFFIN trial, a total of 207 patients with transplant-eligible newly diagnosed multiple myeloma were randomized to intravenous daratumumab plus RVd versus RVd alone, with a primary endpoint of stringent complete response (sCR) by the end of consolidation.
Primary findings, presented in September at the 17th International Myeloma Workshop (IMW) meeting in Boston, indicated an sCR of 42.4% for D-RVd versus 32.0% for RVd at a median follow-up of 13.5 months, a difference that Dr. Voorhees said was statistically significant as defined by the protocol (1-sided P = .068), with an odds ratio of 1.57 (95% confidence interval, 0.87-2.82) in favor of the D-RVd arm.
With longer follow-up data, which Dr. Voorhees reported at ASH, the responses have “deepened over time” in both arms of the study, though he said the daratumumab arm continues to perform better. The sCR with 22.1 months of follow-up was 62.6% for D-RVd versus 45.4% for RVd.
The rates of MRD negativity at this clinical cutoff were 51.0% versus 20.4% for the D-RVd and RVd arms, respectively (P less than .0001), while the 24-month PFS rates were 95.8% for D-RVd and 89.8% for RVd. “Suffice it to say that both groups of patients are doing incredibly well at 2 years,” Dr. Voorhees said.
Rates of grade 3 and 4 neutropenia and thrombocytopenia were higher in the D-RVd arm, and there were more infections, though this was largely driven by an increased incidence of grade 1 or 2 upper respiratory tract infections, according to Dr. Voorhees.
Daratumumab did not impact time to engraftment, with a median CD34+ cell yield of 8.2 x 106 cells/kg for D-RVd and 9.4 x 106 cells/kg for RVd, a difference that Dr. Voorhees said was “not of clinical significance.”
Dr. Voorhees reported disclosures related to Takeda, Oncopeptides, Novartis, GSK, Janssen, Celgene, BMS, Adaptive Biotechnologies, Amgen, and TeneBio.
SOURCE: Voorhees PM et al. ASH 2019, Abstract 691.
ORLANDO – While the benefit of daratumumab added to lenalidomide, bortezomib, and dexamethasone (D-RVd) continues to improve with longer follow-up of the GRIFFIN trial, even early adopters may want to wait for additional data before declaring the combination a first-line standard for transplant-eligible multiple myeloma, according to an investigator on the trial.
D-RVd has significantly improved both response rates and depth of response, compared with RVd alone, Peter M. Voorhees, MD, of Levine Cancer Institute, Atrium Health, Charlotte, N.C., reported at the annual meeting of the American Society of Hematology.
Additionally, rates of response and minimal residual disease (MRD) negativity with D-RVd have increased with longer follow-up beyond posttransplant consolidation, in the ongoing randomized phase 2 trial, Dr. Voorhees said.
“Those of you that are early adopters have good ammunition based on this result, but I would argue that we do need to confirm that the increased MRD-negative rate that we’re seeing translates into a sustained improvement in MRD negativity,” said Dr. Voorhees while presenting the updated results.
Most importantly, it needs to be confirmed that improved depth of response with D-RVd translates into an improvement in progression-free survival, not only in GRIFFIN, he said, but in PERSEUS, a large, randomized European phase 3 trial of subcutaneous daratumumab plus RVd versus RVd alone.
In the GRIFFIN trial, a total of 207 patients with transplant-eligible newly diagnosed multiple myeloma were randomized to intravenous daratumumab plus RVd versus RVd alone, with a primary endpoint of stringent complete response (sCR) by the end of consolidation.
Primary findings, presented in September at the 17th International Myeloma Workshop (IMW) meeting in Boston, indicated an sCR of 42.4% for D-RVd versus 32.0% for RVd at a median follow-up of 13.5 months, a difference that Dr. Voorhees said was statistically significant as defined by the protocol (1-sided P = .068), with an odds ratio of 1.57 (95% confidence interval, 0.87-2.82) in favor of the D-RVd arm.
With longer follow-up data, which Dr. Voorhees reported at ASH, the responses have “deepened over time” in both arms of the study, though he said the daratumumab arm continues to perform better. The sCR with 22.1 months of follow-up was 62.6% for D-RVd versus 45.4% for RVd.
The rates of MRD negativity at this clinical cutoff were 51.0% versus 20.4% for the D-RVd and RVd arms, respectively (P less than .0001), while the 24-month PFS rates were 95.8% for D-RVd and 89.8% for RVd. “Suffice it to say that both groups of patients are doing incredibly well at 2 years,” Dr. Voorhees said.
Rates of grade 3 and 4 neutropenia and thrombocytopenia were higher in the D-RVd arm, and there were more infections, though this was largely driven by an increased incidence of grade 1 or 2 upper respiratory tract infections, according to Dr. Voorhees.
Daratumumab did not impact time to engraftment, with a median CD34+ cell yield of 8.2 x 106 cells/kg for D-RVd and 9.4 x 106 cells/kg for RVd, a difference that Dr. Voorhees said was “not of clinical significance.”
Dr. Voorhees reported disclosures related to Takeda, Oncopeptides, Novartis, GSK, Janssen, Celgene, BMS, Adaptive Biotechnologies, Amgen, and TeneBio.
SOURCE: Voorhees PM et al. ASH 2019, Abstract 691.
REPORTING FROM ASH 2019
Some MCL patients can safely stop venetoclax-ibrutinib, study suggests
ORLANDO – Updated trial results have revealed durable responses with venetoclax and ibrutinib in patients with mantle cell lymphoma (MCL), allowing some patients to stop treatment.
Five of 24 patients were able to stop treatment after achieving minimal residual disease (MRD)-negative complete responses (CRs). Four of these patients remain in CR at up to 18 months off treatment, although one patient ultimately progressed and died.
“Treatment cessation was feasible for patients in MRD-negative complete responses, raising the prospect of limited-duration, targeted-agent therapy in the management of relapsed/refractory mantle cell lymphoma,” said Sasanka M. Handunnetti, MBBS, of Peter MacCallum Cancer Centre in Melbourne. Dr. Handunnetti presented these results, from the AIM trial, at the annual meeting of the American Society of Hematology.
The phase 2 trial enrolled 24 patients. At baseline, patients had a median age of 68 years (range, 47-81 years), and 88% were men. One patient was treatment-naive, but the rest had relapsed/refractory MCL. These patients had received a median of two prior therapies (range, 1-6).
The patients received venetoclax at 400 mg daily and ibrutinib at 560 mg daily.
In the primary analysis, the CR rate was 62% at week 16 and 71% overall, according to positron-emission tomography/computed tomography. MRD negativity was achieved by 67% of patients according to flow cytometry and 38% according to allele-specific oligonucleotide polymerase chain reaction (N Engl J Med. 2018 Mar 29;378[13]:1211-23).
Response and survival
For the current analysis, the median follow up was 37.5 months (range, 1.4-45.3 months). The median duration of response has not been reached, the median progression-free survival is 29 months, and the median overall survival is 32 months.
Thirteen patients have died, 8 of them due to progressive disease. The remaining 11 patients are still alive, and 9 of them are still in CR. One patient is still in partial response, and one has not responded but remains on ibrutinib and venetoclax.
Dr. Handunnetti pointed out that 12 patients had TP53 aberrations, and 8 of them died, but 4 remain alive and in CR. All four patients with SMARCA4 aberrations died.
Treatment status
Five patients are still receiving treatment with ibrutinib and venetoclax, and one patient is receiving only venetoclax. One patient went off study treatment due to a diagnosis of myelodysplastic syndrome, but that patient’s MCL is still in CR.
Five patients were able to stop treatment after achieving MRD-negative CR and were placed under “stringent surveillance,” Dr. Handunnetti said.
One of the five patients who stopped treatment progressed at 7 months and died. The remaining four patients are still alive and in CR at 6 months, 13 months, 17 months, and 18 months off treatment.
Safety update
Within the first 56 weeks of treatment, 15 patients required dose adjustments. Twelve patients required an adjustment to ibrutinib, seven to venetoclax, and four to both drugs. After 56 weeks, there were no dose adjustments.
Two patients developed therapy-related myelodysplastic syndrome. One patient had previously received FCR (fludarabine, cyclophosphamide, and rituximab) and BR (bendamustine and rituximab). The other patient had received R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
This investigator-initiated trial was funded by Janssen and Abbvie. Dr. Handunnetti reported relationships with Abbvie and Gilead.
SOURCE: Handunnetti S et al. ASH 2019. Abstract 756.
ORLANDO – Updated trial results have revealed durable responses with venetoclax and ibrutinib in patients with mantle cell lymphoma (MCL), allowing some patients to stop treatment.
Five of 24 patients were able to stop treatment after achieving minimal residual disease (MRD)-negative complete responses (CRs). Four of these patients remain in CR at up to 18 months off treatment, although one patient ultimately progressed and died.
“Treatment cessation was feasible for patients in MRD-negative complete responses, raising the prospect of limited-duration, targeted-agent therapy in the management of relapsed/refractory mantle cell lymphoma,” said Sasanka M. Handunnetti, MBBS, of Peter MacCallum Cancer Centre in Melbourne. Dr. Handunnetti presented these results, from the AIM trial, at the annual meeting of the American Society of Hematology.
The phase 2 trial enrolled 24 patients. At baseline, patients had a median age of 68 years (range, 47-81 years), and 88% were men. One patient was treatment-naive, but the rest had relapsed/refractory MCL. These patients had received a median of two prior therapies (range, 1-6).
The patients received venetoclax at 400 mg daily and ibrutinib at 560 mg daily.
In the primary analysis, the CR rate was 62% at week 16 and 71% overall, according to positron-emission tomography/computed tomography. MRD negativity was achieved by 67% of patients according to flow cytometry and 38% according to allele-specific oligonucleotide polymerase chain reaction (N Engl J Med. 2018 Mar 29;378[13]:1211-23).
Response and survival
For the current analysis, the median follow up was 37.5 months (range, 1.4-45.3 months). The median duration of response has not been reached, the median progression-free survival is 29 months, and the median overall survival is 32 months.
Thirteen patients have died, 8 of them due to progressive disease. The remaining 11 patients are still alive, and 9 of them are still in CR. One patient is still in partial response, and one has not responded but remains on ibrutinib and venetoclax.
Dr. Handunnetti pointed out that 12 patients had TP53 aberrations, and 8 of them died, but 4 remain alive and in CR. All four patients with SMARCA4 aberrations died.
Treatment status
Five patients are still receiving treatment with ibrutinib and venetoclax, and one patient is receiving only venetoclax. One patient went off study treatment due to a diagnosis of myelodysplastic syndrome, but that patient’s MCL is still in CR.
Five patients were able to stop treatment after achieving MRD-negative CR and were placed under “stringent surveillance,” Dr. Handunnetti said.
One of the five patients who stopped treatment progressed at 7 months and died. The remaining four patients are still alive and in CR at 6 months, 13 months, 17 months, and 18 months off treatment.
Safety update
Within the first 56 weeks of treatment, 15 patients required dose adjustments. Twelve patients required an adjustment to ibrutinib, seven to venetoclax, and four to both drugs. After 56 weeks, there were no dose adjustments.
Two patients developed therapy-related myelodysplastic syndrome. One patient had previously received FCR (fludarabine, cyclophosphamide, and rituximab) and BR (bendamustine and rituximab). The other patient had received R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
This investigator-initiated trial was funded by Janssen and Abbvie. Dr. Handunnetti reported relationships with Abbvie and Gilead.
SOURCE: Handunnetti S et al. ASH 2019. Abstract 756.
ORLANDO – Updated trial results have revealed durable responses with venetoclax and ibrutinib in patients with mantle cell lymphoma (MCL), allowing some patients to stop treatment.
Five of 24 patients were able to stop treatment after achieving minimal residual disease (MRD)-negative complete responses (CRs). Four of these patients remain in CR at up to 18 months off treatment, although one patient ultimately progressed and died.
“Treatment cessation was feasible for patients in MRD-negative complete responses, raising the prospect of limited-duration, targeted-agent therapy in the management of relapsed/refractory mantle cell lymphoma,” said Sasanka M. Handunnetti, MBBS, of Peter MacCallum Cancer Centre in Melbourne. Dr. Handunnetti presented these results, from the AIM trial, at the annual meeting of the American Society of Hematology.
The phase 2 trial enrolled 24 patients. At baseline, patients had a median age of 68 years (range, 47-81 years), and 88% were men. One patient was treatment-naive, but the rest had relapsed/refractory MCL. These patients had received a median of two prior therapies (range, 1-6).
The patients received venetoclax at 400 mg daily and ibrutinib at 560 mg daily.
In the primary analysis, the CR rate was 62% at week 16 and 71% overall, according to positron-emission tomography/computed tomography. MRD negativity was achieved by 67% of patients according to flow cytometry and 38% according to allele-specific oligonucleotide polymerase chain reaction (N Engl J Med. 2018 Mar 29;378[13]:1211-23).
Response and survival
For the current analysis, the median follow up was 37.5 months (range, 1.4-45.3 months). The median duration of response has not been reached, the median progression-free survival is 29 months, and the median overall survival is 32 months.
Thirteen patients have died, 8 of them due to progressive disease. The remaining 11 patients are still alive, and 9 of them are still in CR. One patient is still in partial response, and one has not responded but remains on ibrutinib and venetoclax.
Dr. Handunnetti pointed out that 12 patients had TP53 aberrations, and 8 of them died, but 4 remain alive and in CR. All four patients with SMARCA4 aberrations died.
Treatment status
Five patients are still receiving treatment with ibrutinib and venetoclax, and one patient is receiving only venetoclax. One patient went off study treatment due to a diagnosis of myelodysplastic syndrome, but that patient’s MCL is still in CR.
Five patients were able to stop treatment after achieving MRD-negative CR and were placed under “stringent surveillance,” Dr. Handunnetti said.
One of the five patients who stopped treatment progressed at 7 months and died. The remaining four patients are still alive and in CR at 6 months, 13 months, 17 months, and 18 months off treatment.
Safety update
Within the first 56 weeks of treatment, 15 patients required dose adjustments. Twelve patients required an adjustment to ibrutinib, seven to venetoclax, and four to both drugs. After 56 weeks, there were no dose adjustments.
Two patients developed therapy-related myelodysplastic syndrome. One patient had previously received FCR (fludarabine, cyclophosphamide, and rituximab) and BR (bendamustine and rituximab). The other patient had received R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
This investigator-initiated trial was funded by Janssen and Abbvie. Dr. Handunnetti reported relationships with Abbvie and Gilead.
SOURCE: Handunnetti S et al. ASH 2019. Abstract 756.
REPORTING FROM ASH 2019
KTE-X19 produces highest response rate in MCL subgroup
ORLANDO – KTE-X19, an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, demonstrated unprecedented efficacy in the ZUMA-2 trial, according to an investigator involved in the study.
KTE-X19 produced a 93% overall response rate in patients with relapsed/refractory mantle cell lymphoma (MCL). This is the highest reported response rate in patients who have failed treatment with a Bruton’s tyrosine kinase (BTK) inhibitor, said Michael L. Wang, MD, of the University of Texas MD Anderson Cancer Center in Houston.
Dr. Wang presented results from ZUMA-2 at the annual meeting of the American Society of Hematology.
“Patients with relapsed/refractory MCL have very poor outcomes,” Dr. Wang noted. “In patients who progress after BTK inhibition therapy, the overall response rate is only between 25% and 42%, and the overall survival is only between 6 and 10 months. Few patients proceed to allogeneic transplantation.”
The phase 2 ZUMA-2 trial was designed to test KTE-X19 in these patients. KTE-X19 is an anti-CD19 CAR T-cell therapy containing a CD3-zeta T-cell activation domain and a CD28 signaling domain. KTE-X19 is distinct from axicabtagene ciloleucel (KTE-C19) because the manufacturing process for KTE-X19 removes circulating tumor cells.
The trial enrolled 74 patients, and 68 of them received KTE-X19. Manufacturing failed for three patients, two patients died of progressive disease before they could receive KTE-X19, and one patient was found to be ineligible for treatment.
The 68 patients had a median age of 65 years (range, 38-79 years), and 84% were men. A majority of patients (85%) had stage IV disease and classical (59%) or blastoid (25%) morphology. Most patients (69%) had a Ki-67 proliferation index of 50% or greater, and most (56%) were intermediate- or high-risk according to the Mantle Cell Lymphoma International Prognostic Index (MIPI).
Patients had received a median of three prior therapies (range, one to five). All had been treated with a BTK inhibitor, with 85% receiving ibrutinib, 24% receiving acalabrutinib, and 9% receiving both. Most patients (68%) were refractory to BTK inhibition, and 32% relapsed on or after BTK inhibitor therapy.
In this study, patients could receive bridging therapy to keep their disease stable while KTE-X19 was being manufactured. There were 25 patients who received bridging therapy, which consisted of ibrutinib (n = 14), acalabrutinib (n = 5), dexamethasone (n = 12), and/or methylprednisolone (n = 2). Six patients received both BTK inhibitors and steroids.
All patients received conditioning with fludarabine and cyclophosphamide, followed by a single infusion of KTE-X19 at 2x106.
Efficacy
Sixty patients were evaluable for efficacy, and the median follow-up was 12.3 months (range, 7.0-32.3 months).
The overall response rate was 93%, with 67% of patients achieving a complete response and 27% achieving a partial response. Three percent of patients had stable disease, and 3% had progressive disease.
“The overall response rate was consistent across key subgroups, without any statistical difference,” Dr. Wang said. “This includes Ki-67, MIPI, and prior use of either steroids or bridging therapy.”
The median time to response was 1.0 month, and the median time to complete response was 3.0 months. Responses deepened over time, with 35% of patients converting from a partial response to a complete response, and 5% converting from stable disease to complete response.
The median duration of response has not been reached. At last follow-up, 57% of all patients and 78% of complete responders were still in response.
The median progression-free and overall survival have not been reached. At 12 months, the progression-free survival rate was 61%, and the overall survival rate was 83%.
Safety
All 68 patients were evaluable for safety. The most common adverse events were pyrexia (94%), neutropenia (87%), thrombocytopenia (74%), anemia (68%), and hypotension (51%).
Grade 3/4 adverse events included pyrexia (13%), neutropenia (85%), thrombocytopenia (51%), anemia (50%), hypotension (22%), hypoxia (21%), hypophosphatemia (22%), fatigue (1%), and headache (1%).
There were two grade 5 treatment-related adverse events – organizing pneumonia on day 37 and staphylococcal bacteremia on day 134.
Cytokine release syndrome (CRS) occurred in 91% of patients, with 15% experiencing grade 3 or higher CRS. Patients were treated with tocilizumab or corticosteroids, and all CRS events resolved.
Neurologic adverse events occurred in 63% of patients, with grade 3 or higher events occurring in 31%. Neurologic events were treated with tocilizumab or corticosteroids, and 86% of neurologic events resolved.
This trial was sponsored by Kite, a Gilead company. Dr. Wang reported financial relationships with Kite and other companies.
SOURCE: Wang M et al. ASH 2019. Abstract 754.
ORLANDO – KTE-X19, an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, demonstrated unprecedented efficacy in the ZUMA-2 trial, according to an investigator involved in the study.
KTE-X19 produced a 93% overall response rate in patients with relapsed/refractory mantle cell lymphoma (MCL). This is the highest reported response rate in patients who have failed treatment with a Bruton’s tyrosine kinase (BTK) inhibitor, said Michael L. Wang, MD, of the University of Texas MD Anderson Cancer Center in Houston.
Dr. Wang presented results from ZUMA-2 at the annual meeting of the American Society of Hematology.
“Patients with relapsed/refractory MCL have very poor outcomes,” Dr. Wang noted. “In patients who progress after BTK inhibition therapy, the overall response rate is only between 25% and 42%, and the overall survival is only between 6 and 10 months. Few patients proceed to allogeneic transplantation.”
The phase 2 ZUMA-2 trial was designed to test KTE-X19 in these patients. KTE-X19 is an anti-CD19 CAR T-cell therapy containing a CD3-zeta T-cell activation domain and a CD28 signaling domain. KTE-X19 is distinct from axicabtagene ciloleucel (KTE-C19) because the manufacturing process for KTE-X19 removes circulating tumor cells.
The trial enrolled 74 patients, and 68 of them received KTE-X19. Manufacturing failed for three patients, two patients died of progressive disease before they could receive KTE-X19, and one patient was found to be ineligible for treatment.
The 68 patients had a median age of 65 years (range, 38-79 years), and 84% were men. A majority of patients (85%) had stage IV disease and classical (59%) or blastoid (25%) morphology. Most patients (69%) had a Ki-67 proliferation index of 50% or greater, and most (56%) were intermediate- or high-risk according to the Mantle Cell Lymphoma International Prognostic Index (MIPI).
Patients had received a median of three prior therapies (range, one to five). All had been treated with a BTK inhibitor, with 85% receiving ibrutinib, 24% receiving acalabrutinib, and 9% receiving both. Most patients (68%) were refractory to BTK inhibition, and 32% relapsed on or after BTK inhibitor therapy.
In this study, patients could receive bridging therapy to keep their disease stable while KTE-X19 was being manufactured. There were 25 patients who received bridging therapy, which consisted of ibrutinib (n = 14), acalabrutinib (n = 5), dexamethasone (n = 12), and/or methylprednisolone (n = 2). Six patients received both BTK inhibitors and steroids.
All patients received conditioning with fludarabine and cyclophosphamide, followed by a single infusion of KTE-X19 at 2x106.
Efficacy
Sixty patients were evaluable for efficacy, and the median follow-up was 12.3 months (range, 7.0-32.3 months).
The overall response rate was 93%, with 67% of patients achieving a complete response and 27% achieving a partial response. Three percent of patients had stable disease, and 3% had progressive disease.
“The overall response rate was consistent across key subgroups, without any statistical difference,” Dr. Wang said. “This includes Ki-67, MIPI, and prior use of either steroids or bridging therapy.”
The median time to response was 1.0 month, and the median time to complete response was 3.0 months. Responses deepened over time, with 35% of patients converting from a partial response to a complete response, and 5% converting from stable disease to complete response.
The median duration of response has not been reached. At last follow-up, 57% of all patients and 78% of complete responders were still in response.
The median progression-free and overall survival have not been reached. At 12 months, the progression-free survival rate was 61%, and the overall survival rate was 83%.
Safety
All 68 patients were evaluable for safety. The most common adverse events were pyrexia (94%), neutropenia (87%), thrombocytopenia (74%), anemia (68%), and hypotension (51%).
Grade 3/4 adverse events included pyrexia (13%), neutropenia (85%), thrombocytopenia (51%), anemia (50%), hypotension (22%), hypoxia (21%), hypophosphatemia (22%), fatigue (1%), and headache (1%).
There were two grade 5 treatment-related adverse events – organizing pneumonia on day 37 and staphylococcal bacteremia on day 134.
Cytokine release syndrome (CRS) occurred in 91% of patients, with 15% experiencing grade 3 or higher CRS. Patients were treated with tocilizumab or corticosteroids, and all CRS events resolved.
Neurologic adverse events occurred in 63% of patients, with grade 3 or higher events occurring in 31%. Neurologic events were treated with tocilizumab or corticosteroids, and 86% of neurologic events resolved.
This trial was sponsored by Kite, a Gilead company. Dr. Wang reported financial relationships with Kite and other companies.
SOURCE: Wang M et al. ASH 2019. Abstract 754.
ORLANDO – KTE-X19, an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, demonstrated unprecedented efficacy in the ZUMA-2 trial, according to an investigator involved in the study.
KTE-X19 produced a 93% overall response rate in patients with relapsed/refractory mantle cell lymphoma (MCL). This is the highest reported response rate in patients who have failed treatment with a Bruton’s tyrosine kinase (BTK) inhibitor, said Michael L. Wang, MD, of the University of Texas MD Anderson Cancer Center in Houston.
Dr. Wang presented results from ZUMA-2 at the annual meeting of the American Society of Hematology.
“Patients with relapsed/refractory MCL have very poor outcomes,” Dr. Wang noted. “In patients who progress after BTK inhibition therapy, the overall response rate is only between 25% and 42%, and the overall survival is only between 6 and 10 months. Few patients proceed to allogeneic transplantation.”
The phase 2 ZUMA-2 trial was designed to test KTE-X19 in these patients. KTE-X19 is an anti-CD19 CAR T-cell therapy containing a CD3-zeta T-cell activation domain and a CD28 signaling domain. KTE-X19 is distinct from axicabtagene ciloleucel (KTE-C19) because the manufacturing process for KTE-X19 removes circulating tumor cells.
The trial enrolled 74 patients, and 68 of them received KTE-X19. Manufacturing failed for three patients, two patients died of progressive disease before they could receive KTE-X19, and one patient was found to be ineligible for treatment.
The 68 patients had a median age of 65 years (range, 38-79 years), and 84% were men. A majority of patients (85%) had stage IV disease and classical (59%) or blastoid (25%) morphology. Most patients (69%) had a Ki-67 proliferation index of 50% or greater, and most (56%) were intermediate- or high-risk according to the Mantle Cell Lymphoma International Prognostic Index (MIPI).
Patients had received a median of three prior therapies (range, one to five). All had been treated with a BTK inhibitor, with 85% receiving ibrutinib, 24% receiving acalabrutinib, and 9% receiving both. Most patients (68%) were refractory to BTK inhibition, and 32% relapsed on or after BTK inhibitor therapy.
In this study, patients could receive bridging therapy to keep their disease stable while KTE-X19 was being manufactured. There were 25 patients who received bridging therapy, which consisted of ibrutinib (n = 14), acalabrutinib (n = 5), dexamethasone (n = 12), and/or methylprednisolone (n = 2). Six patients received both BTK inhibitors and steroids.
All patients received conditioning with fludarabine and cyclophosphamide, followed by a single infusion of KTE-X19 at 2x106.
Efficacy
Sixty patients were evaluable for efficacy, and the median follow-up was 12.3 months (range, 7.0-32.3 months).
The overall response rate was 93%, with 67% of patients achieving a complete response and 27% achieving a partial response. Three percent of patients had stable disease, and 3% had progressive disease.
“The overall response rate was consistent across key subgroups, without any statistical difference,” Dr. Wang said. “This includes Ki-67, MIPI, and prior use of either steroids or bridging therapy.”
The median time to response was 1.0 month, and the median time to complete response was 3.0 months. Responses deepened over time, with 35% of patients converting from a partial response to a complete response, and 5% converting from stable disease to complete response.
The median duration of response has not been reached. At last follow-up, 57% of all patients and 78% of complete responders were still in response.
The median progression-free and overall survival have not been reached. At 12 months, the progression-free survival rate was 61%, and the overall survival rate was 83%.
Safety
All 68 patients were evaluable for safety. The most common adverse events were pyrexia (94%), neutropenia (87%), thrombocytopenia (74%), anemia (68%), and hypotension (51%).
Grade 3/4 adverse events included pyrexia (13%), neutropenia (85%), thrombocytopenia (51%), anemia (50%), hypotension (22%), hypoxia (21%), hypophosphatemia (22%), fatigue (1%), and headache (1%).
There were two grade 5 treatment-related adverse events – organizing pneumonia on day 37 and staphylococcal bacteremia on day 134.
Cytokine release syndrome (CRS) occurred in 91% of patients, with 15% experiencing grade 3 or higher CRS. Patients were treated with tocilizumab or corticosteroids, and all CRS events resolved.
Neurologic adverse events occurred in 63% of patients, with grade 3 or higher events occurring in 31%. Neurologic events were treated with tocilizumab or corticosteroids, and 86% of neurologic events resolved.
This trial was sponsored by Kite, a Gilead company. Dr. Wang reported financial relationships with Kite and other companies.
SOURCE: Wang M et al. ASH 2019. Abstract 754.
REPORTING FROM ASH 2019
An off-the-shelf drug to rival CAR T cells: ‘very exciting’
ORLANDO – An investigational drug that can achieve the same results as complex cell therapy is creating a buzz at the American Society of Hematology (ASH) meeting.
For the last few years, attention at this meeting has focused on the chimeric antigen receptor (CAR) T cells, mainly “because of their incredible efficacy,” commented ASH Secretary Robert A. Brodsky, MD, professor of medicine and director of the division of hematology at Johns Hopkins University, Baltimore.
But new results with an off-the-shelf product are “very exciting,” he said, because the drug can be given immediately and appears to achieve similar results.
The new product is mosunetuzumab (Genentech/Roche), a bispecific antibody that targets both CD3 (on the surface of T cells) and CD20 (on the surface of B cells). It works by redirecting T cells to engage and eliminate malignant B cells.
“The concept here is that this monoclonal antibody engages T cells and directs their cytotoxicity against B cells – it’s basically an antibody using the patient’s own T cells to do what a CAR T cell would do,” Dr. Brodsky explained.
However, unlike CAR T cells, which are prepared for each individual patient in a complex process that involves genetic engineering that can take several weeks, mosunetuzumab is an off-the-shelf product that can be given to patients immediately (by intravenous infusion).
This is important, commented Dr. Brodsky, because very-poor-prognosis patients can deteriorate rapidly, and some may not survive while the CAR T cells are being made.
Clinical trial results
Clinical results come from a phase 1/1b trial (known as GO29781) conducted in 270 patients with poor-prognosis refractory/relapsed non-Hodgkin’s lymphoma. These patients had previously been treated with a median of three therapies; in addition, 30 patients (11%) were resistant to or had relapsed after an initial response to CAR T-cell therapy, and 77 patients (29%) had progressed after a stem cell transplant.
“These patients had no available therapy that would be expected to improve survival,” noted lead author Stephen J. Schuster, MD, of Abramson Cancer Center at the University of Pennsylvania in Philadelphia.
All patients received mosunetuzumab with an initial treatment of eight cycles. Patients who achieved complete remission (CR) stopped therapy, while patients who had a partial response or had stable disease, continued treatment for 17 cycles.
Two-thirds of patients (n = 180; 67%) had aggressive lymphomas, mainly diffuse large B-cell lymphoma (DLBCL; n = 117), while 85 patients (31%) had indolent disease, mainly follicular lymphoma (FL; n = 82). Objective responses were seen in 46 of 124 patients (37%) with aggressive lymphomas, and 24 (19%) of these patients achieved a CR.
Among patients with indolent lymphoma, objective responses were seen in 42 of 67 patients (63%), and 29 of 67 (43%) had CR.
The complete remissions appear to be long lasting, Dr. Schuster commented. With a median follow-up of 6 months since achieving CR, 17 of 24 patients (71%) with aggressive lymphoma and 24 of 29 patients (83%) with indolent lymphomas remained free of disease.
“Some patients have remained in remission without additional therapy for more than a year,” he commented.
In the subgroup of 30 patients who had previously received CAR T-cell therapy, the objective response rate was 38.9%, and CR was achieved in 4 patients (22%). These rates are similar to what was seen in patients with aggressive lymphoma who had not previously received CAR T-cell therapy, Dr. Schuster commented.
He also noted that in some of these patients, molecular testing showed that the previously administered CAR T cells increased in number. This suggests that, in addition to its ability to kill cancerous B cells, mosunetuzumab may also help augment the effect of the prior CAR T-cell treatment.
Dr. Schuster also highlighted the results of repeat treatment with mosunetuzumab. Patients who achieved CR stopped treatment – but if they relapsed, they were treated again, and the responses seen on this repeat treatment were similar to those seen with initial treatment. “This is not seen with the CAR T cells,” he noted.
Adverse events with mosunetuzumab were similar to those seen with CAR T cells, he noted, namely cytokine release syndrome, which was mostly mild and seen in 29% of patients, and neurologic toxicity, which was moderately severe in 4% patients.
Overall, the results show that “mosunetuzumab generates long-lasting responses with a very tolerable safety profile in patients with B-cell non-Hodgkin lymphomas for whom multiple prior treatments have failed and whose prognosis is poor. Of particular interest, we are seeing durable complete remissions in patients whose lymphomas progressed after CAR T,” Dr. Schuster commented in a statement.
Approached for comment, Peter Martin MD, chief of the Lymphoma Program at Weill Cornell Medicine, New York, and New York-Presbyterian, said he was excited to see these new data. “It’s good news any time we find something with the potential to save lives.”
“The more options that we have to offer to people with lymphoma the better,” he told Medscape Medical News. “There will always be scenarios where one approach might be better than another. I think there is a good chance that bispecific antibodies will have fairly broad approval in previously treated DLBCL. In many centers, it may be that bispecific antibodies are used most frequently post–CAR T cells, while in other areas people who aren’t candidates for CAR T cells or can’t receive them for whatever reason [could benefit from this new approach].”
Laurie Sehn, MD, MPH, medical oncologist at the University of British Columbia in Vancouver, Canada, and chair of the Lymphoma Tumour Group, as well as an associate editor of ASH journal Blood, also commented for Medscape Medical News.
She agreed that the new data are exciting and noted that this abstract was chosen for the plenary session. She thought the data in the 30 patients who had already been treated with CAR T cells was interesting. “This is a patient population with no other options that offer durable benefit, and mosunetuzumab clearly has clinical activity, with encouraging responses.”
Dr. Sehn also noted that toxicity seen with the drug was “far less” than has been seen with CAR T cells, and the risk of high-grade cytokine release syndrome and neurological toxicity is “very low.”
There are several other new products that are using this bispecific technology, she noted. One example is Regeneron’s REGN1979, a bispecific antibody targeting CD20 and CD3, which is also being investigated in a clinical trial in relapsed/refractory B-cell non-Hodgkin’s lymphoma, including in patients who were previously treated with CAR T cells (abstract 762).
How would it be used clinically?
In response to a question from Medscape Medical News, Dr. Schuster suggested that initial use of mosunetuzumab would be in patients who have already tried CAR T-cell therapy and had either not responded or relapsed – in lymphoma, this is about two-thirds of patients who are treated with this approach. This group of patients represents an unmet medical need, and this indication may be the quickest route to approval, he suggested.
Gary Schiller, MD, from UCLA Health, who moderated the press briefing agreed, and said this would be the quickest route to market because it would need only a phase 2 clinical trial in this specific patient population. But this would likely be only the first use for this product, and then it could be expanded to a broader patient population, he added.
Another use would for mosunetuzumab would be to enhance CAR T-cell responses by redirecting the CAR T cells to other antigens without doing any additional gene editing, Dr. Schuster commented. The idea here is to “revive” previously administered CAR T cells that have stopped working, Dr. Schiller added.
This is a chemotherapy-free approach, Dr. Schuster emphasized. “In patients who have not had a lot of chemotherapy, you can see an increase in T cells,” he commented.
Mosunetuzumab “stimulates and invigorates T cells,” and it could be useful as a pretreatment or a bridge to CAR T-cell therapy, he said.
So the product could be used before CAR T-cell therapy, and equally it could be used after CAR T-cell therapy because it could boost responses in both cases.
“Larger, randomized trials are needed to further confirm these promising data and determine whether the treatment benefit of mosunetuzumab is enhanced when it is used earlier in the course of lymphoma therapy or in combination with other agents,” he added.
Genentech says that mosunetuzumab and another bispecific antibody, CD20-TCB, are being evaluated in a robust clinical development program, both as a monotherapies and in combination with other therapies, in both aggressive and indolent non-Hodgkin’s lymphoma.
Dr. Schuster reported relationships with Celgene, Genentech, Merck, Pharmacyclics, Acerta, AbbVie, Gilead, Nordic Nanovector, Pfizer, AstraZeneca, Loxo Oncology, and Novartis. Coauthors also have multiple disclosures, and several are employees of Genentech and Roche. Dr. Sehn consults with several pharmaceutics companies, including Verastem, Roche/Genentech, Morphosys, Takeda, Janssen, Lundbeck, Amgen, Teva, and AbbVie.
A version of this story originally appeared on Medscape.com.
ORLANDO – An investigational drug that can achieve the same results as complex cell therapy is creating a buzz at the American Society of Hematology (ASH) meeting.
For the last few years, attention at this meeting has focused on the chimeric antigen receptor (CAR) T cells, mainly “because of their incredible efficacy,” commented ASH Secretary Robert A. Brodsky, MD, professor of medicine and director of the division of hematology at Johns Hopkins University, Baltimore.
But new results with an off-the-shelf product are “very exciting,” he said, because the drug can be given immediately and appears to achieve similar results.
The new product is mosunetuzumab (Genentech/Roche), a bispecific antibody that targets both CD3 (on the surface of T cells) and CD20 (on the surface of B cells). It works by redirecting T cells to engage and eliminate malignant B cells.
“The concept here is that this monoclonal antibody engages T cells and directs their cytotoxicity against B cells – it’s basically an antibody using the patient’s own T cells to do what a CAR T cell would do,” Dr. Brodsky explained.
However, unlike CAR T cells, which are prepared for each individual patient in a complex process that involves genetic engineering that can take several weeks, mosunetuzumab is an off-the-shelf product that can be given to patients immediately (by intravenous infusion).
This is important, commented Dr. Brodsky, because very-poor-prognosis patients can deteriorate rapidly, and some may not survive while the CAR T cells are being made.
Clinical trial results
Clinical results come from a phase 1/1b trial (known as GO29781) conducted in 270 patients with poor-prognosis refractory/relapsed non-Hodgkin’s lymphoma. These patients had previously been treated with a median of three therapies; in addition, 30 patients (11%) were resistant to or had relapsed after an initial response to CAR T-cell therapy, and 77 patients (29%) had progressed after a stem cell transplant.
“These patients had no available therapy that would be expected to improve survival,” noted lead author Stephen J. Schuster, MD, of Abramson Cancer Center at the University of Pennsylvania in Philadelphia.
All patients received mosunetuzumab with an initial treatment of eight cycles. Patients who achieved complete remission (CR) stopped therapy, while patients who had a partial response or had stable disease, continued treatment for 17 cycles.
Two-thirds of patients (n = 180; 67%) had aggressive lymphomas, mainly diffuse large B-cell lymphoma (DLBCL; n = 117), while 85 patients (31%) had indolent disease, mainly follicular lymphoma (FL; n = 82). Objective responses were seen in 46 of 124 patients (37%) with aggressive lymphomas, and 24 (19%) of these patients achieved a CR.
Among patients with indolent lymphoma, objective responses were seen in 42 of 67 patients (63%), and 29 of 67 (43%) had CR.
The complete remissions appear to be long lasting, Dr. Schuster commented. With a median follow-up of 6 months since achieving CR, 17 of 24 patients (71%) with aggressive lymphoma and 24 of 29 patients (83%) with indolent lymphomas remained free of disease.
“Some patients have remained in remission without additional therapy for more than a year,” he commented.
In the subgroup of 30 patients who had previously received CAR T-cell therapy, the objective response rate was 38.9%, and CR was achieved in 4 patients (22%). These rates are similar to what was seen in patients with aggressive lymphoma who had not previously received CAR T-cell therapy, Dr. Schuster commented.
He also noted that in some of these patients, molecular testing showed that the previously administered CAR T cells increased in number. This suggests that, in addition to its ability to kill cancerous B cells, mosunetuzumab may also help augment the effect of the prior CAR T-cell treatment.
Dr. Schuster also highlighted the results of repeat treatment with mosunetuzumab. Patients who achieved CR stopped treatment – but if they relapsed, they were treated again, and the responses seen on this repeat treatment were similar to those seen with initial treatment. “This is not seen with the CAR T cells,” he noted.
Adverse events with mosunetuzumab were similar to those seen with CAR T cells, he noted, namely cytokine release syndrome, which was mostly mild and seen in 29% of patients, and neurologic toxicity, which was moderately severe in 4% patients.
Overall, the results show that “mosunetuzumab generates long-lasting responses with a very tolerable safety profile in patients with B-cell non-Hodgkin lymphomas for whom multiple prior treatments have failed and whose prognosis is poor. Of particular interest, we are seeing durable complete remissions in patients whose lymphomas progressed after CAR T,” Dr. Schuster commented in a statement.
Approached for comment, Peter Martin MD, chief of the Lymphoma Program at Weill Cornell Medicine, New York, and New York-Presbyterian, said he was excited to see these new data. “It’s good news any time we find something with the potential to save lives.”
“The more options that we have to offer to people with lymphoma the better,” he told Medscape Medical News. “There will always be scenarios where one approach might be better than another. I think there is a good chance that bispecific antibodies will have fairly broad approval in previously treated DLBCL. In many centers, it may be that bispecific antibodies are used most frequently post–CAR T cells, while in other areas people who aren’t candidates for CAR T cells or can’t receive them for whatever reason [could benefit from this new approach].”
Laurie Sehn, MD, MPH, medical oncologist at the University of British Columbia in Vancouver, Canada, and chair of the Lymphoma Tumour Group, as well as an associate editor of ASH journal Blood, also commented for Medscape Medical News.
She agreed that the new data are exciting and noted that this abstract was chosen for the plenary session. She thought the data in the 30 patients who had already been treated with CAR T cells was interesting. “This is a patient population with no other options that offer durable benefit, and mosunetuzumab clearly has clinical activity, with encouraging responses.”
Dr. Sehn also noted that toxicity seen with the drug was “far less” than has been seen with CAR T cells, and the risk of high-grade cytokine release syndrome and neurological toxicity is “very low.”
There are several other new products that are using this bispecific technology, she noted. One example is Regeneron’s REGN1979, a bispecific antibody targeting CD20 and CD3, which is also being investigated in a clinical trial in relapsed/refractory B-cell non-Hodgkin’s lymphoma, including in patients who were previously treated with CAR T cells (abstract 762).
How would it be used clinically?
In response to a question from Medscape Medical News, Dr. Schuster suggested that initial use of mosunetuzumab would be in patients who have already tried CAR T-cell therapy and had either not responded or relapsed – in lymphoma, this is about two-thirds of patients who are treated with this approach. This group of patients represents an unmet medical need, and this indication may be the quickest route to approval, he suggested.
Gary Schiller, MD, from UCLA Health, who moderated the press briefing agreed, and said this would be the quickest route to market because it would need only a phase 2 clinical trial in this specific patient population. But this would likely be only the first use for this product, and then it could be expanded to a broader patient population, he added.
Another use would for mosunetuzumab would be to enhance CAR T-cell responses by redirecting the CAR T cells to other antigens without doing any additional gene editing, Dr. Schuster commented. The idea here is to “revive” previously administered CAR T cells that have stopped working, Dr. Schiller added.
This is a chemotherapy-free approach, Dr. Schuster emphasized. “In patients who have not had a lot of chemotherapy, you can see an increase in T cells,” he commented.
Mosunetuzumab “stimulates and invigorates T cells,” and it could be useful as a pretreatment or a bridge to CAR T-cell therapy, he said.
So the product could be used before CAR T-cell therapy, and equally it could be used after CAR T-cell therapy because it could boost responses in both cases.
“Larger, randomized trials are needed to further confirm these promising data and determine whether the treatment benefit of mosunetuzumab is enhanced when it is used earlier in the course of lymphoma therapy or in combination with other agents,” he added.
Genentech says that mosunetuzumab and another bispecific antibody, CD20-TCB, are being evaluated in a robust clinical development program, both as a monotherapies and in combination with other therapies, in both aggressive and indolent non-Hodgkin’s lymphoma.
Dr. Schuster reported relationships with Celgene, Genentech, Merck, Pharmacyclics, Acerta, AbbVie, Gilead, Nordic Nanovector, Pfizer, AstraZeneca, Loxo Oncology, and Novartis. Coauthors also have multiple disclosures, and several are employees of Genentech and Roche. Dr. Sehn consults with several pharmaceutics companies, including Verastem, Roche/Genentech, Morphosys, Takeda, Janssen, Lundbeck, Amgen, Teva, and AbbVie.
A version of this story originally appeared on Medscape.com.
ORLANDO – An investigational drug that can achieve the same results as complex cell therapy is creating a buzz at the American Society of Hematology (ASH) meeting.
For the last few years, attention at this meeting has focused on the chimeric antigen receptor (CAR) T cells, mainly “because of their incredible efficacy,” commented ASH Secretary Robert A. Brodsky, MD, professor of medicine and director of the division of hematology at Johns Hopkins University, Baltimore.
But new results with an off-the-shelf product are “very exciting,” he said, because the drug can be given immediately and appears to achieve similar results.
The new product is mosunetuzumab (Genentech/Roche), a bispecific antibody that targets both CD3 (on the surface of T cells) and CD20 (on the surface of B cells). It works by redirecting T cells to engage and eliminate malignant B cells.
“The concept here is that this monoclonal antibody engages T cells and directs their cytotoxicity against B cells – it’s basically an antibody using the patient’s own T cells to do what a CAR T cell would do,” Dr. Brodsky explained.
However, unlike CAR T cells, which are prepared for each individual patient in a complex process that involves genetic engineering that can take several weeks, mosunetuzumab is an off-the-shelf product that can be given to patients immediately (by intravenous infusion).
This is important, commented Dr. Brodsky, because very-poor-prognosis patients can deteriorate rapidly, and some may not survive while the CAR T cells are being made.
Clinical trial results
Clinical results come from a phase 1/1b trial (known as GO29781) conducted in 270 patients with poor-prognosis refractory/relapsed non-Hodgkin’s lymphoma. These patients had previously been treated with a median of three therapies; in addition, 30 patients (11%) were resistant to or had relapsed after an initial response to CAR T-cell therapy, and 77 patients (29%) had progressed after a stem cell transplant.
“These patients had no available therapy that would be expected to improve survival,” noted lead author Stephen J. Schuster, MD, of Abramson Cancer Center at the University of Pennsylvania in Philadelphia.
All patients received mosunetuzumab with an initial treatment of eight cycles. Patients who achieved complete remission (CR) stopped therapy, while patients who had a partial response or had stable disease, continued treatment for 17 cycles.
Two-thirds of patients (n = 180; 67%) had aggressive lymphomas, mainly diffuse large B-cell lymphoma (DLBCL; n = 117), while 85 patients (31%) had indolent disease, mainly follicular lymphoma (FL; n = 82). Objective responses were seen in 46 of 124 patients (37%) with aggressive lymphomas, and 24 (19%) of these patients achieved a CR.
Among patients with indolent lymphoma, objective responses were seen in 42 of 67 patients (63%), and 29 of 67 (43%) had CR.
The complete remissions appear to be long lasting, Dr. Schuster commented. With a median follow-up of 6 months since achieving CR, 17 of 24 patients (71%) with aggressive lymphoma and 24 of 29 patients (83%) with indolent lymphomas remained free of disease.
“Some patients have remained in remission without additional therapy for more than a year,” he commented.
In the subgroup of 30 patients who had previously received CAR T-cell therapy, the objective response rate was 38.9%, and CR was achieved in 4 patients (22%). These rates are similar to what was seen in patients with aggressive lymphoma who had not previously received CAR T-cell therapy, Dr. Schuster commented.
He also noted that in some of these patients, molecular testing showed that the previously administered CAR T cells increased in number. This suggests that, in addition to its ability to kill cancerous B cells, mosunetuzumab may also help augment the effect of the prior CAR T-cell treatment.
Dr. Schuster also highlighted the results of repeat treatment with mosunetuzumab. Patients who achieved CR stopped treatment – but if they relapsed, they were treated again, and the responses seen on this repeat treatment were similar to those seen with initial treatment. “This is not seen with the CAR T cells,” he noted.
Adverse events with mosunetuzumab were similar to those seen with CAR T cells, he noted, namely cytokine release syndrome, which was mostly mild and seen in 29% of patients, and neurologic toxicity, which was moderately severe in 4% patients.
Overall, the results show that “mosunetuzumab generates long-lasting responses with a very tolerable safety profile in patients with B-cell non-Hodgkin lymphomas for whom multiple prior treatments have failed and whose prognosis is poor. Of particular interest, we are seeing durable complete remissions in patients whose lymphomas progressed after CAR T,” Dr. Schuster commented in a statement.
Approached for comment, Peter Martin MD, chief of the Lymphoma Program at Weill Cornell Medicine, New York, and New York-Presbyterian, said he was excited to see these new data. “It’s good news any time we find something with the potential to save lives.”
“The more options that we have to offer to people with lymphoma the better,” he told Medscape Medical News. “There will always be scenarios where one approach might be better than another. I think there is a good chance that bispecific antibodies will have fairly broad approval in previously treated DLBCL. In many centers, it may be that bispecific antibodies are used most frequently post–CAR T cells, while in other areas people who aren’t candidates for CAR T cells or can’t receive them for whatever reason [could benefit from this new approach].”
Laurie Sehn, MD, MPH, medical oncologist at the University of British Columbia in Vancouver, Canada, and chair of the Lymphoma Tumour Group, as well as an associate editor of ASH journal Blood, also commented for Medscape Medical News.
She agreed that the new data are exciting and noted that this abstract was chosen for the plenary session. She thought the data in the 30 patients who had already been treated with CAR T cells was interesting. “This is a patient population with no other options that offer durable benefit, and mosunetuzumab clearly has clinical activity, with encouraging responses.”
Dr. Sehn also noted that toxicity seen with the drug was “far less” than has been seen with CAR T cells, and the risk of high-grade cytokine release syndrome and neurological toxicity is “very low.”
There are several other new products that are using this bispecific technology, she noted. One example is Regeneron’s REGN1979, a bispecific antibody targeting CD20 and CD3, which is also being investigated in a clinical trial in relapsed/refractory B-cell non-Hodgkin’s lymphoma, including in patients who were previously treated with CAR T cells (abstract 762).
How would it be used clinically?
In response to a question from Medscape Medical News, Dr. Schuster suggested that initial use of mosunetuzumab would be in patients who have already tried CAR T-cell therapy and had either not responded or relapsed – in lymphoma, this is about two-thirds of patients who are treated with this approach. This group of patients represents an unmet medical need, and this indication may be the quickest route to approval, he suggested.
Gary Schiller, MD, from UCLA Health, who moderated the press briefing agreed, and said this would be the quickest route to market because it would need only a phase 2 clinical trial in this specific patient population. But this would likely be only the first use for this product, and then it could be expanded to a broader patient population, he added.
Another use would for mosunetuzumab would be to enhance CAR T-cell responses by redirecting the CAR T cells to other antigens without doing any additional gene editing, Dr. Schuster commented. The idea here is to “revive” previously administered CAR T cells that have stopped working, Dr. Schiller added.
This is a chemotherapy-free approach, Dr. Schuster emphasized. “In patients who have not had a lot of chemotherapy, you can see an increase in T cells,” he commented.
Mosunetuzumab “stimulates and invigorates T cells,” and it could be useful as a pretreatment or a bridge to CAR T-cell therapy, he said.
So the product could be used before CAR T-cell therapy, and equally it could be used after CAR T-cell therapy because it could boost responses in both cases.
“Larger, randomized trials are needed to further confirm these promising data and determine whether the treatment benefit of mosunetuzumab is enhanced when it is used earlier in the course of lymphoma therapy or in combination with other agents,” he added.
Genentech says that mosunetuzumab and another bispecific antibody, CD20-TCB, are being evaluated in a robust clinical development program, both as a monotherapies and in combination with other therapies, in both aggressive and indolent non-Hodgkin’s lymphoma.
Dr. Schuster reported relationships with Celgene, Genentech, Merck, Pharmacyclics, Acerta, AbbVie, Gilead, Nordic Nanovector, Pfizer, AstraZeneca, Loxo Oncology, and Novartis. Coauthors also have multiple disclosures, and several are employees of Genentech and Roche. Dr. Sehn consults with several pharmaceutics companies, including Verastem, Roche/Genentech, Morphosys, Takeda, Janssen, Lundbeck, Amgen, Teva, and AbbVie.
A version of this story originally appeared on Medscape.com.
Orelabrutinib could be ‘preferred’ BTK inhibitor for MCL
ORLANDO – A novel Bruton tyrosine kinase inhibitor has produced favorable results in patients with relapsed or refractory mantle cell lymphoma, according to findings presented at the annual meeting of the American Society of Hematology.
In a phase 2 trial, orelabrutinib produced an overall response rate of 86% and a 12-month progression-free survival rate of 64%. Safety results with orelabrutinib were superior to historical results with ibrutinib.
The efficacy and safety profile of orelabrutinib, as well as its “convenient” dosing, may make it the “preferred therapeutic choice for B-cell malignancy,” said Lijuan Deng, MD, PhD, of Peking University Cancer Hospital & Institute, Beijing, who presented the phase 2 trial of orelabrutinib at ASH 2019.
The trial enrolled 106 patients with relapsed/refractory mantle cell lymphoma who were treated at 22 centers in China. At baseline, the patients had a median age of 62 years (range, 37-73 years), and 79.2% were men. Most patients (94.4%) had stage III-IV disease.
Prior therapies included CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone)-based (69.8%), EPOCH (etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin)-based (22.6%), DHAP (dexamethasone, cytarabine, and cisplatin)-based (22.6%), CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone)-based (12.3%), and ESHAP (etoposide, methylprednisolone, cytarabine, and cisplatin)-based (4.7%) regimens, and 88.7% of patients had received prior anti-CD20 therapy.
Patients received orelabrutinib at 100 mg twice daily (n = 20) or 150 mg once a day (n = 86). All 106 patients were evaluable for safety, and 99 were evaluable for efficacy.
Efficacy
“Orelabrutinib achieved high response and durable remissions,” Dr. Deng said.
The overall response rate was 85.9% in the evaluable efficacy population and 83.5% in the 150-mg dosing arm. The complete response rates were 27.3% and 29.1%, respectively. The median time to response, overall, was 1.9 months.
The median duration of response and median progression-free survival were not reached at a median follow-up of 10.5 months. At 12 months, 74.3% of patients were still in response, and the progression-free survival rate was 64%.
Safety
Most adverse events were grade 1-2 in nature. The most common grade 3 or higher events were platelet count decrease (11.3%), neutrophil count decrease (8.5%), anemia (7.5%), hypertension (3.8%), pneumonia (2.8%), white blood count decrease (1.9%), and hypokalemia (1.9%).
Adverse events of interest included grade 3 or higher hypertension (3.8%), diarrhea (6.6%), and infection (10.4%), as well as secondary malignancy (0.9%, n = 1). There were no cases of grade 3 or higher hemorrhage, grade 3 or higher atrial fibrillation/flutter, or grade 5 treatment-related adverse events.
Dr. Deng noted that rates of grade 3 or higher hemorrhage, atrial fibrillation, diarrhea, and infection, as well as rates of secondary malignancies, have historically been higher with ibrutinib (Blood. 2015 Aug 6;126[6]:739-45; Lancet. 2016 Feb 20;387[10020]:770-8).
“Orelabrutinib has an improved safety profile in patients with relapsed or refractory mantle cell lymphoma,” Dr. Deng said. “The most common adverse events were cytopenia and infections, which are considered mechanism based.”
The study was sponsored by InnoCare Pharma. Dr. Deng reported having no conflicts of interest.
SOURCE: Deng L et al. ASH 2019, Abstract 755.
ORLANDO – A novel Bruton tyrosine kinase inhibitor has produced favorable results in patients with relapsed or refractory mantle cell lymphoma, according to findings presented at the annual meeting of the American Society of Hematology.
In a phase 2 trial, orelabrutinib produced an overall response rate of 86% and a 12-month progression-free survival rate of 64%. Safety results with orelabrutinib were superior to historical results with ibrutinib.
The efficacy and safety profile of orelabrutinib, as well as its “convenient” dosing, may make it the “preferred therapeutic choice for B-cell malignancy,” said Lijuan Deng, MD, PhD, of Peking University Cancer Hospital & Institute, Beijing, who presented the phase 2 trial of orelabrutinib at ASH 2019.
The trial enrolled 106 patients with relapsed/refractory mantle cell lymphoma who were treated at 22 centers in China. At baseline, the patients had a median age of 62 years (range, 37-73 years), and 79.2% were men. Most patients (94.4%) had stage III-IV disease.
Prior therapies included CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone)-based (69.8%), EPOCH (etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin)-based (22.6%), DHAP (dexamethasone, cytarabine, and cisplatin)-based (22.6%), CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone)-based (12.3%), and ESHAP (etoposide, methylprednisolone, cytarabine, and cisplatin)-based (4.7%) regimens, and 88.7% of patients had received prior anti-CD20 therapy.
Patients received orelabrutinib at 100 mg twice daily (n = 20) or 150 mg once a day (n = 86). All 106 patients were evaluable for safety, and 99 were evaluable for efficacy.
Efficacy
“Orelabrutinib achieved high response and durable remissions,” Dr. Deng said.
The overall response rate was 85.9% in the evaluable efficacy population and 83.5% in the 150-mg dosing arm. The complete response rates were 27.3% and 29.1%, respectively. The median time to response, overall, was 1.9 months.
The median duration of response and median progression-free survival were not reached at a median follow-up of 10.5 months. At 12 months, 74.3% of patients were still in response, and the progression-free survival rate was 64%.
Safety
Most adverse events were grade 1-2 in nature. The most common grade 3 or higher events were platelet count decrease (11.3%), neutrophil count decrease (8.5%), anemia (7.5%), hypertension (3.8%), pneumonia (2.8%), white blood count decrease (1.9%), and hypokalemia (1.9%).
Adverse events of interest included grade 3 or higher hypertension (3.8%), diarrhea (6.6%), and infection (10.4%), as well as secondary malignancy (0.9%, n = 1). There were no cases of grade 3 or higher hemorrhage, grade 3 or higher atrial fibrillation/flutter, or grade 5 treatment-related adverse events.
Dr. Deng noted that rates of grade 3 or higher hemorrhage, atrial fibrillation, diarrhea, and infection, as well as rates of secondary malignancies, have historically been higher with ibrutinib (Blood. 2015 Aug 6;126[6]:739-45; Lancet. 2016 Feb 20;387[10020]:770-8).
“Orelabrutinib has an improved safety profile in patients with relapsed or refractory mantle cell lymphoma,” Dr. Deng said. “The most common adverse events were cytopenia and infections, which are considered mechanism based.”
The study was sponsored by InnoCare Pharma. Dr. Deng reported having no conflicts of interest.
SOURCE: Deng L et al. ASH 2019, Abstract 755.
ORLANDO – A novel Bruton tyrosine kinase inhibitor has produced favorable results in patients with relapsed or refractory mantle cell lymphoma, according to findings presented at the annual meeting of the American Society of Hematology.
In a phase 2 trial, orelabrutinib produced an overall response rate of 86% and a 12-month progression-free survival rate of 64%. Safety results with orelabrutinib were superior to historical results with ibrutinib.
The efficacy and safety profile of orelabrutinib, as well as its “convenient” dosing, may make it the “preferred therapeutic choice for B-cell malignancy,” said Lijuan Deng, MD, PhD, of Peking University Cancer Hospital & Institute, Beijing, who presented the phase 2 trial of orelabrutinib at ASH 2019.
The trial enrolled 106 patients with relapsed/refractory mantle cell lymphoma who were treated at 22 centers in China. At baseline, the patients had a median age of 62 years (range, 37-73 years), and 79.2% were men. Most patients (94.4%) had stage III-IV disease.
Prior therapies included CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone)-based (69.8%), EPOCH (etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin)-based (22.6%), DHAP (dexamethasone, cytarabine, and cisplatin)-based (22.6%), CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone)-based (12.3%), and ESHAP (etoposide, methylprednisolone, cytarabine, and cisplatin)-based (4.7%) regimens, and 88.7% of patients had received prior anti-CD20 therapy.
Patients received orelabrutinib at 100 mg twice daily (n = 20) or 150 mg once a day (n = 86). All 106 patients were evaluable for safety, and 99 were evaluable for efficacy.
Efficacy
“Orelabrutinib achieved high response and durable remissions,” Dr. Deng said.
The overall response rate was 85.9% in the evaluable efficacy population and 83.5% in the 150-mg dosing arm. The complete response rates were 27.3% and 29.1%, respectively. The median time to response, overall, was 1.9 months.
The median duration of response and median progression-free survival were not reached at a median follow-up of 10.5 months. At 12 months, 74.3% of patients were still in response, and the progression-free survival rate was 64%.
Safety
Most adverse events were grade 1-2 in nature. The most common grade 3 or higher events were platelet count decrease (11.3%), neutrophil count decrease (8.5%), anemia (7.5%), hypertension (3.8%), pneumonia (2.8%), white blood count decrease (1.9%), and hypokalemia (1.9%).
Adverse events of interest included grade 3 or higher hypertension (3.8%), diarrhea (6.6%), and infection (10.4%), as well as secondary malignancy (0.9%, n = 1). There were no cases of grade 3 or higher hemorrhage, grade 3 or higher atrial fibrillation/flutter, or grade 5 treatment-related adverse events.
Dr. Deng noted that rates of grade 3 or higher hemorrhage, atrial fibrillation, diarrhea, and infection, as well as rates of secondary malignancies, have historically been higher with ibrutinib (Blood. 2015 Aug 6;126[6]:739-45; Lancet. 2016 Feb 20;387[10020]:770-8).
“Orelabrutinib has an improved safety profile in patients with relapsed or refractory mantle cell lymphoma,” Dr. Deng said. “The most common adverse events were cytopenia and infections, which are considered mechanism based.”
The study was sponsored by InnoCare Pharma. Dr. Deng reported having no conflicts of interest.
SOURCE: Deng L et al. ASH 2019, Abstract 755.
REPORTING FROM ASH 2019