User login
The future of hospital medicine
Assured? Or a definite maybe?
When I started at SHM in 2000, there were fewer than 1,000 hospitalists in the US, and now there are more than 60,000. SHM (back then, we were the National Association of Inpatient Physicians) had about 300 members; now, we have more than 20,000.
Today, hospitalists are part of the medical staff at virtually every hospital in the country, and hospital medicine is recognized as a unique medical specialty with our own knowledge base, textbooks, competencies, meetings, and medical professional society. In a health care environment swirling with change, we are one of the few specialties forged with the ability to adapt and, at times, lead this change. Yet there is so much disruption and instability that there are still many twists and turns in the road that will affect hospitalists’ ability to carve out an even brighter future.
Consolidation has come to health care on a large scale. Hospitals are merging. Health insurers are combining, and even large hospital medicine companies like TeamHealth, Sound, Envision, and others are merging, growing, and acquiring.
At the same time, outside forces from industries not usually associated with health care or inpatient care are swarming into our world: CVS acquires Aetna and aims to reshape primary care; Amazon dominates health care supply chains and moves into pharmacy benefits, and even gets into health care delivery via their partnership with Berkshire Hathaway and JP Morgan; Walmart merges with Humana to create one of the biggest players in Medicare; and Apple expands their inroads into wearables and chronic disease management.
Employment of clinicians has grown logarithmically, especially with inpatient physicians, reshaping the medical staff compensation and accountability. At the same time, payers, both government and private, are evolving into population health with an emphasis not so much on transactions (visits and procedures), but more aligned with outcomes, effectiveness, and efficiency.
All of this leads to a new paradigm of what is important and a new set of values that seems at times more like corporate America where the loyalty of employees can be torn between their employer and the patient. This is especially troublesome in a field traditionally based on the primacy of the doctor-patient relationship. This can put the hospitalist right in the middle at the time when the patient can be most vulnerable.
This has led to new ways to deliver the care that hospitalists provide. First as a pilot and now moving more mainstream, patients with several diagnoses (e.g., heart failure, dehydration, or pneumonia) are now managed not in bricks and mortar hospitals, but in “hospitals at home.” The last few days of a typical hospitalization now take place outside the hospital in a skilled nursing facility (SNF). Fear of uncompensated and unnecessary readmissions leads hospitals to engage hospitalists to handle the first few post-discharge outpatient visits.
This is just a small part of the expanding scope for hospitalists. In addition to managing SNFs and the discharge clinic, hospitalists are now the major providers of perioperative care and play a growing role in palliative care, especially for inpatients. As other specialties that abut hospital medicine have increasing demands and yet fewer new specialists, hospitalists are taking on more critical care and geriatrics, providing procedures, and occupy an evolving role in the emergency room.
There is a lot of work coming towards hospital medicine, and to expand our workforce, hospital medicine groups have incorporated advanced practice providers, including nurse practitioners and physician assistants. But building a true team of health professionals is not seamless or easy with each constituency having a unique scope of practice, limits on their licensure, their own culture, and a distinct training background.
But wait. There will be more new players on the hospital medicine team going forward – some we cannot even anticipate at the present time. In the future, the hospitalist may not even touch the electronic health record (EHR). Clinicians have never excelled at data entry or analysis, and it is time to use a combination of artificial intelligence (AI), voice-activated gathering of history into the record, and staff trained to manage the EHR on both the input and the output sides.
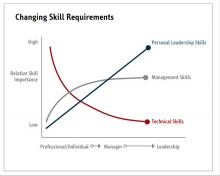
While there may be cheering for this new approach to the EHR – especially because it is a major factor in hospitalist burnout – this will refocus the role and work of the hospitalist to be more of a reviewer and integrator of data, and a strategist and decision-maker overseeing 30 or more patients. As Amazon, CVS, and Walmart move into health care, they will look for the best way to utilize the $300-400/hour hospitalist to the top of our skill level.
In the end, this all comes back to how hospitalists add value, how we can create a career that is rewarding, and how we can help hospitalists be resilient and avoid burnout.
The good news is that hospitalists will not be replaced by AI, nor should we expect to have our incomes cut as less well-trained alternatives replace highly compensated physicians in other specialties. This is a real prospect for many other specialties like dermatology, radiology, pathology, anesthesiology, and even cardiology. But hospitalists will need to adapt to changes in what is valued (i.e., how you can be the most effective and efficient) and to a new job description (i.e., overseeing more patients and managing a team that does more of the H&P, data collecting, and bedside work).
After 20 years of coming out of nowhere to being in the middle of everything in health care, I am confident that hospitalists, with the help of SHM, can continue to forge a path where we can be key difference makers and where we can create a rewarding and sustainable career. It won’t “just happen.” It is not inevitable. But if the past 20 years is any example, we are well-positioned to make the adaptation to succeed in the next 20 years. It is up to all of us to make it happen.
Dr. Wellikson is the CEO of SHM and is retiring from his role in 2020. This article is the second in a series celebrating Dr. Wellikson’s tenure as CEO.
Assured? Or a definite maybe?
Assured? Or a definite maybe?
When I started at SHM in 2000, there were fewer than 1,000 hospitalists in the US, and now there are more than 60,000. SHM (back then, we were the National Association of Inpatient Physicians) had about 300 members; now, we have more than 20,000.
Today, hospitalists are part of the medical staff at virtually every hospital in the country, and hospital medicine is recognized as a unique medical specialty with our own knowledge base, textbooks, competencies, meetings, and medical professional society. In a health care environment swirling with change, we are one of the few specialties forged with the ability to adapt and, at times, lead this change. Yet there is so much disruption and instability that there are still many twists and turns in the road that will affect hospitalists’ ability to carve out an even brighter future.
Consolidation has come to health care on a large scale. Hospitals are merging. Health insurers are combining, and even large hospital medicine companies like TeamHealth, Sound, Envision, and others are merging, growing, and acquiring.
At the same time, outside forces from industries not usually associated with health care or inpatient care are swarming into our world: CVS acquires Aetna and aims to reshape primary care; Amazon dominates health care supply chains and moves into pharmacy benefits, and even gets into health care delivery via their partnership with Berkshire Hathaway and JP Morgan; Walmart merges with Humana to create one of the biggest players in Medicare; and Apple expands their inroads into wearables and chronic disease management.
Employment of clinicians has grown logarithmically, especially with inpatient physicians, reshaping the medical staff compensation and accountability. At the same time, payers, both government and private, are evolving into population health with an emphasis not so much on transactions (visits and procedures), but more aligned with outcomes, effectiveness, and efficiency.
All of this leads to a new paradigm of what is important and a new set of values that seems at times more like corporate America where the loyalty of employees can be torn between their employer and the patient. This is especially troublesome in a field traditionally based on the primacy of the doctor-patient relationship. This can put the hospitalist right in the middle at the time when the patient can be most vulnerable.
This has led to new ways to deliver the care that hospitalists provide. First as a pilot and now moving more mainstream, patients with several diagnoses (e.g., heart failure, dehydration, or pneumonia) are now managed not in bricks and mortar hospitals, but in “hospitals at home.” The last few days of a typical hospitalization now take place outside the hospital in a skilled nursing facility (SNF). Fear of uncompensated and unnecessary readmissions leads hospitals to engage hospitalists to handle the first few post-discharge outpatient visits.
This is just a small part of the expanding scope for hospitalists. In addition to managing SNFs and the discharge clinic, hospitalists are now the major providers of perioperative care and play a growing role in palliative care, especially for inpatients. As other specialties that abut hospital medicine have increasing demands and yet fewer new specialists, hospitalists are taking on more critical care and geriatrics, providing procedures, and occupy an evolving role in the emergency room.
There is a lot of work coming towards hospital medicine, and to expand our workforce, hospital medicine groups have incorporated advanced practice providers, including nurse practitioners and physician assistants. But building a true team of health professionals is not seamless or easy with each constituency having a unique scope of practice, limits on their licensure, their own culture, and a distinct training background.
But wait. There will be more new players on the hospital medicine team going forward – some we cannot even anticipate at the present time. In the future, the hospitalist may not even touch the electronic health record (EHR). Clinicians have never excelled at data entry or analysis, and it is time to use a combination of artificial intelligence (AI), voice-activated gathering of history into the record, and staff trained to manage the EHR on both the input and the output sides.
While there may be cheering for this new approach to the EHR – especially because it is a major factor in hospitalist burnout – this will refocus the role and work of the hospitalist to be more of a reviewer and integrator of data, and a strategist and decision-maker overseeing 30 or more patients. As Amazon, CVS, and Walmart move into health care, they will look for the best way to utilize the $300-400/hour hospitalist to the top of our skill level.
In the end, this all comes back to how hospitalists add value, how we can create a career that is rewarding, and how we can help hospitalists be resilient and avoid burnout.
The good news is that hospitalists will not be replaced by AI, nor should we expect to have our incomes cut as less well-trained alternatives replace highly compensated physicians in other specialties. This is a real prospect for many other specialties like dermatology, radiology, pathology, anesthesiology, and even cardiology. But hospitalists will need to adapt to changes in what is valued (i.e., how you can be the most effective and efficient) and to a new job description (i.e., overseeing more patients and managing a team that does more of the H&P, data collecting, and bedside work).
After 20 years of coming out of nowhere to being in the middle of everything in health care, I am confident that hospitalists, with the help of SHM, can continue to forge a path where we can be key difference makers and where we can create a rewarding and sustainable career. It won’t “just happen.” It is not inevitable. But if the past 20 years is any example, we are well-positioned to make the adaptation to succeed in the next 20 years. It is up to all of us to make it happen.
Dr. Wellikson is the CEO of SHM and is retiring from his role in 2020. This article is the second in a series celebrating Dr. Wellikson’s tenure as CEO.
When I started at SHM in 2000, there were fewer than 1,000 hospitalists in the US, and now there are more than 60,000. SHM (back then, we were the National Association of Inpatient Physicians) had about 300 members; now, we have more than 20,000.
Today, hospitalists are part of the medical staff at virtually every hospital in the country, and hospital medicine is recognized as a unique medical specialty with our own knowledge base, textbooks, competencies, meetings, and medical professional society. In a health care environment swirling with change, we are one of the few specialties forged with the ability to adapt and, at times, lead this change. Yet there is so much disruption and instability that there are still many twists and turns in the road that will affect hospitalists’ ability to carve out an even brighter future.
Consolidation has come to health care on a large scale. Hospitals are merging. Health insurers are combining, and even large hospital medicine companies like TeamHealth, Sound, Envision, and others are merging, growing, and acquiring.
At the same time, outside forces from industries not usually associated with health care or inpatient care are swarming into our world: CVS acquires Aetna and aims to reshape primary care; Amazon dominates health care supply chains and moves into pharmacy benefits, and even gets into health care delivery via their partnership with Berkshire Hathaway and JP Morgan; Walmart merges with Humana to create one of the biggest players in Medicare; and Apple expands their inroads into wearables and chronic disease management.
Employment of clinicians has grown logarithmically, especially with inpatient physicians, reshaping the medical staff compensation and accountability. At the same time, payers, both government and private, are evolving into population health with an emphasis not so much on transactions (visits and procedures), but more aligned with outcomes, effectiveness, and efficiency.
All of this leads to a new paradigm of what is important and a new set of values that seems at times more like corporate America where the loyalty of employees can be torn between their employer and the patient. This is especially troublesome in a field traditionally based on the primacy of the doctor-patient relationship. This can put the hospitalist right in the middle at the time when the patient can be most vulnerable.
This has led to new ways to deliver the care that hospitalists provide. First as a pilot and now moving more mainstream, patients with several diagnoses (e.g., heart failure, dehydration, or pneumonia) are now managed not in bricks and mortar hospitals, but in “hospitals at home.” The last few days of a typical hospitalization now take place outside the hospital in a skilled nursing facility (SNF). Fear of uncompensated and unnecessary readmissions leads hospitals to engage hospitalists to handle the first few post-discharge outpatient visits.
This is just a small part of the expanding scope for hospitalists. In addition to managing SNFs and the discharge clinic, hospitalists are now the major providers of perioperative care and play a growing role in palliative care, especially for inpatients. As other specialties that abut hospital medicine have increasing demands and yet fewer new specialists, hospitalists are taking on more critical care and geriatrics, providing procedures, and occupy an evolving role in the emergency room.
There is a lot of work coming towards hospital medicine, and to expand our workforce, hospital medicine groups have incorporated advanced practice providers, including nurse practitioners and physician assistants. But building a true team of health professionals is not seamless or easy with each constituency having a unique scope of practice, limits on their licensure, their own culture, and a distinct training background.
But wait. There will be more new players on the hospital medicine team going forward – some we cannot even anticipate at the present time. In the future, the hospitalist may not even touch the electronic health record (EHR). Clinicians have never excelled at data entry or analysis, and it is time to use a combination of artificial intelligence (AI), voice-activated gathering of history into the record, and staff trained to manage the EHR on both the input and the output sides.
While there may be cheering for this new approach to the EHR – especially because it is a major factor in hospitalist burnout – this will refocus the role and work of the hospitalist to be more of a reviewer and integrator of data, and a strategist and decision-maker overseeing 30 or more patients. As Amazon, CVS, and Walmart move into health care, they will look for the best way to utilize the $300-400/hour hospitalist to the top of our skill level.
In the end, this all comes back to how hospitalists add value, how we can create a career that is rewarding, and how we can help hospitalists be resilient and avoid burnout.
The good news is that hospitalists will not be replaced by AI, nor should we expect to have our incomes cut as less well-trained alternatives replace highly compensated physicians in other specialties. This is a real prospect for many other specialties like dermatology, radiology, pathology, anesthesiology, and even cardiology. But hospitalists will need to adapt to changes in what is valued (i.e., how you can be the most effective and efficient) and to a new job description (i.e., overseeing more patients and managing a team that does more of the H&P, data collecting, and bedside work).
After 20 years of coming out of nowhere to being in the middle of everything in health care, I am confident that hospitalists, with the help of SHM, can continue to forge a path where we can be key difference makers and where we can create a rewarding and sustainable career. It won’t “just happen.” It is not inevitable. But if the past 20 years is any example, we are well-positioned to make the adaptation to succeed in the next 20 years. It is up to all of us to make it happen.
Dr. Wellikson is the CEO of SHM and is retiring from his role in 2020. This article is the second in a series celebrating Dr. Wellikson’s tenure as CEO.
Meet the new SHM president: Dr. Danielle Scheurer
Danielle Scheurer, MD, MSRC, SFHM, is the chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is the outgoing medical editor of The Hospitalist, and the new president of the Society of Hospital Medicine. She assumes the role from immediate past-president Christopher Frost, MD, SFHM.
As a hospitalist for 17 years, Dr. Scheurer has practiced in both academic tertiary care, as well as community hospital settings. As a chief quality officer, she has worked to improve quality and safety in all health care settings, including ambulatory care, nursing homes, home health, and surgical centers. She brings a broad experience in the medical industry to the SHM presidency.
At what point in your education/training did you decide to practice hospital medicine?
I always loved inpatient medicine throughout my entire meds-peds residency training at Duke University in Durham, N.C. I honestly never had a doubt that hospital medicine was going to be my career. What appeals to me is that each hour and each day is different, which is invigorating.
What are your favorite aspects of clinical practice and of your administrative duties?
I like doing both administrative work and clinical work because I believe having a view of both worlds helps me to be a better physician and a better administrator. It greatly helps me bring realistic solutions to the front lines since I have a good understanding of what needs to be done, but also what is likely to actually work.
As president of SHM over the next year, what are your primary goals?
My primary goal is to deeply connect with the SHM membership and understand what their needs are. There is enormous change happening in the medical industry, and SHM should be a conduit for information sharing, resources, and most importantly, answers to all our difficult problems. Hospitalists are critical to success for our hospitals and our communities during the COVID-19 pandemic. We must be able to give and receive information quickly and seamlessly to effectively help each other across the country and the world. SHM must be seen as a critical convener, especially in times of crisis.
Additionally, SHM has always fostered a “big tent” philosophy, so we will continue to explore ways to expand membership beyond “the core” of internal medicine, family medicine, and pediatrics and reach a better understanding of what our constituents need and how we can add value to their work lives and careers. In addition to expanding membership within our borders, other expansions already include working with international chapters and members with an “all teach, all learn” attitude to better understand mutually beneficial partnerships with international members. Through all these expansions, we will come closer to truly realizing our mission at SHM, which is to “promote exceptional care for hospitalized patients.”
You mention COVID-19. What resources is SHM offering to members?
We have opened up the SHM Learning Portal to help members and non-members address upcoming challenges, such as expanding ICU coverage or cross-training providers for hospital medicine. Several modules in SHM’s “Critical Care for the Hospitalist” series may be especially relevant during the COVID-19 crisis:
- Fluid Resuscitation in the Critically Ill
- Mechanical Ventilation Part I – The Basics
- Mechanical Ventilation Part II – Beyond the Basics
- Mechanical Ventilation Part III – ARDS
Finally, in this time when so many hospitalists are busy dealing with COVID-19, SHM is committed to offering valuable resources and is in the process of offering new material, including Twitter chats, webinars, blogs, and podcasts to help hospitalists share best practices. Please bookmark SHM’s compilation of COVID-19 resources at hospitalmedicine.org/coronavirus.
We also continue to forge ahead with our publications, The Hospitalist and the Journal of Hospital Medicine, by adding online content as it becomes available. Visit the COVID-19 news feed on The Hospitalist website at www.the-hospitalist.org/hospitalist/coronavirus-updates.
In this trying time, we can still connect as a community and continue to learn from each other. We encourage you to use SHM’s online community, HMX, to share resources and crowd-source solutions. Ideas for SHM resources can be submitted via email at [email protected].
What are some of the current challenges for hospital medicine?
The demands placed on hospitalists are greater than ever. With shortening length of stay, rising acuity and complexity, increasing administrative burdens, and high emphasis on care transitions, our skills (and our patience) need to rise to these increasing demands. As a member-based society, SHM (and the board of directors) seeks to ensure we are helping hospitalists be the very best they can be, regardless of hospitalist type or practice setting.
The good news is that we are still in high demand. Within the medical industry, there has been an explosive growth in the need for hospitalists, and we can now be found in almost every hospital setting in the United States. But as a current commodity, it is imperative that we continue to prove the value we are adding to our patients and their families, the systems in which we work, and the industry as a whole.
How will hospital medicine change in the next decade?
I believe one of the biggest changes we will see is the shift to ambulatory settings and the use of telehealth, and we all need to gain significant comfort with both to be effective.
Do you have any advice for students and residents interested in hospital medicine?
It is an incredibly dynamic and invigorating career; I can’t imagine doing anything else.
Danielle Scheurer, MD, MSRC, SFHM, is the chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is the outgoing medical editor of The Hospitalist, and the new president of the Society of Hospital Medicine. She assumes the role from immediate past-president Christopher Frost, MD, SFHM.
As a hospitalist for 17 years, Dr. Scheurer has practiced in both academic tertiary care, as well as community hospital settings. As a chief quality officer, she has worked to improve quality and safety in all health care settings, including ambulatory care, nursing homes, home health, and surgical centers. She brings a broad experience in the medical industry to the SHM presidency.
At what point in your education/training did you decide to practice hospital medicine?
I always loved inpatient medicine throughout my entire meds-peds residency training at Duke University in Durham, N.C. I honestly never had a doubt that hospital medicine was going to be my career. What appeals to me is that each hour and each day is different, which is invigorating.
What are your favorite aspects of clinical practice and of your administrative duties?
I like doing both administrative work and clinical work because I believe having a view of both worlds helps me to be a better physician and a better administrator. It greatly helps me bring realistic solutions to the front lines since I have a good understanding of what needs to be done, but also what is likely to actually work.
As president of SHM over the next year, what are your primary goals?
My primary goal is to deeply connect with the SHM membership and understand what their needs are. There is enormous change happening in the medical industry, and SHM should be a conduit for information sharing, resources, and most importantly, answers to all our difficult problems. Hospitalists are critical to success for our hospitals and our communities during the COVID-19 pandemic. We must be able to give and receive information quickly and seamlessly to effectively help each other across the country and the world. SHM must be seen as a critical convener, especially in times of crisis.
Additionally, SHM has always fostered a “big tent” philosophy, so we will continue to explore ways to expand membership beyond “the core” of internal medicine, family medicine, and pediatrics and reach a better understanding of what our constituents need and how we can add value to their work lives and careers. In addition to expanding membership within our borders, other expansions already include working with international chapters and members with an “all teach, all learn” attitude to better understand mutually beneficial partnerships with international members. Through all these expansions, we will come closer to truly realizing our mission at SHM, which is to “promote exceptional care for hospitalized patients.”
You mention COVID-19. What resources is SHM offering to members?
We have opened up the SHM Learning Portal to help members and non-members address upcoming challenges, such as expanding ICU coverage or cross-training providers for hospital medicine. Several modules in SHM’s “Critical Care for the Hospitalist” series may be especially relevant during the COVID-19 crisis:
- Fluid Resuscitation in the Critically Ill
- Mechanical Ventilation Part I – The Basics
- Mechanical Ventilation Part II – Beyond the Basics
- Mechanical Ventilation Part III – ARDS
Finally, in this time when so many hospitalists are busy dealing with COVID-19, SHM is committed to offering valuable resources and is in the process of offering new material, including Twitter chats, webinars, blogs, and podcasts to help hospitalists share best practices. Please bookmark SHM’s compilation of COVID-19 resources at hospitalmedicine.org/coronavirus.
We also continue to forge ahead with our publications, The Hospitalist and the Journal of Hospital Medicine, by adding online content as it becomes available. Visit the COVID-19 news feed on The Hospitalist website at www.the-hospitalist.org/hospitalist/coronavirus-updates.
In this trying time, we can still connect as a community and continue to learn from each other. We encourage you to use SHM’s online community, HMX, to share resources and crowd-source solutions. Ideas for SHM resources can be submitted via email at [email protected].
What are some of the current challenges for hospital medicine?
The demands placed on hospitalists are greater than ever. With shortening length of stay, rising acuity and complexity, increasing administrative burdens, and high emphasis on care transitions, our skills (and our patience) need to rise to these increasing demands. As a member-based society, SHM (and the board of directors) seeks to ensure we are helping hospitalists be the very best they can be, regardless of hospitalist type or practice setting.
The good news is that we are still in high demand. Within the medical industry, there has been an explosive growth in the need for hospitalists, and we can now be found in almost every hospital setting in the United States. But as a current commodity, it is imperative that we continue to prove the value we are adding to our patients and their families, the systems in which we work, and the industry as a whole.
How will hospital medicine change in the next decade?
I believe one of the biggest changes we will see is the shift to ambulatory settings and the use of telehealth, and we all need to gain significant comfort with both to be effective.
Do you have any advice for students and residents interested in hospital medicine?
It is an incredibly dynamic and invigorating career; I can’t imagine doing anything else.
Danielle Scheurer, MD, MSRC, SFHM, is the chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is the outgoing medical editor of The Hospitalist, and the new president of the Society of Hospital Medicine. She assumes the role from immediate past-president Christopher Frost, MD, SFHM.
As a hospitalist for 17 years, Dr. Scheurer has practiced in both academic tertiary care, as well as community hospital settings. As a chief quality officer, she has worked to improve quality and safety in all health care settings, including ambulatory care, nursing homes, home health, and surgical centers. She brings a broad experience in the medical industry to the SHM presidency.
At what point in your education/training did you decide to practice hospital medicine?
I always loved inpatient medicine throughout my entire meds-peds residency training at Duke University in Durham, N.C. I honestly never had a doubt that hospital medicine was going to be my career. What appeals to me is that each hour and each day is different, which is invigorating.
What are your favorite aspects of clinical practice and of your administrative duties?
I like doing both administrative work and clinical work because I believe having a view of both worlds helps me to be a better physician and a better administrator. It greatly helps me bring realistic solutions to the front lines since I have a good understanding of what needs to be done, but also what is likely to actually work.
As president of SHM over the next year, what are your primary goals?
My primary goal is to deeply connect with the SHM membership and understand what their needs are. There is enormous change happening in the medical industry, and SHM should be a conduit for information sharing, resources, and most importantly, answers to all our difficult problems. Hospitalists are critical to success for our hospitals and our communities during the COVID-19 pandemic. We must be able to give and receive information quickly and seamlessly to effectively help each other across the country and the world. SHM must be seen as a critical convener, especially in times of crisis.
Additionally, SHM has always fostered a “big tent” philosophy, so we will continue to explore ways to expand membership beyond “the core” of internal medicine, family medicine, and pediatrics and reach a better understanding of what our constituents need and how we can add value to their work lives and careers. In addition to expanding membership within our borders, other expansions already include working with international chapters and members with an “all teach, all learn” attitude to better understand mutually beneficial partnerships with international members. Through all these expansions, we will come closer to truly realizing our mission at SHM, which is to “promote exceptional care for hospitalized patients.”
You mention COVID-19. What resources is SHM offering to members?
We have opened up the SHM Learning Portal to help members and non-members address upcoming challenges, such as expanding ICU coverage or cross-training providers for hospital medicine. Several modules in SHM’s “Critical Care for the Hospitalist” series may be especially relevant during the COVID-19 crisis:
- Fluid Resuscitation in the Critically Ill
- Mechanical Ventilation Part I – The Basics
- Mechanical Ventilation Part II – Beyond the Basics
- Mechanical Ventilation Part III – ARDS
Finally, in this time when so many hospitalists are busy dealing with COVID-19, SHM is committed to offering valuable resources and is in the process of offering new material, including Twitter chats, webinars, blogs, and podcasts to help hospitalists share best practices. Please bookmark SHM’s compilation of COVID-19 resources at hospitalmedicine.org/coronavirus.
We also continue to forge ahead with our publications, The Hospitalist and the Journal of Hospital Medicine, by adding online content as it becomes available. Visit the COVID-19 news feed on The Hospitalist website at www.the-hospitalist.org/hospitalist/coronavirus-updates.
In this trying time, we can still connect as a community and continue to learn from each other. We encourage you to use SHM’s online community, HMX, to share resources and crowd-source solutions. Ideas for SHM resources can be submitted via email at [email protected].
What are some of the current challenges for hospital medicine?
The demands placed on hospitalists are greater than ever. With shortening length of stay, rising acuity and complexity, increasing administrative burdens, and high emphasis on care transitions, our skills (and our patience) need to rise to these increasing demands. As a member-based society, SHM (and the board of directors) seeks to ensure we are helping hospitalists be the very best they can be, regardless of hospitalist type or practice setting.
The good news is that we are still in high demand. Within the medical industry, there has been an explosive growth in the need for hospitalists, and we can now be found in almost every hospital setting in the United States. But as a current commodity, it is imperative that we continue to prove the value we are adding to our patients and their families, the systems in which we work, and the industry as a whole.
How will hospital medicine change in the next decade?
I believe one of the biggest changes we will see is the shift to ambulatory settings and the use of telehealth, and we all need to gain significant comfort with both to be effective.
Do you have any advice for students and residents interested in hospital medicine?
It is an incredibly dynamic and invigorating career; I can’t imagine doing anything else.
Two decades of leadership
In recognition of Dr. Larry Wellikson’s contributions to SHM
It’s already been a few years since I exited the Society of Hospital Medicine’s Board of Directors (2 years, or maybe 3 – I’ve already lost count), and sitting in my proverbial rocking chair in the Old Hospitalists’ Home, I heard, as many of you did, that Larry Wellikson, MD, MHM, the first and only CEO in the Society’s history, is stepping down soon.
With all the idle time that I find myself with these days, I have had the opportunity to ruminate on what Larry has brought to SHM in his 2 decades of leadership. And among the many answers, two stand out for me.
The first is Larry’s deep appreciation of the value of relationships that he has developed and nurtured, an attribute which he has imprinted on many of us who have worked with him over the years. Although Larry speaks of the camaraderie of the first years of SHM and the bonds that he, Bob Wachter, Win Whitcomb, and John Nelson established, he also has kept in touch with a vast network of hospitalists over the last 20-plus years.
Go to lunch with Larry, and be amazed at how much he knows about the goings-on of many of our colleagues. The fondness that Larry has for the people in his life is without parallel. These aren’t just professional colleagues who have impacted him in some way – for Larry, every one of these is a true lifetime friendship, and he continues to establish new ones every year. He makes each of his friends feel truly special to him.
The second is the critical value of and need for change and disruption. The specialty of hospital medicine was, from its beginning, disruptive, and from his career as a physician executive, Larry understood and has brought to SHM an understanding of the necessity of disruption to encourage growth and fresh thinking. If one steps back and looks at, for example, the composition of the Board over the years, or the Journal of Hospital Medicine’s editorial staff, or of our committees, one sees a pattern – a commitment to continuously bringing on young leaders who are still on the early and ascending part of their career paths.
Other organizations identify Board candidates at the peak of their careers, but at SHM, many of us were elected when we had just enough experience to contribute but then continued to grow in our careers after finishing our terms. I joined the Board in 2012 (I think) and while I would probably be a more seasoned and stately Board member if I joined at this point in my life, I would also have less new and novel to offer – and therefore be less effective for what the Society needs. While SHM respects its past leaders, it does not revere them. Our past is important, but our present and future are more important. Larry brought that mentality to SHM.
Ironically, the one position within SHM which has not, until this year, been subject to that same kind of transition is the CEO position itself. And this year, that domino will fall as well. While transitions are hard, change is good – and I am confident that our Society’s commitment to seeking out new, talented leaders, and making transitions at all levels – Board, committees, chapters, speakers – with the intent of bringing new perspectives and creativity, is firmly entrenched in our culture. And Larry can join me in the rocking chair as we relive our common SHM experiences together – and create new memories as well.
Congratulations Larry, and thank you.
Dr. Harte is a past president of SHM, and president of Cleveland Clinic Akron (Ohio) General and the Southern Region. He formerly served as president of Cleveland Clinic Hillcrest Hospital and Cleveland Clinic South Pointe Hospital.
In recognition of Dr. Larry Wellikson’s contributions to SHM
In recognition of Dr. Larry Wellikson’s contributions to SHM
It’s already been a few years since I exited the Society of Hospital Medicine’s Board of Directors (2 years, or maybe 3 – I’ve already lost count), and sitting in my proverbial rocking chair in the Old Hospitalists’ Home, I heard, as many of you did, that Larry Wellikson, MD, MHM, the first and only CEO in the Society’s history, is stepping down soon.
With all the idle time that I find myself with these days, I have had the opportunity to ruminate on what Larry has brought to SHM in his 2 decades of leadership. And among the many answers, two stand out for me.
The first is Larry’s deep appreciation of the value of relationships that he has developed and nurtured, an attribute which he has imprinted on many of us who have worked with him over the years. Although Larry speaks of the camaraderie of the first years of SHM and the bonds that he, Bob Wachter, Win Whitcomb, and John Nelson established, he also has kept in touch with a vast network of hospitalists over the last 20-plus years.
Go to lunch with Larry, and be amazed at how much he knows about the goings-on of many of our colleagues. The fondness that Larry has for the people in his life is without parallel. These aren’t just professional colleagues who have impacted him in some way – for Larry, every one of these is a true lifetime friendship, and he continues to establish new ones every year. He makes each of his friends feel truly special to him.
The second is the critical value of and need for change and disruption. The specialty of hospital medicine was, from its beginning, disruptive, and from his career as a physician executive, Larry understood and has brought to SHM an understanding of the necessity of disruption to encourage growth and fresh thinking. If one steps back and looks at, for example, the composition of the Board over the years, or the Journal of Hospital Medicine’s editorial staff, or of our committees, one sees a pattern – a commitment to continuously bringing on young leaders who are still on the early and ascending part of their career paths.
Other organizations identify Board candidates at the peak of their careers, but at SHM, many of us were elected when we had just enough experience to contribute but then continued to grow in our careers after finishing our terms. I joined the Board in 2012 (I think) and while I would probably be a more seasoned and stately Board member if I joined at this point in my life, I would also have less new and novel to offer – and therefore be less effective for what the Society needs. While SHM respects its past leaders, it does not revere them. Our past is important, but our present and future are more important. Larry brought that mentality to SHM.
Ironically, the one position within SHM which has not, until this year, been subject to that same kind of transition is the CEO position itself. And this year, that domino will fall as well. While transitions are hard, change is good – and I am confident that our Society’s commitment to seeking out new, talented leaders, and making transitions at all levels – Board, committees, chapters, speakers – with the intent of bringing new perspectives and creativity, is firmly entrenched in our culture. And Larry can join me in the rocking chair as we relive our common SHM experiences together – and create new memories as well.
Congratulations Larry, and thank you.
Dr. Harte is a past president of SHM, and president of Cleveland Clinic Akron (Ohio) General and the Southern Region. He formerly served as president of Cleveland Clinic Hillcrest Hospital and Cleveland Clinic South Pointe Hospital.
It’s already been a few years since I exited the Society of Hospital Medicine’s Board of Directors (2 years, or maybe 3 – I’ve already lost count), and sitting in my proverbial rocking chair in the Old Hospitalists’ Home, I heard, as many of you did, that Larry Wellikson, MD, MHM, the first and only CEO in the Society’s history, is stepping down soon.
With all the idle time that I find myself with these days, I have had the opportunity to ruminate on what Larry has brought to SHM in his 2 decades of leadership. And among the many answers, two stand out for me.
The first is Larry’s deep appreciation of the value of relationships that he has developed and nurtured, an attribute which he has imprinted on many of us who have worked with him over the years. Although Larry speaks of the camaraderie of the first years of SHM and the bonds that he, Bob Wachter, Win Whitcomb, and John Nelson established, he also has kept in touch with a vast network of hospitalists over the last 20-plus years.
Go to lunch with Larry, and be amazed at how much he knows about the goings-on of many of our colleagues. The fondness that Larry has for the people in his life is without parallel. These aren’t just professional colleagues who have impacted him in some way – for Larry, every one of these is a true lifetime friendship, and he continues to establish new ones every year. He makes each of his friends feel truly special to him.
The second is the critical value of and need for change and disruption. The specialty of hospital medicine was, from its beginning, disruptive, and from his career as a physician executive, Larry understood and has brought to SHM an understanding of the necessity of disruption to encourage growth and fresh thinking. If one steps back and looks at, for example, the composition of the Board over the years, or the Journal of Hospital Medicine’s editorial staff, or of our committees, one sees a pattern – a commitment to continuously bringing on young leaders who are still on the early and ascending part of their career paths.
Other organizations identify Board candidates at the peak of their careers, but at SHM, many of us were elected when we had just enough experience to contribute but then continued to grow in our careers after finishing our terms. I joined the Board in 2012 (I think) and while I would probably be a more seasoned and stately Board member if I joined at this point in my life, I would also have less new and novel to offer – and therefore be less effective for what the Society needs. While SHM respects its past leaders, it does not revere them. Our past is important, but our present and future are more important. Larry brought that mentality to SHM.
Ironically, the one position within SHM which has not, until this year, been subject to that same kind of transition is the CEO position itself. And this year, that domino will fall as well. While transitions are hard, change is good – and I am confident that our Society’s commitment to seeking out new, talented leaders, and making transitions at all levels – Board, committees, chapters, speakers – with the intent of bringing new perspectives and creativity, is firmly entrenched in our culture. And Larry can join me in the rocking chair as we relive our common SHM experiences together – and create new memories as well.
Congratulations Larry, and thank you.
Dr. Harte is a past president of SHM, and president of Cleveland Clinic Akron (Ohio) General and the Southern Region. He formerly served as president of Cleveland Clinic Hillcrest Hospital and Cleveland Clinic South Pointe Hospital.
Step 1 scoring moves to pass/fail: Hospitalists’ role and unintended consequences
The National Board of Medical Examiners recently announced a change in the United States Medical Licensing Examination (USMLE) Step 1 score reporting from a 3-digit score to a pass/fail score beginning in 2022.1 Endorsed by a broad coalition of organizations involved in undergraduate (UME) and graduate medical education (GME), this change is intended as a first step toward systemic improvements in the UME-GME transition to residency by promoting holistic reviews of applicants. Additionally, it is meant to tackle widespread concerns about medical student distress brought about by the residency selection process. For example, switching to pass/fail preclinical curricula has resulted in an improvement in medical student well-being at many medical schools.2 It is the hope that a mirrored change in Step 1 may similarly improve mental health and encourage a growth mindset towards learning.
On the other hand, many residency programs rely on USMLE scores for screening potential candidates, especially as application inflation has burdened programs with thousands of applications.3 The change to a pass/fail Step 1 score will likely shift emphasis and stress to the Step 2 CK Exam, essentially negating the intended effect. Furthermore, for schools still reporting NBME Subject (shelf) Exam scores and Clerkship grades, there will likely be a greater emphasis placed on these metrics as well. The need for objective assessment methods are seen by many as so critical that some GME leaders have advocated for instituting entrance exams or requiring a Standardized Letter of Evaluation as a prerequisite to residency application. Finally, medical students jockeying for competitive residency positions may also feel pressured to distinguish themselves by boosting other aspects of their portfolio by taking a research year or applying for away electives, which risks marginalizing students of lesser means or with family responsibilities.
Ultimately, the change to a pass/fail Step 1 exam will likely do little to address the expanding gulf between the UME and GME communities. Residency program directors are searching for students with qualities of a good physician, such as interpersonal skills, “teamsmanship,” compassion, and professionalism, but reliable, objective, and standardized assessment tools are not available. Currently our best tools are clinical evaluations which are subject to grade inflation and implicit racial and gender biases. Furthermore, other components of a residency application, such as letters of recommendation, Chair’s letters, and the Medical Student Performance Evaluation (Dean’s letter), are regarded to be less informative as schools move toward no student rankings, pass/fail grading schemes, and nonstandardized summative adjectives to describe medical students overall medical school performance.
Finally, medical student distress in the residency application process may stem from the perpetuation of elitism that extends from medical school to fellowship training and academic hospital medicine. Rankings of medical schools, residencies, fellowships, and hospitals serve to create a hierarchical system. Competitive residency applicants see admittance into the best training programs as opening doors to opportunities, while not getting into these programs is seen as closing doors to career paths and opportunities.
With this change in Step 1 score reporting, where do we as hospitalists fit in? Hospitalists are at the forefront of educating and evaluating medical students in academic medical centers, and we are often asked to write letters of recommendation and serve as mentors. If done well, these activities can have a positive impact on medical student applications to residency by alleviating some of the stresses and mitigating the downsides to the new Step 1 scoring system. Writing impactful letters and thoughtful evaluations are all skills that should be incorporated in hospitalist faculty development programs. Moreover, in order to serve as better advocates for our students, it is important that academic hospitalists understand the evolving landscape of the residency application process and are mindful of the stresses that medical students face. Changing Step 1 scoring to pass/fail will likely have unintended consequences for our medical students, and we as hospitalists must be ready to improve our knowledge and skills in order to continue to support and advocate for our medical students.
Dr. Esquivel is a hospitalist and assistant professor at Weill Cornell Medical College in New York; Dr. Chang is associate professor and interprofessional education thread director (MD curriculum) at Washington University, St. Louis; Dr. Ricotta is a hospitalist at Beth Israel Deaconess Medical Center, Boston, and instructor in medicine at Harvard Medical School; Dr. Rendon is a hospitalist at the University of New Mexico in Albuquerque; Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System and associate professor at the University of California, San Diego. He is the chair of SHM’s Physicians in Training committee.
References
1. United States Medical Licensing Examination (2020 Feb). Change to pass/fail score reporting for Step 1.
2. Slavin SJ and Chibnall JT. Finding the why, changing the how: Improving the mental health of medical students, residents, and physicians. Academic Medicine. 2016;91(9):1194‐6.
3. Pereira AG, Chelminski PR, et al. Application inflation for internal medicine applicants in the Match: Drivers, consequences, and potential solutions. Am J Med. 2016 Aug;129(8): 885-91.
The National Board of Medical Examiners recently announced a change in the United States Medical Licensing Examination (USMLE) Step 1 score reporting from a 3-digit score to a pass/fail score beginning in 2022.1 Endorsed by a broad coalition of organizations involved in undergraduate (UME) and graduate medical education (GME), this change is intended as a first step toward systemic improvements in the UME-GME transition to residency by promoting holistic reviews of applicants. Additionally, it is meant to tackle widespread concerns about medical student distress brought about by the residency selection process. For example, switching to pass/fail preclinical curricula has resulted in an improvement in medical student well-being at many medical schools.2 It is the hope that a mirrored change in Step 1 may similarly improve mental health and encourage a growth mindset towards learning.
On the other hand, many residency programs rely on USMLE scores for screening potential candidates, especially as application inflation has burdened programs with thousands of applications.3 The change to a pass/fail Step 1 score will likely shift emphasis and stress to the Step 2 CK Exam, essentially negating the intended effect. Furthermore, for schools still reporting NBME Subject (shelf) Exam scores and Clerkship grades, there will likely be a greater emphasis placed on these metrics as well. The need for objective assessment methods are seen by many as so critical that some GME leaders have advocated for instituting entrance exams or requiring a Standardized Letter of Evaluation as a prerequisite to residency application. Finally, medical students jockeying for competitive residency positions may also feel pressured to distinguish themselves by boosting other aspects of their portfolio by taking a research year or applying for away electives, which risks marginalizing students of lesser means or with family responsibilities.
Ultimately, the change to a pass/fail Step 1 exam will likely do little to address the expanding gulf between the UME and GME communities. Residency program directors are searching for students with qualities of a good physician, such as interpersonal skills, “teamsmanship,” compassion, and professionalism, but reliable, objective, and standardized assessment tools are not available. Currently our best tools are clinical evaluations which are subject to grade inflation and implicit racial and gender biases. Furthermore, other components of a residency application, such as letters of recommendation, Chair’s letters, and the Medical Student Performance Evaluation (Dean’s letter), are regarded to be less informative as schools move toward no student rankings, pass/fail grading schemes, and nonstandardized summative adjectives to describe medical students overall medical school performance.
Finally, medical student distress in the residency application process may stem from the perpetuation of elitism that extends from medical school to fellowship training and academic hospital medicine. Rankings of medical schools, residencies, fellowships, and hospitals serve to create a hierarchical system. Competitive residency applicants see admittance into the best training programs as opening doors to opportunities, while not getting into these programs is seen as closing doors to career paths and opportunities.
With this change in Step 1 score reporting, where do we as hospitalists fit in? Hospitalists are at the forefront of educating and evaluating medical students in academic medical centers, and we are often asked to write letters of recommendation and serve as mentors. If done well, these activities can have a positive impact on medical student applications to residency by alleviating some of the stresses and mitigating the downsides to the new Step 1 scoring system. Writing impactful letters and thoughtful evaluations are all skills that should be incorporated in hospitalist faculty development programs. Moreover, in order to serve as better advocates for our students, it is important that academic hospitalists understand the evolving landscape of the residency application process and are mindful of the stresses that medical students face. Changing Step 1 scoring to pass/fail will likely have unintended consequences for our medical students, and we as hospitalists must be ready to improve our knowledge and skills in order to continue to support and advocate for our medical students.
Dr. Esquivel is a hospitalist and assistant professor at Weill Cornell Medical College in New York; Dr. Chang is associate professor and interprofessional education thread director (MD curriculum) at Washington University, St. Louis; Dr. Ricotta is a hospitalist at Beth Israel Deaconess Medical Center, Boston, and instructor in medicine at Harvard Medical School; Dr. Rendon is a hospitalist at the University of New Mexico in Albuquerque; Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System and associate professor at the University of California, San Diego. He is the chair of SHM’s Physicians in Training committee.
References
1. United States Medical Licensing Examination (2020 Feb). Change to pass/fail score reporting for Step 1.
2. Slavin SJ and Chibnall JT. Finding the why, changing the how: Improving the mental health of medical students, residents, and physicians. Academic Medicine. 2016;91(9):1194‐6.
3. Pereira AG, Chelminski PR, et al. Application inflation for internal medicine applicants in the Match: Drivers, consequences, and potential solutions. Am J Med. 2016 Aug;129(8): 885-91.
The National Board of Medical Examiners recently announced a change in the United States Medical Licensing Examination (USMLE) Step 1 score reporting from a 3-digit score to a pass/fail score beginning in 2022.1 Endorsed by a broad coalition of organizations involved in undergraduate (UME) and graduate medical education (GME), this change is intended as a first step toward systemic improvements in the UME-GME transition to residency by promoting holistic reviews of applicants. Additionally, it is meant to tackle widespread concerns about medical student distress brought about by the residency selection process. For example, switching to pass/fail preclinical curricula has resulted in an improvement in medical student well-being at many medical schools.2 It is the hope that a mirrored change in Step 1 may similarly improve mental health and encourage a growth mindset towards learning.
On the other hand, many residency programs rely on USMLE scores for screening potential candidates, especially as application inflation has burdened programs with thousands of applications.3 The change to a pass/fail Step 1 score will likely shift emphasis and stress to the Step 2 CK Exam, essentially negating the intended effect. Furthermore, for schools still reporting NBME Subject (shelf) Exam scores and Clerkship grades, there will likely be a greater emphasis placed on these metrics as well. The need for objective assessment methods are seen by many as so critical that some GME leaders have advocated for instituting entrance exams or requiring a Standardized Letter of Evaluation as a prerequisite to residency application. Finally, medical students jockeying for competitive residency positions may also feel pressured to distinguish themselves by boosting other aspects of their portfolio by taking a research year or applying for away electives, which risks marginalizing students of lesser means or with family responsibilities.
Ultimately, the change to a pass/fail Step 1 exam will likely do little to address the expanding gulf between the UME and GME communities. Residency program directors are searching for students with qualities of a good physician, such as interpersonal skills, “teamsmanship,” compassion, and professionalism, but reliable, objective, and standardized assessment tools are not available. Currently our best tools are clinical evaluations which are subject to grade inflation and implicit racial and gender biases. Furthermore, other components of a residency application, such as letters of recommendation, Chair’s letters, and the Medical Student Performance Evaluation (Dean’s letter), are regarded to be less informative as schools move toward no student rankings, pass/fail grading schemes, and nonstandardized summative adjectives to describe medical students overall medical school performance.
Finally, medical student distress in the residency application process may stem from the perpetuation of elitism that extends from medical school to fellowship training and academic hospital medicine. Rankings of medical schools, residencies, fellowships, and hospitals serve to create a hierarchical system. Competitive residency applicants see admittance into the best training programs as opening doors to opportunities, while not getting into these programs is seen as closing doors to career paths and opportunities.
With this change in Step 1 score reporting, where do we as hospitalists fit in? Hospitalists are at the forefront of educating and evaluating medical students in academic medical centers, and we are often asked to write letters of recommendation and serve as mentors. If done well, these activities can have a positive impact on medical student applications to residency by alleviating some of the stresses and mitigating the downsides to the new Step 1 scoring system. Writing impactful letters and thoughtful evaluations are all skills that should be incorporated in hospitalist faculty development programs. Moreover, in order to serve as better advocates for our students, it is important that academic hospitalists understand the evolving landscape of the residency application process and are mindful of the stresses that medical students face. Changing Step 1 scoring to pass/fail will likely have unintended consequences for our medical students, and we as hospitalists must be ready to improve our knowledge and skills in order to continue to support and advocate for our medical students.
Dr. Esquivel is a hospitalist and assistant professor at Weill Cornell Medical College in New York; Dr. Chang is associate professor and interprofessional education thread director (MD curriculum) at Washington University, St. Louis; Dr. Ricotta is a hospitalist at Beth Israel Deaconess Medical Center, Boston, and instructor in medicine at Harvard Medical School; Dr. Rendon is a hospitalist at the University of New Mexico in Albuquerque; Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System and associate professor at the University of California, San Diego. He is the chair of SHM’s Physicians in Training committee.
References
1. United States Medical Licensing Examination (2020 Feb). Change to pass/fail score reporting for Step 1.
2. Slavin SJ and Chibnall JT. Finding the why, changing the how: Improving the mental health of medical students, residents, and physicians. Academic Medicine. 2016;91(9):1194‐6.
3. Pereira AG, Chelminski PR, et al. Application inflation for internal medicine applicants in the Match: Drivers, consequences, and potential solutions. Am J Med. 2016 Aug;129(8): 885-91.
Designing an effective onboarding program
It goes beyond welcoming and orientation
As I gear up to welcome and onboard new hires to our hospitalist group, I could not help but reflect on my first day as a hospitalist. Fresh out of residency, my orientation was a day and a half long.
The medical director gave me a brief overview of the program. The program administrator handed me a thick folder of policies followed by a quick tour of the hospital and an afternoon training for the computerized order entry system (that was a time before EHRs). The next morning, I was given my full panel of patients, my new lab coat, and sent off into the battlefield.
I can vividly remember feeling anxious, a bit confused, and quite overwhelmed as I went through my day. The days turned into a week and the next. I kept wondering if I was doing everything right. It took me a month to feel a little more comfortable. It all turned out fine. Since nobody told me otherwise, I assumed it did.
Quite a bit has changed since then in hospital medicine. Hospital medicine groups, nowadays, have to tackle the changing landscape of payment reform, take on responsibility for an increasing range of hospital quality metrics and juggle a swath of subspecialty comanagement agreements. Hospital medicine providers function from the inpatient to the post-acute care arena, all while continuing to demonstrate their value to the hospital administration. Simultaneously, they have to ensure their providers are engaged and functioning at their optimal level while battling the ever-increasing threat of burnout.
Thus, for new hires, all the above aspects of my orientation have become critical but alas terribly insufficient. Well into its third decade, the hospital medicine job market continues to boom but remains a revolving door. Hospital medicine groups continue to grow in size and integrate across hospitals in a given health system. The vast majority of the new hires tend to be fresh out of residency. The first year remains the most vulnerable period for a new hospitalist. Hospital medicine groups must design and implement a robust onboarding program for their new hires. It goes beyond welcoming and orientation of new hires to full integration and assimilation in order to transform them into highly efficient and productive team members. Effective onboarding is table stakes for a successful and thriving hospital medicine group.
The content
An effective onboarding program should focus on three key dimensions: the organizational, the technical, and the social.1
1. The organizational or administrative aspect: The most common aspect of onboarding is providing new hires with information on the group’s policies and procedures: what to do and how to do it. Equally essential is giving them the tools and contacts that will help them understand and navigate their first few months. Information on how to contact consultants, signing on and off shifts, and so on can be easily conveyed through documents. However, having peers and the critical administrative staff communicate other aspects such as a detailed tour of the hospital, scheduling, and vacation policies is far more effective. It provides an excellent opportunity to introduce new hires to the key personnel in the group and vice versa as new hires get familiar with the unofficial workplace language. Breaking down all this information into meaningful, absorbable boluses, spread over time, is key to avoiding information overload. Allowing new hires to assimilate and adapt to the group norms requires follow-up and reinforcement. Group leaders should plan to meet with them at predetermined intervals, such as at 30, 60, 90 days, to engage them in conversations about the group’s values, performance measurements, rewards, and the opportunities for growth that exist within the group and institution.
2. The technical or the clinical aspect: The majority of physicians and advanced providers hired to a hospital medicine group have come immediately from training. Transition into the autonomous role of an attending, or a semi-autonomous role for advanced providers, with a larger patient panel can be quite unnerving and stressful. It can be disorientating even for experienced providers transitioning into a new health system. A well-structured onboarding can allow providers to deploy their training and experience at your organization effectively. Many onboarding programs have a clinical ramp-up period. The providers begin with a limited patient panel and gradually acclimatize into a full patient load. Many programs pair a senior hospitalist with the new hire during this period – a ‘buddy.’ Buddies are available to help new hires navigate the health system and familiarize them with the stakeholders. They help new hires by providing context to understand their new role and how they can contribute to the group’s success. In many instances, buddies help outline the unspoken rules of the group.
3. The social aspect – enculturation and networking: This is probably the most important of the three elements. It is quite common for new hires to feel like a stranger in a new land. A well-designed onboarding program provides new hires the space to forge relationships with each other and existing members of the hospital medicine team. Groups can do this in myriad ways – an informal welcome social, a meet and greet breakfast or lunch, in-person orientation when designing the administrative onboarding, and assignment of buddies or mentors during their clinical ramp-up period. It is all about providing a space to establish and nurture lasting relationships between the new hires and the group. When done well, this helps transform a group into a community. It also lays the groundwork to avoid stress and loneliness, some of the culprits that lead to physician burnout. It is through these interpersonal connections that new hires adapt to a hospital medicine group’s prevailing culture.
The personnel
Effective onboarding should be more than mere orientation. Group leaders should make an active attempt at understanding the core values and needs of the group. A good onboarding process assists new hires to internalize and accept the norms of the group. This process is not just a result of what comes from top management but also what they see and hear from the rank and file providers in the group. Hence it is critical to have the right people who understand and embody these values at the planning table. It is equally essential that necessary time and resources are devoted to building a program that meets the needs of the group. The practice management committee at SHM interviewed five different programs across a spectrum of settings. All of them had a designated onboarding program leader with a planning committee that included the administrative staff and senior frontline hospitalists.
The costs
According to one estimate, the cost of physician turnover is $400,000-$600,000 per provider.2 Given such staggering costs, it is not difficult to justify the financial resources required to structure an effective onboarding program. Activities such as a detailed facility tour, a welcome breakfast, and a peer buddy system cost virtually nothing. They go a long way in building comradery, make new hires feel like they are part of a team, and reduce burnout and turnover. Costs of an onboarding program are typically related to wages during shadowing and clinical ramp-up. However, all the programs we interviewed acknowledged that the costs associated with onboarding, in the broader context, were small and necessary.
The bottom line
An effective onboarding program that is well planned, well structured, and well executed is inherently valuable. It sends a positive signal to new hires, reassuring them that they made a great decision by joining the group. It also reminds the existing providers why they want to be a part of the group and its culture.
It is not about what is said or done during the onboarding process or how long it lasts. It need not be overly complicated. It is how the process makes everyone feel about the group. At the end of the day, like in all aspects of life, that is what ultimately matters.
The SHM Practice Management Committee has created a document that outlines the guiding principles for effective onboarding with attached case studies. Visit the SHM website for more information: https://www.hospitalmedicine.org.
Dr. Irani is a hospitalist affiliated with Baystate Health in Springfield, Mass. He would like to thank Joshua Lapps, Luke Heisenger, and all the members of the SHM Practice Management Committee for their assistance and input in drafting the guiding principles of onboarding and the case studies that have heavily inspired the above article.
References
1. Carucci R. To Retain New Hires, Spend More Time Onboarding Them. Harvard Busines Review. Dec 3, 2018. https://hbr.org/2018/12/to-retain-new-hires-spend-more-time-onboarding-them
2. Franz D. The staggering costs of physician turnover. Today’s Hospitalist. August 2016. https://www.todayshospitalist.com/staggering-costs-physician-turnover/
It goes beyond welcoming and orientation
It goes beyond welcoming and orientation
As I gear up to welcome and onboard new hires to our hospitalist group, I could not help but reflect on my first day as a hospitalist. Fresh out of residency, my orientation was a day and a half long.
The medical director gave me a brief overview of the program. The program administrator handed me a thick folder of policies followed by a quick tour of the hospital and an afternoon training for the computerized order entry system (that was a time before EHRs). The next morning, I was given my full panel of patients, my new lab coat, and sent off into the battlefield.
I can vividly remember feeling anxious, a bit confused, and quite overwhelmed as I went through my day. The days turned into a week and the next. I kept wondering if I was doing everything right. It took me a month to feel a little more comfortable. It all turned out fine. Since nobody told me otherwise, I assumed it did.
Quite a bit has changed since then in hospital medicine. Hospital medicine groups, nowadays, have to tackle the changing landscape of payment reform, take on responsibility for an increasing range of hospital quality metrics and juggle a swath of subspecialty comanagement agreements. Hospital medicine providers function from the inpatient to the post-acute care arena, all while continuing to demonstrate their value to the hospital administration. Simultaneously, they have to ensure their providers are engaged and functioning at their optimal level while battling the ever-increasing threat of burnout.
Thus, for new hires, all the above aspects of my orientation have become critical but alas terribly insufficient. Well into its third decade, the hospital medicine job market continues to boom but remains a revolving door. Hospital medicine groups continue to grow in size and integrate across hospitals in a given health system. The vast majority of the new hires tend to be fresh out of residency. The first year remains the most vulnerable period for a new hospitalist. Hospital medicine groups must design and implement a robust onboarding program for their new hires. It goes beyond welcoming and orientation of new hires to full integration and assimilation in order to transform them into highly efficient and productive team members. Effective onboarding is table stakes for a successful and thriving hospital medicine group.
The content
An effective onboarding program should focus on three key dimensions: the organizational, the technical, and the social.1
1. The organizational or administrative aspect: The most common aspect of onboarding is providing new hires with information on the group’s policies and procedures: what to do and how to do it. Equally essential is giving them the tools and contacts that will help them understand and navigate their first few months. Information on how to contact consultants, signing on and off shifts, and so on can be easily conveyed through documents. However, having peers and the critical administrative staff communicate other aspects such as a detailed tour of the hospital, scheduling, and vacation policies is far more effective. It provides an excellent opportunity to introduce new hires to the key personnel in the group and vice versa as new hires get familiar with the unofficial workplace language. Breaking down all this information into meaningful, absorbable boluses, spread over time, is key to avoiding information overload. Allowing new hires to assimilate and adapt to the group norms requires follow-up and reinforcement. Group leaders should plan to meet with them at predetermined intervals, such as at 30, 60, 90 days, to engage them in conversations about the group’s values, performance measurements, rewards, and the opportunities for growth that exist within the group and institution.
2. The technical or the clinical aspect: The majority of physicians and advanced providers hired to a hospital medicine group have come immediately from training. Transition into the autonomous role of an attending, or a semi-autonomous role for advanced providers, with a larger patient panel can be quite unnerving and stressful. It can be disorientating even for experienced providers transitioning into a new health system. A well-structured onboarding can allow providers to deploy their training and experience at your organization effectively. Many onboarding programs have a clinical ramp-up period. The providers begin with a limited patient panel and gradually acclimatize into a full patient load. Many programs pair a senior hospitalist with the new hire during this period – a ‘buddy.’ Buddies are available to help new hires navigate the health system and familiarize them with the stakeholders. They help new hires by providing context to understand their new role and how they can contribute to the group’s success. In many instances, buddies help outline the unspoken rules of the group.
3. The social aspect – enculturation and networking: This is probably the most important of the three elements. It is quite common for new hires to feel like a stranger in a new land. A well-designed onboarding program provides new hires the space to forge relationships with each other and existing members of the hospital medicine team. Groups can do this in myriad ways – an informal welcome social, a meet and greet breakfast or lunch, in-person orientation when designing the administrative onboarding, and assignment of buddies or mentors during their clinical ramp-up period. It is all about providing a space to establish and nurture lasting relationships between the new hires and the group. When done well, this helps transform a group into a community. It also lays the groundwork to avoid stress and loneliness, some of the culprits that lead to physician burnout. It is through these interpersonal connections that new hires adapt to a hospital medicine group’s prevailing culture.
The personnel
Effective onboarding should be more than mere orientation. Group leaders should make an active attempt at understanding the core values and needs of the group. A good onboarding process assists new hires to internalize and accept the norms of the group. This process is not just a result of what comes from top management but also what they see and hear from the rank and file providers in the group. Hence it is critical to have the right people who understand and embody these values at the planning table. It is equally essential that necessary time and resources are devoted to building a program that meets the needs of the group. The practice management committee at SHM interviewed five different programs across a spectrum of settings. All of them had a designated onboarding program leader with a planning committee that included the administrative staff and senior frontline hospitalists.
The costs
According to one estimate, the cost of physician turnover is $400,000-$600,000 per provider.2 Given such staggering costs, it is not difficult to justify the financial resources required to structure an effective onboarding program. Activities such as a detailed facility tour, a welcome breakfast, and a peer buddy system cost virtually nothing. They go a long way in building comradery, make new hires feel like they are part of a team, and reduce burnout and turnover. Costs of an onboarding program are typically related to wages during shadowing and clinical ramp-up. However, all the programs we interviewed acknowledged that the costs associated with onboarding, in the broader context, were small and necessary.
The bottom line
An effective onboarding program that is well planned, well structured, and well executed is inherently valuable. It sends a positive signal to new hires, reassuring them that they made a great decision by joining the group. It also reminds the existing providers why they want to be a part of the group and its culture.
It is not about what is said or done during the onboarding process or how long it lasts. It need not be overly complicated. It is how the process makes everyone feel about the group. At the end of the day, like in all aspects of life, that is what ultimately matters.
The SHM Practice Management Committee has created a document that outlines the guiding principles for effective onboarding with attached case studies. Visit the SHM website for more information: https://www.hospitalmedicine.org.
Dr. Irani is a hospitalist affiliated with Baystate Health in Springfield, Mass. He would like to thank Joshua Lapps, Luke Heisenger, and all the members of the SHM Practice Management Committee for their assistance and input in drafting the guiding principles of onboarding and the case studies that have heavily inspired the above article.
References
1. Carucci R. To Retain New Hires, Spend More Time Onboarding Them. Harvard Busines Review. Dec 3, 2018. https://hbr.org/2018/12/to-retain-new-hires-spend-more-time-onboarding-them
2. Franz D. The staggering costs of physician turnover. Today’s Hospitalist. August 2016. https://www.todayshospitalist.com/staggering-costs-physician-turnover/
As I gear up to welcome and onboard new hires to our hospitalist group, I could not help but reflect on my first day as a hospitalist. Fresh out of residency, my orientation was a day and a half long.
The medical director gave me a brief overview of the program. The program administrator handed me a thick folder of policies followed by a quick tour of the hospital and an afternoon training for the computerized order entry system (that was a time before EHRs). The next morning, I was given my full panel of patients, my new lab coat, and sent off into the battlefield.
I can vividly remember feeling anxious, a bit confused, and quite overwhelmed as I went through my day. The days turned into a week and the next. I kept wondering if I was doing everything right. It took me a month to feel a little more comfortable. It all turned out fine. Since nobody told me otherwise, I assumed it did.
Quite a bit has changed since then in hospital medicine. Hospital medicine groups, nowadays, have to tackle the changing landscape of payment reform, take on responsibility for an increasing range of hospital quality metrics and juggle a swath of subspecialty comanagement agreements. Hospital medicine providers function from the inpatient to the post-acute care arena, all while continuing to demonstrate their value to the hospital administration. Simultaneously, they have to ensure their providers are engaged and functioning at their optimal level while battling the ever-increasing threat of burnout.
Thus, for new hires, all the above aspects of my orientation have become critical but alas terribly insufficient. Well into its third decade, the hospital medicine job market continues to boom but remains a revolving door. Hospital medicine groups continue to grow in size and integrate across hospitals in a given health system. The vast majority of the new hires tend to be fresh out of residency. The first year remains the most vulnerable period for a new hospitalist. Hospital medicine groups must design and implement a robust onboarding program for their new hires. It goes beyond welcoming and orientation of new hires to full integration and assimilation in order to transform them into highly efficient and productive team members. Effective onboarding is table stakes for a successful and thriving hospital medicine group.
The content
An effective onboarding program should focus on three key dimensions: the organizational, the technical, and the social.1
1. The organizational or administrative aspect: The most common aspect of onboarding is providing new hires with information on the group’s policies and procedures: what to do and how to do it. Equally essential is giving them the tools and contacts that will help them understand and navigate their first few months. Information on how to contact consultants, signing on and off shifts, and so on can be easily conveyed through documents. However, having peers and the critical administrative staff communicate other aspects such as a detailed tour of the hospital, scheduling, and vacation policies is far more effective. It provides an excellent opportunity to introduce new hires to the key personnel in the group and vice versa as new hires get familiar with the unofficial workplace language. Breaking down all this information into meaningful, absorbable boluses, spread over time, is key to avoiding information overload. Allowing new hires to assimilate and adapt to the group norms requires follow-up and reinforcement. Group leaders should plan to meet with them at predetermined intervals, such as at 30, 60, 90 days, to engage them in conversations about the group’s values, performance measurements, rewards, and the opportunities for growth that exist within the group and institution.
2. The technical or the clinical aspect: The majority of physicians and advanced providers hired to a hospital medicine group have come immediately from training. Transition into the autonomous role of an attending, or a semi-autonomous role for advanced providers, with a larger patient panel can be quite unnerving and stressful. It can be disorientating even for experienced providers transitioning into a new health system. A well-structured onboarding can allow providers to deploy their training and experience at your organization effectively. Many onboarding programs have a clinical ramp-up period. The providers begin with a limited patient panel and gradually acclimatize into a full patient load. Many programs pair a senior hospitalist with the new hire during this period – a ‘buddy.’ Buddies are available to help new hires navigate the health system and familiarize them with the stakeholders. They help new hires by providing context to understand their new role and how they can contribute to the group’s success. In many instances, buddies help outline the unspoken rules of the group.
3. The social aspect – enculturation and networking: This is probably the most important of the three elements. It is quite common for new hires to feel like a stranger in a new land. A well-designed onboarding program provides new hires the space to forge relationships with each other and existing members of the hospital medicine team. Groups can do this in myriad ways – an informal welcome social, a meet and greet breakfast or lunch, in-person orientation when designing the administrative onboarding, and assignment of buddies or mentors during their clinical ramp-up period. It is all about providing a space to establish and nurture lasting relationships between the new hires and the group. When done well, this helps transform a group into a community. It also lays the groundwork to avoid stress and loneliness, some of the culprits that lead to physician burnout. It is through these interpersonal connections that new hires adapt to a hospital medicine group’s prevailing culture.
The personnel
Effective onboarding should be more than mere orientation. Group leaders should make an active attempt at understanding the core values and needs of the group. A good onboarding process assists new hires to internalize and accept the norms of the group. This process is not just a result of what comes from top management but also what they see and hear from the rank and file providers in the group. Hence it is critical to have the right people who understand and embody these values at the planning table. It is equally essential that necessary time and resources are devoted to building a program that meets the needs of the group. The practice management committee at SHM interviewed five different programs across a spectrum of settings. All of them had a designated onboarding program leader with a planning committee that included the administrative staff and senior frontline hospitalists.
The costs
According to one estimate, the cost of physician turnover is $400,000-$600,000 per provider.2 Given such staggering costs, it is not difficult to justify the financial resources required to structure an effective onboarding program. Activities such as a detailed facility tour, a welcome breakfast, and a peer buddy system cost virtually nothing. They go a long way in building comradery, make new hires feel like they are part of a team, and reduce burnout and turnover. Costs of an onboarding program are typically related to wages during shadowing and clinical ramp-up. However, all the programs we interviewed acknowledged that the costs associated with onboarding, in the broader context, were small and necessary.
The bottom line
An effective onboarding program that is well planned, well structured, and well executed is inherently valuable. It sends a positive signal to new hires, reassuring them that they made a great decision by joining the group. It also reminds the existing providers why they want to be a part of the group and its culture.
It is not about what is said or done during the onboarding process or how long it lasts. It need not be overly complicated. It is how the process makes everyone feel about the group. At the end of the day, like in all aspects of life, that is what ultimately matters.
The SHM Practice Management Committee has created a document that outlines the guiding principles for effective onboarding with attached case studies. Visit the SHM website for more information: https://www.hospitalmedicine.org.
Dr. Irani is a hospitalist affiliated with Baystate Health in Springfield, Mass. He would like to thank Joshua Lapps, Luke Heisenger, and all the members of the SHM Practice Management Committee for their assistance and input in drafting the guiding principles of onboarding and the case studies that have heavily inspired the above article.
References
1. Carucci R. To Retain New Hires, Spend More Time Onboarding Them. Harvard Busines Review. Dec 3, 2018. https://hbr.org/2018/12/to-retain-new-hires-spend-more-time-onboarding-them
2. Franz D. The staggering costs of physician turnover. Today’s Hospitalist. August 2016. https://www.todayshospitalist.com/staggering-costs-physician-turnover/
Hospitalist movers and shakers – March 2020
Swati Mehta, MD, recently was honored as the lone hospitalist on the National Executive Physician Council for Beryl Institute (Nashville, Tenn.). Only 24 total physicians were selected to the council. Dr. Mehta also was named the 2019 Distinguished Physician Award winner at Vituity (Emeryville, Calif.), where she is the executive director of quality and performance.
A nocturnist at Sequoia Hospital (Redwood City, Calif.), Dr. Mehta is a member of the Society of Hospital Medicine’s Patient Experience interest group.
Shannon Phillips, MD, SFHM, has been named to the National Quality Forum’s Board of Directors for 2020. The chief patient experience officer at Intermountain Healthcare (Salt Lake City, Utah), she also is a recent member of the Performance Measurement and Reporting Committee.
Dr. Phillips, whose focus at Intermountain is on catalyzing safety, quality, and experience of care, was named a 2018 Becker’s Hospital Review Hospital and Health System CXO to Know. Previously, she worked at the Cleveland Clinic, where she was its first patient safety officer and an associate chief quality officer.
Vineet Arora, MD, MHM, has been elected as a new member of the National Academy of Medicine, which honors pioneering scientific and professional achievements within the field.
An academic hospitalist at the University of Chicago, Dr. Arora specializes in improving the learning environment for her medical trainees, as well as maintaining a high level of quality, safety, and care for patients. She also is considered an expert in using social media and other new technology to enhance medical education.
The National Academy of Medicine stated that Dr. Arora’s honor was “for pioneering work to optimize resident fatigue and patient safety during long shifts.”
Edmondo Robinson, MD, SFHM, has been named senior vice president and chief digital innovation officer at Moffitt Cancer Center (Tampa, Fla.). The chief digital innovation officer position is a newly created position that the veteran physician has assumed. Dr. Robinson has 16 years’ experience in clinical and technological work.
In this new position, Dr. Robinson, a practicing academic hospitalist, will head Moffitt’s digital innovation while looking to create and test new services, programs, partnerships, and technologies.
Dr. Robinson comes to Moffitt after serving as chief transformation officer and senior vice president at ChristianaCare (Wilmington, Del.). A teacher at Sidney Kimmel Medical College, Philadelphia, Dr. Robinson was the founding medical director of ChristianaCare Hospitalist Partners.
Relias Healthcare (Tupelo, Miss.) has begun providing hospitalist and emergency medicine services for North Mississippi Health Services’ Gilmore-Amory Trauma Center. Relias, a multistate company that has partnered with more than 150 providers, now has a role at four different North Mississippi Health Services facilities.
Mednax (Sunrise, Fla.) has added Arcenio Chacon and Associated Pediatricians of Homestead, a pediatric critical care and hospital practice, as an affiliate.
Chacon and Associated Pediatricians are based out of Miami and have served Baptist Health South Florida for more than 25 years. The four-physician practice provides critical care and pediatric hospitalist services at Baptist Children’s Hospital (Miami) and hospitalist services at Miami Cancer Institute and Homestead (Fla.) Hospital.
Mednax is a health solutions company that provides subspecialty service in all 50 states. Established in 1979, Mednax partners with hospitals, health systems, and health care facilities to offer clinical services, as well as revenue cycle management, patient engagement, and perioperative improvement consulting services.
Swati Mehta, MD, recently was honored as the lone hospitalist on the National Executive Physician Council for Beryl Institute (Nashville, Tenn.). Only 24 total physicians were selected to the council. Dr. Mehta also was named the 2019 Distinguished Physician Award winner at Vituity (Emeryville, Calif.), where she is the executive director of quality and performance.
A nocturnist at Sequoia Hospital (Redwood City, Calif.), Dr. Mehta is a member of the Society of Hospital Medicine’s Patient Experience interest group.
Shannon Phillips, MD, SFHM, has been named to the National Quality Forum’s Board of Directors for 2020. The chief patient experience officer at Intermountain Healthcare (Salt Lake City, Utah), she also is a recent member of the Performance Measurement and Reporting Committee.
Dr. Phillips, whose focus at Intermountain is on catalyzing safety, quality, and experience of care, was named a 2018 Becker’s Hospital Review Hospital and Health System CXO to Know. Previously, she worked at the Cleveland Clinic, where she was its first patient safety officer and an associate chief quality officer.
Vineet Arora, MD, MHM, has been elected as a new member of the National Academy of Medicine, which honors pioneering scientific and professional achievements within the field.
An academic hospitalist at the University of Chicago, Dr. Arora specializes in improving the learning environment for her medical trainees, as well as maintaining a high level of quality, safety, and care for patients. She also is considered an expert in using social media and other new technology to enhance medical education.
The National Academy of Medicine stated that Dr. Arora’s honor was “for pioneering work to optimize resident fatigue and patient safety during long shifts.”
Edmondo Robinson, MD, SFHM, has been named senior vice president and chief digital innovation officer at Moffitt Cancer Center (Tampa, Fla.). The chief digital innovation officer position is a newly created position that the veteran physician has assumed. Dr. Robinson has 16 years’ experience in clinical and technological work.
In this new position, Dr. Robinson, a practicing academic hospitalist, will head Moffitt’s digital innovation while looking to create and test new services, programs, partnerships, and technologies.
Dr. Robinson comes to Moffitt after serving as chief transformation officer and senior vice president at ChristianaCare (Wilmington, Del.). A teacher at Sidney Kimmel Medical College, Philadelphia, Dr. Robinson was the founding medical director of ChristianaCare Hospitalist Partners.
Relias Healthcare (Tupelo, Miss.) has begun providing hospitalist and emergency medicine services for North Mississippi Health Services’ Gilmore-Amory Trauma Center. Relias, a multistate company that has partnered with more than 150 providers, now has a role at four different North Mississippi Health Services facilities.
Mednax (Sunrise, Fla.) has added Arcenio Chacon and Associated Pediatricians of Homestead, a pediatric critical care and hospital practice, as an affiliate.
Chacon and Associated Pediatricians are based out of Miami and have served Baptist Health South Florida for more than 25 years. The four-physician practice provides critical care and pediatric hospitalist services at Baptist Children’s Hospital (Miami) and hospitalist services at Miami Cancer Institute and Homestead (Fla.) Hospital.
Mednax is a health solutions company that provides subspecialty service in all 50 states. Established in 1979, Mednax partners with hospitals, health systems, and health care facilities to offer clinical services, as well as revenue cycle management, patient engagement, and perioperative improvement consulting services.
Swati Mehta, MD, recently was honored as the lone hospitalist on the National Executive Physician Council for Beryl Institute (Nashville, Tenn.). Only 24 total physicians were selected to the council. Dr. Mehta also was named the 2019 Distinguished Physician Award winner at Vituity (Emeryville, Calif.), where she is the executive director of quality and performance.
A nocturnist at Sequoia Hospital (Redwood City, Calif.), Dr. Mehta is a member of the Society of Hospital Medicine’s Patient Experience interest group.
Shannon Phillips, MD, SFHM, has been named to the National Quality Forum’s Board of Directors for 2020. The chief patient experience officer at Intermountain Healthcare (Salt Lake City, Utah), she also is a recent member of the Performance Measurement and Reporting Committee.
Dr. Phillips, whose focus at Intermountain is on catalyzing safety, quality, and experience of care, was named a 2018 Becker’s Hospital Review Hospital and Health System CXO to Know. Previously, she worked at the Cleveland Clinic, where she was its first patient safety officer and an associate chief quality officer.
Vineet Arora, MD, MHM, has been elected as a new member of the National Academy of Medicine, which honors pioneering scientific and professional achievements within the field.
An academic hospitalist at the University of Chicago, Dr. Arora specializes in improving the learning environment for her medical trainees, as well as maintaining a high level of quality, safety, and care for patients. She also is considered an expert in using social media and other new technology to enhance medical education.
The National Academy of Medicine stated that Dr. Arora’s honor was “for pioneering work to optimize resident fatigue and patient safety during long shifts.”
Edmondo Robinson, MD, SFHM, has been named senior vice president and chief digital innovation officer at Moffitt Cancer Center (Tampa, Fla.). The chief digital innovation officer position is a newly created position that the veteran physician has assumed. Dr. Robinson has 16 years’ experience in clinical and technological work.
In this new position, Dr. Robinson, a practicing academic hospitalist, will head Moffitt’s digital innovation while looking to create and test new services, programs, partnerships, and technologies.
Dr. Robinson comes to Moffitt after serving as chief transformation officer and senior vice president at ChristianaCare (Wilmington, Del.). A teacher at Sidney Kimmel Medical College, Philadelphia, Dr. Robinson was the founding medical director of ChristianaCare Hospitalist Partners.
Relias Healthcare (Tupelo, Miss.) has begun providing hospitalist and emergency medicine services for North Mississippi Health Services’ Gilmore-Amory Trauma Center. Relias, a multistate company that has partnered with more than 150 providers, now has a role at four different North Mississippi Health Services facilities.
Mednax (Sunrise, Fla.) has added Arcenio Chacon and Associated Pediatricians of Homestead, a pediatric critical care and hospital practice, as an affiliate.
Chacon and Associated Pediatricians are based out of Miami and have served Baptist Health South Florida for more than 25 years. The four-physician practice provides critical care and pediatric hospitalist services at Baptist Children’s Hospital (Miami) and hospitalist services at Miami Cancer Institute and Homestead (Fla.) Hospital.
Mednax is a health solutions company that provides subspecialty service in all 50 states. Established in 1979, Mednax partners with hospitals, health systems, and health care facilities to offer clinical services, as well as revenue cycle management, patient engagement, and perioperative improvement consulting services.
Hospital medicine physician leaders
The right skills and time to develop them
“When you get someone who knows what quality looks like and pair that with curiosity about new ways to think about leading, you end up with the people who are able to produce dramatic innovations in the field.”1
In medicine, a physician is trained to take charge in emergent situations and make potentially lifesaving efforts. However, when it comes to leading teams of individuals, not only must successful leaders have the right skills, they also need time to dedicate to the work of leadership.
To better understand current approaches to dedicated hospital medicine group (HMG) leadership time, let’s examine the 2018 State of Hospital Medicine (SoHM) Report. The survey, upon which the Report was based, examined two aspects of leadership: 1) how much dedicated time a leader receives to manage the group; and 2) how the leader’s time is compensated. Looking closely at the data displayed in graphs from the SoHM Report (Figures 1, 2, and 3), we can see that dedicated administrative time is directly proportional to the size of the group.
In my current role as a regional medical director in the Dallas-Fort Worth market, I oversee some programs where the size is greater than 30 full-time equivalents (FTEs), and requires a full-time administrative physician leader to manage the group. Their daily administrative duties include, but are not limited to, addressing physician performance and behaviors, managing team performance metrics, dealing with consultants’ expectations, attending and leading various committee meetings at the hospital or the system level, attending and presenting performance reviews, leading and preparing for team meetings, as well as addressing and being innovative in leading new initiatives from the hospital partner system.
Although physician leaders are paid more for their work, the 2018 SoHM Report reveals a decline in the premium year over year. One of the reasons for the payment decline that I have encountered in various groups is that their incentives for leading the group are based on performance, as opposed to receiving a fixed stipend. Another reason is the presence of dedicated administrative support or the inclusion of a performance improvement staffer, such as an additional nurse or advanced practice provider, in the group.
Evidence suggests that organizations and patients benefit when physicians take on leadership roles. Physician leaders play critical roles in providing high-quality patient care. How can the Society of Hospital Medicine help? Management degrees and leadership workshops have become a common pathway for many physicians, including myself. SHM provides one of the most thorough and relevant experiences through the SHM Leadership Academy. The focus of the Leadership Academy is on developing a broad set of additional leadership competencies across a spectrum of experience.5 As hospitalist physicians are often expected to fulfill a broader leadership void, we must pay attention to developing the leadership skills depicted in Figure 3. Hospital medicine is an ideal “proving ground” for future physician executives and leaders, as they often share the same characteristics required for success.
The leadership paths available in my organization, Sound Physicians, were recently highlighted in a New York Times article.3 Sound Physicians employs more than 3,000 physicians across the country, and has a pipeline for doctors to advance through structured rungs of leadership – emphasizing a different mix of clinical, strategic, and business skills at each stage, from individual practitioner to the C-suite. The training includes in-person and online courses, as well as an annual conference, to help doctors develop management and leadership competencies, and learn how to apply these skills within their organizations. Since introducing its leadership development program, the company reports less turnover, higher morale, and better growth. I personally have gone through the leadership training provided by Sound Physicians, and reflecting back, it has been a transformational experience for me. Leadership is a journey, not a destination, and as physicians we should strive to learn more from the health care leaders around us.
The administrative workload for hospital-based physician leaders will increase with the arrival of value-based programs and alternative payment models promoted by the Centers for Medicare and Medicaid Services. Lead hospitalist duties are not limited to daily operations, but can extend to leading the strategic vision of the hospital or health system. The 2020 SoHM Report will reflect these changes, as well as provide further information about how to manage and set expectations for physician leaders, based on group size and employment model.
Dr. Patel is a regional medical director with Sound Physicians. He manages more than 100 FTE hospitalists and advanced-practice providers (APPs) within multiple health systems and hospitals in the Texas market. He also serves as a member of the SHM Practice Analysis Committee and as a vice president of SHM North Texas Chapter.
References
1. Angood P and Birk S. The Value of Physician Leadership. Physician Exec. 2014 May-Jun;40(3):6-20.
2. Rice JA. Expanding the Need for Physician Leaders. Executive Insight, Advance Healthcare Network, Nov 16, 2011. Available at: http://healthcare-executive-insight.advanceweb.com/Features/Articles/Expanding-the-Need-for-Physician-Leaders.aspx.
3. Khullar D. Good leaders make good doctors. New York Times. 2019 Nov 21.
4. Beresford L. The State of Hospital Medicine in 2018. Hospitalist. 2019;23(1):1-11.
5. Harte B. Hospitalists can meet the demand for physician executives. Hospitalist. 2018 Nov 29.
The right skills and time to develop them
The right skills and time to develop them
“When you get someone who knows what quality looks like and pair that with curiosity about new ways to think about leading, you end up with the people who are able to produce dramatic innovations in the field.”1
In medicine, a physician is trained to take charge in emergent situations and make potentially lifesaving efforts. However, when it comes to leading teams of individuals, not only must successful leaders have the right skills, they also need time to dedicate to the work of leadership.
To better understand current approaches to dedicated hospital medicine group (HMG) leadership time, let’s examine the 2018 State of Hospital Medicine (SoHM) Report. The survey, upon which the Report was based, examined two aspects of leadership: 1) how much dedicated time a leader receives to manage the group; and 2) how the leader’s time is compensated. Looking closely at the data displayed in graphs from the SoHM Report (Figures 1, 2, and 3), we can see that dedicated administrative time is directly proportional to the size of the group.
In my current role as a regional medical director in the Dallas-Fort Worth market, I oversee some programs where the size is greater than 30 full-time equivalents (FTEs), and requires a full-time administrative physician leader to manage the group. Their daily administrative duties include, but are not limited to, addressing physician performance and behaviors, managing team performance metrics, dealing with consultants’ expectations, attending and leading various committee meetings at the hospital or the system level, attending and presenting performance reviews, leading and preparing for team meetings, as well as addressing and being innovative in leading new initiatives from the hospital partner system.
Although physician leaders are paid more for their work, the 2018 SoHM Report reveals a decline in the premium year over year. One of the reasons for the payment decline that I have encountered in various groups is that their incentives for leading the group are based on performance, as opposed to receiving a fixed stipend. Another reason is the presence of dedicated administrative support or the inclusion of a performance improvement staffer, such as an additional nurse or advanced practice provider, in the group.
Evidence suggests that organizations and patients benefit when physicians take on leadership roles. Physician leaders play critical roles in providing high-quality patient care. How can the Society of Hospital Medicine help? Management degrees and leadership workshops have become a common pathway for many physicians, including myself. SHM provides one of the most thorough and relevant experiences through the SHM Leadership Academy. The focus of the Leadership Academy is on developing a broad set of additional leadership competencies across a spectrum of experience.5 As hospitalist physicians are often expected to fulfill a broader leadership void, we must pay attention to developing the leadership skills depicted in Figure 3. Hospital medicine is an ideal “proving ground” for future physician executives and leaders, as they often share the same characteristics required for success.
The leadership paths available in my organization, Sound Physicians, were recently highlighted in a New York Times article.3 Sound Physicians employs more than 3,000 physicians across the country, and has a pipeline for doctors to advance through structured rungs of leadership – emphasizing a different mix of clinical, strategic, and business skills at each stage, from individual practitioner to the C-suite. The training includes in-person and online courses, as well as an annual conference, to help doctors develop management and leadership competencies, and learn how to apply these skills within their organizations. Since introducing its leadership development program, the company reports less turnover, higher morale, and better growth. I personally have gone through the leadership training provided by Sound Physicians, and reflecting back, it has been a transformational experience for me. Leadership is a journey, not a destination, and as physicians we should strive to learn more from the health care leaders around us.
The administrative workload for hospital-based physician leaders will increase with the arrival of value-based programs and alternative payment models promoted by the Centers for Medicare and Medicaid Services. Lead hospitalist duties are not limited to daily operations, but can extend to leading the strategic vision of the hospital or health system. The 2020 SoHM Report will reflect these changes, as well as provide further information about how to manage and set expectations for physician leaders, based on group size and employment model.
Dr. Patel is a regional medical director with Sound Physicians. He manages more than 100 FTE hospitalists and advanced-practice providers (APPs) within multiple health systems and hospitals in the Texas market. He also serves as a member of the SHM Practice Analysis Committee and as a vice president of SHM North Texas Chapter.
References
1. Angood P and Birk S. The Value of Physician Leadership. Physician Exec. 2014 May-Jun;40(3):6-20.
2. Rice JA. Expanding the Need for Physician Leaders. Executive Insight, Advance Healthcare Network, Nov 16, 2011. Available at: http://healthcare-executive-insight.advanceweb.com/Features/Articles/Expanding-the-Need-for-Physician-Leaders.aspx.
3. Khullar D. Good leaders make good doctors. New York Times. 2019 Nov 21.
4. Beresford L. The State of Hospital Medicine in 2018. Hospitalist. 2019;23(1):1-11.
5. Harte B. Hospitalists can meet the demand for physician executives. Hospitalist. 2018 Nov 29.
“When you get someone who knows what quality looks like and pair that with curiosity about new ways to think about leading, you end up with the people who are able to produce dramatic innovations in the field.”1
In medicine, a physician is trained to take charge in emergent situations and make potentially lifesaving efforts. However, when it comes to leading teams of individuals, not only must successful leaders have the right skills, they also need time to dedicate to the work of leadership.
To better understand current approaches to dedicated hospital medicine group (HMG) leadership time, let’s examine the 2018 State of Hospital Medicine (SoHM) Report. The survey, upon which the Report was based, examined two aspects of leadership: 1) how much dedicated time a leader receives to manage the group; and 2) how the leader’s time is compensated. Looking closely at the data displayed in graphs from the SoHM Report (Figures 1, 2, and 3), we can see that dedicated administrative time is directly proportional to the size of the group.
In my current role as a regional medical director in the Dallas-Fort Worth market, I oversee some programs where the size is greater than 30 full-time equivalents (FTEs), and requires a full-time administrative physician leader to manage the group. Their daily administrative duties include, but are not limited to, addressing physician performance and behaviors, managing team performance metrics, dealing with consultants’ expectations, attending and leading various committee meetings at the hospital or the system level, attending and presenting performance reviews, leading and preparing for team meetings, as well as addressing and being innovative in leading new initiatives from the hospital partner system.
Although physician leaders are paid more for their work, the 2018 SoHM Report reveals a decline in the premium year over year. One of the reasons for the payment decline that I have encountered in various groups is that their incentives for leading the group are based on performance, as opposed to receiving a fixed stipend. Another reason is the presence of dedicated administrative support or the inclusion of a performance improvement staffer, such as an additional nurse or advanced practice provider, in the group.
Evidence suggests that organizations and patients benefit when physicians take on leadership roles. Physician leaders play critical roles in providing high-quality patient care. How can the Society of Hospital Medicine help? Management degrees and leadership workshops have become a common pathway for many physicians, including myself. SHM provides one of the most thorough and relevant experiences through the SHM Leadership Academy. The focus of the Leadership Academy is on developing a broad set of additional leadership competencies across a spectrum of experience.5 As hospitalist physicians are often expected to fulfill a broader leadership void, we must pay attention to developing the leadership skills depicted in Figure 3. Hospital medicine is an ideal “proving ground” for future physician executives and leaders, as they often share the same characteristics required for success.
The leadership paths available in my organization, Sound Physicians, were recently highlighted in a New York Times article.3 Sound Physicians employs more than 3,000 physicians across the country, and has a pipeline for doctors to advance through structured rungs of leadership – emphasizing a different mix of clinical, strategic, and business skills at each stage, from individual practitioner to the C-suite. The training includes in-person and online courses, as well as an annual conference, to help doctors develop management and leadership competencies, and learn how to apply these skills within their organizations. Since introducing its leadership development program, the company reports less turnover, higher morale, and better growth. I personally have gone through the leadership training provided by Sound Physicians, and reflecting back, it has been a transformational experience for me. Leadership is a journey, not a destination, and as physicians we should strive to learn more from the health care leaders around us.
The administrative workload for hospital-based physician leaders will increase with the arrival of value-based programs and alternative payment models promoted by the Centers for Medicare and Medicaid Services. Lead hospitalist duties are not limited to daily operations, but can extend to leading the strategic vision of the hospital or health system. The 2020 SoHM Report will reflect these changes, as well as provide further information about how to manage and set expectations for physician leaders, based on group size and employment model.
Dr. Patel is a regional medical director with Sound Physicians. He manages more than 100 FTE hospitalists and advanced-practice providers (APPs) within multiple health systems and hospitals in the Texas market. He also serves as a member of the SHM Practice Analysis Committee and as a vice president of SHM North Texas Chapter.
References
1. Angood P and Birk S. The Value of Physician Leadership. Physician Exec. 2014 May-Jun;40(3):6-20.
2. Rice JA. Expanding the Need for Physician Leaders. Executive Insight, Advance Healthcare Network, Nov 16, 2011. Available at: http://healthcare-executive-insight.advanceweb.com/Features/Articles/Expanding-the-Need-for-Physician-Leaders.aspx.
3. Khullar D. Good leaders make good doctors. New York Times. 2019 Nov 21.
4. Beresford L. The State of Hospital Medicine in 2018. Hospitalist. 2019;23(1):1-11.
5. Harte B. Hospitalists can meet the demand for physician executives. Hospitalist. 2018 Nov 29.
A match made in medicine: Match Day 2020
Match Day is the celebration of the National Resident Matching Program® (NRMP®) results, which seals the fate not only of future medical professionals, but of the program placements dedicated to supporting the acceleration of their careers.
Daniel Ricotta, MD, FHM, an academic hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston, and an active SHM member since 2013, offers unique insight into the value of understanding both sides of this interview table.
As the associate program director of BIDMC’s Internal Medicine Residency Program and the director of Simulation Education at the Carl J. Shapiro Center for Education & Research, Dr. Ricotta is able to act on his passions for medical education and clinical care.
“I was attracted to the breadth of medicine and enjoyed learning everything,” Dr. Ricotta said. “I knew I wanted to do academic medicine and education, and I was able to get involved by working with students and residents early on in my career.”
A natural fit for his current roles, Dr. Ricotta has gained a unique perspective on the match process and how it has evolved since he began his residency nine years ago.
Preparing for Match Day includes an extensive checklist of life-altering to-dos that shape your career trajectory. Medical students must have noteworthy CV points, scholarly recommendations, stand-out interviews, and a thoughtful rank list – among many other things to consider throughout the course of the match. Dr. Ricotta said that while this application process has generally remained the same since his participation, he has noticed that the students themselves have changed.
“Students going into residency are more mature and further along professionally,” he explained. “I’ve seen more students go on to do something else for a while and have gained more experience. They’re taking time off for research or getting dual degrees.”
Additionally, according to Dr. Ricotta, students are applying to double the number of programs than in years past, and are even using technology to their benefit. Because interview slots are limited, some students set up “bot automation” to help lock in interviews.
Amidst what can feel like a free-for-all, Dr. Ricotta reminds his students that the match process is a two-sided relationship.
“I certainly didn’t realize how much work goes into recruitment when I was a student,” Dr. Ricotta admitted. “What students don’t think about is the amount of care that goes into trying to match students who share similar values, the mission, or are a good cultural fit.”
He went on to emphasize the importance of environmental compatibility.
“Go somewhere that you feel you will fit in. Where you will thrive,” he said. “Go somewhere that has a mission that resonates with your mission and think about your fellow applicants and potential mentorship. Could you see yourself being their classmate? Does this program have people there who can help you to achieve your goals?”
Keeping in mind questions like these, it is no surprise that because of hospital medicine’s scheduling flexibility and hands-on learning opportunities that more and more students are interested in exploring this specialty.
“What is amazing about hospital medicine is the ample opportunity for you to get involved earlier in your career and build from that,” he said. “There is more face time with patients, more training for medical students available, countless academic opportunities in research and scholarships, and even conferences.”
Because of the multiple career pathways available in hospital medicine, SHM aims to provide students and residents with professional tools and opportunities as early as possible to allow them to get a preview of what they can expect as a hospitalist – no matter which path they choose.
“SHM is about getting involved,” said Dr. Ricotta. “SHM encourages residents to become actively incorporated into the community through chapters, conferences, and other networking opportunities on both local and national levels. That’s really difficult to do as a resident.”
Whether you’re waiting on the NRMP® results this year or you are in the beginning stages of gathering your application materials, one thing is clear according to Dr. Ricotta, you’re not just an applicant number.
Are you a student interested in exploring a career in hospital medicine? SHM supports educational and professional needs at all stages of your career. When you join SHM during your residency training, you receive access to programs, resources, and opportunities that will enhance your skills and raise your professional profile. For more information about our Residents & Fellows membership opportunity, please visit: hospitalmedicine.org/residents.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
Match Day is the celebration of the National Resident Matching Program® (NRMP®) results, which seals the fate not only of future medical professionals, but of the program placements dedicated to supporting the acceleration of their careers.
Daniel Ricotta, MD, FHM, an academic hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston, and an active SHM member since 2013, offers unique insight into the value of understanding both sides of this interview table.
As the associate program director of BIDMC’s Internal Medicine Residency Program and the director of Simulation Education at the Carl J. Shapiro Center for Education & Research, Dr. Ricotta is able to act on his passions for medical education and clinical care.
“I was attracted to the breadth of medicine and enjoyed learning everything,” Dr. Ricotta said. “I knew I wanted to do academic medicine and education, and I was able to get involved by working with students and residents early on in my career.”
A natural fit for his current roles, Dr. Ricotta has gained a unique perspective on the match process and how it has evolved since he began his residency nine years ago.
Preparing for Match Day includes an extensive checklist of life-altering to-dos that shape your career trajectory. Medical students must have noteworthy CV points, scholarly recommendations, stand-out interviews, and a thoughtful rank list – among many other things to consider throughout the course of the match. Dr. Ricotta said that while this application process has generally remained the same since his participation, he has noticed that the students themselves have changed.
“Students going into residency are more mature and further along professionally,” he explained. “I’ve seen more students go on to do something else for a while and have gained more experience. They’re taking time off for research or getting dual degrees.”
Additionally, according to Dr. Ricotta, students are applying to double the number of programs than in years past, and are even using technology to their benefit. Because interview slots are limited, some students set up “bot automation” to help lock in interviews.
Amidst what can feel like a free-for-all, Dr. Ricotta reminds his students that the match process is a two-sided relationship.
“I certainly didn’t realize how much work goes into recruitment when I was a student,” Dr. Ricotta admitted. “What students don’t think about is the amount of care that goes into trying to match students who share similar values, the mission, or are a good cultural fit.”
He went on to emphasize the importance of environmental compatibility.
“Go somewhere that you feel you will fit in. Where you will thrive,” he said. “Go somewhere that has a mission that resonates with your mission and think about your fellow applicants and potential mentorship. Could you see yourself being their classmate? Does this program have people there who can help you to achieve your goals?”
Keeping in mind questions like these, it is no surprise that because of hospital medicine’s scheduling flexibility and hands-on learning opportunities that more and more students are interested in exploring this specialty.
“What is amazing about hospital medicine is the ample opportunity for you to get involved earlier in your career and build from that,” he said. “There is more face time with patients, more training for medical students available, countless academic opportunities in research and scholarships, and even conferences.”
Because of the multiple career pathways available in hospital medicine, SHM aims to provide students and residents with professional tools and opportunities as early as possible to allow them to get a preview of what they can expect as a hospitalist – no matter which path they choose.
“SHM is about getting involved,” said Dr. Ricotta. “SHM encourages residents to become actively incorporated into the community through chapters, conferences, and other networking opportunities on both local and national levels. That’s really difficult to do as a resident.”
Whether you’re waiting on the NRMP® results this year or you are in the beginning stages of gathering your application materials, one thing is clear according to Dr. Ricotta, you’re not just an applicant number.
Are you a student interested in exploring a career in hospital medicine? SHM supports educational and professional needs at all stages of your career. When you join SHM during your residency training, you receive access to programs, resources, and opportunities that will enhance your skills and raise your professional profile. For more information about our Residents & Fellows membership opportunity, please visit: hospitalmedicine.org/residents.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
Match Day is the celebration of the National Resident Matching Program® (NRMP®) results, which seals the fate not only of future medical professionals, but of the program placements dedicated to supporting the acceleration of their careers.
Daniel Ricotta, MD, FHM, an academic hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston, and an active SHM member since 2013, offers unique insight into the value of understanding both sides of this interview table.
As the associate program director of BIDMC’s Internal Medicine Residency Program and the director of Simulation Education at the Carl J. Shapiro Center for Education & Research, Dr. Ricotta is able to act on his passions for medical education and clinical care.
“I was attracted to the breadth of medicine and enjoyed learning everything,” Dr. Ricotta said. “I knew I wanted to do academic medicine and education, and I was able to get involved by working with students and residents early on in my career.”
A natural fit for his current roles, Dr. Ricotta has gained a unique perspective on the match process and how it has evolved since he began his residency nine years ago.
Preparing for Match Day includes an extensive checklist of life-altering to-dos that shape your career trajectory. Medical students must have noteworthy CV points, scholarly recommendations, stand-out interviews, and a thoughtful rank list – among many other things to consider throughout the course of the match. Dr. Ricotta said that while this application process has generally remained the same since his participation, he has noticed that the students themselves have changed.
“Students going into residency are more mature and further along professionally,” he explained. “I’ve seen more students go on to do something else for a while and have gained more experience. They’re taking time off for research or getting dual degrees.”
Additionally, according to Dr. Ricotta, students are applying to double the number of programs than in years past, and are even using technology to their benefit. Because interview slots are limited, some students set up “bot automation” to help lock in interviews.
Amidst what can feel like a free-for-all, Dr. Ricotta reminds his students that the match process is a two-sided relationship.
“I certainly didn’t realize how much work goes into recruitment when I was a student,” Dr. Ricotta admitted. “What students don’t think about is the amount of care that goes into trying to match students who share similar values, the mission, or are a good cultural fit.”
He went on to emphasize the importance of environmental compatibility.
“Go somewhere that you feel you will fit in. Where you will thrive,” he said. “Go somewhere that has a mission that resonates with your mission and think about your fellow applicants and potential mentorship. Could you see yourself being their classmate? Does this program have people there who can help you to achieve your goals?”
Keeping in mind questions like these, it is no surprise that because of hospital medicine’s scheduling flexibility and hands-on learning opportunities that more and more students are interested in exploring this specialty.
“What is amazing about hospital medicine is the ample opportunity for you to get involved earlier in your career and build from that,” he said. “There is more face time with patients, more training for medical students available, countless academic opportunities in research and scholarships, and even conferences.”
Because of the multiple career pathways available in hospital medicine, SHM aims to provide students and residents with professional tools and opportunities as early as possible to allow them to get a preview of what they can expect as a hospitalist – no matter which path they choose.
“SHM is about getting involved,” said Dr. Ricotta. “SHM encourages residents to become actively incorporated into the community through chapters, conferences, and other networking opportunities on both local and national levels. That’s really difficult to do as a resident.”
Whether you’re waiting on the NRMP® results this year or you are in the beginning stages of gathering your application materials, one thing is clear according to Dr. Ricotta, you’re not just an applicant number.
Are you a student interested in exploring a career in hospital medicine? SHM supports educational and professional needs at all stages of your career. When you join SHM during your residency training, you receive access to programs, resources, and opportunities that will enhance your skills and raise your professional profile. For more information about our Residents & Fellows membership opportunity, please visit: hospitalmedicine.org/residents.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
Hospitalist profile: Charu Puri, MD
Charu Puri, MD, FHM, is a hospitalist and medical informaticist at Sutter East Bay Medical Group in Oakland, Calif. She also serves as medical director for onboarding, mentoring, and physician development.
Dr. Puri has been a member of the Society of Hospital Medicine since 2009, and attended the Society’s Leadership Academy, where she was inspired to create a mentorship program at her own institution. She is a member of the San Francisco Bay chapter of SHM and serves on the Performance Measurement and Reporting Committee.
At what point in your education/training did you decide to practice hospital medicine? What about hospital medicine appealed to you?
It was early on in my residency that it became clear to me that I wanted to pursue the hospitalist track. It was a natural fit, and I gravitated toward the hospitalist side of medicine. What appealed to me most was that we had the opportunity and privilege to provide care to patients in their most vulnerable state and experience the effects of that care in real time. I found that very gratifying.
There is also a sense of community and camaraderie that comes with working in a hospital setting. Everyone is working together, trying to help patients. The collegiality and the relationships that develop are very rewarding. I have been fortunate enough to have built strong friendships with the hospitalists in my group as well as colleagues from other disciplines in medicine that work in the hospital.
What is your current role at Sutter Health?
Alta Bates Summit Medical Center is part of the larger Sutter Health system. I have an administrative role with my medical group in addition to the clinical work I do at the medical center, although first and foremost I identify myself as a hospitalist. About 5 years ago I took on a role in clinical informatics, when our hospital implemented an EHR. Since then I have been working as an inpatient physician informaticist. Most recently I took on a new role as medical director for onboarding, mentoring, and physician development in my medical group.
How do you balance the different duties of your various roles?
I am full time in my administration role, between my informatics role and my onboarding role. I technically don’t have to do clinical shifts if I don’t want to, but it’s important to me to continue clinical practice and maintain my skills and connection to the hospital and colleagues. I do about four clinical shifts a month, and plan to continue doing that. In our group you must do 14 shifts a month to be considered full time, so what I do could be considered about one-third of that.
What are your favorite areas of clinical practice and/or research?
I haven’t had a lot of research experience. My residency program was a community-based program, and my current setting is a community hospital. I haven’t been involved much in the academic side of hospital medicine. As far as clinical practices goes, I think it’s the diversity of hospital medicine that appeals to me. You really get to be a jack of all trades, and experience all the different disciplines of medicine. I like the variety.
Both my informatics and onboarding roles came out of a need that I identified, and just began doing the work before there was an official role. When we implemented our EHR, it was essential to get our doctors organized to make sure they were ready to take care of patients that first day of go live. By the time our hospital went live on the EHR, I had a good understanding of how it worked, and so I was able to create a miniature curriculum for our physicians – templates, order sets, workflows, etc. – to help ensure everything went smoothly. A few months after we implemented the EHR, I was officially offered a physician informaticist role.
The onboarding role came about in an interesting way. I was participating in the leadership course offered by SHM and was lucky enough to be in the pilot for the Capstone course. That leadership course is focused around mentoring and sponsorship, and one of the faculty members was Nancy Spector, MD, the associate dean of faculty development at Drexel University, Philadelphia. She talked a lot about mentoring, and I was inspired to set up a mentoring program for our hospitalists. Dr. Spector graciously agreed to mentor me as I worked on my Capstone project, which was to create a mentoring program in a community-based hospitalist group. As I continued to work on the project, coincidentally our medical group decided to redesign our new physician onboarding process. Because I was already involved in the onboarding and training related to our EHR, I became very involved with our medical group's onboarding redesign.
My group's CEO decided to create a new directorship role for onboarding and mentoring, which I recently interviewed for and was offered about two months ago.
I think setting up systems to support our doctors is the common threat between the informatics and the onboarding roles. I want to implement systems that support our doctors, help them succeed, and hopefully make their jobs a little easier.
What are the most challenging aspects of practicing hospital medicine? What are the most rewarding?
We practice in a very urban environment, with many low-income patients who have limited resources and access to health care. That can be very challenging. You always wonder if these patients have all the support they need after leaving the hospital. Sometimes I feel that I am just putting a band-aid on the medical problem, so to speak, but not solving the underlying issue. But it can be very rewarding during those times when the hospital and the broader community can bring our resources together to create interventions to help at-risk patients. It doesn’t happen as frequently as we would like, but when it does happen it feels good.
Another challenging aspect is related to perception. There are a lot of consultants in the hospital who view hospitalists as "house staff." That can be very frustrating, and it’s important to steer the conversations away from that perspective, and really try to establish ourselves as colleagues and peers.
How will hospital medicine change in the next decade or 2?
It’s a relatively young field, and we’re still figuring it out. I really don’t know how hospital medicine is going to change, but I do know that the field will continue to evolve, given the way U.S. health care is rapidly changing.
Do you have any advice for students and residents interested in hospital medicine?
It’s a fun way to practice medicine and I would encourage students to go into hospital medicine. It’s great for work/life balance. The advice I would give is that it is very important to get involved early in your career. Get involved in medical group or hospital committees. Stay away from the “shift mentality” – that I’m going to work my shifts and leave. That can lead to early burnout, which is a real concern in our field now. Early engagement is essential, so you can help lead these conversations at your hospital.
Charu Puri, MD, FHM, is a hospitalist and medical informaticist at Sutter East Bay Medical Group in Oakland, Calif. She also serves as medical director for onboarding, mentoring, and physician development.
Dr. Puri has been a member of the Society of Hospital Medicine since 2009, and attended the Society’s Leadership Academy, where she was inspired to create a mentorship program at her own institution. She is a member of the San Francisco Bay chapter of SHM and serves on the Performance Measurement and Reporting Committee.
At what point in your education/training did you decide to practice hospital medicine? What about hospital medicine appealed to you?
It was early on in my residency that it became clear to me that I wanted to pursue the hospitalist track. It was a natural fit, and I gravitated toward the hospitalist side of medicine. What appealed to me most was that we had the opportunity and privilege to provide care to patients in their most vulnerable state and experience the effects of that care in real time. I found that very gratifying.
There is also a sense of community and camaraderie that comes with working in a hospital setting. Everyone is working together, trying to help patients. The collegiality and the relationships that develop are very rewarding. I have been fortunate enough to have built strong friendships with the hospitalists in my group as well as colleagues from other disciplines in medicine that work in the hospital.
What is your current role at Sutter Health?
Alta Bates Summit Medical Center is part of the larger Sutter Health system. I have an administrative role with my medical group in addition to the clinical work I do at the medical center, although first and foremost I identify myself as a hospitalist. About 5 years ago I took on a role in clinical informatics, when our hospital implemented an EHR. Since then I have been working as an inpatient physician informaticist. Most recently I took on a new role as medical director for onboarding, mentoring, and physician development in my medical group.
How do you balance the different duties of your various roles?
I am full time in my administration role, between my informatics role and my onboarding role. I technically don’t have to do clinical shifts if I don’t want to, but it’s important to me to continue clinical practice and maintain my skills and connection to the hospital and colleagues. I do about four clinical shifts a month, and plan to continue doing that. In our group you must do 14 shifts a month to be considered full time, so what I do could be considered about one-third of that.
What are your favorite areas of clinical practice and/or research?
I haven’t had a lot of research experience. My residency program was a community-based program, and my current setting is a community hospital. I haven’t been involved much in the academic side of hospital medicine. As far as clinical practices goes, I think it’s the diversity of hospital medicine that appeals to me. You really get to be a jack of all trades, and experience all the different disciplines of medicine. I like the variety.
Both my informatics and onboarding roles came out of a need that I identified, and just began doing the work before there was an official role. When we implemented our EHR, it was essential to get our doctors organized to make sure they were ready to take care of patients that first day of go live. By the time our hospital went live on the EHR, I had a good understanding of how it worked, and so I was able to create a miniature curriculum for our physicians – templates, order sets, workflows, etc. – to help ensure everything went smoothly. A few months after we implemented the EHR, I was officially offered a physician informaticist role.
The onboarding role came about in an interesting way. I was participating in the leadership course offered by SHM and was lucky enough to be in the pilot for the Capstone course. That leadership course is focused around mentoring and sponsorship, and one of the faculty members was Nancy Spector, MD, the associate dean of faculty development at Drexel University, Philadelphia. She talked a lot about mentoring, and I was inspired to set up a mentoring program for our hospitalists. Dr. Spector graciously agreed to mentor me as I worked on my Capstone project, which was to create a mentoring program in a community-based hospitalist group. As I continued to work on the project, coincidentally our medical group decided to redesign our new physician onboarding process. Because I was already involved in the onboarding and training related to our EHR, I became very involved with our medical group's onboarding redesign.
My group's CEO decided to create a new directorship role for onboarding and mentoring, which I recently interviewed for and was offered about two months ago.
I think setting up systems to support our doctors is the common threat between the informatics and the onboarding roles. I want to implement systems that support our doctors, help them succeed, and hopefully make their jobs a little easier.
What are the most challenging aspects of practicing hospital medicine? What are the most rewarding?
We practice in a very urban environment, with many low-income patients who have limited resources and access to health care. That can be very challenging. You always wonder if these patients have all the support they need after leaving the hospital. Sometimes I feel that I am just putting a band-aid on the medical problem, so to speak, but not solving the underlying issue. But it can be very rewarding during those times when the hospital and the broader community can bring our resources together to create interventions to help at-risk patients. It doesn’t happen as frequently as we would like, but when it does happen it feels good.
Another challenging aspect is related to perception. There are a lot of consultants in the hospital who view hospitalists as "house staff." That can be very frustrating, and it’s important to steer the conversations away from that perspective, and really try to establish ourselves as colleagues and peers.
How will hospital medicine change in the next decade or 2?
It’s a relatively young field, and we’re still figuring it out. I really don’t know how hospital medicine is going to change, but I do know that the field will continue to evolve, given the way U.S. health care is rapidly changing.
Do you have any advice for students and residents interested in hospital medicine?
It’s a fun way to practice medicine and I would encourage students to go into hospital medicine. It’s great for work/life balance. The advice I would give is that it is very important to get involved early in your career. Get involved in medical group or hospital committees. Stay away from the “shift mentality” – that I’m going to work my shifts and leave. That can lead to early burnout, which is a real concern in our field now. Early engagement is essential, so you can help lead these conversations at your hospital.
Charu Puri, MD, FHM, is a hospitalist and medical informaticist at Sutter East Bay Medical Group in Oakland, Calif. She also serves as medical director for onboarding, mentoring, and physician development.
Dr. Puri has been a member of the Society of Hospital Medicine since 2009, and attended the Society’s Leadership Academy, where she was inspired to create a mentorship program at her own institution. She is a member of the San Francisco Bay chapter of SHM and serves on the Performance Measurement and Reporting Committee.
At what point in your education/training did you decide to practice hospital medicine? What about hospital medicine appealed to you?
It was early on in my residency that it became clear to me that I wanted to pursue the hospitalist track. It was a natural fit, and I gravitated toward the hospitalist side of medicine. What appealed to me most was that we had the opportunity and privilege to provide care to patients in their most vulnerable state and experience the effects of that care in real time. I found that very gratifying.
There is also a sense of community and camaraderie that comes with working in a hospital setting. Everyone is working together, trying to help patients. The collegiality and the relationships that develop are very rewarding. I have been fortunate enough to have built strong friendships with the hospitalists in my group as well as colleagues from other disciplines in medicine that work in the hospital.
What is your current role at Sutter Health?
Alta Bates Summit Medical Center is part of the larger Sutter Health system. I have an administrative role with my medical group in addition to the clinical work I do at the medical center, although first and foremost I identify myself as a hospitalist. About 5 years ago I took on a role in clinical informatics, when our hospital implemented an EHR. Since then I have been working as an inpatient physician informaticist. Most recently I took on a new role as medical director for onboarding, mentoring, and physician development in my medical group.
How do you balance the different duties of your various roles?
I am full time in my administration role, between my informatics role and my onboarding role. I technically don’t have to do clinical shifts if I don’t want to, but it’s important to me to continue clinical practice and maintain my skills and connection to the hospital and colleagues. I do about four clinical shifts a month, and plan to continue doing that. In our group you must do 14 shifts a month to be considered full time, so what I do could be considered about one-third of that.
What are your favorite areas of clinical practice and/or research?
I haven’t had a lot of research experience. My residency program was a community-based program, and my current setting is a community hospital. I haven’t been involved much in the academic side of hospital medicine. As far as clinical practices goes, I think it’s the diversity of hospital medicine that appeals to me. You really get to be a jack of all trades, and experience all the different disciplines of medicine. I like the variety.
Both my informatics and onboarding roles came out of a need that I identified, and just began doing the work before there was an official role. When we implemented our EHR, it was essential to get our doctors organized to make sure they were ready to take care of patients that first day of go live. By the time our hospital went live on the EHR, I had a good understanding of how it worked, and so I was able to create a miniature curriculum for our physicians – templates, order sets, workflows, etc. – to help ensure everything went smoothly. A few months after we implemented the EHR, I was officially offered a physician informaticist role.
The onboarding role came about in an interesting way. I was participating in the leadership course offered by SHM and was lucky enough to be in the pilot for the Capstone course. That leadership course is focused around mentoring and sponsorship, and one of the faculty members was Nancy Spector, MD, the associate dean of faculty development at Drexel University, Philadelphia. She talked a lot about mentoring, and I was inspired to set up a mentoring program for our hospitalists. Dr. Spector graciously agreed to mentor me as I worked on my Capstone project, which was to create a mentoring program in a community-based hospitalist group. As I continued to work on the project, coincidentally our medical group decided to redesign our new physician onboarding process. Because I was already involved in the onboarding and training related to our EHR, I became very involved with our medical group's onboarding redesign.
My group's CEO decided to create a new directorship role for onboarding and mentoring, which I recently interviewed for and was offered about two months ago.
I think setting up systems to support our doctors is the common threat between the informatics and the onboarding roles. I want to implement systems that support our doctors, help them succeed, and hopefully make their jobs a little easier.
What are the most challenging aspects of practicing hospital medicine? What are the most rewarding?
We practice in a very urban environment, with many low-income patients who have limited resources and access to health care. That can be very challenging. You always wonder if these patients have all the support they need after leaving the hospital. Sometimes I feel that I am just putting a band-aid on the medical problem, so to speak, but not solving the underlying issue. But it can be very rewarding during those times when the hospital and the broader community can bring our resources together to create interventions to help at-risk patients. It doesn’t happen as frequently as we would like, but when it does happen it feels good.
Another challenging aspect is related to perception. There are a lot of consultants in the hospital who view hospitalists as "house staff." That can be very frustrating, and it’s important to steer the conversations away from that perspective, and really try to establish ourselves as colleagues and peers.
How will hospital medicine change in the next decade or 2?
It’s a relatively young field, and we’re still figuring it out. I really don’t know how hospital medicine is going to change, but I do know that the field will continue to evolve, given the way U.S. health care is rapidly changing.
Do you have any advice for students and residents interested in hospital medicine?
It’s a fun way to practice medicine and I would encourage students to go into hospital medicine. It’s great for work/life balance. The advice I would give is that it is very important to get involved early in your career. Get involved in medical group or hospital committees. Stay away from the “shift mentality” – that I’m going to work my shifts and leave. That can lead to early burnout, which is a real concern in our field now. Early engagement is essential, so you can help lead these conversations at your hospital.
HM20 course director influenced by POCUS, global health
Dr. Benji Mathews praises mentors for his SHM roles
Benji K. Mathews, MD, SFHM, CLHM, is chief of hospital medicine at Regions Hospital in St. Paul, Minn., and director of point of care ultrasound (POCUS) for hospital medicine at HealthPartners. He is also the course director for the Society of Hospital Medicine’s 2020 Annual Conference (HM20), to be held April 16-18 in San Diego.
Dr. Mathews, an associate professor of medicine at the University of Minnesota, Minneapolis, is recognized by fellow hospitalists as a pioneer in the use of bedside ultrasound. In fact, his Certificate of Leadership in Hospital Medicine (CLHM) was completed with a focus on ultrasound in hospital medicine, and he is a Fellow in Diagnostic Safety through the Society to Improve Diagnosis in Medicine. “While a resident, I took an interest in the field of improving diagnosis and combined it with the 21st-century innovative tool of bedside ultrasound,” he said. “Now, I continue to teach clinicians, educators, and learners.”
In addition to his interest in POCUS and medical education, Dr. Mathews also has a passion for global health, rooted in a commitment to reducing health care disparities both locally and globally. He has worked with medical missions, nongovernmental organizations, and orphanages in Nepal, India, Bolivia, Honduras, and Costa Rica. This led him to complete the global health course at the University of Minnesota.
Dr. Mathews spent a few minutes with The Hospitalist to discuss his background and his new role of course director of the HM20 Annual Conference.
Can you describe your journey to becoming a hospitalist?
I’ve been a hospitalist for most of the last decade. I was fortunate to be a part of a great residency program at the University of Minnesota Medical School, which started a hospital medicine pathway that had several nationally recognized hospital medicine leaders as mentors. I was lucky to work with several of them through the HealthPartners organization in Saint Paul, and that developed in me a further desire to practice hospital medicine. The group and mentors provided opportunities to develop further niches in my practice, like bedside ultrasound.
How did you first get involved with SHM?
I entered SHM through the influence of mentors at HealthPartners, especially Burke Kealey, MD, SFHM, senior medical director for hospital specialties at HealthPartners Medical Group in Bloomington, Minn. and a past president of the Society, who encouraged me to participate on SHM committees. I eventually applied for the Annual Conference Committee, and somehow was accepted.
At that time, I was a community hospitalist among a lot of academic hospitalists. I thought that my voice could probably diversify the conversation, and bring the perspective of an early-career hospitalist to the discussion around educational offerings at the Annual Conference. I benefited from good mentorship on that committee, and with that experience I started getting involved with our local chapter in Minnesota. That was very important. I became our local chapter president and was able to combine my efforts with SHM nationally with our regional initiatives.
You have a particular interest in point-of-care ultrasound for hospitalists. How did that make its way into your involvement with SHM?
Point-of-care ultrasound and diagnostic error work really took off when I was a resident. My interest in that funneled naturally into the base curriculum of the Annual Conference, where once a year I could come together with 18 of my best hospitalist friends from across the nation to discuss curriculum. We talk about what content is applicable for frontline clinicians, what is right for early learners, and what innovations are coming in the future. Toward that last point, I was always involved as a judge or volunteer for the Research, Innovations and Clinical Vignettes – or RIV – competition at the Annual Conference. That’s the scientific abstract and poster competition at the conference. My interest grew to a point at which I decided to apply for one of the leadership roles in the RIV. I had the opportunity to serve as an Innovations Lead at RIV one year, and then chaired the overall RIV competition. Those opportunities helped me better understand the cutting-edge research that hospitalists should be aware of and which researchers and clinicians we should be in conversation with.
All these roles together have led me to my service as HM20 course director. I see myself as a lucky guy who has benefited from great mentorship, and I want to take advantage of my opportunities to serve.
We’ve been told that your elementary school–age children have learned to use ultrasound!
Well, they’ve learned how to use handheld ultrasound devices on each other. They’re able to find their siblings’ kidneys and hearts. I often show an image of this to encourage hospitalists that, if children can pick it up, highly educated providers can do the same and more.
To register for the Society of Hospital Medicine’s 2020 Annual Conference, please visit the HM20 Registration page.
Dr. Benji Mathews praises mentors for his SHM roles
Dr. Benji Mathews praises mentors for his SHM roles
Benji K. Mathews, MD, SFHM, CLHM, is chief of hospital medicine at Regions Hospital in St. Paul, Minn., and director of point of care ultrasound (POCUS) for hospital medicine at HealthPartners. He is also the course director for the Society of Hospital Medicine’s 2020 Annual Conference (HM20), to be held April 16-18 in San Diego.
Dr. Mathews, an associate professor of medicine at the University of Minnesota, Minneapolis, is recognized by fellow hospitalists as a pioneer in the use of bedside ultrasound. In fact, his Certificate of Leadership in Hospital Medicine (CLHM) was completed with a focus on ultrasound in hospital medicine, and he is a Fellow in Diagnostic Safety through the Society to Improve Diagnosis in Medicine. “While a resident, I took an interest in the field of improving diagnosis and combined it with the 21st-century innovative tool of bedside ultrasound,” he said. “Now, I continue to teach clinicians, educators, and learners.”
In addition to his interest in POCUS and medical education, Dr. Mathews also has a passion for global health, rooted in a commitment to reducing health care disparities both locally and globally. He has worked with medical missions, nongovernmental organizations, and orphanages in Nepal, India, Bolivia, Honduras, and Costa Rica. This led him to complete the global health course at the University of Minnesota.
Dr. Mathews spent a few minutes with The Hospitalist to discuss his background and his new role of course director of the HM20 Annual Conference.
Can you describe your journey to becoming a hospitalist?
I’ve been a hospitalist for most of the last decade. I was fortunate to be a part of a great residency program at the University of Minnesota Medical School, which started a hospital medicine pathway that had several nationally recognized hospital medicine leaders as mentors. I was lucky to work with several of them through the HealthPartners organization in Saint Paul, and that developed in me a further desire to practice hospital medicine. The group and mentors provided opportunities to develop further niches in my practice, like bedside ultrasound.
How did you first get involved with SHM?
I entered SHM through the influence of mentors at HealthPartners, especially Burke Kealey, MD, SFHM, senior medical director for hospital specialties at HealthPartners Medical Group in Bloomington, Minn. and a past president of the Society, who encouraged me to participate on SHM committees. I eventually applied for the Annual Conference Committee, and somehow was accepted.
At that time, I was a community hospitalist among a lot of academic hospitalists. I thought that my voice could probably diversify the conversation, and bring the perspective of an early-career hospitalist to the discussion around educational offerings at the Annual Conference. I benefited from good mentorship on that committee, and with that experience I started getting involved with our local chapter in Minnesota. That was very important. I became our local chapter president and was able to combine my efforts with SHM nationally with our regional initiatives.
You have a particular interest in point-of-care ultrasound for hospitalists. How did that make its way into your involvement with SHM?
Point-of-care ultrasound and diagnostic error work really took off when I was a resident. My interest in that funneled naturally into the base curriculum of the Annual Conference, where once a year I could come together with 18 of my best hospitalist friends from across the nation to discuss curriculum. We talk about what content is applicable for frontline clinicians, what is right for early learners, and what innovations are coming in the future. Toward that last point, I was always involved as a judge or volunteer for the Research, Innovations and Clinical Vignettes – or RIV – competition at the Annual Conference. That’s the scientific abstract and poster competition at the conference. My interest grew to a point at which I decided to apply for one of the leadership roles in the RIV. I had the opportunity to serve as an Innovations Lead at RIV one year, and then chaired the overall RIV competition. Those opportunities helped me better understand the cutting-edge research that hospitalists should be aware of and which researchers and clinicians we should be in conversation with.
All these roles together have led me to my service as HM20 course director. I see myself as a lucky guy who has benefited from great mentorship, and I want to take advantage of my opportunities to serve.
We’ve been told that your elementary school–age children have learned to use ultrasound!
Well, they’ve learned how to use handheld ultrasound devices on each other. They’re able to find their siblings’ kidneys and hearts. I often show an image of this to encourage hospitalists that, if children can pick it up, highly educated providers can do the same and more.
To register for the Society of Hospital Medicine’s 2020 Annual Conference, please visit the HM20 Registration page.
Benji K. Mathews, MD, SFHM, CLHM, is chief of hospital medicine at Regions Hospital in St. Paul, Minn., and director of point of care ultrasound (POCUS) for hospital medicine at HealthPartners. He is also the course director for the Society of Hospital Medicine’s 2020 Annual Conference (HM20), to be held April 16-18 in San Diego.
Dr. Mathews, an associate professor of medicine at the University of Minnesota, Minneapolis, is recognized by fellow hospitalists as a pioneer in the use of bedside ultrasound. In fact, his Certificate of Leadership in Hospital Medicine (CLHM) was completed with a focus on ultrasound in hospital medicine, and he is a Fellow in Diagnostic Safety through the Society to Improve Diagnosis in Medicine. “While a resident, I took an interest in the field of improving diagnosis and combined it with the 21st-century innovative tool of bedside ultrasound,” he said. “Now, I continue to teach clinicians, educators, and learners.”
In addition to his interest in POCUS and medical education, Dr. Mathews also has a passion for global health, rooted in a commitment to reducing health care disparities both locally and globally. He has worked with medical missions, nongovernmental organizations, and orphanages in Nepal, India, Bolivia, Honduras, and Costa Rica. This led him to complete the global health course at the University of Minnesota.
Dr. Mathews spent a few minutes with The Hospitalist to discuss his background and his new role of course director of the HM20 Annual Conference.
Can you describe your journey to becoming a hospitalist?
I’ve been a hospitalist for most of the last decade. I was fortunate to be a part of a great residency program at the University of Minnesota Medical School, which started a hospital medicine pathway that had several nationally recognized hospital medicine leaders as mentors. I was lucky to work with several of them through the HealthPartners organization in Saint Paul, and that developed in me a further desire to practice hospital medicine. The group and mentors provided opportunities to develop further niches in my practice, like bedside ultrasound.
How did you first get involved with SHM?
I entered SHM through the influence of mentors at HealthPartners, especially Burke Kealey, MD, SFHM, senior medical director for hospital specialties at HealthPartners Medical Group in Bloomington, Minn. and a past president of the Society, who encouraged me to participate on SHM committees. I eventually applied for the Annual Conference Committee, and somehow was accepted.
At that time, I was a community hospitalist among a lot of academic hospitalists. I thought that my voice could probably diversify the conversation, and bring the perspective of an early-career hospitalist to the discussion around educational offerings at the Annual Conference. I benefited from good mentorship on that committee, and with that experience I started getting involved with our local chapter in Minnesota. That was very important. I became our local chapter president and was able to combine my efforts with SHM nationally with our regional initiatives.
You have a particular interest in point-of-care ultrasound for hospitalists. How did that make its way into your involvement with SHM?
Point-of-care ultrasound and diagnostic error work really took off when I was a resident. My interest in that funneled naturally into the base curriculum of the Annual Conference, where once a year I could come together with 18 of my best hospitalist friends from across the nation to discuss curriculum. We talk about what content is applicable for frontline clinicians, what is right for early learners, and what innovations are coming in the future. Toward that last point, I was always involved as a judge or volunteer for the Research, Innovations and Clinical Vignettes – or RIV – competition at the Annual Conference. That’s the scientific abstract and poster competition at the conference. My interest grew to a point at which I decided to apply for one of the leadership roles in the RIV. I had the opportunity to serve as an Innovations Lead at RIV one year, and then chaired the overall RIV competition. Those opportunities helped me better understand the cutting-edge research that hospitalists should be aware of and which researchers and clinicians we should be in conversation with.
All these roles together have led me to my service as HM20 course director. I see myself as a lucky guy who has benefited from great mentorship, and I want to take advantage of my opportunities to serve.
We’ve been told that your elementary school–age children have learned to use ultrasound!
Well, they’ve learned how to use handheld ultrasound devices on each other. They’re able to find their siblings’ kidneys and hearts. I often show an image of this to encourage hospitalists that, if children can pick it up, highly educated providers can do the same and more.
To register for the Society of Hospital Medicine’s 2020 Annual Conference, please visit the HM20 Registration page.