User login
AI Algorithm Predicts Transfusion Need, Mortality Risk in Acute GI Bleeds
SAN DIEGO — , researchers reported at Digestive Disease Week® (DDW) 2025.
Acute GI bleeding is the most common cause of digestive disease–related hospitalization, with an estimated 500,000 hospital admissions annually. It’s known that predicting the need for red blood cell transfusion in the first 24 hours may improve resuscitation and decrease both morbidity and mortality.
However, an existing clinical score known as the Rockall Score does not perform well for predicting mortality, Xi (Nicole) Zhang, an MD-PhD student at McGill University, Montreal, Quebec, Canada, told attendees at DDW. With an area under the curve of 0.65-0.75, better prediction is needed, said Zhang, whose coresearchers included Dennis Shung, MD, MHS, PhD, director of Applied Artificial Intelligence at Yale University School of Medicine, New Haven, Connecticut.
“We’d like to predict multiple outcomes in addition to mortality,” said Zhang, who is also a student at the Mila-Quebec Artificial Intelligence Institute.
As a result, the researchers turned to the TFM approach, applying it to ICU patients with acute GI bleeding to predict both the need for transfusion and in-hospital mortality risk. The all-cause mortality rate is up to 11%, according to a 2020 study by James Y. W. Lau, MD, and colleagues. The rebleeding rate of nonvariceal upper GI bleeds is up to 10.4%. Zhang said the rebleeding rate for variceal upper gastrointestinal bleeding is up to 65%.
The AI method the researchers used outperformed a standard deep learning model at predicting the need for transfusion and estimating mortality risk.
Defining the AI Framework
“Probabilistic flow matching is a class of generative artificial intelligence that learns how a simple distribution becomes a more complex distribution with ordinary differential equations,” Zhang told GI & Hepatology News. “For example, if you had a few lines and shapes you could learn how it could become a detailed portrait of a face. In our case, we start with a few blood pressure and heart rate measurements and learn the pattern of blood pressures and heart rates over time, particularly if they reflect clinical deterioration with hemodynamic instability.”
Another way to think about the underlying algorithm, Zhang said, is to think about a river with boats where the river flow determines where the boats end up. “We are trying to direct the boat to the correct dock by adjusting the flow of water in the canal. In this case we are mapping the distribution with the first few data points to the distribution with the entire patient trajectory.”
The information gained, she said, could be helpful in timing endoscopic evaluation or allocating red blood cell products for emergent transfusion.
Study Details
The researchers evaluated a cohort of 2602 patients admitted to the ICU, identified from the publicly available MIMIC-III database. They divided the patients into a training set of 2342 patients and an internal validation set of 260 patients. Input variables were severe liver disease comorbidity, administration of vasopressor medications, mean arterial blood pressure, and heart rate over the first 24 hours.
Excluded was hemoglobin, since the point was to test the trajectory of hemodynamic parameters independent of hemoglobin thresholds used to guide red blood cell transfusion.
The outcome measures were administration of packed red blood cell transfusion within 24 hours and all-cause hospital mortality.
The TFM was more accurate than a standard deep learning model in predicting red blood cell transfusion, with an accuracy of 93.6% vs 43.2%; P ≤ .001. It was also more accurate at predicting all-cause in-hospital mortality, with an accuracy of 89.5% vs 42.5%, P = .01.
The researchers concluded that the TFM approach was able to predict the hemodynamic trajectories of patients with acute GI bleeding defined as deviation and outperformed the baseline from the measured mean arterial pressure and heart rate.
Expert Perspective
“This is an exciting proof-of-concept study that shows generative AI methods may be applied to complex datasets in order to improve on our current predictive models and improve patient care,” said Jeremy Glissen Brown, MD, MSc, an assistant professor of medicine and a practicing gastroenterologist at Duke University who has published research on the use of AI in clinical practice. He reviewed the study for GI & Hepatology News but was not involved in the research.
“Future work will likely look into the implementation of a version of this model on real-time data.” he said. “We are at an exciting inflection point in predictive models within GI and clinical medicine. Predictive models based on deep learning and generative AI hold the promise of improving how we predict and treat disease states, but the excitement being generated with studies such as this needs to be balanced with the trade-offs inherent to the current paradigm of deep learning and generative models compared to more traditional regression-based models. These include many of the same ‘black box’ explainability questions that have risen in the age of convolutional neural networks as well as some method-specific questions due to the continuous and implicit nature of TFM.”
Elaborating on that, Glissen Brown said: “TFM, like many deep learning techniques, raises concerns about explainability that we’ve long seen with convolutional neural networks — the ‘black box’ problem, where it’s difficult to interpret exactly how and why the model arrives at a particular decision. But TFM also introduces unique challenges due to its continuous and implicit formulation. Since it often learns flows without explicitly defining intermediate representations or steps, it can be harder to trace the logic or pathways it uses to connect inputs to outputs. This makes standard interpretability tools less effective and calls for new techniques tailored to these continuous architectures.”
“This approach could have a real clinical impact,” said Robert Hirten, MD, associate professor of medicine and artificial intelligence, Icahn School of Medicine at Mount Sinai, New York City, who also reviewed the study. “Accurately predicting transfusion needs and mortality risk in real time could support earlier, more targeted interventions for high-risk patients. While these findings still need to be validated in prospective studies, it could enhance ICU decision-making and resource allocation.”
“For the practicing gastroenterologist, we envision this system could help them figure out when to perform endoscopy in a patient admitted with acute gastrointestinal bleeding in the ICU at very high risk of exsanguination,” Zhang told GI & Hepatology News.
The approach, the researchers said, will be useful in identifying unique patient characteristics, make possible the identification of high-risk patients and lead to more personalized medicine.
Hirten, Zhang, and Shung had no disclosures. Glissen Brown reported consulting relationships with Medtronic, OdinVision, Doximity, and Olympus. The National Institutes of Health funded this study.
A version of this article appeared on Medscape.com.
SAN DIEGO — , researchers reported at Digestive Disease Week® (DDW) 2025.
Acute GI bleeding is the most common cause of digestive disease–related hospitalization, with an estimated 500,000 hospital admissions annually. It’s known that predicting the need for red blood cell transfusion in the first 24 hours may improve resuscitation and decrease both morbidity and mortality.
However, an existing clinical score known as the Rockall Score does not perform well for predicting mortality, Xi (Nicole) Zhang, an MD-PhD student at McGill University, Montreal, Quebec, Canada, told attendees at DDW. With an area under the curve of 0.65-0.75, better prediction is needed, said Zhang, whose coresearchers included Dennis Shung, MD, MHS, PhD, director of Applied Artificial Intelligence at Yale University School of Medicine, New Haven, Connecticut.
“We’d like to predict multiple outcomes in addition to mortality,” said Zhang, who is also a student at the Mila-Quebec Artificial Intelligence Institute.
As a result, the researchers turned to the TFM approach, applying it to ICU patients with acute GI bleeding to predict both the need for transfusion and in-hospital mortality risk. The all-cause mortality rate is up to 11%, according to a 2020 study by James Y. W. Lau, MD, and colleagues. The rebleeding rate of nonvariceal upper GI bleeds is up to 10.4%. Zhang said the rebleeding rate for variceal upper gastrointestinal bleeding is up to 65%.
The AI method the researchers used outperformed a standard deep learning model at predicting the need for transfusion and estimating mortality risk.
Defining the AI Framework
“Probabilistic flow matching is a class of generative artificial intelligence that learns how a simple distribution becomes a more complex distribution with ordinary differential equations,” Zhang told GI & Hepatology News. “For example, if you had a few lines and shapes you could learn how it could become a detailed portrait of a face. In our case, we start with a few blood pressure and heart rate measurements and learn the pattern of blood pressures and heart rates over time, particularly if they reflect clinical deterioration with hemodynamic instability.”
Another way to think about the underlying algorithm, Zhang said, is to think about a river with boats where the river flow determines where the boats end up. “We are trying to direct the boat to the correct dock by adjusting the flow of water in the canal. In this case we are mapping the distribution with the first few data points to the distribution with the entire patient trajectory.”
The information gained, she said, could be helpful in timing endoscopic evaluation or allocating red blood cell products for emergent transfusion.
Study Details
The researchers evaluated a cohort of 2602 patients admitted to the ICU, identified from the publicly available MIMIC-III database. They divided the patients into a training set of 2342 patients and an internal validation set of 260 patients. Input variables were severe liver disease comorbidity, administration of vasopressor medications, mean arterial blood pressure, and heart rate over the first 24 hours.
Excluded was hemoglobin, since the point was to test the trajectory of hemodynamic parameters independent of hemoglobin thresholds used to guide red blood cell transfusion.
The outcome measures were administration of packed red blood cell transfusion within 24 hours and all-cause hospital mortality.
The TFM was more accurate than a standard deep learning model in predicting red blood cell transfusion, with an accuracy of 93.6% vs 43.2%; P ≤ .001. It was also more accurate at predicting all-cause in-hospital mortality, with an accuracy of 89.5% vs 42.5%, P = .01.
The researchers concluded that the TFM approach was able to predict the hemodynamic trajectories of patients with acute GI bleeding defined as deviation and outperformed the baseline from the measured mean arterial pressure and heart rate.
Expert Perspective
“This is an exciting proof-of-concept study that shows generative AI methods may be applied to complex datasets in order to improve on our current predictive models and improve patient care,” said Jeremy Glissen Brown, MD, MSc, an assistant professor of medicine and a practicing gastroenterologist at Duke University who has published research on the use of AI in clinical practice. He reviewed the study for GI & Hepatology News but was not involved in the research.
“Future work will likely look into the implementation of a version of this model on real-time data.” he said. “We are at an exciting inflection point in predictive models within GI and clinical medicine. Predictive models based on deep learning and generative AI hold the promise of improving how we predict and treat disease states, but the excitement being generated with studies such as this needs to be balanced with the trade-offs inherent to the current paradigm of deep learning and generative models compared to more traditional regression-based models. These include many of the same ‘black box’ explainability questions that have risen in the age of convolutional neural networks as well as some method-specific questions due to the continuous and implicit nature of TFM.”
Elaborating on that, Glissen Brown said: “TFM, like many deep learning techniques, raises concerns about explainability that we’ve long seen with convolutional neural networks — the ‘black box’ problem, where it’s difficult to interpret exactly how and why the model arrives at a particular decision. But TFM also introduces unique challenges due to its continuous and implicit formulation. Since it often learns flows without explicitly defining intermediate representations or steps, it can be harder to trace the logic or pathways it uses to connect inputs to outputs. This makes standard interpretability tools less effective and calls for new techniques tailored to these continuous architectures.”
“This approach could have a real clinical impact,” said Robert Hirten, MD, associate professor of medicine and artificial intelligence, Icahn School of Medicine at Mount Sinai, New York City, who also reviewed the study. “Accurately predicting transfusion needs and mortality risk in real time could support earlier, more targeted interventions for high-risk patients. While these findings still need to be validated in prospective studies, it could enhance ICU decision-making and resource allocation.”
“For the practicing gastroenterologist, we envision this system could help them figure out when to perform endoscopy in a patient admitted with acute gastrointestinal bleeding in the ICU at very high risk of exsanguination,” Zhang told GI & Hepatology News.
The approach, the researchers said, will be useful in identifying unique patient characteristics, make possible the identification of high-risk patients and lead to more personalized medicine.
Hirten, Zhang, and Shung had no disclosures. Glissen Brown reported consulting relationships with Medtronic, OdinVision, Doximity, and Olympus. The National Institutes of Health funded this study.
A version of this article appeared on Medscape.com.
SAN DIEGO — , researchers reported at Digestive Disease Week® (DDW) 2025.
Acute GI bleeding is the most common cause of digestive disease–related hospitalization, with an estimated 500,000 hospital admissions annually. It’s known that predicting the need for red blood cell transfusion in the first 24 hours may improve resuscitation and decrease both morbidity and mortality.
However, an existing clinical score known as the Rockall Score does not perform well for predicting mortality, Xi (Nicole) Zhang, an MD-PhD student at McGill University, Montreal, Quebec, Canada, told attendees at DDW. With an area under the curve of 0.65-0.75, better prediction is needed, said Zhang, whose coresearchers included Dennis Shung, MD, MHS, PhD, director of Applied Artificial Intelligence at Yale University School of Medicine, New Haven, Connecticut.
“We’d like to predict multiple outcomes in addition to mortality,” said Zhang, who is also a student at the Mila-Quebec Artificial Intelligence Institute.
As a result, the researchers turned to the TFM approach, applying it to ICU patients with acute GI bleeding to predict both the need for transfusion and in-hospital mortality risk. The all-cause mortality rate is up to 11%, according to a 2020 study by James Y. W. Lau, MD, and colleagues. The rebleeding rate of nonvariceal upper GI bleeds is up to 10.4%. Zhang said the rebleeding rate for variceal upper gastrointestinal bleeding is up to 65%.
The AI method the researchers used outperformed a standard deep learning model at predicting the need for transfusion and estimating mortality risk.
Defining the AI Framework
“Probabilistic flow matching is a class of generative artificial intelligence that learns how a simple distribution becomes a more complex distribution with ordinary differential equations,” Zhang told GI & Hepatology News. “For example, if you had a few lines and shapes you could learn how it could become a detailed portrait of a face. In our case, we start with a few blood pressure and heart rate measurements and learn the pattern of blood pressures and heart rates over time, particularly if they reflect clinical deterioration with hemodynamic instability.”
Another way to think about the underlying algorithm, Zhang said, is to think about a river with boats where the river flow determines where the boats end up. “We are trying to direct the boat to the correct dock by adjusting the flow of water in the canal. In this case we are mapping the distribution with the first few data points to the distribution with the entire patient trajectory.”
The information gained, she said, could be helpful in timing endoscopic evaluation or allocating red blood cell products for emergent transfusion.
Study Details
The researchers evaluated a cohort of 2602 patients admitted to the ICU, identified from the publicly available MIMIC-III database. They divided the patients into a training set of 2342 patients and an internal validation set of 260 patients. Input variables were severe liver disease comorbidity, administration of vasopressor medications, mean arterial blood pressure, and heart rate over the first 24 hours.
Excluded was hemoglobin, since the point was to test the trajectory of hemodynamic parameters independent of hemoglobin thresholds used to guide red blood cell transfusion.
The outcome measures were administration of packed red blood cell transfusion within 24 hours and all-cause hospital mortality.
The TFM was more accurate than a standard deep learning model in predicting red blood cell transfusion, with an accuracy of 93.6% vs 43.2%; P ≤ .001. It was also more accurate at predicting all-cause in-hospital mortality, with an accuracy of 89.5% vs 42.5%, P = .01.
The researchers concluded that the TFM approach was able to predict the hemodynamic trajectories of patients with acute GI bleeding defined as deviation and outperformed the baseline from the measured mean arterial pressure and heart rate.
Expert Perspective
“This is an exciting proof-of-concept study that shows generative AI methods may be applied to complex datasets in order to improve on our current predictive models and improve patient care,” said Jeremy Glissen Brown, MD, MSc, an assistant professor of medicine and a practicing gastroenterologist at Duke University who has published research on the use of AI in clinical practice. He reviewed the study for GI & Hepatology News but was not involved in the research.
“Future work will likely look into the implementation of a version of this model on real-time data.” he said. “We are at an exciting inflection point in predictive models within GI and clinical medicine. Predictive models based on deep learning and generative AI hold the promise of improving how we predict and treat disease states, but the excitement being generated with studies such as this needs to be balanced with the trade-offs inherent to the current paradigm of deep learning and generative models compared to more traditional regression-based models. These include many of the same ‘black box’ explainability questions that have risen in the age of convolutional neural networks as well as some method-specific questions due to the continuous and implicit nature of TFM.”
Elaborating on that, Glissen Brown said: “TFM, like many deep learning techniques, raises concerns about explainability that we’ve long seen with convolutional neural networks — the ‘black box’ problem, where it’s difficult to interpret exactly how and why the model arrives at a particular decision. But TFM also introduces unique challenges due to its continuous and implicit formulation. Since it often learns flows without explicitly defining intermediate representations or steps, it can be harder to trace the logic or pathways it uses to connect inputs to outputs. This makes standard interpretability tools less effective and calls for new techniques tailored to these continuous architectures.”
“This approach could have a real clinical impact,” said Robert Hirten, MD, associate professor of medicine and artificial intelligence, Icahn School of Medicine at Mount Sinai, New York City, who also reviewed the study. “Accurately predicting transfusion needs and mortality risk in real time could support earlier, more targeted interventions for high-risk patients. While these findings still need to be validated in prospective studies, it could enhance ICU decision-making and resource allocation.”
“For the practicing gastroenterologist, we envision this system could help them figure out when to perform endoscopy in a patient admitted with acute gastrointestinal bleeding in the ICU at very high risk of exsanguination,” Zhang told GI & Hepatology News.
The approach, the researchers said, will be useful in identifying unique patient characteristics, make possible the identification of high-risk patients and lead to more personalized medicine.
Hirten, Zhang, and Shung had no disclosures. Glissen Brown reported consulting relationships with Medtronic, OdinVision, Doximity, and Olympus. The National Institutes of Health funded this study.
A version of this article appeared on Medscape.com.
FROM DDW 2025
Ostomy Innovation Grabs ‘Shark Tank’ Win
The “Shark Tank” winning innovation at the American Gastroenterological Association (AGA) Tech Summit in Chicago this April has “life-altering” potential for ostomy patients, according to one of the judges, and eliminates the need for constant pouch wear.
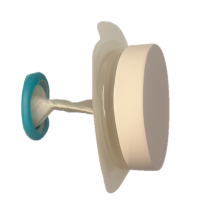
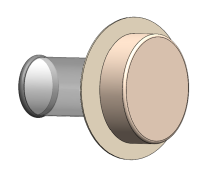
The innovation is called Twistomy and it is designed to replace current ostomy-pouch systems that can cause leaks, odor, skin irritation, embarrassment, and social and emotional distress. The AGA Committee for GI Innovation and Technology (CGIT) organizes the annual Tech Summit.
Twistomy’s winning design includes a flexible ring and sleeve, which are inserted into the stoma and secured on the outside with a set of rings that make up the housing unit attached to a standard wafer. The housing unit twists the sleeve closed, allowing the user to control fecal output. For evacuation, the user attaches a pouch, untwists the sleeve, evacuates cleanly and effectively, and then discards the pouch.
Twistomy cofounders Devon Horton, BS, senior bioengineer, and Lily Williams, BS, biomedical researcher and engineer, both work for the department of surgery at University of Colorado, Denver.
Horton said in an interview that when he was approached with the idea to create a better ostomy solution for a senior-year capstone project he was intrigued because the traditional ostomy system “has not changed in more than 70 years. It was crazy that no one had done anything to change that.”
The Twistomy team also won the Grand Prize this spring at the Emerging Medical Innovation Valuation Competition at the Design of Medical Devices Conference held at the University of Minnesota, Minneapolis.
Witnessing the Struggle as a CNA
Horton also works as a certified nursing assistant at an inpatient unit at University of Colorado Hospital and the ostomy patients he sees there every shift help drive his passion to find a better solution.
He hears the emotional stories of people who manage their ostomy daily.
“Many express feelings of depression and anxiety, feeling isolated with their severe inability to go out and do things because of the fear of the noise the stoma makes, or the crinkling of the plastic bag in a yoga class,” he said. “We want to help them regain that control of quality of life.”
They also hope to cut down on the ostomy management time. “Initial user testing [for Twistomy] was less than 75 seconds to insert and assemble,” he said. “I did an interview with a patient yesterday who said they probably spend an hour a day managing their ostomy,” including cleaning and replacing.
Horton and Williams have a patent on the device and currently use three-dimensional printing for the prototypes.
Williams said they are now conducting consumer discovery studies through the National Science Foundation and are interviewing 30 stakeholders — “anyone who has a relationship with an ostomy,” whether a colorectal surgeon, a gastrointestinal nurse, ostomy patients, or insurers.
Those interviews will help in refining the device so they can start consulting with manufacturers and work toward approval as a Class II medical device from the US Food and Drug Administration (FDA), Williams said.
Saving Healthcare Costs
Another potential benefit for Twistomy is its ability to cut healthcare costs, Horton said. Traditional ostomies are prone to leakage, which can lead to peristomal skin complications.
He pointed to a National Institutes of Health analysis that found that on average peristomal skin complications caused upwards of $80,000 more per ostomy patient in increased healthcare costs over a 3-month period than for those without the complications.
“With Twistomy, we are reducing leakage most likely to zero,” Horton said. “We set out to say if we could reduce [infections] by half or a little less than half, we can cut out those tens of thousands of dollars that insurance companies and payers are spending.”
Permanent and Temporary Ostomy Markets
He pointed out that not all ostomies are permanent ostomies, adding that the reversal rate “is about 65%.” Often those reversal surgeries cannot take place until peristomal skin complications have been healed.
“We’re not only hoping to market to the permanent stoma patients, but the patients with temporary stomas as well,” he said.
The team estimates it will need $4 million–$6 million in funding for manufacturing and consultation costs as well as costs involved in seeking FDA approval.
Horton and Williams project the housing unit cost will be $399 based on known out-of-pocket expenses for patients with ostomy care products and the unit would be replaced annually. Disposable elements would be an additional cost.
Assuming insurance acceptance of the product, he said, “With about an 80/20 insurance coverage, typical for many patients, it would be about $100 in out-of-pocket expenses per month to use our device, which is around the lower end of what a lot of patients are spending out of pocket.”
One of the Tech Summit judges, Somaya Albhaisi, MD, a gastroenterology/hepatology fellow at University of Southern California, Los Angeles, said in an interview that the Shark Tank results were unanimous among the five judges and Twistomy also took the fan favorite vote.
She said the teams were judged on quality of pitch, potential clinical impact, and feasibility of business plan. Teams got 5-7 minutes to pitch and answered questions afterward.
“Deep Understanding” of Patient Need
“They combined smart engineering with deep understanding of patient need, which is restoring control, dignity, and quality of life for ostomy users while also reducing healthcare costs. It is rare to see a solution this scalable and impactful. It was a deeply empathetic solution overall.” She noted that nearly 1 million people in the United States currently use an ostomy.
Ostomy users’ quality of life is compromised, and they often have mental health challenges, Albhaisi said. This innovation appears to offer easy use, more dignity and control.
The other four Shark Tank finalists were:
- AI Lumen, which developed a retroview camera system, which attaches to the colonoscope and enhances imaging to detect hidden polyps that may evade conventional endoscopes.
- Amplified Sciences, which developed an ultrasensitive diagnostic platform that detects biomarker activities in minute volumes of fluid from pancreatic cystic lesions, helping to stratify patients into low risk or potential malignancy, reducing unneeded surgeries, costs, and comorbidities.
- KITE Endoscopic Innovations, which designed the Dynaflex TruCut needle to offer a simpler endoscopic ultrasound (EUS)–guided biopsy procedure with fewer needle passes, deeper insights into tumor pathology, and more tissue for geonomic analysis.
- MicroSteer, which designed a device to facilitate semiautomated endoscopic submucosal dissection (ESD) by decoupling the dissecting knife from the endoscope, enhancing safety and effectiveness during the procedure.
The Twistomy Team “Surprised Everyone”
The competitors’ scores were “very close,” one of the judges, Kevin Berliner, said in an interview. “The Twistomy team surprised everyone — the judges and the crowd — with their succinct, informative, and impactful pitch. That presentation disparity was the tiebreaker for me,” said Berliner, who works for Medtronic, a sponsor of the competition, in Chicago.
He said Horton and Williams were the youngest presenters and had the earliest stage pitch they judged, but they “outpresented other competitors in clarity, simplification, and storytelling.”
Also impressive was their description of their “commercially viable path to success” and their plan for the challenges ahead, he said.
Those challenges to get Twistomy to market center “on the ongoing changing climate we have with research funds lately,” Horton said. “We’re giving it an estimate of 3-5 years.”
Horton, Williams, Albhaisi, and Berliner reported no relevant financial relationships.
The “Shark Tank” winning innovation at the American Gastroenterological Association (AGA) Tech Summit in Chicago this April has “life-altering” potential for ostomy patients, according to one of the judges, and eliminates the need for constant pouch wear.
The innovation is called Twistomy and it is designed to replace current ostomy-pouch systems that can cause leaks, odor, skin irritation, embarrassment, and social and emotional distress. The AGA Committee for GI Innovation and Technology (CGIT) organizes the annual Tech Summit.
Twistomy’s winning design includes a flexible ring and sleeve, which are inserted into the stoma and secured on the outside with a set of rings that make up the housing unit attached to a standard wafer. The housing unit twists the sleeve closed, allowing the user to control fecal output. For evacuation, the user attaches a pouch, untwists the sleeve, evacuates cleanly and effectively, and then discards the pouch.
Twistomy cofounders Devon Horton, BS, senior bioengineer, and Lily Williams, BS, biomedical researcher and engineer, both work for the department of surgery at University of Colorado, Denver.
Horton said in an interview that when he was approached with the idea to create a better ostomy solution for a senior-year capstone project he was intrigued because the traditional ostomy system “has not changed in more than 70 years. It was crazy that no one had done anything to change that.”
The Twistomy team also won the Grand Prize this spring at the Emerging Medical Innovation Valuation Competition at the Design of Medical Devices Conference held at the University of Minnesota, Minneapolis.
Witnessing the Struggle as a CNA
Horton also works as a certified nursing assistant at an inpatient unit at University of Colorado Hospital and the ostomy patients he sees there every shift help drive his passion to find a better solution.
He hears the emotional stories of people who manage their ostomy daily.
“Many express feelings of depression and anxiety, feeling isolated with their severe inability to go out and do things because of the fear of the noise the stoma makes, or the crinkling of the plastic bag in a yoga class,” he said. “We want to help them regain that control of quality of life.”
They also hope to cut down on the ostomy management time. “Initial user testing [for Twistomy] was less than 75 seconds to insert and assemble,” he said. “I did an interview with a patient yesterday who said they probably spend an hour a day managing their ostomy,” including cleaning and replacing.
Horton and Williams have a patent on the device and currently use three-dimensional printing for the prototypes.
Williams said they are now conducting consumer discovery studies through the National Science Foundation and are interviewing 30 stakeholders — “anyone who has a relationship with an ostomy,” whether a colorectal surgeon, a gastrointestinal nurse, ostomy patients, or insurers.
Those interviews will help in refining the device so they can start consulting with manufacturers and work toward approval as a Class II medical device from the US Food and Drug Administration (FDA), Williams said.
Saving Healthcare Costs
Another potential benefit for Twistomy is its ability to cut healthcare costs, Horton said. Traditional ostomies are prone to leakage, which can lead to peristomal skin complications.
He pointed to a National Institutes of Health analysis that found that on average peristomal skin complications caused upwards of $80,000 more per ostomy patient in increased healthcare costs over a 3-month period than for those without the complications.
“With Twistomy, we are reducing leakage most likely to zero,” Horton said. “We set out to say if we could reduce [infections] by half or a little less than half, we can cut out those tens of thousands of dollars that insurance companies and payers are spending.”
Permanent and Temporary Ostomy Markets
He pointed out that not all ostomies are permanent ostomies, adding that the reversal rate “is about 65%.” Often those reversal surgeries cannot take place until peristomal skin complications have been healed.
“We’re not only hoping to market to the permanent stoma patients, but the patients with temporary stomas as well,” he said.
The team estimates it will need $4 million–$6 million in funding for manufacturing and consultation costs as well as costs involved in seeking FDA approval.
Horton and Williams project the housing unit cost will be $399 based on known out-of-pocket expenses for patients with ostomy care products and the unit would be replaced annually. Disposable elements would be an additional cost.
Assuming insurance acceptance of the product, he said, “With about an 80/20 insurance coverage, typical for many patients, it would be about $100 in out-of-pocket expenses per month to use our device, which is around the lower end of what a lot of patients are spending out of pocket.”
One of the Tech Summit judges, Somaya Albhaisi, MD, a gastroenterology/hepatology fellow at University of Southern California, Los Angeles, said in an interview that the Shark Tank results were unanimous among the five judges and Twistomy also took the fan favorite vote.
She said the teams were judged on quality of pitch, potential clinical impact, and feasibility of business plan. Teams got 5-7 minutes to pitch and answered questions afterward.
“Deep Understanding” of Patient Need
“They combined smart engineering with deep understanding of patient need, which is restoring control, dignity, and quality of life for ostomy users while also reducing healthcare costs. It is rare to see a solution this scalable and impactful. It was a deeply empathetic solution overall.” She noted that nearly 1 million people in the United States currently use an ostomy.
Ostomy users’ quality of life is compromised, and they often have mental health challenges, Albhaisi said. This innovation appears to offer easy use, more dignity and control.
The other four Shark Tank finalists were:
- AI Lumen, which developed a retroview camera system, which attaches to the colonoscope and enhances imaging to detect hidden polyps that may evade conventional endoscopes.
- Amplified Sciences, which developed an ultrasensitive diagnostic platform that detects biomarker activities in minute volumes of fluid from pancreatic cystic lesions, helping to stratify patients into low risk or potential malignancy, reducing unneeded surgeries, costs, and comorbidities.
- KITE Endoscopic Innovations, which designed the Dynaflex TruCut needle to offer a simpler endoscopic ultrasound (EUS)–guided biopsy procedure with fewer needle passes, deeper insights into tumor pathology, and more tissue for geonomic analysis.
- MicroSteer, which designed a device to facilitate semiautomated endoscopic submucosal dissection (ESD) by decoupling the dissecting knife from the endoscope, enhancing safety and effectiveness during the procedure.
The Twistomy Team “Surprised Everyone”
The competitors’ scores were “very close,” one of the judges, Kevin Berliner, said in an interview. “The Twistomy team surprised everyone — the judges and the crowd — with their succinct, informative, and impactful pitch. That presentation disparity was the tiebreaker for me,” said Berliner, who works for Medtronic, a sponsor of the competition, in Chicago.
He said Horton and Williams were the youngest presenters and had the earliest stage pitch they judged, but they “outpresented other competitors in clarity, simplification, and storytelling.”
Also impressive was their description of their “commercially viable path to success” and their plan for the challenges ahead, he said.
Those challenges to get Twistomy to market center “on the ongoing changing climate we have with research funds lately,” Horton said. “We’re giving it an estimate of 3-5 years.”
Horton, Williams, Albhaisi, and Berliner reported no relevant financial relationships.
The “Shark Tank” winning innovation at the American Gastroenterological Association (AGA) Tech Summit in Chicago this April has “life-altering” potential for ostomy patients, according to one of the judges, and eliminates the need for constant pouch wear.
The innovation is called Twistomy and it is designed to replace current ostomy-pouch systems that can cause leaks, odor, skin irritation, embarrassment, and social and emotional distress. The AGA Committee for GI Innovation and Technology (CGIT) organizes the annual Tech Summit.
Twistomy’s winning design includes a flexible ring and sleeve, which are inserted into the stoma and secured on the outside with a set of rings that make up the housing unit attached to a standard wafer. The housing unit twists the sleeve closed, allowing the user to control fecal output. For evacuation, the user attaches a pouch, untwists the sleeve, evacuates cleanly and effectively, and then discards the pouch.
Twistomy cofounders Devon Horton, BS, senior bioengineer, and Lily Williams, BS, biomedical researcher and engineer, both work for the department of surgery at University of Colorado, Denver.
Horton said in an interview that when he was approached with the idea to create a better ostomy solution for a senior-year capstone project he was intrigued because the traditional ostomy system “has not changed in more than 70 years. It was crazy that no one had done anything to change that.”
The Twistomy team also won the Grand Prize this spring at the Emerging Medical Innovation Valuation Competition at the Design of Medical Devices Conference held at the University of Minnesota, Minneapolis.
Witnessing the Struggle as a CNA
Horton also works as a certified nursing assistant at an inpatient unit at University of Colorado Hospital and the ostomy patients he sees there every shift help drive his passion to find a better solution.
He hears the emotional stories of people who manage their ostomy daily.
“Many express feelings of depression and anxiety, feeling isolated with their severe inability to go out and do things because of the fear of the noise the stoma makes, or the crinkling of the plastic bag in a yoga class,” he said. “We want to help them regain that control of quality of life.”
They also hope to cut down on the ostomy management time. “Initial user testing [for Twistomy] was less than 75 seconds to insert and assemble,” he said. “I did an interview with a patient yesterday who said they probably spend an hour a day managing their ostomy,” including cleaning and replacing.
Horton and Williams have a patent on the device and currently use three-dimensional printing for the prototypes.
Williams said they are now conducting consumer discovery studies through the National Science Foundation and are interviewing 30 stakeholders — “anyone who has a relationship with an ostomy,” whether a colorectal surgeon, a gastrointestinal nurse, ostomy patients, or insurers.
Those interviews will help in refining the device so they can start consulting with manufacturers and work toward approval as a Class II medical device from the US Food and Drug Administration (FDA), Williams said.
Saving Healthcare Costs
Another potential benefit for Twistomy is its ability to cut healthcare costs, Horton said. Traditional ostomies are prone to leakage, which can lead to peristomal skin complications.
He pointed to a National Institutes of Health analysis that found that on average peristomal skin complications caused upwards of $80,000 more per ostomy patient in increased healthcare costs over a 3-month period than for those without the complications.
“With Twistomy, we are reducing leakage most likely to zero,” Horton said. “We set out to say if we could reduce [infections] by half or a little less than half, we can cut out those tens of thousands of dollars that insurance companies and payers are spending.”
Permanent and Temporary Ostomy Markets
He pointed out that not all ostomies are permanent ostomies, adding that the reversal rate “is about 65%.” Often those reversal surgeries cannot take place until peristomal skin complications have been healed.
“We’re not only hoping to market to the permanent stoma patients, but the patients with temporary stomas as well,” he said.
The team estimates it will need $4 million–$6 million in funding for manufacturing and consultation costs as well as costs involved in seeking FDA approval.
Horton and Williams project the housing unit cost will be $399 based on known out-of-pocket expenses for patients with ostomy care products and the unit would be replaced annually. Disposable elements would be an additional cost.
Assuming insurance acceptance of the product, he said, “With about an 80/20 insurance coverage, typical for many patients, it would be about $100 in out-of-pocket expenses per month to use our device, which is around the lower end of what a lot of patients are spending out of pocket.”
One of the Tech Summit judges, Somaya Albhaisi, MD, a gastroenterology/hepatology fellow at University of Southern California, Los Angeles, said in an interview that the Shark Tank results were unanimous among the five judges and Twistomy also took the fan favorite vote.
She said the teams were judged on quality of pitch, potential clinical impact, and feasibility of business plan. Teams got 5-7 minutes to pitch and answered questions afterward.
“Deep Understanding” of Patient Need
“They combined smart engineering with deep understanding of patient need, which is restoring control, dignity, and quality of life for ostomy users while also reducing healthcare costs. It is rare to see a solution this scalable and impactful. It was a deeply empathetic solution overall.” She noted that nearly 1 million people in the United States currently use an ostomy.
Ostomy users’ quality of life is compromised, and they often have mental health challenges, Albhaisi said. This innovation appears to offer easy use, more dignity and control.
The other four Shark Tank finalists were:
- AI Lumen, which developed a retroview camera system, which attaches to the colonoscope and enhances imaging to detect hidden polyps that may evade conventional endoscopes.
- Amplified Sciences, which developed an ultrasensitive diagnostic platform that detects biomarker activities in minute volumes of fluid from pancreatic cystic lesions, helping to stratify patients into low risk or potential malignancy, reducing unneeded surgeries, costs, and comorbidities.
- KITE Endoscopic Innovations, which designed the Dynaflex TruCut needle to offer a simpler endoscopic ultrasound (EUS)–guided biopsy procedure with fewer needle passes, deeper insights into tumor pathology, and more tissue for geonomic analysis.
- MicroSteer, which designed a device to facilitate semiautomated endoscopic submucosal dissection (ESD) by decoupling the dissecting knife from the endoscope, enhancing safety and effectiveness during the procedure.
The Twistomy Team “Surprised Everyone”
The competitors’ scores were “very close,” one of the judges, Kevin Berliner, said in an interview. “The Twistomy team surprised everyone — the judges and the crowd — with their succinct, informative, and impactful pitch. That presentation disparity was the tiebreaker for me,” said Berliner, who works for Medtronic, a sponsor of the competition, in Chicago.
He said Horton and Williams were the youngest presenters and had the earliest stage pitch they judged, but they “outpresented other competitors in clarity, simplification, and storytelling.”
Also impressive was their description of their “commercially viable path to success” and their plan for the challenges ahead, he said.
Those challenges to get Twistomy to market center “on the ongoing changing climate we have with research funds lately,” Horton said. “We’re giving it an estimate of 3-5 years.”
Horton, Williams, Albhaisi, and Berliner reported no relevant financial relationships.
Chatbot Helps Users Adopt a Low FODMAP Diet
SAN DIEGO — Low fermentable oligo-, di-, and monosaccharides and polyols (FODMAPs) dietary advice has been shown to be effective in easing bloating and abdominal pain, especially in patients with irritable bowel syndrome (IBS), but limited availability of dietitians makes delivering this advice challenging. Researchers from Thailand have successfully enlisted a chatbot to help.
In a randomized controlled trial, they found that chatbot-assisted dietary advice with brief guidance effectively reduced high FODMAP intake, bloating severity, and improved dietary knowledge, particularly in patients with bothersome bloating.
“Chatbot-assisted dietary advice for FODMAPs restriction was feasible and applicable in patients with bloating symptoms that had baseline symptoms of moderate severity,” study chief Pochara Somvanapanich, with the Division of Gastroenterology, Chulalongkorn University and King Chulalongkorn Memorial Hospital, Bangkok, Thailand, told GI & Hepatology News.
Somvanapanich, who developed the chatbot algorithm, presented the study results at Digestive Disease Week (DDW) 2025.
More Knowledge, Less Bloating
The trial enrolled 86 adults with disorders of gut-brain interaction experiencing bloating symptoms for more than 6 months and consuming more than seven high-FODMAPs items per week. Half of them had IBS.
At baseline, gastrointestinal (GI) symptoms and the ability to identify FODMAPs were assessed. All participants received a 5-minute consultation on FODMAPs avoidance from a GI fellow and were randomly allocated (stratified by IBS diagnosis and education) into two groups.
The chatbot-assisted group received real-time dietary advice via a chatbot which helped them identify high, low, and non-FODMAP foods from a list of more than 300 ingredients/dishes of Thai and western cuisines.
The control group received only brief advice on high FODMAPs restriction. Both groups used a diary app to log food intake and postprandial symptoms. Baseline bloating, abdominal pain and global symptoms severity were similar between the two groups. Data on 64 participants (32 in each group) were analyzed.
After 4 weeks, significantly more people in the chatbot group than the control group responded — achieving a 30% or greater reduction in daily worst bloating, abdominal pain or global symptoms (19 [59%] vs 10 [31%], P < .05). Responder rates were similar in the IBS and non-IBS subgroups.
Subgroup analysis revealed significant differences between groups only for participants with bothersome bloating, not those with mild bloating severity.
In those with bothersome bloating severity, the chatbot group had a higher response rate (69.5% vs 36.3%) and fewer bloating symptoms (P < .05). They also had a greater reduction in high FODMAPs intake (10 vs 23 items/week) and demonstrated improved knowledge in identifying FODMAPs (P < .05).
“Responders in a chatbot group consistently engaged more with the app, performing significantly more weekly item searches than nonresponders (P < .05),” the authors noted in their conference abstract.
“Our next step is to develop the chatbot-assisted approach for the reintroduction and personalization phase based on messenger applications (including Facebook Messenger and other messaging platforms),” Somvanapanich told GI & Hepatology News.
“Once we’ve gathered enough data to confirm these are working effectively, we definitely plan to create a one-stop service application for FODMAPs dietary advice,” Somvanapanich added.
Lack of Robust Data on Digital GI Health Apps
Commenting on this research for GI & Hepatology News, Sidhartha R. Sinha, MD, Director of Digital Health and Innovation, Division of Gastroenterology and Hepatology, Stanford University in Stanford, California, noted that there is a “notable lack of robust data supporting digital health tools in gastroenterology. Despite hundreds of apps available, very few are supported by well-designed trials.”
“The study demonstrated that chatbot-assisted dietary advice significantly improved bloating symptoms, reduced intake of high-FODMAP foods, and enhanced patients’ dietary knowledge compared to brief dietary counseling alone, especially in those with bothersome symptoms,” said Sinha, who wasn’t involved in the study.
“Patients actively used the chatbot to manage their symptoms, achieving a higher response rate than those in the control arm who received brief counseling on avoiding high-FODMAP food,” he noted.
Sinha said in his practice at Stanford, “in the heart of Silicon Valley,” patients do use digital resources to manage their GI symptoms, including diseases like IBS and inflammatory bowel disease (IBD) — and he believes this is “increasingly common nationally.”
“However, the need for evidence-based tools is critical and the lack here often prevents many practitioners from regularly recommending them to patients. This study aligns well with clinical practice, and supports the use of this particular app to improve IBS symptoms, particularly when access to dietitians is limited. These results support chatbot-assisted dietary management as a feasible, effective, and scalable approach to patient care,” Sinha told GI & Hepatology News.
The study received no commercial funding. Somvanapanich and Sinha had no relevant disclosures.
A version of this article appeared on Medscape.com.
SAN DIEGO — Low fermentable oligo-, di-, and monosaccharides and polyols (FODMAPs) dietary advice has been shown to be effective in easing bloating and abdominal pain, especially in patients with irritable bowel syndrome (IBS), but limited availability of dietitians makes delivering this advice challenging. Researchers from Thailand have successfully enlisted a chatbot to help.
In a randomized controlled trial, they found that chatbot-assisted dietary advice with brief guidance effectively reduced high FODMAP intake, bloating severity, and improved dietary knowledge, particularly in patients with bothersome bloating.
“Chatbot-assisted dietary advice for FODMAPs restriction was feasible and applicable in patients with bloating symptoms that had baseline symptoms of moderate severity,” study chief Pochara Somvanapanich, with the Division of Gastroenterology, Chulalongkorn University and King Chulalongkorn Memorial Hospital, Bangkok, Thailand, told GI & Hepatology News.
Somvanapanich, who developed the chatbot algorithm, presented the study results at Digestive Disease Week (DDW) 2025.
More Knowledge, Less Bloating
The trial enrolled 86 adults with disorders of gut-brain interaction experiencing bloating symptoms for more than 6 months and consuming more than seven high-FODMAPs items per week. Half of them had IBS.
At baseline, gastrointestinal (GI) symptoms and the ability to identify FODMAPs were assessed. All participants received a 5-minute consultation on FODMAPs avoidance from a GI fellow and were randomly allocated (stratified by IBS diagnosis and education) into two groups.
The chatbot-assisted group received real-time dietary advice via a chatbot which helped them identify high, low, and non-FODMAP foods from a list of more than 300 ingredients/dishes of Thai and western cuisines.
The control group received only brief advice on high FODMAPs restriction. Both groups used a diary app to log food intake and postprandial symptoms. Baseline bloating, abdominal pain and global symptoms severity were similar between the two groups. Data on 64 participants (32 in each group) were analyzed.
After 4 weeks, significantly more people in the chatbot group than the control group responded — achieving a 30% or greater reduction in daily worst bloating, abdominal pain or global symptoms (19 [59%] vs 10 [31%], P < .05). Responder rates were similar in the IBS and non-IBS subgroups.
Subgroup analysis revealed significant differences between groups only for participants with bothersome bloating, not those with mild bloating severity.
In those with bothersome bloating severity, the chatbot group had a higher response rate (69.5% vs 36.3%) and fewer bloating symptoms (P < .05). They also had a greater reduction in high FODMAPs intake (10 vs 23 items/week) and demonstrated improved knowledge in identifying FODMAPs (P < .05).
“Responders in a chatbot group consistently engaged more with the app, performing significantly more weekly item searches than nonresponders (P < .05),” the authors noted in their conference abstract.
“Our next step is to develop the chatbot-assisted approach for the reintroduction and personalization phase based on messenger applications (including Facebook Messenger and other messaging platforms),” Somvanapanich told GI & Hepatology News.
“Once we’ve gathered enough data to confirm these are working effectively, we definitely plan to create a one-stop service application for FODMAPs dietary advice,” Somvanapanich added.
Lack of Robust Data on Digital GI Health Apps
Commenting on this research for GI & Hepatology News, Sidhartha R. Sinha, MD, Director of Digital Health and Innovation, Division of Gastroenterology and Hepatology, Stanford University in Stanford, California, noted that there is a “notable lack of robust data supporting digital health tools in gastroenterology. Despite hundreds of apps available, very few are supported by well-designed trials.”
“The study demonstrated that chatbot-assisted dietary advice significantly improved bloating symptoms, reduced intake of high-FODMAP foods, and enhanced patients’ dietary knowledge compared to brief dietary counseling alone, especially in those with bothersome symptoms,” said Sinha, who wasn’t involved in the study.
“Patients actively used the chatbot to manage their symptoms, achieving a higher response rate than those in the control arm who received brief counseling on avoiding high-FODMAP food,” he noted.
Sinha said in his practice at Stanford, “in the heart of Silicon Valley,” patients do use digital resources to manage their GI symptoms, including diseases like IBS and inflammatory bowel disease (IBD) — and he believes this is “increasingly common nationally.”
“However, the need for evidence-based tools is critical and the lack here often prevents many practitioners from regularly recommending them to patients. This study aligns well with clinical practice, and supports the use of this particular app to improve IBS symptoms, particularly when access to dietitians is limited. These results support chatbot-assisted dietary management as a feasible, effective, and scalable approach to patient care,” Sinha told GI & Hepatology News.
The study received no commercial funding. Somvanapanich and Sinha had no relevant disclosures.
A version of this article appeared on Medscape.com.
SAN DIEGO — Low fermentable oligo-, di-, and monosaccharides and polyols (FODMAPs) dietary advice has been shown to be effective in easing bloating and abdominal pain, especially in patients with irritable bowel syndrome (IBS), but limited availability of dietitians makes delivering this advice challenging. Researchers from Thailand have successfully enlisted a chatbot to help.
In a randomized controlled trial, they found that chatbot-assisted dietary advice with brief guidance effectively reduced high FODMAP intake, bloating severity, and improved dietary knowledge, particularly in patients with bothersome bloating.
“Chatbot-assisted dietary advice for FODMAPs restriction was feasible and applicable in patients with bloating symptoms that had baseline symptoms of moderate severity,” study chief Pochara Somvanapanich, with the Division of Gastroenterology, Chulalongkorn University and King Chulalongkorn Memorial Hospital, Bangkok, Thailand, told GI & Hepatology News.
Somvanapanich, who developed the chatbot algorithm, presented the study results at Digestive Disease Week (DDW) 2025.
More Knowledge, Less Bloating
The trial enrolled 86 adults with disorders of gut-brain interaction experiencing bloating symptoms for more than 6 months and consuming more than seven high-FODMAPs items per week. Half of them had IBS.
At baseline, gastrointestinal (GI) symptoms and the ability to identify FODMAPs were assessed. All participants received a 5-minute consultation on FODMAPs avoidance from a GI fellow and were randomly allocated (stratified by IBS diagnosis and education) into two groups.
The chatbot-assisted group received real-time dietary advice via a chatbot which helped them identify high, low, and non-FODMAP foods from a list of more than 300 ingredients/dishes of Thai and western cuisines.
The control group received only brief advice on high FODMAPs restriction. Both groups used a diary app to log food intake and postprandial symptoms. Baseline bloating, abdominal pain and global symptoms severity were similar between the two groups. Data on 64 participants (32 in each group) were analyzed.
After 4 weeks, significantly more people in the chatbot group than the control group responded — achieving a 30% or greater reduction in daily worst bloating, abdominal pain or global symptoms (19 [59%] vs 10 [31%], P < .05). Responder rates were similar in the IBS and non-IBS subgroups.
Subgroup analysis revealed significant differences between groups only for participants with bothersome bloating, not those with mild bloating severity.
In those with bothersome bloating severity, the chatbot group had a higher response rate (69.5% vs 36.3%) and fewer bloating symptoms (P < .05). They also had a greater reduction in high FODMAPs intake (10 vs 23 items/week) and demonstrated improved knowledge in identifying FODMAPs (P < .05).
“Responders in a chatbot group consistently engaged more with the app, performing significantly more weekly item searches than nonresponders (P < .05),” the authors noted in their conference abstract.
“Our next step is to develop the chatbot-assisted approach for the reintroduction and personalization phase based on messenger applications (including Facebook Messenger and other messaging platforms),” Somvanapanich told GI & Hepatology News.
“Once we’ve gathered enough data to confirm these are working effectively, we definitely plan to create a one-stop service application for FODMAPs dietary advice,” Somvanapanich added.
Lack of Robust Data on Digital GI Health Apps
Commenting on this research for GI & Hepatology News, Sidhartha R. Sinha, MD, Director of Digital Health and Innovation, Division of Gastroenterology and Hepatology, Stanford University in Stanford, California, noted that there is a “notable lack of robust data supporting digital health tools in gastroenterology. Despite hundreds of apps available, very few are supported by well-designed trials.”
“The study demonstrated that chatbot-assisted dietary advice significantly improved bloating symptoms, reduced intake of high-FODMAP foods, and enhanced patients’ dietary knowledge compared to brief dietary counseling alone, especially in those with bothersome symptoms,” said Sinha, who wasn’t involved in the study.
“Patients actively used the chatbot to manage their symptoms, achieving a higher response rate than those in the control arm who received brief counseling on avoiding high-FODMAP food,” he noted.
Sinha said in his practice at Stanford, “in the heart of Silicon Valley,” patients do use digital resources to manage their GI symptoms, including diseases like IBS and inflammatory bowel disease (IBD) — and he believes this is “increasingly common nationally.”
“However, the need for evidence-based tools is critical and the lack here often prevents many practitioners from regularly recommending them to patients. This study aligns well with clinical practice, and supports the use of this particular app to improve IBS symptoms, particularly when access to dietitians is limited. These results support chatbot-assisted dietary management as a feasible, effective, and scalable approach to patient care,” Sinha told GI & Hepatology News.
The study received no commercial funding. Somvanapanich and Sinha had no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM DDW 2025
Blood-Based Test May Predict Crohn’s Disease 2 Years Before Onset
SAN DIEGO — Crohn’s disease (CD) has become more common in the United States, and an estimated 1 million Americans have the condition. Still, much is unknown about how to evaluate the individual risk for the disease.
“It’s pretty much accepted that Crohn’s disease does not begin at diagnosis,” said Ryan Ungaro, MD, associate professor of medicine at the Icahn School of Medicine at Mount Sinai, New York City, speaking at Digestive Disease Week (DDW)® 2025.
Although individual blood markers have been associated with the future risk for CD, what’s needed, he said, is to understand which combination of biomarkers are most predictive.
Now, .
It’s an early version that will likely be further improved and needs additional validation, Ungaro told GI & Hepatology News.
“Once we can accurately identify individuals at risk for developing Crohn’s disease, we can then imagine a number of potential interventions,” Ungaro said.
Approaches would vary depending on how far away the onset is estimated to be. For people who likely wouldn’t develop disease for many years, one intervention might be close monitoring to enable diagnosis in the earliest stages, when treatment works best, he said. Someone at a high risk of developing CD in the next 2 or 3 years, on the other hand, might be offered a pharmaceutical intervention.
Developing and Testing the Risk Score
To develop the risk score, Ungaro and colleagues analyzed data of 200 patients with CD and 100 healthy control participants from PREDICTS, a nested case-controlled study of active US military service members. The study is within the larger Department of Defense Serum Repository, which began in 1985 and has more than 62.5 million samples, all stored at −30 °C.
The researchers collected serum samples at four timepoints up to 6 or more years before the diagnosis. They assayed antimicrobial antibodies using the Prometheus Laboratories platform, proteomic markers using the Olink inflammation panel, and anti–granulocyte macrophage colony-stimulating factor autoantibodies using enzyme-linked immunosorbent assay.
Participants (median age, 33 years for both groups) were randomly divided into equally sized training and testing sets. In both the group, 83% of patients were White and about 90% were men.
Time-varying trajectories of marker abundance were estimated for each biomarker. Then, logistic regression modeled disease status as a function of each marker for different timepoints and multivariate modeling was performed via logistic LASSO regression.
A risk score to predict CD onset within 2 years was developed. Prediction models were fit on the testing set and predictive performance evaluated using receiver operating characteristic curves and area under the curve (AUC).
Blood proteins and antibodies have differing associations with CD depending on the time before diagnosis, the researchers found.
The integrative model to predict CD onset within 2 years incorporated 10 biomarkers associated significantly with CD onset.
The AUC for the model was 0.87 (considered good, with 1 indicating perfect discrimination). It produced a specificity of 99% and a positive predictive value of 84%.
The researchers stratified the model scores into quartiles and found the CD incidence within 2 years increased from 2% in the first quartile to 57.7% in the fourth. The relative risk of developing CD in the top quartile individuals vs lower quartile individuals was 10.4.
The serologic and proteomic markers show dynamic changes years before the diagnosis, Ungaro said.
A Strong Start
The research represents “an ambitious and exciting frontier for the future of IBD [inflammatory bowel disease] care,” said Victor G. Chedid, MD, MS, consultant and assistant professor of medicine at Mayo Clinic, Rochester, Minnesota, who reviewed the findings but was not involved in the study.
Currently, physicians treat IBD once it manifests, and it’s difficult to predict who will get CD, he said.
The integrative model’s AUC of 0.87 is impressive, and its specificity and positive predictive value levels show it is highly accurate in predicting the onset of CD within 2 years, Chedid added.
Further validation in larger and more diverse population is needed, Chedid said, but he sees the potential for the model to be practical in clinical practice.
“Additionally, the use of blood-based biomarkers makes the model relatively noninvasive and easy to implement in a clinical setting,” he said.
Now, the research goal is to understand the best biomarkers for characterizing the different preclinical phases of CD and to test different interventions in prevention trials, Ungaro told GI & Hepatology News.
A few trials are planned or ongoing, he noted. The trial PIONIR trial will look at the impact of a specific diet on the risk of developing CD, and the INTERCEPT trial aims to develop a blood-based risk score that can identify individuals with a high risk of developing CD within 5 years after initial evaluation.
Ungaro reported being on the advisory board of and/or receiving speaker or consulting fees from AbbVie, Bristol Myer Squibb, Celltrion, ECM Therapeutics, Genentech, Jansen, Eli Lilly, Pfizer, Roivant, Sanofi, and Takeda. Chedid reported having no relevant disclosures.
The PROMISE Consortium is funded by the Helmsley Charitable Trust.
A version of this article appeared on Medscape.com.
SAN DIEGO — Crohn’s disease (CD) has become more common in the United States, and an estimated 1 million Americans have the condition. Still, much is unknown about how to evaluate the individual risk for the disease.
“It’s pretty much accepted that Crohn’s disease does not begin at diagnosis,” said Ryan Ungaro, MD, associate professor of medicine at the Icahn School of Medicine at Mount Sinai, New York City, speaking at Digestive Disease Week (DDW)® 2025.
Although individual blood markers have been associated with the future risk for CD, what’s needed, he said, is to understand which combination of biomarkers are most predictive.
Now, .
It’s an early version that will likely be further improved and needs additional validation, Ungaro told GI & Hepatology News.
“Once we can accurately identify individuals at risk for developing Crohn’s disease, we can then imagine a number of potential interventions,” Ungaro said.
Approaches would vary depending on how far away the onset is estimated to be. For people who likely wouldn’t develop disease for many years, one intervention might be close monitoring to enable diagnosis in the earliest stages, when treatment works best, he said. Someone at a high risk of developing CD in the next 2 or 3 years, on the other hand, might be offered a pharmaceutical intervention.
Developing and Testing the Risk Score
To develop the risk score, Ungaro and colleagues analyzed data of 200 patients with CD and 100 healthy control participants from PREDICTS, a nested case-controlled study of active US military service members. The study is within the larger Department of Defense Serum Repository, which began in 1985 and has more than 62.5 million samples, all stored at −30 °C.
The researchers collected serum samples at four timepoints up to 6 or more years before the diagnosis. They assayed antimicrobial antibodies using the Prometheus Laboratories platform, proteomic markers using the Olink inflammation panel, and anti–granulocyte macrophage colony-stimulating factor autoantibodies using enzyme-linked immunosorbent assay.
Participants (median age, 33 years for both groups) were randomly divided into equally sized training and testing sets. In both the group, 83% of patients were White and about 90% were men.
Time-varying trajectories of marker abundance were estimated for each biomarker. Then, logistic regression modeled disease status as a function of each marker for different timepoints and multivariate modeling was performed via logistic LASSO regression.
A risk score to predict CD onset within 2 years was developed. Prediction models were fit on the testing set and predictive performance evaluated using receiver operating characteristic curves and area under the curve (AUC).
Blood proteins and antibodies have differing associations with CD depending on the time before diagnosis, the researchers found.
The integrative model to predict CD onset within 2 years incorporated 10 biomarkers associated significantly with CD onset.
The AUC for the model was 0.87 (considered good, with 1 indicating perfect discrimination). It produced a specificity of 99% and a positive predictive value of 84%.
The researchers stratified the model scores into quartiles and found the CD incidence within 2 years increased from 2% in the first quartile to 57.7% in the fourth. The relative risk of developing CD in the top quartile individuals vs lower quartile individuals was 10.4.
The serologic and proteomic markers show dynamic changes years before the diagnosis, Ungaro said.
A Strong Start
The research represents “an ambitious and exciting frontier for the future of IBD [inflammatory bowel disease] care,” said Victor G. Chedid, MD, MS, consultant and assistant professor of medicine at Mayo Clinic, Rochester, Minnesota, who reviewed the findings but was not involved in the study.
Currently, physicians treat IBD once it manifests, and it’s difficult to predict who will get CD, he said.
The integrative model’s AUC of 0.87 is impressive, and its specificity and positive predictive value levels show it is highly accurate in predicting the onset of CD within 2 years, Chedid added.
Further validation in larger and more diverse population is needed, Chedid said, but he sees the potential for the model to be practical in clinical practice.
“Additionally, the use of blood-based biomarkers makes the model relatively noninvasive and easy to implement in a clinical setting,” he said.
Now, the research goal is to understand the best biomarkers for characterizing the different preclinical phases of CD and to test different interventions in prevention trials, Ungaro told GI & Hepatology News.
A few trials are planned or ongoing, he noted. The trial PIONIR trial will look at the impact of a specific diet on the risk of developing CD, and the INTERCEPT trial aims to develop a blood-based risk score that can identify individuals with a high risk of developing CD within 5 years after initial evaluation.
Ungaro reported being on the advisory board of and/or receiving speaker or consulting fees from AbbVie, Bristol Myer Squibb, Celltrion, ECM Therapeutics, Genentech, Jansen, Eli Lilly, Pfizer, Roivant, Sanofi, and Takeda. Chedid reported having no relevant disclosures.
The PROMISE Consortium is funded by the Helmsley Charitable Trust.
A version of this article appeared on Medscape.com.
SAN DIEGO — Crohn’s disease (CD) has become more common in the United States, and an estimated 1 million Americans have the condition. Still, much is unknown about how to evaluate the individual risk for the disease.
“It’s pretty much accepted that Crohn’s disease does not begin at diagnosis,” said Ryan Ungaro, MD, associate professor of medicine at the Icahn School of Medicine at Mount Sinai, New York City, speaking at Digestive Disease Week (DDW)® 2025.
Although individual blood markers have been associated with the future risk for CD, what’s needed, he said, is to understand which combination of biomarkers are most predictive.
Now, .
It’s an early version that will likely be further improved and needs additional validation, Ungaro told GI & Hepatology News.
“Once we can accurately identify individuals at risk for developing Crohn’s disease, we can then imagine a number of potential interventions,” Ungaro said.
Approaches would vary depending on how far away the onset is estimated to be. For people who likely wouldn’t develop disease for many years, one intervention might be close monitoring to enable diagnosis in the earliest stages, when treatment works best, he said. Someone at a high risk of developing CD in the next 2 or 3 years, on the other hand, might be offered a pharmaceutical intervention.
Developing and Testing the Risk Score
To develop the risk score, Ungaro and colleagues analyzed data of 200 patients with CD and 100 healthy control participants from PREDICTS, a nested case-controlled study of active US military service members. The study is within the larger Department of Defense Serum Repository, which began in 1985 and has more than 62.5 million samples, all stored at −30 °C.
The researchers collected serum samples at four timepoints up to 6 or more years before the diagnosis. They assayed antimicrobial antibodies using the Prometheus Laboratories platform, proteomic markers using the Olink inflammation panel, and anti–granulocyte macrophage colony-stimulating factor autoantibodies using enzyme-linked immunosorbent assay.
Participants (median age, 33 years for both groups) were randomly divided into equally sized training and testing sets. In both the group, 83% of patients were White and about 90% were men.
Time-varying trajectories of marker abundance were estimated for each biomarker. Then, logistic regression modeled disease status as a function of each marker for different timepoints and multivariate modeling was performed via logistic LASSO regression.
A risk score to predict CD onset within 2 years was developed. Prediction models were fit on the testing set and predictive performance evaluated using receiver operating characteristic curves and area under the curve (AUC).
Blood proteins and antibodies have differing associations with CD depending on the time before diagnosis, the researchers found.
The integrative model to predict CD onset within 2 years incorporated 10 biomarkers associated significantly with CD onset.
The AUC for the model was 0.87 (considered good, with 1 indicating perfect discrimination). It produced a specificity of 99% and a positive predictive value of 84%.
The researchers stratified the model scores into quartiles and found the CD incidence within 2 years increased from 2% in the first quartile to 57.7% in the fourth. The relative risk of developing CD in the top quartile individuals vs lower quartile individuals was 10.4.
The serologic and proteomic markers show dynamic changes years before the diagnosis, Ungaro said.
A Strong Start
The research represents “an ambitious and exciting frontier for the future of IBD [inflammatory bowel disease] care,” said Victor G. Chedid, MD, MS, consultant and assistant professor of medicine at Mayo Clinic, Rochester, Minnesota, who reviewed the findings but was not involved in the study.
Currently, physicians treat IBD once it manifests, and it’s difficult to predict who will get CD, he said.
The integrative model’s AUC of 0.87 is impressive, and its specificity and positive predictive value levels show it is highly accurate in predicting the onset of CD within 2 years, Chedid added.
Further validation in larger and more diverse population is needed, Chedid said, but he sees the potential for the model to be practical in clinical practice.
“Additionally, the use of blood-based biomarkers makes the model relatively noninvasive and easy to implement in a clinical setting,” he said.
Now, the research goal is to understand the best biomarkers for characterizing the different preclinical phases of CD and to test different interventions in prevention trials, Ungaro told GI & Hepatology News.
A few trials are planned or ongoing, he noted. The trial PIONIR trial will look at the impact of a specific diet on the risk of developing CD, and the INTERCEPT trial aims to develop a blood-based risk score that can identify individuals with a high risk of developing CD within 5 years after initial evaluation.
Ungaro reported being on the advisory board of and/or receiving speaker or consulting fees from AbbVie, Bristol Myer Squibb, Celltrion, ECM Therapeutics, Genentech, Jansen, Eli Lilly, Pfizer, Roivant, Sanofi, and Takeda. Chedid reported having no relevant disclosures.
The PROMISE Consortium is funded by the Helmsley Charitable Trust.
A version of this article appeared on Medscape.com.
FROM DDW 2025
Precision-Medicine Approach Improves IBD Infliximab Outcomes
SAN DIEGO — In tough-to-treat chronic inflammatory bowel disease (IBD), a precision-medicine strategy based on patients’ molecular profiles showed efficacy in guiding anti–tumor necrosis factor (TNF) therapy treatment decisions to improve outcomes.
“,” said first author Florian Tran, MD, in presenting the late-breaking study at Digestive Disease Week (DDW) 2025.
“We have now been able to demonstrate for the first time that precision medicine can be successfully applied in the context of chronic inflammatory bowel diseases, leading to improved long-term outcomes,” said Tran, a professor of pathophysiology of chronic inflammation at the Institute of Clinical Molecular Biology and department of internal medicine, Kiel University and University Hospital Schleswig Holstein, Kiel, Germany.
Anti-TNF therapies can be highly effective in a range of immune-mediated inflammatory diseases, including IBD, but not all patients respond. Key singular candidates of biomarkers that could better predict a response show relatively low predictive power or a failure to replicate in independent studies.
In previous research, Tran and colleagues reported identification of early dynamic molecular changes in the blood that are more robustly predictive of responses to anti-TNF therapy.
“We have generated compelling evidence that therapy-induced changes in inflammatory pathways can reliably predict patient outcomes,” he said.
Among them are dynamic transcriptome changes that emerge early during treatment and can predict response to anti-TNF therapy, as well as clinical response trajectories that differ based on subgroups.
To further investigate the benefits of the multi-biomarker signatures collectively, as opposed to single biomarker–based algorithms, Tran and colleagues conducted the phase 3, open-label GUIDE-IBD trial, enrolling 102 adults with a confirmed diagnosis of Crohn’s disease (CD) or ulcerative colitis (UC) at three German university hospitals between February 2021 and January 2024.
All patients had been assigned the anti-TNF drug infliximab for the first time.
Study participants were randomized to receive either the molecular-guided care or standard medical care, with stratifications based on diagnosis, recruiting center, and baseline corticosteroid use.
Those in the molecular group received real-time molecular assessments at baseline and weeks 2, 6, 14, and 26, which included peripheral blood samples and biopsies of known messenger ribonucleic acid–based biomarkers.
The assessments also looked at infliximab and anti-drug antibody levels.
Molecular reports were then provided through molecular medicine boards for patients in the molecular-guidance group at weeks 2, 14, 26, and 52, whereas data from the standard-care group was not communicated.
Based on the biomarker data, therapy decisions were made such as adjustments to dosing, intervals, comedication, and switches in therapy.
The primary endpoint was the combined end point of disease control, defined as clinical remission (CD Activity Index < 150, partial Mayo score < 2), endoscopic remission (simplified endoscopic score for CD ≤ 4 [≤ 2 for isolated ileal disease], endoscopic Mayo score ≤ 1), or biochemical remission (C-reactive protein < 5 mg/L, fecal calprotectin < 250 mg/g).
A total of 87 patients completed the study with available primary endpoint data to week 52; there were 38 in the molecular care group and 49 in the standard care group. In each group, approximately half of the patients had CD and half had UC.
For the primary endpoint, comprehensive disease control was significantly more frequent in the molecular care group at week 52 (55.3%) than in the standard-care group (26.5%), with an absolute difference of 29% (P = .0072).
Furthermore, the secondary endpoint of the combined rate of endoscopic and clinical remission at week 52 was also higher in the molecular group (60.5%) than in the standard-care group (32.7%; P = .0163).
An exploratory analysis further showed therapy switches were more common in the molecular group (47%) than in the standard-care group (29%), with an increased rate of drug switching between 14 weeks and 26 weeks.
More patients in the molecular guidance group achieved comprehensive disease control (deep remission) at week 52 (P = .0135).
“The [molecular guidance] group was more likely to switch therapies after the induction period, reducing the number of patients who are suboptimally treated under infliximab,” Tran noted.
The results underscore that “even in the absence of a single ‘magic’ biomarker, precision medicine can materially improve patient outcomes by integrating complex molecular data into everyday clinical decisions, enabling more effective therapy choices and reducing unnecessary drug side effects,” he said.
Approach Pioneered in Oncology
Tran noted that the collaboration necessary for the approach was based on strategies pioneered in cancer centers, which have resulted in significant improvements in cancer therapy outcomes.
“For the first time in IBD, we have now integrated multidimensional molecular data and innovative drug-dosing models into these inflammation boards,” he said.
Key components of the intervention include a highly structured patient care process with fixed assessment timepoints, as well as “a multidisciplinary, quality-controlled decision-making process that is meticulously documented,” he explained.
The results underscore that “we must move away from sole physician–driven treatment decisions in IBD toward a structured expert-board model for therapy decision-making.”
Benefits in Other IBD Therapies Unclear
Commenting on the study, Ashwin N. Ananthakrishnan, MBBS, MPH, AGAF, an associate professor of medicine with Massachusetts General Hospital, Boston, noted that “this approach may help optimize existing treatment early and ensure that ineffective treatments don’t get dragged on.”
Importantly, however, a key limitation is that “this does not tell you upfront whether a treatment is likely to work or what the best treatment is,” Ananthakrishnan said in an interview. “That is a critically important unmet need in IBD.”
While doses are escalated, if needed, with infliximab and other biologic drugs, that may not be the case with other therapies, he explained.
“For other agents, such as JAK [Janus kinase] inhibitors, we actually start at a higher dose and then reduce for maintenance,” said Ananthakrishnan.
How this approach would work for these drugs or “for drugs where blood levels are not reflective of efficacy is also not clear,” he said.
Tran’s disclosures included relationships with AbbVie, Bristol-Myers-Squibb, CED Service, Celltrion Healthcare, Eli Lilly, Ferring Pharmaceutical, Janssen, Johnson & Johnson, Takeda, LEK Consulting, and Sanofi/Regeneron. Ananthakrishnan had no disclosures to report.
A version of this article appeared on Medscape.com.
SAN DIEGO — In tough-to-treat chronic inflammatory bowel disease (IBD), a precision-medicine strategy based on patients’ molecular profiles showed efficacy in guiding anti–tumor necrosis factor (TNF) therapy treatment decisions to improve outcomes.
“,” said first author Florian Tran, MD, in presenting the late-breaking study at Digestive Disease Week (DDW) 2025.
“We have now been able to demonstrate for the first time that precision medicine can be successfully applied in the context of chronic inflammatory bowel diseases, leading to improved long-term outcomes,” said Tran, a professor of pathophysiology of chronic inflammation at the Institute of Clinical Molecular Biology and department of internal medicine, Kiel University and University Hospital Schleswig Holstein, Kiel, Germany.
Anti-TNF therapies can be highly effective in a range of immune-mediated inflammatory diseases, including IBD, but not all patients respond. Key singular candidates of biomarkers that could better predict a response show relatively low predictive power or a failure to replicate in independent studies.
In previous research, Tran and colleagues reported identification of early dynamic molecular changes in the blood that are more robustly predictive of responses to anti-TNF therapy.
“We have generated compelling evidence that therapy-induced changes in inflammatory pathways can reliably predict patient outcomes,” he said.
Among them are dynamic transcriptome changes that emerge early during treatment and can predict response to anti-TNF therapy, as well as clinical response trajectories that differ based on subgroups.
To further investigate the benefits of the multi-biomarker signatures collectively, as opposed to single biomarker–based algorithms, Tran and colleagues conducted the phase 3, open-label GUIDE-IBD trial, enrolling 102 adults with a confirmed diagnosis of Crohn’s disease (CD) or ulcerative colitis (UC) at three German university hospitals between February 2021 and January 2024.
All patients had been assigned the anti-TNF drug infliximab for the first time.
Study participants were randomized to receive either the molecular-guided care or standard medical care, with stratifications based on diagnosis, recruiting center, and baseline corticosteroid use.
Those in the molecular group received real-time molecular assessments at baseline and weeks 2, 6, 14, and 26, which included peripheral blood samples and biopsies of known messenger ribonucleic acid–based biomarkers.
The assessments also looked at infliximab and anti-drug antibody levels.
Molecular reports were then provided through molecular medicine boards for patients in the molecular-guidance group at weeks 2, 14, 26, and 52, whereas data from the standard-care group was not communicated.
Based on the biomarker data, therapy decisions were made such as adjustments to dosing, intervals, comedication, and switches in therapy.
The primary endpoint was the combined end point of disease control, defined as clinical remission (CD Activity Index < 150, partial Mayo score < 2), endoscopic remission (simplified endoscopic score for CD ≤ 4 [≤ 2 for isolated ileal disease], endoscopic Mayo score ≤ 1), or biochemical remission (C-reactive protein < 5 mg/L, fecal calprotectin < 250 mg/g).
A total of 87 patients completed the study with available primary endpoint data to week 52; there were 38 in the molecular care group and 49 in the standard care group. In each group, approximately half of the patients had CD and half had UC.
For the primary endpoint, comprehensive disease control was significantly more frequent in the molecular care group at week 52 (55.3%) than in the standard-care group (26.5%), with an absolute difference of 29% (P = .0072).
Furthermore, the secondary endpoint of the combined rate of endoscopic and clinical remission at week 52 was also higher in the molecular group (60.5%) than in the standard-care group (32.7%; P = .0163).
An exploratory analysis further showed therapy switches were more common in the molecular group (47%) than in the standard-care group (29%), with an increased rate of drug switching between 14 weeks and 26 weeks.
More patients in the molecular guidance group achieved comprehensive disease control (deep remission) at week 52 (P = .0135).
“The [molecular guidance] group was more likely to switch therapies after the induction period, reducing the number of patients who are suboptimally treated under infliximab,” Tran noted.
The results underscore that “even in the absence of a single ‘magic’ biomarker, precision medicine can materially improve patient outcomes by integrating complex molecular data into everyday clinical decisions, enabling more effective therapy choices and reducing unnecessary drug side effects,” he said.
Approach Pioneered in Oncology
Tran noted that the collaboration necessary for the approach was based on strategies pioneered in cancer centers, which have resulted in significant improvements in cancer therapy outcomes.
“For the first time in IBD, we have now integrated multidimensional molecular data and innovative drug-dosing models into these inflammation boards,” he said.
Key components of the intervention include a highly structured patient care process with fixed assessment timepoints, as well as “a multidisciplinary, quality-controlled decision-making process that is meticulously documented,” he explained.
The results underscore that “we must move away from sole physician–driven treatment decisions in IBD toward a structured expert-board model for therapy decision-making.”
Benefits in Other IBD Therapies Unclear
Commenting on the study, Ashwin N. Ananthakrishnan, MBBS, MPH, AGAF, an associate professor of medicine with Massachusetts General Hospital, Boston, noted that “this approach may help optimize existing treatment early and ensure that ineffective treatments don’t get dragged on.”
Importantly, however, a key limitation is that “this does not tell you upfront whether a treatment is likely to work or what the best treatment is,” Ananthakrishnan said in an interview. “That is a critically important unmet need in IBD.”
While doses are escalated, if needed, with infliximab and other biologic drugs, that may not be the case with other therapies, he explained.
“For other agents, such as JAK [Janus kinase] inhibitors, we actually start at a higher dose and then reduce for maintenance,” said Ananthakrishnan.
How this approach would work for these drugs or “for drugs where blood levels are not reflective of efficacy is also not clear,” he said.
Tran’s disclosures included relationships with AbbVie, Bristol-Myers-Squibb, CED Service, Celltrion Healthcare, Eli Lilly, Ferring Pharmaceutical, Janssen, Johnson & Johnson, Takeda, LEK Consulting, and Sanofi/Regeneron. Ananthakrishnan had no disclosures to report.
A version of this article appeared on Medscape.com.
SAN DIEGO — In tough-to-treat chronic inflammatory bowel disease (IBD), a precision-medicine strategy based on patients’ molecular profiles showed efficacy in guiding anti–tumor necrosis factor (TNF) therapy treatment decisions to improve outcomes.
“,” said first author Florian Tran, MD, in presenting the late-breaking study at Digestive Disease Week (DDW) 2025.
“We have now been able to demonstrate for the first time that precision medicine can be successfully applied in the context of chronic inflammatory bowel diseases, leading to improved long-term outcomes,” said Tran, a professor of pathophysiology of chronic inflammation at the Institute of Clinical Molecular Biology and department of internal medicine, Kiel University and University Hospital Schleswig Holstein, Kiel, Germany.
Anti-TNF therapies can be highly effective in a range of immune-mediated inflammatory diseases, including IBD, but not all patients respond. Key singular candidates of biomarkers that could better predict a response show relatively low predictive power or a failure to replicate in independent studies.
In previous research, Tran and colleagues reported identification of early dynamic molecular changes in the blood that are more robustly predictive of responses to anti-TNF therapy.
“We have generated compelling evidence that therapy-induced changes in inflammatory pathways can reliably predict patient outcomes,” he said.
Among them are dynamic transcriptome changes that emerge early during treatment and can predict response to anti-TNF therapy, as well as clinical response trajectories that differ based on subgroups.
To further investigate the benefits of the multi-biomarker signatures collectively, as opposed to single biomarker–based algorithms, Tran and colleagues conducted the phase 3, open-label GUIDE-IBD trial, enrolling 102 adults with a confirmed diagnosis of Crohn’s disease (CD) or ulcerative colitis (UC) at three German university hospitals between February 2021 and January 2024.
All patients had been assigned the anti-TNF drug infliximab for the first time.
Study participants were randomized to receive either the molecular-guided care or standard medical care, with stratifications based on diagnosis, recruiting center, and baseline corticosteroid use.
Those in the molecular group received real-time molecular assessments at baseline and weeks 2, 6, 14, and 26, which included peripheral blood samples and biopsies of known messenger ribonucleic acid–based biomarkers.
The assessments also looked at infliximab and anti-drug antibody levels.
Molecular reports were then provided through molecular medicine boards for patients in the molecular-guidance group at weeks 2, 14, 26, and 52, whereas data from the standard-care group was not communicated.
Based on the biomarker data, therapy decisions were made such as adjustments to dosing, intervals, comedication, and switches in therapy.
The primary endpoint was the combined end point of disease control, defined as clinical remission (CD Activity Index < 150, partial Mayo score < 2), endoscopic remission (simplified endoscopic score for CD ≤ 4 [≤ 2 for isolated ileal disease], endoscopic Mayo score ≤ 1), or biochemical remission (C-reactive protein < 5 mg/L, fecal calprotectin < 250 mg/g).
A total of 87 patients completed the study with available primary endpoint data to week 52; there were 38 in the molecular care group and 49 in the standard care group. In each group, approximately half of the patients had CD and half had UC.
For the primary endpoint, comprehensive disease control was significantly more frequent in the molecular care group at week 52 (55.3%) than in the standard-care group (26.5%), with an absolute difference of 29% (P = .0072).
Furthermore, the secondary endpoint of the combined rate of endoscopic and clinical remission at week 52 was also higher in the molecular group (60.5%) than in the standard-care group (32.7%; P = .0163).
An exploratory analysis further showed therapy switches were more common in the molecular group (47%) than in the standard-care group (29%), with an increased rate of drug switching between 14 weeks and 26 weeks.
More patients in the molecular guidance group achieved comprehensive disease control (deep remission) at week 52 (P = .0135).
“The [molecular guidance] group was more likely to switch therapies after the induction period, reducing the number of patients who are suboptimally treated under infliximab,” Tran noted.
The results underscore that “even in the absence of a single ‘magic’ biomarker, precision medicine can materially improve patient outcomes by integrating complex molecular data into everyday clinical decisions, enabling more effective therapy choices and reducing unnecessary drug side effects,” he said.
Approach Pioneered in Oncology
Tran noted that the collaboration necessary for the approach was based on strategies pioneered in cancer centers, which have resulted in significant improvements in cancer therapy outcomes.
“For the first time in IBD, we have now integrated multidimensional molecular data and innovative drug-dosing models into these inflammation boards,” he said.
Key components of the intervention include a highly structured patient care process with fixed assessment timepoints, as well as “a multidisciplinary, quality-controlled decision-making process that is meticulously documented,” he explained.
The results underscore that “we must move away from sole physician–driven treatment decisions in IBD toward a structured expert-board model for therapy decision-making.”
Benefits in Other IBD Therapies Unclear
Commenting on the study, Ashwin N. Ananthakrishnan, MBBS, MPH, AGAF, an associate professor of medicine with Massachusetts General Hospital, Boston, noted that “this approach may help optimize existing treatment early and ensure that ineffective treatments don’t get dragged on.”
Importantly, however, a key limitation is that “this does not tell you upfront whether a treatment is likely to work or what the best treatment is,” Ananthakrishnan said in an interview. “That is a critically important unmet need in IBD.”
While doses are escalated, if needed, with infliximab and other biologic drugs, that may not be the case with other therapies, he explained.
“For other agents, such as JAK [Janus kinase] inhibitors, we actually start at a higher dose and then reduce for maintenance,” said Ananthakrishnan.
How this approach would work for these drugs or “for drugs where blood levels are not reflective of efficacy is also not clear,” he said.
Tran’s disclosures included relationships with AbbVie, Bristol-Myers-Squibb, CED Service, Celltrion Healthcare, Eli Lilly, Ferring Pharmaceutical, Janssen, Johnson & Johnson, Takeda, LEK Consulting, and Sanofi/Regeneron. Ananthakrishnan had no disclosures to report.
A version of this article appeared on Medscape.com.
FROM DDW 2025
IgG-Guided Elimination Diet Beats Sham Diet for IBS Pain
An irritable bowel syndrome (IBS) elimination diet based on a novel IBS–specific, immunoglobulin G (IgG) was superior to a sham diet for abdominal pain, an 8-center, randomized double-blind controlled trial found.
While elimination diets can provide a personalized approach to dietary therapy, existing studies have had serious methodological issues, noted lead author Prashant Singh, MBBS, of the Division of Gastroenterology and Hepatology, Department of Internal Medicine, Michigan Medicine, Ann Arbor, Mich., and colleagues in Gastroenterology.
For example, previous studies on IgG-based diets used assays developed without determining IBS trigger foods or establishing a 95% confidence interval–based cutoff using a healthy control comparison group.
Study Details
From June 2018 to December 2021, 238 IBS patients testing positive for at least one food on 18-food IgG ELISA (enzyme-linked immunosorbent assay) testing and an average daily abdominal pain intensity score of 3.0 to 7.5 on an 11.0-point scale during a 2-week run-in period were randomized for 8 weeks to an experimental antibody-guided diet or to a sham diet. The primary outcome was a 30% decrease in abdominal pain intensity (API) for 2 of the last 4 weeks of treatment.
The overall study population had a mean age of about 40 years, and more than three-quarters were female. The 3 IBS types – constipation-predominant (IBS-C), diarrhea-predominant (IBS-D), and mixed bowel habits-predominant (IBS-M) – accounted for about a third each in both arms.
The experimental diet eliminated foods based on a positive ELISA result. Its sham counterpart had the same number of foods removed as the number of positive-testing food sensitivities, but the foods eliminated in the sham diet had tested negative on the IgG assay.
Participants reported daily abdominal pain intensity, bloating, and stool consistency, and frequency. They also reported dietary compliance and daily medication use.
Of the 238 randomized adults, 223 were included in the modified intention-to-treat analysis. A significantly greater proportion of subjects in the experimental group met the primary outcome than those in the sham group: 59.6% vs 42.1%, P = .02). “This highlights the potential effectiveness of a personalized elimination diet based on a novel IBS-specific IgG assay,” the authors wrote.
Symptom improvement between arms began to separate out at around 2 weeks, suggesting the effect of the experimental diet was relatively rapid in onset, and continued for at least 8 weeks. The durability of response, however, needs to be assessed in future studies “and it is unclear if there is a role for repeat IgG testing to monitor treatment response,” the authors wrote.
Subgroup analysis revealed that a higher proportion of those with IBS-C and IBS-M in the experimental diet group met the primary endpoint vs the sham group: 67.1% vs 35.8% and 66% vs 29.5%, respectively.
Interestingly, more patients in the experimental arm were noncompliant with their diet. “It is possible that subjects found the experimental diet more difficult to comply with compared with the sham diet or that because the experimental diet was more likely to improve symptoms, dietary indiscretion may have been more common in this group (a phenomenon seen with other elimination diets such as gluten-free diet in celiac disease),” the authors wrote.
Adverse events, deemed unrelated to either regimen, were 3 in the experimental arm vs 8 in the sham arm, which had 2 urinary tract infections.
The authors called for a larger, adequately powered study to assess the efficacy of an elimination diet based on this novel immunoglobulin G assay in patients with IBS-C and IBS-M. Future studies should perform detailed adherence assessments using food diaries.
“Mechanisms of how immunoglobulin G-antibody response to food antigen generates symptoms in irritable bowel syndrome are not well understood. Delineating this might provide new insights into food-related irritable bowel syndrome pathophysiology,” they concluded.
This study was funded by Biomerica Inc.
Symptoms in most people with irritable bowel syndrome (IBS) are perceived to be closely linked to diet. The low FODMAP diet has been pivotal for the treatment of IBS, and a range of other diet approaches are now on the research horizon.
Whilst IgE-mediated allergy is relatively rare, there has been research suggesting a role of IgG-mediated food sensitivity in causing symptoms in IBS, although the role of IgG testing and dietary elimination has been controversial. This study from Singh and colleagues suggests an IgG-based elimination diet could improve abdominal pain and global symptoms in two thirds of people with Rome IV IBS. Critically, the study is one of the largest so far and provides the most robust and detailed description of the trial diets to date.
The potential of a new diet approach is extremely appealing, especially as the low FODMAP diet is not universally effective. However, there is still some work to be done to transition the IgG-based elimination diet into guidelines and routine practice. Notably, some common foods restricted in IgG-based elimination diets are also high in FODMAPs leaving questions about the true driver of symptom benefit. Should convincing mechanistic studies and further additional RCT data validate these findings, this could present a major step forward for personalised nutrition in IBS.
Heidi Staudacher, PhD, is associate professor in the School of Translational Medicine, Monash University, Melbourne, Australia. She declared no conflicts of interest.
Symptoms in most people with irritable bowel syndrome (IBS) are perceived to be closely linked to diet. The low FODMAP diet has been pivotal for the treatment of IBS, and a range of other diet approaches are now on the research horizon.
Whilst IgE-mediated allergy is relatively rare, there has been research suggesting a role of IgG-mediated food sensitivity in causing symptoms in IBS, although the role of IgG testing and dietary elimination has been controversial. This study from Singh and colleagues suggests an IgG-based elimination diet could improve abdominal pain and global symptoms in two thirds of people with Rome IV IBS. Critically, the study is one of the largest so far and provides the most robust and detailed description of the trial diets to date.
The potential of a new diet approach is extremely appealing, especially as the low FODMAP diet is not universally effective. However, there is still some work to be done to transition the IgG-based elimination diet into guidelines and routine practice. Notably, some common foods restricted in IgG-based elimination diets are also high in FODMAPs leaving questions about the true driver of symptom benefit. Should convincing mechanistic studies and further additional RCT data validate these findings, this could present a major step forward for personalised nutrition in IBS.
Heidi Staudacher, PhD, is associate professor in the School of Translational Medicine, Monash University, Melbourne, Australia. She declared no conflicts of interest.
Symptoms in most people with irritable bowel syndrome (IBS) are perceived to be closely linked to diet. The low FODMAP diet has been pivotal for the treatment of IBS, and a range of other diet approaches are now on the research horizon.
Whilst IgE-mediated allergy is relatively rare, there has been research suggesting a role of IgG-mediated food sensitivity in causing symptoms in IBS, although the role of IgG testing and dietary elimination has been controversial. This study from Singh and colleagues suggests an IgG-based elimination diet could improve abdominal pain and global symptoms in two thirds of people with Rome IV IBS. Critically, the study is one of the largest so far and provides the most robust and detailed description of the trial diets to date.
The potential of a new diet approach is extremely appealing, especially as the low FODMAP diet is not universally effective. However, there is still some work to be done to transition the IgG-based elimination diet into guidelines and routine practice. Notably, some common foods restricted in IgG-based elimination diets are also high in FODMAPs leaving questions about the true driver of symptom benefit. Should convincing mechanistic studies and further additional RCT data validate these findings, this could present a major step forward for personalised nutrition in IBS.
Heidi Staudacher, PhD, is associate professor in the School of Translational Medicine, Monash University, Melbourne, Australia. She declared no conflicts of interest.
An irritable bowel syndrome (IBS) elimination diet based on a novel IBS–specific, immunoglobulin G (IgG) was superior to a sham diet for abdominal pain, an 8-center, randomized double-blind controlled trial found.
While elimination diets can provide a personalized approach to dietary therapy, existing studies have had serious methodological issues, noted lead author Prashant Singh, MBBS, of the Division of Gastroenterology and Hepatology, Department of Internal Medicine, Michigan Medicine, Ann Arbor, Mich., and colleagues in Gastroenterology.
For example, previous studies on IgG-based diets used assays developed without determining IBS trigger foods or establishing a 95% confidence interval–based cutoff using a healthy control comparison group.
Study Details
From June 2018 to December 2021, 238 IBS patients testing positive for at least one food on 18-food IgG ELISA (enzyme-linked immunosorbent assay) testing and an average daily abdominal pain intensity score of 3.0 to 7.5 on an 11.0-point scale during a 2-week run-in period were randomized for 8 weeks to an experimental antibody-guided diet or to a sham diet. The primary outcome was a 30% decrease in abdominal pain intensity (API) for 2 of the last 4 weeks of treatment.
The overall study population had a mean age of about 40 years, and more than three-quarters were female. The 3 IBS types – constipation-predominant (IBS-C), diarrhea-predominant (IBS-D), and mixed bowel habits-predominant (IBS-M) – accounted for about a third each in both arms.
The experimental diet eliminated foods based on a positive ELISA result. Its sham counterpart had the same number of foods removed as the number of positive-testing food sensitivities, but the foods eliminated in the sham diet had tested negative on the IgG assay.
Participants reported daily abdominal pain intensity, bloating, and stool consistency, and frequency. They also reported dietary compliance and daily medication use.
Of the 238 randomized adults, 223 were included in the modified intention-to-treat analysis. A significantly greater proportion of subjects in the experimental group met the primary outcome than those in the sham group: 59.6% vs 42.1%, P = .02). “This highlights the potential effectiveness of a personalized elimination diet based on a novel IBS-specific IgG assay,” the authors wrote.
Symptom improvement between arms began to separate out at around 2 weeks, suggesting the effect of the experimental diet was relatively rapid in onset, and continued for at least 8 weeks. The durability of response, however, needs to be assessed in future studies “and it is unclear if there is a role for repeat IgG testing to monitor treatment response,” the authors wrote.
Subgroup analysis revealed that a higher proportion of those with IBS-C and IBS-M in the experimental diet group met the primary endpoint vs the sham group: 67.1% vs 35.8% and 66% vs 29.5%, respectively.
Interestingly, more patients in the experimental arm were noncompliant with their diet. “It is possible that subjects found the experimental diet more difficult to comply with compared with the sham diet or that because the experimental diet was more likely to improve symptoms, dietary indiscretion may have been more common in this group (a phenomenon seen with other elimination diets such as gluten-free diet in celiac disease),” the authors wrote.
Adverse events, deemed unrelated to either regimen, were 3 in the experimental arm vs 8 in the sham arm, which had 2 urinary tract infections.
The authors called for a larger, adequately powered study to assess the efficacy of an elimination diet based on this novel immunoglobulin G assay in patients with IBS-C and IBS-M. Future studies should perform detailed adherence assessments using food diaries.
“Mechanisms of how immunoglobulin G-antibody response to food antigen generates symptoms in irritable bowel syndrome are not well understood. Delineating this might provide new insights into food-related irritable bowel syndrome pathophysiology,” they concluded.
This study was funded by Biomerica Inc.
An irritable bowel syndrome (IBS) elimination diet based on a novel IBS–specific, immunoglobulin G (IgG) was superior to a sham diet for abdominal pain, an 8-center, randomized double-blind controlled trial found.
While elimination diets can provide a personalized approach to dietary therapy, existing studies have had serious methodological issues, noted lead author Prashant Singh, MBBS, of the Division of Gastroenterology and Hepatology, Department of Internal Medicine, Michigan Medicine, Ann Arbor, Mich., and colleagues in Gastroenterology.
For example, previous studies on IgG-based diets used assays developed without determining IBS trigger foods or establishing a 95% confidence interval–based cutoff using a healthy control comparison group.
Study Details
From June 2018 to December 2021, 238 IBS patients testing positive for at least one food on 18-food IgG ELISA (enzyme-linked immunosorbent assay) testing and an average daily abdominal pain intensity score of 3.0 to 7.5 on an 11.0-point scale during a 2-week run-in period were randomized for 8 weeks to an experimental antibody-guided diet or to a sham diet. The primary outcome was a 30% decrease in abdominal pain intensity (API) for 2 of the last 4 weeks of treatment.
The overall study population had a mean age of about 40 years, and more than three-quarters were female. The 3 IBS types – constipation-predominant (IBS-C), diarrhea-predominant (IBS-D), and mixed bowel habits-predominant (IBS-M) – accounted for about a third each in both arms.
The experimental diet eliminated foods based on a positive ELISA result. Its sham counterpart had the same number of foods removed as the number of positive-testing food sensitivities, but the foods eliminated in the sham diet had tested negative on the IgG assay.
Participants reported daily abdominal pain intensity, bloating, and stool consistency, and frequency. They also reported dietary compliance and daily medication use.
Of the 238 randomized adults, 223 were included in the modified intention-to-treat analysis. A significantly greater proportion of subjects in the experimental group met the primary outcome than those in the sham group: 59.6% vs 42.1%, P = .02). “This highlights the potential effectiveness of a personalized elimination diet based on a novel IBS-specific IgG assay,” the authors wrote.
Symptom improvement between arms began to separate out at around 2 weeks, suggesting the effect of the experimental diet was relatively rapid in onset, and continued for at least 8 weeks. The durability of response, however, needs to be assessed in future studies “and it is unclear if there is a role for repeat IgG testing to monitor treatment response,” the authors wrote.
Subgroup analysis revealed that a higher proportion of those with IBS-C and IBS-M in the experimental diet group met the primary endpoint vs the sham group: 67.1% vs 35.8% and 66% vs 29.5%, respectively.
Interestingly, more patients in the experimental arm were noncompliant with their diet. “It is possible that subjects found the experimental diet more difficult to comply with compared with the sham diet or that because the experimental diet was more likely to improve symptoms, dietary indiscretion may have been more common in this group (a phenomenon seen with other elimination diets such as gluten-free diet in celiac disease),” the authors wrote.
Adverse events, deemed unrelated to either regimen, were 3 in the experimental arm vs 8 in the sham arm, which had 2 urinary tract infections.
The authors called for a larger, adequately powered study to assess the efficacy of an elimination diet based on this novel immunoglobulin G assay in patients with IBS-C and IBS-M. Future studies should perform detailed adherence assessments using food diaries.
“Mechanisms of how immunoglobulin G-antibody response to food antigen generates symptoms in irritable bowel syndrome are not well understood. Delineating this might provide new insights into food-related irritable bowel syndrome pathophysiology,” they concluded.
This study was funded by Biomerica Inc.
FROM GASTROENTEROLOGY
Weekend Workout, Regular Exercise Are Equals at Lowering GI Disease Risk
SAN DIEGO — The session started with a question that many in the audience at Digestive Disease Week (DDW) 2025 seemed to relate to: “How many of you find yourself squeezing workouts into a weekend after a hectic work week?”
Although regular exercise three or more times a week is often viewed as preferable, Shiyi Yu, MD, a resident physician in the Department of Gastroenterology at Guangdong Provincial People’s Hospital in Guangzhou, China, had good news for weekend warriors.
Both patterns reduce digestive disease almost equally.
Her study compared weekend warriors with those she called “active regulars” and sedentary folks to see how activity patterns affect digestive disease risks.
Her bottom line: “Your gut does not care about your schedule.”
The researchers analyzed wrist-based accelerometer data from 89,595 participants in the UK Biobank. To categorize participants as active or inactive, they used the World Health Organization 2020 guidelines for physical activity, which recommend at least 150-300 minutes of moderate-intensity aerobic physical activity or at least 75-150 minutes of vigorous-intensity aerobic physical activity, or an equivalent combination throughout the week. Median age of participants was 63.3 years and 48.8% were men.
They divided participants into three groups:
- About 43% were weekend warriors who met or exceeded 150 minutes of moderate to vigorous physical activity (MVPA), with 50% or more of total MVPA achieved in 1-2 days.
- About 23% were active regulars who met or exceeded 150 minutes a week but spread over more days.
- About 34% were inactive participants who were active less than 150 minutes a week.
The researchers followed the participants for a median of 7.9 years, looking for the incidence of multiple digestive diseases, identified using the International Classification of Diseases, 10th Revision, codes. These included diverticulosis, constipation, metabolic dysfunction–associated steatotic liver disease, cholelithiasis, and gastroesophageal reflux disease.
,” Yu said. At the threshold ≥ 150 minutes, for instance, hazard ratios for any digestive disease were 0.83 for weekend warriors and 0.79 for active regulars, compared with sedentary participants.
The analysis was repeated using a median threshold ≥ 230.4 minutes of MVPA a week, and the researchers found the same results.
As a validation cohort, the researchers used more than 6,000 participants from the National Institutes of Health’s All of Us Research Program with over 6 months of wrist-based accelerometer data.
A recent meta-epidemiology study found that the weekend warrior pattern offers other health benefits, including reducing the risk for cardiovascular disease mortality, mental disorders, and metabolic syndrome.
A Pleasant Surprise
The digestive disease study’s findings were “a surprise and a pleasant one,” said Aasma Shaukat, MD, MPH, AGAF, professor of medicine and a gastroenterologist at NYU Grossman School of Medicine, New York City.
“We often think if we’re not able to exercise regularly, then there’s no hope for us,” said Shaukat, who moderated the session. “But this implies that even if we have time only during the weekend to engage in physical activity, it still confers benefits in reducing our risk of any GI health disorder, as well as cardiovascular or other health disorders, compared to people inactive at baseline.”
“It gives us flexibility in terms of how we structure our exercise. Obviously, people should try to get into the habit of doing regular activity; it’s more sustainable. But a good alternative, according to this research, is that packing all of that in over the weekend seems to confer benefit. So all is not lost.”
Will this change her conversation with patients moving forward? Absolutely, Shaukat said. She generally recommends physical activity for at least 30 minutes three times a week. Now Shaukat said she can tell patients: “If that’s not possible, take that time out during the weekend for your health”.
This study was funded by grants from the National Natural Science Foundation of China and its Regional Innovation and Development Joint Foundation. Yu and Shaukat reported no disclosures.
A version of this article appeared on Medscape.com.
SAN DIEGO — The session started with a question that many in the audience at Digestive Disease Week (DDW) 2025 seemed to relate to: “How many of you find yourself squeezing workouts into a weekend after a hectic work week?”
Although regular exercise three or more times a week is often viewed as preferable, Shiyi Yu, MD, a resident physician in the Department of Gastroenterology at Guangdong Provincial People’s Hospital in Guangzhou, China, had good news for weekend warriors.
Both patterns reduce digestive disease almost equally.
Her study compared weekend warriors with those she called “active regulars” and sedentary folks to see how activity patterns affect digestive disease risks.
Her bottom line: “Your gut does not care about your schedule.”
The researchers analyzed wrist-based accelerometer data from 89,595 participants in the UK Biobank. To categorize participants as active or inactive, they used the World Health Organization 2020 guidelines for physical activity, which recommend at least 150-300 minutes of moderate-intensity aerobic physical activity or at least 75-150 minutes of vigorous-intensity aerobic physical activity, or an equivalent combination throughout the week. Median age of participants was 63.3 years and 48.8% were men.
They divided participants into three groups:
- About 43% were weekend warriors who met or exceeded 150 minutes of moderate to vigorous physical activity (MVPA), with 50% or more of total MVPA achieved in 1-2 days.
- About 23% were active regulars who met or exceeded 150 minutes a week but spread over more days.
- About 34% were inactive participants who were active less than 150 minutes a week.
The researchers followed the participants for a median of 7.9 years, looking for the incidence of multiple digestive diseases, identified using the International Classification of Diseases, 10th Revision, codes. These included diverticulosis, constipation, metabolic dysfunction–associated steatotic liver disease, cholelithiasis, and gastroesophageal reflux disease.
,” Yu said. At the threshold ≥ 150 minutes, for instance, hazard ratios for any digestive disease were 0.83 for weekend warriors and 0.79 for active regulars, compared with sedentary participants.
The analysis was repeated using a median threshold ≥ 230.4 minutes of MVPA a week, and the researchers found the same results.
As a validation cohort, the researchers used more than 6,000 participants from the National Institutes of Health’s All of Us Research Program with over 6 months of wrist-based accelerometer data.
A recent meta-epidemiology study found that the weekend warrior pattern offers other health benefits, including reducing the risk for cardiovascular disease mortality, mental disorders, and metabolic syndrome.
A Pleasant Surprise
The digestive disease study’s findings were “a surprise and a pleasant one,” said Aasma Shaukat, MD, MPH, AGAF, professor of medicine and a gastroenterologist at NYU Grossman School of Medicine, New York City.
“We often think if we’re not able to exercise regularly, then there’s no hope for us,” said Shaukat, who moderated the session. “But this implies that even if we have time only during the weekend to engage in physical activity, it still confers benefits in reducing our risk of any GI health disorder, as well as cardiovascular or other health disorders, compared to people inactive at baseline.”
“It gives us flexibility in terms of how we structure our exercise. Obviously, people should try to get into the habit of doing regular activity; it’s more sustainable. But a good alternative, according to this research, is that packing all of that in over the weekend seems to confer benefit. So all is not lost.”
Will this change her conversation with patients moving forward? Absolutely, Shaukat said. She generally recommends physical activity for at least 30 minutes three times a week. Now Shaukat said she can tell patients: “If that’s not possible, take that time out during the weekend for your health”.
This study was funded by grants from the National Natural Science Foundation of China and its Regional Innovation and Development Joint Foundation. Yu and Shaukat reported no disclosures.
A version of this article appeared on Medscape.com.
SAN DIEGO — The session started with a question that many in the audience at Digestive Disease Week (DDW) 2025 seemed to relate to: “How many of you find yourself squeezing workouts into a weekend after a hectic work week?”
Although regular exercise three or more times a week is often viewed as preferable, Shiyi Yu, MD, a resident physician in the Department of Gastroenterology at Guangdong Provincial People’s Hospital in Guangzhou, China, had good news for weekend warriors.
Both patterns reduce digestive disease almost equally.
Her study compared weekend warriors with those she called “active regulars” and sedentary folks to see how activity patterns affect digestive disease risks.
Her bottom line: “Your gut does not care about your schedule.”
The researchers analyzed wrist-based accelerometer data from 89,595 participants in the UK Biobank. To categorize participants as active or inactive, they used the World Health Organization 2020 guidelines for physical activity, which recommend at least 150-300 minutes of moderate-intensity aerobic physical activity or at least 75-150 minutes of vigorous-intensity aerobic physical activity, or an equivalent combination throughout the week. Median age of participants was 63.3 years and 48.8% were men.
They divided participants into three groups:
- About 43% were weekend warriors who met or exceeded 150 minutes of moderate to vigorous physical activity (MVPA), with 50% or more of total MVPA achieved in 1-2 days.
- About 23% were active regulars who met or exceeded 150 minutes a week but spread over more days.
- About 34% were inactive participants who were active less than 150 minutes a week.
The researchers followed the participants for a median of 7.9 years, looking for the incidence of multiple digestive diseases, identified using the International Classification of Diseases, 10th Revision, codes. These included diverticulosis, constipation, metabolic dysfunction–associated steatotic liver disease, cholelithiasis, and gastroesophageal reflux disease.
,” Yu said. At the threshold ≥ 150 minutes, for instance, hazard ratios for any digestive disease were 0.83 for weekend warriors and 0.79 for active regulars, compared with sedentary participants.
The analysis was repeated using a median threshold ≥ 230.4 minutes of MVPA a week, and the researchers found the same results.
As a validation cohort, the researchers used more than 6,000 participants from the National Institutes of Health’s All of Us Research Program with over 6 months of wrist-based accelerometer data.
A recent meta-epidemiology study found that the weekend warrior pattern offers other health benefits, including reducing the risk for cardiovascular disease mortality, mental disorders, and metabolic syndrome.
A Pleasant Surprise
The digestive disease study’s findings were “a surprise and a pleasant one,” said Aasma Shaukat, MD, MPH, AGAF, professor of medicine and a gastroenterologist at NYU Grossman School of Medicine, New York City.
“We often think if we’re not able to exercise regularly, then there’s no hope for us,” said Shaukat, who moderated the session. “But this implies that even if we have time only during the weekend to engage in physical activity, it still confers benefits in reducing our risk of any GI health disorder, as well as cardiovascular or other health disorders, compared to people inactive at baseline.”
“It gives us flexibility in terms of how we structure our exercise. Obviously, people should try to get into the habit of doing regular activity; it’s more sustainable. But a good alternative, according to this research, is that packing all of that in over the weekend seems to confer benefit. So all is not lost.”
Will this change her conversation with patients moving forward? Absolutely, Shaukat said. She generally recommends physical activity for at least 30 minutes three times a week. Now Shaukat said she can tell patients: “If that’s not possible, take that time out during the weekend for your health”.
This study was funded by grants from the National Natural Science Foundation of China and its Regional Innovation and Development Joint Foundation. Yu and Shaukat reported no disclosures.
A version of this article appeared on Medscape.com.
FROM DDW 2025
AI-Enhanced Digital Collaborative Care Improves IBS Symptoms
SAN DIEGO — seen at Cleveland Clinic, Cleveland, Ohio, an observational study found.
Symptom tracking at 4-week intervals showed that “almost everybody got better” regardless of IBS subtype, with relief starting in the first 4 weeks, Stephen Lupe, PsyD, gastrointestinal psychologist and director of Behavioral Medicine, Department of Gastroenterology, Hepatology, and Nutrition at Cleveland Clinic, Cleveland, said in an interview with GI & Hepatology News.
The findings were presented at Digestive Disease Week (DDW) 2025.
Digital Boost to Collaborative Care Model
The combination of dietary interventions and brain-gut behavioral therapy has demonstrated excellent outcomes for patients with IBS, but patients struggle to access these needed services, Lupe noted. A medical home collaborative care model in which patients get care from a multidisciplinary team has been shown to be a good way to successfully deliver this combination of care.
“When you do collaborative in-person care, people get better quicker,” Lupe said.
However, scaling access to this model remains a challenge. For their study, Cleveland Clinic researchers added an AI-enhanced digital platform, Ayble Health, to the in-person collaborative care model to expand access to disease-management services and evaluated whether it improved clinical outcomes for study’s 171 participants, who were recruited via social media advertisements.
Here’s how the platform works. Once a patient enrolls in Ayble Health, a personalized care plan is recommended based on a virtual visit, screening questionnaire, and baseline survey.
The platform includes brain-gut programs, including guided audio content on mindfulness, hypnosis, meditation, cognitive behavioral therapy, and breathing techniques; personalized nutrition support to find and remove trigger foods, a food barcode scanner, and a comprehensive groceries database; and AI-powered wellness tools to help manage and track symptoms. Lupe worked with Ayble Health to develop the platform’s behavioral health content and care pathways.
Patients may choose to follow any combination of three care pathways: A care team overseen by gastro-psychologists, dietitians, and gastroenterologists; a holistic nutrition program including a personalized elimination diet; and a brain-gut behavioral therapy program with gut-directed hypnosis, cognitive behavioral therapy, and acceptance and commitment therapy. They go at their own pace, can connect with Ayble Health’s virtual care team to help with education and goal setting, and continue to consult their Cleveland Clinic providers as needed for evaluation and treatment.
“The care team is still there. We’ve just augmented it to make sure that as many people as possible get behavioral skills training and dietary support, with monitoring between visits — instead of the traditional, ‘I’ll see you in 6 months approach,” Lupe explained.
IBS Symptom Scores Improve
Of the study’s 171 patients, 20 had IBS-diarrhea, 23 had IBS-constipation, 32 had IBS-mixed, and 8 had IBS-unspecified. The remaining 88 patients reported IBS without indication of subtype.
At intake, all patients had active IBS symptoms, with scores ≥ 75 on the IBS symptom severity scale (IBS-SSS). Most patients enrolled in more than one care pathway, and 95% of participants completed at least 4 weeks on their chosen pathways.
Overall, patients saw an average 140-point decrease in IBS-SSS from intake through follow-up lasting up to 42 weeks. A drop in IBS-SSS score ≥ 50 points was considered a clinically meaningful change.
Symptom improvements occurred as early as week 4, were sustained and were uniform across IBS subtypes, suggesting that the AI-enhanced digital collaborative care model has wide utility in patients with IBS, Lupe said.
Patients with the most severe IBS symptoms showed the greatest improvement, but even 50% of those with mild symptoms had clinically meaningful changes in IBS-SSS.
Improvement in IBS symptoms was seen across all care pathways, but the combination of multiple pathways improved outcomes better than a single care pathway alone. The combination of nutrition and brain-gut behavioral therapy demonstrated the greatest reduction in IBS-SSS scores and proportion of patients achieving clinically meaningful results (95%).
The digital comprehensive car model for IBS is now “up and running” at Cleveland Clinic, and the team plans to proactively reach out to patients with gastrointestinal disorders recently seen at their center to alert them to the availability of this tool, Lupe said.
A randomized controlled trial is planned to further validate these observational findings, he added.
‘Wave of the Future’
The digital collaborative care model is “innovative, and I think is the wave of the future,” Kyle Staller, MD, MPH, gastroenterologist and director of the Gastrointestinal Motility Laboratory at Massachusetts General Hospital, Boston, who wasn’t involved in the study, told GI & Hepatology News.
“These digital platforms bundle nondrug options, such as cognitive-behavioral therapy, dietary therapy, hypnotherapy, so patients can choose what suits them, rather than the gastroenterologist hunting down each individual resource, which requires a lot of work,” Staller said.
The study “provides real-world evidence that a deliberative, digital, collaborative care model that houses various types of nondrug IBS treatment under one roof can provide meaningful benefit to patients,” Staller told GI & Hepatology News.
Importantly, he said, “patients chose which option they wanted. At the end of the day, the way that we should be thinking about IBS care is really making sure that we engage the patient with treatment choices,” Staller said.
This study had no specific funding. Three authors had relationships with Ayble Health. Lupe is a scientific advisor for Boomerang Health and paid lecturer for Takeda Pharmaceuticals. Staller disclosed having relationships with Mahana Therapeutics, Ardelyx Inc, Gemelli Biotech, Salix Pharmaceuticals, and Takeda Pharmaceuticals.
A version of this article appeared on Medscape.com.
SAN DIEGO — seen at Cleveland Clinic, Cleveland, Ohio, an observational study found.
Symptom tracking at 4-week intervals showed that “almost everybody got better” regardless of IBS subtype, with relief starting in the first 4 weeks, Stephen Lupe, PsyD, gastrointestinal psychologist and director of Behavioral Medicine, Department of Gastroenterology, Hepatology, and Nutrition at Cleveland Clinic, Cleveland, said in an interview with GI & Hepatology News.
The findings were presented at Digestive Disease Week (DDW) 2025.
Digital Boost to Collaborative Care Model
The combination of dietary interventions and brain-gut behavioral therapy has demonstrated excellent outcomes for patients with IBS, but patients struggle to access these needed services, Lupe noted. A medical home collaborative care model in which patients get care from a multidisciplinary team has been shown to be a good way to successfully deliver this combination of care.
“When you do collaborative in-person care, people get better quicker,” Lupe said.
However, scaling access to this model remains a challenge. For their study, Cleveland Clinic researchers added an AI-enhanced digital platform, Ayble Health, to the in-person collaborative care model to expand access to disease-management services and evaluated whether it improved clinical outcomes for study’s 171 participants, who were recruited via social media advertisements.
Here’s how the platform works. Once a patient enrolls in Ayble Health, a personalized care plan is recommended based on a virtual visit, screening questionnaire, and baseline survey.
The platform includes brain-gut programs, including guided audio content on mindfulness, hypnosis, meditation, cognitive behavioral therapy, and breathing techniques; personalized nutrition support to find and remove trigger foods, a food barcode scanner, and a comprehensive groceries database; and AI-powered wellness tools to help manage and track symptoms. Lupe worked with Ayble Health to develop the platform’s behavioral health content and care pathways.
Patients may choose to follow any combination of three care pathways: A care team overseen by gastro-psychologists, dietitians, and gastroenterologists; a holistic nutrition program including a personalized elimination diet; and a brain-gut behavioral therapy program with gut-directed hypnosis, cognitive behavioral therapy, and acceptance and commitment therapy. They go at their own pace, can connect with Ayble Health’s virtual care team to help with education and goal setting, and continue to consult their Cleveland Clinic providers as needed for evaluation and treatment.
“The care team is still there. We’ve just augmented it to make sure that as many people as possible get behavioral skills training and dietary support, with monitoring between visits — instead of the traditional, ‘I’ll see you in 6 months approach,” Lupe explained.
IBS Symptom Scores Improve
Of the study’s 171 patients, 20 had IBS-diarrhea, 23 had IBS-constipation, 32 had IBS-mixed, and 8 had IBS-unspecified. The remaining 88 patients reported IBS without indication of subtype.
At intake, all patients had active IBS symptoms, with scores ≥ 75 on the IBS symptom severity scale (IBS-SSS). Most patients enrolled in more than one care pathway, and 95% of participants completed at least 4 weeks on their chosen pathways.
Overall, patients saw an average 140-point decrease in IBS-SSS from intake through follow-up lasting up to 42 weeks. A drop in IBS-SSS score ≥ 50 points was considered a clinically meaningful change.
Symptom improvements occurred as early as week 4, were sustained and were uniform across IBS subtypes, suggesting that the AI-enhanced digital collaborative care model has wide utility in patients with IBS, Lupe said.
Patients with the most severe IBS symptoms showed the greatest improvement, but even 50% of those with mild symptoms had clinically meaningful changes in IBS-SSS.
Improvement in IBS symptoms was seen across all care pathways, but the combination of multiple pathways improved outcomes better than a single care pathway alone. The combination of nutrition and brain-gut behavioral therapy demonstrated the greatest reduction in IBS-SSS scores and proportion of patients achieving clinically meaningful results (95%).
The digital comprehensive car model for IBS is now “up and running” at Cleveland Clinic, and the team plans to proactively reach out to patients with gastrointestinal disorders recently seen at their center to alert them to the availability of this tool, Lupe said.
A randomized controlled trial is planned to further validate these observational findings, he added.
‘Wave of the Future’
The digital collaborative care model is “innovative, and I think is the wave of the future,” Kyle Staller, MD, MPH, gastroenterologist and director of the Gastrointestinal Motility Laboratory at Massachusetts General Hospital, Boston, who wasn’t involved in the study, told GI & Hepatology News.
“These digital platforms bundle nondrug options, such as cognitive-behavioral therapy, dietary therapy, hypnotherapy, so patients can choose what suits them, rather than the gastroenterologist hunting down each individual resource, which requires a lot of work,” Staller said.
The study “provides real-world evidence that a deliberative, digital, collaborative care model that houses various types of nondrug IBS treatment under one roof can provide meaningful benefit to patients,” Staller told GI & Hepatology News.
Importantly, he said, “patients chose which option they wanted. At the end of the day, the way that we should be thinking about IBS care is really making sure that we engage the patient with treatment choices,” Staller said.
This study had no specific funding. Three authors had relationships with Ayble Health. Lupe is a scientific advisor for Boomerang Health and paid lecturer for Takeda Pharmaceuticals. Staller disclosed having relationships with Mahana Therapeutics, Ardelyx Inc, Gemelli Biotech, Salix Pharmaceuticals, and Takeda Pharmaceuticals.
A version of this article appeared on Medscape.com.
SAN DIEGO — seen at Cleveland Clinic, Cleveland, Ohio, an observational study found.
Symptom tracking at 4-week intervals showed that “almost everybody got better” regardless of IBS subtype, with relief starting in the first 4 weeks, Stephen Lupe, PsyD, gastrointestinal psychologist and director of Behavioral Medicine, Department of Gastroenterology, Hepatology, and Nutrition at Cleveland Clinic, Cleveland, said in an interview with GI & Hepatology News.
The findings were presented at Digestive Disease Week (DDW) 2025.
Digital Boost to Collaborative Care Model
The combination of dietary interventions and brain-gut behavioral therapy has demonstrated excellent outcomes for patients with IBS, but patients struggle to access these needed services, Lupe noted. A medical home collaborative care model in which patients get care from a multidisciplinary team has been shown to be a good way to successfully deliver this combination of care.
“When you do collaborative in-person care, people get better quicker,” Lupe said.
However, scaling access to this model remains a challenge. For their study, Cleveland Clinic researchers added an AI-enhanced digital platform, Ayble Health, to the in-person collaborative care model to expand access to disease-management services and evaluated whether it improved clinical outcomes for study’s 171 participants, who were recruited via social media advertisements.
Here’s how the platform works. Once a patient enrolls in Ayble Health, a personalized care plan is recommended based on a virtual visit, screening questionnaire, and baseline survey.
The platform includes brain-gut programs, including guided audio content on mindfulness, hypnosis, meditation, cognitive behavioral therapy, and breathing techniques; personalized nutrition support to find and remove trigger foods, a food barcode scanner, and a comprehensive groceries database; and AI-powered wellness tools to help manage and track symptoms. Lupe worked with Ayble Health to develop the platform’s behavioral health content and care pathways.
Patients may choose to follow any combination of three care pathways: A care team overseen by gastro-psychologists, dietitians, and gastroenterologists; a holistic nutrition program including a personalized elimination diet; and a brain-gut behavioral therapy program with gut-directed hypnosis, cognitive behavioral therapy, and acceptance and commitment therapy. They go at their own pace, can connect with Ayble Health’s virtual care team to help with education and goal setting, and continue to consult their Cleveland Clinic providers as needed for evaluation and treatment.
“The care team is still there. We’ve just augmented it to make sure that as many people as possible get behavioral skills training and dietary support, with monitoring between visits — instead of the traditional, ‘I’ll see you in 6 months approach,” Lupe explained.
IBS Symptom Scores Improve
Of the study’s 171 patients, 20 had IBS-diarrhea, 23 had IBS-constipation, 32 had IBS-mixed, and 8 had IBS-unspecified. The remaining 88 patients reported IBS without indication of subtype.
At intake, all patients had active IBS symptoms, with scores ≥ 75 on the IBS symptom severity scale (IBS-SSS). Most patients enrolled in more than one care pathway, and 95% of participants completed at least 4 weeks on their chosen pathways.
Overall, patients saw an average 140-point decrease in IBS-SSS from intake through follow-up lasting up to 42 weeks. A drop in IBS-SSS score ≥ 50 points was considered a clinically meaningful change.
Symptom improvements occurred as early as week 4, were sustained and were uniform across IBS subtypes, suggesting that the AI-enhanced digital collaborative care model has wide utility in patients with IBS, Lupe said.
Patients with the most severe IBS symptoms showed the greatest improvement, but even 50% of those with mild symptoms had clinically meaningful changes in IBS-SSS.
Improvement in IBS symptoms was seen across all care pathways, but the combination of multiple pathways improved outcomes better than a single care pathway alone. The combination of nutrition and brain-gut behavioral therapy demonstrated the greatest reduction in IBS-SSS scores and proportion of patients achieving clinically meaningful results (95%).
The digital comprehensive car model for IBS is now “up and running” at Cleveland Clinic, and the team plans to proactively reach out to patients with gastrointestinal disorders recently seen at their center to alert them to the availability of this tool, Lupe said.
A randomized controlled trial is planned to further validate these observational findings, he added.
‘Wave of the Future’
The digital collaborative care model is “innovative, and I think is the wave of the future,” Kyle Staller, MD, MPH, gastroenterologist and director of the Gastrointestinal Motility Laboratory at Massachusetts General Hospital, Boston, who wasn’t involved in the study, told GI & Hepatology News.
“These digital platforms bundle nondrug options, such as cognitive-behavioral therapy, dietary therapy, hypnotherapy, so patients can choose what suits them, rather than the gastroenterologist hunting down each individual resource, which requires a lot of work,” Staller said.
The study “provides real-world evidence that a deliberative, digital, collaborative care model that houses various types of nondrug IBS treatment under one roof can provide meaningful benefit to patients,” Staller told GI & Hepatology News.
Importantly, he said, “patients chose which option they wanted. At the end of the day, the way that we should be thinking about IBS care is really making sure that we engage the patient with treatment choices,” Staller said.
This study had no specific funding. Three authors had relationships with Ayble Health. Lupe is a scientific advisor for Boomerang Health and paid lecturer for Takeda Pharmaceuticals. Staller disclosed having relationships with Mahana Therapeutics, Ardelyx Inc, Gemelli Biotech, Salix Pharmaceuticals, and Takeda Pharmaceuticals.
A version of this article appeared on Medscape.com.
FROM DDW 2025
IBS: Mental Health Factors and Comorbidities
IBS: Mental Health Factors and Comorbidities
Click to view more from Gastroenterology Data Trends 2025.
- Staudacher HM, Black CJ, Teasdale SB, Mikocka-Walus A, Keefer L. Irritable bowel syndrome and mental health comorbidity - approach to multidisciplinary management. Nat Rev Gastroenterol Hepatol. 2023;20(9):582-596. doi:10.1038/s41575-023-00794-z
- Ballou S, Vasant DH, Guadagnoli L, et al. A primer for the gastroenterology provider on psychosocial assessment of patients with disorders of gut-brain interaction. Neurogastroenterol Motil. 2024;36(12):e14894. doi:10.1111/nmo.14894
- Keefer L, Ballou SK, Drossman DA, Ringstrom G, Elsenbruch S, Ljótsson B. A Rome Working Team Report on Brain-Gut Behavior Therapies for Disorders of Gut-Brain Interaction. Gastroenterology. 2022;162(1):300-315. doi:10.1053/j.gastro.2021.09.015
- Goodoory VC, Khasawneh M, Thakur ER, et al. Effect of Brain-Gut Behavioral Treatments on Abdominal Pain in Irritable Bowel Syndrome: Systematic Review and Network Meta-Analysis. Gastroenterology. 2024;167(5):934-943.e5. doi:10.1053/j.gastro.2024.05.010
- Chang L, Sultan S, Lembo A, Verne GN, Smalley W, Heidelbaugh JJ. AGA Clinical Practice Guideline on the Pharmacological Management of Irritable Bowel Syndrome With Constipation. Gastroenterology. 2022;163(1):118-136. doi:10.1053/j.gastro.2022.04.016
- Drossman DA, Tack J, Ford AC, Szigethy E, Törnblom H, Van Oudenhove L. Neuromodulators for Functional Gastrointestinal Disorders (Disorders of Gut-Brain Interaction): A Rome Foundation Working Team Report. Gastroenterology. 2018;154(4):1140-1171.e1. doi:10.1053/j.gastro.2017.11.279
- Hasan SS, Ballou S, Keefer L, Vasant DH. Improving access to gut-directed hypnotherapy for irritable bowel syndrome in the digital therapeutics’ era: Are mobile applications a “smart” solution? Neurogastroenterol Motil. 2023;35(4):e14554. doi:10.1111/nmo.14554
- Tarar ZI, Farooq U, Zafar Y, et al. Burden of anxiety and depression among hospitalized patients with irritable bowel syndrome: a nationwide analysis. Ir J Med Sci. 2023;192(5):2159-2166. doi:10.1007/s11845-022-03258-6
- Barbara G, Aziz I, Ballou S, et al. Rome Foundation Working Team Report on overlap in disorders of gut-brain interaction. Nat Rev Gastroenterol Hepatol. doi:10.1038/s41575-024-01033-9
- Thakur ER, Kunik M, Jarbrink-Sehgal ME, Lackner J, Dindo L, El-Serag H. Behavior Medicine Management of Irritable Bowel Syndrome: A Referral Toolkit for Gastroenterology Providers. 2018. Accessed February 19, 2025. https://www.mirecc.va.gov/VISN16/docs/ibs-referral-toolkit.pdf
- Irritable bowel syndrome (IBS). Johns Hopkins Medicine website. Accessed February 19, 2025. https://www.hopkinsmedicine.org/health/conditionsanddiseases/irritable-bowel-syndrome-ibs
- Burton-Murray H, Guadagnoli L, Kamp K, et al. Rome Foundation Working Team Report: Consensus Statement on the Design and Conduct of Behavioural Clinical Trials for Disorders of Gut-Brain Interaction. Aliment Pharmacol Ther. 2025;61(5):787-802. doi:10.1111/apt.18482
- Rome GastroPsych. Rome Foundation website. Accessed February 19, 2025. https://romegipsych.org/
- Scarlata K, Riehl M. Mind Your Gut: The Science-based, Whole-body Guide to Living Well with IBS. Hachette Book Group, 2025.
- IFFGD International Foundation for Gastrointestinal Disorders. IFFGD website. January 10, 2025. Accessed February 19, 2025. https://iffgd.org/
- GI Psychology: Mind Your Gut website. April 2, 2024. Accessed February 19, 2025. https://www.gipsychology.com/
- Drossman DA, Ruddy J. Gut Feelings: Disorders of the Gut-Brain Interaction (DGBI) and the Patient-Doctor Relationship. DrossmanCare Chapel Hill, 2020.
- Tuesday Night IBS website. Accessed February 19, 2025. https://www.tuesdaynightibs.com/
Click to view more from Gastroenterology Data Trends 2025.
Click to view more from Gastroenterology Data Trends 2025.
- Staudacher HM, Black CJ, Teasdale SB, Mikocka-Walus A, Keefer L. Irritable bowel syndrome and mental health comorbidity - approach to multidisciplinary management. Nat Rev Gastroenterol Hepatol. 2023;20(9):582-596. doi:10.1038/s41575-023-00794-z
- Ballou S, Vasant DH, Guadagnoli L, et al. A primer for the gastroenterology provider on psychosocial assessment of patients with disorders of gut-brain interaction. Neurogastroenterol Motil. 2024;36(12):e14894. doi:10.1111/nmo.14894
- Keefer L, Ballou SK, Drossman DA, Ringstrom G, Elsenbruch S, Ljótsson B. A Rome Working Team Report on Brain-Gut Behavior Therapies for Disorders of Gut-Brain Interaction. Gastroenterology. 2022;162(1):300-315. doi:10.1053/j.gastro.2021.09.015
- Goodoory VC, Khasawneh M, Thakur ER, et al. Effect of Brain-Gut Behavioral Treatments on Abdominal Pain in Irritable Bowel Syndrome: Systematic Review and Network Meta-Analysis. Gastroenterology. 2024;167(5):934-943.e5. doi:10.1053/j.gastro.2024.05.010
- Chang L, Sultan S, Lembo A, Verne GN, Smalley W, Heidelbaugh JJ. AGA Clinical Practice Guideline on the Pharmacological Management of Irritable Bowel Syndrome With Constipation. Gastroenterology. 2022;163(1):118-136. doi:10.1053/j.gastro.2022.04.016
- Drossman DA, Tack J, Ford AC, Szigethy E, Törnblom H, Van Oudenhove L. Neuromodulators for Functional Gastrointestinal Disorders (Disorders of Gut-Brain Interaction): A Rome Foundation Working Team Report. Gastroenterology. 2018;154(4):1140-1171.e1. doi:10.1053/j.gastro.2017.11.279
- Hasan SS, Ballou S, Keefer L, Vasant DH. Improving access to gut-directed hypnotherapy for irritable bowel syndrome in the digital therapeutics’ era: Are mobile applications a “smart” solution? Neurogastroenterol Motil. 2023;35(4):e14554. doi:10.1111/nmo.14554
- Tarar ZI, Farooq U, Zafar Y, et al. Burden of anxiety and depression among hospitalized patients with irritable bowel syndrome: a nationwide analysis. Ir J Med Sci. 2023;192(5):2159-2166. doi:10.1007/s11845-022-03258-6
- Barbara G, Aziz I, Ballou S, et al. Rome Foundation Working Team Report on overlap in disorders of gut-brain interaction. Nat Rev Gastroenterol Hepatol. doi:10.1038/s41575-024-01033-9
- Thakur ER, Kunik M, Jarbrink-Sehgal ME, Lackner J, Dindo L, El-Serag H. Behavior Medicine Management of Irritable Bowel Syndrome: A Referral Toolkit for Gastroenterology Providers. 2018. Accessed February 19, 2025. https://www.mirecc.va.gov/VISN16/docs/ibs-referral-toolkit.pdf
- Irritable bowel syndrome (IBS). Johns Hopkins Medicine website. Accessed February 19, 2025. https://www.hopkinsmedicine.org/health/conditionsanddiseases/irritable-bowel-syndrome-ibs
- Burton-Murray H, Guadagnoli L, Kamp K, et al. Rome Foundation Working Team Report: Consensus Statement on the Design and Conduct of Behavioural Clinical Trials for Disorders of Gut-Brain Interaction. Aliment Pharmacol Ther. 2025;61(5):787-802. doi:10.1111/apt.18482
- Rome GastroPsych. Rome Foundation website. Accessed February 19, 2025. https://romegipsych.org/
- Scarlata K, Riehl M. Mind Your Gut: The Science-based, Whole-body Guide to Living Well with IBS. Hachette Book Group, 2025.
- IFFGD International Foundation for Gastrointestinal Disorders. IFFGD website. January 10, 2025. Accessed February 19, 2025. https://iffgd.org/
- GI Psychology: Mind Your Gut website. April 2, 2024. Accessed February 19, 2025. https://www.gipsychology.com/
- Drossman DA, Ruddy J. Gut Feelings: Disorders of the Gut-Brain Interaction (DGBI) and the Patient-Doctor Relationship. DrossmanCare Chapel Hill, 2020.
- Tuesday Night IBS website. Accessed February 19, 2025. https://www.tuesdaynightibs.com/
- Staudacher HM, Black CJ, Teasdale SB, Mikocka-Walus A, Keefer L. Irritable bowel syndrome and mental health comorbidity - approach to multidisciplinary management. Nat Rev Gastroenterol Hepatol. 2023;20(9):582-596. doi:10.1038/s41575-023-00794-z
- Ballou S, Vasant DH, Guadagnoli L, et al. A primer for the gastroenterology provider on psychosocial assessment of patients with disorders of gut-brain interaction. Neurogastroenterol Motil. 2024;36(12):e14894. doi:10.1111/nmo.14894
- Keefer L, Ballou SK, Drossman DA, Ringstrom G, Elsenbruch S, Ljótsson B. A Rome Working Team Report on Brain-Gut Behavior Therapies for Disorders of Gut-Brain Interaction. Gastroenterology. 2022;162(1):300-315. doi:10.1053/j.gastro.2021.09.015
- Goodoory VC, Khasawneh M, Thakur ER, et al. Effect of Brain-Gut Behavioral Treatments on Abdominal Pain in Irritable Bowel Syndrome: Systematic Review and Network Meta-Analysis. Gastroenterology. 2024;167(5):934-943.e5. doi:10.1053/j.gastro.2024.05.010
- Chang L, Sultan S, Lembo A, Verne GN, Smalley W, Heidelbaugh JJ. AGA Clinical Practice Guideline on the Pharmacological Management of Irritable Bowel Syndrome With Constipation. Gastroenterology. 2022;163(1):118-136. doi:10.1053/j.gastro.2022.04.016
- Drossman DA, Tack J, Ford AC, Szigethy E, Törnblom H, Van Oudenhove L. Neuromodulators for Functional Gastrointestinal Disorders (Disorders of Gut-Brain Interaction): A Rome Foundation Working Team Report. Gastroenterology. 2018;154(4):1140-1171.e1. doi:10.1053/j.gastro.2017.11.279
- Hasan SS, Ballou S, Keefer L, Vasant DH. Improving access to gut-directed hypnotherapy for irritable bowel syndrome in the digital therapeutics’ era: Are mobile applications a “smart” solution? Neurogastroenterol Motil. 2023;35(4):e14554. doi:10.1111/nmo.14554
- Tarar ZI, Farooq U, Zafar Y, et al. Burden of anxiety and depression among hospitalized patients with irritable bowel syndrome: a nationwide analysis. Ir J Med Sci. 2023;192(5):2159-2166. doi:10.1007/s11845-022-03258-6
- Barbara G, Aziz I, Ballou S, et al. Rome Foundation Working Team Report on overlap in disorders of gut-brain interaction. Nat Rev Gastroenterol Hepatol. doi:10.1038/s41575-024-01033-9
- Thakur ER, Kunik M, Jarbrink-Sehgal ME, Lackner J, Dindo L, El-Serag H. Behavior Medicine Management of Irritable Bowel Syndrome: A Referral Toolkit for Gastroenterology Providers. 2018. Accessed February 19, 2025. https://www.mirecc.va.gov/VISN16/docs/ibs-referral-toolkit.pdf
- Irritable bowel syndrome (IBS). Johns Hopkins Medicine website. Accessed February 19, 2025. https://www.hopkinsmedicine.org/health/conditionsanddiseases/irritable-bowel-syndrome-ibs
- Burton-Murray H, Guadagnoli L, Kamp K, et al. Rome Foundation Working Team Report: Consensus Statement on the Design and Conduct of Behavioural Clinical Trials for Disorders of Gut-Brain Interaction. Aliment Pharmacol Ther. 2025;61(5):787-802. doi:10.1111/apt.18482
- Rome GastroPsych. Rome Foundation website. Accessed February 19, 2025. https://romegipsych.org/
- Scarlata K, Riehl M. Mind Your Gut: The Science-based, Whole-body Guide to Living Well with IBS. Hachette Book Group, 2025.
- IFFGD International Foundation for Gastrointestinal Disorders. IFFGD website. January 10, 2025. Accessed February 19, 2025. https://iffgd.org/
- GI Psychology: Mind Your Gut website. April 2, 2024. Accessed February 19, 2025. https://www.gipsychology.com/
- Drossman DA, Ruddy J. Gut Feelings: Disorders of the Gut-Brain Interaction (DGBI) and the Patient-Doctor Relationship. DrossmanCare Chapel Hill, 2020.
- Tuesday Night IBS website. Accessed February 19, 2025. https://www.tuesdaynightibs.com/
IBS: Mental Health Factors and Comorbidities
IBS: Mental Health Factors and Comorbidities
New Fecal Product Expected to Enhance Microbiome Research
According to AGA’s Center for Gut Microbiome Research & Education, this critical resource will help advance the utility and reproducibility of microbiome-based diagnostics — “which still remain relatively meaningless clinically, although patients continue to buy direct-to-consumer tests, and a standard reference material will mean there’s a better way to ensure quality control and accuracy.”
Though not a therapeutic, Human Fecal Material RM is expected to speed up gastrointestinal (GI) therapeutics since many microbiome-based drugs are inspired by fecal transplants with human stool as the developmental starting point. A standardized reference material will be an important resource as industry develops and tests new drugs. It can be purchased online at the NIST Store (shop.nist.gov).
The product consists of eight frozen vials of exhaustively studied human feces suspended in aqueous solution. Available are more than 25 pages of data identifying the key microbes and biomolecules in the material. Scientists, including those working at biopharmaceutical and biotech companies, can use this material to further their research and develop new drugs that target the microbiome, including treatments that contain living bacteria.
Development
According to NIST, the stool material is “the most precisely measured, scientifically analyzed, and richly characterized human fecal standard ever produced.
“The project ran for about 6 years from start to finish, the last 2 for manufacturing, characterization, and writing,” said NIST molecular geneticist Scott A. Jackson, PhD, who helped develop the product. “We hope our reference material will lay the foundation for gut microbiome research to thrive and reach its full potential.”
As founder of NIST’s Complex Microbial Systems Group, Jackson is leading international efforts to improve microbiome and metagenomic measurements by organizing inter-lab studies and refining reference materials and methods.
The project collected stool from two cohorts of donors, ie, vegetarians and omnivores, with each cohort comprising four to six donors. Material from each cohort was pooled and homogenized before being aliquoted into 5000 vials per cohort. About 300 tubes from each cohort were picked, and aliquots then underwent multiomic analyses.
Offering his perspective on the new product, Sudhir K. Dutta, MBBS, associate professor in the Division of Gastroenterology and Hepatology at Johns Hopkins University School of Medicine, Baltimore, said, “This tool will be 100% useful for microbiome research.”
And according to Lori Holtz, MD, MSPH, professor of pediatric gastroenterology, hepatology, and nutrition at Washington University School of Medicine in St. Louis, Missouri, the material will aid microbiome research by allowing interpretability and repeatability across studies. “Microbiome research is a relatively new field, and protocols differ from group to group and lab to lab, so it’s been difficult to compare results across studies,” she told GI & Hepatology News. “A standard stool product will allow for greater comparability in preclinical studies and later clinical trials testing interventions to alter the microbiome.”
The NIST developers are looking forward to reaction from the GI research community. “Over the last several years, we’ve released smaller pilot batches of material to smaller groups of stakeholders,” said Jackson. “We’ve used the feedback on these earlier batches to inform the manufacturing and characterization of the final batch that was released in March, but we don’t yet have any feedback yet on the current material.”
Jackson, Dutta, and Holtz disclosed having no relevant competing interests.
A version of this article appeared on Medscape.com.
According to AGA’s Center for Gut Microbiome Research & Education, this critical resource will help advance the utility and reproducibility of microbiome-based diagnostics — “which still remain relatively meaningless clinically, although patients continue to buy direct-to-consumer tests, and a standard reference material will mean there’s a better way to ensure quality control and accuracy.”
Though not a therapeutic, Human Fecal Material RM is expected to speed up gastrointestinal (GI) therapeutics since many microbiome-based drugs are inspired by fecal transplants with human stool as the developmental starting point. A standardized reference material will be an important resource as industry develops and tests new drugs. It can be purchased online at the NIST Store (shop.nist.gov).
The product consists of eight frozen vials of exhaustively studied human feces suspended in aqueous solution. Available are more than 25 pages of data identifying the key microbes and biomolecules in the material. Scientists, including those working at biopharmaceutical and biotech companies, can use this material to further their research and develop new drugs that target the microbiome, including treatments that contain living bacteria.
Development
According to NIST, the stool material is “the most precisely measured, scientifically analyzed, and richly characterized human fecal standard ever produced.
“The project ran for about 6 years from start to finish, the last 2 for manufacturing, characterization, and writing,” said NIST molecular geneticist Scott A. Jackson, PhD, who helped develop the product. “We hope our reference material will lay the foundation for gut microbiome research to thrive and reach its full potential.”
As founder of NIST’s Complex Microbial Systems Group, Jackson is leading international efforts to improve microbiome and metagenomic measurements by organizing inter-lab studies and refining reference materials and methods.
The project collected stool from two cohorts of donors, ie, vegetarians and omnivores, with each cohort comprising four to six donors. Material from each cohort was pooled and homogenized before being aliquoted into 5000 vials per cohort. About 300 tubes from each cohort were picked, and aliquots then underwent multiomic analyses.
Offering his perspective on the new product, Sudhir K. Dutta, MBBS, associate professor in the Division of Gastroenterology and Hepatology at Johns Hopkins University School of Medicine, Baltimore, said, “This tool will be 100% useful for microbiome research.”
And according to Lori Holtz, MD, MSPH, professor of pediatric gastroenterology, hepatology, and nutrition at Washington University School of Medicine in St. Louis, Missouri, the material will aid microbiome research by allowing interpretability and repeatability across studies. “Microbiome research is a relatively new field, and protocols differ from group to group and lab to lab, so it’s been difficult to compare results across studies,” she told GI & Hepatology News. “A standard stool product will allow for greater comparability in preclinical studies and later clinical trials testing interventions to alter the microbiome.”
The NIST developers are looking forward to reaction from the GI research community. “Over the last several years, we’ve released smaller pilot batches of material to smaller groups of stakeholders,” said Jackson. “We’ve used the feedback on these earlier batches to inform the manufacturing and characterization of the final batch that was released in March, but we don’t yet have any feedback yet on the current material.”
Jackson, Dutta, and Holtz disclosed having no relevant competing interests.
A version of this article appeared on Medscape.com.
According to AGA’s Center for Gut Microbiome Research & Education, this critical resource will help advance the utility and reproducibility of microbiome-based diagnostics — “which still remain relatively meaningless clinically, although patients continue to buy direct-to-consumer tests, and a standard reference material will mean there’s a better way to ensure quality control and accuracy.”
Though not a therapeutic, Human Fecal Material RM is expected to speed up gastrointestinal (GI) therapeutics since many microbiome-based drugs are inspired by fecal transplants with human stool as the developmental starting point. A standardized reference material will be an important resource as industry develops and tests new drugs. It can be purchased online at the NIST Store (shop.nist.gov).
The product consists of eight frozen vials of exhaustively studied human feces suspended in aqueous solution. Available are more than 25 pages of data identifying the key microbes and biomolecules in the material. Scientists, including those working at biopharmaceutical and biotech companies, can use this material to further their research and develop new drugs that target the microbiome, including treatments that contain living bacteria.
Development
According to NIST, the stool material is “the most precisely measured, scientifically analyzed, and richly characterized human fecal standard ever produced.
“The project ran for about 6 years from start to finish, the last 2 for manufacturing, characterization, and writing,” said NIST molecular geneticist Scott A. Jackson, PhD, who helped develop the product. “We hope our reference material will lay the foundation for gut microbiome research to thrive and reach its full potential.”
As founder of NIST’s Complex Microbial Systems Group, Jackson is leading international efforts to improve microbiome and metagenomic measurements by organizing inter-lab studies and refining reference materials and methods.
The project collected stool from two cohorts of donors, ie, vegetarians and omnivores, with each cohort comprising four to six donors. Material from each cohort was pooled and homogenized before being aliquoted into 5000 vials per cohort. About 300 tubes from each cohort were picked, and aliquots then underwent multiomic analyses.
Offering his perspective on the new product, Sudhir K. Dutta, MBBS, associate professor in the Division of Gastroenterology and Hepatology at Johns Hopkins University School of Medicine, Baltimore, said, “This tool will be 100% useful for microbiome research.”
And according to Lori Holtz, MD, MSPH, professor of pediatric gastroenterology, hepatology, and nutrition at Washington University School of Medicine in St. Louis, Missouri, the material will aid microbiome research by allowing interpretability and repeatability across studies. “Microbiome research is a relatively new field, and protocols differ from group to group and lab to lab, so it’s been difficult to compare results across studies,” she told GI & Hepatology News. “A standard stool product will allow for greater comparability in preclinical studies and later clinical trials testing interventions to alter the microbiome.”
The NIST developers are looking forward to reaction from the GI research community. “Over the last several years, we’ve released smaller pilot batches of material to smaller groups of stakeholders,” said Jackson. “We’ve used the feedback on these earlier batches to inform the manufacturing and characterization of the final batch that was released in March, but we don’t yet have any feedback yet on the current material.”
Jackson, Dutta, and Holtz disclosed having no relevant competing interests.
A version of this article appeared on Medscape.com.