User login
‘Dramatic’ Phase 2 Results for Survodutide in MASH, Fibrosis
MILAN — , according to phase 2 results presented here at the European Association for the Study of the Liver (EASL) Congress 2024.
The data were simultaneously published in The New England Journal of Medicine .
The primary endpoint data, reported earlier this year in a press release, showed that up to 83% of participants on survodutide showed a statistically significant improvement in MASH compared with those on placebo (18.2%) based on paired biopsy results.
In addition, 75% of patients treated with survodutide experienced resolution of MASH with no worsening of fibrosis compared with 15% of patients on placebo, and in patients with F2/F3 fibrosis, 64.5% achieved improvement in fibrosis without worsening of MASH, reported Arun J. Sanyal, MD, principal study investigator and director of the Virginia Commonwealth University (VCU) Stravitz-Sanyal Institute for Liver Disease and Metabolic Health, VCU School of Medicine, Richmond, Virginia.
What’s so amazing is that this “exceptional improvement” is after 48 weeks of therapy with a class of molecule that is already known to also have cardiometabolic benefits, Dr. Sanyal said in an interview.
“At the highest dose of survodutide [6.0 mg], two thirds of patients in whom we have biopsy data, at both the beginning and the end, actually showed fibrosis regression within 48 weeks,” he said. “This is pretty dramatic.”
Efficacy and Safety of Survodutide
A total of 293 participants with biopsy-confirmed MASH and fibrosis stages F1-F3 were randomly assigned (1:1:1:1) to receive once-weekly subcutaneous injections of survodutide 2.4 mg (n = 73), 4.8 mg (n = 72), or 6.0 mg (n = 74) or placebo (n = 74).
Around half of study participants were women, with mean age around 50 years and a body mass index around 35 kg/m2. Overall, 26%-30% had type 2 diabetes, 24%-36% had F2 fibrosis, and 23%-30% had F3 fibrosis. The total Nonalcoholic Fatty Liver Disease Activity Score was 5.2.
After completing a 24-week rapid-dose-escalation phase, participants followed a 24-week maintenance phase. Histologic improvement (reduction) in MASH without worsening of fibrosis after 48 weeks of treatment comprised the primary endpoint, whereas a reduction in liver fat content by at least 30% and biopsy-assessed reduction in fibrosis by at least one stage were among the secondary endpoints.
The main analyses of the trial were based on two treatment sets: Actual treatment (the actual dose received at the start of the maintenance phase; per protocol) and planned treatment (the maintenance dose assigned to participants at randomization). Dr. Sanyal mainly reported results based on actual treatment, which were used for the primary analysis.
The overall primary endpoint data, including nonresponders, showed a 47% improvement in MASH in the 2.4-mg treatment group, 62% in the 4.8 mg group, and 43% in the 6.0-mg group compared with 13.5% in the placebo group (P < .001).
In addition, 50% of patients on 2.4- and 6-mg doses experienced a statistically significant improvement in fibrosis (F1-F3) without worsening of MASH. In patients with F2/F3 fibrosis, 64.5% of participants in the 6-mg survodutide group showed improvement vs 25.9% in the placebo group.
Reduction in liver fat by at least 30% was achieved by up to 87% in the 6-mg group according to MRI-estimated proton density fat fraction; when nonresponders were included, the percentage was 76.9% of the 6-mg group. Other outcomes included weight loss and reductions in A1c.
The results did not differ markedly between doses, which “is really exciting news,” Dr. Sanyal said.
Patients who are intolerant of the highest dose can switch to a lower dose without a big loss of efficacy, he said, adding that even the low dose was sufficient to get near maximal glucagon effect.
Adverse events were similar between survodutide and placebo, except for gastrointestinal events, including nausea, diarrhea, and vomiting. The occurrence of serious adverse events also was similar between survodutide and placebo.
Discontinuation due to adverse events was 20% across all the survodutide groups (with 16% due to gastrointestinal events) vs 3% in the placebo group.
Dual Agonist vs Monoagonist Therapy
The dual agonist approach may confer clinical advantages over GLP-1 receptor monoagonist pharmacotherapies for MASH.
“GLP has no receptors in the liver, so all its effects are mediated outside the liver, particularly for weight loss and improvement in metabolic status, increase in insulin secretion and sensitivity, and overall systemic glycemia,” Dr. Sanyal explained.
“People with established fibrosis take longer to respond in terms of downstream liver scarring with extrahepatic changes alone,” he added.
With “glucagon directly targeting the liver, we believe this reduces oxidative stress and possibly stimulates FGF-21 secretion [liver-derived factor that regulates lipid and glucose metabolism] in the liver, so there are likely multiple mechanisms driving the antifibrogenic benefits,” Dr. Sanyal said.
In comparison, the study authors highlighted that data on the GLP-1 receptor monoagonist semaglutide suggest a significantly higher proportion of patients on semaglutide achieve MASH resolution than those on placebo but that it does not result in “a significantly higher percentage of patients with improvement in fibrosis stage.
“It might be that it takes longer to get an effect in the liver with semaglutide,” Dr. Sanyal said.
By year-end, we’ll know how the GLP-1 alone approach (eg, semaglutide) and the dual agonist approach work, and we’ll eventually have data on triple agonists, Dr. Sanyal added.
The Burden of Liver Disease
Comoderator Debbie Shawcross, MBBS, PhD, professor of hepatology and chronic liver failure, King’s College, London, England, remarked on the importance of new drugs, including survodutide, in reducing the burden of steatotic liver disease.
Approximately one third of the world’s population and between 7% and 9% of children have steatotic liver disease, she noted. The buildup of fat causes inflammation and scarring of the liver, which may then progress to liver cirrhosis and primary liver cancers.
Survodutide offers much hope “as a drug that will reduce both liver inflammation and scarring, while also providing the benefit of improved diabetic control,” Dr. Shawcross said.
Reflecting on the dual agonism, she said that both the glucagon and GLP-1 receptors are critical to controlling metabolic functions.
Survodutide is currently being investigated in five phase 3 studies for people living with overweight and obesity, both of which are associated with MASH. There is also a trial looking at people with overweight/obesity with confirmed or presumed diagnosis of MASH, according to a company press release.
Dr. Sanyal reported grants, consultancy fees, and speaker fees from a wide range of companies working in the field of liver medicine. Dr. Shawcross reported no conflicts in relation to this drug and advisory board membership/consultancy for EnteroBiotix, Norgine, Satellite Bio, and MRN Health.
A version of this article first appeared on Medscape.com.
MILAN — , according to phase 2 results presented here at the European Association for the Study of the Liver (EASL) Congress 2024.
The data were simultaneously published in The New England Journal of Medicine .
The primary endpoint data, reported earlier this year in a press release, showed that up to 83% of participants on survodutide showed a statistically significant improvement in MASH compared with those on placebo (18.2%) based on paired biopsy results.
In addition, 75% of patients treated with survodutide experienced resolution of MASH with no worsening of fibrosis compared with 15% of patients on placebo, and in patients with F2/F3 fibrosis, 64.5% achieved improvement in fibrosis without worsening of MASH, reported Arun J. Sanyal, MD, principal study investigator and director of the Virginia Commonwealth University (VCU) Stravitz-Sanyal Institute for Liver Disease and Metabolic Health, VCU School of Medicine, Richmond, Virginia.
What’s so amazing is that this “exceptional improvement” is after 48 weeks of therapy with a class of molecule that is already known to also have cardiometabolic benefits, Dr. Sanyal said in an interview.
“At the highest dose of survodutide [6.0 mg], two thirds of patients in whom we have biopsy data, at both the beginning and the end, actually showed fibrosis regression within 48 weeks,” he said. “This is pretty dramatic.”
Efficacy and Safety of Survodutide
A total of 293 participants with biopsy-confirmed MASH and fibrosis stages F1-F3 were randomly assigned (1:1:1:1) to receive once-weekly subcutaneous injections of survodutide 2.4 mg (n = 73), 4.8 mg (n = 72), or 6.0 mg (n = 74) or placebo (n = 74).
Around half of study participants were women, with mean age around 50 years and a body mass index around 35 kg/m2. Overall, 26%-30% had type 2 diabetes, 24%-36% had F2 fibrosis, and 23%-30% had F3 fibrosis. The total Nonalcoholic Fatty Liver Disease Activity Score was 5.2.
After completing a 24-week rapid-dose-escalation phase, participants followed a 24-week maintenance phase. Histologic improvement (reduction) in MASH without worsening of fibrosis after 48 weeks of treatment comprised the primary endpoint, whereas a reduction in liver fat content by at least 30% and biopsy-assessed reduction in fibrosis by at least one stage were among the secondary endpoints.
The main analyses of the trial were based on two treatment sets: Actual treatment (the actual dose received at the start of the maintenance phase; per protocol) and planned treatment (the maintenance dose assigned to participants at randomization). Dr. Sanyal mainly reported results based on actual treatment, which were used for the primary analysis.
The overall primary endpoint data, including nonresponders, showed a 47% improvement in MASH in the 2.4-mg treatment group, 62% in the 4.8 mg group, and 43% in the 6.0-mg group compared with 13.5% in the placebo group (P < .001).
In addition, 50% of patients on 2.4- and 6-mg doses experienced a statistically significant improvement in fibrosis (F1-F3) without worsening of MASH. In patients with F2/F3 fibrosis, 64.5% of participants in the 6-mg survodutide group showed improvement vs 25.9% in the placebo group.
Reduction in liver fat by at least 30% was achieved by up to 87% in the 6-mg group according to MRI-estimated proton density fat fraction; when nonresponders were included, the percentage was 76.9% of the 6-mg group. Other outcomes included weight loss and reductions in A1c.
The results did not differ markedly between doses, which “is really exciting news,” Dr. Sanyal said.
Patients who are intolerant of the highest dose can switch to a lower dose without a big loss of efficacy, he said, adding that even the low dose was sufficient to get near maximal glucagon effect.
Adverse events were similar between survodutide and placebo, except for gastrointestinal events, including nausea, diarrhea, and vomiting. The occurrence of serious adverse events also was similar between survodutide and placebo.
Discontinuation due to adverse events was 20% across all the survodutide groups (with 16% due to gastrointestinal events) vs 3% in the placebo group.
Dual Agonist vs Monoagonist Therapy
The dual agonist approach may confer clinical advantages over GLP-1 receptor monoagonist pharmacotherapies for MASH.
“GLP has no receptors in the liver, so all its effects are mediated outside the liver, particularly for weight loss and improvement in metabolic status, increase in insulin secretion and sensitivity, and overall systemic glycemia,” Dr. Sanyal explained.
“People with established fibrosis take longer to respond in terms of downstream liver scarring with extrahepatic changes alone,” he added.
With “glucagon directly targeting the liver, we believe this reduces oxidative stress and possibly stimulates FGF-21 secretion [liver-derived factor that regulates lipid and glucose metabolism] in the liver, so there are likely multiple mechanisms driving the antifibrogenic benefits,” Dr. Sanyal said.
In comparison, the study authors highlighted that data on the GLP-1 receptor monoagonist semaglutide suggest a significantly higher proportion of patients on semaglutide achieve MASH resolution than those on placebo but that it does not result in “a significantly higher percentage of patients with improvement in fibrosis stage.
“It might be that it takes longer to get an effect in the liver with semaglutide,” Dr. Sanyal said.
By year-end, we’ll know how the GLP-1 alone approach (eg, semaglutide) and the dual agonist approach work, and we’ll eventually have data on triple agonists, Dr. Sanyal added.
The Burden of Liver Disease
Comoderator Debbie Shawcross, MBBS, PhD, professor of hepatology and chronic liver failure, King’s College, London, England, remarked on the importance of new drugs, including survodutide, in reducing the burden of steatotic liver disease.
Approximately one third of the world’s population and between 7% and 9% of children have steatotic liver disease, she noted. The buildup of fat causes inflammation and scarring of the liver, which may then progress to liver cirrhosis and primary liver cancers.
Survodutide offers much hope “as a drug that will reduce both liver inflammation and scarring, while also providing the benefit of improved diabetic control,” Dr. Shawcross said.
Reflecting on the dual agonism, she said that both the glucagon and GLP-1 receptors are critical to controlling metabolic functions.
Survodutide is currently being investigated in five phase 3 studies for people living with overweight and obesity, both of which are associated with MASH. There is also a trial looking at people with overweight/obesity with confirmed or presumed diagnosis of MASH, according to a company press release.
Dr. Sanyal reported grants, consultancy fees, and speaker fees from a wide range of companies working in the field of liver medicine. Dr. Shawcross reported no conflicts in relation to this drug and advisory board membership/consultancy for EnteroBiotix, Norgine, Satellite Bio, and MRN Health.
A version of this article first appeared on Medscape.com.
MILAN — , according to phase 2 results presented here at the European Association for the Study of the Liver (EASL) Congress 2024.
The data were simultaneously published in The New England Journal of Medicine .
The primary endpoint data, reported earlier this year in a press release, showed that up to 83% of participants on survodutide showed a statistically significant improvement in MASH compared with those on placebo (18.2%) based on paired biopsy results.
In addition, 75% of patients treated with survodutide experienced resolution of MASH with no worsening of fibrosis compared with 15% of patients on placebo, and in patients with F2/F3 fibrosis, 64.5% achieved improvement in fibrosis without worsening of MASH, reported Arun J. Sanyal, MD, principal study investigator and director of the Virginia Commonwealth University (VCU) Stravitz-Sanyal Institute for Liver Disease and Metabolic Health, VCU School of Medicine, Richmond, Virginia.
What’s so amazing is that this “exceptional improvement” is after 48 weeks of therapy with a class of molecule that is already known to also have cardiometabolic benefits, Dr. Sanyal said in an interview.
“At the highest dose of survodutide [6.0 mg], two thirds of patients in whom we have biopsy data, at both the beginning and the end, actually showed fibrosis regression within 48 weeks,” he said. “This is pretty dramatic.”
Efficacy and Safety of Survodutide
A total of 293 participants with biopsy-confirmed MASH and fibrosis stages F1-F3 were randomly assigned (1:1:1:1) to receive once-weekly subcutaneous injections of survodutide 2.4 mg (n = 73), 4.8 mg (n = 72), or 6.0 mg (n = 74) or placebo (n = 74).
Around half of study participants were women, with mean age around 50 years and a body mass index around 35 kg/m2. Overall, 26%-30% had type 2 diabetes, 24%-36% had F2 fibrosis, and 23%-30% had F3 fibrosis. The total Nonalcoholic Fatty Liver Disease Activity Score was 5.2.
After completing a 24-week rapid-dose-escalation phase, participants followed a 24-week maintenance phase. Histologic improvement (reduction) in MASH without worsening of fibrosis after 48 weeks of treatment comprised the primary endpoint, whereas a reduction in liver fat content by at least 30% and biopsy-assessed reduction in fibrosis by at least one stage were among the secondary endpoints.
The main analyses of the trial were based on two treatment sets: Actual treatment (the actual dose received at the start of the maintenance phase; per protocol) and planned treatment (the maintenance dose assigned to participants at randomization). Dr. Sanyal mainly reported results based on actual treatment, which were used for the primary analysis.
The overall primary endpoint data, including nonresponders, showed a 47% improvement in MASH in the 2.4-mg treatment group, 62% in the 4.8 mg group, and 43% in the 6.0-mg group compared with 13.5% in the placebo group (P < .001).
In addition, 50% of patients on 2.4- and 6-mg doses experienced a statistically significant improvement in fibrosis (F1-F3) without worsening of MASH. In patients with F2/F3 fibrosis, 64.5% of participants in the 6-mg survodutide group showed improvement vs 25.9% in the placebo group.
Reduction in liver fat by at least 30% was achieved by up to 87% in the 6-mg group according to MRI-estimated proton density fat fraction; when nonresponders were included, the percentage was 76.9% of the 6-mg group. Other outcomes included weight loss and reductions in A1c.
The results did not differ markedly between doses, which “is really exciting news,” Dr. Sanyal said.
Patients who are intolerant of the highest dose can switch to a lower dose without a big loss of efficacy, he said, adding that even the low dose was sufficient to get near maximal glucagon effect.
Adverse events were similar between survodutide and placebo, except for gastrointestinal events, including nausea, diarrhea, and vomiting. The occurrence of serious adverse events also was similar between survodutide and placebo.
Discontinuation due to adverse events was 20% across all the survodutide groups (with 16% due to gastrointestinal events) vs 3% in the placebo group.
Dual Agonist vs Monoagonist Therapy
The dual agonist approach may confer clinical advantages over GLP-1 receptor monoagonist pharmacotherapies for MASH.
“GLP has no receptors in the liver, so all its effects are mediated outside the liver, particularly for weight loss and improvement in metabolic status, increase in insulin secretion and sensitivity, and overall systemic glycemia,” Dr. Sanyal explained.
“People with established fibrosis take longer to respond in terms of downstream liver scarring with extrahepatic changes alone,” he added.
With “glucagon directly targeting the liver, we believe this reduces oxidative stress and possibly stimulates FGF-21 secretion [liver-derived factor that regulates lipid and glucose metabolism] in the liver, so there are likely multiple mechanisms driving the antifibrogenic benefits,” Dr. Sanyal said.
In comparison, the study authors highlighted that data on the GLP-1 receptor monoagonist semaglutide suggest a significantly higher proportion of patients on semaglutide achieve MASH resolution than those on placebo but that it does not result in “a significantly higher percentage of patients with improvement in fibrosis stage.
“It might be that it takes longer to get an effect in the liver with semaglutide,” Dr. Sanyal said.
By year-end, we’ll know how the GLP-1 alone approach (eg, semaglutide) and the dual agonist approach work, and we’ll eventually have data on triple agonists, Dr. Sanyal added.
The Burden of Liver Disease
Comoderator Debbie Shawcross, MBBS, PhD, professor of hepatology and chronic liver failure, King’s College, London, England, remarked on the importance of new drugs, including survodutide, in reducing the burden of steatotic liver disease.
Approximately one third of the world’s population and between 7% and 9% of children have steatotic liver disease, she noted. The buildup of fat causes inflammation and scarring of the liver, which may then progress to liver cirrhosis and primary liver cancers.
Survodutide offers much hope “as a drug that will reduce both liver inflammation and scarring, while also providing the benefit of improved diabetic control,” Dr. Shawcross said.
Reflecting on the dual agonism, she said that both the glucagon and GLP-1 receptors are critical to controlling metabolic functions.
Survodutide is currently being investigated in five phase 3 studies for people living with overweight and obesity, both of which are associated with MASH. There is also a trial looking at people with overweight/obesity with confirmed or presumed diagnosis of MASH, according to a company press release.
Dr. Sanyal reported grants, consultancy fees, and speaker fees from a wide range of companies working in the field of liver medicine. Dr. Shawcross reported no conflicts in relation to this drug and advisory board membership/consultancy for EnteroBiotix, Norgine, Satellite Bio, and MRN Health.
A version of this article first appeared on Medscape.com.
FROM EASL 2024
Seladelpar Shows Clinically Meaningful Improvements in PBC
MILAN — according to two interim analyses of the ASSURE long-term extension study.
The first analysis of 337 patients with PBC, with and without cirrhosis, showed that treatment with seladelpar had a durable effect up to 2 years on cholestasis and markers of liver injury, as well as a sustained reduction in pruritus, Palak Trivedi, MD, associate professor at the National Institute for Health Research Birmingham Biomedical Research Centre, University of Birmingham, Birmingham, England, reported in a poster presented at the European Association for the Study of the Liver (EASL) Congress 2024.
The 2-year analysis also showed that seladelpar, a first-in-class, orally active agent, was safe and well tolerated in this patient population, he added.
These “results are consistent with the pivotal phase 3 RESPONSE study,” Dr. Trivedi noted. The RESPONSE study showed that seladelpar significantly improved liver biomarkers of disease activity and symptoms of pruritus at 12 months in patients with PBC who had an inadequate response or intolerance to ursodeoxycholic acid (UDCA), the standard of care, and had no history of hepatic decompensation. Patients with cirrhosis were allowed to enroll.
A total of 158 patients from the RESPONSE trial, both from the placebo and from the active treatment arm, were rolled over into the ASSURE trial. Another subset of 179 patients were drawn from prior seladelpar placebo-controlled studies (referred to as “legacy studies”), including the ENHANCE study. All participants in the current analysis received 10 mg of seladelpar, once daily, for up to 155 weeks.
Of the participants from the legacy studies, 99 completed 24 months of treatment with seladelpar, and 164 completed 12 months of treatment. In the 24-month treatment group, 70% met the composite response endpoint, which included alkaline phosphatase (ALP) levels below 1.67 times the upper limit of normal, a decrease in ALP levels of at least 15%, and total bilirubin levels at or below the upper limit of normal, according to a press release of the study findings. In addition, 42% of these participants achieved ALP normalization at 24 months, a marker of liver disease progression. In the 12-month treatment group, 73% achieved the clinically meaningful composite response endpoint, with 42% experiencing ALP normalization.
For patients rolled over from RESPONSE, 102 received 18 months of treatment with seladelpar, and 29 received 24 months of treatment. A total of 62% of patients in the 18-month group achieved the composite endpoint, and 33% achieved ALP normalization, while 72% of the 24-month group reached the composite endpoint, and 17% had ALP normalization.
Of patients who had received a placebo in the RESPONSE trial and went on to receive treatment with seladelpar, 75% achieved the composite endpoint, 27% had ALP normalization at 6 months, and 94% achieved the composite endpoint and 50% reached ALP normalization at 12 months.
Key secondary endpoints included ALP normalization and changes in liver enzymes (ALP, total bilirubin, gamma-glutamyl transferase [GGT], alanine transaminase [ALT], and aspartate aminotransferase [AST]).
Pruritus Relief Important for Quality of Life
Among study participants who reported a four or more at baseline on the numerical rating scale (NRS) for pruritus, legacy patients at 12 months and 24 months of treatment reported a mean reduction of 3.8 and 3.1, respectively. Participants from RESPONSE also reported a mean reduction of 3.8.
This level of reduction in NRS is “considered clinically significant” and takes patients from a level of moderate to severe itching down to mild, said Carrie Frenette, MD, executive director, Global Medical Affairs, Liver Diseases, Gilead Sciences, Foster City, California, and a former hepatologist of 20 years with a special interest in liver transplantation.
This “is a huge benefit in quality of life for these patients,” Dr. Frenette said in an interview.
Dr. Frenette also noted that UDCA, the current first-line treatment for PBC, is inadequate in up to 40% of patients, and second-line treatments, notably obeticholic acid, can cause itching.
Eleonora De Martin, MD, transplant hepatologist at Centre Hépato-Biliaire, Paul Brousse Hospital, Paris, France, who comoderated the session, pointed out that PBC is a complex disease.
“We need both disease control and symptom control, and they’re not always compatible,” she said. “Sometimes you can control the disease but not the symptoms, and symptomatic control is so important,” especially with pruritus.
Patients With PBC and Cirrhosis
A separate analysis from ASSURE looked at a subset of 17 patients with PBC and cirrhosis who completed 24 months of treatment. The findings were presented by Stuart Gordon, MD, professor of medicine, Wayne State University School of Medicine, and hepatologist at Henry Ford Hospital, both in Detroit.
In this analysis, the mean patient age was 60.8 years, 91.4% were female, 88.6% were Child-Pugh A, and 22.9% had portal hypertension, while the mean baseline liver stiffness by FibroScan was 19.9 kPa.
Baseline biochemical measures were mean ALP of 245.4 U/L, mean total bilirubin of 0.995 mg/dL, mean GGT of 216.1 U/L, and mean ALT of 36.6 U/L.
A total of 11 participants (65%) met the composite endpoint at 24 months, with ALP normalization in 4 patients (24%). The overall mean percent change from baseline in ALP was approximately −30% and in total bilirubin was around −14%. Other changes in biochemical markers included reductions from baseline in GGT and ALT of approximately −30% and −10%, respectively. No change was observed in AST.
While 80% of patients with cirrhosis “had an adverse event of some form,” there were no treatment-related serious adverse events.
“It’s interesting to see results in these patients who have advanced disease and are cirrhotic because it might stabilize disease or even provide improvement,” Dr. De Martin commented. “However, the numbers in the study are very small, so it’s hard to draw firm conclusions yet, but it is a first step in showing that this drug is safe.”
Seladelpar is an “important step forward in PBC because we’ve been stuck with ursodeoxycholic acid for so many years,” Dr. De Martin added. “We’ve seen in liver disease with other etiologies that sometimes just one drug can make a difference, and you can change the natural history of the disease.”
Dr. Frenette is an employee and stockholder of Gilead Sciences. Dr. Gordon declared grants and support from AbbVie, Arbutus, CymaBay, Cour Pharmaceuticals, GlaxoSmithKline (GSK), Ipsen, and Mirum Pharmaceuticals; and advisory board activity from CymaBay, GSK, and Ipsen Pharmaceuticals. Dr. De Martin had no disclosures of relevance to seladelpar but has received speaker fees from other companies, including GSK, Ipsen, and Astellas. Dr. Trivedi reports institutional funding support from National Institute for Health Research Birmingham (UK); lecture fees from Advanz Pharma/Intercept Pharmaceuticals, Albireo/Ipsen, and Dr. Falk Pharma; advisory board/consulting fees from Advanz Pharma/Intercept Pharmaceuticals, Albireo/Ipsen, Chemomab Therapeutics, CymaBay, Dr. Falk Pharma, Gilead Sciences, Perspectum, and Pliant Therapeutics; and grant support from Advanz Pharma/Intercept Pharmaceuticals, Albireo/Ipsen, Bristol-Myers Squibb, Core (Guts UK), EASL, Gilead Sciences, GSK, LifeArc, NIHR, Mirum Pharma, PSC Support, The Wellcome Trust, The Medical Research Foundation (UK), and Regeneron.
A version of this article first appeared on Medscape.com.
MILAN — according to two interim analyses of the ASSURE long-term extension study.
The first analysis of 337 patients with PBC, with and without cirrhosis, showed that treatment with seladelpar had a durable effect up to 2 years on cholestasis and markers of liver injury, as well as a sustained reduction in pruritus, Palak Trivedi, MD, associate professor at the National Institute for Health Research Birmingham Biomedical Research Centre, University of Birmingham, Birmingham, England, reported in a poster presented at the European Association for the Study of the Liver (EASL) Congress 2024.
The 2-year analysis also showed that seladelpar, a first-in-class, orally active agent, was safe and well tolerated in this patient population, he added.
These “results are consistent with the pivotal phase 3 RESPONSE study,” Dr. Trivedi noted. The RESPONSE study showed that seladelpar significantly improved liver biomarkers of disease activity and symptoms of pruritus at 12 months in patients with PBC who had an inadequate response or intolerance to ursodeoxycholic acid (UDCA), the standard of care, and had no history of hepatic decompensation. Patients with cirrhosis were allowed to enroll.
A total of 158 patients from the RESPONSE trial, both from the placebo and from the active treatment arm, were rolled over into the ASSURE trial. Another subset of 179 patients were drawn from prior seladelpar placebo-controlled studies (referred to as “legacy studies”), including the ENHANCE study. All participants in the current analysis received 10 mg of seladelpar, once daily, for up to 155 weeks.
Of the participants from the legacy studies, 99 completed 24 months of treatment with seladelpar, and 164 completed 12 months of treatment. In the 24-month treatment group, 70% met the composite response endpoint, which included alkaline phosphatase (ALP) levels below 1.67 times the upper limit of normal, a decrease in ALP levels of at least 15%, and total bilirubin levels at or below the upper limit of normal, according to a press release of the study findings. In addition, 42% of these participants achieved ALP normalization at 24 months, a marker of liver disease progression. In the 12-month treatment group, 73% achieved the clinically meaningful composite response endpoint, with 42% experiencing ALP normalization.
For patients rolled over from RESPONSE, 102 received 18 months of treatment with seladelpar, and 29 received 24 months of treatment. A total of 62% of patients in the 18-month group achieved the composite endpoint, and 33% achieved ALP normalization, while 72% of the 24-month group reached the composite endpoint, and 17% had ALP normalization.
Of patients who had received a placebo in the RESPONSE trial and went on to receive treatment with seladelpar, 75% achieved the composite endpoint, 27% had ALP normalization at 6 months, and 94% achieved the composite endpoint and 50% reached ALP normalization at 12 months.
Key secondary endpoints included ALP normalization and changes in liver enzymes (ALP, total bilirubin, gamma-glutamyl transferase [GGT], alanine transaminase [ALT], and aspartate aminotransferase [AST]).
Pruritus Relief Important for Quality of Life
Among study participants who reported a four or more at baseline on the numerical rating scale (NRS) for pruritus, legacy patients at 12 months and 24 months of treatment reported a mean reduction of 3.8 and 3.1, respectively. Participants from RESPONSE also reported a mean reduction of 3.8.
This level of reduction in NRS is “considered clinically significant” and takes patients from a level of moderate to severe itching down to mild, said Carrie Frenette, MD, executive director, Global Medical Affairs, Liver Diseases, Gilead Sciences, Foster City, California, and a former hepatologist of 20 years with a special interest in liver transplantation.
This “is a huge benefit in quality of life for these patients,” Dr. Frenette said in an interview.
Dr. Frenette also noted that UDCA, the current first-line treatment for PBC, is inadequate in up to 40% of patients, and second-line treatments, notably obeticholic acid, can cause itching.
Eleonora De Martin, MD, transplant hepatologist at Centre Hépato-Biliaire, Paul Brousse Hospital, Paris, France, who comoderated the session, pointed out that PBC is a complex disease.
“We need both disease control and symptom control, and they’re not always compatible,” she said. “Sometimes you can control the disease but not the symptoms, and symptomatic control is so important,” especially with pruritus.
Patients With PBC and Cirrhosis
A separate analysis from ASSURE looked at a subset of 17 patients with PBC and cirrhosis who completed 24 months of treatment. The findings were presented by Stuart Gordon, MD, professor of medicine, Wayne State University School of Medicine, and hepatologist at Henry Ford Hospital, both in Detroit.
In this analysis, the mean patient age was 60.8 years, 91.4% were female, 88.6% were Child-Pugh A, and 22.9% had portal hypertension, while the mean baseline liver stiffness by FibroScan was 19.9 kPa.
Baseline biochemical measures were mean ALP of 245.4 U/L, mean total bilirubin of 0.995 mg/dL, mean GGT of 216.1 U/L, and mean ALT of 36.6 U/L.
A total of 11 participants (65%) met the composite endpoint at 24 months, with ALP normalization in 4 patients (24%). The overall mean percent change from baseline in ALP was approximately −30% and in total bilirubin was around −14%. Other changes in biochemical markers included reductions from baseline in GGT and ALT of approximately −30% and −10%, respectively. No change was observed in AST.
While 80% of patients with cirrhosis “had an adverse event of some form,” there were no treatment-related serious adverse events.
“It’s interesting to see results in these patients who have advanced disease and are cirrhotic because it might stabilize disease or even provide improvement,” Dr. De Martin commented. “However, the numbers in the study are very small, so it’s hard to draw firm conclusions yet, but it is a first step in showing that this drug is safe.”
Seladelpar is an “important step forward in PBC because we’ve been stuck with ursodeoxycholic acid for so many years,” Dr. De Martin added. “We’ve seen in liver disease with other etiologies that sometimes just one drug can make a difference, and you can change the natural history of the disease.”
Dr. Frenette is an employee and stockholder of Gilead Sciences. Dr. Gordon declared grants and support from AbbVie, Arbutus, CymaBay, Cour Pharmaceuticals, GlaxoSmithKline (GSK), Ipsen, and Mirum Pharmaceuticals; and advisory board activity from CymaBay, GSK, and Ipsen Pharmaceuticals. Dr. De Martin had no disclosures of relevance to seladelpar but has received speaker fees from other companies, including GSK, Ipsen, and Astellas. Dr. Trivedi reports institutional funding support from National Institute for Health Research Birmingham (UK); lecture fees from Advanz Pharma/Intercept Pharmaceuticals, Albireo/Ipsen, and Dr. Falk Pharma; advisory board/consulting fees from Advanz Pharma/Intercept Pharmaceuticals, Albireo/Ipsen, Chemomab Therapeutics, CymaBay, Dr. Falk Pharma, Gilead Sciences, Perspectum, and Pliant Therapeutics; and grant support from Advanz Pharma/Intercept Pharmaceuticals, Albireo/Ipsen, Bristol-Myers Squibb, Core (Guts UK), EASL, Gilead Sciences, GSK, LifeArc, NIHR, Mirum Pharma, PSC Support, The Wellcome Trust, The Medical Research Foundation (UK), and Regeneron.
A version of this article first appeared on Medscape.com.
MILAN — according to two interim analyses of the ASSURE long-term extension study.
The first analysis of 337 patients with PBC, with and without cirrhosis, showed that treatment with seladelpar had a durable effect up to 2 years on cholestasis and markers of liver injury, as well as a sustained reduction in pruritus, Palak Trivedi, MD, associate professor at the National Institute for Health Research Birmingham Biomedical Research Centre, University of Birmingham, Birmingham, England, reported in a poster presented at the European Association for the Study of the Liver (EASL) Congress 2024.
The 2-year analysis also showed that seladelpar, a first-in-class, orally active agent, was safe and well tolerated in this patient population, he added.
These “results are consistent with the pivotal phase 3 RESPONSE study,” Dr. Trivedi noted. The RESPONSE study showed that seladelpar significantly improved liver biomarkers of disease activity and symptoms of pruritus at 12 months in patients with PBC who had an inadequate response or intolerance to ursodeoxycholic acid (UDCA), the standard of care, and had no history of hepatic decompensation. Patients with cirrhosis were allowed to enroll.
A total of 158 patients from the RESPONSE trial, both from the placebo and from the active treatment arm, were rolled over into the ASSURE trial. Another subset of 179 patients were drawn from prior seladelpar placebo-controlled studies (referred to as “legacy studies”), including the ENHANCE study. All participants in the current analysis received 10 mg of seladelpar, once daily, for up to 155 weeks.
Of the participants from the legacy studies, 99 completed 24 months of treatment with seladelpar, and 164 completed 12 months of treatment. In the 24-month treatment group, 70% met the composite response endpoint, which included alkaline phosphatase (ALP) levels below 1.67 times the upper limit of normal, a decrease in ALP levels of at least 15%, and total bilirubin levels at or below the upper limit of normal, according to a press release of the study findings. In addition, 42% of these participants achieved ALP normalization at 24 months, a marker of liver disease progression. In the 12-month treatment group, 73% achieved the clinically meaningful composite response endpoint, with 42% experiencing ALP normalization.
For patients rolled over from RESPONSE, 102 received 18 months of treatment with seladelpar, and 29 received 24 months of treatment. A total of 62% of patients in the 18-month group achieved the composite endpoint, and 33% achieved ALP normalization, while 72% of the 24-month group reached the composite endpoint, and 17% had ALP normalization.
Of patients who had received a placebo in the RESPONSE trial and went on to receive treatment with seladelpar, 75% achieved the composite endpoint, 27% had ALP normalization at 6 months, and 94% achieved the composite endpoint and 50% reached ALP normalization at 12 months.
Key secondary endpoints included ALP normalization and changes in liver enzymes (ALP, total bilirubin, gamma-glutamyl transferase [GGT], alanine transaminase [ALT], and aspartate aminotransferase [AST]).
Pruritus Relief Important for Quality of Life
Among study participants who reported a four or more at baseline on the numerical rating scale (NRS) for pruritus, legacy patients at 12 months and 24 months of treatment reported a mean reduction of 3.8 and 3.1, respectively. Participants from RESPONSE also reported a mean reduction of 3.8.
This level of reduction in NRS is “considered clinically significant” and takes patients from a level of moderate to severe itching down to mild, said Carrie Frenette, MD, executive director, Global Medical Affairs, Liver Diseases, Gilead Sciences, Foster City, California, and a former hepatologist of 20 years with a special interest in liver transplantation.
This “is a huge benefit in quality of life for these patients,” Dr. Frenette said in an interview.
Dr. Frenette also noted that UDCA, the current first-line treatment for PBC, is inadequate in up to 40% of patients, and second-line treatments, notably obeticholic acid, can cause itching.
Eleonora De Martin, MD, transplant hepatologist at Centre Hépato-Biliaire, Paul Brousse Hospital, Paris, France, who comoderated the session, pointed out that PBC is a complex disease.
“We need both disease control and symptom control, and they’re not always compatible,” she said. “Sometimes you can control the disease but not the symptoms, and symptomatic control is so important,” especially with pruritus.
Patients With PBC and Cirrhosis
A separate analysis from ASSURE looked at a subset of 17 patients with PBC and cirrhosis who completed 24 months of treatment. The findings were presented by Stuart Gordon, MD, professor of medicine, Wayne State University School of Medicine, and hepatologist at Henry Ford Hospital, both in Detroit.
In this analysis, the mean patient age was 60.8 years, 91.4% were female, 88.6% were Child-Pugh A, and 22.9% had portal hypertension, while the mean baseline liver stiffness by FibroScan was 19.9 kPa.
Baseline biochemical measures were mean ALP of 245.4 U/L, mean total bilirubin of 0.995 mg/dL, mean GGT of 216.1 U/L, and mean ALT of 36.6 U/L.
A total of 11 participants (65%) met the composite endpoint at 24 months, with ALP normalization in 4 patients (24%). The overall mean percent change from baseline in ALP was approximately −30% and in total bilirubin was around −14%. Other changes in biochemical markers included reductions from baseline in GGT and ALT of approximately −30% and −10%, respectively. No change was observed in AST.
While 80% of patients with cirrhosis “had an adverse event of some form,” there were no treatment-related serious adverse events.
“It’s interesting to see results in these patients who have advanced disease and are cirrhotic because it might stabilize disease or even provide improvement,” Dr. De Martin commented. “However, the numbers in the study are very small, so it’s hard to draw firm conclusions yet, but it is a first step in showing that this drug is safe.”
Seladelpar is an “important step forward in PBC because we’ve been stuck with ursodeoxycholic acid for so many years,” Dr. De Martin added. “We’ve seen in liver disease with other etiologies that sometimes just one drug can make a difference, and you can change the natural history of the disease.”
Dr. Frenette is an employee and stockholder of Gilead Sciences. Dr. Gordon declared grants and support from AbbVie, Arbutus, CymaBay, Cour Pharmaceuticals, GlaxoSmithKline (GSK), Ipsen, and Mirum Pharmaceuticals; and advisory board activity from CymaBay, GSK, and Ipsen Pharmaceuticals. Dr. De Martin had no disclosures of relevance to seladelpar but has received speaker fees from other companies, including GSK, Ipsen, and Astellas. Dr. Trivedi reports institutional funding support from National Institute for Health Research Birmingham (UK); lecture fees from Advanz Pharma/Intercept Pharmaceuticals, Albireo/Ipsen, and Dr. Falk Pharma; advisory board/consulting fees from Advanz Pharma/Intercept Pharmaceuticals, Albireo/Ipsen, Chemomab Therapeutics, CymaBay, Dr. Falk Pharma, Gilead Sciences, Perspectum, and Pliant Therapeutics; and grant support from Advanz Pharma/Intercept Pharmaceuticals, Albireo/Ipsen, Bristol-Myers Squibb, Core (Guts UK), EASL, Gilead Sciences, GSK, LifeArc, NIHR, Mirum Pharma, PSC Support, The Wellcome Trust, The Medical Research Foundation (UK), and Regeneron.
A version of this article first appeared on Medscape.com.
FROM EASL 2024
Tirzepatide Shows Improvements in MASH Resolution, Fibrosis
MILAN — , according to the results of the phase 2 SYNERGY-NASH trial.
Specifically, 44%-62% of participants with MASH and moderate or severe fibrosis treated with 5-15 mg of tirzepatide achieved MASH resolution without worsening of fibrosis compared with 10% on placebo; 51%-55% of those on tirzepatide achieved at least one stage of fibrosis improvement without worsening of MASH compared with 30% on placebo. Tirzepatide also led to weight loss.
The study (Abstract LBO-001) was presented at the European Association for the Study of the Liver (EASL) Congress 2024 by Rohit Loomba, MD, professor of medicine, NAFLD Research Center, University of California at San Diego in La Jolla, and published simultaneously in The New England Journal of Medicine.
“The results are clinically meaningful,” Dr. Loomba said in an interview.
Both of the endpoints — improvements in MASH resolution and fibrosis — are considered approvable endpoints for MASH therapeutic development, and therefore, increase the likelihood of success of using such a strategy in a phase 3 setting, Dr. Loomba said.
MASH Resolution, No Worsening of Fibrosis
The dose-finding, multicenter, double-blind, placebo-controlled trial randomly assigned a total of 190 participants to receive once-weekly subcutaneous tirzepatide (5 mg, 10 mg, or 15 mg) or placebo for 52 weeks. Participants had biopsy-confirmed MASH and stage F2 or F3 (moderate or severe) fibrosis.
Overall, approximately 42% of participants had F2 fibrosis and over 57% had F3 fibrosis. The proportion of F3 fibrosis was numerically higher in the placebo (64.6%) and 5-mg tirzepatide (63.8%) groups.
The mean age of the study cohort was 54 years; 57% were female, 86% were White, and 36% were Hispanic; the mean body mass index was 36; 58% had type 2 diabetes; and A1c was 6.5. NAFLD activity score (NAS) was 5.3. Baseline noninvasive test results were consistent with the study population of MASH with F2/F3 fibrosis and NAS ≥ 4.
The primary endpoint was resolution of MASH without worsening of fibrosis at 52 weeks, and the key secondary endpoint was an improvement (decrease) of at least one fibrosis stage without worsening of MASH. Other secondary endpoints included a ≥ 2-point decrease in NAS with ≤ 1-point decrease in two or more NAS components.
A total of 157 participants (83%) underwent liver biopsies at week 52, providing results for the current analysis.
Among tirzepatide-treated patients, 43.6% in the 5-mg group, 55.5% in the 10-mg group, and 62.4% in the 15-mg group met the criteria for resolution of MASH without worsening of fibrosis compared with 10% in the placebo group (P < .001 for all three comparisons).
Fibrosis improved by at least one stage without worsening of MASH in 54.9% of participants in the 5-mg tirzepatide group, 51.3% in the 10-mg tirzepatide group, and 51.0% in the 15-mg tirzepatide group compared with 29.7% in the placebo group (P < .001 for all risk differences with placebo).
Changes in NAS and subscores for the individual components of NAS, including steatosis, lobular inflammation, and hepatocellular ballooning, were also seen in participants on tirzepatide.
The researchers used a composite endpoint of a ≥ 2-point decrease in NAS with a ≥ 1-point decrease in at least two NAS components. Of the tirzepatide-treated groups, 71.7%,78.3%, and 76.6% in the 5-mg, 10-mg, and 15-mg groups, respectively, met this endpoint compared with 36.7% in placebo.
Imaging of liver fat with MRI-based proton density fat fraction (MRI-PDFF) showed reductions from baseline of -45.7, -41.3, -57.0 in participants on 5-mg, 10-mg, and 15-mg tirzepatide, respectively. Differences from placebo were all statistically significant.
Percentage of body weight change from baseline was -10.7%, -13.3%, and -15.6% in the 5-mg, 10-mg, and 15-mg tirzepatide groups, respectively, compared with weight loss of -0.8% in the placebo group.
“Tirzepatide led to significant weight loss in both patients with diabetes and those without diabetes,” reported Dr. Loomba.
There were more adverse events in patients on tirzepatide (92.3%) compared with patients on placebo (83.3%).
“The most common adverse events were gastrointestinal in nature, with 96% of them mild to moderate in severity,” said Dr. Loomba. “Discontinuations occurred in 4.2% of participants, which was similar between patients on tirzepatide and those on placebo.”
He pointed out that the safety profile of tirzepatide in a MASH population “was generally similar to that observed in the phase 3 trials of type 2 diabetes and obesity.”
Incidence of serious adverse events was also similar at 6.3% for participants on tirzepatide vs 6.2% for those on placebo; 2.8% on tirzepatide and 4.2% on placebo progressed to cirrhosis. There was no evidence of drug-induced liver injury.
‘Convincing Results’
Commenting on the study, co-moderator Sven Francque, MD, hepatologist and head of department at the University Hospital of Antwerp, Belgium, said that the study was in a relatively “severe” patient population, which was one of its strengths.
“These are convincing results in terms of MASH resolution, showing a strong response and dose-dependence,” he said.
“In terms of fibrosis, the results look numerically strong but are somewhat more puzzling to interpret, as there was no dose-response relationship and no data on NITs [noninvasive tests] that could support the results,” he added.
“Patients with no-end-of-treatment biopsies were handled differently than in previous trials, which makes it difficult to appreciate antifibrotic potency,” he said. But “such a strong effect on MASH should translate into a reduction in fibrosis even in the absence of direct antifibrotic effects.”
Given that “about one third of patients in the active treatment arms” did not have end-of-treatment biopsy, these “are rather small numbers precluding firm conclusions,” he added.
However, Dr. Francque said that he believes the findings are compelling enough for the drug to go into phase 3 trials.
Dr. Francque has no disclosures of relevance to this study. Dr. Loomba serves as a consultant to Aardvark Therapeutics, Altimmune, Anylam/Regeneron, Amgen, Arrowhead Pharmaceuticals, AstraZeneca, Bristol Myers Squibb, CohBar, Eli Lilly, Galmed, Gilead, Glympse Bio, Hightide, Inipharma, Intercept, Inventiva, Ionis, Janssen, Madrigal, Metacrine, NGM Biopharmaceuticals, Novartis, Novo Nordisk, Merck, Pfizer, Sagimet, Theratechnologies, 89 bio, Terns Pharmaceuticals and Viking Therapeutics. In addition, his institutions received research grants from Arrowhead Pharmaceuticals, AstraZeneca, Boehringer-Ingelheim, Bristol Myers Squibb, Eli Lilly, Galectin Therapeutics, Galmed Pharmaceuticals, Gilead, Intercept, Hanmi, Intercept, Inventiva, Ionis, Janssen, Madrigal Pharmaceuticals, Merck, NGM Biopharmaceuticals, Novo Nordisk, Merck, Pfizer, Sonic Incytes, and Terns Pharmaceuticals. Dr. Loomba is a co-founder of LipoNexus.
A version of this article first appeared on Medscape.com.
MILAN — , according to the results of the phase 2 SYNERGY-NASH trial.
Specifically, 44%-62% of participants with MASH and moderate or severe fibrosis treated with 5-15 mg of tirzepatide achieved MASH resolution without worsening of fibrosis compared with 10% on placebo; 51%-55% of those on tirzepatide achieved at least one stage of fibrosis improvement without worsening of MASH compared with 30% on placebo. Tirzepatide also led to weight loss.
The study (Abstract LBO-001) was presented at the European Association for the Study of the Liver (EASL) Congress 2024 by Rohit Loomba, MD, professor of medicine, NAFLD Research Center, University of California at San Diego in La Jolla, and published simultaneously in The New England Journal of Medicine.
“The results are clinically meaningful,” Dr. Loomba said in an interview.
Both of the endpoints — improvements in MASH resolution and fibrosis — are considered approvable endpoints for MASH therapeutic development, and therefore, increase the likelihood of success of using such a strategy in a phase 3 setting, Dr. Loomba said.
MASH Resolution, No Worsening of Fibrosis
The dose-finding, multicenter, double-blind, placebo-controlled trial randomly assigned a total of 190 participants to receive once-weekly subcutaneous tirzepatide (5 mg, 10 mg, or 15 mg) or placebo for 52 weeks. Participants had biopsy-confirmed MASH and stage F2 or F3 (moderate or severe) fibrosis.
Overall, approximately 42% of participants had F2 fibrosis and over 57% had F3 fibrosis. The proportion of F3 fibrosis was numerically higher in the placebo (64.6%) and 5-mg tirzepatide (63.8%) groups.
The mean age of the study cohort was 54 years; 57% were female, 86% were White, and 36% were Hispanic; the mean body mass index was 36; 58% had type 2 diabetes; and A1c was 6.5. NAFLD activity score (NAS) was 5.3. Baseline noninvasive test results were consistent with the study population of MASH with F2/F3 fibrosis and NAS ≥ 4.
The primary endpoint was resolution of MASH without worsening of fibrosis at 52 weeks, and the key secondary endpoint was an improvement (decrease) of at least one fibrosis stage without worsening of MASH. Other secondary endpoints included a ≥ 2-point decrease in NAS with ≤ 1-point decrease in two or more NAS components.
A total of 157 participants (83%) underwent liver biopsies at week 52, providing results for the current analysis.
Among tirzepatide-treated patients, 43.6% in the 5-mg group, 55.5% in the 10-mg group, and 62.4% in the 15-mg group met the criteria for resolution of MASH without worsening of fibrosis compared with 10% in the placebo group (P < .001 for all three comparisons).
Fibrosis improved by at least one stage without worsening of MASH in 54.9% of participants in the 5-mg tirzepatide group, 51.3% in the 10-mg tirzepatide group, and 51.0% in the 15-mg tirzepatide group compared with 29.7% in the placebo group (P < .001 for all risk differences with placebo).
Changes in NAS and subscores for the individual components of NAS, including steatosis, lobular inflammation, and hepatocellular ballooning, were also seen in participants on tirzepatide.
The researchers used a composite endpoint of a ≥ 2-point decrease in NAS with a ≥ 1-point decrease in at least two NAS components. Of the tirzepatide-treated groups, 71.7%,78.3%, and 76.6% in the 5-mg, 10-mg, and 15-mg groups, respectively, met this endpoint compared with 36.7% in placebo.
Imaging of liver fat with MRI-based proton density fat fraction (MRI-PDFF) showed reductions from baseline of -45.7, -41.3, -57.0 in participants on 5-mg, 10-mg, and 15-mg tirzepatide, respectively. Differences from placebo were all statistically significant.
Percentage of body weight change from baseline was -10.7%, -13.3%, and -15.6% in the 5-mg, 10-mg, and 15-mg tirzepatide groups, respectively, compared with weight loss of -0.8% in the placebo group.
“Tirzepatide led to significant weight loss in both patients with diabetes and those without diabetes,” reported Dr. Loomba.
There were more adverse events in patients on tirzepatide (92.3%) compared with patients on placebo (83.3%).
“The most common adverse events were gastrointestinal in nature, with 96% of them mild to moderate in severity,” said Dr. Loomba. “Discontinuations occurred in 4.2% of participants, which was similar between patients on tirzepatide and those on placebo.”
He pointed out that the safety profile of tirzepatide in a MASH population “was generally similar to that observed in the phase 3 trials of type 2 diabetes and obesity.”
Incidence of serious adverse events was also similar at 6.3% for participants on tirzepatide vs 6.2% for those on placebo; 2.8% on tirzepatide and 4.2% on placebo progressed to cirrhosis. There was no evidence of drug-induced liver injury.
‘Convincing Results’
Commenting on the study, co-moderator Sven Francque, MD, hepatologist and head of department at the University Hospital of Antwerp, Belgium, said that the study was in a relatively “severe” patient population, which was one of its strengths.
“These are convincing results in terms of MASH resolution, showing a strong response and dose-dependence,” he said.
“In terms of fibrosis, the results look numerically strong but are somewhat more puzzling to interpret, as there was no dose-response relationship and no data on NITs [noninvasive tests] that could support the results,” he added.
“Patients with no-end-of-treatment biopsies were handled differently than in previous trials, which makes it difficult to appreciate antifibrotic potency,” he said. But “such a strong effect on MASH should translate into a reduction in fibrosis even in the absence of direct antifibrotic effects.”
Given that “about one third of patients in the active treatment arms” did not have end-of-treatment biopsy, these “are rather small numbers precluding firm conclusions,” he added.
However, Dr. Francque said that he believes the findings are compelling enough for the drug to go into phase 3 trials.
Dr. Francque has no disclosures of relevance to this study. Dr. Loomba serves as a consultant to Aardvark Therapeutics, Altimmune, Anylam/Regeneron, Amgen, Arrowhead Pharmaceuticals, AstraZeneca, Bristol Myers Squibb, CohBar, Eli Lilly, Galmed, Gilead, Glympse Bio, Hightide, Inipharma, Intercept, Inventiva, Ionis, Janssen, Madrigal, Metacrine, NGM Biopharmaceuticals, Novartis, Novo Nordisk, Merck, Pfizer, Sagimet, Theratechnologies, 89 bio, Terns Pharmaceuticals and Viking Therapeutics. In addition, his institutions received research grants from Arrowhead Pharmaceuticals, AstraZeneca, Boehringer-Ingelheim, Bristol Myers Squibb, Eli Lilly, Galectin Therapeutics, Galmed Pharmaceuticals, Gilead, Intercept, Hanmi, Intercept, Inventiva, Ionis, Janssen, Madrigal Pharmaceuticals, Merck, NGM Biopharmaceuticals, Novo Nordisk, Merck, Pfizer, Sonic Incytes, and Terns Pharmaceuticals. Dr. Loomba is a co-founder of LipoNexus.
A version of this article first appeared on Medscape.com.
MILAN — , according to the results of the phase 2 SYNERGY-NASH trial.
Specifically, 44%-62% of participants with MASH and moderate or severe fibrosis treated with 5-15 mg of tirzepatide achieved MASH resolution without worsening of fibrosis compared with 10% on placebo; 51%-55% of those on tirzepatide achieved at least one stage of fibrosis improvement without worsening of MASH compared with 30% on placebo. Tirzepatide also led to weight loss.
The study (Abstract LBO-001) was presented at the European Association for the Study of the Liver (EASL) Congress 2024 by Rohit Loomba, MD, professor of medicine, NAFLD Research Center, University of California at San Diego in La Jolla, and published simultaneously in The New England Journal of Medicine.
“The results are clinically meaningful,” Dr. Loomba said in an interview.
Both of the endpoints — improvements in MASH resolution and fibrosis — are considered approvable endpoints for MASH therapeutic development, and therefore, increase the likelihood of success of using such a strategy in a phase 3 setting, Dr. Loomba said.
MASH Resolution, No Worsening of Fibrosis
The dose-finding, multicenter, double-blind, placebo-controlled trial randomly assigned a total of 190 participants to receive once-weekly subcutaneous tirzepatide (5 mg, 10 mg, or 15 mg) or placebo for 52 weeks. Participants had biopsy-confirmed MASH and stage F2 or F3 (moderate or severe) fibrosis.
Overall, approximately 42% of participants had F2 fibrosis and over 57% had F3 fibrosis. The proportion of F3 fibrosis was numerically higher in the placebo (64.6%) and 5-mg tirzepatide (63.8%) groups.
The mean age of the study cohort was 54 years; 57% were female, 86% were White, and 36% were Hispanic; the mean body mass index was 36; 58% had type 2 diabetes; and A1c was 6.5. NAFLD activity score (NAS) was 5.3. Baseline noninvasive test results were consistent with the study population of MASH with F2/F3 fibrosis and NAS ≥ 4.
The primary endpoint was resolution of MASH without worsening of fibrosis at 52 weeks, and the key secondary endpoint was an improvement (decrease) of at least one fibrosis stage without worsening of MASH. Other secondary endpoints included a ≥ 2-point decrease in NAS with ≤ 1-point decrease in two or more NAS components.
A total of 157 participants (83%) underwent liver biopsies at week 52, providing results for the current analysis.
Among tirzepatide-treated patients, 43.6% in the 5-mg group, 55.5% in the 10-mg group, and 62.4% in the 15-mg group met the criteria for resolution of MASH without worsening of fibrosis compared with 10% in the placebo group (P < .001 for all three comparisons).
Fibrosis improved by at least one stage without worsening of MASH in 54.9% of participants in the 5-mg tirzepatide group, 51.3% in the 10-mg tirzepatide group, and 51.0% in the 15-mg tirzepatide group compared with 29.7% in the placebo group (P < .001 for all risk differences with placebo).
Changes in NAS and subscores for the individual components of NAS, including steatosis, lobular inflammation, and hepatocellular ballooning, were also seen in participants on tirzepatide.
The researchers used a composite endpoint of a ≥ 2-point decrease in NAS with a ≥ 1-point decrease in at least two NAS components. Of the tirzepatide-treated groups, 71.7%,78.3%, and 76.6% in the 5-mg, 10-mg, and 15-mg groups, respectively, met this endpoint compared with 36.7% in placebo.
Imaging of liver fat with MRI-based proton density fat fraction (MRI-PDFF) showed reductions from baseline of -45.7, -41.3, -57.0 in participants on 5-mg, 10-mg, and 15-mg tirzepatide, respectively. Differences from placebo were all statistically significant.
Percentage of body weight change from baseline was -10.7%, -13.3%, and -15.6% in the 5-mg, 10-mg, and 15-mg tirzepatide groups, respectively, compared with weight loss of -0.8% in the placebo group.
“Tirzepatide led to significant weight loss in both patients with diabetes and those without diabetes,” reported Dr. Loomba.
There were more adverse events in patients on tirzepatide (92.3%) compared with patients on placebo (83.3%).
“The most common adverse events were gastrointestinal in nature, with 96% of them mild to moderate in severity,” said Dr. Loomba. “Discontinuations occurred in 4.2% of participants, which was similar between patients on tirzepatide and those on placebo.”
He pointed out that the safety profile of tirzepatide in a MASH population “was generally similar to that observed in the phase 3 trials of type 2 diabetes and obesity.”
Incidence of serious adverse events was also similar at 6.3% for participants on tirzepatide vs 6.2% for those on placebo; 2.8% on tirzepatide and 4.2% on placebo progressed to cirrhosis. There was no evidence of drug-induced liver injury.
‘Convincing Results’
Commenting on the study, co-moderator Sven Francque, MD, hepatologist and head of department at the University Hospital of Antwerp, Belgium, said that the study was in a relatively “severe” patient population, which was one of its strengths.
“These are convincing results in terms of MASH resolution, showing a strong response and dose-dependence,” he said.
“In terms of fibrosis, the results look numerically strong but are somewhat more puzzling to interpret, as there was no dose-response relationship and no data on NITs [noninvasive tests] that could support the results,” he added.
“Patients with no-end-of-treatment biopsies were handled differently than in previous trials, which makes it difficult to appreciate antifibrotic potency,” he said. But “such a strong effect on MASH should translate into a reduction in fibrosis even in the absence of direct antifibrotic effects.”
Given that “about one third of patients in the active treatment arms” did not have end-of-treatment biopsy, these “are rather small numbers precluding firm conclusions,” he added.
However, Dr. Francque said that he believes the findings are compelling enough for the drug to go into phase 3 trials.
Dr. Francque has no disclosures of relevance to this study. Dr. Loomba serves as a consultant to Aardvark Therapeutics, Altimmune, Anylam/Regeneron, Amgen, Arrowhead Pharmaceuticals, AstraZeneca, Bristol Myers Squibb, CohBar, Eli Lilly, Galmed, Gilead, Glympse Bio, Hightide, Inipharma, Intercept, Inventiva, Ionis, Janssen, Madrigal, Metacrine, NGM Biopharmaceuticals, Novartis, Novo Nordisk, Merck, Pfizer, Sagimet, Theratechnologies, 89 bio, Terns Pharmaceuticals and Viking Therapeutics. In addition, his institutions received research grants from Arrowhead Pharmaceuticals, AstraZeneca, Boehringer-Ingelheim, Bristol Myers Squibb, Eli Lilly, Galectin Therapeutics, Galmed Pharmaceuticals, Gilead, Intercept, Hanmi, Intercept, Inventiva, Ionis, Janssen, Madrigal Pharmaceuticals, Merck, NGM Biopharmaceuticals, Novo Nordisk, Merck, Pfizer, Sonic Incytes, and Terns Pharmaceuticals. Dr. Loomba is a co-founder of LipoNexus.
A version of this article first appeared on Medscape.com.
FROM EASL 2024
Facial Temperature Can Reveal Age and Disease
This transcript has been edited for clarity.
My oldest daughter is at sleepaway camp for a couple of weeks, and the camp has a photographer who goes around all day taking pictures of the kids, which get uploaded to a private Facebook group. In the past, I would go online every day (or, okay, several times a day) and scroll through all those pictures looking for one that features my kid.
I don’t have to do that anymore. This year, I simply uploaded a picture of my daughter to an app and artificial intelligence (AI) takes care of the rest, recognizing her face amidst the sea of smiling children, and flagging just those photos for me to peruse. It’s amazing, really. And a bit scary.
The fact that facial recognition has penetrated the summer camp market should tell you that the tech is truly ubiquitous. But today we’re going to think a bit more about what AI can do with a picture of your face, because the power of facial recognition is not just skin deep.
What’s got me hot and bothered about facial images is this paper, appearing in Cell Metabolism, which adds a new layer to the standard facial-analysis playbook: facial temperature.
To understand this paper, you need to understand a whole field of research that is developing various different “clocks” for age.
It turns out that age really is just a number. Our cells, our proteins, our biochemistry can be analyzed to give different numbers. These “clocks,” as distinct from the calendar we usually use to measure our age, might have more predictive power than the number itself.
There are numerous molecular clocks, such as telomere length, that not only correlate with calendar age but are superior to calendar age in predicting age-related complications. Testing telomere length typically requires a blood sample — and remains costly. But we can use other sources to estimate age; how about a photo?
I mean, we do this all the time when we meet someone new or, as a physician, when we meet a new patient. I have often written that a patient “appears younger than their stated age,” and we’ve all had the experience of hearing how old someone is and being shocked. I mean, have you seen Sharon Stone recently? She’s 66 years old. Okay — to be fair, there might be some outside help there. But you get the point.
Back to the Cell Metabolism paper. Researchers report on multiple algorithms to obtain an “age” from a picture of an individual’s face.
The first algorithm is pretty straightforward. Researchers collected 2811 images, all of Han Chinese individuals ranging in age from 20 to 90 years, and reconstructed a 3D facial map from those. 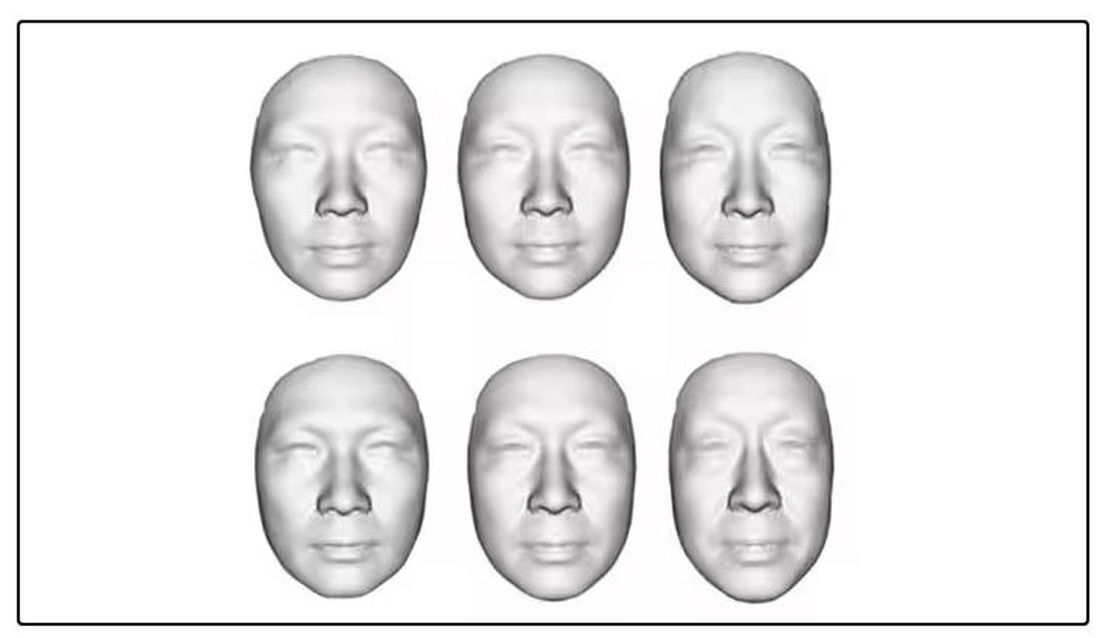
They then trained a convolutional neural network to predict the individuals’ ages from the pictures. It was quite accurate, as you can see here.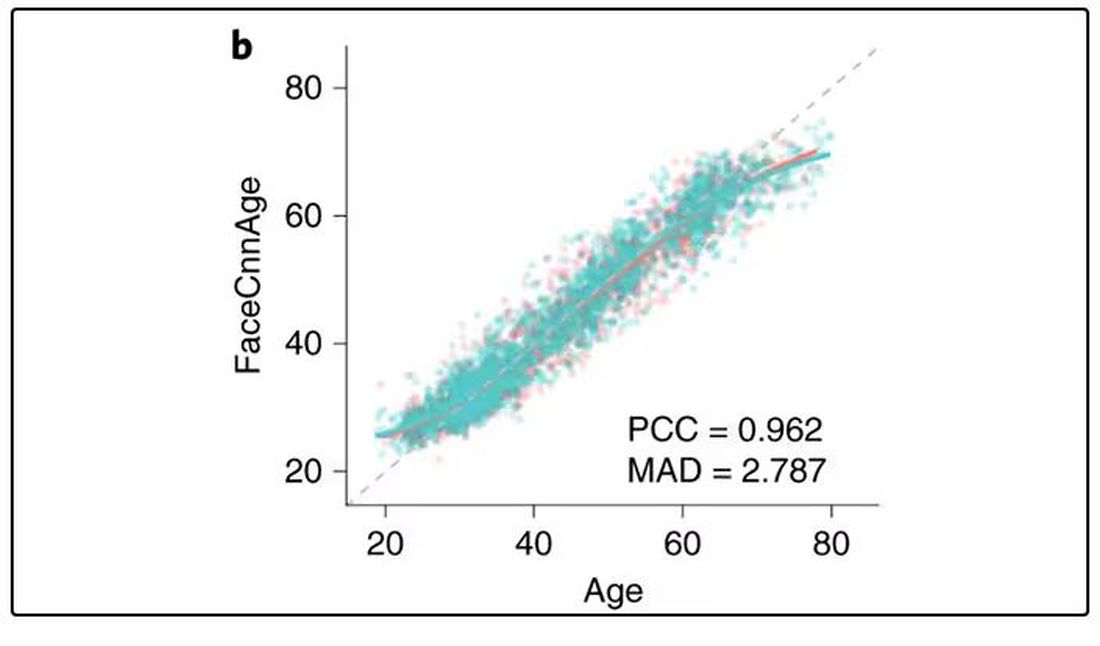
In the AI age, this may not seem that impressive. A brief search online turned up dozens of apps that promised to guess my age from a photo.
I sent this rather unflattering picture of myself to ChatGPT which, after initially demurring and saying it was not designed to guess ages, pegged me at somewhere between 35 and 45, which I am taking as a major victory.
But the Cell Metabolism paper goes deeper. Literally. 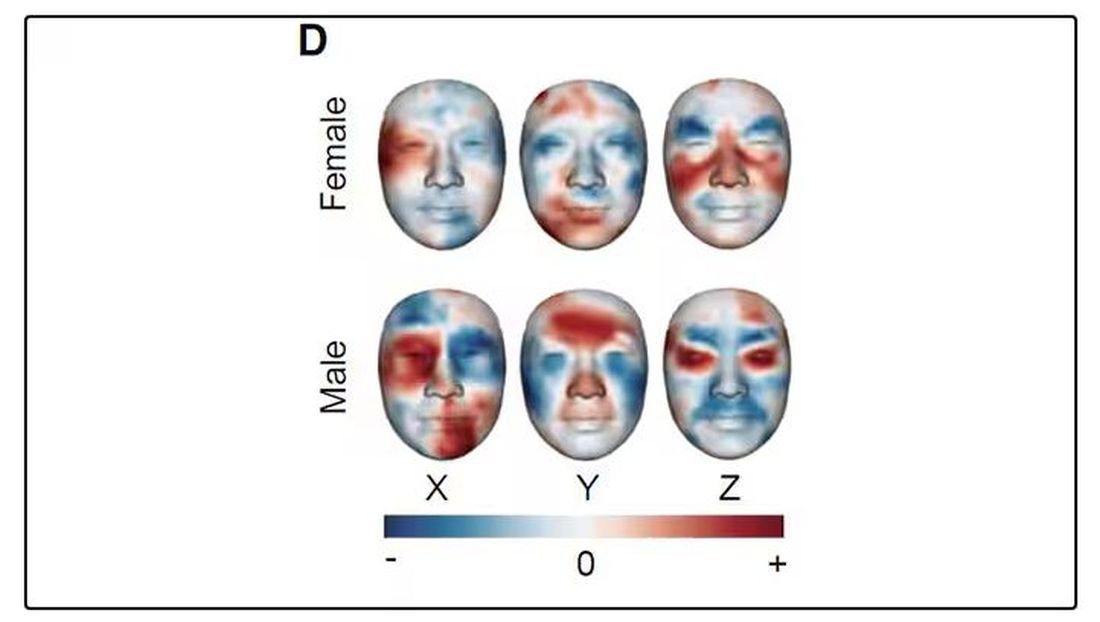
And this is where things start to get interesting. Because sure, the visible part of your face can change depending on makeup, expression, plastic surgery, and the like. But the temperature? That’s harder to fake.
It turns out that the temperature distribution in your face changes as you get older. There is a cooling of the nose and the cheeks, for example.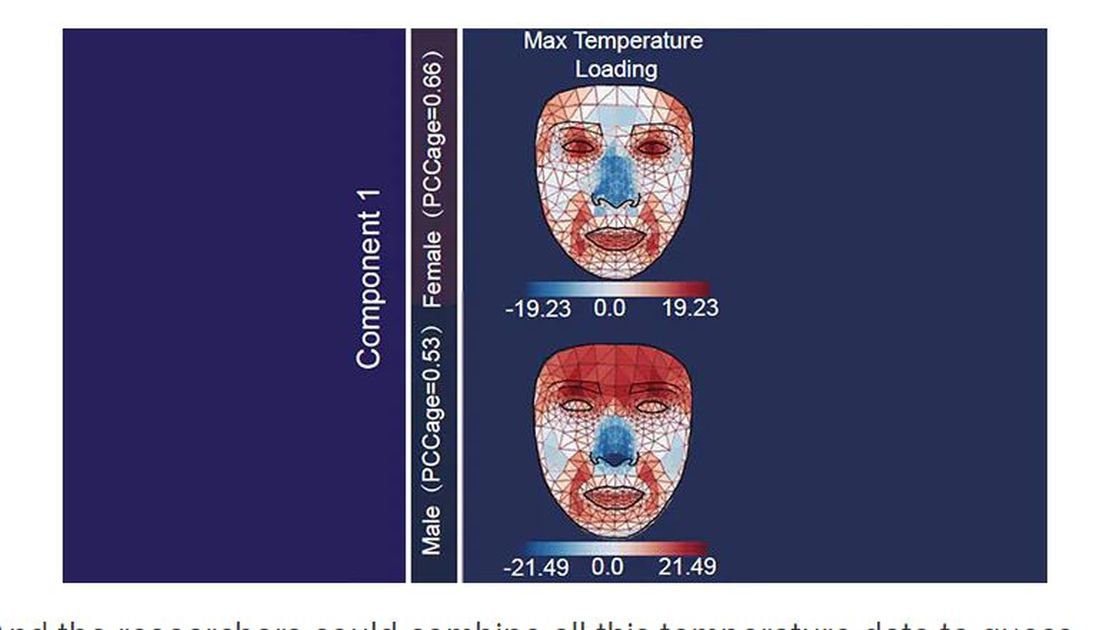
And the researchers could combine all this temperature data to guess someone’s calendar age fairly accurately, though notably not as accurately as the model that just looks at the pictures.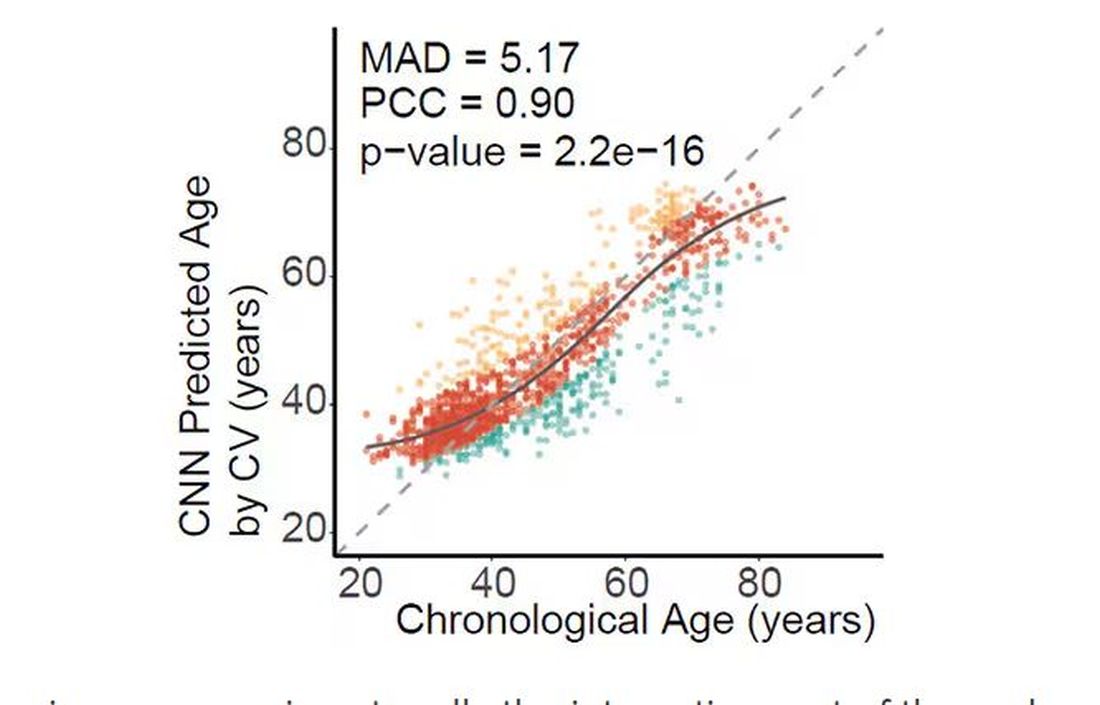
But guessing your age is not really the interesting part of thermal imaging of the face. It’s guessing — or, rather, predicting — the state of your metabolism. All these study participants had extensive metabolic testing performed, as well as detailed analysis of their lifestyle behaviors. And facial images could be used to predict those factors.
For example, the 3D reconstruction of the faces could predict who ate seafood (they tend to look younger than their actual age) compared with who ate poultry and meat (they tend to look older). The thermal imaging could predict who got more sleep (they look younger from a temperature perspective) and who ate more yogurt (also younger-appearing, temperature-wise). Facial temperature patterns could identify those with higher BMI, higher blood pressure, higher fasting glucose.
The researchers used the difference between actual and predicted age as a metric to measure illness as well. You can see here how, on average, individuals with hypertension, diabetes, and even liver cysts are “older,” at least by face temperature.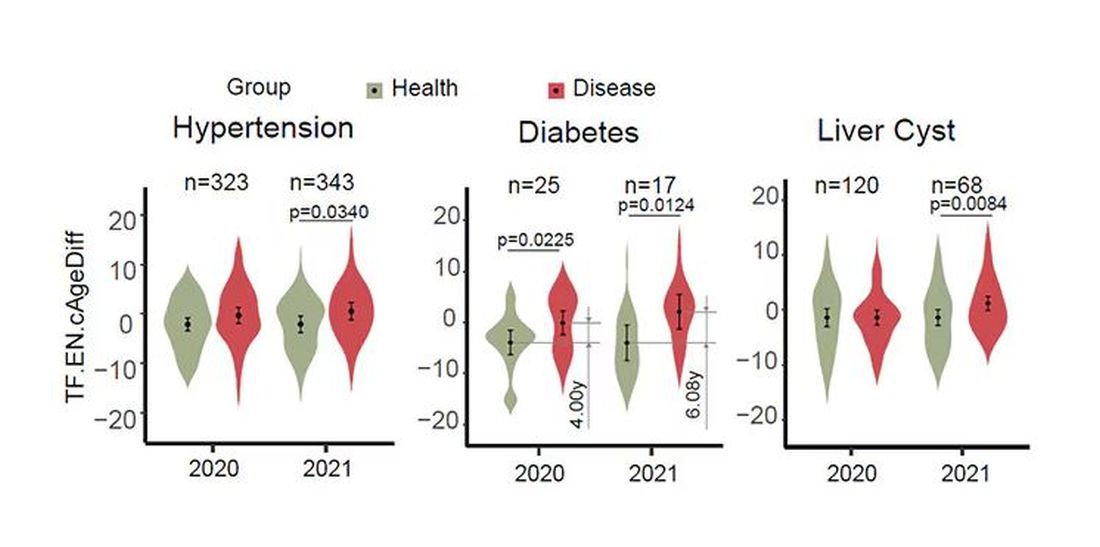
It may even be possible to use facial temperature as biofeedback. In a small study, the researchers measured the difference between facial temperature age and real age before and after 2 weeks of jump-roping. It turns out that 2 weeks of jump-roping can make you look about 5 years younger, at least as judged by a thermal camera. Or like the Predator.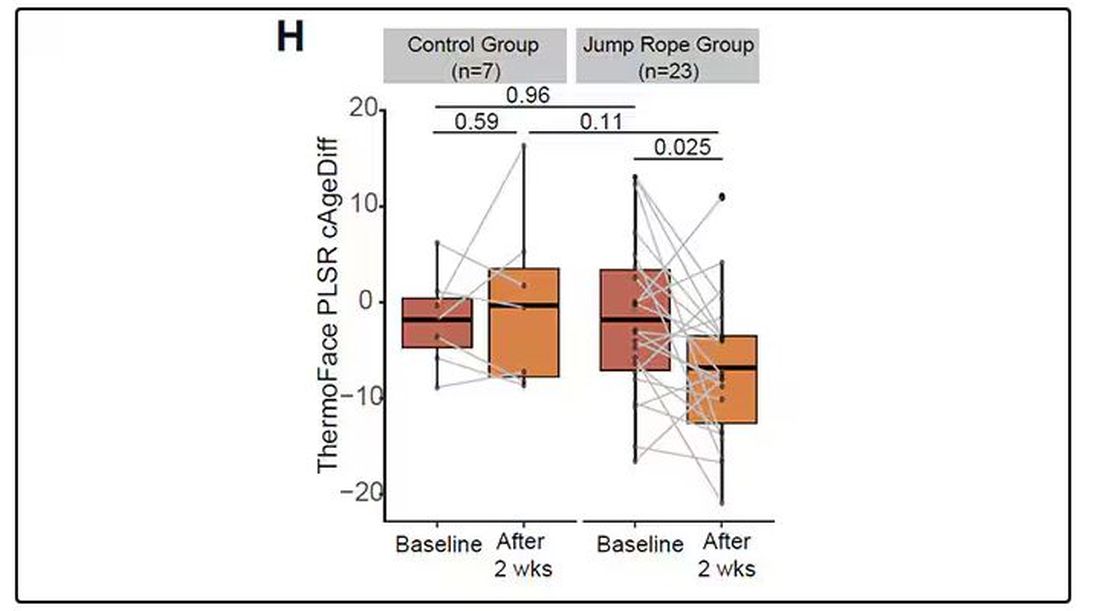
Okay, this is all very cool, but I’m not saying we’ll all be doing facial temperature tests in the near future. No; what this study highlights for me is how much information about ourselves is available to those who know how to decode it. Maybe those data come from the wrinkles in our faces, or the angles of our smiles, or the speed with which we type, or the temperature of our elbows. The data have always been there, actually, but we’ve never had the tools powerful enough to analyze them until now.
When I was a kid, I was obsessed with Star Trek — I know, you’re shocked — and, of course, the famous tricorder, a scanner that could tell everything about someone’s state of health in 5 seconds from 3 feet away. That’s how I thought medicine really would be in the future. Once I got to medical school, I was disabused of that notion. But the age of data, the age of AI, may mean the tricorder age is not actually that far away.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
My oldest daughter is at sleepaway camp for a couple of weeks, and the camp has a photographer who goes around all day taking pictures of the kids, which get uploaded to a private Facebook group. In the past, I would go online every day (or, okay, several times a day) and scroll through all those pictures looking for one that features my kid.
I don’t have to do that anymore. This year, I simply uploaded a picture of my daughter to an app and artificial intelligence (AI) takes care of the rest, recognizing her face amidst the sea of smiling children, and flagging just those photos for me to peruse. It’s amazing, really. And a bit scary.
The fact that facial recognition has penetrated the summer camp market should tell you that the tech is truly ubiquitous. But today we’re going to think a bit more about what AI can do with a picture of your face, because the power of facial recognition is not just skin deep.
What’s got me hot and bothered about facial images is this paper, appearing in Cell Metabolism, which adds a new layer to the standard facial-analysis playbook: facial temperature.
To understand this paper, you need to understand a whole field of research that is developing various different “clocks” for age.
It turns out that age really is just a number. Our cells, our proteins, our biochemistry can be analyzed to give different numbers. These “clocks,” as distinct from the calendar we usually use to measure our age, might have more predictive power than the number itself.
There are numerous molecular clocks, such as telomere length, that not only correlate with calendar age but are superior to calendar age in predicting age-related complications. Testing telomere length typically requires a blood sample — and remains costly. But we can use other sources to estimate age; how about a photo?
I mean, we do this all the time when we meet someone new or, as a physician, when we meet a new patient. I have often written that a patient “appears younger than their stated age,” and we’ve all had the experience of hearing how old someone is and being shocked. I mean, have you seen Sharon Stone recently? She’s 66 years old. Okay — to be fair, there might be some outside help there. But you get the point.
Back to the Cell Metabolism paper. Researchers report on multiple algorithms to obtain an “age” from a picture of an individual’s face.
The first algorithm is pretty straightforward. Researchers collected 2811 images, all of Han Chinese individuals ranging in age from 20 to 90 years, and reconstructed a 3D facial map from those. 
They then trained a convolutional neural network to predict the individuals’ ages from the pictures. It was quite accurate, as you can see here.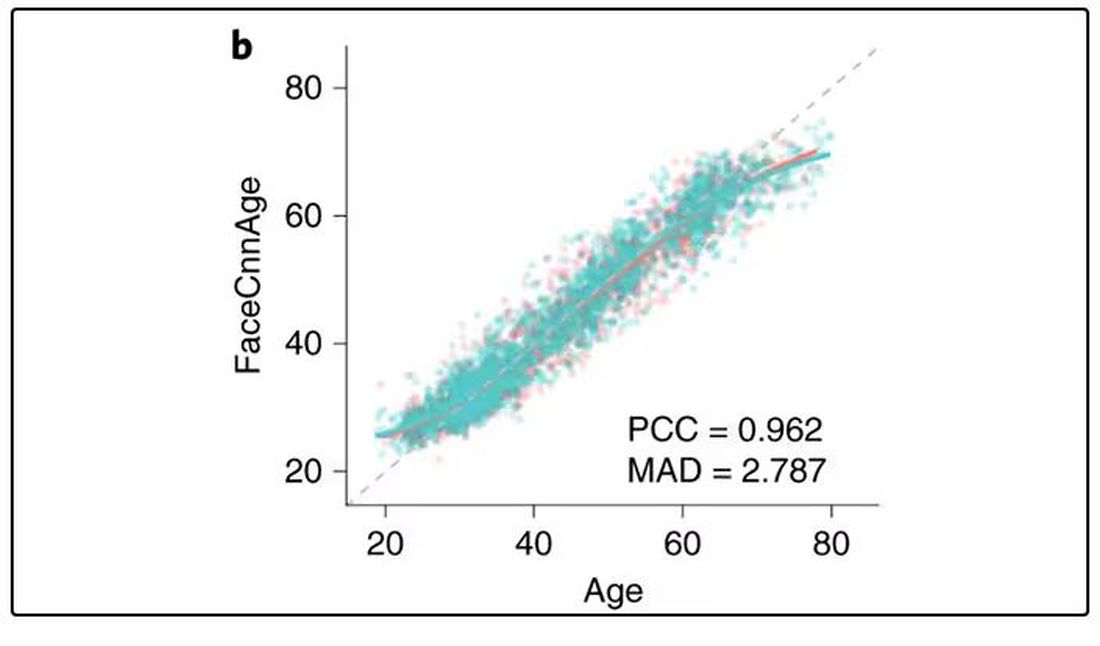
In the AI age, this may not seem that impressive. A brief search online turned up dozens of apps that promised to guess my age from a photo.
I sent this rather unflattering picture of myself to ChatGPT which, after initially demurring and saying it was not designed to guess ages, pegged me at somewhere between 35 and 45, which I am taking as a major victory.
But the Cell Metabolism paper goes deeper. Literally. 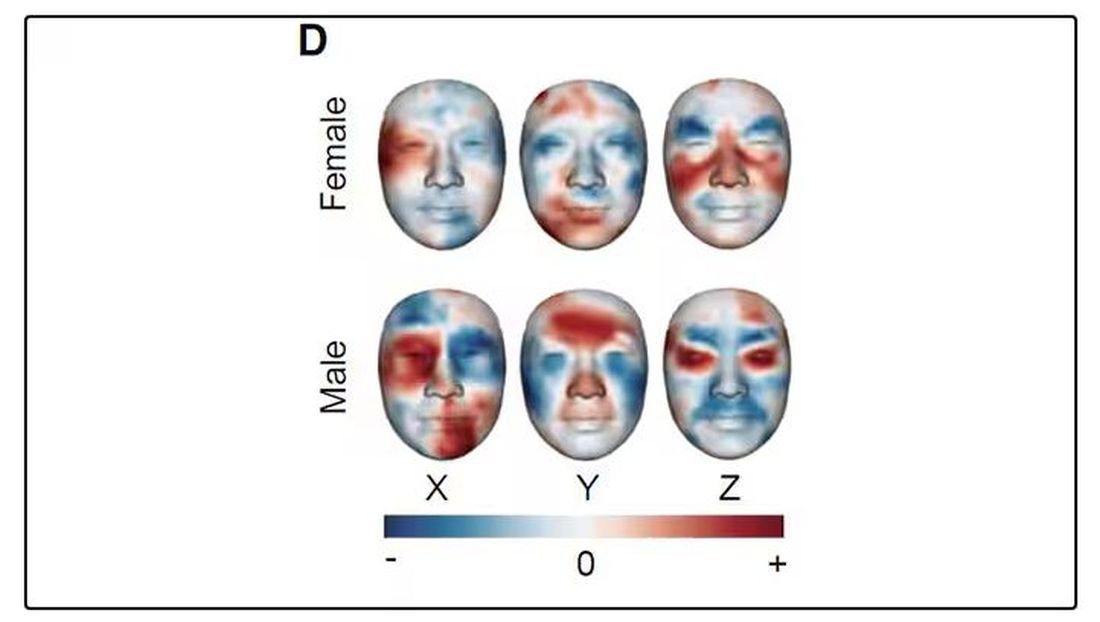
And this is where things start to get interesting. Because sure, the visible part of your face can change depending on makeup, expression, plastic surgery, and the like. But the temperature? That’s harder to fake.
It turns out that the temperature distribution in your face changes as you get older. There is a cooling of the nose and the cheeks, for example.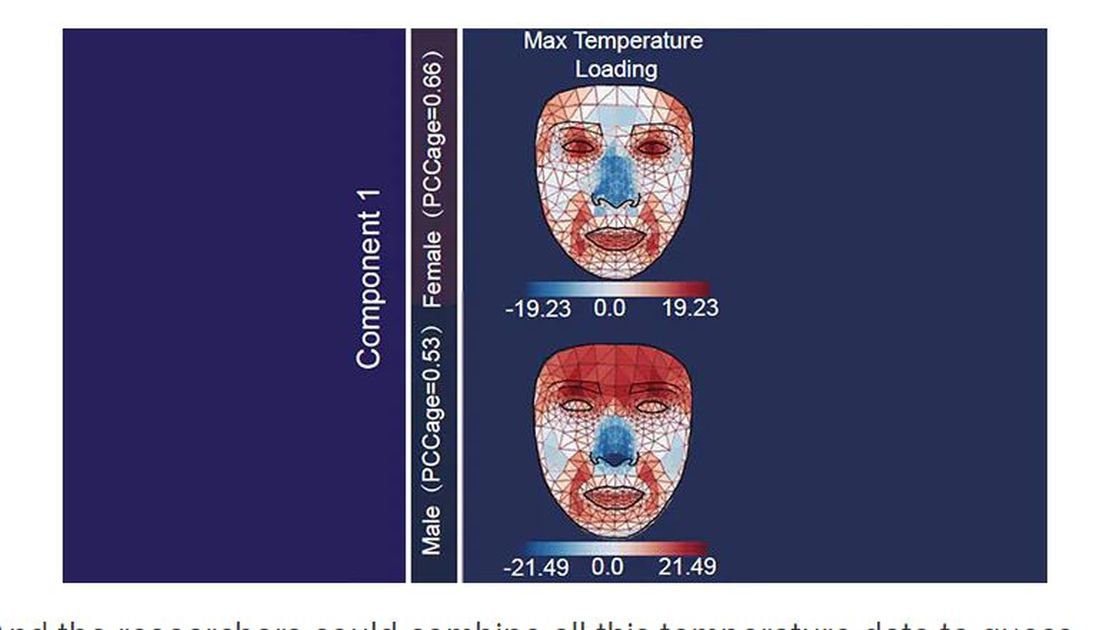
And the researchers could combine all this temperature data to guess someone’s calendar age fairly accurately, though notably not as accurately as the model that just looks at the pictures.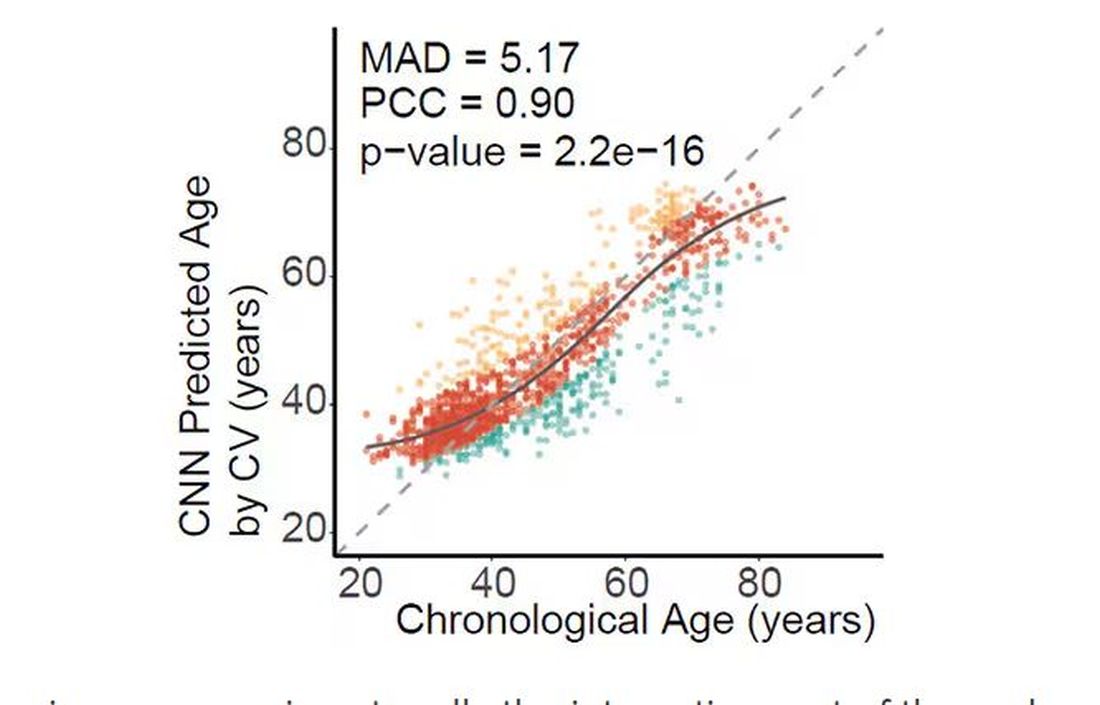
But guessing your age is not really the interesting part of thermal imaging of the face. It’s guessing — or, rather, predicting — the state of your metabolism. All these study participants had extensive metabolic testing performed, as well as detailed analysis of their lifestyle behaviors. And facial images could be used to predict those factors.
For example, the 3D reconstruction of the faces could predict who ate seafood (they tend to look younger than their actual age) compared with who ate poultry and meat (they tend to look older). The thermal imaging could predict who got more sleep (they look younger from a temperature perspective) and who ate more yogurt (also younger-appearing, temperature-wise). Facial temperature patterns could identify those with higher BMI, higher blood pressure, higher fasting glucose.
The researchers used the difference between actual and predicted age as a metric to measure illness as well. You can see here how, on average, individuals with hypertension, diabetes, and even liver cysts are “older,” at least by face temperature.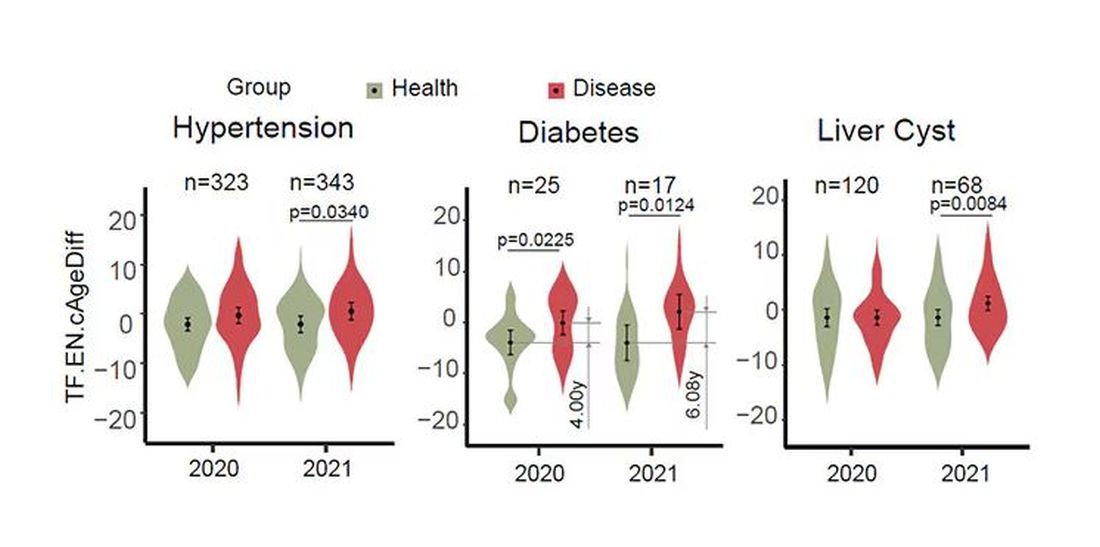
It may even be possible to use facial temperature as biofeedback. In a small study, the researchers measured the difference between facial temperature age and real age before and after 2 weeks of jump-roping. It turns out that 2 weeks of jump-roping can make you look about 5 years younger, at least as judged by a thermal camera. Or like the Predator.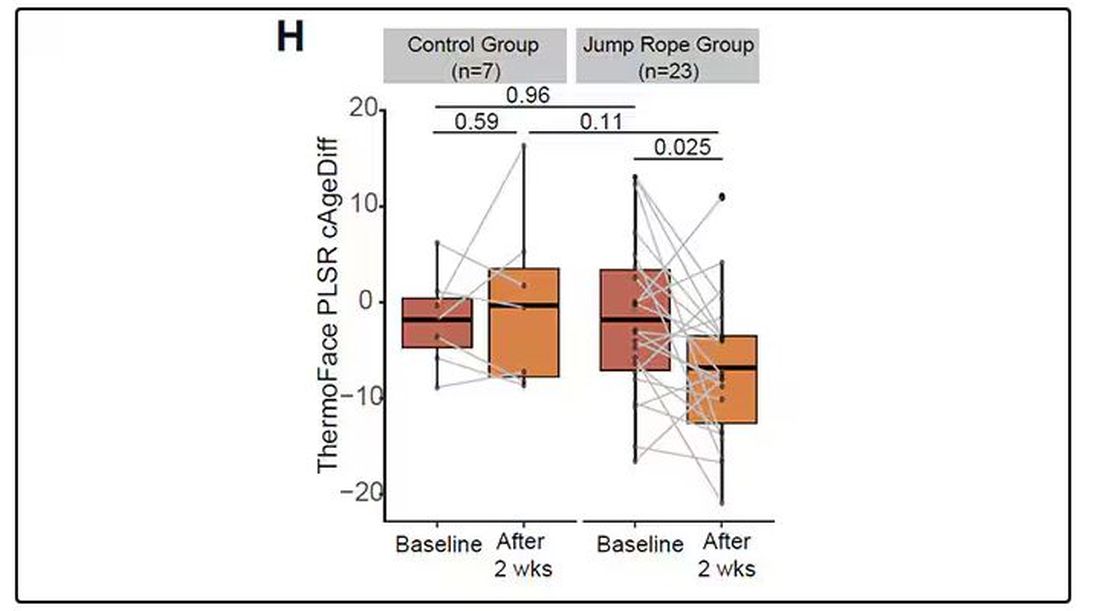
Okay, this is all very cool, but I’m not saying we’ll all be doing facial temperature tests in the near future. No; what this study highlights for me is how much information about ourselves is available to those who know how to decode it. Maybe those data come from the wrinkles in our faces, or the angles of our smiles, or the speed with which we type, or the temperature of our elbows. The data have always been there, actually, but we’ve never had the tools powerful enough to analyze them until now.
When I was a kid, I was obsessed with Star Trek — I know, you’re shocked — and, of course, the famous tricorder, a scanner that could tell everything about someone’s state of health in 5 seconds from 3 feet away. That’s how I thought medicine really would be in the future. Once I got to medical school, I was disabused of that notion. But the age of data, the age of AI, may mean the tricorder age is not actually that far away.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
My oldest daughter is at sleepaway camp for a couple of weeks, and the camp has a photographer who goes around all day taking pictures of the kids, which get uploaded to a private Facebook group. In the past, I would go online every day (or, okay, several times a day) and scroll through all those pictures looking for one that features my kid.
I don’t have to do that anymore. This year, I simply uploaded a picture of my daughter to an app and artificial intelligence (AI) takes care of the rest, recognizing her face amidst the sea of smiling children, and flagging just those photos for me to peruse. It’s amazing, really. And a bit scary.
The fact that facial recognition has penetrated the summer camp market should tell you that the tech is truly ubiquitous. But today we’re going to think a bit more about what AI can do with a picture of your face, because the power of facial recognition is not just skin deep.
What’s got me hot and bothered about facial images is this paper, appearing in Cell Metabolism, which adds a new layer to the standard facial-analysis playbook: facial temperature.
To understand this paper, you need to understand a whole field of research that is developing various different “clocks” for age.
It turns out that age really is just a number. Our cells, our proteins, our biochemistry can be analyzed to give different numbers. These “clocks,” as distinct from the calendar we usually use to measure our age, might have more predictive power than the number itself.
There are numerous molecular clocks, such as telomere length, that not only correlate with calendar age but are superior to calendar age in predicting age-related complications. Testing telomere length typically requires a blood sample — and remains costly. But we can use other sources to estimate age; how about a photo?
I mean, we do this all the time when we meet someone new or, as a physician, when we meet a new patient. I have often written that a patient “appears younger than their stated age,” and we’ve all had the experience of hearing how old someone is and being shocked. I mean, have you seen Sharon Stone recently? She’s 66 years old. Okay — to be fair, there might be some outside help there. But you get the point.
Back to the Cell Metabolism paper. Researchers report on multiple algorithms to obtain an “age” from a picture of an individual’s face.
The first algorithm is pretty straightforward. Researchers collected 2811 images, all of Han Chinese individuals ranging in age from 20 to 90 years, and reconstructed a 3D facial map from those. 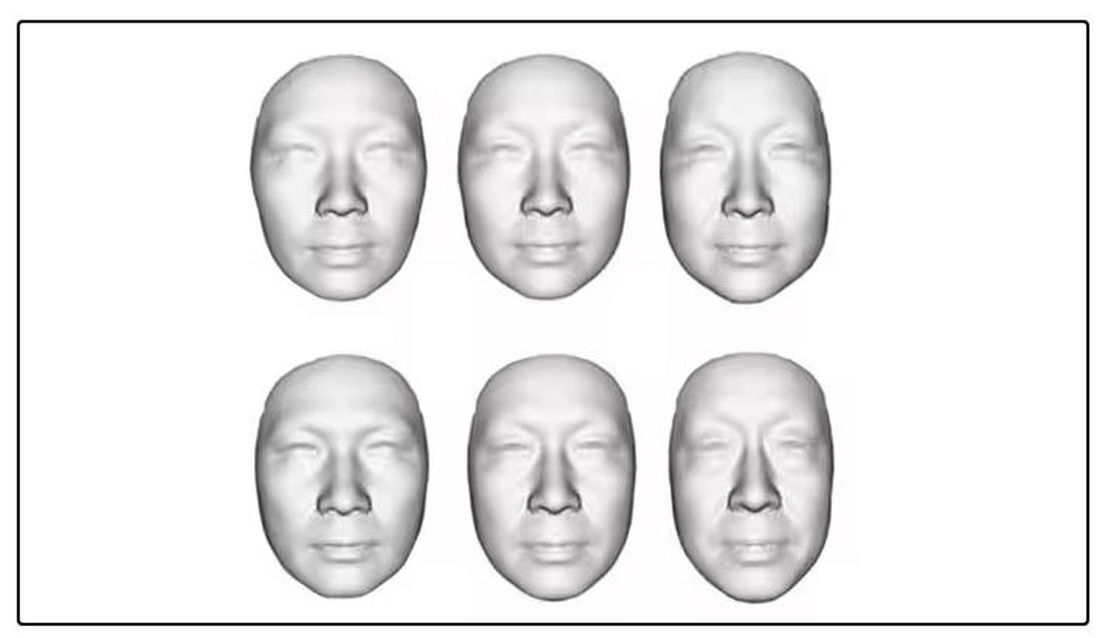
They then trained a convolutional neural network to predict the individuals’ ages from the pictures. It was quite accurate, as you can see here.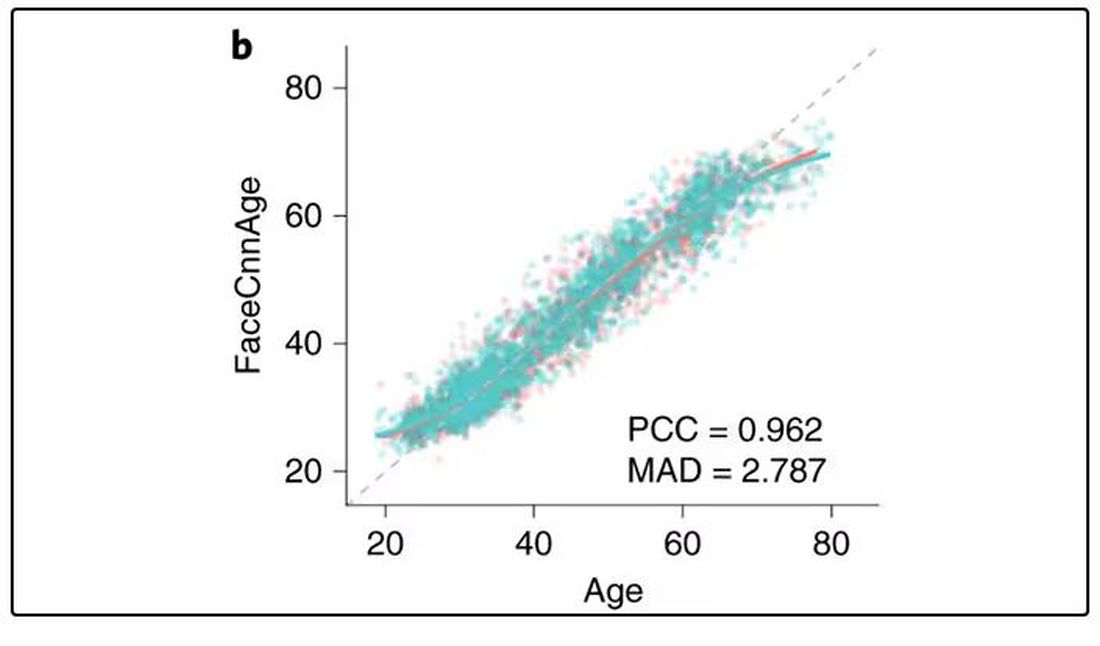
In the AI age, this may not seem that impressive. A brief search online turned up dozens of apps that promised to guess my age from a photo.
I sent this rather unflattering picture of myself to ChatGPT which, after initially demurring and saying it was not designed to guess ages, pegged me at somewhere between 35 and 45, which I am taking as a major victory.
But the Cell Metabolism paper goes deeper. Literally. 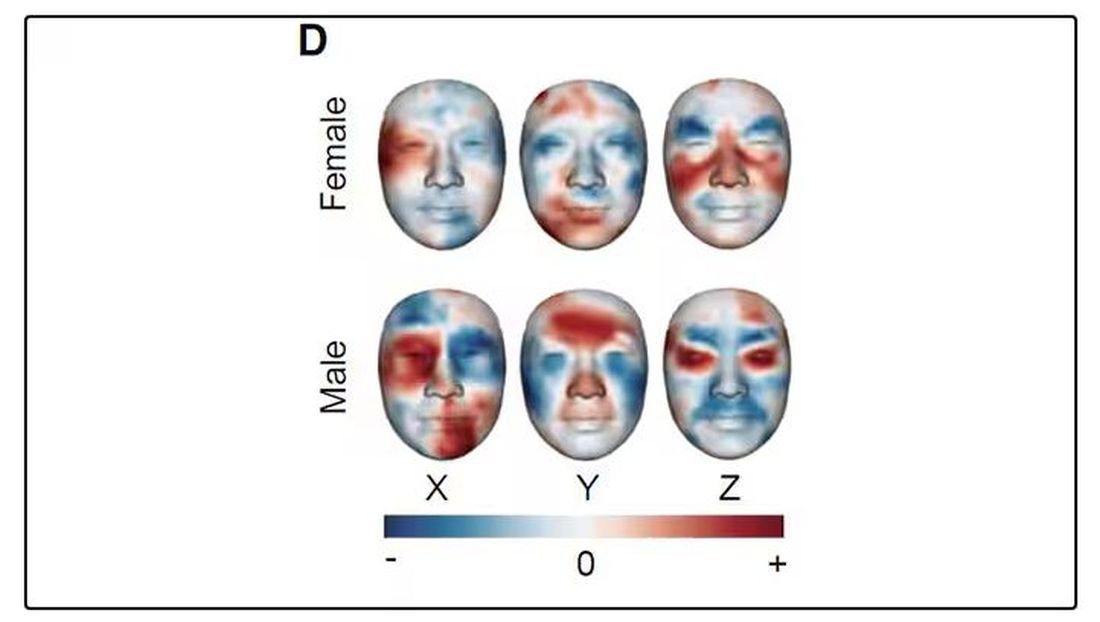
And this is where things start to get interesting. Because sure, the visible part of your face can change depending on makeup, expression, plastic surgery, and the like. But the temperature? That’s harder to fake.
It turns out that the temperature distribution in your face changes as you get older. There is a cooling of the nose and the cheeks, for example.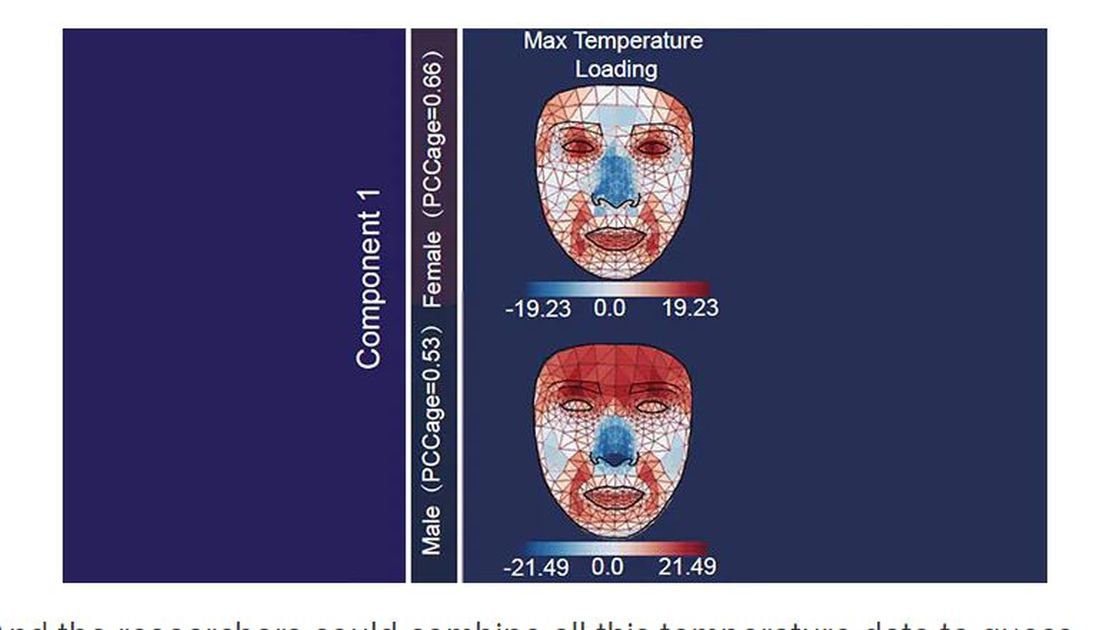
And the researchers could combine all this temperature data to guess someone’s calendar age fairly accurately, though notably not as accurately as the model that just looks at the pictures.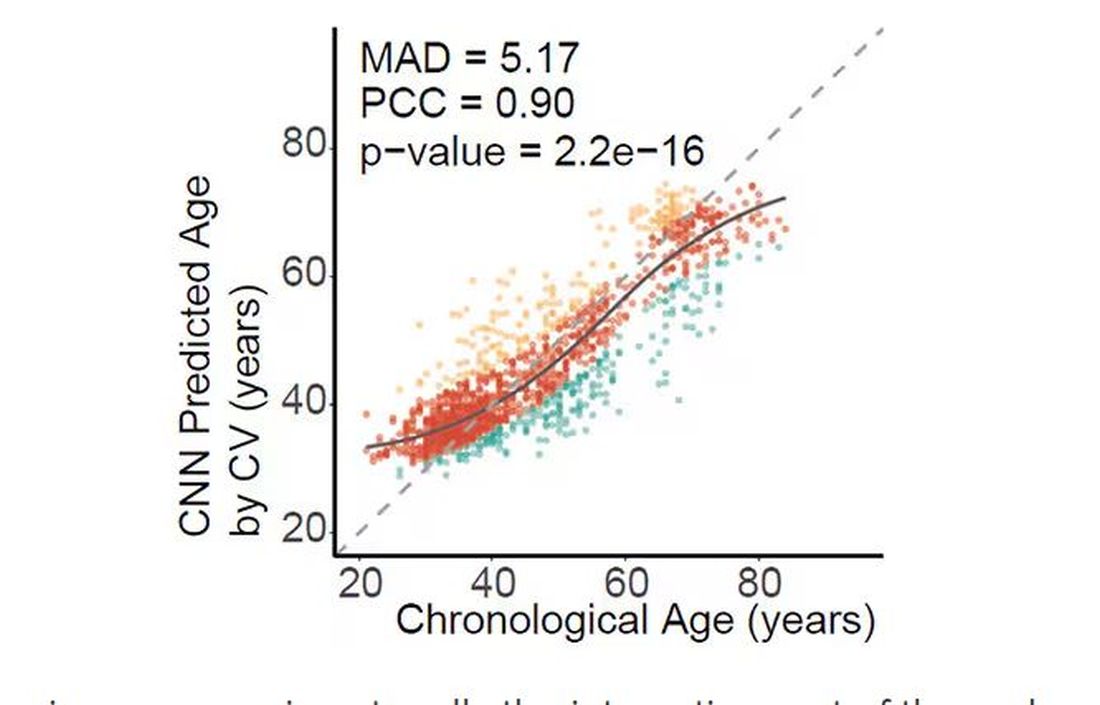
But guessing your age is not really the interesting part of thermal imaging of the face. It’s guessing — or, rather, predicting — the state of your metabolism. All these study participants had extensive metabolic testing performed, as well as detailed analysis of their lifestyle behaviors. And facial images could be used to predict those factors.
For example, the 3D reconstruction of the faces could predict who ate seafood (they tend to look younger than their actual age) compared with who ate poultry and meat (they tend to look older). The thermal imaging could predict who got more sleep (they look younger from a temperature perspective) and who ate more yogurt (also younger-appearing, temperature-wise). Facial temperature patterns could identify those with higher BMI, higher blood pressure, higher fasting glucose.
The researchers used the difference between actual and predicted age as a metric to measure illness as well. You can see here how, on average, individuals with hypertension, diabetes, and even liver cysts are “older,” at least by face temperature.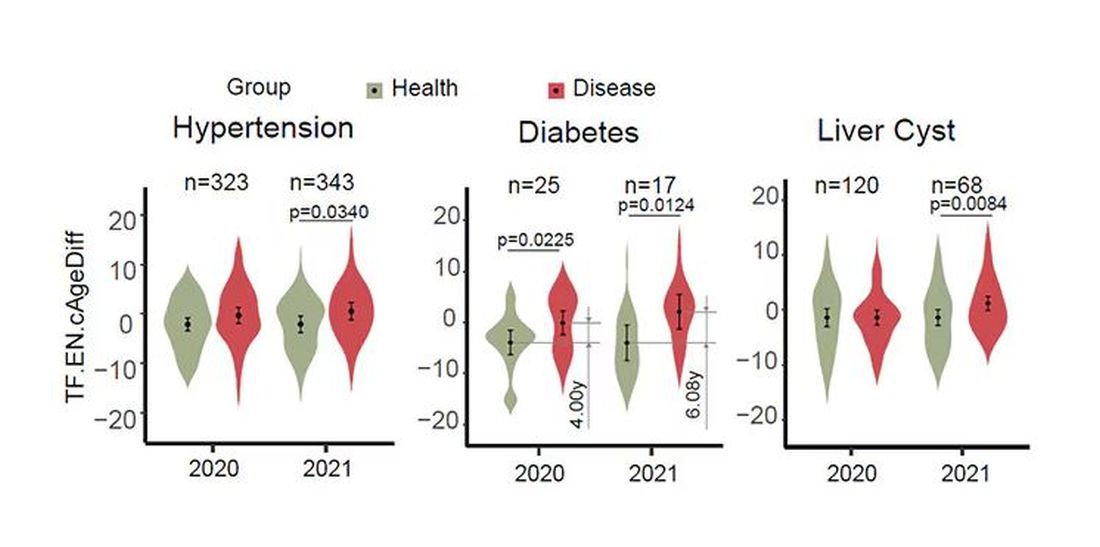
It may even be possible to use facial temperature as biofeedback. In a small study, the researchers measured the difference between facial temperature age and real age before and after 2 weeks of jump-roping. It turns out that 2 weeks of jump-roping can make you look about 5 years younger, at least as judged by a thermal camera. Or like the Predator.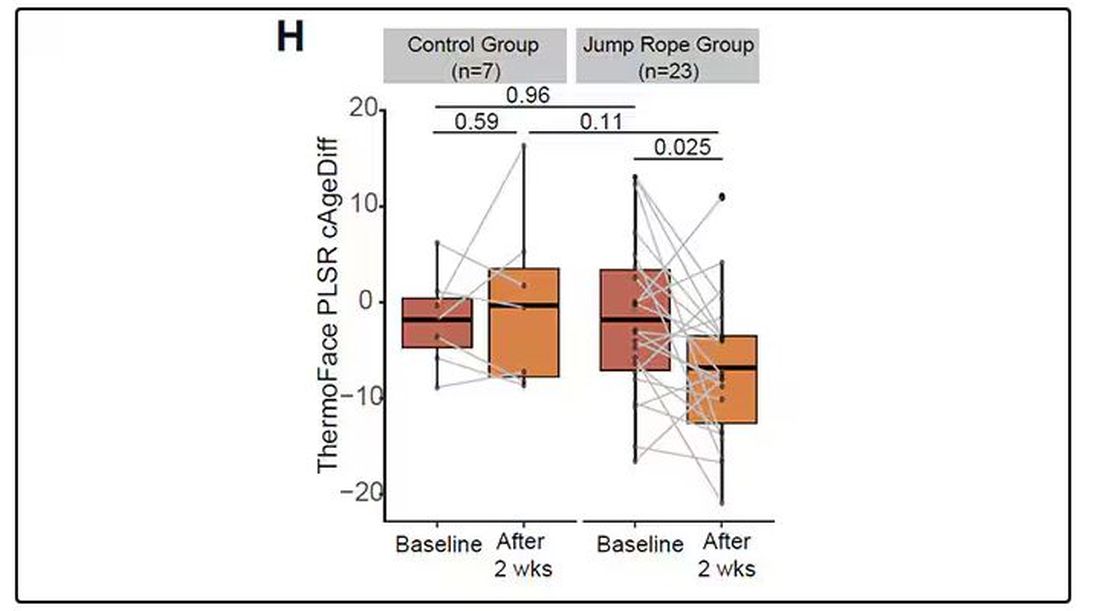
Okay, this is all very cool, but I’m not saying we’ll all be doing facial temperature tests in the near future. No; what this study highlights for me is how much information about ourselves is available to those who know how to decode it. Maybe those data come from the wrinkles in our faces, or the angles of our smiles, or the speed with which we type, or the temperature of our elbows. The data have always been there, actually, but we’ve never had the tools powerful enough to analyze them until now.
When I was a kid, I was obsessed with Star Trek — I know, you’re shocked — and, of course, the famous tricorder, a scanner that could tell everything about someone’s state of health in 5 seconds from 3 feet away. That’s how I thought medicine really would be in the future. Once I got to medical school, I was disabused of that notion. But the age of data, the age of AI, may mean the tricorder age is not actually that far away.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sex Hormones Linked to Fatty Liver in Men With T2D
TOPLINE:
In men with type 2 diabetes (T2D), higher serum levels of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) were associated with a lower risk for metabolic dysfunction–associated fatty liver disease (MAFLD), whereas higher progesterone levels were associated with a higher risk. In women with T2D, sex- or thyroid-related hormones were not independently associated with the risk for MAFLD.
METHODOLOGY:
- People with T2D may have FLD, and this study explored the link between sex-related and thyroid-related hormone levels and MAFLD to explore and confirm risk factors.
- The researchers used a 2020 definition of MAFLD, now defined in patients as both hepatic steatosis and the presence of overweight/obesity, T2D, or evidence of metabolic dysfunction in lean individuals.
- This cross-sectional study conducted in one hospital in China included 432 patients hospitalized because of T2D and its complications from January 2018 to April 2020 (median T2D duration, 6 years; mean age, 55.8 years; 247 men and 185 postmenopausal women).
- Researchers measured and later adjusted for potential confounding factors, including weight, height, waist circumference, arterial blood pressure, glycemic parameters, liver function, and lipid profiles.
- They assessed blood levels of sex and thyroid hormones by chemiluminescent immunoassays; MAFLD was diagnosed by either ultrasonography findings of hepatic steatosis or a high liver fat index score (fatty liver index > 60).
TAKEAWAY:
- Overall, 275 (63.7%) patients were diagnosed with MAFLD; after adjusting for potential confounding factors, none of the sex- and thyroid-related hormones were independently associated with the risk for MAFLD in all patients with T2D.
- In men with T2D, higher serum levels of FSH (adjusted odds ratio [aOR], 0.919; P = .019) and LH (aOR, 0.888; P = .022) were associated with a reduced risk for MAFLD.
- Higher serum levels of progesterone were associated with an increased risk for MAFLD in men with T2D (aOR, 8.069; P = .003).
- In women with T2D, sex hormones and thyroid hormones were not significantly linked to the risk of developing MAFLD.
IN PRACTICE:
“Our findings could be used to imply that screening for MAFLD and monitoring sex-related hormones are important for T2D patients, especially in men,” the authors wrote.
SOURCE:
This study was led by Weihong Lu, Xiamen Clinical Research Center for Cancer Therapy, Xiamen, China; Shangjian Li, Zhongshan Hospital (Xiamen), Fudan University, Xiamen, China; and Yuhua Li, China University of Mining & Technology-Beijing, Beijing, and was published online in BMC Endocrine Disorders.
LIMITATIONS:
Temporal sequences of the associations between sex-related and thyroid-related hormones and MAFLD were not evaluated because of the cross-sectional nature of the study. The small sample size from a single institution may have introduced selection bias. Serum levels of sex hormone-binding globulin and free testosterone were not assessed. The postmenopausal status of women in the study may have affected the ability to find sex-hormone related associations. The findings can only be limitedly extrapolated to similar patients with T2D but not the general population.
DISCLOSURES:
The study was supported by the Fujian Province Nature Science Foundations, China, and the Guiding Project on Medicine and Health in Xiamen, China. The authors declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
In men with type 2 diabetes (T2D), higher serum levels of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) were associated with a lower risk for metabolic dysfunction–associated fatty liver disease (MAFLD), whereas higher progesterone levels were associated with a higher risk. In women with T2D, sex- or thyroid-related hormones were not independently associated with the risk for MAFLD.
METHODOLOGY:
- People with T2D may have FLD, and this study explored the link between sex-related and thyroid-related hormone levels and MAFLD to explore and confirm risk factors.
- The researchers used a 2020 definition of MAFLD, now defined in patients as both hepatic steatosis and the presence of overweight/obesity, T2D, or evidence of metabolic dysfunction in lean individuals.
- This cross-sectional study conducted in one hospital in China included 432 patients hospitalized because of T2D and its complications from January 2018 to April 2020 (median T2D duration, 6 years; mean age, 55.8 years; 247 men and 185 postmenopausal women).
- Researchers measured and later adjusted for potential confounding factors, including weight, height, waist circumference, arterial blood pressure, glycemic parameters, liver function, and lipid profiles.
- They assessed blood levels of sex and thyroid hormones by chemiluminescent immunoassays; MAFLD was diagnosed by either ultrasonography findings of hepatic steatosis or a high liver fat index score (fatty liver index > 60).
TAKEAWAY:
- Overall, 275 (63.7%) patients were diagnosed with MAFLD; after adjusting for potential confounding factors, none of the sex- and thyroid-related hormones were independently associated with the risk for MAFLD in all patients with T2D.
- In men with T2D, higher serum levels of FSH (adjusted odds ratio [aOR], 0.919; P = .019) and LH (aOR, 0.888; P = .022) were associated with a reduced risk for MAFLD.
- Higher serum levels of progesterone were associated with an increased risk for MAFLD in men with T2D (aOR, 8.069; P = .003).
- In women with T2D, sex hormones and thyroid hormones were not significantly linked to the risk of developing MAFLD.
IN PRACTICE:
“Our findings could be used to imply that screening for MAFLD and monitoring sex-related hormones are important for T2D patients, especially in men,” the authors wrote.
SOURCE:
This study was led by Weihong Lu, Xiamen Clinical Research Center for Cancer Therapy, Xiamen, China; Shangjian Li, Zhongshan Hospital (Xiamen), Fudan University, Xiamen, China; and Yuhua Li, China University of Mining & Technology-Beijing, Beijing, and was published online in BMC Endocrine Disorders.
LIMITATIONS:
Temporal sequences of the associations between sex-related and thyroid-related hormones and MAFLD were not evaluated because of the cross-sectional nature of the study. The small sample size from a single institution may have introduced selection bias. Serum levels of sex hormone-binding globulin and free testosterone were not assessed. The postmenopausal status of women in the study may have affected the ability to find sex-hormone related associations. The findings can only be limitedly extrapolated to similar patients with T2D but not the general population.
DISCLOSURES:
The study was supported by the Fujian Province Nature Science Foundations, China, and the Guiding Project on Medicine and Health in Xiamen, China. The authors declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
In men with type 2 diabetes (T2D), higher serum levels of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) were associated with a lower risk for metabolic dysfunction–associated fatty liver disease (MAFLD), whereas higher progesterone levels were associated with a higher risk. In women with T2D, sex- or thyroid-related hormones were not independently associated with the risk for MAFLD.
METHODOLOGY:
- People with T2D may have FLD, and this study explored the link between sex-related and thyroid-related hormone levels and MAFLD to explore and confirm risk factors.
- The researchers used a 2020 definition of MAFLD, now defined in patients as both hepatic steatosis and the presence of overweight/obesity, T2D, or evidence of metabolic dysfunction in lean individuals.
- This cross-sectional study conducted in one hospital in China included 432 patients hospitalized because of T2D and its complications from January 2018 to April 2020 (median T2D duration, 6 years; mean age, 55.8 years; 247 men and 185 postmenopausal women).
- Researchers measured and later adjusted for potential confounding factors, including weight, height, waist circumference, arterial blood pressure, glycemic parameters, liver function, and lipid profiles.
- They assessed blood levels of sex and thyroid hormones by chemiluminescent immunoassays; MAFLD was diagnosed by either ultrasonography findings of hepatic steatosis or a high liver fat index score (fatty liver index > 60).
TAKEAWAY:
- Overall, 275 (63.7%) patients were diagnosed with MAFLD; after adjusting for potential confounding factors, none of the sex- and thyroid-related hormones were independently associated with the risk for MAFLD in all patients with T2D.
- In men with T2D, higher serum levels of FSH (adjusted odds ratio [aOR], 0.919; P = .019) and LH (aOR, 0.888; P = .022) were associated with a reduced risk for MAFLD.
- Higher serum levels of progesterone were associated with an increased risk for MAFLD in men with T2D (aOR, 8.069; P = .003).
- In women with T2D, sex hormones and thyroid hormones were not significantly linked to the risk of developing MAFLD.
IN PRACTICE:
“Our findings could be used to imply that screening for MAFLD and monitoring sex-related hormones are important for T2D patients, especially in men,” the authors wrote.
SOURCE:
This study was led by Weihong Lu, Xiamen Clinical Research Center for Cancer Therapy, Xiamen, China; Shangjian Li, Zhongshan Hospital (Xiamen), Fudan University, Xiamen, China; and Yuhua Li, China University of Mining & Technology-Beijing, Beijing, and was published online in BMC Endocrine Disorders.
LIMITATIONS:
Temporal sequences of the associations between sex-related and thyroid-related hormones and MAFLD were not evaluated because of the cross-sectional nature of the study. The small sample size from a single institution may have introduced selection bias. Serum levels of sex hormone-binding globulin and free testosterone were not assessed. The postmenopausal status of women in the study may have affected the ability to find sex-hormone related associations. The findings can only be limitedly extrapolated to similar patients with T2D but not the general population.
DISCLOSURES:
The study was supported by the Fujian Province Nature Science Foundations, China, and the Guiding Project on Medicine and Health in Xiamen, China. The authors declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
Women with Autoimmune Liver Diseases Still Face Increased CVD Risks
WASHINGTON – , according to a study presented at the annual Digestive Disease Week® (DDW).
In particular, women with autoimmune hepatitis (AIH) and primary biliary cholangitis (PBC) appear to have higher risks than women without AIH or PBC. Those with primary sclerosing cholangitis (PSC) don’t seem to have increased risks.
“We know that cardiovascular disease remains the number one cause of death, but the mortality rate for women over the last decade has plateaued, whereas in men it’s actually declining due to interventions,” said lead author Rachel Redfield, MD, a transplant hepatology fellow at Thomas Jefferson University Hospital in Philadelphia.
“This is likely because we don’t have adequate risk stratification, especially for women,” she said. “We know that immune-mediated diseases — such as rheumatoid arthritis and psoriasis — carry a higher risk of cardiovascular disease, but there’s not a lot of data on our autoimmune liver disease patients.”
Although being a female can offer protection against some CVD risks, the atherosclerotic cardiovascular disease (ASCVD) 10-year risk score calculator recommended by the American College of Cardiology doesn’t include chronic inflammatory diseases associated with increased CVD risk, including AILD.
Dr. Redfield and colleagues conducted a multicenter, retrospective cohort study of patients with AIH, PBC, and PSC from 1999-2019. Using TriNetX data, the researchers looked at women with AILD who also had diabetes mellitus, hypertension, and hyperlipidemia, as well as a control group of men and women with these same disorders, excluding those who used biologics, immune modulators, and steroids or had other autoimmune disorders.
The research team used 1:1 propensity-score matching for women in the study group and in the control group based on age, race, ethnicity, ASCVD risk factors, and tobacco use. Women in the study group and men in the control group were matched for age, race, ethnicity, and tobacco use.
The primary outcome was summative cardiovascular risk, including unstable angina, acute myocardial infarction, presence of coronary angioplasty implant, coronary artery bypass, percutaneous coronary intervention, and cerebral infarction.
Overall, women with AIH had a significantly higher cardiovascular risk compared to women without AIH, at 25.4% versus 20.6% (P = .0007).
Specifically, women with PBC had a significantly higher cardiovascular risk compared to women without PBC, at 27.05% versus 20.9% (P < .0001).
There wasn’t a significant difference in risk between women with and without PSC, at 27.5% versus 21.8% (P = .27).
When compared to men without disease, women with AIH didn’t have a statistically significant higher risk, at 25.3% versus 24.2% (P = .44). Similarly, there didn’t appear to be a significant difference between women with PBC and men without PBC, at 26.9% versus 25.9% (P = .52), or between women with PSC and men without PSC, at 27.7% versus 26.2% (P = .78).
Dr. Redfield and colleagues then compared the ASCVD-calculated risk versus database risk, finding that in each group of women with AILD — including AIH, PBC, and PSC — the ASCVD-calculated risk was around 11%, compared with database risk scores of 25% for AIH, 27% for PBC, and 28% for PSC. These database risks appeared similar to both the ASCVD and database risk percentages for men.
“So potentially there’s an oversight in women with any kind of inflammatory disease, but specifically here, autoimmune liver diseases,” she said. “We really need to enhance our risk assessment strategies to take into account their risk and optimize patient outcomes.”
Dr. Redfield noted the limitations with using TriNetX data, including coding consistency among providers and healthcare organizations, unknown patient follow-up dates, and the inability to capture various inflammatory disease phenotypes, such as autoimmune hepatitis with multiple flares, which may be associated with higher cardiovascular risks.
As an attendee of the DDW session, Kenneth Kelson, MD, a gastroenterologist with Fremont Medical Group and Washington Hospital Healthcare System in Fremont, California, noted the importance of investigating the effects of different types of statins in these patients. Although the research team looked at top-level differences among statin users, finding that women with AILD were more likely to be on a statin, they didn’t incorporate statin therapy in the propensity-score matching model.
“Lipid-soluble statins are known to cause more liver trouble, even though it’s pretty low,” Dr. Kelson said. “Whereas the water-soluble statins have a lower incidence of liver issues.”
Dr. Redfield and Dr. Kelson reported no relevant disclosures.
WASHINGTON – , according to a study presented at the annual Digestive Disease Week® (DDW).
In particular, women with autoimmune hepatitis (AIH) and primary biliary cholangitis (PBC) appear to have higher risks than women without AIH or PBC. Those with primary sclerosing cholangitis (PSC) don’t seem to have increased risks.
“We know that cardiovascular disease remains the number one cause of death, but the mortality rate for women over the last decade has plateaued, whereas in men it’s actually declining due to interventions,” said lead author Rachel Redfield, MD, a transplant hepatology fellow at Thomas Jefferson University Hospital in Philadelphia.
“This is likely because we don’t have adequate risk stratification, especially for women,” she said. “We know that immune-mediated diseases — such as rheumatoid arthritis and psoriasis — carry a higher risk of cardiovascular disease, but there’s not a lot of data on our autoimmune liver disease patients.”
Although being a female can offer protection against some CVD risks, the atherosclerotic cardiovascular disease (ASCVD) 10-year risk score calculator recommended by the American College of Cardiology doesn’t include chronic inflammatory diseases associated with increased CVD risk, including AILD.
Dr. Redfield and colleagues conducted a multicenter, retrospective cohort study of patients with AIH, PBC, and PSC from 1999-2019. Using TriNetX data, the researchers looked at women with AILD who also had diabetes mellitus, hypertension, and hyperlipidemia, as well as a control group of men and women with these same disorders, excluding those who used biologics, immune modulators, and steroids or had other autoimmune disorders.
The research team used 1:1 propensity-score matching for women in the study group and in the control group based on age, race, ethnicity, ASCVD risk factors, and tobacco use. Women in the study group and men in the control group were matched for age, race, ethnicity, and tobacco use.
The primary outcome was summative cardiovascular risk, including unstable angina, acute myocardial infarction, presence of coronary angioplasty implant, coronary artery bypass, percutaneous coronary intervention, and cerebral infarction.
Overall, women with AIH had a significantly higher cardiovascular risk compared to women without AIH, at 25.4% versus 20.6% (P = .0007).
Specifically, women with PBC had a significantly higher cardiovascular risk compared to women without PBC, at 27.05% versus 20.9% (P < .0001).
There wasn’t a significant difference in risk between women with and without PSC, at 27.5% versus 21.8% (P = .27).
When compared to men without disease, women with AIH didn’t have a statistically significant higher risk, at 25.3% versus 24.2% (P = .44). Similarly, there didn’t appear to be a significant difference between women with PBC and men without PBC, at 26.9% versus 25.9% (P = .52), or between women with PSC and men without PSC, at 27.7% versus 26.2% (P = .78).
Dr. Redfield and colleagues then compared the ASCVD-calculated risk versus database risk, finding that in each group of women with AILD — including AIH, PBC, and PSC — the ASCVD-calculated risk was around 11%, compared with database risk scores of 25% for AIH, 27% for PBC, and 28% for PSC. These database risks appeared similar to both the ASCVD and database risk percentages for men.
“So potentially there’s an oversight in women with any kind of inflammatory disease, but specifically here, autoimmune liver diseases,” she said. “We really need to enhance our risk assessment strategies to take into account their risk and optimize patient outcomes.”
Dr. Redfield noted the limitations with using TriNetX data, including coding consistency among providers and healthcare organizations, unknown patient follow-up dates, and the inability to capture various inflammatory disease phenotypes, such as autoimmune hepatitis with multiple flares, which may be associated with higher cardiovascular risks.
As an attendee of the DDW session, Kenneth Kelson, MD, a gastroenterologist with Fremont Medical Group and Washington Hospital Healthcare System in Fremont, California, noted the importance of investigating the effects of different types of statins in these patients. Although the research team looked at top-level differences among statin users, finding that women with AILD were more likely to be on a statin, they didn’t incorporate statin therapy in the propensity-score matching model.
“Lipid-soluble statins are known to cause more liver trouble, even though it’s pretty low,” Dr. Kelson said. “Whereas the water-soluble statins have a lower incidence of liver issues.”
Dr. Redfield and Dr. Kelson reported no relevant disclosures.
WASHINGTON – , according to a study presented at the annual Digestive Disease Week® (DDW).
In particular, women with autoimmune hepatitis (AIH) and primary biliary cholangitis (PBC) appear to have higher risks than women without AIH or PBC. Those with primary sclerosing cholangitis (PSC) don’t seem to have increased risks.
“We know that cardiovascular disease remains the number one cause of death, but the mortality rate for women over the last decade has plateaued, whereas in men it’s actually declining due to interventions,” said lead author Rachel Redfield, MD, a transplant hepatology fellow at Thomas Jefferson University Hospital in Philadelphia.
“This is likely because we don’t have adequate risk stratification, especially for women,” she said. “We know that immune-mediated diseases — such as rheumatoid arthritis and psoriasis — carry a higher risk of cardiovascular disease, but there’s not a lot of data on our autoimmune liver disease patients.”
Although being a female can offer protection against some CVD risks, the atherosclerotic cardiovascular disease (ASCVD) 10-year risk score calculator recommended by the American College of Cardiology doesn’t include chronic inflammatory diseases associated with increased CVD risk, including AILD.
Dr. Redfield and colleagues conducted a multicenter, retrospective cohort study of patients with AIH, PBC, and PSC from 1999-2019. Using TriNetX data, the researchers looked at women with AILD who also had diabetes mellitus, hypertension, and hyperlipidemia, as well as a control group of men and women with these same disorders, excluding those who used biologics, immune modulators, and steroids or had other autoimmune disorders.
The research team used 1:1 propensity-score matching for women in the study group and in the control group based on age, race, ethnicity, ASCVD risk factors, and tobacco use. Women in the study group and men in the control group were matched for age, race, ethnicity, and tobacco use.
The primary outcome was summative cardiovascular risk, including unstable angina, acute myocardial infarction, presence of coronary angioplasty implant, coronary artery bypass, percutaneous coronary intervention, and cerebral infarction.
Overall, women with AIH had a significantly higher cardiovascular risk compared to women without AIH, at 25.4% versus 20.6% (P = .0007).
Specifically, women with PBC had a significantly higher cardiovascular risk compared to women without PBC, at 27.05% versus 20.9% (P < .0001).
There wasn’t a significant difference in risk between women with and without PSC, at 27.5% versus 21.8% (P = .27).
When compared to men without disease, women with AIH didn’t have a statistically significant higher risk, at 25.3% versus 24.2% (P = .44). Similarly, there didn’t appear to be a significant difference between women with PBC and men without PBC, at 26.9% versus 25.9% (P = .52), or between women with PSC and men without PSC, at 27.7% versus 26.2% (P = .78).
Dr. Redfield and colleagues then compared the ASCVD-calculated risk versus database risk, finding that in each group of women with AILD — including AIH, PBC, and PSC — the ASCVD-calculated risk was around 11%, compared with database risk scores of 25% for AIH, 27% for PBC, and 28% for PSC. These database risks appeared similar to both the ASCVD and database risk percentages for men.
“So potentially there’s an oversight in women with any kind of inflammatory disease, but specifically here, autoimmune liver diseases,” she said. “We really need to enhance our risk assessment strategies to take into account their risk and optimize patient outcomes.”
Dr. Redfield noted the limitations with using TriNetX data, including coding consistency among providers and healthcare organizations, unknown patient follow-up dates, and the inability to capture various inflammatory disease phenotypes, such as autoimmune hepatitis with multiple flares, which may be associated with higher cardiovascular risks.
As an attendee of the DDW session, Kenneth Kelson, MD, a gastroenterologist with Fremont Medical Group and Washington Hospital Healthcare System in Fremont, California, noted the importance of investigating the effects of different types of statins in these patients. Although the research team looked at top-level differences among statin users, finding that women with AILD were more likely to be on a statin, they didn’t incorporate statin therapy in the propensity-score matching model.
“Lipid-soluble statins are known to cause more liver trouble, even though it’s pretty low,” Dr. Kelson said. “Whereas the water-soluble statins have a lower incidence of liver issues.”
Dr. Redfield and Dr. Kelson reported no relevant disclosures.
FROM DDW 2024
Intelligent Liver Function Testing Helps Detect, Diagnose Chronic Liver Disease
TOPLINE:
, new data show.
METHODOLOGY:
- At the European Association for the Study of the Liver (EASL) Congress 2024, researchers presented 5-year, real-world data of the iLFT platform from its use in NHS Tayside in Dundee, Scotland, which serves a population of 400,000. The platform has been available since 2018.
- The iLFT platform uses an automated algorithm that analyzes standard liver function test results.
- Abnormal results prompt the system to initiate further fibrosis scoring and relevant etiologic testing to determine the cause of liver dysfunction.
- The results of these tests combined with practitioner-entered clinical information produce a probable diagnosis and recommend a patient-management strategy.
TAKEAWAY:
- Of the 26,459 iLFT tests performed between 2018 and 2023, 68.3% (18,079) required further testing beyond the initial liver function test, whereas 31.7% (8380) did not.
- Further testing generated 20,895 outcomes, of which, isolated abnormal alanine transaminase (ALT) without fibrosis was most frequent (23.7%). Abnormal ALT was found to be most likely due to metabolic dysfunction–associated steatotic liver disease (MASLD).
- Overall, half of cascaded samples had a positive etiologic diagnosis. Alcoholic liver disease (ALD) and MASLD were the most common etiologic outcomes identified.
- In addition, 20% of cascaded tests identified potentially significant liver fibrosis.
- A total of 69.9% of outcomes recommended that patients could be safely managed in primary care. The inclusion of automatic Enhanced Liver Fibrosis (ELF) testing in 2020 further reduced the requirement for referral to secondary care by 34%.
IN PRACTICE:
“Without this algorithm, the 18,000 patients who had algorithm-directed further testing would have had to go back to the [primary care practitioner] to obtain the additional tests, and the [primary care practitioner] would need to interpret them too,” said Damien Leith, MD, trainee hepatologist at Ninewells Hospital, Dundee, Scotland, who presented the findings. “iLFTs ensure the right patients get automated, appropriate follow-up testing and subsequent recommendation of referral to secondary care if necessary, and importantly iLFT helps the primary care practitioner identify the cause of chronic liver disease.”
SOURCE:
This study was presented on June 6, 2024 at the EASL Congress 2024 (abstract OS-007-YI).
LIMITATIONS:
Limitations include the need for further refinement of the algorithm to increase the proportion of positive etiologic iLFT outcomes. More analysis is needed to optimize the cost-effectiveness of iLFT.
DISCLOSURES:
Dr. Leith reports no relevant financial relationships.
A version of this article appeared on Medscape.com.
TOPLINE:
, new data show.
METHODOLOGY:
- At the European Association for the Study of the Liver (EASL) Congress 2024, researchers presented 5-year, real-world data of the iLFT platform from its use in NHS Tayside in Dundee, Scotland, which serves a population of 400,000. The platform has been available since 2018.
- The iLFT platform uses an automated algorithm that analyzes standard liver function test results.
- Abnormal results prompt the system to initiate further fibrosis scoring and relevant etiologic testing to determine the cause of liver dysfunction.
- The results of these tests combined with practitioner-entered clinical information produce a probable diagnosis and recommend a patient-management strategy.
TAKEAWAY:
- Of the 26,459 iLFT tests performed between 2018 and 2023, 68.3% (18,079) required further testing beyond the initial liver function test, whereas 31.7% (8380) did not.
- Further testing generated 20,895 outcomes, of which, isolated abnormal alanine transaminase (ALT) without fibrosis was most frequent (23.7%). Abnormal ALT was found to be most likely due to metabolic dysfunction–associated steatotic liver disease (MASLD).
- Overall, half of cascaded samples had a positive etiologic diagnosis. Alcoholic liver disease (ALD) and MASLD were the most common etiologic outcomes identified.
- In addition, 20% of cascaded tests identified potentially significant liver fibrosis.
- A total of 69.9% of outcomes recommended that patients could be safely managed in primary care. The inclusion of automatic Enhanced Liver Fibrosis (ELF) testing in 2020 further reduced the requirement for referral to secondary care by 34%.
IN PRACTICE:
“Without this algorithm, the 18,000 patients who had algorithm-directed further testing would have had to go back to the [primary care practitioner] to obtain the additional tests, and the [primary care practitioner] would need to interpret them too,” said Damien Leith, MD, trainee hepatologist at Ninewells Hospital, Dundee, Scotland, who presented the findings. “iLFTs ensure the right patients get automated, appropriate follow-up testing and subsequent recommendation of referral to secondary care if necessary, and importantly iLFT helps the primary care practitioner identify the cause of chronic liver disease.”
SOURCE:
This study was presented on June 6, 2024 at the EASL Congress 2024 (abstract OS-007-YI).
LIMITATIONS:
Limitations include the need for further refinement of the algorithm to increase the proportion of positive etiologic iLFT outcomes. More analysis is needed to optimize the cost-effectiveness of iLFT.
DISCLOSURES:
Dr. Leith reports no relevant financial relationships.
A version of this article appeared on Medscape.com.
TOPLINE:
, new data show.
METHODOLOGY:
- At the European Association for the Study of the Liver (EASL) Congress 2024, researchers presented 5-year, real-world data of the iLFT platform from its use in NHS Tayside in Dundee, Scotland, which serves a population of 400,000. The platform has been available since 2018.
- The iLFT platform uses an automated algorithm that analyzes standard liver function test results.
- Abnormal results prompt the system to initiate further fibrosis scoring and relevant etiologic testing to determine the cause of liver dysfunction.
- The results of these tests combined with practitioner-entered clinical information produce a probable diagnosis and recommend a patient-management strategy.
TAKEAWAY:
- Of the 26,459 iLFT tests performed between 2018 and 2023, 68.3% (18,079) required further testing beyond the initial liver function test, whereas 31.7% (8380) did not.
- Further testing generated 20,895 outcomes, of which, isolated abnormal alanine transaminase (ALT) without fibrosis was most frequent (23.7%). Abnormal ALT was found to be most likely due to metabolic dysfunction–associated steatotic liver disease (MASLD).
- Overall, half of cascaded samples had a positive etiologic diagnosis. Alcoholic liver disease (ALD) and MASLD were the most common etiologic outcomes identified.
- In addition, 20% of cascaded tests identified potentially significant liver fibrosis.
- A total of 69.9% of outcomes recommended that patients could be safely managed in primary care. The inclusion of automatic Enhanced Liver Fibrosis (ELF) testing in 2020 further reduced the requirement for referral to secondary care by 34%.
IN PRACTICE:
“Without this algorithm, the 18,000 patients who had algorithm-directed further testing would have had to go back to the [primary care practitioner] to obtain the additional tests, and the [primary care practitioner] would need to interpret them too,” said Damien Leith, MD, trainee hepatologist at Ninewells Hospital, Dundee, Scotland, who presented the findings. “iLFTs ensure the right patients get automated, appropriate follow-up testing and subsequent recommendation of referral to secondary care if necessary, and importantly iLFT helps the primary care practitioner identify the cause of chronic liver disease.”
SOURCE:
This study was presented on June 6, 2024 at the EASL Congress 2024 (abstract OS-007-YI).
LIMITATIONS:
Limitations include the need for further refinement of the algorithm to increase the proportion of positive etiologic iLFT outcomes. More analysis is needed to optimize the cost-effectiveness of iLFT.
DISCLOSURES:
Dr. Leith reports no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM EASL 2024
FDA OKs Iqirvo, First-in-Class PPAR Treatment for Primary Biliary Cholangitis
in combination with ursodeoxycholic acid (UDCA) in adults who do not respond adequately to UDCA or as monotherapy in patients unable to tolerate UDCA.
PBC is a rare, chronic cholestatic liver disease that destroys interlobular bile ducts and leads to cholestasis and liver fibrosis. Left untreated, the disease can worsen over time, leading to cirrhosis and liver transplant and, in some cases, premature death. PBC also harms quality of life, with patients often experiencing severe fatigue and pruritus.
Iqirvo, an oral dual peroxisome proliferator–activated receptor (PPAR) alpha and delta agonist, is the first new drug approved in nearly a decade for treatment of PBC.
Accelerated approval of Iqirvo for PBC was based on data from the phase 3 ELATIVE trial published last year in The New England Journal of Medicine.
The trial randomly assigned patients with PBC who had an inadequate response to or unacceptable side effects with UDCA to receive either once-daily elafibranor (80 mg) or placebo.
The primary endpoint was a biochemical response, defined as an alkaline phosphatase (ALP) level < 1.67 times the upper limit of the normal range, with a reduction ≥ 15% from baseline, as well as normal total bilirubin levels.
Among 161 patients, a biochemical response was seen in 55 of 108 (51%) who received elafibranor vs 2 of 53 (4%) who received placebo.
At week 52, the ALP level normalized in 15% of patients in the elafibranor group and none of the patients in the placebo group.
In a news release announcing approval of Iqirvo, the company notes that improvement in survival and prevention of liver decompensation events have not been demonstrated and that continued approval for PBC may be contingent upon verification and description of clinical benefit in confirmatory trials.
The most common adverse effects with Iqirvo, reported in ≥ 10% of study participants, were weight gain, abdominal pain, diarrhea, nausea, and vomiting. Iqirvo is not recommended for people who have or develop decompensated cirrhosis. Full prescribing information is available online.
The data show that Iqirvo is “an effective second-line treatment for patients with PBC with favorable benefit and risk data,” Kris Kowdley, MD, AGAF, director of the Liver Institute Northwest in Seattle, Washington, and a primary investigator on the ELATIVE study, said in the news release.
The approval of Iqirvo “will allow healthcare providers in the US to address an unmet need with the potential to significantly reduce ALP levels for our patients with PBC,” Dr. Kowdley said.
A version of this article appeared on Medscape.com.
in combination with ursodeoxycholic acid (UDCA) in adults who do not respond adequately to UDCA or as monotherapy in patients unable to tolerate UDCA.
PBC is a rare, chronic cholestatic liver disease that destroys interlobular bile ducts and leads to cholestasis and liver fibrosis. Left untreated, the disease can worsen over time, leading to cirrhosis and liver transplant and, in some cases, premature death. PBC also harms quality of life, with patients often experiencing severe fatigue and pruritus.
Iqirvo, an oral dual peroxisome proliferator–activated receptor (PPAR) alpha and delta agonist, is the first new drug approved in nearly a decade for treatment of PBC.
Accelerated approval of Iqirvo for PBC was based on data from the phase 3 ELATIVE trial published last year in The New England Journal of Medicine.
The trial randomly assigned patients with PBC who had an inadequate response to or unacceptable side effects with UDCA to receive either once-daily elafibranor (80 mg) or placebo.
The primary endpoint was a biochemical response, defined as an alkaline phosphatase (ALP) level < 1.67 times the upper limit of the normal range, with a reduction ≥ 15% from baseline, as well as normal total bilirubin levels.
Among 161 patients, a biochemical response was seen in 55 of 108 (51%) who received elafibranor vs 2 of 53 (4%) who received placebo.
At week 52, the ALP level normalized in 15% of patients in the elafibranor group and none of the patients in the placebo group.
In a news release announcing approval of Iqirvo, the company notes that improvement in survival and prevention of liver decompensation events have not been demonstrated and that continued approval for PBC may be contingent upon verification and description of clinical benefit in confirmatory trials.
The most common adverse effects with Iqirvo, reported in ≥ 10% of study participants, were weight gain, abdominal pain, diarrhea, nausea, and vomiting. Iqirvo is not recommended for people who have or develop decompensated cirrhosis. Full prescribing information is available online.
The data show that Iqirvo is “an effective second-line treatment for patients with PBC with favorable benefit and risk data,” Kris Kowdley, MD, AGAF, director of the Liver Institute Northwest in Seattle, Washington, and a primary investigator on the ELATIVE study, said in the news release.
The approval of Iqirvo “will allow healthcare providers in the US to address an unmet need with the potential to significantly reduce ALP levels for our patients with PBC,” Dr. Kowdley said.
A version of this article appeared on Medscape.com.
in combination with ursodeoxycholic acid (UDCA) in adults who do not respond adequately to UDCA or as monotherapy in patients unable to tolerate UDCA.
PBC is a rare, chronic cholestatic liver disease that destroys interlobular bile ducts and leads to cholestasis and liver fibrosis. Left untreated, the disease can worsen over time, leading to cirrhosis and liver transplant and, in some cases, premature death. PBC also harms quality of life, with patients often experiencing severe fatigue and pruritus.
Iqirvo, an oral dual peroxisome proliferator–activated receptor (PPAR) alpha and delta agonist, is the first new drug approved in nearly a decade for treatment of PBC.
Accelerated approval of Iqirvo for PBC was based on data from the phase 3 ELATIVE trial published last year in The New England Journal of Medicine.
The trial randomly assigned patients with PBC who had an inadequate response to or unacceptable side effects with UDCA to receive either once-daily elafibranor (80 mg) or placebo.
The primary endpoint was a biochemical response, defined as an alkaline phosphatase (ALP) level < 1.67 times the upper limit of the normal range, with a reduction ≥ 15% from baseline, as well as normal total bilirubin levels.
Among 161 patients, a biochemical response was seen in 55 of 108 (51%) who received elafibranor vs 2 of 53 (4%) who received placebo.
At week 52, the ALP level normalized in 15% of patients in the elafibranor group and none of the patients in the placebo group.
In a news release announcing approval of Iqirvo, the company notes that improvement in survival and prevention of liver decompensation events have not been demonstrated and that continued approval for PBC may be contingent upon verification and description of clinical benefit in confirmatory trials.
The most common adverse effects with Iqirvo, reported in ≥ 10% of study participants, were weight gain, abdominal pain, diarrhea, nausea, and vomiting. Iqirvo is not recommended for people who have or develop decompensated cirrhosis. Full prescribing information is available online.
The data show that Iqirvo is “an effective second-line treatment for patients with PBC with favorable benefit and risk data,” Kris Kowdley, MD, AGAF, director of the Liver Institute Northwest in Seattle, Washington, and a primary investigator on the ELATIVE study, said in the news release.
The approval of Iqirvo “will allow healthcare providers in the US to address an unmet need with the potential to significantly reduce ALP levels for our patients with PBC,” Dr. Kowdley said.
A version of this article appeared on Medscape.com.
FMT Could Prevent Recurrence of Hepatic Encephalopathy in Patients With Cirrhosis
MILAN — , results of a phase 2 randomized controlled trial show.
“Not only was FMT more beneficial, but also it didn’t matter which route of administration was used — oral or enema — which is good because people don’t really like enemas,” said Jasmohan S. Bajaj, MD, AGAF, professor, School of Medicine, Virginia Commonwealth University, Richmond, and hepatologist at Richmond VA Medical Center.
Donor background (including vegan or omnivore) and dose range also did not affect the efficacy of FMT, Dr. Bajaj said.
Dr. Bajaj presented the findings (Abstract GS-001) at the opening session of the annual European Association for the Study of the Liver (EASL) Congress 2024.
Hepatic encephalopathy is a complication of advanced liver disease that causes a dementia-like state. Standard treatment with lactulose and rifaximin often results in a lack of patient response, meaning the patient is constantly being readmitted to the hospital, Dr. Bajaj said.
“This is a burden for the family as well as the patients,” and is very difficult to manage from a clinical and psychosocial perspective, he said in an interview.
With FMT, “we are transferring an ecosystem of good microbes,” which modifies the gut microbiome in patients with advanced liver disease and reduces associated brain toxicity, Dr. Bajaj explained.
Resetting the Gut
The double-blind, randomized, placebo-controlled trial enrolled a total of 60 patients with cirrhosis who had experienced hepatic encephalopathy. Aged 61-65 years, participants had Model for End-Stage Liver Disease (MELD) scores of 12-13, all were taking lactulose and rifaximin, and all had experienced their last hepatic encephalopathy episode 8-13 months prior.
Participants had similar baseline cognition, Sickness Impact Profile (SIP), and cirrhosis severity. Those with recent infections, taking other antibiotics, with a MELD score > 22, had received a transplant, or were immunosuppressed were excluded.
Study participants were divided into four dose administration groups (n = 15 each): oral and enema active FMT therapy (group 1), oral active FMT and enema placebo (group 2), oral placebo and enema active FMT (group 3), and oral and enema placebo (group 4).
The range of FMT dose frequency was zero (all placebo), or one, two, or three FMT administrations, each given 1 month apart.
Two thirds of those receiving active FMT were given omnivore-donor FMT, and one third were given vegan-donor FMT, in addition to receiving standard of care.
“Colony-forming units were standard and the same whether given via oral capsule or enema,” Dr. Bajaj said. This is “similar to what we used in our phase 1 study.”
Intent-to-treat (ITT) analysis was performed with 6-month data. The primary outcomes were safety and hepatic encephalopathy recurrence defined as ≥ grade 2 on West-Haven criteria. Secondary outcomes included other adverse events, changes in infections, severity of cirrhosis and cognition, and patient-reported outcomes. A statistical regression for hepatic encephalopathy recurrence was also performed. Patients were followed for 6 months or until death.
One Dose of FMT Better Than None
Hepatic encephalopathy recurrence was highest (40%) in group 4 patients, compared with those in group 1 (13%), group 2 (13%), and group 3 (0%), as were liver-related hospitalizations (47% vs 7%-20%).
SIP total/physical and psych scores improved with FMT (P = .003).
When all patients were included in the analysis, the hepatic encephalopathy recurrence was related to dose number (odds radio [OR], 0.27; 95% CI, 0.10-0.79; P = .02), male sex (OR, 0.16; 95% CI, 0.03-0.89; P = .04), and physical SIP (OR, 1.05; 95% CI, 1.01-1.10, P = .05). However, when analyzing results from FMT recipients only, FMT dose, route of administration, and donor source were not found to affect recurrence.
Of those on placebo alone, six patients (40%) had a recurrence, compared with four on FMT (8.8%) in the combined FMT groups.
“As long as a patient received at least one FMT dose, they had a better response than a patient who had none,” Dr. Bajaj said.
Six patients dropped out; two in group 1 died after hepatic encephalopathy and falls, and one in group 2 died after a seizure. Three others did not return for follow-up visits. Four patients developed infections, including spontaneous bacterial peritonitis, cholecystitis, and cellulitis, all unrelated to FMT.
“I think many patients in Western countries are underserved because apart from lactulose and rifaximin, there is little else to give them,” Dr. Bajaj said. “The assumption is because rifaximin kills everything, we shouldn’t give FMT. But here, we administered it to a harsh and hostile wasteland of microbiota, and it still got a toehold and generated a reduction in hepatic encephalopathy.”
He pointed out that in smaller prior studies, the effects lasted up to 1 year.
Setting the Stage for Phase 3 Trials
Dr. Bajaj noted that this phase 2 study sets the stage for larger phase 3 trials in patients not responding to first-line therapy.
“Given how well-tolerated and effective FMT appears to be in these patients, if the larger phase 3 trial shows similar results, I can imagine FMT becoming a standard therapy,” said Colleen R. Kelly, MD, AGAF, gastroenterologist at Brigham and Women’s Hospital and Harvard Medical School, Boston, who was not involved in the study.
This study was built on Dr. Bajaj’s prior work that established the safety of FMT by enema, she added, stressing that this new research was incredibly important in these immunocompromised patients who are at higher risk for infection transmission.
That the administration route doesn’t matter is also an important finding as oral administration is much more feasible than enema, said Dr. Kelly, who went on to point out the importance of finding an alternative to rifaximin and lactulose, which are often poorly tolerated.
The study highlights the central role played by the gut microbiota in dysbiosis in the pathophysiology of hepatic encephalopathy, Dr. Kelly said. “It is another exciting example of how gut microbiota can be manipulated to treat disease.”
Dr. Bajaj and Dr. Kelly report no relevant financial relationships to this study.
A version of this article appeared on Medscape.com.
MILAN — , results of a phase 2 randomized controlled trial show.
“Not only was FMT more beneficial, but also it didn’t matter which route of administration was used — oral or enema — which is good because people don’t really like enemas,” said Jasmohan S. Bajaj, MD, AGAF, professor, School of Medicine, Virginia Commonwealth University, Richmond, and hepatologist at Richmond VA Medical Center.
Donor background (including vegan or omnivore) and dose range also did not affect the efficacy of FMT, Dr. Bajaj said.
Dr. Bajaj presented the findings (Abstract GS-001) at the opening session of the annual European Association for the Study of the Liver (EASL) Congress 2024.
Hepatic encephalopathy is a complication of advanced liver disease that causes a dementia-like state. Standard treatment with lactulose and rifaximin often results in a lack of patient response, meaning the patient is constantly being readmitted to the hospital, Dr. Bajaj said.
“This is a burden for the family as well as the patients,” and is very difficult to manage from a clinical and psychosocial perspective, he said in an interview.
With FMT, “we are transferring an ecosystem of good microbes,” which modifies the gut microbiome in patients with advanced liver disease and reduces associated brain toxicity, Dr. Bajaj explained.
Resetting the Gut
The double-blind, randomized, placebo-controlled trial enrolled a total of 60 patients with cirrhosis who had experienced hepatic encephalopathy. Aged 61-65 years, participants had Model for End-Stage Liver Disease (MELD) scores of 12-13, all were taking lactulose and rifaximin, and all had experienced their last hepatic encephalopathy episode 8-13 months prior.
Participants had similar baseline cognition, Sickness Impact Profile (SIP), and cirrhosis severity. Those with recent infections, taking other antibiotics, with a MELD score > 22, had received a transplant, or were immunosuppressed were excluded.
Study participants were divided into four dose administration groups (n = 15 each): oral and enema active FMT therapy (group 1), oral active FMT and enema placebo (group 2), oral placebo and enema active FMT (group 3), and oral and enema placebo (group 4).
The range of FMT dose frequency was zero (all placebo), or one, two, or three FMT administrations, each given 1 month apart.
Two thirds of those receiving active FMT were given omnivore-donor FMT, and one third were given vegan-donor FMT, in addition to receiving standard of care.
“Colony-forming units were standard and the same whether given via oral capsule or enema,” Dr. Bajaj said. This is “similar to what we used in our phase 1 study.”
Intent-to-treat (ITT) analysis was performed with 6-month data. The primary outcomes were safety and hepatic encephalopathy recurrence defined as ≥ grade 2 on West-Haven criteria. Secondary outcomes included other adverse events, changes in infections, severity of cirrhosis and cognition, and patient-reported outcomes. A statistical regression for hepatic encephalopathy recurrence was also performed. Patients were followed for 6 months or until death.
One Dose of FMT Better Than None
Hepatic encephalopathy recurrence was highest (40%) in group 4 patients, compared with those in group 1 (13%), group 2 (13%), and group 3 (0%), as were liver-related hospitalizations (47% vs 7%-20%).
SIP total/physical and psych scores improved with FMT (P = .003).
When all patients were included in the analysis, the hepatic encephalopathy recurrence was related to dose number (odds radio [OR], 0.27; 95% CI, 0.10-0.79; P = .02), male sex (OR, 0.16; 95% CI, 0.03-0.89; P = .04), and physical SIP (OR, 1.05; 95% CI, 1.01-1.10, P = .05). However, when analyzing results from FMT recipients only, FMT dose, route of administration, and donor source were not found to affect recurrence.
Of those on placebo alone, six patients (40%) had a recurrence, compared with four on FMT (8.8%) in the combined FMT groups.
“As long as a patient received at least one FMT dose, they had a better response than a patient who had none,” Dr. Bajaj said.
Six patients dropped out; two in group 1 died after hepatic encephalopathy and falls, and one in group 2 died after a seizure. Three others did not return for follow-up visits. Four patients developed infections, including spontaneous bacterial peritonitis, cholecystitis, and cellulitis, all unrelated to FMT.
“I think many patients in Western countries are underserved because apart from lactulose and rifaximin, there is little else to give them,” Dr. Bajaj said. “The assumption is because rifaximin kills everything, we shouldn’t give FMT. But here, we administered it to a harsh and hostile wasteland of microbiota, and it still got a toehold and generated a reduction in hepatic encephalopathy.”
He pointed out that in smaller prior studies, the effects lasted up to 1 year.
Setting the Stage for Phase 3 Trials
Dr. Bajaj noted that this phase 2 study sets the stage for larger phase 3 trials in patients not responding to first-line therapy.
“Given how well-tolerated and effective FMT appears to be in these patients, if the larger phase 3 trial shows similar results, I can imagine FMT becoming a standard therapy,” said Colleen R. Kelly, MD, AGAF, gastroenterologist at Brigham and Women’s Hospital and Harvard Medical School, Boston, who was not involved in the study.
This study was built on Dr. Bajaj’s prior work that established the safety of FMT by enema, she added, stressing that this new research was incredibly important in these immunocompromised patients who are at higher risk for infection transmission.
That the administration route doesn’t matter is also an important finding as oral administration is much more feasible than enema, said Dr. Kelly, who went on to point out the importance of finding an alternative to rifaximin and lactulose, which are often poorly tolerated.
The study highlights the central role played by the gut microbiota in dysbiosis in the pathophysiology of hepatic encephalopathy, Dr. Kelly said. “It is another exciting example of how gut microbiota can be manipulated to treat disease.”
Dr. Bajaj and Dr. Kelly report no relevant financial relationships to this study.
A version of this article appeared on Medscape.com.
MILAN — , results of a phase 2 randomized controlled trial show.
“Not only was FMT more beneficial, but also it didn’t matter which route of administration was used — oral or enema — which is good because people don’t really like enemas,” said Jasmohan S. Bajaj, MD, AGAF, professor, School of Medicine, Virginia Commonwealth University, Richmond, and hepatologist at Richmond VA Medical Center.
Donor background (including vegan or omnivore) and dose range also did not affect the efficacy of FMT, Dr. Bajaj said.
Dr. Bajaj presented the findings (Abstract GS-001) at the opening session of the annual European Association for the Study of the Liver (EASL) Congress 2024.
Hepatic encephalopathy is a complication of advanced liver disease that causes a dementia-like state. Standard treatment with lactulose and rifaximin often results in a lack of patient response, meaning the patient is constantly being readmitted to the hospital, Dr. Bajaj said.
“This is a burden for the family as well as the patients,” and is very difficult to manage from a clinical and psychosocial perspective, he said in an interview.
With FMT, “we are transferring an ecosystem of good microbes,” which modifies the gut microbiome in patients with advanced liver disease and reduces associated brain toxicity, Dr. Bajaj explained.
Resetting the Gut
The double-blind, randomized, placebo-controlled trial enrolled a total of 60 patients with cirrhosis who had experienced hepatic encephalopathy. Aged 61-65 years, participants had Model for End-Stage Liver Disease (MELD) scores of 12-13, all were taking lactulose and rifaximin, and all had experienced their last hepatic encephalopathy episode 8-13 months prior.
Participants had similar baseline cognition, Sickness Impact Profile (SIP), and cirrhosis severity. Those with recent infections, taking other antibiotics, with a MELD score > 22, had received a transplant, or were immunosuppressed were excluded.
Study participants were divided into four dose administration groups (n = 15 each): oral and enema active FMT therapy (group 1), oral active FMT and enema placebo (group 2), oral placebo and enema active FMT (group 3), and oral and enema placebo (group 4).
The range of FMT dose frequency was zero (all placebo), or one, two, or three FMT administrations, each given 1 month apart.
Two thirds of those receiving active FMT were given omnivore-donor FMT, and one third were given vegan-donor FMT, in addition to receiving standard of care.
“Colony-forming units were standard and the same whether given via oral capsule or enema,” Dr. Bajaj said. This is “similar to what we used in our phase 1 study.”
Intent-to-treat (ITT) analysis was performed with 6-month data. The primary outcomes were safety and hepatic encephalopathy recurrence defined as ≥ grade 2 on West-Haven criteria. Secondary outcomes included other adverse events, changes in infections, severity of cirrhosis and cognition, and patient-reported outcomes. A statistical regression for hepatic encephalopathy recurrence was also performed. Patients were followed for 6 months or until death.
One Dose of FMT Better Than None
Hepatic encephalopathy recurrence was highest (40%) in group 4 patients, compared with those in group 1 (13%), group 2 (13%), and group 3 (0%), as were liver-related hospitalizations (47% vs 7%-20%).
SIP total/physical and psych scores improved with FMT (P = .003).
When all patients were included in the analysis, the hepatic encephalopathy recurrence was related to dose number (odds radio [OR], 0.27; 95% CI, 0.10-0.79; P = .02), male sex (OR, 0.16; 95% CI, 0.03-0.89; P = .04), and physical SIP (OR, 1.05; 95% CI, 1.01-1.10, P = .05). However, when analyzing results from FMT recipients only, FMT dose, route of administration, and donor source were not found to affect recurrence.
Of those on placebo alone, six patients (40%) had a recurrence, compared with four on FMT (8.8%) in the combined FMT groups.
“As long as a patient received at least one FMT dose, they had a better response than a patient who had none,” Dr. Bajaj said.
Six patients dropped out; two in group 1 died after hepatic encephalopathy and falls, and one in group 2 died after a seizure. Three others did not return for follow-up visits. Four patients developed infections, including spontaneous bacterial peritonitis, cholecystitis, and cellulitis, all unrelated to FMT.
“I think many patients in Western countries are underserved because apart from lactulose and rifaximin, there is little else to give them,” Dr. Bajaj said. “The assumption is because rifaximin kills everything, we shouldn’t give FMT. But here, we administered it to a harsh and hostile wasteland of microbiota, and it still got a toehold and generated a reduction in hepatic encephalopathy.”
He pointed out that in smaller prior studies, the effects lasted up to 1 year.
Setting the Stage for Phase 3 Trials
Dr. Bajaj noted that this phase 2 study sets the stage for larger phase 3 trials in patients not responding to first-line therapy.
“Given how well-tolerated and effective FMT appears to be in these patients, if the larger phase 3 trial shows similar results, I can imagine FMT becoming a standard therapy,” said Colleen R. Kelly, MD, AGAF, gastroenterologist at Brigham and Women’s Hospital and Harvard Medical School, Boston, who was not involved in the study.
This study was built on Dr. Bajaj’s prior work that established the safety of FMT by enema, she added, stressing that this new research was incredibly important in these immunocompromised patients who are at higher risk for infection transmission.
That the administration route doesn’t matter is also an important finding as oral administration is much more feasible than enema, said Dr. Kelly, who went on to point out the importance of finding an alternative to rifaximin and lactulose, which are often poorly tolerated.
The study highlights the central role played by the gut microbiota in dysbiosis in the pathophysiology of hepatic encephalopathy, Dr. Kelly said. “It is another exciting example of how gut microbiota can be manipulated to treat disease.”
Dr. Bajaj and Dr. Kelly report no relevant financial relationships to this study.
A version of this article appeared on Medscape.com.
FROM EASL 2024
Emerging Evidence Supports Dietary Management of MASLD Through Gut-Liver Axis
WASHINGTON — , according to a study presented at the annual Digestive Disease Week® (DDW).
For instance, patients with MASLD had lower intake of fiber and omega-3 fatty acids but higher consumption of added sugars and ultraprocessed foods, which correlated with the associated bacterial species and functional pathways.
“MASLD is an escalating concern globally, which highlights the need for innovative targets for disease prevention and management,” said lead author Georgina Williams, PhD, a postdoctoral researcher in diet and gastroenterology at the University of Newcastle, Australia.
“Therapeutic options often rely on lifestyle modifications, with a focus on weight loss,” she said. “Diet is considered a key component of disease management.”
Although calorie restriction with a 3%-5% fat loss is associated with hepatic benefits in MASLD, Dr. Williams noted, researchers have considered whole dietary patterns and the best fit for patients. Aspects of the Mediterranean diet may be effective, as reflected in recommendations from the American Association for the Study of Liver Disease (AASLD), which highlight dietary components such as limited carbohydrates and saturated fat, along with high fiber and unsaturated fats. The gut microbiome may be essential to consider as well, she said, given MASLD-associated differences in bile acid metabolism, inflammation, and ethanol production.
Dr. Williams and colleagues conducted a retrospective case-control study in an outpatient liver clinic to understand diet and dysbiosis in MASLD, looking at differences in diet, gut microbiota composition, and functional pathways in those with and without MASLD. The researchers investigated daily average intake, serum, and stool samples among 50 people (25 per group) matched for age and gender, comparing fibrosis-4, MASLD severity scores, macronutrients, micronutrients, food groups, metagenomic sequencing, and inflammatory markers such as interleukin (IL)-1ß, IL-6, tumor necrosis factor (TNF)-α, cytokeratin (CK)-18, and high-sensitivity C-reactive protein (hsCRP).
Dietary Characteristics
At baseline, the groups differed by ethnicity, prescription medication use, and body mass index (BMI), where the MASLD group had greater ethnic diversity, medication use, and BMI. In addition, the MASLD group had a zero to mild score of fibrosis.
Overall, energy intake didn’t differ significantly between the two groups. The control group had higher alcohol intake, likely since the MASLD group was recommended to reduce alcohol intake, though the difference was about 5 grams per day. The MASLD group also had less caffeine intake than the control group, as well as slightly lower protein intake, though the differences weren’t statistically significant.
While consumption of total carbohydrates didn’t differ significantly between the groups, participants with MASLD consumed more calories from carbohydrates than did the controls. The MASLD group consumed more calories from added and free sugars and didn’t meet recommendations for dietary fiber.
With particular food groups, participants with MASLD ate significantly fewer whole grains, red and orange fruits, and leafy green vegetables. When consuming fruit, those with MASLD were more likely to drink juice than eat whole fruit. These findings could be relevant when considering high sugar intake and low dietary fiber, Dr. Williams said.
With dietary fat, there were no differences in total fat between the groups, but the fat profiles differed. The control group was significantly more likely to consume omega-3 fatty acids, including alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA), and docosahexaenoic acid (DHA). The MASLD group was less likely to consume seafood, nuts, seeds, avocado, and olive oil.
With inflammatory markers, hsCRP and CK-18 were increased in MASLD, while IL-1ß was increased in controls, which was consistently associated with higher alcohol intake among the control group. IL-6 and TNF-α didn’t differ between the groups.
Notably, dietary fats were most consistently associated with inflammatory markers, Dr. Williams said, with inflammation being positively associated with saturated fats and negatively associated with unsaturated fats.
Looking at microbiota, the alpha diversity was no different, but the beta diversity was across 162 taxa. Per bacterial species, there was an inverse relationship between MASLD and associations with unsaturated fat, as well as positive indicators of high sugar and fructose intake and low unsaturated fat and dietary fiber intake.
Beyond that, the functional pathways enriched in MASLD were associated with increased sugar and carbohydrates, reduced fiber, and reduced unsaturated fat. Lower butyrate production in MASLD was associated with low intake of nuts, seeds, and unsaturated fat.
In Clinical Practice
Dr. Williams suggested reinforcing AASLD guidelines and looking at diet quality, not just diet quantity. Although an energy deficit remains relevant in MASLD, macronutrient consumption matters across dietary fats, fibers, and sugars.
Future avenues for research include metabolomic pathways related to bile acids and fatty acids, she said, as well as disentangling metabolic syndrome from MASLD outcomes.
Session moderator Olivier Barbier, PhD, professor of pharmacy at Laval University in Quebec, Canada, asked about microbiome differences across countries. Dr. Williams noted the limitations in this study of looking at differences across geography and ethnicity, particularly in Australia, but said the species identified were consistent with those found in most literature globally.
In response to other questions after the presentation, Dr. Williams said supplements (such as omega-3 fatty acids) were included in total intake, and those taking prebiotics or probiotics were excluded from the study. In an upcoming clinical trial, she and colleagues plan to control for household microbiomes as well.
“The premise is that microbiomes are shared between households, so when you’re doing these sorts of large-scale clinical studies, if you’re going to look at the microbiome, then you should control for one of the major confounding variables,” said Mark Sundrud, PhD, professor of medicine at the Dartmouth Center for Digestive Health in Lebanon, New Hampshire. Dr. Sundrud, who wasn’t involved with this study, presented on the role of bile acids in mucosal immune cell function at DDW.
“We’ve done a collaborative study looking at microbiomes and bile acids in inflammatory bowel disease (IBD) patients versus controls,” which included consideration of households, he said. “We were able to see more intrinsic disease-specific changes.”
Dr. Williams declared no relevant disclosures. Dr. Sundrud has served as a scientific adviser to Sage Therapeutics.
WASHINGTON — , according to a study presented at the annual Digestive Disease Week® (DDW).
For instance, patients with MASLD had lower intake of fiber and omega-3 fatty acids but higher consumption of added sugars and ultraprocessed foods, which correlated with the associated bacterial species and functional pathways.
“MASLD is an escalating concern globally, which highlights the need for innovative targets for disease prevention and management,” said lead author Georgina Williams, PhD, a postdoctoral researcher in diet and gastroenterology at the University of Newcastle, Australia.
“Therapeutic options often rely on lifestyle modifications, with a focus on weight loss,” she said. “Diet is considered a key component of disease management.”
Although calorie restriction with a 3%-5% fat loss is associated with hepatic benefits in MASLD, Dr. Williams noted, researchers have considered whole dietary patterns and the best fit for patients. Aspects of the Mediterranean diet may be effective, as reflected in recommendations from the American Association for the Study of Liver Disease (AASLD), which highlight dietary components such as limited carbohydrates and saturated fat, along with high fiber and unsaturated fats. The gut microbiome may be essential to consider as well, she said, given MASLD-associated differences in bile acid metabolism, inflammation, and ethanol production.
Dr. Williams and colleagues conducted a retrospective case-control study in an outpatient liver clinic to understand diet and dysbiosis in MASLD, looking at differences in diet, gut microbiota composition, and functional pathways in those with and without MASLD. The researchers investigated daily average intake, serum, and stool samples among 50 people (25 per group) matched for age and gender, comparing fibrosis-4, MASLD severity scores, macronutrients, micronutrients, food groups, metagenomic sequencing, and inflammatory markers such as interleukin (IL)-1ß, IL-6, tumor necrosis factor (TNF)-α, cytokeratin (CK)-18, and high-sensitivity C-reactive protein (hsCRP).
Dietary Characteristics
At baseline, the groups differed by ethnicity, prescription medication use, and body mass index (BMI), where the MASLD group had greater ethnic diversity, medication use, and BMI. In addition, the MASLD group had a zero to mild score of fibrosis.
Overall, energy intake didn’t differ significantly between the two groups. The control group had higher alcohol intake, likely since the MASLD group was recommended to reduce alcohol intake, though the difference was about 5 grams per day. The MASLD group also had less caffeine intake than the control group, as well as slightly lower protein intake, though the differences weren’t statistically significant.
While consumption of total carbohydrates didn’t differ significantly between the groups, participants with MASLD consumed more calories from carbohydrates than did the controls. The MASLD group consumed more calories from added and free sugars and didn’t meet recommendations for dietary fiber.
With particular food groups, participants with MASLD ate significantly fewer whole grains, red and orange fruits, and leafy green vegetables. When consuming fruit, those with MASLD were more likely to drink juice than eat whole fruit. These findings could be relevant when considering high sugar intake and low dietary fiber, Dr. Williams said.
With dietary fat, there were no differences in total fat between the groups, but the fat profiles differed. The control group was significantly more likely to consume omega-3 fatty acids, including alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA), and docosahexaenoic acid (DHA). The MASLD group was less likely to consume seafood, nuts, seeds, avocado, and olive oil.
With inflammatory markers, hsCRP and CK-18 were increased in MASLD, while IL-1ß was increased in controls, which was consistently associated with higher alcohol intake among the control group. IL-6 and TNF-α didn’t differ between the groups.
Notably, dietary fats were most consistently associated with inflammatory markers, Dr. Williams said, with inflammation being positively associated with saturated fats and negatively associated with unsaturated fats.
Looking at microbiota, the alpha diversity was no different, but the beta diversity was across 162 taxa. Per bacterial species, there was an inverse relationship between MASLD and associations with unsaturated fat, as well as positive indicators of high sugar and fructose intake and low unsaturated fat and dietary fiber intake.
Beyond that, the functional pathways enriched in MASLD were associated with increased sugar and carbohydrates, reduced fiber, and reduced unsaturated fat. Lower butyrate production in MASLD was associated with low intake of nuts, seeds, and unsaturated fat.
In Clinical Practice
Dr. Williams suggested reinforcing AASLD guidelines and looking at diet quality, not just diet quantity. Although an energy deficit remains relevant in MASLD, macronutrient consumption matters across dietary fats, fibers, and sugars.
Future avenues for research include metabolomic pathways related to bile acids and fatty acids, she said, as well as disentangling metabolic syndrome from MASLD outcomes.
Session moderator Olivier Barbier, PhD, professor of pharmacy at Laval University in Quebec, Canada, asked about microbiome differences across countries. Dr. Williams noted the limitations in this study of looking at differences across geography and ethnicity, particularly in Australia, but said the species identified were consistent with those found in most literature globally.
In response to other questions after the presentation, Dr. Williams said supplements (such as omega-3 fatty acids) were included in total intake, and those taking prebiotics or probiotics were excluded from the study. In an upcoming clinical trial, she and colleagues plan to control for household microbiomes as well.
“The premise is that microbiomes are shared between households, so when you’re doing these sorts of large-scale clinical studies, if you’re going to look at the microbiome, then you should control for one of the major confounding variables,” said Mark Sundrud, PhD, professor of medicine at the Dartmouth Center for Digestive Health in Lebanon, New Hampshire. Dr. Sundrud, who wasn’t involved with this study, presented on the role of bile acids in mucosal immune cell function at DDW.
“We’ve done a collaborative study looking at microbiomes and bile acids in inflammatory bowel disease (IBD) patients versus controls,” which included consideration of households, he said. “We were able to see more intrinsic disease-specific changes.”
Dr. Williams declared no relevant disclosures. Dr. Sundrud has served as a scientific adviser to Sage Therapeutics.
WASHINGTON — , according to a study presented at the annual Digestive Disease Week® (DDW).
For instance, patients with MASLD had lower intake of fiber and omega-3 fatty acids but higher consumption of added sugars and ultraprocessed foods, which correlated with the associated bacterial species and functional pathways.
“MASLD is an escalating concern globally, which highlights the need for innovative targets for disease prevention and management,” said lead author Georgina Williams, PhD, a postdoctoral researcher in diet and gastroenterology at the University of Newcastle, Australia.
“Therapeutic options often rely on lifestyle modifications, with a focus on weight loss,” she said. “Diet is considered a key component of disease management.”
Although calorie restriction with a 3%-5% fat loss is associated with hepatic benefits in MASLD, Dr. Williams noted, researchers have considered whole dietary patterns and the best fit for patients. Aspects of the Mediterranean diet may be effective, as reflected in recommendations from the American Association for the Study of Liver Disease (AASLD), which highlight dietary components such as limited carbohydrates and saturated fat, along with high fiber and unsaturated fats. The gut microbiome may be essential to consider as well, she said, given MASLD-associated differences in bile acid metabolism, inflammation, and ethanol production.
Dr. Williams and colleagues conducted a retrospective case-control study in an outpatient liver clinic to understand diet and dysbiosis in MASLD, looking at differences in diet, gut microbiota composition, and functional pathways in those with and without MASLD. The researchers investigated daily average intake, serum, and stool samples among 50 people (25 per group) matched for age and gender, comparing fibrosis-4, MASLD severity scores, macronutrients, micronutrients, food groups, metagenomic sequencing, and inflammatory markers such as interleukin (IL)-1ß, IL-6, tumor necrosis factor (TNF)-α, cytokeratin (CK)-18, and high-sensitivity C-reactive protein (hsCRP).
Dietary Characteristics
At baseline, the groups differed by ethnicity, prescription medication use, and body mass index (BMI), where the MASLD group had greater ethnic diversity, medication use, and BMI. In addition, the MASLD group had a zero to mild score of fibrosis.
Overall, energy intake didn’t differ significantly between the two groups. The control group had higher alcohol intake, likely since the MASLD group was recommended to reduce alcohol intake, though the difference was about 5 grams per day. The MASLD group also had less caffeine intake than the control group, as well as slightly lower protein intake, though the differences weren’t statistically significant.
While consumption of total carbohydrates didn’t differ significantly between the groups, participants with MASLD consumed more calories from carbohydrates than did the controls. The MASLD group consumed more calories from added and free sugars and didn’t meet recommendations for dietary fiber.
With particular food groups, participants with MASLD ate significantly fewer whole grains, red and orange fruits, and leafy green vegetables. When consuming fruit, those with MASLD were more likely to drink juice than eat whole fruit. These findings could be relevant when considering high sugar intake and low dietary fiber, Dr. Williams said.
With dietary fat, there were no differences in total fat between the groups, but the fat profiles differed. The control group was significantly more likely to consume omega-3 fatty acids, including alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA), and docosahexaenoic acid (DHA). The MASLD group was less likely to consume seafood, nuts, seeds, avocado, and olive oil.
With inflammatory markers, hsCRP and CK-18 were increased in MASLD, while IL-1ß was increased in controls, which was consistently associated with higher alcohol intake among the control group. IL-6 and TNF-α didn’t differ between the groups.
Notably, dietary fats were most consistently associated with inflammatory markers, Dr. Williams said, with inflammation being positively associated with saturated fats and negatively associated with unsaturated fats.
Looking at microbiota, the alpha diversity was no different, but the beta diversity was across 162 taxa. Per bacterial species, there was an inverse relationship between MASLD and associations with unsaturated fat, as well as positive indicators of high sugar and fructose intake and low unsaturated fat and dietary fiber intake.
Beyond that, the functional pathways enriched in MASLD were associated with increased sugar and carbohydrates, reduced fiber, and reduced unsaturated fat. Lower butyrate production in MASLD was associated with low intake of nuts, seeds, and unsaturated fat.
In Clinical Practice
Dr. Williams suggested reinforcing AASLD guidelines and looking at diet quality, not just diet quantity. Although an energy deficit remains relevant in MASLD, macronutrient consumption matters across dietary fats, fibers, and sugars.
Future avenues for research include metabolomic pathways related to bile acids and fatty acids, she said, as well as disentangling metabolic syndrome from MASLD outcomes.
Session moderator Olivier Barbier, PhD, professor of pharmacy at Laval University in Quebec, Canada, asked about microbiome differences across countries. Dr. Williams noted the limitations in this study of looking at differences across geography and ethnicity, particularly in Australia, but said the species identified were consistent with those found in most literature globally.
In response to other questions after the presentation, Dr. Williams said supplements (such as omega-3 fatty acids) were included in total intake, and those taking prebiotics or probiotics were excluded from the study. In an upcoming clinical trial, she and colleagues plan to control for household microbiomes as well.
“The premise is that microbiomes are shared between households, so when you’re doing these sorts of large-scale clinical studies, if you’re going to look at the microbiome, then you should control for one of the major confounding variables,” said Mark Sundrud, PhD, professor of medicine at the Dartmouth Center for Digestive Health in Lebanon, New Hampshire. Dr. Sundrud, who wasn’t involved with this study, presented on the role of bile acids in mucosal immune cell function at DDW.
“We’ve done a collaborative study looking at microbiomes and bile acids in inflammatory bowel disease (IBD) patients versus controls,” which included consideration of households, he said. “We were able to see more intrinsic disease-specific changes.”
Dr. Williams declared no relevant disclosures. Dr. Sundrud has served as a scientific adviser to Sage Therapeutics.
FROM DDW 2024