User login
Valproate, topiramate prescribed in young women despite known teratogenicity risks
results of a retrospective analysis suggest.
Topiramate, linked to increased risk of cleft palate and smaller-than-gestational-age newborns, was among the top three antiepileptic drugs (AEDs) prescribed to women 15-44 years of age in the population-based cohort study.
Valproate, linked to increases in both anatomic and behavioral teratogenicity, was less often prescribed, but nevertheless still prescribed in a considerable proportion of patients in the study, which looked at U.S. commercial, Medicare, and Medicaid claims data from 2009 to 2013.
Presence of comorbidities could be influencing whether or not a woman of childbearing age receives one of these AEDs, the investigators said. Specifically, they found valproate more often prescribed for women with epilepsy who also had mood or anxiety and dissociative disorder, while topiramate was more often prescribed in women with headaches or migraines.
Taken together, these findings suggest a lack of awareness of the teratogenic risks of valproate and topiramate, said the investigators, led by Hyunmi Kim, MD, PhD, MPH, of the department of neurology at Stanford (Calif.) University.
“To improve current practice, knowledge of the teratogenicity of certain AEDs should be disseminated to health care professionals and patients,” they wrote. The report is in JAMA Neurology.
The findings of Dr. Kim and her colleagues were based on data for 46,767 women of childbearing age: 8,003 incident (new) cases with a mean age of 27 years, and 38,764 prevalent cases with a mean age of 30 years.
Topiramate was the second- or third-most prescribed AED in the analyses, alongside levetiracetam and lamotrigine. In particular, topiramate prescriptions were found in incident cases receiving first-line monotherapy (15%), prevalent cases receiving first-line monotherapy (13%), and prevalent cases receiving polytherapy (29%).
Valproate was the fifth-most prescribed AED for incident and prevalent cases receiving first-line monotherapy (5% and 10%, respectively), and came in fourth place among prevalent cases receiving polytherapy (22%).
The somewhat lower rate of valproate prescriptions tracks with other recent analyses showing that valproate use decreased among women of childbearing age following recommendations against its use during pregnancy, according to Dr. Kim and her coauthors.
However, topiramate is another story: “Although the magnitude of risk and range of adverse reproductive outcomes associated with topiramate use appear substantially less than those associated with valproate, some reduction in the use of topiramate in this population might be expected after evidence emerged in 2008 of its association with cleft palate,” they said in their report.
UCB Pharma sponsored this study. Study authors reported disclosures related to UCB Pharma, Biogen, Eisai, SK Life Science, Brain Sentinel, UCB Pharma, and the University of Alabama at Birmingham.
SOURCE: Kim H et al. JAMA Neurol. 2019 Apr 1. doi: 10.1001/jamaneurol.2019.0447.
results of a retrospective analysis suggest.
Topiramate, linked to increased risk of cleft palate and smaller-than-gestational-age newborns, was among the top three antiepileptic drugs (AEDs) prescribed to women 15-44 years of age in the population-based cohort study.
Valproate, linked to increases in both anatomic and behavioral teratogenicity, was less often prescribed, but nevertheless still prescribed in a considerable proportion of patients in the study, which looked at U.S. commercial, Medicare, and Medicaid claims data from 2009 to 2013.
Presence of comorbidities could be influencing whether or not a woman of childbearing age receives one of these AEDs, the investigators said. Specifically, they found valproate more often prescribed for women with epilepsy who also had mood or anxiety and dissociative disorder, while topiramate was more often prescribed in women with headaches or migraines.
Taken together, these findings suggest a lack of awareness of the teratogenic risks of valproate and topiramate, said the investigators, led by Hyunmi Kim, MD, PhD, MPH, of the department of neurology at Stanford (Calif.) University.
“To improve current practice, knowledge of the teratogenicity of certain AEDs should be disseminated to health care professionals and patients,” they wrote. The report is in JAMA Neurology.
The findings of Dr. Kim and her colleagues were based on data for 46,767 women of childbearing age: 8,003 incident (new) cases with a mean age of 27 years, and 38,764 prevalent cases with a mean age of 30 years.
Topiramate was the second- or third-most prescribed AED in the analyses, alongside levetiracetam and lamotrigine. In particular, topiramate prescriptions were found in incident cases receiving first-line monotherapy (15%), prevalent cases receiving first-line monotherapy (13%), and prevalent cases receiving polytherapy (29%).
Valproate was the fifth-most prescribed AED for incident and prevalent cases receiving first-line monotherapy (5% and 10%, respectively), and came in fourth place among prevalent cases receiving polytherapy (22%).
The somewhat lower rate of valproate prescriptions tracks with other recent analyses showing that valproate use decreased among women of childbearing age following recommendations against its use during pregnancy, according to Dr. Kim and her coauthors.
However, topiramate is another story: “Although the magnitude of risk and range of adverse reproductive outcomes associated with topiramate use appear substantially less than those associated with valproate, some reduction in the use of topiramate in this population might be expected after evidence emerged in 2008 of its association with cleft palate,” they said in their report.
UCB Pharma sponsored this study. Study authors reported disclosures related to UCB Pharma, Biogen, Eisai, SK Life Science, Brain Sentinel, UCB Pharma, and the University of Alabama at Birmingham.
SOURCE: Kim H et al. JAMA Neurol. 2019 Apr 1. doi: 10.1001/jamaneurol.2019.0447.
results of a retrospective analysis suggest.
Topiramate, linked to increased risk of cleft palate and smaller-than-gestational-age newborns, was among the top three antiepileptic drugs (AEDs) prescribed to women 15-44 years of age in the population-based cohort study.
Valproate, linked to increases in both anatomic and behavioral teratogenicity, was less often prescribed, but nevertheless still prescribed in a considerable proportion of patients in the study, which looked at U.S. commercial, Medicare, and Medicaid claims data from 2009 to 2013.
Presence of comorbidities could be influencing whether or not a woman of childbearing age receives one of these AEDs, the investigators said. Specifically, they found valproate more often prescribed for women with epilepsy who also had mood or anxiety and dissociative disorder, while topiramate was more often prescribed in women with headaches or migraines.
Taken together, these findings suggest a lack of awareness of the teratogenic risks of valproate and topiramate, said the investigators, led by Hyunmi Kim, MD, PhD, MPH, of the department of neurology at Stanford (Calif.) University.
“To improve current practice, knowledge of the teratogenicity of certain AEDs should be disseminated to health care professionals and patients,” they wrote. The report is in JAMA Neurology.
The findings of Dr. Kim and her colleagues were based on data for 46,767 women of childbearing age: 8,003 incident (new) cases with a mean age of 27 years, and 38,764 prevalent cases with a mean age of 30 years.
Topiramate was the second- or third-most prescribed AED in the analyses, alongside levetiracetam and lamotrigine. In particular, topiramate prescriptions were found in incident cases receiving first-line monotherapy (15%), prevalent cases receiving first-line monotherapy (13%), and prevalent cases receiving polytherapy (29%).
Valproate was the fifth-most prescribed AED for incident and prevalent cases receiving first-line monotherapy (5% and 10%, respectively), and came in fourth place among prevalent cases receiving polytherapy (22%).
The somewhat lower rate of valproate prescriptions tracks with other recent analyses showing that valproate use decreased among women of childbearing age following recommendations against its use during pregnancy, according to Dr. Kim and her coauthors.
However, topiramate is another story: “Although the magnitude of risk and range of adverse reproductive outcomes associated with topiramate use appear substantially less than those associated with valproate, some reduction in the use of topiramate in this population might be expected after evidence emerged in 2008 of its association with cleft palate,” they said in their report.
UCB Pharma sponsored this study. Study authors reported disclosures related to UCB Pharma, Biogen, Eisai, SK Life Science, Brain Sentinel, UCB Pharma, and the University of Alabama at Birmingham.
SOURCE: Kim H et al. JAMA Neurol. 2019 Apr 1. doi: 10.1001/jamaneurol.2019.0447.
FROM JAMA NEUROLOGY
Key clinical point: Both valproate and topiramate are prescribed relatively often in women of childbearing age despite known teratogenic risks.
Major finding: Topiramate was the second- or third-most prescribed AED in the analyses. Valproate was the fifth-most prescribed AED for incident and prevalent cases receiving first-line monotherapy.
Study details: Retrospective cohort study including nearly 47,000 women of childbearing age enrolled in claims databases between 2009 and 2013.
Disclosures: UCB Pharma sponsored the study. Study authors reported disclosures related to UCB Pharma, Biogen, Eisai, SK Life Science, Brain Sentinel, UCB Pharma, and the University of Alabama at Birmingham.
Source: Kim H et al. JAMA Neurol. 2019 Apr 1. doi: 10.1001/jamaneurol.2019.0447.
Many EMS protocols for status epilepticus do not follow evidence-based guidelines
“Many protocols did not follow evidence-based guidelines and did not accurately define generalized convulsive status epilepticus,” said John P. Betjemann, MD, associate professor of neurology at the University of California, San Francisco, and his colleagues. They reported their findings in the March 26 issue of JAMA.
Generalized convulsive status epilepticus is a neurologic emergency, and trials published in 2001 and 2012 found that benzodiazepines are effective prehospital treatments for patients with generalized convulsive status epilepticus. These trials informed a 2016 evidence-based guideline that cites level A evidence for intramuscular midazolam, IV lorazepam, and IV diazepam as initial treatment options for adults.
To determine whether EMS system protocols follow these recommendations, the investigators reviewed treatment protocols from 33 EMS systems that cover the 58 counties in California. The researchers reviewed EMS system protocols between May and June 2018 to determine when they were last updated and whether they defined generalized convulsive status epilepticus according to the guideline (namely, 5 or more minutes of continuous seizure or two or more discrete seizures between which a patient has incomplete recovery of consciousness). They also determined whether the protocols included any of the three benzodiazepines in the guideline and, if so, at what dose and using which route of administration.
Protocols’ most recent revision dates ranged between 2007 and 2018. Twenty-seven protocols (81.8%) were revised after the second clinical trial was published in 2012, and 17 (51.5%) were revised after the 2016 guideline. Seven EMS system protocols (21.2%) defined generalized convulsive status epilepticus according to the guideline. Thirty-two protocols (97.0%) included intramuscular midazolam, 2 (6.1%) included IV lorazepam, and 5 (15.2%) included IV diazepam.
Although the protocols “appropriately emphasized” intramuscular midazolam, the protocol doses often were lower than those used in the trials or recommended in the guideline. In addition, most protocols listed IV and intraosseous midazolam as options, although these treatments were not studied in the trials nor recommended in the guideline. In all, six of the protocols (18.2%) recommended at least one medication by the route and dose suggested in the trials or in the guideline.
“Why EMS system protocols deviate from the evidence and how this affects patient outcomes deserves further study,” the authors said.
The researchers noted that they examined EMS protocols in only one state and that “protocols may not necessarily reflect what emergency medical technicians actually do in practice.” In addition, the researchers accessed the most recent protocols by consulting EMS system websites rather than by contacting each EMS system for its most up-to-date protocol.
The authors reported personal compensation from JAMA Neurology and from Continuum Audio unrelated to the present study, as well as grants from the National Institutes of Health.
SOURCE: Betjemann JP et al. JAMA. 2019 Mar 26.
“Many protocols did not follow evidence-based guidelines and did not accurately define generalized convulsive status epilepticus,” said John P. Betjemann, MD, associate professor of neurology at the University of California, San Francisco, and his colleagues. They reported their findings in the March 26 issue of JAMA.
Generalized convulsive status epilepticus is a neurologic emergency, and trials published in 2001 and 2012 found that benzodiazepines are effective prehospital treatments for patients with generalized convulsive status epilepticus. These trials informed a 2016 evidence-based guideline that cites level A evidence for intramuscular midazolam, IV lorazepam, and IV diazepam as initial treatment options for adults.
To determine whether EMS system protocols follow these recommendations, the investigators reviewed treatment protocols from 33 EMS systems that cover the 58 counties in California. The researchers reviewed EMS system protocols between May and June 2018 to determine when they were last updated and whether they defined generalized convulsive status epilepticus according to the guideline (namely, 5 or more minutes of continuous seizure or two or more discrete seizures between which a patient has incomplete recovery of consciousness). They also determined whether the protocols included any of the three benzodiazepines in the guideline and, if so, at what dose and using which route of administration.
Protocols’ most recent revision dates ranged between 2007 and 2018. Twenty-seven protocols (81.8%) were revised after the second clinical trial was published in 2012, and 17 (51.5%) were revised after the 2016 guideline. Seven EMS system protocols (21.2%) defined generalized convulsive status epilepticus according to the guideline. Thirty-two protocols (97.0%) included intramuscular midazolam, 2 (6.1%) included IV lorazepam, and 5 (15.2%) included IV diazepam.
Although the protocols “appropriately emphasized” intramuscular midazolam, the protocol doses often were lower than those used in the trials or recommended in the guideline. In addition, most protocols listed IV and intraosseous midazolam as options, although these treatments were not studied in the trials nor recommended in the guideline. In all, six of the protocols (18.2%) recommended at least one medication by the route and dose suggested in the trials or in the guideline.
“Why EMS system protocols deviate from the evidence and how this affects patient outcomes deserves further study,” the authors said.
The researchers noted that they examined EMS protocols in only one state and that “protocols may not necessarily reflect what emergency medical technicians actually do in practice.” In addition, the researchers accessed the most recent protocols by consulting EMS system websites rather than by contacting each EMS system for its most up-to-date protocol.
The authors reported personal compensation from JAMA Neurology and from Continuum Audio unrelated to the present study, as well as grants from the National Institutes of Health.
SOURCE: Betjemann JP et al. JAMA. 2019 Mar 26.
“Many protocols did not follow evidence-based guidelines and did not accurately define generalized convulsive status epilepticus,” said John P. Betjemann, MD, associate professor of neurology at the University of California, San Francisco, and his colleagues. They reported their findings in the March 26 issue of JAMA.
Generalized convulsive status epilepticus is a neurologic emergency, and trials published in 2001 and 2012 found that benzodiazepines are effective prehospital treatments for patients with generalized convulsive status epilepticus. These trials informed a 2016 evidence-based guideline that cites level A evidence for intramuscular midazolam, IV lorazepam, and IV diazepam as initial treatment options for adults.
To determine whether EMS system protocols follow these recommendations, the investigators reviewed treatment protocols from 33 EMS systems that cover the 58 counties in California. The researchers reviewed EMS system protocols between May and June 2018 to determine when they were last updated and whether they defined generalized convulsive status epilepticus according to the guideline (namely, 5 or more minutes of continuous seizure or two or more discrete seizures between which a patient has incomplete recovery of consciousness). They also determined whether the protocols included any of the three benzodiazepines in the guideline and, if so, at what dose and using which route of administration.
Protocols’ most recent revision dates ranged between 2007 and 2018. Twenty-seven protocols (81.8%) were revised after the second clinical trial was published in 2012, and 17 (51.5%) were revised after the 2016 guideline. Seven EMS system protocols (21.2%) defined generalized convulsive status epilepticus according to the guideline. Thirty-two protocols (97.0%) included intramuscular midazolam, 2 (6.1%) included IV lorazepam, and 5 (15.2%) included IV diazepam.
Although the protocols “appropriately emphasized” intramuscular midazolam, the protocol doses often were lower than those used in the trials or recommended in the guideline. In addition, most protocols listed IV and intraosseous midazolam as options, although these treatments were not studied in the trials nor recommended in the guideline. In all, six of the protocols (18.2%) recommended at least one medication by the route and dose suggested in the trials or in the guideline.
“Why EMS system protocols deviate from the evidence and how this affects patient outcomes deserves further study,” the authors said.
The researchers noted that they examined EMS protocols in only one state and that “protocols may not necessarily reflect what emergency medical technicians actually do in practice.” In addition, the researchers accessed the most recent protocols by consulting EMS system websites rather than by contacting each EMS system for its most up-to-date protocol.
The authors reported personal compensation from JAMA Neurology and from Continuum Audio unrelated to the present study, as well as grants from the National Institutes of Health.
SOURCE: Betjemann JP et al. JAMA. 2019 Mar 26.
FROM JAMA
Key clinical point: Many emergency medical services (EMS) system protocols may not follow evidence-based guidelines or accurately define generalized convulsive status epilepticus.
Major finding: In all, 18.2% of the protocols recommended at least one medication by the route and at the dose suggested in clinical trials or in an evidence-based guideline.
Study details: A review of treatment protocols from 33 EMS systems that cover the 58 counties in California.
Disclosures: The authors reported personal compensation from JAMA Neurology and Continuum Audio unrelated to the present study and grants from the National Institutes of Health.
Source: Betjemann JP et al. JAMA. 2019 March 26.
‘Trigger zone’ resection ups seizure-free odds in temporal lobe epilepsy
Resection of a brain area implicated in seizure modulation improves the odds of being seizure free in patients with temporal lobe epilepsy, according to results of a recent multicenter analysis.
Patients with long-term postoperative freedom from seizures had a larger proportion of the piriform cortex resected versus patients who were not seizure free. Removing at least half the piriform cortex was associated with a 1500% increase in odds of seizure freedom, first author Marian Galovic, MD, of the department of clinical and experimental epilepsy at the University College London’s Queen Square Institute of Neurology and his colleagues reported in JAMA Neurology.
“If confirmed in prospective interventional trials, these findings will have practical implications for guiding neurosurgeons about the extent of the surgical resection,” Dr. Galovic and his coinvestigators wrote.
The area tempestas in the piriform cortex has been identified as an epileptic trigger zone in animal studies, but to date, evidence of a human epileptic trigger zone in this area remain limited, according to the investigators.
To evaluate the impact of resection in this area, Dr. Galovic and his colleagues evaluated 107 patients with temporal lobe epilepsy from an ongoing, single-center, prospective study, and validated their findings with 31 patients from two other independent cohorts.
Of the 107 patients in the main cohort, 46% were completely seizure free for a median of 5 years after epilepsy surgery, with results of voxel-based morphometry showing that those patients had a more pronounced loss of gray matter in the ipsilateral piriform, compared with non–seizure-free patients.
The seizure-free patients had a median of 83% of the piriform cortex resected, compared with 52% for the non–seizure-free patients (P less than .001), results of a volumetric analysis confirmed.
Anxiety or psychosis outcomes were not influenced by the extent of piriform cortex resection, the investigators wrote, adding that poor verbal memory outcome was linked to the extent of resection of other brain regions, but not the piriform cortex.
The investigators confirmed these findings in the 31 patients of the validation cohort, with significant associations between extent of piriform cortex resection and postsurgical outcomes.
Resecting at least half of the region increased odds of being seizure free by a factor of 16 (95% CI, 5-47; P less than .001), Dr. Galovic and his colleagues added.
“Our results provide evidence suggesting that the human piriform cortex has a role in the generation of seizures that involve the temporal lobe,” they wrote in a discussion of their results.
The findings, if confirmed, could have implications not only for surgical practice, they wrote, but also for the understanding of the mechanisms underlying epileptic networks, which could lead to new drug and nondrug interventions to mitigate seizure activity.
Dr. Galovic reported receiving a grant from the Medical Research Council. His coauthors reported disclosures with the Medical Research Council, Wellcome Trust, Medtronic, Neuropace, Nevro, Eisai, UCB, and Mallinckrodt, among other entities.
SOURCE: Galovic M et al. JAMA Neurol. 2019 Mar 11. doi: 10.1001/jamaneurol.2019.0204.
Resection of a brain area implicated in seizure modulation improves the odds of being seizure free in patients with temporal lobe epilepsy, according to results of a recent multicenter analysis.
Patients with long-term postoperative freedom from seizures had a larger proportion of the piriform cortex resected versus patients who were not seizure free. Removing at least half the piriform cortex was associated with a 1500% increase in odds of seizure freedom, first author Marian Galovic, MD, of the department of clinical and experimental epilepsy at the University College London’s Queen Square Institute of Neurology and his colleagues reported in JAMA Neurology.
“If confirmed in prospective interventional trials, these findings will have practical implications for guiding neurosurgeons about the extent of the surgical resection,” Dr. Galovic and his coinvestigators wrote.
The area tempestas in the piriform cortex has been identified as an epileptic trigger zone in animal studies, but to date, evidence of a human epileptic trigger zone in this area remain limited, according to the investigators.
To evaluate the impact of resection in this area, Dr. Galovic and his colleagues evaluated 107 patients with temporal lobe epilepsy from an ongoing, single-center, prospective study, and validated their findings with 31 patients from two other independent cohorts.
Of the 107 patients in the main cohort, 46% were completely seizure free for a median of 5 years after epilepsy surgery, with results of voxel-based morphometry showing that those patients had a more pronounced loss of gray matter in the ipsilateral piriform, compared with non–seizure-free patients.
The seizure-free patients had a median of 83% of the piriform cortex resected, compared with 52% for the non–seizure-free patients (P less than .001), results of a volumetric analysis confirmed.
Anxiety or psychosis outcomes were not influenced by the extent of piriform cortex resection, the investigators wrote, adding that poor verbal memory outcome was linked to the extent of resection of other brain regions, but not the piriform cortex.
The investigators confirmed these findings in the 31 patients of the validation cohort, with significant associations between extent of piriform cortex resection and postsurgical outcomes.
Resecting at least half of the region increased odds of being seizure free by a factor of 16 (95% CI, 5-47; P less than .001), Dr. Galovic and his colleagues added.
“Our results provide evidence suggesting that the human piriform cortex has a role in the generation of seizures that involve the temporal lobe,” they wrote in a discussion of their results.
The findings, if confirmed, could have implications not only for surgical practice, they wrote, but also for the understanding of the mechanisms underlying epileptic networks, which could lead to new drug and nondrug interventions to mitigate seizure activity.
Dr. Galovic reported receiving a grant from the Medical Research Council. His coauthors reported disclosures with the Medical Research Council, Wellcome Trust, Medtronic, Neuropace, Nevro, Eisai, UCB, and Mallinckrodt, among other entities.
SOURCE: Galovic M et al. JAMA Neurol. 2019 Mar 11. doi: 10.1001/jamaneurol.2019.0204.
Resection of a brain area implicated in seizure modulation improves the odds of being seizure free in patients with temporal lobe epilepsy, according to results of a recent multicenter analysis.
Patients with long-term postoperative freedom from seizures had a larger proportion of the piriform cortex resected versus patients who were not seizure free. Removing at least half the piriform cortex was associated with a 1500% increase in odds of seizure freedom, first author Marian Galovic, MD, of the department of clinical and experimental epilepsy at the University College London’s Queen Square Institute of Neurology and his colleagues reported in JAMA Neurology.
“If confirmed in prospective interventional trials, these findings will have practical implications for guiding neurosurgeons about the extent of the surgical resection,” Dr. Galovic and his coinvestigators wrote.
The area tempestas in the piriform cortex has been identified as an epileptic trigger zone in animal studies, but to date, evidence of a human epileptic trigger zone in this area remain limited, according to the investigators.
To evaluate the impact of resection in this area, Dr. Galovic and his colleagues evaluated 107 patients with temporal lobe epilepsy from an ongoing, single-center, prospective study, and validated their findings with 31 patients from two other independent cohorts.
Of the 107 patients in the main cohort, 46% were completely seizure free for a median of 5 years after epilepsy surgery, with results of voxel-based morphometry showing that those patients had a more pronounced loss of gray matter in the ipsilateral piriform, compared with non–seizure-free patients.
The seizure-free patients had a median of 83% of the piriform cortex resected, compared with 52% for the non–seizure-free patients (P less than .001), results of a volumetric analysis confirmed.
Anxiety or psychosis outcomes were not influenced by the extent of piriform cortex resection, the investigators wrote, adding that poor verbal memory outcome was linked to the extent of resection of other brain regions, but not the piriform cortex.
The investigators confirmed these findings in the 31 patients of the validation cohort, with significant associations between extent of piriform cortex resection and postsurgical outcomes.
Resecting at least half of the region increased odds of being seizure free by a factor of 16 (95% CI, 5-47; P less than .001), Dr. Galovic and his colleagues added.
“Our results provide evidence suggesting that the human piriform cortex has a role in the generation of seizures that involve the temporal lobe,” they wrote in a discussion of their results.
The findings, if confirmed, could have implications not only for surgical practice, they wrote, but also for the understanding of the mechanisms underlying epileptic networks, which could lead to new drug and nondrug interventions to mitigate seizure activity.
Dr. Galovic reported receiving a grant from the Medical Research Council. His coauthors reported disclosures with the Medical Research Council, Wellcome Trust, Medtronic, Neuropace, Nevro, Eisai, UCB, and Mallinckrodt, among other entities.
SOURCE: Galovic M et al. JAMA Neurol. 2019 Mar 11. doi: 10.1001/jamaneurol.2019.0204.
FROM JAMA NEUROLOGY
Better epilepsy outcomes with stereoelectroencephalography versus subdural electrode
Robotic stereoelectroencephalography for the localization of seizures in epilepsy is associated with less procedural morbidity, such as infection and hemorrhage, and better outcomes, compared with subdural electrode implantation.
A paper published in JAMA Neurology detailed the results of a retrospective cohort study of the outcomes of 239 patients with medically intractable epilepsy, 121 of whom underwent stereoelectroencephalography (SEEG) and 139 underwent subdural electrode (SDE) implantation.
The authors noted a significant difference between the two groups in complication rates. There were seven symptomatic hemorrhagic sequelae and three infections related to SDE implantation, and in one of these cases the patient suffered long-term neurologic consequences.
In contrast, there were no symptomatic complications in the SEEG cohort, although two patients were found to have small asymptomatic subdural hematomas that were spotted on CT scans.
Patients in the implantation group also received significantly more narcotics and had a much higher rate of perioperative blood transfusions (13.7% vs. 0.8%, P less than .001), compared with those in the SEEG group.
The study also looked at epilepsy outcomes in the two groups. Significantly more of the patients who had subdural electrodes underwent resection or ablative surgery with laser interstitial thermal therapy, compared with the patients who had SEEG (91.4% vs. 74.4%, P less than .001).
“Thus, the SEEG and SDE cohorts were significantly different in the proportions of cases that were lesional, suggesting that these modalities were used to evaluate somewhat different populations, although the same group of physicians at the same center managed and referred these cases,” wrote Nitin Tandon, MD, from the University of Texas, Houston, and his coauthors. “However, this shift in the patient pool would be expected to bias outcomes against SEEG, because these patients generally have less favorable outcomes.”
Yet the authors saw that a significantly greater proportion of the SEEG patients were free of disabling seizures, compared with the SDE implant group at 6 months (83.9% vs. 66.1%) and 1 year (76% vs. 54.6%) after resection.
To account for the difference between the two groups in the proportion of cases that were lesional, the authors conducted a subgroup analysis of patients with abnormalities on imaging. Again, they saw that a significantly greater proportion of the SEEG patients achieved good outcomes at 6 months and 1 year, compared with the electrode group.
While subdural electrodes have long been the standard approach for delineating epileptogenic zones, the authors wrote that SEEG offers improved coverage and precise targeting of deeper structures. “In addition, the ability of the SEEG method to map distributed epileptic networks involved in epileptic activity has been hypothesized to be responsible for improved outcomes in patients with epilepsy that is difficult to localize.”
They also commented that, in their institution, they saw much greater patient tolerance for SEEG and slightly better outcomes in those patients who underwent resection or ablation.
One author reported a position with a company specializing in outpatient clinical neurophysiological testing services. No other conflicts of interest were reported.
SOURCE: Tandon N et al. JAMA Neurol. 2019 Mar 4. doi: 10.1001/jamaneurol.2019.0098.
Robotic stereoelectroencephalography for the localization of seizures in epilepsy is associated with less procedural morbidity, such as infection and hemorrhage, and better outcomes, compared with subdural electrode implantation.
A paper published in JAMA Neurology detailed the results of a retrospective cohort study of the outcomes of 239 patients with medically intractable epilepsy, 121 of whom underwent stereoelectroencephalography (SEEG) and 139 underwent subdural electrode (SDE) implantation.
The authors noted a significant difference between the two groups in complication rates. There were seven symptomatic hemorrhagic sequelae and three infections related to SDE implantation, and in one of these cases the patient suffered long-term neurologic consequences.
In contrast, there were no symptomatic complications in the SEEG cohort, although two patients were found to have small asymptomatic subdural hematomas that were spotted on CT scans.
Patients in the implantation group also received significantly more narcotics and had a much higher rate of perioperative blood transfusions (13.7% vs. 0.8%, P less than .001), compared with those in the SEEG group.
The study also looked at epilepsy outcomes in the two groups. Significantly more of the patients who had subdural electrodes underwent resection or ablative surgery with laser interstitial thermal therapy, compared with the patients who had SEEG (91.4% vs. 74.4%, P less than .001).
“Thus, the SEEG and SDE cohorts were significantly different in the proportions of cases that were lesional, suggesting that these modalities were used to evaluate somewhat different populations, although the same group of physicians at the same center managed and referred these cases,” wrote Nitin Tandon, MD, from the University of Texas, Houston, and his coauthors. “However, this shift in the patient pool would be expected to bias outcomes against SEEG, because these patients generally have less favorable outcomes.”
Yet the authors saw that a significantly greater proportion of the SEEG patients were free of disabling seizures, compared with the SDE implant group at 6 months (83.9% vs. 66.1%) and 1 year (76% vs. 54.6%) after resection.
To account for the difference between the two groups in the proportion of cases that were lesional, the authors conducted a subgroup analysis of patients with abnormalities on imaging. Again, they saw that a significantly greater proportion of the SEEG patients achieved good outcomes at 6 months and 1 year, compared with the electrode group.
While subdural electrodes have long been the standard approach for delineating epileptogenic zones, the authors wrote that SEEG offers improved coverage and precise targeting of deeper structures. “In addition, the ability of the SEEG method to map distributed epileptic networks involved in epileptic activity has been hypothesized to be responsible for improved outcomes in patients with epilepsy that is difficult to localize.”
They also commented that, in their institution, they saw much greater patient tolerance for SEEG and slightly better outcomes in those patients who underwent resection or ablation.
One author reported a position with a company specializing in outpatient clinical neurophysiological testing services. No other conflicts of interest were reported.
SOURCE: Tandon N et al. JAMA Neurol. 2019 Mar 4. doi: 10.1001/jamaneurol.2019.0098.
Robotic stereoelectroencephalography for the localization of seizures in epilepsy is associated with less procedural morbidity, such as infection and hemorrhage, and better outcomes, compared with subdural electrode implantation.
A paper published in JAMA Neurology detailed the results of a retrospective cohort study of the outcomes of 239 patients with medically intractable epilepsy, 121 of whom underwent stereoelectroencephalography (SEEG) and 139 underwent subdural electrode (SDE) implantation.
The authors noted a significant difference between the two groups in complication rates. There were seven symptomatic hemorrhagic sequelae and three infections related to SDE implantation, and in one of these cases the patient suffered long-term neurologic consequences.
In contrast, there were no symptomatic complications in the SEEG cohort, although two patients were found to have small asymptomatic subdural hematomas that were spotted on CT scans.
Patients in the implantation group also received significantly more narcotics and had a much higher rate of perioperative blood transfusions (13.7% vs. 0.8%, P less than .001), compared with those in the SEEG group.
The study also looked at epilepsy outcomes in the two groups. Significantly more of the patients who had subdural electrodes underwent resection or ablative surgery with laser interstitial thermal therapy, compared with the patients who had SEEG (91.4% vs. 74.4%, P less than .001).
“Thus, the SEEG and SDE cohorts were significantly different in the proportions of cases that were lesional, suggesting that these modalities were used to evaluate somewhat different populations, although the same group of physicians at the same center managed and referred these cases,” wrote Nitin Tandon, MD, from the University of Texas, Houston, and his coauthors. “However, this shift in the patient pool would be expected to bias outcomes against SEEG, because these patients generally have less favorable outcomes.”
Yet the authors saw that a significantly greater proportion of the SEEG patients were free of disabling seizures, compared with the SDE implant group at 6 months (83.9% vs. 66.1%) and 1 year (76% vs. 54.6%) after resection.
To account for the difference between the two groups in the proportion of cases that were lesional, the authors conducted a subgroup analysis of patients with abnormalities on imaging. Again, they saw that a significantly greater proportion of the SEEG patients achieved good outcomes at 6 months and 1 year, compared with the electrode group.
While subdural electrodes have long been the standard approach for delineating epileptogenic zones, the authors wrote that SEEG offers improved coverage and precise targeting of deeper structures. “In addition, the ability of the SEEG method to map distributed epileptic networks involved in epileptic activity has been hypothesized to be responsible for improved outcomes in patients with epilepsy that is difficult to localize.”
They also commented that, in their institution, they saw much greater patient tolerance for SEEG and slightly better outcomes in those patients who underwent resection or ablation.
One author reported a position with a company specializing in outpatient clinical neurophysiological testing services. No other conflicts of interest were reported.
SOURCE: Tandon N et al. JAMA Neurol. 2019 Mar 4. doi: 10.1001/jamaneurol.2019.0098.
FROM JAMA NEUROLOGY
Key clinical point: Stereoelectroencephalography in epilepsy associated with fewer complications than subdural electrode implantation
Major finding: Subdural electrode implantation is associated with significantly more hemorrhagic complications and infections than stereoelectroencephalography.
Study details: A retrospective cohort study in 239 patients with medically intractable epilepsy.
Disclosures: One author reported a position with a company specializing in outpatient clinical neurophysiological testing services. No other conflicts of interest were reported.
Source: Tandon N et al. JAMA Neurol. 2019 Mar 4. doi: 10.1001/jamaneurol.2019.0098.
When to suspect a severe skin reaction to an AED
NEW ORLEANS – Most skin eruptions in patients taking antiepileptic drugs (AEDs) are relatively benign. With close supervision, some patients with epilepsy may continue treatment despite having a benign drug rash, according to a lecture at the annual meeting of the American Epilepsy Society.
“When do you know that you’re not dealing with that kind of eruption?” said Jeanne M. Young, MD, assistant professor of dermatology at the University of Virginia in Charlottesville.
Signs and symptoms that raise concerns about severe cutaneous reactions include swelling of the face; lesions that are fluid-filled, dusky, or painful; mucus membrane involvement; and signs of systemic involvement.
Associations with anticonvulsants
Diffuse swelling of the face is a hallmark symptom of DRESS. Fluid-filled lesions such as pustules, vesicles, and bullae indicate a condition other than a benign drug eruption. Signs of systemic involvement may include fever, marked eosinophilia, transaminitis, and evidence of lymphocyte activation. “In general, I want to see systemic involvement that can’t be explained by the patient’s other systemic diseases,” Dr. Young said.
A 2018 study found that AEDs are associated with SJS and TEN, and the labels for lamotrigine and carbamazepine include black box warnings about the risk of severe cutaneous adverse events. Carbamazepine’s warning, which was added in 2007, notes that SJS and TEN are significantly more common in patients of Asian ancestry with the human leukocyte antigen allele HLA-B*1502 and that physicians should screen at-risk patients before starting treatment.
Benign drug rashes
Morbilliform drug eruptions, sometimes called benign exanthems, are “by far the most common drug rash that we see” and typically are “the rashes that people refer to as drug rashes,” Dr. Young said. The mechanisms appear to be primarily immune complex mediated and cell mediated. “When the drug is stopped, these rashes tend to go away quite predictably in 2-3 weeks.”
For any class of drug, about 1% of people taking that medication may have this type of reaction, Dr. Young said. “We expect to see erythematous papules and plaques that oftentimes become confluent on the skin.” These reactions generally occur 7-10 days after the first exposure to the medication, and most patients do not have other symptoms, although the rash may itch. In addition, patients may have erythroderma with desquamation. “I think it’s important to point out the difference between desquamation, which is loss of the stratum corneum, and epidermal sloughing, which is what you see in something like [SJS] or TEN, where you’re actually losing the entire epidermis,” Dr. Young said. Recovering from desquamation is “sort of like recovering from a sun burn, and it’s not particularly dangerous.” Management of morbilliform drug eruptions is largely symptomatic.
Treat through, taper, or rechallenge
In the case a benign drug rash, “if you feel like you … need to keep a patient on a drug, you do have that option with close supervision,” Dr. Young said. “Communicate that with the dermatologist. Say, ‘I have really struggled getting this patient stabilized. Can we keep them on this drug?’ ”
The dermatologist may not fully realize the implications of stopping an effective AED in a patient with seizures that have been difficult to control. If the drug rash is benign, treating through may be an option. Patients often resolve the rash while continuing the medication, which may be because of desensitization, Dr. Young said. If a patient’s symptoms are too great to continue the drug, neurologists have the option of slowly tapering the drug and reinitiating with a new drug, Dr. Young said. Neurologists also may choose to rechallenge.
If a patient is on several medications, making it difficult to elucidate a causative agent, after stopping those drugs and allowing the rash to resolve, “there is little danger in restarting a medication,” she said.
Benign rash or DRESS?
“When I see a morbilliform eruption, usually what’s on my mind is, ‘Is this just a drug rash or is this DRESS?’ ” Dr. Young said. DRESS often starts with a morbilliform eruption that is indistinguishable from a benign drug eruption.
“Timing is a major difference,” she said. “If a patient develops a morbilliform drug eruption much later than I would expect, then my suspicion [for DRESS] goes up.” Patients with DRESS often have fever and systemic symptoms. Proposed DRESS diagnostic criteria can be useful, but clinical judgment still plays a key role. If a patient does not satisfy diagnostic criteria but has some signs and is taking a drug that is associated with DRESS, “it is going to make me more suspicious and maybe make me recommend stopping that drug sooner,” she said. Anticonvulsants such as carbamazepine, lamotrigine, and phenobarbital are among the drugs most commonly associated with DRESS.
Toxic erythemas
Patients may present with toxic erythemas, such as fixed drug reactions, erythema multiforme, SJS, and TEN. These drug reactions appear similar on biopsy but have different courses.
A patient with a fixed drug reaction often has a single lesion, and the lesion will occur in the same location every time the patient is exposed to the drug. Patients may develop additional lesions with subsequent exposures. These lesions typically are large, erythematous, well-demarcated plaques with central duskiness. “They can be bullous in the center, and they typically will heal with pigmentation, which is unique to this particular drug reaction,” said Dr. Young. “When it gets more concerning and most important to differentiate is when you get generalized bullous fixed drug eruption.” Generalized bullous fixed drug eruptions mimic and are difficult to clinically distinguish from TEN, which has a much has a much poorer prognosis.
Patients with a fixed drug eruption are not as ill as patients with TEN and tend not to slough their skin to the extent seen with TEN. Interferon gamma, perforin, and Fas ligand have been implicated as mechanisms involved in fixed drug reactions. Unlike in TEN, regulatory T cells are abundant, which may explain why TEN and fixed drug reactions progress differently even though they appear to share pathologic mechanisms, Dr. Young said.
Erythema multiforme generally presents with classic target lesions and little mucosal involvement. Infections, most commonly herpes simplex virus (HSV) 1 and 2, may trigger erythema multiforme. Dr. Young recommends evaluating patients for HSV and checking serologies, even if patients have never had a herpes outbreak. “If you have no evidence for infection, you do have to consider discontinuing a medication,” she said.
Stevens–Johnson syndrome and TEN
SJS and TEN are “the rarest of the severe cutaneous adverse drug reactions” and have “the highest morbidity and mortality,” Dr. Young said. They appear to exist on a continuum where SJS may represent early TEN.
“This is a situation where you expect to see blistering of the skin [and] always mucosal involvement. You need to stop the drug immediately when you suspect this drug reaction,” Dr. Young said.
One reason to distinguish SJS or early TEN from later TEN is that high-dose steroids may play a role in the treatment of SJS or early TEN. “Once you get past about 10% total body surface area, there is good evidence that steroids actually increase morbidity and mortality,” she said.
If the eruption has occurred before, that factor suggests that a diagnosis of erythema multiforme or fixed drug reaction may be more likely than TEN.
An apparent lack of regulatory T cells in TEN could explain why patients with HIV infection are at much higher risk of developing SJS and TEN. Understanding the role that regulatory T cells play in severe drug eruptions may lead to new therapeutic options in the future, Dr. Young said.
Dr. Young had no disclosures.
NEW ORLEANS – Most skin eruptions in patients taking antiepileptic drugs (AEDs) are relatively benign. With close supervision, some patients with epilepsy may continue treatment despite having a benign drug rash, according to a lecture at the annual meeting of the American Epilepsy Society.
“When do you know that you’re not dealing with that kind of eruption?” said Jeanne M. Young, MD, assistant professor of dermatology at the University of Virginia in Charlottesville.
Signs and symptoms that raise concerns about severe cutaneous reactions include swelling of the face; lesions that are fluid-filled, dusky, or painful; mucus membrane involvement; and signs of systemic involvement.
Associations with anticonvulsants
Diffuse swelling of the face is a hallmark symptom of DRESS. Fluid-filled lesions such as pustules, vesicles, and bullae indicate a condition other than a benign drug eruption. Signs of systemic involvement may include fever, marked eosinophilia, transaminitis, and evidence of lymphocyte activation. “In general, I want to see systemic involvement that can’t be explained by the patient’s other systemic diseases,” Dr. Young said.
A 2018 study found that AEDs are associated with SJS and TEN, and the labels for lamotrigine and carbamazepine include black box warnings about the risk of severe cutaneous adverse events. Carbamazepine’s warning, which was added in 2007, notes that SJS and TEN are significantly more common in patients of Asian ancestry with the human leukocyte antigen allele HLA-B*1502 and that physicians should screen at-risk patients before starting treatment.
Benign drug rashes
Morbilliform drug eruptions, sometimes called benign exanthems, are “by far the most common drug rash that we see” and typically are “the rashes that people refer to as drug rashes,” Dr. Young said. The mechanisms appear to be primarily immune complex mediated and cell mediated. “When the drug is stopped, these rashes tend to go away quite predictably in 2-3 weeks.”
For any class of drug, about 1% of people taking that medication may have this type of reaction, Dr. Young said. “We expect to see erythematous papules and plaques that oftentimes become confluent on the skin.” These reactions generally occur 7-10 days after the first exposure to the medication, and most patients do not have other symptoms, although the rash may itch. In addition, patients may have erythroderma with desquamation. “I think it’s important to point out the difference between desquamation, which is loss of the stratum corneum, and epidermal sloughing, which is what you see in something like [SJS] or TEN, where you’re actually losing the entire epidermis,” Dr. Young said. Recovering from desquamation is “sort of like recovering from a sun burn, and it’s not particularly dangerous.” Management of morbilliform drug eruptions is largely symptomatic.
Treat through, taper, or rechallenge
In the case a benign drug rash, “if you feel like you … need to keep a patient on a drug, you do have that option with close supervision,” Dr. Young said. “Communicate that with the dermatologist. Say, ‘I have really struggled getting this patient stabilized. Can we keep them on this drug?’ ”
The dermatologist may not fully realize the implications of stopping an effective AED in a patient with seizures that have been difficult to control. If the drug rash is benign, treating through may be an option. Patients often resolve the rash while continuing the medication, which may be because of desensitization, Dr. Young said. If a patient’s symptoms are too great to continue the drug, neurologists have the option of slowly tapering the drug and reinitiating with a new drug, Dr. Young said. Neurologists also may choose to rechallenge.
If a patient is on several medications, making it difficult to elucidate a causative agent, after stopping those drugs and allowing the rash to resolve, “there is little danger in restarting a medication,” she said.
Benign rash or DRESS?
“When I see a morbilliform eruption, usually what’s on my mind is, ‘Is this just a drug rash or is this DRESS?’ ” Dr. Young said. DRESS often starts with a morbilliform eruption that is indistinguishable from a benign drug eruption.
“Timing is a major difference,” she said. “If a patient develops a morbilliform drug eruption much later than I would expect, then my suspicion [for DRESS] goes up.” Patients with DRESS often have fever and systemic symptoms. Proposed DRESS diagnostic criteria can be useful, but clinical judgment still plays a key role. If a patient does not satisfy diagnostic criteria but has some signs and is taking a drug that is associated with DRESS, “it is going to make me more suspicious and maybe make me recommend stopping that drug sooner,” she said. Anticonvulsants such as carbamazepine, lamotrigine, and phenobarbital are among the drugs most commonly associated with DRESS.
Toxic erythemas
Patients may present with toxic erythemas, such as fixed drug reactions, erythema multiforme, SJS, and TEN. These drug reactions appear similar on biopsy but have different courses.
A patient with a fixed drug reaction often has a single lesion, and the lesion will occur in the same location every time the patient is exposed to the drug. Patients may develop additional lesions with subsequent exposures. These lesions typically are large, erythematous, well-demarcated plaques with central duskiness. “They can be bullous in the center, and they typically will heal with pigmentation, which is unique to this particular drug reaction,” said Dr. Young. “When it gets more concerning and most important to differentiate is when you get generalized bullous fixed drug eruption.” Generalized bullous fixed drug eruptions mimic and are difficult to clinically distinguish from TEN, which has a much has a much poorer prognosis.
Patients with a fixed drug eruption are not as ill as patients with TEN and tend not to slough their skin to the extent seen with TEN. Interferon gamma, perforin, and Fas ligand have been implicated as mechanisms involved in fixed drug reactions. Unlike in TEN, regulatory T cells are abundant, which may explain why TEN and fixed drug reactions progress differently even though they appear to share pathologic mechanisms, Dr. Young said.
Erythema multiforme generally presents with classic target lesions and little mucosal involvement. Infections, most commonly herpes simplex virus (HSV) 1 and 2, may trigger erythema multiforme. Dr. Young recommends evaluating patients for HSV and checking serologies, even if patients have never had a herpes outbreak. “If you have no evidence for infection, you do have to consider discontinuing a medication,” she said.
Stevens–Johnson syndrome and TEN
SJS and TEN are “the rarest of the severe cutaneous adverse drug reactions” and have “the highest morbidity and mortality,” Dr. Young said. They appear to exist on a continuum where SJS may represent early TEN.
“This is a situation where you expect to see blistering of the skin [and] always mucosal involvement. You need to stop the drug immediately when you suspect this drug reaction,” Dr. Young said.
One reason to distinguish SJS or early TEN from later TEN is that high-dose steroids may play a role in the treatment of SJS or early TEN. “Once you get past about 10% total body surface area, there is good evidence that steroids actually increase morbidity and mortality,” she said.
If the eruption has occurred before, that factor suggests that a diagnosis of erythema multiforme or fixed drug reaction may be more likely than TEN.
An apparent lack of regulatory T cells in TEN could explain why patients with HIV infection are at much higher risk of developing SJS and TEN. Understanding the role that regulatory T cells play in severe drug eruptions may lead to new therapeutic options in the future, Dr. Young said.
Dr. Young had no disclosures.
NEW ORLEANS – Most skin eruptions in patients taking antiepileptic drugs (AEDs) are relatively benign. With close supervision, some patients with epilepsy may continue treatment despite having a benign drug rash, according to a lecture at the annual meeting of the American Epilepsy Society.
“When do you know that you’re not dealing with that kind of eruption?” said Jeanne M. Young, MD, assistant professor of dermatology at the University of Virginia in Charlottesville.
Signs and symptoms that raise concerns about severe cutaneous reactions include swelling of the face; lesions that are fluid-filled, dusky, or painful; mucus membrane involvement; and signs of systemic involvement.
Associations with anticonvulsants
Diffuse swelling of the face is a hallmark symptom of DRESS. Fluid-filled lesions such as pustules, vesicles, and bullae indicate a condition other than a benign drug eruption. Signs of systemic involvement may include fever, marked eosinophilia, transaminitis, and evidence of lymphocyte activation. “In general, I want to see systemic involvement that can’t be explained by the patient’s other systemic diseases,” Dr. Young said.
A 2018 study found that AEDs are associated with SJS and TEN, and the labels for lamotrigine and carbamazepine include black box warnings about the risk of severe cutaneous adverse events. Carbamazepine’s warning, which was added in 2007, notes that SJS and TEN are significantly more common in patients of Asian ancestry with the human leukocyte antigen allele HLA-B*1502 and that physicians should screen at-risk patients before starting treatment.
Benign drug rashes
Morbilliform drug eruptions, sometimes called benign exanthems, are “by far the most common drug rash that we see” and typically are “the rashes that people refer to as drug rashes,” Dr. Young said. The mechanisms appear to be primarily immune complex mediated and cell mediated. “When the drug is stopped, these rashes tend to go away quite predictably in 2-3 weeks.”
For any class of drug, about 1% of people taking that medication may have this type of reaction, Dr. Young said. “We expect to see erythematous papules and plaques that oftentimes become confluent on the skin.” These reactions generally occur 7-10 days after the first exposure to the medication, and most patients do not have other symptoms, although the rash may itch. In addition, patients may have erythroderma with desquamation. “I think it’s important to point out the difference between desquamation, which is loss of the stratum corneum, and epidermal sloughing, which is what you see in something like [SJS] or TEN, where you’re actually losing the entire epidermis,” Dr. Young said. Recovering from desquamation is “sort of like recovering from a sun burn, and it’s not particularly dangerous.” Management of morbilliform drug eruptions is largely symptomatic.
Treat through, taper, or rechallenge
In the case a benign drug rash, “if you feel like you … need to keep a patient on a drug, you do have that option with close supervision,” Dr. Young said. “Communicate that with the dermatologist. Say, ‘I have really struggled getting this patient stabilized. Can we keep them on this drug?’ ”
The dermatologist may not fully realize the implications of stopping an effective AED in a patient with seizures that have been difficult to control. If the drug rash is benign, treating through may be an option. Patients often resolve the rash while continuing the medication, which may be because of desensitization, Dr. Young said. If a patient’s symptoms are too great to continue the drug, neurologists have the option of slowly tapering the drug and reinitiating with a new drug, Dr. Young said. Neurologists also may choose to rechallenge.
If a patient is on several medications, making it difficult to elucidate a causative agent, after stopping those drugs and allowing the rash to resolve, “there is little danger in restarting a medication,” she said.
Benign rash or DRESS?
“When I see a morbilliform eruption, usually what’s on my mind is, ‘Is this just a drug rash or is this DRESS?’ ” Dr. Young said. DRESS often starts with a morbilliform eruption that is indistinguishable from a benign drug eruption.
“Timing is a major difference,” she said. “If a patient develops a morbilliform drug eruption much later than I would expect, then my suspicion [for DRESS] goes up.” Patients with DRESS often have fever and systemic symptoms. Proposed DRESS diagnostic criteria can be useful, but clinical judgment still plays a key role. If a patient does not satisfy diagnostic criteria but has some signs and is taking a drug that is associated with DRESS, “it is going to make me more suspicious and maybe make me recommend stopping that drug sooner,” she said. Anticonvulsants such as carbamazepine, lamotrigine, and phenobarbital are among the drugs most commonly associated with DRESS.
Toxic erythemas
Patients may present with toxic erythemas, such as fixed drug reactions, erythema multiforme, SJS, and TEN. These drug reactions appear similar on biopsy but have different courses.
A patient with a fixed drug reaction often has a single lesion, and the lesion will occur in the same location every time the patient is exposed to the drug. Patients may develop additional lesions with subsequent exposures. These lesions typically are large, erythematous, well-demarcated plaques with central duskiness. “They can be bullous in the center, and they typically will heal with pigmentation, which is unique to this particular drug reaction,” said Dr. Young. “When it gets more concerning and most important to differentiate is when you get generalized bullous fixed drug eruption.” Generalized bullous fixed drug eruptions mimic and are difficult to clinically distinguish from TEN, which has a much has a much poorer prognosis.
Patients with a fixed drug eruption are not as ill as patients with TEN and tend not to slough their skin to the extent seen with TEN. Interferon gamma, perforin, and Fas ligand have been implicated as mechanisms involved in fixed drug reactions. Unlike in TEN, regulatory T cells are abundant, which may explain why TEN and fixed drug reactions progress differently even though they appear to share pathologic mechanisms, Dr. Young said.
Erythema multiforme generally presents with classic target lesions and little mucosal involvement. Infections, most commonly herpes simplex virus (HSV) 1 and 2, may trigger erythema multiforme. Dr. Young recommends evaluating patients for HSV and checking serologies, even if patients have never had a herpes outbreak. “If you have no evidence for infection, you do have to consider discontinuing a medication,” she said.
Stevens–Johnson syndrome and TEN
SJS and TEN are “the rarest of the severe cutaneous adverse drug reactions” and have “the highest morbidity and mortality,” Dr. Young said. They appear to exist on a continuum where SJS may represent early TEN.
“This is a situation where you expect to see blistering of the skin [and] always mucosal involvement. You need to stop the drug immediately when you suspect this drug reaction,” Dr. Young said.
One reason to distinguish SJS or early TEN from later TEN is that high-dose steroids may play a role in the treatment of SJS or early TEN. “Once you get past about 10% total body surface area, there is good evidence that steroids actually increase morbidity and mortality,” she said.
If the eruption has occurred before, that factor suggests that a diagnosis of erythema multiforme or fixed drug reaction may be more likely than TEN.
An apparent lack of regulatory T cells in TEN could explain why patients with HIV infection are at much higher risk of developing SJS and TEN. Understanding the role that regulatory T cells play in severe drug eruptions may lead to new therapeutic options in the future, Dr. Young said.
Dr. Young had no disclosures.
EXPERT ANALYSIS FROM AES 2018
Routine clinical data may predict psychiatric adverse effects from levetiracetam
Among patients with epilepsy, a simple model that incorporates factors such as a patient’s sex and history of depression, anxiety, and recreational drug use may help predict the risk of a psychiatric adverse effect from levetiracetam, according to a study published in JAMA Neurology.
“This study derived 2 simple models that predict the risk of a psychiatric adverse effect from levetiracetam” and can “guide prescription in clinical practice,” said Colin B. Josephson, MD, of the department of clinical neurosciences at the University of Calgary (Canada) and his research colleagues.
Levetiracetam is a commonly used first-line treatment for epilepsy because of its ease of use, broad spectrum of action, and safety profile, the researchers said. Still, psychiatric adverse reactions occur in as many as 16% of patients and frequently require treatment discontinuation.
To evaluate whether routine clinical data can predict which patients with epilepsy will experience a psychiatric adverse event from levetiracetam, the investigators analyzed data from The Health Improvement Network (THIN) database, which includes anonymized patient records from general practices in the United Kingdom. They assessed 21 variables for possible inclusion in prediction models. They identified these variables by searching the literature and weighing input from a panel of experts.
Their analysis included data from Jan. 1, 2000–May 31, 2012. Among the more than 11 million patients in THIN, the researchers identified 7,300 incident cases of epilepsy. The researchers examined when patients received a first prescription for levetiracetam and whether patients experienced a psychiatric symptom or disorder within 2 years of the prescription.
Among 1,173 patients with epilepsy receiving levetiracetam, the median age was 39 years; about half were women. In all, 14.1% experienced a psychiatric symptom or disorder within 2 years of prescription. Women were more likely to report a psychiatric symptom (odds ratio, 1.41), as were patients with a history of social deprivation (OR, 1.15), anxiety (OR, 1.74), recreational drug use (OR, 2.02), or depression (OR, 2.20).
The final model included female sex, history of depression, history of anxiety, and history of recreational drug use. Low socioeconomic status was not included because “it would be challenging to assign this score in clinic,” the authors said.
“There was a gradient in risk probabilities increasing from 8% for 0 risk factors to 11%-17% for 1, 17% to 31% for 2, 30%-42% for 3, and 49% when all risk factors were present,” Dr. Josephson and his colleagues indicated. “The discovered incremental probability of reporting a psychiatric sign can help generate an index of suspicion to counsel patients.”
Using the example of a woman patient with depression, the model “suggests she would be at risk,” with a 22% chance of a psychiatric adverse event in the 2 years after receiving a levetiracetam prescription.
The researchers created a second prediction algorithm based on data from patients without documentation of a mental health sign, symptom, or disorder prior to their levetiracetam prescription. This model incorporated age, sex, recreational drug use, and levetiracetam daily dose; it performed comparably well and might be used to determine safety of prescription, according to Dr. Josephson and his colleagues.
The authors noted that the study was limited by an inability to evaluate medication adherence and seizure type and frequency. One advantage of the study’s design is that it may have circumvented expectation bias because general practitioners were not prone to anticipating psychiatric adverse events or to have a lower threshold for diagnosing them.
The authors disclosed research fellowships and support from foundations and federal agencies.
SOURCE: Josephson CB et al. JAMA Neurol. 2019 Jan 28. doi: 10.1001/jamaneurol.2018.4561.
Among patients with epilepsy, a simple model that incorporates factors such as a patient’s sex and history of depression, anxiety, and recreational drug use may help predict the risk of a psychiatric adverse effect from levetiracetam, according to a study published in JAMA Neurology.
“This study derived 2 simple models that predict the risk of a psychiatric adverse effect from levetiracetam” and can “guide prescription in clinical practice,” said Colin B. Josephson, MD, of the department of clinical neurosciences at the University of Calgary (Canada) and his research colleagues.
Levetiracetam is a commonly used first-line treatment for epilepsy because of its ease of use, broad spectrum of action, and safety profile, the researchers said. Still, psychiatric adverse reactions occur in as many as 16% of patients and frequently require treatment discontinuation.
To evaluate whether routine clinical data can predict which patients with epilepsy will experience a psychiatric adverse event from levetiracetam, the investigators analyzed data from The Health Improvement Network (THIN) database, which includes anonymized patient records from general practices in the United Kingdom. They assessed 21 variables for possible inclusion in prediction models. They identified these variables by searching the literature and weighing input from a panel of experts.
Their analysis included data from Jan. 1, 2000–May 31, 2012. Among the more than 11 million patients in THIN, the researchers identified 7,300 incident cases of epilepsy. The researchers examined when patients received a first prescription for levetiracetam and whether patients experienced a psychiatric symptom or disorder within 2 years of the prescription.
Among 1,173 patients with epilepsy receiving levetiracetam, the median age was 39 years; about half were women. In all, 14.1% experienced a psychiatric symptom or disorder within 2 years of prescription. Women were more likely to report a psychiatric symptom (odds ratio, 1.41), as were patients with a history of social deprivation (OR, 1.15), anxiety (OR, 1.74), recreational drug use (OR, 2.02), or depression (OR, 2.20).
The final model included female sex, history of depression, history of anxiety, and history of recreational drug use. Low socioeconomic status was not included because “it would be challenging to assign this score in clinic,” the authors said.
“There was a gradient in risk probabilities increasing from 8% for 0 risk factors to 11%-17% for 1, 17% to 31% for 2, 30%-42% for 3, and 49% when all risk factors were present,” Dr. Josephson and his colleagues indicated. “The discovered incremental probability of reporting a psychiatric sign can help generate an index of suspicion to counsel patients.”
Using the example of a woman patient with depression, the model “suggests she would be at risk,” with a 22% chance of a psychiatric adverse event in the 2 years after receiving a levetiracetam prescription.
The researchers created a second prediction algorithm based on data from patients without documentation of a mental health sign, symptom, or disorder prior to their levetiracetam prescription. This model incorporated age, sex, recreational drug use, and levetiracetam daily dose; it performed comparably well and might be used to determine safety of prescription, according to Dr. Josephson and his colleagues.
The authors noted that the study was limited by an inability to evaluate medication adherence and seizure type and frequency. One advantage of the study’s design is that it may have circumvented expectation bias because general practitioners were not prone to anticipating psychiatric adverse events or to have a lower threshold for diagnosing them.
The authors disclosed research fellowships and support from foundations and federal agencies.
SOURCE: Josephson CB et al. JAMA Neurol. 2019 Jan 28. doi: 10.1001/jamaneurol.2018.4561.
Among patients with epilepsy, a simple model that incorporates factors such as a patient’s sex and history of depression, anxiety, and recreational drug use may help predict the risk of a psychiatric adverse effect from levetiracetam, according to a study published in JAMA Neurology.
“This study derived 2 simple models that predict the risk of a psychiatric adverse effect from levetiracetam” and can “guide prescription in clinical practice,” said Colin B. Josephson, MD, of the department of clinical neurosciences at the University of Calgary (Canada) and his research colleagues.
Levetiracetam is a commonly used first-line treatment for epilepsy because of its ease of use, broad spectrum of action, and safety profile, the researchers said. Still, psychiatric adverse reactions occur in as many as 16% of patients and frequently require treatment discontinuation.
To evaluate whether routine clinical data can predict which patients with epilepsy will experience a psychiatric adverse event from levetiracetam, the investigators analyzed data from The Health Improvement Network (THIN) database, which includes anonymized patient records from general practices in the United Kingdom. They assessed 21 variables for possible inclusion in prediction models. They identified these variables by searching the literature and weighing input from a panel of experts.
Their analysis included data from Jan. 1, 2000–May 31, 2012. Among the more than 11 million patients in THIN, the researchers identified 7,300 incident cases of epilepsy. The researchers examined when patients received a first prescription for levetiracetam and whether patients experienced a psychiatric symptom or disorder within 2 years of the prescription.
Among 1,173 patients with epilepsy receiving levetiracetam, the median age was 39 years; about half were women. In all, 14.1% experienced a psychiatric symptom or disorder within 2 years of prescription. Women were more likely to report a psychiatric symptom (odds ratio, 1.41), as were patients with a history of social deprivation (OR, 1.15), anxiety (OR, 1.74), recreational drug use (OR, 2.02), or depression (OR, 2.20).
The final model included female sex, history of depression, history of anxiety, and history of recreational drug use. Low socioeconomic status was not included because “it would be challenging to assign this score in clinic,” the authors said.
“There was a gradient in risk probabilities increasing from 8% for 0 risk factors to 11%-17% for 1, 17% to 31% for 2, 30%-42% for 3, and 49% when all risk factors were present,” Dr. Josephson and his colleagues indicated. “The discovered incremental probability of reporting a psychiatric sign can help generate an index of suspicion to counsel patients.”
Using the example of a woman patient with depression, the model “suggests she would be at risk,” with a 22% chance of a psychiatric adverse event in the 2 years after receiving a levetiracetam prescription.
The researchers created a second prediction algorithm based on data from patients without documentation of a mental health sign, symptom, or disorder prior to their levetiracetam prescription. This model incorporated age, sex, recreational drug use, and levetiracetam daily dose; it performed comparably well and might be used to determine safety of prescription, according to Dr. Josephson and his colleagues.
The authors noted that the study was limited by an inability to evaluate medication adherence and seizure type and frequency. One advantage of the study’s design is that it may have circumvented expectation bias because general practitioners were not prone to anticipating psychiatric adverse events or to have a lower threshold for diagnosing them.
The authors disclosed research fellowships and support from foundations and federal agencies.
SOURCE: Josephson CB et al. JAMA Neurol. 2019 Jan 28. doi: 10.1001/jamaneurol.2018.4561.
FROM JAMA NEUROLOGY
Key clinical point: Among patients with epilepsy, a simple model may help predict the risk of a psychiatric adverse effect from levetiracetam.
Major finding: The likelihood of a psychiatric adverse event increases from 8% for patients with no risk factors to 49% with all risk factors present.
Study details: A retrospective open cohort study of 1,173 patients with epilepsy receiving levetiracetam in the United Kingdom.
Disclosures: The authors disclosed research fellowships and support from foundations and federal agencies.
Source: Josephson CB et al. JAMA Neurol. 2019 Jan 28. doi: 10.1001/jamaneurol.2018.4561
How seizure prediction may benefit patients with epilepsy
NEW ORLEANS – For people with epilepsy, “the sudden and apparently unpredictable nature of seizures is one of the most disabling aspects of having the disorder,” said Michael Privitera, MD.
If a patient knew that “tomorrow will be a dangerous day” with a 50% chance of having a seizure, the patient could avoid hazardous activities, try to reduce stress, or increase supervision to reduce the risk of sudden, unexpected death in epilepsy, said Dr. Privitera, professor of neurology and director of the epilepsy center at the University of Cincinnati Gardner Neuroscience Institute. Physicians might be able to intervene during high-risk periods by altering antiepileptic drug regimens.
Evidence suggests that seizure prediction is possible today and that advances in wearable devices and analysis of chronic EEG recordings likely will improve the ability to predict seizures, Dr. Privitera said at the annual meeting of the American Epilepsy Society. Studies have found that some patients can predict the likelihood of seizures in the next 24 hours better than chance. In the future, algorithms that incorporate variables such as pulse, stress, mood, electrodermal activity, circadian rhythms, and EEG may further refine seizure prediction.
A complex picture
One problem with predicting seizures is that “you can have substantial changes in the seizure tendency, but not have a seizure,” Dr. Privitera said. Stress, alcohol, and missed medications, for example, may affect the seizure threshold. “They may be additive, and it may be when those things all hit at once that a seizure happens.”
Many patients report prodromal or premonitory symptoms before a seizure. “Most of us as clinicians will say, ‘Well, maybe you have some inkling, but I don’t think you’re really able to predict it,’ ” Dr. Privitera said.
Sheryl R. Haut, MD, professor of neurology at the Albert Einstein College of Medicine, New York, and her colleagues prospectively looked at patient self-prediction in 2007 (Neurology. 2007 Jan 23;68[4]:262-6). The investigators followed 74 people with epilepsy who completed a daily diary in which they predicted the likelihood of a seizure occurring in the next 24 hours. Their analysis included approximately 15,000 diary days and 1,400 seizure days.
A subset of participants, about 20%, was significantly better than chance at predicting when a seizure would happen. If a patient in this subgroup said that a seizure was extremely likely, then a seizure occurred approximately 37% of the time. If a patient predicted that a seizure was extremely unlikely, there was about a 10% chance of having a seizure.
“This was a pretty substantial difference,” Dr. Privitera said. Combining patients’ predictions with their self-reported stress levels seemed to yield the most accurate predictions.
Stress and the SMILE study
About 90% of people with epilepsy identify at least one seizure precipitant, and the most commonly cited trigger is stress. When Dr. Privitera and his colleagues surveyed patients in their clinic, 82% identified stress as a trigger (Epilepsy Behav. 2014 Dec;41:74-7). More than half of these patients had used some form of stress reduction, such as exercise, yoga, or meditation; 88% of those patients thought that stress reduction helped their seizures.
Underlying anxiety was the only difference between patients who thought that their seizures were triggered by stress and those who did not. Patients who did not think that stress triggered their seizures had significantly lower scores on the Generalized Anxiety Disorders–7.
Subsequently, Dr. Haut, Dr. Privitera, and colleagues conducted the Stress Management Intervention for Living with Epilepsy (SMILE) study, a prospective, controlled trial assessing the efficacy of a stress reduction intervention for reducing seizures, as well as measuring seizure self-prediction (Neurology. 2018 Mar 13;90[11]:e963-70). The researchers randomized patients to a progressive muscle relaxation intervention or to a control group; patients in the control group wrote down their activities for the day.
Patients posted diary entries twice daily into a smartphone, reporting stress levels and mood-related variables. As in Dr. Haut’s earlier study, patients predicted whether having a seizure was extremely unlikely, unlikely, neutral, likely, or extremely likely. Mood and stress variables (such as feeling unpleasant or pleasant, relaxed or stressed, and not worried or extremely worried) were ranked on a visual analog scale from 0 to 100.
The trial included participants who had at least two seizures per month and any seizure trigger. Medications were kept stable throughout the study. During a 2-month baseline, patients tracked their seizures and stress levels. During the 3-month treatment period, patients received the active or control intervention.
In all, 64 subjects completed the study, completing all diary entries on 94% of the days. In the active-treatment group, median seizure frequency decreased by 29%, compared with a 25% decrease in the control group. However, the difference between the groups was not statistically significant. Although the 25% reduction in the control group probably is partly attributable to the placebo effect, part of the decrease may be related to a mindfulness effect from completing the diary, Dr. Privitera said.
The active-treatment group had a statistically significant reduction in self-reported stress, compared with the control group, but this decrease did not correlate with seizure reduction. Changes in anxiety levels also did not correlate with seizures.
“It does not disprove the [stress] hypothesis, but it does tell us that there is more going on with stress and seizure triggers than just patients’ self-reported stress,” Dr. Privitera said.
Patients’ predictions
The seizure prediction findings in SMILE were similar to those of Dr. Haut’s earlier study. Among the 10 highest predictors out of the 64 participants, “when they said that a seizure was extremely likely, they were 8.36 times more likely to have a seizure than when they said a seizure was extremely unlikely,” Dr. Privitera said.
Many patients seemed to increase their predicted seizure probabilities in the days after having a seizure. In addition, feeling sad, nervous, worried, tense, or stressed significantly increased the likelihood that a patient would predict that a seizure was coming. However, these feelings were “not very accurate [for predicting] actual seizures,” he said. “Some people are better predictors, but really the basis of that prediction remains to be seen. One of my hypotheses is that some of these people may actually be responding to subclinical EEG changes.”
Together, these self-prediction studies include data from 4,500 seizures and 26,000 diary entries and show that “there is some information in patient self-report that can help us in understanding how to predict and when to predict seizures,” Dr. Privitera said.
Incorporating cardiac, EEG, and other variables
Various other factors may warrant inclusion in a seizure forecasting system. A new vagus nerve stimulation system responds to heart rate changes that occur at seizure onset. And for decades, researchers have studied the potential for EEG readings to predict seizures. A 2008 analysis of 47 reports concluded that limited progress had been made in predicting a seizure from interictal EEG (Epilepsy Behav. 2008 Jan;12[1]:128-35). Now, however, long-term intracranial recordings are providing new and important information about EEG patterns.
Whereas early studies examined EEG recordings from epilepsy monitoring units – when patients may have been sleep deprived, had medications removed, or recently undergone surgery – chronic intracranial recordings from devices such as the RNS (responsive neurostimulation) System have allowed researchers to look long term at EEG changes that are more representative of patients’ typical EEG patterns.
The RNS System detects interictal spikes and seizure discharges and then provides an electrical stimulation to stop seizures. “When you look at these recordings, there are a lot more electrographic seizures than clinical seizures that trigger these stimulations,” said Dr. Privitera. “If you look at somebody with a typical RNS, they may have 100 stimulations in a day and no clinical seizures. There are lots and lots of subclinical electrographic bursts – and not just spikes, but things that look like short electrographic seizures – that occur throughout the day.”
A handheld device
Researchers in Melbourne designed a system that uses implanted electrodes to provide chronic recordings (Lancet Neurol. 2013 Jun;12[6]:563-71). An algorithm then learned to predict the likelihood of a seizure from the patient’s data as the system recorded over time. The system could indicate when a seizure was likely by displaying a light on a handheld device. Patients were recorded for between 6 months and 3 years.
“There was a statistically significant ability to predict when seizures were happening,” Dr. Privitera said. “There is information in long-term intracranial recordings in many of these people that will help allow us to do a better prediction than what we are able to do right now, which is essentially not much.”
This research suggests that pooling data across patients may not be an effective seizure prediction strategy because different epilepsy types have different patterns. In addition, an individual’s patterns may differ from a group’s patterns. Complicating matters, individual patients may have multiple seizure types with different onset mechanisms.
“Another important lesson is that false positives in a deterministic sense may not represent false positives in a probabilistic sense,” Dr. Privitera said. “That is, when the seizure prediction program – whether it is the diary or the intracranial EEG or anything else – says the threshold changed, but you did not have a seizure, it does not mean that your prediction system was wrong. If the seizure tendency is going up … and your system says the seizure tendency went up, but all you are measuring is actual seizures, it looks like it is a false positive prediction of seizures. But in fact it is a true positive prediction of the seizure tendency changing but not necessarily reaching seizure threshold.”
Multiday patterns
Recent research shows that “we are just at the start,” Dr. Privitera said. “There are patterns underlying seizure frequency that … we are only beginning to be able to look at because of these chronic recordings.”
Baud et al. analyzed interictal epileptiform activity and seizures in patients who have had responsive neurostimulators for as long as 10 years (Nat Commun. 2018 Jan 8;9[1]:88). “What they found was that interictal spikes and rhythmic discharges oscillate with circadian and multiday periods that differ from person to person,” Dr. Privitera said. “There were multiday periodicities, most commonly in the 20- to 30-day duration, that were relatively stable over periods of time that lasted up to years.”
Researchers knew that seizures in women of childbearing age can cluster in association with the menstrual cycle, but similar cycles also were seen in men. In addition, the researchers found that seizures “occur preferentially during the rising phase of these multiday interictal rhythms,” which has implications for seizure forecasts, Dr. Privitera noted.
Stress biomarkers and wearables
Future seizure prediction methods may incorporate other biomarkers, such as stress hormones. A researcher at the University of Cincinnati, Jason Heikenfeld, PhD, is conducting research with a sensor that sticks to the wrist and measures sweat content, Dr. Privitera said. The technology originally was developed to measure sodium and potassium in sweat, but Dr. Privitera’s group has been working with him to measure cortisol, which may be a biomarker for stress and be useful for seizure prediction.
“Multivariate models are needed. We have lots of different ways that we can look at seizure prediction, and most likely the most accurate seizure prediction programs will incorporate multiple different areas,” Dr. Privitera said. “Seizure forecasting is possible. We can do it now. We can probably do it better than chance in many patients. ... It is important because changes in seizure likelihood could lead to pharmacologic or device or behavioral interventions that may help prevent seizures.”
Dr. Privitera reported conducting contracted research for Greenwich and SK Life Science and receiving consulting fees from Upsher-Smith and Astellas.
SOURCE: Privitera M. AES 2018, Judith Hoyer Lecture in Epilepsy.
NEW ORLEANS – For people with epilepsy, “the sudden and apparently unpredictable nature of seizures is one of the most disabling aspects of having the disorder,” said Michael Privitera, MD.
If a patient knew that “tomorrow will be a dangerous day” with a 50% chance of having a seizure, the patient could avoid hazardous activities, try to reduce stress, or increase supervision to reduce the risk of sudden, unexpected death in epilepsy, said Dr. Privitera, professor of neurology and director of the epilepsy center at the University of Cincinnati Gardner Neuroscience Institute. Physicians might be able to intervene during high-risk periods by altering antiepileptic drug regimens.
Evidence suggests that seizure prediction is possible today and that advances in wearable devices and analysis of chronic EEG recordings likely will improve the ability to predict seizures, Dr. Privitera said at the annual meeting of the American Epilepsy Society. Studies have found that some patients can predict the likelihood of seizures in the next 24 hours better than chance. In the future, algorithms that incorporate variables such as pulse, stress, mood, electrodermal activity, circadian rhythms, and EEG may further refine seizure prediction.
A complex picture
One problem with predicting seizures is that “you can have substantial changes in the seizure tendency, but not have a seizure,” Dr. Privitera said. Stress, alcohol, and missed medications, for example, may affect the seizure threshold. “They may be additive, and it may be when those things all hit at once that a seizure happens.”
Many patients report prodromal or premonitory symptoms before a seizure. “Most of us as clinicians will say, ‘Well, maybe you have some inkling, but I don’t think you’re really able to predict it,’ ” Dr. Privitera said.
Sheryl R. Haut, MD, professor of neurology at the Albert Einstein College of Medicine, New York, and her colleagues prospectively looked at patient self-prediction in 2007 (Neurology. 2007 Jan 23;68[4]:262-6). The investigators followed 74 people with epilepsy who completed a daily diary in which they predicted the likelihood of a seizure occurring in the next 24 hours. Their analysis included approximately 15,000 diary days and 1,400 seizure days.
A subset of participants, about 20%, was significantly better than chance at predicting when a seizure would happen. If a patient in this subgroup said that a seizure was extremely likely, then a seizure occurred approximately 37% of the time. If a patient predicted that a seizure was extremely unlikely, there was about a 10% chance of having a seizure.
“This was a pretty substantial difference,” Dr. Privitera said. Combining patients’ predictions with their self-reported stress levels seemed to yield the most accurate predictions.
Stress and the SMILE study
About 90% of people with epilepsy identify at least one seizure precipitant, and the most commonly cited trigger is stress. When Dr. Privitera and his colleagues surveyed patients in their clinic, 82% identified stress as a trigger (Epilepsy Behav. 2014 Dec;41:74-7). More than half of these patients had used some form of stress reduction, such as exercise, yoga, or meditation; 88% of those patients thought that stress reduction helped their seizures.
Underlying anxiety was the only difference between patients who thought that their seizures were triggered by stress and those who did not. Patients who did not think that stress triggered their seizures had significantly lower scores on the Generalized Anxiety Disorders–7.
Subsequently, Dr. Haut, Dr. Privitera, and colleagues conducted the Stress Management Intervention for Living with Epilepsy (SMILE) study, a prospective, controlled trial assessing the efficacy of a stress reduction intervention for reducing seizures, as well as measuring seizure self-prediction (Neurology. 2018 Mar 13;90[11]:e963-70). The researchers randomized patients to a progressive muscle relaxation intervention or to a control group; patients in the control group wrote down their activities for the day.
Patients posted diary entries twice daily into a smartphone, reporting stress levels and mood-related variables. As in Dr. Haut’s earlier study, patients predicted whether having a seizure was extremely unlikely, unlikely, neutral, likely, or extremely likely. Mood and stress variables (such as feeling unpleasant or pleasant, relaxed or stressed, and not worried or extremely worried) were ranked on a visual analog scale from 0 to 100.
The trial included participants who had at least two seizures per month and any seizure trigger. Medications were kept stable throughout the study. During a 2-month baseline, patients tracked their seizures and stress levels. During the 3-month treatment period, patients received the active or control intervention.
In all, 64 subjects completed the study, completing all diary entries on 94% of the days. In the active-treatment group, median seizure frequency decreased by 29%, compared with a 25% decrease in the control group. However, the difference between the groups was not statistically significant. Although the 25% reduction in the control group probably is partly attributable to the placebo effect, part of the decrease may be related to a mindfulness effect from completing the diary, Dr. Privitera said.
The active-treatment group had a statistically significant reduction in self-reported stress, compared with the control group, but this decrease did not correlate with seizure reduction. Changes in anxiety levels also did not correlate with seizures.
“It does not disprove the [stress] hypothesis, but it does tell us that there is more going on with stress and seizure triggers than just patients’ self-reported stress,” Dr. Privitera said.
Patients’ predictions
The seizure prediction findings in SMILE were similar to those of Dr. Haut’s earlier study. Among the 10 highest predictors out of the 64 participants, “when they said that a seizure was extremely likely, they were 8.36 times more likely to have a seizure than when they said a seizure was extremely unlikely,” Dr. Privitera said.
Many patients seemed to increase their predicted seizure probabilities in the days after having a seizure. In addition, feeling sad, nervous, worried, tense, or stressed significantly increased the likelihood that a patient would predict that a seizure was coming. However, these feelings were “not very accurate [for predicting] actual seizures,” he said. “Some people are better predictors, but really the basis of that prediction remains to be seen. One of my hypotheses is that some of these people may actually be responding to subclinical EEG changes.”
Together, these self-prediction studies include data from 4,500 seizures and 26,000 diary entries and show that “there is some information in patient self-report that can help us in understanding how to predict and when to predict seizures,” Dr. Privitera said.
Incorporating cardiac, EEG, and other variables
Various other factors may warrant inclusion in a seizure forecasting system. A new vagus nerve stimulation system responds to heart rate changes that occur at seizure onset. And for decades, researchers have studied the potential for EEG readings to predict seizures. A 2008 analysis of 47 reports concluded that limited progress had been made in predicting a seizure from interictal EEG (Epilepsy Behav. 2008 Jan;12[1]:128-35). Now, however, long-term intracranial recordings are providing new and important information about EEG patterns.
Whereas early studies examined EEG recordings from epilepsy monitoring units – when patients may have been sleep deprived, had medications removed, or recently undergone surgery – chronic intracranial recordings from devices such as the RNS (responsive neurostimulation) System have allowed researchers to look long term at EEG changes that are more representative of patients’ typical EEG patterns.
The RNS System detects interictal spikes and seizure discharges and then provides an electrical stimulation to stop seizures. “When you look at these recordings, there are a lot more electrographic seizures than clinical seizures that trigger these stimulations,” said Dr. Privitera. “If you look at somebody with a typical RNS, they may have 100 stimulations in a day and no clinical seizures. There are lots and lots of subclinical electrographic bursts – and not just spikes, but things that look like short electrographic seizures – that occur throughout the day.”
A handheld device
Researchers in Melbourne designed a system that uses implanted electrodes to provide chronic recordings (Lancet Neurol. 2013 Jun;12[6]:563-71). An algorithm then learned to predict the likelihood of a seizure from the patient’s data as the system recorded over time. The system could indicate when a seizure was likely by displaying a light on a handheld device. Patients were recorded for between 6 months and 3 years.
“There was a statistically significant ability to predict when seizures were happening,” Dr. Privitera said. “There is information in long-term intracranial recordings in many of these people that will help allow us to do a better prediction than what we are able to do right now, which is essentially not much.”
This research suggests that pooling data across patients may not be an effective seizure prediction strategy because different epilepsy types have different patterns. In addition, an individual’s patterns may differ from a group’s patterns. Complicating matters, individual patients may have multiple seizure types with different onset mechanisms.
“Another important lesson is that false positives in a deterministic sense may not represent false positives in a probabilistic sense,” Dr. Privitera said. “That is, when the seizure prediction program – whether it is the diary or the intracranial EEG or anything else – says the threshold changed, but you did not have a seizure, it does not mean that your prediction system was wrong. If the seizure tendency is going up … and your system says the seizure tendency went up, but all you are measuring is actual seizures, it looks like it is a false positive prediction of seizures. But in fact it is a true positive prediction of the seizure tendency changing but not necessarily reaching seizure threshold.”
Multiday patterns
Recent research shows that “we are just at the start,” Dr. Privitera said. “There are patterns underlying seizure frequency that … we are only beginning to be able to look at because of these chronic recordings.”
Baud et al. analyzed interictal epileptiform activity and seizures in patients who have had responsive neurostimulators for as long as 10 years (Nat Commun. 2018 Jan 8;9[1]:88). “What they found was that interictal spikes and rhythmic discharges oscillate with circadian and multiday periods that differ from person to person,” Dr. Privitera said. “There were multiday periodicities, most commonly in the 20- to 30-day duration, that were relatively stable over periods of time that lasted up to years.”
Researchers knew that seizures in women of childbearing age can cluster in association with the menstrual cycle, but similar cycles also were seen in men. In addition, the researchers found that seizures “occur preferentially during the rising phase of these multiday interictal rhythms,” which has implications for seizure forecasts, Dr. Privitera noted.
Stress biomarkers and wearables
Future seizure prediction methods may incorporate other biomarkers, such as stress hormones. A researcher at the University of Cincinnati, Jason Heikenfeld, PhD, is conducting research with a sensor that sticks to the wrist and measures sweat content, Dr. Privitera said. The technology originally was developed to measure sodium and potassium in sweat, but Dr. Privitera’s group has been working with him to measure cortisol, which may be a biomarker for stress and be useful for seizure prediction.
“Multivariate models are needed. We have lots of different ways that we can look at seizure prediction, and most likely the most accurate seizure prediction programs will incorporate multiple different areas,” Dr. Privitera said. “Seizure forecasting is possible. We can do it now. We can probably do it better than chance in many patients. ... It is important because changes in seizure likelihood could lead to pharmacologic or device or behavioral interventions that may help prevent seizures.”
Dr. Privitera reported conducting contracted research for Greenwich and SK Life Science and receiving consulting fees from Upsher-Smith and Astellas.
SOURCE: Privitera M. AES 2018, Judith Hoyer Lecture in Epilepsy.
NEW ORLEANS – For people with epilepsy, “the sudden and apparently unpredictable nature of seizures is one of the most disabling aspects of having the disorder,” said Michael Privitera, MD.
If a patient knew that “tomorrow will be a dangerous day” with a 50% chance of having a seizure, the patient could avoid hazardous activities, try to reduce stress, or increase supervision to reduce the risk of sudden, unexpected death in epilepsy, said Dr. Privitera, professor of neurology and director of the epilepsy center at the University of Cincinnati Gardner Neuroscience Institute. Physicians might be able to intervene during high-risk periods by altering antiepileptic drug regimens.
Evidence suggests that seizure prediction is possible today and that advances in wearable devices and analysis of chronic EEG recordings likely will improve the ability to predict seizures, Dr. Privitera said at the annual meeting of the American Epilepsy Society. Studies have found that some patients can predict the likelihood of seizures in the next 24 hours better than chance. In the future, algorithms that incorporate variables such as pulse, stress, mood, electrodermal activity, circadian rhythms, and EEG may further refine seizure prediction.
A complex picture
One problem with predicting seizures is that “you can have substantial changes in the seizure tendency, but not have a seizure,” Dr. Privitera said. Stress, alcohol, and missed medications, for example, may affect the seizure threshold. “They may be additive, and it may be when those things all hit at once that a seizure happens.”
Many patients report prodromal or premonitory symptoms before a seizure. “Most of us as clinicians will say, ‘Well, maybe you have some inkling, but I don’t think you’re really able to predict it,’ ” Dr. Privitera said.
Sheryl R. Haut, MD, professor of neurology at the Albert Einstein College of Medicine, New York, and her colleagues prospectively looked at patient self-prediction in 2007 (Neurology. 2007 Jan 23;68[4]:262-6). The investigators followed 74 people with epilepsy who completed a daily diary in which they predicted the likelihood of a seizure occurring in the next 24 hours. Their analysis included approximately 15,000 diary days and 1,400 seizure days.
A subset of participants, about 20%, was significantly better than chance at predicting when a seizure would happen. If a patient in this subgroup said that a seizure was extremely likely, then a seizure occurred approximately 37% of the time. If a patient predicted that a seizure was extremely unlikely, there was about a 10% chance of having a seizure.
“This was a pretty substantial difference,” Dr. Privitera said. Combining patients’ predictions with their self-reported stress levels seemed to yield the most accurate predictions.
Stress and the SMILE study
About 90% of people with epilepsy identify at least one seizure precipitant, and the most commonly cited trigger is stress. When Dr. Privitera and his colleagues surveyed patients in their clinic, 82% identified stress as a trigger (Epilepsy Behav. 2014 Dec;41:74-7). More than half of these patients had used some form of stress reduction, such as exercise, yoga, or meditation; 88% of those patients thought that stress reduction helped their seizures.
Underlying anxiety was the only difference between patients who thought that their seizures were triggered by stress and those who did not. Patients who did not think that stress triggered their seizures had significantly lower scores on the Generalized Anxiety Disorders–7.
Subsequently, Dr. Haut, Dr. Privitera, and colleagues conducted the Stress Management Intervention for Living with Epilepsy (SMILE) study, a prospective, controlled trial assessing the efficacy of a stress reduction intervention for reducing seizures, as well as measuring seizure self-prediction (Neurology. 2018 Mar 13;90[11]:e963-70). The researchers randomized patients to a progressive muscle relaxation intervention or to a control group; patients in the control group wrote down their activities for the day.
Patients posted diary entries twice daily into a smartphone, reporting stress levels and mood-related variables. As in Dr. Haut’s earlier study, patients predicted whether having a seizure was extremely unlikely, unlikely, neutral, likely, or extremely likely. Mood and stress variables (such as feeling unpleasant or pleasant, relaxed or stressed, and not worried or extremely worried) were ranked on a visual analog scale from 0 to 100.
The trial included participants who had at least two seizures per month and any seizure trigger. Medications were kept stable throughout the study. During a 2-month baseline, patients tracked their seizures and stress levels. During the 3-month treatment period, patients received the active or control intervention.
In all, 64 subjects completed the study, completing all diary entries on 94% of the days. In the active-treatment group, median seizure frequency decreased by 29%, compared with a 25% decrease in the control group. However, the difference between the groups was not statistically significant. Although the 25% reduction in the control group probably is partly attributable to the placebo effect, part of the decrease may be related to a mindfulness effect from completing the diary, Dr. Privitera said.
The active-treatment group had a statistically significant reduction in self-reported stress, compared with the control group, but this decrease did not correlate with seizure reduction. Changes in anxiety levels also did not correlate with seizures.
“It does not disprove the [stress] hypothesis, but it does tell us that there is more going on with stress and seizure triggers than just patients’ self-reported stress,” Dr. Privitera said.
Patients’ predictions
The seizure prediction findings in SMILE were similar to those of Dr. Haut’s earlier study. Among the 10 highest predictors out of the 64 participants, “when they said that a seizure was extremely likely, they were 8.36 times more likely to have a seizure than when they said a seizure was extremely unlikely,” Dr. Privitera said.
Many patients seemed to increase their predicted seizure probabilities in the days after having a seizure. In addition, feeling sad, nervous, worried, tense, or stressed significantly increased the likelihood that a patient would predict that a seizure was coming. However, these feelings were “not very accurate [for predicting] actual seizures,” he said. “Some people are better predictors, but really the basis of that prediction remains to be seen. One of my hypotheses is that some of these people may actually be responding to subclinical EEG changes.”
Together, these self-prediction studies include data from 4,500 seizures and 26,000 diary entries and show that “there is some information in patient self-report that can help us in understanding how to predict and when to predict seizures,” Dr. Privitera said.
Incorporating cardiac, EEG, and other variables
Various other factors may warrant inclusion in a seizure forecasting system. A new vagus nerve stimulation system responds to heart rate changes that occur at seizure onset. And for decades, researchers have studied the potential for EEG readings to predict seizures. A 2008 analysis of 47 reports concluded that limited progress had been made in predicting a seizure from interictal EEG (Epilepsy Behav. 2008 Jan;12[1]:128-35). Now, however, long-term intracranial recordings are providing new and important information about EEG patterns.
Whereas early studies examined EEG recordings from epilepsy monitoring units – when patients may have been sleep deprived, had medications removed, or recently undergone surgery – chronic intracranial recordings from devices such as the RNS (responsive neurostimulation) System have allowed researchers to look long term at EEG changes that are more representative of patients’ typical EEG patterns.
The RNS System detects interictal spikes and seizure discharges and then provides an electrical stimulation to stop seizures. “When you look at these recordings, there are a lot more electrographic seizures than clinical seizures that trigger these stimulations,” said Dr. Privitera. “If you look at somebody with a typical RNS, they may have 100 stimulations in a day and no clinical seizures. There are lots and lots of subclinical electrographic bursts – and not just spikes, but things that look like short electrographic seizures – that occur throughout the day.”
A handheld device
Researchers in Melbourne designed a system that uses implanted electrodes to provide chronic recordings (Lancet Neurol. 2013 Jun;12[6]:563-71). An algorithm then learned to predict the likelihood of a seizure from the patient’s data as the system recorded over time. The system could indicate when a seizure was likely by displaying a light on a handheld device. Patients were recorded for between 6 months and 3 years.
“There was a statistically significant ability to predict when seizures were happening,” Dr. Privitera said. “There is information in long-term intracranial recordings in many of these people that will help allow us to do a better prediction than what we are able to do right now, which is essentially not much.”
This research suggests that pooling data across patients may not be an effective seizure prediction strategy because different epilepsy types have different patterns. In addition, an individual’s patterns may differ from a group’s patterns. Complicating matters, individual patients may have multiple seizure types with different onset mechanisms.
“Another important lesson is that false positives in a deterministic sense may not represent false positives in a probabilistic sense,” Dr. Privitera said. “That is, when the seizure prediction program – whether it is the diary or the intracranial EEG or anything else – says the threshold changed, but you did not have a seizure, it does not mean that your prediction system was wrong. If the seizure tendency is going up … and your system says the seizure tendency went up, but all you are measuring is actual seizures, it looks like it is a false positive prediction of seizures. But in fact it is a true positive prediction of the seizure tendency changing but not necessarily reaching seizure threshold.”
Multiday patterns
Recent research shows that “we are just at the start,” Dr. Privitera said. “There are patterns underlying seizure frequency that … we are only beginning to be able to look at because of these chronic recordings.”
Baud et al. analyzed interictal epileptiform activity and seizures in patients who have had responsive neurostimulators for as long as 10 years (Nat Commun. 2018 Jan 8;9[1]:88). “What they found was that interictal spikes and rhythmic discharges oscillate with circadian and multiday periods that differ from person to person,” Dr. Privitera said. “There were multiday periodicities, most commonly in the 20- to 30-day duration, that were relatively stable over periods of time that lasted up to years.”
Researchers knew that seizures in women of childbearing age can cluster in association with the menstrual cycle, but similar cycles also were seen in men. In addition, the researchers found that seizures “occur preferentially during the rising phase of these multiday interictal rhythms,” which has implications for seizure forecasts, Dr. Privitera noted.
Stress biomarkers and wearables
Future seizure prediction methods may incorporate other biomarkers, such as stress hormones. A researcher at the University of Cincinnati, Jason Heikenfeld, PhD, is conducting research with a sensor that sticks to the wrist and measures sweat content, Dr. Privitera said. The technology originally was developed to measure sodium and potassium in sweat, but Dr. Privitera’s group has been working with him to measure cortisol, which may be a biomarker for stress and be useful for seizure prediction.
“Multivariate models are needed. We have lots of different ways that we can look at seizure prediction, and most likely the most accurate seizure prediction programs will incorporate multiple different areas,” Dr. Privitera said. “Seizure forecasting is possible. We can do it now. We can probably do it better than chance in many patients. ... It is important because changes in seizure likelihood could lead to pharmacologic or device or behavioral interventions that may help prevent seizures.”
Dr. Privitera reported conducting contracted research for Greenwich and SK Life Science and receiving consulting fees from Upsher-Smith and Astellas.
SOURCE: Privitera M. AES 2018, Judith Hoyer Lecture in Epilepsy.
REPORTING FROM AES 2018
FDA approves generic version of vigabatrin
The drug is approved for the adjunctive treatment of focal seizures in patients aged 10 years and older who have not had an adequate response to other therapies.
The approval was granted to Teva Pharmaceuticals.
An FDA announcement noted that the agency has prioritized the approval of generic versions of drugs to improve access to treatments and to lower drug costs. Vigabatrin had been included on an FDA list of off-patent, off-exclusivity branded drugs without approved generics. The approval of generic vigabatrin “demonstrates that there is an open pathway to approving products like this one,” said FDA Commissioner Scott Gottlieb, MD.
The label for vigabatrin tablets includes a boxed warning for permanent vision loss. The generic vigabatrin tablets are part of a single shared-system Risk Evaluation and Mitigation Strategy (REMS) program with other drug products containing vigabatrin.
The most common side effects associated with vigabatrin tablets include dizziness, fatigue, sleepiness, involuntary eye movement, tremor, blurred vision, memory impairment, weight gain, joint pain, upper respiratory tract infection, aggression, double vision, abnormal coordination, and a confused state. Serious side effects associated with vigabatrin tablets include permanent vision loss and risk of suicidal thoughts or actions.
The drug is approved for the adjunctive treatment of focal seizures in patients aged 10 years and older who have not had an adequate response to other therapies.
The approval was granted to Teva Pharmaceuticals.
An FDA announcement noted that the agency has prioritized the approval of generic versions of drugs to improve access to treatments and to lower drug costs. Vigabatrin had been included on an FDA list of off-patent, off-exclusivity branded drugs without approved generics. The approval of generic vigabatrin “demonstrates that there is an open pathway to approving products like this one,” said FDA Commissioner Scott Gottlieb, MD.
The label for vigabatrin tablets includes a boxed warning for permanent vision loss. The generic vigabatrin tablets are part of a single shared-system Risk Evaluation and Mitigation Strategy (REMS) program with other drug products containing vigabatrin.
The most common side effects associated with vigabatrin tablets include dizziness, fatigue, sleepiness, involuntary eye movement, tremor, blurred vision, memory impairment, weight gain, joint pain, upper respiratory tract infection, aggression, double vision, abnormal coordination, and a confused state. Serious side effects associated with vigabatrin tablets include permanent vision loss and risk of suicidal thoughts or actions.
The drug is approved for the adjunctive treatment of focal seizures in patients aged 10 years and older who have not had an adequate response to other therapies.
The approval was granted to Teva Pharmaceuticals.
An FDA announcement noted that the agency has prioritized the approval of generic versions of drugs to improve access to treatments and to lower drug costs. Vigabatrin had been included on an FDA list of off-patent, off-exclusivity branded drugs without approved generics. The approval of generic vigabatrin “demonstrates that there is an open pathway to approving products like this one,” said FDA Commissioner Scott Gottlieb, MD.
The label for vigabatrin tablets includes a boxed warning for permanent vision loss. The generic vigabatrin tablets are part of a single shared-system Risk Evaluation and Mitigation Strategy (REMS) program with other drug products containing vigabatrin.
The most common side effects associated with vigabatrin tablets include dizziness, fatigue, sleepiness, involuntary eye movement, tremor, blurred vision, memory impairment, weight gain, joint pain, upper respiratory tract infection, aggression, double vision, abnormal coordination, and a confused state. Serious side effects associated with vigabatrin tablets include permanent vision loss and risk of suicidal thoughts or actions.
Know the red flags for synaptic autoimmune psychosis
BARCELONA – Consider the possibility of an autoantibody-related etiology in all cases of first-onset psychosis, Josep Dalmau, MD, PhD, urged at the annual congress of the European College of Neuropsychopharmacology.
“There are patients in our clinics all of us – neurologists and psychiatrists – are missing. These patients are believed to have psychiatric presentations, but they do not. They are autoimmune,” said Dr. Dalmau, professor of neurology at the University of Barcelona.
Dr. Dalmau urged psychiatrists to become familiar with the red flags suggestive of synaptic autoimmunity as the underlying cause of first-episode, out-of-the-blue psychosis.
“If you have a patient with a classical presentation of schizophrenia or bipolar disorder, you probably won’t find antibodies,” according to the neurologist.
It’s important to have a high index of suspicion, because anti–NMDA receptor encephalitis is treatable with immunotherapy. And firm evidence shows that earlier recognition and treatment lead to improved outcomes. Also, the disorder is refractory to antipsychotics; indeed, 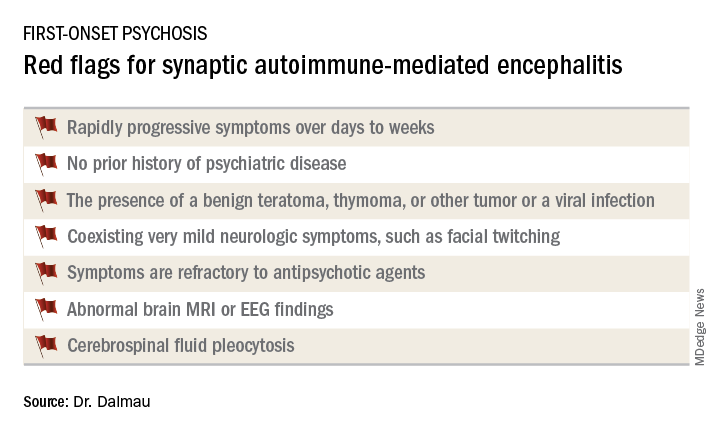
Manifestations of anti–NMDA receptor encephalitis follow a characteristic pattern, beginning with a prodromal flulike phase lasting several days to a week. This is followed by acute-onset bizarre behavioral changes, irritability, and psychosis with delusions and/or hallucinations, often progressing to catatonia. After 1-4 weeks of this, florid neurologic symptoms usually appear, including seizures, abnormal movements, autonomic dysregulation, and hypoventilation requiring prolonged ICU support for weeks to months. This is followed by a prolonged recovery phase lasting 5-24 months, and a period marked by deficits in executive function and working memory, impulsivity, and disinhibition. Impressively, the patient has no memory of the illness.
In one large series of patients with confirmed anti–NMDA receptor encephalitis reported by Dr. Dalmau and coinvestigators, psychiatric symptoms occurred in isolation without subsequent neurologic involvement in just 4% of cases (JAMA Neurol. 2013 Sep 1;70[9]:1133-9).
Dr. Dalmau was senior author of an international cohort study including 577 patients with anti-NMDA receptor encephalitis with serial follow-up for 24 months. The study provided an unprecedented picture of the epidemiology and clinical features of the disorder.
“It’s a disease predominantly of women and young people,” he observed.
Indeed, the median age of the study population was 21 years, and 37% of subjects were less than 18 years of age. Roughly 80% of patients were female and most of them had a benign ovarian teratoma, which played a key role in their neuropsychiatric disease (Lancet Neurol. 2013 Feb;12[2]:157-65). These benign tumors express the NMDA receptor in ectopic nerve tissue, triggering a systemic immune response.
One or more relapses – again treatable via immunotherapy – occurred in 12% of patients during 24 months of follow-up.
When a red flag suggestive of synaptic autoimmunity is present, it’s important to obtain a cerebrospinal fluid (CSF) sample for analysis, along with an EEG and/or brain MRI.
“I don’t know if you as psychiatrists are set up to do spinal taps in all persons with first presentation of psychosis, but this would be my suggestion. It’s extremely useful in this situation,” Dr. Dalmau said.
The vast majority of patients with anti–NMDA receptor encephalitis have CSF pleocytosis with a mild lymphocytic predominance. The MRI is abnormal in about 35% of cases. EEG abnormalities are common but nonspecific. The diagnosis is confirmed by identification of anti–NMDA receptor antibodies in the CSF.
First-line therapy is corticosteroids, intravenous immunoglobulin, and/or plasma exchange to remove the pathogenic antibodies, along with resection of the tumor if present. These treatments are effective in almost half of affected patients. When they’re not, the second-line options are rituximab (Rituxan) and cyclophosphamide, alone or combined.
Antibodies to the NMDA receptor are far and away the most common cause of synaptic autoimmunity-induced psychosis, but other targets of autoimmunity have been documented as well, including the alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor, contactin-associated protein-like 2 (CASPR2), and neurexin-3-alpha.
Dr. Dalmau and various collaborators continue to advance the understanding of this novel category of neuropsychiatric disease. They have developed a simple 5-point score, known as the NEOS score, that predicts 1-year functional status in patients with anti–NMDA receptor encephalitis (Neurology. 2018 Dec 21. doi: 10.1212/WNL.0000000000006783). He and his colleagues have also recently shown in a prospective study that herpes simplex encephalitis can result in an autoimmune encephalitis, with NMDA receptor antibodies present in most cases (Lancet Neurol. 2018 Sep;17[9]:760-72).
Dr. Dalmau’s research is supported by the U.S. National Institute of Neurological Disorders and Stroke, the Spanish Ministry of Health, and Spanish research foundations. He reported receiving royalties from the use of several neuronal antibody tests.
BARCELONA – Consider the possibility of an autoantibody-related etiology in all cases of first-onset psychosis, Josep Dalmau, MD, PhD, urged at the annual congress of the European College of Neuropsychopharmacology.
“There are patients in our clinics all of us – neurologists and psychiatrists – are missing. These patients are believed to have psychiatric presentations, but they do not. They are autoimmune,” said Dr. Dalmau, professor of neurology at the University of Barcelona.
Dr. Dalmau urged psychiatrists to become familiar with the red flags suggestive of synaptic autoimmunity as the underlying cause of first-episode, out-of-the-blue psychosis.
“If you have a patient with a classical presentation of schizophrenia or bipolar disorder, you probably won’t find antibodies,” according to the neurologist.
It’s important to have a high index of suspicion, because anti–NMDA receptor encephalitis is treatable with immunotherapy. And firm evidence shows that earlier recognition and treatment lead to improved outcomes. Also, the disorder is refractory to antipsychotics; indeed, 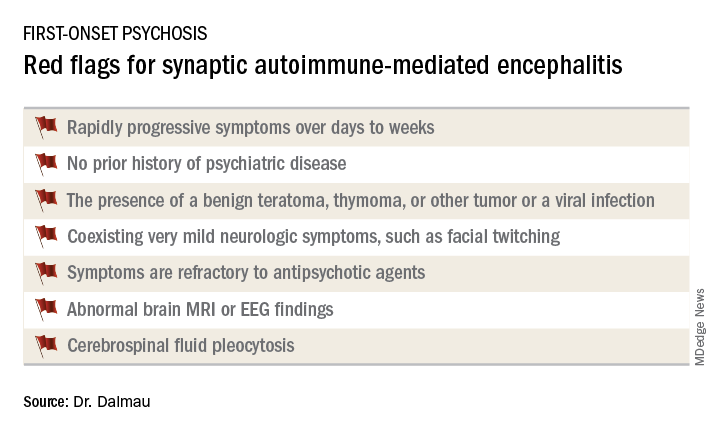
Manifestations of anti–NMDA receptor encephalitis follow a characteristic pattern, beginning with a prodromal flulike phase lasting several days to a week. This is followed by acute-onset bizarre behavioral changes, irritability, and psychosis with delusions and/or hallucinations, often progressing to catatonia. After 1-4 weeks of this, florid neurologic symptoms usually appear, including seizures, abnormal movements, autonomic dysregulation, and hypoventilation requiring prolonged ICU support for weeks to months. This is followed by a prolonged recovery phase lasting 5-24 months, and a period marked by deficits in executive function and working memory, impulsivity, and disinhibition. Impressively, the patient has no memory of the illness.
In one large series of patients with confirmed anti–NMDA receptor encephalitis reported by Dr. Dalmau and coinvestigators, psychiatric symptoms occurred in isolation without subsequent neurologic involvement in just 4% of cases (JAMA Neurol. 2013 Sep 1;70[9]:1133-9).
Dr. Dalmau was senior author of an international cohort study including 577 patients with anti-NMDA receptor encephalitis with serial follow-up for 24 months. The study provided an unprecedented picture of the epidemiology and clinical features of the disorder.
“It’s a disease predominantly of women and young people,” he observed.
Indeed, the median age of the study population was 21 years, and 37% of subjects were less than 18 years of age. Roughly 80% of patients were female and most of them had a benign ovarian teratoma, which played a key role in their neuropsychiatric disease (Lancet Neurol. 2013 Feb;12[2]:157-65). These benign tumors express the NMDA receptor in ectopic nerve tissue, triggering a systemic immune response.
One or more relapses – again treatable via immunotherapy – occurred in 12% of patients during 24 months of follow-up.
When a red flag suggestive of synaptic autoimmunity is present, it’s important to obtain a cerebrospinal fluid (CSF) sample for analysis, along with an EEG and/or brain MRI.
“I don’t know if you as psychiatrists are set up to do spinal taps in all persons with first presentation of psychosis, but this would be my suggestion. It’s extremely useful in this situation,” Dr. Dalmau said.
The vast majority of patients with anti–NMDA receptor encephalitis have CSF pleocytosis with a mild lymphocytic predominance. The MRI is abnormal in about 35% of cases. EEG abnormalities are common but nonspecific. The diagnosis is confirmed by identification of anti–NMDA receptor antibodies in the CSF.
First-line therapy is corticosteroids, intravenous immunoglobulin, and/or plasma exchange to remove the pathogenic antibodies, along with resection of the tumor if present. These treatments are effective in almost half of affected patients. When they’re not, the second-line options are rituximab (Rituxan) and cyclophosphamide, alone or combined.
Antibodies to the NMDA receptor are far and away the most common cause of synaptic autoimmunity-induced psychosis, but other targets of autoimmunity have been documented as well, including the alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor, contactin-associated protein-like 2 (CASPR2), and neurexin-3-alpha.
Dr. Dalmau and various collaborators continue to advance the understanding of this novel category of neuropsychiatric disease. They have developed a simple 5-point score, known as the NEOS score, that predicts 1-year functional status in patients with anti–NMDA receptor encephalitis (Neurology. 2018 Dec 21. doi: 10.1212/WNL.0000000000006783). He and his colleagues have also recently shown in a prospective study that herpes simplex encephalitis can result in an autoimmune encephalitis, with NMDA receptor antibodies present in most cases (Lancet Neurol. 2018 Sep;17[9]:760-72).
Dr. Dalmau’s research is supported by the U.S. National Institute of Neurological Disorders and Stroke, the Spanish Ministry of Health, and Spanish research foundations. He reported receiving royalties from the use of several neuronal antibody tests.
BARCELONA – Consider the possibility of an autoantibody-related etiology in all cases of first-onset psychosis, Josep Dalmau, MD, PhD, urged at the annual congress of the European College of Neuropsychopharmacology.
“There are patients in our clinics all of us – neurologists and psychiatrists – are missing. These patients are believed to have psychiatric presentations, but they do not. They are autoimmune,” said Dr. Dalmau, professor of neurology at the University of Barcelona.
Dr. Dalmau urged psychiatrists to become familiar with the red flags suggestive of synaptic autoimmunity as the underlying cause of first-episode, out-of-the-blue psychosis.
“If you have a patient with a classical presentation of schizophrenia or bipolar disorder, you probably won’t find antibodies,” according to the neurologist.
It’s important to have a high index of suspicion, because anti–NMDA receptor encephalitis is treatable with immunotherapy. And firm evidence shows that earlier recognition and treatment lead to improved outcomes. Also, the disorder is refractory to antipsychotics; indeed, 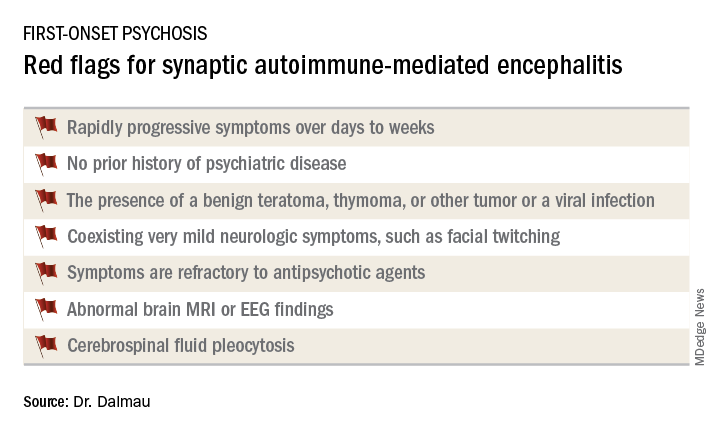
Manifestations of anti–NMDA receptor encephalitis follow a characteristic pattern, beginning with a prodromal flulike phase lasting several days to a week. This is followed by acute-onset bizarre behavioral changes, irritability, and psychosis with delusions and/or hallucinations, often progressing to catatonia. After 1-4 weeks of this, florid neurologic symptoms usually appear, including seizures, abnormal movements, autonomic dysregulation, and hypoventilation requiring prolonged ICU support for weeks to months. This is followed by a prolonged recovery phase lasting 5-24 months, and a period marked by deficits in executive function and working memory, impulsivity, and disinhibition. Impressively, the patient has no memory of the illness.
In one large series of patients with confirmed anti–NMDA receptor encephalitis reported by Dr. Dalmau and coinvestigators, psychiatric symptoms occurred in isolation without subsequent neurologic involvement in just 4% of cases (JAMA Neurol. 2013 Sep 1;70[9]:1133-9).
Dr. Dalmau was senior author of an international cohort study including 577 patients with anti-NMDA receptor encephalitis with serial follow-up for 24 months. The study provided an unprecedented picture of the epidemiology and clinical features of the disorder.
“It’s a disease predominantly of women and young people,” he observed.
Indeed, the median age of the study population was 21 years, and 37% of subjects were less than 18 years of age. Roughly 80% of patients were female and most of them had a benign ovarian teratoma, which played a key role in their neuropsychiatric disease (Lancet Neurol. 2013 Feb;12[2]:157-65). These benign tumors express the NMDA receptor in ectopic nerve tissue, triggering a systemic immune response.
One or more relapses – again treatable via immunotherapy – occurred in 12% of patients during 24 months of follow-up.
When a red flag suggestive of synaptic autoimmunity is present, it’s important to obtain a cerebrospinal fluid (CSF) sample for analysis, along with an EEG and/or brain MRI.
“I don’t know if you as psychiatrists are set up to do spinal taps in all persons with first presentation of psychosis, but this would be my suggestion. It’s extremely useful in this situation,” Dr. Dalmau said.
The vast majority of patients with anti–NMDA receptor encephalitis have CSF pleocytosis with a mild lymphocytic predominance. The MRI is abnormal in about 35% of cases. EEG abnormalities are common but nonspecific. The diagnosis is confirmed by identification of anti–NMDA receptor antibodies in the CSF.
First-line therapy is corticosteroids, intravenous immunoglobulin, and/or plasma exchange to remove the pathogenic antibodies, along with resection of the tumor if present. These treatments are effective in almost half of affected patients. When they’re not, the second-line options are rituximab (Rituxan) and cyclophosphamide, alone or combined.
Antibodies to the NMDA receptor are far and away the most common cause of synaptic autoimmunity-induced psychosis, but other targets of autoimmunity have been documented as well, including the alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor, contactin-associated protein-like 2 (CASPR2), and neurexin-3-alpha.
Dr. Dalmau and various collaborators continue to advance the understanding of this novel category of neuropsychiatric disease. They have developed a simple 5-point score, known as the NEOS score, that predicts 1-year functional status in patients with anti–NMDA receptor encephalitis (Neurology. 2018 Dec 21. doi: 10.1212/WNL.0000000000006783). He and his colleagues have also recently shown in a prospective study that herpes simplex encephalitis can result in an autoimmune encephalitis, with NMDA receptor antibodies present in most cases (Lancet Neurol. 2018 Sep;17[9]:760-72).
Dr. Dalmau’s research is supported by the U.S. National Institute of Neurological Disorders and Stroke, the Spanish Ministry of Health, and Spanish research foundations. He reported receiving royalties from the use of several neuronal antibody tests.
REPORTING FROM THE ECNP CONGRESS
Population-level rate of SUDEP may have decreased
NEW ORLEANS – according to data described at the annual meeting of the American Epilepsy Society. Whether this decrease resulted from an improved understanding of SUDEP risk or a focus on risk-reduction strategies is unknown, said Daniel Friedman, MD, associate professor of neurology at the New York University Langone Health.
In addition, the rates of SUDEP in various populations differ according to their socioeconomic status. Differences in access to care are a potential, but unconfirmed, explanation for this association, said Dr. Friedman. Another possible explanation is that confounders such as mental health disorders, substance abuse, and insufficient social support affect individuals’ ability to manage their disorder.
Dr. Friedman and colleagues initially examined SUDEP rates over time in a cohort of patients who received vagus nerve stimulator (VNS) implantation for drug-resistant epilepsy. They analyzed data for 40,443 patients who underwent surgery during 1988-2012. The age-adjusted SUDEP rate per 1,000 person-years of follow-up decreased significantly from 2.47 in years 1-2 to 1.68 in years 3-10. “There was no control group, so we couldn’t necessarily attribute the SUDEP rate reduction to the intervention,” said Dr. Friedman. A study by Tomson et al of patients with epilepsy who received VNS implantation had similar findings.
The literature about the mechanisms of SUDEP and reduction of SUDEP risk has increased in recent years. Neurologists have advocated for greater disclosure to patients of SUDEP risk, as well as better risk counseling. Dr. Friedman and his colleagues decided to investigate whether these factors have affected the risk of SUDEP during the past decade.
They retrospectively examined data for people whose deaths had been investigated at medical examiner’s offices in New York City, San Diego County, and Maryland. They focused on decedents for whom epilepsy or seizure was listed as a cause or contributor to death or as a comorbid condition on the death certificate. They reviewed all available reports, including investigator notes, autopsy reports, and medical records. Next, Dr. Friedman and his colleagues calculated the annual SUDEP rate as a proportion of the general population, estimated using annual Census and American Community Survey data. They used the Mann-Kendall test to analyze the trends in SUDEP rate during 2009-2015.
Of 1,466 deaths in people with epilepsy during this period, 1,124 were classified as definite SUDEP, probable SUDEP, or near SUDEP. Approximately 63% of SUDEP cases were male, and 45% were African-American. The mean age at death was 38 years.
Dr. Friedman’s group found a significant decrease in the overall incidence of SUDEP in the total population during 2009-2015. When they examined the three regions separately, they found decreases in SUDEP incidence in New York City and Maryland, but not in San Diego County. They found no difference in SUDEP rates by season or by day of the week.
In a subsequent analysis, Dr. Friedman and his colleagues adjudicated all deaths related to seizure and epilepsy in the three regions during 2009-2010 and 2014-2015 and identified all cases of definite and probable SUDEP. The estimated rate of SUDEP decreased by about 36% from the first period to the second period. SUDEP rates as a proportion of the total population in those regions also declined.
The investigators also examined differences in estimated SUDEP rates in the United States according to median household income. In New York, the zip codes with the highest SUDEP rates tended to have the lowest median household incomes. The zip codes in the lowest quartile of family household income had a SUDEP rate more than twice as high as that in the zip codes in the highest income quartile. This association held true for the period from 2009-2010 and for 2014-2015.
Dr. Friedman and colleagues received funding from Finding a Cure for Epilepsy and Seizures, which is affiliated with the NYU Comprehensive Epilepsy Center and NYU Langone Health.
SOURCE: Cihan E et al. AES 2018, Abstract 2.419.
NEW ORLEANS – according to data described at the annual meeting of the American Epilepsy Society. Whether this decrease resulted from an improved understanding of SUDEP risk or a focus on risk-reduction strategies is unknown, said Daniel Friedman, MD, associate professor of neurology at the New York University Langone Health.
In addition, the rates of SUDEP in various populations differ according to their socioeconomic status. Differences in access to care are a potential, but unconfirmed, explanation for this association, said Dr. Friedman. Another possible explanation is that confounders such as mental health disorders, substance abuse, and insufficient social support affect individuals’ ability to manage their disorder.
Dr. Friedman and colleagues initially examined SUDEP rates over time in a cohort of patients who received vagus nerve stimulator (VNS) implantation for drug-resistant epilepsy. They analyzed data for 40,443 patients who underwent surgery during 1988-2012. The age-adjusted SUDEP rate per 1,000 person-years of follow-up decreased significantly from 2.47 in years 1-2 to 1.68 in years 3-10. “There was no control group, so we couldn’t necessarily attribute the SUDEP rate reduction to the intervention,” said Dr. Friedman. A study by Tomson et al of patients with epilepsy who received VNS implantation had similar findings.
The literature about the mechanisms of SUDEP and reduction of SUDEP risk has increased in recent years. Neurologists have advocated for greater disclosure to patients of SUDEP risk, as well as better risk counseling. Dr. Friedman and his colleagues decided to investigate whether these factors have affected the risk of SUDEP during the past decade.
They retrospectively examined data for people whose deaths had been investigated at medical examiner’s offices in New York City, San Diego County, and Maryland. They focused on decedents for whom epilepsy or seizure was listed as a cause or contributor to death or as a comorbid condition on the death certificate. They reviewed all available reports, including investigator notes, autopsy reports, and medical records. Next, Dr. Friedman and his colleagues calculated the annual SUDEP rate as a proportion of the general population, estimated using annual Census and American Community Survey data. They used the Mann-Kendall test to analyze the trends in SUDEP rate during 2009-2015.
Of 1,466 deaths in people with epilepsy during this period, 1,124 were classified as definite SUDEP, probable SUDEP, or near SUDEP. Approximately 63% of SUDEP cases were male, and 45% were African-American. The mean age at death was 38 years.
Dr. Friedman’s group found a significant decrease in the overall incidence of SUDEP in the total population during 2009-2015. When they examined the three regions separately, they found decreases in SUDEP incidence in New York City and Maryland, but not in San Diego County. They found no difference in SUDEP rates by season or by day of the week.
In a subsequent analysis, Dr. Friedman and his colleagues adjudicated all deaths related to seizure and epilepsy in the three regions during 2009-2010 and 2014-2015 and identified all cases of definite and probable SUDEP. The estimated rate of SUDEP decreased by about 36% from the first period to the second period. SUDEP rates as a proportion of the total population in those regions also declined.
The investigators also examined differences in estimated SUDEP rates in the United States according to median household income. In New York, the zip codes with the highest SUDEP rates tended to have the lowest median household incomes. The zip codes in the lowest quartile of family household income had a SUDEP rate more than twice as high as that in the zip codes in the highest income quartile. This association held true for the period from 2009-2010 and for 2014-2015.
Dr. Friedman and colleagues received funding from Finding a Cure for Epilepsy and Seizures, which is affiliated with the NYU Comprehensive Epilepsy Center and NYU Langone Health.
SOURCE: Cihan E et al. AES 2018, Abstract 2.419.
NEW ORLEANS – according to data described at the annual meeting of the American Epilepsy Society. Whether this decrease resulted from an improved understanding of SUDEP risk or a focus on risk-reduction strategies is unknown, said Daniel Friedman, MD, associate professor of neurology at the New York University Langone Health.
In addition, the rates of SUDEP in various populations differ according to their socioeconomic status. Differences in access to care are a potential, but unconfirmed, explanation for this association, said Dr. Friedman. Another possible explanation is that confounders such as mental health disorders, substance abuse, and insufficient social support affect individuals’ ability to manage their disorder.
Dr. Friedman and colleagues initially examined SUDEP rates over time in a cohort of patients who received vagus nerve stimulator (VNS) implantation for drug-resistant epilepsy. They analyzed data for 40,443 patients who underwent surgery during 1988-2012. The age-adjusted SUDEP rate per 1,000 person-years of follow-up decreased significantly from 2.47 in years 1-2 to 1.68 in years 3-10. “There was no control group, so we couldn’t necessarily attribute the SUDEP rate reduction to the intervention,” said Dr. Friedman. A study by Tomson et al of patients with epilepsy who received VNS implantation had similar findings.
The literature about the mechanisms of SUDEP and reduction of SUDEP risk has increased in recent years. Neurologists have advocated for greater disclosure to patients of SUDEP risk, as well as better risk counseling. Dr. Friedman and his colleagues decided to investigate whether these factors have affected the risk of SUDEP during the past decade.
They retrospectively examined data for people whose deaths had been investigated at medical examiner’s offices in New York City, San Diego County, and Maryland. They focused on decedents for whom epilepsy or seizure was listed as a cause or contributor to death or as a comorbid condition on the death certificate. They reviewed all available reports, including investigator notes, autopsy reports, and medical records. Next, Dr. Friedman and his colleagues calculated the annual SUDEP rate as a proportion of the general population, estimated using annual Census and American Community Survey data. They used the Mann-Kendall test to analyze the trends in SUDEP rate during 2009-2015.
Of 1,466 deaths in people with epilepsy during this period, 1,124 were classified as definite SUDEP, probable SUDEP, or near SUDEP. Approximately 63% of SUDEP cases were male, and 45% were African-American. The mean age at death was 38 years.
Dr. Friedman’s group found a significant decrease in the overall incidence of SUDEP in the total population during 2009-2015. When they examined the three regions separately, they found decreases in SUDEP incidence in New York City and Maryland, but not in San Diego County. They found no difference in SUDEP rates by season or by day of the week.
In a subsequent analysis, Dr. Friedman and his colleagues adjudicated all deaths related to seizure and epilepsy in the three regions during 2009-2010 and 2014-2015 and identified all cases of definite and probable SUDEP. The estimated rate of SUDEP decreased by about 36% from the first period to the second period. SUDEP rates as a proportion of the total population in those regions also declined.
The investigators also examined differences in estimated SUDEP rates in the United States according to median household income. In New York, the zip codes with the highest SUDEP rates tended to have the lowest median household incomes. The zip codes in the lowest quartile of family household income had a SUDEP rate more than twice as high as that in the zip codes in the highest income quartile. This association held true for the period from 2009-2010 and for 2014-2015.
Dr. Friedman and colleagues received funding from Finding a Cure for Epilepsy and Seizures, which is affiliated with the NYU Comprehensive Epilepsy Center and NYU Langone Health.
SOURCE: Cihan E et al. AES 2018, Abstract 2.419.
REPORTING FROM AES 2018
Key clinical point: Data indicate a decline over time in the incidence of SUDEP.
Major finding: The incidence of SUDEP declined by 36% from 2009-2010 to 2014-2015.
Study details: A retrospective analysis of medical examiner data on 1,466 deaths in people with epilepsy.
Disclosures: Finding a Cure for Epilepsy and Seizures provided funding for the study.
Source: Cihan E et al. AES 2018, Abstract 2.419.











