User login
Neonates at highest risk for Ebstein's malformation treatment
LOS ANGELES – Ebstein’s malformation is a rare congenital cardiac anomaly. Surgery for Ebstein’s involves a range of procedures, and with low institutional volumes, the only available data on treatment are limited to individual reports demonstrating highly variable approaches. Neonates in particular are at risk for poor outcomes, showing significantly higher mortality than infants, children, and adults, according to a database study presented by Dr. Ryan R. Davies at the annual meeting of the Society of Thoracic Surgeons.
Dr. Davies of the Nemours/A.I. duPont Hospital for Children, Wilmington, Del., and his colleagues performed a retrospective study of procedures performed on patients with a primary diagnosis of Ebstein’s malformation (2002-2009) in the STS Congenital Heart Surgery Database.
A total of 595 operations on patients with Ebstein’s were included: 116 on neonates (19%), 122 on infants (21%), 264 on children (44%), and 93 on adults (16%). The authors found that average annual institutional case volumes were low (median, 1 case/year), and procedures varied according to age. Neonates had a high rate of palliative procedures: tricuspid valve (TV) closure (16%) and systemic-to-pulmonary shunts with or without TV closure (37%) and isolated TV closure (8.6%), with Ebstein’s repair or TV valvuloplasty performed in 32%.
Infants usually underwent superior cavopulmonary connections (52%).
Among older patients, procedures were mostly in three categories: TV surgery (children, 55%; adults, 69%), arrhythmia procedures (children, 9%; adults, 17%), and Fontan (children, 16%). In-hospital mortality was higher among neonatal patients (23%) than in infants (4%), children (0.8%), and adults (1.1%).
Among neonates, 36 subsequent procedures were performed during the same hospitalization in 27 patients (23%); including TV closure (11%); shunt (15%); Ebstein’s repair (17%) or TV replacement (15%); and heart transplantation (7.4%). Mortality was similar among neonates who had a second procedure and those who did not (27% vs. 23%, respectively). ECMO (extracorporeal membrane oxygenation) was used in 9% of neonates but in less than 2% of patients in other age groups.
"This study represents a broad overview of the diverse options for surgical treatment of Ebstein’s anomaly. It shows the challenges faced in caring for extremely ill neonatal patients. We have also shown that repair of Ebstein’s anomaly is performed infrequently at most centers, limiting the ability of individual series to define optimal management strategies," Dr. Davies said in an interview.
"Unfortunately, currently available databases do not contain information that may be important in defining such strategies (both surgical and nonsurgical), including anatomic and physiologic variables – whether they are neonates presenting in severe heart failure or older patients presenting for tricuspid valve repair or replacement," he added.
"We feel that in this setting, a prospective multi-institutional study would be of significant value. It should include operative and nonoperative patients, as well as precise diagnostic information and procedural details, to evaluate long-term outcomes including survival, reoperation and other reinterventions, as well as neurodevelopmental outcomes, functional health status, and quality of life," Dr. Davies concluded.
Dr. Davies and his colleagues reported having no relevant disclosures.
LOS ANGELES – Ebstein’s malformation is a rare congenital cardiac anomaly. Surgery for Ebstein’s involves a range of procedures, and with low institutional volumes, the only available data on treatment are limited to individual reports demonstrating highly variable approaches. Neonates in particular are at risk for poor outcomes, showing significantly higher mortality than infants, children, and adults, according to a database study presented by Dr. Ryan R. Davies at the annual meeting of the Society of Thoracic Surgeons.
Dr. Davies of the Nemours/A.I. duPont Hospital for Children, Wilmington, Del., and his colleagues performed a retrospective study of procedures performed on patients with a primary diagnosis of Ebstein’s malformation (2002-2009) in the STS Congenital Heart Surgery Database.
A total of 595 operations on patients with Ebstein’s were included: 116 on neonates (19%), 122 on infants (21%), 264 on children (44%), and 93 on adults (16%). The authors found that average annual institutional case volumes were low (median, 1 case/year), and procedures varied according to age. Neonates had a high rate of palliative procedures: tricuspid valve (TV) closure (16%) and systemic-to-pulmonary shunts with or without TV closure (37%) and isolated TV closure (8.6%), with Ebstein’s repair or TV valvuloplasty performed in 32%.
Infants usually underwent superior cavopulmonary connections (52%).
Among older patients, procedures were mostly in three categories: TV surgery (children, 55%; adults, 69%), arrhythmia procedures (children, 9%; adults, 17%), and Fontan (children, 16%). In-hospital mortality was higher among neonatal patients (23%) than in infants (4%), children (0.8%), and adults (1.1%).
Among neonates, 36 subsequent procedures were performed during the same hospitalization in 27 patients (23%); including TV closure (11%); shunt (15%); Ebstein’s repair (17%) or TV replacement (15%); and heart transplantation (7.4%). Mortality was similar among neonates who had a second procedure and those who did not (27% vs. 23%, respectively). ECMO (extracorporeal membrane oxygenation) was used in 9% of neonates but in less than 2% of patients in other age groups.
"This study represents a broad overview of the diverse options for surgical treatment of Ebstein’s anomaly. It shows the challenges faced in caring for extremely ill neonatal patients. We have also shown that repair of Ebstein’s anomaly is performed infrequently at most centers, limiting the ability of individual series to define optimal management strategies," Dr. Davies said in an interview.
"Unfortunately, currently available databases do not contain information that may be important in defining such strategies (both surgical and nonsurgical), including anatomic and physiologic variables – whether they are neonates presenting in severe heart failure or older patients presenting for tricuspid valve repair or replacement," he added.
"We feel that in this setting, a prospective multi-institutional study would be of significant value. It should include operative and nonoperative patients, as well as precise diagnostic information and procedural details, to evaluate long-term outcomes including survival, reoperation and other reinterventions, as well as neurodevelopmental outcomes, functional health status, and quality of life," Dr. Davies concluded.
Dr. Davies and his colleagues reported having no relevant disclosures.
LOS ANGELES – Ebstein’s malformation is a rare congenital cardiac anomaly. Surgery for Ebstein’s involves a range of procedures, and with low institutional volumes, the only available data on treatment are limited to individual reports demonstrating highly variable approaches. Neonates in particular are at risk for poor outcomes, showing significantly higher mortality than infants, children, and adults, according to a database study presented by Dr. Ryan R. Davies at the annual meeting of the Society of Thoracic Surgeons.
Dr. Davies of the Nemours/A.I. duPont Hospital for Children, Wilmington, Del., and his colleagues performed a retrospective study of procedures performed on patients with a primary diagnosis of Ebstein’s malformation (2002-2009) in the STS Congenital Heart Surgery Database.
A total of 595 operations on patients with Ebstein’s were included: 116 on neonates (19%), 122 on infants (21%), 264 on children (44%), and 93 on adults (16%). The authors found that average annual institutional case volumes were low (median, 1 case/year), and procedures varied according to age. Neonates had a high rate of palliative procedures: tricuspid valve (TV) closure (16%) and systemic-to-pulmonary shunts with or without TV closure (37%) and isolated TV closure (8.6%), with Ebstein’s repair or TV valvuloplasty performed in 32%.
Infants usually underwent superior cavopulmonary connections (52%).
Among older patients, procedures were mostly in three categories: TV surgery (children, 55%; adults, 69%), arrhythmia procedures (children, 9%; adults, 17%), and Fontan (children, 16%). In-hospital mortality was higher among neonatal patients (23%) than in infants (4%), children (0.8%), and adults (1.1%).
Among neonates, 36 subsequent procedures were performed during the same hospitalization in 27 patients (23%); including TV closure (11%); shunt (15%); Ebstein’s repair (17%) or TV replacement (15%); and heart transplantation (7.4%). Mortality was similar among neonates who had a second procedure and those who did not (27% vs. 23%, respectively). ECMO (extracorporeal membrane oxygenation) was used in 9% of neonates but in less than 2% of patients in other age groups.
"This study represents a broad overview of the diverse options for surgical treatment of Ebstein’s anomaly. It shows the challenges faced in caring for extremely ill neonatal patients. We have also shown that repair of Ebstein’s anomaly is performed infrequently at most centers, limiting the ability of individual series to define optimal management strategies," Dr. Davies said in an interview.
"Unfortunately, currently available databases do not contain information that may be important in defining such strategies (both surgical and nonsurgical), including anatomic and physiologic variables – whether they are neonates presenting in severe heart failure or older patients presenting for tricuspid valve repair or replacement," he added.
"We feel that in this setting, a prospective multi-institutional study would be of significant value. It should include operative and nonoperative patients, as well as precise diagnostic information and procedural details, to evaluate long-term outcomes including survival, reoperation and other reinterventions, as well as neurodevelopmental outcomes, functional health status, and quality of life," Dr. Davies concluded.
Dr. Davies and his colleagues reported having no relevant disclosures.
AT THE STS ANNUAL MEETING
Major Finding: In-hospital mortality was higher among neonatal patients (23%) than in infants (4%), children (0.8%), and adults (1.1%).
Data Source: A retrospective database analysis of 595 operations on patients with Ebstein’s malformation.
Disclosures: Dr. Davies and his colleagues reported having no relevant disclosures.
Valve-sparing root replacement carries the day
SNOWMASS, COLO. – Valve-sparing root replacement has emerged as the procedure of choice in patients with isolated aortic root disease and a normally functioning aortic valve, according to Dr. Thoralf M. Sundt III.
"The valve-sparing root operations, in contrast to some of the other things we surgeons have come up with over the last decade or so, are increasing in popularity. They’re more and more commonly done, and that’s a good sign. I think the marketplace has spoken and this is clearly a good operation. It’s an operation that can be learned, and surgeons can do it with good results," he said at the Annual Cardiovascular Conference at Snowmass.
Valve-sparing root replacement (VSRR) spares a patient from the complications associated with lifelong anticoagulation for a mechanical valve, and the durability of VSRR appears to be superior to that of third-generation bioprostheses, the surgeon added.
"They’re holding up pretty well. The outcomes approach those with mechanical valves," said Dr. Sundt, chief of cardiac surgery at Massachusetts General Hospital and professor of surgery at Harvard Medical School, Boston.
Moreover, he continued, VSRR has another big advantage over bioprosthetic valves: "If you have to re-operate, it’s a whole lot more fun to do so on someone who’s had a VSRR and put a new biologic valve inside a native annulus than it is to try to take out that old bioprosthesis and put a new bioprosthesis in."
A meta-analysis of 11 studies comparing VSRR with total root replacement in patients with Marfan syndrome concluded that composite valve-related event rates for the two surgical strategies were not significantly different. The thromboembolic event rate was 0.3% per year in VSRR-treated patients, significantly lower than the still-quite-reasonable 0.7% per year rate after total root replacement (Heart 2011;97:955-8).
A recent study by surgeons at Stanford (Calif.) University gave VSRR a thumbs up regarding mid-term durability of outcomes through 6 years of follow-up, with a mean 2.9-year and maximum 6-year follow-up. The series included 75 patients with bicuspid aortic valve disease treated by VSRR.
Six-year actuarial survival was 99%, with 90% freedom from reoperation and no strokes. Thirty-one percent of patients had 2+ aortic regurgitation preoperatively; at echocardiographic follow-up a mean of 2.9 years post surgery, only a couple of patients had 2+ aortic regurgitation and no one was more severely affected. The Stanford investigators plan to update their results when follow-up reaches 10 years or more (J. Thorac. Cardiovasc. Surg. Dec. 20, 2012 [doi:10.1016/j.jtcvs.2012.11.043]).
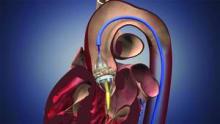
The VSRR was developed by Dr. Tirone David of the University of Toronto. The procedure involves skeletonizing the root while preserving the leaflets and their attachments to the aortic wall. The aortic valve is then reimplanted inside a tubular Dacron graft, and then the coronary arteries are reimplanted.
"It’s probably the neatest development in terms of surgical options for the aortic valve in a long time," Dr. Sundt said.
He reported having no financial conflicts.
SNOWMASS, COLO. – Valve-sparing root replacement has emerged as the procedure of choice in patients with isolated aortic root disease and a normally functioning aortic valve, according to Dr. Thoralf M. Sundt III.
"The valve-sparing root operations, in contrast to some of the other things we surgeons have come up with over the last decade or so, are increasing in popularity. They’re more and more commonly done, and that’s a good sign. I think the marketplace has spoken and this is clearly a good operation. It’s an operation that can be learned, and surgeons can do it with good results," he said at the Annual Cardiovascular Conference at Snowmass.
Valve-sparing root replacement (VSRR) spares a patient from the complications associated with lifelong anticoagulation for a mechanical valve, and the durability of VSRR appears to be superior to that of third-generation bioprostheses, the surgeon added.
"They’re holding up pretty well. The outcomes approach those with mechanical valves," said Dr. Sundt, chief of cardiac surgery at Massachusetts General Hospital and professor of surgery at Harvard Medical School, Boston.
Moreover, he continued, VSRR has another big advantage over bioprosthetic valves: "If you have to re-operate, it’s a whole lot more fun to do so on someone who’s had a VSRR and put a new biologic valve inside a native annulus than it is to try to take out that old bioprosthesis and put a new bioprosthesis in."
A meta-analysis of 11 studies comparing VSRR with total root replacement in patients with Marfan syndrome concluded that composite valve-related event rates for the two surgical strategies were not significantly different. The thromboembolic event rate was 0.3% per year in VSRR-treated patients, significantly lower than the still-quite-reasonable 0.7% per year rate after total root replacement (Heart 2011;97:955-8).
A recent study by surgeons at Stanford (Calif.) University gave VSRR a thumbs up regarding mid-term durability of outcomes through 6 years of follow-up, with a mean 2.9-year and maximum 6-year follow-up. The series included 75 patients with bicuspid aortic valve disease treated by VSRR.
Six-year actuarial survival was 99%, with 90% freedom from reoperation and no strokes. Thirty-one percent of patients had 2+ aortic regurgitation preoperatively; at echocardiographic follow-up a mean of 2.9 years post surgery, only a couple of patients had 2+ aortic regurgitation and no one was more severely affected. The Stanford investigators plan to update their results when follow-up reaches 10 years or more (J. Thorac. Cardiovasc. Surg. Dec. 20, 2012 [doi:10.1016/j.jtcvs.2012.11.043]).
The VSRR was developed by Dr. Tirone David of the University of Toronto. The procedure involves skeletonizing the root while preserving the leaflets and their attachments to the aortic wall. The aortic valve is then reimplanted inside a tubular Dacron graft, and then the coronary arteries are reimplanted.
"It’s probably the neatest development in terms of surgical options for the aortic valve in a long time," Dr. Sundt said.
He reported having no financial conflicts.
SNOWMASS, COLO. – Valve-sparing root replacement has emerged as the procedure of choice in patients with isolated aortic root disease and a normally functioning aortic valve, according to Dr. Thoralf M. Sundt III.
"The valve-sparing root operations, in contrast to some of the other things we surgeons have come up with over the last decade or so, are increasing in popularity. They’re more and more commonly done, and that’s a good sign. I think the marketplace has spoken and this is clearly a good operation. It’s an operation that can be learned, and surgeons can do it with good results," he said at the Annual Cardiovascular Conference at Snowmass.
Valve-sparing root replacement (VSRR) spares a patient from the complications associated with lifelong anticoagulation for a mechanical valve, and the durability of VSRR appears to be superior to that of third-generation bioprostheses, the surgeon added.
"They’re holding up pretty well. The outcomes approach those with mechanical valves," said Dr. Sundt, chief of cardiac surgery at Massachusetts General Hospital and professor of surgery at Harvard Medical School, Boston.
Moreover, he continued, VSRR has another big advantage over bioprosthetic valves: "If you have to re-operate, it’s a whole lot more fun to do so on someone who’s had a VSRR and put a new biologic valve inside a native annulus than it is to try to take out that old bioprosthesis and put a new bioprosthesis in."
A meta-analysis of 11 studies comparing VSRR with total root replacement in patients with Marfan syndrome concluded that composite valve-related event rates for the two surgical strategies were not significantly different. The thromboembolic event rate was 0.3% per year in VSRR-treated patients, significantly lower than the still-quite-reasonable 0.7% per year rate after total root replacement (Heart 2011;97:955-8).
A recent study by surgeons at Stanford (Calif.) University gave VSRR a thumbs up regarding mid-term durability of outcomes through 6 years of follow-up, with a mean 2.9-year and maximum 6-year follow-up. The series included 75 patients with bicuspid aortic valve disease treated by VSRR.
Six-year actuarial survival was 99%, with 90% freedom from reoperation and no strokes. Thirty-one percent of patients had 2+ aortic regurgitation preoperatively; at echocardiographic follow-up a mean of 2.9 years post surgery, only a couple of patients had 2+ aortic regurgitation and no one was more severely affected. The Stanford investigators plan to update their results when follow-up reaches 10 years or more (J. Thorac. Cardiovasc. Surg. Dec. 20, 2012 [doi:10.1016/j.jtcvs.2012.11.043]).
The VSRR was developed by Dr. Tirone David of the University of Toronto. The procedure involves skeletonizing the root while preserving the leaflets and their attachments to the aortic wall. The aortic valve is then reimplanted inside a tubular Dacron graft, and then the coronary arteries are reimplanted.
"It’s probably the neatest development in terms of surgical options for the aortic valve in a long time," Dr. Sundt said.
He reported having no financial conflicts.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
TAVR trial to assess alternative access sites
Two heart societies, a device maker, and two federal agencies have collaborated to develop a trial for transcatheter aortic valve replacement, once again extending the concept of teamwork, which is the cornerstone of this technology, far beyond the operating room walls.
During the past year, the Society of Thoracic Surgeons and the American College of Cardiology worked with the Food and Drug Administration, the Centers for Medicare and Medicaid Services (CMS), and Edwards Lifesciences to develop a trial that assesses the safety and efficacy of nontransfemoral approaches for TAVR, using the already-approved Edwards SAPIEN valves.
"What makes it unusual is, to the best of our knowledge, this is the first investigational device exemption [IDE] granted by the FDA to medical societies who operate national clinical registries," said ACC President Dr. William Zoghbi.
The societies will run the trial with funding from Edwards, and Medicare will pay for the procedures.
"This allows physicians to get reimbursed for off-label use," said Dr. Michael J. Mack, past president of STS and chair of the STS/ACC TVT (Transcatheter Valvular Therapy) Registry Steering Committee. "And it also allows for controlled off-label use, in which the outcomes can be captured and the sites can be paid while this information is being captured. People should be excited about it."
The goal of the trial is to expand the field and to extend TAVR to a broader group of patients, the societies said.
"A similar mechanism has been used in the past for the implantation of ICDs [implantable cardioverter-defibrillators] for patients who met particular criteria and get the funding as the registry moves forward," said Dr. Sidney Goldstein, professor of medicine at Wayne State University in Detroit, who is not involved in the trial or registry.
But currently, "the ICD Registry is not conducting an IDE to evaluate and reimburse for other possible indications of ICDs," said Dr. Zoghbi.
In the United States, an estimated one in four inoperable patients with severe aortic stenosis is not eligible for TAVR through a transfemoral or transapical approach because of vessel size, vessel disease, or other anatomical restrictions, according to the societies. Alternative routes, such as the transaortic approach, could provide an option for them.
STS and ACC are also working to get FDA approval for two more studies.
"The collaboration and use of registries for research in this pilot can be a model for specialty societies, industry, and federal regulators," Dr. Zoghbi said in a statement. "We have aligned our efforts to ensure patient access to a new technology in a safe and cost-effective way."
The study also stands out in the list of TAVR clinical trials approved by CMS, which began covering TAVR in May 2012: The other five are sponsored by Edwards or Medtronic.
The earlier collaboration of the entities that have developed this trial resulted in the STS/ACC TVT Registry, which captures TAVR-related patient demographics, procedure details, and facility and physician information.
The observational study is conducted in the TVT Registry, and will follow 1,000 patients. Any of the nearly 180 sites using the TVT Registry can participate in the study.
The trial will gather 30-day safety endpoints for patients who undergo alternative access approaches such as transapical and transaortic routes. The lumped data will then be compared with the 30-day outcomes of the transapical approach reported in Cohort A of the PARTNER trial.
Because the trial is covered by Medicare, it has to adhere to conditions set by the agency. The requirements will ensure better patient care, Dr. Jeffrey B. Rich, the STS immediate past president, said in a statement, because the "preoperative evaluation, interoperative deployment of the valve, and postoperative care must be jointly shared by cardiologists and cardiothoracic surgeons, utilizing the heart team approach."
Alternative access approaches in the trial include the left ventricular apex (transapical), ascending aorta, subclavian and axillary arteries, and distal aorta, as well as retroperitoneal access to the iliac artery.
The approaches have several advantages, according to the societies. For one, the risks associated with inserting large-caliber catheters into small, diseased femoral arteries are reduced. Also, nonfemoral access sites can provide for better catheter control and safer closure of the access site.
But since some of the alternative approaches, such as the transaortic approach, have not been approved, the operator training lags behind the already-approved transfemoral and transapical approaches. To address this, the societies and Edwards will probably have to create a contract to train the surgeons and cardiologists for the specific purpose of this trial, said Dr. Mack.
The alternative approaches also require additional equipment, and operators may be exposed to greater amounts of radiation. They may also lead to longer recovery and more incisional pain for patients, according to the societies.
Dr. Mack said that the trial will likely be completed in 6 months or less from its start date.
"Using registries for this kind of study has the potential to make new technology available in a timely manner while protecting patient safety," ACC Immediate Past President Dr. David Holmes said in a statement.
None of the physicians had relevant disclosures.
On Twitter @NaseemSMiller
Two heart societies, a device maker, and two federal agencies have collaborated to develop a trial for transcatheter aortic valve replacement, once again extending the concept of teamwork, which is the cornerstone of this technology, far beyond the operating room walls.
During the past year, the Society of Thoracic Surgeons and the American College of Cardiology worked with the Food and Drug Administration, the Centers for Medicare and Medicaid Services (CMS), and Edwards Lifesciences to develop a trial that assesses the safety and efficacy of nontransfemoral approaches for TAVR, using the already-approved Edwards SAPIEN valves.
"What makes it unusual is, to the best of our knowledge, this is the first investigational device exemption [IDE] granted by the FDA to medical societies who operate national clinical registries," said ACC President Dr. William Zoghbi.
The societies will run the trial with funding from Edwards, and Medicare will pay for the procedures.
"This allows physicians to get reimbursed for off-label use," said Dr. Michael J. Mack, past president of STS and chair of the STS/ACC TVT (Transcatheter Valvular Therapy) Registry Steering Committee. "And it also allows for controlled off-label use, in which the outcomes can be captured and the sites can be paid while this information is being captured. People should be excited about it."
The goal of the trial is to expand the field and to extend TAVR to a broader group of patients, the societies said.
"A similar mechanism has been used in the past for the implantation of ICDs [implantable cardioverter-defibrillators] for patients who met particular criteria and get the funding as the registry moves forward," said Dr. Sidney Goldstein, professor of medicine at Wayne State University in Detroit, who is not involved in the trial or registry.
But currently, "the ICD Registry is not conducting an IDE to evaluate and reimburse for other possible indications of ICDs," said Dr. Zoghbi.
In the United States, an estimated one in four inoperable patients with severe aortic stenosis is not eligible for TAVR through a transfemoral or transapical approach because of vessel size, vessel disease, or other anatomical restrictions, according to the societies. Alternative routes, such as the transaortic approach, could provide an option for them.
STS and ACC are also working to get FDA approval for two more studies.
"The collaboration and use of registries for research in this pilot can be a model for specialty societies, industry, and federal regulators," Dr. Zoghbi said in a statement. "We have aligned our efforts to ensure patient access to a new technology in a safe and cost-effective way."
The study also stands out in the list of TAVR clinical trials approved by CMS, which began covering TAVR in May 2012: The other five are sponsored by Edwards or Medtronic.
The earlier collaboration of the entities that have developed this trial resulted in the STS/ACC TVT Registry, which captures TAVR-related patient demographics, procedure details, and facility and physician information.
The observational study is conducted in the TVT Registry, and will follow 1,000 patients. Any of the nearly 180 sites using the TVT Registry can participate in the study.
The trial will gather 30-day safety endpoints for patients who undergo alternative access approaches such as transapical and transaortic routes. The lumped data will then be compared with the 30-day outcomes of the transapical approach reported in Cohort A of the PARTNER trial.
Because the trial is covered by Medicare, it has to adhere to conditions set by the agency. The requirements will ensure better patient care, Dr. Jeffrey B. Rich, the STS immediate past president, said in a statement, because the "preoperative evaluation, interoperative deployment of the valve, and postoperative care must be jointly shared by cardiologists and cardiothoracic surgeons, utilizing the heart team approach."
Alternative access approaches in the trial include the left ventricular apex (transapical), ascending aorta, subclavian and axillary arteries, and distal aorta, as well as retroperitoneal access to the iliac artery.
The approaches have several advantages, according to the societies. For one, the risks associated with inserting large-caliber catheters into small, diseased femoral arteries are reduced. Also, nonfemoral access sites can provide for better catheter control and safer closure of the access site.
But since some of the alternative approaches, such as the transaortic approach, have not been approved, the operator training lags behind the already-approved transfemoral and transapical approaches. To address this, the societies and Edwards will probably have to create a contract to train the surgeons and cardiologists for the specific purpose of this trial, said Dr. Mack.
The alternative approaches also require additional equipment, and operators may be exposed to greater amounts of radiation. They may also lead to longer recovery and more incisional pain for patients, according to the societies.
Dr. Mack said that the trial will likely be completed in 6 months or less from its start date.
"Using registries for this kind of study has the potential to make new technology available in a timely manner while protecting patient safety," ACC Immediate Past President Dr. David Holmes said in a statement.
None of the physicians had relevant disclosures.
On Twitter @NaseemSMiller
Two heart societies, a device maker, and two federal agencies have collaborated to develop a trial for transcatheter aortic valve replacement, once again extending the concept of teamwork, which is the cornerstone of this technology, far beyond the operating room walls.
During the past year, the Society of Thoracic Surgeons and the American College of Cardiology worked with the Food and Drug Administration, the Centers for Medicare and Medicaid Services (CMS), and Edwards Lifesciences to develop a trial that assesses the safety and efficacy of nontransfemoral approaches for TAVR, using the already-approved Edwards SAPIEN valves.
"What makes it unusual is, to the best of our knowledge, this is the first investigational device exemption [IDE] granted by the FDA to medical societies who operate national clinical registries," said ACC President Dr. William Zoghbi.
The societies will run the trial with funding from Edwards, and Medicare will pay for the procedures.
"This allows physicians to get reimbursed for off-label use," said Dr. Michael J. Mack, past president of STS and chair of the STS/ACC TVT (Transcatheter Valvular Therapy) Registry Steering Committee. "And it also allows for controlled off-label use, in which the outcomes can be captured and the sites can be paid while this information is being captured. People should be excited about it."
The goal of the trial is to expand the field and to extend TAVR to a broader group of patients, the societies said.
"A similar mechanism has been used in the past for the implantation of ICDs [implantable cardioverter-defibrillators] for patients who met particular criteria and get the funding as the registry moves forward," said Dr. Sidney Goldstein, professor of medicine at Wayne State University in Detroit, who is not involved in the trial or registry.
But currently, "the ICD Registry is not conducting an IDE to evaluate and reimburse for other possible indications of ICDs," said Dr. Zoghbi.
In the United States, an estimated one in four inoperable patients with severe aortic stenosis is not eligible for TAVR through a transfemoral or transapical approach because of vessel size, vessel disease, or other anatomical restrictions, according to the societies. Alternative routes, such as the transaortic approach, could provide an option for them.
STS and ACC are also working to get FDA approval for two more studies.
"The collaboration and use of registries for research in this pilot can be a model for specialty societies, industry, and federal regulators," Dr. Zoghbi said in a statement. "We have aligned our efforts to ensure patient access to a new technology in a safe and cost-effective way."
The study also stands out in the list of TAVR clinical trials approved by CMS, which began covering TAVR in May 2012: The other five are sponsored by Edwards or Medtronic.
The earlier collaboration of the entities that have developed this trial resulted in the STS/ACC TVT Registry, which captures TAVR-related patient demographics, procedure details, and facility and physician information.
The observational study is conducted in the TVT Registry, and will follow 1,000 patients. Any of the nearly 180 sites using the TVT Registry can participate in the study.
The trial will gather 30-day safety endpoints for patients who undergo alternative access approaches such as transapical and transaortic routes. The lumped data will then be compared with the 30-day outcomes of the transapical approach reported in Cohort A of the PARTNER trial.
Because the trial is covered by Medicare, it has to adhere to conditions set by the agency. The requirements will ensure better patient care, Dr. Jeffrey B. Rich, the STS immediate past president, said in a statement, because the "preoperative evaluation, interoperative deployment of the valve, and postoperative care must be jointly shared by cardiologists and cardiothoracic surgeons, utilizing the heart team approach."
Alternative access approaches in the trial include the left ventricular apex (transapical), ascending aorta, subclavian and axillary arteries, and distal aorta, as well as retroperitoneal access to the iliac artery.
The approaches have several advantages, according to the societies. For one, the risks associated with inserting large-caliber catheters into small, diseased femoral arteries are reduced. Also, nonfemoral access sites can provide for better catheter control and safer closure of the access site.
But since some of the alternative approaches, such as the transaortic approach, have not been approved, the operator training lags behind the already-approved transfemoral and transapical approaches. To address this, the societies and Edwards will probably have to create a contract to train the surgeons and cardiologists for the specific purpose of this trial, said Dr. Mack.
The alternative approaches also require additional equipment, and operators may be exposed to greater amounts of radiation. They may also lead to longer recovery and more incisional pain for patients, according to the societies.
Dr. Mack said that the trial will likely be completed in 6 months or less from its start date.
"Using registries for this kind of study has the potential to make new technology available in a timely manner while protecting patient safety," ACC Immediate Past President Dr. David Holmes said in a statement.
None of the physicians had relevant disclosures.
On Twitter @NaseemSMiller
No early cancer risk with donor lungs from heavy smokers
LOS ANGELES – Use of lungs from donors who smoked heavily does not worsen lung transplantation outcomes including risk for lung cancer death, at least in the medium term.
At a median follow-up of 2 years for 5,900 adults who had double-lung transplants, those who received lungs from heavy smokers had an actuarial median overall survival of roughly 5.5 years, and their lung function was essentially the same as that of patients who received lungs from other donors, Dr. Sharven Taghavi reported at the annual meeting of the Society of Thoracic Surgeons.
The study data came from the United Network for Organ Sharing (UNOS) database. A team led by Dr. Taghavi, of Temple University Hospital in Philadelphia, compared data for double-lung transplants from 2005-2011, comparing donors with a history of smoking exceeding 20 pack-years with other donors.
About 13% of the study patients received lungs from donors who had smoked heavily. Compared with other recipients, these recipients were more likely to have a primary diagnosis of chronic obstructive pulmonary disease and less likely to have a diagnosis of idiopathic pulmonary fibrosis. Otherwise, they were similar.
The rate of deaths due to cancer was based on case reports, as UNOS does not capture this outcome. Cancer deaths were 5.8% among recipients of lungs from heavy smokers and 3.6% among other recipients.
"There is a fairly low capture rate for this field, so it’s difficult to draw significant conclusions from it," cautioned Dr. Taghavi.
Patients who received lungs from heavy smokers had a 1-day longer length of stay in the hospital (18 days vs. 17 days), which "may not really be clinically relevant." Rates of acute rejection during hospitalization were comparable (10.7% vs. 8.8%), as was post-transplant airway dehiscence (1.8% vs. 1.8%).
Post-transplant peak forced expiratory volume in 1 second (FEV1) was the same (80% vs. 79%), as was decline in this measure over time. Median duration of freedom from bronchiolitis obliterans syndrome was 1,583 days vs. 1,827 days.
Risk-adjusted median all-cause survival – the study’s primary endpoint – did not differ significantly between the recipients given lungs from donors who smoked heavily and the other recipients (2,043 vs. 1,928 days).
The rate of cancer deaths did not differ significantly; however, the follow-up time is too short to address this concern in a meaningful way, Dr. Taghavi said.
"Currently, we recommend when evaluating a donor who has a heavy smoking history, that they undergo a thorough examination for lung tumors or evidence of cancer. This includes obtaining a chest x-ray, CT scans, and bronchoscopies. In addition, when the lungs are procured, they should undergo a very thorough visual inspection," he advised.
"Informed consent is very important. You have to discuss the donor’s smoking status with the recipient and explain the risks and the benefits," Dr. Taghavi said. Lung cancer risk, given the donor’s history, is about 1% to 2% annually, and that needs to be considered against the high likelihood of dying within 1 or 2 years without a transplant.
"One thing that is unquestionable is that survival will be better accepting these lungs than it will be sitting on a waiting list," he added. Only about half of the people listed for lung transplant in the United States each year actually undergo the surgery.
Recipients of lungs from heavy smokers do not need any extra follow-up or surveillance, as they are already diligently tested and monitored, according to Dr. Taghavi. The recipient’s immunosuppression does theoretically put one at additional risk for lung cancer.
Current guidelines of the International Society of Heart and Lung Transplantation advise against considering use of lungs from donors who have a smoking history of more than 20 pack-years, Dr. Taghavi noted. But he stopped short of saying that the study should prompt a formal revision of those guidelines.
"I think the findings start the conversation," he commented. "We should consider looking at these potential donors," especially when a recipient’s situation is dire.
Dr. Taghavi disclosed no conflicts of interest.
LOS ANGELES – Use of lungs from donors who smoked heavily does not worsen lung transplantation outcomes including risk for lung cancer death, at least in the medium term.
At a median follow-up of 2 years for 5,900 adults who had double-lung transplants, those who received lungs from heavy smokers had an actuarial median overall survival of roughly 5.5 years, and their lung function was essentially the same as that of patients who received lungs from other donors, Dr. Sharven Taghavi reported at the annual meeting of the Society of Thoracic Surgeons.
The study data came from the United Network for Organ Sharing (UNOS) database. A team led by Dr. Taghavi, of Temple University Hospital in Philadelphia, compared data for double-lung transplants from 2005-2011, comparing donors with a history of smoking exceeding 20 pack-years with other donors.
About 13% of the study patients received lungs from donors who had smoked heavily. Compared with other recipients, these recipients were more likely to have a primary diagnosis of chronic obstructive pulmonary disease and less likely to have a diagnosis of idiopathic pulmonary fibrosis. Otherwise, they were similar.
The rate of deaths due to cancer was based on case reports, as UNOS does not capture this outcome. Cancer deaths were 5.8% among recipients of lungs from heavy smokers and 3.6% among other recipients.
"There is a fairly low capture rate for this field, so it’s difficult to draw significant conclusions from it," cautioned Dr. Taghavi.
Patients who received lungs from heavy smokers had a 1-day longer length of stay in the hospital (18 days vs. 17 days), which "may not really be clinically relevant." Rates of acute rejection during hospitalization were comparable (10.7% vs. 8.8%), as was post-transplant airway dehiscence (1.8% vs. 1.8%).
Post-transplant peak forced expiratory volume in 1 second (FEV1) was the same (80% vs. 79%), as was decline in this measure over time. Median duration of freedom from bronchiolitis obliterans syndrome was 1,583 days vs. 1,827 days.
Risk-adjusted median all-cause survival – the study’s primary endpoint – did not differ significantly between the recipients given lungs from donors who smoked heavily and the other recipients (2,043 vs. 1,928 days).
The rate of cancer deaths did not differ significantly; however, the follow-up time is too short to address this concern in a meaningful way, Dr. Taghavi said.
"Currently, we recommend when evaluating a donor who has a heavy smoking history, that they undergo a thorough examination for lung tumors or evidence of cancer. This includes obtaining a chest x-ray, CT scans, and bronchoscopies. In addition, when the lungs are procured, they should undergo a very thorough visual inspection," he advised.
"Informed consent is very important. You have to discuss the donor’s smoking status with the recipient and explain the risks and the benefits," Dr. Taghavi said. Lung cancer risk, given the donor’s history, is about 1% to 2% annually, and that needs to be considered against the high likelihood of dying within 1 or 2 years without a transplant.
"One thing that is unquestionable is that survival will be better accepting these lungs than it will be sitting on a waiting list," he added. Only about half of the people listed for lung transplant in the United States each year actually undergo the surgery.
Recipients of lungs from heavy smokers do not need any extra follow-up or surveillance, as they are already diligently tested and monitored, according to Dr. Taghavi. The recipient’s immunosuppression does theoretically put one at additional risk for lung cancer.
Current guidelines of the International Society of Heart and Lung Transplantation advise against considering use of lungs from donors who have a smoking history of more than 20 pack-years, Dr. Taghavi noted. But he stopped short of saying that the study should prompt a formal revision of those guidelines.
"I think the findings start the conversation," he commented. "We should consider looking at these potential donors," especially when a recipient’s situation is dire.
Dr. Taghavi disclosed no conflicts of interest.
LOS ANGELES – Use of lungs from donors who smoked heavily does not worsen lung transplantation outcomes including risk for lung cancer death, at least in the medium term.
At a median follow-up of 2 years for 5,900 adults who had double-lung transplants, those who received lungs from heavy smokers had an actuarial median overall survival of roughly 5.5 years, and their lung function was essentially the same as that of patients who received lungs from other donors, Dr. Sharven Taghavi reported at the annual meeting of the Society of Thoracic Surgeons.
The study data came from the United Network for Organ Sharing (UNOS) database. A team led by Dr. Taghavi, of Temple University Hospital in Philadelphia, compared data for double-lung transplants from 2005-2011, comparing donors with a history of smoking exceeding 20 pack-years with other donors.
About 13% of the study patients received lungs from donors who had smoked heavily. Compared with other recipients, these recipients were more likely to have a primary diagnosis of chronic obstructive pulmonary disease and less likely to have a diagnosis of idiopathic pulmonary fibrosis. Otherwise, they were similar.
The rate of deaths due to cancer was based on case reports, as UNOS does not capture this outcome. Cancer deaths were 5.8% among recipients of lungs from heavy smokers and 3.6% among other recipients.
"There is a fairly low capture rate for this field, so it’s difficult to draw significant conclusions from it," cautioned Dr. Taghavi.
Patients who received lungs from heavy smokers had a 1-day longer length of stay in the hospital (18 days vs. 17 days), which "may not really be clinically relevant." Rates of acute rejection during hospitalization were comparable (10.7% vs. 8.8%), as was post-transplant airway dehiscence (1.8% vs. 1.8%).
Post-transplant peak forced expiratory volume in 1 second (FEV1) was the same (80% vs. 79%), as was decline in this measure over time. Median duration of freedom from bronchiolitis obliterans syndrome was 1,583 days vs. 1,827 days.
Risk-adjusted median all-cause survival – the study’s primary endpoint – did not differ significantly between the recipients given lungs from donors who smoked heavily and the other recipients (2,043 vs. 1,928 days).
The rate of cancer deaths did not differ significantly; however, the follow-up time is too short to address this concern in a meaningful way, Dr. Taghavi said.
"Currently, we recommend when evaluating a donor who has a heavy smoking history, that they undergo a thorough examination for lung tumors or evidence of cancer. This includes obtaining a chest x-ray, CT scans, and bronchoscopies. In addition, when the lungs are procured, they should undergo a very thorough visual inspection," he advised.
"Informed consent is very important. You have to discuss the donor’s smoking status with the recipient and explain the risks and the benefits," Dr. Taghavi said. Lung cancer risk, given the donor’s history, is about 1% to 2% annually, and that needs to be considered against the high likelihood of dying within 1 or 2 years without a transplant.
"One thing that is unquestionable is that survival will be better accepting these lungs than it will be sitting on a waiting list," he added. Only about half of the people listed for lung transplant in the United States each year actually undergo the surgery.
Recipients of lungs from heavy smokers do not need any extra follow-up or surveillance, as they are already diligently tested and monitored, according to Dr. Taghavi. The recipient’s immunosuppression does theoretically put one at additional risk for lung cancer.
Current guidelines of the International Society of Heart and Lung Transplantation advise against considering use of lungs from donors who have a smoking history of more than 20 pack-years, Dr. Taghavi noted. But he stopped short of saying that the study should prompt a formal revision of those guidelines.
"I think the findings start the conversation," he commented. "We should consider looking at these potential donors," especially when a recipient’s situation is dire.
Dr. Taghavi disclosed no conflicts of interest.
AT THE ANNUAL MEETING OF THE SOCIETY OF THROACIC SURGEONS
Major Finding: Risk-adjusted median all-cause survival did not differ significantly between patients given lungs from donors who smoked heavily and those receiving lungs from donors who did not smoke heavily (2,043 vs. 1,928 days).
Data Source: An observational cohort study of 5,900 adult primary double-lung transplant recipients in the UNOS database
Disclosures: Dr. Taghavi disclosed no relevant conflicts of interest.
Neurologic Improvements Possible in Neonatal ASO
FT. LAUDERDALE, FLA. – The use of full-flow cardiopulmonary bypass, coupled with neurological monitoring, improved cognitive and motor outcomes in a prospective neurologic outcome study of 97 neonates with transposition of the great arteries (both single- and two-ventricle lesions) who underwent an arterial switch operation.
The cohort study, conducted by Dr. Dean B. Andropoulos and his colleagues at the Texas Children’s Hospital in Houston, examined early MRI changes and longer-term neurodevelopmental outcomes after the arterial switch operation (ASO) was performed using a cardiopulmonary bypass (CPB) protocol that avoided deep hypothermic circulatory arrest (DHCA) and low-flow CPB.
The ASO was performed by using CPB with 150-mL/kg per min flows with no low-flow CPB or DHCA; pH stat management; hematocrit 30% or higher; and hypothermia to 24° -28° C. Regional oxygen saturation greater than 50% was maintained by using near infrared spectroscopic monitoring.
Neurologic assessment was performed using brain MRI performed immediately before the operation and 7 days postoperatively. The Bayley Scales of Infant and Toddler Development, Third Edition were used at 12 and 36 months (mean score of 100).
Dextrotransposition of the great arteries was present in 31 of the 97 enrolled patients. Ten of these 31 (32%) had preoperative MRI change, and 19 of 31 (61%) showed new postoperative MRI change, with 75% showing minimal new white matter injury, he said at the annual meeting of the Society of Thoracic Surgeons.
At 2 months, Bayley Scales were performed on 17 of the patients. Their mean cognitive score was 106.5, mean motor score was 90.4, and mean language score was 89.4. Twelve patients had Bayley III testing at 36 months, with a cognitive score of 106.5, motor score of 107.4, and language score of 98.2.
"Our series demonstrates a significant incidence of pre-existing MRI changes, and 61% have new postoperative changes, but all changes in this series were mild," said Dr. Andropoulos.
"At 12 months, the cognitive score of these children was above the population mean, but their motor and language performance was lower. By 36 months, language and motor scores had improved significantly. Thus, full-flow CPB coupled to cerebral monitoring may improve neurological outcomes."
Because of these results, "future studies of ASO patients should include short- and long-term neurodevelopmental studies," he said.
With greatly improved 30-day neonatal arterial switch operation mortality rates (for example, at the Texas Children’s Hospital in Houston there were no 30-day hospital mortalities for 175 ASOs since 2000), there are increasing expectations for better neurologic outcomes, according to Dr. Andropoulos, and such considerations are increasingly important.
Dr. Andropoulos reported having no financial conflicts.
FT. LAUDERDALE, FLA. – The use of full-flow cardiopulmonary bypass, coupled with neurological monitoring, improved cognitive and motor outcomes in a prospective neurologic outcome study of 97 neonates with transposition of the great arteries (both single- and two-ventricle lesions) who underwent an arterial switch operation.
The cohort study, conducted by Dr. Dean B. Andropoulos and his colleagues at the Texas Children’s Hospital in Houston, examined early MRI changes and longer-term neurodevelopmental outcomes after the arterial switch operation (ASO) was performed using a cardiopulmonary bypass (CPB) protocol that avoided deep hypothermic circulatory arrest (DHCA) and low-flow CPB.
The ASO was performed by using CPB with 150-mL/kg per min flows with no low-flow CPB or DHCA; pH stat management; hematocrit 30% or higher; and hypothermia to 24° -28° C. Regional oxygen saturation greater than 50% was maintained by using near infrared spectroscopic monitoring.
Neurologic assessment was performed using brain MRI performed immediately before the operation and 7 days postoperatively. The Bayley Scales of Infant and Toddler Development, Third Edition were used at 12 and 36 months (mean score of 100).
Dextrotransposition of the great arteries was present in 31 of the 97 enrolled patients. Ten of these 31 (32%) had preoperative MRI change, and 19 of 31 (61%) showed new postoperative MRI change, with 75% showing minimal new white matter injury, he said at the annual meeting of the Society of Thoracic Surgeons.
At 2 months, Bayley Scales were performed on 17 of the patients. Their mean cognitive score was 106.5, mean motor score was 90.4, and mean language score was 89.4. Twelve patients had Bayley III testing at 36 months, with a cognitive score of 106.5, motor score of 107.4, and language score of 98.2.
"Our series demonstrates a significant incidence of pre-existing MRI changes, and 61% have new postoperative changes, but all changes in this series were mild," said Dr. Andropoulos.
"At 12 months, the cognitive score of these children was above the population mean, but their motor and language performance was lower. By 36 months, language and motor scores had improved significantly. Thus, full-flow CPB coupled to cerebral monitoring may improve neurological outcomes."
Because of these results, "future studies of ASO patients should include short- and long-term neurodevelopmental studies," he said.
With greatly improved 30-day neonatal arterial switch operation mortality rates (for example, at the Texas Children’s Hospital in Houston there were no 30-day hospital mortalities for 175 ASOs since 2000), there are increasing expectations for better neurologic outcomes, according to Dr. Andropoulos, and such considerations are increasingly important.
Dr. Andropoulos reported having no financial conflicts.
FT. LAUDERDALE, FLA. – The use of full-flow cardiopulmonary bypass, coupled with neurological monitoring, improved cognitive and motor outcomes in a prospective neurologic outcome study of 97 neonates with transposition of the great arteries (both single- and two-ventricle lesions) who underwent an arterial switch operation.
The cohort study, conducted by Dr. Dean B. Andropoulos and his colleagues at the Texas Children’s Hospital in Houston, examined early MRI changes and longer-term neurodevelopmental outcomes after the arterial switch operation (ASO) was performed using a cardiopulmonary bypass (CPB) protocol that avoided deep hypothermic circulatory arrest (DHCA) and low-flow CPB.
The ASO was performed by using CPB with 150-mL/kg per min flows with no low-flow CPB or DHCA; pH stat management; hematocrit 30% or higher; and hypothermia to 24° -28° C. Regional oxygen saturation greater than 50% was maintained by using near infrared spectroscopic monitoring.
Neurologic assessment was performed using brain MRI performed immediately before the operation and 7 days postoperatively. The Bayley Scales of Infant and Toddler Development, Third Edition were used at 12 and 36 months (mean score of 100).
Dextrotransposition of the great arteries was present in 31 of the 97 enrolled patients. Ten of these 31 (32%) had preoperative MRI change, and 19 of 31 (61%) showed new postoperative MRI change, with 75% showing minimal new white matter injury, he said at the annual meeting of the Society of Thoracic Surgeons.
At 2 months, Bayley Scales were performed on 17 of the patients. Their mean cognitive score was 106.5, mean motor score was 90.4, and mean language score was 89.4. Twelve patients had Bayley III testing at 36 months, with a cognitive score of 106.5, motor score of 107.4, and language score of 98.2.
"Our series demonstrates a significant incidence of pre-existing MRI changes, and 61% have new postoperative changes, but all changes in this series were mild," said Dr. Andropoulos.
"At 12 months, the cognitive score of these children was above the population mean, but their motor and language performance was lower. By 36 months, language and motor scores had improved significantly. Thus, full-flow CPB coupled to cerebral monitoring may improve neurological outcomes."
Because of these results, "future studies of ASO patients should include short- and long-term neurodevelopmental studies," he said.
With greatly improved 30-day neonatal arterial switch operation mortality rates (for example, at the Texas Children’s Hospital in Houston there were no 30-day hospital mortalities for 175 ASOs since 2000), there are increasing expectations for better neurologic outcomes, according to Dr. Andropoulos, and such considerations are increasingly important.
Dr. Andropoulos reported having no financial conflicts.
FROM THE ANNUAL MEETING OF THE SOCIETY OF THORACIC SURGEONS
Major Finding: The series demonstrated a significant incidence of preexisting MRI changes, and 61% had new postoperative changes, but all changes in the series were deemed mild.
Data Source: A prospective cohort study was performed examining early MRI changes and longer-term neurodevelopmental outcomes in 97 neonates with transposition of the great arteries.
Disclosures: Dr. Andropoulos reported having no financial disclosures.
Poorer Outcomes Associated With Earlier VSD Repair
FT. LAUDERDALE, FLA – Early repair – within one week – of acquired ventral septal defect in patients with myocardial infarction was associated with a significantly higher mortality rate than was later repair in a retrospective review.
Acquired ventral septal defect (VSD), a relatively rare but devastating complication of myocardial infarction, frequently leads to cardiogenic shock and death. Surgical repair is generally required, although there is a high mortality.
To identify risk factors for poor patient outcomes, a study of the Society for Thoracic Surgeons National Database was performed to characterize patients undergoing post-MI VSD surgical repair, Dr. George J. Arnaoutakis said at the annual meeting of the Society of Thoracic Surgeons.
This retrospective review identified all adults (patients greater than 18 years of age) who underwent post-MI VSD repair between 1999 and 2010. The primary outcome measure was operative mortality and patients with congenital VSD were excluded.
"This largest to date study examining post-MI VSD repair was done in part to provide a surgical benchmark for future comparisons as percutaneous closure devices emerge to treat this condition," noted Dr. Arnaoutakis of the division of cardiac surgery at Johns Hopkins University, Baltimore.
The demographics of the 2,876 patients included in the study were a mean age of 68 years; 56.5% of the patients were men; and 7.5% of patients had prior coronary artery bypass grafting (CABG) surgery. Operative characteristics included preoperative support with an intraaortic balloon pump (65%); urgent status (35%); emergent status (49.7%); and concomitant CABG (63.9%).
Timing of surgery was found to be an important predictor of risk, with 54% mortality occurring in patients who had repair less than 7 days after MI, and 18% mortality in those patients who had their surgery greater than 7 days after MI. Multivariate analysis also showed that the timing of MI with relation to VSD repair was independently associated with operative mortality.
Overall, major morbidity and mortality was high, at nearly 77%. Other surgical characteristics significantly associated with higher mortality included longer cardiopulmonary bypass time, preoperative dialysis, emergent surgery, and shock.
"Ventricular septal rupture remains a devastating complication after myocardial infarction," he said, with a shorter time interval between MI and surgical repair of the VSD, being highly associated with operative mortality, Dr Arnaoutakis summarized.
He did point out that one flaw in this study based on the STS Database was that it could not account for patients who died while waiting for VSD repair, which might influence the results. In addition the overall incidence of acquired VSD was too low to determine the effect of individual surgeon or center volume on mortality rates.
Dr. Arnaoutakis agreed with audience suggestions that given the high overall mortality rate of surgical VSD closure, perhaps consideration of the new percutaneous closure devices and the possibility of ventricular assist device support might be reasonable options.
Dr. Arnaoutakis reported having no financial conflicts. Another researcher on the project reported research support from HeartWare International Inc. and Thoratec Corp.
FT. LAUDERDALE, FLA – Early repair – within one week – of acquired ventral septal defect in patients with myocardial infarction was associated with a significantly higher mortality rate than was later repair in a retrospective review.
Acquired ventral septal defect (VSD), a relatively rare but devastating complication of myocardial infarction, frequently leads to cardiogenic shock and death. Surgical repair is generally required, although there is a high mortality.
To identify risk factors for poor patient outcomes, a study of the Society for Thoracic Surgeons National Database was performed to characterize patients undergoing post-MI VSD surgical repair, Dr. George J. Arnaoutakis said at the annual meeting of the Society of Thoracic Surgeons.
This retrospective review identified all adults (patients greater than 18 years of age) who underwent post-MI VSD repair between 1999 and 2010. The primary outcome measure was operative mortality and patients with congenital VSD were excluded.
"This largest to date study examining post-MI VSD repair was done in part to provide a surgical benchmark for future comparisons as percutaneous closure devices emerge to treat this condition," noted Dr. Arnaoutakis of the division of cardiac surgery at Johns Hopkins University, Baltimore.
The demographics of the 2,876 patients included in the study were a mean age of 68 years; 56.5% of the patients were men; and 7.5% of patients had prior coronary artery bypass grafting (CABG) surgery. Operative characteristics included preoperative support with an intraaortic balloon pump (65%); urgent status (35%); emergent status (49.7%); and concomitant CABG (63.9%).
Timing of surgery was found to be an important predictor of risk, with 54% mortality occurring in patients who had repair less than 7 days after MI, and 18% mortality in those patients who had their surgery greater than 7 days after MI. Multivariate analysis also showed that the timing of MI with relation to VSD repair was independently associated with operative mortality.
Overall, major morbidity and mortality was high, at nearly 77%. Other surgical characteristics significantly associated with higher mortality included longer cardiopulmonary bypass time, preoperative dialysis, emergent surgery, and shock.
"Ventricular septal rupture remains a devastating complication after myocardial infarction," he said, with a shorter time interval between MI and surgical repair of the VSD, being highly associated with operative mortality, Dr Arnaoutakis summarized.
He did point out that one flaw in this study based on the STS Database was that it could not account for patients who died while waiting for VSD repair, which might influence the results. In addition the overall incidence of acquired VSD was too low to determine the effect of individual surgeon or center volume on mortality rates.
Dr. Arnaoutakis agreed with audience suggestions that given the high overall mortality rate of surgical VSD closure, perhaps consideration of the new percutaneous closure devices and the possibility of ventricular assist device support might be reasonable options.
Dr. Arnaoutakis reported having no financial conflicts. Another researcher on the project reported research support from HeartWare International Inc. and Thoratec Corp.
FT. LAUDERDALE, FLA – Early repair – within one week – of acquired ventral septal defect in patients with myocardial infarction was associated with a significantly higher mortality rate than was later repair in a retrospective review.
Acquired ventral septal defect (VSD), a relatively rare but devastating complication of myocardial infarction, frequently leads to cardiogenic shock and death. Surgical repair is generally required, although there is a high mortality.
To identify risk factors for poor patient outcomes, a study of the Society for Thoracic Surgeons National Database was performed to characterize patients undergoing post-MI VSD surgical repair, Dr. George J. Arnaoutakis said at the annual meeting of the Society of Thoracic Surgeons.
This retrospective review identified all adults (patients greater than 18 years of age) who underwent post-MI VSD repair between 1999 and 2010. The primary outcome measure was operative mortality and patients with congenital VSD were excluded.
"This largest to date study examining post-MI VSD repair was done in part to provide a surgical benchmark for future comparisons as percutaneous closure devices emerge to treat this condition," noted Dr. Arnaoutakis of the division of cardiac surgery at Johns Hopkins University, Baltimore.
The demographics of the 2,876 patients included in the study were a mean age of 68 years; 56.5% of the patients were men; and 7.5% of patients had prior coronary artery bypass grafting (CABG) surgery. Operative characteristics included preoperative support with an intraaortic balloon pump (65%); urgent status (35%); emergent status (49.7%); and concomitant CABG (63.9%).
Timing of surgery was found to be an important predictor of risk, with 54% mortality occurring in patients who had repair less than 7 days after MI, and 18% mortality in those patients who had their surgery greater than 7 days after MI. Multivariate analysis also showed that the timing of MI with relation to VSD repair was independently associated with operative mortality.
Overall, major morbidity and mortality was high, at nearly 77%. Other surgical characteristics significantly associated with higher mortality included longer cardiopulmonary bypass time, preoperative dialysis, emergent surgery, and shock.
"Ventricular septal rupture remains a devastating complication after myocardial infarction," he said, with a shorter time interval between MI and surgical repair of the VSD, being highly associated with operative mortality, Dr Arnaoutakis summarized.
He did point out that one flaw in this study based on the STS Database was that it could not account for patients who died while waiting for VSD repair, which might influence the results. In addition the overall incidence of acquired VSD was too low to determine the effect of individual surgeon or center volume on mortality rates.
Dr. Arnaoutakis agreed with audience suggestions that given the high overall mortality rate of surgical VSD closure, perhaps consideration of the new percutaneous closure devices and the possibility of ventricular assist device support might be reasonable options.
Dr. Arnaoutakis reported having no financial conflicts. Another researcher on the project reported research support from HeartWare International Inc. and Thoratec Corp.
FROM THE ANNUAL MEETING OF THE SOCIETY OF THORACIC SURGEONS
Major Finding: Mortality was 54% in patients who had repair less than 7 days after MI, and 18% in those who had their surgery more than 7 days after MI.
Data Source: The study was a retrospective review of 2,876 patients in the STS National Database.
Disclosures: Dr. Arnaoutakis reported having no financial disclosures. Another researcher on the project reported research support from HeartWare International and Thoratec Corp.
Hepatitis E Screening Advised for Transplant Recipients
SAN FRANCISCO – Hepatitis E is an uncommon but often serious infection in immunosuppressed heart transplant recipients that warrants routine screening, according to investigators at Erasmus University Medical Center in Rotterdam, the Netherlands.
In a study of 263 recipients, 3% were found to have become infected with hepatitis E, most with symptomatic chronic disease. The infections ranged in severity from mild, transient viremia to severe and possibly progressive hepatitis with marked steatosis on liver biopsy.
"Chronic hepatitis E virus infection can have serious consequences in this group of patients," Dr. Annemiek A. van der Eijk said in presenting the findings at the annual meeting of the American Association for the Study of Liver Diseases (AASLD). "We advise systematic hepatitis E virus RNA screening in solid organ transplant recipients. In cases in which liver enzymes are increased, additional hepatitis E virus screening should be implemented."
"Chronic hepatitis E virus infection ... is a treatable disease," she added. Some patients were able to clear the virus when their immunosuppressants were tapered, but doing so also sometimes triggered rejection, which necessitated a resumption of therapy. "In our center, we are now treating patients with ribavirin (Copegus, Rebetol), but there are no large, randomized, controlled trials about the dose and duration of therapy."
"We advise systematic hepatitis E virus RNA screening in solid organ transplant recipients."
Importantly, she stressed, physicians should include hepatitis E infection in the differential diagnosis when transplant recipients have signs and symptoms of liver dysfunction, as it could be mistaken for a variety of other conditions having distinctly different treatments.
Chronicity "is not something we often associate with hepatitis E; it really doesn’t cause chronic infection like hepatitis B or C. But in this kind of immunosuppressed situation, it could," commented Dr. T. Jake Liang, president of the AASLD and chief of the Liver Diseases Branch at the National Institute of Diabetes and Digestive and Kidney Diseases.
"This [study] makes us aware of another cause of chronic liver disease, especially in people who are immunosuppressed, or receiving chemotherapy, or undergoing transplantation with lifelong immunosuppression," he said in a press conference.
Hepatitis E is transmitted mainly by the fecal-oral route (especially through contaminated water) but it can also be acquired by consuming raw or undercooked meat, through parenteral and vertical transmission, and – rarely – by person-to-person contact.
Swine are known to carry the virus. "In the Netherlands, more than 50% of the pig population is infected with hepatitis E virus, and 7% of the livers sold in supermarkets are hepatitis E virus RNA positive," Dr. van der Eijk noted.
Infection is especially worrisome in immunocompromised patients, as they can develop persistent elevation of liver enzymes and chronic hepatitis, with some reports also suggesting the possibility of rapid progression to cirrhosis.
In a cross-sectional study, the investigators tested serum samples from orthotopic heart transplant recipients at the center who were alive in 2010 and 2011 and had banked serum. The patients were receiving tacrolimus (Prograf)- and prednisolone-based immunosuppression.
Samples were tested by both polymerase chain reaction (PCR) for viral RNA – which was used to define infection – and serologic assays for antibodies to the virus. "We decided to screen all of our patients with PCR because we know serology outcomes differ greatly between the different tests used," Dr. van der Eijk explained.
Overall, 7 of the 263 patients studied were found to be infected with hepatitis E virus, for a point prevalence of 3%, and six of them had chronic infection (defined as PCR positivity for more than 6 months). The six men and one woman had a median age of 53 years. Retrospective serum testing showed that the time between transplantation and infection was a median of 8 years, but it ranged widely, from 1 to 20 years.
Viral genotyping showed that all of the patients were infected with genotype 3, which is associated with sporadic cases of hepatitis E in Western countries unrelated to travel and is likely of swine origin. Phylogenetic testing showed no evidence that the infections shared a common source or were acquired nosocomially.
Only two patients had virus-specific IgM antibodies at the time of initial PCR-detected infection and, on average, the PCR became positive 143 days before IgM antibodies were detectable. Thus, "PCR is superior [to serology] to detect infection in immunocompromised patients," Dr. van der Eijk commented.
The patients with chronic infection had elevations to varying extents of alanine aminotransferase levels, gamma-glutamyl transferase levels, or both. On liver biopsy, their Histologic Activity Index scores also ranged considerably, but three patients had scores of 10, indicating moderate disease, with features such as hepatocyte degeneration and fibrosis.
Although all of the patients with chronic hepatitis E had fecal shedding of the virus, none of their spouses was found to be infected on either serologic or PCR testing.
Dr. van der Eijk and Dr. Liang reported that they had no relevant conflicts of interest.
SAN FRANCISCO – Hepatitis E is an uncommon but often serious infection in immunosuppressed heart transplant recipients that warrants routine screening, according to investigators at Erasmus University Medical Center in Rotterdam, the Netherlands.
In a study of 263 recipients, 3% were found to have become infected with hepatitis E, most with symptomatic chronic disease. The infections ranged in severity from mild, transient viremia to severe and possibly progressive hepatitis with marked steatosis on liver biopsy.
"Chronic hepatitis E virus infection can have serious consequences in this group of patients," Dr. Annemiek A. van der Eijk said in presenting the findings at the annual meeting of the American Association for the Study of Liver Diseases (AASLD). "We advise systematic hepatitis E virus RNA screening in solid organ transplant recipients. In cases in which liver enzymes are increased, additional hepatitis E virus screening should be implemented."
"Chronic hepatitis E virus infection ... is a treatable disease," she added. Some patients were able to clear the virus when their immunosuppressants were tapered, but doing so also sometimes triggered rejection, which necessitated a resumption of therapy. "In our center, we are now treating patients with ribavirin (Copegus, Rebetol), but there are no large, randomized, controlled trials about the dose and duration of therapy."
"We advise systematic hepatitis E virus RNA screening in solid organ transplant recipients."
Importantly, she stressed, physicians should include hepatitis E infection in the differential diagnosis when transplant recipients have signs and symptoms of liver dysfunction, as it could be mistaken for a variety of other conditions having distinctly different treatments.
Chronicity "is not something we often associate with hepatitis E; it really doesn’t cause chronic infection like hepatitis B or C. But in this kind of immunosuppressed situation, it could," commented Dr. T. Jake Liang, president of the AASLD and chief of the Liver Diseases Branch at the National Institute of Diabetes and Digestive and Kidney Diseases.
"This [study] makes us aware of another cause of chronic liver disease, especially in people who are immunosuppressed, or receiving chemotherapy, or undergoing transplantation with lifelong immunosuppression," he said in a press conference.
Hepatitis E is transmitted mainly by the fecal-oral route (especially through contaminated water) but it can also be acquired by consuming raw or undercooked meat, through parenteral and vertical transmission, and – rarely – by person-to-person contact.
Swine are known to carry the virus. "In the Netherlands, more than 50% of the pig population is infected with hepatitis E virus, and 7% of the livers sold in supermarkets are hepatitis E virus RNA positive," Dr. van der Eijk noted.
Infection is especially worrisome in immunocompromised patients, as they can develop persistent elevation of liver enzymes and chronic hepatitis, with some reports also suggesting the possibility of rapid progression to cirrhosis.
In a cross-sectional study, the investigators tested serum samples from orthotopic heart transplant recipients at the center who were alive in 2010 and 2011 and had banked serum. The patients were receiving tacrolimus (Prograf)- and prednisolone-based immunosuppression.
Samples were tested by both polymerase chain reaction (PCR) for viral RNA – which was used to define infection – and serologic assays for antibodies to the virus. "We decided to screen all of our patients with PCR because we know serology outcomes differ greatly between the different tests used," Dr. van der Eijk explained.
Overall, 7 of the 263 patients studied were found to be infected with hepatitis E virus, for a point prevalence of 3%, and six of them had chronic infection (defined as PCR positivity for more than 6 months). The six men and one woman had a median age of 53 years. Retrospective serum testing showed that the time between transplantation and infection was a median of 8 years, but it ranged widely, from 1 to 20 years.
Viral genotyping showed that all of the patients were infected with genotype 3, which is associated with sporadic cases of hepatitis E in Western countries unrelated to travel and is likely of swine origin. Phylogenetic testing showed no evidence that the infections shared a common source or were acquired nosocomially.
Only two patients had virus-specific IgM antibodies at the time of initial PCR-detected infection and, on average, the PCR became positive 143 days before IgM antibodies were detectable. Thus, "PCR is superior [to serology] to detect infection in immunocompromised patients," Dr. van der Eijk commented.
The patients with chronic infection had elevations to varying extents of alanine aminotransferase levels, gamma-glutamyl transferase levels, or both. On liver biopsy, their Histologic Activity Index scores also ranged considerably, but three patients had scores of 10, indicating moderate disease, with features such as hepatocyte degeneration and fibrosis.
Although all of the patients with chronic hepatitis E had fecal shedding of the virus, none of their spouses was found to be infected on either serologic or PCR testing.
Dr. van der Eijk and Dr. Liang reported that they had no relevant conflicts of interest.
SAN FRANCISCO – Hepatitis E is an uncommon but often serious infection in immunosuppressed heart transplant recipients that warrants routine screening, according to investigators at Erasmus University Medical Center in Rotterdam, the Netherlands.
In a study of 263 recipients, 3% were found to have become infected with hepatitis E, most with symptomatic chronic disease. The infections ranged in severity from mild, transient viremia to severe and possibly progressive hepatitis with marked steatosis on liver biopsy.
"Chronic hepatitis E virus infection can have serious consequences in this group of patients," Dr. Annemiek A. van der Eijk said in presenting the findings at the annual meeting of the American Association for the Study of Liver Diseases (AASLD). "We advise systematic hepatitis E virus RNA screening in solid organ transplant recipients. In cases in which liver enzymes are increased, additional hepatitis E virus screening should be implemented."
"Chronic hepatitis E virus infection ... is a treatable disease," she added. Some patients were able to clear the virus when their immunosuppressants were tapered, but doing so also sometimes triggered rejection, which necessitated a resumption of therapy. "In our center, we are now treating patients with ribavirin (Copegus, Rebetol), but there are no large, randomized, controlled trials about the dose and duration of therapy."
"We advise systematic hepatitis E virus RNA screening in solid organ transplant recipients."
Importantly, she stressed, physicians should include hepatitis E infection in the differential diagnosis when transplant recipients have signs and symptoms of liver dysfunction, as it could be mistaken for a variety of other conditions having distinctly different treatments.
Chronicity "is not something we often associate with hepatitis E; it really doesn’t cause chronic infection like hepatitis B or C. But in this kind of immunosuppressed situation, it could," commented Dr. T. Jake Liang, president of the AASLD and chief of the Liver Diseases Branch at the National Institute of Diabetes and Digestive and Kidney Diseases.
"This [study] makes us aware of another cause of chronic liver disease, especially in people who are immunosuppressed, or receiving chemotherapy, or undergoing transplantation with lifelong immunosuppression," he said in a press conference.
Hepatitis E is transmitted mainly by the fecal-oral route (especially through contaminated water) but it can also be acquired by consuming raw or undercooked meat, through parenteral and vertical transmission, and – rarely – by person-to-person contact.
Swine are known to carry the virus. "In the Netherlands, more than 50% of the pig population is infected with hepatitis E virus, and 7% of the livers sold in supermarkets are hepatitis E virus RNA positive," Dr. van der Eijk noted.
Infection is especially worrisome in immunocompromised patients, as they can develop persistent elevation of liver enzymes and chronic hepatitis, with some reports also suggesting the possibility of rapid progression to cirrhosis.
In a cross-sectional study, the investigators tested serum samples from orthotopic heart transplant recipients at the center who were alive in 2010 and 2011 and had banked serum. The patients were receiving tacrolimus (Prograf)- and prednisolone-based immunosuppression.
Samples were tested by both polymerase chain reaction (PCR) for viral RNA – which was used to define infection – and serologic assays for antibodies to the virus. "We decided to screen all of our patients with PCR because we know serology outcomes differ greatly between the different tests used," Dr. van der Eijk explained.
Overall, 7 of the 263 patients studied were found to be infected with hepatitis E virus, for a point prevalence of 3%, and six of them had chronic infection (defined as PCR positivity for more than 6 months). The six men and one woman had a median age of 53 years. Retrospective serum testing showed that the time between transplantation and infection was a median of 8 years, but it ranged widely, from 1 to 20 years.
Viral genotyping showed that all of the patients were infected with genotype 3, which is associated with sporadic cases of hepatitis E in Western countries unrelated to travel and is likely of swine origin. Phylogenetic testing showed no evidence that the infections shared a common source or were acquired nosocomially.
Only two patients had virus-specific IgM antibodies at the time of initial PCR-detected infection and, on average, the PCR became positive 143 days before IgM antibodies were detectable. Thus, "PCR is superior [to serology] to detect infection in immunocompromised patients," Dr. van der Eijk commented.
The patients with chronic infection had elevations to varying extents of alanine aminotransferase levels, gamma-glutamyl transferase levels, or both. On liver biopsy, their Histologic Activity Index scores also ranged considerably, but three patients had scores of 10, indicating moderate disease, with features such as hepatocyte degeneration and fibrosis.
Although all of the patients with chronic hepatitis E had fecal shedding of the virus, none of their spouses was found to be infected on either serologic or PCR testing.
Dr. van der Eijk and Dr. Liang reported that they had no relevant conflicts of interest.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THE STUDY OF LIVER DISEASES
Major Finding: In all, 3% of patients were found to have acquired hepatitis E. Most had symptomatic chronic infection.
Data Source: A cross-sectional study of 263 heart transplant recipients.
Disclosures: Dr. van der Eijk and Dr. Liang reported that they had no relevant conflicts of interest.
New-Onset AF Seen in One-Third of TAVI Patients
New-onset atrial fibrillation, or NOAF, occurred in nearly a third of 138 patients who underwent transcatheter aortic valve implantation in a prospective study, and the condition was associated with a significantly higher rate of cardioembolic events at 30-day and 12-month follow-up.
NOAF occurred in 44 patients at a median of 48 hours after transcatheter aortic valve implantation (TAVI), with 10 episodes resolving spontaneously within 12 hours, and 34 episodes requiring pharmacologic intervention. The rate of the combined end point of stroke and systemic embolism was 13.6% at 30 days in the NOAF group, compared with 3.2% in those who did not experience NOAF (odds ratio, 4.79); the rate was 15.9% vs. 3.2% at 12 months (OR, 5.0), Dr. Ignacio J. Amat-Santos of Laval University, Quebec City, and his colleagues reported online on Dec. 14 the Journal of the American College of Cardiology.
Significant independent predictors of NOAF included left atrial size (OR of 1.21/each increase of 1 mm/m2) and use of the transapical approach (OR, 4.08). An atrial size of 27 mm/m2 or greater as measured by echocardiography was identified as the cutoff point with the best sensitivity and specificity for predicting NOAF within 30 days of TAVI, the investigators said (J. Am. Coll. Cardiol. 2011 [doi:10/1016/j.jacc.2011.09.061]).
Furthermore, the incidence of NOAF in those with an atrial size of 27 mm/m2 or greater undergoing TAVI by the transapical approach vs. the transfemoral approach was 57% vs. 12%, respectively, they noted.
Mortality, which was 16% and 21% in those with and without NOAF at 12 months, respectively, did not differ significantly between the groups at either follow-up, they noted.
Patients in the study had severe symptomatic aortic stenosis, but no history of chronic/paroxysmal atrial fibrillation. They underwent TAVI with a balloon-expandable valve by either the transapical or transfemoral approach, were enrolled consecutively between May 2007 and May 2011, and underwent continuous electrocardiographic monitoring during hospitalization. NOAF was defined as any episode of AF lasting longer than 30 seconds.
NOAF is a known complication in patients undergoing cardiovascular interventions, but this is one of the first studies to verify an increased risk of the condition in patients undergoing TAVI, which has emerged as an alternative treatment for patients with severe symptomatic aortic stenosis and high or prohibitive operative risk. The study is also among the first to characterize predictive factors for NOAF.
"The occurrence of cerebrovascular events is probably the most worrisome complication associated with TAVI, with an incidence of about 4%, one of the highest ever reported in the field of interventional cardiology," the investigators said, noting that the fact that more than 50% of the complications occur several days after TAVI suggests that "mechanisms other than those directly related to the procedure may be involved."
Indeed, the findings of this study suggest NOAF may be an important mechanism for late neurological events after TAVI, and if confirmed in larger studies, the findings may have implications for the development of prevention trials.
"Knowing the predictive factors of NOAF following TAVI should allow us to select the patients at higher risk for NOAF preventive studies in the setting of TAVI," they investigators said.
Also of note, some of the cardioembolic events in this study seemed to be related to the non-initiation of anticoagulant therapy, the investigators said, adding that the risk of a cardioembolic event was as high as 40% in those who had NOAF and who did not receive anticoagulant therapy.
This underscores the clinical relevance of optimizing antithrombotic treatment in this high-risk subset of patients, they concluded.
Dr. Amat-Santos disclosed that he received support from the Institute of Heart Sciences. Other authors disclosed having served as consultants for Edwards Lifesciences, and/or St. Jude Medical.
The research by Dr. Amat-Santos and his colleagues deserves attention because of its originality and because of its potential implications for managing TAVI patients, according to Dr. Bernard Iung, Dr. Dominique Himbert, and Dr. Alex Vahanian.
In an accompanying editorial, they note that besides frequency and predictive factors of NOAF in patients who undergo TAVI, one of the most clinically relevant issues addressed by the study is the assessment of its impact following the procedure. While the findings should be interpreted with caution given the small number of embolic events, they represent a "relevant contribution in the analysis of the potential causes of embolic events after TAVI," they said (J. Am. Coll. Cardiol. 2012 [doi:10.1016/j.jacc2011.11.005]).
"Despite the number of mechanisms that may be involved in stroke after TAVI, the particularly strong relationship between post-procedural AF and stroke occurring after 24 h suggests that a cardioembolic origin significantly contributes to stroke after TAVI," they added, noting that the association raises questions about the most appropriate post-procedure antithrombotic therapy, and highlights the need for larger randomized trials to optimize antithrombotic therapy in TAVI patients.
The association also highlights the need for improving the identification of patients at risk, and testing pharmacological approaches to reducing atrial fibrillation incidence, they concluded.
Dr. Iung, Dr. Himbert, and Dr. Vahanian are with Bichat Hospital, Paris. Dr. Iung disclosed that he has received consulting fees from Servier, Boehringer Ingelheim, Bayer, Valtech, and Abbott, as well as speakers fees from Edwards Lifesciences, St. Jude Medical, and Sanofi-Aventis. Dr. Himbert disclosed receiving proctoring fees from Edwards Lifesciences and Medtronic. Dr. Vahanian disclosed serving as an advisory board member for Medtronic, Abbott, Valtech, and Boehringer Ingelheim, and receiving speakers fees from Edwards Lifesciences and Siemens.
The research by Dr. Amat-Santos and his colleagues deserves attention because of its originality and because of its potential implications for managing TAVI patients, according to Dr. Bernard Iung, Dr. Dominique Himbert, and Dr. Alex Vahanian.
In an accompanying editorial, they note that besides frequency and predictive factors of NOAF in patients who undergo TAVI, one of the most clinically relevant issues addressed by the study is the assessment of its impact following the procedure. While the findings should be interpreted with caution given the small number of embolic events, they represent a "relevant contribution in the analysis of the potential causes of embolic events after TAVI," they said (J. Am. Coll. Cardiol. 2012 [doi:10.1016/j.jacc2011.11.005]).
"Despite the number of mechanisms that may be involved in stroke after TAVI, the particularly strong relationship between post-procedural AF and stroke occurring after 24 h suggests that a cardioembolic origin significantly contributes to stroke after TAVI," they added, noting that the association raises questions about the most appropriate post-procedure antithrombotic therapy, and highlights the need for larger randomized trials to optimize antithrombotic therapy in TAVI patients.
The association also highlights the need for improving the identification of patients at risk, and testing pharmacological approaches to reducing atrial fibrillation incidence, they concluded.
Dr. Iung, Dr. Himbert, and Dr. Vahanian are with Bichat Hospital, Paris. Dr. Iung disclosed that he has received consulting fees from Servier, Boehringer Ingelheim, Bayer, Valtech, and Abbott, as well as speakers fees from Edwards Lifesciences, St. Jude Medical, and Sanofi-Aventis. Dr. Himbert disclosed receiving proctoring fees from Edwards Lifesciences and Medtronic. Dr. Vahanian disclosed serving as an advisory board member for Medtronic, Abbott, Valtech, and Boehringer Ingelheim, and receiving speakers fees from Edwards Lifesciences and Siemens.
The research by Dr. Amat-Santos and his colleagues deserves attention because of its originality and because of its potential implications for managing TAVI patients, according to Dr. Bernard Iung, Dr. Dominique Himbert, and Dr. Alex Vahanian.
In an accompanying editorial, they note that besides frequency and predictive factors of NOAF in patients who undergo TAVI, one of the most clinically relevant issues addressed by the study is the assessment of its impact following the procedure. While the findings should be interpreted with caution given the small number of embolic events, they represent a "relevant contribution in the analysis of the potential causes of embolic events after TAVI," they said (J. Am. Coll. Cardiol. 2012 [doi:10.1016/j.jacc2011.11.005]).
"Despite the number of mechanisms that may be involved in stroke after TAVI, the particularly strong relationship between post-procedural AF and stroke occurring after 24 h suggests that a cardioembolic origin significantly contributes to stroke after TAVI," they added, noting that the association raises questions about the most appropriate post-procedure antithrombotic therapy, and highlights the need for larger randomized trials to optimize antithrombotic therapy in TAVI patients.
The association also highlights the need for improving the identification of patients at risk, and testing pharmacological approaches to reducing atrial fibrillation incidence, they concluded.
Dr. Iung, Dr. Himbert, and Dr. Vahanian are with Bichat Hospital, Paris. Dr. Iung disclosed that he has received consulting fees from Servier, Boehringer Ingelheim, Bayer, Valtech, and Abbott, as well as speakers fees from Edwards Lifesciences, St. Jude Medical, and Sanofi-Aventis. Dr. Himbert disclosed receiving proctoring fees from Edwards Lifesciences and Medtronic. Dr. Vahanian disclosed serving as an advisory board member for Medtronic, Abbott, Valtech, and Boehringer Ingelheim, and receiving speakers fees from Edwards Lifesciences and Siemens.
New-onset atrial fibrillation, or NOAF, occurred in nearly a third of 138 patients who underwent transcatheter aortic valve implantation in a prospective study, and the condition was associated with a significantly higher rate of cardioembolic events at 30-day and 12-month follow-up.
NOAF occurred in 44 patients at a median of 48 hours after transcatheter aortic valve implantation (TAVI), with 10 episodes resolving spontaneously within 12 hours, and 34 episodes requiring pharmacologic intervention. The rate of the combined end point of stroke and systemic embolism was 13.6% at 30 days in the NOAF group, compared with 3.2% in those who did not experience NOAF (odds ratio, 4.79); the rate was 15.9% vs. 3.2% at 12 months (OR, 5.0), Dr. Ignacio J. Amat-Santos of Laval University, Quebec City, and his colleagues reported online on Dec. 14 the Journal of the American College of Cardiology.
Significant independent predictors of NOAF included left atrial size (OR of 1.21/each increase of 1 mm/m2) and use of the transapical approach (OR, 4.08). An atrial size of 27 mm/m2 or greater as measured by echocardiography was identified as the cutoff point with the best sensitivity and specificity for predicting NOAF within 30 days of TAVI, the investigators said (J. Am. Coll. Cardiol. 2011 [doi:10/1016/j.jacc.2011.09.061]).
Furthermore, the incidence of NOAF in those with an atrial size of 27 mm/m2 or greater undergoing TAVI by the transapical approach vs. the transfemoral approach was 57% vs. 12%, respectively, they noted.
Mortality, which was 16% and 21% in those with and without NOAF at 12 months, respectively, did not differ significantly between the groups at either follow-up, they noted.
Patients in the study had severe symptomatic aortic stenosis, but no history of chronic/paroxysmal atrial fibrillation. They underwent TAVI with a balloon-expandable valve by either the transapical or transfemoral approach, were enrolled consecutively between May 2007 and May 2011, and underwent continuous electrocardiographic monitoring during hospitalization. NOAF was defined as any episode of AF lasting longer than 30 seconds.
NOAF is a known complication in patients undergoing cardiovascular interventions, but this is one of the first studies to verify an increased risk of the condition in patients undergoing TAVI, which has emerged as an alternative treatment for patients with severe symptomatic aortic stenosis and high or prohibitive operative risk. The study is also among the first to characterize predictive factors for NOAF.
"The occurrence of cerebrovascular events is probably the most worrisome complication associated with TAVI, with an incidence of about 4%, one of the highest ever reported in the field of interventional cardiology," the investigators said, noting that the fact that more than 50% of the complications occur several days after TAVI suggests that "mechanisms other than those directly related to the procedure may be involved."
Indeed, the findings of this study suggest NOAF may be an important mechanism for late neurological events after TAVI, and if confirmed in larger studies, the findings may have implications for the development of prevention trials.
"Knowing the predictive factors of NOAF following TAVI should allow us to select the patients at higher risk for NOAF preventive studies in the setting of TAVI," they investigators said.
Also of note, some of the cardioembolic events in this study seemed to be related to the non-initiation of anticoagulant therapy, the investigators said, adding that the risk of a cardioembolic event was as high as 40% in those who had NOAF and who did not receive anticoagulant therapy.
This underscores the clinical relevance of optimizing antithrombotic treatment in this high-risk subset of patients, they concluded.
Dr. Amat-Santos disclosed that he received support from the Institute of Heart Sciences. Other authors disclosed having served as consultants for Edwards Lifesciences, and/or St. Jude Medical.
New-onset atrial fibrillation, or NOAF, occurred in nearly a third of 138 patients who underwent transcatheter aortic valve implantation in a prospective study, and the condition was associated with a significantly higher rate of cardioembolic events at 30-day and 12-month follow-up.
NOAF occurred in 44 patients at a median of 48 hours after transcatheter aortic valve implantation (TAVI), with 10 episodes resolving spontaneously within 12 hours, and 34 episodes requiring pharmacologic intervention. The rate of the combined end point of stroke and systemic embolism was 13.6% at 30 days in the NOAF group, compared with 3.2% in those who did not experience NOAF (odds ratio, 4.79); the rate was 15.9% vs. 3.2% at 12 months (OR, 5.0), Dr. Ignacio J. Amat-Santos of Laval University, Quebec City, and his colleagues reported online on Dec. 14 the Journal of the American College of Cardiology.
Significant independent predictors of NOAF included left atrial size (OR of 1.21/each increase of 1 mm/m2) and use of the transapical approach (OR, 4.08). An atrial size of 27 mm/m2 or greater as measured by echocardiography was identified as the cutoff point with the best sensitivity and specificity for predicting NOAF within 30 days of TAVI, the investigators said (J. Am. Coll. Cardiol. 2011 [doi:10/1016/j.jacc.2011.09.061]).
Furthermore, the incidence of NOAF in those with an atrial size of 27 mm/m2 or greater undergoing TAVI by the transapical approach vs. the transfemoral approach was 57% vs. 12%, respectively, they noted.
Mortality, which was 16% and 21% in those with and without NOAF at 12 months, respectively, did not differ significantly between the groups at either follow-up, they noted.
Patients in the study had severe symptomatic aortic stenosis, but no history of chronic/paroxysmal atrial fibrillation. They underwent TAVI with a balloon-expandable valve by either the transapical or transfemoral approach, were enrolled consecutively between May 2007 and May 2011, and underwent continuous electrocardiographic monitoring during hospitalization. NOAF was defined as any episode of AF lasting longer than 30 seconds.
NOAF is a known complication in patients undergoing cardiovascular interventions, but this is one of the first studies to verify an increased risk of the condition in patients undergoing TAVI, which has emerged as an alternative treatment for patients with severe symptomatic aortic stenosis and high or prohibitive operative risk. The study is also among the first to characterize predictive factors for NOAF.
"The occurrence of cerebrovascular events is probably the most worrisome complication associated with TAVI, with an incidence of about 4%, one of the highest ever reported in the field of interventional cardiology," the investigators said, noting that the fact that more than 50% of the complications occur several days after TAVI suggests that "mechanisms other than those directly related to the procedure may be involved."
Indeed, the findings of this study suggest NOAF may be an important mechanism for late neurological events after TAVI, and if confirmed in larger studies, the findings may have implications for the development of prevention trials.
"Knowing the predictive factors of NOAF following TAVI should allow us to select the patients at higher risk for NOAF preventive studies in the setting of TAVI," they investigators said.
Also of note, some of the cardioembolic events in this study seemed to be related to the non-initiation of anticoagulant therapy, the investigators said, adding that the risk of a cardioembolic event was as high as 40% in those who had NOAF and who did not receive anticoagulant therapy.
This underscores the clinical relevance of optimizing antithrombotic treatment in this high-risk subset of patients, they concluded.
Dr. Amat-Santos disclosed that he received support from the Institute of Heart Sciences. Other authors disclosed having served as consultants for Edwards Lifesciences, and/or St. Jude Medical.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Major Finding: NOAF occurred in 44 patients at a median of 48 hours after transcatheter aortic valve implantation (TAVI), with 10 episodes resolving spontaneously within 12 hours, and 34 requiring pharmacologic intervention. The rate of the combined end point of stroke and systemic embolism was 13.6% at 30 days in the NOAF group, compared with 3.2% (odds ratio 4.79) in those who did not experience NOAF; the rate was 15.9% vs. 3.2% at 12 months (odds ratio 5.0).
Data Source: A prospective study of 138 patients undergoing TAVI.
Disclosures: Dr. Amat-Santos disclosed that he received support from the Institute of Heart Sciences. Other authors disclosed that they have consulted for Edwards Lifesciences Inc., and/or St. Jude Medical.
Predictors Identified for Hospital Readmission After CABG
SAN FRANCISCO – Awareness of four factors that predict increased risk for hospital readmission after coronary artery bypass grafting may improve physicians’ ability to reduce early readmission rates among patients undergoing the procedure.
The four factors that independently predicted increased risk for hospital readmission after CABG in a study of 818 patients were preoperative congestive heart failure, chronic lung disease, a body mass index of 40 kg/m2 or greater, and longer time spent on cardiopulmonary bypass, Dr. Kelly B. Currie said at the annual clinical congress of the American College of Surgeons.
Medicare payments to hospitals with high readmission rates will be reduced starting in October 2012 under provisions of the Patient Protection and Affordable Care Act. Payments will change from a fee-for-service model to a value-based model.
Readmission rates within 30 days of CABG range from 6% to 21% in the medical literature. In the third quarter of 2010, 10% of patients in the Society of Thoracic Surgeons (STS) database who underwent CABG were readmitted within 30 days, said Dr. Currie, a surgery resident at Bassett Medical Center, Cooperstown, N.Y.
She and her associates analyzed data from 460 patients undergoing CABG at their center from 2003 to 2010 and from 358 patients in the STS Heartsource database. Once they identified independent predictors of readmission, they conducted a second logistic regression analysis on the 358 patients in the STS database and created a "probability calculator" of readmission risk.
Congestive heart failure was associated with a 77% increase in risk for early readmission after CABG, and chronic lung disease was associated with an 82% increase in risk. The risk of readmission increased significantly by 0.6% with longer perfusion time, and increased nearly fourfold in obese patients with a body mass index of 40 or greater compared with normal-weight patients.
The risk for readmission decreased significantly by 40% in patients who underwent endoscopic vein harvest, she added.
Physicians may want to focus resources on the high-risk patients to decrease readmissions, Dr. Curry said. Readmissions might be lessened by instituting follow-up calls within a day of discharge, and/or having patients see their primary care physicians within 7 days of discharge. Efforts to improve verbal handoffs of patient care between inpatient nurses and visiting nurses, as well as the use of telemedicine, might be other effective ways to help avoid readmissions, she suggested.
"These are things we are going to be implementing in the near future, hopefully," she said.
The readmission risk calculator developed in this study probably cannot be applied to a broad population of patients because some of the variables are specific to the cardiac surgery population, she noted. The study’s techniques could be applied, however, to develop risk calculators for other populations.
Dr. Currie is collaborating with researchers at Columbia University in New York to develop an improved calculator by studying data on an expected 1,400 adult cardiac surgery cases at nine hospitals in five states.
Dr. Currie said she has no relevant conflicts of interest.
This is a very important and timely topic. Like it or not, value-based payments and accountable care organizations are upon us. We are going to be expected and probably mandated to provide the same high-quality care at lower and more reasonable cost. Complications – including readmissions – are expensive not only in terms of dollars but also in terms of quality and, at times, quantity of life.
Yogi Berra once said, "It’s difficult to make predictions, especially about the future." Dr. Currie and her colleagues should be commended because they have taken on that very difficult task of trying to predict the future. Using a data analysis of coronary artery bypass patients, they have developed a method by which we can predict, and hopefully avoid, hospital readmissions after CABG.
Trying to decrease hospital length of stay, which over the last decade has been a very important cost-saving measure, seems to be diametrically opposed to trying to decrease readmissions. We follow those pathways that, based on diagnosis and on procedure, dictate a one-size-fits-all method of how long the length of stay is supposed to be. I wonder if Dr. Currie’s model is robust enough that, based on patients’ individual data, we can come up with what should be a more sensible and reasonable length of stay.
Dr. Thomas E. MacGillivray is co-director of the Thoracic Aortic Center at Massachusetts General Hospital, Boston. He made these comments as the discussant of Dr. Currie’s presentation at the meeting.
hospital readmission rate, reducing hospital readmissions, congestive heart failure
This is a very important and timely topic. Like it or not, value-based payments and accountable care organizations are upon us. We are going to be expected and probably mandated to provide the same high-quality care at lower and more reasonable cost. Complications – including readmissions – are expensive not only in terms of dollars but also in terms of quality and, at times, quantity of life.
Yogi Berra once said, "It’s difficult to make predictions, especially about the future." Dr. Currie and her colleagues should be commended because they have taken on that very difficult task of trying to predict the future. Using a data analysis of coronary artery bypass patients, they have developed a method by which we can predict, and hopefully avoid, hospital readmissions after CABG.
Trying to decrease hospital length of stay, which over the last decade has been a very important cost-saving measure, seems to be diametrically opposed to trying to decrease readmissions. We follow those pathways that, based on diagnosis and on procedure, dictate a one-size-fits-all method of how long the length of stay is supposed to be. I wonder if Dr. Currie’s model is robust enough that, based on patients’ individual data, we can come up with what should be a more sensible and reasonable length of stay.
Dr. Thomas E. MacGillivray is co-director of the Thoracic Aortic Center at Massachusetts General Hospital, Boston. He made these comments as the discussant of Dr. Currie’s presentation at the meeting.
This is a very important and timely topic. Like it or not, value-based payments and accountable care organizations are upon us. We are going to be expected and probably mandated to provide the same high-quality care at lower and more reasonable cost. Complications – including readmissions – are expensive not only in terms of dollars but also in terms of quality and, at times, quantity of life.
Yogi Berra once said, "It’s difficult to make predictions, especially about the future." Dr. Currie and her colleagues should be commended because they have taken on that very difficult task of trying to predict the future. Using a data analysis of coronary artery bypass patients, they have developed a method by which we can predict, and hopefully avoid, hospital readmissions after CABG.
Trying to decrease hospital length of stay, which over the last decade has been a very important cost-saving measure, seems to be diametrically opposed to trying to decrease readmissions. We follow those pathways that, based on diagnosis and on procedure, dictate a one-size-fits-all method of how long the length of stay is supposed to be. I wonder if Dr. Currie’s model is robust enough that, based on patients’ individual data, we can come up with what should be a more sensible and reasonable length of stay.
Dr. Thomas E. MacGillivray is co-director of the Thoracic Aortic Center at Massachusetts General Hospital, Boston. He made these comments as the discussant of Dr. Currie’s presentation at the meeting.
SAN FRANCISCO – Awareness of four factors that predict increased risk for hospital readmission after coronary artery bypass grafting may improve physicians’ ability to reduce early readmission rates among patients undergoing the procedure.
The four factors that independently predicted increased risk for hospital readmission after CABG in a study of 818 patients were preoperative congestive heart failure, chronic lung disease, a body mass index of 40 kg/m2 or greater, and longer time spent on cardiopulmonary bypass, Dr. Kelly B. Currie said at the annual clinical congress of the American College of Surgeons.
Medicare payments to hospitals with high readmission rates will be reduced starting in October 2012 under provisions of the Patient Protection and Affordable Care Act. Payments will change from a fee-for-service model to a value-based model.
Readmission rates within 30 days of CABG range from 6% to 21% in the medical literature. In the third quarter of 2010, 10% of patients in the Society of Thoracic Surgeons (STS) database who underwent CABG were readmitted within 30 days, said Dr. Currie, a surgery resident at Bassett Medical Center, Cooperstown, N.Y.
She and her associates analyzed data from 460 patients undergoing CABG at their center from 2003 to 2010 and from 358 patients in the STS Heartsource database. Once they identified independent predictors of readmission, they conducted a second logistic regression analysis on the 358 patients in the STS database and created a "probability calculator" of readmission risk.
Congestive heart failure was associated with a 77% increase in risk for early readmission after CABG, and chronic lung disease was associated with an 82% increase in risk. The risk of readmission increased significantly by 0.6% with longer perfusion time, and increased nearly fourfold in obese patients with a body mass index of 40 or greater compared with normal-weight patients.
The risk for readmission decreased significantly by 40% in patients who underwent endoscopic vein harvest, she added.
Physicians may want to focus resources on the high-risk patients to decrease readmissions, Dr. Curry said. Readmissions might be lessened by instituting follow-up calls within a day of discharge, and/or having patients see their primary care physicians within 7 days of discharge. Efforts to improve verbal handoffs of patient care between inpatient nurses and visiting nurses, as well as the use of telemedicine, might be other effective ways to help avoid readmissions, she suggested.
"These are things we are going to be implementing in the near future, hopefully," she said.
The readmission risk calculator developed in this study probably cannot be applied to a broad population of patients because some of the variables are specific to the cardiac surgery population, she noted. The study’s techniques could be applied, however, to develop risk calculators for other populations.
Dr. Currie is collaborating with researchers at Columbia University in New York to develop an improved calculator by studying data on an expected 1,400 adult cardiac surgery cases at nine hospitals in five states.
Dr. Currie said she has no relevant conflicts of interest.
SAN FRANCISCO – Awareness of four factors that predict increased risk for hospital readmission after coronary artery bypass grafting may improve physicians’ ability to reduce early readmission rates among patients undergoing the procedure.
The four factors that independently predicted increased risk for hospital readmission after CABG in a study of 818 patients were preoperative congestive heart failure, chronic lung disease, a body mass index of 40 kg/m2 or greater, and longer time spent on cardiopulmonary bypass, Dr. Kelly B. Currie said at the annual clinical congress of the American College of Surgeons.
Medicare payments to hospitals with high readmission rates will be reduced starting in October 2012 under provisions of the Patient Protection and Affordable Care Act. Payments will change from a fee-for-service model to a value-based model.
Readmission rates within 30 days of CABG range from 6% to 21% in the medical literature. In the third quarter of 2010, 10% of patients in the Society of Thoracic Surgeons (STS) database who underwent CABG were readmitted within 30 days, said Dr. Currie, a surgery resident at Bassett Medical Center, Cooperstown, N.Y.
She and her associates analyzed data from 460 patients undergoing CABG at their center from 2003 to 2010 and from 358 patients in the STS Heartsource database. Once they identified independent predictors of readmission, they conducted a second logistic regression analysis on the 358 patients in the STS database and created a "probability calculator" of readmission risk.
Congestive heart failure was associated with a 77% increase in risk for early readmission after CABG, and chronic lung disease was associated with an 82% increase in risk. The risk of readmission increased significantly by 0.6% with longer perfusion time, and increased nearly fourfold in obese patients with a body mass index of 40 or greater compared with normal-weight patients.
The risk for readmission decreased significantly by 40% in patients who underwent endoscopic vein harvest, she added.
Physicians may want to focus resources on the high-risk patients to decrease readmissions, Dr. Curry said. Readmissions might be lessened by instituting follow-up calls within a day of discharge, and/or having patients see their primary care physicians within 7 days of discharge. Efforts to improve verbal handoffs of patient care between inpatient nurses and visiting nurses, as well as the use of telemedicine, might be other effective ways to help avoid readmissions, she suggested.
"These are things we are going to be implementing in the near future, hopefully," she said.
The readmission risk calculator developed in this study probably cannot be applied to a broad population of patients because some of the variables are specific to the cardiac surgery population, she noted. The study’s techniques could be applied, however, to develop risk calculators for other populations.
Dr. Currie is collaborating with researchers at Columbia University in New York to develop an improved calculator by studying data on an expected 1,400 adult cardiac surgery cases at nine hospitals in five states.
Dr. Currie said she has no relevant conflicts of interest.
hospital readmission rate, reducing hospital readmissions, congestive heart failure
hospital readmission rate, reducing hospital readmissions, congestive heart failure
FROM THE ANNUAL CLINICAL CONGRESS OF THE AMERICAN COLLEGE OF SURGEONS
Major Finding: Four factors predicted readmission within 30 days of CABG: preoperative congestive heart failure, chronic lung disease, a body mass index of 40 kg/m2 or greater, and longer time on cardiopulmonary bypass.
Data Source: Retrospective analyses of data on 818 adults after CABG, 460 from one institution and 358 from an STS database.
Disclosures: Dr. Currie said she has no relevant conflicts of interest.
Cut Readmissions After Pediatric Heart Surgery by Fact Finding
COLORADO SPRINGS – Physicians at Emory University Hospital now have a firmer grip on what they’re dealing with in reducing 30-day readmissions.
The knowledge that there are three major risk factors – preoperative failure to thrive, an initial length of stay greater than 10 days, and Hispanic ethnicity – for readmission following pediatric congenital heart disease surgery is a tool for improvement, said Dr. Brian E. Kogon of Emory University, Atlanta.
"These data are obviously our data and are very specific to our hospital, our location, and our patient population. I would think that it’s going to be very different throughout the country based on whether you’re at an academic center or private center, urban versus rural setting, and even in adult cardiac, general thoracic, and pediatric practices," Dr. Kogon said in presenting the study findings at the annual meeting of the Western Thoracic Surgical Association.
The important thing is for physicians and surgeons to analyze their own hospital’s readmission experience, identify the risk factors, and then address the potentially modifiable ones in an effort to drive that readmission rate down, added Dr. Kogon, director of the congenital cardiac surgery fellowship program at Emory.
Studying Readmissions Following Pediatric Surgery
Readmissions within 30 days are increasingly viewed by third-party payers as preventable complications warranting stiff payment penalties. The focus thus far has been on the adult world, but at some point pediatric care will come under scrutiny as well. This realization led Dr. Kogon and his coworkers to analyze their institutional experience via a retrospective cohort study.
During 2002-2009, the annual 30-day readmission rates following pediatric surgery for congenital heart disease were 5.9%-10.4%, with a median of 8.7%. Those rates are relatively low; other centers typically report readmission rates of 10%-20%, he noted.
In 2009, 685 patients were discharged after pediatric congenital heart disease surgery; 70 of them had 74 readmissions. Among the key findings: only 15% of readmissions were for cardiac reasons. Indeed, the top three reasons for readmission were pleural or pericardial effusions, accounting for 26% of all readmissions; gastrointestinal problems, 24%; and infection, 19%.
Readmissions were costly. A total of 69% of patients were readmitted to a ward, 31% to the ICU. Upon readmission these patients spent a total of 653 additional days – almost 22 months – in the hospital.
The investigators scrutinized numerous potential demographic, preoperative, operative, and postoperative risk factors for readmission. Only three proved significant in a multivariate analysis: an initial length of stay greater than 10 days was associated with a 4.4-fold increased risk of readmission; a preoperative diagnosis of failure to thrive was associated with a 2.7-fold risk; and Hispanic ethnicity was associated with a 1.87-fold increased risk.
These readmissions occurred despite an intense discharge process and close follow-up. All families at the pediatric heart surgery unit attend a discharge class and a CPR training class. A pharmacist is on hand at the discharge class to review medications. Shunt recipients and newborns receive additional education. All case-management issues, such as formula supplies and home health equipment, are resolved before discharge. Patients meet with a cardiothoracic surgeon during their first week out of hospital, a cardiologist the second week, and thereafter with their primary care provider.
The median time to the first scheduled outpatient appointment was 4.5 days postdischarge. The median time to readmission was 8 days. Thirty-one percent of patients were readmitted prior to their first clinic appointment, 10% directly from the clinic, and 50% after their first clinic visit. The rest were readmitted after being no-shows for their clinic visit.
Dr. Kogon said he suspects that Hispanics were at increased risk for readmission because of educational and language barriers. Although a Spanish-language interpreter is present at the discharge class as needed, Dr. Kogon and his colleagues have observed that many Hispanic families nonetheless return unclear about medication and feeding regimens.
"I think there’s still a gap in our education of those patients," he said.
Discussant Dr. David R. Clarke said it might be argued that if a hospital doesn’t have a certain number of readmissions, then patients are being kept in the hospital too long.
"On a practical level, how much do we spend during the initial admission to ensure no readmissions? Do we automatically keep patients identified as high risk, such as Hispanics, 2, 3, or 4 extra days to minimize their readmission rate? And even if we do that and other things, is it really possible to prevent readmissions?" wondered Dr. Clarke of Children’s Hospital Colorado, Denver.
Dr. Kogon replied that this is the key question his colleagues raised when he shared the study findings. The group has decided to modify the discharge process for their high-risk patients, keeping them in the hospital a day or so longer while continuing to collect data in order to see if this pays off in fewer readmissions.
Dr. Kogon declared having no financial conflicts.
COLORADO SPRINGS – Physicians at Emory University Hospital now have a firmer grip on what they’re dealing with in reducing 30-day readmissions.
The knowledge that there are three major risk factors – preoperative failure to thrive, an initial length of stay greater than 10 days, and Hispanic ethnicity – for readmission following pediatric congenital heart disease surgery is a tool for improvement, said Dr. Brian E. Kogon of Emory University, Atlanta.
"These data are obviously our data and are very specific to our hospital, our location, and our patient population. I would think that it’s going to be very different throughout the country based on whether you’re at an academic center or private center, urban versus rural setting, and even in adult cardiac, general thoracic, and pediatric practices," Dr. Kogon said in presenting the study findings at the annual meeting of the Western Thoracic Surgical Association.
The important thing is for physicians and surgeons to analyze their own hospital’s readmission experience, identify the risk factors, and then address the potentially modifiable ones in an effort to drive that readmission rate down, added Dr. Kogon, director of the congenital cardiac surgery fellowship program at Emory.
Studying Readmissions Following Pediatric Surgery
Readmissions within 30 days are increasingly viewed by third-party payers as preventable complications warranting stiff payment penalties. The focus thus far has been on the adult world, but at some point pediatric care will come under scrutiny as well. This realization led Dr. Kogon and his coworkers to analyze their institutional experience via a retrospective cohort study.
During 2002-2009, the annual 30-day readmission rates following pediatric surgery for congenital heart disease were 5.9%-10.4%, with a median of 8.7%. Those rates are relatively low; other centers typically report readmission rates of 10%-20%, he noted.
In 2009, 685 patients were discharged after pediatric congenital heart disease surgery; 70 of them had 74 readmissions. Among the key findings: only 15% of readmissions were for cardiac reasons. Indeed, the top three reasons for readmission were pleural or pericardial effusions, accounting for 26% of all readmissions; gastrointestinal problems, 24%; and infection, 19%.
Readmissions were costly. A total of 69% of patients were readmitted to a ward, 31% to the ICU. Upon readmission these patients spent a total of 653 additional days – almost 22 months – in the hospital.
The investigators scrutinized numerous potential demographic, preoperative, operative, and postoperative risk factors for readmission. Only three proved significant in a multivariate analysis: an initial length of stay greater than 10 days was associated with a 4.4-fold increased risk of readmission; a preoperative diagnosis of failure to thrive was associated with a 2.7-fold risk; and Hispanic ethnicity was associated with a 1.87-fold increased risk.
These readmissions occurred despite an intense discharge process and close follow-up. All families at the pediatric heart surgery unit attend a discharge class and a CPR training class. A pharmacist is on hand at the discharge class to review medications. Shunt recipients and newborns receive additional education. All case-management issues, such as formula supplies and home health equipment, are resolved before discharge. Patients meet with a cardiothoracic surgeon during their first week out of hospital, a cardiologist the second week, and thereafter with their primary care provider.
The median time to the first scheduled outpatient appointment was 4.5 days postdischarge. The median time to readmission was 8 days. Thirty-one percent of patients were readmitted prior to their first clinic appointment, 10% directly from the clinic, and 50% after their first clinic visit. The rest were readmitted after being no-shows for their clinic visit.
Dr. Kogon said he suspects that Hispanics were at increased risk for readmission because of educational and language barriers. Although a Spanish-language interpreter is present at the discharge class as needed, Dr. Kogon and his colleagues have observed that many Hispanic families nonetheless return unclear about medication and feeding regimens.
"I think there’s still a gap in our education of those patients," he said.
Discussant Dr. David R. Clarke said it might be argued that if a hospital doesn’t have a certain number of readmissions, then patients are being kept in the hospital too long.
"On a practical level, how much do we spend during the initial admission to ensure no readmissions? Do we automatically keep patients identified as high risk, such as Hispanics, 2, 3, or 4 extra days to minimize their readmission rate? And even if we do that and other things, is it really possible to prevent readmissions?" wondered Dr. Clarke of Children’s Hospital Colorado, Denver.
Dr. Kogon replied that this is the key question his colleagues raised when he shared the study findings. The group has decided to modify the discharge process for their high-risk patients, keeping them in the hospital a day or so longer while continuing to collect data in order to see if this pays off in fewer readmissions.
Dr. Kogon declared having no financial conflicts.
COLORADO SPRINGS – Physicians at Emory University Hospital now have a firmer grip on what they’re dealing with in reducing 30-day readmissions.
The knowledge that there are three major risk factors – preoperative failure to thrive, an initial length of stay greater than 10 days, and Hispanic ethnicity – for readmission following pediatric congenital heart disease surgery is a tool for improvement, said Dr. Brian E. Kogon of Emory University, Atlanta.
"These data are obviously our data and are very specific to our hospital, our location, and our patient population. I would think that it’s going to be very different throughout the country based on whether you’re at an academic center or private center, urban versus rural setting, and even in adult cardiac, general thoracic, and pediatric practices," Dr. Kogon said in presenting the study findings at the annual meeting of the Western Thoracic Surgical Association.
The important thing is for physicians and surgeons to analyze their own hospital’s readmission experience, identify the risk factors, and then address the potentially modifiable ones in an effort to drive that readmission rate down, added Dr. Kogon, director of the congenital cardiac surgery fellowship program at Emory.
Studying Readmissions Following Pediatric Surgery
Readmissions within 30 days are increasingly viewed by third-party payers as preventable complications warranting stiff payment penalties. The focus thus far has been on the adult world, but at some point pediatric care will come under scrutiny as well. This realization led Dr. Kogon and his coworkers to analyze their institutional experience via a retrospective cohort study.
During 2002-2009, the annual 30-day readmission rates following pediatric surgery for congenital heart disease were 5.9%-10.4%, with a median of 8.7%. Those rates are relatively low; other centers typically report readmission rates of 10%-20%, he noted.
In 2009, 685 patients were discharged after pediatric congenital heart disease surgery; 70 of them had 74 readmissions. Among the key findings: only 15% of readmissions were for cardiac reasons. Indeed, the top three reasons for readmission were pleural or pericardial effusions, accounting for 26% of all readmissions; gastrointestinal problems, 24%; and infection, 19%.
Readmissions were costly. A total of 69% of patients were readmitted to a ward, 31% to the ICU. Upon readmission these patients spent a total of 653 additional days – almost 22 months – in the hospital.
The investigators scrutinized numerous potential demographic, preoperative, operative, and postoperative risk factors for readmission. Only three proved significant in a multivariate analysis: an initial length of stay greater than 10 days was associated with a 4.4-fold increased risk of readmission; a preoperative diagnosis of failure to thrive was associated with a 2.7-fold risk; and Hispanic ethnicity was associated with a 1.87-fold increased risk.
These readmissions occurred despite an intense discharge process and close follow-up. All families at the pediatric heart surgery unit attend a discharge class and a CPR training class. A pharmacist is on hand at the discharge class to review medications. Shunt recipients and newborns receive additional education. All case-management issues, such as formula supplies and home health equipment, are resolved before discharge. Patients meet with a cardiothoracic surgeon during their first week out of hospital, a cardiologist the second week, and thereafter with their primary care provider.
The median time to the first scheduled outpatient appointment was 4.5 days postdischarge. The median time to readmission was 8 days. Thirty-one percent of patients were readmitted prior to their first clinic appointment, 10% directly from the clinic, and 50% after their first clinic visit. The rest were readmitted after being no-shows for their clinic visit.
Dr. Kogon said he suspects that Hispanics were at increased risk for readmission because of educational and language barriers. Although a Spanish-language interpreter is present at the discharge class as needed, Dr. Kogon and his colleagues have observed that many Hispanic families nonetheless return unclear about medication and feeding regimens.
"I think there’s still a gap in our education of those patients," he said.
Discussant Dr. David R. Clarke said it might be argued that if a hospital doesn’t have a certain number of readmissions, then patients are being kept in the hospital too long.
"On a practical level, how much do we spend during the initial admission to ensure no readmissions? Do we automatically keep patients identified as high risk, such as Hispanics, 2, 3, or 4 extra days to minimize their readmission rate? And even if we do that and other things, is it really possible to prevent readmissions?" wondered Dr. Clarke of Children’s Hospital Colorado, Denver.
Dr. Kogon replied that this is the key question his colleagues raised when he shared the study findings. The group has decided to modify the discharge process for their high-risk patients, keeping them in the hospital a day or so longer while continuing to collect data in order to see if this pays off in fewer readmissions.
Dr. Kogon declared having no financial conflicts.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE WESTERN THORACIC SURGICAL ASSOCIATION