User login
Medicaid expansion meant earlier presentation, better surgical outcomes
The for five common surgical conditions, according to a Jan. 24 report in JAMA Surgery.
“Given current debate on the ACA [Affordable Care Act] and reforms to the Medicaid program, evidence on the effects of these policies is critical ... As policy makers weigh changes to or a potential repeal of the ACA, these findings provide important new data on the early clinical effects of the law’s coverage expansion,” said investigators led by Andrew Loehrer, MD, of the department of surgical oncology at MD Anderson Cancer Center, Houston.
For a baseline, the team used hospital administrative data from the Vizient Clinical Data Base and Resource Manager to assess outcomes for appendicitis, cholecystitis, diverticulitis, peripheral artery disease, and aortic aneurysm in 42 states during 2010-2013, before the ACA took effect in 2014. They then compared outcomes during 2014-2015 in the 27 states that expanded Medicaid programs under the ACA with 15 states that did not. The study included 225,572 hospital admissions in the Medicaid expansion states and 67,957 in the nonexpansion states at more than 200 academic medical centers and affiliated hospitals.
Medicaid expansion in the 27 states was associated with a 7.5-percentage point decreased probability of patients being uninsured (95% confidence interval, –12.2 to –2.9; P = .002) and an 8.6-percentage point increased probability of having Medicaid (95% CI, 6.1-11.1; P less than .001).
Medicaid expansion was also associated with a 1.8-percentage point increase in the probability of early, uncomplicated presentation (95% CI, 0.7-2.9; P = .001) and a 2.6-percentage point increase in the probability of receiving optimal management after admission, most likely due to the earlier presentation (95% CI, 0.8-4.4; P = .006).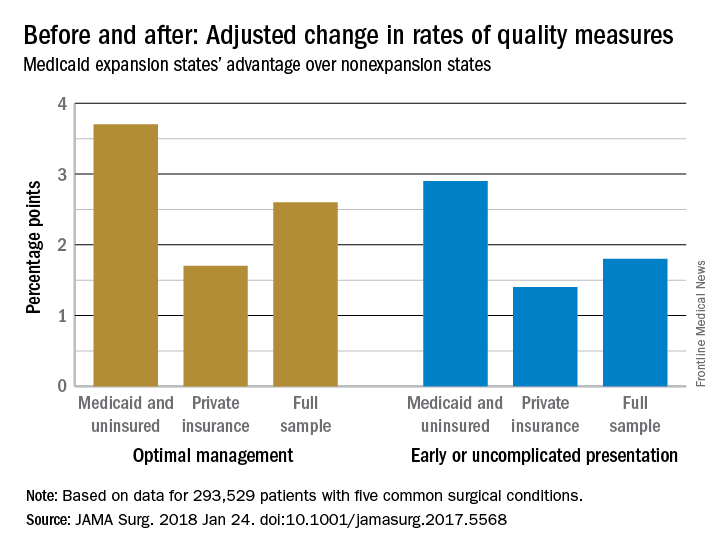
The improvements were concentrated among Medicaid and uninsured patients, who were most likely to benefit from coverage expansion, rather than those with private insurance.
The investigators acknowledged the limitations of their data for tracking changes access and quality of care for surgical patients. “We recognize that the data on improved quality of care are not as clear. Our use of composite outcomes has specific limitations,” they wrote.
“As expected for the conditions studied, our analysis found no significant change in the overall number of individuals treated but rather a change in the timeliness in which individuals received care.” Meanwhile, “our sample revealed an increase in the percentage of surgical patients who were uninsured in nonexpansion states after 2014,” which was associated with “worsening of outcomes ... whereas expansion states had stabilization or improvement,” they said. In Medicaid expansion states, the number of uninsured dropped from 14.% to 6.8%, but in the nonexpansion states, the number of uninsured actually increased slightly from 21.2% to 21.9%.
There was no funding source reported for the study. The authors had no conflicts of interest.
SOURCE: Loehrer AP et. al. JAMA Surg. 2018 Jan 24. doi: 10.1001/jamasurg.2017.5568
The for five common surgical conditions, according to a Jan. 24 report in JAMA Surgery.
“Given current debate on the ACA [Affordable Care Act] and reforms to the Medicaid program, evidence on the effects of these policies is critical ... As policy makers weigh changes to or a potential repeal of the ACA, these findings provide important new data on the early clinical effects of the law’s coverage expansion,” said investigators led by Andrew Loehrer, MD, of the department of surgical oncology at MD Anderson Cancer Center, Houston.
For a baseline, the team used hospital administrative data from the Vizient Clinical Data Base and Resource Manager to assess outcomes for appendicitis, cholecystitis, diverticulitis, peripheral artery disease, and aortic aneurysm in 42 states during 2010-2013, before the ACA took effect in 2014. They then compared outcomes during 2014-2015 in the 27 states that expanded Medicaid programs under the ACA with 15 states that did not. The study included 225,572 hospital admissions in the Medicaid expansion states and 67,957 in the nonexpansion states at more than 200 academic medical centers and affiliated hospitals.
Medicaid expansion in the 27 states was associated with a 7.5-percentage point decreased probability of patients being uninsured (95% confidence interval, –12.2 to –2.9; P = .002) and an 8.6-percentage point increased probability of having Medicaid (95% CI, 6.1-11.1; P less than .001).
Medicaid expansion was also associated with a 1.8-percentage point increase in the probability of early, uncomplicated presentation (95% CI, 0.7-2.9; P = .001) and a 2.6-percentage point increase in the probability of receiving optimal management after admission, most likely due to the earlier presentation (95% CI, 0.8-4.4; P = .006).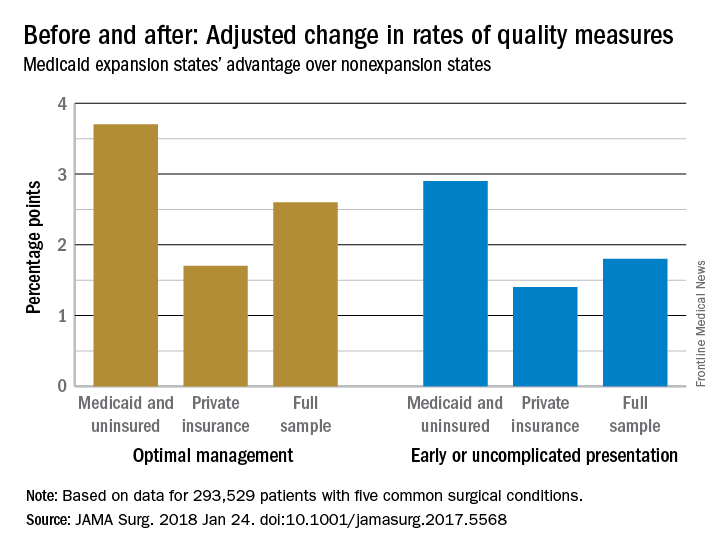
The improvements were concentrated among Medicaid and uninsured patients, who were most likely to benefit from coverage expansion, rather than those with private insurance.
The investigators acknowledged the limitations of their data for tracking changes access and quality of care for surgical patients. “We recognize that the data on improved quality of care are not as clear. Our use of composite outcomes has specific limitations,” they wrote.
“As expected for the conditions studied, our analysis found no significant change in the overall number of individuals treated but rather a change in the timeliness in which individuals received care.” Meanwhile, “our sample revealed an increase in the percentage of surgical patients who were uninsured in nonexpansion states after 2014,” which was associated with “worsening of outcomes ... whereas expansion states had stabilization or improvement,” they said. In Medicaid expansion states, the number of uninsured dropped from 14.% to 6.8%, but in the nonexpansion states, the number of uninsured actually increased slightly from 21.2% to 21.9%.
There was no funding source reported for the study. The authors had no conflicts of interest.
SOURCE: Loehrer AP et. al. JAMA Surg. 2018 Jan 24. doi: 10.1001/jamasurg.2017.5568
The for five common surgical conditions, according to a Jan. 24 report in JAMA Surgery.
“Given current debate on the ACA [Affordable Care Act] and reforms to the Medicaid program, evidence on the effects of these policies is critical ... As policy makers weigh changes to or a potential repeal of the ACA, these findings provide important new data on the early clinical effects of the law’s coverage expansion,” said investigators led by Andrew Loehrer, MD, of the department of surgical oncology at MD Anderson Cancer Center, Houston.
For a baseline, the team used hospital administrative data from the Vizient Clinical Data Base and Resource Manager to assess outcomes for appendicitis, cholecystitis, diverticulitis, peripheral artery disease, and aortic aneurysm in 42 states during 2010-2013, before the ACA took effect in 2014. They then compared outcomes during 2014-2015 in the 27 states that expanded Medicaid programs under the ACA with 15 states that did not. The study included 225,572 hospital admissions in the Medicaid expansion states and 67,957 in the nonexpansion states at more than 200 academic medical centers and affiliated hospitals.
Medicaid expansion in the 27 states was associated with a 7.5-percentage point decreased probability of patients being uninsured (95% confidence interval, –12.2 to –2.9; P = .002) and an 8.6-percentage point increased probability of having Medicaid (95% CI, 6.1-11.1; P less than .001).
Medicaid expansion was also associated with a 1.8-percentage point increase in the probability of early, uncomplicated presentation (95% CI, 0.7-2.9; P = .001) and a 2.6-percentage point increase in the probability of receiving optimal management after admission, most likely due to the earlier presentation (95% CI, 0.8-4.4; P = .006).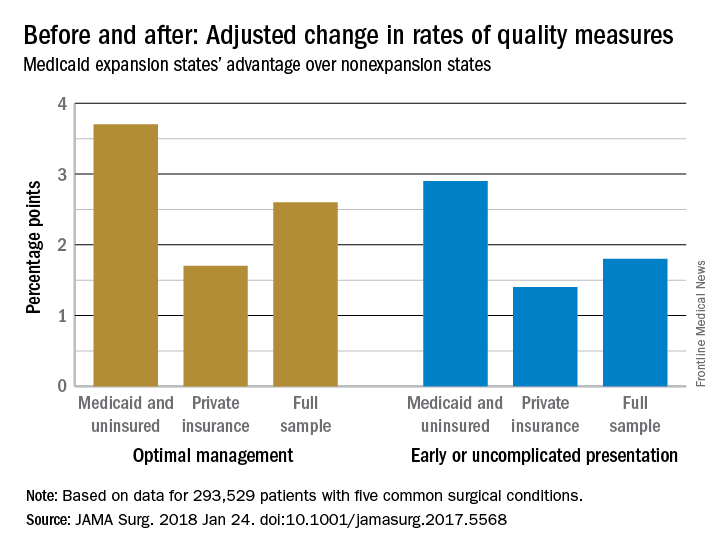
The improvements were concentrated among Medicaid and uninsured patients, who were most likely to benefit from coverage expansion, rather than those with private insurance.
The investigators acknowledged the limitations of their data for tracking changes access and quality of care for surgical patients. “We recognize that the data on improved quality of care are not as clear. Our use of composite outcomes has specific limitations,” they wrote.
“As expected for the conditions studied, our analysis found no significant change in the overall number of individuals treated but rather a change in the timeliness in which individuals received care.” Meanwhile, “our sample revealed an increase in the percentage of surgical patients who were uninsured in nonexpansion states after 2014,” which was associated with “worsening of outcomes ... whereas expansion states had stabilization or improvement,” they said. In Medicaid expansion states, the number of uninsured dropped from 14.% to 6.8%, but in the nonexpansion states, the number of uninsured actually increased slightly from 21.2% to 21.9%.
There was no funding source reported for the study. The authors had no conflicts of interest.
SOURCE: Loehrer AP et. al. JAMA Surg. 2018 Jan 24. doi: 10.1001/jamasurg.2017.5568
FROM JAMA SURGERY
Key clinical point: The Patient Protection and Affordable Care Act’s Medicaid expansion led to increased coverage of patients, earlier presentation, and improved care for five common surgical conditions.
Major finding: Medicaid expansion was associated with a 2.6 percentage-point increase in the probability of receiving optimal management after admission, most likely due to the earlier presentation.
Study details: Review of more than 200,000 patients, pre- and post-ACA
Disclosures: The authors had no disclosures.
Source: Loehrer AP et. al. JAMA Surg. 2018 Jan 24. doi: 10.1001/jamasurg.2017.5568
Gastrointestinal complications are a key risk factor for death after AEF repair
Aortoenteric fistulas (AEFs) are an uncommon but lethal form of aortic graft infection with morbidity and mortality rates reported in the literature to range from 14% to 75%. Over a 20-year period, researchers found that nearly half of their patients undergoing repair of their aortoenteric fistulas died within 60 days. The presence of gastrointestinal complications increased the risk of mortality more than threefold, according to the results of a single-center retrospective review of consecutive AEF repairs.
The researchers assessed 50 patients who presented with AEF and had repair during 1995-2014. Sixty percent of the patients were men, and the overall median age was 70 years. The median follow-up for the entire cohort was 14 months. The duodenum was the most common location of the enteric defect, found in 80% of the infections. Overall, 23 patients (46%) died by day 60, according to the report published in the July Journal of the American College of Surgeons.
Univariate analysis showed that advanced age, chronic renal insufficiency, any complications, and GI complications in particular (occurring in 26% of patients) were all associated with an increase in overall mortality (P less than .05). But upon multivariate analysis, gastrointestinal complications (hazard ratio, 3.23; P = .015) and advanced age (HR, 1.07; P = .01) were the only independent predictors of mortality, Atish Chopra, MD, of the division of vascular surgery, Oregon Health & Science University, Portland, and his colleagues wrote.
The institution changed operative procedures in 2007, based upon an earlier assessment of the importance of GI complications performed by the researchers, with greater emphasis placed on ensuring a viable GI reconstruction, and early intervention for mesenteric ischemia. In addition, they surmised that, after 2007, there was improved adherence to achieving wide debridement of nonviable and infected tissue, and to creating a tension-free anastomosis to healthy tissue edges while optimizing nutritional, medical, and antibiotic therapy, according to the researchers.
“When comparing the patients undergoing repair before 2007 with those compared after 2007 [38 and 12 AEF patients, respectively], we found that in-hospitality mortality decreased from 37% to 8% (P = .08), 60-day mortality decreased from 53% to 8% (P less than .01), and mortality at last follow-up decreased from 55% to 17% (P = .02). Dr. Chopra and his colleagues also found that mortality after GI complications decreased from 90% for those operated on before 2007 to 33% in those operated on after 2007 (P = .01).
“Methods to decrease and improvement management of GI complications may prove most effective at improving mortality rates for this lethal pathology,” the researchers concluded.
The authors reported that they had nothing to disclose.
SOURCE: Chopra A et al. J Am Coll Surg 2017 Jul;225(1):9-18.
While secondary aortoenteric fistulas fortunately are a rare occurrence after open aortic repair (less than 1%), the reported results of treatment are disappointing (up to 75% mortality). The authors have demonstrated significant improvement in overall mortality in their series by paying more attention to the GI component of the procedure and postoperative management of the patient.
When we published our institutions experience with AEFs from 1991 to 2004, the study included 29 patients with one-third of patients presenting in shock. Extra-anatomic repair was performed in 86% (68% single stage). Mortality was 24%, with shock, blood transfusions, and suprarenal clamping associated with a worse outcome. Our 5-year survival was 61% and freedom from recurrent infection or amputation was 86% and 88% respectively. While our experience favors an extra-anatomic reconstruction, there has been increased utilization of in-situ repair in recent years. The current authors have extensive experience with the Neoaortoiliac System (NAIS) procedure and have had minimal complications associated with the extensive vein harvest necessary for NAIS; however, this is not universal. Wound complications, compartment syndrome, and chronic venous insufficiency are not uncommon complications. Improved results using cryopreserved aortoiliac allografts (CAA) were reported by The Vascular Low-Frequency Disease Consortium. In a 2014 publication on 220 patients receiving CAA for aortic reconstruction for aortic graft infection, freedom from graft-related complications, graft explant, and limb loss was 80%, 88%, and 97%, respectively, at 5 years. This compares favorably with extra-anatomic reconstruction and other techniques. In suprarenal reconstructions, allografts have been favored since the natural branches can be used to simplify multiple vessel reconstruction. In cases of low-grade infection (Staphylococcus epidermidis), excellent results have been demonstrated with wide debridement, in-situ replacement with rifampin-bonded grafts and omental coverage.
AEF can also occur after endovascular abdominal aortic aneurysm (AAA) repair and a management strategy for removing the endograft should be considered in the planning of these cases. The authors describe their technique, which involves constraining the endograft using an umbilical tape. Another technique that I prefer uses a 20-cc syringe with the tip cut off. The endograft is constrained by advancing the syringe proximally over the endograft. The syringe collapses the device and can be used to constrain the proximal fixation stents of a suprarenal graft, simplifying removal of the stent graft. Infected EVAR will likely become more common as an etiology as we continue to expand EVAR utilization for AAA repair. Another Low-Frequency Consortium paper reviewed the treatment and outcome of EVAR infection. In that report of 206 infected EVAR (endovascular aneurysm repair) and TEVAR (thoracic endovascular aortic repair) patients, 90% had in situ replacement with a 30-day mortality of 11% and morbidity of 35%.
As in previous reports on AEF, the authors highlight the importance of high clinical suspicion in making an expeditious diagnosis. Many imaging modalities can be used, but often operative exploration is required for a definitive diagnosis. Complete graft excision and wide debridement are critical to minimize the risk of recurrent infection. Optimal revascularization techniques should be determined by the experience of the operator, current experience demonstrating nearly equivalent outcomes with extra-anatomic and in situ replacement. Careful GI reconstruction and post-operative nutrition, culture-specific antibiotics, and ICU care are likely more important than the mode of reconstruction. Lifelong surveillance to detect recurrent infections also is recommended.
Murray L. Shames, MD , is professor of surgery and radiology and chief of the division of vascular surgery at the University of South Florida, Tampa, and director of the Tampa General Hospital aortic program.
While secondary aortoenteric fistulas fortunately are a rare occurrence after open aortic repair (less than 1%), the reported results of treatment are disappointing (up to 75% mortality). The authors have demonstrated significant improvement in overall mortality in their series by paying more attention to the GI component of the procedure and postoperative management of the patient.
When we published our institutions experience with AEFs from 1991 to 2004, the study included 29 patients with one-third of patients presenting in shock. Extra-anatomic repair was performed in 86% (68% single stage). Mortality was 24%, with shock, blood transfusions, and suprarenal clamping associated with a worse outcome. Our 5-year survival was 61% and freedom from recurrent infection or amputation was 86% and 88% respectively. While our experience favors an extra-anatomic reconstruction, there has been increased utilization of in-situ repair in recent years. The current authors have extensive experience with the Neoaortoiliac System (NAIS) procedure and have had minimal complications associated with the extensive vein harvest necessary for NAIS; however, this is not universal. Wound complications, compartment syndrome, and chronic venous insufficiency are not uncommon complications. Improved results using cryopreserved aortoiliac allografts (CAA) were reported by The Vascular Low-Frequency Disease Consortium. In a 2014 publication on 220 patients receiving CAA for aortic reconstruction for aortic graft infection, freedom from graft-related complications, graft explant, and limb loss was 80%, 88%, and 97%, respectively, at 5 years. This compares favorably with extra-anatomic reconstruction and other techniques. In suprarenal reconstructions, allografts have been favored since the natural branches can be used to simplify multiple vessel reconstruction. In cases of low-grade infection (Staphylococcus epidermidis), excellent results have been demonstrated with wide debridement, in-situ replacement with rifampin-bonded grafts and omental coverage.
AEF can also occur after endovascular abdominal aortic aneurysm (AAA) repair and a management strategy for removing the endograft should be considered in the planning of these cases. The authors describe their technique, which involves constraining the endograft using an umbilical tape. Another technique that I prefer uses a 20-cc syringe with the tip cut off. The endograft is constrained by advancing the syringe proximally over the endograft. The syringe collapses the device and can be used to constrain the proximal fixation stents of a suprarenal graft, simplifying removal of the stent graft. Infected EVAR will likely become more common as an etiology as we continue to expand EVAR utilization for AAA repair. Another Low-Frequency Consortium paper reviewed the treatment and outcome of EVAR infection. In that report of 206 infected EVAR (endovascular aneurysm repair) and TEVAR (thoracic endovascular aortic repair) patients, 90% had in situ replacement with a 30-day mortality of 11% and morbidity of 35%.
As in previous reports on AEF, the authors highlight the importance of high clinical suspicion in making an expeditious diagnosis. Many imaging modalities can be used, but often operative exploration is required for a definitive diagnosis. Complete graft excision and wide debridement are critical to minimize the risk of recurrent infection. Optimal revascularization techniques should be determined by the experience of the operator, current experience demonstrating nearly equivalent outcomes with extra-anatomic and in situ replacement. Careful GI reconstruction and post-operative nutrition, culture-specific antibiotics, and ICU care are likely more important than the mode of reconstruction. Lifelong surveillance to detect recurrent infections also is recommended.
Murray L. Shames, MD , is professor of surgery and radiology and chief of the division of vascular surgery at the University of South Florida, Tampa, and director of the Tampa General Hospital aortic program.
While secondary aortoenteric fistulas fortunately are a rare occurrence after open aortic repair (less than 1%), the reported results of treatment are disappointing (up to 75% mortality). The authors have demonstrated significant improvement in overall mortality in their series by paying more attention to the GI component of the procedure and postoperative management of the patient.
When we published our institutions experience with AEFs from 1991 to 2004, the study included 29 patients with one-third of patients presenting in shock. Extra-anatomic repair was performed in 86% (68% single stage). Mortality was 24%, with shock, blood transfusions, and suprarenal clamping associated with a worse outcome. Our 5-year survival was 61% and freedom from recurrent infection or amputation was 86% and 88% respectively. While our experience favors an extra-anatomic reconstruction, there has been increased utilization of in-situ repair in recent years. The current authors have extensive experience with the Neoaortoiliac System (NAIS) procedure and have had minimal complications associated with the extensive vein harvest necessary for NAIS; however, this is not universal. Wound complications, compartment syndrome, and chronic venous insufficiency are not uncommon complications. Improved results using cryopreserved aortoiliac allografts (CAA) were reported by The Vascular Low-Frequency Disease Consortium. In a 2014 publication on 220 patients receiving CAA for aortic reconstruction for aortic graft infection, freedom from graft-related complications, graft explant, and limb loss was 80%, 88%, and 97%, respectively, at 5 years. This compares favorably with extra-anatomic reconstruction and other techniques. In suprarenal reconstructions, allografts have been favored since the natural branches can be used to simplify multiple vessel reconstruction. In cases of low-grade infection (Staphylococcus epidermidis), excellent results have been demonstrated with wide debridement, in-situ replacement with rifampin-bonded grafts and omental coverage.
AEF can also occur after endovascular abdominal aortic aneurysm (AAA) repair and a management strategy for removing the endograft should be considered in the planning of these cases. The authors describe their technique, which involves constraining the endograft using an umbilical tape. Another technique that I prefer uses a 20-cc syringe with the tip cut off. The endograft is constrained by advancing the syringe proximally over the endograft. The syringe collapses the device and can be used to constrain the proximal fixation stents of a suprarenal graft, simplifying removal of the stent graft. Infected EVAR will likely become more common as an etiology as we continue to expand EVAR utilization for AAA repair. Another Low-Frequency Consortium paper reviewed the treatment and outcome of EVAR infection. In that report of 206 infected EVAR (endovascular aneurysm repair) and TEVAR (thoracic endovascular aortic repair) patients, 90% had in situ replacement with a 30-day mortality of 11% and morbidity of 35%.
As in previous reports on AEF, the authors highlight the importance of high clinical suspicion in making an expeditious diagnosis. Many imaging modalities can be used, but often operative exploration is required for a definitive diagnosis. Complete graft excision and wide debridement are critical to minimize the risk of recurrent infection. Optimal revascularization techniques should be determined by the experience of the operator, current experience demonstrating nearly equivalent outcomes with extra-anatomic and in situ replacement. Careful GI reconstruction and post-operative nutrition, culture-specific antibiotics, and ICU care are likely more important than the mode of reconstruction. Lifelong surveillance to detect recurrent infections also is recommended.
Murray L. Shames, MD , is professor of surgery and radiology and chief of the division of vascular surgery at the University of South Florida, Tampa, and director of the Tampa General Hospital aortic program.
Aortoenteric fistulas (AEFs) are an uncommon but lethal form of aortic graft infection with morbidity and mortality rates reported in the literature to range from 14% to 75%. Over a 20-year period, researchers found that nearly half of their patients undergoing repair of their aortoenteric fistulas died within 60 days. The presence of gastrointestinal complications increased the risk of mortality more than threefold, according to the results of a single-center retrospective review of consecutive AEF repairs.
The researchers assessed 50 patients who presented with AEF and had repair during 1995-2014. Sixty percent of the patients were men, and the overall median age was 70 years. The median follow-up for the entire cohort was 14 months. The duodenum was the most common location of the enteric defect, found in 80% of the infections. Overall, 23 patients (46%) died by day 60, according to the report published in the July Journal of the American College of Surgeons.
Univariate analysis showed that advanced age, chronic renal insufficiency, any complications, and GI complications in particular (occurring in 26% of patients) were all associated with an increase in overall mortality (P less than .05). But upon multivariate analysis, gastrointestinal complications (hazard ratio, 3.23; P = .015) and advanced age (HR, 1.07; P = .01) were the only independent predictors of mortality, Atish Chopra, MD, of the division of vascular surgery, Oregon Health & Science University, Portland, and his colleagues wrote.
The institution changed operative procedures in 2007, based upon an earlier assessment of the importance of GI complications performed by the researchers, with greater emphasis placed on ensuring a viable GI reconstruction, and early intervention for mesenteric ischemia. In addition, they surmised that, after 2007, there was improved adherence to achieving wide debridement of nonviable and infected tissue, and to creating a tension-free anastomosis to healthy tissue edges while optimizing nutritional, medical, and antibiotic therapy, according to the researchers.
“When comparing the patients undergoing repair before 2007 with those compared after 2007 [38 and 12 AEF patients, respectively], we found that in-hospitality mortality decreased from 37% to 8% (P = .08), 60-day mortality decreased from 53% to 8% (P less than .01), and mortality at last follow-up decreased from 55% to 17% (P = .02). Dr. Chopra and his colleagues also found that mortality after GI complications decreased from 90% for those operated on before 2007 to 33% in those operated on after 2007 (P = .01).
“Methods to decrease and improvement management of GI complications may prove most effective at improving mortality rates for this lethal pathology,” the researchers concluded.
The authors reported that they had nothing to disclose.
SOURCE: Chopra A et al. J Am Coll Surg 2017 Jul;225(1):9-18.
Aortoenteric fistulas (AEFs) are an uncommon but lethal form of aortic graft infection with morbidity and mortality rates reported in the literature to range from 14% to 75%. Over a 20-year period, researchers found that nearly half of their patients undergoing repair of their aortoenteric fistulas died within 60 days. The presence of gastrointestinal complications increased the risk of mortality more than threefold, according to the results of a single-center retrospective review of consecutive AEF repairs.
The researchers assessed 50 patients who presented with AEF and had repair during 1995-2014. Sixty percent of the patients were men, and the overall median age was 70 years. The median follow-up for the entire cohort was 14 months. The duodenum was the most common location of the enteric defect, found in 80% of the infections. Overall, 23 patients (46%) died by day 60, according to the report published in the July Journal of the American College of Surgeons.
Univariate analysis showed that advanced age, chronic renal insufficiency, any complications, and GI complications in particular (occurring in 26% of patients) were all associated with an increase in overall mortality (P less than .05). But upon multivariate analysis, gastrointestinal complications (hazard ratio, 3.23; P = .015) and advanced age (HR, 1.07; P = .01) were the only independent predictors of mortality, Atish Chopra, MD, of the division of vascular surgery, Oregon Health & Science University, Portland, and his colleagues wrote.
The institution changed operative procedures in 2007, based upon an earlier assessment of the importance of GI complications performed by the researchers, with greater emphasis placed on ensuring a viable GI reconstruction, and early intervention for mesenteric ischemia. In addition, they surmised that, after 2007, there was improved adherence to achieving wide debridement of nonviable and infected tissue, and to creating a tension-free anastomosis to healthy tissue edges while optimizing nutritional, medical, and antibiotic therapy, according to the researchers.
“When comparing the patients undergoing repair before 2007 with those compared after 2007 [38 and 12 AEF patients, respectively], we found that in-hospitality mortality decreased from 37% to 8% (P = .08), 60-day mortality decreased from 53% to 8% (P less than .01), and mortality at last follow-up decreased from 55% to 17% (P = .02). Dr. Chopra and his colleagues also found that mortality after GI complications decreased from 90% for those operated on before 2007 to 33% in those operated on after 2007 (P = .01).
“Methods to decrease and improvement management of GI complications may prove most effective at improving mortality rates for this lethal pathology,” the researchers concluded.
The authors reported that they had nothing to disclose.
SOURCE: Chopra A et al. J Am Coll Surg 2017 Jul;225(1):9-18.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Nearly half of patients undergoing aortoenteric fistula repair died within 60 days.
Major finding: The presence of gastrointestinal complications increased the risk of mortality for AEF repair more than threefold.
Study details: A single center, retrospective review of 50 consecutive patients with AEF repairs during 1995-2014.
Disclosures: The authors reported that they had nothing to disclose.
Source: Chopra A et al. J Am Coll Surg. 2017 Jul;225:9-18.
Point/Counterpoint: Should FEVAR be used for a short neck?
FEVAR is generally the best option
The advent of endovascular aortic aneurysm repair (EVAR) has steadily become the standard of care in the management of infrarenal abdominal aortic aneurysms (AAAs). In fact, it has now surpassed open surgical repair and is the predominant therapeutic modality in managing this disease entity. Clearly, there are specific anatomic and technical factors that may preclude the use of traditional EVAR – most notably, challenging proximal neck anatomy, be it insufficient length or severe angulation.
It is estimated that up to 30%-40% of patients are unsuitable candidates because of these concerns.1 Such patients are thus relegated to traditional open repair with the associated concerns for supravisceral clamping, including dramatic changes in hemodynamics and prolonged ICU and hospital stays.
Open surgical repair of pararenal, juxtarenal, and suprarenal AAAs is tried, tested, and durable. Knott and the group from Mayo Clinic reviewed their repair of 126 consecutive elective juxtarenal AAAs requiring suprarenal aortic clamping noting a 30-day mortality of .8%.2 More recent data from Kabbani and the Henry Ford group involved their 27-year clinical experience suggesting that open repair of complex proximal aortic aneurysms can be performed with clinical outcomes that are similar to those of open infrarenal repair.3 I respectfully accept this traditional – and historic – treatment modality.
However, we vascular surgeons are progressive and resilient in our quest to innovate and modernize – some of us even modified the traditional endografts on the back table. We charged forward despite the initial paucity of data on infrarenal EVAR compared to traditional open repair of aneurysms in the past. Now, a large percentage of infrarenal AAA repairs are performed via EVAR. In fact, our steadfast progression to advanced endovascular techniques has raised the concern that our graduating trainees are no longer proficient, competent, or even capable, in open complex aneurysm repair!
Tsilimparis and colleagues reported the first outcomes comparing open repair and FEVAR.4 They queried the NSQIP database comparing 1,091 patients undergoing open repair with 264 in the FEVAR group. There was an increased risk of morbidity in all combined endpoints including pulmonary and cardiovascular complications as well as length of stay in patients undergoing the open repair group. A larger comprehensive review pooled the results from 8 FEVAR and 12 open repair series. Analysis of the data found the groups to be identical. Open repair, however, was found to have an increased 30-day mortality when compared to FEVAR (relative risk 1.03, 2% increased absolute mortality).5
Gupta and colleagues reported the latest multi-institutional data noting that open repair was associated with higher risk than FEVAR for 30-day mortality, cardiac and pulmonary complications, renal failure requiring dialysis, return to the operating room, and in this age of cost-containment, length of stay (2 days vs. 7 days; P less than .0001).6
A further study by Donas and colleagues evaluated 90 consecutive patients with primary degenerative juxtarenal AAAs to different operative strategies based on morphologic and clinical characteristics – 29 FEVAR, 30 chEVAR, and 31 open repair.7 Early procedure-related and all-cause 30-day mortality was 0% in the endovascular group and 6.4% in the open group.
Although open repair for juxtarenal AAAs is the gold standard, short- and mid-term data on the outcomes for complex endovascular repair are excellent. Data on long-term durability, graft fixation/migration as well as the integrity of the graft and concerns for endoleaks and branch vessel patency, however, are limited. We do not have long-term data because we have not been doing these newer procedures for that long – but the data thus far show great promise.
We need to continue to challenge the status quo, particularly when the current data are satisfactory and the procedure feasible. With our continued appraisal of the data we publish as vascular surgeons, we can then identify if these innovations and techniques will withstand the test of time. After all, we are vascular surgeons (particularly those of us who have trained extensively in open repair) – and if open repair is necessary, then we will be ready.
But, if I can avoid a thoracoabdominal incision for a few percutaneous access sites, then sign me up!
Dr. Mouawad is chief of vascular and endovascular surgery, medical director of the vascular laboratory, and vice-chair of the department of surgery at McLaren Bay Region, Bay City, Mich. He is assistant professor of surgery at Michigan State University and Central Michigan University.
References
1. Perspect Vasc Surg Endovasc Ther. 2009;21:13-8.
2. J Vasc Surg. 2008;47:695-701.
3. J Vasc Surg. 2014;59:1488-94.
4. Ann Vasc Surg. 2013;27(3):267-73.
5. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
6. J Vasc Surg. 2017 Dec;66(6):1653-8.
7. J Vasc Surg. 2012 Aug;56(2):285-90.
FEVAR may not be the best choice
Over the past 3 decades, EVAR, with its very low periprocedural morbidity and mortality, and satisfactory long-term results, has become the primary treatment modality for the majority of infrarenal AAAs. The success of stent grafts for the repair of AAA relies heavily on satisfactory proximal and distal seal zones. Each commercially available standard EVAR graft has a manufacturer’s instructions for use requiring a proximal landing zone length of between 10 and 15 mm. Patients with less than this required length are considered to have “short necks.” Evaluation of this group of patients has demonstrated that this is not an uncommon finding and that EVAR performed outside the instructions for use has been associated with an increased risk of intraoperative failure, aneurysm expansion, and later complications.1-3
Current treatment options for patients with short necks include open surgical repair (OSR), FEVAR, and EVAR with the chimney graft technique (Ch-EVAR).
Thus, current knowledge acquired from case series, registries, and clinical experience must be used in deciding which therapeutic option to offer patients. Relevant factors influencing this decision include the availability and adaptability of the technique, early outcomes including technical success, morbidity and mortality, and late outcomes including survival, need for reintervention, and other late morbidity. Finally, in an era of value-based medical care, cost also must be considered.
Currently there is only one Food and Drug Administration–approved fenestrated graft. When used in properly selected patients, excellent periprocedural results have been reported approaching those of standard EVAR. However, there are limitations in both the availability and adaptability of FEVAR. These grafts are custom made for each patient, often requiring several weeks of lead time. Adaptability also has its limitations, including access vessels, severe neck angulation, calcification, mural thrombus, and branch vessel size, number, location, and associated arterial disease. Any of these factors may preclude the use of this technology. Open repair, on the other hand, is not limited by graft availability and allows for custom modification for each patient’s specific disease morphology. The essential limitation for open repair is the patient’s physiological ability to withstand the operation.
Several studies attempting to compare the early outcomes of FEVAR versus comparable patients undergoing OSR of similar aneurysms have reported significantly lower 30-day mortality and major morbidity rates for FEVAR.4,5 However, Rao et al., in a recent systematic review and meta-analysis that included data on 2,326 patients from 35 case series reporting on elective repair of juxtarenal aneurysms by either OSR or FEVAR, found perioperative mortality to not be significantly different (4.1% for both). Also, no significant difference was found between the two groups when evaluating postoperative renal insufficiency and need for permanent dialysis. However, OSR did have significantly higher major complication rates (25% vs. 15.7%).6 These findings suggest that both modalities can be performed successfully, but that long term outcomes need to be considered to determine if the increased initial morbidity of OSR is justified by differences in long term results between the two modalities.
Open surgical repair of juxtarenal AAA has been shown to be a durable repair.7 While early and even intermediate results of FEVAR appear to be satisfactory, long-term durability has yet to be determined.4,8 Along with continuing to exclude the aneurysm sac, as with standard EVAR, there is the additional concern regarding the outcome of the organs supplied by the fenestrated/stent-grafted branches with FEVAR. Longer-term follow-up in the same review by Rao et al. showed that significantly more FEVAR patients developed renal failure compared with OSR patients (19.7% vs. 7.7%). FEVAR patients also had a higher rate of reintervention.
And finally, long-term survival was significantly greater in OSR patients compared to FEVAR at 3 and 5 years (80% vs. 74% vs. 73% vs. 55%). These authors concluded that open repair remains the gold standard while FEVAR is a favorable option for high risk patients.6
These new and innovative stent graft devices come at considerable expense. While this aspect of FEVAR has not been extensively studied, Michel et al., in their report from the multicenter prospective Windows registry, attempted to evaluate the economic aspect of FEVAR. They compared a group of patients who underwent FEVAR to patients from a large national hospital discharge database who underwent OSR. No difference in 30-day mortality was noted between these two groups; however, there was a significantly greater cost with FEVAR. The authors concluded that FEVAR did not appear to be justified for patients fit for open surgery with juxtarenal AAA.9
For now, the roles of OSR and FEVAR would appear to be complementary. Current evidence suggests that OSR is the most appropriate intervention for good risk patients with an anticipated longer life expectancy. Patients with appropriate anatomy for FEVAR and who are at higher risk for open repair would benefit from FEVAR. As further experience and outcomes are accumulated, our ability to select the appropriate therapy for individual patients should improve.
Dr. Weaver is an assistant clinical professor for surgery at Wayne State School of Medicine, Detroit, and an attending in the division of vascular surgery, Henry Ford Hospital.
References
1. Ir J Med Sci. 2015;184(1):249-55.
2. Circulation. 2011;123(24):2848-55.
3. J Endovasc Therapy. 2001;8(5):457-64.
4. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
5. Ann Vasc Surg. 2013;27(3):267-73.
6. J Vasc Surg. 2015;61(1):242-55.
7. J Vasc Surg. 2012;56(1):2-7.
8. J Cardiovasc Surg. 2015;56(3):331-7.
9. Eur J Vasc Endovasc Surg. 2015;50(2):189-96.
FEVAR is generally the best option
The advent of endovascular aortic aneurysm repair (EVAR) has steadily become the standard of care in the management of infrarenal abdominal aortic aneurysms (AAAs). In fact, it has now surpassed open surgical repair and is the predominant therapeutic modality in managing this disease entity. Clearly, there are specific anatomic and technical factors that may preclude the use of traditional EVAR – most notably, challenging proximal neck anatomy, be it insufficient length or severe angulation.
It is estimated that up to 30%-40% of patients are unsuitable candidates because of these concerns.1 Such patients are thus relegated to traditional open repair with the associated concerns for supravisceral clamping, including dramatic changes in hemodynamics and prolonged ICU and hospital stays.
Open surgical repair of pararenal, juxtarenal, and suprarenal AAAs is tried, tested, and durable. Knott and the group from Mayo Clinic reviewed their repair of 126 consecutive elective juxtarenal AAAs requiring suprarenal aortic clamping noting a 30-day mortality of .8%.2 More recent data from Kabbani and the Henry Ford group involved their 27-year clinical experience suggesting that open repair of complex proximal aortic aneurysms can be performed with clinical outcomes that are similar to those of open infrarenal repair.3 I respectfully accept this traditional – and historic – treatment modality.
However, we vascular surgeons are progressive and resilient in our quest to innovate and modernize – some of us even modified the traditional endografts on the back table. We charged forward despite the initial paucity of data on infrarenal EVAR compared to traditional open repair of aneurysms in the past. Now, a large percentage of infrarenal AAA repairs are performed via EVAR. In fact, our steadfast progression to advanced endovascular techniques has raised the concern that our graduating trainees are no longer proficient, competent, or even capable, in open complex aneurysm repair!
Tsilimparis and colleagues reported the first outcomes comparing open repair and FEVAR.4 They queried the NSQIP database comparing 1,091 patients undergoing open repair with 264 in the FEVAR group. There was an increased risk of morbidity in all combined endpoints including pulmonary and cardiovascular complications as well as length of stay in patients undergoing the open repair group. A larger comprehensive review pooled the results from 8 FEVAR and 12 open repair series. Analysis of the data found the groups to be identical. Open repair, however, was found to have an increased 30-day mortality when compared to FEVAR (relative risk 1.03, 2% increased absolute mortality).5
Gupta and colleagues reported the latest multi-institutional data noting that open repair was associated with higher risk than FEVAR for 30-day mortality, cardiac and pulmonary complications, renal failure requiring dialysis, return to the operating room, and in this age of cost-containment, length of stay (2 days vs. 7 days; P less than .0001).6
A further study by Donas and colleagues evaluated 90 consecutive patients with primary degenerative juxtarenal AAAs to different operative strategies based on morphologic and clinical characteristics – 29 FEVAR, 30 chEVAR, and 31 open repair.7 Early procedure-related and all-cause 30-day mortality was 0% in the endovascular group and 6.4% in the open group.
Although open repair for juxtarenal AAAs is the gold standard, short- and mid-term data on the outcomes for complex endovascular repair are excellent. Data on long-term durability, graft fixation/migration as well as the integrity of the graft and concerns for endoleaks and branch vessel patency, however, are limited. We do not have long-term data because we have not been doing these newer procedures for that long – but the data thus far show great promise.
We need to continue to challenge the status quo, particularly when the current data are satisfactory and the procedure feasible. With our continued appraisal of the data we publish as vascular surgeons, we can then identify if these innovations and techniques will withstand the test of time. After all, we are vascular surgeons (particularly those of us who have trained extensively in open repair) – and if open repair is necessary, then we will be ready.
But, if I can avoid a thoracoabdominal incision for a few percutaneous access sites, then sign me up!
Dr. Mouawad is chief of vascular and endovascular surgery, medical director of the vascular laboratory, and vice-chair of the department of surgery at McLaren Bay Region, Bay City, Mich. He is assistant professor of surgery at Michigan State University and Central Michigan University.
References
1. Perspect Vasc Surg Endovasc Ther. 2009;21:13-8.
2. J Vasc Surg. 2008;47:695-701.
3. J Vasc Surg. 2014;59:1488-94.
4. Ann Vasc Surg. 2013;27(3):267-73.
5. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
6. J Vasc Surg. 2017 Dec;66(6):1653-8.
7. J Vasc Surg. 2012 Aug;56(2):285-90.
FEVAR may not be the best choice
Over the past 3 decades, EVAR, with its very low periprocedural morbidity and mortality, and satisfactory long-term results, has become the primary treatment modality for the majority of infrarenal AAAs. The success of stent grafts for the repair of AAA relies heavily on satisfactory proximal and distal seal zones. Each commercially available standard EVAR graft has a manufacturer’s instructions for use requiring a proximal landing zone length of between 10 and 15 mm. Patients with less than this required length are considered to have “short necks.” Evaluation of this group of patients has demonstrated that this is not an uncommon finding and that EVAR performed outside the instructions for use has been associated with an increased risk of intraoperative failure, aneurysm expansion, and later complications.1-3
Current treatment options for patients with short necks include open surgical repair (OSR), FEVAR, and EVAR with the chimney graft technique (Ch-EVAR).
Thus, current knowledge acquired from case series, registries, and clinical experience must be used in deciding which therapeutic option to offer patients. Relevant factors influencing this decision include the availability and adaptability of the technique, early outcomes including technical success, morbidity and mortality, and late outcomes including survival, need for reintervention, and other late morbidity. Finally, in an era of value-based medical care, cost also must be considered.
Currently there is only one Food and Drug Administration–approved fenestrated graft. When used in properly selected patients, excellent periprocedural results have been reported approaching those of standard EVAR. However, there are limitations in both the availability and adaptability of FEVAR. These grafts are custom made for each patient, often requiring several weeks of lead time. Adaptability also has its limitations, including access vessels, severe neck angulation, calcification, mural thrombus, and branch vessel size, number, location, and associated arterial disease. Any of these factors may preclude the use of this technology. Open repair, on the other hand, is not limited by graft availability and allows for custom modification for each patient’s specific disease morphology. The essential limitation for open repair is the patient’s physiological ability to withstand the operation.
Several studies attempting to compare the early outcomes of FEVAR versus comparable patients undergoing OSR of similar aneurysms have reported significantly lower 30-day mortality and major morbidity rates for FEVAR.4,5 However, Rao et al., in a recent systematic review and meta-analysis that included data on 2,326 patients from 35 case series reporting on elective repair of juxtarenal aneurysms by either OSR or FEVAR, found perioperative mortality to not be significantly different (4.1% for both). Also, no significant difference was found between the two groups when evaluating postoperative renal insufficiency and need for permanent dialysis. However, OSR did have significantly higher major complication rates (25% vs. 15.7%).6 These findings suggest that both modalities can be performed successfully, but that long term outcomes need to be considered to determine if the increased initial morbidity of OSR is justified by differences in long term results between the two modalities.
Open surgical repair of juxtarenal AAA has been shown to be a durable repair.7 While early and even intermediate results of FEVAR appear to be satisfactory, long-term durability has yet to be determined.4,8 Along with continuing to exclude the aneurysm sac, as with standard EVAR, there is the additional concern regarding the outcome of the organs supplied by the fenestrated/stent-grafted branches with FEVAR. Longer-term follow-up in the same review by Rao et al. showed that significantly more FEVAR patients developed renal failure compared with OSR patients (19.7% vs. 7.7%). FEVAR patients also had a higher rate of reintervention.
And finally, long-term survival was significantly greater in OSR patients compared to FEVAR at 3 and 5 years (80% vs. 74% vs. 73% vs. 55%). These authors concluded that open repair remains the gold standard while FEVAR is a favorable option for high risk patients.6
These new and innovative stent graft devices come at considerable expense. While this aspect of FEVAR has not been extensively studied, Michel et al., in their report from the multicenter prospective Windows registry, attempted to evaluate the economic aspect of FEVAR. They compared a group of patients who underwent FEVAR to patients from a large national hospital discharge database who underwent OSR. No difference in 30-day mortality was noted between these two groups; however, there was a significantly greater cost with FEVAR. The authors concluded that FEVAR did not appear to be justified for patients fit for open surgery with juxtarenal AAA.9
For now, the roles of OSR and FEVAR would appear to be complementary. Current evidence suggests that OSR is the most appropriate intervention for good risk patients with an anticipated longer life expectancy. Patients with appropriate anatomy for FEVAR and who are at higher risk for open repair would benefit from FEVAR. As further experience and outcomes are accumulated, our ability to select the appropriate therapy for individual patients should improve.
Dr. Weaver is an assistant clinical professor for surgery at Wayne State School of Medicine, Detroit, and an attending in the division of vascular surgery, Henry Ford Hospital.
References
1. Ir J Med Sci. 2015;184(1):249-55.
2. Circulation. 2011;123(24):2848-55.
3. J Endovasc Therapy. 2001;8(5):457-64.
4. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
5. Ann Vasc Surg. 2013;27(3):267-73.
6. J Vasc Surg. 2015;61(1):242-55.
7. J Vasc Surg. 2012;56(1):2-7.
8. J Cardiovasc Surg. 2015;56(3):331-7.
9. Eur J Vasc Endovasc Surg. 2015;50(2):189-96.
FEVAR is generally the best option
The advent of endovascular aortic aneurysm repair (EVAR) has steadily become the standard of care in the management of infrarenal abdominal aortic aneurysms (AAAs). In fact, it has now surpassed open surgical repair and is the predominant therapeutic modality in managing this disease entity. Clearly, there are specific anatomic and technical factors that may preclude the use of traditional EVAR – most notably, challenging proximal neck anatomy, be it insufficient length or severe angulation.
It is estimated that up to 30%-40% of patients are unsuitable candidates because of these concerns.1 Such patients are thus relegated to traditional open repair with the associated concerns for supravisceral clamping, including dramatic changes in hemodynamics and prolonged ICU and hospital stays.
Open surgical repair of pararenal, juxtarenal, and suprarenal AAAs is tried, tested, and durable. Knott and the group from Mayo Clinic reviewed their repair of 126 consecutive elective juxtarenal AAAs requiring suprarenal aortic clamping noting a 30-day mortality of .8%.2 More recent data from Kabbani and the Henry Ford group involved their 27-year clinical experience suggesting that open repair of complex proximal aortic aneurysms can be performed with clinical outcomes that are similar to those of open infrarenal repair.3 I respectfully accept this traditional – and historic – treatment modality.
However, we vascular surgeons are progressive and resilient in our quest to innovate and modernize – some of us even modified the traditional endografts on the back table. We charged forward despite the initial paucity of data on infrarenal EVAR compared to traditional open repair of aneurysms in the past. Now, a large percentage of infrarenal AAA repairs are performed via EVAR. In fact, our steadfast progression to advanced endovascular techniques has raised the concern that our graduating trainees are no longer proficient, competent, or even capable, in open complex aneurysm repair!
Tsilimparis and colleagues reported the first outcomes comparing open repair and FEVAR.4 They queried the NSQIP database comparing 1,091 patients undergoing open repair with 264 in the FEVAR group. There was an increased risk of morbidity in all combined endpoints including pulmonary and cardiovascular complications as well as length of stay in patients undergoing the open repair group. A larger comprehensive review pooled the results from 8 FEVAR and 12 open repair series. Analysis of the data found the groups to be identical. Open repair, however, was found to have an increased 30-day mortality when compared to FEVAR (relative risk 1.03, 2% increased absolute mortality).5
Gupta and colleagues reported the latest multi-institutional data noting that open repair was associated with higher risk than FEVAR for 30-day mortality, cardiac and pulmonary complications, renal failure requiring dialysis, return to the operating room, and in this age of cost-containment, length of stay (2 days vs. 7 days; P less than .0001).6
A further study by Donas and colleagues evaluated 90 consecutive patients with primary degenerative juxtarenal AAAs to different operative strategies based on morphologic and clinical characteristics – 29 FEVAR, 30 chEVAR, and 31 open repair.7 Early procedure-related and all-cause 30-day mortality was 0% in the endovascular group and 6.4% in the open group.
Although open repair for juxtarenal AAAs is the gold standard, short- and mid-term data on the outcomes for complex endovascular repair are excellent. Data on long-term durability, graft fixation/migration as well as the integrity of the graft and concerns for endoleaks and branch vessel patency, however, are limited. We do not have long-term data because we have not been doing these newer procedures for that long – but the data thus far show great promise.
We need to continue to challenge the status quo, particularly when the current data are satisfactory and the procedure feasible. With our continued appraisal of the data we publish as vascular surgeons, we can then identify if these innovations and techniques will withstand the test of time. After all, we are vascular surgeons (particularly those of us who have trained extensively in open repair) – and if open repair is necessary, then we will be ready.
But, if I can avoid a thoracoabdominal incision for a few percutaneous access sites, then sign me up!
Dr. Mouawad is chief of vascular and endovascular surgery, medical director of the vascular laboratory, and vice-chair of the department of surgery at McLaren Bay Region, Bay City, Mich. He is assistant professor of surgery at Michigan State University and Central Michigan University.
References
1. Perspect Vasc Surg Endovasc Ther. 2009;21:13-8.
2. J Vasc Surg. 2008;47:695-701.
3. J Vasc Surg. 2014;59:1488-94.
4. Ann Vasc Surg. 2013;27(3):267-73.
5. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
6. J Vasc Surg. 2017 Dec;66(6):1653-8.
7. J Vasc Surg. 2012 Aug;56(2):285-90.
FEVAR may not be the best choice
Over the past 3 decades, EVAR, with its very low periprocedural morbidity and mortality, and satisfactory long-term results, has become the primary treatment modality for the majority of infrarenal AAAs. The success of stent grafts for the repair of AAA relies heavily on satisfactory proximal and distal seal zones. Each commercially available standard EVAR graft has a manufacturer’s instructions for use requiring a proximal landing zone length of between 10 and 15 mm. Patients with less than this required length are considered to have “short necks.” Evaluation of this group of patients has demonstrated that this is not an uncommon finding and that EVAR performed outside the instructions for use has been associated with an increased risk of intraoperative failure, aneurysm expansion, and later complications.1-3
Current treatment options for patients with short necks include open surgical repair (OSR), FEVAR, and EVAR with the chimney graft technique (Ch-EVAR).
Thus, current knowledge acquired from case series, registries, and clinical experience must be used in deciding which therapeutic option to offer patients. Relevant factors influencing this decision include the availability and adaptability of the technique, early outcomes including technical success, morbidity and mortality, and late outcomes including survival, need for reintervention, and other late morbidity. Finally, in an era of value-based medical care, cost also must be considered.
Currently there is only one Food and Drug Administration–approved fenestrated graft. When used in properly selected patients, excellent periprocedural results have been reported approaching those of standard EVAR. However, there are limitations in both the availability and adaptability of FEVAR. These grafts are custom made for each patient, often requiring several weeks of lead time. Adaptability also has its limitations, including access vessels, severe neck angulation, calcification, mural thrombus, and branch vessel size, number, location, and associated arterial disease. Any of these factors may preclude the use of this technology. Open repair, on the other hand, is not limited by graft availability and allows for custom modification for each patient’s specific disease morphology. The essential limitation for open repair is the patient’s physiological ability to withstand the operation.
Several studies attempting to compare the early outcomes of FEVAR versus comparable patients undergoing OSR of similar aneurysms have reported significantly lower 30-day mortality and major morbidity rates for FEVAR.4,5 However, Rao et al., in a recent systematic review and meta-analysis that included data on 2,326 patients from 35 case series reporting on elective repair of juxtarenal aneurysms by either OSR or FEVAR, found perioperative mortality to not be significantly different (4.1% for both). Also, no significant difference was found between the two groups when evaluating postoperative renal insufficiency and need for permanent dialysis. However, OSR did have significantly higher major complication rates (25% vs. 15.7%).6 These findings suggest that both modalities can be performed successfully, but that long term outcomes need to be considered to determine if the increased initial morbidity of OSR is justified by differences in long term results between the two modalities.
Open surgical repair of juxtarenal AAA has been shown to be a durable repair.7 While early and even intermediate results of FEVAR appear to be satisfactory, long-term durability has yet to be determined.4,8 Along with continuing to exclude the aneurysm sac, as with standard EVAR, there is the additional concern regarding the outcome of the organs supplied by the fenestrated/stent-grafted branches with FEVAR. Longer-term follow-up in the same review by Rao et al. showed that significantly more FEVAR patients developed renal failure compared with OSR patients (19.7% vs. 7.7%). FEVAR patients also had a higher rate of reintervention.
And finally, long-term survival was significantly greater in OSR patients compared to FEVAR at 3 and 5 years (80% vs. 74% vs. 73% vs. 55%). These authors concluded that open repair remains the gold standard while FEVAR is a favorable option for high risk patients.6
These new and innovative stent graft devices come at considerable expense. While this aspect of FEVAR has not been extensively studied, Michel et al., in their report from the multicenter prospective Windows registry, attempted to evaluate the economic aspect of FEVAR. They compared a group of patients who underwent FEVAR to patients from a large national hospital discharge database who underwent OSR. No difference in 30-day mortality was noted between these two groups; however, there was a significantly greater cost with FEVAR. The authors concluded that FEVAR did not appear to be justified for patients fit for open surgery with juxtarenal AAA.9
For now, the roles of OSR and FEVAR would appear to be complementary. Current evidence suggests that OSR is the most appropriate intervention for good risk patients with an anticipated longer life expectancy. Patients with appropriate anatomy for FEVAR and who are at higher risk for open repair would benefit from FEVAR. As further experience and outcomes are accumulated, our ability to select the appropriate therapy for individual patients should improve.
Dr. Weaver is an assistant clinical professor for surgery at Wayne State School of Medicine, Detroit, and an attending in the division of vascular surgery, Henry Ford Hospital.
References
1. Ir J Med Sci. 2015;184(1):249-55.
2. Circulation. 2011;123(24):2848-55.
3. J Endovasc Therapy. 2001;8(5):457-64.
4. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
5. Ann Vasc Surg. 2013;27(3):267-73.
6. J Vasc Surg. 2015;61(1):242-55.
7. J Vasc Surg. 2012;56(1):2-7.
8. J Cardiovasc Surg. 2015;56(3):331-7.
9. Eur J Vasc Endovasc Surg. 2015;50(2):189-96.
EVAR, venous CPT coding revamped for 2018
CHICAGO – Current Procedural Terminology coding for endovascular aneurysm repair has been totally overhauled for 2018 with the introduction of a family of 20 new codes and codes for other vascular procedures have also been updated.
The new EVAR CPT codes attempt to capture the work involved in performing the procedures based upon the anatomy of the aneurysm and the treated vessels rather than being device-based, as previously, Matthew J. Sideman, MD, explained in presenting the coding and reimbursement for 2018 at a symposium on vascular surgery sponsored by Northwestern University.
“The new EVAR codes for 2018 have got a lot of gains. There are some losses as well, but overall, I think it’s going to be very positive moving forward,” according to Dr. Sideman, a vascular surgeon at the University of Texas, San Antonio, who serves as chair of the Society for Vascular Surgery Coding and Reimbursement Committee and an adviser to the American Medical Association Relative Value Scale Update Committee (RUC).
“What we gained was a new code for ruptured aneurysm repair, a new code for enhanced fixation, a new code for percutaneous access, new codes for alternative access options, and now all the access codes are add-on codes. But what we traded off was loss due to bundling. So catheterization is now bundled into the main procedure, radiographic supervision and interpretation is now bundled. The big thing that really hurt was we lost all proximal extensions to the renal arteries and all distal extensions to the iliac bifurcations – they’re also bundled into the main procedure,” he said.
Restructuring the EVAR codes was a multiyear collaborative project of the SVS, the American College of Surgeons, the Society of Interventional Radiology, the Society of Thoracic Surgery, the American College of Cardiology, and the Society for Cardiovascular Angiography and Interventions. The impetus was twofold: recognition that the existing codes seriously undervalued the work involved in EVAR because, for example, they didn’t distinguish between ruptured and elective aneurysm repair, nor did they recognize the unique challenges and advantages of percutaneous access.
Also, representatives of the professional societies involved with vascular medicine recognized that they had to develop a detailed proposal for coding restructuring or matters might be taken out of their hands. Bundling of codes has become the prevailing dogma at the RUC and the Centers for Medicare and Medicaid. Their current policy is that when analysis of coding patterns indicates two codes are billed together at least 51% of the time, that’s considered a ‘typical’ situation and a new code must be created combining them. The harsh reality for clinicians is that under what Dr. Sideman called “RUC math,” the new bundled codes invariably pay less than the two old ones.
“There was a little bit of smoke and mirrors – ‘Look at the pretty flashing lights and not what’s going on behind over here’ – as we tried to maintain value as we bundled these EVAR codes,” Dr. Sideman recalled. “I can stand here and tell you I did my very best to push for the best values possible. It can be a painful process, but I thought we came out ok.”
How the new EVAR codes work
Dr. Sideman explained that the impact of the new EVAR codes will depend upon a surgeon’s practice pattern.
He offered as a concrete example a patient undergoing elective EVAR of the aorta and both iliac arteries with percutaneous access and placement of a bifurcated device with one docking limb. In 2017, this might have been handled using CPT codes 34802, 36200-50, and 75952-26, for a total of 31.05 Relative Value Units (RVUs) of work.
In 2018, however, this same surgical strategy would be coded as 34705 (elective endovascular repair of infrarenal aorta and/or iliac artery or arteries) plus 34713 x 2 (percutaneous access and closure), for a total of 34.58 RVUs. Thus, the surgeon would come out 3.53 RVUs ahead in 2018, which at a conversion factor of $35.78/RVU translates to an extra $126.30.
On the other hand, if the surgeon chose to use a bifurcated device with one docking limb, a left iliac bell-bottom extension, a right iliac bell-bottom extension, and percutaneous access, in 2017, this would have been coded as 34802, 34825, 34826, 36200-50, 75952-26, and 75953-26 x 2, for a total of 44.29 RVUs of work. In 2018, this same treatment strategy would be coded as 34705 plus 34713 x 2, for a total of 34.58 RVUs, or a knockdown of 9.71 fewer RVUs compared with the year before, which translates to $347.42 less.
“The more extensions you use, the more you’re going to come out behind going forward,” according to Dr. Sideman.
Other coding changes in 2018
Sclerotherapy of single and multiple veins (codes 36470 and 36471) got down-valued from 1.10 and 2.49 to 0.75 and 1.5 RVUs, respectively.
Angiography of the extremities (75710 and 75716) will be better reimbursed in 2018. In what Dr. Sideman called “a good win,” unilateral angiography will be rated as 1.75 RVUs, up from 1.14 in 2017, while bilateral angiography increased from 1.31 to 1.97 RVUs.
“The other nice thing I can tell you is that through campaigning and lobbying and comments to CMS [Centers for Medicare & Medicaid Services], we got them to reverse their recommendations from 2017 to 2018 on the dialysis family of codes,” the surgeon continued.
Reimbursement for the dialysis codes took a big hit from 2016 to 2017, amounting to several hundred million dollars less in reimbursement, but CMS has reversed its policy on that score. The RVUs for the various dialysis codes have increased from 2017 to 2018 by 5%-21%, with central venous angioplasty (CPT 36907) garnering the biggest increase.
Existing RVUs were retained for 2018 in three of the four selective catheter placement codes. However, reimbursement for 36215 (first order catheterization of the thoracic or brachiocephalic branch) dropped from 4.67 to 4.17 RVUs because physician surveys showed the time involved was less than previously rated. Once the RUC and CMS saw that the time involved in a procedure has decreased, it became impossible to maintain the RVU, Dr. Sideman explained.
And speaking of time involved in procedures, Dr. Sideman offered a final plea to his vascular medicine colleagues:
“When you get surveys from the RUC asking for your input, please, please, please, fill them out because that’s how we get our direct physician input into the valuation of codes.”
He reported having no financial conflicts of interest regarding his presentation.
A detailed listing of many of the codes and changes can be found at the American College of Radiology website, and the Society for Vascular Surgery has coding resources available on their website, as well.
CHICAGO – Current Procedural Terminology coding for endovascular aneurysm repair has been totally overhauled for 2018 with the introduction of a family of 20 new codes and codes for other vascular procedures have also been updated.
The new EVAR CPT codes attempt to capture the work involved in performing the procedures based upon the anatomy of the aneurysm and the treated vessels rather than being device-based, as previously, Matthew J. Sideman, MD, explained in presenting the coding and reimbursement for 2018 at a symposium on vascular surgery sponsored by Northwestern University.
“The new EVAR codes for 2018 have got a lot of gains. There are some losses as well, but overall, I think it’s going to be very positive moving forward,” according to Dr. Sideman, a vascular surgeon at the University of Texas, San Antonio, who serves as chair of the Society for Vascular Surgery Coding and Reimbursement Committee and an adviser to the American Medical Association Relative Value Scale Update Committee (RUC).
“What we gained was a new code for ruptured aneurysm repair, a new code for enhanced fixation, a new code for percutaneous access, new codes for alternative access options, and now all the access codes are add-on codes. But what we traded off was loss due to bundling. So catheterization is now bundled into the main procedure, radiographic supervision and interpretation is now bundled. The big thing that really hurt was we lost all proximal extensions to the renal arteries and all distal extensions to the iliac bifurcations – they’re also bundled into the main procedure,” he said.
Restructuring the EVAR codes was a multiyear collaborative project of the SVS, the American College of Surgeons, the Society of Interventional Radiology, the Society of Thoracic Surgery, the American College of Cardiology, and the Society for Cardiovascular Angiography and Interventions. The impetus was twofold: recognition that the existing codes seriously undervalued the work involved in EVAR because, for example, they didn’t distinguish between ruptured and elective aneurysm repair, nor did they recognize the unique challenges and advantages of percutaneous access.
Also, representatives of the professional societies involved with vascular medicine recognized that they had to develop a detailed proposal for coding restructuring or matters might be taken out of their hands. Bundling of codes has become the prevailing dogma at the RUC and the Centers for Medicare and Medicaid. Their current policy is that when analysis of coding patterns indicates two codes are billed together at least 51% of the time, that’s considered a ‘typical’ situation and a new code must be created combining them. The harsh reality for clinicians is that under what Dr. Sideman called “RUC math,” the new bundled codes invariably pay less than the two old ones.
“There was a little bit of smoke and mirrors – ‘Look at the pretty flashing lights and not what’s going on behind over here’ – as we tried to maintain value as we bundled these EVAR codes,” Dr. Sideman recalled. “I can stand here and tell you I did my very best to push for the best values possible. It can be a painful process, but I thought we came out ok.”
How the new EVAR codes work
Dr. Sideman explained that the impact of the new EVAR codes will depend upon a surgeon’s practice pattern.
He offered as a concrete example a patient undergoing elective EVAR of the aorta and both iliac arteries with percutaneous access and placement of a bifurcated device with one docking limb. In 2017, this might have been handled using CPT codes 34802, 36200-50, and 75952-26, for a total of 31.05 Relative Value Units (RVUs) of work.
In 2018, however, this same surgical strategy would be coded as 34705 (elective endovascular repair of infrarenal aorta and/or iliac artery or arteries) plus 34713 x 2 (percutaneous access and closure), for a total of 34.58 RVUs. Thus, the surgeon would come out 3.53 RVUs ahead in 2018, which at a conversion factor of $35.78/RVU translates to an extra $126.30.
On the other hand, if the surgeon chose to use a bifurcated device with one docking limb, a left iliac bell-bottom extension, a right iliac bell-bottom extension, and percutaneous access, in 2017, this would have been coded as 34802, 34825, 34826, 36200-50, 75952-26, and 75953-26 x 2, for a total of 44.29 RVUs of work. In 2018, this same treatment strategy would be coded as 34705 plus 34713 x 2, for a total of 34.58 RVUs, or a knockdown of 9.71 fewer RVUs compared with the year before, which translates to $347.42 less.
“The more extensions you use, the more you’re going to come out behind going forward,” according to Dr. Sideman.
Other coding changes in 2018
Sclerotherapy of single and multiple veins (codes 36470 and 36471) got down-valued from 1.10 and 2.49 to 0.75 and 1.5 RVUs, respectively.
Angiography of the extremities (75710 and 75716) will be better reimbursed in 2018. In what Dr. Sideman called “a good win,” unilateral angiography will be rated as 1.75 RVUs, up from 1.14 in 2017, while bilateral angiography increased from 1.31 to 1.97 RVUs.
“The other nice thing I can tell you is that through campaigning and lobbying and comments to CMS [Centers for Medicare & Medicaid Services], we got them to reverse their recommendations from 2017 to 2018 on the dialysis family of codes,” the surgeon continued.
Reimbursement for the dialysis codes took a big hit from 2016 to 2017, amounting to several hundred million dollars less in reimbursement, but CMS has reversed its policy on that score. The RVUs for the various dialysis codes have increased from 2017 to 2018 by 5%-21%, with central venous angioplasty (CPT 36907) garnering the biggest increase.
Existing RVUs were retained for 2018 in three of the four selective catheter placement codes. However, reimbursement for 36215 (first order catheterization of the thoracic or brachiocephalic branch) dropped from 4.67 to 4.17 RVUs because physician surveys showed the time involved was less than previously rated. Once the RUC and CMS saw that the time involved in a procedure has decreased, it became impossible to maintain the RVU, Dr. Sideman explained.
And speaking of time involved in procedures, Dr. Sideman offered a final plea to his vascular medicine colleagues:
“When you get surveys from the RUC asking for your input, please, please, please, fill them out because that’s how we get our direct physician input into the valuation of codes.”
He reported having no financial conflicts of interest regarding his presentation.
A detailed listing of many of the codes and changes can be found at the American College of Radiology website, and the Society for Vascular Surgery has coding resources available on their website, as well.
CHICAGO – Current Procedural Terminology coding for endovascular aneurysm repair has been totally overhauled for 2018 with the introduction of a family of 20 new codes and codes for other vascular procedures have also been updated.
The new EVAR CPT codes attempt to capture the work involved in performing the procedures based upon the anatomy of the aneurysm and the treated vessels rather than being device-based, as previously, Matthew J. Sideman, MD, explained in presenting the coding and reimbursement for 2018 at a symposium on vascular surgery sponsored by Northwestern University.
“The new EVAR codes for 2018 have got a lot of gains. There are some losses as well, but overall, I think it’s going to be very positive moving forward,” according to Dr. Sideman, a vascular surgeon at the University of Texas, San Antonio, who serves as chair of the Society for Vascular Surgery Coding and Reimbursement Committee and an adviser to the American Medical Association Relative Value Scale Update Committee (RUC).
“What we gained was a new code for ruptured aneurysm repair, a new code for enhanced fixation, a new code for percutaneous access, new codes for alternative access options, and now all the access codes are add-on codes. But what we traded off was loss due to bundling. So catheterization is now bundled into the main procedure, radiographic supervision and interpretation is now bundled. The big thing that really hurt was we lost all proximal extensions to the renal arteries and all distal extensions to the iliac bifurcations – they’re also bundled into the main procedure,” he said.
Restructuring the EVAR codes was a multiyear collaborative project of the SVS, the American College of Surgeons, the Society of Interventional Radiology, the Society of Thoracic Surgery, the American College of Cardiology, and the Society for Cardiovascular Angiography and Interventions. The impetus was twofold: recognition that the existing codes seriously undervalued the work involved in EVAR because, for example, they didn’t distinguish between ruptured and elective aneurysm repair, nor did they recognize the unique challenges and advantages of percutaneous access.
Also, representatives of the professional societies involved with vascular medicine recognized that they had to develop a detailed proposal for coding restructuring or matters might be taken out of their hands. Bundling of codes has become the prevailing dogma at the RUC and the Centers for Medicare and Medicaid. Their current policy is that when analysis of coding patterns indicates two codes are billed together at least 51% of the time, that’s considered a ‘typical’ situation and a new code must be created combining them. The harsh reality for clinicians is that under what Dr. Sideman called “RUC math,” the new bundled codes invariably pay less than the two old ones.
“There was a little bit of smoke and mirrors – ‘Look at the pretty flashing lights and not what’s going on behind over here’ – as we tried to maintain value as we bundled these EVAR codes,” Dr. Sideman recalled. “I can stand here and tell you I did my very best to push for the best values possible. It can be a painful process, but I thought we came out ok.”
How the new EVAR codes work
Dr. Sideman explained that the impact of the new EVAR codes will depend upon a surgeon’s practice pattern.
He offered as a concrete example a patient undergoing elective EVAR of the aorta and both iliac arteries with percutaneous access and placement of a bifurcated device with one docking limb. In 2017, this might have been handled using CPT codes 34802, 36200-50, and 75952-26, for a total of 31.05 Relative Value Units (RVUs) of work.
In 2018, however, this same surgical strategy would be coded as 34705 (elective endovascular repair of infrarenal aorta and/or iliac artery or arteries) plus 34713 x 2 (percutaneous access and closure), for a total of 34.58 RVUs. Thus, the surgeon would come out 3.53 RVUs ahead in 2018, which at a conversion factor of $35.78/RVU translates to an extra $126.30.
On the other hand, if the surgeon chose to use a bifurcated device with one docking limb, a left iliac bell-bottom extension, a right iliac bell-bottom extension, and percutaneous access, in 2017, this would have been coded as 34802, 34825, 34826, 36200-50, 75952-26, and 75953-26 x 2, for a total of 44.29 RVUs of work. In 2018, this same treatment strategy would be coded as 34705 plus 34713 x 2, for a total of 34.58 RVUs, or a knockdown of 9.71 fewer RVUs compared with the year before, which translates to $347.42 less.
“The more extensions you use, the more you’re going to come out behind going forward,” according to Dr. Sideman.
Other coding changes in 2018
Sclerotherapy of single and multiple veins (codes 36470 and 36471) got down-valued from 1.10 and 2.49 to 0.75 and 1.5 RVUs, respectively.
Angiography of the extremities (75710 and 75716) will be better reimbursed in 2018. In what Dr. Sideman called “a good win,” unilateral angiography will be rated as 1.75 RVUs, up from 1.14 in 2017, while bilateral angiography increased from 1.31 to 1.97 RVUs.
“The other nice thing I can tell you is that through campaigning and lobbying and comments to CMS [Centers for Medicare & Medicaid Services], we got them to reverse their recommendations from 2017 to 2018 on the dialysis family of codes,” the surgeon continued.
Reimbursement for the dialysis codes took a big hit from 2016 to 2017, amounting to several hundred million dollars less in reimbursement, but CMS has reversed its policy on that score. The RVUs for the various dialysis codes have increased from 2017 to 2018 by 5%-21%, with central venous angioplasty (CPT 36907) garnering the biggest increase.
Existing RVUs were retained for 2018 in three of the four selective catheter placement codes. However, reimbursement for 36215 (first order catheterization of the thoracic or brachiocephalic branch) dropped from 4.67 to 4.17 RVUs because physician surveys showed the time involved was less than previously rated. Once the RUC and CMS saw that the time involved in a procedure has decreased, it became impossible to maintain the RVU, Dr. Sideman explained.
And speaking of time involved in procedures, Dr. Sideman offered a final plea to his vascular medicine colleagues:
“When you get surveys from the RUC asking for your input, please, please, please, fill them out because that’s how we get our direct physician input into the valuation of codes.”
He reported having no financial conflicts of interest regarding his presentation.
A detailed listing of many of the codes and changes can be found at the American College of Radiology website, and the Society for Vascular Surgery has coding resources available on their website, as well.
EXPERT ANALYSIS FROM THE NORTHWESTERN VASCULAR SYMPOSIUM
Open vs. endo repair for ruptured AAA
Open repair should be offered to all patients with rAAA
With the advent of endovascular repair of abdominal aortic aneurysms (EVAR), the treatment of elective AAAs was revolutionized. Since ruptured abdominal aortic aneurysms (rAAAs) carry a higher morbidity and mortality than elective AAA repair the use of EVAR has been advocated for these patients.1 Dr. Aziz contends that EVAR should be utilized in all patients presenting with a rAAA. It is my contention that endovascular repair cannot replace open aneurysm repair in all situations. The best treatment option should be offered taking patient and institutional considerations into account. Forcing a given procedure and trying to “make it work” is not best for the patient.
In a systematic literature review of patients presenting with rAAAs, selection bias regarding treatment choice (EVAR vs. open repair) was found consistently.2 In an effort to show that EVAR is superior to open repair for rAAA, Hinchliffe et al. published a randomized trial that showed no difference in 30-day mortality (53%) in each treatment group.3 The AJAX trial randomized 116 patients and did not show benefit for EVAR with respect to 30-day morbidity or mortality.4 The ECAR trial randomized 107 patients and also failed to show a difference in mortality between EVAR and open techniques for rAAA.5
Determining suitability for EVAR includes assessing diameter of the neck of the aneurysm, angulation, size of iliac arteries, presence of atherosclerotic occlusive disease, presence of accessory renal arteries, and presence of concurrent aneurysms of the iliac arteries.7,8 In the IMPROVE trial, patients were randomized depending on anatomic suitability for EVAR.9 Anatomy was determined by imaging in those patients stable enough to undergo preoperative computed tomography angiogram (CTA). Therefore, given anatomic differences, patients presenting with rAAA were not randomized without significant treatment bias.
A true pararenal or paravisceral rupture certainly elevates the complexity of the case. Open repair can deal with this difficult challenge by adapting additional established techniques to the situation. Although some authors have advocated EVAR for rAAA using snorkels and chimneys, these techniques may not be appropriate in the treatment of rAAA in most institutions.10 These procedures take longer, require considerable experience and resources and are therefore not appropriate in unstable patients. No randomized control trial exists at this time to address superiority of EVAR to open repair in patients with complex anatomy.
Patients presenting with rAAA that have had prior endovascular intervention also pose complex anatomic and technical challenges.11 These patients can present with hemodynamic instability and rupture but now are complicated by having device failure. Salvage using endovascular means may not be possible. The risk of re-intervention with endovascular repair for rAAA is much higher than with open repair.12
Emergency vascular surgery is best approached with protocols and systems in place no matter what approach is chosen.13 Skilled staff in the emergency department and in the operating room must be available without delay especially for rAAA, as time is of the essence. Skilled surgeons, skilled operating room staff, knowledgeable anesthesia staff are necessary to quickly move a patient from the emergency department to the operating room for definitive treatment. Other ancillary services, such as blood banks and laboratories are necessary to assist in the care for the patient intraoperatively. In endovascular surgery, trained technologists, fluoroscopy, a full armamentarium of interventional equipment (wires, balloons, stents, etc.), and a full stock of stent grafts and associated ancillary equipment are mandatory. Many hospitals may not have the variety of stent grafts available for emergency use. Regionalization of care has been suggested to improve outcomes in the treatment of rAAAs.14 In a study by Warner et al., mortality was decreased by 20% at the tertiary center compared to the smaller community hospitals in both EVAR and open repairs for rAAA. Zettervall et al. published data that showed that significant regional variation exists in perioperative outcomes and length of stay, and mortality in repair for rAAA approached with open or endovascular means.15 Low volume centers have worse outcomes, and teaching hospitals may have better outcomes treating AAA.16
EVAR is also reported to be associated with a 27-36% higher cost of care than open surgery for rAAA.17 Many institutions may not have the means to provide the resources needed to support such a program.
There is no question that EVAR has greatly impacted the treatment of aortic aneurysms. However, not every aneurysm is appropriate for endovascular repair at this time. For the many reasons cited, we cannot permit open repair to become an extinct skill. Vascular training programs must include open repair of rAAA just as it should for other vascular conditions.
I would agree with Dr. Aziz that we do not yet have a prospective, randomized study and Level 1 evidence to support either view and given the complexity and urgency associated with these patients, such a study may not be forthcoming. Till then, patients with a RAAA should have ‘all of the above’ approach including open surgery depending on the institutional experience and resources and urgency of the situation.
References
1. J Vasc Surg 2016; 2:297-305
2. J Vasc Surg 2009; 49:1077-1080.
3. Eur J Vasc Endovasc Surg 2006; 32:506-513
4. Ann Surg 2013. Aug 258 (2) 248-56
5. J Vasc Surg 2010; 51:267-70
6. Ann Vasc Surg 2017; 38:59-63
7. J Vasc Surg 2009: 50:243-50
8. J Endovasc Ther 2016; 23: 919-927
9. BJM 2014; 101:216-224
10. Radiographics 2015; 35:593-615.
11. Ann Vasc Surg 2013; 27:844-50
12. J Vasc Surg 2017; 65:52-57
13. Semin Vasc Surg 2016; 29:35-40
14. J Vasc Surg 2014; 59:1512-7
15. Ann Surg 2017; 264:538-43
16. J Vasc Surg 2016; 22 pii W0741-5214 (16) 31247-2
17. J Vasc Surg 2008; 47:1165-70
Dr. Ozsvatrh is a professor of surgery at Albany Medical College, Albany, N.Y., and a vascular attending, at Albany Medical Center Hospital, Albany, and chief, department of surgery, Samaritan Hospital, Troy, N.Y.
EVAR should be offered to all patients with rAAA
Since the inception of EVAR two decades ago, it has largely replaced open abdominal aortic aneurysm repair as the operation of choice for elective treatment of abdominal aortic aneurysms. Shorter duration of operation, avoiding general anesthesia and aortic cross clamping, ability to obtain balloon control of aorta, fast recovery time and reduced hospital length of hospital stay are among the most commonly cited reasons for this change in paradigm for treatment of abdominal aortic aneurysms. Since vascular surgeons have adopted the widespread use of EVAR, the total number of aneurysm related deaths has significantly reduced.1 While EVAR has become the most commonly used operation to treat AAAs electively, it’s utility to treat ruptured AAAs has been questioned. Recent analysis of nationwide trends for the operations for the diagnosis of ruptured AAA show that almost half of the patients with ruptured AAA are still treated with open surgical repair.2
Opponents of REVAR (EVAR for rAAA) cite comparable outcomes of open surgery and REVAR in randomized controlled trials, requirement of a specific REVAR protocol, increased cost and lack of resources and more importantly, lack of level I evidence to support it’s use in all cases of rAAA.
It is no surprise that REVAR is associated with significantly lower perioperative mortality (24%) as compared to open repair of ruptured AAA (44%).3 Mortality after open repair of ruptured AAA can vary anywhere from 30-70%.4,5 Improved mortality rates after REVAR are not only limited to stable patients, but also extend to those patients with ruptured AAA who are considered hemodynamically unstable at the time of initial presentation.6
The survival advantage among REVAR patients is not only evident in short term (30-days), but it also extends up to 5 years after the operation.3 Patients undergoing REVAR are less likely to require intra-operative blood transfusions, as compared to patients who undergo open repair of rAAA.7 Development of acute renal failure after surgical treatment of rAAAs is associated with significant mortality and REVAR has been associated with significantly lower incidence of acute renal failure as compared to open repair of ruptured AAA.2
Due to inherent issues of patient instability, emergent presentation and inequality among hospital resources and patient volumes, it is difficult to design a flawless, randomized controlled trial to compare REVAR with open surgical repair. The results from published randomized controlled trials on this topic should be interpreted with caution. The Nottingham trial from the United Kingdom8 showed similar mortality (53%) between REVAR and open surgical operation, however, out of the 203 patients enrolled in the trial, 70% were not randomized and REVAR was offered to only 15 patients. Likewise, the AJAX Trial from Netherlands9 showed that there was no significant difference in mortality between the two treatment groups (42% with REVAR and 47% with open repair), however almost 80% of enrolled patients were not randomized and there was a disagreement between the interpreters about CTA diagnosis of rAAA. In addition, the conversion rates from REVAR to open repair were unexpectedly high (14%), pointing to the surgeons’ inexperience.
Similarly, the IMPROVE trial from United Kingdom10 suffered from poor rates of randomization (50% of enrolled patients) and poor methodology (obtaining CTA after randomization, and making requirement of CTA optional for patients allocated to open surgery group). The trial showed equivalent mortality rates between the two surgical groups (35% with REVAR and 37% with open repair).
Due to flawed methodology and poor rates of randomization, results of these trials do not provide us with level I evidence, which is required to make any scientific recommendations about the treatment of choice for the treatment of rAAAs. Hence, the large body of evidence, obtained from retrospective studies should be used while comparing the outcomes of operations for ruptured AAAs. So far, all retrospective analyses, comparing REVAR with open repair in national registries, such as National Inpatient Sample (NIS) database11,12 American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database7 and Medicare database13 have clearly shown that the outcomes of REVAR are better than open surgical repair of ruptured AAA. Likewise, multi-center observational studies14,15 have demonstrated superiority of REVAR over open surgical repair.
To summarize, REVAR is a safe procedure, can be performed under local anesthetic, has shorter operative time and is associated with improved outcomes as compared to open surgery. REVAR should be the treatment of choice for all patients who meet the anatomic criteria for endovascular repair. With increasing experience of vascular surgeons with the endovascular technology, it is foreseeable that REVAR will soon become the treatment of choice for ruptured abdominal aortic aneurysms.
References
1. J Vasc Surg 2009;49:543-50; discussion 50-1.
2. Ann Vasc Surg 2016;35:147-55.
3. J Vasc Surg 2013;57:368-75.
4. J Vasc Surg 2001;34:41-6.
5. J Vasc Surg 1991;13:240-5; discussion 5-7.
6. J Vasc Surg 2014;60:1439-45.
7. J Vasc Surg 2010;51:305-9 e1.
8. Eur J Vasc Endovasc Surg 2006;32:506-13; discussion 14-5.
9. Ann Surg 2013;258:248-56.
10. BMJ 2014;348:f7661.
11. J Vasc Surg 2009;49:817-26.
12. J Vasc Surg 2008;47:1165-70; discussion 70-1.
13. J Vasc Surg 2014;59:575-82.
14. Ann Surg 2012;256:688-95; discussion 95-6.
15. Ann Surg 2009;250:818-24.
Dr. Aziz is in the division of vascular surgery, Penn State Heart and Vascular Institute, Pennsylvania State University College of Medicine, Hershey, Penn.
Open repair should be offered to all patients with rAAA
With the advent of endovascular repair of abdominal aortic aneurysms (EVAR), the treatment of elective AAAs was revolutionized. Since ruptured abdominal aortic aneurysms (rAAAs) carry a higher morbidity and mortality than elective AAA repair the use of EVAR has been advocated for these patients.1 Dr. Aziz contends that EVAR should be utilized in all patients presenting with a rAAA. It is my contention that endovascular repair cannot replace open aneurysm repair in all situations. The best treatment option should be offered taking patient and institutional considerations into account. Forcing a given procedure and trying to “make it work” is not best for the patient.
In a systematic literature review of patients presenting with rAAAs, selection bias regarding treatment choice (EVAR vs. open repair) was found consistently.2 In an effort to show that EVAR is superior to open repair for rAAA, Hinchliffe et al. published a randomized trial that showed no difference in 30-day mortality (53%) in each treatment group.3 The AJAX trial randomized 116 patients and did not show benefit for EVAR with respect to 30-day morbidity or mortality.4 The ECAR trial randomized 107 patients and also failed to show a difference in mortality between EVAR and open techniques for rAAA.5
Determining suitability for EVAR includes assessing diameter of the neck of the aneurysm, angulation, size of iliac arteries, presence of atherosclerotic occlusive disease, presence of accessory renal arteries, and presence of concurrent aneurysms of the iliac arteries.7,8 In the IMPROVE trial, patients were randomized depending on anatomic suitability for EVAR.9 Anatomy was determined by imaging in those patients stable enough to undergo preoperative computed tomography angiogram (CTA). Therefore, given anatomic differences, patients presenting with rAAA were not randomized without significant treatment bias.
A true pararenal or paravisceral rupture certainly elevates the complexity of the case. Open repair can deal with this difficult challenge by adapting additional established techniques to the situation. Although some authors have advocated EVAR for rAAA using snorkels and chimneys, these techniques may not be appropriate in the treatment of rAAA in most institutions.10 These procedures take longer, require considerable experience and resources and are therefore not appropriate in unstable patients. No randomized control trial exists at this time to address superiority of EVAR to open repair in patients with complex anatomy.
Patients presenting with rAAA that have had prior endovascular intervention also pose complex anatomic and technical challenges.11 These patients can present with hemodynamic instability and rupture but now are complicated by having device failure. Salvage using endovascular means may not be possible. The risk of re-intervention with endovascular repair for rAAA is much higher than with open repair.12
Emergency vascular surgery is best approached with protocols and systems in place no matter what approach is chosen.13 Skilled staff in the emergency department and in the operating room must be available without delay especially for rAAA, as time is of the essence. Skilled surgeons, skilled operating room staff, knowledgeable anesthesia staff are necessary to quickly move a patient from the emergency department to the operating room for definitive treatment. Other ancillary services, such as blood banks and laboratories are necessary to assist in the care for the patient intraoperatively. In endovascular surgery, trained technologists, fluoroscopy, a full armamentarium of interventional equipment (wires, balloons, stents, etc.), and a full stock of stent grafts and associated ancillary equipment are mandatory. Many hospitals may not have the variety of stent grafts available for emergency use. Regionalization of care has been suggested to improve outcomes in the treatment of rAAAs.14 In a study by Warner et al., mortality was decreased by 20% at the tertiary center compared to the smaller community hospitals in both EVAR and open repairs for rAAA. Zettervall et al. published data that showed that significant regional variation exists in perioperative outcomes and length of stay, and mortality in repair for rAAA approached with open or endovascular means.15 Low volume centers have worse outcomes, and teaching hospitals may have better outcomes treating AAA.16
EVAR is also reported to be associated with a 27-36% higher cost of care than open surgery for rAAA.17 Many institutions may not have the means to provide the resources needed to support such a program.
There is no question that EVAR has greatly impacted the treatment of aortic aneurysms. However, not every aneurysm is appropriate for endovascular repair at this time. For the many reasons cited, we cannot permit open repair to become an extinct skill. Vascular training programs must include open repair of rAAA just as it should for other vascular conditions.
I would agree with Dr. Aziz that we do not yet have a prospective, randomized study and Level 1 evidence to support either view and given the complexity and urgency associated with these patients, such a study may not be forthcoming. Till then, patients with a RAAA should have ‘all of the above’ approach including open surgery depending on the institutional experience and resources and urgency of the situation.
References
1. J Vasc Surg 2016; 2:297-305
2. J Vasc Surg 2009; 49:1077-1080.
3. Eur J Vasc Endovasc Surg 2006; 32:506-513
4. Ann Surg 2013. Aug 258 (2) 248-56
5. J Vasc Surg 2010; 51:267-70
6. Ann Vasc Surg 2017; 38:59-63
7. J Vasc Surg 2009: 50:243-50
8. J Endovasc Ther 2016; 23: 919-927
9. BJM 2014; 101:216-224
10. Radiographics 2015; 35:593-615.
11. Ann Vasc Surg 2013; 27:844-50
12. J Vasc Surg 2017; 65:52-57
13. Semin Vasc Surg 2016; 29:35-40
14. J Vasc Surg 2014; 59:1512-7
15. Ann Surg 2017; 264:538-43
16. J Vasc Surg 2016; 22 pii W0741-5214 (16) 31247-2
17. J Vasc Surg 2008; 47:1165-70
Dr. Ozsvatrh is a professor of surgery at Albany Medical College, Albany, N.Y., and a vascular attending, at Albany Medical Center Hospital, Albany, and chief, department of surgery, Samaritan Hospital, Troy, N.Y.
EVAR should be offered to all patients with rAAA
Since the inception of EVAR two decades ago, it has largely replaced open abdominal aortic aneurysm repair as the operation of choice for elective treatment of abdominal aortic aneurysms. Shorter duration of operation, avoiding general anesthesia and aortic cross clamping, ability to obtain balloon control of aorta, fast recovery time and reduced hospital length of hospital stay are among the most commonly cited reasons for this change in paradigm for treatment of abdominal aortic aneurysms. Since vascular surgeons have adopted the widespread use of EVAR, the total number of aneurysm related deaths has significantly reduced.1 While EVAR has become the most commonly used operation to treat AAAs electively, it’s utility to treat ruptured AAAs has been questioned. Recent analysis of nationwide trends for the operations for the diagnosis of ruptured AAA show that almost half of the patients with ruptured AAA are still treated with open surgical repair.2
Opponents of REVAR (EVAR for rAAA) cite comparable outcomes of open surgery and REVAR in randomized controlled trials, requirement of a specific REVAR protocol, increased cost and lack of resources and more importantly, lack of level I evidence to support it’s use in all cases of rAAA.
It is no surprise that REVAR is associated with significantly lower perioperative mortality (24%) as compared to open repair of ruptured AAA (44%).3 Mortality after open repair of ruptured AAA can vary anywhere from 30-70%.4,5 Improved mortality rates after REVAR are not only limited to stable patients, but also extend to those patients with ruptured AAA who are considered hemodynamically unstable at the time of initial presentation.6
The survival advantage among REVAR patients is not only evident in short term (30-days), but it also extends up to 5 years after the operation.3 Patients undergoing REVAR are less likely to require intra-operative blood transfusions, as compared to patients who undergo open repair of rAAA.7 Development of acute renal failure after surgical treatment of rAAAs is associated with significant mortality and REVAR has been associated with significantly lower incidence of acute renal failure as compared to open repair of ruptured AAA.2
Due to inherent issues of patient instability, emergent presentation and inequality among hospital resources and patient volumes, it is difficult to design a flawless, randomized controlled trial to compare REVAR with open surgical repair. The results from published randomized controlled trials on this topic should be interpreted with caution. The Nottingham trial from the United Kingdom8 showed similar mortality (53%) between REVAR and open surgical operation, however, out of the 203 patients enrolled in the trial, 70% were not randomized and REVAR was offered to only 15 patients. Likewise, the AJAX Trial from Netherlands9 showed that there was no significant difference in mortality between the two treatment groups (42% with REVAR and 47% with open repair), however almost 80% of enrolled patients were not randomized and there was a disagreement between the interpreters about CTA diagnosis of rAAA. In addition, the conversion rates from REVAR to open repair were unexpectedly high (14%), pointing to the surgeons’ inexperience.
Similarly, the IMPROVE trial from United Kingdom10 suffered from poor rates of randomization (50% of enrolled patients) and poor methodology (obtaining CTA after randomization, and making requirement of CTA optional for patients allocated to open surgery group). The trial showed equivalent mortality rates between the two surgical groups (35% with REVAR and 37% with open repair).
Due to flawed methodology and poor rates of randomization, results of these trials do not provide us with level I evidence, which is required to make any scientific recommendations about the treatment of choice for the treatment of rAAAs. Hence, the large body of evidence, obtained from retrospective studies should be used while comparing the outcomes of operations for ruptured AAAs. So far, all retrospective analyses, comparing REVAR with open repair in national registries, such as National Inpatient Sample (NIS) database11,12 American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database7 and Medicare database13 have clearly shown that the outcomes of REVAR are better than open surgical repair of ruptured AAA. Likewise, multi-center observational studies14,15 have demonstrated superiority of REVAR over open surgical repair.
To summarize, REVAR is a safe procedure, can be performed under local anesthetic, has shorter operative time and is associated with improved outcomes as compared to open surgery. REVAR should be the treatment of choice for all patients who meet the anatomic criteria for endovascular repair. With increasing experience of vascular surgeons with the endovascular technology, it is foreseeable that REVAR will soon become the treatment of choice for ruptured abdominal aortic aneurysms.
References
1. J Vasc Surg 2009;49:543-50; discussion 50-1.
2. Ann Vasc Surg 2016;35:147-55.
3. J Vasc Surg 2013;57:368-75.
4. J Vasc Surg 2001;34:41-6.
5. J Vasc Surg 1991;13:240-5; discussion 5-7.
6. J Vasc Surg 2014;60:1439-45.
7. J Vasc Surg 2010;51:305-9 e1.
8. Eur J Vasc Endovasc Surg 2006;32:506-13; discussion 14-5.
9. Ann Surg 2013;258:248-56.
10. BMJ 2014;348:f7661.
11. J Vasc Surg 2009;49:817-26.
12. J Vasc Surg 2008;47:1165-70; discussion 70-1.
13. J Vasc Surg 2014;59:575-82.
14. Ann Surg 2012;256:688-95; discussion 95-6.
15. Ann Surg 2009;250:818-24.
Dr. Aziz is in the division of vascular surgery, Penn State Heart and Vascular Institute, Pennsylvania State University College of Medicine, Hershey, Penn.
Open repair should be offered to all patients with rAAA
With the advent of endovascular repair of abdominal aortic aneurysms (EVAR), the treatment of elective AAAs was revolutionized. Since ruptured abdominal aortic aneurysms (rAAAs) carry a higher morbidity and mortality than elective AAA repair the use of EVAR has been advocated for these patients.1 Dr. Aziz contends that EVAR should be utilized in all patients presenting with a rAAA. It is my contention that endovascular repair cannot replace open aneurysm repair in all situations. The best treatment option should be offered taking patient and institutional considerations into account. Forcing a given procedure and trying to “make it work” is not best for the patient.
In a systematic literature review of patients presenting with rAAAs, selection bias regarding treatment choice (EVAR vs. open repair) was found consistently.2 In an effort to show that EVAR is superior to open repair for rAAA, Hinchliffe et al. published a randomized trial that showed no difference in 30-day mortality (53%) in each treatment group.3 The AJAX trial randomized 116 patients and did not show benefit for EVAR with respect to 30-day morbidity or mortality.4 The ECAR trial randomized 107 patients and also failed to show a difference in mortality between EVAR and open techniques for rAAA.5
Determining suitability for EVAR includes assessing diameter of the neck of the aneurysm, angulation, size of iliac arteries, presence of atherosclerotic occlusive disease, presence of accessory renal arteries, and presence of concurrent aneurysms of the iliac arteries.7,8 In the IMPROVE trial, patients were randomized depending on anatomic suitability for EVAR.9 Anatomy was determined by imaging in those patients stable enough to undergo preoperative computed tomography angiogram (CTA). Therefore, given anatomic differences, patients presenting with rAAA were not randomized without significant treatment bias.
A true pararenal or paravisceral rupture certainly elevates the complexity of the case. Open repair can deal with this difficult challenge by adapting additional established techniques to the situation. Although some authors have advocated EVAR for rAAA using snorkels and chimneys, these techniques may not be appropriate in the treatment of rAAA in most institutions.10 These procedures take longer, require considerable experience and resources and are therefore not appropriate in unstable patients. No randomized control trial exists at this time to address superiority of EVAR to open repair in patients with complex anatomy.
Patients presenting with rAAA that have had prior endovascular intervention also pose complex anatomic and technical challenges.11 These patients can present with hemodynamic instability and rupture but now are complicated by having device failure. Salvage using endovascular means may not be possible. The risk of re-intervention with endovascular repair for rAAA is much higher than with open repair.12
Emergency vascular surgery is best approached with protocols and systems in place no matter what approach is chosen.13 Skilled staff in the emergency department and in the operating room must be available without delay especially for rAAA, as time is of the essence. Skilled surgeons, skilled operating room staff, knowledgeable anesthesia staff are necessary to quickly move a patient from the emergency department to the operating room for definitive treatment. Other ancillary services, such as blood banks and laboratories are necessary to assist in the care for the patient intraoperatively. In endovascular surgery, trained technologists, fluoroscopy, a full armamentarium of interventional equipment (wires, balloons, stents, etc.), and a full stock of stent grafts and associated ancillary equipment are mandatory. Many hospitals may not have the variety of stent grafts available for emergency use. Regionalization of care has been suggested to improve outcomes in the treatment of rAAAs.14 In a study by Warner et al., mortality was decreased by 20% at the tertiary center compared to the smaller community hospitals in both EVAR and open repairs for rAAA. Zettervall et al. published data that showed that significant regional variation exists in perioperative outcomes and length of stay, and mortality in repair for rAAA approached with open or endovascular means.15 Low volume centers have worse outcomes, and teaching hospitals may have better outcomes treating AAA.16
EVAR is also reported to be associated with a 27-36% higher cost of care than open surgery for rAAA.17 Many institutions may not have the means to provide the resources needed to support such a program.
There is no question that EVAR has greatly impacted the treatment of aortic aneurysms. However, not every aneurysm is appropriate for endovascular repair at this time. For the many reasons cited, we cannot permit open repair to become an extinct skill. Vascular training programs must include open repair of rAAA just as it should for other vascular conditions.
I would agree with Dr. Aziz that we do not yet have a prospective, randomized study and Level 1 evidence to support either view and given the complexity and urgency associated with these patients, such a study may not be forthcoming. Till then, patients with a RAAA should have ‘all of the above’ approach including open surgery depending on the institutional experience and resources and urgency of the situation.
References
1. J Vasc Surg 2016; 2:297-305
2. J Vasc Surg 2009; 49:1077-1080.
3. Eur J Vasc Endovasc Surg 2006; 32:506-513
4. Ann Surg 2013. Aug 258 (2) 248-56
5. J Vasc Surg 2010; 51:267-70
6. Ann Vasc Surg 2017; 38:59-63
7. J Vasc Surg 2009: 50:243-50
8. J Endovasc Ther 2016; 23: 919-927
9. BJM 2014; 101:216-224
10. Radiographics 2015; 35:593-615.
11. Ann Vasc Surg 2013; 27:844-50
12. J Vasc Surg 2017; 65:52-57
13. Semin Vasc Surg 2016; 29:35-40
14. J Vasc Surg 2014; 59:1512-7
15. Ann Surg 2017; 264:538-43
16. J Vasc Surg 2016; 22 pii W0741-5214 (16) 31247-2
17. J Vasc Surg 2008; 47:1165-70
Dr. Ozsvatrh is a professor of surgery at Albany Medical College, Albany, N.Y., and a vascular attending, at Albany Medical Center Hospital, Albany, and chief, department of surgery, Samaritan Hospital, Troy, N.Y.
EVAR should be offered to all patients with rAAA
Since the inception of EVAR two decades ago, it has largely replaced open abdominal aortic aneurysm repair as the operation of choice for elective treatment of abdominal aortic aneurysms. Shorter duration of operation, avoiding general anesthesia and aortic cross clamping, ability to obtain balloon control of aorta, fast recovery time and reduced hospital length of hospital stay are among the most commonly cited reasons for this change in paradigm for treatment of abdominal aortic aneurysms. Since vascular surgeons have adopted the widespread use of EVAR, the total number of aneurysm related deaths has significantly reduced.1 While EVAR has become the most commonly used operation to treat AAAs electively, it’s utility to treat ruptured AAAs has been questioned. Recent analysis of nationwide trends for the operations for the diagnosis of ruptured AAA show that almost half of the patients with ruptured AAA are still treated with open surgical repair.2
Opponents of REVAR (EVAR for rAAA) cite comparable outcomes of open surgery and REVAR in randomized controlled trials, requirement of a specific REVAR protocol, increased cost and lack of resources and more importantly, lack of level I evidence to support it’s use in all cases of rAAA.
It is no surprise that REVAR is associated with significantly lower perioperative mortality (24%) as compared to open repair of ruptured AAA (44%).3 Mortality after open repair of ruptured AAA can vary anywhere from 30-70%.4,5 Improved mortality rates after REVAR are not only limited to stable patients, but also extend to those patients with ruptured AAA who are considered hemodynamically unstable at the time of initial presentation.6
The survival advantage among REVAR patients is not only evident in short term (30-days), but it also extends up to 5 years after the operation.3 Patients undergoing REVAR are less likely to require intra-operative blood transfusions, as compared to patients who undergo open repair of rAAA.7 Development of acute renal failure after surgical treatment of rAAAs is associated with significant mortality and REVAR has been associated with significantly lower incidence of acute renal failure as compared to open repair of ruptured AAA.2
Due to inherent issues of patient instability, emergent presentation and inequality among hospital resources and patient volumes, it is difficult to design a flawless, randomized controlled trial to compare REVAR with open surgical repair. The results from published randomized controlled trials on this topic should be interpreted with caution. The Nottingham trial from the United Kingdom8 showed similar mortality (53%) between REVAR and open surgical operation, however, out of the 203 patients enrolled in the trial, 70% were not randomized and REVAR was offered to only 15 patients. Likewise, the AJAX Trial from Netherlands9 showed that there was no significant difference in mortality between the two treatment groups (42% with REVAR and 47% with open repair), however almost 80% of enrolled patients were not randomized and there was a disagreement between the interpreters about CTA diagnosis of rAAA. In addition, the conversion rates from REVAR to open repair were unexpectedly high (14%), pointing to the surgeons’ inexperience.
Similarly, the IMPROVE trial from United Kingdom10 suffered from poor rates of randomization (50% of enrolled patients) and poor methodology (obtaining CTA after randomization, and making requirement of CTA optional for patients allocated to open surgery group). The trial showed equivalent mortality rates between the two surgical groups (35% with REVAR and 37% with open repair).
Due to flawed methodology and poor rates of randomization, results of these trials do not provide us with level I evidence, which is required to make any scientific recommendations about the treatment of choice for the treatment of rAAAs. Hence, the large body of evidence, obtained from retrospective studies should be used while comparing the outcomes of operations for ruptured AAAs. So far, all retrospective analyses, comparing REVAR with open repair in national registries, such as National Inpatient Sample (NIS) database11,12 American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database7 and Medicare database13 have clearly shown that the outcomes of REVAR are better than open surgical repair of ruptured AAA. Likewise, multi-center observational studies14,15 have demonstrated superiority of REVAR over open surgical repair.
To summarize, REVAR is a safe procedure, can be performed under local anesthetic, has shorter operative time and is associated with improved outcomes as compared to open surgery. REVAR should be the treatment of choice for all patients who meet the anatomic criteria for endovascular repair. With increasing experience of vascular surgeons with the endovascular technology, it is foreseeable that REVAR will soon become the treatment of choice for ruptured abdominal aortic aneurysms.
References
1. J Vasc Surg 2009;49:543-50; discussion 50-1.
2. Ann Vasc Surg 2016;35:147-55.
3. J Vasc Surg 2013;57:368-75.
4. J Vasc Surg 2001;34:41-6.
5. J Vasc Surg 1991;13:240-5; discussion 5-7.
6. J Vasc Surg 2014;60:1439-45.
7. J Vasc Surg 2010;51:305-9 e1.
8. Eur J Vasc Endovasc Surg 2006;32:506-13; discussion 14-5.
9. Ann Surg 2013;258:248-56.
10. BMJ 2014;348:f7661.
11. J Vasc Surg 2009;49:817-26.
12. J Vasc Surg 2008;47:1165-70; discussion 70-1.
13. J Vasc Surg 2014;59:575-82.
14. Ann Surg 2012;256:688-95; discussion 95-6.
15. Ann Surg 2009;250:818-24.
Dr. Aziz is in the division of vascular surgery, Penn State Heart and Vascular Institute, Pennsylvania State University College of Medicine, Hershey, Penn.
FDA warns of endoleaks associated with endovascular grafts for AAA
The Food and Drug Administration has reported an apparent increase in device-related adverse events from the use of endovascular graft repair (EVAR) to treat abdominal aortic aneurysms (AAA).
In a Letter to Health Care Providers issued on Sept. 28, the FDA indicated that “recent information from several sources, including FDA’s Medical Device Reporting system and Annual Clinical Updates to Physicians by the manufacturers, suggests an increase in the occurrence of Type III endoleaks.”
A Type III endoleak is defined by the failure to completely exclude the AAA from blood flow, thereby allowing a systematic arterial pressurization of the aneurysm sac, increasing the risk of rupture, which is a life-threatening event.
The FDA stated that predictors of Type III endoleaks included treatment with early-generation graft materials, the presence of calcified plaque, and inadequate overlap between graft components.
Secondary interventions to treat Type III endoleaks carry their own risk of adverse events.
It is recommended that health care providers should do the following:
- Consider lifelong surveillance of patients who have been treated with EVAR.
- Consider type III endoleaks in the differential diagnosis of patients who present with symptoms of potential aneurysm expansion or rupture.
- Discuss all treatment options in depth with patients before deciding on the best treatment for Type III endoleaks.
- Report any early or late device-related adverse events, including Type IIIa and Type IIIb endoleaks, associated with EVAR, as well as any device-related adverse events that occur as the result of a secondary intervention to treat Type III endoleaks.
These events should be reported to MedWatch, using the FDA’s Safety Information and Adverse Event Reporting Program Online Voluntary Reporting Form. A form also can be requested by calling 800-332-1088.
The FDA stated that it “continues to work with all manufacturers of endovascular graft systems to better understand this issue,” and that the agency would keep the public informed when significant new information becomes available.
The Food and Drug Administration has reported an apparent increase in device-related adverse events from the use of endovascular graft repair (EVAR) to treat abdominal aortic aneurysms (AAA).
In a Letter to Health Care Providers issued on Sept. 28, the FDA indicated that “recent information from several sources, including FDA’s Medical Device Reporting system and Annual Clinical Updates to Physicians by the manufacturers, suggests an increase in the occurrence of Type III endoleaks.”
A Type III endoleak is defined by the failure to completely exclude the AAA from blood flow, thereby allowing a systematic arterial pressurization of the aneurysm sac, increasing the risk of rupture, which is a life-threatening event.
The FDA stated that predictors of Type III endoleaks included treatment with early-generation graft materials, the presence of calcified plaque, and inadequate overlap between graft components.
Secondary interventions to treat Type III endoleaks carry their own risk of adverse events.
It is recommended that health care providers should do the following:
- Consider lifelong surveillance of patients who have been treated with EVAR.
- Consider type III endoleaks in the differential diagnosis of patients who present with symptoms of potential aneurysm expansion or rupture.
- Discuss all treatment options in depth with patients before deciding on the best treatment for Type III endoleaks.
- Report any early or late device-related adverse events, including Type IIIa and Type IIIb endoleaks, associated with EVAR, as well as any device-related adverse events that occur as the result of a secondary intervention to treat Type III endoleaks.
These events should be reported to MedWatch, using the FDA’s Safety Information and Adverse Event Reporting Program Online Voluntary Reporting Form. A form also can be requested by calling 800-332-1088.
The FDA stated that it “continues to work with all manufacturers of endovascular graft systems to better understand this issue,” and that the agency would keep the public informed when significant new information becomes available.
The Food and Drug Administration has reported an apparent increase in device-related adverse events from the use of endovascular graft repair (EVAR) to treat abdominal aortic aneurysms (AAA).
In a Letter to Health Care Providers issued on Sept. 28, the FDA indicated that “recent information from several sources, including FDA’s Medical Device Reporting system and Annual Clinical Updates to Physicians by the manufacturers, suggests an increase in the occurrence of Type III endoleaks.”
A Type III endoleak is defined by the failure to completely exclude the AAA from blood flow, thereby allowing a systematic arterial pressurization of the aneurysm sac, increasing the risk of rupture, which is a life-threatening event.
The FDA stated that predictors of Type III endoleaks included treatment with early-generation graft materials, the presence of calcified plaque, and inadequate overlap between graft components.
Secondary interventions to treat Type III endoleaks carry their own risk of adverse events.
It is recommended that health care providers should do the following:
- Consider lifelong surveillance of patients who have been treated with EVAR.
- Consider type III endoleaks in the differential diagnosis of patients who present with symptoms of potential aneurysm expansion or rupture.
- Discuss all treatment options in depth with patients before deciding on the best treatment for Type III endoleaks.
- Report any early or late device-related adverse events, including Type IIIa and Type IIIb endoleaks, associated with EVAR, as well as any device-related adverse events that occur as the result of a secondary intervention to treat Type III endoleaks.
These events should be reported to MedWatch, using the FDA’s Safety Information and Adverse Event Reporting Program Online Voluntary Reporting Form. A form also can be requested by calling 800-332-1088.
The FDA stated that it “continues to work with all manufacturers of endovascular graft systems to better understand this issue,” and that the agency would keep the public informed when significant new information becomes available.
Key clinical point:
Major finding: FDA monitoring sources have detected an apparent increase in the occurrence of Type III endoleaks following EVAR.
Data source: FDA’s Medical Device Reporting System and the Annual Clinical Updates to Physicians by the manufacturers.
Disclosures: None.
EVAR registry results show equivalence between the sexes
A global registry showed that men and women had equivalent outcomes after endovascular abdominal aortic aneurysm repair (EVAR) despite significant differences in baseline characteristics, anatomy, and off-instruction stent use.
The 5-year ENGAGE (Endurant Stent Graft Natural Selection Global Postmarket Registry) data were presented by Marc Schermerhorn, MD, chief, division of vascular and endovascular surgery, Beth Israel Deaconess Medical Center, Boston, in a late-breaking clinical trial at the Vascular Interventional Advances (VIVA) 2017 conference in Las Vegas.
The registry comprises data from 1,263 patients (133 women and 1,130 men) in 30 countries who received the Endurant II stent graft during for endovascular repair of the abdominal aortic aneurysm. ENGAGE participants are consecutively enrolled, and have 30-day and subsequent yearly evaluations, with independent data monitoring and event adjudication.
Despite many other equivalent demographic and clinical characteristics, including smoking status, hypertension, diabetes, and pulmonary disease, overall women were statistically significantly older, had less cardiac disease, had shorter and more angulated aneurysm necks, and had smaller iliac arteries. In addition they were more likely to be treated outside of the Endurant II instructions for use (IFU), according to Dr. Schemerhorn.
Women also had significantly longer hospital stays than men (7.9 days vs. 6.4 days), respectively, but had equivalent procedure duration, ICU times, and similarly successful stent delivery and deployment (99%).
But despite these differences in baseline characteristics and anatomy, the 5-year data showed equivalent outcomes between women and men at 30 days, and 1 year, and through 5 years. There were no significant differences across these periods in freedom from all-cause mortality (67.5% in men, 65.6% in women, P = 0.87), 5-year freedom from aneurysm-related mortality (97.5% men, 100% women, P = .09), 5-year freedom from rupture (98.4% men, 100% women, P = .23), and 5-year freedom from conversion (97.8% men, 99.2% women, P = .48). There were also no significant differences in type 1 endoleaks, 5-year freedom from conversion, and sac diameter changes, Dr. Schermerhorn concluded.
The ENGAGE registry is sponsored by Medtronic. Dr. Schermerhorn disclosed that he was a consultant for several medical device companies and a shareholder and owner of a health care company, but that he did not have any potential conflicts of interest for this particular study.
[email protected]
A global registry showed that men and women had equivalent outcomes after endovascular abdominal aortic aneurysm repair (EVAR) despite significant differences in baseline characteristics, anatomy, and off-instruction stent use.
The 5-year ENGAGE (Endurant Stent Graft Natural Selection Global Postmarket Registry) data were presented by Marc Schermerhorn, MD, chief, division of vascular and endovascular surgery, Beth Israel Deaconess Medical Center, Boston, in a late-breaking clinical trial at the Vascular Interventional Advances (VIVA) 2017 conference in Las Vegas.
The registry comprises data from 1,263 patients (133 women and 1,130 men) in 30 countries who received the Endurant II stent graft during for endovascular repair of the abdominal aortic aneurysm. ENGAGE participants are consecutively enrolled, and have 30-day and subsequent yearly evaluations, with independent data monitoring and event adjudication.
Despite many other equivalent demographic and clinical characteristics, including smoking status, hypertension, diabetes, and pulmonary disease, overall women were statistically significantly older, had less cardiac disease, had shorter and more angulated aneurysm necks, and had smaller iliac arteries. In addition they were more likely to be treated outside of the Endurant II instructions for use (IFU), according to Dr. Schemerhorn.
Women also had significantly longer hospital stays than men (7.9 days vs. 6.4 days), respectively, but had equivalent procedure duration, ICU times, and similarly successful stent delivery and deployment (99%).
But despite these differences in baseline characteristics and anatomy, the 5-year data showed equivalent outcomes between women and men at 30 days, and 1 year, and through 5 years. There were no significant differences across these periods in freedom from all-cause mortality (67.5% in men, 65.6% in women, P = 0.87), 5-year freedom from aneurysm-related mortality (97.5% men, 100% women, P = .09), 5-year freedom from rupture (98.4% men, 100% women, P = .23), and 5-year freedom from conversion (97.8% men, 99.2% women, P = .48). There were also no significant differences in type 1 endoleaks, 5-year freedom from conversion, and sac diameter changes, Dr. Schermerhorn concluded.
The ENGAGE registry is sponsored by Medtronic. Dr. Schermerhorn disclosed that he was a consultant for several medical device companies and a shareholder and owner of a health care company, but that he did not have any potential conflicts of interest for this particular study.
[email protected]
A global registry showed that men and women had equivalent outcomes after endovascular abdominal aortic aneurysm repair (EVAR) despite significant differences in baseline characteristics, anatomy, and off-instruction stent use.
The 5-year ENGAGE (Endurant Stent Graft Natural Selection Global Postmarket Registry) data were presented by Marc Schermerhorn, MD, chief, division of vascular and endovascular surgery, Beth Israel Deaconess Medical Center, Boston, in a late-breaking clinical trial at the Vascular Interventional Advances (VIVA) 2017 conference in Las Vegas.
The registry comprises data from 1,263 patients (133 women and 1,130 men) in 30 countries who received the Endurant II stent graft during for endovascular repair of the abdominal aortic aneurysm. ENGAGE participants are consecutively enrolled, and have 30-day and subsequent yearly evaluations, with independent data monitoring and event adjudication.
Despite many other equivalent demographic and clinical characteristics, including smoking status, hypertension, diabetes, and pulmonary disease, overall women were statistically significantly older, had less cardiac disease, had shorter and more angulated aneurysm necks, and had smaller iliac arteries. In addition they were more likely to be treated outside of the Endurant II instructions for use (IFU), according to Dr. Schemerhorn.
Women also had significantly longer hospital stays than men (7.9 days vs. 6.4 days), respectively, but had equivalent procedure duration, ICU times, and similarly successful stent delivery and deployment (99%).
But despite these differences in baseline characteristics and anatomy, the 5-year data showed equivalent outcomes between women and men at 30 days, and 1 year, and through 5 years. There were no significant differences across these periods in freedom from all-cause mortality (67.5% in men, 65.6% in women, P = 0.87), 5-year freedom from aneurysm-related mortality (97.5% men, 100% women, P = .09), 5-year freedom from rupture (98.4% men, 100% women, P = .23), and 5-year freedom from conversion (97.8% men, 99.2% women, P = .48). There were also no significant differences in type 1 endoleaks, 5-year freedom from conversion, and sac diameter changes, Dr. Schermerhorn concluded.
The ENGAGE registry is sponsored by Medtronic. Dr. Schermerhorn disclosed that he was a consultant for several medical device companies and a shareholder and owner of a health care company, but that he did not have any potential conflicts of interest for this particular study.
[email protected]
FROM VIVA 17
Key clinical point:
Major finding: The 5-year data showed equivalent outcomes between women and men at 30 days, and 1 year, and through 5 years.
Data source: ENGAGE global registry data from 1,263 patients (133 women and 1,130 men).
Disclosures: The ENGAGE registry is sponsored by Medtronic. Dr. Schermerhorn reported that he had no potential conflicts of interest for this study.
Older men benefit from vascular screening
BARCELONA – Population screening for abdominal aortic aneurysms, peripheral arterial disease, and hypertension targeted to men aged 65-74 years saved lives in a highly cost-effective way in a Danish randomized study of more than 50,000 men.
During a median follow-up of 4.4 years, total mortality was 7% lower among men invited for this triple-screening panel, compared with uninvited controls – a statistically significant difference achieved without causing any identified serious adverse effects. The cost ran 2,148 euro (about $2,600) per quality adjusted year, making it very “cost attractive,” Jes S. Lindholt, DMSci, said at the annual congress of the European Society of Cardiology.
Dr. Lindholt also said that ongoing studies are assessing the clinical- and cost- effectiveness of screening for AAA and PAD in women in a targeted age range. But for the time being, “we believe the greatest benefit is in men.”
The Viborg Vascular (VIVA) screening trial (ClinicalTrials.gov NCT00662480) randomized all 50,156 men aged 65-74 years living in the central region of Denmark to either receive an invitation to triple disease screening or to receive no invitation and form the control group. Three-quarters of those invited for screening came to screening clinics at 14 regional centers. The examinations identified an AAA in 3%, PAD in 11%, and hypertension in 10%. About a third of people identified with AAA or PAD started treatment with aspirin, a statin, or both, and a small number of those with an AAA underwent surgical repair during the following 5 years. About a third of those newly diagnosed with hypertension began treatment with antihypertensive drugs.
The results showed that for every 169 men invited for screening the program saved one life during follow-up, compared with men in the control arm. “To our knowledge, no prior population-based screening program has shown an impact on overall mortality,” Dr. Lindholt said. Concurrently with his report, the results appeared online (Lancet. 2017 Aug 28. doi: 10.1016/S0140-6736(17)32250-X).
VIVA received no commercial funding. Dr. Lindholt had no disclosures.
[email protected]
On Twitter @mitchelzoler
Triple screening for abdominal aortic aneurysms, peripheral arterial disease, and hypertension is a good idea, and the new results from the VIVA trial serve as a call for broader screening initiatives.
Although the patients identified with one or more of the conditions screened received a relatively low rate of interventions, the program nonetheless produced a net benefit. The cost effectiveness of screening was very acceptable, and could potentially further improve if people identified with disease receive treatment sooner. The data showed a modest impact on quality of life, but the findings provided assurance that the screening program produced no excess adverse effects and no decrement in quality of life.

The study was also large and had a median follow-up of more than 4 years. The results also showed the risk for overdiagnosis was no worse than is seen with breast cancer screening.
Andrew M. Kates, MD , is a cardiologist and professor of medicine at Washington University in St. Louis. He had no disclosures. He made these comments as designated discussant for the VIVA trial.
Triple screening for abdominal aortic aneurysms, peripheral arterial disease, and hypertension is a good idea, and the new results from the VIVA trial serve as a call for broader screening initiatives.
Although the patients identified with one or more of the conditions screened received a relatively low rate of interventions, the program nonetheless produced a net benefit. The cost effectiveness of screening was very acceptable, and could potentially further improve if people identified with disease receive treatment sooner. The data showed a modest impact on quality of life, but the findings provided assurance that the screening program produced no excess adverse effects and no decrement in quality of life.

The study was also large and had a median follow-up of more than 4 years. The results also showed the risk for overdiagnosis was no worse than is seen with breast cancer screening.
Andrew M. Kates, MD , is a cardiologist and professor of medicine at Washington University in St. Louis. He had no disclosures. He made these comments as designated discussant for the VIVA trial.
Triple screening for abdominal aortic aneurysms, peripheral arterial disease, and hypertension is a good idea, and the new results from the VIVA trial serve as a call for broader screening initiatives.
Although the patients identified with one or more of the conditions screened received a relatively low rate of interventions, the program nonetheless produced a net benefit. The cost effectiveness of screening was very acceptable, and could potentially further improve if people identified with disease receive treatment sooner. The data showed a modest impact on quality of life, but the findings provided assurance that the screening program produced no excess adverse effects and no decrement in quality of life.

The study was also large and had a median follow-up of more than 4 years. The results also showed the risk for overdiagnosis was no worse than is seen with breast cancer screening.
Andrew M. Kates, MD , is a cardiologist and professor of medicine at Washington University in St. Louis. He had no disclosures. He made these comments as designated discussant for the VIVA trial.
BARCELONA – Population screening for abdominal aortic aneurysms, peripheral arterial disease, and hypertension targeted to men aged 65-74 years saved lives in a highly cost-effective way in a Danish randomized study of more than 50,000 men.
During a median follow-up of 4.4 years, total mortality was 7% lower among men invited for this triple-screening panel, compared with uninvited controls – a statistically significant difference achieved without causing any identified serious adverse effects. The cost ran 2,148 euro (about $2,600) per quality adjusted year, making it very “cost attractive,” Jes S. Lindholt, DMSci, said at the annual congress of the European Society of Cardiology.
Dr. Lindholt also said that ongoing studies are assessing the clinical- and cost- effectiveness of screening for AAA and PAD in women in a targeted age range. But for the time being, “we believe the greatest benefit is in men.”
The Viborg Vascular (VIVA) screening trial (ClinicalTrials.gov NCT00662480) randomized all 50,156 men aged 65-74 years living in the central region of Denmark to either receive an invitation to triple disease screening or to receive no invitation and form the control group. Three-quarters of those invited for screening came to screening clinics at 14 regional centers. The examinations identified an AAA in 3%, PAD in 11%, and hypertension in 10%. About a third of people identified with AAA or PAD started treatment with aspirin, a statin, or both, and a small number of those with an AAA underwent surgical repair during the following 5 years. About a third of those newly diagnosed with hypertension began treatment with antihypertensive drugs.
The results showed that for every 169 men invited for screening the program saved one life during follow-up, compared with men in the control arm. “To our knowledge, no prior population-based screening program has shown an impact on overall mortality,” Dr. Lindholt said. Concurrently with his report, the results appeared online (Lancet. 2017 Aug 28. doi: 10.1016/S0140-6736(17)32250-X).
VIVA received no commercial funding. Dr. Lindholt had no disclosures.
[email protected]
On Twitter @mitchelzoler
BARCELONA – Population screening for abdominal aortic aneurysms, peripheral arterial disease, and hypertension targeted to men aged 65-74 years saved lives in a highly cost-effective way in a Danish randomized study of more than 50,000 men.
During a median follow-up of 4.4 years, total mortality was 7% lower among men invited for this triple-screening panel, compared with uninvited controls – a statistically significant difference achieved without causing any identified serious adverse effects. The cost ran 2,148 euro (about $2,600) per quality adjusted year, making it very “cost attractive,” Jes S. Lindholt, DMSci, said at the annual congress of the European Society of Cardiology.
Dr. Lindholt also said that ongoing studies are assessing the clinical- and cost- effectiveness of screening for AAA and PAD in women in a targeted age range. But for the time being, “we believe the greatest benefit is in men.”
The Viborg Vascular (VIVA) screening trial (ClinicalTrials.gov NCT00662480) randomized all 50,156 men aged 65-74 years living in the central region of Denmark to either receive an invitation to triple disease screening or to receive no invitation and form the control group. Three-quarters of those invited for screening came to screening clinics at 14 regional centers. The examinations identified an AAA in 3%, PAD in 11%, and hypertension in 10%. About a third of people identified with AAA or PAD started treatment with aspirin, a statin, or both, and a small number of those with an AAA underwent surgical repair during the following 5 years. About a third of those newly diagnosed with hypertension began treatment with antihypertensive drugs.
The results showed that for every 169 men invited for screening the program saved one life during follow-up, compared with men in the control arm. “To our knowledge, no prior population-based screening program has shown an impact on overall mortality,” Dr. Lindholt said. Concurrently with his report, the results appeared online (Lancet. 2017 Aug 28. doi: 10.1016/S0140-6736(17)32250-X).
VIVA received no commercial funding. Dr. Lindholt had no disclosures.
[email protected]
On Twitter @mitchelzoler
AT THE ESC CONGRESS 2017
Key clinical point:
Major finding: Overall mortality during median follow-up of 4 years was 7% lower among men invited to screening, compared with unscreened controls.
Data source: VIVA, a randomized, multicenter trial of 50,156 Danish men.
Disclosures: VIVA received no commercial funding. Dr. Lindholt had no disclosures.
Elective open conversion after failed EVAR safer than emergent
Emergency open conversion after failed endovascular aortic aneurysm repair shows significantly higher mortality and morbidity, compared with elective conversion, according to the results of a retrospective, observational study of 31 patients at a single institution.
The primary endpoints of the study were 30-day and in-hospital mortality. Secondary endpoints included moderate to severe complications, secondary interventions, length of ICU stay, and length of hospital stay (LOS), according to I. Ben Abdallah, MD, of the Hôpital Européen Georges Pompidou and his colleagues.
During the study period, a total of 338 patients received EVAR at the institution. Of these, 31 patients underwent open conversion (19 elective, 12 emergent) after EVAR between August 2008 and September 2016. The median time from the index EVAR to the open conversion was 35 months, with the most common indications for intervention being endoleaks (24 patients, 77%), stent graft infection (3, 10%), thrombosis (3, 10%) and kinking (1, 3%). Stents removed were manufactured by various device makers, according to the report (Eur J Vasc Endovasc Surg. 2017;53:831-6).
The patient population had a mean age of 73 years and comprised 84% men. The two groups, elective and emergent, were highly similar in numerous comorbidities, with the only significant difference between them being a greater incidence of chronic renal disease among the emergent group, as compared with the elective (42% vs. 5%).
Overall in-hospital mortality was 10%, and significantly greater in emergent vs. elective conversion (25% vs. 0%). Renal and pulmonary complications were significantly higher in the emergency group (42% vs. 5% and 42% vs. 0%, respectively). There was no significant difference between elective and emergent hospital stay (14 days vs. 20 days), but ICU stay was significantly shorter for elective conversion (2 days vs. 7 days).
There were no late complications or death seen in either group after a mean follow-up of 18 months.
“In this series, open conversion seems to be significantly safer and more effective when performed electively with no mortality, a lower incidence of morbidity (renal and pulmonary), and shorter ICU stay. These results underline that close surveillance, allowing planned elective open conversion, is the key to better outcomes after failed EVAR,” the researchers concluded.
The authors reported that they had no conflicts of interest, and the study received no outside funding.
Emergency open conversion after failed endovascular aortic aneurysm repair shows significantly higher mortality and morbidity, compared with elective conversion, according to the results of a retrospective, observational study of 31 patients at a single institution.
The primary endpoints of the study were 30-day and in-hospital mortality. Secondary endpoints included moderate to severe complications, secondary interventions, length of ICU stay, and length of hospital stay (LOS), according to I. Ben Abdallah, MD, of the Hôpital Européen Georges Pompidou and his colleagues.
During the study period, a total of 338 patients received EVAR at the institution. Of these, 31 patients underwent open conversion (19 elective, 12 emergent) after EVAR between August 2008 and September 2016. The median time from the index EVAR to the open conversion was 35 months, with the most common indications for intervention being endoleaks (24 patients, 77%), stent graft infection (3, 10%), thrombosis (3, 10%) and kinking (1, 3%). Stents removed were manufactured by various device makers, according to the report (Eur J Vasc Endovasc Surg. 2017;53:831-6).
The patient population had a mean age of 73 years and comprised 84% men. The two groups, elective and emergent, were highly similar in numerous comorbidities, with the only significant difference between them being a greater incidence of chronic renal disease among the emergent group, as compared with the elective (42% vs. 5%).
Overall in-hospital mortality was 10%, and significantly greater in emergent vs. elective conversion (25% vs. 0%). Renal and pulmonary complications were significantly higher in the emergency group (42% vs. 5% and 42% vs. 0%, respectively). There was no significant difference between elective and emergent hospital stay (14 days vs. 20 days), but ICU stay was significantly shorter for elective conversion (2 days vs. 7 days).
There were no late complications or death seen in either group after a mean follow-up of 18 months.
“In this series, open conversion seems to be significantly safer and more effective when performed electively with no mortality, a lower incidence of morbidity (renal and pulmonary), and shorter ICU stay. These results underline that close surveillance, allowing planned elective open conversion, is the key to better outcomes after failed EVAR,” the researchers concluded.
The authors reported that they had no conflicts of interest, and the study received no outside funding.
Emergency open conversion after failed endovascular aortic aneurysm repair shows significantly higher mortality and morbidity, compared with elective conversion, according to the results of a retrospective, observational study of 31 patients at a single institution.
The primary endpoints of the study were 30-day and in-hospital mortality. Secondary endpoints included moderate to severe complications, secondary interventions, length of ICU stay, and length of hospital stay (LOS), according to I. Ben Abdallah, MD, of the Hôpital Européen Georges Pompidou and his colleagues.
During the study period, a total of 338 patients received EVAR at the institution. Of these, 31 patients underwent open conversion (19 elective, 12 emergent) after EVAR between August 2008 and September 2016. The median time from the index EVAR to the open conversion was 35 months, with the most common indications for intervention being endoleaks (24 patients, 77%), stent graft infection (3, 10%), thrombosis (3, 10%) and kinking (1, 3%). Stents removed were manufactured by various device makers, according to the report (Eur J Vasc Endovasc Surg. 2017;53:831-6).
The patient population had a mean age of 73 years and comprised 84% men. The two groups, elective and emergent, were highly similar in numerous comorbidities, with the only significant difference between them being a greater incidence of chronic renal disease among the emergent group, as compared with the elective (42% vs. 5%).
Overall in-hospital mortality was 10%, and significantly greater in emergent vs. elective conversion (25% vs. 0%). Renal and pulmonary complications were significantly higher in the emergency group (42% vs. 5% and 42% vs. 0%, respectively). There was no significant difference between elective and emergent hospital stay (14 days vs. 20 days), but ICU stay was significantly shorter for elective conversion (2 days vs. 7 days).
There were no late complications or death seen in either group after a mean follow-up of 18 months.
“In this series, open conversion seems to be significantly safer and more effective when performed electively with no mortality, a lower incidence of morbidity (renal and pulmonary), and shorter ICU stay. These results underline that close surveillance, allowing planned elective open conversion, is the key to better outcomes after failed EVAR,” the researchers concluded.
The authors reported that they had no conflicts of interest, and the study received no outside funding.
FROM THE EUROPEAN JOURNAL OF VASCULAR AND ENDOVASCULAR SURGERY
Key clinical point:
Major finding: Overall in-hospital mortality was 10% and significantly greater in emergent vs. elective conversion (25% vs. 0%).
Data source: A retrospective database analysis of 31 patients undergoing EVAR open conversion at a single institution.
Disclosures: The authors reported that they had no conflicts of interest, and the study received no outside funding.
Very-low-volume vascular surgery practice linked to worse outcomes
The very-low-volume practice of surgeons performing no more than one open abdominal aortic aneurysm repair (OAR) or carotid endarterectomy (CEA) per year has persisted in New York State and was associated with worse postoperative outcomes and longer lengths of stay in a cohort study of statewide hospital data.
The study examined inpatient data on elective OARs and CEAs performed from 2000 to 2014 in every hospital in the state.
While the numbers and proportions of very-low-volume surgeons decreased (44.6%-23% for OAR and 35.2%-18.1% for CEA) and the number of procedures performed by these surgeons also decreased (QAR, 346-47; CEA, 395-90), the data are “concerning” and elucidate the “persistence” of very-low-volume practice in open vascular surgery, said Jialin Mao, MD, of Cornell University, New York, and associates (JAMA Surg. doi: 10:1001/jamasurg.2017.1100).
Very-low-volume surgeons were significantly less likely to be vascular surgeons, compared with higher-volume surgeons for both OAR (23.9% vs. 63.9%) and CEA (14.6% vs. 51.7%), they reported.
Compared with patients treated by higher-volume surgeons, those whose OAR was performed by very-low-volume surgeons had a twofold higher risk of postoperative death (6.7% vs. 3.5%) after adjusting for patient risk factors, surgeon specialty, and facility characteristics. Patients of very-low-volume surgeons also had significantly higher odds of sepsis or shock (odds ratio, 1.45), prolonged length of stay (OR, 1.37) and 30-day readmission (OR, 1.19), although the latter was not significant.
Similarly, patients whose CEA was performed by very-low-volume surgeons had a significant 1.8-fold higher odds of experiencing postoperative acute myocardial infarction (1.5% vs. 0.5%) and stroke (3.5% vs. 2.1%). They also were significantly more likely to have 30-day readmission (OR, 1.30).
With both procedures, patients treated by very-low-volume surgeons tended to be younger and healthier (less likely to have two or more comorbidities). They also were more likely to be nonwhite or insured by Medicaid.
“It is reasonable to speculate,” the researchers wrote, “that those treated by very-low-volume surgeons were more likely to be socioeconomically disadvantaged.”
Notably, 30% of the very-low-volume practice occurred in New York City, “where accessibility to high-volume practitioners should generally be higher,” they said.
The findings “indicate the need to eliminate this type of practice, to restrict the practice of these very-low-volume surgeons or to force referrals to higher-volume and specialized surgeons, and to improve disparity in access to high-quality care for all patients,” they said.
The study was funded in part by the U.S. Food and Drug Administration. The researchers reported having no relevant conflicts of interest.
The delineation of a threshold number of cases of OAR and CEA below which surgeons should not be credentialed remains unclear, despite much discussion of the volume-outcome relationship in vascular surgery.
In the current endovascular era, OAR in particular has become increasingly less frequent, with a dramatic effect on trainee experiences. It is often proposed that these cases be limited to high-volume surgeons. Some are concerned, however, that this action will leave rural surgeons unprepared to deal with ruptured abdominal aortic aneurysm and will force patients to travel long distances.
Sarah E. Deery, MD, and Marc L. Schermerhorn, MD, are in the division of vascular and endovascular surgery at Beth Israel Deaconess Medical Center in Boston. These remarks are adapted from an editorial accompanying the study. They reported having no disclosures.
The delineation of a threshold number of cases of OAR and CEA below which surgeons should not be credentialed remains unclear, despite much discussion of the volume-outcome relationship in vascular surgery.
In the current endovascular era, OAR in particular has become increasingly less frequent, with a dramatic effect on trainee experiences. It is often proposed that these cases be limited to high-volume surgeons. Some are concerned, however, that this action will leave rural surgeons unprepared to deal with ruptured abdominal aortic aneurysm and will force patients to travel long distances.
Sarah E. Deery, MD, and Marc L. Schermerhorn, MD, are in the division of vascular and endovascular surgery at Beth Israel Deaconess Medical Center in Boston. These remarks are adapted from an editorial accompanying the study. They reported having no disclosures.
The delineation of a threshold number of cases of OAR and CEA below which surgeons should not be credentialed remains unclear, despite much discussion of the volume-outcome relationship in vascular surgery.
In the current endovascular era, OAR in particular has become increasingly less frequent, with a dramatic effect on trainee experiences. It is often proposed that these cases be limited to high-volume surgeons. Some are concerned, however, that this action will leave rural surgeons unprepared to deal with ruptured abdominal aortic aneurysm and will force patients to travel long distances.
Sarah E. Deery, MD, and Marc L. Schermerhorn, MD, are in the division of vascular and endovascular surgery at Beth Israel Deaconess Medical Center in Boston. These remarks are adapted from an editorial accompanying the study. They reported having no disclosures.
The very-low-volume practice of surgeons performing no more than one open abdominal aortic aneurysm repair (OAR) or carotid endarterectomy (CEA) per year has persisted in New York State and was associated with worse postoperative outcomes and longer lengths of stay in a cohort study of statewide hospital data.
The study examined inpatient data on elective OARs and CEAs performed from 2000 to 2014 in every hospital in the state.
While the numbers and proportions of very-low-volume surgeons decreased (44.6%-23% for OAR and 35.2%-18.1% for CEA) and the number of procedures performed by these surgeons also decreased (QAR, 346-47; CEA, 395-90), the data are “concerning” and elucidate the “persistence” of very-low-volume practice in open vascular surgery, said Jialin Mao, MD, of Cornell University, New York, and associates (JAMA Surg. doi: 10:1001/jamasurg.2017.1100).
Very-low-volume surgeons were significantly less likely to be vascular surgeons, compared with higher-volume surgeons for both OAR (23.9% vs. 63.9%) and CEA (14.6% vs. 51.7%), they reported.
Compared with patients treated by higher-volume surgeons, those whose OAR was performed by very-low-volume surgeons had a twofold higher risk of postoperative death (6.7% vs. 3.5%) after adjusting for patient risk factors, surgeon specialty, and facility characteristics. Patients of very-low-volume surgeons also had significantly higher odds of sepsis or shock (odds ratio, 1.45), prolonged length of stay (OR, 1.37) and 30-day readmission (OR, 1.19), although the latter was not significant.
Similarly, patients whose CEA was performed by very-low-volume surgeons had a significant 1.8-fold higher odds of experiencing postoperative acute myocardial infarction (1.5% vs. 0.5%) and stroke (3.5% vs. 2.1%). They also were significantly more likely to have 30-day readmission (OR, 1.30).
With both procedures, patients treated by very-low-volume surgeons tended to be younger and healthier (less likely to have two or more comorbidities). They also were more likely to be nonwhite or insured by Medicaid.
“It is reasonable to speculate,” the researchers wrote, “that those treated by very-low-volume surgeons were more likely to be socioeconomically disadvantaged.”
Notably, 30% of the very-low-volume practice occurred in New York City, “where accessibility to high-volume practitioners should generally be higher,” they said.
The findings “indicate the need to eliminate this type of practice, to restrict the practice of these very-low-volume surgeons or to force referrals to higher-volume and specialized surgeons, and to improve disparity in access to high-quality care for all patients,” they said.
The study was funded in part by the U.S. Food and Drug Administration. The researchers reported having no relevant conflicts of interest.
The very-low-volume practice of surgeons performing no more than one open abdominal aortic aneurysm repair (OAR) or carotid endarterectomy (CEA) per year has persisted in New York State and was associated with worse postoperative outcomes and longer lengths of stay in a cohort study of statewide hospital data.
The study examined inpatient data on elective OARs and CEAs performed from 2000 to 2014 in every hospital in the state.
While the numbers and proportions of very-low-volume surgeons decreased (44.6%-23% for OAR and 35.2%-18.1% for CEA) and the number of procedures performed by these surgeons also decreased (QAR, 346-47; CEA, 395-90), the data are “concerning” and elucidate the “persistence” of very-low-volume practice in open vascular surgery, said Jialin Mao, MD, of Cornell University, New York, and associates (JAMA Surg. doi: 10:1001/jamasurg.2017.1100).
Very-low-volume surgeons were significantly less likely to be vascular surgeons, compared with higher-volume surgeons for both OAR (23.9% vs. 63.9%) and CEA (14.6% vs. 51.7%), they reported.
Compared with patients treated by higher-volume surgeons, those whose OAR was performed by very-low-volume surgeons had a twofold higher risk of postoperative death (6.7% vs. 3.5%) after adjusting for patient risk factors, surgeon specialty, and facility characteristics. Patients of very-low-volume surgeons also had significantly higher odds of sepsis or shock (odds ratio, 1.45), prolonged length of stay (OR, 1.37) and 30-day readmission (OR, 1.19), although the latter was not significant.
Similarly, patients whose CEA was performed by very-low-volume surgeons had a significant 1.8-fold higher odds of experiencing postoperative acute myocardial infarction (1.5% vs. 0.5%) and stroke (3.5% vs. 2.1%). They also were significantly more likely to have 30-day readmission (OR, 1.30).
With both procedures, patients treated by very-low-volume surgeons tended to be younger and healthier (less likely to have two or more comorbidities). They also were more likely to be nonwhite or insured by Medicaid.
“It is reasonable to speculate,” the researchers wrote, “that those treated by very-low-volume surgeons were more likely to be socioeconomically disadvantaged.”
Notably, 30% of the very-low-volume practice occurred in New York City, “where accessibility to high-volume practitioners should generally be higher,” they said.
The findings “indicate the need to eliminate this type of practice, to restrict the practice of these very-low-volume surgeons or to force referrals to higher-volume and specialized surgeons, and to improve disparity in access to high-quality care for all patients,” they said.
The study was funded in part by the U.S. Food and Drug Administration. The researchers reported having no relevant conflicts of interest.
FROM JAMA SURGERY
Key clinical point: The very-low-volume practice of open abdominal aortic aneurysm repair and carotid endarterectomy (one or fewer annual procedures) is associated with worse postoperative outcomes and greater length of stay.
Major finding: Patients whose procedure was performed by very-low-volume surgeons had a twofold higher risk of postoperative death after OAR or 1.8-fold higher odds of experiencing postoperative acute myocardial infarction or stroke after CEA.
Data source: The study was funded in part by the U.S. Food and Drug Administration.
Disclosures: The researchers reported having no relevant conflicts of interest.

















