User login
Groups release guidelines for CAR T treatment in children
emphasize the need for a flexible approach to detect early signs of serious complications for younger patients treated with this emerging class of medicines.
Researchers at the University of Texas MD Anderson Cancer Center, Houston, and the Pediatric Acute Lung Injury and Sepsis Investigators Network (PALISI) developed the guidelines, which were published in Nature Reviews Clinical Oncology. The recommendations build on the guidelines for more general use of these medicines from MD Anderson’s CARTOX Program, which Nature Reviews Clinical Oncology published in 2017.
Among the chief concerns with this new class of medicines are cytokine-release syndrome (CRS) and CAR T cell-related encephalopathy syndrome (CRES), according to Kris Michael Mahadeo, MD MPH, of the MD Anderson Cancer Center and his coauthors of the new paper.
Some of the tools used for older patients in screening for complications with CAR T drugs don’t work as well with younger ones, Dr. Mahadeo said in an interview. For instance, at MD Anderson, a handwriting sample is used to monitor patients for CAR T cell-related encephalopathy syndrome, which has symptoms of confusion and delirium. Patients provide a baseline handwriting sample of a single sentence that’s scanned into the medical record, and then they are asked to write this again during their time in the hospital, he said. But this tool may not work for children too young to write well.
The new guidelines suggest using the Cornell Assessment of Pediatric Delirium (CAPD) or to evaluate a child’s mental state, asking questions about eye contact, and level of awareness and mood, Dr. Mahadeo said. An alternative for patients aged 12 years and older with greater cognitive ability is the CARTOX-10 grading system.
“The nurses who spent most of the day with these patients will observe them over their shift and kind of get an idea of what was normal and answer a series of questions” through the CAPD tool, which is already used in ICUs, Dr. Mahadeo said. “It takes into consideration both the nurses’ perception and the parents, or whoever is at the bedside with the child. So that if they have a concern, it gives them a point that actually escalates things upward.”
The newly published recommendations also remind physicians and others caring for young patients to pay attention to these reports.
“Parent and/or caregiver concerns should be addressed because early signs or symptoms of CRS can be subtle and best recognized by those who know the child best,” Dr. Mahadeo and his colleagues wrote in a summary of key recommendations in the paper.
The recommendations also noted a need for close monitoring for complications such as hypotension, hypocalcemia, and catheter-related pain in young patients who require a leukapheresis catheter for cell collection. Infant and younger children “might not verbalize these symptoms,” according to the researchers.
Other recommendations include:
- Obtaining the child’s assent when appropriate, with psychological services often aiding in this goal. Dr. Mahadeo and his colleagues recommend considering “age-appropriate advance directives.”
- Maintaining high vigilance for sinus tachycardia as an early sign of CRS, using age-specific normal range or baseline values.
- Giving pediatric dosing of tocilizumab, with patients weighing less than 30 kg receiving 12 mg/kg, and those weighing 30 kg or greater receiving 8 mg/kg.
- Considering participation with a prospective collaboration with intensive-care registries that could allow accurate data entry of cell-therapy variables into the Center for International Blood and Marrow Transplant Research registry by cell-therapy programs.
The Food and Drug Administration approved the first two CAR T-cell therapies in the United States in 2017: Novartis’ tisagenlecleucel (Kymriah) for children and young adults with B-cell precursor acute lymphoblastic leukemia and later for adults with large B-cell lymphoma; and axicabtagene ciloleucel (Yescarta), sold by Gilead, for adults with large B-cell lymphoma. The therapies involve reengineering a patient’s T cells such that they recognize the threat of cancer, and then introducing them back into the body. The European Medicines Agency’s Committee for Medicinal Products for Human Use in June recommended granting marketing authorization to these drugs.
In the new pediatric guidelines, Dr. Mahadeo and his colleagues noted the use of CAR T-cell therapies for treatment of solid tumors and other malignancies in children already “is being explored.” “Moreover, consideration of earlier or upfront use of CAR T-cell therapy might spare patients the acute and long-term toxicities associated with traditional chemotherapy and/or radiation regimens,” they wrote.
There’s been great interest in learning how to most safely use the CAR T cell therapies, said Helen Heslop, MD, of Baylor College of Medicine.
She pointed to a 2014 publication in the journal Blood from Daniel W. Lee and his colleagues as an earlier example of this research. By now, cancer centers will have worked out their own procedures for pediatric use of CAR T therapies, hewing to standards set by the Foundation for the Accreditation of Cellular Therapy (FACT), Dr. Heslop said.
Dr. Heslop also stressed the role of the FDA in requiring risk evaluation and management strategy programs for these drugs. All of this, including the new guidelines from Dr. Mahadeo and his colleagues, is part of a growing body of research into safe use of CAR T therapies, Dr. Heslop said.
“It’s an active area of research,” she said. “Most centers will look at all of it and then develop what works best in their own individual center for providing the best care for the patients.”
The newly published guidelines could prove an “important contribution” to managing the risk of CAR T therapies, Phyllis I. Warkentin, MD, chief medical officer for FACT, said in an interview, while stressing that they were not more or less important than other similar efforts. Physicians learning how to use the CAR T therapies may welcome new input, as most of what’s been published has been about adults, she said.
“You don’t have the luxury of a lot of time to be learning on the job, so to speak,” with CAR T therapies, she said. “Many of the toxicities are fairly severe and fairly sudden.”
Dr. Heslop has been on advisory board for Gilead and Novartis. Dr. Warkentin and Dr. Mahadeo each reported having no financial disclosures. Other authors of the guidelines paper reported a patent with applications in the field of gene-modified T cell therapy for cancer, as well as financial ties to Cellectis, NexImmune, Torque Pharma, Kite Pharma (a Gilead company), Poseida Therapeutics, Celgene, Novartis, and Unum Therapeutics.
SOURCE: Mahadeo KM et al. Nat Rev Clin Oncol. 2018 Aug 6. doi: 10.1038/s41571-018-0075-2.
emphasize the need for a flexible approach to detect early signs of serious complications for younger patients treated with this emerging class of medicines.
Researchers at the University of Texas MD Anderson Cancer Center, Houston, and the Pediatric Acute Lung Injury and Sepsis Investigators Network (PALISI) developed the guidelines, which were published in Nature Reviews Clinical Oncology. The recommendations build on the guidelines for more general use of these medicines from MD Anderson’s CARTOX Program, which Nature Reviews Clinical Oncology published in 2017.
Among the chief concerns with this new class of medicines are cytokine-release syndrome (CRS) and CAR T cell-related encephalopathy syndrome (CRES), according to Kris Michael Mahadeo, MD MPH, of the MD Anderson Cancer Center and his coauthors of the new paper.
Some of the tools used for older patients in screening for complications with CAR T drugs don’t work as well with younger ones, Dr. Mahadeo said in an interview. For instance, at MD Anderson, a handwriting sample is used to monitor patients for CAR T cell-related encephalopathy syndrome, which has symptoms of confusion and delirium. Patients provide a baseline handwriting sample of a single sentence that’s scanned into the medical record, and then they are asked to write this again during their time in the hospital, he said. But this tool may not work for children too young to write well.
The new guidelines suggest using the Cornell Assessment of Pediatric Delirium (CAPD) or to evaluate a child’s mental state, asking questions about eye contact, and level of awareness and mood, Dr. Mahadeo said. An alternative for patients aged 12 years and older with greater cognitive ability is the CARTOX-10 grading system.
“The nurses who spent most of the day with these patients will observe them over their shift and kind of get an idea of what was normal and answer a series of questions” through the CAPD tool, which is already used in ICUs, Dr. Mahadeo said. “It takes into consideration both the nurses’ perception and the parents, or whoever is at the bedside with the child. So that if they have a concern, it gives them a point that actually escalates things upward.”
The newly published recommendations also remind physicians and others caring for young patients to pay attention to these reports.
“Parent and/or caregiver concerns should be addressed because early signs or symptoms of CRS can be subtle and best recognized by those who know the child best,” Dr. Mahadeo and his colleagues wrote in a summary of key recommendations in the paper.
The recommendations also noted a need for close monitoring for complications such as hypotension, hypocalcemia, and catheter-related pain in young patients who require a leukapheresis catheter for cell collection. Infant and younger children “might not verbalize these symptoms,” according to the researchers.
Other recommendations include:
- Obtaining the child’s assent when appropriate, with psychological services often aiding in this goal. Dr. Mahadeo and his colleagues recommend considering “age-appropriate advance directives.”
- Maintaining high vigilance for sinus tachycardia as an early sign of CRS, using age-specific normal range or baseline values.
- Giving pediatric dosing of tocilizumab, with patients weighing less than 30 kg receiving 12 mg/kg, and those weighing 30 kg or greater receiving 8 mg/kg.
- Considering participation with a prospective collaboration with intensive-care registries that could allow accurate data entry of cell-therapy variables into the Center for International Blood and Marrow Transplant Research registry by cell-therapy programs.
The Food and Drug Administration approved the first two CAR T-cell therapies in the United States in 2017: Novartis’ tisagenlecleucel (Kymriah) for children and young adults with B-cell precursor acute lymphoblastic leukemia and later for adults with large B-cell lymphoma; and axicabtagene ciloleucel (Yescarta), sold by Gilead, for adults with large B-cell lymphoma. The therapies involve reengineering a patient’s T cells such that they recognize the threat of cancer, and then introducing them back into the body. The European Medicines Agency’s Committee for Medicinal Products for Human Use in June recommended granting marketing authorization to these drugs.
In the new pediatric guidelines, Dr. Mahadeo and his colleagues noted the use of CAR T-cell therapies for treatment of solid tumors and other malignancies in children already “is being explored.” “Moreover, consideration of earlier or upfront use of CAR T-cell therapy might spare patients the acute and long-term toxicities associated with traditional chemotherapy and/or radiation regimens,” they wrote.
There’s been great interest in learning how to most safely use the CAR T cell therapies, said Helen Heslop, MD, of Baylor College of Medicine.
She pointed to a 2014 publication in the journal Blood from Daniel W. Lee and his colleagues as an earlier example of this research. By now, cancer centers will have worked out their own procedures for pediatric use of CAR T therapies, hewing to standards set by the Foundation for the Accreditation of Cellular Therapy (FACT), Dr. Heslop said.
Dr. Heslop also stressed the role of the FDA in requiring risk evaluation and management strategy programs for these drugs. All of this, including the new guidelines from Dr. Mahadeo and his colleagues, is part of a growing body of research into safe use of CAR T therapies, Dr. Heslop said.
“It’s an active area of research,” she said. “Most centers will look at all of it and then develop what works best in their own individual center for providing the best care for the patients.”
The newly published guidelines could prove an “important contribution” to managing the risk of CAR T therapies, Phyllis I. Warkentin, MD, chief medical officer for FACT, said in an interview, while stressing that they were not more or less important than other similar efforts. Physicians learning how to use the CAR T therapies may welcome new input, as most of what’s been published has been about adults, she said.
“You don’t have the luxury of a lot of time to be learning on the job, so to speak,” with CAR T therapies, she said. “Many of the toxicities are fairly severe and fairly sudden.”
Dr. Heslop has been on advisory board for Gilead and Novartis. Dr. Warkentin and Dr. Mahadeo each reported having no financial disclosures. Other authors of the guidelines paper reported a patent with applications in the field of gene-modified T cell therapy for cancer, as well as financial ties to Cellectis, NexImmune, Torque Pharma, Kite Pharma (a Gilead company), Poseida Therapeutics, Celgene, Novartis, and Unum Therapeutics.
SOURCE: Mahadeo KM et al. Nat Rev Clin Oncol. 2018 Aug 6. doi: 10.1038/s41571-018-0075-2.
emphasize the need for a flexible approach to detect early signs of serious complications for younger patients treated with this emerging class of medicines.
Researchers at the University of Texas MD Anderson Cancer Center, Houston, and the Pediatric Acute Lung Injury and Sepsis Investigators Network (PALISI) developed the guidelines, which were published in Nature Reviews Clinical Oncology. The recommendations build on the guidelines for more general use of these medicines from MD Anderson’s CARTOX Program, which Nature Reviews Clinical Oncology published in 2017.
Among the chief concerns with this new class of medicines are cytokine-release syndrome (CRS) and CAR T cell-related encephalopathy syndrome (CRES), according to Kris Michael Mahadeo, MD MPH, of the MD Anderson Cancer Center and his coauthors of the new paper.
Some of the tools used for older patients in screening for complications with CAR T drugs don’t work as well with younger ones, Dr. Mahadeo said in an interview. For instance, at MD Anderson, a handwriting sample is used to monitor patients for CAR T cell-related encephalopathy syndrome, which has symptoms of confusion and delirium. Patients provide a baseline handwriting sample of a single sentence that’s scanned into the medical record, and then they are asked to write this again during their time in the hospital, he said. But this tool may not work for children too young to write well.
The new guidelines suggest using the Cornell Assessment of Pediatric Delirium (CAPD) or to evaluate a child’s mental state, asking questions about eye contact, and level of awareness and mood, Dr. Mahadeo said. An alternative for patients aged 12 years and older with greater cognitive ability is the CARTOX-10 grading system.
“The nurses who spent most of the day with these patients will observe them over their shift and kind of get an idea of what was normal and answer a series of questions” through the CAPD tool, which is already used in ICUs, Dr. Mahadeo said. “It takes into consideration both the nurses’ perception and the parents, or whoever is at the bedside with the child. So that if they have a concern, it gives them a point that actually escalates things upward.”
The newly published recommendations also remind physicians and others caring for young patients to pay attention to these reports.
“Parent and/or caregiver concerns should be addressed because early signs or symptoms of CRS can be subtle and best recognized by those who know the child best,” Dr. Mahadeo and his colleagues wrote in a summary of key recommendations in the paper.
The recommendations also noted a need for close monitoring for complications such as hypotension, hypocalcemia, and catheter-related pain in young patients who require a leukapheresis catheter for cell collection. Infant and younger children “might not verbalize these symptoms,” according to the researchers.
Other recommendations include:
- Obtaining the child’s assent when appropriate, with psychological services often aiding in this goal. Dr. Mahadeo and his colleagues recommend considering “age-appropriate advance directives.”
- Maintaining high vigilance for sinus tachycardia as an early sign of CRS, using age-specific normal range or baseline values.
- Giving pediatric dosing of tocilizumab, with patients weighing less than 30 kg receiving 12 mg/kg, and those weighing 30 kg or greater receiving 8 mg/kg.
- Considering participation with a prospective collaboration with intensive-care registries that could allow accurate data entry of cell-therapy variables into the Center for International Blood and Marrow Transplant Research registry by cell-therapy programs.
The Food and Drug Administration approved the first two CAR T-cell therapies in the United States in 2017: Novartis’ tisagenlecleucel (Kymriah) for children and young adults with B-cell precursor acute lymphoblastic leukemia and later for adults with large B-cell lymphoma; and axicabtagene ciloleucel (Yescarta), sold by Gilead, for adults with large B-cell lymphoma. The therapies involve reengineering a patient’s T cells such that they recognize the threat of cancer, and then introducing them back into the body. The European Medicines Agency’s Committee for Medicinal Products for Human Use in June recommended granting marketing authorization to these drugs.
In the new pediatric guidelines, Dr. Mahadeo and his colleagues noted the use of CAR T-cell therapies for treatment of solid tumors and other malignancies in children already “is being explored.” “Moreover, consideration of earlier or upfront use of CAR T-cell therapy might spare patients the acute and long-term toxicities associated with traditional chemotherapy and/or radiation regimens,” they wrote.
There’s been great interest in learning how to most safely use the CAR T cell therapies, said Helen Heslop, MD, of Baylor College of Medicine.
She pointed to a 2014 publication in the journal Blood from Daniel W. Lee and his colleagues as an earlier example of this research. By now, cancer centers will have worked out their own procedures for pediatric use of CAR T therapies, hewing to standards set by the Foundation for the Accreditation of Cellular Therapy (FACT), Dr. Heslop said.
Dr. Heslop also stressed the role of the FDA in requiring risk evaluation and management strategy programs for these drugs. All of this, including the new guidelines from Dr. Mahadeo and his colleagues, is part of a growing body of research into safe use of CAR T therapies, Dr. Heslop said.
“It’s an active area of research,” she said. “Most centers will look at all of it and then develop what works best in their own individual center for providing the best care for the patients.”
The newly published guidelines could prove an “important contribution” to managing the risk of CAR T therapies, Phyllis I. Warkentin, MD, chief medical officer for FACT, said in an interview, while stressing that they were not more or less important than other similar efforts. Physicians learning how to use the CAR T therapies may welcome new input, as most of what’s been published has been about adults, she said.
“You don’t have the luxury of a lot of time to be learning on the job, so to speak,” with CAR T therapies, she said. “Many of the toxicities are fairly severe and fairly sudden.”
Dr. Heslop has been on advisory board for Gilead and Novartis. Dr. Warkentin and Dr. Mahadeo each reported having no financial disclosures. Other authors of the guidelines paper reported a patent with applications in the field of gene-modified T cell therapy for cancer, as well as financial ties to Cellectis, NexImmune, Torque Pharma, Kite Pharma (a Gilead company), Poseida Therapeutics, Celgene, Novartis, and Unum Therapeutics.
SOURCE: Mahadeo KM et al. Nat Rev Clin Oncol. 2018 Aug 6. doi: 10.1038/s41571-018-0075-2.
FROM NATURE REVIEWS CLINICAL ONCOLOGY
Key clinical point: Multidisciplinary approach aids in managing CAR T-cell therapy’s severe potential toxicities in children.
Major finding: The guideline calls for pediatric dosing of tocilizumab, with patients weighing less than 30 kg receiving 12 mg/kg, and those weighing 30 kg or greater receiving 8 mg/kg.
Study details: Consensus guidelines on the care of children receiving CAR T-cell therapy from the Pediatric Acute Lung Injury and Sepsis Investigators and the MD Anderson Cancer Center CARTOX program.
Disclosures: Dr. Mahadeo reported having no financial disclosures. Other coauthors reported a patent with applications in the field of gene-modified T cell therapy for cancer, as well as financial ties to Cellectis, NexImmune, Torque Pharma, Kite Pharma (a Gilead company), Poseida Therapeutics, Celgene, Novartis, and Unum Therapeutics.
Source: Mahadeo KM et al. Nat Rev Clin Oncol. 2018 Aug 6. doi: 10.1038/s41571-018-0075-2.
Drug could be repurposed for T-ALL
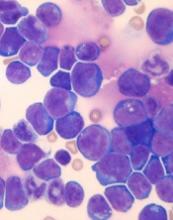
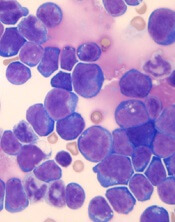
Venetoclax might improve the treatment of certain patients with T-cell acute lymphoblastic leukemia (T-ALL), according to preclinical research published in Leukemia.
Researchers found that a ribosomal defect—the R98S mutation in ribosomal protein L10 (RPL10 R98S)—causes overexpression of BCL-2 in T-ALL.
The BCL-2 inhibitor venetoclax induced apoptosis of RPL10 R98S T-ALL cells and inhibited leukemia progression in mouse models of RPL10 R98S T-ALL.
The researchers therefore believe venetoclax could be used, in combination with other drugs, to treat T-ALL patients with RPL10 R98S.
“In the past couple of years, it has become clear that ribosome defects play a role in different types of cancer,” said study author Kim De Keersmaecker, PhD, of KU Leuven in Leuven, Belgium.
“In the case of a ribosome defect, the cells still produce proteins, but the balance between their quantities is slightly off, which leads to cancer.”
Dr De Keersmaecker and her colleagues noted that RPL10 R98S affects 8% of pediatric patients with T-ALL.
With this study, the researchers found that RPL10 R98S mutant cells were more resilient than wild-type (WT) cells. In overgrowth condition, Ba/F3 RPL10 R98S mutant cells “displayed a clear survival benefit” over RPL10 WT cells.
Likewise, RPL10 R98S Jurkat cells exhibited a survival benefit over WT Jurkat cells in overgrowth condition. And RPL10 R98S Jurkat cells were more resistant to treatment with doxorubicin.
Dr De Keersmaecker and her colleagues said the increased survival they observed in RPL10 R98S mutant cells is associated with enhanced BCL-2 expression. So the team decided to test a BCL-2 inhibitor in RPL10 R98S leukemic cells.
In vitro, venetoclax induced slightly more apoptosis in Jurkat RPL10 R98S cells than WT Jurkat cells. In vivo, venetoclax induced apoptosis in RPL10 R98S T-ALL cells but not WT T-ALL cells.
The researchers also found that venetoclax could re-sensitize RPL10 R98S cells to doxorubicin.
Finally, the team injected RPL10 WT and R98S samples from pediatric T-ALL patients into mice and treated the animals with DMSO or venetoclax (50 mg/kg) once a week.
Venetoclax had very little effect on the RPL10 WT mice. Percentages of human CD45 T-ALL cells in the peripheral blood were similar whether mice received DMSO or venetoclax.
However, in the RPL10 R98S mice, those that received DMSO experienced disease progression, while there were no signs of leukemia progression in the peripheral blood of mice that received venetoclax.
The splenomegaly observed in DMSO-treated mice was “almost completely suppressed” in mice that received venetoclax, according to the researchers.
The team also said they observed a 30% to 50% suppression of human CD45 leukemia cell engraftment in the bone marrow and the presence of 30% to 40% mouse CD45 cells in mice treated with venetoclax.
On the other hand, mice treated with DMSO had more than 95% human leukemia infiltration in the bone marrow and no mouse CD45-expressing cells.
Dr De Keersmaecker and her colleagues said these results suggest RPL10 R98S pediatric T-ALL is sensitive to BCL-2 targeted therapies such as venetoclax. However, venetoclax alone would not be sufficient to treat this type of T-ALL.
“Patients with leukemia often get a drug cocktail, while our study only tested the BCL-2 inhibitor,” Dr De Keersmaecker said. “That’s why our follow-up study will focus on a cocktail of this BCL-2 inhibitor and other drugs. For patients with the ribosome defect analyzed in our study, this avenue is definitely worth examining in greater detail.”
Venetoclax might improve the treatment of certain patients with T-cell acute lymphoblastic leukemia (T-ALL), according to preclinical research published in Leukemia.
Researchers found that a ribosomal defect—the R98S mutation in ribosomal protein L10 (RPL10 R98S)—causes overexpression of BCL-2 in T-ALL.
The BCL-2 inhibitor venetoclax induced apoptosis of RPL10 R98S T-ALL cells and inhibited leukemia progression in mouse models of RPL10 R98S T-ALL.
The researchers therefore believe venetoclax could be used, in combination with other drugs, to treat T-ALL patients with RPL10 R98S.
“In the past couple of years, it has become clear that ribosome defects play a role in different types of cancer,” said study author Kim De Keersmaecker, PhD, of KU Leuven in Leuven, Belgium.
“In the case of a ribosome defect, the cells still produce proteins, but the balance between their quantities is slightly off, which leads to cancer.”
Dr De Keersmaecker and her colleagues noted that RPL10 R98S affects 8% of pediatric patients with T-ALL.
With this study, the researchers found that RPL10 R98S mutant cells were more resilient than wild-type (WT) cells. In overgrowth condition, Ba/F3 RPL10 R98S mutant cells “displayed a clear survival benefit” over RPL10 WT cells.
Likewise, RPL10 R98S Jurkat cells exhibited a survival benefit over WT Jurkat cells in overgrowth condition. And RPL10 R98S Jurkat cells were more resistant to treatment with doxorubicin.
Dr De Keersmaecker and her colleagues said the increased survival they observed in RPL10 R98S mutant cells is associated with enhanced BCL-2 expression. So the team decided to test a BCL-2 inhibitor in RPL10 R98S leukemic cells.
In vitro, venetoclax induced slightly more apoptosis in Jurkat RPL10 R98S cells than WT Jurkat cells. In vivo, venetoclax induced apoptosis in RPL10 R98S T-ALL cells but not WT T-ALL cells.
The researchers also found that venetoclax could re-sensitize RPL10 R98S cells to doxorubicin.
Finally, the team injected RPL10 WT and R98S samples from pediatric T-ALL patients into mice and treated the animals with DMSO or venetoclax (50 mg/kg) once a week.
Venetoclax had very little effect on the RPL10 WT mice. Percentages of human CD45 T-ALL cells in the peripheral blood were similar whether mice received DMSO or venetoclax.
However, in the RPL10 R98S mice, those that received DMSO experienced disease progression, while there were no signs of leukemia progression in the peripheral blood of mice that received venetoclax.
The splenomegaly observed in DMSO-treated mice was “almost completely suppressed” in mice that received venetoclax, according to the researchers.
The team also said they observed a 30% to 50% suppression of human CD45 leukemia cell engraftment in the bone marrow and the presence of 30% to 40% mouse CD45 cells in mice treated with venetoclax.
On the other hand, mice treated with DMSO had more than 95% human leukemia infiltration in the bone marrow and no mouse CD45-expressing cells.
Dr De Keersmaecker and her colleagues said these results suggest RPL10 R98S pediatric T-ALL is sensitive to BCL-2 targeted therapies such as venetoclax. However, venetoclax alone would not be sufficient to treat this type of T-ALL.
“Patients with leukemia often get a drug cocktail, while our study only tested the BCL-2 inhibitor,” Dr De Keersmaecker said. “That’s why our follow-up study will focus on a cocktail of this BCL-2 inhibitor and other drugs. For patients with the ribosome defect analyzed in our study, this avenue is definitely worth examining in greater detail.”
Venetoclax might improve the treatment of certain patients with T-cell acute lymphoblastic leukemia (T-ALL), according to preclinical research published in Leukemia.
Researchers found that a ribosomal defect—the R98S mutation in ribosomal protein L10 (RPL10 R98S)—causes overexpression of BCL-2 in T-ALL.
The BCL-2 inhibitor venetoclax induced apoptosis of RPL10 R98S T-ALL cells and inhibited leukemia progression in mouse models of RPL10 R98S T-ALL.
The researchers therefore believe venetoclax could be used, in combination with other drugs, to treat T-ALL patients with RPL10 R98S.
“In the past couple of years, it has become clear that ribosome defects play a role in different types of cancer,” said study author Kim De Keersmaecker, PhD, of KU Leuven in Leuven, Belgium.
“In the case of a ribosome defect, the cells still produce proteins, but the balance between their quantities is slightly off, which leads to cancer.”
Dr De Keersmaecker and her colleagues noted that RPL10 R98S affects 8% of pediatric patients with T-ALL.
With this study, the researchers found that RPL10 R98S mutant cells were more resilient than wild-type (WT) cells. In overgrowth condition, Ba/F3 RPL10 R98S mutant cells “displayed a clear survival benefit” over RPL10 WT cells.
Likewise, RPL10 R98S Jurkat cells exhibited a survival benefit over WT Jurkat cells in overgrowth condition. And RPL10 R98S Jurkat cells were more resistant to treatment with doxorubicin.
Dr De Keersmaecker and her colleagues said the increased survival they observed in RPL10 R98S mutant cells is associated with enhanced BCL-2 expression. So the team decided to test a BCL-2 inhibitor in RPL10 R98S leukemic cells.
In vitro, venetoclax induced slightly more apoptosis in Jurkat RPL10 R98S cells than WT Jurkat cells. In vivo, venetoclax induced apoptosis in RPL10 R98S T-ALL cells but not WT T-ALL cells.
The researchers also found that venetoclax could re-sensitize RPL10 R98S cells to doxorubicin.
Finally, the team injected RPL10 WT and R98S samples from pediatric T-ALL patients into mice and treated the animals with DMSO or venetoclax (50 mg/kg) once a week.
Venetoclax had very little effect on the RPL10 WT mice. Percentages of human CD45 T-ALL cells in the peripheral blood were similar whether mice received DMSO or venetoclax.
However, in the RPL10 R98S mice, those that received DMSO experienced disease progression, while there were no signs of leukemia progression in the peripheral blood of mice that received venetoclax.
The splenomegaly observed in DMSO-treated mice was “almost completely suppressed” in mice that received venetoclax, according to the researchers.
The team also said they observed a 30% to 50% suppression of human CD45 leukemia cell engraftment in the bone marrow and the presence of 30% to 40% mouse CD45 cells in mice treated with venetoclax.
On the other hand, mice treated with DMSO had more than 95% human leukemia infiltration in the bone marrow and no mouse CD45-expressing cells.
Dr De Keersmaecker and her colleagues said these results suggest RPL10 R98S pediatric T-ALL is sensitive to BCL-2 targeted therapies such as venetoclax. However, venetoclax alone would not be sufficient to treat this type of T-ALL.
“Patients with leukemia often get a drug cocktail, while our study only tested the BCL-2 inhibitor,” Dr De Keersmaecker said. “That’s why our follow-up study will focus on a cocktail of this BCL-2 inhibitor and other drugs. For patients with the ribosome defect analyzed in our study, this avenue is definitely worth examining in greater detail.”
Treatment guidelines for CAR T-cell therapy
Researchers have developed treatment guidelines for pediatric patients receiving chimeric antigen receptor (CAR) T-cell therapy.
The guidelines include recommendations for patient selection and consent, treatment details, and advice on managing cytokine release syndrome (CRS) and other adverse events associated with CAR T-cell therapy.
The guidelines were published in Nature Reviews Clinical Oncology.
“CAR T-cell therapy has been associated with remarkable response rates for children and young adults with ALL [acute lymphoblastic leukemia], yet this innovative form of cellular immunotherapy has resulted in unique and severe toxicities which can lead to rapid cardiorespiratory and/or neurological deterioration,” said guidelines author Kris Mahadeo, MD, of The University of Texas MD Anderson Cancer Center in Houston.
“This novel therapy requires the medical vigilance of a diverse multi-disciplinary team and associated clinical infrastructure to ensure optimal patient outcomes.”
Pediatric patient selection and consent
The guidelines state that providers of CAR T-cell therapies should adhere to product information labels and guidance from risk evaluation and mitigation strategy programs (level of evidence: IV, grade: D).
In addition, patient selection should be based on the indications approved by the US Food and Drug Administration and criteria used in pivotal studies. However, this can change as new information becomes available (level of evidence: IV, grade: D).
Informed consent should include descriptions of the risks and benefits associated with leukapheresis, lymphodepletion, CRS, CAR T-cell-related encephalopathy syndrome (CRES), bridging chemotherapy, intensive care support, and anti-IL-6 therapy (level of evidence: IIA, grade: B).
Providers should obtain child assent when appropriate and may benefit from incorporating child life and psychological services in assent discussions (level of evidence: IV, grade: D).
Treatment specifics
The guidelines recommend cyclophosphamide–fludarabine regimens for lymphodepletion, although exceptions can be considered in cases of hemorrhagic cystitis and/or resistance to a prior cyclophosphamide-based regimen (level of evidence: IIA, grade: B).
Providers should consider inpatient admission for a minimum of 3 to 7 days after receipt of tisagenlecleucel. This was based on the experience in pediatric and young adult patients with CD19+ relapsed and/or refractory B-cell acute lymphoblastic leukemia (level of evidence: IIA, grade: B).
Patients should be closely monitored for hypotension, hypocalcemia, and catheter-related pain during leukapheresis (level of evidence: IIA, grade: B).
For patients receiving tocilizumab, those weighing <30 kg should receive 12 mg/kg, and those weighing ≥30 kg should receive 8 mg/kg (level of evidence: IIA, grade: B).
Adverse events
The guidelines say parent and/or caregiver concerns should be addressed as these individuals may be best equipped to recognize early signs or symptoms of CRS (level of evidence: III, grade: C).
When CAR T-cell therapy is administered in an outpatient setting, there should be a low threshold for patient admission upon the development of signs or symptoms suggestive of CRS and/or CRES (level of evidence: IIA, grade: B).
CRS grading should be performed at least once every 12 hours (level of evidence: IIA, grade: B). Detailed information on grading is provided in the guidelines.
Providers should suspect CRS if any of the following signs/symptoms are present within the first 2 weeks of CAR T-cell infusion:
- Fever ≥38 °C
- Hypotension
- Hypoxia with an arterial oxygen saturation of <90% on room air
- Evidence of organ toxicity as determined by the most recent CTCAE grading system and considerations detailed in the guidelines (level of evidence: IIA, grade: C).
The guidelines also recommend “high vigilance” for sinus tachycardia as an early sign of CRS (level of evidence: IIA, grade: B) as well as application of the PALICC (Pediatric Acute Lung Injury Consensus Conference) at-risk P-ARDS (pediatric acute respiratory distress syndrome) criteria for the CRS grading of hypoxia (level of evidence: IIA, grade: B).
Hemophagocytic lymphohistiocytosis and/or macrophage-activation syndrome can be treated with anti-IL-6 therapy and corticosteroids. However, refractory cases may require systemic and/or intrathecal therapy or use of the IL-1 receptor antagonist anakinra (level of evidence: IIA, grade: C).
The guidelines recommend that delirium screening be performed at least twice per 24-hour period among admitted patients and at least daily among outpatients during the high-risk periods for CRES (level of evidence: IIA, grade: C). Delirium screening should be performed with the CAPD (Cornell Assessment of Pediatric Delirium) tool or CARTOX-10 (CAR T-Cell Therapy-Associated Toxicity 10-point assessment scale) for patients age 12 and older who have sufficient cognitive abilities.
Acute kidney injury in children can be graded according to the CTCAE (Common Terminology Criteria for Adverse Events) using pRIFLE (Pediatric Risk, Injury, Failure, Loss, End-Stage Renal Disease) and KDIGO (Kidney Disease: Improving Global Outcomes) definitions of oliguria (level of evidence: IIA, grade: B).
Other considerations
The guidelines “strongly encourage” consideration of quality-adjusted life-years gained for pediatric patients who might achieve long-term remission from CAR T-cell therapy and encourage efforts to reduce the cost of care (level of evidence: IV, grade: D).
The guidelines also recommend that CAR T-cell programs seek FACT IEC (Foundation for the Accreditation of Cellular Therapy for Immune Effector Cells) accreditation to ensure adherence to quality standards (level of evidence: IV, grade: D).
Finally, the guidelines suggest the possibility of a prospective collaboration with intensive-care registries, which could allow accurate data entry of cell therapy variables into the CIBMTR registry with concurrent entry of intensive-care variables into an appropriate registry by pediatric critical care teams (level of evidence: IV, grade: D).
Researchers have developed treatment guidelines for pediatric patients receiving chimeric antigen receptor (CAR) T-cell therapy.
The guidelines include recommendations for patient selection and consent, treatment details, and advice on managing cytokine release syndrome (CRS) and other adverse events associated with CAR T-cell therapy.
The guidelines were published in Nature Reviews Clinical Oncology.
“CAR T-cell therapy has been associated with remarkable response rates for children and young adults with ALL [acute lymphoblastic leukemia], yet this innovative form of cellular immunotherapy has resulted in unique and severe toxicities which can lead to rapid cardiorespiratory and/or neurological deterioration,” said guidelines author Kris Mahadeo, MD, of The University of Texas MD Anderson Cancer Center in Houston.
“This novel therapy requires the medical vigilance of a diverse multi-disciplinary team and associated clinical infrastructure to ensure optimal patient outcomes.”
Pediatric patient selection and consent
The guidelines state that providers of CAR T-cell therapies should adhere to product information labels and guidance from risk evaluation and mitigation strategy programs (level of evidence: IV, grade: D).
In addition, patient selection should be based on the indications approved by the US Food and Drug Administration and criteria used in pivotal studies. However, this can change as new information becomes available (level of evidence: IV, grade: D).
Informed consent should include descriptions of the risks and benefits associated with leukapheresis, lymphodepletion, CRS, CAR T-cell-related encephalopathy syndrome (CRES), bridging chemotherapy, intensive care support, and anti-IL-6 therapy (level of evidence: IIA, grade: B).
Providers should obtain child assent when appropriate and may benefit from incorporating child life and psychological services in assent discussions (level of evidence: IV, grade: D).
Treatment specifics
The guidelines recommend cyclophosphamide–fludarabine regimens for lymphodepletion, although exceptions can be considered in cases of hemorrhagic cystitis and/or resistance to a prior cyclophosphamide-based regimen (level of evidence: IIA, grade: B).
Providers should consider inpatient admission for a minimum of 3 to 7 days after receipt of tisagenlecleucel. This was based on the experience in pediatric and young adult patients with CD19+ relapsed and/or refractory B-cell acute lymphoblastic leukemia (level of evidence: IIA, grade: B).
Patients should be closely monitored for hypotension, hypocalcemia, and catheter-related pain during leukapheresis (level of evidence: IIA, grade: B).
For patients receiving tocilizumab, those weighing <30 kg should receive 12 mg/kg, and those weighing ≥30 kg should receive 8 mg/kg (level of evidence: IIA, grade: B).
Adverse events
The guidelines say parent and/or caregiver concerns should be addressed as these individuals may be best equipped to recognize early signs or symptoms of CRS (level of evidence: III, grade: C).
When CAR T-cell therapy is administered in an outpatient setting, there should be a low threshold for patient admission upon the development of signs or symptoms suggestive of CRS and/or CRES (level of evidence: IIA, grade: B).
CRS grading should be performed at least once every 12 hours (level of evidence: IIA, grade: B). Detailed information on grading is provided in the guidelines.
Providers should suspect CRS if any of the following signs/symptoms are present within the first 2 weeks of CAR T-cell infusion:
- Fever ≥38 °C
- Hypotension
- Hypoxia with an arterial oxygen saturation of <90% on room air
- Evidence of organ toxicity as determined by the most recent CTCAE grading system and considerations detailed in the guidelines (level of evidence: IIA, grade: C).
The guidelines also recommend “high vigilance” for sinus tachycardia as an early sign of CRS (level of evidence: IIA, grade: B) as well as application of the PALICC (Pediatric Acute Lung Injury Consensus Conference) at-risk P-ARDS (pediatric acute respiratory distress syndrome) criteria for the CRS grading of hypoxia (level of evidence: IIA, grade: B).
Hemophagocytic lymphohistiocytosis and/or macrophage-activation syndrome can be treated with anti-IL-6 therapy and corticosteroids. However, refractory cases may require systemic and/or intrathecal therapy or use of the IL-1 receptor antagonist anakinra (level of evidence: IIA, grade: C).
The guidelines recommend that delirium screening be performed at least twice per 24-hour period among admitted patients and at least daily among outpatients during the high-risk periods for CRES (level of evidence: IIA, grade: C). Delirium screening should be performed with the CAPD (Cornell Assessment of Pediatric Delirium) tool or CARTOX-10 (CAR T-Cell Therapy-Associated Toxicity 10-point assessment scale) for patients age 12 and older who have sufficient cognitive abilities.
Acute kidney injury in children can be graded according to the CTCAE (Common Terminology Criteria for Adverse Events) using pRIFLE (Pediatric Risk, Injury, Failure, Loss, End-Stage Renal Disease) and KDIGO (Kidney Disease: Improving Global Outcomes) definitions of oliguria (level of evidence: IIA, grade: B).
Other considerations
The guidelines “strongly encourage” consideration of quality-adjusted life-years gained for pediatric patients who might achieve long-term remission from CAR T-cell therapy and encourage efforts to reduce the cost of care (level of evidence: IV, grade: D).
The guidelines also recommend that CAR T-cell programs seek FACT IEC (Foundation for the Accreditation of Cellular Therapy for Immune Effector Cells) accreditation to ensure adherence to quality standards (level of evidence: IV, grade: D).
Finally, the guidelines suggest the possibility of a prospective collaboration with intensive-care registries, which could allow accurate data entry of cell therapy variables into the CIBMTR registry with concurrent entry of intensive-care variables into an appropriate registry by pediatric critical care teams (level of evidence: IV, grade: D).
Researchers have developed treatment guidelines for pediatric patients receiving chimeric antigen receptor (CAR) T-cell therapy.
The guidelines include recommendations for patient selection and consent, treatment details, and advice on managing cytokine release syndrome (CRS) and other adverse events associated with CAR T-cell therapy.
The guidelines were published in Nature Reviews Clinical Oncology.
“CAR T-cell therapy has been associated with remarkable response rates for children and young adults with ALL [acute lymphoblastic leukemia], yet this innovative form of cellular immunotherapy has resulted in unique and severe toxicities which can lead to rapid cardiorespiratory and/or neurological deterioration,” said guidelines author Kris Mahadeo, MD, of The University of Texas MD Anderson Cancer Center in Houston.
“This novel therapy requires the medical vigilance of a diverse multi-disciplinary team and associated clinical infrastructure to ensure optimal patient outcomes.”
Pediatric patient selection and consent
The guidelines state that providers of CAR T-cell therapies should adhere to product information labels and guidance from risk evaluation and mitigation strategy programs (level of evidence: IV, grade: D).
In addition, patient selection should be based on the indications approved by the US Food and Drug Administration and criteria used in pivotal studies. However, this can change as new information becomes available (level of evidence: IV, grade: D).
Informed consent should include descriptions of the risks and benefits associated with leukapheresis, lymphodepletion, CRS, CAR T-cell-related encephalopathy syndrome (CRES), bridging chemotherapy, intensive care support, and anti-IL-6 therapy (level of evidence: IIA, grade: B).
Providers should obtain child assent when appropriate and may benefit from incorporating child life and psychological services in assent discussions (level of evidence: IV, grade: D).
Treatment specifics
The guidelines recommend cyclophosphamide–fludarabine regimens for lymphodepletion, although exceptions can be considered in cases of hemorrhagic cystitis and/or resistance to a prior cyclophosphamide-based regimen (level of evidence: IIA, grade: B).
Providers should consider inpatient admission for a minimum of 3 to 7 days after receipt of tisagenlecleucel. This was based on the experience in pediatric and young adult patients with CD19+ relapsed and/or refractory B-cell acute lymphoblastic leukemia (level of evidence: IIA, grade: B).
Patients should be closely monitored for hypotension, hypocalcemia, and catheter-related pain during leukapheresis (level of evidence: IIA, grade: B).
For patients receiving tocilizumab, those weighing <30 kg should receive 12 mg/kg, and those weighing ≥30 kg should receive 8 mg/kg (level of evidence: IIA, grade: B).
Adverse events
The guidelines say parent and/or caregiver concerns should be addressed as these individuals may be best equipped to recognize early signs or symptoms of CRS (level of evidence: III, grade: C).
When CAR T-cell therapy is administered in an outpatient setting, there should be a low threshold for patient admission upon the development of signs or symptoms suggestive of CRS and/or CRES (level of evidence: IIA, grade: B).
CRS grading should be performed at least once every 12 hours (level of evidence: IIA, grade: B). Detailed information on grading is provided in the guidelines.
Providers should suspect CRS if any of the following signs/symptoms are present within the first 2 weeks of CAR T-cell infusion:
- Fever ≥38 °C
- Hypotension
- Hypoxia with an arterial oxygen saturation of <90% on room air
- Evidence of organ toxicity as determined by the most recent CTCAE grading system and considerations detailed in the guidelines (level of evidence: IIA, grade: C).
The guidelines also recommend “high vigilance” for sinus tachycardia as an early sign of CRS (level of evidence: IIA, grade: B) as well as application of the PALICC (Pediatric Acute Lung Injury Consensus Conference) at-risk P-ARDS (pediatric acute respiratory distress syndrome) criteria for the CRS grading of hypoxia (level of evidence: IIA, grade: B).
Hemophagocytic lymphohistiocytosis and/or macrophage-activation syndrome can be treated with anti-IL-6 therapy and corticosteroids. However, refractory cases may require systemic and/or intrathecal therapy or use of the IL-1 receptor antagonist anakinra (level of evidence: IIA, grade: C).
The guidelines recommend that delirium screening be performed at least twice per 24-hour period among admitted patients and at least daily among outpatients during the high-risk periods for CRES (level of evidence: IIA, grade: C). Delirium screening should be performed with the CAPD (Cornell Assessment of Pediatric Delirium) tool or CARTOX-10 (CAR T-Cell Therapy-Associated Toxicity 10-point assessment scale) for patients age 12 and older who have sufficient cognitive abilities.
Acute kidney injury in children can be graded according to the CTCAE (Common Terminology Criteria for Adverse Events) using pRIFLE (Pediatric Risk, Injury, Failure, Loss, End-Stage Renal Disease) and KDIGO (Kidney Disease: Improving Global Outcomes) definitions of oliguria (level of evidence: IIA, grade: B).
Other considerations
The guidelines “strongly encourage” consideration of quality-adjusted life-years gained for pediatric patients who might achieve long-term remission from CAR T-cell therapy and encourage efforts to reduce the cost of care (level of evidence: IV, grade: D).
The guidelines also recommend that CAR T-cell programs seek FACT IEC (Foundation for the Accreditation of Cellular Therapy for Immune Effector Cells) accreditation to ensure adherence to quality standards (level of evidence: IV, grade: D).
Finally, the guidelines suggest the possibility of a prospective collaboration with intensive-care registries, which could allow accurate data entry of cell therapy variables into the CIBMTR registry with concurrent entry of intensive-care variables into an appropriate registry by pediatric critical care teams (level of evidence: IV, grade: D).
Adult CCSs report financial hardships
Health-related financial hardship is common among adult survivors of childhood cancer, according to a study published in the Journal of the National Cancer Institute.
Researchers analyzed more than 2800 long-term childhood cancer survivors (CCSs) and found that 65% had financial challenges related to their cancer diagnosis.
“These findings suggest primary care doctors and oncologists should routinely screen childhood cancer survivors for possible financial hardship,” said I-Chan Huang, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Specifically, Dr Huang recommends that healthcare providers routinely ask CCSs if they are unable to purchase medications, ever skip appointments for economic reasons, or worry about how to pay their medical bills.
For this study, Dr Huang and his colleagues analyzed data from 2811 CCSs. The subjects had a mean age of 31.8 (range, 18 to 65) and were a mean of 23.6 years from cancer diagnosis. Most (57.8%) had been diagnosed with hematologic malignancies, 32.0% with solid tumors, and 10.1% with central nervous system malignancies.
All subjects had been treated at St. Jude and enrolled in the St. Jude LIFE study. Participants return to St. Jude periodically for several days of clinical and functional assessments. Data for this study were collected during the CCSs’ first St. Jude LIFE evaluations.
Assessing hardship
The researchers measured 3 types of financial hardship—material, psychological, and coping/behavioral.
About 1 in 5 CCSs (22.4%) reported material financial hardship. In other words, their cancer had an impact on their financial situation.
More than half of CCSs (51.1%) reported psychological hardship—concern about their ability to pay for medical expenses.
And 33% of CCSs reported coping/behavioral hardship—an inability to see a doctor or go to the hospital due to finances.
Roughly 65% of CCSs reported at least 1 type of financial hardship.
All 3 types of hardship were significantly associated with somatization (all P<0.001), anxiety (all P<0.001), depression (all P<0.001), suicidal thoughts (all P<0.05), and difficulty in retirement planning (all P<0.001).
Furthermore, CCSs who reported financial hardship had significantly lower health-related quality of life (P<0.001 for all 3 domains), sensation abnormality (all P<0.001), pulmonary symptoms (all P<0.05), and cardiac symptoms (all P<0.05).
Predicting hardship
Intensive cancer treatment, chronic health conditions, second cancers, age at the time of study evaluation, education level, and annual household income were all significantly associated with a greater risk of financial hardship.
CCSs age 40 and older had an increased risk of psychological and coping/behavioral hardship (P<0.001 for both domains).
CCSs with an annual household income of less than $40,000 had an increased risk of material, psychological, and coping/behavioral hardship, compared to CCSs with an income of $80,000 or more (P<0.001 for all domains).
CCSs who did not obtain a high school diploma had an increased risk of material (P<0.001), psychological (P<0.01), and coping/behavioral hardship (P<0.001) compared to college graduates.
CCSs who received cancer treatments associated with a high-risk disease burden (vs low-risk) had an increased risk of material (P=0.01) and psychological (P=0.004) hardship.
Health conditions associated with material financial hardship included grade 2-4 myocardial infarction (P<0.001), peripheral neuropathy (P<0.001), subsequent neoplasm (P<0.001), seizure (P=0.007), reproductive disorders (P=0.01), stroke (P=0.02), amputation (P=0.02), upper gastrointestinal disease (P=0.04), and hearing loss (P=0.05).
Grade 2-4 myocardial infarction and reproductive disorders were significantly associated with psychological financial hardship (P=0.02 for both).
“Severe late effects that emerge early in life and disrupt education and training opportunities are a double hit for survivors,” Dr Huang said. “These health problems decrease the survivors’ earning mobility and financial security later in life. The phenomenon leaves them at risk for poor health and psychological outcomes compared to healthier survivors.”
Health-related financial hardship is common among adult survivors of childhood cancer, according to a study published in the Journal of the National Cancer Institute.
Researchers analyzed more than 2800 long-term childhood cancer survivors (CCSs) and found that 65% had financial challenges related to their cancer diagnosis.
“These findings suggest primary care doctors and oncologists should routinely screen childhood cancer survivors for possible financial hardship,” said I-Chan Huang, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Specifically, Dr Huang recommends that healthcare providers routinely ask CCSs if they are unable to purchase medications, ever skip appointments for economic reasons, or worry about how to pay their medical bills.
For this study, Dr Huang and his colleagues analyzed data from 2811 CCSs. The subjects had a mean age of 31.8 (range, 18 to 65) and were a mean of 23.6 years from cancer diagnosis. Most (57.8%) had been diagnosed with hematologic malignancies, 32.0% with solid tumors, and 10.1% with central nervous system malignancies.
All subjects had been treated at St. Jude and enrolled in the St. Jude LIFE study. Participants return to St. Jude periodically for several days of clinical and functional assessments. Data for this study were collected during the CCSs’ first St. Jude LIFE evaluations.
Assessing hardship
The researchers measured 3 types of financial hardship—material, psychological, and coping/behavioral.
About 1 in 5 CCSs (22.4%) reported material financial hardship. In other words, their cancer had an impact on their financial situation.
More than half of CCSs (51.1%) reported psychological hardship—concern about their ability to pay for medical expenses.
And 33% of CCSs reported coping/behavioral hardship—an inability to see a doctor or go to the hospital due to finances.
Roughly 65% of CCSs reported at least 1 type of financial hardship.
All 3 types of hardship were significantly associated with somatization (all P<0.001), anxiety (all P<0.001), depression (all P<0.001), suicidal thoughts (all P<0.05), and difficulty in retirement planning (all P<0.001).
Furthermore, CCSs who reported financial hardship had significantly lower health-related quality of life (P<0.001 for all 3 domains), sensation abnormality (all P<0.001), pulmonary symptoms (all P<0.05), and cardiac symptoms (all P<0.05).
Predicting hardship
Intensive cancer treatment, chronic health conditions, second cancers, age at the time of study evaluation, education level, and annual household income were all significantly associated with a greater risk of financial hardship.
CCSs age 40 and older had an increased risk of psychological and coping/behavioral hardship (P<0.001 for both domains).
CCSs with an annual household income of less than $40,000 had an increased risk of material, psychological, and coping/behavioral hardship, compared to CCSs with an income of $80,000 or more (P<0.001 for all domains).
CCSs who did not obtain a high school diploma had an increased risk of material (P<0.001), psychological (P<0.01), and coping/behavioral hardship (P<0.001) compared to college graduates.
CCSs who received cancer treatments associated with a high-risk disease burden (vs low-risk) had an increased risk of material (P=0.01) and psychological (P=0.004) hardship.
Health conditions associated with material financial hardship included grade 2-4 myocardial infarction (P<0.001), peripheral neuropathy (P<0.001), subsequent neoplasm (P<0.001), seizure (P=0.007), reproductive disorders (P=0.01), stroke (P=0.02), amputation (P=0.02), upper gastrointestinal disease (P=0.04), and hearing loss (P=0.05).
Grade 2-4 myocardial infarction and reproductive disorders were significantly associated with psychological financial hardship (P=0.02 for both).
“Severe late effects that emerge early in life and disrupt education and training opportunities are a double hit for survivors,” Dr Huang said. “These health problems decrease the survivors’ earning mobility and financial security later in life. The phenomenon leaves them at risk for poor health and psychological outcomes compared to healthier survivors.”
Health-related financial hardship is common among adult survivors of childhood cancer, according to a study published in the Journal of the National Cancer Institute.
Researchers analyzed more than 2800 long-term childhood cancer survivors (CCSs) and found that 65% had financial challenges related to their cancer diagnosis.
“These findings suggest primary care doctors and oncologists should routinely screen childhood cancer survivors for possible financial hardship,” said I-Chan Huang, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Specifically, Dr Huang recommends that healthcare providers routinely ask CCSs if they are unable to purchase medications, ever skip appointments for economic reasons, or worry about how to pay their medical bills.
For this study, Dr Huang and his colleagues analyzed data from 2811 CCSs. The subjects had a mean age of 31.8 (range, 18 to 65) and were a mean of 23.6 years from cancer diagnosis. Most (57.8%) had been diagnosed with hematologic malignancies, 32.0% with solid tumors, and 10.1% with central nervous system malignancies.
All subjects had been treated at St. Jude and enrolled in the St. Jude LIFE study. Participants return to St. Jude periodically for several days of clinical and functional assessments. Data for this study were collected during the CCSs’ first St. Jude LIFE evaluations.
Assessing hardship
The researchers measured 3 types of financial hardship—material, psychological, and coping/behavioral.
About 1 in 5 CCSs (22.4%) reported material financial hardship. In other words, their cancer had an impact on their financial situation.
More than half of CCSs (51.1%) reported psychological hardship—concern about their ability to pay for medical expenses.
And 33% of CCSs reported coping/behavioral hardship—an inability to see a doctor or go to the hospital due to finances.
Roughly 65% of CCSs reported at least 1 type of financial hardship.
All 3 types of hardship were significantly associated with somatization (all P<0.001), anxiety (all P<0.001), depression (all P<0.001), suicidal thoughts (all P<0.05), and difficulty in retirement planning (all P<0.001).
Furthermore, CCSs who reported financial hardship had significantly lower health-related quality of life (P<0.001 for all 3 domains), sensation abnormality (all P<0.001), pulmonary symptoms (all P<0.05), and cardiac symptoms (all P<0.05).
Predicting hardship
Intensive cancer treatment, chronic health conditions, second cancers, age at the time of study evaluation, education level, and annual household income were all significantly associated with a greater risk of financial hardship.
CCSs age 40 and older had an increased risk of psychological and coping/behavioral hardship (P<0.001 for both domains).
CCSs with an annual household income of less than $40,000 had an increased risk of material, psychological, and coping/behavioral hardship, compared to CCSs with an income of $80,000 or more (P<0.001 for all domains).
CCSs who did not obtain a high school diploma had an increased risk of material (P<0.001), psychological (P<0.01), and coping/behavioral hardship (P<0.001) compared to college graduates.
CCSs who received cancer treatments associated with a high-risk disease burden (vs low-risk) had an increased risk of material (P=0.01) and psychological (P=0.004) hardship.
Health conditions associated with material financial hardship included grade 2-4 myocardial infarction (P<0.001), peripheral neuropathy (P<0.001), subsequent neoplasm (P<0.001), seizure (P=0.007), reproductive disorders (P=0.01), stroke (P=0.02), amputation (P=0.02), upper gastrointestinal disease (P=0.04), and hearing loss (P=0.05).
Grade 2-4 myocardial infarction and reproductive disorders were significantly associated with psychological financial hardship (P=0.02 for both).
“Severe late effects that emerge early in life and disrupt education and training opportunities are a double hit for survivors,” Dr Huang said. “These health problems decrease the survivors’ earning mobility and financial security later in life. The phenomenon leaves them at risk for poor health and psychological outcomes compared to healthier survivors.”
CHMP announces 2 opinions on blinatumomab
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has released 2 new opinions regarding blinatumomab (Blincyto).
The CHMP recommended expanding the approved use of blinatumomab to include pediatric patients, but the committee also recommended against approving blinatumomab to treat patients with minimal residual disease (MRD).
Blinatumomab is already approved by the European Commission (EC) as monotherapy for adults with Philadelphia chromosome-negative (Ph-), CD19-positive, relapsed or refractory B-cell precursor acute lymphoblastic leukemia (BCP-ALL).
Now, the CHMP has recommended expanding this use to include blinatumomab as monotherapy for patients age 1 and older with Ph-, CD19-positive, relapsed/refractory BCP-ALL. These patients must have at least 2 prior therapies or have relapsed after allogeneic hematopoietic stem cell transplant.
This recommendation was supported by data from Study ‘205. Results from this phase 1/2 study were published in the Journal of Clinical Oncology in 2016.
The CHMP has also recommended against approving blinatumomab to treat BCP-ALL patients with MRD.
This decision was influenced by data from the BLAST study. Results from this phase 2 study were published in Blood earlier this year.
The CHMP noted that, although blinatumomab helped clear away residual cells in many patients in the BLAST trial, there is no strong evidence that this leads to improved survival.
Given the uncertainty, the CHMP was of the opinion that the benefits of blinatumomab do not outweigh its risks in MRD-positive BCP-ALL patients.
Amgen, the company developing and marketing blinatumomab, can request a re-examination of the CHMP’s opinion within 15 days of receiving it.
The CHMP’s recommendations are reviewed by the EC, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The EC usually makes a decision within 67 days of CHMP recommendations.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has released 2 new opinions regarding blinatumomab (Blincyto).
The CHMP recommended expanding the approved use of blinatumomab to include pediatric patients, but the committee also recommended against approving blinatumomab to treat patients with minimal residual disease (MRD).
Blinatumomab is already approved by the European Commission (EC) as monotherapy for adults with Philadelphia chromosome-negative (Ph-), CD19-positive, relapsed or refractory B-cell precursor acute lymphoblastic leukemia (BCP-ALL).
Now, the CHMP has recommended expanding this use to include blinatumomab as monotherapy for patients age 1 and older with Ph-, CD19-positive, relapsed/refractory BCP-ALL. These patients must have at least 2 prior therapies or have relapsed after allogeneic hematopoietic stem cell transplant.
This recommendation was supported by data from Study ‘205. Results from this phase 1/2 study were published in the Journal of Clinical Oncology in 2016.
The CHMP has also recommended against approving blinatumomab to treat BCP-ALL patients with MRD.
This decision was influenced by data from the BLAST study. Results from this phase 2 study were published in Blood earlier this year.
The CHMP noted that, although blinatumomab helped clear away residual cells in many patients in the BLAST trial, there is no strong evidence that this leads to improved survival.
Given the uncertainty, the CHMP was of the opinion that the benefits of blinatumomab do not outweigh its risks in MRD-positive BCP-ALL patients.
Amgen, the company developing and marketing blinatumomab, can request a re-examination of the CHMP’s opinion within 15 days of receiving it.
The CHMP’s recommendations are reviewed by the EC, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The EC usually makes a decision within 67 days of CHMP recommendations.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has released 2 new opinions regarding blinatumomab (Blincyto).
The CHMP recommended expanding the approved use of blinatumomab to include pediatric patients, but the committee also recommended against approving blinatumomab to treat patients with minimal residual disease (MRD).
Blinatumomab is already approved by the European Commission (EC) as monotherapy for adults with Philadelphia chromosome-negative (Ph-), CD19-positive, relapsed or refractory B-cell precursor acute lymphoblastic leukemia (BCP-ALL).
Now, the CHMP has recommended expanding this use to include blinatumomab as monotherapy for patients age 1 and older with Ph-, CD19-positive, relapsed/refractory BCP-ALL. These patients must have at least 2 prior therapies or have relapsed after allogeneic hematopoietic stem cell transplant.
This recommendation was supported by data from Study ‘205. Results from this phase 1/2 study were published in the Journal of Clinical Oncology in 2016.
The CHMP has also recommended against approving blinatumomab to treat BCP-ALL patients with MRD.
This decision was influenced by data from the BLAST study. Results from this phase 2 study were published in Blood earlier this year.
The CHMP noted that, although blinatumomab helped clear away residual cells in many patients in the BLAST trial, there is no strong evidence that this leads to improved survival.
Given the uncertainty, the CHMP was of the opinion that the benefits of blinatumomab do not outweigh its risks in MRD-positive BCP-ALL patients.
Amgen, the company developing and marketing blinatumomab, can request a re-examination of the CHMP’s opinion within 15 days of receiving it.
The CHMP’s recommendations are reviewed by the EC, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The EC usually makes a decision within 67 days of CHMP recommendations.
Global burden of hematologic malignancies
Research has shown an increase in the global incidence of leukemia and non-Hodgkin lymphoma (NHL) in recent years.
The Global Burden of Disease (GBD) study showed that, from 2006 to 2016, the incidence of NHL increased 45%, and the incidence of leukemia increased 26%.
These increases were largely due to population growth and aging.
Results from the GDB study were published in JAMA Oncology.
The study indicated that, in 2016, there were 17.2 million cases of cancer worldwide and 8.9 million cancer deaths.
One in 3 men were likely to get cancer during their lifetime, as were 1 in 5 women. Cancer was associated with 213.2 million disability-adjusted life years (DALYs).
The following table lists the 2016 global incidence and mortality figures for all cancers combined and for individual hematologic malignancies.
| Cancer type | Cases, thousands | Deaths, thousands |
| All cancers | 17,228 | 8927 |
| Leukemias | 467 | 310 |
| Acute lymphoid leukemia | 76 | 51 |
| Chronic lymphoid leukemia | 105 | 35 |
| Acute myeloid leukemia | 103 | 85 |
| Chronic myeloid leukemia | 32 | 22 |
| Other leukemias | 150 | 117 |
| Hodgkin lymphoma | 73 | 29 |
| NHL | 461 | 240 |
| Multiple myeloma | 139 | 98 |
Leukemia
In 2016, there were 467,000 new cases of leukemia and 310,000 leukemia deaths. Leukemia was responsible for 10.2 million DALYs. Leukemia developed in 1 in 118 men and 1 in 194 women worldwide.
Between 2006 and 2016, the global leukemia incidence increased by 26%—from 370,482 to 466,802 cases.
The researchers said the factors contributing to this increase were population growth (12%), population aging (10%), and an increase in age-specific incidence rates (3%).
NHL
In 2016, there were 461,000 new cases of NHL and 240,000 NHL deaths. NHL was responsible for 6.8 million DALYs. NHL developed in 1 in 110 men and 1 in 161 women worldwide.
Between 2006 and 2016, NHL increased by 45%, from 319,078 to 461,164 cases.
The factors contributing to this increase were increasing age-specific incidence rates (17%), changing population age structure (15%), and population growth (12%).
“A large proportion of the increase in cancer incidence can be explained by improving life expectancy and population growth—a development that can at least partially be attributed to a reduced burden from other common diseases,” the study authors wrote.
The authors also pointed out that prevention efforts are less effective for hematologic malignancies than for other cancers.
Research has shown an increase in the global incidence of leukemia and non-Hodgkin lymphoma (NHL) in recent years.
The Global Burden of Disease (GBD) study showed that, from 2006 to 2016, the incidence of NHL increased 45%, and the incidence of leukemia increased 26%.
These increases were largely due to population growth and aging.
Results from the GDB study were published in JAMA Oncology.
The study indicated that, in 2016, there were 17.2 million cases of cancer worldwide and 8.9 million cancer deaths.
One in 3 men were likely to get cancer during their lifetime, as were 1 in 5 women. Cancer was associated with 213.2 million disability-adjusted life years (DALYs).
The following table lists the 2016 global incidence and mortality figures for all cancers combined and for individual hematologic malignancies.
| Cancer type | Cases, thousands | Deaths, thousands |
| All cancers | 17,228 | 8927 |
| Leukemias | 467 | 310 |
| Acute lymphoid leukemia | 76 | 51 |
| Chronic lymphoid leukemia | 105 | 35 |
| Acute myeloid leukemia | 103 | 85 |
| Chronic myeloid leukemia | 32 | 22 |
| Other leukemias | 150 | 117 |
| Hodgkin lymphoma | 73 | 29 |
| NHL | 461 | 240 |
| Multiple myeloma | 139 | 98 |
Leukemia
In 2016, there were 467,000 new cases of leukemia and 310,000 leukemia deaths. Leukemia was responsible for 10.2 million DALYs. Leukemia developed in 1 in 118 men and 1 in 194 women worldwide.
Between 2006 and 2016, the global leukemia incidence increased by 26%—from 370,482 to 466,802 cases.
The researchers said the factors contributing to this increase were population growth (12%), population aging (10%), and an increase in age-specific incidence rates (3%).
NHL
In 2016, there were 461,000 new cases of NHL and 240,000 NHL deaths. NHL was responsible for 6.8 million DALYs. NHL developed in 1 in 110 men and 1 in 161 women worldwide.
Between 2006 and 2016, NHL increased by 45%, from 319,078 to 461,164 cases.
The factors contributing to this increase were increasing age-specific incidence rates (17%), changing population age structure (15%), and population growth (12%).
“A large proportion of the increase in cancer incidence can be explained by improving life expectancy and population growth—a development that can at least partially be attributed to a reduced burden from other common diseases,” the study authors wrote.
The authors also pointed out that prevention efforts are less effective for hematologic malignancies than for other cancers.
Research has shown an increase in the global incidence of leukemia and non-Hodgkin lymphoma (NHL) in recent years.
The Global Burden of Disease (GBD) study showed that, from 2006 to 2016, the incidence of NHL increased 45%, and the incidence of leukemia increased 26%.
These increases were largely due to population growth and aging.
Results from the GDB study were published in JAMA Oncology.
The study indicated that, in 2016, there were 17.2 million cases of cancer worldwide and 8.9 million cancer deaths.
One in 3 men were likely to get cancer during their lifetime, as were 1 in 5 women. Cancer was associated with 213.2 million disability-adjusted life years (DALYs).
The following table lists the 2016 global incidence and mortality figures for all cancers combined and for individual hematologic malignancies.
| Cancer type | Cases, thousands | Deaths, thousands |
| All cancers | 17,228 | 8927 |
| Leukemias | 467 | 310 |
| Acute lymphoid leukemia | 76 | 51 |
| Chronic lymphoid leukemia | 105 | 35 |
| Acute myeloid leukemia | 103 | 85 |
| Chronic myeloid leukemia | 32 | 22 |
| Other leukemias | 150 | 117 |
| Hodgkin lymphoma | 73 | 29 |
| NHL | 461 | 240 |
| Multiple myeloma | 139 | 98 |
Leukemia
In 2016, there were 467,000 new cases of leukemia and 310,000 leukemia deaths. Leukemia was responsible for 10.2 million DALYs. Leukemia developed in 1 in 118 men and 1 in 194 women worldwide.
Between 2006 and 2016, the global leukemia incidence increased by 26%—from 370,482 to 466,802 cases.
The researchers said the factors contributing to this increase were population growth (12%), population aging (10%), and an increase in age-specific incidence rates (3%).
NHL
In 2016, there were 461,000 new cases of NHL and 240,000 NHL deaths. NHL was responsible for 6.8 million DALYs. NHL developed in 1 in 110 men and 1 in 161 women worldwide.
Between 2006 and 2016, NHL increased by 45%, from 319,078 to 461,164 cases.
The factors contributing to this increase were increasing age-specific incidence rates (17%), changing population age structure (15%), and population growth (12%).
“A large proportion of the increase in cancer incidence can be explained by improving life expectancy and population growth—a development that can at least partially be attributed to a reduced burden from other common diseases,” the study authors wrote.
The authors also pointed out that prevention efforts are less effective for hematologic malignancies than for other cancers.
Intrathecal methotrexate dosing in acute leukemia falls short
STOCKHOLM – Although intrathecal chemoprophylaxis for prevention of central nervous system involvement is an essential component of modern regimens to treat acute lymphoblastic leukemia (ALL), patients don’t always receive the recommended number of doses, potentially compromising remissions.
But as a large-scale audit of health care delivery in the United Kingdom has suggested, many of the possible causes for suboptimal delivery of intrathecal methotrexate (IT MTX) appear to be modifiable, reported Sven A. Sommerfeld, MD, and his colleagues from the Christie Hospital in Manchester, England.
“In our clinical observations, and confirmed in this audit, patients on intensive chemotherapy, including induction and consolidation protocols for acute lymphoblastic leukemia, can develop a number of issues and toxicities, which can interfere with the administration of IT MTX,” they wrote in a poster presented at the annual congress of the European Hematology Association.
Reasons for canceling or postponing scheduled doses of IT MTX range from “fairly compelling clinical reasons affecting patient safety or tolerance” to more mundane issues, such as scheduling and staffing problems, the investigators found.
“I think there are a number of factors that can improve compliance, including having your cancellation rate as low as possible. You have already prescribed the treatment, the patient is supposed to be attending [clinic], yet for some reason you cannot go ahead,” Dr. Sommerfeld said in an interview. “I think blood product support is important, but there are capacity issues. Organization of complex treatment protocols that involve systemic chemotherapy and concurrent intrathecal administration can be difficult as different people oversee both of these treatments.”
For example, protocols specify delivery of intrathecal chemoprophylaxis on specific days and induction chemotherapy on other days, and it may be difficult to coordinate the care so that the doses don’t overlap, he said.
Dr. Sommerfeld and his colleagues conducted an audit of standard of care for patients aged 16-60 years who were diagnosed with B-cell or T-cell ALL and received IT MTX under one of two clinical protocols: UKALL 2011 or UKALL 14.
The investigators examined data on IT MTX compliance and assigned each patient a compliance score calculated by the number of administered doses divided by protocol-defined number of doses. They also examined pharmacy records of cancellations of protocol-scheduled IT MTX from January 2016 through July 2017.
They found that the total number of IT MTX prescriptions delivered as a proportion of the number prescribed ranged from a low of 61.8% in 2009 to a high of 84.2% in 2007.
When the investigators looked at records for individual patients, including 29 adolescent and young adults receiving IT MTX under the UKALL 2011 protocol and 27 adults receiving it under the UKALL 14 protocol, they found that failure to maintain coagulation levels within parameters accounted for 23% of cancellations. The next most common reasons for cancellation were rescheduling for administrative or clinical reasons in 20% of canceled doses, low platelet levels in 19% of cases, and patient nonattendance or communication failure in 16% of cases. Other factors included problems with lumbar access, vincristine schedule for the same day, recent anticoagulation, and delay of blood results.
“Notable is the variable approach to IT MTX in patients requiring therapeutic dose anticoagulation, reflecting clinical decisions of different physicians on a case-by-case basis. Whilst a full discussion of this topic and management of asparaginase-associated [venous thromboembolism] is beyond the scope of this audit, we generally recognize today that many affected patients can be managed to continue therapy as per protocol,” the investigators wrote.
Integrating relevant prescriptions into a single information system, monitoring clinics for treatment backlogs, and improving clinical resources, such as staffing, could help to improve the efficacy of IT MTX therapy, they suggested.
The study was supported by the National Health Service Foundation Trust. Dr. Sommerfeld reported having no relevant financial disclosures.
SOURCE: Sommerfeld SA et al. EHA Congress, Abstract PS930.
STOCKHOLM – Although intrathecal chemoprophylaxis for prevention of central nervous system involvement is an essential component of modern regimens to treat acute lymphoblastic leukemia (ALL), patients don’t always receive the recommended number of doses, potentially compromising remissions.
But as a large-scale audit of health care delivery in the United Kingdom has suggested, many of the possible causes for suboptimal delivery of intrathecal methotrexate (IT MTX) appear to be modifiable, reported Sven A. Sommerfeld, MD, and his colleagues from the Christie Hospital in Manchester, England.
“In our clinical observations, and confirmed in this audit, patients on intensive chemotherapy, including induction and consolidation protocols for acute lymphoblastic leukemia, can develop a number of issues and toxicities, which can interfere with the administration of IT MTX,” they wrote in a poster presented at the annual congress of the European Hematology Association.
Reasons for canceling or postponing scheduled doses of IT MTX range from “fairly compelling clinical reasons affecting patient safety or tolerance” to more mundane issues, such as scheduling and staffing problems, the investigators found.
“I think there are a number of factors that can improve compliance, including having your cancellation rate as low as possible. You have already prescribed the treatment, the patient is supposed to be attending [clinic], yet for some reason you cannot go ahead,” Dr. Sommerfeld said in an interview. “I think blood product support is important, but there are capacity issues. Organization of complex treatment protocols that involve systemic chemotherapy and concurrent intrathecal administration can be difficult as different people oversee both of these treatments.”
For example, protocols specify delivery of intrathecal chemoprophylaxis on specific days and induction chemotherapy on other days, and it may be difficult to coordinate the care so that the doses don’t overlap, he said.
Dr. Sommerfeld and his colleagues conducted an audit of standard of care for patients aged 16-60 years who were diagnosed with B-cell or T-cell ALL and received IT MTX under one of two clinical protocols: UKALL 2011 or UKALL 14.
The investigators examined data on IT MTX compliance and assigned each patient a compliance score calculated by the number of administered doses divided by protocol-defined number of doses. They also examined pharmacy records of cancellations of protocol-scheduled IT MTX from January 2016 through July 2017.
They found that the total number of IT MTX prescriptions delivered as a proportion of the number prescribed ranged from a low of 61.8% in 2009 to a high of 84.2% in 2007.
When the investigators looked at records for individual patients, including 29 adolescent and young adults receiving IT MTX under the UKALL 2011 protocol and 27 adults receiving it under the UKALL 14 protocol, they found that failure to maintain coagulation levels within parameters accounted for 23% of cancellations. The next most common reasons for cancellation were rescheduling for administrative or clinical reasons in 20% of canceled doses, low platelet levels in 19% of cases, and patient nonattendance or communication failure in 16% of cases. Other factors included problems with lumbar access, vincristine schedule for the same day, recent anticoagulation, and delay of blood results.
“Notable is the variable approach to IT MTX in patients requiring therapeutic dose anticoagulation, reflecting clinical decisions of different physicians on a case-by-case basis. Whilst a full discussion of this topic and management of asparaginase-associated [venous thromboembolism] is beyond the scope of this audit, we generally recognize today that many affected patients can be managed to continue therapy as per protocol,” the investigators wrote.
Integrating relevant prescriptions into a single information system, monitoring clinics for treatment backlogs, and improving clinical resources, such as staffing, could help to improve the efficacy of IT MTX therapy, they suggested.
The study was supported by the National Health Service Foundation Trust. Dr. Sommerfeld reported having no relevant financial disclosures.
SOURCE: Sommerfeld SA et al. EHA Congress, Abstract PS930.
STOCKHOLM – Although intrathecal chemoprophylaxis for prevention of central nervous system involvement is an essential component of modern regimens to treat acute lymphoblastic leukemia (ALL), patients don’t always receive the recommended number of doses, potentially compromising remissions.
But as a large-scale audit of health care delivery in the United Kingdom has suggested, many of the possible causes for suboptimal delivery of intrathecal methotrexate (IT MTX) appear to be modifiable, reported Sven A. Sommerfeld, MD, and his colleagues from the Christie Hospital in Manchester, England.
“In our clinical observations, and confirmed in this audit, patients on intensive chemotherapy, including induction and consolidation protocols for acute lymphoblastic leukemia, can develop a number of issues and toxicities, which can interfere with the administration of IT MTX,” they wrote in a poster presented at the annual congress of the European Hematology Association.
Reasons for canceling or postponing scheduled doses of IT MTX range from “fairly compelling clinical reasons affecting patient safety or tolerance” to more mundane issues, such as scheduling and staffing problems, the investigators found.
“I think there are a number of factors that can improve compliance, including having your cancellation rate as low as possible. You have already prescribed the treatment, the patient is supposed to be attending [clinic], yet for some reason you cannot go ahead,” Dr. Sommerfeld said in an interview. “I think blood product support is important, but there are capacity issues. Organization of complex treatment protocols that involve systemic chemotherapy and concurrent intrathecal administration can be difficult as different people oversee both of these treatments.”
For example, protocols specify delivery of intrathecal chemoprophylaxis on specific days and induction chemotherapy on other days, and it may be difficult to coordinate the care so that the doses don’t overlap, he said.
Dr. Sommerfeld and his colleagues conducted an audit of standard of care for patients aged 16-60 years who were diagnosed with B-cell or T-cell ALL and received IT MTX under one of two clinical protocols: UKALL 2011 or UKALL 14.
The investigators examined data on IT MTX compliance and assigned each patient a compliance score calculated by the number of administered doses divided by protocol-defined number of doses. They also examined pharmacy records of cancellations of protocol-scheduled IT MTX from January 2016 through July 2017.
They found that the total number of IT MTX prescriptions delivered as a proportion of the number prescribed ranged from a low of 61.8% in 2009 to a high of 84.2% in 2007.
When the investigators looked at records for individual patients, including 29 adolescent and young adults receiving IT MTX under the UKALL 2011 protocol and 27 adults receiving it under the UKALL 14 protocol, they found that failure to maintain coagulation levels within parameters accounted for 23% of cancellations. The next most common reasons for cancellation were rescheduling for administrative or clinical reasons in 20% of canceled doses, low platelet levels in 19% of cases, and patient nonattendance or communication failure in 16% of cases. Other factors included problems with lumbar access, vincristine schedule for the same day, recent anticoagulation, and delay of blood results.
“Notable is the variable approach to IT MTX in patients requiring therapeutic dose anticoagulation, reflecting clinical decisions of different physicians on a case-by-case basis. Whilst a full discussion of this topic and management of asparaginase-associated [venous thromboembolism] is beyond the scope of this audit, we generally recognize today that many affected patients can be managed to continue therapy as per protocol,” the investigators wrote.
Integrating relevant prescriptions into a single information system, monitoring clinics for treatment backlogs, and improving clinical resources, such as staffing, could help to improve the efficacy of IT MTX therapy, they suggested.
The study was supported by the National Health Service Foundation Trust. Dr. Sommerfeld reported having no relevant financial disclosures.
SOURCE: Sommerfeld SA et al. EHA Congress, Abstract PS930.
REPORTING FROM THE EHA CONGRESS
Key clinical point:
Major finding: The total number of intrathecal methotrexate prescriptions delivered as a proportion of the number prescribed ranged from a low of 61.8% in 2009 to a high of 84.2% in 2007.
Study details: Audit of standard of care delivery of intrathecal methotrexate in the United Kingdom.
Disclosures: The study was supported by the National Health Service Foundation Trust. Dr. Sommerfeld reported having no relevant financial disclosures.
Source: Sommerfeld SA et al. EHA Congress, Abstract PS930.
Treatments, disease affect spermatogonia in boys
Alkylating agents, hydroxyurea (HU), and certain non-malignant diseases can significantly deplete spermatogonial cell counts in young boys, according to research published in Human Reproduction.
Boys who received alkylating agents to treat cancer had significantly lower spermatogonial cell counts than control subjects or boys with malignant/nonmalignant diseases treated with non-alkylating agents.
Five of 6 SCD patients treated with HU had a totally depleted spermatogonial pool, and the remaining patient had a low spermatogonial cell count.
Five boys with non-malignant diseases who were not exposed to chemotherapy had significantly lower spermatogonial cell counts than controls.
“Our findings of a dramatic decrease in germ cell numbers in boys treated with alkylating agents and in sickle cell disease patients treated with hydroxyurea suggest that storing frozen testicular tissue from these boys should be performed before these treatments are initiated,” said study author Cecilia Petersen, MD, PhD, of Karolinska Institutet and University Hospital in Stockholm, Sweden.
“This needs to be communicated to physicians as well as patients and their parents or carers. However, until sperm that are able to fertilize eggs are produced from stored testicular tissue, we cannot confirm that germ cell quantity might determine the success of transplantation of the tissue in adulthood. Further research on this is needed to establish a realistic fertility preservation technique.”
Dr Petersen and her colleagues also noted that preserving testicular tissue may not be a viable option for boys who have low spermatogonial cell counts prior to treatment.
Patients and controls
For this study, the researchers analyzed testicular tissue from 32 boys facing treatments that carried a high risk of infertility—testicular irradiation, chemotherapy, or radiotherapy in advance of stem cell transplant.
Twenty boys had the tissue taken after initial chemotherapy, and 12 had it taken before starting any treatment.1
Eight patients had received chemotherapy with non-alkylating agents, 6 (all with malignancies) had received alkylating agents, and 6 (all with SCD) had received HU.
Diseases included acute lymphoblastic leukemia (n=6), SCD (n=6), acute myeloid leukemia (n=3), thalassemia major (n=3), neuroblastoma (n=2), juvenile myelomonocytic leukemia (n=2), myelodysplastic syndromes (n=2), primary immunodeficiency (n=2), Wilms tumor (n=1), adrenoleukodystrophy (n=1), hepatoblastoma (n=1), primitive neuroectodermal tumor (n=1), severe aplastic anemia (n=1), and Fanconi anemia (n=1).
The researchers compared samples from these 32 patients to 14 healthy testicular tissue samples stored in the biobank at the Karolinska University Hospital.
For both sample types, the team counted the number of spermatogonial cells found in a cross-section of seminiferous tubules.
“We could compare the number of spermatogonia with those found in the healthy boys as a way to estimate the effect of medical treatment or the disease itself on the future fertility of a patient,” explained study author Jan-Bernd Stukenborg, PhD, of Karolinska Institutet and University Hospital.
Impact of treatment
There was no significant difference in the mean quantity of spermatogonia per transverse tubular cross-section (S/T) between patients exposed to non-alkylating agents (1.7 ± 1.0, n=8) and biobank controls (4.1 ± 4.6, n=14).
However, samples from patients who received alkylating agents had a significantly lower mean S/T value (0.2 ± 0.3, n=6) than samples from patients treated with non-alkylating agents (P=0.003) and biobank controls (P<0.001).
“We found that the numbers of germ cells present in the cross-sections of the seminiferous tubules were significantly depleted and close to 0 in patients treated with alkylating agents,” Dr Stukenborg said.
Samples from the SCD patients also had a significantly lower mean S/T value (0.3 ± 0.6, n=6) than biobank controls (P=0.003).
Dr Stukenborg noted that the germ cell pool was totally depleted in 5 of the boys with SCD, and the pool was “very low” in the sixth SCD patient.
“This was not seen in patients who had not started treatment or were treated with non-alkylating agents or in the biobank tissues,” Dr Stukenborg said.2
He and his colleagues noted that it is possible for germ cells to recover to normal levels after treatment that is highly toxic to the testes, but high doses of alkylating agents and radiotherapy to the testicles are strongly associated with permanent or long-term infertility.
“The first group of boys who received bone marrow transplants are now reaching their thirties,” said study author Kirsi Jahnukainen, MD, PhD, of Helsinki University Central Hospital in Finland.
“Recent data suggest they may have a high chance of their sperm production recovering, even if they received high-dose alkylating therapies, so long as they had no testicular irradiation.”
Impact of disease
The researchers also found evidence to suggest that, for some boys, their disease may have affected spermatogonial cell counts before any treatment began.
Five patients with non-malignant disease who had not been exposed to chemotherapy (3 with thalassemia major, 1 with Fanconi anemia, and 1 with primary immunodeficiency) had a significantly lower mean S/T value (0.4 ± 0.5) than controls (P=0.006).
“Among patients who had not been treated previously with chemotherapy, there were several boys with a low number of germ cells for their age,” Dr Jahnukainen said.
“This suggests that some non-malignant diseases that require bone marrow transplants may affect the fertility of young boys even before exposure to therapy that is toxic for the testes.”
The researchers noted that a limitation of this study was that biobank samples had no detailed information regarding previous medical treatments and testicular volumes.
1. Testicular tissue is taken from patients under general anesthesia. The surgeon removes approximately 20% of the tissue from the testicular capsule in one of the testicles. For this study, a third of the tissue was taken to the Karolinska Institutet for analysis.
2. A recent meta-analysis showed that normal testicular tissue samples of newborns contain approximately 2.5 germ cells per tubular cross-section. This number decreases to approximately 1.2 within the first 3 years of age, followed by an increase up to 2.6 germ cells per tubular cross-section at 6 to 7 years, reaching a plateau until the age of 11. At the onset of puberty, an increase of up to 7 spermatogonia per tubular cross-section could be observed.
Alkylating agents, hydroxyurea (HU), and certain non-malignant diseases can significantly deplete spermatogonial cell counts in young boys, according to research published in Human Reproduction.
Boys who received alkylating agents to treat cancer had significantly lower spermatogonial cell counts than control subjects or boys with malignant/nonmalignant diseases treated with non-alkylating agents.
Five of 6 SCD patients treated with HU had a totally depleted spermatogonial pool, and the remaining patient had a low spermatogonial cell count.
Five boys with non-malignant diseases who were not exposed to chemotherapy had significantly lower spermatogonial cell counts than controls.
“Our findings of a dramatic decrease in germ cell numbers in boys treated with alkylating agents and in sickle cell disease patients treated with hydroxyurea suggest that storing frozen testicular tissue from these boys should be performed before these treatments are initiated,” said study author Cecilia Petersen, MD, PhD, of Karolinska Institutet and University Hospital in Stockholm, Sweden.
“This needs to be communicated to physicians as well as patients and their parents or carers. However, until sperm that are able to fertilize eggs are produced from stored testicular tissue, we cannot confirm that germ cell quantity might determine the success of transplantation of the tissue in adulthood. Further research on this is needed to establish a realistic fertility preservation technique.”
Dr Petersen and her colleagues also noted that preserving testicular tissue may not be a viable option for boys who have low spermatogonial cell counts prior to treatment.
Patients and controls
For this study, the researchers analyzed testicular tissue from 32 boys facing treatments that carried a high risk of infertility—testicular irradiation, chemotherapy, or radiotherapy in advance of stem cell transplant.
Twenty boys had the tissue taken after initial chemotherapy, and 12 had it taken before starting any treatment.1
Eight patients had received chemotherapy with non-alkylating agents, 6 (all with malignancies) had received alkylating agents, and 6 (all with SCD) had received HU.
Diseases included acute lymphoblastic leukemia (n=6), SCD (n=6), acute myeloid leukemia (n=3), thalassemia major (n=3), neuroblastoma (n=2), juvenile myelomonocytic leukemia (n=2), myelodysplastic syndromes (n=2), primary immunodeficiency (n=2), Wilms tumor (n=1), adrenoleukodystrophy (n=1), hepatoblastoma (n=1), primitive neuroectodermal tumor (n=1), severe aplastic anemia (n=1), and Fanconi anemia (n=1).
The researchers compared samples from these 32 patients to 14 healthy testicular tissue samples stored in the biobank at the Karolinska University Hospital.
For both sample types, the team counted the number of spermatogonial cells found in a cross-section of seminiferous tubules.
“We could compare the number of spermatogonia with those found in the healthy boys as a way to estimate the effect of medical treatment or the disease itself on the future fertility of a patient,” explained study author Jan-Bernd Stukenborg, PhD, of Karolinska Institutet and University Hospital.
Impact of treatment
There was no significant difference in the mean quantity of spermatogonia per transverse tubular cross-section (S/T) between patients exposed to non-alkylating agents (1.7 ± 1.0, n=8) and biobank controls (4.1 ± 4.6, n=14).
However, samples from patients who received alkylating agents had a significantly lower mean S/T value (0.2 ± 0.3, n=6) than samples from patients treated with non-alkylating agents (P=0.003) and biobank controls (P<0.001).
“We found that the numbers of germ cells present in the cross-sections of the seminiferous tubules were significantly depleted and close to 0 in patients treated with alkylating agents,” Dr Stukenborg said.
Samples from the SCD patients also had a significantly lower mean S/T value (0.3 ± 0.6, n=6) than biobank controls (P=0.003).
Dr Stukenborg noted that the germ cell pool was totally depleted in 5 of the boys with SCD, and the pool was “very low” in the sixth SCD patient.
“This was not seen in patients who had not started treatment or were treated with non-alkylating agents or in the biobank tissues,” Dr Stukenborg said.2
He and his colleagues noted that it is possible for germ cells to recover to normal levels after treatment that is highly toxic to the testes, but high doses of alkylating agents and radiotherapy to the testicles are strongly associated with permanent or long-term infertility.
“The first group of boys who received bone marrow transplants are now reaching their thirties,” said study author Kirsi Jahnukainen, MD, PhD, of Helsinki University Central Hospital in Finland.
“Recent data suggest they may have a high chance of their sperm production recovering, even if they received high-dose alkylating therapies, so long as they had no testicular irradiation.”
Impact of disease
The researchers also found evidence to suggest that, for some boys, their disease may have affected spermatogonial cell counts before any treatment began.
Five patients with non-malignant disease who had not been exposed to chemotherapy (3 with thalassemia major, 1 with Fanconi anemia, and 1 with primary immunodeficiency) had a significantly lower mean S/T value (0.4 ± 0.5) than controls (P=0.006).
“Among patients who had not been treated previously with chemotherapy, there were several boys with a low number of germ cells for their age,” Dr Jahnukainen said.
“This suggests that some non-malignant diseases that require bone marrow transplants may affect the fertility of young boys even before exposure to therapy that is toxic for the testes.”
The researchers noted that a limitation of this study was that biobank samples had no detailed information regarding previous medical treatments and testicular volumes.
1. Testicular tissue is taken from patients under general anesthesia. The surgeon removes approximately 20% of the tissue from the testicular capsule in one of the testicles. For this study, a third of the tissue was taken to the Karolinska Institutet for analysis.
2. A recent meta-analysis showed that normal testicular tissue samples of newborns contain approximately 2.5 germ cells per tubular cross-section. This number decreases to approximately 1.2 within the first 3 years of age, followed by an increase up to 2.6 germ cells per tubular cross-section at 6 to 7 years, reaching a plateau until the age of 11. At the onset of puberty, an increase of up to 7 spermatogonia per tubular cross-section could be observed.
Alkylating agents, hydroxyurea (HU), and certain non-malignant diseases can significantly deplete spermatogonial cell counts in young boys, according to research published in Human Reproduction.
Boys who received alkylating agents to treat cancer had significantly lower spermatogonial cell counts than control subjects or boys with malignant/nonmalignant diseases treated with non-alkylating agents.
Five of 6 SCD patients treated with HU had a totally depleted spermatogonial pool, and the remaining patient had a low spermatogonial cell count.
Five boys with non-malignant diseases who were not exposed to chemotherapy had significantly lower spermatogonial cell counts than controls.
“Our findings of a dramatic decrease in germ cell numbers in boys treated with alkylating agents and in sickle cell disease patients treated with hydroxyurea suggest that storing frozen testicular tissue from these boys should be performed before these treatments are initiated,” said study author Cecilia Petersen, MD, PhD, of Karolinska Institutet and University Hospital in Stockholm, Sweden.
“This needs to be communicated to physicians as well as patients and their parents or carers. However, until sperm that are able to fertilize eggs are produced from stored testicular tissue, we cannot confirm that germ cell quantity might determine the success of transplantation of the tissue in adulthood. Further research on this is needed to establish a realistic fertility preservation technique.”
Dr Petersen and her colleagues also noted that preserving testicular tissue may not be a viable option for boys who have low spermatogonial cell counts prior to treatment.
Patients and controls
For this study, the researchers analyzed testicular tissue from 32 boys facing treatments that carried a high risk of infertility—testicular irradiation, chemotherapy, or radiotherapy in advance of stem cell transplant.
Twenty boys had the tissue taken after initial chemotherapy, and 12 had it taken before starting any treatment.1
Eight patients had received chemotherapy with non-alkylating agents, 6 (all with malignancies) had received alkylating agents, and 6 (all with SCD) had received HU.
Diseases included acute lymphoblastic leukemia (n=6), SCD (n=6), acute myeloid leukemia (n=3), thalassemia major (n=3), neuroblastoma (n=2), juvenile myelomonocytic leukemia (n=2), myelodysplastic syndromes (n=2), primary immunodeficiency (n=2), Wilms tumor (n=1), adrenoleukodystrophy (n=1), hepatoblastoma (n=1), primitive neuroectodermal tumor (n=1), severe aplastic anemia (n=1), and Fanconi anemia (n=1).
The researchers compared samples from these 32 patients to 14 healthy testicular tissue samples stored in the biobank at the Karolinska University Hospital.
For both sample types, the team counted the number of spermatogonial cells found in a cross-section of seminiferous tubules.
“We could compare the number of spermatogonia with those found in the healthy boys as a way to estimate the effect of medical treatment or the disease itself on the future fertility of a patient,” explained study author Jan-Bernd Stukenborg, PhD, of Karolinska Institutet and University Hospital.
Impact of treatment
There was no significant difference in the mean quantity of spermatogonia per transverse tubular cross-section (S/T) between patients exposed to non-alkylating agents (1.7 ± 1.0, n=8) and biobank controls (4.1 ± 4.6, n=14).
However, samples from patients who received alkylating agents had a significantly lower mean S/T value (0.2 ± 0.3, n=6) than samples from patients treated with non-alkylating agents (P=0.003) and biobank controls (P<0.001).
“We found that the numbers of germ cells present in the cross-sections of the seminiferous tubules were significantly depleted and close to 0 in patients treated with alkylating agents,” Dr Stukenborg said.
Samples from the SCD patients also had a significantly lower mean S/T value (0.3 ± 0.6, n=6) than biobank controls (P=0.003).
Dr Stukenborg noted that the germ cell pool was totally depleted in 5 of the boys with SCD, and the pool was “very low” in the sixth SCD patient.
“This was not seen in patients who had not started treatment or were treated with non-alkylating agents or in the biobank tissues,” Dr Stukenborg said.2
He and his colleagues noted that it is possible for germ cells to recover to normal levels after treatment that is highly toxic to the testes, but high doses of alkylating agents and radiotherapy to the testicles are strongly associated with permanent or long-term infertility.
“The first group of boys who received bone marrow transplants are now reaching their thirties,” said study author Kirsi Jahnukainen, MD, PhD, of Helsinki University Central Hospital in Finland.
“Recent data suggest they may have a high chance of their sperm production recovering, even if they received high-dose alkylating therapies, so long as they had no testicular irradiation.”
Impact of disease
The researchers also found evidence to suggest that, for some boys, their disease may have affected spermatogonial cell counts before any treatment began.
Five patients with non-malignant disease who had not been exposed to chemotherapy (3 with thalassemia major, 1 with Fanconi anemia, and 1 with primary immunodeficiency) had a significantly lower mean S/T value (0.4 ± 0.5) than controls (P=0.006).
“Among patients who had not been treated previously with chemotherapy, there were several boys with a low number of germ cells for their age,” Dr Jahnukainen said.
“This suggests that some non-malignant diseases that require bone marrow transplants may affect the fertility of young boys even before exposure to therapy that is toxic for the testes.”
The researchers noted that a limitation of this study was that biobank samples had no detailed information regarding previous medical treatments and testicular volumes.
1. Testicular tissue is taken from patients under general anesthesia. The surgeon removes approximately 20% of the tissue from the testicular capsule in one of the testicles. For this study, a third of the tissue was taken to the Karolinska Institutet for analysis.
2. A recent meta-analysis showed that normal testicular tissue samples of newborns contain approximately 2.5 germ cells per tubular cross-section. This number decreases to approximately 1.2 within the first 3 years of age, followed by an increase up to 2.6 germ cells per tubular cross-section at 6 to 7 years, reaching a plateau until the age of 11. At the onset of puberty, an increase of up to 7 spermatogonia per tubular cross-section could be observed.
Team finds potential therapeutic targets for T-ALL
Researchers have found the NOTCH1 pathway “hijacks” heat shock transcription factor 1 (HSF1) signaling in T-cell acute lymphoblastic leukemia (T-ALL).
Therefore, blocking one or more genes in the HSF1 pathway could represent a new approach to treating T-ALL.
An experimental drug, PU-H71, is already in development against one of these targets, heat shock protein 90 (HSP90).
The researchers found that PU-H71 was active against T-ALL in vitro and in vivo.
The team recounted these findings in Nature Medicine.
“Our study shows how the NOTCH1 pathway hijacks the heat shock transcription factor 1 pathway to promote tumor growth,” said study author Iannis Aifantis, PhD, of NYU School of Medicine in New York, New York.
“The cancer cells are sending into overdrive a system that helps healthy cells respond to stress.”
Dr Aifantis and his colleagues found that HSF1 is involved in the pathogenesis of T-ALL. When they knocked down HSF1 in T-ALL cell lines, the researchers observed an increase in apoptosis, defective proteostasis, and a decrease in the growth of leukemic cells.
Similarly, HSF1 was deemed necessary for disease progression in mouse models of T-ALL. When the researchers deleted HSF1, mice experienced “striking” reductions in leukemic burden and “dramatic” improvements in survival. However, HSF1 deletion did not affect normal hematopoiesis.
Dr Aifantis and his colleagues also showed that NOTCH1 regulates the epichaperome in T-ALL. The team said previous studies have shown that, in the presence of oncogenic stress, heat shock proteins participate in a network nucleated by HSP90 and HSP70 chaperones—the epichaperome.
The researchers found that an intact epichaperome was critical for T-ALL by showing that pharmacologic inhibition of HSP90 and HSP70 significantly hindered the growth of human T-ALL in vitro. The team also found the HSP90 inhibitor PU-H71 reduced leukemic burden and extended survival in a NOTCH1-inducible T-ALL mouse model.
Then, the researchers found NOTCH1 levels could predict response to HSP90 inhibition in vitro. T-ALL patient samples expressing high levels of nuclear NOTCH1 and high levels of epichaperome were significantly more sensitive to treatment with PU-H71.
PU-H71 is already in early clinical trials of patients with breast cancer. If further testing proves successful, PU-H71 could be quickly adapted for trials in T-ALL patients, according to Dr Aifantis.
In the meantime, he and his colleagues plan to evaluate the effects of another 8 proteins produced by genes active in the HSF1 pathway to see if any show promising anticancer activity in T-ALL.
Researchers have found the NOTCH1 pathway “hijacks” heat shock transcription factor 1 (HSF1) signaling in T-cell acute lymphoblastic leukemia (T-ALL).
Therefore, blocking one or more genes in the HSF1 pathway could represent a new approach to treating T-ALL.
An experimental drug, PU-H71, is already in development against one of these targets, heat shock protein 90 (HSP90).
The researchers found that PU-H71 was active against T-ALL in vitro and in vivo.
The team recounted these findings in Nature Medicine.
“Our study shows how the NOTCH1 pathway hijacks the heat shock transcription factor 1 pathway to promote tumor growth,” said study author Iannis Aifantis, PhD, of NYU School of Medicine in New York, New York.
“The cancer cells are sending into overdrive a system that helps healthy cells respond to stress.”
Dr Aifantis and his colleagues found that HSF1 is involved in the pathogenesis of T-ALL. When they knocked down HSF1 in T-ALL cell lines, the researchers observed an increase in apoptosis, defective proteostasis, and a decrease in the growth of leukemic cells.
Similarly, HSF1 was deemed necessary for disease progression in mouse models of T-ALL. When the researchers deleted HSF1, mice experienced “striking” reductions in leukemic burden and “dramatic” improvements in survival. However, HSF1 deletion did not affect normal hematopoiesis.
Dr Aifantis and his colleagues also showed that NOTCH1 regulates the epichaperome in T-ALL. The team said previous studies have shown that, in the presence of oncogenic stress, heat shock proteins participate in a network nucleated by HSP90 and HSP70 chaperones—the epichaperome.
The researchers found that an intact epichaperome was critical for T-ALL by showing that pharmacologic inhibition of HSP90 and HSP70 significantly hindered the growth of human T-ALL in vitro. The team also found the HSP90 inhibitor PU-H71 reduced leukemic burden and extended survival in a NOTCH1-inducible T-ALL mouse model.
Then, the researchers found NOTCH1 levels could predict response to HSP90 inhibition in vitro. T-ALL patient samples expressing high levels of nuclear NOTCH1 and high levels of epichaperome were significantly more sensitive to treatment with PU-H71.
PU-H71 is already in early clinical trials of patients with breast cancer. If further testing proves successful, PU-H71 could be quickly adapted for trials in T-ALL patients, according to Dr Aifantis.
In the meantime, he and his colleagues plan to evaluate the effects of another 8 proteins produced by genes active in the HSF1 pathway to see if any show promising anticancer activity in T-ALL.
Researchers have found the NOTCH1 pathway “hijacks” heat shock transcription factor 1 (HSF1) signaling in T-cell acute lymphoblastic leukemia (T-ALL).
Therefore, blocking one or more genes in the HSF1 pathway could represent a new approach to treating T-ALL.
An experimental drug, PU-H71, is already in development against one of these targets, heat shock protein 90 (HSP90).
The researchers found that PU-H71 was active against T-ALL in vitro and in vivo.
The team recounted these findings in Nature Medicine.
“Our study shows how the NOTCH1 pathway hijacks the heat shock transcription factor 1 pathway to promote tumor growth,” said study author Iannis Aifantis, PhD, of NYU School of Medicine in New York, New York.
“The cancer cells are sending into overdrive a system that helps healthy cells respond to stress.”
Dr Aifantis and his colleagues found that HSF1 is involved in the pathogenesis of T-ALL. When they knocked down HSF1 in T-ALL cell lines, the researchers observed an increase in apoptosis, defective proteostasis, and a decrease in the growth of leukemic cells.
Similarly, HSF1 was deemed necessary for disease progression in mouse models of T-ALL. When the researchers deleted HSF1, mice experienced “striking” reductions in leukemic burden and “dramatic” improvements in survival. However, HSF1 deletion did not affect normal hematopoiesis.
Dr Aifantis and his colleagues also showed that NOTCH1 regulates the epichaperome in T-ALL. The team said previous studies have shown that, in the presence of oncogenic stress, heat shock proteins participate in a network nucleated by HSP90 and HSP70 chaperones—the epichaperome.
The researchers found that an intact epichaperome was critical for T-ALL by showing that pharmacologic inhibition of HSP90 and HSP70 significantly hindered the growth of human T-ALL in vitro. The team also found the HSP90 inhibitor PU-H71 reduced leukemic burden and extended survival in a NOTCH1-inducible T-ALL mouse model.
Then, the researchers found NOTCH1 levels could predict response to HSP90 inhibition in vitro. T-ALL patient samples expressing high levels of nuclear NOTCH1 and high levels of epichaperome were significantly more sensitive to treatment with PU-H71.
PU-H71 is already in early clinical trials of patients with breast cancer. If further testing proves successful, PU-H71 could be quickly adapted for trials in T-ALL patients, according to Dr Aifantis.
In the meantime, he and his colleagues plan to evaluate the effects of another 8 proteins produced by genes active in the HSF1 pathway to see if any show promising anticancer activity in T-ALL.
FDA approves biosimilar filgrastim
The US Food and Drug Administration (FDA) has approved the leukocyte growth factor Nivestym™ (filgrastim-aafi), a biosimilar to Neupogen (filgrastim).
Nivestym is approved to treat patients with nonmyeloid malignancies who are receiving myelosuppressive chemotherapy or undergoing bone marrow transplant, acute myeloid leukemia patients receiving induction or consolidation chemotherapy, patients undergoing autologous peripheral blood progenitor cell collection, and patients with severe chronic neutropenia.
The FDA’s approval of Nivestym was based on a review of evidence suggesting the drug is highly similar to Neupogen, according to Pfizer, the company developing Nivestym.
The full approved indication for Nivestym is as follows:
- To decrease the incidence of infection, as manifested by febrile neutropenia, in patients with nonmyeloid malignancies receiving myelosuppressive anticancer drugs associated with a significant incidence of severe neutropenia with fever
- To reduce the time to neutrophil recovery and the duration of fever following induction or consolidation chemotherapy in patients with acute myeloid leukemia
- To reduce the duration of neutropenia and neutropenia-related clinical sequelae (eg, febrile neutropenia) in patients with nonmyeloid malignancies undergoing myeloablative chemotherapy followed by bone marrow transplant
- For the mobilization of autologous hematopoietic progenitor cells into the peripheral blood for collection by leukapheresis
- For chronic administration to reduce the incidence and duration of sequelae of severe neutropenia (eg, fever, infections, oropharyngeal ulcers) in symptomatic patients with congenital neutropenia, cyclic neutropenia, or idiopathic neutropenia.
For more details on Nivestym, see the full prescribing information.
The US Food and Drug Administration (FDA) has approved the leukocyte growth factor Nivestym™ (filgrastim-aafi), a biosimilar to Neupogen (filgrastim).
Nivestym is approved to treat patients with nonmyeloid malignancies who are receiving myelosuppressive chemotherapy or undergoing bone marrow transplant, acute myeloid leukemia patients receiving induction or consolidation chemotherapy, patients undergoing autologous peripheral blood progenitor cell collection, and patients with severe chronic neutropenia.
The FDA’s approval of Nivestym was based on a review of evidence suggesting the drug is highly similar to Neupogen, according to Pfizer, the company developing Nivestym.
The full approved indication for Nivestym is as follows:
- To decrease the incidence of infection, as manifested by febrile neutropenia, in patients with nonmyeloid malignancies receiving myelosuppressive anticancer drugs associated with a significant incidence of severe neutropenia with fever
- To reduce the time to neutrophil recovery and the duration of fever following induction or consolidation chemotherapy in patients with acute myeloid leukemia
- To reduce the duration of neutropenia and neutropenia-related clinical sequelae (eg, febrile neutropenia) in patients with nonmyeloid malignancies undergoing myeloablative chemotherapy followed by bone marrow transplant
- For the mobilization of autologous hematopoietic progenitor cells into the peripheral blood for collection by leukapheresis
- For chronic administration to reduce the incidence and duration of sequelae of severe neutropenia (eg, fever, infections, oropharyngeal ulcers) in symptomatic patients with congenital neutropenia, cyclic neutropenia, or idiopathic neutropenia.
For more details on Nivestym, see the full prescribing information.
The US Food and Drug Administration (FDA) has approved the leukocyte growth factor Nivestym™ (filgrastim-aafi), a biosimilar to Neupogen (filgrastim).
Nivestym is approved to treat patients with nonmyeloid malignancies who are receiving myelosuppressive chemotherapy or undergoing bone marrow transplant, acute myeloid leukemia patients receiving induction or consolidation chemotherapy, patients undergoing autologous peripheral blood progenitor cell collection, and patients with severe chronic neutropenia.
The FDA’s approval of Nivestym was based on a review of evidence suggesting the drug is highly similar to Neupogen, according to Pfizer, the company developing Nivestym.
The full approved indication for Nivestym is as follows:
- To decrease the incidence of infection, as manifested by febrile neutropenia, in patients with nonmyeloid malignancies receiving myelosuppressive anticancer drugs associated with a significant incidence of severe neutropenia with fever
- To reduce the time to neutrophil recovery and the duration of fever following induction or consolidation chemotherapy in patients with acute myeloid leukemia
- To reduce the duration of neutropenia and neutropenia-related clinical sequelae (eg, febrile neutropenia) in patients with nonmyeloid malignancies undergoing myeloablative chemotherapy followed by bone marrow transplant
- For the mobilization of autologous hematopoietic progenitor cells into the peripheral blood for collection by leukapheresis
- For chronic administration to reduce the incidence and duration of sequelae of severe neutropenia (eg, fever, infections, oropharyngeal ulcers) in symptomatic patients with congenital neutropenia, cyclic neutropenia, or idiopathic neutropenia.
For more details on Nivestym, see the full prescribing information.