User login
High-dose donepezil or memantine: Next step for Alzheimer’s disease?
Although cholinesterase inhibitors (ChEIs) and memantine at standard doses may slow the progression of Alzheimer’s disease (AD) as assessed by cognitive, functional, and global measures, this effect is relatively modest. For the estimated 5.4 million Americans with AD1—more than one-half of whom have moderate to severe disease2—there is a great need for new approaches to slow AD progression.
High doses of donepezil or memantine may be the next step in achieving better results than standard pharmacologic treatments for AD. This article presents the possible benefits and indications for high doses of donepezil (23 mg/d) and memantine (28 mg/d) for managing moderate to severe AD and their safety and tolerability profiles.
Current treatments offer modest benefits
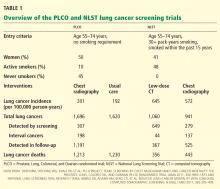
AD treatments comprise 2 categories: ChEIs (donepezil, rivastigmine, and galantamine) and the N-methyl-D-aspartate (NMDA) receptor antagonist memantine (Table 1).3,4 All ChEIs are FDA-approved for mild to moderate AD; donepezil also is approved for severe AD. Memantine is approved for moderate to severe AD, either alone or in combination with ChEIs. Until recently, the maximum FDA-approved doses were donepezil, 10 mg/d, and memantine, 20 mg/d. However, these dosages are associated with only modest beneficial effects in managing cognitive deterioration in patients with moderate to severe dementia.5,6 Studies have reported that combining a ChEI, such as donepezil, and memantine is well tolerated and may result in synergistic benefits by affecting different neurotransmitters in patients with moderate to severe AD.7,8
Recently, the FDA approved higher daily doses of donepezil (23 mg) and memantine (28 mg) for moderate to severe AD on the basis of positive phase III trial results.9-11 Donepezil, 23 mg/d, currently is marketed in the United States; the availability date for memantine, 28 mg/d, was undetermined at press time.
Table 1
FDA-approved treatments for Alzheimer’s disease
| Drug | Maximum daily dose | Mechanism of action | Indication | Common side effects/comments |
|---|---|---|---|---|
| Tacrine | 160 mg/d | ChEI | Mild to moderate AD | Nausea, vomiting, loss of appetite, diarrhea. First ChEI to be approved, but rarely used because of associated possible hepatotoxicity |
| Donepezil | 10 mg/d | ChEI | All stages of AD | Nausea, vomiting, loss of appetite, diarrhea, sleep disturbance |
| Rivastigmine | 12 mg/d | ChEI | Mild to moderate AD | Nausea, vomiting, diarrhea, weight loss, loss of appetite |
| Galantamine | 24 mg/d | ChEI | Mild to moderate AD | Nausea, vomiting, diarrhea, weight loss, loss of appetite |
| Memantine | 20 mg/d | NMDA receptor antagonist | Moderate to severe AD | Dizziness, headache, constipation, confusion |
| Galantamine ER | 24 mg/d | ChEI | Mild to moderate AD | Nausea, vomiting, diarrhea, weight loss, loss of appetite |
| Rivastigmine transdermal system | 9.5 mg/d | ChEI | Mild to moderate AD | Nausea, vomiting, diarrhea, weight loss, loss of appetite |
| Donepezil 23 | 23 mg/d | ChEI | Moderate to severe AD | Nausea, vomiting, diarrhea |
| Memantine ER | 28 mg/d | NMDA receptor antagonist | Moderate to severe AD | Dizziness, headache, constipation, confusion |
| AD: Alzheimer’s disease; ChEI: cholinesterase inhibitor; ER: extended release; NMDA: N-methyl-D-aspartate Source: References 3,4 | ||||
High-dose donepezil (23 mg/d)
Cognitive decline with AD has been associated with increasing loss of cholinergic neurons and cholinergic activities, particularly in areas associated with memory/cognition and learning, including cortical areas involving the temporal lobe, hippocampus, and nucleus basalis of Meynert.12-14 In addition, evidence suggests that increasing levels of acetylcholine by using ChEIs can enhance cognitive function.13,15
Donepezil is a selective, reversible ChEI believed to enhance central cholinergic function.15 Randomized clinical trials assessing dose-response with donepezil, 5 mg/d and 10 mg/d, have demonstrated more benefit in cognition with either dose than placebo. The 10 mg/d dose was more effective than 5 mg/d in patients with mild to moderate and severe AD.16-18 In patients with advanced AD who are stable on 5 mg/d, increasing to 10 mg/d could slow the progression of cognitive decline.18
Rationale for higher doses. Positron emission tomography studies have shown that at stable doses of donepezil, 5 mg/d or 10 mg/d, average cortical acetylcholinesterase (AChE) inhibition was <30%.19,20 Based on these findings, researchers thought that cortical AChE inhibition may be suboptimal with donepezil, 10 mg/d, and that higher doses of ChEI may be required in patients with more advanced AD—and therefore more cholinergic loss—for adequate cholinesterase inhibition. In a pilot study of patients with mild to moderate AD, higher doses of donepezil (15 mg/d and 20 mg/d) were reported to be safe and well tolerated.21
The 23-mg/d donepezil formulation was developed to provide a higher dose administered once daily without a sharp rise in peak concentration. The FDA approved donepezil, 23 mg/d, for patients with moderate to severe AD on the basis of phase III trial results.9,22 In a randomized, double-blind, multicenter, head-to-head clinical trial, >1,400 patients with moderate to severe AD (Mini-Mental State Exam [MMSE]: 0 to 20) on a stable dose of donepezil, 10 mg/d, for ≥3 months were randomly assigned to receive high-dose donepezil (23 mg/d) or standard-dose donepezil (10 mg/d) for 24 weeks.9,22 Patients in the 23-mg/d group showed a statistically significant improvement in cognition compared with the 10-mg/d group. The difference between groups on a measure of global improvement was not significant.9,22 However, in a post-hoc analysis, it was demonstrated that a subgroup of patients with more severe cognitive impairment (baseline MMSE: 0 to 16), showed significant improvement in cognition as well as global functioning.9
Overall, treatment-emergent adverse events (TEAEs) during the study were higher in patients receiving 23 mg/d (74%) than those receiving 10 mg/d (64%). The most common TEAEs in the 23-mg/d and 10-mg/d groups were nausea (12% vs 3%, respectively), vomiting (9% vs 3%), and diarrhea (8% vs 5%) (Table 2).22 These gastrointestinal adverse effects were more frequent during the first month of treatment and were relatively infrequent beyond 1 month. Serious TEAEs, such as falls, urinary tract infection, pneumonia, syncope, aggression, and confusional state, were noted in a similar proportion of patients in the 23-mg/d and 10-mg/d groups; most of these were considered unrelated to treatment. No drug-related deaths occurred during the study. High-dose (23 mg/d) donepezil generally was well tolerated, with a typical ChEI safety profile but superior efficacy.
A recent commentary discussed the issue of effect size and whether a 2.2-point difference on a 100-point scale (the Severe Impairment Battery [SIB]) is clinically meaningful.23 As with all anti-dementia therapies, in any cohort some patients will gain considerably more than 2.2 points on the SIB, which is clinically significant. A 6-month trial is recommended to identify these optimal responders.
Table 2
High-dose vs standard-dose donepezil: Treatment-emergent adverse events
| Adverse event | Donepezil, 23 mg/d | Donepezil,10 mg/d |
|---|---|---|
| Nausea | 12% | 3% |
| Vomiting | 9% | 3% |
| Diarrhea | 8% | 5% |
| Anorexia | 5% | 2% |
| Dizziness | 5% | 3% |
| Weight decrease | 5% | 3% |
| Headache | 4% | 3% |
| Insomnia | 3% | 2% |
| Urinary incontinence | 3% | 1% |
| Fatigue | 2% | 1% |
| Weakness | 2% | 1% |
| Somnolence | 2% | 1% |
| Contusion | 2% | 0% |
| Source: Reference 22 | ||
High-dose memantine
Memantine is an NMDA receptor antagonist, which works on glutamate, an ubiquitous neurotransmitter in the brain that serves many functions. For reasons that are not fully understood, in AD glutamate becomes excitotoxic and causes neuronal death.
Some researchers have hypothesized that if safe and well tolerated, a memantine dose >20 mg/d may have better efficacy than a lower dose. Memantine’s manufacturer has developed an extended-release (ER), once-daily formulation of memantine, 28 mg/d, to improve adherence and possibly increase efficacy.10,11 Because of memantine ER’s relatively slow absorption rate and longer median Tmax, of 12 hours, there is minimal fluctuation in plasma levels during steady-state dosing intervals compared with the immediate-release (IR) formulation.10
In a phase I study of 24 healthy volunteers that investigated the safety, tolerability, and pharmacokinetics of memantine ER, 28 mg/d, TEAEs were mild; the most common were headache, somnolence, and dizziness.10 During memantine treatment, there were no serious adverse events, potential significant changes in patients’ vital signs, or deaths.
Memantine ER plus ChEI. A multicenter, multinational, randomized, double-blind study compared memantine ER, 28 mg/d, and placebo in patients with moderate to severe AD (MMSE: 3 to 14).11 All patients were receiving concurrent, stable ChEI treatment (donepezil, rivastigmine, or galantamine) for ≥3 months before the study. Patients treated with memantine ER, 28 mg/d, and ChEI (n = 342) showed a significant improvement compared with the placebo/ChEI group (n = 335) in cognition and global functioning. Patients receiving memantine/ChEI also showed statistically significant benefits on behavior and verbal fluency testing compared with patients receiving placebo/ChEI. Memantine was well tolerated; most adverse events were mild or moderate. The most common adverse events in the memantine/ChEI group that occurred at a higher rate relative to the placebo/ChEI group were headache (5.6% vs 5.1%, respectively), diarrhea (5.0% vs 3.9%), and dizziness (4.7% vs 1.5%). There were no deaths related to memantine (Table 3).11
Memantine ER, 28 mg/d, may be tolerated better than the IR formulation because of less plasma level fluctuation during the steady-state dosing interval. Also, memantine ER, 28 mg/d, may offer better efficacy over memantine IR, 20 mg/d, because of dose-dependent cognitive, global, and behavioral effects. In addition, once-daily dosing of memantine ER may improve adherence compared with the IR formulation.24
In patients with severe renal impairment, dosage of memantine IR should be reduced from 20 mg/d to 10 mg/d.25 However, there is no available information regarding the dosing, safety, and tolerability of memantine ER, 28 mg/d, in patients with renal disease.
Table3
High-dose memantine: Treatment-emergent adverse eventsa
| Adverse event | Placebo (n = 335) | Memantine ER (n = 341) |
|---|---|---|
| Any TEAE | 214 (63.9%) | 214 (62.8%) |
| Fall | 26 (7.8%) | 19 (5.6%) |
| Urinary tract infection | 24 (7.2%) | 19 (5.6%) |
| Headache | 17 (5.1%) | 19 (5.6%) |
| Diarrhea | 13 (3.9%) | 17 (5.0%) |
| Dizziness | 5 (1.5%) | 16 (4.7%) |
| Influenza | 9 (2.7%) | 15 (4.4%) |
| Insomnia | 16 (4.8%) | 14 (4.1%) |
| Agitation | 15 (4.5%) | 14 (4.1%) |
| Hypertension | 8 (2.4%) | 13 (3.8%) |
| Anxiety | 9 (2.7%) | 12 (3.5%) |
| Depression | 5 (1.5%) | 11 (3.2%) |
| Weight increased | 3 (0.9%) | 11 (3.2%) |
| Constipation | 4 (1.2%) | 10 (2.9%) |
| Somnolence | 4 (1.2%) | 10 (2.9%) |
| Back pain | 2 (0.6%) | 9 (2.6%) |
| Aggression | 5 (1.5%) | 8 (2.3%) |
| Hypotension | 5 (1.5%) | 7 (2.1%) |
| Vomiting | 4 (1.2%) | 7 (2.1%) |
| Abdominal pain | 2 (0.6%) | 7 (2.1%) |
| Nasopharyngitis | 10 (3.0%) | 6 (1.8%) |
| Confusional state | 7 (2.1%) | 6 (1.8%) |
| Weight decreased | 11 (3.3%) | 5 (1.5%) |
| Nausea | 7 (2.1%) | 5 (1.5%) |
| Irritability | 8 (2.4%) | 4 (1.2%) |
| Cough | 8 (2.4%) | 3 (0.9%) |
| aData [n (%)] include all adverse events experienced by ≥2% patients in either group (safety population). Adverse events that were experienced at twice the rate in 1 group compared with the other are indicated by bold type ER: extended-release (28 mg); TEAE: treatment-emergent adverse event Source: Reference 11 | ||
Recommendations
Because there are few FDA-approved treatments for AD, higher doses of donepezil or memantine may be an option for patients who have “maxed out” on their AD therapy or no longer respond to lower doses. Higher doses of donepezil (23 mg/d) and memantine (28 mg/d) could improve medication adherence because both are once-daily preparations. In clinical trials, donepezil, 23 mg/d, was more effective than donepezil, 10 mg/d.9 Whether memantine ER, 28 mg/d, is superior to memantine IR, 20 mg/d, needs to be investigated in head-to-head, double-blind, controlled studies.
For patients with moderate to severe AD, donepezil, 23 mg, is associated with greater benefits in cognition compared with donepezil, 10 mg/d.9 Similarly, because of potentially superior efficacy because of a higher dose, memantine ER, 28 mg, might best help patients with moderate to severe AD, specifically those who either don’t respond or lose response to memantine IR, 20 mg/d. Combining a ChEI, such as donepezil, with memantine is associated with slower cognitive decline and short and long-term benefits on measures of cognition, activities of daily living, global outcome, and behavior.7,26 However, additional clinical trials are needed to assess the safety, tolerability, and efficacy of combination therapy with higher doses of donepezil and memantine ER.
Related Resources
- Alzheimer’s Disease Education and Referral Center. www.nia.nih.gov/Alzheimers.
- Lleó A, Greenberg SM, Growdon JH. Current pharmacotherapy for Alzheimer’s disease. Annu Rev Med. 2006;57:513-533.
Drug Brand Names
- Donepezil • Aricept
- Galantamine • Razadyne
- Memantine • Namenda
- Rivastigmine • Exelon
- Tacrine • Cognex
Disclosures
Dr. Grossberg’s academic department has received research funding from Forest Pharmaceuticals and Pfizer Inc. Dr. Grossberg has received grant/research support from Baxter BioScience, Forest Pharmaceuticals, Janssen, the National Institutes of Health, Novartis, and Pfizer, Inc.; is a consultant to Baxter BioScience, Forest Pharmaceuticals, Merck, Novartis, and Otsuka; and is on the Safety Monitoring Committee for Merck.
Dr. Singh reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Alzheimer’s Association, Thies W, Bleiler L. 2011 Alzheimer’s disease facts and figures. Alzheimers Dement. 2011;7(2):208-244.
2. Hebert LE, Scherr PA, Bienias JL, et al. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol. 2003;60(8):1119-1122.
3. Alzheimer’s Disease Education and Referral Center. Alzheimer’s disease medications. http://www.nia.nih.gov/alzheimers/publication/alzheimers-disease-medications-fact-sheet. Accessed May 10 2012.
4. Osborn GG, Saunders AV. Current treatments for patients with Alzheimer disease. J Am Osteopath Assoc. 2010;110(9 suppl 8):S16-S26.
5. Raina P, Santaguida P, Ismaila A, et al. Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline. Ann Intern Med. 2008;148(5):379-397.
6. Cummings JL. Alzheimer’s disease. N Engl J Med. 2004;351(1):56-67.
7. Tariot PN, Farlow MR, Grossberg GT, et al. Memantine Study Group. Memantine treatment in patients with moderate to severe Alzheimer disease already receiving donepezil: a randomized controlled trial. JAMA. 2004;291(3):317-324.
8. Xiong G, Doraiswamy PM. Combination drug therapy for Alzheimer’s disease: what is evidence-based and what is not? Geriatrics. 2005;60(6):22-26.
9. Farlow MR, Salloway S, Tariot PN, et al. Effectiveness and tolerability of high (23 mg/d) versus standard-dose (10 mg/d) donepezil in moderate to severe Alzheimer’s disease: a 24-week, randomized, double-blind study. Clin Ther. 2010;32(7):1234-1251.
10. Periclou A, Hu Y. Extended-release memantine capsule (28 mg once daily): a multiple dose, open-label study evaluating steady-state pharmacokinetics in healthy volunteers. Poster presented at 11th International Conference on Alzheimer’s Disease; July 26-31, 2008; Chicago, IL.
11. Grossberg GT, Manes F, Allegri R, et al. A multinational, randomized, double-blind, placebo-controlled, parallel-group trial of memantine extended-release capsule (28 mg, once daily) in patients with moderate to severe Alzheimer’s disease. Poster presented at 11th International Conference on Alzheimer’s Disease; July 26-31, 2008; Chicago, IL.
12. Geula C, Mesulam MM. Systematic regional variations in the loss of cortical cholinergic fibers in Alzheimer’s disease. Cereb Cortex. 1996;6(2):165-177.
13. Whitehouse PJ. The cholinergic deficit in Alzheimer’s disease. J Clin Psychiatry. 1998;59(suppl 13):19-22.
14. Teipel SJ, Flatz WH, Heinsen H, et al. Measurement of basal forebrain atrophy in Alzheimer’s disease using MRI. Brain. 2005;128(11):2626-2644.
15. Shintani EY, Uchida KM. Donepezil: an anticholinesterase inhibitor for Alzheimer’s disease. Am J Health Syst Pharm. 1997;54(24):2805-2810.
16. Homma A, Imai Y, Tago H, et al. Donepezil treatment of patients with severe Alzheimer’s disease in a Japanese population: results from a 24-week, double-blind, placebo-controlled, randomized trial. Dement Geriatr Cogn Disord. 2008;25(5):399-407.
17. Whitehead A, Perdomo C, Pratt RD, et al. Donepezil for the symptomatic treatment of patients with mild to moderate Alzheimer’s disease: a meta-analysis of individual patient data from randomised controlled trials. Int J Geriatr Psychiatry. 2004;19(7):624-633.
18. Nozawa M, Ichimiya Y, Nozawa E, et al. Clinical effects of high oral dose of donepezil for patients with Alzheimer’s disease in Japan. Psychogeriatrics. 2009;9(2):50-55.
19. Kuhl DE, Minoshima S, Frey KA, et al. Limited donepezil inhibition of acetylcholinesterase measured with positron emission tomography in living Alzheimer cerebral cortex. Ann Neurol. 2000;48(3):391-395.
20. Bohnen NI, Kaufer DI, Hendrickson R, et al. Degree of inhibition of cortical acetylcholinesterase activity and cognitive effects by donepezil treatment in Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 2005;76(3):315-319.
21. Doody RS, Corey-Bloom J, Zhang R, et al. Safety and tolerability of donepezil at doses up to 20 mg/day: results from a pilot study in patients with Alzheimer’s disease. Drugs Aging. 2008;25(2):163-174.
22. Aricept [package insert]. Woodcliff Lake NJ: Eisai Co.; 2012.
23. Schwartz LM, Woloshin S. How the FDA forgot the evidence: the case of donepezil 23 mg. BMJ. 2012;344:e1086.-doi: 10.1136/bmj.e1086.
24. Saini SD, Schoenfeld P, Kaulback K, et al. Effect of medication dosing frequency on adherence in chronic diseases. Am J Manag Care. 2009;15(6):e22-e33.
25. Periclou A, Ventura D, Rao N, et al. Pharmacokinetic study of memantine in healthy and renally impaired subjects. Clin Pharmacol Ther. 2006;79(1):134-143.
26. Atri A, Shaughnessy LW, Locascio JJ, et al. Long-term course and effectiveness of combination therapy in Alzheimer disease. Alzheimer Dis Assoc Disord. 2008;22(3):209-221.
Although cholinesterase inhibitors (ChEIs) and memantine at standard doses may slow the progression of Alzheimer’s disease (AD) as assessed by cognitive, functional, and global measures, this effect is relatively modest. For the estimated 5.4 million Americans with AD1—more than one-half of whom have moderate to severe disease2—there is a great need for new approaches to slow AD progression.
High doses of donepezil or memantine may be the next step in achieving better results than standard pharmacologic treatments for AD. This article presents the possible benefits and indications for high doses of donepezil (23 mg/d) and memantine (28 mg/d) for managing moderate to severe AD and their safety and tolerability profiles.
Current treatments offer modest benefits
AD treatments comprise 2 categories: ChEIs (donepezil, rivastigmine, and galantamine) and the N-methyl-D-aspartate (NMDA) receptor antagonist memantine (Table 1).3,4 All ChEIs are FDA-approved for mild to moderate AD; donepezil also is approved for severe AD. Memantine is approved for moderate to severe AD, either alone or in combination with ChEIs. Until recently, the maximum FDA-approved doses were donepezil, 10 mg/d, and memantine, 20 mg/d. However, these dosages are associated with only modest beneficial effects in managing cognitive deterioration in patients with moderate to severe dementia.5,6 Studies have reported that combining a ChEI, such as donepezil, and memantine is well tolerated and may result in synergistic benefits by affecting different neurotransmitters in patients with moderate to severe AD.7,8
Recently, the FDA approved higher daily doses of donepezil (23 mg) and memantine (28 mg) for moderate to severe AD on the basis of positive phase III trial results.9-11 Donepezil, 23 mg/d, currently is marketed in the United States; the availability date for memantine, 28 mg/d, was undetermined at press time.
Table 1
FDA-approved treatments for Alzheimer’s disease
| Drug | Maximum daily dose | Mechanism of action | Indication | Common side effects/comments |
|---|---|---|---|---|
| Tacrine | 160 mg/d | ChEI | Mild to moderate AD | Nausea, vomiting, loss of appetite, diarrhea. First ChEI to be approved, but rarely used because of associated possible hepatotoxicity |
| Donepezil | 10 mg/d | ChEI | All stages of AD | Nausea, vomiting, loss of appetite, diarrhea, sleep disturbance |
| Rivastigmine | 12 mg/d | ChEI | Mild to moderate AD | Nausea, vomiting, diarrhea, weight loss, loss of appetite |
| Galantamine | 24 mg/d | ChEI | Mild to moderate AD | Nausea, vomiting, diarrhea, weight loss, loss of appetite |
| Memantine | 20 mg/d | NMDA receptor antagonist | Moderate to severe AD | Dizziness, headache, constipation, confusion |
| Galantamine ER | 24 mg/d | ChEI | Mild to moderate AD | Nausea, vomiting, diarrhea, weight loss, loss of appetite |
| Rivastigmine transdermal system | 9.5 mg/d | ChEI | Mild to moderate AD | Nausea, vomiting, diarrhea, weight loss, loss of appetite |
| Donepezil 23 | 23 mg/d | ChEI | Moderate to severe AD | Nausea, vomiting, diarrhea |
| Memantine ER | 28 mg/d | NMDA receptor antagonist | Moderate to severe AD | Dizziness, headache, constipation, confusion |
| AD: Alzheimer’s disease; ChEI: cholinesterase inhibitor; ER: extended release; NMDA: N-methyl-D-aspartate Source: References 3,4 | ||||
High-dose donepezil (23 mg/d)
Cognitive decline with AD has been associated with increasing loss of cholinergic neurons and cholinergic activities, particularly in areas associated with memory/cognition and learning, including cortical areas involving the temporal lobe, hippocampus, and nucleus basalis of Meynert.12-14 In addition, evidence suggests that increasing levels of acetylcholine by using ChEIs can enhance cognitive function.13,15
Donepezil is a selective, reversible ChEI believed to enhance central cholinergic function.15 Randomized clinical trials assessing dose-response with donepezil, 5 mg/d and 10 mg/d, have demonstrated more benefit in cognition with either dose than placebo. The 10 mg/d dose was more effective than 5 mg/d in patients with mild to moderate and severe AD.16-18 In patients with advanced AD who are stable on 5 mg/d, increasing to 10 mg/d could slow the progression of cognitive decline.18
Rationale for higher doses. Positron emission tomography studies have shown that at stable doses of donepezil, 5 mg/d or 10 mg/d, average cortical acetylcholinesterase (AChE) inhibition was <30%.19,20 Based on these findings, researchers thought that cortical AChE inhibition may be suboptimal with donepezil, 10 mg/d, and that higher doses of ChEI may be required in patients with more advanced AD—and therefore more cholinergic loss—for adequate cholinesterase inhibition. In a pilot study of patients with mild to moderate AD, higher doses of donepezil (15 mg/d and 20 mg/d) were reported to be safe and well tolerated.21
The 23-mg/d donepezil formulation was developed to provide a higher dose administered once daily without a sharp rise in peak concentration. The FDA approved donepezil, 23 mg/d, for patients with moderate to severe AD on the basis of phase III trial results.9,22 In a randomized, double-blind, multicenter, head-to-head clinical trial, >1,400 patients with moderate to severe AD (Mini-Mental State Exam [MMSE]: 0 to 20) on a stable dose of donepezil, 10 mg/d, for ≥3 months were randomly assigned to receive high-dose donepezil (23 mg/d) or standard-dose donepezil (10 mg/d) for 24 weeks.9,22 Patients in the 23-mg/d group showed a statistically significant improvement in cognition compared with the 10-mg/d group. The difference between groups on a measure of global improvement was not significant.9,22 However, in a post-hoc analysis, it was demonstrated that a subgroup of patients with more severe cognitive impairment (baseline MMSE: 0 to 16), showed significant improvement in cognition as well as global functioning.9
Overall, treatment-emergent adverse events (TEAEs) during the study were higher in patients receiving 23 mg/d (74%) than those receiving 10 mg/d (64%). The most common TEAEs in the 23-mg/d and 10-mg/d groups were nausea (12% vs 3%, respectively), vomiting (9% vs 3%), and diarrhea (8% vs 5%) (Table 2).22 These gastrointestinal adverse effects were more frequent during the first month of treatment and were relatively infrequent beyond 1 month. Serious TEAEs, such as falls, urinary tract infection, pneumonia, syncope, aggression, and confusional state, were noted in a similar proportion of patients in the 23-mg/d and 10-mg/d groups; most of these were considered unrelated to treatment. No drug-related deaths occurred during the study. High-dose (23 mg/d) donepezil generally was well tolerated, with a typical ChEI safety profile but superior efficacy.
A recent commentary discussed the issue of effect size and whether a 2.2-point difference on a 100-point scale (the Severe Impairment Battery [SIB]) is clinically meaningful.23 As with all anti-dementia therapies, in any cohort some patients will gain considerably more than 2.2 points on the SIB, which is clinically significant. A 6-month trial is recommended to identify these optimal responders.
Table 2
High-dose vs standard-dose donepezil: Treatment-emergent adverse events
| Adverse event | Donepezil, 23 mg/d | Donepezil,10 mg/d |
|---|---|---|
| Nausea | 12% | 3% |
| Vomiting | 9% | 3% |
| Diarrhea | 8% | 5% |
| Anorexia | 5% | 2% |
| Dizziness | 5% | 3% |
| Weight decrease | 5% | 3% |
| Headache | 4% | 3% |
| Insomnia | 3% | 2% |
| Urinary incontinence | 3% | 1% |
| Fatigue | 2% | 1% |
| Weakness | 2% | 1% |
| Somnolence | 2% | 1% |
| Contusion | 2% | 0% |
| Source: Reference 22 | ||
High-dose memantine
Memantine is an NMDA receptor antagonist, which works on glutamate, an ubiquitous neurotransmitter in the brain that serves many functions. For reasons that are not fully understood, in AD glutamate becomes excitotoxic and causes neuronal death.
Some researchers have hypothesized that if safe and well tolerated, a memantine dose >20 mg/d may have better efficacy than a lower dose. Memantine’s manufacturer has developed an extended-release (ER), once-daily formulation of memantine, 28 mg/d, to improve adherence and possibly increase efficacy.10,11 Because of memantine ER’s relatively slow absorption rate and longer median Tmax, of 12 hours, there is minimal fluctuation in plasma levels during steady-state dosing intervals compared with the immediate-release (IR) formulation.10
In a phase I study of 24 healthy volunteers that investigated the safety, tolerability, and pharmacokinetics of memantine ER, 28 mg/d, TEAEs were mild; the most common were headache, somnolence, and dizziness.10 During memantine treatment, there were no serious adverse events, potential significant changes in patients’ vital signs, or deaths.
Memantine ER plus ChEI. A multicenter, multinational, randomized, double-blind study compared memantine ER, 28 mg/d, and placebo in patients with moderate to severe AD (MMSE: 3 to 14).11 All patients were receiving concurrent, stable ChEI treatment (donepezil, rivastigmine, or galantamine) for ≥3 months before the study. Patients treated with memantine ER, 28 mg/d, and ChEI (n = 342) showed a significant improvement compared with the placebo/ChEI group (n = 335) in cognition and global functioning. Patients receiving memantine/ChEI also showed statistically significant benefits on behavior and verbal fluency testing compared with patients receiving placebo/ChEI. Memantine was well tolerated; most adverse events were mild or moderate. The most common adverse events in the memantine/ChEI group that occurred at a higher rate relative to the placebo/ChEI group were headache (5.6% vs 5.1%, respectively), diarrhea (5.0% vs 3.9%), and dizziness (4.7% vs 1.5%). There were no deaths related to memantine (Table 3).11
Memantine ER, 28 mg/d, may be tolerated better than the IR formulation because of less plasma level fluctuation during the steady-state dosing interval. Also, memantine ER, 28 mg/d, may offer better efficacy over memantine IR, 20 mg/d, because of dose-dependent cognitive, global, and behavioral effects. In addition, once-daily dosing of memantine ER may improve adherence compared with the IR formulation.24
In patients with severe renal impairment, dosage of memantine IR should be reduced from 20 mg/d to 10 mg/d.25 However, there is no available information regarding the dosing, safety, and tolerability of memantine ER, 28 mg/d, in patients with renal disease.
Table3
High-dose memantine: Treatment-emergent adverse eventsa
| Adverse event | Placebo (n = 335) | Memantine ER (n = 341) |
|---|---|---|
| Any TEAE | 214 (63.9%) | 214 (62.8%) |
| Fall | 26 (7.8%) | 19 (5.6%) |
| Urinary tract infection | 24 (7.2%) | 19 (5.6%) |
| Headache | 17 (5.1%) | 19 (5.6%) |
| Diarrhea | 13 (3.9%) | 17 (5.0%) |
| Dizziness | 5 (1.5%) | 16 (4.7%) |
| Influenza | 9 (2.7%) | 15 (4.4%) |
| Insomnia | 16 (4.8%) | 14 (4.1%) |
| Agitation | 15 (4.5%) | 14 (4.1%) |
| Hypertension | 8 (2.4%) | 13 (3.8%) |
| Anxiety | 9 (2.7%) | 12 (3.5%) |
| Depression | 5 (1.5%) | 11 (3.2%) |
| Weight increased | 3 (0.9%) | 11 (3.2%) |
| Constipation | 4 (1.2%) | 10 (2.9%) |
| Somnolence | 4 (1.2%) | 10 (2.9%) |
| Back pain | 2 (0.6%) | 9 (2.6%) |
| Aggression | 5 (1.5%) | 8 (2.3%) |
| Hypotension | 5 (1.5%) | 7 (2.1%) |
| Vomiting | 4 (1.2%) | 7 (2.1%) |
| Abdominal pain | 2 (0.6%) | 7 (2.1%) |
| Nasopharyngitis | 10 (3.0%) | 6 (1.8%) |
| Confusional state | 7 (2.1%) | 6 (1.8%) |
| Weight decreased | 11 (3.3%) | 5 (1.5%) |
| Nausea | 7 (2.1%) | 5 (1.5%) |
| Irritability | 8 (2.4%) | 4 (1.2%) |
| Cough | 8 (2.4%) | 3 (0.9%) |
| aData [n (%)] include all adverse events experienced by ≥2% patients in either group (safety population). Adverse events that were experienced at twice the rate in 1 group compared with the other are indicated by bold type ER: extended-release (28 mg); TEAE: treatment-emergent adverse event Source: Reference 11 | ||
Recommendations
Because there are few FDA-approved treatments for AD, higher doses of donepezil or memantine may be an option for patients who have “maxed out” on their AD therapy or no longer respond to lower doses. Higher doses of donepezil (23 mg/d) and memantine (28 mg/d) could improve medication adherence because both are once-daily preparations. In clinical trials, donepezil, 23 mg/d, was more effective than donepezil, 10 mg/d.9 Whether memantine ER, 28 mg/d, is superior to memantine IR, 20 mg/d, needs to be investigated in head-to-head, double-blind, controlled studies.
For patients with moderate to severe AD, donepezil, 23 mg, is associated with greater benefits in cognition compared with donepezil, 10 mg/d.9 Similarly, because of potentially superior efficacy because of a higher dose, memantine ER, 28 mg, might best help patients with moderate to severe AD, specifically those who either don’t respond or lose response to memantine IR, 20 mg/d. Combining a ChEI, such as donepezil, with memantine is associated with slower cognitive decline and short and long-term benefits on measures of cognition, activities of daily living, global outcome, and behavior.7,26 However, additional clinical trials are needed to assess the safety, tolerability, and efficacy of combination therapy with higher doses of donepezil and memantine ER.
Related Resources
- Alzheimer’s Disease Education and Referral Center. www.nia.nih.gov/Alzheimers.
- Lleó A, Greenberg SM, Growdon JH. Current pharmacotherapy for Alzheimer’s disease. Annu Rev Med. 2006;57:513-533.
Drug Brand Names
- Donepezil • Aricept
- Galantamine • Razadyne
- Memantine • Namenda
- Rivastigmine • Exelon
- Tacrine • Cognex
Disclosures
Dr. Grossberg’s academic department has received research funding from Forest Pharmaceuticals and Pfizer Inc. Dr. Grossberg has received grant/research support from Baxter BioScience, Forest Pharmaceuticals, Janssen, the National Institutes of Health, Novartis, and Pfizer, Inc.; is a consultant to Baxter BioScience, Forest Pharmaceuticals, Merck, Novartis, and Otsuka; and is on the Safety Monitoring Committee for Merck.
Dr. Singh reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Although cholinesterase inhibitors (ChEIs) and memantine at standard doses may slow the progression of Alzheimer’s disease (AD) as assessed by cognitive, functional, and global measures, this effect is relatively modest. For the estimated 5.4 million Americans with AD1—more than one-half of whom have moderate to severe disease2—there is a great need for new approaches to slow AD progression.
High doses of donepezil or memantine may be the next step in achieving better results than standard pharmacologic treatments for AD. This article presents the possible benefits and indications for high doses of donepezil (23 mg/d) and memantine (28 mg/d) for managing moderate to severe AD and their safety and tolerability profiles.
Current treatments offer modest benefits
AD treatments comprise 2 categories: ChEIs (donepezil, rivastigmine, and galantamine) and the N-methyl-D-aspartate (NMDA) receptor antagonist memantine (Table 1).3,4 All ChEIs are FDA-approved for mild to moderate AD; donepezil also is approved for severe AD. Memantine is approved for moderate to severe AD, either alone or in combination with ChEIs. Until recently, the maximum FDA-approved doses were donepezil, 10 mg/d, and memantine, 20 mg/d. However, these dosages are associated with only modest beneficial effects in managing cognitive deterioration in patients with moderate to severe dementia.5,6 Studies have reported that combining a ChEI, such as donepezil, and memantine is well tolerated and may result in synergistic benefits by affecting different neurotransmitters in patients with moderate to severe AD.7,8
Recently, the FDA approved higher daily doses of donepezil (23 mg) and memantine (28 mg) for moderate to severe AD on the basis of positive phase III trial results.9-11 Donepezil, 23 mg/d, currently is marketed in the United States; the availability date for memantine, 28 mg/d, was undetermined at press time.
Table 1
FDA-approved treatments for Alzheimer’s disease
| Drug | Maximum daily dose | Mechanism of action | Indication | Common side effects/comments |
|---|---|---|---|---|
| Tacrine | 160 mg/d | ChEI | Mild to moderate AD | Nausea, vomiting, loss of appetite, diarrhea. First ChEI to be approved, but rarely used because of associated possible hepatotoxicity |
| Donepezil | 10 mg/d | ChEI | All stages of AD | Nausea, vomiting, loss of appetite, diarrhea, sleep disturbance |
| Rivastigmine | 12 mg/d | ChEI | Mild to moderate AD | Nausea, vomiting, diarrhea, weight loss, loss of appetite |
| Galantamine | 24 mg/d | ChEI | Mild to moderate AD | Nausea, vomiting, diarrhea, weight loss, loss of appetite |
| Memantine | 20 mg/d | NMDA receptor antagonist | Moderate to severe AD | Dizziness, headache, constipation, confusion |
| Galantamine ER | 24 mg/d | ChEI | Mild to moderate AD | Nausea, vomiting, diarrhea, weight loss, loss of appetite |
| Rivastigmine transdermal system | 9.5 mg/d | ChEI | Mild to moderate AD | Nausea, vomiting, diarrhea, weight loss, loss of appetite |
| Donepezil 23 | 23 mg/d | ChEI | Moderate to severe AD | Nausea, vomiting, diarrhea |
| Memantine ER | 28 mg/d | NMDA receptor antagonist | Moderate to severe AD | Dizziness, headache, constipation, confusion |
| AD: Alzheimer’s disease; ChEI: cholinesterase inhibitor; ER: extended release; NMDA: N-methyl-D-aspartate Source: References 3,4 | ||||
High-dose donepezil (23 mg/d)
Cognitive decline with AD has been associated with increasing loss of cholinergic neurons and cholinergic activities, particularly in areas associated with memory/cognition and learning, including cortical areas involving the temporal lobe, hippocampus, and nucleus basalis of Meynert.12-14 In addition, evidence suggests that increasing levels of acetylcholine by using ChEIs can enhance cognitive function.13,15
Donepezil is a selective, reversible ChEI believed to enhance central cholinergic function.15 Randomized clinical trials assessing dose-response with donepezil, 5 mg/d and 10 mg/d, have demonstrated more benefit in cognition with either dose than placebo. The 10 mg/d dose was more effective than 5 mg/d in patients with mild to moderate and severe AD.16-18 In patients with advanced AD who are stable on 5 mg/d, increasing to 10 mg/d could slow the progression of cognitive decline.18
Rationale for higher doses. Positron emission tomography studies have shown that at stable doses of donepezil, 5 mg/d or 10 mg/d, average cortical acetylcholinesterase (AChE) inhibition was <30%.19,20 Based on these findings, researchers thought that cortical AChE inhibition may be suboptimal with donepezil, 10 mg/d, and that higher doses of ChEI may be required in patients with more advanced AD—and therefore more cholinergic loss—for adequate cholinesterase inhibition. In a pilot study of patients with mild to moderate AD, higher doses of donepezil (15 mg/d and 20 mg/d) were reported to be safe and well tolerated.21
The 23-mg/d donepezil formulation was developed to provide a higher dose administered once daily without a sharp rise in peak concentration. The FDA approved donepezil, 23 mg/d, for patients with moderate to severe AD on the basis of phase III trial results.9,22 In a randomized, double-blind, multicenter, head-to-head clinical trial, >1,400 patients with moderate to severe AD (Mini-Mental State Exam [MMSE]: 0 to 20) on a stable dose of donepezil, 10 mg/d, for ≥3 months were randomly assigned to receive high-dose donepezil (23 mg/d) or standard-dose donepezil (10 mg/d) for 24 weeks.9,22 Patients in the 23-mg/d group showed a statistically significant improvement in cognition compared with the 10-mg/d group. The difference between groups on a measure of global improvement was not significant.9,22 However, in a post-hoc analysis, it was demonstrated that a subgroup of patients with more severe cognitive impairment (baseline MMSE: 0 to 16), showed significant improvement in cognition as well as global functioning.9
Overall, treatment-emergent adverse events (TEAEs) during the study were higher in patients receiving 23 mg/d (74%) than those receiving 10 mg/d (64%). The most common TEAEs in the 23-mg/d and 10-mg/d groups were nausea (12% vs 3%, respectively), vomiting (9% vs 3%), and diarrhea (8% vs 5%) (Table 2).22 These gastrointestinal adverse effects were more frequent during the first month of treatment and were relatively infrequent beyond 1 month. Serious TEAEs, such as falls, urinary tract infection, pneumonia, syncope, aggression, and confusional state, were noted in a similar proportion of patients in the 23-mg/d and 10-mg/d groups; most of these were considered unrelated to treatment. No drug-related deaths occurred during the study. High-dose (23 mg/d) donepezil generally was well tolerated, with a typical ChEI safety profile but superior efficacy.
A recent commentary discussed the issue of effect size and whether a 2.2-point difference on a 100-point scale (the Severe Impairment Battery [SIB]) is clinically meaningful.23 As with all anti-dementia therapies, in any cohort some patients will gain considerably more than 2.2 points on the SIB, which is clinically significant. A 6-month trial is recommended to identify these optimal responders.
Table 2
High-dose vs standard-dose donepezil: Treatment-emergent adverse events
| Adverse event | Donepezil, 23 mg/d | Donepezil,10 mg/d |
|---|---|---|
| Nausea | 12% | 3% |
| Vomiting | 9% | 3% |
| Diarrhea | 8% | 5% |
| Anorexia | 5% | 2% |
| Dizziness | 5% | 3% |
| Weight decrease | 5% | 3% |
| Headache | 4% | 3% |
| Insomnia | 3% | 2% |
| Urinary incontinence | 3% | 1% |
| Fatigue | 2% | 1% |
| Weakness | 2% | 1% |
| Somnolence | 2% | 1% |
| Contusion | 2% | 0% |
| Source: Reference 22 | ||
High-dose memantine
Memantine is an NMDA receptor antagonist, which works on glutamate, an ubiquitous neurotransmitter in the brain that serves many functions. For reasons that are not fully understood, in AD glutamate becomes excitotoxic and causes neuronal death.
Some researchers have hypothesized that if safe and well tolerated, a memantine dose >20 mg/d may have better efficacy than a lower dose. Memantine’s manufacturer has developed an extended-release (ER), once-daily formulation of memantine, 28 mg/d, to improve adherence and possibly increase efficacy.10,11 Because of memantine ER’s relatively slow absorption rate and longer median Tmax, of 12 hours, there is minimal fluctuation in plasma levels during steady-state dosing intervals compared with the immediate-release (IR) formulation.10
In a phase I study of 24 healthy volunteers that investigated the safety, tolerability, and pharmacokinetics of memantine ER, 28 mg/d, TEAEs were mild; the most common were headache, somnolence, and dizziness.10 During memantine treatment, there were no serious adverse events, potential significant changes in patients’ vital signs, or deaths.
Memantine ER plus ChEI. A multicenter, multinational, randomized, double-blind study compared memantine ER, 28 mg/d, and placebo in patients with moderate to severe AD (MMSE: 3 to 14).11 All patients were receiving concurrent, stable ChEI treatment (donepezil, rivastigmine, or galantamine) for ≥3 months before the study. Patients treated with memantine ER, 28 mg/d, and ChEI (n = 342) showed a significant improvement compared with the placebo/ChEI group (n = 335) in cognition and global functioning. Patients receiving memantine/ChEI also showed statistically significant benefits on behavior and verbal fluency testing compared with patients receiving placebo/ChEI. Memantine was well tolerated; most adverse events were mild or moderate. The most common adverse events in the memantine/ChEI group that occurred at a higher rate relative to the placebo/ChEI group were headache (5.6% vs 5.1%, respectively), diarrhea (5.0% vs 3.9%), and dizziness (4.7% vs 1.5%). There were no deaths related to memantine (Table 3).11
Memantine ER, 28 mg/d, may be tolerated better than the IR formulation because of less plasma level fluctuation during the steady-state dosing interval. Also, memantine ER, 28 mg/d, may offer better efficacy over memantine IR, 20 mg/d, because of dose-dependent cognitive, global, and behavioral effects. In addition, once-daily dosing of memantine ER may improve adherence compared with the IR formulation.24
In patients with severe renal impairment, dosage of memantine IR should be reduced from 20 mg/d to 10 mg/d.25 However, there is no available information regarding the dosing, safety, and tolerability of memantine ER, 28 mg/d, in patients with renal disease.
Table3
High-dose memantine: Treatment-emergent adverse eventsa
| Adverse event | Placebo (n = 335) | Memantine ER (n = 341) |
|---|---|---|
| Any TEAE | 214 (63.9%) | 214 (62.8%) |
| Fall | 26 (7.8%) | 19 (5.6%) |
| Urinary tract infection | 24 (7.2%) | 19 (5.6%) |
| Headache | 17 (5.1%) | 19 (5.6%) |
| Diarrhea | 13 (3.9%) | 17 (5.0%) |
| Dizziness | 5 (1.5%) | 16 (4.7%) |
| Influenza | 9 (2.7%) | 15 (4.4%) |
| Insomnia | 16 (4.8%) | 14 (4.1%) |
| Agitation | 15 (4.5%) | 14 (4.1%) |
| Hypertension | 8 (2.4%) | 13 (3.8%) |
| Anxiety | 9 (2.7%) | 12 (3.5%) |
| Depression | 5 (1.5%) | 11 (3.2%) |
| Weight increased | 3 (0.9%) | 11 (3.2%) |
| Constipation | 4 (1.2%) | 10 (2.9%) |
| Somnolence | 4 (1.2%) | 10 (2.9%) |
| Back pain | 2 (0.6%) | 9 (2.6%) |
| Aggression | 5 (1.5%) | 8 (2.3%) |
| Hypotension | 5 (1.5%) | 7 (2.1%) |
| Vomiting | 4 (1.2%) | 7 (2.1%) |
| Abdominal pain | 2 (0.6%) | 7 (2.1%) |
| Nasopharyngitis | 10 (3.0%) | 6 (1.8%) |
| Confusional state | 7 (2.1%) | 6 (1.8%) |
| Weight decreased | 11 (3.3%) | 5 (1.5%) |
| Nausea | 7 (2.1%) | 5 (1.5%) |
| Irritability | 8 (2.4%) | 4 (1.2%) |
| Cough | 8 (2.4%) | 3 (0.9%) |
| aData [n (%)] include all adverse events experienced by ≥2% patients in either group (safety population). Adverse events that were experienced at twice the rate in 1 group compared with the other are indicated by bold type ER: extended-release (28 mg); TEAE: treatment-emergent adverse event Source: Reference 11 | ||
Recommendations
Because there are few FDA-approved treatments for AD, higher doses of donepezil or memantine may be an option for patients who have “maxed out” on their AD therapy or no longer respond to lower doses. Higher doses of donepezil (23 mg/d) and memantine (28 mg/d) could improve medication adherence because both are once-daily preparations. In clinical trials, donepezil, 23 mg/d, was more effective than donepezil, 10 mg/d.9 Whether memantine ER, 28 mg/d, is superior to memantine IR, 20 mg/d, needs to be investigated in head-to-head, double-blind, controlled studies.
For patients with moderate to severe AD, donepezil, 23 mg, is associated with greater benefits in cognition compared with donepezil, 10 mg/d.9 Similarly, because of potentially superior efficacy because of a higher dose, memantine ER, 28 mg, might best help patients with moderate to severe AD, specifically those who either don’t respond or lose response to memantine IR, 20 mg/d. Combining a ChEI, such as donepezil, with memantine is associated with slower cognitive decline and short and long-term benefits on measures of cognition, activities of daily living, global outcome, and behavior.7,26 However, additional clinical trials are needed to assess the safety, tolerability, and efficacy of combination therapy with higher doses of donepezil and memantine ER.
Related Resources
- Alzheimer’s Disease Education and Referral Center. www.nia.nih.gov/Alzheimers.
- Lleó A, Greenberg SM, Growdon JH. Current pharmacotherapy for Alzheimer’s disease. Annu Rev Med. 2006;57:513-533.
Drug Brand Names
- Donepezil • Aricept
- Galantamine • Razadyne
- Memantine • Namenda
- Rivastigmine • Exelon
- Tacrine • Cognex
Disclosures
Dr. Grossberg’s academic department has received research funding from Forest Pharmaceuticals and Pfizer Inc. Dr. Grossberg has received grant/research support from Baxter BioScience, Forest Pharmaceuticals, Janssen, the National Institutes of Health, Novartis, and Pfizer, Inc.; is a consultant to Baxter BioScience, Forest Pharmaceuticals, Merck, Novartis, and Otsuka; and is on the Safety Monitoring Committee for Merck.
Dr. Singh reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Alzheimer’s Association, Thies W, Bleiler L. 2011 Alzheimer’s disease facts and figures. Alzheimers Dement. 2011;7(2):208-244.
2. Hebert LE, Scherr PA, Bienias JL, et al. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol. 2003;60(8):1119-1122.
3. Alzheimer’s Disease Education and Referral Center. Alzheimer’s disease medications. http://www.nia.nih.gov/alzheimers/publication/alzheimers-disease-medications-fact-sheet. Accessed May 10 2012.
4. Osborn GG, Saunders AV. Current treatments for patients with Alzheimer disease. J Am Osteopath Assoc. 2010;110(9 suppl 8):S16-S26.
5. Raina P, Santaguida P, Ismaila A, et al. Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline. Ann Intern Med. 2008;148(5):379-397.
6. Cummings JL. Alzheimer’s disease. N Engl J Med. 2004;351(1):56-67.
7. Tariot PN, Farlow MR, Grossberg GT, et al. Memantine Study Group. Memantine treatment in patients with moderate to severe Alzheimer disease already receiving donepezil: a randomized controlled trial. JAMA. 2004;291(3):317-324.
8. Xiong G, Doraiswamy PM. Combination drug therapy for Alzheimer’s disease: what is evidence-based and what is not? Geriatrics. 2005;60(6):22-26.
9. Farlow MR, Salloway S, Tariot PN, et al. Effectiveness and tolerability of high (23 mg/d) versus standard-dose (10 mg/d) donepezil in moderate to severe Alzheimer’s disease: a 24-week, randomized, double-blind study. Clin Ther. 2010;32(7):1234-1251.
10. Periclou A, Hu Y. Extended-release memantine capsule (28 mg once daily): a multiple dose, open-label study evaluating steady-state pharmacokinetics in healthy volunteers. Poster presented at 11th International Conference on Alzheimer’s Disease; July 26-31, 2008; Chicago, IL.
11. Grossberg GT, Manes F, Allegri R, et al. A multinational, randomized, double-blind, placebo-controlled, parallel-group trial of memantine extended-release capsule (28 mg, once daily) in patients with moderate to severe Alzheimer’s disease. Poster presented at 11th International Conference on Alzheimer’s Disease; July 26-31, 2008; Chicago, IL.
12. Geula C, Mesulam MM. Systematic regional variations in the loss of cortical cholinergic fibers in Alzheimer’s disease. Cereb Cortex. 1996;6(2):165-177.
13. Whitehouse PJ. The cholinergic deficit in Alzheimer’s disease. J Clin Psychiatry. 1998;59(suppl 13):19-22.
14. Teipel SJ, Flatz WH, Heinsen H, et al. Measurement of basal forebrain atrophy in Alzheimer’s disease using MRI. Brain. 2005;128(11):2626-2644.
15. Shintani EY, Uchida KM. Donepezil: an anticholinesterase inhibitor for Alzheimer’s disease. Am J Health Syst Pharm. 1997;54(24):2805-2810.
16. Homma A, Imai Y, Tago H, et al. Donepezil treatment of patients with severe Alzheimer’s disease in a Japanese population: results from a 24-week, double-blind, placebo-controlled, randomized trial. Dement Geriatr Cogn Disord. 2008;25(5):399-407.
17. Whitehead A, Perdomo C, Pratt RD, et al. Donepezil for the symptomatic treatment of patients with mild to moderate Alzheimer’s disease: a meta-analysis of individual patient data from randomised controlled trials. Int J Geriatr Psychiatry. 2004;19(7):624-633.
18. Nozawa M, Ichimiya Y, Nozawa E, et al. Clinical effects of high oral dose of donepezil for patients with Alzheimer’s disease in Japan. Psychogeriatrics. 2009;9(2):50-55.
19. Kuhl DE, Minoshima S, Frey KA, et al. Limited donepezil inhibition of acetylcholinesterase measured with positron emission tomography in living Alzheimer cerebral cortex. Ann Neurol. 2000;48(3):391-395.
20. Bohnen NI, Kaufer DI, Hendrickson R, et al. Degree of inhibition of cortical acetylcholinesterase activity and cognitive effects by donepezil treatment in Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 2005;76(3):315-319.
21. Doody RS, Corey-Bloom J, Zhang R, et al. Safety and tolerability of donepezil at doses up to 20 mg/day: results from a pilot study in patients with Alzheimer’s disease. Drugs Aging. 2008;25(2):163-174.
22. Aricept [package insert]. Woodcliff Lake NJ: Eisai Co.; 2012.
23. Schwartz LM, Woloshin S. How the FDA forgot the evidence: the case of donepezil 23 mg. BMJ. 2012;344:e1086.-doi: 10.1136/bmj.e1086.
24. Saini SD, Schoenfeld P, Kaulback K, et al. Effect of medication dosing frequency on adherence in chronic diseases. Am J Manag Care. 2009;15(6):e22-e33.
25. Periclou A, Ventura D, Rao N, et al. Pharmacokinetic study of memantine in healthy and renally impaired subjects. Clin Pharmacol Ther. 2006;79(1):134-143.
26. Atri A, Shaughnessy LW, Locascio JJ, et al. Long-term course and effectiveness of combination therapy in Alzheimer disease. Alzheimer Dis Assoc Disord. 2008;22(3):209-221.
1. Alzheimer’s Association, Thies W, Bleiler L. 2011 Alzheimer’s disease facts and figures. Alzheimers Dement. 2011;7(2):208-244.
2. Hebert LE, Scherr PA, Bienias JL, et al. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol. 2003;60(8):1119-1122.
3. Alzheimer’s Disease Education and Referral Center. Alzheimer’s disease medications. http://www.nia.nih.gov/alzheimers/publication/alzheimers-disease-medications-fact-sheet. Accessed May 10 2012.
4. Osborn GG, Saunders AV. Current treatments for patients with Alzheimer disease. J Am Osteopath Assoc. 2010;110(9 suppl 8):S16-S26.
5. Raina P, Santaguida P, Ismaila A, et al. Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline. Ann Intern Med. 2008;148(5):379-397.
6. Cummings JL. Alzheimer’s disease. N Engl J Med. 2004;351(1):56-67.
7. Tariot PN, Farlow MR, Grossberg GT, et al. Memantine Study Group. Memantine treatment in patients with moderate to severe Alzheimer disease already receiving donepezil: a randomized controlled trial. JAMA. 2004;291(3):317-324.
8. Xiong G, Doraiswamy PM. Combination drug therapy for Alzheimer’s disease: what is evidence-based and what is not? Geriatrics. 2005;60(6):22-26.
9. Farlow MR, Salloway S, Tariot PN, et al. Effectiveness and tolerability of high (23 mg/d) versus standard-dose (10 mg/d) donepezil in moderate to severe Alzheimer’s disease: a 24-week, randomized, double-blind study. Clin Ther. 2010;32(7):1234-1251.
10. Periclou A, Hu Y. Extended-release memantine capsule (28 mg once daily): a multiple dose, open-label study evaluating steady-state pharmacokinetics in healthy volunteers. Poster presented at 11th International Conference on Alzheimer’s Disease; July 26-31, 2008; Chicago, IL.
11. Grossberg GT, Manes F, Allegri R, et al. A multinational, randomized, double-blind, placebo-controlled, parallel-group trial of memantine extended-release capsule (28 mg, once daily) in patients with moderate to severe Alzheimer’s disease. Poster presented at 11th International Conference on Alzheimer’s Disease; July 26-31, 2008; Chicago, IL.
12. Geula C, Mesulam MM. Systematic regional variations in the loss of cortical cholinergic fibers in Alzheimer’s disease. Cereb Cortex. 1996;6(2):165-177.
13. Whitehouse PJ. The cholinergic deficit in Alzheimer’s disease. J Clin Psychiatry. 1998;59(suppl 13):19-22.
14. Teipel SJ, Flatz WH, Heinsen H, et al. Measurement of basal forebrain atrophy in Alzheimer’s disease using MRI. Brain. 2005;128(11):2626-2644.
15. Shintani EY, Uchida KM. Donepezil: an anticholinesterase inhibitor for Alzheimer’s disease. Am J Health Syst Pharm. 1997;54(24):2805-2810.
16. Homma A, Imai Y, Tago H, et al. Donepezil treatment of patients with severe Alzheimer’s disease in a Japanese population: results from a 24-week, double-blind, placebo-controlled, randomized trial. Dement Geriatr Cogn Disord. 2008;25(5):399-407.
17. Whitehead A, Perdomo C, Pratt RD, et al. Donepezil for the symptomatic treatment of patients with mild to moderate Alzheimer’s disease: a meta-analysis of individual patient data from randomised controlled trials. Int J Geriatr Psychiatry. 2004;19(7):624-633.
18. Nozawa M, Ichimiya Y, Nozawa E, et al. Clinical effects of high oral dose of donepezil for patients with Alzheimer’s disease in Japan. Psychogeriatrics. 2009;9(2):50-55.
19. Kuhl DE, Minoshima S, Frey KA, et al. Limited donepezil inhibition of acetylcholinesterase measured with positron emission tomography in living Alzheimer cerebral cortex. Ann Neurol. 2000;48(3):391-395.
20. Bohnen NI, Kaufer DI, Hendrickson R, et al. Degree of inhibition of cortical acetylcholinesterase activity and cognitive effects by donepezil treatment in Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 2005;76(3):315-319.
21. Doody RS, Corey-Bloom J, Zhang R, et al. Safety and tolerability of donepezil at doses up to 20 mg/day: results from a pilot study in patients with Alzheimer’s disease. Drugs Aging. 2008;25(2):163-174.
22. Aricept [package insert]. Woodcliff Lake NJ: Eisai Co.; 2012.
23. Schwartz LM, Woloshin S. How the FDA forgot the evidence: the case of donepezil 23 mg. BMJ. 2012;344:e1086.-doi: 10.1136/bmj.e1086.
24. Saini SD, Schoenfeld P, Kaulback K, et al. Effect of medication dosing frequency on adherence in chronic diseases. Am J Manag Care. 2009;15(6):e22-e33.
25. Periclou A, Ventura D, Rao N, et al. Pharmacokinetic study of memantine in healthy and renally impaired subjects. Clin Pharmacol Ther. 2006;79(1):134-143.
26. Atri A, Shaughnessy LW, Locascio JJ, et al. Long-term course and effectiveness of combination therapy in Alzheimer disease. Alzheimer Dis Assoc Disord. 2008;22(3):209-221.
Does bupropion exacerbate anxiety?
For many clinicians, bupropion is the “go-to” medication for treating depressed patients who smoke, have concerns about sexual dysfunction side effects, and/or worry about weight gain. Bupropion is FDA-approved for preventing seasonal major depressive episodes in patients with seasonal affective disorder and is indicated as a smoking cessation aid.
“Anxious depression”—defined as depression with high levels of anxiety—is associated with poorer outcomes than “non-anxious” depression.1 Prescribing medications for these patients can be challenging. Some clinicians believe that bupropion exacerbates anxiety and should not be used to treat patients who experience both anxiety and depression.
Reports from our patients and our cumulative clinical experience are key factors in developing expertise in selecting appropriate medications. When informing our patients about what to expect from medications, however, it can be useful to combine anecdotal evidence with knowledge of the facts or lack thereof. Are there data to support or contradict the idea that bupropion can cause anxiety while treating depression?
What the research shows
The drug manufacturer reports a “substantial proportion of patients treated with Wellbutrin experience some degree of increased restlessness, agitation, anxiety, and insomnia, especially shortly after initiation of treatment.”2
In 2001, Rush et al3 published the results of a 16-week study (n=248) assessing pre-treatment anxiety levels and response to sertraline or bupropion. The authors concluded that anxious and depressed patients who received sertraline didn’t experience a superior anxiolytic or antidepressant response compared with bupropion.3 The same authors came to similar conclusions in a retrospective analysis of a pair of 8-week randomized, controlled, double-blind trials of selective serotonin reuptake inhibitors (SSRIs) and bupropion.4
In 2001, Nieuwstraten et al5 compared bupropion with SSRIs for treating depression by reviewing several randomized, double-blind, controlled trials. The relative risk of developing “anxiety/agitation” was 1.32 (95% confidence interval, 0.85 to 2.04), which was not statistically significant.
In a 2008 meta-analysis, Papakostas et al6 pooled individual patient data from 10 randomized, double-blind, placebo-controlled trials. Their aim was to compare the efficacy of bupropion to SSRIs in treating “anxious depression.” They found no difference in timing or degree of improvement in anxiety symptoms between groups based on Hamilton Anxiety Scale or Hamilton Depression Rating Scale—Anxiety-Somatization (HDRS-AS) scores. The authors recommended that antidepressant choice should not be based on concerns about worsening anxiety symptoms in depressed patients.6
Another meta-analysis by Papakostas et al7 of the same 10 randomized, double-blind, placebo-controlled trials suggested SSRIs may confer an advantage over bupropion in treating a subset of patients with “anxious depression,” which they defined as a HDRS-AS score ≥7. The authors noted the advantage was statistically significant, although “modest.”
Other smaller studies suggest that bupropion does not increase anxiety.8,9 A pilot study (N = 24, no placebo control) concluded that bupropion XL was comparable to escitalopram in treating anxiety in outpatients with generalized anxiety disorder.8
Because designing and executing drug trials can be expensive, it is not surprising that most of the evidence cited above derives from pharmaceutical company-sponsored or industry-affiliated work. As such, we should evaluate available evidence within the context of what we hear from and observe in our patients.
Our opinion
When assessing patients with depression and anxiety, we must carefully evaluate symptoms to distinguish between depression with associated anxiety symptoms and depression with a comorbid anxiety disorder.
If a patient suffers from depression with associated anxiety symptoms (“anxious depression”), keep in mind that although some data demonstrate a superior response to SSRIs, other studies show no difference in effect. Some research—albeit smaller, less compelling studies—suggests that bupropion may decrease anxiety.
If your patient suffers from comorbid depression and an anxiety disorder, bupropion would not be a first-line choice because it is not FDA-approved to treat anxiety disorders. Although it is possible that anxiety/agitation could result from bupropion use, there is not sufficient data to support its reputation as ”anxiogenic.”
What is your experience?
Do you agree with the authors? Send comments to [email protected] or share your thoughts on http://www.facebook.com/CurrentPsychiatry.
Related Resource
- American Psychiatric Association. Mixed anxiety-depressive disorder. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000:780-781.
Drug Brand Names
- Bupropion • Wellbutrin, Zyban
- Escitalopram • Lexapro
- Sertraline • Zoloft
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Fava M, Rush AJ, Alpert JE, et al. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry. 2008;165(3):342-351.
2. Wellbutrin [package insert]. Research Triangle Park NC: GlaxoSmithKline; 2008.
3. Rush AJ, Trivedi MH, Carmody TJ, et al. Response in relation to baseline anxiety levels in major depressive disorder treated with bupropion sustained release or sertraline. Neuropsychopharmacology. 2001;25(1):131-138.
4. Trivedi MH, Rush AJ, Carmody TJ, et al. Do bupropion SR and sertraline differ in their effects on anxiety in depressed patients? J Clin Psychiatry. 2001;62(10):776-781.
5. Nieuwstraten CE, Dolovich LR. Bupropion versus selective serotonin-reuptake inhibitors for treatment of depression. Ann Pharmacother. 2001;35(12):1608-1613.
6. Papakostas GI, Trivedi MH, Alpert JE, et al. Efficacy of bupropion and the selective serotonin reuptake inhibitors in the treatment of anxiety symptoms in major depressive disorder: a meta-analysis of individual patient data from 10 double-blind, randomized clinical trials. J Psychiatr Res. 2008;42(2):134-140.
7. Papakostas GI, Stahl SM, Krishen A, et al. Efficacy of bupropion and the selective serotonin reuptake inhibitors in the treatment of major depressive disorder with high levels of anxiety (anxious depression): a pooled analysis of 10 studies. J Clin Psychiatry. 2008;69(8):1287-1292.
8. Bystritsky A, Kerwin L, Feusner JD, et al. A pilot controlled trial of bupropion XL versus escitalopram in generalized anxiety disorder. Psychopharmacol Bull. 2008;41(1):46-51.
9. Feighner JP, Gardner EA, Johnston JA, et al. Double-blind comparison of bupropion and fluoxetine in depressed outpatients. J Clin Psychiatry. 1991;52(8):329-335.
For many clinicians, bupropion is the “go-to” medication for treating depressed patients who smoke, have concerns about sexual dysfunction side effects, and/or worry about weight gain. Bupropion is FDA-approved for preventing seasonal major depressive episodes in patients with seasonal affective disorder and is indicated as a smoking cessation aid.
“Anxious depression”—defined as depression with high levels of anxiety—is associated with poorer outcomes than “non-anxious” depression.1 Prescribing medications for these patients can be challenging. Some clinicians believe that bupropion exacerbates anxiety and should not be used to treat patients who experience both anxiety and depression.
Reports from our patients and our cumulative clinical experience are key factors in developing expertise in selecting appropriate medications. When informing our patients about what to expect from medications, however, it can be useful to combine anecdotal evidence with knowledge of the facts or lack thereof. Are there data to support or contradict the idea that bupropion can cause anxiety while treating depression?
What the research shows
The drug manufacturer reports a “substantial proportion of patients treated with Wellbutrin experience some degree of increased restlessness, agitation, anxiety, and insomnia, especially shortly after initiation of treatment.”2
In 2001, Rush et al3 published the results of a 16-week study (n=248) assessing pre-treatment anxiety levels and response to sertraline or bupropion. The authors concluded that anxious and depressed patients who received sertraline didn’t experience a superior anxiolytic or antidepressant response compared with bupropion.3 The same authors came to similar conclusions in a retrospective analysis of a pair of 8-week randomized, controlled, double-blind trials of selective serotonin reuptake inhibitors (SSRIs) and bupropion.4
In 2001, Nieuwstraten et al5 compared bupropion with SSRIs for treating depression by reviewing several randomized, double-blind, controlled trials. The relative risk of developing “anxiety/agitation” was 1.32 (95% confidence interval, 0.85 to 2.04), which was not statistically significant.
In a 2008 meta-analysis, Papakostas et al6 pooled individual patient data from 10 randomized, double-blind, placebo-controlled trials. Their aim was to compare the efficacy of bupropion to SSRIs in treating “anxious depression.” They found no difference in timing or degree of improvement in anxiety symptoms between groups based on Hamilton Anxiety Scale or Hamilton Depression Rating Scale—Anxiety-Somatization (HDRS-AS) scores. The authors recommended that antidepressant choice should not be based on concerns about worsening anxiety symptoms in depressed patients.6
Another meta-analysis by Papakostas et al7 of the same 10 randomized, double-blind, placebo-controlled trials suggested SSRIs may confer an advantage over bupropion in treating a subset of patients with “anxious depression,” which they defined as a HDRS-AS score ≥7. The authors noted the advantage was statistically significant, although “modest.”
Other smaller studies suggest that bupropion does not increase anxiety.8,9 A pilot study (N = 24, no placebo control) concluded that bupropion XL was comparable to escitalopram in treating anxiety in outpatients with generalized anxiety disorder.8
Because designing and executing drug trials can be expensive, it is not surprising that most of the evidence cited above derives from pharmaceutical company-sponsored or industry-affiliated work. As such, we should evaluate available evidence within the context of what we hear from and observe in our patients.
Our opinion
When assessing patients with depression and anxiety, we must carefully evaluate symptoms to distinguish between depression with associated anxiety symptoms and depression with a comorbid anxiety disorder.
If a patient suffers from depression with associated anxiety symptoms (“anxious depression”), keep in mind that although some data demonstrate a superior response to SSRIs, other studies show no difference in effect. Some research—albeit smaller, less compelling studies—suggests that bupropion may decrease anxiety.
If your patient suffers from comorbid depression and an anxiety disorder, bupropion would not be a first-line choice because it is not FDA-approved to treat anxiety disorders. Although it is possible that anxiety/agitation could result from bupropion use, there is not sufficient data to support its reputation as ”anxiogenic.”
What is your experience?
Do you agree with the authors? Send comments to [email protected] or share your thoughts on http://www.facebook.com/CurrentPsychiatry.
Related Resource
- American Psychiatric Association. Mixed anxiety-depressive disorder. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000:780-781.
Drug Brand Names
- Bupropion • Wellbutrin, Zyban
- Escitalopram • Lexapro
- Sertraline • Zoloft
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
For many clinicians, bupropion is the “go-to” medication for treating depressed patients who smoke, have concerns about sexual dysfunction side effects, and/or worry about weight gain. Bupropion is FDA-approved for preventing seasonal major depressive episodes in patients with seasonal affective disorder and is indicated as a smoking cessation aid.
“Anxious depression”—defined as depression with high levels of anxiety—is associated with poorer outcomes than “non-anxious” depression.1 Prescribing medications for these patients can be challenging. Some clinicians believe that bupropion exacerbates anxiety and should not be used to treat patients who experience both anxiety and depression.
Reports from our patients and our cumulative clinical experience are key factors in developing expertise in selecting appropriate medications. When informing our patients about what to expect from medications, however, it can be useful to combine anecdotal evidence with knowledge of the facts or lack thereof. Are there data to support or contradict the idea that bupropion can cause anxiety while treating depression?
What the research shows
The drug manufacturer reports a “substantial proportion of patients treated with Wellbutrin experience some degree of increased restlessness, agitation, anxiety, and insomnia, especially shortly after initiation of treatment.”2
In 2001, Rush et al3 published the results of a 16-week study (n=248) assessing pre-treatment anxiety levels and response to sertraline or bupropion. The authors concluded that anxious and depressed patients who received sertraline didn’t experience a superior anxiolytic or antidepressant response compared with bupropion.3 The same authors came to similar conclusions in a retrospective analysis of a pair of 8-week randomized, controlled, double-blind trials of selective serotonin reuptake inhibitors (SSRIs) and bupropion.4
In 2001, Nieuwstraten et al5 compared bupropion with SSRIs for treating depression by reviewing several randomized, double-blind, controlled trials. The relative risk of developing “anxiety/agitation” was 1.32 (95% confidence interval, 0.85 to 2.04), which was not statistically significant.
In a 2008 meta-analysis, Papakostas et al6 pooled individual patient data from 10 randomized, double-blind, placebo-controlled trials. Their aim was to compare the efficacy of bupropion to SSRIs in treating “anxious depression.” They found no difference in timing or degree of improvement in anxiety symptoms between groups based on Hamilton Anxiety Scale or Hamilton Depression Rating Scale—Anxiety-Somatization (HDRS-AS) scores. The authors recommended that antidepressant choice should not be based on concerns about worsening anxiety symptoms in depressed patients.6
Another meta-analysis by Papakostas et al7 of the same 10 randomized, double-blind, placebo-controlled trials suggested SSRIs may confer an advantage over bupropion in treating a subset of patients with “anxious depression,” which they defined as a HDRS-AS score ≥7. The authors noted the advantage was statistically significant, although “modest.”
Other smaller studies suggest that bupropion does not increase anxiety.8,9 A pilot study (N = 24, no placebo control) concluded that bupropion XL was comparable to escitalopram in treating anxiety in outpatients with generalized anxiety disorder.8
Because designing and executing drug trials can be expensive, it is not surprising that most of the evidence cited above derives from pharmaceutical company-sponsored or industry-affiliated work. As such, we should evaluate available evidence within the context of what we hear from and observe in our patients.
Our opinion
When assessing patients with depression and anxiety, we must carefully evaluate symptoms to distinguish between depression with associated anxiety symptoms and depression with a comorbid anxiety disorder.
If a patient suffers from depression with associated anxiety symptoms (“anxious depression”), keep in mind that although some data demonstrate a superior response to SSRIs, other studies show no difference in effect. Some research—albeit smaller, less compelling studies—suggests that bupropion may decrease anxiety.
If your patient suffers from comorbid depression and an anxiety disorder, bupropion would not be a first-line choice because it is not FDA-approved to treat anxiety disorders. Although it is possible that anxiety/agitation could result from bupropion use, there is not sufficient data to support its reputation as ”anxiogenic.”
What is your experience?
Do you agree with the authors? Send comments to [email protected] or share your thoughts on http://www.facebook.com/CurrentPsychiatry.
Related Resource
- American Psychiatric Association. Mixed anxiety-depressive disorder. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000:780-781.
Drug Brand Names
- Bupropion • Wellbutrin, Zyban
- Escitalopram • Lexapro
- Sertraline • Zoloft
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Fava M, Rush AJ, Alpert JE, et al. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry. 2008;165(3):342-351.
2. Wellbutrin [package insert]. Research Triangle Park NC: GlaxoSmithKline; 2008.
3. Rush AJ, Trivedi MH, Carmody TJ, et al. Response in relation to baseline anxiety levels in major depressive disorder treated with bupropion sustained release or sertraline. Neuropsychopharmacology. 2001;25(1):131-138.
4. Trivedi MH, Rush AJ, Carmody TJ, et al. Do bupropion SR and sertraline differ in their effects on anxiety in depressed patients? J Clin Psychiatry. 2001;62(10):776-781.
5. Nieuwstraten CE, Dolovich LR. Bupropion versus selective serotonin-reuptake inhibitors for treatment of depression. Ann Pharmacother. 2001;35(12):1608-1613.
6. Papakostas GI, Trivedi MH, Alpert JE, et al. Efficacy of bupropion and the selective serotonin reuptake inhibitors in the treatment of anxiety symptoms in major depressive disorder: a meta-analysis of individual patient data from 10 double-blind, randomized clinical trials. J Psychiatr Res. 2008;42(2):134-140.
7. Papakostas GI, Stahl SM, Krishen A, et al. Efficacy of bupropion and the selective serotonin reuptake inhibitors in the treatment of major depressive disorder with high levels of anxiety (anxious depression): a pooled analysis of 10 studies. J Clin Psychiatry. 2008;69(8):1287-1292.
8. Bystritsky A, Kerwin L, Feusner JD, et al. A pilot controlled trial of bupropion XL versus escitalopram in generalized anxiety disorder. Psychopharmacol Bull. 2008;41(1):46-51.
9. Feighner JP, Gardner EA, Johnston JA, et al. Double-blind comparison of bupropion and fluoxetine in depressed outpatients. J Clin Psychiatry. 1991;52(8):329-335.
1. Fava M, Rush AJ, Alpert JE, et al. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry. 2008;165(3):342-351.
2. Wellbutrin [package insert]. Research Triangle Park NC: GlaxoSmithKline; 2008.
3. Rush AJ, Trivedi MH, Carmody TJ, et al. Response in relation to baseline anxiety levels in major depressive disorder treated with bupropion sustained release or sertraline. Neuropsychopharmacology. 2001;25(1):131-138.
4. Trivedi MH, Rush AJ, Carmody TJ, et al. Do bupropion SR and sertraline differ in their effects on anxiety in depressed patients? J Clin Psychiatry. 2001;62(10):776-781.
5. Nieuwstraten CE, Dolovich LR. Bupropion versus selective serotonin-reuptake inhibitors for treatment of depression. Ann Pharmacother. 2001;35(12):1608-1613.
6. Papakostas GI, Trivedi MH, Alpert JE, et al. Efficacy of bupropion and the selective serotonin reuptake inhibitors in the treatment of anxiety symptoms in major depressive disorder: a meta-analysis of individual patient data from 10 double-blind, randomized clinical trials. J Psychiatr Res. 2008;42(2):134-140.
7. Papakostas GI, Stahl SM, Krishen A, et al. Efficacy of bupropion and the selective serotonin reuptake inhibitors in the treatment of major depressive disorder with high levels of anxiety (anxious depression): a pooled analysis of 10 studies. J Clin Psychiatry. 2008;69(8):1287-1292.
8. Bystritsky A, Kerwin L, Feusner JD, et al. A pilot controlled trial of bupropion XL versus escitalopram in generalized anxiety disorder. Psychopharmacol Bull. 2008;41(1):46-51.
9. Feighner JP, Gardner EA, Johnston JA, et al. Double-blind comparison of bupropion and fluoxetine in depressed outpatients. J Clin Psychiatry. 1991;52(8):329-335.
Recognizing mimics of depression: The ‘8 Ds’
Discuss this article at www.facebook.com/CurrentPsychiatry
Many psychiatric and medical illnesses—as well as normal reactions to stressors—have symptoms that overlap with those of depressive disorders, including outwardly sad or dysphoric appearance, irritability, apathy or amotivation, fatigue, difficulty making decisions, social withdrawal, and sleep disturbances. This cluster of symptoms forms a readily observable behavioral phenotype that clinicians may label as depression before considering a broader differential diagnosis.
To better understand what other conditions belong in the differential diagnosis, we reviewed a sample of 100 consecutive medical/surgical inpatients referred to our consultation-liaison psychiatry practice for evaluation of “depression.” Ultimately, only 29 of these patients received a depression diagnosis. Many of the other diagnoses given in our sample required attention during inpatient medical or surgical care because they were potentially life-threatening if left unaddressed—such as delirium—or they interfered with managing the primary medical or surgical condition for which the patient was hospitalized.
Hurried or uncertain primary care clinicians frequently use “depression” as a catch-all term when requesting psychiatric consultation for patients who seem depressed. A wide range of conditions can mimic depression, and the art of psychosomatic psychiatry includes considering protean possibilities when assessing a patient. We identified 7 diagnoses that mimic major depression and developed our “8 D” differential to help clinicians properly diagnose “depressed” patients who have something other than a depressive disorder. Although our sample consisted of hospitalized patients, these mimics of depression may be found among patients referred from other clinical settings for evaluation of possible depression.
The perils of misdiagnosis
Depression is common among patients hospitalized with medical or surgical conditions. DSM-IV-TR diagnostic criteria for a major depressive episode (MDE) include the presence of low mood and/or anhedonia, plus ≥4 other depressive symptoms for ≥2 weeks.1 Growing evidence suggests that the relationship between depression and morbidity and mortality in medical illness is bidirectional, and nonpsychiatrists are becoming increasingly aware of major depression’s serious impact on their patients’ physical health.2-5
Although improving nonpsychiatrists’ recognition of depression in medically ill patients is laudable, it comes with a high false-positive rate. In a study of primary care outpatients, Berardi et al found that 45% of patients labeled “depressed” did not meet ICD-10 criteria for major depression, but >25% of those patients were prescribed an antidepressant.6 In a large retrospective study, Boland et al found that approximately 40% of patients referred to an inpatient psychiatric consultation service for depression did not meet criteria for a depressive illness, and primary medical services often confused organic syndromes such as delirium and dementia with depression.7 Similarly, Clarke et al found that 26% of medical and surgical inpatients referred to psychiatry with “depression” had another diagnosis—commonly delirium—that better accounted for their symptoms.8
What is the harm in overdiagnosing depression? Missing a serious or life-threatening diagnosis is a primary concern. For example, unrecognized delirium, which frequently was misdiagnosed as depression in the Berardi,6 Boland,7 and Clarke8 studies, is associated with myriad difficulties, including higher morbidity and mortality.9 Substance use disorders, which also commonly masquerade as depression, frequently are comorbid with medical illness. Delays in appropriate treatment of withdrawal syndromes—particularly of alcohol and sedative/hypnotic medications—are risk factors for increased mortality in these illnesses.10
Inappropriate, potentially harmful interventions are another concern. Many patients diagnosed with depression are prescribed antidepressants, but this is not always a benign intervention. Smith et al found that >10% of adult medical inpatients referred to a psychiatry consultation service who were started on an antidepressant had an adverse drug reaction severe enough to warrant discontinuing the medication.11 Antidepressant side effects relevant to medically ill patients include hyponatremia, serotonin syndrome, and exacerbation of delirium.12
Polypharmacy in medically ill patients increases the risk for serious drug-drug interactions. For example, serotonergic antidepressants can increase the risk for serotonin syndrome when combined with the analgesic tramadol, which has serotonergic activity,13 or the antibiotic linezolid, which is a reversible monoamine oxidase inhibitor.14 Many antidepressants—including paroxetine, fluoxetine, bupropion, sertraline, and duloxetine—are moderate to strong inhibitors of cytochrome P450 2D6 and therefore affect metabolism of many medications, including several beta blockers and antiarrhythmics, as well as the anti-estrogen tamoxifen. In the case of tamoxifen, which is a prodrug converted to active form by 2D6, concomitant use of a 2D6 inhibitor can substantially reduce the medication’s in vivo efficacy and lead to higher morbidity and mortality in breast cancer patients.15 As with any treatment, a decision to prescribe antidepressants needs to carefully be weighed in light of individual risks and benefits. This analysis starts by ensuring that an antidepressant is indicated.
Another concern is failing to recognize immediate human suffering for what it is. Hospitals and doctors’ offices are places of pain and loss as patients encounter morbidity and mortality in themselves and their loved ones. Rushing to pathologize the psychological or social manifestations of this pain can be invalidating to patients and may impair the doctor-patient relationship.
The 8 Ds
To determine what these “depression lookalike” syndromes could be, we identified 100 consecutive consultations to our adult inpatient psychiatry consultation-liaison team with a question of “depression.” We reviewed each patient’s chart, and recorded the diagnosis the psychiatrist gave to explain the patient’s depressed appearance. Data were recorded without patient identifiers, and the Mayo Clinic institutional review board (IRB) determined this study was exempt from IRB review.
Our sample included 45 men and 55 women with an average age of 48 (range: 18 to 91). On evaluation, 3 patients were given no psychiatric diagnosis, 29 were categorized as depressed, and 68 fell into one of 7 other “D” categories we describe below.
Depressed. These patients met criteria for a MDE in the context of major depressive disorder (MDD) or bipolar disorder, dysthymic disorder, mood disorder due to a general medical condition, substance-induced mood disorder, or depressive disorder not otherwise specified.
Demoralized. Patients who had difficulty adjusting to or coping with illness, and received a DSM-IV-TR diagnosis of adjustment disorder with the illness as the inciting stressor were placed in this category. Consistent with adjustment disorder criteria, these patients did not have depressive symptoms of sufficient intensity or duration to meet criteria for MDD or another primary mood disorder.
Difficult. For these patients, the primary issue was a breakdown in the therapeutic alliance with their treatment team. They received DSM-IV-TR diagnoses of personality disorder, noncompliance with treatment, or adult antisocial behavior.
Drugged. Patients in this category appeared depressed as a result of illicit substance use or misuse of alcohol or pharmaceuticals. DSM-IV-TR diagnoses included substance intoxication or withdrawal and substance abuse or dependence.
Delirious. This group consisted of patients with acute disruption in attention and level of consciousness that met DSM-IV-TR criteria for delirium. Patients whose delirious appearance was the result of illicit substance use or pharmaceutical misuse were categorized as “Drugged” rather than “Delirious.”
Disaffiliated. Patients in this category had dysphoria not commensurate with a full-blown mood disorder but attributable to grief from losing a major relationship to death, separation, or divorce. These patients received a DSM-IV-TR diagnosis of bereavement or a partner relational problem.
Delusional. These patients demonstrated amotivation and affective blunting as a result of a primary psychotic disorder such as schizophrenia. In preparation for emergent surgery, these patients had been prevented from taking anything orally, including antipsychotics, and their antipsychotics had not been restarted, which precipitated a gradual return of psychotic symptoms in the days after surgery.
Dulled. Two patients in our sample had irreversible cognitive deficits that explained their withdrawal and blunted affect; 1 had dementia and the other had mental retardation.
Managing the other Ds
In our sample, the most commonly misdiagnosed patients were those having difficulty adjusting to illness (Demoralized) or to other life events (Disaffiliated) (Table 1). In these cases, misdiagnosis has substantial treatment implications because these patients are better served by acute, illness-specific interventions that bolster coping skills, rather than pharmacotherapy or psychotherapy that targets entrenched depressive symptoms. For these patients, psychiatrists may “prescribe” interventions such as visits with a chaplain or other spiritual advisor, telephone calls or visits from family, friends, and other social supports, participation in physical or occupational therapy to improve adaptive functioning, or connecting with other patients in similar situations. Often, the key with these patients is to identify ways they have managed previous stressors and creatively use those resources to adapt to their new situation.
A second large group in our sample consisted of patients actively or passively fighting with their treatment team—the Difficult (Table 2). The treatment team or the patient’s caregivers and loved ones often are more distressed by the “difficult” patient’s symptoms than the patient, who may instead focus on his or her disappointment with caregivers who are unable to meet the patient’s unreasonable expectations. These challenges typically can be addressed by clarifying the salient issues for both the patient and team and establishing a liaison between patient and team to improve communication among all parties. Multidisciplinary care conferences can be an excellent way to ensure that the care team provides the patient with consistent communication and care.
A third group had potentially life-threatening conditions such as substance abuse/withdrawal or delirium as the cause of their “depressive” symptoms—the Drugged and the Delirious (Table 3). Recognizing an organic etiology of mood or behavioral symptoms is important because managing the underlying problem is the primary treatment strategy, not psychopharmacologic or psychotherapeutic intervention. Early identification and appropriate management of these patients could prevent further deterioration, improve medical outcomes, and shorten length of hospital stay.
A final group of patients was those whose chronic psychiatric and cognitive issues may go unrecognized or unappreciated until they interfere with the patient’s medical care—the Delusional and the Dulled (Table 2). In these cases, the correct diagnosis often hinges on obtaining a thorough history through collateral sources. The consulting psychiatrist can be crucial in co-managing these patients by establishing a liaison with outpatient providers, suggesting in-hospital management strategies such as alternate routes of administration of antipsychotics for patients with psychotic disorders, and connecting patients with outpatient supports after hospitalization. Continuity between inpatient and outpatient management is necessary to ensure a successful medical and psychiatric outcome.
Our 8 Ds are limited to the subset of patients referred by their medical teams with a question of depression. These referrals may have been motivated by a variety of patient, family, and team factors above and beyond the categories discussed in this article, and therefore may not accurately represent all patients who present with depressive symptoms in an inpatient setting. However, we hope that providing a mnemonic that suggests an extensive differential for a depressed phenotype may improve identification and management of these issues.
Table 1
Psychological crises that may look like depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Depressed” patients met DSM-IV-TR criteria for a depressive disorder | 29% | Emotional symptoms: Depressed mood, anhedonia Cognitive symptoms: concentration problems, indecisiveness, negative thoughts, irrational guilt Physical symptoms: changes in sleep, appetite, energy | Initiate psychotherapy with or without antidepressants |
| “Demoralized” patients had difficulty coping with a medical illness | 23% | Close temporal association with illness. Few neurovegetative symptoms. Able to maintain future orientation/hope | Provide compassion, recognition, and normalization. Connect patients with illness-specific supports (groups, social work, chaplaincy). Implement interventions to improve functioning (eg, PT/OT). Encourage patients to engage in activities that have helped them cope in the past |
| “Disaffiliated” patients had dysphoria attributable to grief from losing a major relationship | 3% | Few neurovegetative symptoms. Able to maintain future orientation/hope. Improvement typical as time since loss increases | Encourage patients to connect with other supportive relationships. Refer patients to grief resources (eg, hospice, spiritual supports) |
| OT: occupational therapy; PT: physical therapy | |||
Table 2
Differentiating patients with social challenges from those with depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Difficult” patients have a breakdown in the therapeutic alliance with their treatment team | 15% | Mood changes often intense, immediate, and reactive to situation. Frequent breakdowns in communication with care team. Care team more distressed by patient’s symptoms than the patient | Establish frequent communication among care team members. Use multidisciplinary care conferences to clarify salient issues for patients and their team. Provide patients with consistent information and expectations |
| “Delusional” patients had affective blunting as a result of a psychotic disorder | 2% | Suspicious about care team/procedures. Seems frightened or scans the room. On antipsychotics at admission. Slowly developing symptoms over several days after home medications are held | Acquire collateral history (an assigned community case manager or social worker can be an important source). Establish a plan for administering psychotropics in chronically mentally ill patients; consider IM or orally disintegrating formulations |
| “Dulled” patients had irreversible cognitive deficits | 2% | Baseline impairments in memory and/or independent functioning | Acquire collateral history. Perform a safety assessment of home environment with attention to need for additional supports |
| IM: intramuscular | |||
Table 3
Substance abuse and delirium can mimic depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Drugged” patients appeared depressed as a result of substance use/ withdrawal | 12% | Acute presentation closely mimicking mood, anxiety, or psychotic disorders. Emotional symptoms present when intoxicated or withdrawing and resolved during sobriety | Implement safety interventions to prevent self-harm or aggression during acute phase. Support and monitor withdrawal as indicated. Reassess mood state and symptoms once the patient is sober. Refer for chemical dependency evaluation |
| “Delirious” patients met DSM-IV-TR criteria for delirium | 11% | Disoriented and inattentive. Onset over hours to days. Waxing and waning throughout the day. Possible hallucinations (often visual or tactile) | Identify and correct underlying medical cause(s). Restore the patient’s sleep-wake cycle. Provide frequent reorientation and reassurance |
Related Resources
- Stern TA, Fricchione GL, Cassem NH, et al, eds. Massachusetts General Hospital handbook of general hospital psychiatry, 6th ed. Philadelphia, PA: Saunders Elsevier; 2010.
- Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. 2nd ed. Arlington, VA: American Psychiatric Publishing, Inc.; 2011.
- Academy of Psychosomatic Medicine. www.apm.org.
- Caplan JP, Stern TA. Mnemonics in a mnutshell: 32 aids to psychiatric diagnosis. Current Psychiatry. 2008;7(10):27-33.
Drug Brand Names
- Bupropion • Wellbutrin, Zyban
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Linezolid • Zyvox
- Paroxetine • Paxil
- Sertraline • Zoloft
- Tamoxifen • Nolvadex
- Tramadol • Ultracet
Disclosures
Dr. Bostwick reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Rackley receives research/grant support from the Maternal and Child Health Bureau, Health Resources and Services Administration, U.S. Department of Health and Human Services, for a Collaborative Office Rounds program with primary care pediatricians.
1. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Hansen MS, Fink P, Frydenberg M, et al. Use of health services, mental illness, and self-rated disability and health in medical inpatients. Psychosom Med. 2002;64(4):668-675.
3. Hosaka T, Aoki T, Watanabe T, et al. Comorbidity of depression among physically ill patients and its effect on the length of hospital stay. Psychiatry Clin Neurosci. 1999;53(4):491-495.
4. McCusker J, Cole M, Ciampi A, et al. Major depression in older medical inpatients predicts poor physical and mental health status over 12 months. Gen Hosp Psychiatry. 2007;29(4):340-348.
5. McCusker J, Cole M, Dufouil C, et al. The prevalence and correlates of major and minor depression in older medical inpatients. J Am Geriatr Soc. 2005;53(8):1344-1353.
6. Berardi D, Menchetti M, Cevenini N, et al. Increased recognition of depression in primary care. Comparison between primary-care physician and ICD-10 diagnosis of depression. Psychother Psychosom. 2005;74(4):225-230.
7. Boland RJ, Diaz S, Lamdan RM, et al. Overdiagnosis of depression in the general hospital. Gen Hosp Psychiatry. 1996;18(1):28-35.
8. Clarke DM, McKenzie DP, Smith GC. The recognition of depression in patients referred to a consultation-liaison service. J Psychosom Res. 1995;39(3):327-334.
9. Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35(4):350-364.
10. Franklin JE, Levenson JL, McCance-Katz EF. Substance-related disorders. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Washington, DC: American Psychiatric Publishing, Inc.; 2005:387–420.
11. Smith GC, Clarke DM, Handrinos D, et al. Consultation-liaison psychiatrists’ use of antidepressants in the physically ill. Psychosomatics. 2002;43(3):221-227.
12. Robinson MJ, Owen JA. Psychopharmacology. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Washington, DC: American Psychiatric Publishing, Inc.; 2005:387–420.
13. Hersh EV, Pinto A, Moore PA. Adverse drug interactions involving common prescription and over-the-counter analgesic agents. Clin Ther. 2007;29(suppl):2477-2497.
14. Sola CL, Bostwick JM, Hart DA, et al. Anticipating potential linezolid-SSRI interactions in the general hospital setting: an MAOI in disguise. Mayo Clin Proc. 2006;81(3):330-334.
15. Stearns V, Johnson MD, Rae JM, et al. Active tamoxifen metabolite plasma concentrations after coadministration of tamoxifen and the selective serotonin reuptake inhibitor paroxetine. J Natl Cancer Inst. 2003;95(23):1758-1764.
Discuss this article at www.facebook.com/CurrentPsychiatry
Many psychiatric and medical illnesses—as well as normal reactions to stressors—have symptoms that overlap with those of depressive disorders, including outwardly sad or dysphoric appearance, irritability, apathy or amotivation, fatigue, difficulty making decisions, social withdrawal, and sleep disturbances. This cluster of symptoms forms a readily observable behavioral phenotype that clinicians may label as depression before considering a broader differential diagnosis.
To better understand what other conditions belong in the differential diagnosis, we reviewed a sample of 100 consecutive medical/surgical inpatients referred to our consultation-liaison psychiatry practice for evaluation of “depression.” Ultimately, only 29 of these patients received a depression diagnosis. Many of the other diagnoses given in our sample required attention during inpatient medical or surgical care because they were potentially life-threatening if left unaddressed—such as delirium—or they interfered with managing the primary medical or surgical condition for which the patient was hospitalized.
Hurried or uncertain primary care clinicians frequently use “depression” as a catch-all term when requesting psychiatric consultation for patients who seem depressed. A wide range of conditions can mimic depression, and the art of psychosomatic psychiatry includes considering protean possibilities when assessing a patient. We identified 7 diagnoses that mimic major depression and developed our “8 D” differential to help clinicians properly diagnose “depressed” patients who have something other than a depressive disorder. Although our sample consisted of hospitalized patients, these mimics of depression may be found among patients referred from other clinical settings for evaluation of possible depression.
The perils of misdiagnosis
Depression is common among patients hospitalized with medical or surgical conditions. DSM-IV-TR diagnostic criteria for a major depressive episode (MDE) include the presence of low mood and/or anhedonia, plus ≥4 other depressive symptoms for ≥2 weeks.1 Growing evidence suggests that the relationship between depression and morbidity and mortality in medical illness is bidirectional, and nonpsychiatrists are becoming increasingly aware of major depression’s serious impact on their patients’ physical health.2-5
Although improving nonpsychiatrists’ recognition of depression in medically ill patients is laudable, it comes with a high false-positive rate. In a study of primary care outpatients, Berardi et al found that 45% of patients labeled “depressed” did not meet ICD-10 criteria for major depression, but >25% of those patients were prescribed an antidepressant.6 In a large retrospective study, Boland et al found that approximately 40% of patients referred to an inpatient psychiatric consultation service for depression did not meet criteria for a depressive illness, and primary medical services often confused organic syndromes such as delirium and dementia with depression.7 Similarly, Clarke et al found that 26% of medical and surgical inpatients referred to psychiatry with “depression” had another diagnosis—commonly delirium—that better accounted for their symptoms.8
What is the harm in overdiagnosing depression? Missing a serious or life-threatening diagnosis is a primary concern. For example, unrecognized delirium, which frequently was misdiagnosed as depression in the Berardi,6 Boland,7 and Clarke8 studies, is associated with myriad difficulties, including higher morbidity and mortality.9 Substance use disorders, which also commonly masquerade as depression, frequently are comorbid with medical illness. Delays in appropriate treatment of withdrawal syndromes—particularly of alcohol and sedative/hypnotic medications—are risk factors for increased mortality in these illnesses.10
Inappropriate, potentially harmful interventions are another concern. Many patients diagnosed with depression are prescribed antidepressants, but this is not always a benign intervention. Smith et al found that >10% of adult medical inpatients referred to a psychiatry consultation service who were started on an antidepressant had an adverse drug reaction severe enough to warrant discontinuing the medication.11 Antidepressant side effects relevant to medically ill patients include hyponatremia, serotonin syndrome, and exacerbation of delirium.12
Polypharmacy in medically ill patients increases the risk for serious drug-drug interactions. For example, serotonergic antidepressants can increase the risk for serotonin syndrome when combined with the analgesic tramadol, which has serotonergic activity,13 or the antibiotic linezolid, which is a reversible monoamine oxidase inhibitor.14 Many antidepressants—including paroxetine, fluoxetine, bupropion, sertraline, and duloxetine—are moderate to strong inhibitors of cytochrome P450 2D6 and therefore affect metabolism of many medications, including several beta blockers and antiarrhythmics, as well as the anti-estrogen tamoxifen. In the case of tamoxifen, which is a prodrug converted to active form by 2D6, concomitant use of a 2D6 inhibitor can substantially reduce the medication’s in vivo efficacy and lead to higher morbidity and mortality in breast cancer patients.15 As with any treatment, a decision to prescribe antidepressants needs to carefully be weighed in light of individual risks and benefits. This analysis starts by ensuring that an antidepressant is indicated.
Another concern is failing to recognize immediate human suffering for what it is. Hospitals and doctors’ offices are places of pain and loss as patients encounter morbidity and mortality in themselves and their loved ones. Rushing to pathologize the psychological or social manifestations of this pain can be invalidating to patients and may impair the doctor-patient relationship.
The 8 Ds
To determine what these “depression lookalike” syndromes could be, we identified 100 consecutive consultations to our adult inpatient psychiatry consultation-liaison team with a question of “depression.” We reviewed each patient’s chart, and recorded the diagnosis the psychiatrist gave to explain the patient’s depressed appearance. Data were recorded without patient identifiers, and the Mayo Clinic institutional review board (IRB) determined this study was exempt from IRB review.
Our sample included 45 men and 55 women with an average age of 48 (range: 18 to 91). On evaluation, 3 patients were given no psychiatric diagnosis, 29 were categorized as depressed, and 68 fell into one of 7 other “D” categories we describe below.
Depressed. These patients met criteria for a MDE in the context of major depressive disorder (MDD) or bipolar disorder, dysthymic disorder, mood disorder due to a general medical condition, substance-induced mood disorder, or depressive disorder not otherwise specified.
Demoralized. Patients who had difficulty adjusting to or coping with illness, and received a DSM-IV-TR diagnosis of adjustment disorder with the illness as the inciting stressor were placed in this category. Consistent with adjustment disorder criteria, these patients did not have depressive symptoms of sufficient intensity or duration to meet criteria for MDD or another primary mood disorder.
Difficult. For these patients, the primary issue was a breakdown in the therapeutic alliance with their treatment team. They received DSM-IV-TR diagnoses of personality disorder, noncompliance with treatment, or adult antisocial behavior.
Drugged. Patients in this category appeared depressed as a result of illicit substance use or misuse of alcohol or pharmaceuticals. DSM-IV-TR diagnoses included substance intoxication or withdrawal and substance abuse or dependence.
Delirious. This group consisted of patients with acute disruption in attention and level of consciousness that met DSM-IV-TR criteria for delirium. Patients whose delirious appearance was the result of illicit substance use or pharmaceutical misuse were categorized as “Drugged” rather than “Delirious.”
Disaffiliated. Patients in this category had dysphoria not commensurate with a full-blown mood disorder but attributable to grief from losing a major relationship to death, separation, or divorce. These patients received a DSM-IV-TR diagnosis of bereavement or a partner relational problem.
Delusional. These patients demonstrated amotivation and affective blunting as a result of a primary psychotic disorder such as schizophrenia. In preparation for emergent surgery, these patients had been prevented from taking anything orally, including antipsychotics, and their antipsychotics had not been restarted, which precipitated a gradual return of psychotic symptoms in the days after surgery.
Dulled. Two patients in our sample had irreversible cognitive deficits that explained their withdrawal and blunted affect; 1 had dementia and the other had mental retardation.
Managing the other Ds
In our sample, the most commonly misdiagnosed patients were those having difficulty adjusting to illness (Demoralized) or to other life events (Disaffiliated) (Table 1). In these cases, misdiagnosis has substantial treatment implications because these patients are better served by acute, illness-specific interventions that bolster coping skills, rather than pharmacotherapy or psychotherapy that targets entrenched depressive symptoms. For these patients, psychiatrists may “prescribe” interventions such as visits with a chaplain or other spiritual advisor, telephone calls or visits from family, friends, and other social supports, participation in physical or occupational therapy to improve adaptive functioning, or connecting with other patients in similar situations. Often, the key with these patients is to identify ways they have managed previous stressors and creatively use those resources to adapt to their new situation.
A second large group in our sample consisted of patients actively or passively fighting with their treatment team—the Difficult (Table 2). The treatment team or the patient’s caregivers and loved ones often are more distressed by the “difficult” patient’s symptoms than the patient, who may instead focus on his or her disappointment with caregivers who are unable to meet the patient’s unreasonable expectations. These challenges typically can be addressed by clarifying the salient issues for both the patient and team and establishing a liaison between patient and team to improve communication among all parties. Multidisciplinary care conferences can be an excellent way to ensure that the care team provides the patient with consistent communication and care.
A third group had potentially life-threatening conditions such as substance abuse/withdrawal or delirium as the cause of their “depressive” symptoms—the Drugged and the Delirious (Table 3). Recognizing an organic etiology of mood or behavioral symptoms is important because managing the underlying problem is the primary treatment strategy, not psychopharmacologic or psychotherapeutic intervention. Early identification and appropriate management of these patients could prevent further deterioration, improve medical outcomes, and shorten length of hospital stay.
A final group of patients was those whose chronic psychiatric and cognitive issues may go unrecognized or unappreciated until they interfere with the patient’s medical care—the Delusional and the Dulled (Table 2). In these cases, the correct diagnosis often hinges on obtaining a thorough history through collateral sources. The consulting psychiatrist can be crucial in co-managing these patients by establishing a liaison with outpatient providers, suggesting in-hospital management strategies such as alternate routes of administration of antipsychotics for patients with psychotic disorders, and connecting patients with outpatient supports after hospitalization. Continuity between inpatient and outpatient management is necessary to ensure a successful medical and psychiatric outcome.
Our 8 Ds are limited to the subset of patients referred by their medical teams with a question of depression. These referrals may have been motivated by a variety of patient, family, and team factors above and beyond the categories discussed in this article, and therefore may not accurately represent all patients who present with depressive symptoms in an inpatient setting. However, we hope that providing a mnemonic that suggests an extensive differential for a depressed phenotype may improve identification and management of these issues.
Table 1
Psychological crises that may look like depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Depressed” patients met DSM-IV-TR criteria for a depressive disorder | 29% | Emotional symptoms: Depressed mood, anhedonia Cognitive symptoms: concentration problems, indecisiveness, negative thoughts, irrational guilt Physical symptoms: changes in sleep, appetite, energy | Initiate psychotherapy with or without antidepressants |
| “Demoralized” patients had difficulty coping with a medical illness | 23% | Close temporal association with illness. Few neurovegetative symptoms. Able to maintain future orientation/hope | Provide compassion, recognition, and normalization. Connect patients with illness-specific supports (groups, social work, chaplaincy). Implement interventions to improve functioning (eg, PT/OT). Encourage patients to engage in activities that have helped them cope in the past |
| “Disaffiliated” patients had dysphoria attributable to grief from losing a major relationship | 3% | Few neurovegetative symptoms. Able to maintain future orientation/hope. Improvement typical as time since loss increases | Encourage patients to connect with other supportive relationships. Refer patients to grief resources (eg, hospice, spiritual supports) |
| OT: occupational therapy; PT: physical therapy | |||
Table 2
Differentiating patients with social challenges from those with depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Difficult” patients have a breakdown in the therapeutic alliance with their treatment team | 15% | Mood changes often intense, immediate, and reactive to situation. Frequent breakdowns in communication with care team. Care team more distressed by patient’s symptoms than the patient | Establish frequent communication among care team members. Use multidisciplinary care conferences to clarify salient issues for patients and their team. Provide patients with consistent information and expectations |
| “Delusional” patients had affective blunting as a result of a psychotic disorder | 2% | Suspicious about care team/procedures. Seems frightened or scans the room. On antipsychotics at admission. Slowly developing symptoms over several days after home medications are held | Acquire collateral history (an assigned community case manager or social worker can be an important source). Establish a plan for administering psychotropics in chronically mentally ill patients; consider IM or orally disintegrating formulations |
| “Dulled” patients had irreversible cognitive deficits | 2% | Baseline impairments in memory and/or independent functioning | Acquire collateral history. Perform a safety assessment of home environment with attention to need for additional supports |
| IM: intramuscular | |||
Table 3
Substance abuse and delirium can mimic depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Drugged” patients appeared depressed as a result of substance use/ withdrawal | 12% | Acute presentation closely mimicking mood, anxiety, or psychotic disorders. Emotional symptoms present when intoxicated or withdrawing and resolved during sobriety | Implement safety interventions to prevent self-harm or aggression during acute phase. Support and monitor withdrawal as indicated. Reassess mood state and symptoms once the patient is sober. Refer for chemical dependency evaluation |
| “Delirious” patients met DSM-IV-TR criteria for delirium | 11% | Disoriented and inattentive. Onset over hours to days. Waxing and waning throughout the day. Possible hallucinations (often visual or tactile) | Identify and correct underlying medical cause(s). Restore the patient’s sleep-wake cycle. Provide frequent reorientation and reassurance |
Related Resources
- Stern TA, Fricchione GL, Cassem NH, et al, eds. Massachusetts General Hospital handbook of general hospital psychiatry, 6th ed. Philadelphia, PA: Saunders Elsevier; 2010.
- Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. 2nd ed. Arlington, VA: American Psychiatric Publishing, Inc.; 2011.
- Academy of Psychosomatic Medicine. www.apm.org.
- Caplan JP, Stern TA. Mnemonics in a mnutshell: 32 aids to psychiatric diagnosis. Current Psychiatry. 2008;7(10):27-33.
Drug Brand Names
- Bupropion • Wellbutrin, Zyban
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Linezolid • Zyvox
- Paroxetine • Paxil
- Sertraline • Zoloft
- Tamoxifen • Nolvadex
- Tramadol • Ultracet
Disclosures
Dr. Bostwick reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Rackley receives research/grant support from the Maternal and Child Health Bureau, Health Resources and Services Administration, U.S. Department of Health and Human Services, for a Collaborative Office Rounds program with primary care pediatricians.
Discuss this article at www.facebook.com/CurrentPsychiatry
Many psychiatric and medical illnesses—as well as normal reactions to stressors—have symptoms that overlap with those of depressive disorders, including outwardly sad or dysphoric appearance, irritability, apathy or amotivation, fatigue, difficulty making decisions, social withdrawal, and sleep disturbances. This cluster of symptoms forms a readily observable behavioral phenotype that clinicians may label as depression before considering a broader differential diagnosis.
To better understand what other conditions belong in the differential diagnosis, we reviewed a sample of 100 consecutive medical/surgical inpatients referred to our consultation-liaison psychiatry practice for evaluation of “depression.” Ultimately, only 29 of these patients received a depression diagnosis. Many of the other diagnoses given in our sample required attention during inpatient medical or surgical care because they were potentially life-threatening if left unaddressed—such as delirium—or they interfered with managing the primary medical or surgical condition for which the patient was hospitalized.
Hurried or uncertain primary care clinicians frequently use “depression” as a catch-all term when requesting psychiatric consultation for patients who seem depressed. A wide range of conditions can mimic depression, and the art of psychosomatic psychiatry includes considering protean possibilities when assessing a patient. We identified 7 diagnoses that mimic major depression and developed our “8 D” differential to help clinicians properly diagnose “depressed” patients who have something other than a depressive disorder. Although our sample consisted of hospitalized patients, these mimics of depression may be found among patients referred from other clinical settings for evaluation of possible depression.
The perils of misdiagnosis
Depression is common among patients hospitalized with medical or surgical conditions. DSM-IV-TR diagnostic criteria for a major depressive episode (MDE) include the presence of low mood and/or anhedonia, plus ≥4 other depressive symptoms for ≥2 weeks.1 Growing evidence suggests that the relationship between depression and morbidity and mortality in medical illness is bidirectional, and nonpsychiatrists are becoming increasingly aware of major depression’s serious impact on their patients’ physical health.2-5
Although improving nonpsychiatrists’ recognition of depression in medically ill patients is laudable, it comes with a high false-positive rate. In a study of primary care outpatients, Berardi et al found that 45% of patients labeled “depressed” did not meet ICD-10 criteria for major depression, but >25% of those patients were prescribed an antidepressant.6 In a large retrospective study, Boland et al found that approximately 40% of patients referred to an inpatient psychiatric consultation service for depression did not meet criteria for a depressive illness, and primary medical services often confused organic syndromes such as delirium and dementia with depression.7 Similarly, Clarke et al found that 26% of medical and surgical inpatients referred to psychiatry with “depression” had another diagnosis—commonly delirium—that better accounted for their symptoms.8
What is the harm in overdiagnosing depression? Missing a serious or life-threatening diagnosis is a primary concern. For example, unrecognized delirium, which frequently was misdiagnosed as depression in the Berardi,6 Boland,7 and Clarke8 studies, is associated with myriad difficulties, including higher morbidity and mortality.9 Substance use disorders, which also commonly masquerade as depression, frequently are comorbid with medical illness. Delays in appropriate treatment of withdrawal syndromes—particularly of alcohol and sedative/hypnotic medications—are risk factors for increased mortality in these illnesses.10
Inappropriate, potentially harmful interventions are another concern. Many patients diagnosed with depression are prescribed antidepressants, but this is not always a benign intervention. Smith et al found that >10% of adult medical inpatients referred to a psychiatry consultation service who were started on an antidepressant had an adverse drug reaction severe enough to warrant discontinuing the medication.11 Antidepressant side effects relevant to medically ill patients include hyponatremia, serotonin syndrome, and exacerbation of delirium.12
Polypharmacy in medically ill patients increases the risk for serious drug-drug interactions. For example, serotonergic antidepressants can increase the risk for serotonin syndrome when combined with the analgesic tramadol, which has serotonergic activity,13 or the antibiotic linezolid, which is a reversible monoamine oxidase inhibitor.14 Many antidepressants—including paroxetine, fluoxetine, bupropion, sertraline, and duloxetine—are moderate to strong inhibitors of cytochrome P450 2D6 and therefore affect metabolism of many medications, including several beta blockers and antiarrhythmics, as well as the anti-estrogen tamoxifen. In the case of tamoxifen, which is a prodrug converted to active form by 2D6, concomitant use of a 2D6 inhibitor can substantially reduce the medication’s in vivo efficacy and lead to higher morbidity and mortality in breast cancer patients.15 As with any treatment, a decision to prescribe antidepressants needs to carefully be weighed in light of individual risks and benefits. This analysis starts by ensuring that an antidepressant is indicated.
Another concern is failing to recognize immediate human suffering for what it is. Hospitals and doctors’ offices are places of pain and loss as patients encounter morbidity and mortality in themselves and their loved ones. Rushing to pathologize the psychological or social manifestations of this pain can be invalidating to patients and may impair the doctor-patient relationship.
The 8 Ds
To determine what these “depression lookalike” syndromes could be, we identified 100 consecutive consultations to our adult inpatient psychiatry consultation-liaison team with a question of “depression.” We reviewed each patient’s chart, and recorded the diagnosis the psychiatrist gave to explain the patient’s depressed appearance. Data were recorded without patient identifiers, and the Mayo Clinic institutional review board (IRB) determined this study was exempt from IRB review.
Our sample included 45 men and 55 women with an average age of 48 (range: 18 to 91). On evaluation, 3 patients were given no psychiatric diagnosis, 29 were categorized as depressed, and 68 fell into one of 7 other “D” categories we describe below.
Depressed. These patients met criteria for a MDE in the context of major depressive disorder (MDD) or bipolar disorder, dysthymic disorder, mood disorder due to a general medical condition, substance-induced mood disorder, or depressive disorder not otherwise specified.
Demoralized. Patients who had difficulty adjusting to or coping with illness, and received a DSM-IV-TR diagnosis of adjustment disorder with the illness as the inciting stressor were placed in this category. Consistent with adjustment disorder criteria, these patients did not have depressive symptoms of sufficient intensity or duration to meet criteria for MDD or another primary mood disorder.
Difficult. For these patients, the primary issue was a breakdown in the therapeutic alliance with their treatment team. They received DSM-IV-TR diagnoses of personality disorder, noncompliance with treatment, or adult antisocial behavior.
Drugged. Patients in this category appeared depressed as a result of illicit substance use or misuse of alcohol or pharmaceuticals. DSM-IV-TR diagnoses included substance intoxication or withdrawal and substance abuse or dependence.
Delirious. This group consisted of patients with acute disruption in attention and level of consciousness that met DSM-IV-TR criteria for delirium. Patients whose delirious appearance was the result of illicit substance use or pharmaceutical misuse were categorized as “Drugged” rather than “Delirious.”
Disaffiliated. Patients in this category had dysphoria not commensurate with a full-blown mood disorder but attributable to grief from losing a major relationship to death, separation, or divorce. These patients received a DSM-IV-TR diagnosis of bereavement or a partner relational problem.
Delusional. These patients demonstrated amotivation and affective blunting as a result of a primary psychotic disorder such as schizophrenia. In preparation for emergent surgery, these patients had been prevented from taking anything orally, including antipsychotics, and their antipsychotics had not been restarted, which precipitated a gradual return of psychotic symptoms in the days after surgery.
Dulled. Two patients in our sample had irreversible cognitive deficits that explained their withdrawal and blunted affect; 1 had dementia and the other had mental retardation.
Managing the other Ds
In our sample, the most commonly misdiagnosed patients were those having difficulty adjusting to illness (Demoralized) or to other life events (Disaffiliated) (Table 1). In these cases, misdiagnosis has substantial treatment implications because these patients are better served by acute, illness-specific interventions that bolster coping skills, rather than pharmacotherapy or psychotherapy that targets entrenched depressive symptoms. For these patients, psychiatrists may “prescribe” interventions such as visits with a chaplain or other spiritual advisor, telephone calls or visits from family, friends, and other social supports, participation in physical or occupational therapy to improve adaptive functioning, or connecting with other patients in similar situations. Often, the key with these patients is to identify ways they have managed previous stressors and creatively use those resources to adapt to their new situation.
A second large group in our sample consisted of patients actively or passively fighting with their treatment team—the Difficult (Table 2). The treatment team or the patient’s caregivers and loved ones often are more distressed by the “difficult” patient’s symptoms than the patient, who may instead focus on his or her disappointment with caregivers who are unable to meet the patient’s unreasonable expectations. These challenges typically can be addressed by clarifying the salient issues for both the patient and team and establishing a liaison between patient and team to improve communication among all parties. Multidisciplinary care conferences can be an excellent way to ensure that the care team provides the patient with consistent communication and care.
A third group had potentially life-threatening conditions such as substance abuse/withdrawal or delirium as the cause of their “depressive” symptoms—the Drugged and the Delirious (Table 3). Recognizing an organic etiology of mood or behavioral symptoms is important because managing the underlying problem is the primary treatment strategy, not psychopharmacologic or psychotherapeutic intervention. Early identification and appropriate management of these patients could prevent further deterioration, improve medical outcomes, and shorten length of hospital stay.
A final group of patients was those whose chronic psychiatric and cognitive issues may go unrecognized or unappreciated until they interfere with the patient’s medical care—the Delusional and the Dulled (Table 2). In these cases, the correct diagnosis often hinges on obtaining a thorough history through collateral sources. The consulting psychiatrist can be crucial in co-managing these patients by establishing a liaison with outpatient providers, suggesting in-hospital management strategies such as alternate routes of administration of antipsychotics for patients with psychotic disorders, and connecting patients with outpatient supports after hospitalization. Continuity between inpatient and outpatient management is necessary to ensure a successful medical and psychiatric outcome.
Our 8 Ds are limited to the subset of patients referred by their medical teams with a question of depression. These referrals may have been motivated by a variety of patient, family, and team factors above and beyond the categories discussed in this article, and therefore may not accurately represent all patients who present with depressive symptoms in an inpatient setting. However, we hope that providing a mnemonic that suggests an extensive differential for a depressed phenotype may improve identification and management of these issues.
Table 1
Psychological crises that may look like depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Depressed” patients met DSM-IV-TR criteria for a depressive disorder | 29% | Emotional symptoms: Depressed mood, anhedonia Cognitive symptoms: concentration problems, indecisiveness, negative thoughts, irrational guilt Physical symptoms: changes in sleep, appetite, energy | Initiate psychotherapy with or without antidepressants |
| “Demoralized” patients had difficulty coping with a medical illness | 23% | Close temporal association with illness. Few neurovegetative symptoms. Able to maintain future orientation/hope | Provide compassion, recognition, and normalization. Connect patients with illness-specific supports (groups, social work, chaplaincy). Implement interventions to improve functioning (eg, PT/OT). Encourage patients to engage in activities that have helped them cope in the past |
| “Disaffiliated” patients had dysphoria attributable to grief from losing a major relationship | 3% | Few neurovegetative symptoms. Able to maintain future orientation/hope. Improvement typical as time since loss increases | Encourage patients to connect with other supportive relationships. Refer patients to grief resources (eg, hospice, spiritual supports) |
| OT: occupational therapy; PT: physical therapy | |||
Table 2
Differentiating patients with social challenges from those with depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Difficult” patients have a breakdown in the therapeutic alliance with their treatment team | 15% | Mood changes often intense, immediate, and reactive to situation. Frequent breakdowns in communication with care team. Care team more distressed by patient’s symptoms than the patient | Establish frequent communication among care team members. Use multidisciplinary care conferences to clarify salient issues for patients and their team. Provide patients with consistent information and expectations |
| “Delusional” patients had affective blunting as a result of a psychotic disorder | 2% | Suspicious about care team/procedures. Seems frightened or scans the room. On antipsychotics at admission. Slowly developing symptoms over several days after home medications are held | Acquire collateral history (an assigned community case manager or social worker can be an important source). Establish a plan for administering psychotropics in chronically mentally ill patients; consider IM or orally disintegrating formulations |
| “Dulled” patients had irreversible cognitive deficits | 2% | Baseline impairments in memory and/or independent functioning | Acquire collateral history. Perform a safety assessment of home environment with attention to need for additional supports |
| IM: intramuscular | |||
Table 3
Substance abuse and delirium can mimic depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Drugged” patients appeared depressed as a result of substance use/ withdrawal | 12% | Acute presentation closely mimicking mood, anxiety, or psychotic disorders. Emotional symptoms present when intoxicated or withdrawing and resolved during sobriety | Implement safety interventions to prevent self-harm or aggression during acute phase. Support and monitor withdrawal as indicated. Reassess mood state and symptoms once the patient is sober. Refer for chemical dependency evaluation |
| “Delirious” patients met DSM-IV-TR criteria for delirium | 11% | Disoriented and inattentive. Onset over hours to days. Waxing and waning throughout the day. Possible hallucinations (often visual or tactile) | Identify and correct underlying medical cause(s). Restore the patient’s sleep-wake cycle. Provide frequent reorientation and reassurance |
Related Resources
- Stern TA, Fricchione GL, Cassem NH, et al, eds. Massachusetts General Hospital handbook of general hospital psychiatry, 6th ed. Philadelphia, PA: Saunders Elsevier; 2010.
- Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. 2nd ed. Arlington, VA: American Psychiatric Publishing, Inc.; 2011.
- Academy of Psychosomatic Medicine. www.apm.org.
- Caplan JP, Stern TA. Mnemonics in a mnutshell: 32 aids to psychiatric diagnosis. Current Psychiatry. 2008;7(10):27-33.
Drug Brand Names
- Bupropion • Wellbutrin, Zyban
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Linezolid • Zyvox
- Paroxetine • Paxil
- Sertraline • Zoloft
- Tamoxifen • Nolvadex
- Tramadol • Ultracet
Disclosures
Dr. Bostwick reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Rackley receives research/grant support from the Maternal and Child Health Bureau, Health Resources and Services Administration, U.S. Department of Health and Human Services, for a Collaborative Office Rounds program with primary care pediatricians.
1. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Hansen MS, Fink P, Frydenberg M, et al. Use of health services, mental illness, and self-rated disability and health in medical inpatients. Psychosom Med. 2002;64(4):668-675.
3. Hosaka T, Aoki T, Watanabe T, et al. Comorbidity of depression among physically ill patients and its effect on the length of hospital stay. Psychiatry Clin Neurosci. 1999;53(4):491-495.
4. McCusker J, Cole M, Ciampi A, et al. Major depression in older medical inpatients predicts poor physical and mental health status over 12 months. Gen Hosp Psychiatry. 2007;29(4):340-348.
5. McCusker J, Cole M, Dufouil C, et al. The prevalence and correlates of major and minor depression in older medical inpatients. J Am Geriatr Soc. 2005;53(8):1344-1353.
6. Berardi D, Menchetti M, Cevenini N, et al. Increased recognition of depression in primary care. Comparison between primary-care physician and ICD-10 diagnosis of depression. Psychother Psychosom. 2005;74(4):225-230.
7. Boland RJ, Diaz S, Lamdan RM, et al. Overdiagnosis of depression in the general hospital. Gen Hosp Psychiatry. 1996;18(1):28-35.
8. Clarke DM, McKenzie DP, Smith GC. The recognition of depression in patients referred to a consultation-liaison service. J Psychosom Res. 1995;39(3):327-334.
9. Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35(4):350-364.
10. Franklin JE, Levenson JL, McCance-Katz EF. Substance-related disorders. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Washington, DC: American Psychiatric Publishing, Inc.; 2005:387–420.
11. Smith GC, Clarke DM, Handrinos D, et al. Consultation-liaison psychiatrists’ use of antidepressants in the physically ill. Psychosomatics. 2002;43(3):221-227.
12. Robinson MJ, Owen JA. Psychopharmacology. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Washington, DC: American Psychiatric Publishing, Inc.; 2005:387–420.
13. Hersh EV, Pinto A, Moore PA. Adverse drug interactions involving common prescription and over-the-counter analgesic agents. Clin Ther. 2007;29(suppl):2477-2497.
14. Sola CL, Bostwick JM, Hart DA, et al. Anticipating potential linezolid-SSRI interactions in the general hospital setting: an MAOI in disguise. Mayo Clin Proc. 2006;81(3):330-334.
15. Stearns V, Johnson MD, Rae JM, et al. Active tamoxifen metabolite plasma concentrations after coadministration of tamoxifen and the selective serotonin reuptake inhibitor paroxetine. J Natl Cancer Inst. 2003;95(23):1758-1764.
1. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Hansen MS, Fink P, Frydenberg M, et al. Use of health services, mental illness, and self-rated disability and health in medical inpatients. Psychosom Med. 2002;64(4):668-675.
3. Hosaka T, Aoki T, Watanabe T, et al. Comorbidity of depression among physically ill patients and its effect on the length of hospital stay. Psychiatry Clin Neurosci. 1999;53(4):491-495.
4. McCusker J, Cole M, Ciampi A, et al. Major depression in older medical inpatients predicts poor physical and mental health status over 12 months. Gen Hosp Psychiatry. 2007;29(4):340-348.
5. McCusker J, Cole M, Dufouil C, et al. The prevalence and correlates of major and minor depression in older medical inpatients. J Am Geriatr Soc. 2005;53(8):1344-1353.
6. Berardi D, Menchetti M, Cevenini N, et al. Increased recognition of depression in primary care. Comparison between primary-care physician and ICD-10 diagnosis of depression. Psychother Psychosom. 2005;74(4):225-230.
7. Boland RJ, Diaz S, Lamdan RM, et al. Overdiagnosis of depression in the general hospital. Gen Hosp Psychiatry. 1996;18(1):28-35.
8. Clarke DM, McKenzie DP, Smith GC. The recognition of depression in patients referred to a consultation-liaison service. J Psychosom Res. 1995;39(3):327-334.
9. Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35(4):350-364.
10. Franklin JE, Levenson JL, McCance-Katz EF. Substance-related disorders. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Washington, DC: American Psychiatric Publishing, Inc.; 2005:387–420.
11. Smith GC, Clarke DM, Handrinos D, et al. Consultation-liaison psychiatrists’ use of antidepressants in the physically ill. Psychosomatics. 2002;43(3):221-227.
12. Robinson MJ, Owen JA. Psychopharmacology. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Washington, DC: American Psychiatric Publishing, Inc.; 2005:387–420.
13. Hersh EV, Pinto A, Moore PA. Adverse drug interactions involving common prescription and over-the-counter analgesic agents. Clin Ther. 2007;29(suppl):2477-2497.
14. Sola CL, Bostwick JM, Hart DA, et al. Anticipating potential linezolid-SSRI interactions in the general hospital setting: an MAOI in disguise. Mayo Clin Proc. 2006;81(3):330-334.
15. Stearns V, Johnson MD, Rae JM, et al. Active tamoxifen metabolite plasma concentrations after coadministration of tamoxifen and the selective serotonin reuptake inhibitor paroxetine. J Natl Cancer Inst. 2003;95(23):1758-1764.
Recurrent non–small-cell lung cancer in elderly patients: a case-based review of current clinical practice
Management of recurrent non-small cell lung cancer (NSCLC) is a clinical challenge. Around one third of patients who are diagnosed with NSCLC will experience a localregional or advanced stage recurrence. The median time to recurrence from initial diagnosis is 11.5 months. The median age of initial diagnosis of NSCLC is 71 years of age, patients with recurrent disease tend therefore to be even older. Treatment is a challenge, as this elderly patient population tends to have multiple comorbidities, polypharmacy and socioeconomic factors, that have not been accounted for in clinical trials in patients that define our current treatment recommendations. This case-based review outlines some of these challenges and outlines the need for further research.
*For a PDF of the full article, click in the link to the left of this introduction.
Management of recurrent non-small cell lung cancer (NSCLC) is a clinical challenge. Around one third of patients who are diagnosed with NSCLC will experience a localregional or advanced stage recurrence. The median time to recurrence from initial diagnosis is 11.5 months. The median age of initial diagnosis of NSCLC is 71 years of age, patients with recurrent disease tend therefore to be even older. Treatment is a challenge, as this elderly patient population tends to have multiple comorbidities, polypharmacy and socioeconomic factors, that have not been accounted for in clinical trials in patients that define our current treatment recommendations. This case-based review outlines some of these challenges and outlines the need for further research.
*For a PDF of the full article, click in the link to the left of this introduction.
Management of recurrent non-small cell lung cancer (NSCLC) is a clinical challenge. Around one third of patients who are diagnosed with NSCLC will experience a localregional or advanced stage recurrence. The median time to recurrence from initial diagnosis is 11.5 months. The median age of initial diagnosis of NSCLC is 71 years of age, patients with recurrent disease tend therefore to be even older. Treatment is a challenge, as this elderly patient population tends to have multiple comorbidities, polypharmacy and socioeconomic factors, that have not been accounted for in clinical trials in patients that define our current treatment recommendations. This case-based review outlines some of these challenges and outlines the need for further research.
*For a PDF of the full article, click in the link to the left of this introduction.
Transformation of Acute Cancer Pain to Chronic Cancer Pain Syndromes
Early detection and advances in cancer treatments have resulted in improved control over progression of malignancies, turning cancer into a chronic disease for many long-term cancer survivors. Approximately 12 million people with a previous diagnosis of cancer are living in the United States, and more than two-thirds of individuals diagnosed with cancer are expected to live at least 5 years after diagnosis. The National Coalition for Cancer Survivorship notes that from “the moment of diagnosis and for the balance of life, an individual diagnosed with cancer is a survivor.” Cancer survivorship may also be described as constituting three distinct phases of treatment: the acute phase (from diagnosis until completion of the initial treatment), the extended phase (the period of partial or complete remission after the initial treatment), and the permanent survival phase (a period of low likelihood of primary disease returning). Despite the advances in cancer therapies, survivors face a number of challenges, including an increased risk of recurrent cancer and other medical treatment-related toxicities. Mariotto et al estimated that as of January 1, 2005, there were more than 300,000 survivors of childhood cancer in the United States. Of these survivors, approximately one-quarter have lived for more than 30 years; however, only a small fraction of survivors (3%) exceeded 60 years of age. The most common cancer diagnoses among the survivors were brain cancer, acute lymphoblastic leukemia, germ cell tumors, and Hodgkin’s lymphoma. Another report showed that 75% of childhood cancer survivors experienced at least one adverse event.
*For a PDF of the full article and accompanying viewpoints by Tom Strouse and Howard Rosner along with Laura Audell, click in the links to the left of this introduction.
Early detection and advances in cancer treatments have resulted in improved control over progression of malignancies, turning cancer into a chronic disease for many long-term cancer survivors. Approximately 12 million people with a previous diagnosis of cancer are living in the United States, and more than two-thirds of individuals diagnosed with cancer are expected to live at least 5 years after diagnosis. The National Coalition for Cancer Survivorship notes that from “the moment of diagnosis and for the balance of life, an individual diagnosed with cancer is a survivor.” Cancer survivorship may also be described as constituting three distinct phases of treatment: the acute phase (from diagnosis until completion of the initial treatment), the extended phase (the period of partial or complete remission after the initial treatment), and the permanent survival phase (a period of low likelihood of primary disease returning). Despite the advances in cancer therapies, survivors face a number of challenges, including an increased risk of recurrent cancer and other medical treatment-related toxicities. Mariotto et al estimated that as of January 1, 2005, there were more than 300,000 survivors of childhood cancer in the United States. Of these survivors, approximately one-quarter have lived for more than 30 years; however, only a small fraction of survivors (3%) exceeded 60 years of age. The most common cancer diagnoses among the survivors were brain cancer, acute lymphoblastic leukemia, germ cell tumors, and Hodgkin’s lymphoma. Another report showed that 75% of childhood cancer survivors experienced at least one adverse event.
*For a PDF of the full article and accompanying viewpoints by Tom Strouse and Howard Rosner along with Laura Audell, click in the links to the left of this introduction.
Early detection and advances in cancer treatments have resulted in improved control over progression of malignancies, turning cancer into a chronic disease for many long-term cancer survivors. Approximately 12 million people with a previous diagnosis of cancer are living in the United States, and more than two-thirds of individuals diagnosed with cancer are expected to live at least 5 years after diagnosis. The National Coalition for Cancer Survivorship notes that from “the moment of diagnosis and for the balance of life, an individual diagnosed with cancer is a survivor.” Cancer survivorship may also be described as constituting three distinct phases of treatment: the acute phase (from diagnosis until completion of the initial treatment), the extended phase (the period of partial or complete remission after the initial treatment), and the permanent survival phase (a period of low likelihood of primary disease returning). Despite the advances in cancer therapies, survivors face a number of challenges, including an increased risk of recurrent cancer and other medical treatment-related toxicities. Mariotto et al estimated that as of January 1, 2005, there were more than 300,000 survivors of childhood cancer in the United States. Of these survivors, approximately one-quarter have lived for more than 30 years; however, only a small fraction of survivors (3%) exceeded 60 years of age. The most common cancer diagnoses among the survivors were brain cancer, acute lymphoblastic leukemia, germ cell tumors, and Hodgkin’s lymphoma. Another report showed that 75% of childhood cancer survivors experienced at least one adverse event.
*For a PDF of the full article and accompanying viewpoints by Tom Strouse and Howard Rosner along with Laura Audell, click in the links to the left of this introduction.
Chronic Lymphocytic Leukemia
Series Editor: Eric D. Jacobsen, MD
Chronic lymphocytic leukemia (CLL) is the most common hematologic malignancy in the Western world, representing 30% of leukemias. The median age at diagnosis is 72 years, and fewer than 10% of patients are under 60. CLL occurs more frequently in Caucasians than in other ethnic groups and more often in men than in women. The age-adjusted incidence rate is 4.2 per 100,000 population. Although CLL is generally considered indolent, it is a heterogeneous disease, and while many patients have slowly progressive disease, a proportion of patients have disease that will have a more aggressive course, requiring treatment soon after diagnosis. Over the past 3 decades, increasing knowledge about the mechanism of CLL and the introduction of new chemotherapeutic and biologic agents has led to better treatments, improved risk stratification, and more durable remissions. Despite these advances in treatment, CLL remains incurable outside the setting of hematopoietic stem cell transplant.
To read the full article in PDF:
Series Editor: Eric D. Jacobsen, MD
Chronic lymphocytic leukemia (CLL) is the most common hematologic malignancy in the Western world, representing 30% of leukemias. The median age at diagnosis is 72 years, and fewer than 10% of patients are under 60. CLL occurs more frequently in Caucasians than in other ethnic groups and more often in men than in women. The age-adjusted incidence rate is 4.2 per 100,000 population. Although CLL is generally considered indolent, it is a heterogeneous disease, and while many patients have slowly progressive disease, a proportion of patients have disease that will have a more aggressive course, requiring treatment soon after diagnosis. Over the past 3 decades, increasing knowledge about the mechanism of CLL and the introduction of new chemotherapeutic and biologic agents has led to better treatments, improved risk stratification, and more durable remissions. Despite these advances in treatment, CLL remains incurable outside the setting of hematopoietic stem cell transplant.
To read the full article in PDF:
Series Editor: Eric D. Jacobsen, MD
Chronic lymphocytic leukemia (CLL) is the most common hematologic malignancy in the Western world, representing 30% of leukemias. The median age at diagnosis is 72 years, and fewer than 10% of patients are under 60. CLL occurs more frequently in Caucasians than in other ethnic groups and more often in men than in women. The age-adjusted incidence rate is 4.2 per 100,000 population. Although CLL is generally considered indolent, it is a heterogeneous disease, and while many patients have slowly progressive disease, a proportion of patients have disease that will have a more aggressive course, requiring treatment soon after diagnosis. Over the past 3 decades, increasing knowledge about the mechanism of CLL and the introduction of new chemotherapeutic and biologic agents has led to better treatments, improved risk stratification, and more durable remissions. Despite these advances in treatment, CLL remains incurable outside the setting of hematopoietic stem cell transplant.
To read the full article in PDF:
A geriatric patient-centered medical home: How to obtain NCQA certification
The concept of the patient-centered medical home began as a solution for children with multiple chronic conditions.1 It has since been touted as a solution for all patients with chronic diseases, for problems with continuity of care, for restructuring primary care flow, for quality and safety, and for reining in cost.2–4 The key to the medical home concept is that the primary care provider helps to coordinate a patient’s care across a variety of settings and specialists and that patients are active participants in their own care. The National Committee for Quality Assurance (NCQA) is a nonprofit organization that certifies a practice as a medical home.
Regardless of whether one accepts all of these potential wide-ranging benefits, the process of becoming a patient-centered medical home can help to transform your practice and provide benefits to patients and staff alike.4,5
This review outlines the background of the patient-centered medical home and details some of the building blocks needed to get started on the NCQA certification process. It also describes the process of choosing the three required and clinically important conditions geared to an older patient population. We then describe the “must-pass” standards in detail, highlight specific geriatric issues, and outline the final submission process.
WHY EXTEND THE MEDICAL HOME CONCEPT TO GERIATRICS?
Although this concept began in pediatrics, it is also well suited for geriatrics. Its features include many that have long been the mainstay of geriatric care: whole-person orientation; partnerships between providers, patients, and families; coordinated and integrated care; enhanced access; a focus on quality; and a focus on management of chronic diseases.2
Traditionally, the management of chronic disease has focused on diseases such as diabetes and congestive heart failure. These diseases have evidence-based interventions, available metrics, and known benefits for both cost and patient outcomes.
However, many of these measures of quality were derived from studies of middle-aged patients with few comorbidities, and they do not necessarily apply to the geriatric population. Moreover, these studies generally do not address functional status, the time frame for expected benefit vs projected life expectancy, the risk-benefit ratio related to managing these conditions, or the patient’s own values and goals.
Therefore, “quality-care” interventions that work well for younger adults may actually harm frail elderly patients.6 An important aspect of building a geriatric medical home is making sure that the changes you implement in care and quality improvement will actually benefit your patients.
WHY WORK TOWARD CERTIFICATION?
In reviewing all the steps involved and the tremendous work required for a successful geriatric medical home, it is worth asking the question: Why work toward NCQA patient-centered medical home certification?
In the end, the goal of undertaking this project is to provide patient care in a way that is comprehensive and efficient. This is the same goal we have always strived for in geriatrics, but now we have an opportunity to measure it and to receive recognition for our work.
In the process of preparing for this application, the practice will have the opportunity to reexamine many of its processes of care, to discover deficits, and to address them. This is something that should be done continuously on some level in any good office practice on a regular basis; the patient-centered medical home application just intensifies the process.
Taking into account the needs of your practice’s geriatric population is a critical component of how one structures the patient-centered medical home. The need to take into account the frail elderly population with limited life expectancy and the lack of evidenced-based data in some areas changes how we manage many chronic illnesses. Geriatrics should take the lead in creating appropriate quality measures for this patient population. Incorporating these concepts into the medical home model is the right way to create a geriatric medical home and helps to lend validity to this concept to insurers and national organizations.
GETTING STARTED
Before getting started, it is important to have adequate support systems in place.
Go electronic. Although the NCQA provides chart-audit tools to facilitate the examination of patient subsets, it is extremely difficult to obtain medical home certification without an electronic health record system. You need to be able to collect and analyze data on your patients, their outcomes, their satisfaction, and other variables important to the practice’s patient population. It is also critical to have personnel with good computer skills, to have administrative support, and to have adequate staffing to support the processes to be put in place.
Talk to major health insurance providers in your area to see if they are interested in supporting your practice. Insurers have a vested interest in their members’ care, and they may have resources to assist with the medical home application.
Learn more. The NCQA provides seminars, online programs (www.ncqa.org/tabid/631/default.aspx), and full-length conferences. These courses provide real examples of documentation that demonstrated compliance with the standards as well as examples of documentation that failed. Learning how to create detailed documentation for the NCQA elements is important.
A good overall resource is the free user’s guide that is available from NCQA. This publication contains step-by-step screen shots to assist in navigating the survey tool, linking documents, and submitting the final survey. Several other organizations have online resources to assist with this process, including the American College of Physicians’ Medical Home Builder (www.acponline.org/running_practice/pcmh/help.htm).7
Gather your documents. The application can be ordered at www.ncqa.org. You can also apply online, and users must purchase a license for the Web application. Final submission of an application involves the following items:
- A completed business associates agreement and the patient-centered medical home recognition program agreement
- A practice profile of all physicians
- The online application form
- The application fee, which ranges from $500 to $4,000, based on the number of physicians in the practice.
Get everyone on board. Most important at this juncture is getting “buy-in.” Studies have shown that becoming a patient-centered medical home requires transformation of the entire practice, including physicians and staff. Shared leadership and protected group reflection time are also helpful.8
In embarking on this journey, the practice should set goals and a realistic time line with an understanding that this is a long and laborious process.
The reward of this major undertaking is the opportunity to examine every aspect of how your practice delivers care and to make meaningful improvements where needed. Practices should not make the mistake of just trying to meet the standards without actually improving quality.
CHOOSE THREE IMPORTANT CONDITIONS FOR QUALITY IMPROVEMENT
One of the most important first steps is to choose three “important” clinical conditions that will be the focus of quality improvement. According to the NCQA, important conditions include unhealthy behaviors, substance abuse, and mental health issues with evidence-based clinical guidelines that affect a large number of people or that consume a disproportionate amount of health care resources.9
The health care providers in your practice should all agree that the chosen conditions are important both to themselves and to their patients and that the proposed interventions will improve the quality of care. At the same time, the conditions and measures of quality need to be relatively easy to define and measure.
The 2011 standards require that at least one of the conditions be related to an unhealthy behavior (eg, obesity, smoking), a mental health issue (eg, depression, anxiety, Alzheimer disease), or substance abuse.
How can quality of care be measured in frail elderly patients?
A special consideration in geriatrics is the frailty of our patients and their limited life expectancy. Chronic care management has not been well studied in the frail elderly, and the benefits of controlling various markers of a chronic illness—for example, diabetes—all have differing time horizons that, depending on patient prognosis, may never be realized.
For some chronic diseases, the practice may need to develop new quality measures that are appropriate for its patient population. These measures must be evidence-based, or, where evidence is lacking, expert consensus must be attained. The American Geriatrics Society has several clinical practice guidelines, including the treatment of diabetes in older persons, the prevention of falls, and the pharmacologic management of persistent pain.10
Another option is to rely on the traditional Healthcare Effectiveness Data and Information Set quality measures for your chosen chronic condition, but to target appropriate patients for the interventions. One way to do this is to incorporate a prognostic indicator such as the Vulnerable Elders Survey11 or gait speed12 into your office flow so that you can categorize patients into groups and then target interventions.
One more option is to choose a geriatric syndrome that is equally relevant to all your geriatric patients regardless of frailty. However, you must be able to measure aspects of the syndrome and have interventions that will improve specific outcomes.
SETTING PRIORITIES
At the outset, it is important to review the NCQA’s standards for a patient-centered medical home and to identify standards for which you have appropriate processes in place, standards in which you are deficient but which can be fixed, and standards that will be more difficult to address.
One way to do this is to complete the Web-based self-assessment survey, which provides a score by element. Each deficiency discovered is an opportunity to brainstorm solutions and to embark upon a rapid cycle of improvement (“plan, do, study, act”).13 Deficiencies should be tackled over time, however, to avoid overwhelming the practice. It is particularly helpful to create small work-groups, to assign tasks with definite deadlines, and to meet regularly to review progress and assign new tasks.
The NCQA released new standards in 2011. A new requirement is that the practice’s electronic health record system must incorporate Meaningful Use Criteria of the Centers for Medicare and Medicaid Services (CMS). These criteria show that the practice is using the electronic health record effectively. As a result, attaining medical home certification will ensure that the practice also meets CMS Meaningful Use Criteria.
Six standards for a patient-centered medical home
The NCQA has six standards for a patient-centered medical home, which align with the core components of primary care14:
- Standard 1: Enhance access and continuity
- Standard 2: Identify and manage patient populations
- Standard 3: Plan and manage care
- Standard 4: Provide self-care support and community resources
- Standard 5: Track and coordinate care
- Standard 6: Measure and improve performance.
Each of these standards is broken down into elements, designated A, B, C, and so on—27 in all. Each element is scored on the basis of the number of “factors” the practice meets in each element. For example, element E in standard 1 has four factors, and the practice will receive 100% of the two possible points if all four factors are met, 50% of all points if the practice meets two factors, and no points if the practice meets none of the factors.
NCQA now designates a “critical factor” for some elements. These are factors thought to be “central to the concept being assessed within particular elements,”9 and they must be met to score any points for the element. In the same element as above, for example, having regular team meetings or a structured communication process is designated as a critical factor. A practice must meet this factor in order to achieve any of the four points assigned to the element.
SIX ‘MUST-PASS’ ELEMENTS
Of the 27 elements, six are considered essential, and the practice must get a score of at least 50% in all six of these to pass. Since they are the most critical elements, it is often useful to focus on them first to ensure that your practice puts into place policies and other building blocks necessary to make these important elements happen.
Policies must be in place for at least 3 months before submission. Most practices will discover many unwritten workflows as they review these processes.
What follows is a summary of the must-pass elements and their requirements. This is meant to be used only as an overview to better understand the scope of the medical home requirements; the actual requirements should be obtained from the NCQA Web site.
Standard 1, element A: Provide timely access during office hours
This element requires that your office have a policy or process in place for patient access. Same-day appointment availability is deemed a critical factor and must be met to receive any score on the whole element.
The practice needs to measure availability for several different appointment types—new, urgent, and routine—and show that same-day access is available. This can be done by completing at least a 5-day audit measuring the length of time from when a patient contacts the practice to request an appointment to the third next available appointment on his or her clinician’s schedule. It is not enough to simply double-book patients in an already full schedule.
The remaining aspects of this element require being able to provide timely clinical advice by telephone or by secure electronic messages, or both, during office hours, and to document it. The practice must have policies in place that define “timely.” It also must audit phone calls to prove adherence to that policy. The audit should cover at least 5 days. The practice then needs to show at least three examples of clinical advice documented in patients’ charts. We recommend not monitoring all the components during the same week, since the monitoring is laborious and would be overwhelming if attempted all at once.
Standard 2, element D: Use data for population management
This element requires that your practice be able to generate lists of patients and send out reminders of needed services; both are also CMS Meaningful Use Criteria.
Specifically, the NCQA requires that you be able to generate lists of patients’ preventive care and chronic care services and be able to reach out to patients who have deficiencies. The practice must target at least three preventive care services and at least three chronic care services.
One can (and should) link this element to the three important conditions that have been chosen for the practice. For example, if osteoporosis is one of the important conditions, it also can be one of the three preventive care services; a possible quality improvement intervention could be to send reminders to patients to have bone density screening if they have not done so within a certain time frame.
In addition, the practice should have the ability to generate a list of patients who have not been seen at an appropriate interval, as well as a list of patients who are taking certain medications that require regular monitoring. To complete the audit, the practice must produce the four lists just described. Each must then be examined for the previous 12-month period, and documentation must be provided to show how patients with deficiencies were contacted.
Local insurance health plans may be able to help with this element, as these types of lists are often standard practice. Submitting the health plans’ lists is acceptable as long as you can show that they account for at least 75% of the practice.
Standard 3, element C: Manage care for your three conditions
This element focuses on the three clinically important chronic conditions you have chosen. It demonstrates that your practice is following these patients’ outcomes and targeting patients who require more attention to improve their outcomes. Doing so requires documenting pre-visit planning and individualized care plans and treatment goals.
The patient or the family, or both, should be given a written plan of care and a clinical summary at each visit. Barriers to progress need to be assessed, and patients should be contacted if they do not come to scheduled appointments. Patients who have significant barriers should be assessed for additional care management support. This is particularly important for a geriatric population, which may have significant psychosocial barriers such as financial problems, transportation issues, cognitive decline, and overall lack of support.
For each factor in this element, the office must create policies and protocols and assign tasks to appropriate members of the care team. For example, a nurse can make phone calls to targeted patients before their appointments to review goals of care using a standardized form. The form can be given to the physician at the time of the appointment for review and incorporation into the medical record.
Documentation for this element requires that the practice evaluate the number of patients with each chronic condition (the denominator) and the number of patients in each group for whom the above standards have been completed (the numerator) over the previous 3 months. At least 75% compliance is required for each of the three conditions to achieve a passing score for this factor.
This element is very time-consuming, even with an electronic health record. The practice team members should work together to create the systems and tools, but, if possible, it is worth trying to acquire help from an intern or a student. Working on the medical home can be a wonderful educational experience.
Standard 4, element A: Support self-care
For this element, one must show that the practice has educational and self-monitoring tools that are given to all patients depending upon their needs. Involving the patient or family or caregiver in managing the patient’s health is an integral part of the patient-centered medical home.
This is particularly challenging in geriatrics, as many patients may be cognitively unable to participate, and it will be necessary to develop self-management tools that are meaningful for caregivers. When choosing the three clinically important conditions, one needs to keep this element in mind, as the practice must be able to create good educational and self-management tools that are relevant to the important conditions and applicable to the geriatric patient population.
To meet the specific requirements for this element, the practice must show that at least 50% of patients or families receive educational resources and have documented self-management plans, tools, and counseling, and an assessment of their self-management abilities. In addition, one can show that the electronic health record is used to identify patient-specific educational resources in at least 10% of patients. This last factor is also one of the CMS Meaningful Use Criteria.
To document that the practice is completing all the requirements for this element, one must look back 12 months (or at least 3 months if earlier data are unavailable) and use the list of patients with the three clinically important conditions. In addition, the practice needs to identify its high-risk or complex patients over the same time period. These two lists comprise the denominator. The numerator is the number of patients for which you can show documentation of each of the above items.
Because this audit is also time-consuming, it and standard 3, element C (care management) should be combined and performed simultaneously.
Standard 5, element B: Track referrals and follow-up
This is often the most difficult must-pass element to fulfill because it requires coordination with health care providers outside one’s practice. To complete this element, the office must have a system in place to track referrals originating within the practice and to ensure that all relevant information is both sent to and received back from the consultant. This tracking must include the reason for and the urgency of the referral, as well as relevant clinical information. One can also establish comanagement when needed for patients who are seen regularly by a specific specialist.
Making sure that the consultant’s report gets back to the practice is, for most sites, the most difficult part. It is often not feasible to do this entirely through the electronic health record, as it is unlikely that all your consultants have the same electronic health record as your practice. Therefore, this often requires at least a partially paper-based system, creating a file that must be checked on a regular basis to ensure that the appointment with the consultant has been completed and that he or she has sent a note back. If the information is not all there, there must be documentation of a phone call that tried to obtain the necessary information or to document the patient’s refusal to follow up.
Two factors in this element also meet CMS Meaningful Use Criteria: demonstrating the capability for electronic exchange of key clinical information between clinicians, and providing an electronic summary of the care record for more than 50% of referrals. To complete the documentation for this element, the practice must do an audit that reviews at least a week’s worth of referrals.
Standard 6, element C: Implement continuous quality improvement
This element requires demonstration of continuous quality improvement activities in specific domains that are outlined in standard 6, elements A and B. Element A includes preventive care measures, chronic or acute care clinical measures, and measures that affect health care costs or help to assess disparities in vulnerable patients’ care. Element B includes surveying access, communication, coordination, and self-management support or obtaining feedback from vulnerable patient groups or patients and their families.
Once again, there is the potential for considerable overlap in the work that your practice does with the clinically important conditions, and with standard 1 (access), standard 2 (population reminders for preventive services), standard 3 (care management), and standard 4 (self-management). This overlap provides the opportunity to go into more depth and to show significant quality outcomes for some of the chosen measures.
This element requires the practice to set goals and to act to improve at least three measures from element A and at least one measure from element B. Points are also awarded for addressing at least one disparity in care or service for vulnerable populations. In geriatrics, some examples of vulnerable populations include the very frail, patients and families with significant psychosocial issues, those at the end of life, or patients with significant financial burdens (especially related to health care costs). Finally, points are awarded for involving patients or families in quality improvement teams.
To document adherence to this element, the practice must demonstrate quality improvement reports for all the selected measures as well as actions taken in response to the data. The goal is to meet the desired level of achievement that is established by your practice. If patients or families are asked to join quality improvement teams, the practice must describe the process employed for inclusion and details of the frequency of meetings and agendas.
OTHER ELEMENTS
Besides the must-pass elements, there are 21 additional elements, each with its own specific requirements and documentation. Some of these overlap with the concepts in the must-pass elements, so it is important to create processes that work for all the factors in all the related elements.
It is also important to understand that one does not need to master all the other elements— the practice can choose ones that are most meaningful for its patient population. One can also elect to skip ones that require particularly labor-intensive audits and that do not add much to the quality of geriatric patient care. The team should focus on making changes that help patient care and flow. All recognition levels require a minimum 50% score for the six must-pass elements, and the final recognition level is based on the following three criteria:
- Level 1: 35–59 points and all six must-pass elements
- Level 2: 60–84 points and all six must-pass elements
- Level 3: 85–100 points and all six must-pass elements.
FINAL SUBMISSION
Final submission involves completion of the application materials mentioned above, payment of the application fee, and attachment of files that have been linked to elements from the document library.
The process of uploading files for submission can be complex when multiple staff members are working on the documents. Files must be uploaded from shared drives, which should be set up when one begins the process of gathering documents. As a last step, the document library must be uploaded to the NCQA server. It is best to do this in batches of files. The time needed to upload depends on the speed of the Internet service. The survey form will indicate if each file has been successfully uploaded to the NCQA server.
The submitted survey tool is assigned a project number that can be used as a reference for inquiries to the NCQA. It is best to keep a copy of the final submission information for future use. Before submitting, it is a good idea to ask someone not involved in your practice to review the documents for clarity and consistency. Remember, the survey tool is a “read-only” document after submission, so no changes can be made to it after final submission.
- Sia C, Tonniges TF, Osterhus E, Taba S. Pediatrics. History of the medical home concept. Pediatrics 2004; 113( suppl 5):1473–1478.
- Robert Graham Center: Center for Policy Standards in Family Medicine and Primary Care. The patient centered medical home: history, seven core features, evidence and transformational change. November 2007. http://www.graham-center.org/online/graham/home/publications/monographs-books/2007/rgcmo-medical-home.html. Accessed April 4, 2012.
- Lee JG, Dayal G, Fontaine D. Starting a medical home: better health at lower cost. Healthcare Financial Management Association. June 2011. http://www.hfma.org/Templates/InteriorMaster.aspx?id=27048. Accessed April 4, 2012.
- Grumbach K, Grundy P. Outcomes of implementing patient centered medical home interventions: a review of the evidence from prospective evaluation studies in the United States. Patient-Centered Primary Care Collaborative. November 2010. http://www.pcpcc.net/content/patient-centered-medical-home. Accessed April 4, 2012.
- Reid RJ, Coleman K, Johnson EA, et al. The group health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood) 2010; 29:835–843.
- Huang ES, Zhang Q, Gandra N, Chin MH, Meltzer DO. The effect of comorbid illness and functional status on the expected benefits of intensive glucose control in older patients with type 2 diabetes: a decision analysis. Ann Intern Med 2008; 149:11–19.
- American College of Physicians. Medical home builder. http://www.Medicalhomebuilder.org. Accessed April 4, 2012.
- Nutting PA, Miller WL, Crabtree BF, Jaen CR, Stewart EE, Stange KC. Initial lessons from the first national demonstration project on practice transformation to a patient-centered medical home. Ann Fam Med 2009; 7:254–260.
- National Committee for Quality Assurance (NCQA). Standards and guidelines for NCQA’s patient-centered medical home (PCMH). March 2011. www.chcact.org/images/customer-files//Appendix3_PCMH2011glossary.pdf. Accessed April 4, 2012.
- American Geriatrics Society. http://www.americangeriatrics.org/health_care_professionals/clinical_practice/clinical_guidelines_recommendations/. Accessed April 4, 2012.
- Min LC, Elliott MN, Wenger NS, Saliba D. Higher vulnerable elders survey scores predict death and functional decline in vulnerable older people. J Am Geriatr Soc 2006; 54:507–511.
- Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA 2011; 305:50–58.
- Plan, do, check, act. In:Karlof B, Lovingsson F, editors. A to Z of Management Concepts & Models. London: Thorogood Publishing; 2005.
- National Committee for Quality Assurance (NCQA). NCQA 2011 Requirements. www.ncqa.org/tabid/1405/Default.aspx. Accessed April 4, 2012.
The concept of the patient-centered medical home began as a solution for children with multiple chronic conditions.1 It has since been touted as a solution for all patients with chronic diseases, for problems with continuity of care, for restructuring primary care flow, for quality and safety, and for reining in cost.2–4 The key to the medical home concept is that the primary care provider helps to coordinate a patient’s care across a variety of settings and specialists and that patients are active participants in their own care. The National Committee for Quality Assurance (NCQA) is a nonprofit organization that certifies a practice as a medical home.
Regardless of whether one accepts all of these potential wide-ranging benefits, the process of becoming a patient-centered medical home can help to transform your practice and provide benefits to patients and staff alike.4,5
This review outlines the background of the patient-centered medical home and details some of the building blocks needed to get started on the NCQA certification process. It also describes the process of choosing the three required and clinically important conditions geared to an older patient population. We then describe the “must-pass” standards in detail, highlight specific geriatric issues, and outline the final submission process.
WHY EXTEND THE MEDICAL HOME CONCEPT TO GERIATRICS?
Although this concept began in pediatrics, it is also well suited for geriatrics. Its features include many that have long been the mainstay of geriatric care: whole-person orientation; partnerships between providers, patients, and families; coordinated and integrated care; enhanced access; a focus on quality; and a focus on management of chronic diseases.2
Traditionally, the management of chronic disease has focused on diseases such as diabetes and congestive heart failure. These diseases have evidence-based interventions, available metrics, and known benefits for both cost and patient outcomes.
However, many of these measures of quality were derived from studies of middle-aged patients with few comorbidities, and they do not necessarily apply to the geriatric population. Moreover, these studies generally do not address functional status, the time frame for expected benefit vs projected life expectancy, the risk-benefit ratio related to managing these conditions, or the patient’s own values and goals.
Therefore, “quality-care” interventions that work well for younger adults may actually harm frail elderly patients.6 An important aspect of building a geriatric medical home is making sure that the changes you implement in care and quality improvement will actually benefit your patients.
WHY WORK TOWARD CERTIFICATION?
In reviewing all the steps involved and the tremendous work required for a successful geriatric medical home, it is worth asking the question: Why work toward NCQA patient-centered medical home certification?
In the end, the goal of undertaking this project is to provide patient care in a way that is comprehensive and efficient. This is the same goal we have always strived for in geriatrics, but now we have an opportunity to measure it and to receive recognition for our work.
In the process of preparing for this application, the practice will have the opportunity to reexamine many of its processes of care, to discover deficits, and to address them. This is something that should be done continuously on some level in any good office practice on a regular basis; the patient-centered medical home application just intensifies the process.
Taking into account the needs of your practice’s geriatric population is a critical component of how one structures the patient-centered medical home. The need to take into account the frail elderly population with limited life expectancy and the lack of evidenced-based data in some areas changes how we manage many chronic illnesses. Geriatrics should take the lead in creating appropriate quality measures for this patient population. Incorporating these concepts into the medical home model is the right way to create a geriatric medical home and helps to lend validity to this concept to insurers and national organizations.
GETTING STARTED
Before getting started, it is important to have adequate support systems in place.
Go electronic. Although the NCQA provides chart-audit tools to facilitate the examination of patient subsets, it is extremely difficult to obtain medical home certification without an electronic health record system. You need to be able to collect and analyze data on your patients, their outcomes, their satisfaction, and other variables important to the practice’s patient population. It is also critical to have personnel with good computer skills, to have administrative support, and to have adequate staffing to support the processes to be put in place.
Talk to major health insurance providers in your area to see if they are interested in supporting your practice. Insurers have a vested interest in their members’ care, and they may have resources to assist with the medical home application.
Learn more. The NCQA provides seminars, online programs (www.ncqa.org/tabid/631/default.aspx), and full-length conferences. These courses provide real examples of documentation that demonstrated compliance with the standards as well as examples of documentation that failed. Learning how to create detailed documentation for the NCQA elements is important.
A good overall resource is the free user’s guide that is available from NCQA. This publication contains step-by-step screen shots to assist in navigating the survey tool, linking documents, and submitting the final survey. Several other organizations have online resources to assist with this process, including the American College of Physicians’ Medical Home Builder (www.acponline.org/running_practice/pcmh/help.htm).7
Gather your documents. The application can be ordered at www.ncqa.org. You can also apply online, and users must purchase a license for the Web application. Final submission of an application involves the following items:
- A completed business associates agreement and the patient-centered medical home recognition program agreement
- A practice profile of all physicians
- The online application form
- The application fee, which ranges from $500 to $4,000, based on the number of physicians in the practice.
Get everyone on board. Most important at this juncture is getting “buy-in.” Studies have shown that becoming a patient-centered medical home requires transformation of the entire practice, including physicians and staff. Shared leadership and protected group reflection time are also helpful.8
In embarking on this journey, the practice should set goals and a realistic time line with an understanding that this is a long and laborious process.
The reward of this major undertaking is the opportunity to examine every aspect of how your practice delivers care and to make meaningful improvements where needed. Practices should not make the mistake of just trying to meet the standards without actually improving quality.
CHOOSE THREE IMPORTANT CONDITIONS FOR QUALITY IMPROVEMENT
One of the most important first steps is to choose three “important” clinical conditions that will be the focus of quality improvement. According to the NCQA, important conditions include unhealthy behaviors, substance abuse, and mental health issues with evidence-based clinical guidelines that affect a large number of people or that consume a disproportionate amount of health care resources.9
The health care providers in your practice should all agree that the chosen conditions are important both to themselves and to their patients and that the proposed interventions will improve the quality of care. At the same time, the conditions and measures of quality need to be relatively easy to define and measure.
The 2011 standards require that at least one of the conditions be related to an unhealthy behavior (eg, obesity, smoking), a mental health issue (eg, depression, anxiety, Alzheimer disease), or substance abuse.
How can quality of care be measured in frail elderly patients?
A special consideration in geriatrics is the frailty of our patients and their limited life expectancy. Chronic care management has not been well studied in the frail elderly, and the benefits of controlling various markers of a chronic illness—for example, diabetes—all have differing time horizons that, depending on patient prognosis, may never be realized.
For some chronic diseases, the practice may need to develop new quality measures that are appropriate for its patient population. These measures must be evidence-based, or, where evidence is lacking, expert consensus must be attained. The American Geriatrics Society has several clinical practice guidelines, including the treatment of diabetes in older persons, the prevention of falls, and the pharmacologic management of persistent pain.10
Another option is to rely on the traditional Healthcare Effectiveness Data and Information Set quality measures for your chosen chronic condition, but to target appropriate patients for the interventions. One way to do this is to incorporate a prognostic indicator such as the Vulnerable Elders Survey11 or gait speed12 into your office flow so that you can categorize patients into groups and then target interventions.
One more option is to choose a geriatric syndrome that is equally relevant to all your geriatric patients regardless of frailty. However, you must be able to measure aspects of the syndrome and have interventions that will improve specific outcomes.
SETTING PRIORITIES
At the outset, it is important to review the NCQA’s standards for a patient-centered medical home and to identify standards for which you have appropriate processes in place, standards in which you are deficient but which can be fixed, and standards that will be more difficult to address.
One way to do this is to complete the Web-based self-assessment survey, which provides a score by element. Each deficiency discovered is an opportunity to brainstorm solutions and to embark upon a rapid cycle of improvement (“plan, do, study, act”).13 Deficiencies should be tackled over time, however, to avoid overwhelming the practice. It is particularly helpful to create small work-groups, to assign tasks with definite deadlines, and to meet regularly to review progress and assign new tasks.
The NCQA released new standards in 2011. A new requirement is that the practice’s electronic health record system must incorporate Meaningful Use Criteria of the Centers for Medicare and Medicaid Services (CMS). These criteria show that the practice is using the electronic health record effectively. As a result, attaining medical home certification will ensure that the practice also meets CMS Meaningful Use Criteria.
Six standards for a patient-centered medical home
The NCQA has six standards for a patient-centered medical home, which align with the core components of primary care14:
- Standard 1: Enhance access and continuity
- Standard 2: Identify and manage patient populations
- Standard 3: Plan and manage care
- Standard 4: Provide self-care support and community resources
- Standard 5: Track and coordinate care
- Standard 6: Measure and improve performance.
Each of these standards is broken down into elements, designated A, B, C, and so on—27 in all. Each element is scored on the basis of the number of “factors” the practice meets in each element. For example, element E in standard 1 has four factors, and the practice will receive 100% of the two possible points if all four factors are met, 50% of all points if the practice meets two factors, and no points if the practice meets none of the factors.
NCQA now designates a “critical factor” for some elements. These are factors thought to be “central to the concept being assessed within particular elements,”9 and they must be met to score any points for the element. In the same element as above, for example, having regular team meetings or a structured communication process is designated as a critical factor. A practice must meet this factor in order to achieve any of the four points assigned to the element.
SIX ‘MUST-PASS’ ELEMENTS
Of the 27 elements, six are considered essential, and the practice must get a score of at least 50% in all six of these to pass. Since they are the most critical elements, it is often useful to focus on them first to ensure that your practice puts into place policies and other building blocks necessary to make these important elements happen.
Policies must be in place for at least 3 months before submission. Most practices will discover many unwritten workflows as they review these processes.
What follows is a summary of the must-pass elements and their requirements. This is meant to be used only as an overview to better understand the scope of the medical home requirements; the actual requirements should be obtained from the NCQA Web site.
Standard 1, element A: Provide timely access during office hours
This element requires that your office have a policy or process in place for patient access. Same-day appointment availability is deemed a critical factor and must be met to receive any score on the whole element.
The practice needs to measure availability for several different appointment types—new, urgent, and routine—and show that same-day access is available. This can be done by completing at least a 5-day audit measuring the length of time from when a patient contacts the practice to request an appointment to the third next available appointment on his or her clinician’s schedule. It is not enough to simply double-book patients in an already full schedule.
The remaining aspects of this element require being able to provide timely clinical advice by telephone or by secure electronic messages, or both, during office hours, and to document it. The practice must have policies in place that define “timely.” It also must audit phone calls to prove adherence to that policy. The audit should cover at least 5 days. The practice then needs to show at least three examples of clinical advice documented in patients’ charts. We recommend not monitoring all the components during the same week, since the monitoring is laborious and would be overwhelming if attempted all at once.
Standard 2, element D: Use data for population management
This element requires that your practice be able to generate lists of patients and send out reminders of needed services; both are also CMS Meaningful Use Criteria.
Specifically, the NCQA requires that you be able to generate lists of patients’ preventive care and chronic care services and be able to reach out to patients who have deficiencies. The practice must target at least three preventive care services and at least three chronic care services.
One can (and should) link this element to the three important conditions that have been chosen for the practice. For example, if osteoporosis is one of the important conditions, it also can be one of the three preventive care services; a possible quality improvement intervention could be to send reminders to patients to have bone density screening if they have not done so within a certain time frame.
In addition, the practice should have the ability to generate a list of patients who have not been seen at an appropriate interval, as well as a list of patients who are taking certain medications that require regular monitoring. To complete the audit, the practice must produce the four lists just described. Each must then be examined for the previous 12-month period, and documentation must be provided to show how patients with deficiencies were contacted.
Local insurance health plans may be able to help with this element, as these types of lists are often standard practice. Submitting the health plans’ lists is acceptable as long as you can show that they account for at least 75% of the practice.
Standard 3, element C: Manage care for your three conditions
This element focuses on the three clinically important chronic conditions you have chosen. It demonstrates that your practice is following these patients’ outcomes and targeting patients who require more attention to improve their outcomes. Doing so requires documenting pre-visit planning and individualized care plans and treatment goals.
The patient or the family, or both, should be given a written plan of care and a clinical summary at each visit. Barriers to progress need to be assessed, and patients should be contacted if they do not come to scheduled appointments. Patients who have significant barriers should be assessed for additional care management support. This is particularly important for a geriatric population, which may have significant psychosocial barriers such as financial problems, transportation issues, cognitive decline, and overall lack of support.
For each factor in this element, the office must create policies and protocols and assign tasks to appropriate members of the care team. For example, a nurse can make phone calls to targeted patients before their appointments to review goals of care using a standardized form. The form can be given to the physician at the time of the appointment for review and incorporation into the medical record.
Documentation for this element requires that the practice evaluate the number of patients with each chronic condition (the denominator) and the number of patients in each group for whom the above standards have been completed (the numerator) over the previous 3 months. At least 75% compliance is required for each of the three conditions to achieve a passing score for this factor.
This element is very time-consuming, even with an electronic health record. The practice team members should work together to create the systems and tools, but, if possible, it is worth trying to acquire help from an intern or a student. Working on the medical home can be a wonderful educational experience.
Standard 4, element A: Support self-care
For this element, one must show that the practice has educational and self-monitoring tools that are given to all patients depending upon their needs. Involving the patient or family or caregiver in managing the patient’s health is an integral part of the patient-centered medical home.
This is particularly challenging in geriatrics, as many patients may be cognitively unable to participate, and it will be necessary to develop self-management tools that are meaningful for caregivers. When choosing the three clinically important conditions, one needs to keep this element in mind, as the practice must be able to create good educational and self-management tools that are relevant to the important conditions and applicable to the geriatric patient population.
To meet the specific requirements for this element, the practice must show that at least 50% of patients or families receive educational resources and have documented self-management plans, tools, and counseling, and an assessment of their self-management abilities. In addition, one can show that the electronic health record is used to identify patient-specific educational resources in at least 10% of patients. This last factor is also one of the CMS Meaningful Use Criteria.
To document that the practice is completing all the requirements for this element, one must look back 12 months (or at least 3 months if earlier data are unavailable) and use the list of patients with the three clinically important conditions. In addition, the practice needs to identify its high-risk or complex patients over the same time period. These two lists comprise the denominator. The numerator is the number of patients for which you can show documentation of each of the above items.
Because this audit is also time-consuming, it and standard 3, element C (care management) should be combined and performed simultaneously.
Standard 5, element B: Track referrals and follow-up
This is often the most difficult must-pass element to fulfill because it requires coordination with health care providers outside one’s practice. To complete this element, the office must have a system in place to track referrals originating within the practice and to ensure that all relevant information is both sent to and received back from the consultant. This tracking must include the reason for and the urgency of the referral, as well as relevant clinical information. One can also establish comanagement when needed for patients who are seen regularly by a specific specialist.
Making sure that the consultant’s report gets back to the practice is, for most sites, the most difficult part. It is often not feasible to do this entirely through the electronic health record, as it is unlikely that all your consultants have the same electronic health record as your practice. Therefore, this often requires at least a partially paper-based system, creating a file that must be checked on a regular basis to ensure that the appointment with the consultant has been completed and that he or she has sent a note back. If the information is not all there, there must be documentation of a phone call that tried to obtain the necessary information or to document the patient’s refusal to follow up.
Two factors in this element also meet CMS Meaningful Use Criteria: demonstrating the capability for electronic exchange of key clinical information between clinicians, and providing an electronic summary of the care record for more than 50% of referrals. To complete the documentation for this element, the practice must do an audit that reviews at least a week’s worth of referrals.
Standard 6, element C: Implement continuous quality improvement
This element requires demonstration of continuous quality improvement activities in specific domains that are outlined in standard 6, elements A and B. Element A includes preventive care measures, chronic or acute care clinical measures, and measures that affect health care costs or help to assess disparities in vulnerable patients’ care. Element B includes surveying access, communication, coordination, and self-management support or obtaining feedback from vulnerable patient groups or patients and their families.
Once again, there is the potential for considerable overlap in the work that your practice does with the clinically important conditions, and with standard 1 (access), standard 2 (population reminders for preventive services), standard 3 (care management), and standard 4 (self-management). This overlap provides the opportunity to go into more depth and to show significant quality outcomes for some of the chosen measures.
This element requires the practice to set goals and to act to improve at least three measures from element A and at least one measure from element B. Points are also awarded for addressing at least one disparity in care or service for vulnerable populations. In geriatrics, some examples of vulnerable populations include the very frail, patients and families with significant psychosocial issues, those at the end of life, or patients with significant financial burdens (especially related to health care costs). Finally, points are awarded for involving patients or families in quality improvement teams.
To document adherence to this element, the practice must demonstrate quality improvement reports for all the selected measures as well as actions taken in response to the data. The goal is to meet the desired level of achievement that is established by your practice. If patients or families are asked to join quality improvement teams, the practice must describe the process employed for inclusion and details of the frequency of meetings and agendas.
OTHER ELEMENTS
Besides the must-pass elements, there are 21 additional elements, each with its own specific requirements and documentation. Some of these overlap with the concepts in the must-pass elements, so it is important to create processes that work for all the factors in all the related elements.
It is also important to understand that one does not need to master all the other elements— the practice can choose ones that are most meaningful for its patient population. One can also elect to skip ones that require particularly labor-intensive audits and that do not add much to the quality of geriatric patient care. The team should focus on making changes that help patient care and flow. All recognition levels require a minimum 50% score for the six must-pass elements, and the final recognition level is based on the following three criteria:
- Level 1: 35–59 points and all six must-pass elements
- Level 2: 60–84 points and all six must-pass elements
- Level 3: 85–100 points and all six must-pass elements.
FINAL SUBMISSION
Final submission involves completion of the application materials mentioned above, payment of the application fee, and attachment of files that have been linked to elements from the document library.
The process of uploading files for submission can be complex when multiple staff members are working on the documents. Files must be uploaded from shared drives, which should be set up when one begins the process of gathering documents. As a last step, the document library must be uploaded to the NCQA server. It is best to do this in batches of files. The time needed to upload depends on the speed of the Internet service. The survey form will indicate if each file has been successfully uploaded to the NCQA server.
The submitted survey tool is assigned a project number that can be used as a reference for inquiries to the NCQA. It is best to keep a copy of the final submission information for future use. Before submitting, it is a good idea to ask someone not involved in your practice to review the documents for clarity and consistency. Remember, the survey tool is a “read-only” document after submission, so no changes can be made to it after final submission.
The concept of the patient-centered medical home began as a solution for children with multiple chronic conditions.1 It has since been touted as a solution for all patients with chronic diseases, for problems with continuity of care, for restructuring primary care flow, for quality and safety, and for reining in cost.2–4 The key to the medical home concept is that the primary care provider helps to coordinate a patient’s care across a variety of settings and specialists and that patients are active participants in their own care. The National Committee for Quality Assurance (NCQA) is a nonprofit organization that certifies a practice as a medical home.
Regardless of whether one accepts all of these potential wide-ranging benefits, the process of becoming a patient-centered medical home can help to transform your practice and provide benefits to patients and staff alike.4,5
This review outlines the background of the patient-centered medical home and details some of the building blocks needed to get started on the NCQA certification process. It also describes the process of choosing the three required and clinically important conditions geared to an older patient population. We then describe the “must-pass” standards in detail, highlight specific geriatric issues, and outline the final submission process.
WHY EXTEND THE MEDICAL HOME CONCEPT TO GERIATRICS?
Although this concept began in pediatrics, it is also well suited for geriatrics. Its features include many that have long been the mainstay of geriatric care: whole-person orientation; partnerships between providers, patients, and families; coordinated and integrated care; enhanced access; a focus on quality; and a focus on management of chronic diseases.2
Traditionally, the management of chronic disease has focused on diseases such as diabetes and congestive heart failure. These diseases have evidence-based interventions, available metrics, and known benefits for both cost and patient outcomes.
However, many of these measures of quality were derived from studies of middle-aged patients with few comorbidities, and they do not necessarily apply to the geriatric population. Moreover, these studies generally do not address functional status, the time frame for expected benefit vs projected life expectancy, the risk-benefit ratio related to managing these conditions, or the patient’s own values and goals.
Therefore, “quality-care” interventions that work well for younger adults may actually harm frail elderly patients.6 An important aspect of building a geriatric medical home is making sure that the changes you implement in care and quality improvement will actually benefit your patients.
WHY WORK TOWARD CERTIFICATION?
In reviewing all the steps involved and the tremendous work required for a successful geriatric medical home, it is worth asking the question: Why work toward NCQA patient-centered medical home certification?
In the end, the goal of undertaking this project is to provide patient care in a way that is comprehensive and efficient. This is the same goal we have always strived for in geriatrics, but now we have an opportunity to measure it and to receive recognition for our work.
In the process of preparing for this application, the practice will have the opportunity to reexamine many of its processes of care, to discover deficits, and to address them. This is something that should be done continuously on some level in any good office practice on a regular basis; the patient-centered medical home application just intensifies the process.
Taking into account the needs of your practice’s geriatric population is a critical component of how one structures the patient-centered medical home. The need to take into account the frail elderly population with limited life expectancy and the lack of evidenced-based data in some areas changes how we manage many chronic illnesses. Geriatrics should take the lead in creating appropriate quality measures for this patient population. Incorporating these concepts into the medical home model is the right way to create a geriatric medical home and helps to lend validity to this concept to insurers and national organizations.
GETTING STARTED
Before getting started, it is important to have adequate support systems in place.
Go electronic. Although the NCQA provides chart-audit tools to facilitate the examination of patient subsets, it is extremely difficult to obtain medical home certification without an electronic health record system. You need to be able to collect and analyze data on your patients, their outcomes, their satisfaction, and other variables important to the practice’s patient population. It is also critical to have personnel with good computer skills, to have administrative support, and to have adequate staffing to support the processes to be put in place.
Talk to major health insurance providers in your area to see if they are interested in supporting your practice. Insurers have a vested interest in their members’ care, and they may have resources to assist with the medical home application.
Learn more. The NCQA provides seminars, online programs (www.ncqa.org/tabid/631/default.aspx), and full-length conferences. These courses provide real examples of documentation that demonstrated compliance with the standards as well as examples of documentation that failed. Learning how to create detailed documentation for the NCQA elements is important.
A good overall resource is the free user’s guide that is available from NCQA. This publication contains step-by-step screen shots to assist in navigating the survey tool, linking documents, and submitting the final survey. Several other organizations have online resources to assist with this process, including the American College of Physicians’ Medical Home Builder (www.acponline.org/running_practice/pcmh/help.htm).7
Gather your documents. The application can be ordered at www.ncqa.org. You can also apply online, and users must purchase a license for the Web application. Final submission of an application involves the following items:
- A completed business associates agreement and the patient-centered medical home recognition program agreement
- A practice profile of all physicians
- The online application form
- The application fee, which ranges from $500 to $4,000, based on the number of physicians in the practice.
Get everyone on board. Most important at this juncture is getting “buy-in.” Studies have shown that becoming a patient-centered medical home requires transformation of the entire practice, including physicians and staff. Shared leadership and protected group reflection time are also helpful.8
In embarking on this journey, the practice should set goals and a realistic time line with an understanding that this is a long and laborious process.
The reward of this major undertaking is the opportunity to examine every aspect of how your practice delivers care and to make meaningful improvements where needed. Practices should not make the mistake of just trying to meet the standards without actually improving quality.
CHOOSE THREE IMPORTANT CONDITIONS FOR QUALITY IMPROVEMENT
One of the most important first steps is to choose three “important” clinical conditions that will be the focus of quality improvement. According to the NCQA, important conditions include unhealthy behaviors, substance abuse, and mental health issues with evidence-based clinical guidelines that affect a large number of people or that consume a disproportionate amount of health care resources.9
The health care providers in your practice should all agree that the chosen conditions are important both to themselves and to their patients and that the proposed interventions will improve the quality of care. At the same time, the conditions and measures of quality need to be relatively easy to define and measure.
The 2011 standards require that at least one of the conditions be related to an unhealthy behavior (eg, obesity, smoking), a mental health issue (eg, depression, anxiety, Alzheimer disease), or substance abuse.
How can quality of care be measured in frail elderly patients?
A special consideration in geriatrics is the frailty of our patients and their limited life expectancy. Chronic care management has not been well studied in the frail elderly, and the benefits of controlling various markers of a chronic illness—for example, diabetes—all have differing time horizons that, depending on patient prognosis, may never be realized.
For some chronic diseases, the practice may need to develop new quality measures that are appropriate for its patient population. These measures must be evidence-based, or, where evidence is lacking, expert consensus must be attained. The American Geriatrics Society has several clinical practice guidelines, including the treatment of diabetes in older persons, the prevention of falls, and the pharmacologic management of persistent pain.10
Another option is to rely on the traditional Healthcare Effectiveness Data and Information Set quality measures for your chosen chronic condition, but to target appropriate patients for the interventions. One way to do this is to incorporate a prognostic indicator such as the Vulnerable Elders Survey11 or gait speed12 into your office flow so that you can categorize patients into groups and then target interventions.
One more option is to choose a geriatric syndrome that is equally relevant to all your geriatric patients regardless of frailty. However, you must be able to measure aspects of the syndrome and have interventions that will improve specific outcomes.
SETTING PRIORITIES
At the outset, it is important to review the NCQA’s standards for a patient-centered medical home and to identify standards for which you have appropriate processes in place, standards in which you are deficient but which can be fixed, and standards that will be more difficult to address.
One way to do this is to complete the Web-based self-assessment survey, which provides a score by element. Each deficiency discovered is an opportunity to brainstorm solutions and to embark upon a rapid cycle of improvement (“plan, do, study, act”).13 Deficiencies should be tackled over time, however, to avoid overwhelming the practice. It is particularly helpful to create small work-groups, to assign tasks with definite deadlines, and to meet regularly to review progress and assign new tasks.
The NCQA released new standards in 2011. A new requirement is that the practice’s electronic health record system must incorporate Meaningful Use Criteria of the Centers for Medicare and Medicaid Services (CMS). These criteria show that the practice is using the electronic health record effectively. As a result, attaining medical home certification will ensure that the practice also meets CMS Meaningful Use Criteria.
Six standards for a patient-centered medical home
The NCQA has six standards for a patient-centered medical home, which align with the core components of primary care14:
- Standard 1: Enhance access and continuity
- Standard 2: Identify and manage patient populations
- Standard 3: Plan and manage care
- Standard 4: Provide self-care support and community resources
- Standard 5: Track and coordinate care
- Standard 6: Measure and improve performance.
Each of these standards is broken down into elements, designated A, B, C, and so on—27 in all. Each element is scored on the basis of the number of “factors” the practice meets in each element. For example, element E in standard 1 has four factors, and the practice will receive 100% of the two possible points if all four factors are met, 50% of all points if the practice meets two factors, and no points if the practice meets none of the factors.
NCQA now designates a “critical factor” for some elements. These are factors thought to be “central to the concept being assessed within particular elements,”9 and they must be met to score any points for the element. In the same element as above, for example, having regular team meetings or a structured communication process is designated as a critical factor. A practice must meet this factor in order to achieve any of the four points assigned to the element.
SIX ‘MUST-PASS’ ELEMENTS
Of the 27 elements, six are considered essential, and the practice must get a score of at least 50% in all six of these to pass. Since they are the most critical elements, it is often useful to focus on them first to ensure that your practice puts into place policies and other building blocks necessary to make these important elements happen.
Policies must be in place for at least 3 months before submission. Most practices will discover many unwritten workflows as they review these processes.
What follows is a summary of the must-pass elements and their requirements. This is meant to be used only as an overview to better understand the scope of the medical home requirements; the actual requirements should be obtained from the NCQA Web site.
Standard 1, element A: Provide timely access during office hours
This element requires that your office have a policy or process in place for patient access. Same-day appointment availability is deemed a critical factor and must be met to receive any score on the whole element.
The practice needs to measure availability for several different appointment types—new, urgent, and routine—and show that same-day access is available. This can be done by completing at least a 5-day audit measuring the length of time from when a patient contacts the practice to request an appointment to the third next available appointment on his or her clinician’s schedule. It is not enough to simply double-book patients in an already full schedule.
The remaining aspects of this element require being able to provide timely clinical advice by telephone or by secure electronic messages, or both, during office hours, and to document it. The practice must have policies in place that define “timely.” It also must audit phone calls to prove adherence to that policy. The audit should cover at least 5 days. The practice then needs to show at least three examples of clinical advice documented in patients’ charts. We recommend not monitoring all the components during the same week, since the monitoring is laborious and would be overwhelming if attempted all at once.
Standard 2, element D: Use data for population management
This element requires that your practice be able to generate lists of patients and send out reminders of needed services; both are also CMS Meaningful Use Criteria.
Specifically, the NCQA requires that you be able to generate lists of patients’ preventive care and chronic care services and be able to reach out to patients who have deficiencies. The practice must target at least three preventive care services and at least three chronic care services.
One can (and should) link this element to the three important conditions that have been chosen for the practice. For example, if osteoporosis is one of the important conditions, it also can be one of the three preventive care services; a possible quality improvement intervention could be to send reminders to patients to have bone density screening if they have not done so within a certain time frame.
In addition, the practice should have the ability to generate a list of patients who have not been seen at an appropriate interval, as well as a list of patients who are taking certain medications that require regular monitoring. To complete the audit, the practice must produce the four lists just described. Each must then be examined for the previous 12-month period, and documentation must be provided to show how patients with deficiencies were contacted.
Local insurance health plans may be able to help with this element, as these types of lists are often standard practice. Submitting the health plans’ lists is acceptable as long as you can show that they account for at least 75% of the practice.
Standard 3, element C: Manage care for your three conditions
This element focuses on the three clinically important chronic conditions you have chosen. It demonstrates that your practice is following these patients’ outcomes and targeting patients who require more attention to improve their outcomes. Doing so requires documenting pre-visit planning and individualized care plans and treatment goals.
The patient or the family, or both, should be given a written plan of care and a clinical summary at each visit. Barriers to progress need to be assessed, and patients should be contacted if they do not come to scheduled appointments. Patients who have significant barriers should be assessed for additional care management support. This is particularly important for a geriatric population, which may have significant psychosocial barriers such as financial problems, transportation issues, cognitive decline, and overall lack of support.
For each factor in this element, the office must create policies and protocols and assign tasks to appropriate members of the care team. For example, a nurse can make phone calls to targeted patients before their appointments to review goals of care using a standardized form. The form can be given to the physician at the time of the appointment for review and incorporation into the medical record.
Documentation for this element requires that the practice evaluate the number of patients with each chronic condition (the denominator) and the number of patients in each group for whom the above standards have been completed (the numerator) over the previous 3 months. At least 75% compliance is required for each of the three conditions to achieve a passing score for this factor.
This element is very time-consuming, even with an electronic health record. The practice team members should work together to create the systems and tools, but, if possible, it is worth trying to acquire help from an intern or a student. Working on the medical home can be a wonderful educational experience.
Standard 4, element A: Support self-care
For this element, one must show that the practice has educational and self-monitoring tools that are given to all patients depending upon their needs. Involving the patient or family or caregiver in managing the patient’s health is an integral part of the patient-centered medical home.
This is particularly challenging in geriatrics, as many patients may be cognitively unable to participate, and it will be necessary to develop self-management tools that are meaningful for caregivers. When choosing the three clinically important conditions, one needs to keep this element in mind, as the practice must be able to create good educational and self-management tools that are relevant to the important conditions and applicable to the geriatric patient population.
To meet the specific requirements for this element, the practice must show that at least 50% of patients or families receive educational resources and have documented self-management plans, tools, and counseling, and an assessment of their self-management abilities. In addition, one can show that the electronic health record is used to identify patient-specific educational resources in at least 10% of patients. This last factor is also one of the CMS Meaningful Use Criteria.
To document that the practice is completing all the requirements for this element, one must look back 12 months (or at least 3 months if earlier data are unavailable) and use the list of patients with the three clinically important conditions. In addition, the practice needs to identify its high-risk or complex patients over the same time period. These two lists comprise the denominator. The numerator is the number of patients for which you can show documentation of each of the above items.
Because this audit is also time-consuming, it and standard 3, element C (care management) should be combined and performed simultaneously.
Standard 5, element B: Track referrals and follow-up
This is often the most difficult must-pass element to fulfill because it requires coordination with health care providers outside one’s practice. To complete this element, the office must have a system in place to track referrals originating within the practice and to ensure that all relevant information is both sent to and received back from the consultant. This tracking must include the reason for and the urgency of the referral, as well as relevant clinical information. One can also establish comanagement when needed for patients who are seen regularly by a specific specialist.
Making sure that the consultant’s report gets back to the practice is, for most sites, the most difficult part. It is often not feasible to do this entirely through the electronic health record, as it is unlikely that all your consultants have the same electronic health record as your practice. Therefore, this often requires at least a partially paper-based system, creating a file that must be checked on a regular basis to ensure that the appointment with the consultant has been completed and that he or she has sent a note back. If the information is not all there, there must be documentation of a phone call that tried to obtain the necessary information or to document the patient’s refusal to follow up.
Two factors in this element also meet CMS Meaningful Use Criteria: demonstrating the capability for electronic exchange of key clinical information between clinicians, and providing an electronic summary of the care record for more than 50% of referrals. To complete the documentation for this element, the practice must do an audit that reviews at least a week’s worth of referrals.
Standard 6, element C: Implement continuous quality improvement
This element requires demonstration of continuous quality improvement activities in specific domains that are outlined in standard 6, elements A and B. Element A includes preventive care measures, chronic or acute care clinical measures, and measures that affect health care costs or help to assess disparities in vulnerable patients’ care. Element B includes surveying access, communication, coordination, and self-management support or obtaining feedback from vulnerable patient groups or patients and their families.
Once again, there is the potential for considerable overlap in the work that your practice does with the clinically important conditions, and with standard 1 (access), standard 2 (population reminders for preventive services), standard 3 (care management), and standard 4 (self-management). This overlap provides the opportunity to go into more depth and to show significant quality outcomes for some of the chosen measures.
This element requires the practice to set goals and to act to improve at least three measures from element A and at least one measure from element B. Points are also awarded for addressing at least one disparity in care or service for vulnerable populations. In geriatrics, some examples of vulnerable populations include the very frail, patients and families with significant psychosocial issues, those at the end of life, or patients with significant financial burdens (especially related to health care costs). Finally, points are awarded for involving patients or families in quality improvement teams.
To document adherence to this element, the practice must demonstrate quality improvement reports for all the selected measures as well as actions taken in response to the data. The goal is to meet the desired level of achievement that is established by your practice. If patients or families are asked to join quality improvement teams, the practice must describe the process employed for inclusion and details of the frequency of meetings and agendas.
OTHER ELEMENTS
Besides the must-pass elements, there are 21 additional elements, each with its own specific requirements and documentation. Some of these overlap with the concepts in the must-pass elements, so it is important to create processes that work for all the factors in all the related elements.
It is also important to understand that one does not need to master all the other elements— the practice can choose ones that are most meaningful for its patient population. One can also elect to skip ones that require particularly labor-intensive audits and that do not add much to the quality of geriatric patient care. The team should focus on making changes that help patient care and flow. All recognition levels require a minimum 50% score for the six must-pass elements, and the final recognition level is based on the following three criteria:
- Level 1: 35–59 points and all six must-pass elements
- Level 2: 60–84 points and all six must-pass elements
- Level 3: 85–100 points and all six must-pass elements.
FINAL SUBMISSION
Final submission involves completion of the application materials mentioned above, payment of the application fee, and attachment of files that have been linked to elements from the document library.
The process of uploading files for submission can be complex when multiple staff members are working on the documents. Files must be uploaded from shared drives, which should be set up when one begins the process of gathering documents. As a last step, the document library must be uploaded to the NCQA server. It is best to do this in batches of files. The time needed to upload depends on the speed of the Internet service. The survey form will indicate if each file has been successfully uploaded to the NCQA server.
The submitted survey tool is assigned a project number that can be used as a reference for inquiries to the NCQA. It is best to keep a copy of the final submission information for future use. Before submitting, it is a good idea to ask someone not involved in your practice to review the documents for clarity and consistency. Remember, the survey tool is a “read-only” document after submission, so no changes can be made to it after final submission.
- Sia C, Tonniges TF, Osterhus E, Taba S. Pediatrics. History of the medical home concept. Pediatrics 2004; 113( suppl 5):1473–1478.
- Robert Graham Center: Center for Policy Standards in Family Medicine and Primary Care. The patient centered medical home: history, seven core features, evidence and transformational change. November 2007. http://www.graham-center.org/online/graham/home/publications/monographs-books/2007/rgcmo-medical-home.html. Accessed April 4, 2012.
- Lee JG, Dayal G, Fontaine D. Starting a medical home: better health at lower cost. Healthcare Financial Management Association. June 2011. http://www.hfma.org/Templates/InteriorMaster.aspx?id=27048. Accessed April 4, 2012.
- Grumbach K, Grundy P. Outcomes of implementing patient centered medical home interventions: a review of the evidence from prospective evaluation studies in the United States. Patient-Centered Primary Care Collaborative. November 2010. http://www.pcpcc.net/content/patient-centered-medical-home. Accessed April 4, 2012.
- Reid RJ, Coleman K, Johnson EA, et al. The group health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood) 2010; 29:835–843.
- Huang ES, Zhang Q, Gandra N, Chin MH, Meltzer DO. The effect of comorbid illness and functional status on the expected benefits of intensive glucose control in older patients with type 2 diabetes: a decision analysis. Ann Intern Med 2008; 149:11–19.
- American College of Physicians. Medical home builder. http://www.Medicalhomebuilder.org. Accessed April 4, 2012.
- Nutting PA, Miller WL, Crabtree BF, Jaen CR, Stewart EE, Stange KC. Initial lessons from the first national demonstration project on practice transformation to a patient-centered medical home. Ann Fam Med 2009; 7:254–260.
- National Committee for Quality Assurance (NCQA). Standards and guidelines for NCQA’s patient-centered medical home (PCMH). March 2011. www.chcact.org/images/customer-files//Appendix3_PCMH2011glossary.pdf. Accessed April 4, 2012.
- American Geriatrics Society. http://www.americangeriatrics.org/health_care_professionals/clinical_practice/clinical_guidelines_recommendations/. Accessed April 4, 2012.
- Min LC, Elliott MN, Wenger NS, Saliba D. Higher vulnerable elders survey scores predict death and functional decline in vulnerable older people. J Am Geriatr Soc 2006; 54:507–511.
- Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA 2011; 305:50–58.
- Plan, do, check, act. In:Karlof B, Lovingsson F, editors. A to Z of Management Concepts & Models. London: Thorogood Publishing; 2005.
- National Committee for Quality Assurance (NCQA). NCQA 2011 Requirements. www.ncqa.org/tabid/1405/Default.aspx. Accessed April 4, 2012.
- Sia C, Tonniges TF, Osterhus E, Taba S. Pediatrics. History of the medical home concept. Pediatrics 2004; 113( suppl 5):1473–1478.
- Robert Graham Center: Center for Policy Standards in Family Medicine and Primary Care. The patient centered medical home: history, seven core features, evidence and transformational change. November 2007. http://www.graham-center.org/online/graham/home/publications/monographs-books/2007/rgcmo-medical-home.html. Accessed April 4, 2012.
- Lee JG, Dayal G, Fontaine D. Starting a medical home: better health at lower cost. Healthcare Financial Management Association. June 2011. http://www.hfma.org/Templates/InteriorMaster.aspx?id=27048. Accessed April 4, 2012.
- Grumbach K, Grundy P. Outcomes of implementing patient centered medical home interventions: a review of the evidence from prospective evaluation studies in the United States. Patient-Centered Primary Care Collaborative. November 2010. http://www.pcpcc.net/content/patient-centered-medical-home. Accessed April 4, 2012.
- Reid RJ, Coleman K, Johnson EA, et al. The group health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood) 2010; 29:835–843.
- Huang ES, Zhang Q, Gandra N, Chin MH, Meltzer DO. The effect of comorbid illness and functional status on the expected benefits of intensive glucose control in older patients with type 2 diabetes: a decision analysis. Ann Intern Med 2008; 149:11–19.
- American College of Physicians. Medical home builder. http://www.Medicalhomebuilder.org. Accessed April 4, 2012.
- Nutting PA, Miller WL, Crabtree BF, Jaen CR, Stewart EE, Stange KC. Initial lessons from the first national demonstration project on practice transformation to a patient-centered medical home. Ann Fam Med 2009; 7:254–260.
- National Committee for Quality Assurance (NCQA). Standards and guidelines for NCQA’s patient-centered medical home (PCMH). March 2011. www.chcact.org/images/customer-files//Appendix3_PCMH2011glossary.pdf. Accessed April 4, 2012.
- American Geriatrics Society. http://www.americangeriatrics.org/health_care_professionals/clinical_practice/clinical_guidelines_recommendations/. Accessed April 4, 2012.
- Min LC, Elliott MN, Wenger NS, Saliba D. Higher vulnerable elders survey scores predict death and functional decline in vulnerable older people. J Am Geriatr Soc 2006; 54:507–511.
- Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA 2011; 305:50–58.
- Plan, do, check, act. In:Karlof B, Lovingsson F, editors. A to Z of Management Concepts & Models. London: Thorogood Publishing; 2005.
- National Committee for Quality Assurance (NCQA). NCQA 2011 Requirements. www.ncqa.org/tabid/1405/Default.aspx. Accessed April 4, 2012.
KEY POINTS
- The NCQA has six broad standards for patient-centered medical homes: practices must enhance access and continuity, identify and manage patient populations, plan and manage care, provide self-care support and community resources, track and coordinate care, and measure and improve performance.
- Each standard has a number of elements, of which six are “must-pass.” These deal with access, data for population management, care management, support for self-care, referral tracking and follow-up, and continuous quality improvement. All must be rigorously documented.
- Practices must identify three important medical conditions for continuous quality improvement.
- Applying for certification is hard work but, if accompanied by real changes to your practice, should improve the care you deliver.
The rationale for, and design of, a lung cancer screening program
In 2011, two papers were published that will shape the way we think about lung cancer screening for years to come.
See related patient information sheet
While the ability to screen for lung cancer is a major positive change, it also raises many thorny questions, such as who should be screened, how often should they be screened, and how should we respond when a nodule is detected.
To answer some of these questions, we will outline how Cleveland Clinic has structured its lung cancer screening program, and the rationale we used for making pragmatic patient-care decisions within this program. We will conclude with our thoughts about the potential evolution of lung cancer screening programs.
THE 40-YEAR QUEST FOR EFFECTIVE LUNG CANCER SCREENING
Lung cancer kills more people in the United States than the next four most lethal types of cancer combined.3 It is curable if found early in its course. Unfortunately, most people who develop lung cancer feel no symptoms when it is early in its course, and therefore it is too often diagnosed at a late stage. Treatment for late-stage lung cancer is effective, but it is rarely curative.
Screening refers to testing people at risk of developing a disease before its symptoms or signs have appeared. The goal of screening is to reduce the disease-specific mortality rate. For this to happen, the disease must be detectable in a preclinical form, and treatment must be more successful when applied early. Ideally, the screening test should pose little risk to the patient, be sensitive for detecting the disease early in its course, give few false-positive results, be acceptable to the patient, and be relatively inexpensive to the health system.
Over the past 4 decades, a large volume of research has been done in the hope of proving that conventional radiography or CT could be an effective screening test for lung cancer.4,5
Cohort studies (ie, in which all the patients were screened) of radiography or CT have shown a longer survival from the time of lung cancer diagnosis than would be expected without screening. These studies were not designed to prove a reduction in the lung cancer-specific mortality rate.
Controlled trials (in which half the patients received the screening and the other half did not) of chest radiography have been interpreted as not showing a reduction in lung cancer mortality rates, though debate about the interpretation of these trials persisted until this past year. Biases inherent in using duration of survival rather than the mortality rate as an end point have been suggested as the reason for the apparent benefit in survival without a reduction in the mortality rate.
Controlled trials of CT screening were started nearly a decade ago. Until 2011, the results of these trials were not mature enough to comment on.
THE PROSTATE, LUNG, COLORECTAL, AND OVARIAN TRIAL
The lung cancer screening portion of the PLCO trial aimed to determine the effect of screening chest radiography on lung cancer-specific mortality rates.1
In this trial, 154,901 people were randomized to undergo either posteroanterior chest radiography every year for 4 years or usual care, ie, no lung cancer screening. Participants were men and women age 55 to 74 with no history of prostate, lung, colorectal, or ovarian cancer. They did not need to be a smoker to participate. Those who had never smoked and who were randomized to the screening group received only 3 years of testing. All were followed for 13 years or until the conclusion of the study (8 years after the final participant was enrolled). About half were women, and nearly two-thirds were age 55 through 64. Only 10% were current smokers, while a full 45% had never smoked.
Results. Adherence to screening in the screening group ranged from 79% to 86.6% over the years of screening, and 11% of the usual-care group was estimated to have undergone screening chest radiography.
Cumulative lung cancer incidence rates were 201 per 100,000 person-years in the screening group and 192 in the usual-care group.
In the screening group, there were a total of 1,696 lung cancers during the entire study. Of these, 307 (18%) were detected by screening, 198 (12%) were interval cancers (diagnosed during the screening period but not by the screening test), and the remainder were diagnosed after the screening period during the years of follow-up. In the screening group, the cancers detected by screening were more likely to be adenocarcinomas and less likely to be small-cell carcinomas than those not detected by screening. Also in the screening group, the cancers detected by screening were more likely to be stage I (50%) than those not detected by screening.
The cumulative number of deaths from lung cancer was slightly but not significantly lower in the screening group from years 4 through 11. However, by the end of follow-up, the number of lung cancer deaths was equal between the groups (1,213 in the screening group vs 1,230 in the usual-care group). The cumulative overall mortality rate was also similar between the groups. For the subgroup who would have qualified for the NLST (see below), the lung cancer mortality rate was statistically similar between the two groups.
Comments. The results of the PLCO screening trial will be interpreted as the final word in lung cancer screening with standard chest radiography. The conclusion is that annual screening with chest radiography does not reduce lung cancer mortality rates and thus should not be performed in this context.
THE NATIONAL LUNG SCREENING TRIAL
The NLST aimed to determine if screening with low-dose chest CT could reduce lung cancer mortality rates.2
This controlled trial enrolled 53,454 people, who were randomized to undergo either low-dose chest CT or posteroanterior chest radiography at baseline and then yearly for 2 years.
Participants were men and women age 55 to 74 with at least 30 pack-years of cigarette smoking. If they had quit smoking, they had to have quit within the past 15 years. All were followed until study conclusion (median 6.5 years, maximum 7.4). About 41% were women, and nearly three-quarters were age 55 through 64. More than 48% were current smokers, with the rest being former smokers.
Results. Adherence to screening was 95% in the CT group and 93% in the radiography group, with a 4.3% annual rate of CT outside the study during the screening phase.
Cumulative lung cancer incidence rates were 645 per 100,000 person-years in the CT group and 572 in the radiography group.
In the CT group there were a total of 1,060 lung cancers during the entire study. Of these, 649 (61%) were detected by screening, 44 (4%) were interval cancers, and the rest were diagnosed after the screening period during follow-up.
In the chest radiography group, there were a total of 941 lung cancers during the entire study. Of these, 279 (30%) were detected by screening, 137 (15%) were interval cancers, and the rest were diagnosed after the screening period. Within the CT group, the cancers detected by screening were more likely to be adenocarcinomas and less likely to be small-cell carcinomas than those not detected by screening. Also within the CT group, the cancers detected by screening were more likely to be stage I (63%) than those not detected by screening.
The cumulative number of deaths from lung cancer was 443 in the radiography group, but only 356 in the CT group—20.0% lower (P =.004). The cumulative overall mortality rate was 6.7% lower in the CT group (P = .02).
Comments. The results of the NLST provide the first evidence that lung cancer mortality rates can be reduced by screening. Though many questions remain, the conclusions of this study are that screening a well-defined high-risk group with low-dose CT reduces the rate of death from lung cancer.
REMAINING CHALLENGES
The NLST showed that lung cancer screening with low-dose CT can meet the most important criterion for a successful screening program, ie, a reduction in the disease-specific mortality rate. Many challenges remain in meeting the other criteria for a successful or ideal screening program (low risk, few false-positive results, acceptability to the patient, and affordability). The issues with low-dose CT-based screening that challenge these ideals are outlined in this section.
Lung nodules: Benign or malignant?
A meta-analysis of CT screening studies found that for every 1,000 people screened at baseline, 9 were found to have stage I non-small-cell lung cancer, 235 had false-positive nodules, and 4 underwent thoracotomy for benign lesions.6
The NLST results were similar. In this trial, only nodules that were 4 mm or greater in diameter were reported. Using these criteria, over 27% of all study participants were found to have a lung nodule on CT at baseline and at year 1. The rate fell to nearly 17% at year 2, as nodules present from baseline were not reported. Of all the lung nodules detected, only 3.6% were ultimately proven to represent lung cancer.2
Many issues with small lung nodules need to be considered. The nodules are difficult to find, with highly variable reporting even by expert radiologists.7 They are difficult to measure accurately and thus are difficult to assess for growth.8 Adjunctive imaging and nonsurgical biopsy have a low yield for small nodules.9–11 Follow-up of these lung nodules includes additional imaging and nonsurgical and surgical biopsy procedures, adding expense to the program and risk to the patient. Finally, knowing that they have a lung nodule makes patients feel anxious and thus negatively affects their quality of life.12,13
Radiation exposure: How great is the risk?
There is a great deal of concern about radiation exposure from medical imaging, as many people receive a substantial amount of radiation each year from medical testing.14 A single low-dose scan with chest CT delivers a whole-body effective dose of about 1.5 mSv—less than one-fifth of the radiation dose of a typical diagnostic CT scan.
Many have tried to estimate the consequences of radiation exposure from low-dose CT screening. All estimates are extrapolations from unrelated radiation exposures. The increase in risk of death ranged from 0.01% to a few percent,15 and the increase in cancers was as high as 1.8% over a 25-year screening period.16 In general, the risks are felt to be very low but not negligible.
Cost-effectiveness is unknown
The cost-effectiveness of lung cancer screening is also unknown. Many highly variable estimates have been published.17–20 The studies have differed in the perspective taken, the costs of testing assumed, and the rounds of screening included. The most cost-effective estimates are in populations with the highest risk of cancer, in programs that achieve the greatest reduction in mortality rate, and in programs that lead to high rates of smoking cessation.
Screening in the real world as opposed to a clinical trial may involve different risks, benefits, and costs. Compliance with screening and with nodule management algorithms may be lower outside of a study. One study suggested that those at highest risk of developing lung cancer would be the least likely to enroll in a screening program and the least likely to accept curative-intent surgery for screening-detected cancer.21
We expect that the NLST data will be analyzed for cost-effectiveness. This should provide the most accurate estimates for the group that was studied.
WE SET OUT TO DESIGN A SCREENING PROGRAM
With the evidence supporting a reduction in the rate of lung cancer mortality, and knowing the remaining challenges, we set out to provide a lung cancer screening program within Cleveland Clinic. In the design of our program, we considered several questions, outlined below.
Who should be offered low-dose CT screening?
The results of the NLST led to a great deal of excitement about lung cancer screening in both the medical community and the general public. The positive side of this publicity is that lung cancer is receiving attention that may lead to support for further advances. The negative side is that many patients who may seek out lung cancer screening are not at high enough risk of lung cancer to clearly benefit from it.
In the NLST, a very high-risk cohort was studied, as defined by clinical variables (age 55 to 74, at least 30 pack-years of smoking, and if a former smoker, had quit within the past 15 years). In this high-risk group, 320 patients needed to be screened (with three yearly chest CT scans) for one life to be saved from lung cancer, and only 3.6% of all lung nodules found (4 mm or larger) were actually lung cancer. In a group at lower risk, the number that needed to be screened to save one life would be higher, and the percentage of lung nodules that truly were lung cancer would be lower. This would lead to higher risks and costs related to screening, without a proven benefit to members of the lower-risk group.
The risk of the NLST cohort developing lung cancer was approximately 0.6% per year. Lung cancer risk-prediction models have been developed and published. Up to 2011, the three most commonly used models had only moderate accuracy at predicting risk.22–25 In 2011 a risk model based on the PLCO cohort was developed and published.26 This model seemed to be more accurate but perhaps a bit harder to apply in practice.
We discussed whether using a validated risk predictor with a target of 0.6% per year (ie, the risk in the NLST trial) would be an adequate means of deciding on candidacy for lung cancer screening or if we should strictly adhere to the inclusion criteria of the NLST cohort. We feel that the NLST cohort is the only group with true evidence of benefit (a reduction in the lung cancer-specific mortality rate). Thus, for our program’s entry criteria, we decided to use the same clinical predictors used for entry in the NLST.
How will the right patients get scheduled for low-dose screening CT?
Patients who enter the lung cancer screening program from our health system will require a physician’s order.
We are fortunate to have an electronic medical record in place. We have created an order set within the electronic record for low-dose chest CT. The order will eventually be able to be entered as “CT lung screening w/o” (ie, without contrast).
For patients from outside of our health system who would like to enter the lung cancer screening program, the entry criteria will be the same (see above). We will ask for the name of the patient’s primary care practitioner. If the patient does not have one, a member of our Respiratory Institute will see and enroll the patient.
How often should patients be screened, and for how many years?
Unfortunately, questions about the frequency of screening and how many years it should continue remain unanswered.
In the NLST, a similar number of early-stage lung cancers were detected during each of the three screening rounds. In both the NLST and PLCO trials, differences in the mortality rate curves began to narrow during the observation period, when active screening was no longer occurring. Thus, it is possible that a longer duration of screening could lead to a further reduction in mortality rates. Others have questioned whether a similar benefit, with less cost and risk, could be obtained by screening every 2 years.
The large amount of data obtained from the NLST and other CT-based studies is being reviewed so that models can be developed to help answer these questions. For now, we suggest at least three yearly CT screenings, with the hope that we will have clearer answers to these questions over time.
How will low-dose CT be performed and interpreted?
The parameters for low-dose CT were very tightly controlled and monitored during the NLST. This quality-control effort, designed to improve consistency across sites and to minimize risk to patients, should be carried into lung cancer screening programs.
Our program will closely mimic the CT performance criteria used in the NLST (tube current-time product 40 mAs for all patients, field of view lungs only, lung kernel images 3 mm at 1.5-mm intervals, and soft-tissue kernel images 5 mm at 2.5-mm intervals).27 In the initial phase of the program, all screening scans will be performed at Cleveland Clinic’s main imaging facility.
Small lung nodules remain quite challenging to detect and measure. To minimize variability in scan interpretation, the NLST readers were all expertly trained radiologists. Despite this, much variability was noted in the number of nodules detected, their measured size, and the follow-up recommendations. All of the screening CT images for our program will be interpreted by board-certified radiologists with expertise in chest imaging.
Other screening studies have included novel imaging assessment in their testing algorithms, particularly volumetric analysis of lung nodules.28 These tools may prove to assist in nodule detection, measurement, and management over time. At this point, we do not think they have been studied and standardized enough to include them in a standard-of-care screening program. We hope that they will evolve to the point of clinical utility in the near future.
Lung cancer screening is not currently covered by most insurers, including Medicare, although one major insurer has recently started to cover it. We expect decisions on coverage from other insurers in the next 12 months. In the meantime, we offer a low-dose screening chest CT to our patients for $125, which includes the radiologist’s fee for interpreting the scan.
Smoking cessation
The NLST showed that low-dose CT screening can reduce lung cancer mortality rates by 20% in a high-risk group. A 50-year-old active smoker who quits smoking reduces his or her risk of dying of lung cancer by more than 50%.29 Entry into a lung cancer screening program provides an opportunity for education and assistance with tobacco dependency.
At Cleveland Clinic, we have an active Tobacco Treatment Center within our Wellness Institute. All lung cancer screening participants who are identified as active smokers will be given a program brochure and will be offered a consult in the program.
What do we identify as a lung nodule, and how should they be managed?
Studies of CT-based screening have highlighted the tremendous number of lung nodules that are identified and the low likelihood of malignancy in those that are less than 1 cm in diameter. Many screening studies define a positive result as a lung nodule above a particular size. The NLST used 4 mm or greater as the cutoff. The lower the cutoff, the greater the number of nodules found, and the lower the overall likelihood of malignancy in the nodules.
Studies in which annual CT screening was the intervention are able to use size criteria in part because the study design ensures another CT will be performed 12 months later. Current nodule management guidelines suggest 12-month CT follow-up of incidentally discovered lung nodules, 4 mm or smaller, in at-risk patients.30 In a screening program, particularly one for which the patient must pay, the 12-month screening CT cannot be guaranteed. This makes it more difficult to ignore the smallest nodules identified on CT screening. Given this, we will be reporting all lung nodules identified, regardless of size on the initial screening.
Most studies of CT screening have reported any new nodule identified in subsequent screening rounds regardless of size. Though it is intuitive that a new nodule would have a high likelihood of malignancy in a high-risk cohort, malignancy rates have been reported to be as low as 1% for new nodules. As with the initial round of screening, we will report all new lung nodules identified in subsequent screening rounds.
The recommendations for the evaluation of lung nodules, both within the report and at the lung nodule clinic, are in keeping with currently available guidelines, such as those from the Fleischner Society30 and the American College of Chest Physicians.31 For incidentally discovered lung nodules in patients at high risk, the Fleischner Society recommendations are as follows30:
- For nodules 4 mm or smaller, follow-up in 12 months; if no growth, then no further follow-up
- For nodules 4 to 6 mm, follow-up at 6 to 12 months, then 18 to 24 months if no growth
- For nodules 6 to 8 mm, follow-up at 3 to 6 months, then 9 to 12 months, then 24 months if no growth
- For nodules 8 mm or larger, follow-up at 3, 9, and 24 months, or positron emission tomography, or biopsy, or both.
If the nodule is large enough or is deemed to be of high enough risk, adjuvant testing with diagnostic imaging, guided bronchoscopy, transthoracic needle aspiration, or minimally invasive resection will be offered. All patients with nodules believed to require biopsy will be discussed at our multidisciplinary lung cancer tumor board before biopsy.
How do we make practitioners and patients aware of the program and its indications, risks, and benefits?
Education will be the key to having lung cancer screening adopted as the standard of care, to lung cancer screening being provided within a well-designed and capable system, and to ensuring that patients have realistic expectations about screening. Articles such as this and grand rounds presentations within our health system will help provide education to our colleagues. Broader marketing campaigns will be considered in the future once demand and system capabilities are clearly identified. A patient information brochure will be provided at the time of the screening test (see the patient information sheet that accompanies this article).
How do we help to advance best practice?
As excited as we are that low-dose CT-based lung cancer screening has been proven to reduce lung cancer mortality rates, it is clear that there is a lot of room to improve the programs that are developed based on current data.
Advances in our ability to accurately predict an individual’s risk of developing lung cancer will allow us to offer screening to those it is most likely to benefit.
Advances in smoking cessation and chemoprevention will help to minimize the number of lung cancers that develop.
Advances in our ability to determine the nature of lung nodules will allow us to accelerate treatment of very early lung cancer while minimizing additional testing on benign nodules; advances in our ability to treat localized and advanced disease will improve the outcome for those identified as having lung cancer.
To help move the science of screening forward, we will develop a screening program registry that can be populated from the order set and the templated report. The registry can be used to ensure appropriate patient care, while studying relevant epidemiologic, quality, and cost-related questions.
We hope to assess novel imaging software capable of assisting with the detection and characterization of lung nodules.
We have an active biomarker development program to assess the ability of breath and blood-based biomarkers to identify those at risk of developing lung cancer; to assist with the management of screening-detected lung nodules; to assist with the diagnosis of early stage lung cancer; and to characterize the nature of the cancers identified. Accurate biomarkers could lead to further decreases in mortality rates while reducing the risks and costs of a screening program.
We have strong surgical, medical, and radiation oncology programs, actively pursuing advances in minimally invasive resection procedures and ablative and targeted therapies.
ENTERING A NEW ERA
We are entering a new era of lung cancer screening. The NLST has shown that lung cancer morality rates can be reduced through low-dose CT screening in a high-risk population. Many challenges remain, such as managing the nodules that are discovered, determining if the program is cost-effective, and minimizing radiation exposure. These need to be considered when designing a lung cancer screening program. Advances over time will help us optimize the programs that are developed.
- Oken MM, Hocking WG, Kvale PA, et al; PLCO Project Team. Screening by chest radiograph and lung cancer mortality: the Prostate, Lung, Colorectal, and Ovarian (PLCO) randomized trial. JAMA 2011; 306:1865–1873.
- National Lung Screening Trial Research Team; Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011; 365:395–409.
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin 2012; 62:10–29.
- Mazzone PJ, Mekhail T. Lung cancer screening. Curr Oncol Rep 2007; 9:265–274.
- Mazzone PJ. Lung cancer screening: an update, discussion, and look ahead. Curr Oncol Rep 2010; 12:226–234.
- Gopal M, Abdullah SE, Grady JJ, Goodwin JS. Screening for lung cancer with low-dose computed tomography: a systematic review and meta-analysis of the baseline findings of randomized controlled trials. J Thorac Oncol 2010; 5:1233–1239.
- Gierada DS, Pilgram TK, Ford M, et al. Lung cancer: interobserver agreement on interpretation of pulmonary findings at low-dose CT screening. Radiology 2008; 246:265–272.
- Singh S, Pinsky P, Fineberg NS, et al. Evaluation of reader variability in the interpretation of follow-up CT scans at lung cancer screening. Radiology 2011; 259:263–270.
- Lindell RM, Hartman TE, Swensen SJ, et al. Lung cancer screening experience: a retrospective review of PET in 22 non-small cell lung carcinomas detected on screening chest CT in a high-risk population. AJR Am J Roentgenol 2005; 185:126–131.
- Baaklini WA, Reinoso MA, Gorin AB, Sharafkaneh A, Manian P. Diagnostic yield of fiberoptic bronchoscopy in evaluating solitary pulmonary nodules. Chest 2000; 117:1049–1054.
- Kothary N, Lock L, Sze DY, Hofmann LV. Computed tomography-guided percutaneous needle biopsy of pulmonary nodules: impact of nodule size on diagnostic accuracy. Clin Lung Cancer 2009; 10:360–363.
- van den Bergh KA, Essink-Bot ML, Borsboom GJ, et al. Short-term health-related quality of life consequences in a lung cancer CT screening trial (NELSON). Br J Cancer 2010; 102:27–34.
- Lemonnier I, Baumann C, Jolly D, et al. Solitary pulmonary nodules: consequences for patient quality of life. Qual Life Res 2011; 20:101–109.
- Fazel R, Krumholz HM, Wang Y, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 2009; 361:849–857.
- Buls N, de Mey J, Covens P, Stadnik T. Health screening with CT: prospective assessment of radiation dose and associated detriment. JBR-BTR 2005; 88:12–16.
- Brenner DJ. Radiation risks potentially associated with low-dose CT screening of adult smokers for lung cancer. Radiology 2004; 231:440–445.
- Mahadevia PJ, Fleisher LA, Frick KD, Eng J, Goodman SN, Powe NR. Lung cancer screening with helical computed tomography in older adult smokers: a decision and cost-effectiveness analysis. JAMA 2003; 289:313–322.
- Wisnivesky JP, Mushlin AI, Sicherman N, Henschke C. The cost-effectiveness of low-dose CT screening for lung cancer: preliminary results of baseline screening. Chest 2003; 124:614–621.
- Manser R, Dalton A, Carter R, Byrnes G, Elwood M, Campbell DA. Cost-effectiveness analysis of screening for lung cancer with low dose spiral CT (computed tomography) in the Australian setting. Lung Cancer 2005; 48:171–185.
- McMahon PM, Kong CY, Bouzan C, et al. Cost-effectiveness of computed tomography screening for lung cancer in the United States. J Thorac Oncol 2011; 6:1841–1848.
- Silvestri GA, Nietert PJ, Zoller J, Carter C, Bradford D. Attitudes towards screening for lung cancer among smokers and their nonsmoking counterparts. Thorax 2007; 62:126–130.
- Bach PB, Kattan MW, Thornquist MD, et al. Variations in lung cancer risk among smokers. J Natl Cancer Inst 2003; 95:470–478.
- Spitz MR, Hong WK, Amos CI, et al. A risk model for prediction of lung cancer. J Natl Cancer Inst 2007; 99:715–726.
- Cassidy A, Myles JP, van Tongeren M, et al. The LLP risk model: an individual risk prediction model for lung cancer. Br J Cancer 2008; 98:270–276.
- D’Amelio AM, Cassidy A, Asomaning K, et al. Comparison of discriminatory power and accuracy of three lung cancer risk models. Br J Cancer 2010; 103:423–429.
- Tammemagi CM, Pinsky PF, Caporaso NE, et al. Lung cancer risk prediction: Prostate, Lung, Colorectal And Ovarian Cancer Screening Trial models and validation. J Natl Cancer Inst 2011; 103:1058–1068.
- National Lung Screening Trial Research Team; Aberle DR, Berg CD, Black WC, et al. The National Lung Screening Trial: overview and study design. Radiology 2011; 258:243–253.
- van Klaveren RJ, Oudkerk M, Prokop M, et al. Management of lung nodules detected by volume CT scanning. N Engl J Med 2009; 361:2221–2229.
- Peto R, Darby S, Deo H, Silcocks P, Whitley E, Doll R. Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies. BMJ 2000; 321:323–329.
- MacMahon H, Austin JH, Gamsu G, et al; Fleischner Society. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology 2005; 237:395–400.
- Gould MK, Fletcher J, Iannettoni MD, et al; American College of Chest Physicians. Evaluation of patients with pulmonary nodules: when is it lung cancer?: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007; 132(suppl 3):108S–130S.
In 2011, two papers were published that will shape the way we think about lung cancer screening for years to come.
See related patient information sheet
While the ability to screen for lung cancer is a major positive change, it also raises many thorny questions, such as who should be screened, how often should they be screened, and how should we respond when a nodule is detected.
To answer some of these questions, we will outline how Cleveland Clinic has structured its lung cancer screening program, and the rationale we used for making pragmatic patient-care decisions within this program. We will conclude with our thoughts about the potential evolution of lung cancer screening programs.
THE 40-YEAR QUEST FOR EFFECTIVE LUNG CANCER SCREENING
Lung cancer kills more people in the United States than the next four most lethal types of cancer combined.3 It is curable if found early in its course. Unfortunately, most people who develop lung cancer feel no symptoms when it is early in its course, and therefore it is too often diagnosed at a late stage. Treatment for late-stage lung cancer is effective, but it is rarely curative.
Screening refers to testing people at risk of developing a disease before its symptoms or signs have appeared. The goal of screening is to reduce the disease-specific mortality rate. For this to happen, the disease must be detectable in a preclinical form, and treatment must be more successful when applied early. Ideally, the screening test should pose little risk to the patient, be sensitive for detecting the disease early in its course, give few false-positive results, be acceptable to the patient, and be relatively inexpensive to the health system.
Over the past 4 decades, a large volume of research has been done in the hope of proving that conventional radiography or CT could be an effective screening test for lung cancer.4,5
Cohort studies (ie, in which all the patients were screened) of radiography or CT have shown a longer survival from the time of lung cancer diagnosis than would be expected without screening. These studies were not designed to prove a reduction in the lung cancer-specific mortality rate.
Controlled trials (in which half the patients received the screening and the other half did not) of chest radiography have been interpreted as not showing a reduction in lung cancer mortality rates, though debate about the interpretation of these trials persisted until this past year. Biases inherent in using duration of survival rather than the mortality rate as an end point have been suggested as the reason for the apparent benefit in survival without a reduction in the mortality rate.
Controlled trials of CT screening were started nearly a decade ago. Until 2011, the results of these trials were not mature enough to comment on.
THE PROSTATE, LUNG, COLORECTAL, AND OVARIAN TRIAL
The lung cancer screening portion of the PLCO trial aimed to determine the effect of screening chest radiography on lung cancer-specific mortality rates.1
In this trial, 154,901 people were randomized to undergo either posteroanterior chest radiography every year for 4 years or usual care, ie, no lung cancer screening. Participants were men and women age 55 to 74 with no history of prostate, lung, colorectal, or ovarian cancer. They did not need to be a smoker to participate. Those who had never smoked and who were randomized to the screening group received only 3 years of testing. All were followed for 13 years or until the conclusion of the study (8 years after the final participant was enrolled). About half were women, and nearly two-thirds were age 55 through 64. Only 10% were current smokers, while a full 45% had never smoked.
Results. Adherence to screening in the screening group ranged from 79% to 86.6% over the years of screening, and 11% of the usual-care group was estimated to have undergone screening chest radiography.
Cumulative lung cancer incidence rates were 201 per 100,000 person-years in the screening group and 192 in the usual-care group.
In the screening group, there were a total of 1,696 lung cancers during the entire study. Of these, 307 (18%) were detected by screening, 198 (12%) were interval cancers (diagnosed during the screening period but not by the screening test), and the remainder were diagnosed after the screening period during the years of follow-up. In the screening group, the cancers detected by screening were more likely to be adenocarcinomas and less likely to be small-cell carcinomas than those not detected by screening. Also in the screening group, the cancers detected by screening were more likely to be stage I (50%) than those not detected by screening.
The cumulative number of deaths from lung cancer was slightly but not significantly lower in the screening group from years 4 through 11. However, by the end of follow-up, the number of lung cancer deaths was equal between the groups (1,213 in the screening group vs 1,230 in the usual-care group). The cumulative overall mortality rate was also similar between the groups. For the subgroup who would have qualified for the NLST (see below), the lung cancer mortality rate was statistically similar between the two groups.
Comments. The results of the PLCO screening trial will be interpreted as the final word in lung cancer screening with standard chest radiography. The conclusion is that annual screening with chest radiography does not reduce lung cancer mortality rates and thus should not be performed in this context.
THE NATIONAL LUNG SCREENING TRIAL
The NLST aimed to determine if screening with low-dose chest CT could reduce lung cancer mortality rates.2
This controlled trial enrolled 53,454 people, who were randomized to undergo either low-dose chest CT or posteroanterior chest radiography at baseline and then yearly for 2 years.
Participants were men and women age 55 to 74 with at least 30 pack-years of cigarette smoking. If they had quit smoking, they had to have quit within the past 15 years. All were followed until study conclusion (median 6.5 years, maximum 7.4). About 41% were women, and nearly three-quarters were age 55 through 64. More than 48% were current smokers, with the rest being former smokers.
Results. Adherence to screening was 95% in the CT group and 93% in the radiography group, with a 4.3% annual rate of CT outside the study during the screening phase.
Cumulative lung cancer incidence rates were 645 per 100,000 person-years in the CT group and 572 in the radiography group.
In the CT group there were a total of 1,060 lung cancers during the entire study. Of these, 649 (61%) were detected by screening, 44 (4%) were interval cancers, and the rest were diagnosed after the screening period during follow-up.
In the chest radiography group, there were a total of 941 lung cancers during the entire study. Of these, 279 (30%) were detected by screening, 137 (15%) were interval cancers, and the rest were diagnosed after the screening period. Within the CT group, the cancers detected by screening were more likely to be adenocarcinomas and less likely to be small-cell carcinomas than those not detected by screening. Also within the CT group, the cancers detected by screening were more likely to be stage I (63%) than those not detected by screening.
The cumulative number of deaths from lung cancer was 443 in the radiography group, but only 356 in the CT group—20.0% lower (P =.004). The cumulative overall mortality rate was 6.7% lower in the CT group (P = .02).
Comments. The results of the NLST provide the first evidence that lung cancer mortality rates can be reduced by screening. Though many questions remain, the conclusions of this study are that screening a well-defined high-risk group with low-dose CT reduces the rate of death from lung cancer.
REMAINING CHALLENGES
The NLST showed that lung cancer screening with low-dose CT can meet the most important criterion for a successful screening program, ie, a reduction in the disease-specific mortality rate. Many challenges remain in meeting the other criteria for a successful or ideal screening program (low risk, few false-positive results, acceptability to the patient, and affordability). The issues with low-dose CT-based screening that challenge these ideals are outlined in this section.
Lung nodules: Benign or malignant?
A meta-analysis of CT screening studies found that for every 1,000 people screened at baseline, 9 were found to have stage I non-small-cell lung cancer, 235 had false-positive nodules, and 4 underwent thoracotomy for benign lesions.6
The NLST results were similar. In this trial, only nodules that were 4 mm or greater in diameter were reported. Using these criteria, over 27% of all study participants were found to have a lung nodule on CT at baseline and at year 1. The rate fell to nearly 17% at year 2, as nodules present from baseline were not reported. Of all the lung nodules detected, only 3.6% were ultimately proven to represent lung cancer.2
Many issues with small lung nodules need to be considered. The nodules are difficult to find, with highly variable reporting even by expert radiologists.7 They are difficult to measure accurately and thus are difficult to assess for growth.8 Adjunctive imaging and nonsurgical biopsy have a low yield for small nodules.9–11 Follow-up of these lung nodules includes additional imaging and nonsurgical and surgical biopsy procedures, adding expense to the program and risk to the patient. Finally, knowing that they have a lung nodule makes patients feel anxious and thus negatively affects their quality of life.12,13
Radiation exposure: How great is the risk?
There is a great deal of concern about radiation exposure from medical imaging, as many people receive a substantial amount of radiation each year from medical testing.14 A single low-dose scan with chest CT delivers a whole-body effective dose of about 1.5 mSv—less than one-fifth of the radiation dose of a typical diagnostic CT scan.
Many have tried to estimate the consequences of radiation exposure from low-dose CT screening. All estimates are extrapolations from unrelated radiation exposures. The increase in risk of death ranged from 0.01% to a few percent,15 and the increase in cancers was as high as 1.8% over a 25-year screening period.16 In general, the risks are felt to be very low but not negligible.
Cost-effectiveness is unknown
The cost-effectiveness of lung cancer screening is also unknown. Many highly variable estimates have been published.17–20 The studies have differed in the perspective taken, the costs of testing assumed, and the rounds of screening included. The most cost-effective estimates are in populations with the highest risk of cancer, in programs that achieve the greatest reduction in mortality rate, and in programs that lead to high rates of smoking cessation.
Screening in the real world as opposed to a clinical trial may involve different risks, benefits, and costs. Compliance with screening and with nodule management algorithms may be lower outside of a study. One study suggested that those at highest risk of developing lung cancer would be the least likely to enroll in a screening program and the least likely to accept curative-intent surgery for screening-detected cancer.21
We expect that the NLST data will be analyzed for cost-effectiveness. This should provide the most accurate estimates for the group that was studied.
WE SET OUT TO DESIGN A SCREENING PROGRAM
With the evidence supporting a reduction in the rate of lung cancer mortality, and knowing the remaining challenges, we set out to provide a lung cancer screening program within Cleveland Clinic. In the design of our program, we considered several questions, outlined below.
Who should be offered low-dose CT screening?
The results of the NLST led to a great deal of excitement about lung cancer screening in both the medical community and the general public. The positive side of this publicity is that lung cancer is receiving attention that may lead to support for further advances. The negative side is that many patients who may seek out lung cancer screening are not at high enough risk of lung cancer to clearly benefit from it.
In the NLST, a very high-risk cohort was studied, as defined by clinical variables (age 55 to 74, at least 30 pack-years of smoking, and if a former smoker, had quit within the past 15 years). In this high-risk group, 320 patients needed to be screened (with three yearly chest CT scans) for one life to be saved from lung cancer, and only 3.6% of all lung nodules found (4 mm or larger) were actually lung cancer. In a group at lower risk, the number that needed to be screened to save one life would be higher, and the percentage of lung nodules that truly were lung cancer would be lower. This would lead to higher risks and costs related to screening, without a proven benefit to members of the lower-risk group.
The risk of the NLST cohort developing lung cancer was approximately 0.6% per year. Lung cancer risk-prediction models have been developed and published. Up to 2011, the three most commonly used models had only moderate accuracy at predicting risk.22–25 In 2011 a risk model based on the PLCO cohort was developed and published.26 This model seemed to be more accurate but perhaps a bit harder to apply in practice.
We discussed whether using a validated risk predictor with a target of 0.6% per year (ie, the risk in the NLST trial) would be an adequate means of deciding on candidacy for lung cancer screening or if we should strictly adhere to the inclusion criteria of the NLST cohort. We feel that the NLST cohort is the only group with true evidence of benefit (a reduction in the lung cancer-specific mortality rate). Thus, for our program’s entry criteria, we decided to use the same clinical predictors used for entry in the NLST.
How will the right patients get scheduled for low-dose screening CT?
Patients who enter the lung cancer screening program from our health system will require a physician’s order.
We are fortunate to have an electronic medical record in place. We have created an order set within the electronic record for low-dose chest CT. The order will eventually be able to be entered as “CT lung screening w/o” (ie, without contrast).
For patients from outside of our health system who would like to enter the lung cancer screening program, the entry criteria will be the same (see above). We will ask for the name of the patient’s primary care practitioner. If the patient does not have one, a member of our Respiratory Institute will see and enroll the patient.
How often should patients be screened, and for how many years?
Unfortunately, questions about the frequency of screening and how many years it should continue remain unanswered.
In the NLST, a similar number of early-stage lung cancers were detected during each of the three screening rounds. In both the NLST and PLCO trials, differences in the mortality rate curves began to narrow during the observation period, when active screening was no longer occurring. Thus, it is possible that a longer duration of screening could lead to a further reduction in mortality rates. Others have questioned whether a similar benefit, with less cost and risk, could be obtained by screening every 2 years.
The large amount of data obtained from the NLST and other CT-based studies is being reviewed so that models can be developed to help answer these questions. For now, we suggest at least three yearly CT screenings, with the hope that we will have clearer answers to these questions over time.
How will low-dose CT be performed and interpreted?
The parameters for low-dose CT were very tightly controlled and monitored during the NLST. This quality-control effort, designed to improve consistency across sites and to minimize risk to patients, should be carried into lung cancer screening programs.
Our program will closely mimic the CT performance criteria used in the NLST (tube current-time product 40 mAs for all patients, field of view lungs only, lung kernel images 3 mm at 1.5-mm intervals, and soft-tissue kernel images 5 mm at 2.5-mm intervals).27 In the initial phase of the program, all screening scans will be performed at Cleveland Clinic’s main imaging facility.
Small lung nodules remain quite challenging to detect and measure. To minimize variability in scan interpretation, the NLST readers were all expertly trained radiologists. Despite this, much variability was noted in the number of nodules detected, their measured size, and the follow-up recommendations. All of the screening CT images for our program will be interpreted by board-certified radiologists with expertise in chest imaging.
Other screening studies have included novel imaging assessment in their testing algorithms, particularly volumetric analysis of lung nodules.28 These tools may prove to assist in nodule detection, measurement, and management over time. At this point, we do not think they have been studied and standardized enough to include them in a standard-of-care screening program. We hope that they will evolve to the point of clinical utility in the near future.
Lung cancer screening is not currently covered by most insurers, including Medicare, although one major insurer has recently started to cover it. We expect decisions on coverage from other insurers in the next 12 months. In the meantime, we offer a low-dose screening chest CT to our patients for $125, which includes the radiologist’s fee for interpreting the scan.
Smoking cessation
The NLST showed that low-dose CT screening can reduce lung cancer mortality rates by 20% in a high-risk group. A 50-year-old active smoker who quits smoking reduces his or her risk of dying of lung cancer by more than 50%.29 Entry into a lung cancer screening program provides an opportunity for education and assistance with tobacco dependency.
At Cleveland Clinic, we have an active Tobacco Treatment Center within our Wellness Institute. All lung cancer screening participants who are identified as active smokers will be given a program brochure and will be offered a consult in the program.
What do we identify as a lung nodule, and how should they be managed?
Studies of CT-based screening have highlighted the tremendous number of lung nodules that are identified and the low likelihood of malignancy in those that are less than 1 cm in diameter. Many screening studies define a positive result as a lung nodule above a particular size. The NLST used 4 mm or greater as the cutoff. The lower the cutoff, the greater the number of nodules found, and the lower the overall likelihood of malignancy in the nodules.
Studies in which annual CT screening was the intervention are able to use size criteria in part because the study design ensures another CT will be performed 12 months later. Current nodule management guidelines suggest 12-month CT follow-up of incidentally discovered lung nodules, 4 mm or smaller, in at-risk patients.30 In a screening program, particularly one for which the patient must pay, the 12-month screening CT cannot be guaranteed. This makes it more difficult to ignore the smallest nodules identified on CT screening. Given this, we will be reporting all lung nodules identified, regardless of size on the initial screening.
Most studies of CT screening have reported any new nodule identified in subsequent screening rounds regardless of size. Though it is intuitive that a new nodule would have a high likelihood of malignancy in a high-risk cohort, malignancy rates have been reported to be as low as 1% for new nodules. As with the initial round of screening, we will report all new lung nodules identified in subsequent screening rounds.
The recommendations for the evaluation of lung nodules, both within the report and at the lung nodule clinic, are in keeping with currently available guidelines, such as those from the Fleischner Society30 and the American College of Chest Physicians.31 For incidentally discovered lung nodules in patients at high risk, the Fleischner Society recommendations are as follows30:
- For nodules 4 mm or smaller, follow-up in 12 months; if no growth, then no further follow-up
- For nodules 4 to 6 mm, follow-up at 6 to 12 months, then 18 to 24 months if no growth
- For nodules 6 to 8 mm, follow-up at 3 to 6 months, then 9 to 12 months, then 24 months if no growth
- For nodules 8 mm or larger, follow-up at 3, 9, and 24 months, or positron emission tomography, or biopsy, or both.
If the nodule is large enough or is deemed to be of high enough risk, adjuvant testing with diagnostic imaging, guided bronchoscopy, transthoracic needle aspiration, or minimally invasive resection will be offered. All patients with nodules believed to require biopsy will be discussed at our multidisciplinary lung cancer tumor board before biopsy.
How do we make practitioners and patients aware of the program and its indications, risks, and benefits?
Education will be the key to having lung cancer screening adopted as the standard of care, to lung cancer screening being provided within a well-designed and capable system, and to ensuring that patients have realistic expectations about screening. Articles such as this and grand rounds presentations within our health system will help provide education to our colleagues. Broader marketing campaigns will be considered in the future once demand and system capabilities are clearly identified. A patient information brochure will be provided at the time of the screening test (see the patient information sheet that accompanies this article).
How do we help to advance best practice?
As excited as we are that low-dose CT-based lung cancer screening has been proven to reduce lung cancer mortality rates, it is clear that there is a lot of room to improve the programs that are developed based on current data.
Advances in our ability to accurately predict an individual’s risk of developing lung cancer will allow us to offer screening to those it is most likely to benefit.
Advances in smoking cessation and chemoprevention will help to minimize the number of lung cancers that develop.
Advances in our ability to determine the nature of lung nodules will allow us to accelerate treatment of very early lung cancer while minimizing additional testing on benign nodules; advances in our ability to treat localized and advanced disease will improve the outcome for those identified as having lung cancer.
To help move the science of screening forward, we will develop a screening program registry that can be populated from the order set and the templated report. The registry can be used to ensure appropriate patient care, while studying relevant epidemiologic, quality, and cost-related questions.
We hope to assess novel imaging software capable of assisting with the detection and characterization of lung nodules.
We have an active biomarker development program to assess the ability of breath and blood-based biomarkers to identify those at risk of developing lung cancer; to assist with the management of screening-detected lung nodules; to assist with the diagnosis of early stage lung cancer; and to characterize the nature of the cancers identified. Accurate biomarkers could lead to further decreases in mortality rates while reducing the risks and costs of a screening program.
We have strong surgical, medical, and radiation oncology programs, actively pursuing advances in minimally invasive resection procedures and ablative and targeted therapies.
ENTERING A NEW ERA
We are entering a new era of lung cancer screening. The NLST has shown that lung cancer morality rates can be reduced through low-dose CT screening in a high-risk population. Many challenges remain, such as managing the nodules that are discovered, determining if the program is cost-effective, and minimizing radiation exposure. These need to be considered when designing a lung cancer screening program. Advances over time will help us optimize the programs that are developed.
In 2011, two papers were published that will shape the way we think about lung cancer screening for years to come.
See related patient information sheet
While the ability to screen for lung cancer is a major positive change, it also raises many thorny questions, such as who should be screened, how often should they be screened, and how should we respond when a nodule is detected.
To answer some of these questions, we will outline how Cleveland Clinic has structured its lung cancer screening program, and the rationale we used for making pragmatic patient-care decisions within this program. We will conclude with our thoughts about the potential evolution of lung cancer screening programs.
THE 40-YEAR QUEST FOR EFFECTIVE LUNG CANCER SCREENING
Lung cancer kills more people in the United States than the next four most lethal types of cancer combined.3 It is curable if found early in its course. Unfortunately, most people who develop lung cancer feel no symptoms when it is early in its course, and therefore it is too often diagnosed at a late stage. Treatment for late-stage lung cancer is effective, but it is rarely curative.
Screening refers to testing people at risk of developing a disease before its symptoms or signs have appeared. The goal of screening is to reduce the disease-specific mortality rate. For this to happen, the disease must be detectable in a preclinical form, and treatment must be more successful when applied early. Ideally, the screening test should pose little risk to the patient, be sensitive for detecting the disease early in its course, give few false-positive results, be acceptable to the patient, and be relatively inexpensive to the health system.
Over the past 4 decades, a large volume of research has been done in the hope of proving that conventional radiography or CT could be an effective screening test for lung cancer.4,5
Cohort studies (ie, in which all the patients were screened) of radiography or CT have shown a longer survival from the time of lung cancer diagnosis than would be expected without screening. These studies were not designed to prove a reduction in the lung cancer-specific mortality rate.
Controlled trials (in which half the patients received the screening and the other half did not) of chest radiography have been interpreted as not showing a reduction in lung cancer mortality rates, though debate about the interpretation of these trials persisted until this past year. Biases inherent in using duration of survival rather than the mortality rate as an end point have been suggested as the reason for the apparent benefit in survival without a reduction in the mortality rate.
Controlled trials of CT screening were started nearly a decade ago. Until 2011, the results of these trials were not mature enough to comment on.
THE PROSTATE, LUNG, COLORECTAL, AND OVARIAN TRIAL
The lung cancer screening portion of the PLCO trial aimed to determine the effect of screening chest radiography on lung cancer-specific mortality rates.1
In this trial, 154,901 people were randomized to undergo either posteroanterior chest radiography every year for 4 years or usual care, ie, no lung cancer screening. Participants were men and women age 55 to 74 with no history of prostate, lung, colorectal, or ovarian cancer. They did not need to be a smoker to participate. Those who had never smoked and who were randomized to the screening group received only 3 years of testing. All were followed for 13 years or until the conclusion of the study (8 years after the final participant was enrolled). About half were women, and nearly two-thirds were age 55 through 64. Only 10% were current smokers, while a full 45% had never smoked.
Results. Adherence to screening in the screening group ranged from 79% to 86.6% over the years of screening, and 11% of the usual-care group was estimated to have undergone screening chest radiography.
Cumulative lung cancer incidence rates were 201 per 100,000 person-years in the screening group and 192 in the usual-care group.
In the screening group, there were a total of 1,696 lung cancers during the entire study. Of these, 307 (18%) were detected by screening, 198 (12%) were interval cancers (diagnosed during the screening period but not by the screening test), and the remainder were diagnosed after the screening period during the years of follow-up. In the screening group, the cancers detected by screening were more likely to be adenocarcinomas and less likely to be small-cell carcinomas than those not detected by screening. Also in the screening group, the cancers detected by screening were more likely to be stage I (50%) than those not detected by screening.
The cumulative number of deaths from lung cancer was slightly but not significantly lower in the screening group from years 4 through 11. However, by the end of follow-up, the number of lung cancer deaths was equal between the groups (1,213 in the screening group vs 1,230 in the usual-care group). The cumulative overall mortality rate was also similar between the groups. For the subgroup who would have qualified for the NLST (see below), the lung cancer mortality rate was statistically similar between the two groups.
Comments. The results of the PLCO screening trial will be interpreted as the final word in lung cancer screening with standard chest radiography. The conclusion is that annual screening with chest radiography does not reduce lung cancer mortality rates and thus should not be performed in this context.
THE NATIONAL LUNG SCREENING TRIAL
The NLST aimed to determine if screening with low-dose chest CT could reduce lung cancer mortality rates.2
This controlled trial enrolled 53,454 people, who were randomized to undergo either low-dose chest CT or posteroanterior chest radiography at baseline and then yearly for 2 years.
Participants were men and women age 55 to 74 with at least 30 pack-years of cigarette smoking. If they had quit smoking, they had to have quit within the past 15 years. All were followed until study conclusion (median 6.5 years, maximum 7.4). About 41% were women, and nearly three-quarters were age 55 through 64. More than 48% were current smokers, with the rest being former smokers.
Results. Adherence to screening was 95% in the CT group and 93% in the radiography group, with a 4.3% annual rate of CT outside the study during the screening phase.
Cumulative lung cancer incidence rates were 645 per 100,000 person-years in the CT group and 572 in the radiography group.
In the CT group there were a total of 1,060 lung cancers during the entire study. Of these, 649 (61%) were detected by screening, 44 (4%) were interval cancers, and the rest were diagnosed after the screening period during follow-up.
In the chest radiography group, there were a total of 941 lung cancers during the entire study. Of these, 279 (30%) were detected by screening, 137 (15%) were interval cancers, and the rest were diagnosed after the screening period. Within the CT group, the cancers detected by screening were more likely to be adenocarcinomas and less likely to be small-cell carcinomas than those not detected by screening. Also within the CT group, the cancers detected by screening were more likely to be stage I (63%) than those not detected by screening.
The cumulative number of deaths from lung cancer was 443 in the radiography group, but only 356 in the CT group—20.0% lower (P =.004). The cumulative overall mortality rate was 6.7% lower in the CT group (P = .02).
Comments. The results of the NLST provide the first evidence that lung cancer mortality rates can be reduced by screening. Though many questions remain, the conclusions of this study are that screening a well-defined high-risk group with low-dose CT reduces the rate of death from lung cancer.
REMAINING CHALLENGES
The NLST showed that lung cancer screening with low-dose CT can meet the most important criterion for a successful screening program, ie, a reduction in the disease-specific mortality rate. Many challenges remain in meeting the other criteria for a successful or ideal screening program (low risk, few false-positive results, acceptability to the patient, and affordability). The issues with low-dose CT-based screening that challenge these ideals are outlined in this section.
Lung nodules: Benign or malignant?
A meta-analysis of CT screening studies found that for every 1,000 people screened at baseline, 9 were found to have stage I non-small-cell lung cancer, 235 had false-positive nodules, and 4 underwent thoracotomy for benign lesions.6
The NLST results were similar. In this trial, only nodules that were 4 mm or greater in diameter were reported. Using these criteria, over 27% of all study participants were found to have a lung nodule on CT at baseline and at year 1. The rate fell to nearly 17% at year 2, as nodules present from baseline were not reported. Of all the lung nodules detected, only 3.6% were ultimately proven to represent lung cancer.2
Many issues with small lung nodules need to be considered. The nodules are difficult to find, with highly variable reporting even by expert radiologists.7 They are difficult to measure accurately and thus are difficult to assess for growth.8 Adjunctive imaging and nonsurgical biopsy have a low yield for small nodules.9–11 Follow-up of these lung nodules includes additional imaging and nonsurgical and surgical biopsy procedures, adding expense to the program and risk to the patient. Finally, knowing that they have a lung nodule makes patients feel anxious and thus negatively affects their quality of life.12,13
Radiation exposure: How great is the risk?
There is a great deal of concern about radiation exposure from medical imaging, as many people receive a substantial amount of radiation each year from medical testing.14 A single low-dose scan with chest CT delivers a whole-body effective dose of about 1.5 mSv—less than one-fifth of the radiation dose of a typical diagnostic CT scan.
Many have tried to estimate the consequences of radiation exposure from low-dose CT screening. All estimates are extrapolations from unrelated radiation exposures. The increase in risk of death ranged from 0.01% to a few percent,15 and the increase in cancers was as high as 1.8% over a 25-year screening period.16 In general, the risks are felt to be very low but not negligible.
Cost-effectiveness is unknown
The cost-effectiveness of lung cancer screening is also unknown. Many highly variable estimates have been published.17–20 The studies have differed in the perspective taken, the costs of testing assumed, and the rounds of screening included. The most cost-effective estimates are in populations with the highest risk of cancer, in programs that achieve the greatest reduction in mortality rate, and in programs that lead to high rates of smoking cessation.
Screening in the real world as opposed to a clinical trial may involve different risks, benefits, and costs. Compliance with screening and with nodule management algorithms may be lower outside of a study. One study suggested that those at highest risk of developing lung cancer would be the least likely to enroll in a screening program and the least likely to accept curative-intent surgery for screening-detected cancer.21
We expect that the NLST data will be analyzed for cost-effectiveness. This should provide the most accurate estimates for the group that was studied.
WE SET OUT TO DESIGN A SCREENING PROGRAM
With the evidence supporting a reduction in the rate of lung cancer mortality, and knowing the remaining challenges, we set out to provide a lung cancer screening program within Cleveland Clinic. In the design of our program, we considered several questions, outlined below.
Who should be offered low-dose CT screening?
The results of the NLST led to a great deal of excitement about lung cancer screening in both the medical community and the general public. The positive side of this publicity is that lung cancer is receiving attention that may lead to support for further advances. The negative side is that many patients who may seek out lung cancer screening are not at high enough risk of lung cancer to clearly benefit from it.
In the NLST, a very high-risk cohort was studied, as defined by clinical variables (age 55 to 74, at least 30 pack-years of smoking, and if a former smoker, had quit within the past 15 years). In this high-risk group, 320 patients needed to be screened (with three yearly chest CT scans) for one life to be saved from lung cancer, and only 3.6% of all lung nodules found (4 mm or larger) were actually lung cancer. In a group at lower risk, the number that needed to be screened to save one life would be higher, and the percentage of lung nodules that truly were lung cancer would be lower. This would lead to higher risks and costs related to screening, without a proven benefit to members of the lower-risk group.
The risk of the NLST cohort developing lung cancer was approximately 0.6% per year. Lung cancer risk-prediction models have been developed and published. Up to 2011, the three most commonly used models had only moderate accuracy at predicting risk.22–25 In 2011 a risk model based on the PLCO cohort was developed and published.26 This model seemed to be more accurate but perhaps a bit harder to apply in practice.
We discussed whether using a validated risk predictor with a target of 0.6% per year (ie, the risk in the NLST trial) would be an adequate means of deciding on candidacy for lung cancer screening or if we should strictly adhere to the inclusion criteria of the NLST cohort. We feel that the NLST cohort is the only group with true evidence of benefit (a reduction in the lung cancer-specific mortality rate). Thus, for our program’s entry criteria, we decided to use the same clinical predictors used for entry in the NLST.
How will the right patients get scheduled for low-dose screening CT?
Patients who enter the lung cancer screening program from our health system will require a physician’s order.
We are fortunate to have an electronic medical record in place. We have created an order set within the electronic record for low-dose chest CT. The order will eventually be able to be entered as “CT lung screening w/o” (ie, without contrast).
For patients from outside of our health system who would like to enter the lung cancer screening program, the entry criteria will be the same (see above). We will ask for the name of the patient’s primary care practitioner. If the patient does not have one, a member of our Respiratory Institute will see and enroll the patient.
How often should patients be screened, and for how many years?
Unfortunately, questions about the frequency of screening and how many years it should continue remain unanswered.
In the NLST, a similar number of early-stage lung cancers were detected during each of the three screening rounds. In both the NLST and PLCO trials, differences in the mortality rate curves began to narrow during the observation period, when active screening was no longer occurring. Thus, it is possible that a longer duration of screening could lead to a further reduction in mortality rates. Others have questioned whether a similar benefit, with less cost and risk, could be obtained by screening every 2 years.
The large amount of data obtained from the NLST and other CT-based studies is being reviewed so that models can be developed to help answer these questions. For now, we suggest at least three yearly CT screenings, with the hope that we will have clearer answers to these questions over time.
How will low-dose CT be performed and interpreted?
The parameters for low-dose CT were very tightly controlled and monitored during the NLST. This quality-control effort, designed to improve consistency across sites and to minimize risk to patients, should be carried into lung cancer screening programs.
Our program will closely mimic the CT performance criteria used in the NLST (tube current-time product 40 mAs for all patients, field of view lungs only, lung kernel images 3 mm at 1.5-mm intervals, and soft-tissue kernel images 5 mm at 2.5-mm intervals).27 In the initial phase of the program, all screening scans will be performed at Cleveland Clinic’s main imaging facility.
Small lung nodules remain quite challenging to detect and measure. To minimize variability in scan interpretation, the NLST readers were all expertly trained radiologists. Despite this, much variability was noted in the number of nodules detected, their measured size, and the follow-up recommendations. All of the screening CT images for our program will be interpreted by board-certified radiologists with expertise in chest imaging.
Other screening studies have included novel imaging assessment in their testing algorithms, particularly volumetric analysis of lung nodules.28 These tools may prove to assist in nodule detection, measurement, and management over time. At this point, we do not think they have been studied and standardized enough to include them in a standard-of-care screening program. We hope that they will evolve to the point of clinical utility in the near future.
Lung cancer screening is not currently covered by most insurers, including Medicare, although one major insurer has recently started to cover it. We expect decisions on coverage from other insurers in the next 12 months. In the meantime, we offer a low-dose screening chest CT to our patients for $125, which includes the radiologist’s fee for interpreting the scan.
Smoking cessation
The NLST showed that low-dose CT screening can reduce lung cancer mortality rates by 20% in a high-risk group. A 50-year-old active smoker who quits smoking reduces his or her risk of dying of lung cancer by more than 50%.29 Entry into a lung cancer screening program provides an opportunity for education and assistance with tobacco dependency.
At Cleveland Clinic, we have an active Tobacco Treatment Center within our Wellness Institute. All lung cancer screening participants who are identified as active smokers will be given a program brochure and will be offered a consult in the program.
What do we identify as a lung nodule, and how should they be managed?
Studies of CT-based screening have highlighted the tremendous number of lung nodules that are identified and the low likelihood of malignancy in those that are less than 1 cm in diameter. Many screening studies define a positive result as a lung nodule above a particular size. The NLST used 4 mm or greater as the cutoff. The lower the cutoff, the greater the number of nodules found, and the lower the overall likelihood of malignancy in the nodules.
Studies in which annual CT screening was the intervention are able to use size criteria in part because the study design ensures another CT will be performed 12 months later. Current nodule management guidelines suggest 12-month CT follow-up of incidentally discovered lung nodules, 4 mm or smaller, in at-risk patients.30 In a screening program, particularly one for which the patient must pay, the 12-month screening CT cannot be guaranteed. This makes it more difficult to ignore the smallest nodules identified on CT screening. Given this, we will be reporting all lung nodules identified, regardless of size on the initial screening.
Most studies of CT screening have reported any new nodule identified in subsequent screening rounds regardless of size. Though it is intuitive that a new nodule would have a high likelihood of malignancy in a high-risk cohort, malignancy rates have been reported to be as low as 1% for new nodules. As with the initial round of screening, we will report all new lung nodules identified in subsequent screening rounds.
The recommendations for the evaluation of lung nodules, both within the report and at the lung nodule clinic, are in keeping with currently available guidelines, such as those from the Fleischner Society30 and the American College of Chest Physicians.31 For incidentally discovered lung nodules in patients at high risk, the Fleischner Society recommendations are as follows30:
- For nodules 4 mm or smaller, follow-up in 12 months; if no growth, then no further follow-up
- For nodules 4 to 6 mm, follow-up at 6 to 12 months, then 18 to 24 months if no growth
- For nodules 6 to 8 mm, follow-up at 3 to 6 months, then 9 to 12 months, then 24 months if no growth
- For nodules 8 mm or larger, follow-up at 3, 9, and 24 months, or positron emission tomography, or biopsy, or both.
If the nodule is large enough or is deemed to be of high enough risk, adjuvant testing with diagnostic imaging, guided bronchoscopy, transthoracic needle aspiration, or minimally invasive resection will be offered. All patients with nodules believed to require biopsy will be discussed at our multidisciplinary lung cancer tumor board before biopsy.
How do we make practitioners and patients aware of the program and its indications, risks, and benefits?
Education will be the key to having lung cancer screening adopted as the standard of care, to lung cancer screening being provided within a well-designed and capable system, and to ensuring that patients have realistic expectations about screening. Articles such as this and grand rounds presentations within our health system will help provide education to our colleagues. Broader marketing campaigns will be considered in the future once demand and system capabilities are clearly identified. A patient information brochure will be provided at the time of the screening test (see the patient information sheet that accompanies this article).
How do we help to advance best practice?
As excited as we are that low-dose CT-based lung cancer screening has been proven to reduce lung cancer mortality rates, it is clear that there is a lot of room to improve the programs that are developed based on current data.
Advances in our ability to accurately predict an individual’s risk of developing lung cancer will allow us to offer screening to those it is most likely to benefit.
Advances in smoking cessation and chemoprevention will help to minimize the number of lung cancers that develop.
Advances in our ability to determine the nature of lung nodules will allow us to accelerate treatment of very early lung cancer while minimizing additional testing on benign nodules; advances in our ability to treat localized and advanced disease will improve the outcome for those identified as having lung cancer.
To help move the science of screening forward, we will develop a screening program registry that can be populated from the order set and the templated report. The registry can be used to ensure appropriate patient care, while studying relevant epidemiologic, quality, and cost-related questions.
We hope to assess novel imaging software capable of assisting with the detection and characterization of lung nodules.
We have an active biomarker development program to assess the ability of breath and blood-based biomarkers to identify those at risk of developing lung cancer; to assist with the management of screening-detected lung nodules; to assist with the diagnosis of early stage lung cancer; and to characterize the nature of the cancers identified. Accurate biomarkers could lead to further decreases in mortality rates while reducing the risks and costs of a screening program.
We have strong surgical, medical, and radiation oncology programs, actively pursuing advances in minimally invasive resection procedures and ablative and targeted therapies.
ENTERING A NEW ERA
We are entering a new era of lung cancer screening. The NLST has shown that lung cancer morality rates can be reduced through low-dose CT screening in a high-risk population. Many challenges remain, such as managing the nodules that are discovered, determining if the program is cost-effective, and minimizing radiation exposure. These need to be considered when designing a lung cancer screening program. Advances over time will help us optimize the programs that are developed.
- Oken MM, Hocking WG, Kvale PA, et al; PLCO Project Team. Screening by chest radiograph and lung cancer mortality: the Prostate, Lung, Colorectal, and Ovarian (PLCO) randomized trial. JAMA 2011; 306:1865–1873.
- National Lung Screening Trial Research Team; Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011; 365:395–409.
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin 2012; 62:10–29.
- Mazzone PJ, Mekhail T. Lung cancer screening. Curr Oncol Rep 2007; 9:265–274.
- Mazzone PJ. Lung cancer screening: an update, discussion, and look ahead. Curr Oncol Rep 2010; 12:226–234.
- Gopal M, Abdullah SE, Grady JJ, Goodwin JS. Screening for lung cancer with low-dose computed tomography: a systematic review and meta-analysis of the baseline findings of randomized controlled trials. J Thorac Oncol 2010; 5:1233–1239.
- Gierada DS, Pilgram TK, Ford M, et al. Lung cancer: interobserver agreement on interpretation of pulmonary findings at low-dose CT screening. Radiology 2008; 246:265–272.
- Singh S, Pinsky P, Fineberg NS, et al. Evaluation of reader variability in the interpretation of follow-up CT scans at lung cancer screening. Radiology 2011; 259:263–270.
- Lindell RM, Hartman TE, Swensen SJ, et al. Lung cancer screening experience: a retrospective review of PET in 22 non-small cell lung carcinomas detected on screening chest CT in a high-risk population. AJR Am J Roentgenol 2005; 185:126–131.
- Baaklini WA, Reinoso MA, Gorin AB, Sharafkaneh A, Manian P. Diagnostic yield of fiberoptic bronchoscopy in evaluating solitary pulmonary nodules. Chest 2000; 117:1049–1054.
- Kothary N, Lock L, Sze DY, Hofmann LV. Computed tomography-guided percutaneous needle biopsy of pulmonary nodules: impact of nodule size on diagnostic accuracy. Clin Lung Cancer 2009; 10:360–363.
- van den Bergh KA, Essink-Bot ML, Borsboom GJ, et al. Short-term health-related quality of life consequences in a lung cancer CT screening trial (NELSON). Br J Cancer 2010; 102:27–34.
- Lemonnier I, Baumann C, Jolly D, et al. Solitary pulmonary nodules: consequences for patient quality of life. Qual Life Res 2011; 20:101–109.
- Fazel R, Krumholz HM, Wang Y, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 2009; 361:849–857.
- Buls N, de Mey J, Covens P, Stadnik T. Health screening with CT: prospective assessment of radiation dose and associated detriment. JBR-BTR 2005; 88:12–16.
- Brenner DJ. Radiation risks potentially associated with low-dose CT screening of adult smokers for lung cancer. Radiology 2004; 231:440–445.
- Mahadevia PJ, Fleisher LA, Frick KD, Eng J, Goodman SN, Powe NR. Lung cancer screening with helical computed tomography in older adult smokers: a decision and cost-effectiveness analysis. JAMA 2003; 289:313–322.
- Wisnivesky JP, Mushlin AI, Sicherman N, Henschke C. The cost-effectiveness of low-dose CT screening for lung cancer: preliminary results of baseline screening. Chest 2003; 124:614–621.
- Manser R, Dalton A, Carter R, Byrnes G, Elwood M, Campbell DA. Cost-effectiveness analysis of screening for lung cancer with low dose spiral CT (computed tomography) in the Australian setting. Lung Cancer 2005; 48:171–185.
- McMahon PM, Kong CY, Bouzan C, et al. Cost-effectiveness of computed tomography screening for lung cancer in the United States. J Thorac Oncol 2011; 6:1841–1848.
- Silvestri GA, Nietert PJ, Zoller J, Carter C, Bradford D. Attitudes towards screening for lung cancer among smokers and their nonsmoking counterparts. Thorax 2007; 62:126–130.
- Bach PB, Kattan MW, Thornquist MD, et al. Variations in lung cancer risk among smokers. J Natl Cancer Inst 2003; 95:470–478.
- Spitz MR, Hong WK, Amos CI, et al. A risk model for prediction of lung cancer. J Natl Cancer Inst 2007; 99:715–726.
- Cassidy A, Myles JP, van Tongeren M, et al. The LLP risk model: an individual risk prediction model for lung cancer. Br J Cancer 2008; 98:270–276.
- D’Amelio AM, Cassidy A, Asomaning K, et al. Comparison of discriminatory power and accuracy of three lung cancer risk models. Br J Cancer 2010; 103:423–429.
- Tammemagi CM, Pinsky PF, Caporaso NE, et al. Lung cancer risk prediction: Prostate, Lung, Colorectal And Ovarian Cancer Screening Trial models and validation. J Natl Cancer Inst 2011; 103:1058–1068.
- National Lung Screening Trial Research Team; Aberle DR, Berg CD, Black WC, et al. The National Lung Screening Trial: overview and study design. Radiology 2011; 258:243–253.
- van Klaveren RJ, Oudkerk M, Prokop M, et al. Management of lung nodules detected by volume CT scanning. N Engl J Med 2009; 361:2221–2229.
- Peto R, Darby S, Deo H, Silcocks P, Whitley E, Doll R. Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies. BMJ 2000; 321:323–329.
- MacMahon H, Austin JH, Gamsu G, et al; Fleischner Society. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology 2005; 237:395–400.
- Gould MK, Fletcher J, Iannettoni MD, et al; American College of Chest Physicians. Evaluation of patients with pulmonary nodules: when is it lung cancer?: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007; 132(suppl 3):108S–130S.
- Oken MM, Hocking WG, Kvale PA, et al; PLCO Project Team. Screening by chest radiograph and lung cancer mortality: the Prostate, Lung, Colorectal, and Ovarian (PLCO) randomized trial. JAMA 2011; 306:1865–1873.
- National Lung Screening Trial Research Team; Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011; 365:395–409.
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin 2012; 62:10–29.
- Mazzone PJ, Mekhail T. Lung cancer screening. Curr Oncol Rep 2007; 9:265–274.
- Mazzone PJ. Lung cancer screening: an update, discussion, and look ahead. Curr Oncol Rep 2010; 12:226–234.
- Gopal M, Abdullah SE, Grady JJ, Goodwin JS. Screening for lung cancer with low-dose computed tomography: a systematic review and meta-analysis of the baseline findings of randomized controlled trials. J Thorac Oncol 2010; 5:1233–1239.
- Gierada DS, Pilgram TK, Ford M, et al. Lung cancer: interobserver agreement on interpretation of pulmonary findings at low-dose CT screening. Radiology 2008; 246:265–272.
- Singh S, Pinsky P, Fineberg NS, et al. Evaluation of reader variability in the interpretation of follow-up CT scans at lung cancer screening. Radiology 2011; 259:263–270.
- Lindell RM, Hartman TE, Swensen SJ, et al. Lung cancer screening experience: a retrospective review of PET in 22 non-small cell lung carcinomas detected on screening chest CT in a high-risk population. AJR Am J Roentgenol 2005; 185:126–131.
- Baaklini WA, Reinoso MA, Gorin AB, Sharafkaneh A, Manian P. Diagnostic yield of fiberoptic bronchoscopy in evaluating solitary pulmonary nodules. Chest 2000; 117:1049–1054.
- Kothary N, Lock L, Sze DY, Hofmann LV. Computed tomography-guided percutaneous needle biopsy of pulmonary nodules: impact of nodule size on diagnostic accuracy. Clin Lung Cancer 2009; 10:360–363.
- van den Bergh KA, Essink-Bot ML, Borsboom GJ, et al. Short-term health-related quality of life consequences in a lung cancer CT screening trial (NELSON). Br J Cancer 2010; 102:27–34.
- Lemonnier I, Baumann C, Jolly D, et al. Solitary pulmonary nodules: consequences for patient quality of life. Qual Life Res 2011; 20:101–109.
- Fazel R, Krumholz HM, Wang Y, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 2009; 361:849–857.
- Buls N, de Mey J, Covens P, Stadnik T. Health screening with CT: prospective assessment of radiation dose and associated detriment. JBR-BTR 2005; 88:12–16.
- Brenner DJ. Radiation risks potentially associated with low-dose CT screening of adult smokers for lung cancer. Radiology 2004; 231:440–445.
- Mahadevia PJ, Fleisher LA, Frick KD, Eng J, Goodman SN, Powe NR. Lung cancer screening with helical computed tomography in older adult smokers: a decision and cost-effectiveness analysis. JAMA 2003; 289:313–322.
- Wisnivesky JP, Mushlin AI, Sicherman N, Henschke C. The cost-effectiveness of low-dose CT screening for lung cancer: preliminary results of baseline screening. Chest 2003; 124:614–621.
- Manser R, Dalton A, Carter R, Byrnes G, Elwood M, Campbell DA. Cost-effectiveness analysis of screening for lung cancer with low dose spiral CT (computed tomography) in the Australian setting. Lung Cancer 2005; 48:171–185.
- McMahon PM, Kong CY, Bouzan C, et al. Cost-effectiveness of computed tomography screening for lung cancer in the United States. J Thorac Oncol 2011; 6:1841–1848.
- Silvestri GA, Nietert PJ, Zoller J, Carter C, Bradford D. Attitudes towards screening for lung cancer among smokers and their nonsmoking counterparts. Thorax 2007; 62:126–130.
- Bach PB, Kattan MW, Thornquist MD, et al. Variations in lung cancer risk among smokers. J Natl Cancer Inst 2003; 95:470–478.
- Spitz MR, Hong WK, Amos CI, et al. A risk model for prediction of lung cancer. J Natl Cancer Inst 2007; 99:715–726.
- Cassidy A, Myles JP, van Tongeren M, et al. The LLP risk model: an individual risk prediction model for lung cancer. Br J Cancer 2008; 98:270–276.
- D’Amelio AM, Cassidy A, Asomaning K, et al. Comparison of discriminatory power and accuracy of three lung cancer risk models. Br J Cancer 2010; 103:423–429.
- Tammemagi CM, Pinsky PF, Caporaso NE, et al. Lung cancer risk prediction: Prostate, Lung, Colorectal And Ovarian Cancer Screening Trial models and validation. J Natl Cancer Inst 2011; 103:1058–1068.
- National Lung Screening Trial Research Team; Aberle DR, Berg CD, Black WC, et al. The National Lung Screening Trial: overview and study design. Radiology 2011; 258:243–253.
- van Klaveren RJ, Oudkerk M, Prokop M, et al. Management of lung nodules detected by volume CT scanning. N Engl J Med 2009; 361:2221–2229.
- Peto R, Darby S, Deo H, Silcocks P, Whitley E, Doll R. Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies. BMJ 2000; 321:323–329.
- MacMahon H, Austin JH, Gamsu G, et al; Fleischner Society. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology 2005; 237:395–400.
- Gould MK, Fletcher J, Iannettoni MD, et al; American College of Chest Physicians. Evaluation of patients with pulmonary nodules: when is it lung cancer?: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007; 132(suppl 3):108S–130S.
KEY POINTS
- The NLST documented a 20% reduction in the rate of death from lung cancer with low-dose CT screening compared with chest radiography screening (number needed to treat = 320). This was in a population at high risk (age 55–74 with a smoking history of at least 30 pack-years, at least some of it within the past 15 years).
- CT screening detects many lung nodules, of which only a few (3.6% in the NLST) prove to be cancer.
- In view of the positive results of the NLST, Cleveland Clinic has begun a lung cancer screening program, using the same entry criteria as those in the NLST.
- Of possibly greater impact than detecting lung cancer will be the opportunity to promote smoking cessation.
Lay midwives and the ObGyn: Is collaboration risky?
“We have indeed in America medical practitioners not inferior to the best elsewhere; but there is probably no other country in the world in which there is so great a distance and so fatal a difference between the best, the average, and the worst.”
—Flexner report from 19101
ObGyn is a risky specialty, with no guarantee of a perfect outcome, even with the best education, training, and skills. Does collaboration make it riskier? Or can collaboration help you deliver high-quality care to your patients?
This article explores these questions as they relate to provision of health care in collaboration with midwives—specifically, certified nurse midwives (CNMs), who are approved by the American Midwifery Certification Board, and certified professional midwives (CPMs), who are not. (See thebox for a more detailed discussion of different types of midwives in practice today.)
Got acronym fatigue? Here’s a rundown of the various credentials and certifying organizations.
The American College of Nurse-Midwives (ACNM) is a professional organization established in 1955 for certified nurse midwives and certified midwives. ACNM sets standards for academic preparation and clinical practice. For more information, visit http://www.midwife.org.
The American Midwifery Certification Board (AMCB) is the certification organization affiliated with ACNM. This board was formerly called the ACNM Certification Council (ACC). Certification by AMCB is equivalent to certification by ACC.
In 1997, AMCB opened its national certification exam to non-nurse graduates of midwifery education programs and issued the first certified midwife credential. Since 2010, a graduate degree has been required for entry into clinical practice for both certified nurse midwives and certified midwives. http://www.amcbmidwife.org
Certified midwife (CM). In 1996, the ACNM adopted standards for the certification of direct-entry midwives. These midwives undergo the same certification process as certified nurse midwives, but their training does not include education in nursing. CMs must pass the same certification exam as CNMs and must have a master’s degree.
CMs are licensed in only three states: New Jersey, New York, and Rhode Island. New York had the first CM training program and was the first state to recognize the CM credential. It is the only state that has one unified framework for licensing all midwives—both CNMs and CMs.
Certified nurse midwife (CNM). A midwife who has training in both nursing and midwifery. A master’s degree is required for certification. These midwives typically have prescriptive authority for most drugs; are eligible for third-party reimbursement, including Medicaid; and practice independently or in collaborative practice with physicians.
Certified professional midwife (CPM). In the mid 1990s, the CPM credential was developed jointly by the Midwives Alliance of North America (MANA), the North American Registry of Midwives (NARM), and the Midwifery Education Accreditation Council (MEAC). There is no single standard for education; both apprentice-only–trained midwives and midwives who undergo university-affiliated training use the title CPM.
A CPM can learn through a structured program, through apprenticeship, or through self-study. Another route to the credential is current legal recognition to practice in the United Kingdom. CPMs must pass a written and practical exam for certification.
According to MANA, 24 states recognize the CPM credential as the basis for licensure or use the NARM written exam. Some of these states use a different nomenclature. For example, licensed midwife (LM) is used in California, Idaho, Oregon, and Washington; licensed direct-entry midwife (LDM) is used in Utah; and registered midwife (RM) is used in Colorado.
SOURCE: ACOG10
Moving away from a physician-oriented system
Like it or not, change is under way. Subtle but important shifts are taking place in the way maternity care is provided in your community.
The challenges facing our specialty? Ensuring that the highest levels of patient safety and quality care are maintained. And educating federal and state lawmakers, insurers, and the public accordingly.
Free-standing birth centers are gaining prominence
The Patient Protection and Affordable Care Act (ACA) establishes alternative pathways for maternity care. Congress, state lawmakers, and insurers want to know: Can access to quality maternity care be provided at lower cost outside of hospitals or by nonphysicians? The answer isn’t clear.
Under the ACA, free-standing birth centers are a Medicaid maternity-care choice for low-income women. Birth centers appeal to lawmakers and insurers because of their lower cost. For example, in 2008, the average facility cost for a vaginal delivery in a hospital, with no complications and no newborn charges, was $8,920. In 2010, the average facility cost for a similar delivery at a birth center was $2,277.2,3
We know that dollars alone don’t tell the full story—but they’re easy listening to lawmakers’ ears.
Since 2010, Medicaid payments are allowed to go to state-licensed, free-standing birth centers even if they are not operated by or under the supervision of a physician. Before the ACA became law, Medicaid paid only for services provided in ambulatory centers under the supervision or oversight of a physician.
Another important change: Medicaid now reimburses for the services of any provider who practices in a state-licensed, free-standing birth center as long as that provider is practicing within the state’s scope of practice laws and regulations. That means that if a state allows doulas or lay midwives to provide childbirth care in free-standing birth centers, the federal and state Medicaid programs will pay for this care. This policy is consistent with “any willing provider” rules found elsewhere in Medicaid.
There are 215 birth centers in the United States, with more in development. The number of birth centers has increased more than 20% over the past 5 years; they are regulated in 41 states.4
ACOG’s Guidelines for Perinatal Care asserts: “The hospital, including a birthing center within a hospital complex, or free-standing birthing centers that meet the standards of the Accreditation Association of Birth Centers, provide the safest setting for labor, delivery, and the postpartum period.”5
Reimbursements for nonphysicians are increasing
Beginning in 2011, the Medicare program began reimbursing CNMs, the most highly trained midwives, at 100% of the physician payment rate for obstetric services. Until 2011, CNMs were paid at 65% of the physician’s rate for the same billed services.
In addition, from 2011 through 2015, CNMs whose primary care services account for at least 60% of their Medicare-allowed charges will receive Medicare bonus payments of 10%, reflecting Congress’ concern that our nation faces a serious shortage of primary care providers.
Another important provision goes into effect in 2014: All health plans offered in a state insurance exchange must accept and pay any provider recognized under state law for services covered by that plan. CPMs, some of whom are among the least highly trained providers, are licensed to provide maternity care in 24 states. This provision may put pressure on health insurers to pay for maternity care provided by CPMs, regardless of their training and certification, even if the insurer doesn’t contract with these providers.
“Even a normal pregnancy can become high-risk”
In 2008, the Massachusetts legislature debated expanding childbirth care to encompass less highly trained providers. ACOG President Kenneth L. Noller, MD, MS, cautioned them about the move, saying: “Even a normal pregnancy can become high-risk with little or no warning, and serious, sometimes life-threatening complications may arise for the woman and her fetus.”
He noted that shoulder dystocia occurs in one in every 200 births and listed the frequency of other complications:
- prolapsed umbilical cord: 1 in every 200 births
- life-threatening maternal hemorrhage: 1 in 250
- eclamptic seizures: 1 in 500
- uterine inversion: 1 in 700
- Apgar score of 0–3 at 5 minutes: 1 in 100 to 200.
Three years later, ACOG President Richard A. Waldman, MD, and American College of Nurse Midwives (ACNM) President Holly Powell Kennedy, CNM, PhD, wrote: “Collaborative practice [is] the provision of health care by an interdisciplinary team of professionals who collaborate to accomplish a common goal, and is associated with increased efficiency, improved clinical outcomes, and enhanced provider satisfaction.”5
These messages demonstrate the importance of careful use of collaboration to manage risk and maintain the highest standards of patient care. The questions for ObGyns who are considering collaborative practice:
- What is careful use?
- How do you collaborate carefully, without increasing the risks faced by your patients and your practice?
- How do you make collaboration a success?
- ACOG has taken on these questions and offers sound practical advice.

ACOG recommends high standards and clear practice agreements
ObGyns have a long history of collaboration with our nurse-midwife colleagues—possibly one of the strongest collaborative traditions in medicine. ACOG supports the practice and licensure of trained midwives credentialed by the ACNM. CNMs are well-educated, highly trained, and well-integrated into the health-care system.
In addition to the ACNM standards, ACOG supports the “global standards for midwifery education” established by the International Confederation of Midwives (ICM) in 2010:
- The minimum entry level of students is completion of secondary education
- The minimum length of a direct-entry midwifery education program is 3 years
- The minimum length of a post-nursing/health-care provider program is 18 months
- Standards are congruent with current core ICM documents and position statements.
ACOG strongly encourages that in no case should the professional standards of any maternity provider be less than the standards established or accepted by ACOG or the ACNM.
Effective collaboration depends on clear practice agreements between physicians and CNMs, consistent use of shared practice guidelines, and malpractice insurance coverage of all parties. A collaborative agreement that clearly spells out the mechanism for consultation, collaboration, and referral is essential to assure the best care.
The picture gets a little trickier—and riskier—when we look at less-trained maternity providers.
A majority of CPMs lack adequate training
Few of the nation’s 1,400 CPMs in practice today meet the educational and training standards accepted by ACOG and the ACNM. The educational background of CPMs—known in some states as direct entry or lay midwives—varies widely across the nation. Unlike CNMs, CPMs are not required to have a nursing background. They practice primarily in out-of-hospital settings, including birthing centers and private homes. Many CPMs have no formal academic education or medical training, and their training requirements fall short of internationally established standards for midwives and traditional birth attendants.
Other relevant points:
- A person without a high school degree could be licensed as a CPM if he or she passed the certifying exam, observed 20 deliveries, and participated as the primary attendant in 10
- As a group, CPMs have not adopted home-birth patient-selection criteria that are based on generally accepted medical evidence or public safety
- The curriculum, clinical skills training, and experience of CPMs have not been approved by the American Midwifery Certification Board. Nor are they reviewed by the American Board of Obstetrics and Gynecology or the American Board of Family Medicine—recognized authorities in the certification of knowledge and skills associated with the practice of obstetrics.
- The North American Registry of Midwives’ Portfolio Evaluation Process requires midwives to be the primary care provider during 50 home births and to have 3 years’ experience. The average ObGyn resident gets this much experience in 1 month.
CPMs who lack a high school diploma and are apprentice-trained only (without core curriculum training and formal academic experience) clearly do not meet ACOG standards. Therefore, ACOG cautions its Fellows and the public that, for quality and safety reasons, it “does not support the provision of care by … midwives who are not certified by the American Midwifery Certification Board” [ACNM’s accreditation body]. Certification by this board, then, is a good indication of skill.
Requirements for successful collaborative practice
Where can you look for examples of collaboration that work, and for data on the effects of collaboration on health-care outcomes? Four articles in the September 2011 issue of Obstetrics and Gynecology highlight successful models of collaboration between ObGyns and CNMs in very different, well-established maternity programs.6-9 In each article, the authors describe their collaborative practice model in some detail, offering guidance to others interested in successful collaboration. Common threads run through these narratives:
- trust
- communication
- mutual respect
- administrative support for continuing medical education
- consensus meetings
- common adherence to accepted guidelines
- an established support network for back-up and transfer.
The benefits to ObGyns include greater job satisfaction. Benefits to patients include improved health outcomes, as demonstrated, for example, in a model from Washington State: a high rate of vaginal delivery, low rate of cesarean birth, high rate of successful vaginal birth after cesarean (VBAC), and low rate of repeat cesarean delivery.7
ACOG’s policy on collaborative practice finds its origins just over 100 years ago in the Flexner report, quoted at the beginning of this article, which emphasized the need to ensure that medical care in the United States is of no less quality than in other parts of the world.1
Medical education and quality of care have improved dramatically over the past century. ACOG is working to ensure the highest standards of care for pregnant women, standards no lower than for the rest of the population.
Collaboration is a time-honored tradition in ObGyn. Doing it right is key to patient safety.
- How state budget crises are putting the squeeze on Medicaid (and you)
(February 2012) - Is private ObGyn practice on its way out?
with Janelle Yates (October 2011) - 14 questions (and answers) about health reform and you
with Janelle Yates (August 2010)
Acknowledgment
The author acknowledges and thanks ACOG Executive Vice President Hal C. Lawrence III, MD, for his helpful review and comments
We want to hear from you! Tell us what you think.
1. Flexner A. Medical Education in the United States and Canada. A Report to the Carnegie Foundation for the Advancement of Teaching. Bulletin No. 4. 1910. Boston Mass: D. B. Updike, Merrymount Press; 1972.
2. American Association of Birth Centers Uniform Data Set. 2010 Data. Perkiomenville Pa: ASBC; 2011.
3. Facts and Figures 2008. Healthcare Cost and Utilization Project (HCUP). October 2010. Agency for Healthcare Research and Quality Rockville, MD. www.hcup-us.ahrq.gov/reports/factsandfigures/2008/TOC_2008.jsp. Accessed March 30, 2012.
4. American Association of Birth Centers. http://www.birthcenters.org.Accessed March 30, 2012.
5. Waldman RN, Kennedy HP. Collaborative practice between obstetricians and midwives. Obstet Gynecol. 2011;118(3):503-504.
6. Shaw-Battista J, Fineberg A, Boehler B, Skubic B, Woolley D, Tilton Z. Obstetrician and nurse-midwife collaboration: successful public health and private practice partnership. Obstet Gynecol. 2011;118(3):663-672.
7. Darlington A, McBroom K, Warwick S. A Northwest collaborative practice model. Obstet Gynecol. 2011;118(3):673-677.
8. Hutchison MS, Ennis L, Shaw-Battista J, et al. Great minds don’t think alike: collaborative maternity care at San Francisco General Hospital. Obstet Gynecol. 2011;118(3):678-682.
9. DeJoy S, Burkman RT, Graves BW, et al. Making it work: successful collaborative practice. Obstet Gynecol. 2011;118(3):683-686.
10. American Congress of Obstetricians and Gynecologists Glossary of Midwifery Organizations and Terms. Washington DC; 2010.
“We have indeed in America medical practitioners not inferior to the best elsewhere; but there is probably no other country in the world in which there is so great a distance and so fatal a difference between the best, the average, and the worst.”
—Flexner report from 19101
ObGyn is a risky specialty, with no guarantee of a perfect outcome, even with the best education, training, and skills. Does collaboration make it riskier? Or can collaboration help you deliver high-quality care to your patients?
This article explores these questions as they relate to provision of health care in collaboration with midwives—specifically, certified nurse midwives (CNMs), who are approved by the American Midwifery Certification Board, and certified professional midwives (CPMs), who are not. (See thebox for a more detailed discussion of different types of midwives in practice today.)
Got acronym fatigue? Here’s a rundown of the various credentials and certifying organizations.
The American College of Nurse-Midwives (ACNM) is a professional organization established in 1955 for certified nurse midwives and certified midwives. ACNM sets standards for academic preparation and clinical practice. For more information, visit http://www.midwife.org.
The American Midwifery Certification Board (AMCB) is the certification organization affiliated with ACNM. This board was formerly called the ACNM Certification Council (ACC). Certification by AMCB is equivalent to certification by ACC.
In 1997, AMCB opened its national certification exam to non-nurse graduates of midwifery education programs and issued the first certified midwife credential. Since 2010, a graduate degree has been required for entry into clinical practice for both certified nurse midwives and certified midwives. http://www.amcbmidwife.org
Certified midwife (CM). In 1996, the ACNM adopted standards for the certification of direct-entry midwives. These midwives undergo the same certification process as certified nurse midwives, but their training does not include education in nursing. CMs must pass the same certification exam as CNMs and must have a master’s degree.
CMs are licensed in only three states: New Jersey, New York, and Rhode Island. New York had the first CM training program and was the first state to recognize the CM credential. It is the only state that has one unified framework for licensing all midwives—both CNMs and CMs.
Certified nurse midwife (CNM). A midwife who has training in both nursing and midwifery. A master’s degree is required for certification. These midwives typically have prescriptive authority for most drugs; are eligible for third-party reimbursement, including Medicaid; and practice independently or in collaborative practice with physicians.
Certified professional midwife (CPM). In the mid 1990s, the CPM credential was developed jointly by the Midwives Alliance of North America (MANA), the North American Registry of Midwives (NARM), and the Midwifery Education Accreditation Council (MEAC). There is no single standard for education; both apprentice-only–trained midwives and midwives who undergo university-affiliated training use the title CPM.
A CPM can learn through a structured program, through apprenticeship, or through self-study. Another route to the credential is current legal recognition to practice in the United Kingdom. CPMs must pass a written and practical exam for certification.
According to MANA, 24 states recognize the CPM credential as the basis for licensure or use the NARM written exam. Some of these states use a different nomenclature. For example, licensed midwife (LM) is used in California, Idaho, Oregon, and Washington; licensed direct-entry midwife (LDM) is used in Utah; and registered midwife (RM) is used in Colorado.
SOURCE: ACOG10
Moving away from a physician-oriented system
Like it or not, change is under way. Subtle but important shifts are taking place in the way maternity care is provided in your community.
The challenges facing our specialty? Ensuring that the highest levels of patient safety and quality care are maintained. And educating federal and state lawmakers, insurers, and the public accordingly.
Free-standing birth centers are gaining prominence
The Patient Protection and Affordable Care Act (ACA) establishes alternative pathways for maternity care. Congress, state lawmakers, and insurers want to know: Can access to quality maternity care be provided at lower cost outside of hospitals or by nonphysicians? The answer isn’t clear.
Under the ACA, free-standing birth centers are a Medicaid maternity-care choice for low-income women. Birth centers appeal to lawmakers and insurers because of their lower cost. For example, in 2008, the average facility cost for a vaginal delivery in a hospital, with no complications and no newborn charges, was $8,920. In 2010, the average facility cost for a similar delivery at a birth center was $2,277.2,3
We know that dollars alone don’t tell the full story—but they’re easy listening to lawmakers’ ears.
Since 2010, Medicaid payments are allowed to go to state-licensed, free-standing birth centers even if they are not operated by or under the supervision of a physician. Before the ACA became law, Medicaid paid only for services provided in ambulatory centers under the supervision or oversight of a physician.
Another important change: Medicaid now reimburses for the services of any provider who practices in a state-licensed, free-standing birth center as long as that provider is practicing within the state’s scope of practice laws and regulations. That means that if a state allows doulas or lay midwives to provide childbirth care in free-standing birth centers, the federal and state Medicaid programs will pay for this care. This policy is consistent with “any willing provider” rules found elsewhere in Medicaid.
There are 215 birth centers in the United States, with more in development. The number of birth centers has increased more than 20% over the past 5 years; they are regulated in 41 states.4
ACOG’s Guidelines for Perinatal Care asserts: “The hospital, including a birthing center within a hospital complex, or free-standing birthing centers that meet the standards of the Accreditation Association of Birth Centers, provide the safest setting for labor, delivery, and the postpartum period.”5
Reimbursements for nonphysicians are increasing
Beginning in 2011, the Medicare program began reimbursing CNMs, the most highly trained midwives, at 100% of the physician payment rate for obstetric services. Until 2011, CNMs were paid at 65% of the physician’s rate for the same billed services.
In addition, from 2011 through 2015, CNMs whose primary care services account for at least 60% of their Medicare-allowed charges will receive Medicare bonus payments of 10%, reflecting Congress’ concern that our nation faces a serious shortage of primary care providers.
Another important provision goes into effect in 2014: All health plans offered in a state insurance exchange must accept and pay any provider recognized under state law for services covered by that plan. CPMs, some of whom are among the least highly trained providers, are licensed to provide maternity care in 24 states. This provision may put pressure on health insurers to pay for maternity care provided by CPMs, regardless of their training and certification, even if the insurer doesn’t contract with these providers.
“Even a normal pregnancy can become high-risk”
In 2008, the Massachusetts legislature debated expanding childbirth care to encompass less highly trained providers. ACOG President Kenneth L. Noller, MD, MS, cautioned them about the move, saying: “Even a normal pregnancy can become high-risk with little or no warning, and serious, sometimes life-threatening complications may arise for the woman and her fetus.”
He noted that shoulder dystocia occurs in one in every 200 births and listed the frequency of other complications:
- prolapsed umbilical cord: 1 in every 200 births
- life-threatening maternal hemorrhage: 1 in 250
- eclamptic seizures: 1 in 500
- uterine inversion: 1 in 700
- Apgar score of 0–3 at 5 minutes: 1 in 100 to 200.
Three years later, ACOG President Richard A. Waldman, MD, and American College of Nurse Midwives (ACNM) President Holly Powell Kennedy, CNM, PhD, wrote: “Collaborative practice [is] the provision of health care by an interdisciplinary team of professionals who collaborate to accomplish a common goal, and is associated with increased efficiency, improved clinical outcomes, and enhanced provider satisfaction.”5
These messages demonstrate the importance of careful use of collaboration to manage risk and maintain the highest standards of patient care. The questions for ObGyns who are considering collaborative practice:
- What is careful use?
- How do you collaborate carefully, without increasing the risks faced by your patients and your practice?
- How do you make collaboration a success?
- ACOG has taken on these questions and offers sound practical advice.

ACOG recommends high standards and clear practice agreements
ObGyns have a long history of collaboration with our nurse-midwife colleagues—possibly one of the strongest collaborative traditions in medicine. ACOG supports the practice and licensure of trained midwives credentialed by the ACNM. CNMs are well-educated, highly trained, and well-integrated into the health-care system.
In addition to the ACNM standards, ACOG supports the “global standards for midwifery education” established by the International Confederation of Midwives (ICM) in 2010:
- The minimum entry level of students is completion of secondary education
- The minimum length of a direct-entry midwifery education program is 3 years
- The minimum length of a post-nursing/health-care provider program is 18 months
- Standards are congruent with current core ICM documents and position statements.
ACOG strongly encourages that in no case should the professional standards of any maternity provider be less than the standards established or accepted by ACOG or the ACNM.
Effective collaboration depends on clear practice agreements between physicians and CNMs, consistent use of shared practice guidelines, and malpractice insurance coverage of all parties. A collaborative agreement that clearly spells out the mechanism for consultation, collaboration, and referral is essential to assure the best care.
The picture gets a little trickier—and riskier—when we look at less-trained maternity providers.
A majority of CPMs lack adequate training
Few of the nation’s 1,400 CPMs in practice today meet the educational and training standards accepted by ACOG and the ACNM. The educational background of CPMs—known in some states as direct entry or lay midwives—varies widely across the nation. Unlike CNMs, CPMs are not required to have a nursing background. They practice primarily in out-of-hospital settings, including birthing centers and private homes. Many CPMs have no formal academic education or medical training, and their training requirements fall short of internationally established standards for midwives and traditional birth attendants.
Other relevant points:
- A person without a high school degree could be licensed as a CPM if he or she passed the certifying exam, observed 20 deliveries, and participated as the primary attendant in 10
- As a group, CPMs have not adopted home-birth patient-selection criteria that are based on generally accepted medical evidence or public safety
- The curriculum, clinical skills training, and experience of CPMs have not been approved by the American Midwifery Certification Board. Nor are they reviewed by the American Board of Obstetrics and Gynecology or the American Board of Family Medicine—recognized authorities in the certification of knowledge and skills associated with the practice of obstetrics.
- The North American Registry of Midwives’ Portfolio Evaluation Process requires midwives to be the primary care provider during 50 home births and to have 3 years’ experience. The average ObGyn resident gets this much experience in 1 month.
CPMs who lack a high school diploma and are apprentice-trained only (without core curriculum training and formal academic experience) clearly do not meet ACOG standards. Therefore, ACOG cautions its Fellows and the public that, for quality and safety reasons, it “does not support the provision of care by … midwives who are not certified by the American Midwifery Certification Board” [ACNM’s accreditation body]. Certification by this board, then, is a good indication of skill.
Requirements for successful collaborative practice
Where can you look for examples of collaboration that work, and for data on the effects of collaboration on health-care outcomes? Four articles in the September 2011 issue of Obstetrics and Gynecology highlight successful models of collaboration between ObGyns and CNMs in very different, well-established maternity programs.6-9 In each article, the authors describe their collaborative practice model in some detail, offering guidance to others interested in successful collaboration. Common threads run through these narratives:
- trust
- communication
- mutual respect
- administrative support for continuing medical education
- consensus meetings
- common adherence to accepted guidelines
- an established support network for back-up and transfer.
The benefits to ObGyns include greater job satisfaction. Benefits to patients include improved health outcomes, as demonstrated, for example, in a model from Washington State: a high rate of vaginal delivery, low rate of cesarean birth, high rate of successful vaginal birth after cesarean (VBAC), and low rate of repeat cesarean delivery.7
ACOG’s policy on collaborative practice finds its origins just over 100 years ago in the Flexner report, quoted at the beginning of this article, which emphasized the need to ensure that medical care in the United States is of no less quality than in other parts of the world.1
Medical education and quality of care have improved dramatically over the past century. ACOG is working to ensure the highest standards of care for pregnant women, standards no lower than for the rest of the population.
Collaboration is a time-honored tradition in ObGyn. Doing it right is key to patient safety.
- How state budget crises are putting the squeeze on Medicaid (and you)
(February 2012) - Is private ObGyn practice on its way out?
with Janelle Yates (October 2011) - 14 questions (and answers) about health reform and you
with Janelle Yates (August 2010)
Acknowledgment
The author acknowledges and thanks ACOG Executive Vice President Hal C. Lawrence III, MD, for his helpful review and comments
We want to hear from you! Tell us what you think.
“We have indeed in America medical practitioners not inferior to the best elsewhere; but there is probably no other country in the world in which there is so great a distance and so fatal a difference between the best, the average, and the worst.”
—Flexner report from 19101
ObGyn is a risky specialty, with no guarantee of a perfect outcome, even with the best education, training, and skills. Does collaboration make it riskier? Or can collaboration help you deliver high-quality care to your patients?
This article explores these questions as they relate to provision of health care in collaboration with midwives—specifically, certified nurse midwives (CNMs), who are approved by the American Midwifery Certification Board, and certified professional midwives (CPMs), who are not. (See thebox for a more detailed discussion of different types of midwives in practice today.)
Got acronym fatigue? Here’s a rundown of the various credentials and certifying organizations.
The American College of Nurse-Midwives (ACNM) is a professional organization established in 1955 for certified nurse midwives and certified midwives. ACNM sets standards for academic preparation and clinical practice. For more information, visit http://www.midwife.org.
The American Midwifery Certification Board (AMCB) is the certification organization affiliated with ACNM. This board was formerly called the ACNM Certification Council (ACC). Certification by AMCB is equivalent to certification by ACC.
In 1997, AMCB opened its national certification exam to non-nurse graduates of midwifery education programs and issued the first certified midwife credential. Since 2010, a graduate degree has been required for entry into clinical practice for both certified nurse midwives and certified midwives. http://www.amcbmidwife.org
Certified midwife (CM). In 1996, the ACNM adopted standards for the certification of direct-entry midwives. These midwives undergo the same certification process as certified nurse midwives, but their training does not include education in nursing. CMs must pass the same certification exam as CNMs and must have a master’s degree.
CMs are licensed in only three states: New Jersey, New York, and Rhode Island. New York had the first CM training program and was the first state to recognize the CM credential. It is the only state that has one unified framework for licensing all midwives—both CNMs and CMs.
Certified nurse midwife (CNM). A midwife who has training in both nursing and midwifery. A master’s degree is required for certification. These midwives typically have prescriptive authority for most drugs; are eligible for third-party reimbursement, including Medicaid; and practice independently or in collaborative practice with physicians.
Certified professional midwife (CPM). In the mid 1990s, the CPM credential was developed jointly by the Midwives Alliance of North America (MANA), the North American Registry of Midwives (NARM), and the Midwifery Education Accreditation Council (MEAC). There is no single standard for education; both apprentice-only–trained midwives and midwives who undergo university-affiliated training use the title CPM.
A CPM can learn through a structured program, through apprenticeship, or through self-study. Another route to the credential is current legal recognition to practice in the United Kingdom. CPMs must pass a written and practical exam for certification.
According to MANA, 24 states recognize the CPM credential as the basis for licensure or use the NARM written exam. Some of these states use a different nomenclature. For example, licensed midwife (LM) is used in California, Idaho, Oregon, and Washington; licensed direct-entry midwife (LDM) is used in Utah; and registered midwife (RM) is used in Colorado.
SOURCE: ACOG10
Moving away from a physician-oriented system
Like it or not, change is under way. Subtle but important shifts are taking place in the way maternity care is provided in your community.
The challenges facing our specialty? Ensuring that the highest levels of patient safety and quality care are maintained. And educating federal and state lawmakers, insurers, and the public accordingly.
Free-standing birth centers are gaining prominence
The Patient Protection and Affordable Care Act (ACA) establishes alternative pathways for maternity care. Congress, state lawmakers, and insurers want to know: Can access to quality maternity care be provided at lower cost outside of hospitals or by nonphysicians? The answer isn’t clear.
Under the ACA, free-standing birth centers are a Medicaid maternity-care choice for low-income women. Birth centers appeal to lawmakers and insurers because of their lower cost. For example, in 2008, the average facility cost for a vaginal delivery in a hospital, with no complications and no newborn charges, was $8,920. In 2010, the average facility cost for a similar delivery at a birth center was $2,277.2,3
We know that dollars alone don’t tell the full story—but they’re easy listening to lawmakers’ ears.
Since 2010, Medicaid payments are allowed to go to state-licensed, free-standing birth centers even if they are not operated by or under the supervision of a physician. Before the ACA became law, Medicaid paid only for services provided in ambulatory centers under the supervision or oversight of a physician.
Another important change: Medicaid now reimburses for the services of any provider who practices in a state-licensed, free-standing birth center as long as that provider is practicing within the state’s scope of practice laws and regulations. That means that if a state allows doulas or lay midwives to provide childbirth care in free-standing birth centers, the federal and state Medicaid programs will pay for this care. This policy is consistent with “any willing provider” rules found elsewhere in Medicaid.
There are 215 birth centers in the United States, with more in development. The number of birth centers has increased more than 20% over the past 5 years; they are regulated in 41 states.4
ACOG’s Guidelines for Perinatal Care asserts: “The hospital, including a birthing center within a hospital complex, or free-standing birthing centers that meet the standards of the Accreditation Association of Birth Centers, provide the safest setting for labor, delivery, and the postpartum period.”5
Reimbursements for nonphysicians are increasing
Beginning in 2011, the Medicare program began reimbursing CNMs, the most highly trained midwives, at 100% of the physician payment rate for obstetric services. Until 2011, CNMs were paid at 65% of the physician’s rate for the same billed services.
In addition, from 2011 through 2015, CNMs whose primary care services account for at least 60% of their Medicare-allowed charges will receive Medicare bonus payments of 10%, reflecting Congress’ concern that our nation faces a serious shortage of primary care providers.
Another important provision goes into effect in 2014: All health plans offered in a state insurance exchange must accept and pay any provider recognized under state law for services covered by that plan. CPMs, some of whom are among the least highly trained providers, are licensed to provide maternity care in 24 states. This provision may put pressure on health insurers to pay for maternity care provided by CPMs, regardless of their training and certification, even if the insurer doesn’t contract with these providers.
“Even a normal pregnancy can become high-risk”
In 2008, the Massachusetts legislature debated expanding childbirth care to encompass less highly trained providers. ACOG President Kenneth L. Noller, MD, MS, cautioned them about the move, saying: “Even a normal pregnancy can become high-risk with little or no warning, and serious, sometimes life-threatening complications may arise for the woman and her fetus.”
He noted that shoulder dystocia occurs in one in every 200 births and listed the frequency of other complications:
- prolapsed umbilical cord: 1 in every 200 births
- life-threatening maternal hemorrhage: 1 in 250
- eclamptic seizures: 1 in 500
- uterine inversion: 1 in 700
- Apgar score of 0–3 at 5 minutes: 1 in 100 to 200.
Three years later, ACOG President Richard A. Waldman, MD, and American College of Nurse Midwives (ACNM) President Holly Powell Kennedy, CNM, PhD, wrote: “Collaborative practice [is] the provision of health care by an interdisciplinary team of professionals who collaborate to accomplish a common goal, and is associated with increased efficiency, improved clinical outcomes, and enhanced provider satisfaction.”5
These messages demonstrate the importance of careful use of collaboration to manage risk and maintain the highest standards of patient care. The questions for ObGyns who are considering collaborative practice:
- What is careful use?
- How do you collaborate carefully, without increasing the risks faced by your patients and your practice?
- How do you make collaboration a success?
- ACOG has taken on these questions and offers sound practical advice.

ACOG recommends high standards and clear practice agreements
ObGyns have a long history of collaboration with our nurse-midwife colleagues—possibly one of the strongest collaborative traditions in medicine. ACOG supports the practice and licensure of trained midwives credentialed by the ACNM. CNMs are well-educated, highly trained, and well-integrated into the health-care system.
In addition to the ACNM standards, ACOG supports the “global standards for midwifery education” established by the International Confederation of Midwives (ICM) in 2010:
- The minimum entry level of students is completion of secondary education
- The minimum length of a direct-entry midwifery education program is 3 years
- The minimum length of a post-nursing/health-care provider program is 18 months
- Standards are congruent with current core ICM documents and position statements.
ACOG strongly encourages that in no case should the professional standards of any maternity provider be less than the standards established or accepted by ACOG or the ACNM.
Effective collaboration depends on clear practice agreements between physicians and CNMs, consistent use of shared practice guidelines, and malpractice insurance coverage of all parties. A collaborative agreement that clearly spells out the mechanism for consultation, collaboration, and referral is essential to assure the best care.
The picture gets a little trickier—and riskier—when we look at less-trained maternity providers.
A majority of CPMs lack adequate training
Few of the nation’s 1,400 CPMs in practice today meet the educational and training standards accepted by ACOG and the ACNM. The educational background of CPMs—known in some states as direct entry or lay midwives—varies widely across the nation. Unlike CNMs, CPMs are not required to have a nursing background. They practice primarily in out-of-hospital settings, including birthing centers and private homes. Many CPMs have no formal academic education or medical training, and their training requirements fall short of internationally established standards for midwives and traditional birth attendants.
Other relevant points:
- A person without a high school degree could be licensed as a CPM if he or she passed the certifying exam, observed 20 deliveries, and participated as the primary attendant in 10
- As a group, CPMs have not adopted home-birth patient-selection criteria that are based on generally accepted medical evidence or public safety
- The curriculum, clinical skills training, and experience of CPMs have not been approved by the American Midwifery Certification Board. Nor are they reviewed by the American Board of Obstetrics and Gynecology or the American Board of Family Medicine—recognized authorities in the certification of knowledge and skills associated with the practice of obstetrics.
- The North American Registry of Midwives’ Portfolio Evaluation Process requires midwives to be the primary care provider during 50 home births and to have 3 years’ experience. The average ObGyn resident gets this much experience in 1 month.
CPMs who lack a high school diploma and are apprentice-trained only (without core curriculum training and formal academic experience) clearly do not meet ACOG standards. Therefore, ACOG cautions its Fellows and the public that, for quality and safety reasons, it “does not support the provision of care by … midwives who are not certified by the American Midwifery Certification Board” [ACNM’s accreditation body]. Certification by this board, then, is a good indication of skill.
Requirements for successful collaborative practice
Where can you look for examples of collaboration that work, and for data on the effects of collaboration on health-care outcomes? Four articles in the September 2011 issue of Obstetrics and Gynecology highlight successful models of collaboration between ObGyns and CNMs in very different, well-established maternity programs.6-9 In each article, the authors describe their collaborative practice model in some detail, offering guidance to others interested in successful collaboration. Common threads run through these narratives:
- trust
- communication
- mutual respect
- administrative support for continuing medical education
- consensus meetings
- common adherence to accepted guidelines
- an established support network for back-up and transfer.
The benefits to ObGyns include greater job satisfaction. Benefits to patients include improved health outcomes, as demonstrated, for example, in a model from Washington State: a high rate of vaginal delivery, low rate of cesarean birth, high rate of successful vaginal birth after cesarean (VBAC), and low rate of repeat cesarean delivery.7
ACOG’s policy on collaborative practice finds its origins just over 100 years ago in the Flexner report, quoted at the beginning of this article, which emphasized the need to ensure that medical care in the United States is of no less quality than in other parts of the world.1
Medical education and quality of care have improved dramatically over the past century. ACOG is working to ensure the highest standards of care for pregnant women, standards no lower than for the rest of the population.
Collaboration is a time-honored tradition in ObGyn. Doing it right is key to patient safety.
- How state budget crises are putting the squeeze on Medicaid (and you)
(February 2012) - Is private ObGyn practice on its way out?
with Janelle Yates (October 2011) - 14 questions (and answers) about health reform and you
with Janelle Yates (August 2010)
Acknowledgment
The author acknowledges and thanks ACOG Executive Vice President Hal C. Lawrence III, MD, for his helpful review and comments
We want to hear from you! Tell us what you think.
1. Flexner A. Medical Education in the United States and Canada. A Report to the Carnegie Foundation for the Advancement of Teaching. Bulletin No. 4. 1910. Boston Mass: D. B. Updike, Merrymount Press; 1972.
2. American Association of Birth Centers Uniform Data Set. 2010 Data. Perkiomenville Pa: ASBC; 2011.
3. Facts and Figures 2008. Healthcare Cost and Utilization Project (HCUP). October 2010. Agency for Healthcare Research and Quality Rockville, MD. www.hcup-us.ahrq.gov/reports/factsandfigures/2008/TOC_2008.jsp. Accessed March 30, 2012.
4. American Association of Birth Centers. http://www.birthcenters.org.Accessed March 30, 2012.
5. Waldman RN, Kennedy HP. Collaborative practice between obstetricians and midwives. Obstet Gynecol. 2011;118(3):503-504.
6. Shaw-Battista J, Fineberg A, Boehler B, Skubic B, Woolley D, Tilton Z. Obstetrician and nurse-midwife collaboration: successful public health and private practice partnership. Obstet Gynecol. 2011;118(3):663-672.
7. Darlington A, McBroom K, Warwick S. A Northwest collaborative practice model. Obstet Gynecol. 2011;118(3):673-677.
8. Hutchison MS, Ennis L, Shaw-Battista J, et al. Great minds don’t think alike: collaborative maternity care at San Francisco General Hospital. Obstet Gynecol. 2011;118(3):678-682.
9. DeJoy S, Burkman RT, Graves BW, et al. Making it work: successful collaborative practice. Obstet Gynecol. 2011;118(3):683-686.
10. American Congress of Obstetricians and Gynecologists Glossary of Midwifery Organizations and Terms. Washington DC; 2010.
1. Flexner A. Medical Education in the United States and Canada. A Report to the Carnegie Foundation for the Advancement of Teaching. Bulletin No. 4. 1910. Boston Mass: D. B. Updike, Merrymount Press; 1972.
2. American Association of Birth Centers Uniform Data Set. 2010 Data. Perkiomenville Pa: ASBC; 2011.
3. Facts and Figures 2008. Healthcare Cost and Utilization Project (HCUP). October 2010. Agency for Healthcare Research and Quality Rockville, MD. www.hcup-us.ahrq.gov/reports/factsandfigures/2008/TOC_2008.jsp. Accessed March 30, 2012.
4. American Association of Birth Centers. http://www.birthcenters.org.Accessed March 30, 2012.
5. Waldman RN, Kennedy HP. Collaborative practice between obstetricians and midwives. Obstet Gynecol. 2011;118(3):503-504.
6. Shaw-Battista J, Fineberg A, Boehler B, Skubic B, Woolley D, Tilton Z. Obstetrician and nurse-midwife collaboration: successful public health and private practice partnership. Obstet Gynecol. 2011;118(3):663-672.
7. Darlington A, McBroom K, Warwick S. A Northwest collaborative practice model. Obstet Gynecol. 2011;118(3):673-677.
8. Hutchison MS, Ennis L, Shaw-Battista J, et al. Great minds don’t think alike: collaborative maternity care at San Francisco General Hospital. Obstet Gynecol. 2011;118(3):678-682.
9. DeJoy S, Burkman RT, Graves BW, et al. Making it work: successful collaborative practice. Obstet Gynecol. 2011;118(3):683-686.
10. American Congress of Obstetricians and Gynecologists Glossary of Midwifery Organizations and Terms. Washington DC; 2010.
Mother dies 10 h post-delivery … and more

AT 38 WEEKS’ GESTATION, a 20-year-old woman had preeclampsia and a borderline-low platelet count. She was admitted to a US Navy hospital for induction of labor.
When labor failed to progress after 53 hours, a cesarean delivery was performed. The patient suffered uncontrolled bleeding and developed HELLP syndrome (hemolysis, elevated liver enzymes, low platelet count). A platelet transfusion was needed, but the nearest supply was at a city hospital approximately 60 miles away. Because of bad weather, the patient could not be flown to the city. She died 10 hours after delivery.
ESTATE’S CLAIM A cesarean delivery should have been performed earlier. Lab results showing the severity of the mother’s condition at delivery were not read for 5 hours.
DEFENDANTS’ DEFENSE The case was settled before trial.
VERDICT A $2.1 million Missouri settlement was reached.
Did OB’s errors cause this child’s injuries?
A CHILD WAS BORN with a left brachial plexus injury and fractured left clavicle.
PATIENT’S CLAIM The ObGyn failed to diagnose shoulder dystocia, failed to perform appropriate maneuvers to free the entrapped anterior shoulder, and applied excessive lateral traction to deliver the child.
PHYSICIAN’S DEFENSE There was no shoulder dystocia. The child’s injuries were caused by the natural forces of labor.
VERDICT A $1,314,600 Iowa verdict was returned.
Sedation for surgery leads to brain damage
A 20-YEAR-OLD WOMAN with sickle-cell anemia (SCA) was sent to an ambulatory surgery center for surgical treatment of cervical dysplasia.
A certified nurse anesthetist (CRNA) sedated the patient at the surgery center. The patient went into cardiac arrest and was transferred to a hospital. She suffered a brain injury caused by oxygen deprivation. Her IQ dropped by 11 points; with the brain damage, she was unable to retain her driver’s license.
PATIENT’S CLAIM The procedure could have been performed safely in the doctor’s office under local anesthesia. The gynecologist had signed off on the anesthesia plan, although he knew of the risks of giving general anesthesia to someone with SCA. She was sent to the surgery center only because of the gynecologist’s desire to generate revenue.
DEFENDANTS’ DEFENSE The gynecologist blamed the CRNA, who, allegedly, allowed a kink to form in the IV anesthesia line. When the line cleared, sedative flooded into the patient, causing her heart to stop. The gynecologist admitted that general anesthesia was unnecessary; local anesthesia would have been safer. The CRNA argued that the surgery center was at fault; she had followed the center’s standard operating procedure. The surgery center denied negligence.
VERDICT An $851,000 South Carolina settlement was reached with the gynecologist, CRNA, and surgery center.
Pain from retained sponge, surgical ring
TWINS WERE BORN BY CESAREAN delivery to a 40-year-old woman. She developed abdominal pain and reported it to her ObGyn several times. Four months after delivery, the ObGyn found a retained sponge and surgical ring during exploratory laparotomy.
PATIENT’S CLAIM The ObGyn did not adequately inspect the operative area before closing. Although the patient reported abdominal pain immediately after delivery, her complaints were ignored for several months.
PHYSICIAN’S DEFENSE The nurses are responsible for any errors in the sponge count. The patient’s complaints were not brought to his attention until four months after delivery.
VERDICT The patient reached a confidential settlement with the delivery nurses, an assisting physician, and the hospital. A New York jury found the ObGyn 60% at fault; a $1.5 million verdict was returned. The patient agreed to a $550,000 posttrial settlement with the ObGyn’s insurer.
Patient falls from exam table during non-stress test
IN HER EIGHTH GESTATIONAL MONTH, a woman in her 30s underwent a non-stress test because of five prior miscarriages. She became ill just as the test was beginning, turned to her side to vomit, and fell off the examination table. She fractured her cervical spine.
An emergency cesarean delivery resulted in the birth of a healthy baby. The woman then underwent fusion surgery to repair the cervical fracture. She required physical therapy, and made a good recovery.
PATIENT’S CLAIM The examination table should have had side rails, which would have prevented the fall.
DEFENDANTS’ DEFENSE Side rails were not required on an examination table. This was an unforeseeable event that occurred while a nurse was setting up the procedure and reaching for a blood-pressure cuff.
VERDICT A Connecticut defense verdict was returned.
Sexually abused by nursing assistant: $67 million verdict
A 38-YEAR-OLD WOMAN UNDERWENT laparoscopic ovarian cyst removal. While hospitalized, a male nursing assistant sexually assaulted her by digital penetration of the vagina without wearing gloves. The employee was arrested for the assault, but allegedly fled the country after posting bail.
PATIENT’S CLAIM At least five similar incidents involving the same nursing assistant reportedly occurred in the hospital over a 16-month period. At trial, four patients and an employee testified that they had been similarly assaulted and had reported the incidents to hospital staff. The nursing assistant should have been removed from his position after the first reported incident, and a thorough investigation conducted. The patient suffered post-traumatic stress disorder because of her experience.
DEFENDANTS’ DEFENSE A proper investigation was made. Often, female patients are uncomfortable with male nurses. The hospital denied being notified of some incidents, and maintained it had suspended the male nursing assistant when it became aware of the incident under litigation.
VERDICT A $67,359,753 California verdict included $65 million in punitive damages against the hospital and its former corporate owner.
Salpingectomy results in death
TO INCREASE HER CHANCES of becoming pregnant using IVF, a woman in her 30s underwent adhesiolysis and salpingectomy. She was discharged the same day.
The next day, she complained of abdominal pain to her ObGyn. She died two days after surgery from septic shock due to a perforated bowel.
ESTATE’S CLAIM The ObGyn was negligent in discharging her, especially because the surgeon had identified a superficial injury to the bowel during surgery. She should have been examined the day after surgery when she first complained of abdominal pain.
PHYSICIANS’ DEFENSE The ObGyn acted appropriately in relying on the surgeon’s recommendation for discharge. He had contacted the patient twice after her initial call regarding abdominal pain, and was told both times that she was feeling better.
VERDICT A Virginia defense verdict was returned.
Disastrous D&C after miscarriage
A 29-YEAR-OLD WOMAN miscarried at 14 weeks’ gestation. An ObGyn recommended that she undergo dilation and curettage (D&C).
With the ObGyn in attendance, a resident sedated the patient and performed the D&C. When the resident perforated the uterus, the ObGyn took over, inserting ring forceps to remove the remains. The forceps went through the perforation and tore the top half of the rectum and a portion of bowel.
A rectal surgeon, called in to repair the injury, performed an ileostomy and created an ileostomy pouch. The ileo-stomy was later successfully reversed.
PATIENT’S CLAIM The woman was at risk of injury because her uterus was anteverted and she had under-gone a cesarean delivery; an experienced physician should have performed the procedure.
When the perforation first occurred, ultrasonography should have been used to identify the puncture and prevent in-jury to the rectum and bowel.
DEFENDANTS’ DEFENSE The patient gave informed consent. The injury is a known risk of the procedure.
VERDICT A $2.5 million Michigan verdict was returned against the ObGyn and hospital, but was reduced to $1.25 million under the statutory cap.
These cases were selected by the editors of OBG MANAGEMENT from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.

AT 38 WEEKS’ GESTATION, a 20-year-old woman had preeclampsia and a borderline-low platelet count. She was admitted to a US Navy hospital for induction of labor.
When labor failed to progress after 53 hours, a cesarean delivery was performed. The patient suffered uncontrolled bleeding and developed HELLP syndrome (hemolysis, elevated liver enzymes, low platelet count). A platelet transfusion was needed, but the nearest supply was at a city hospital approximately 60 miles away. Because of bad weather, the patient could not be flown to the city. She died 10 hours after delivery.
ESTATE’S CLAIM A cesarean delivery should have been performed earlier. Lab results showing the severity of the mother’s condition at delivery were not read for 5 hours.
DEFENDANTS’ DEFENSE The case was settled before trial.
VERDICT A $2.1 million Missouri settlement was reached.
Did OB’s errors cause this child’s injuries?
A CHILD WAS BORN with a left brachial plexus injury and fractured left clavicle.
PATIENT’S CLAIM The ObGyn failed to diagnose shoulder dystocia, failed to perform appropriate maneuvers to free the entrapped anterior shoulder, and applied excessive lateral traction to deliver the child.
PHYSICIAN’S DEFENSE There was no shoulder dystocia. The child’s injuries were caused by the natural forces of labor.
VERDICT A $1,314,600 Iowa verdict was returned.
Sedation for surgery leads to brain damage
A 20-YEAR-OLD WOMAN with sickle-cell anemia (SCA) was sent to an ambulatory surgery center for surgical treatment of cervical dysplasia.
A certified nurse anesthetist (CRNA) sedated the patient at the surgery center. The patient went into cardiac arrest and was transferred to a hospital. She suffered a brain injury caused by oxygen deprivation. Her IQ dropped by 11 points; with the brain damage, she was unable to retain her driver’s license.
PATIENT’S CLAIM The procedure could have been performed safely in the doctor’s office under local anesthesia. The gynecologist had signed off on the anesthesia plan, although he knew of the risks of giving general anesthesia to someone with SCA. She was sent to the surgery center only because of the gynecologist’s desire to generate revenue.
DEFENDANTS’ DEFENSE The gynecologist blamed the CRNA, who, allegedly, allowed a kink to form in the IV anesthesia line. When the line cleared, sedative flooded into the patient, causing her heart to stop. The gynecologist admitted that general anesthesia was unnecessary; local anesthesia would have been safer. The CRNA argued that the surgery center was at fault; she had followed the center’s standard operating procedure. The surgery center denied negligence.
VERDICT An $851,000 South Carolina settlement was reached with the gynecologist, CRNA, and surgery center.
Pain from retained sponge, surgical ring
TWINS WERE BORN BY CESAREAN delivery to a 40-year-old woman. She developed abdominal pain and reported it to her ObGyn several times. Four months after delivery, the ObGyn found a retained sponge and surgical ring during exploratory laparotomy.
PATIENT’S CLAIM The ObGyn did not adequately inspect the operative area before closing. Although the patient reported abdominal pain immediately after delivery, her complaints were ignored for several months.
PHYSICIAN’S DEFENSE The nurses are responsible for any errors in the sponge count. The patient’s complaints were not brought to his attention until four months after delivery.
VERDICT The patient reached a confidential settlement with the delivery nurses, an assisting physician, and the hospital. A New York jury found the ObGyn 60% at fault; a $1.5 million verdict was returned. The patient agreed to a $550,000 posttrial settlement with the ObGyn’s insurer.
Patient falls from exam table during non-stress test
IN HER EIGHTH GESTATIONAL MONTH, a woman in her 30s underwent a non-stress test because of five prior miscarriages. She became ill just as the test was beginning, turned to her side to vomit, and fell off the examination table. She fractured her cervical spine.
An emergency cesarean delivery resulted in the birth of a healthy baby. The woman then underwent fusion surgery to repair the cervical fracture. She required physical therapy, and made a good recovery.
PATIENT’S CLAIM The examination table should have had side rails, which would have prevented the fall.
DEFENDANTS’ DEFENSE Side rails were not required on an examination table. This was an unforeseeable event that occurred while a nurse was setting up the procedure and reaching for a blood-pressure cuff.
VERDICT A Connecticut defense verdict was returned.
Sexually abused by nursing assistant: $67 million verdict
A 38-YEAR-OLD WOMAN UNDERWENT laparoscopic ovarian cyst removal. While hospitalized, a male nursing assistant sexually assaulted her by digital penetration of the vagina without wearing gloves. The employee was arrested for the assault, but allegedly fled the country after posting bail.
PATIENT’S CLAIM At least five similar incidents involving the same nursing assistant reportedly occurred in the hospital over a 16-month period. At trial, four patients and an employee testified that they had been similarly assaulted and had reported the incidents to hospital staff. The nursing assistant should have been removed from his position after the first reported incident, and a thorough investigation conducted. The patient suffered post-traumatic stress disorder because of her experience.
DEFENDANTS’ DEFENSE A proper investigation was made. Often, female patients are uncomfortable with male nurses. The hospital denied being notified of some incidents, and maintained it had suspended the male nursing assistant when it became aware of the incident under litigation.
VERDICT A $67,359,753 California verdict included $65 million in punitive damages against the hospital and its former corporate owner.
Salpingectomy results in death
TO INCREASE HER CHANCES of becoming pregnant using IVF, a woman in her 30s underwent adhesiolysis and salpingectomy. She was discharged the same day.
The next day, she complained of abdominal pain to her ObGyn. She died two days after surgery from septic shock due to a perforated bowel.
ESTATE’S CLAIM The ObGyn was negligent in discharging her, especially because the surgeon had identified a superficial injury to the bowel during surgery. She should have been examined the day after surgery when she first complained of abdominal pain.
PHYSICIANS’ DEFENSE The ObGyn acted appropriately in relying on the surgeon’s recommendation for discharge. He had contacted the patient twice after her initial call regarding abdominal pain, and was told both times that she was feeling better.
VERDICT A Virginia defense verdict was returned.
Disastrous D&C after miscarriage
A 29-YEAR-OLD WOMAN miscarried at 14 weeks’ gestation. An ObGyn recommended that she undergo dilation and curettage (D&C).
With the ObGyn in attendance, a resident sedated the patient and performed the D&C. When the resident perforated the uterus, the ObGyn took over, inserting ring forceps to remove the remains. The forceps went through the perforation and tore the top half of the rectum and a portion of bowel.
A rectal surgeon, called in to repair the injury, performed an ileostomy and created an ileostomy pouch. The ileo-stomy was later successfully reversed.
PATIENT’S CLAIM The woman was at risk of injury because her uterus was anteverted and she had under-gone a cesarean delivery; an experienced physician should have performed the procedure.
When the perforation first occurred, ultrasonography should have been used to identify the puncture and prevent in-jury to the rectum and bowel.
DEFENDANTS’ DEFENSE The patient gave informed consent. The injury is a known risk of the procedure.
VERDICT A $2.5 million Michigan verdict was returned against the ObGyn and hospital, but was reduced to $1.25 million under the statutory cap.

AT 38 WEEKS’ GESTATION, a 20-year-old woman had preeclampsia and a borderline-low platelet count. She was admitted to a US Navy hospital for induction of labor.
When labor failed to progress after 53 hours, a cesarean delivery was performed. The patient suffered uncontrolled bleeding and developed HELLP syndrome (hemolysis, elevated liver enzymes, low platelet count). A platelet transfusion was needed, but the nearest supply was at a city hospital approximately 60 miles away. Because of bad weather, the patient could not be flown to the city. She died 10 hours after delivery.
ESTATE’S CLAIM A cesarean delivery should have been performed earlier. Lab results showing the severity of the mother’s condition at delivery were not read for 5 hours.
DEFENDANTS’ DEFENSE The case was settled before trial.
VERDICT A $2.1 million Missouri settlement was reached.
Did OB’s errors cause this child’s injuries?
A CHILD WAS BORN with a left brachial plexus injury and fractured left clavicle.
PATIENT’S CLAIM The ObGyn failed to diagnose shoulder dystocia, failed to perform appropriate maneuvers to free the entrapped anterior shoulder, and applied excessive lateral traction to deliver the child.
PHYSICIAN’S DEFENSE There was no shoulder dystocia. The child’s injuries were caused by the natural forces of labor.
VERDICT A $1,314,600 Iowa verdict was returned.
Sedation for surgery leads to brain damage
A 20-YEAR-OLD WOMAN with sickle-cell anemia (SCA) was sent to an ambulatory surgery center for surgical treatment of cervical dysplasia.
A certified nurse anesthetist (CRNA) sedated the patient at the surgery center. The patient went into cardiac arrest and was transferred to a hospital. She suffered a brain injury caused by oxygen deprivation. Her IQ dropped by 11 points; with the brain damage, she was unable to retain her driver’s license.
PATIENT’S CLAIM The procedure could have been performed safely in the doctor’s office under local anesthesia. The gynecologist had signed off on the anesthesia plan, although he knew of the risks of giving general anesthesia to someone with SCA. She was sent to the surgery center only because of the gynecologist’s desire to generate revenue.
DEFENDANTS’ DEFENSE The gynecologist blamed the CRNA, who, allegedly, allowed a kink to form in the IV anesthesia line. When the line cleared, sedative flooded into the patient, causing her heart to stop. The gynecologist admitted that general anesthesia was unnecessary; local anesthesia would have been safer. The CRNA argued that the surgery center was at fault; she had followed the center’s standard operating procedure. The surgery center denied negligence.
VERDICT An $851,000 South Carolina settlement was reached with the gynecologist, CRNA, and surgery center.
Pain from retained sponge, surgical ring
TWINS WERE BORN BY CESAREAN delivery to a 40-year-old woman. She developed abdominal pain and reported it to her ObGyn several times. Four months after delivery, the ObGyn found a retained sponge and surgical ring during exploratory laparotomy.
PATIENT’S CLAIM The ObGyn did not adequately inspect the operative area before closing. Although the patient reported abdominal pain immediately after delivery, her complaints were ignored for several months.
PHYSICIAN’S DEFENSE The nurses are responsible for any errors in the sponge count. The patient’s complaints were not brought to his attention until four months after delivery.
VERDICT The patient reached a confidential settlement with the delivery nurses, an assisting physician, and the hospital. A New York jury found the ObGyn 60% at fault; a $1.5 million verdict was returned. The patient agreed to a $550,000 posttrial settlement with the ObGyn’s insurer.
Patient falls from exam table during non-stress test
IN HER EIGHTH GESTATIONAL MONTH, a woman in her 30s underwent a non-stress test because of five prior miscarriages. She became ill just as the test was beginning, turned to her side to vomit, and fell off the examination table. She fractured her cervical spine.
An emergency cesarean delivery resulted in the birth of a healthy baby. The woman then underwent fusion surgery to repair the cervical fracture. She required physical therapy, and made a good recovery.
PATIENT’S CLAIM The examination table should have had side rails, which would have prevented the fall.
DEFENDANTS’ DEFENSE Side rails were not required on an examination table. This was an unforeseeable event that occurred while a nurse was setting up the procedure and reaching for a blood-pressure cuff.
VERDICT A Connecticut defense verdict was returned.
Sexually abused by nursing assistant: $67 million verdict
A 38-YEAR-OLD WOMAN UNDERWENT laparoscopic ovarian cyst removal. While hospitalized, a male nursing assistant sexually assaulted her by digital penetration of the vagina without wearing gloves. The employee was arrested for the assault, but allegedly fled the country after posting bail.
PATIENT’S CLAIM At least five similar incidents involving the same nursing assistant reportedly occurred in the hospital over a 16-month period. At trial, four patients and an employee testified that they had been similarly assaulted and had reported the incidents to hospital staff. The nursing assistant should have been removed from his position after the first reported incident, and a thorough investigation conducted. The patient suffered post-traumatic stress disorder because of her experience.
DEFENDANTS’ DEFENSE A proper investigation was made. Often, female patients are uncomfortable with male nurses. The hospital denied being notified of some incidents, and maintained it had suspended the male nursing assistant when it became aware of the incident under litigation.
VERDICT A $67,359,753 California verdict included $65 million in punitive damages against the hospital and its former corporate owner.
Salpingectomy results in death
TO INCREASE HER CHANCES of becoming pregnant using IVF, a woman in her 30s underwent adhesiolysis and salpingectomy. She was discharged the same day.
The next day, she complained of abdominal pain to her ObGyn. She died two days after surgery from septic shock due to a perforated bowel.
ESTATE’S CLAIM The ObGyn was negligent in discharging her, especially because the surgeon had identified a superficial injury to the bowel during surgery. She should have been examined the day after surgery when she first complained of abdominal pain.
PHYSICIANS’ DEFENSE The ObGyn acted appropriately in relying on the surgeon’s recommendation for discharge. He had contacted the patient twice after her initial call regarding abdominal pain, and was told both times that she was feeling better.
VERDICT A Virginia defense verdict was returned.
Disastrous D&C after miscarriage
A 29-YEAR-OLD WOMAN miscarried at 14 weeks’ gestation. An ObGyn recommended that she undergo dilation and curettage (D&C).
With the ObGyn in attendance, a resident sedated the patient and performed the D&C. When the resident perforated the uterus, the ObGyn took over, inserting ring forceps to remove the remains. The forceps went through the perforation and tore the top half of the rectum and a portion of bowel.
A rectal surgeon, called in to repair the injury, performed an ileostomy and created an ileostomy pouch. The ileo-stomy was later successfully reversed.
PATIENT’S CLAIM The woman was at risk of injury because her uterus was anteverted and she had under-gone a cesarean delivery; an experienced physician should have performed the procedure.
When the perforation first occurred, ultrasonography should have been used to identify the puncture and prevent in-jury to the rectum and bowel.
DEFENDANTS’ DEFENSE The patient gave informed consent. The injury is a known risk of the procedure.
VERDICT A $2.5 million Michigan verdict was returned against the ObGyn and hospital, but was reduced to $1.25 million under the statutory cap.
These cases were selected by the editors of OBG MANAGEMENT from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.
These cases were selected by the editors of OBG MANAGEMENT from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.