User login
Severe Pain Following Car Crash
ANSWER
The radiograph shows malalignment at the L3-L4 level. There is a slight retrolisthesis, as well as widening of the interspinous disc space and the facets at this level. No compression fracture is seen.
Such findings are suggestive of a Chance fracture as a result of a hyperflexion injury. CT confirmed these findings. Such injuries are considered unstable and generally require surgical stabilization.
ANSWER
The radiograph shows malalignment at the L3-L4 level. There is a slight retrolisthesis, as well as widening of the interspinous disc space and the facets at this level. No compression fracture is seen.
Such findings are suggestive of a Chance fracture as a result of a hyperflexion injury. CT confirmed these findings. Such injuries are considered unstable and generally require surgical stabilization.
ANSWER
The radiograph shows malalignment at the L3-L4 level. There is a slight retrolisthesis, as well as widening of the interspinous disc space and the facets at this level. No compression fracture is seen.
Such findings are suggestive of a Chance fracture as a result of a hyperflexion injury. CT confirmed these findings. Such injuries are considered unstable and generally require surgical stabilization.
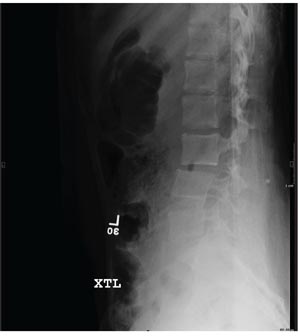
A 15-year-old girl is brought to your facility following a motor vehicle crash. She was a restrained back seat passenger in a vehicle that was struck from behind at a moderate rate of speed. Extensive damage to the vehicle was noted. The patient is complaining of severe abdominal and back pain. Medical history is unremarkable and vital signs are normal. Physical exam shows a female teen who is anxious but in no obvious distress. Her abdomen is firm, with diffuse tenderness and mild guarding. Palpation of her back reveals moderate tenderness in the lower lumbar spine. She is able to move all extremities well, with no other neurologic deficits noted. She is being sent for CT of the chest, abdomen, and pelvis; but first, a lateral radiograph of the lumbar spine is obtained (shown). What is your impression?
Woman With Back Pain Unable To Walk
ANSWER
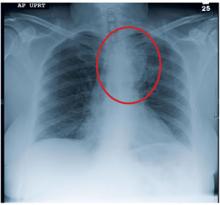
The radiograph demonstrates a fairly large mass on the medial aspect of the left upper lobe. Such findings are usually associated with bronchogenic carcinomas.
Among the documentation from the transferring facility was a copy of a CT scan of the patient’s chest. On that study, the mass is seen; it appears to extend to the posterior chest wall, with extensive involvement and destruction of the ribs and posterior elements of T4 and T5. There is also evidence of some spinal cord compression, which would explain the patient’s presenting complaint.
Subsequent CT-guided biopsy demonstrated the lesion to be a non–small cell carcinoma. Due to the already extensive involvement, surgery was not an option, and the patient was referred for palliative radiation therapy.
ANSWER
The radiograph demonstrates a fairly large mass on the medial aspect of the left upper lobe. Such findings are usually associated with bronchogenic carcinomas.
Among the documentation from the transferring facility was a copy of a CT scan of the patient’s chest. On that study, the mass is seen; it appears to extend to the posterior chest wall, with extensive involvement and destruction of the ribs and posterior elements of T4 and T5. There is also evidence of some spinal cord compression, which would explain the patient’s presenting complaint.
Subsequent CT-guided biopsy demonstrated the lesion to be a non–small cell carcinoma. Due to the already extensive involvement, surgery was not an option, and the patient was referred for palliative radiation therapy.
ANSWER
The radiograph demonstrates a fairly large mass on the medial aspect of the left upper lobe. Such findings are usually associated with bronchogenic carcinomas.
Among the documentation from the transferring facility was a copy of a CT scan of the patient’s chest. On that study, the mass is seen; it appears to extend to the posterior chest wall, with extensive involvement and destruction of the ribs and posterior elements of T4 and T5. There is also evidence of some spinal cord compression, which would explain the patient’s presenting complaint.
Subsequent CT-guided biopsy demonstrated the lesion to be a non–small cell carcinoma. Due to the already extensive involvement, surgery was not an option, and the patient was referred for palliative radiation therapy.
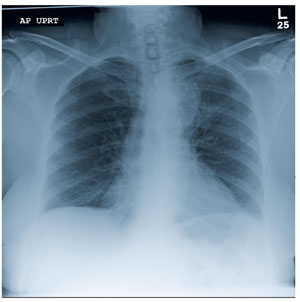
A 63-year-old woman is transferred to your facility for evaluation of acute lower extremity paralysis. She has had ongoing back pain for the past several months. Yesterday, she noticed her legs were dragging; last night, she was unable to walk, which prompted her trip to the local emergency department. She says she had “some sort of scan” there and was told that she had a tumor on her spine. She denies any injury or trauma. Her medical history is significant for reflux, hypertension, and extensive tobacco use. She is in no obvious distress, and her vital signs are normal. Physical exam demonstrates extreme weakness in both lower extremities, from the hips down and worse on the left side. She has decreased sensation and reflexes as well. As you review the rest of her transfer paperwork and try to find any imaging studies or reports, the radiology technician collects the patient for a chest radiograph (the result of which is shown). What is your impression?
Woman with Malaise, Cough, and Shoulder Pain
ANSWER
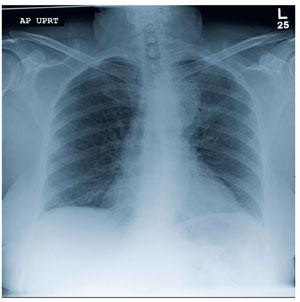
The radiograph demonstrates a slightly elevated left hemidiaphragm, which is nonspecific, as well as normal to slightly increased lung markings. There is no definite infiltrate or consolidation noted.
Of note, there is a displaced fracture of the mid-distal left clavicle, which may be partially healed. There appears to be a focal lytic lesion within that area. The surrounding bone is extremely osteopenic as well.
These findings, especially in the absence of injury or trauma, raise the question of a pathologic fracture, and further workup is warranted. Subsequent workup on this patient demonstrated a large renal mass, which was felt to be, most likely, a metastatic lesion.
ANSWER
The radiograph demonstrates a slightly elevated left hemidiaphragm, which is nonspecific, as well as normal to slightly increased lung markings. There is no definite infiltrate or consolidation noted.
Of note, there is a displaced fracture of the mid-distal left clavicle, which may be partially healed. There appears to be a focal lytic lesion within that area. The surrounding bone is extremely osteopenic as well.
These findings, especially in the absence of injury or trauma, raise the question of a pathologic fracture, and further workup is warranted. Subsequent workup on this patient demonstrated a large renal mass, which was felt to be, most likely, a metastatic lesion.
ANSWER
The radiograph demonstrates a slightly elevated left hemidiaphragm, which is nonspecific, as well as normal to slightly increased lung markings. There is no definite infiltrate or consolidation noted.
Of note, there is a displaced fracture of the mid-distal left clavicle, which may be partially healed. There appears to be a focal lytic lesion within that area. The surrounding bone is extremely osteopenic as well.
These findings, especially in the absence of injury or trauma, raise the question of a pathologic fracture, and further workup is warranted. Subsequent workup on this patient demonstrated a large renal mass, which was felt to be, most likely, a metastatic lesion.
A 63-year-old woman presents to your clinic with complaints of general malaise, weakness, and occasional cough—symptoms that started a couple of days ago. Also, her left shoulder has been hurting her “more than usual.” She denies any fever, chills, nausea, or vomiting. She admits to smoking two packs of cigarettes per day and having hypertension. Otherwise, her medical history is unremarkable. During the physical exam, you observe that the patient is an older female in no obvious distress. She is afebrile, and the rest of her vital signs, including pulse oximetry, are normal. Her breath sounds demonstrate scattered rhonchi but overall are clear. She does have localized tenderness over her left shoulder, with decreased range of motion in that arm secondary to the pain and stiffness in it. You send a blood sample to the lab to check her complete blood count and obtain a chest radiograph, which is shown. What is your impression?
Man Fell Off Roof
ANSWER
The radiograph shows a comminuted fracture of the os calcis, as well as a comminuted fracture of the navicular bone. CT on this patient was pending to further assess for additional fractures, and the patient will likely undergo open reduction and internal fixation for definitive treatment.
ANSWER
The radiograph shows a comminuted fracture of the os calcis, as well as a comminuted fracture of the navicular bone. CT on this patient was pending to further assess for additional fractures, and the patient will likely undergo open reduction and internal fixation for definitive treatment.
ANSWER
The radiograph shows a comminuted fracture of the os calcis, as well as a comminuted fracture of the navicular bone. CT on this patient was pending to further assess for additional fractures, and the patient will likely undergo open reduction and internal fixation for definitive treatment.

A 51-year-old man is brought to your facility for evaluation of right foot pain after sustaining a fall. He was working on top of his house when he lost his balance and fell approximately 15 to 20 feet. He states he landed on his feet and has the above complaint. His medical history is significant for hypertension and heart disease. He regularly works as a truck driver and smokes one to two packs of cigarettes per day. His exam shows a middle-aged male who is uncomfortable but in no obvious distress. Primary survey is normal. His right foot shows no obvious deformity. There is some swelling and moderate tenderness over the dorsal aspect, as well as in the area of the heel. Pulses are present, sensation is intact, and good capillary refill time is noted. Portable radiograph of the right foot is obtained. What is your impression?
Woman with Abdominal Pain Following Severe Car Crash
ANSWER
The radiograph shows a comminuted fracture at the midshaft of the tibia. In addition, there is a comminuted fracture of the proximal tibial metaphysis extending to the tibia plateau. Also noted is a comminuted fracture of the distal femur metaphysis extending to the intercondylar notch
ANSWER
The radiograph shows a comminuted fracture at the midshaft of the tibia. In addition, there is a comminuted fracture of the proximal tibial metaphysis extending to the tibia plateau. Also noted is a comminuted fracture of the distal femur metaphysis extending to the intercondylar notch
ANSWER
The radiograph shows a comminuted fracture at the midshaft of the tibia. In addition, there is a comminuted fracture of the proximal tibial metaphysis extending to the tibia plateau. Also noted is a comminuted fracture of the distal femur metaphysis extending to the intercondylar notch

A 43-year-old woman is airlifted to your facility from an outlying area following a severe motor vehicle collision. Details are unclear, but there were known fatalities at the scene. Her primary complaints are abdominal pain and noted deformities of the lower extremities, according to the transporting medical personnel. On arrival, she is noted to be semi-arousable and is moving distal portions of all four extremities. Her heart rate is 150 beats/min, with a blood pressure of 80/40 mm Hg. She responds to initial fluid and volume resuscitation. She has no pertinent medical history. Her response to the fluid resuscitation is sufficient to stabilize her for transport to the CT scanner for additional imaging. Prior to the transfer, though, a portable radiograph of her right tibia is obtained. What is your impression?
Man Run Over By Vehicle
ANSWER
The radiograph shows some deformity within the mid-to-distal diaphysis of both the radius and ulna; however, no acute fracture is seen. This is most likely related to remote trauma.
Of note, closer to the elbow, there are some small avulsion fractures near the area of the lateral epicondyle. The patient was treated with a posterior splint and referred to orthopedics.
ANSWER
The radiograph shows some deformity within the mid-to-distal diaphysis of both the radius and ulna; however, no acute fracture is seen. This is most likely related to remote trauma.
Of note, closer to the elbow, there are some small avulsion fractures near the area of the lateral epicondyle. The patient was treated with a posterior splint and referred to orthopedics.
ANSWER
The radiograph shows some deformity within the mid-to-distal diaphysis of both the radius and ulna; however, no acute fracture is seen. This is most likely related to remote trauma.
Of note, closer to the elbow, there are some small avulsion fractures near the area of the lateral epicondyle. The patient was treated with a posterior splint and referred to orthopedics.

After accidentally being run over by a vehicle, a 54-year-old man presents to the emergency department for evaluation of pain in his elbow and left arm. He was leaning down behind the vehicle and was not seen when the driver backed up. The patient states that one of the tires went over his left shoulder and arm. Primary complaint is pain and decreased range of motion. He denies any significant medical history, except for medication-controlled hypertension and gallbladder surgery. His vital signs are stable. Exammination of the left arm demonstrates some abrasions and contusions over the shoulder and forearm, as well as some swelling over the elbow. The patient has good color, distal pulses, and sensation. There is localized tenderness over the elbow and midforearm. Flexion of the elbow is somewhat limited secondary to pain. Radiograph of the forearm is obtained and shown. What is your impression?
Man with Debilitating Back Pain
ANSWER
The radiograph demonstrates generalized degenerative changes. Of note are fairly significant destructive changes in the endplate at the L3-4 level. Such changes are generally consistent with osteomyelitis and diskitis.
On further questioning, the patient reported that when he was admitted previously, he was told that he had an “infection in his back” and was treated with IV antibiotics. This patient was again admitted for additional workup and treatment.
ANSWER
The radiograph demonstrates generalized degenerative changes. Of note are fairly significant destructive changes in the endplate at the L3-4 level. Such changes are generally consistent with osteomyelitis and diskitis.
On further questioning, the patient reported that when he was admitted previously, he was told that he had an “infection in his back” and was treated with IV antibiotics. This patient was again admitted for additional workup and treatment.
ANSWER
The radiograph demonstrates generalized degenerative changes. Of note are fairly significant destructive changes in the endplate at the L3-4 level. Such changes are generally consistent with osteomyelitis and diskitis.
On further questioning, the patient reported that when he was admitted previously, he was told that he had an “infection in his back” and was treated with IV antibiotics. This patient was again admitted for additional workup and treatment.

A 54-year-old man presents with a complaint of a two-week history of severe low back pain. He denies any injury or trauma. The pain is so severe that it limits his ability to walk. He states he had similar episodes earlier this year, some of which required him to be admitted to the hospital. His medical history is significant for hypertension, diabetes, and coronary artery disease. He admits to recently having subjective fever and chills, as well as some nausea. Physical exam shows a deconditioned male who is uncomfortable but in no obvious distress. He is afebrile, with a blood pressure of 92/57 mm Hg, a heart rate of 97 beats/min, and a respiratory rate of 20 breaths/min. He has mild tenderness to his lumbosacral area; no deformity, step-off, or crepitus is appreciated. He does have decreased range of motion in his lower extremities, although this may be a consequence of his back pain. While trying to pull up his previous medical records, you order some basic labwork and lumbar spine radiographs. Lateral lumbar spine radiograph is shown; what is your impression?
Woman with Foot Pain After Neurosurgery Service
ANSWER
The radiograph demonstrates mild soft-tissue swelling and an oblique, mildly displaced fracture of the distal fibula. In addition, there is a small bone density adjacent to the medial malleolus, which could represent either an unfused accessory ossification center or a sequela of prior trauma.
On closer questioning, the patient acknowledged that a few months prior, she had stepped in a hole and been treated for a “broken bone.” She had been in a cast for an undisclosed period of time; at a follow-up appointment, the cast had been removed and the bone had been declared “healed.”
A new orthopedic consultation was obtained prior to the patient’s discharge from the hospital, which resulted in placement of a short leg cast.
ANSWER
The radiograph demonstrates mild soft-tissue swelling and an oblique, mildly displaced fracture of the distal fibula. In addition, there is a small bone density adjacent to the medial malleolus, which could represent either an unfused accessory ossification center or a sequela of prior trauma.
On closer questioning, the patient acknowledged that a few months prior, she had stepped in a hole and been treated for a “broken bone.” She had been in a cast for an undisclosed period of time; at a follow-up appointment, the cast had been removed and the bone had been declared “healed.”
A new orthopedic consultation was obtained prior to the patient’s discharge from the hospital, which resulted in placement of a short leg cast.
ANSWER
The radiograph demonstrates mild soft-tissue swelling and an oblique, mildly displaced fracture of the distal fibula. In addition, there is a small bone density adjacent to the medial malleolus, which could represent either an unfused accessory ossification center or a sequela of prior trauma.
On closer questioning, the patient acknowledged that a few months prior, she had stepped in a hole and been treated for a “broken bone.” She had been in a cast for an undisclosed period of time; at a follow-up appointment, the cast had been removed and the bone had been declared “healed.”
A new orthopedic consultation was obtained prior to the patient’s discharge from the hospital, which resulted in placement of a short leg cast.

A 60-year-old woman is admitted electively to the neurosurgery service for a multilevel posterior cervical decompression and fusion. The procedure is completed uneventfully and without complication. The patient is admitted to the neurosurgical floor. In the middle of the night, you receive a call from the nurse stating that the patient is complaining of moderate pain and swelling in her left ankle and foot, which occurred after she got up to use the bathroom. The patient denies injuring herself. She complains of pain with weight-bearing. Since the pain is tolerable and pain medication has already been given, it is decided to assess the complaint later in the morning. On evaluation, the left foot and ankle are mildly swollen, with tenderness on the lateral aspect. There is minimal tenderness on the foot. Distal pulses and color are good. The calf is nontender. The patient’s medical history is significant only for mild hypertension. Radiographs of the left ankle are obtained. What is your impression?
Dehydration Leads to Incidental Finding
ANSWER
The radiograph demonstrates that the nasogastric tube is within a decompressed stomach. Normal gas pattern is noted within the bowel and colon.
Of note, however, are tiny calcifications within the right upper quadrant. This finding is suggestive of cholelithiasis—in this case, likely an incidental finding.
ANSWER
The radiograph demonstrates that the nasogastric tube is within a decompressed stomach. Normal gas pattern is noted within the bowel and colon.
Of note, however, are tiny calcifications within the right upper quadrant. This finding is suggestive of cholelithiasis—in this case, likely an incidental finding.
ANSWER
The radiograph demonstrates that the nasogastric tube is within a decompressed stomach. Normal gas pattern is noted within the bowel and colon.
Of note, however, are tiny calcifications within the right upper quadrant. This finding is suggestive of cholelithiasis—in this case, likely an incidental finding.

A 57-year-old man is admitted to your facility for weakness and dehydration. His medical history is significant for rectal carcinoma, diabetes, and hypertension. His family states that his oral intake has been progressively less in the past several weeks. The patient’s vital signs are stable. Overall examination demonstrates a weak, frail-appearing man with dry mucous membranes and no other acute abnormalities. Lab work reveals that his serum sodium level and BUN/creatinine ratio are slightly elevated. To facilitate hydration, administration of medications, and nourishment, placement of a nasogastric tube is ordered; this is done just prior to your arrival at the patient’s room during rounds. As per protocol, an abdominal radiograph is obtained, and the nurses ask you to check it to confirm placement. The radiograph is shown. What is your impression?
Post PICC Placement
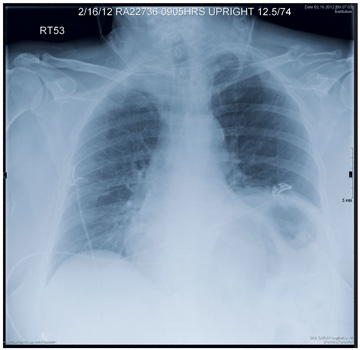
ANSWER
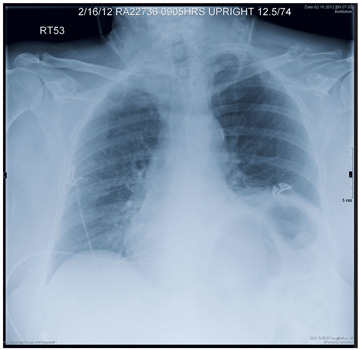
The radiograph demonstrates a right PICC line terminating at the superior vena cava. There is no evidence of pneumothorax.
Of note, however, is a large oval density within the right upper lobe, measuring 4.5 x 7 cm. This lesion could represent a loculated mass such as an abscess or hematoma. Further workup with additional imaging is warranted.
The working theory on this patient was that the density likely represented abscess or infection. Contrast-enhanced CT of the chest suggested likely abscess. The patient then underwent successful CT-guided needle biopsy, which returned positive results for Cryptococcus.
ANSWER
The radiograph demonstrates a right PICC line terminating at the superior vena cava. There is no evidence of pneumothorax.
Of note, however, is a large oval density within the right upper lobe, measuring 4.5 x 7 cm. This lesion could represent a loculated mass such as an abscess or hematoma. Further workup with additional imaging is warranted.
The working theory on this patient was that the density likely represented abscess or infection. Contrast-enhanced CT of the chest suggested likely abscess. The patient then underwent successful CT-guided needle biopsy, which returned positive results for Cryptococcus.
ANSWER
The radiograph demonstrates a right PICC line terminating at the superior vena cava. There is no evidence of pneumothorax.
Of note, however, is a large oval density within the right upper lobe, measuring 4.5 x 7 cm. This lesion could represent a loculated mass such as an abscess or hematoma. Further workup with additional imaging is warranted.
The working theory on this patient was that the density likely represented abscess or infection. Contrast-enhanced CT of the chest suggested likely abscess. The patient then underwent successful CT-guided needle biopsy, which returned positive results for Cryptococcus.

A 31-year-old man is admitted to your facility with presumed cryptococcal meningitis. He has a one-month history of progressively worsening headaches, malaise, weight loss, and blurred vision. A lumbar puncture demonstrates an extremely elevated opening pressure and yields samples that are positive for Cryptococcus on microscopic examination. The patient denies any significant medical history. Specifically, there is no history of HIV, which was confirmed by recent serologic testing at another hospital. As a result of poor peripheral access and with anticipated need for lengthy IV antifungal therapy, a PICC (peripherally inserted central catheter) line is ordered. It is placed without incident at the bedside, and as per protocol, a post-placement portable chest radiograph is obtained. What is your impression?