User login
Sneak Peek: Journal of Hospital Medicine
Background: Frailty, history of dementia (HoD), and acute confusional states (ACS) are common in older patients admitted to hospital.
Objective: To study the association of frailty (≥six points in the Clinical Frailty Scale [CFS]), HoD, and ACS with hospital outcomes, controlling for age, gender, acute illness severity (measured by a Modified Early Warning Score in the emergency department), comorbidity (Charlson Comorbidity Index), and discharging specialty (general medicine, geriatric medicine, surgery).
Design: Retrospective, observational study.
Setting: Large university hospital in England.
Patients: We analyzed 8,202 first nonelective inpatient episodes of people ages 75 years and older between October 2014 and October 2015.
Measurements: The outcomes studied were prolonged length of stay (LOS 10 days), inpatient mortality, delayed discharge, institutionalization, and 30-day readmission. Statistical analyses were based on multivariate regression models.
Results: Independently of controlling variables, prolonged LOS was predicted by CFS greater than or equal to 6: odds ratio (OR) = 1.55; 95% confidence interval (CI), 1.36-1.77; P less than .001; HOD: OR = 2.16; 95% CI, 1.79-2.61; P less than .001; and ACS: OR = 3.31; 95% CI, 2.64-4.15; P less than .001. Inpatient mortality was predicted by CFS greater than or equal to 6: OR = 2.29; 95% CI, 1.79-2.94, P less than .001. Delayed discharge was predicted by CFS greater than or equal to 6: OR = 1.46; 95% CI, 1.27-1.67; P less than .001; HOD: OR = 2.17; 95% CI, 1.80-2.62; P less than .001, and ACS: OR = 2.29; 95% CI: 1.83-2.85; P less than .001. Institutionalization was predicted by CFS greater than or equal to 6: OR=2.56; 95% CI, 2.09-3.14; P less than .001; HOD: OR = 2.51; 95% CI, 2.00-3.14; P less than .001; and ACS: OR = 1.93; 95% CI, 1.46-2.56; P less than .001. Readmission was predicted by ACS: OR = 1.36; 95% CI, 1.09-1.71; P = .006.
Conclusion: Routine screening for frailty, HoD, and ACS in hospitals may aid the development of acute care pathways for older adults.
Read the full article at journalofhospitalmedicine.com.
Also in JHM this month…
- Screening for Depression in Hospitalized Medical Patients
AUTHORS: Waguih William IsHak, MD, FAPA, Katherine Collison, Itai Danovitch, MD, MBA, Lili Shek, MD, Payam Kharazi, Tae Kim, DO Candidate, Karim Y. Jaffer, MD Candidate, Lancer Naghdechi, DO Candidate, Enrique Lopez, PsyD, Teryl Nuckols, MD, MSHS, FHM
- Patient-Level Exclusions from mHealth in a Safety-Net Health System
AUTHORS: Keiki Hinami, MD, MS, Bhrandon A. Harris, MD, Ricardo Uriostegui, MD, Wilnise Jasmin, MD, MBA, Mario Lopez, MD, William E. Trick, MD
- Medical and Economic Burden of Heparin-Induced Thrombocytopenia: A Retrospective Nationwide Inpatient Sample (NIS) Study
AUTHORS: Ranjan Pathak, MD, Vijaya Raj Bhatt, MD, Paras Karmacharya, MD, Madan Raj Aryal, MD, Anthony A. Donato, MD, MHPE
- Assessment of the Readability, Understandability and Completeness of Pediatric Hospital Medicine Discharge Instructions
AUTHORS: Ndidi I. Unaka, MD, Med, Angela Statile, MD, Med, Julianne Haney, Andrew F. Beck, MD, MPH, Patrick W. Brady, MD, MSc, Karen E. Jerardi, MD, MEd
- Impact of Patient-Centered Discharge Tools: A Systematic Review
AUTHORS: Karen Okrainec, MD, MSc, Davina Lau, BSc, Howard B Abrams, MD, Shoshanna Hahn-Goldberg, PhD, Ronak Brahmbhatt, MBBS, MPH, Tai Huynh, MBA, Kenneth Lam, MD, Chaim M Bell, MD, PhD
Background: Frailty, history of dementia (HoD), and acute confusional states (ACS) are common in older patients admitted to hospital.
Objective: To study the association of frailty (≥six points in the Clinical Frailty Scale [CFS]), HoD, and ACS with hospital outcomes, controlling for age, gender, acute illness severity (measured by a Modified Early Warning Score in the emergency department), comorbidity (Charlson Comorbidity Index), and discharging specialty (general medicine, geriatric medicine, surgery).
Design: Retrospective, observational study.
Setting: Large university hospital in England.
Patients: We analyzed 8,202 first nonelective inpatient episodes of people ages 75 years and older between October 2014 and October 2015.
Measurements: The outcomes studied were prolonged length of stay (LOS 10 days), inpatient mortality, delayed discharge, institutionalization, and 30-day readmission. Statistical analyses were based on multivariate regression models.
Results: Independently of controlling variables, prolonged LOS was predicted by CFS greater than or equal to 6: odds ratio (OR) = 1.55; 95% confidence interval (CI), 1.36-1.77; P less than .001; HOD: OR = 2.16; 95% CI, 1.79-2.61; P less than .001; and ACS: OR = 3.31; 95% CI, 2.64-4.15; P less than .001. Inpatient mortality was predicted by CFS greater than or equal to 6: OR = 2.29; 95% CI, 1.79-2.94, P less than .001. Delayed discharge was predicted by CFS greater than or equal to 6: OR = 1.46; 95% CI, 1.27-1.67; P less than .001; HOD: OR = 2.17; 95% CI, 1.80-2.62; P less than .001, and ACS: OR = 2.29; 95% CI: 1.83-2.85; P less than .001. Institutionalization was predicted by CFS greater than or equal to 6: OR=2.56; 95% CI, 2.09-3.14; P less than .001; HOD: OR = 2.51; 95% CI, 2.00-3.14; P less than .001; and ACS: OR = 1.93; 95% CI, 1.46-2.56; P less than .001. Readmission was predicted by ACS: OR = 1.36; 95% CI, 1.09-1.71; P = .006.
Conclusion: Routine screening for frailty, HoD, and ACS in hospitals may aid the development of acute care pathways for older adults.
Read the full article at journalofhospitalmedicine.com.
Also in JHM this month…
- Screening for Depression in Hospitalized Medical Patients
AUTHORS: Waguih William IsHak, MD, FAPA, Katherine Collison, Itai Danovitch, MD, MBA, Lili Shek, MD, Payam Kharazi, Tae Kim, DO Candidate, Karim Y. Jaffer, MD Candidate, Lancer Naghdechi, DO Candidate, Enrique Lopez, PsyD, Teryl Nuckols, MD, MSHS, FHM
- Patient-Level Exclusions from mHealth in a Safety-Net Health System
AUTHORS: Keiki Hinami, MD, MS, Bhrandon A. Harris, MD, Ricardo Uriostegui, MD, Wilnise Jasmin, MD, MBA, Mario Lopez, MD, William E. Trick, MD
- Medical and Economic Burden of Heparin-Induced Thrombocytopenia: A Retrospective Nationwide Inpatient Sample (NIS) Study
AUTHORS: Ranjan Pathak, MD, Vijaya Raj Bhatt, MD, Paras Karmacharya, MD, Madan Raj Aryal, MD, Anthony A. Donato, MD, MHPE
- Assessment of the Readability, Understandability and Completeness of Pediatric Hospital Medicine Discharge Instructions
AUTHORS: Ndidi I. Unaka, MD, Med, Angela Statile, MD, Med, Julianne Haney, Andrew F. Beck, MD, MPH, Patrick W. Brady, MD, MSc, Karen E. Jerardi, MD, MEd
- Impact of Patient-Centered Discharge Tools: A Systematic Review
AUTHORS: Karen Okrainec, MD, MSc, Davina Lau, BSc, Howard B Abrams, MD, Shoshanna Hahn-Goldberg, PhD, Ronak Brahmbhatt, MBBS, MPH, Tai Huynh, MBA, Kenneth Lam, MD, Chaim M Bell, MD, PhD
Background: Frailty, history of dementia (HoD), and acute confusional states (ACS) are common in older patients admitted to hospital.
Objective: To study the association of frailty (≥six points in the Clinical Frailty Scale [CFS]), HoD, and ACS with hospital outcomes, controlling for age, gender, acute illness severity (measured by a Modified Early Warning Score in the emergency department), comorbidity (Charlson Comorbidity Index), and discharging specialty (general medicine, geriatric medicine, surgery).
Design: Retrospective, observational study.
Setting: Large university hospital in England.
Patients: We analyzed 8,202 first nonelective inpatient episodes of people ages 75 years and older between October 2014 and October 2015.
Measurements: The outcomes studied were prolonged length of stay (LOS 10 days), inpatient mortality, delayed discharge, institutionalization, and 30-day readmission. Statistical analyses were based on multivariate regression models.
Results: Independently of controlling variables, prolonged LOS was predicted by CFS greater than or equal to 6: odds ratio (OR) = 1.55; 95% confidence interval (CI), 1.36-1.77; P less than .001; HOD: OR = 2.16; 95% CI, 1.79-2.61; P less than .001; and ACS: OR = 3.31; 95% CI, 2.64-4.15; P less than .001. Inpatient mortality was predicted by CFS greater than or equal to 6: OR = 2.29; 95% CI, 1.79-2.94, P less than .001. Delayed discharge was predicted by CFS greater than or equal to 6: OR = 1.46; 95% CI, 1.27-1.67; P less than .001; HOD: OR = 2.17; 95% CI, 1.80-2.62; P less than .001, and ACS: OR = 2.29; 95% CI: 1.83-2.85; P less than .001. Institutionalization was predicted by CFS greater than or equal to 6: OR=2.56; 95% CI, 2.09-3.14; P less than .001; HOD: OR = 2.51; 95% CI, 2.00-3.14; P less than .001; and ACS: OR = 1.93; 95% CI, 1.46-2.56; P less than .001. Readmission was predicted by ACS: OR = 1.36; 95% CI, 1.09-1.71; P = .006.
Conclusion: Routine screening for frailty, HoD, and ACS in hospitals may aid the development of acute care pathways for older adults.
Read the full article at journalofhospitalmedicine.com.
Also in JHM this month…
- Screening for Depression in Hospitalized Medical Patients
AUTHORS: Waguih William IsHak, MD, FAPA, Katherine Collison, Itai Danovitch, MD, MBA, Lili Shek, MD, Payam Kharazi, Tae Kim, DO Candidate, Karim Y. Jaffer, MD Candidate, Lancer Naghdechi, DO Candidate, Enrique Lopez, PsyD, Teryl Nuckols, MD, MSHS, FHM
- Patient-Level Exclusions from mHealth in a Safety-Net Health System
AUTHORS: Keiki Hinami, MD, MS, Bhrandon A. Harris, MD, Ricardo Uriostegui, MD, Wilnise Jasmin, MD, MBA, Mario Lopez, MD, William E. Trick, MD
- Medical and Economic Burden of Heparin-Induced Thrombocytopenia: A Retrospective Nationwide Inpatient Sample (NIS) Study
AUTHORS: Ranjan Pathak, MD, Vijaya Raj Bhatt, MD, Paras Karmacharya, MD, Madan Raj Aryal, MD, Anthony A. Donato, MD, MHPE
- Assessment of the Readability, Understandability and Completeness of Pediatric Hospital Medicine Discharge Instructions
AUTHORS: Ndidi I. Unaka, MD, Med, Angela Statile, MD, Med, Julianne Haney, Andrew F. Beck, MD, MPH, Patrick W. Brady, MD, MSc, Karen E. Jerardi, MD, MEd
- Impact of Patient-Centered Discharge Tools: A Systematic Review
AUTHORS: Karen Okrainec, MD, MSc, Davina Lau, BSc, Howard B Abrams, MD, Shoshanna Hahn-Goldberg, PhD, Ronak Brahmbhatt, MBBS, MPH, Tai Huynh, MBA, Kenneth Lam, MD, Chaim M Bell, MD, PhD
Have you Googled yourself lately?
The online rating business is proliferating in the medical industry. This should really come as no surprise as health care is a service industry and online ratings have long been a staple in most other service industries. It has become routine practice for most of us to search such online reviews when seeking a pair of shoes, a toaster, or a restaurant; we almost can’t help but scour these sites to help us make the best decision possible.
Not dissimilarly, patients these days seek care and make decisions by using a variety of inputs, including:
- Anticipated cost (is the physician or practice in or out of network?).
- Availability or access to the service (location of the practice and how long it will take to be seen).
- How good the services and care will be when they get there.
That same article found that for those who used online physician ratings, about one-third had selected a physician based on good ratings, and about one-third had avoided a physician based on poor ratings. So patients do seem to be paying attention to these sites and seeking or avoiding care based on what information they find.
Based on that evidence, it is not surprising that so many physician rating sites have sprung up; not only is there a market demand for the availability of this information, the rating sites are also profitable for the host companies. Vitals.com, for example, makes most of its revenue from advertisements and turns a sizable profit every year. Other profitable health care rating sites include Healthgrades, Yelp, Zocdoc, and WebMD.
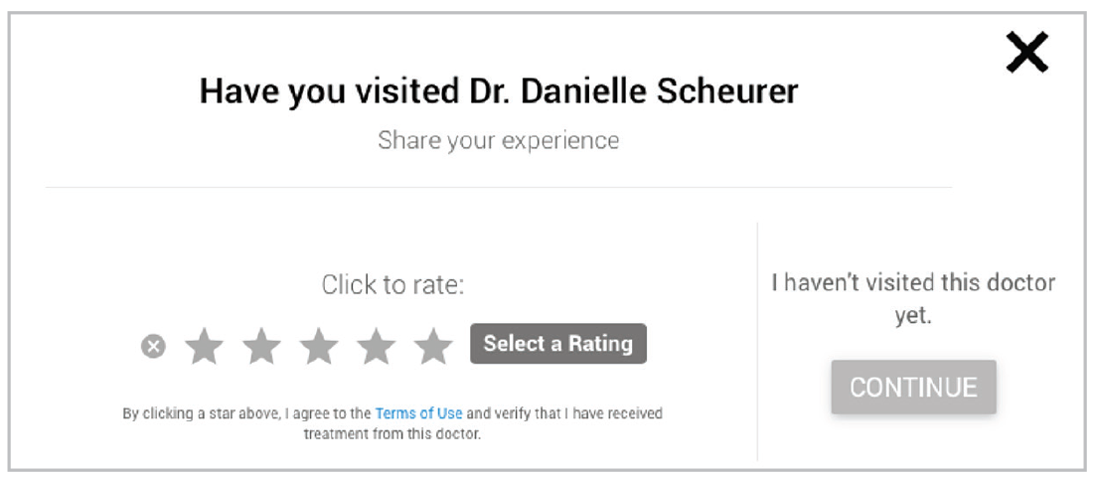
When I Google my own name, for example, Vitals.com is the first ratings website that appears in the search results. The first pop-up asks you to rate me and then it takes you to a site with all sorts of facts about me (most of which are notably inaccurate). If I had any online ratings (which I do not currently), you would then see my star ratings and any comments.
The second rating site that comes up for me via Google search is PhysicianWiki.com.There is a whole host of information on me (most of which is accurate), along with a set of personal ratings, including my office, my staff, and my waiting times (which, of course, do not make any sense given I am a hospitalist!). It is unclear how those ratings were generated or what volume of responses they represent.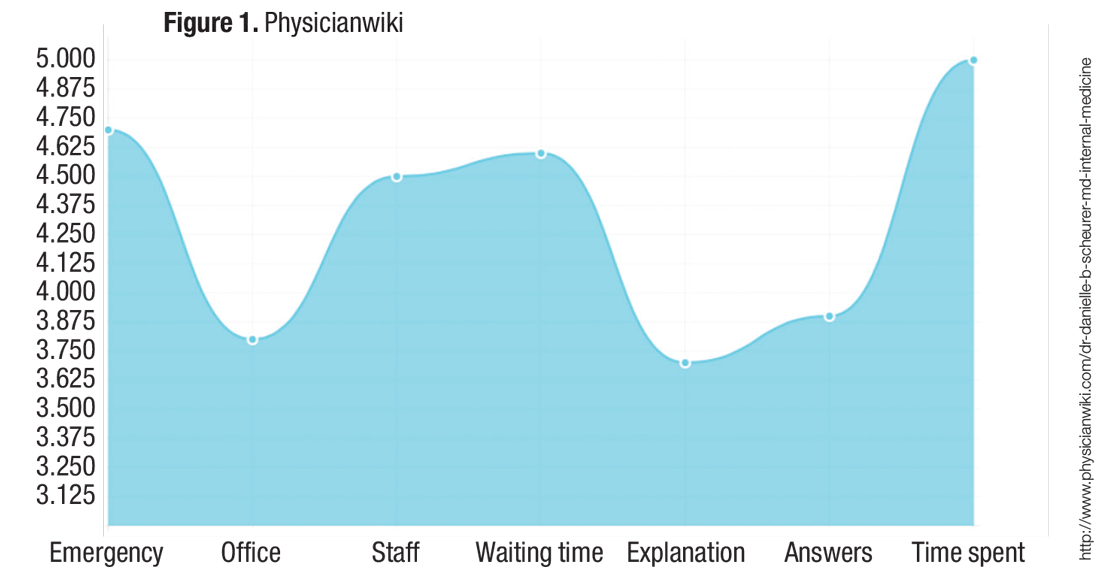
My health care system proposed rolling out a similar online rating system, and it was met with great skepticism from many physicians. There were two primary concerns:
- They felt it was “tacky” and that the profession of medicine should not be relegated to oversimplified service ratings. They worried that they would feel pressured to please the patient rather than “do the right thing” for the patient. For example, they would be less likely to give difficult advice (such as lose weight or stop smoking) or to resist prescribing medications that they deemed unnecessary or frankly dangerous (for example, antibiotics or narcotics).
Although these are valid concerns, it is hard to ignore the proliferation and traffic of these online websites. For you and your team, I would recommend taking a look at what is online about the members of your group and thinking about online strategies to take control of the conversation.
I don’t think the controversy over online physician ratings will wane anytime soon, but there is no doubt that they are profitable for companies and are therefore highly likely to continue to multiply.
References
1.Hanauer DA, Zheng K, Singer DC, Gebremariam A, Davis MM. Public awareness, perception, and use of online physician rating sites. JAMA. 2014;311(7):734-735. 2. A to Z provider listing: find a U of U Health Care physician by last name. University of Utah website. Available at http://healthcare.utah.edu/fad. Accessed Nov. 16, 2016.
Danielle Scheurer, MD, MSc, SFHM, is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
The online rating business is proliferating in the medical industry. This should really come as no surprise as health care is a service industry and online ratings have long been a staple in most other service industries. It has become routine practice for most of us to search such online reviews when seeking a pair of shoes, a toaster, or a restaurant; we almost can’t help but scour these sites to help us make the best decision possible.
Not dissimilarly, patients these days seek care and make decisions by using a variety of inputs, including:
- Anticipated cost (is the physician or practice in or out of network?).
- Availability or access to the service (location of the practice and how long it will take to be seen).
- How good the services and care will be when they get there.
That same article found that for those who used online physician ratings, about one-third had selected a physician based on good ratings, and about one-third had avoided a physician based on poor ratings. So patients do seem to be paying attention to these sites and seeking or avoiding care based on what information they find.
Based on that evidence, it is not surprising that so many physician rating sites have sprung up; not only is there a market demand for the availability of this information, the rating sites are also profitable for the host companies. Vitals.com, for example, makes most of its revenue from advertisements and turns a sizable profit every year. Other profitable health care rating sites include Healthgrades, Yelp, Zocdoc, and WebMD.
When I Google my own name, for example, Vitals.com is the first ratings website that appears in the search results. The first pop-up asks you to rate me and then it takes you to a site with all sorts of facts about me (most of which are notably inaccurate). If I had any online ratings (which I do not currently), you would then see my star ratings and any comments.
The second rating site that comes up for me via Google search is PhysicianWiki.com.There is a whole host of information on me (most of which is accurate), along with a set of personal ratings, including my office, my staff, and my waiting times (which, of course, do not make any sense given I am a hospitalist!). It is unclear how those ratings were generated or what volume of responses they represent.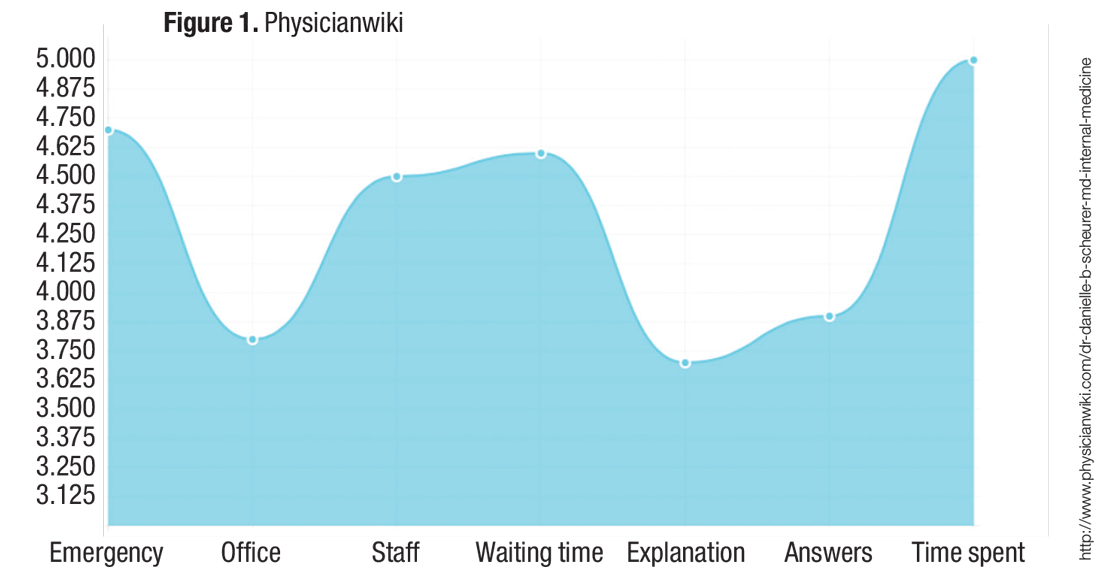
My health care system proposed rolling out a similar online rating system, and it was met with great skepticism from many physicians. There were two primary concerns:
- They felt it was “tacky” and that the profession of medicine should not be relegated to oversimplified service ratings. They worried that they would feel pressured to please the patient rather than “do the right thing” for the patient. For example, they would be less likely to give difficult advice (such as lose weight or stop smoking) or to resist prescribing medications that they deemed unnecessary or frankly dangerous (for example, antibiotics or narcotics).
Although these are valid concerns, it is hard to ignore the proliferation and traffic of these online websites. For you and your team, I would recommend taking a look at what is online about the members of your group and thinking about online strategies to take control of the conversation.
I don’t think the controversy over online physician ratings will wane anytime soon, but there is no doubt that they are profitable for companies and are therefore highly likely to continue to multiply.
References
1.Hanauer DA, Zheng K, Singer DC, Gebremariam A, Davis MM. Public awareness, perception, and use of online physician rating sites. JAMA. 2014;311(7):734-735. 2. A to Z provider listing: find a U of U Health Care physician by last name. University of Utah website. Available at http://healthcare.utah.edu/fad. Accessed Nov. 16, 2016.
Danielle Scheurer, MD, MSc, SFHM, is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
The online rating business is proliferating in the medical industry. This should really come as no surprise as health care is a service industry and online ratings have long been a staple in most other service industries. It has become routine practice for most of us to search such online reviews when seeking a pair of shoes, a toaster, or a restaurant; we almost can’t help but scour these sites to help us make the best decision possible.
Not dissimilarly, patients these days seek care and make decisions by using a variety of inputs, including:
- Anticipated cost (is the physician or practice in or out of network?).
- Availability or access to the service (location of the practice and how long it will take to be seen).
- How good the services and care will be when they get there.
That same article found that for those who used online physician ratings, about one-third had selected a physician based on good ratings, and about one-third had avoided a physician based on poor ratings. So patients do seem to be paying attention to these sites and seeking or avoiding care based on what information they find.
Based on that evidence, it is not surprising that so many physician rating sites have sprung up; not only is there a market demand for the availability of this information, the rating sites are also profitable for the host companies. Vitals.com, for example, makes most of its revenue from advertisements and turns a sizable profit every year. Other profitable health care rating sites include Healthgrades, Yelp, Zocdoc, and WebMD.
When I Google my own name, for example, Vitals.com is the first ratings website that appears in the search results. The first pop-up asks you to rate me and then it takes you to a site with all sorts of facts about me (most of which are notably inaccurate). If I had any online ratings (which I do not currently), you would then see my star ratings and any comments.
The second rating site that comes up for me via Google search is PhysicianWiki.com.There is a whole host of information on me (most of which is accurate), along with a set of personal ratings, including my office, my staff, and my waiting times (which, of course, do not make any sense given I am a hospitalist!). It is unclear how those ratings were generated or what volume of responses they represent.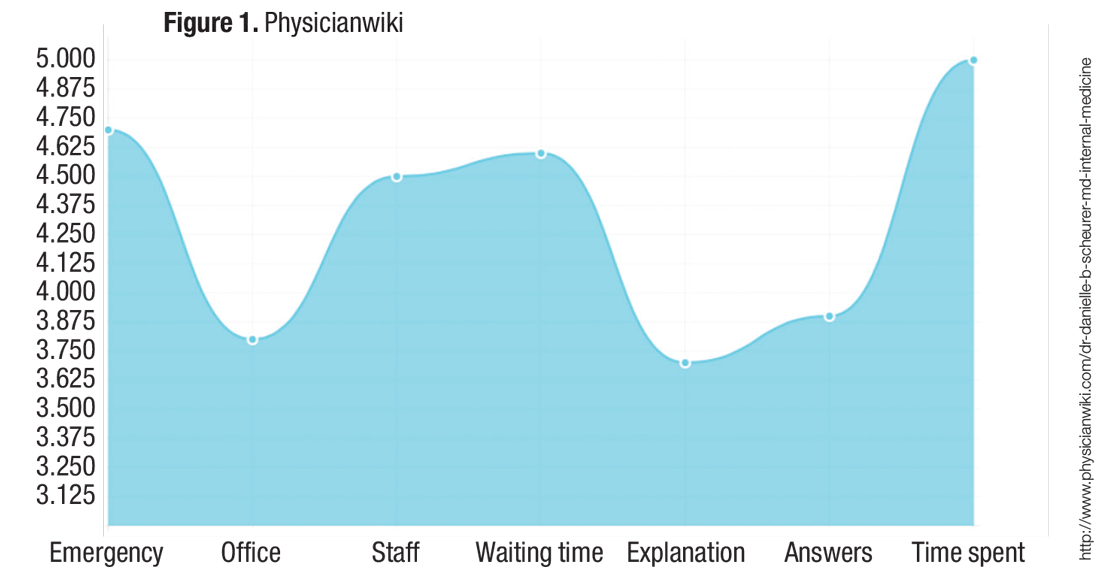
My health care system proposed rolling out a similar online rating system, and it was met with great skepticism from many physicians. There were two primary concerns:
- They felt it was “tacky” and that the profession of medicine should not be relegated to oversimplified service ratings. They worried that they would feel pressured to please the patient rather than “do the right thing” for the patient. For example, they would be less likely to give difficult advice (such as lose weight or stop smoking) or to resist prescribing medications that they deemed unnecessary or frankly dangerous (for example, antibiotics or narcotics).
Although these are valid concerns, it is hard to ignore the proliferation and traffic of these online websites. For you and your team, I would recommend taking a look at what is online about the members of your group and thinking about online strategies to take control of the conversation.
I don’t think the controversy over online physician ratings will wane anytime soon, but there is no doubt that they are profitable for companies and are therefore highly likely to continue to multiply.
References
1.Hanauer DA, Zheng K, Singer DC, Gebremariam A, Davis MM. Public awareness, perception, and use of online physician rating sites. JAMA. 2014;311(7):734-735. 2. A to Z provider listing: find a U of U Health Care physician by last name. University of Utah website. Available at http://healthcare.utah.edu/fad. Accessed Nov. 16, 2016.
Danielle Scheurer, MD, MSc, SFHM, is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
U.S. health care policy: What lies ahead?
The New Year brings new leadership in the United States, with President-elect Donald Trump taking office later this month. With a Republican-controlled Congress, party leaders have the opportunity to shape the nation’s policies around conservative ideals. This includes health care.
Since the Affordable Care Act (ACA) was passed in 2010, Republicans have vowed to repeal and replace it. This could be their opportunity.
However, “there is no clear coalescence around specific policy reforms that would replace the Affordable Care Act,” says Christine Eibner, PhD, a senior economist at Rand and a professor at the Pardee Rand Graduate School.
As a candidate, Trump did little to advance policy ideas around health care. Meanwhile, House Speaker Paul Ryan (R-Wis.) and others have, over the years, proposed reforms with which Trump may or may not agree.
“The Republicans now have a hard issue in their hands,” says Allison Hoffman, JD, professor of law at UCLA School of Law and an expert on health care law and policy. “It was hard before the Affordable Care Act, and it will be hard after. There is not an easy solution.”
By 2016, the ACA had expanded health coverage to 20 million people through Medicaid and private insurance on health care marketplaces. It extended the solvency of the Medicare Hospital Insurance Trust Fund. It accelerated the pace of delivery system and payment reform through creation of the Center for Medicare & Medicaid Innovation.
The law, however, has not been without its challenges.
“It was a strong achievement to get 20 million people insured, but it’s not clear that it bent the cost curve,” says Dr. Eibner. “There are high premiums on the individual market and still 31 million people without coverage. There is still opportunity to improve.”
Where we stand January 2017
Whether the Republicans can or will repeal the ACA in its entirety and improve it remains unknown. But, the experts say, the landmark law has left its mark on the American health care system.
“Everyone is complaining about the uncertainty created by the election, but we have been dealing with a highly uncertain environment for many years,” says Ron Greeno, MD, FCCP, MHM, senior advisor for medical affairs at TeamHealth, chair of the SHM Public Policy Committee, and SHM president-elect. “There will be changes, but things were going to change no matter the outcome of the election. It continues to require tolerance for change and tolerance for uncertainty.”
In an analysis for the Commonwealth Fund, Dr. Eibner investigated the economic implications of aspects of Trump’s plans as a candidate. Using a computer model that incorporates economic theory and data to simulate the effects of health policy changes, Dr. Eibner found that Trump’s plans (full repeal alone or repeal with tax deductions for health care premiums, Medicaid block grants, or selling health insurance across state lines) would increase the number of uninsured people by 16 million to 25 million, disproportionately impact low-income and sicker patients, expose individual market enrollees to higher out-of-pocket costs, and increase the federal deficit by $0.5 billion to $41 billion.1 The Congressional Budget Office (CBO) estimates full repeal could increase the federal deficit by $137 billion to $353 billion by 2025.2 Rep. Ryan’s plan, A Better Way, proposes providing people more control over their health care, giving tax credits instead of subsidies for premiums, capping the employer-sponsored health insurance tax exclusion, and expanding use of health savings accounts.3 However, Rep. Ryan’s plan “doesn’t reduce the cost of health care. It puts more onus on individuals, and their costs go up,” Ms. Hoffman says. “The weight of that will be more on people who have preexisting conditions.”
Joshua Lenchus, DO, RPh, FACP, SFHM, a member of SHM’s Public Policy Committee and hospitalist at the University of Miami/Jackson Memorial Hospital in Florida, is no fan of entitlement programs like Medicaid but says, “The safety-net hospital where I work would rather have people covered with something than nothing.”
Dr. Lenchus is optimistic that economic reforms under Trump will lead to more jobs, increasing the number of people covered by employer plans. “The economy drives health care reform,” he says. “He has to up his ante now and show people that he can stimulate job growth in this country so we don’t have this middle class that is continuously squeezed.”
Dr. Greeno and Ms. Hoffman, who is also a faculty associate at the UCLA Center for Health Policy Research and vice chair of the Insurance Law Section of the Association of American Law Schools, suggest hospitalists get involved as rules are being shaped and written.
“We want to help reform the delivery system, and we want it to be done right and to be done fairly. We want to have say in how our patients are treated,” Dr. Greeno says.
Key provisions: A delicate balance
Many people equate the ACA with the individual mandate, which requires nearly all Americans to purchase health insurance or pay a fine. The federal government provides subsidies to enrollees between 138% and 400% of the federal poverty level so their out-of-pocket costs never exceed a defined threshold even if premiums go up. These could be on the chopping block.
“The last bill Congress passed to repeal the Affordable Care Act, which Obama vetoed, repealed the individual mandate and subsidies for people to buy insurance,” Ms. Hoffman says. “If they do repeal it, private insurance through the exchanges will crumble.”
Mr. Trump’s tax deductions to offset premium costs are based on income, making them more generous for higher-income earners than low-income ones, Hoffman adds.
As a result, she says, people may choose high-deductible plans and face high out-of-pocket costs if they do seek care.
“It’s asking individuals to save by deciding how they’re going to ration care, where someone says they’re not going to go to the doctor today or fill a prescription drug they need,” Ms. Hoffman says.
Meanwhile, Mr. Trump has said he would like to keep the provision of the ACA that bans insurers from denying individuals with preexisting conditions. This, experts agree, may not be possible if other parts of the law are repealed and not replaced with similar protections for insurers.
“If you try to keep the rules about not including preexisting conditions and get rid of subsidies and the individual mandate, it just won’t work,” Ms. Hoffman says. “You end up with extraordinarily expensive health insurance.”
Rep. Ryan’s plan would prohibit insurers from denying patients with preexisting conditions but only if patients maintain continuous coverage, with a single open-enrollment period. He has promised to provide at least $25 billion in federal funding for state high-risk pools.
Prior to the passage of the ACA, 35 states offered high-risk pools to people excluded from the individual market. The Kaiser Family Foundation shows the net annual losses in these states averaged $5,510 per enrollee in 2011. Premiums ranged from 100% to 200% higher than non–high-risk group coverage. Government subsidies to cover losses amounted to $1 billion in each state.4
Meanwhile, both Mr. Trump and Rep. Ryan have proposed profound changes for Medicaid. Dr. Greeno calls this a “massive political challenge” unless they can provide an alternative way to cover people who currently rely on the federal-state entitlement, as well as those who gained coverage through ACA expansion. Currently, 70 million people are enrolled in Medicaid and the Children’s Health Insurance Program.5 Through Mr. Trump’s suggested block grants, states would receive a fixed amount of money to administer their program with increased flexibility. Rep. Ryan’s plan calls for enrollment caps that would distribute a dollar amount to each participant in the program with no limit on the number of enrollees. Either would be adjusted for inflation.
States could implement work requirements for beneficiaries or ask them to pay a small amount toward their premiums. Expansion states could also lower the Medicaid threshold below 138%.
Some states will struggle to provide for all their enrollees, Ms. Hoffman says, particularly since health spending generally outpaces inflation. Dr. Lenchus is more optimistic. “I believe states that didn’t expand Medicaid, one way or another, will figure out a way to deal with that population,” he says.
And … Medicare
The other entitlement program facing abrupt change is Medicare, typically considered the third rail of American politics.
“This is the hot political moment,” Ms. Hoffman says. “This is the point where the Republicans think they can tick off their wish list. For many Republicans, this kind of entitlement program is the opposite of what they believe in.”
Though Mr. Trump has said before he would not alter Medicare, he remained quiet on this point in the aftermath of the election. Repealing the ACA would affect Medicare by potentially reopening the Part D prescription drug doughnut hole and eliminating some of the savings provisions in the law. In fact, the CBO estimates Medicare’s direct spending would increase $802 billion between 2016 and 2025.1 Rep. Ryan has talked about privatizing Medicare by offering seniors who rely on it vouchers to apply toward private insurance.
“At the highest level, it’s moving Medicare from a defined benefit to a defined contribution program,” Ms. Hoffman says. “It shifts financial risk from the federal government onto beneficiaries. If Medicare spending continues to grow faster than the rest of the economy, Medicare beneficiaries will pay more and more.”
Seniors may also find themselves rationing or skimping on care.
Despite Rep. Ryan’s statements to the contrary, Medicare is not broken because of the ACA, Ms. Hoffman says. Its solvency has been prolonged, and though the reasons are not clear, Medicare spending has slowed since the passage of the ACA.6
MACRA launch
Another key factor in the health care policy landscape is MACRA, the Medicare Access and CHIP Reauthorization Act, which fundamentally shifts the way the government administrates and reimburses physicians for health care. MACRA begins in 2017. Dr. Greeno is concerned that changes to the ACA will impact the testing of payment models CMS is testing.
“There are hundreds of hospitals and thousands of physicians already invested in different models, so I don’t expect anybody has any desire to pull the rug from under physicians who are testing alternative payment models [APMs],” he says. “MACRA was passed on a strong bipartisan vote, and it created an APM track. Obviously, Congress intended APM models to continue to expand.”
Dr. Greeno says hospitalists are helping “shape these models,” working with the CMS and the Physician-Focused Payment Model Technical Advisory Committee (PTAC) “to ensure physicians participate in APMs and feel engaged rather than being a worker in a model someone else controls.”
On the campaign trail, Mr. Trump spoke of importing pharmaceuticals from overseas in an effort to control high prices. This policy is no longer part of his online plan. He also proposes allowing the sale of health insurance across state lines.
“It would be giving enrollees in states with stricter regulations the opportunity to circumvent to a looser state, which undermines the state with the stricter regulations,” Dr. Eibner says. “That would really create winners and losers. People who are healthy can buy a policy in a state with looser regulations, and their costs would likely fall. But someone sicker and older, it would be harder.”
Ms. Hoffman defines such a plan as a “race to the bottom.” Without well-established networks of physicians and hospitals, startup costs in new states are prohibitive, and many insurers may not wish to compete across state lines, she adds.
Repeal of the ACA could also limit some of the health benefits it required of plans on the individual market. For example, policymakers might be allowed to strip the contraceptive coverage regulation, which provides for free birth control.
“The reality is a lot of things changing in health care now were changing before the Affordable Care Act passed – PQRS, value-based purchasing, hospital-acquired infections,” Dr. Greeno says. “MACRA will continue the journey away from fee-for-service toward outcome-based models.”
At such a pivotal time, he strongly encourages hospitalists to join SHM if they are not already members and to get involved in SHM’s Grassroots Network.
“For a society of our age – young – and size, we’ve been tremendously impactful in helping with delivery system reform,” Dr. Greeno says. “I think it’s because we’re supporting change, not trying to stop it. We just want it to be intelligent change.”
He also is “convinced” hospitalists will be “critical to the redesign of the health care system. Since we are going to be taking care of the majority of hospitalized adult patients in hospitals, hospitalists want to have our say.”
Kelly April Tyrrell is a freelance writer in Madison, Wis.
References
1. Eibner C. Donald Trump’s health care reform proposals: Anticipated effects on insurance coverage, out-of-pocket costs, and the federal deficit. The Commonweath Fund website. Available at: http://www.commonwealthfund.org/publications/issue-briefs/2016/sep/trump-presidential-health-care-proposal. Accessed Nov. 17, 2016.
2. Budgetary and economic effects of repealing the Affordable Care Act. Congressional Budget Office website. Available at: https://www.cbo.gov/sites/default/files/114th-congress-2015-2016/reports/50252-Effects_of_ACA_Repeal.pdf. Accessed Nov. 15, 2016.
3. Our vision for a confident America. A Better Way website. Available at: http://abetterway.speaker.gov. Accessed Nov. 17, 2016.
4. Pollitz K. High-risk pools for uninsurable individuals. Kaiser Family Foundation website. Available at: http://kff.org/health-reform/issue-brief/high-risk-pools-for-uninsurable-individuals/. Accessed Nov. 17, 2016.
5. How accessible is individual health insurance for consumers in less-than-ideal health? Kaiser Family Foundation website. Available at: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/how-accessible-is-individual-health-insurance-for-consumer-in-less-than-perfect-health-report.pdf. Accessed Nov. 17, 2016.
6. The Affordable Care Act and Medicare. The Commonwealth Fund website. Available at: http://www.commonwealthfund.org/publications/fund-reports/2015/jun/medicare-affordable-care-act Accessed Nov. 17, 2016.
The New Year brings new leadership in the United States, with President-elect Donald Trump taking office later this month. With a Republican-controlled Congress, party leaders have the opportunity to shape the nation’s policies around conservative ideals. This includes health care.
Since the Affordable Care Act (ACA) was passed in 2010, Republicans have vowed to repeal and replace it. This could be their opportunity.
However, “there is no clear coalescence around specific policy reforms that would replace the Affordable Care Act,” says Christine Eibner, PhD, a senior economist at Rand and a professor at the Pardee Rand Graduate School.
As a candidate, Trump did little to advance policy ideas around health care. Meanwhile, House Speaker Paul Ryan (R-Wis.) and others have, over the years, proposed reforms with which Trump may or may not agree.
“The Republicans now have a hard issue in their hands,” says Allison Hoffman, JD, professor of law at UCLA School of Law and an expert on health care law and policy. “It was hard before the Affordable Care Act, and it will be hard after. There is not an easy solution.”
By 2016, the ACA had expanded health coverage to 20 million people through Medicaid and private insurance on health care marketplaces. It extended the solvency of the Medicare Hospital Insurance Trust Fund. It accelerated the pace of delivery system and payment reform through creation of the Center for Medicare & Medicaid Innovation.
The law, however, has not been without its challenges.
“It was a strong achievement to get 20 million people insured, but it’s not clear that it bent the cost curve,” says Dr. Eibner. “There are high premiums on the individual market and still 31 million people without coverage. There is still opportunity to improve.”
Where we stand January 2017
Whether the Republicans can or will repeal the ACA in its entirety and improve it remains unknown. But, the experts say, the landmark law has left its mark on the American health care system.
“Everyone is complaining about the uncertainty created by the election, but we have been dealing with a highly uncertain environment for many years,” says Ron Greeno, MD, FCCP, MHM, senior advisor for medical affairs at TeamHealth, chair of the SHM Public Policy Committee, and SHM president-elect. “There will be changes, but things were going to change no matter the outcome of the election. It continues to require tolerance for change and tolerance for uncertainty.”
In an analysis for the Commonwealth Fund, Dr. Eibner investigated the economic implications of aspects of Trump’s plans as a candidate. Using a computer model that incorporates economic theory and data to simulate the effects of health policy changes, Dr. Eibner found that Trump’s plans (full repeal alone or repeal with tax deductions for health care premiums, Medicaid block grants, or selling health insurance across state lines) would increase the number of uninsured people by 16 million to 25 million, disproportionately impact low-income and sicker patients, expose individual market enrollees to higher out-of-pocket costs, and increase the federal deficit by $0.5 billion to $41 billion.1 The Congressional Budget Office (CBO) estimates full repeal could increase the federal deficit by $137 billion to $353 billion by 2025.2 Rep. Ryan’s plan, A Better Way, proposes providing people more control over their health care, giving tax credits instead of subsidies for premiums, capping the employer-sponsored health insurance tax exclusion, and expanding use of health savings accounts.3 However, Rep. Ryan’s plan “doesn’t reduce the cost of health care. It puts more onus on individuals, and their costs go up,” Ms. Hoffman says. “The weight of that will be more on people who have preexisting conditions.”
Joshua Lenchus, DO, RPh, FACP, SFHM, a member of SHM’s Public Policy Committee and hospitalist at the University of Miami/Jackson Memorial Hospital in Florida, is no fan of entitlement programs like Medicaid but says, “The safety-net hospital where I work would rather have people covered with something than nothing.”
Dr. Lenchus is optimistic that economic reforms under Trump will lead to more jobs, increasing the number of people covered by employer plans. “The economy drives health care reform,” he says. “He has to up his ante now and show people that he can stimulate job growth in this country so we don’t have this middle class that is continuously squeezed.”
Dr. Greeno and Ms. Hoffman, who is also a faculty associate at the UCLA Center for Health Policy Research and vice chair of the Insurance Law Section of the Association of American Law Schools, suggest hospitalists get involved as rules are being shaped and written.
“We want to help reform the delivery system, and we want it to be done right and to be done fairly. We want to have say in how our patients are treated,” Dr. Greeno says.
Key provisions: A delicate balance
Many people equate the ACA with the individual mandate, which requires nearly all Americans to purchase health insurance or pay a fine. The federal government provides subsidies to enrollees between 138% and 400% of the federal poverty level so their out-of-pocket costs never exceed a defined threshold even if premiums go up. These could be on the chopping block.
“The last bill Congress passed to repeal the Affordable Care Act, which Obama vetoed, repealed the individual mandate and subsidies for people to buy insurance,” Ms. Hoffman says. “If they do repeal it, private insurance through the exchanges will crumble.”
Mr. Trump’s tax deductions to offset premium costs are based on income, making them more generous for higher-income earners than low-income ones, Hoffman adds.
As a result, she says, people may choose high-deductible plans and face high out-of-pocket costs if they do seek care.
“It’s asking individuals to save by deciding how they’re going to ration care, where someone says they’re not going to go to the doctor today or fill a prescription drug they need,” Ms. Hoffman says.
Meanwhile, Mr. Trump has said he would like to keep the provision of the ACA that bans insurers from denying individuals with preexisting conditions. This, experts agree, may not be possible if other parts of the law are repealed and not replaced with similar protections for insurers.
“If you try to keep the rules about not including preexisting conditions and get rid of subsidies and the individual mandate, it just won’t work,” Ms. Hoffman says. “You end up with extraordinarily expensive health insurance.”
Rep. Ryan’s plan would prohibit insurers from denying patients with preexisting conditions but only if patients maintain continuous coverage, with a single open-enrollment period. He has promised to provide at least $25 billion in federal funding for state high-risk pools.
Prior to the passage of the ACA, 35 states offered high-risk pools to people excluded from the individual market. The Kaiser Family Foundation shows the net annual losses in these states averaged $5,510 per enrollee in 2011. Premiums ranged from 100% to 200% higher than non–high-risk group coverage. Government subsidies to cover losses amounted to $1 billion in each state.4
Meanwhile, both Mr. Trump and Rep. Ryan have proposed profound changes for Medicaid. Dr. Greeno calls this a “massive political challenge” unless they can provide an alternative way to cover people who currently rely on the federal-state entitlement, as well as those who gained coverage through ACA expansion. Currently, 70 million people are enrolled in Medicaid and the Children’s Health Insurance Program.5 Through Mr. Trump’s suggested block grants, states would receive a fixed amount of money to administer their program with increased flexibility. Rep. Ryan’s plan calls for enrollment caps that would distribute a dollar amount to each participant in the program with no limit on the number of enrollees. Either would be adjusted for inflation.
States could implement work requirements for beneficiaries or ask them to pay a small amount toward their premiums. Expansion states could also lower the Medicaid threshold below 138%.
Some states will struggle to provide for all their enrollees, Ms. Hoffman says, particularly since health spending generally outpaces inflation. Dr. Lenchus is more optimistic. “I believe states that didn’t expand Medicaid, one way or another, will figure out a way to deal with that population,” he says.
And … Medicare
The other entitlement program facing abrupt change is Medicare, typically considered the third rail of American politics.
“This is the hot political moment,” Ms. Hoffman says. “This is the point where the Republicans think they can tick off their wish list. For many Republicans, this kind of entitlement program is the opposite of what they believe in.”
Though Mr. Trump has said before he would not alter Medicare, he remained quiet on this point in the aftermath of the election. Repealing the ACA would affect Medicare by potentially reopening the Part D prescription drug doughnut hole and eliminating some of the savings provisions in the law. In fact, the CBO estimates Medicare’s direct spending would increase $802 billion between 2016 and 2025.1 Rep. Ryan has talked about privatizing Medicare by offering seniors who rely on it vouchers to apply toward private insurance.
“At the highest level, it’s moving Medicare from a defined benefit to a defined contribution program,” Ms. Hoffman says. “It shifts financial risk from the federal government onto beneficiaries. If Medicare spending continues to grow faster than the rest of the economy, Medicare beneficiaries will pay more and more.”
Seniors may also find themselves rationing or skimping on care.
Despite Rep. Ryan’s statements to the contrary, Medicare is not broken because of the ACA, Ms. Hoffman says. Its solvency has been prolonged, and though the reasons are not clear, Medicare spending has slowed since the passage of the ACA.6
MACRA launch
Another key factor in the health care policy landscape is MACRA, the Medicare Access and CHIP Reauthorization Act, which fundamentally shifts the way the government administrates and reimburses physicians for health care. MACRA begins in 2017. Dr. Greeno is concerned that changes to the ACA will impact the testing of payment models CMS is testing.
“There are hundreds of hospitals and thousands of physicians already invested in different models, so I don’t expect anybody has any desire to pull the rug from under physicians who are testing alternative payment models [APMs],” he says. “MACRA was passed on a strong bipartisan vote, and it created an APM track. Obviously, Congress intended APM models to continue to expand.”
Dr. Greeno says hospitalists are helping “shape these models,” working with the CMS and the Physician-Focused Payment Model Technical Advisory Committee (PTAC) “to ensure physicians participate in APMs and feel engaged rather than being a worker in a model someone else controls.”
On the campaign trail, Mr. Trump spoke of importing pharmaceuticals from overseas in an effort to control high prices. This policy is no longer part of his online plan. He also proposes allowing the sale of health insurance across state lines.
“It would be giving enrollees in states with stricter regulations the opportunity to circumvent to a looser state, which undermines the state with the stricter regulations,” Dr. Eibner says. “That would really create winners and losers. People who are healthy can buy a policy in a state with looser regulations, and their costs would likely fall. But someone sicker and older, it would be harder.”
Ms. Hoffman defines such a plan as a “race to the bottom.” Without well-established networks of physicians and hospitals, startup costs in new states are prohibitive, and many insurers may not wish to compete across state lines, she adds.
Repeal of the ACA could also limit some of the health benefits it required of plans on the individual market. For example, policymakers might be allowed to strip the contraceptive coverage regulation, which provides for free birth control.
“The reality is a lot of things changing in health care now were changing before the Affordable Care Act passed – PQRS, value-based purchasing, hospital-acquired infections,” Dr. Greeno says. “MACRA will continue the journey away from fee-for-service toward outcome-based models.”
At such a pivotal time, he strongly encourages hospitalists to join SHM if they are not already members and to get involved in SHM’s Grassroots Network.
“For a society of our age – young – and size, we’ve been tremendously impactful in helping with delivery system reform,” Dr. Greeno says. “I think it’s because we’re supporting change, not trying to stop it. We just want it to be intelligent change.”
He also is “convinced” hospitalists will be “critical to the redesign of the health care system. Since we are going to be taking care of the majority of hospitalized adult patients in hospitals, hospitalists want to have our say.”
Kelly April Tyrrell is a freelance writer in Madison, Wis.
References
1. Eibner C. Donald Trump’s health care reform proposals: Anticipated effects on insurance coverage, out-of-pocket costs, and the federal deficit. The Commonweath Fund website. Available at: http://www.commonwealthfund.org/publications/issue-briefs/2016/sep/trump-presidential-health-care-proposal. Accessed Nov. 17, 2016.
2. Budgetary and economic effects of repealing the Affordable Care Act. Congressional Budget Office website. Available at: https://www.cbo.gov/sites/default/files/114th-congress-2015-2016/reports/50252-Effects_of_ACA_Repeal.pdf. Accessed Nov. 15, 2016.
3. Our vision for a confident America. A Better Way website. Available at: http://abetterway.speaker.gov. Accessed Nov. 17, 2016.
4. Pollitz K. High-risk pools for uninsurable individuals. Kaiser Family Foundation website. Available at: http://kff.org/health-reform/issue-brief/high-risk-pools-for-uninsurable-individuals/. Accessed Nov. 17, 2016.
5. How accessible is individual health insurance for consumers in less-than-ideal health? Kaiser Family Foundation website. Available at: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/how-accessible-is-individual-health-insurance-for-consumer-in-less-than-perfect-health-report.pdf. Accessed Nov. 17, 2016.
6. The Affordable Care Act and Medicare. The Commonwealth Fund website. Available at: http://www.commonwealthfund.org/publications/fund-reports/2015/jun/medicare-affordable-care-act Accessed Nov. 17, 2016.
The New Year brings new leadership in the United States, with President-elect Donald Trump taking office later this month. With a Republican-controlled Congress, party leaders have the opportunity to shape the nation’s policies around conservative ideals. This includes health care.
Since the Affordable Care Act (ACA) was passed in 2010, Republicans have vowed to repeal and replace it. This could be their opportunity.
However, “there is no clear coalescence around specific policy reforms that would replace the Affordable Care Act,” says Christine Eibner, PhD, a senior economist at Rand and a professor at the Pardee Rand Graduate School.
As a candidate, Trump did little to advance policy ideas around health care. Meanwhile, House Speaker Paul Ryan (R-Wis.) and others have, over the years, proposed reforms with which Trump may or may not agree.
“The Republicans now have a hard issue in their hands,” says Allison Hoffman, JD, professor of law at UCLA School of Law and an expert on health care law and policy. “It was hard before the Affordable Care Act, and it will be hard after. There is not an easy solution.”
By 2016, the ACA had expanded health coverage to 20 million people through Medicaid and private insurance on health care marketplaces. It extended the solvency of the Medicare Hospital Insurance Trust Fund. It accelerated the pace of delivery system and payment reform through creation of the Center for Medicare & Medicaid Innovation.
The law, however, has not been without its challenges.
“It was a strong achievement to get 20 million people insured, but it’s not clear that it bent the cost curve,” says Dr. Eibner. “There are high premiums on the individual market and still 31 million people without coverage. There is still opportunity to improve.”
Where we stand January 2017
Whether the Republicans can or will repeal the ACA in its entirety and improve it remains unknown. But, the experts say, the landmark law has left its mark on the American health care system.
“Everyone is complaining about the uncertainty created by the election, but we have been dealing with a highly uncertain environment for many years,” says Ron Greeno, MD, FCCP, MHM, senior advisor for medical affairs at TeamHealth, chair of the SHM Public Policy Committee, and SHM president-elect. “There will be changes, but things were going to change no matter the outcome of the election. It continues to require tolerance for change and tolerance for uncertainty.”
In an analysis for the Commonwealth Fund, Dr. Eibner investigated the economic implications of aspects of Trump’s plans as a candidate. Using a computer model that incorporates economic theory and data to simulate the effects of health policy changes, Dr. Eibner found that Trump’s plans (full repeal alone or repeal with tax deductions for health care premiums, Medicaid block grants, or selling health insurance across state lines) would increase the number of uninsured people by 16 million to 25 million, disproportionately impact low-income and sicker patients, expose individual market enrollees to higher out-of-pocket costs, and increase the federal deficit by $0.5 billion to $41 billion.1 The Congressional Budget Office (CBO) estimates full repeal could increase the federal deficit by $137 billion to $353 billion by 2025.2 Rep. Ryan’s plan, A Better Way, proposes providing people more control over their health care, giving tax credits instead of subsidies for premiums, capping the employer-sponsored health insurance tax exclusion, and expanding use of health savings accounts.3 However, Rep. Ryan’s plan “doesn’t reduce the cost of health care. It puts more onus on individuals, and their costs go up,” Ms. Hoffman says. “The weight of that will be more on people who have preexisting conditions.”
Joshua Lenchus, DO, RPh, FACP, SFHM, a member of SHM’s Public Policy Committee and hospitalist at the University of Miami/Jackson Memorial Hospital in Florida, is no fan of entitlement programs like Medicaid but says, “The safety-net hospital where I work would rather have people covered with something than nothing.”
Dr. Lenchus is optimistic that economic reforms under Trump will lead to more jobs, increasing the number of people covered by employer plans. “The economy drives health care reform,” he says. “He has to up his ante now and show people that he can stimulate job growth in this country so we don’t have this middle class that is continuously squeezed.”
Dr. Greeno and Ms. Hoffman, who is also a faculty associate at the UCLA Center for Health Policy Research and vice chair of the Insurance Law Section of the Association of American Law Schools, suggest hospitalists get involved as rules are being shaped and written.
“We want to help reform the delivery system, and we want it to be done right and to be done fairly. We want to have say in how our patients are treated,” Dr. Greeno says.
Key provisions: A delicate balance
Many people equate the ACA with the individual mandate, which requires nearly all Americans to purchase health insurance or pay a fine. The federal government provides subsidies to enrollees between 138% and 400% of the federal poverty level so their out-of-pocket costs never exceed a defined threshold even if premiums go up. These could be on the chopping block.
“The last bill Congress passed to repeal the Affordable Care Act, which Obama vetoed, repealed the individual mandate and subsidies for people to buy insurance,” Ms. Hoffman says. “If they do repeal it, private insurance through the exchanges will crumble.”
Mr. Trump’s tax deductions to offset premium costs are based on income, making them more generous for higher-income earners than low-income ones, Hoffman adds.
As a result, she says, people may choose high-deductible plans and face high out-of-pocket costs if they do seek care.
“It’s asking individuals to save by deciding how they’re going to ration care, where someone says they’re not going to go to the doctor today or fill a prescription drug they need,” Ms. Hoffman says.
Meanwhile, Mr. Trump has said he would like to keep the provision of the ACA that bans insurers from denying individuals with preexisting conditions. This, experts agree, may not be possible if other parts of the law are repealed and not replaced with similar protections for insurers.
“If you try to keep the rules about not including preexisting conditions and get rid of subsidies and the individual mandate, it just won’t work,” Ms. Hoffman says. “You end up with extraordinarily expensive health insurance.”
Rep. Ryan’s plan would prohibit insurers from denying patients with preexisting conditions but only if patients maintain continuous coverage, with a single open-enrollment period. He has promised to provide at least $25 billion in federal funding for state high-risk pools.
Prior to the passage of the ACA, 35 states offered high-risk pools to people excluded from the individual market. The Kaiser Family Foundation shows the net annual losses in these states averaged $5,510 per enrollee in 2011. Premiums ranged from 100% to 200% higher than non–high-risk group coverage. Government subsidies to cover losses amounted to $1 billion in each state.4
Meanwhile, both Mr. Trump and Rep. Ryan have proposed profound changes for Medicaid. Dr. Greeno calls this a “massive political challenge” unless they can provide an alternative way to cover people who currently rely on the federal-state entitlement, as well as those who gained coverage through ACA expansion. Currently, 70 million people are enrolled in Medicaid and the Children’s Health Insurance Program.5 Through Mr. Trump’s suggested block grants, states would receive a fixed amount of money to administer their program with increased flexibility. Rep. Ryan’s plan calls for enrollment caps that would distribute a dollar amount to each participant in the program with no limit on the number of enrollees. Either would be adjusted for inflation.
States could implement work requirements for beneficiaries or ask them to pay a small amount toward their premiums. Expansion states could also lower the Medicaid threshold below 138%.
Some states will struggle to provide for all their enrollees, Ms. Hoffman says, particularly since health spending generally outpaces inflation. Dr. Lenchus is more optimistic. “I believe states that didn’t expand Medicaid, one way or another, will figure out a way to deal with that population,” he says.
And … Medicare
The other entitlement program facing abrupt change is Medicare, typically considered the third rail of American politics.
“This is the hot political moment,” Ms. Hoffman says. “This is the point where the Republicans think they can tick off their wish list. For many Republicans, this kind of entitlement program is the opposite of what they believe in.”
Though Mr. Trump has said before he would not alter Medicare, he remained quiet on this point in the aftermath of the election. Repealing the ACA would affect Medicare by potentially reopening the Part D prescription drug doughnut hole and eliminating some of the savings provisions in the law. In fact, the CBO estimates Medicare’s direct spending would increase $802 billion between 2016 and 2025.1 Rep. Ryan has talked about privatizing Medicare by offering seniors who rely on it vouchers to apply toward private insurance.
“At the highest level, it’s moving Medicare from a defined benefit to a defined contribution program,” Ms. Hoffman says. “It shifts financial risk from the federal government onto beneficiaries. If Medicare spending continues to grow faster than the rest of the economy, Medicare beneficiaries will pay more and more.”
Seniors may also find themselves rationing or skimping on care.
Despite Rep. Ryan’s statements to the contrary, Medicare is not broken because of the ACA, Ms. Hoffman says. Its solvency has been prolonged, and though the reasons are not clear, Medicare spending has slowed since the passage of the ACA.6
MACRA launch
Another key factor in the health care policy landscape is MACRA, the Medicare Access and CHIP Reauthorization Act, which fundamentally shifts the way the government administrates and reimburses physicians for health care. MACRA begins in 2017. Dr. Greeno is concerned that changes to the ACA will impact the testing of payment models CMS is testing.
“There are hundreds of hospitals and thousands of physicians already invested in different models, so I don’t expect anybody has any desire to pull the rug from under physicians who are testing alternative payment models [APMs],” he says. “MACRA was passed on a strong bipartisan vote, and it created an APM track. Obviously, Congress intended APM models to continue to expand.”
Dr. Greeno says hospitalists are helping “shape these models,” working with the CMS and the Physician-Focused Payment Model Technical Advisory Committee (PTAC) “to ensure physicians participate in APMs and feel engaged rather than being a worker in a model someone else controls.”
On the campaign trail, Mr. Trump spoke of importing pharmaceuticals from overseas in an effort to control high prices. This policy is no longer part of his online plan. He also proposes allowing the sale of health insurance across state lines.
“It would be giving enrollees in states with stricter regulations the opportunity to circumvent to a looser state, which undermines the state with the stricter regulations,” Dr. Eibner says. “That would really create winners and losers. People who are healthy can buy a policy in a state with looser regulations, and their costs would likely fall. But someone sicker and older, it would be harder.”
Ms. Hoffman defines such a plan as a “race to the bottom.” Without well-established networks of physicians and hospitals, startup costs in new states are prohibitive, and many insurers may not wish to compete across state lines, she adds.
Repeal of the ACA could also limit some of the health benefits it required of plans on the individual market. For example, policymakers might be allowed to strip the contraceptive coverage regulation, which provides for free birth control.
“The reality is a lot of things changing in health care now were changing before the Affordable Care Act passed – PQRS, value-based purchasing, hospital-acquired infections,” Dr. Greeno says. “MACRA will continue the journey away from fee-for-service toward outcome-based models.”
At such a pivotal time, he strongly encourages hospitalists to join SHM if they are not already members and to get involved in SHM’s Grassroots Network.
“For a society of our age – young – and size, we’ve been tremendously impactful in helping with delivery system reform,” Dr. Greeno says. “I think it’s because we’re supporting change, not trying to stop it. We just want it to be intelligent change.”
He also is “convinced” hospitalists will be “critical to the redesign of the health care system. Since we are going to be taking care of the majority of hospitalized adult patients in hospitals, hospitalists want to have our say.”
Kelly April Tyrrell is a freelance writer in Madison, Wis.
References
1. Eibner C. Donald Trump’s health care reform proposals: Anticipated effects on insurance coverage, out-of-pocket costs, and the federal deficit. The Commonweath Fund website. Available at: http://www.commonwealthfund.org/publications/issue-briefs/2016/sep/trump-presidential-health-care-proposal. Accessed Nov. 17, 2016.
2. Budgetary and economic effects of repealing the Affordable Care Act. Congressional Budget Office website. Available at: https://www.cbo.gov/sites/default/files/114th-congress-2015-2016/reports/50252-Effects_of_ACA_Repeal.pdf. Accessed Nov. 15, 2016.
3. Our vision for a confident America. A Better Way website. Available at: http://abetterway.speaker.gov. Accessed Nov. 17, 2016.
4. Pollitz K. High-risk pools for uninsurable individuals. Kaiser Family Foundation website. Available at: http://kff.org/health-reform/issue-brief/high-risk-pools-for-uninsurable-individuals/. Accessed Nov. 17, 2016.
5. How accessible is individual health insurance for consumers in less-than-ideal health? Kaiser Family Foundation website. Available at: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/how-accessible-is-individual-health-insurance-for-consumer-in-less-than-perfect-health-report.pdf. Accessed Nov. 17, 2016.
6. The Affordable Care Act and Medicare. The Commonwealth Fund website. Available at: http://www.commonwealthfund.org/publications/fund-reports/2015/jun/medicare-affordable-care-act Accessed Nov. 17, 2016.
Nonischemic cardiomyopathy does not benefit from prophylactic ICDs
Clinical question: Do prophylactic implantable cardioverter defibrillators (ICDs) reduce long-term mortality in patients with symptomatic nonischemic systolic heart failure (NISHF)?
Study design: Multicenter, nonblinded, randomized controlled prospective trial.
Setting: Danish ICD centers.
Synopsis: A total of 1,116 patients with symptomatic NISHF (left ventricular ejection fraction of less than 35%) were randomized to either receive an ICD or usual clinical care. The primary outcome, death from any cause, occurred in 120 patients (21.6%) in the ICD group (4.4 events/100 person-years) and in 131 patients (23.4%) in the control group. The hazard ratio for death from any cause in the ICD group, as compared with the control group, was 0.87 (95% CI , 0.68-1.12; P = .28). The HR for death from any cause in the ICD group, as compared with the control group, was 0.87 (95% CI, 0.68-1.12; P = .28)
Bottom line: Prophylactic ICD implantation in patients with symptomatic NISHF does not reduce long-term mortality.
Citation: Kober L, Thune JJ, Nielsen JC, et al. Defibrillator implantation in patients with nonischemic systolic heart failure. N Engl J Med. 2016;375:1221-1230.
Clinical question: Do prophylactic implantable cardioverter defibrillators (ICDs) reduce long-term mortality in patients with symptomatic nonischemic systolic heart failure (NISHF)?
Study design: Multicenter, nonblinded, randomized controlled prospective trial.
Setting: Danish ICD centers.
Synopsis: A total of 1,116 patients with symptomatic NISHF (left ventricular ejection fraction of less than 35%) were randomized to either receive an ICD or usual clinical care. The primary outcome, death from any cause, occurred in 120 patients (21.6%) in the ICD group (4.4 events/100 person-years) and in 131 patients (23.4%) in the control group. The hazard ratio for death from any cause in the ICD group, as compared with the control group, was 0.87 (95% CI , 0.68-1.12; P = .28). The HR for death from any cause in the ICD group, as compared with the control group, was 0.87 (95% CI, 0.68-1.12; P = .28)
Bottom line: Prophylactic ICD implantation in patients with symptomatic NISHF does not reduce long-term mortality.
Citation: Kober L, Thune JJ, Nielsen JC, et al. Defibrillator implantation in patients with nonischemic systolic heart failure. N Engl J Med. 2016;375:1221-1230.
Clinical question: Do prophylactic implantable cardioverter defibrillators (ICDs) reduce long-term mortality in patients with symptomatic nonischemic systolic heart failure (NISHF)?
Study design: Multicenter, nonblinded, randomized controlled prospective trial.
Setting: Danish ICD centers.
Synopsis: A total of 1,116 patients with symptomatic NISHF (left ventricular ejection fraction of less than 35%) were randomized to either receive an ICD or usual clinical care. The primary outcome, death from any cause, occurred in 120 patients (21.6%) in the ICD group (4.4 events/100 person-years) and in 131 patients (23.4%) in the control group. The hazard ratio for death from any cause in the ICD group, as compared with the control group, was 0.87 (95% CI , 0.68-1.12; P = .28). The HR for death from any cause in the ICD group, as compared with the control group, was 0.87 (95% CI, 0.68-1.12; P = .28)
Bottom line: Prophylactic ICD implantation in patients with symptomatic NISHF does not reduce long-term mortality.
Citation: Kober L, Thune JJ, Nielsen JC, et al. Defibrillator implantation in patients with nonischemic systolic heart failure. N Engl J Med. 2016;375:1221-1230.
Everything We Say and Do
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I inform my patients that I have reviewed their chart and that I am familiar with their diagnosis.
Why I do it
In the hospital setting, in particular, patients are concerned about communication between their various healthcare professionals. Many times, the patient’s primary-care provider works strictly in the outpatient setting, so the hospitalist is the person who assumes total care of the patient throughout hospitalization. This understandably creates anxiety for patients and families because they wonder if the hospitalist really knows their medical history. One way to alleviate this anxiety is to review your patients’ charts prior to speaking with them and to verbally let your patients know you are familiar with their diagnoses.
How I do it
Step 1: Before entering the room, I review my patient’s chart. If I am taking over the service from my colleague, I review all notes from the current hospitalization to ensure I understand everything that has happened. I also review tests, procedures, and radiographic studies. To gain a better understanding of my patient, I read the most recent discharge summary and outpatient clinic note. Likewise, if I am admitting a new patient to the hospital, before entering the room to do the history and physical examination, I review recent hospitalizations, clinic notes, and emergency department visits.
I also like to review the chart to see if I have taken care of the patient before. Patients often remember me even though I may not remember them, so reviewing my prior notes may be helpful. Thankfully, my electronic health record (EHR) has a search function where I can enter my name or any other keyword and it searches for patient records based on this keyword.
Step 2: Even though reading the chart and being informed about my patient is important, it is only the first step. The next step is to let my patient and family know that I have read the chart and that I am up-to-date on my patient’s diagnosis. I feel it is very important for me to verbalize that I have read the chart because without doing this, my patients never really know that I took the time prior to entering the room to learn about them.
I might say:
- “I was reviewing your chart before I came in, and I saw that your daughter brought you to the hospital for chest pain.”
- “I read your chart and saw that you have been to the emergency room twice in the last week.”
- “I read your primary-care doctor’s note, and I saw that she recently treated you for pneumonia.”
- “I read your chart, and I wanted to confirm a few things I read to ensure we are on the same page.”
There are many different ways you can phrase this, but the important point is to make sure your patients know you read the chart by specifically referencing something you learned. This helps your patients feel more confident that you know their medical history.
I know some of the doctors reading this column see patients in the outpatient setting. One way to help yourself remember pertinent facts about a patient’s medical history is to include these facts in a specific place in your clinic note. That way, prior to seeing the patient, you can always review your last note and know the important information about your patient’s medical history will always be in the same place in each note. Another tip is to use your EHR’s note function. My EHR has “sticky notes,” and they provide a place for the PCP to store information about the patient without it becoming part of the permanent medical record.
These notes allow the PCP to record important events that happen between one clinic visit and the next. Thus, when the patient returns to the clinic, the PCP opens the chart, reviews the sticky note, and enters the exam room prepared to discuss significant events in the patient’s recent medical history.
In the end, it does not matter which technique you use. It simply matters that you take time to review your patient’s chart prior to entering the room and that you verbalize what you have learned. In patients, this inspires confidence and trust and helps alleviate concerns that the physician does not know important information in their medical history.
Dr. Dorrah is regional medical director for quality and the patient experience at Baylor Scott & White Health in Round Rock, Tex. She is a member of SHM’s Patient Experience Committee.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I inform my patients that I have reviewed their chart and that I am familiar with their diagnosis.
Why I do it
In the hospital setting, in particular, patients are concerned about communication between their various healthcare professionals. Many times, the patient’s primary-care provider works strictly in the outpatient setting, so the hospitalist is the person who assumes total care of the patient throughout hospitalization. This understandably creates anxiety for patients and families because they wonder if the hospitalist really knows their medical history. One way to alleviate this anxiety is to review your patients’ charts prior to speaking with them and to verbally let your patients know you are familiar with their diagnoses.
How I do it
Step 1: Before entering the room, I review my patient’s chart. If I am taking over the service from my colleague, I review all notes from the current hospitalization to ensure I understand everything that has happened. I also review tests, procedures, and radiographic studies. To gain a better understanding of my patient, I read the most recent discharge summary and outpatient clinic note. Likewise, if I am admitting a new patient to the hospital, before entering the room to do the history and physical examination, I review recent hospitalizations, clinic notes, and emergency department visits.
I also like to review the chart to see if I have taken care of the patient before. Patients often remember me even though I may not remember them, so reviewing my prior notes may be helpful. Thankfully, my electronic health record (EHR) has a search function where I can enter my name or any other keyword and it searches for patient records based on this keyword.
Step 2: Even though reading the chart and being informed about my patient is important, it is only the first step. The next step is to let my patient and family know that I have read the chart and that I am up-to-date on my patient’s diagnosis. I feel it is very important for me to verbalize that I have read the chart because without doing this, my patients never really know that I took the time prior to entering the room to learn about them.
I might say:
- “I was reviewing your chart before I came in, and I saw that your daughter brought you to the hospital for chest pain.”
- “I read your chart and saw that you have been to the emergency room twice in the last week.”
- “I read your primary-care doctor’s note, and I saw that she recently treated you for pneumonia.”
- “I read your chart, and I wanted to confirm a few things I read to ensure we are on the same page.”
There are many different ways you can phrase this, but the important point is to make sure your patients know you read the chart by specifically referencing something you learned. This helps your patients feel more confident that you know their medical history.
I know some of the doctors reading this column see patients in the outpatient setting. One way to help yourself remember pertinent facts about a patient’s medical history is to include these facts in a specific place in your clinic note. That way, prior to seeing the patient, you can always review your last note and know the important information about your patient’s medical history will always be in the same place in each note. Another tip is to use your EHR’s note function. My EHR has “sticky notes,” and they provide a place for the PCP to store information about the patient without it becoming part of the permanent medical record.
These notes allow the PCP to record important events that happen between one clinic visit and the next. Thus, when the patient returns to the clinic, the PCP opens the chart, reviews the sticky note, and enters the exam room prepared to discuss significant events in the patient’s recent medical history.
In the end, it does not matter which technique you use. It simply matters that you take time to review your patient’s chart prior to entering the room and that you verbalize what you have learned. In patients, this inspires confidence and trust and helps alleviate concerns that the physician does not know important information in their medical history.
Dr. Dorrah is regional medical director for quality and the patient experience at Baylor Scott & White Health in Round Rock, Tex. She is a member of SHM’s Patient Experience Committee.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I inform my patients that I have reviewed their chart and that I am familiar with their diagnosis.
Why I do it
In the hospital setting, in particular, patients are concerned about communication between their various healthcare professionals. Many times, the patient’s primary-care provider works strictly in the outpatient setting, so the hospitalist is the person who assumes total care of the patient throughout hospitalization. This understandably creates anxiety for patients and families because they wonder if the hospitalist really knows their medical history. One way to alleviate this anxiety is to review your patients’ charts prior to speaking with them and to verbally let your patients know you are familiar with their diagnoses.
How I do it
Step 1: Before entering the room, I review my patient’s chart. If I am taking over the service from my colleague, I review all notes from the current hospitalization to ensure I understand everything that has happened. I also review tests, procedures, and radiographic studies. To gain a better understanding of my patient, I read the most recent discharge summary and outpatient clinic note. Likewise, if I am admitting a new patient to the hospital, before entering the room to do the history and physical examination, I review recent hospitalizations, clinic notes, and emergency department visits.
I also like to review the chart to see if I have taken care of the patient before. Patients often remember me even though I may not remember them, so reviewing my prior notes may be helpful. Thankfully, my electronic health record (EHR) has a search function where I can enter my name or any other keyword and it searches for patient records based on this keyword.
Step 2: Even though reading the chart and being informed about my patient is important, it is only the first step. The next step is to let my patient and family know that I have read the chart and that I am up-to-date on my patient’s diagnosis. I feel it is very important for me to verbalize that I have read the chart because without doing this, my patients never really know that I took the time prior to entering the room to learn about them.
I might say:
- “I was reviewing your chart before I came in, and I saw that your daughter brought you to the hospital for chest pain.”
- “I read your chart and saw that you have been to the emergency room twice in the last week.”
- “I read your primary-care doctor’s note, and I saw that she recently treated you for pneumonia.”
- “I read your chart, and I wanted to confirm a few things I read to ensure we are on the same page.”
There are many different ways you can phrase this, but the important point is to make sure your patients know you read the chart by specifically referencing something you learned. This helps your patients feel more confident that you know their medical history.
I know some of the doctors reading this column see patients in the outpatient setting. One way to help yourself remember pertinent facts about a patient’s medical history is to include these facts in a specific place in your clinic note. That way, prior to seeing the patient, you can always review your last note and know the important information about your patient’s medical history will always be in the same place in each note. Another tip is to use your EHR’s note function. My EHR has “sticky notes,” and they provide a place for the PCP to store information about the patient without it becoming part of the permanent medical record.
These notes allow the PCP to record important events that happen between one clinic visit and the next. Thus, when the patient returns to the clinic, the PCP opens the chart, reviews the sticky note, and enters the exam room prepared to discuss significant events in the patient’s recent medical history.
In the end, it does not matter which technique you use. It simply matters that you take time to review your patient’s chart prior to entering the room and that you verbalize what you have learned. In patients, this inspires confidence and trust and helps alleviate concerns that the physician does not know important information in their medical history.
Dr. Dorrah is regional medical director for quality and the patient experience at Baylor Scott & White Health in Round Rock, Tex. She is a member of SHM’s Patient Experience Committee.
Seeing the Future of Hospital Medicine
Hospitalists touch the lives of patients and shape health systems’ practices and health policy on a national and international scale according to an editorial titled “The Next 20 Years of Hospital Medicine: Continuing to Foster the Mind, Heart, and Soul of Our Field.”1
“This editorial was my reflection on the ‘Year of the Hospitalist’ and where I think the field needs to go in terms of its professionalism, patient-centeredness, and science,” says author Andrew D. Auerbach, MD, MPH, SFHM, who has worked as a hospitalist for more than 20 years. “We’ve grown extraordinarily fast, but some important aspects of our work need to be fleshed out.”
One example: Hospital medicine has been growing research capacity at a rate that is slower than the field overall, a problem due in part to funding limitations for fellowships and early-career awards, which has restricted the pipeline of young researchers. “Slow growth may also be a result of an emphasis on health systems rather than diseases,” Dr. Auerbach says.
Dr. Auerbach also is concerned about making sure the field of hospital medicine is attractive and sustainable as a career.
“A large amount of burnout can be attributed to things like EHRs, billing, etc., that are real dissatisfiers, but another broad area is in reconnecting with our professional/personal reasons for becoming physicians,” he says. “That needs to be reinvigorated. I also feel very strongly that we need to develop our own research agenda and grow research networks, but even those will need to be reconnected to patient needs more directly.”
Reference
- Auerbach AD. The next 20 years of hospital medicine: continuing to foster the mind, heart, and soul of our field [published online ahead of print July 4, 2016]. J Hosp Med. doi:10.1002/jhm.2631.
Hospitalists touch the lives of patients and shape health systems’ practices and health policy on a national and international scale according to an editorial titled “The Next 20 Years of Hospital Medicine: Continuing to Foster the Mind, Heart, and Soul of Our Field.”1
“This editorial was my reflection on the ‘Year of the Hospitalist’ and where I think the field needs to go in terms of its professionalism, patient-centeredness, and science,” says author Andrew D. Auerbach, MD, MPH, SFHM, who has worked as a hospitalist for more than 20 years. “We’ve grown extraordinarily fast, but some important aspects of our work need to be fleshed out.”
One example: Hospital medicine has been growing research capacity at a rate that is slower than the field overall, a problem due in part to funding limitations for fellowships and early-career awards, which has restricted the pipeline of young researchers. “Slow growth may also be a result of an emphasis on health systems rather than diseases,” Dr. Auerbach says.
Dr. Auerbach also is concerned about making sure the field of hospital medicine is attractive and sustainable as a career.
“A large amount of burnout can be attributed to things like EHRs, billing, etc., that are real dissatisfiers, but another broad area is in reconnecting with our professional/personal reasons for becoming physicians,” he says. “That needs to be reinvigorated. I also feel very strongly that we need to develop our own research agenda and grow research networks, but even those will need to be reconnected to patient needs more directly.”
Reference
- Auerbach AD. The next 20 years of hospital medicine: continuing to foster the mind, heart, and soul of our field [published online ahead of print July 4, 2016]. J Hosp Med. doi:10.1002/jhm.2631.
Hospitalists touch the lives of patients and shape health systems’ practices and health policy on a national and international scale according to an editorial titled “The Next 20 Years of Hospital Medicine: Continuing to Foster the Mind, Heart, and Soul of Our Field.”1
“This editorial was my reflection on the ‘Year of the Hospitalist’ and where I think the field needs to go in terms of its professionalism, patient-centeredness, and science,” says author Andrew D. Auerbach, MD, MPH, SFHM, who has worked as a hospitalist for more than 20 years. “We’ve grown extraordinarily fast, but some important aspects of our work need to be fleshed out.”
One example: Hospital medicine has been growing research capacity at a rate that is slower than the field overall, a problem due in part to funding limitations for fellowships and early-career awards, which has restricted the pipeline of young researchers. “Slow growth may also be a result of an emphasis on health systems rather than diseases,” Dr. Auerbach says.
Dr. Auerbach also is concerned about making sure the field of hospital medicine is attractive and sustainable as a career.
“A large amount of burnout can be attributed to things like EHRs, billing, etc., that are real dissatisfiers, but another broad area is in reconnecting with our professional/personal reasons for becoming physicians,” he says. “That needs to be reinvigorated. I also feel very strongly that we need to develop our own research agenda and grow research networks, but even those will need to be reconnected to patient needs more directly.”
Reference
- Auerbach AD. The next 20 years of hospital medicine: continuing to foster the mind, heart, and soul of our field [published online ahead of print July 4, 2016]. J Hosp Med. doi:10.1002/jhm.2631.
Promoting the Health of Healthcare Employees
Provisions in the Affordable Care Act (ACA) encourage hospitals to work with their communities to improve population health. Like so many things, these efforts can and should begin at home—in this case, the hospital itself. Health and wellness programs for healthcare workers need to be emphasized, according to “Health and Wellness Programs for Hospital Employees: Results from a 2015 American Hospital Association Survey.”1
Such efforts allow healthcare workers to lead by example.
“To help create a culture of health, hospitals and health systems can provide leadership, and hospital employees can be role models, for health and wellness in their communities,” according to the report. “Developing health and wellness strategies and programs at hospitals will help establish an environment that provides the support, resources, and incentives for hospital employees to serve as such role models.”
Developing health and wellness programs can also help hospitals achieve the public health goals of the Healthy People 2020 initiative from the Office of Disease Prevention and Health Promotion.
To find out how hospitals are doing in this work, the 26-question survey was done in 2010 and again in 2015 and sent to approximately 6,000 hospitals in the United States. Response rate was 15% in 2010 and 18% in 2015. Some of the findings include:
- About the same number of hospitals have a health and wellness program or other initiative(s) for employees (86% in 2010 and 87% in 2015); however, the types of health and wellness programs and benefits that hospitals offer to their employees increased.
- The number of hospitals with 70% to 90% or more of employees participating in health and wellness programs increased from 19% in 2010 to 31% in 2015.
- The number of hospitals offering health and wellness programs to people in the community increased from 19% in 2010 to 66% in 2015.
- The number of hospitals offering incentives for participating in health and wellness programs increased as did the value of incentives, with more hospitals giving $500 or more to employees (7% in 2010 and 29% in 2015).
Reference
- Health Research & Educational Trust. Health and wellness programs for hospital employees: results from a 2015 American Hospital Association survey. Hospitals in Pursuit of Excellence website.
Provisions in the Affordable Care Act (ACA) encourage hospitals to work with their communities to improve population health. Like so many things, these efforts can and should begin at home—in this case, the hospital itself. Health and wellness programs for healthcare workers need to be emphasized, according to “Health and Wellness Programs for Hospital Employees: Results from a 2015 American Hospital Association Survey.”1
Such efforts allow healthcare workers to lead by example.
“To help create a culture of health, hospitals and health systems can provide leadership, and hospital employees can be role models, for health and wellness in their communities,” according to the report. “Developing health and wellness strategies and programs at hospitals will help establish an environment that provides the support, resources, and incentives for hospital employees to serve as such role models.”
Developing health and wellness programs can also help hospitals achieve the public health goals of the Healthy People 2020 initiative from the Office of Disease Prevention and Health Promotion.
To find out how hospitals are doing in this work, the 26-question survey was done in 2010 and again in 2015 and sent to approximately 6,000 hospitals in the United States. Response rate was 15% in 2010 and 18% in 2015. Some of the findings include:
- About the same number of hospitals have a health and wellness program or other initiative(s) for employees (86% in 2010 and 87% in 2015); however, the types of health and wellness programs and benefits that hospitals offer to their employees increased.
- The number of hospitals with 70% to 90% or more of employees participating in health and wellness programs increased from 19% in 2010 to 31% in 2015.
- The number of hospitals offering health and wellness programs to people in the community increased from 19% in 2010 to 66% in 2015.
- The number of hospitals offering incentives for participating in health and wellness programs increased as did the value of incentives, with more hospitals giving $500 or more to employees (7% in 2010 and 29% in 2015).
Reference
- Health Research & Educational Trust. Health and wellness programs for hospital employees: results from a 2015 American Hospital Association survey. Hospitals in Pursuit of Excellence website.
Provisions in the Affordable Care Act (ACA) encourage hospitals to work with their communities to improve population health. Like so many things, these efforts can and should begin at home—in this case, the hospital itself. Health and wellness programs for healthcare workers need to be emphasized, according to “Health and Wellness Programs for Hospital Employees: Results from a 2015 American Hospital Association Survey.”1
Such efforts allow healthcare workers to lead by example.
“To help create a culture of health, hospitals and health systems can provide leadership, and hospital employees can be role models, for health and wellness in their communities,” according to the report. “Developing health and wellness strategies and programs at hospitals will help establish an environment that provides the support, resources, and incentives for hospital employees to serve as such role models.”
Developing health and wellness programs can also help hospitals achieve the public health goals of the Healthy People 2020 initiative from the Office of Disease Prevention and Health Promotion.
To find out how hospitals are doing in this work, the 26-question survey was done in 2010 and again in 2015 and sent to approximately 6,000 hospitals in the United States. Response rate was 15% in 2010 and 18% in 2015. Some of the findings include:
- About the same number of hospitals have a health and wellness program or other initiative(s) for employees (86% in 2010 and 87% in 2015); however, the types of health and wellness programs and benefits that hospitals offer to their employees increased.
- The number of hospitals with 70% to 90% or more of employees participating in health and wellness programs increased from 19% in 2010 to 31% in 2015.
- The number of hospitals offering health and wellness programs to people in the community increased from 19% in 2010 to 66% in 2015.
- The number of hospitals offering incentives for participating in health and wellness programs increased as did the value of incentives, with more hospitals giving $500 or more to employees (7% in 2010 and 29% in 2015).
Reference
- Health Research & Educational Trust. Health and wellness programs for hospital employees: results from a 2015 American Hospital Association survey. Hospitals in Pursuit of Excellence website.
Thinking Outside the DRG Box
When choosing quality improvement activities, hospitalists have no shortage of choices. In this column, I offer a strategic guide for hospitalists as they assess where best to spend their energy as the shift to value-based care progresses. This includes the introduction of MACRA, the landmark new payment program for doctors and other clinicians (aka the Medicare Access and CHIP Reauthorization Act of 2015), with its incentives for participation in alternative payment models.
Since 1983, Medicare has reimbursed hospitals using a lump-sum payment known as a diagnosis-related group, or DRG. Since then, hospitals have focused a good deal of their energy on removing needless expenses from the hospitalization to improve their bottom line, recognizing the DRG payment they receive is relatively fixed. To this end, a major strategy has been to use hospitalists to decrease length of stay and “right size” the utilization of in-hospital tests and treatments.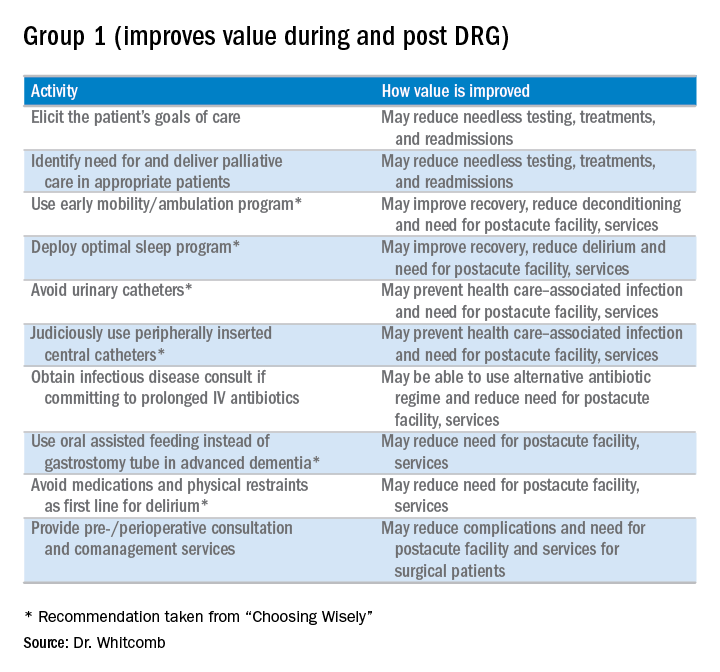
However, things are changing as we enter the era of alternative payment models such as accountable care organizations (ACOs) and bundled payments. The lens Medicare (and, to a great extent, commercial payors) peers through to assess inpatient hospital costs is the DRG payment amount. Beyond that, Medicare has little visibility into the actual costs hospitals incur. Since hospital spending equates to the payment amount for a DRG, it becomes apparent that the incremental opportunity for hospitalists to improve value (quality divided by cost) in alternative payment models stems from payments outside the DRG. Such payments include those related to the post-acute period such as nursing and rehabilitation facilities, readmissions, and part B activity (e.g., consultants and outpatient tests).
What does this mean for hospitalists? MACRA begins in 2019, but initial payments will be based on 2017 performance. The associated advantage of participating in an “advanced alternative payment model” where there is accountability for care beyond the hospitalization is that hospitalists will be rewarded for taking costs out of the post-acute time period.
To be clear, hospitalists should remain agents of in-hospital efficiency and quality. After all, that is how we add value to the hospitals in which we practice. All things being equal, however, hospitalists should focus on practices that will improve value beyond the four walls of the hospital.
Here is my shortlist of these practices. While there is crossover between the categories, I divide the practices into those that improve value during the DRG period and also post-DRG and those that improve value primarily post-DRG (thanks to Choosing Wisely for contributing to the recommendations with an asterisk1):
Thinking outside the DRG box will require an adjustment to the approach taken by hospitalists because the current demands are often more than enough for a day’s work. Hospitalists will be called upon to innovate and fashion better approaches to care. This will require support by other members of the healthcare team so hospitalists can work smarter, not harder, to meet the requirements of a changing healthcare system. A prerequisite is better payment models that align financial incentives so that providing higher-value care is sustainable and appropriately rewarded.

Reference
Clinician lists. Choosing Wisely website. Accessed October 25, 2016.
When choosing quality improvement activities, hospitalists have no shortage of choices. In this column, I offer a strategic guide for hospitalists as they assess where best to spend their energy as the shift to value-based care progresses. This includes the introduction of MACRA, the landmark new payment program for doctors and other clinicians (aka the Medicare Access and CHIP Reauthorization Act of 2015), with its incentives for participation in alternative payment models.
Since 1983, Medicare has reimbursed hospitals using a lump-sum payment known as a diagnosis-related group, or DRG. Since then, hospitals have focused a good deal of their energy on removing needless expenses from the hospitalization to improve their bottom line, recognizing the DRG payment they receive is relatively fixed. To this end, a major strategy has been to use hospitalists to decrease length of stay and “right size” the utilization of in-hospital tests and treatments.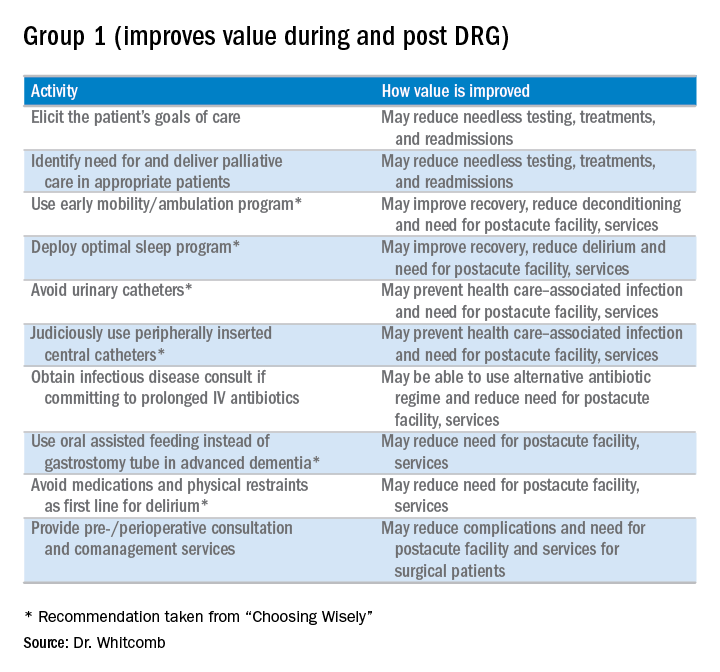
However, things are changing as we enter the era of alternative payment models such as accountable care organizations (ACOs) and bundled payments. The lens Medicare (and, to a great extent, commercial payors) peers through to assess inpatient hospital costs is the DRG payment amount. Beyond that, Medicare has little visibility into the actual costs hospitals incur. Since hospital spending equates to the payment amount for a DRG, it becomes apparent that the incremental opportunity for hospitalists to improve value (quality divided by cost) in alternative payment models stems from payments outside the DRG. Such payments include those related to the post-acute period such as nursing and rehabilitation facilities, readmissions, and part B activity (e.g., consultants and outpatient tests).
What does this mean for hospitalists? MACRA begins in 2019, but initial payments will be based on 2017 performance. The associated advantage of participating in an “advanced alternative payment model” where there is accountability for care beyond the hospitalization is that hospitalists will be rewarded for taking costs out of the post-acute time period.
To be clear, hospitalists should remain agents of in-hospital efficiency and quality. After all, that is how we add value to the hospitals in which we practice. All things being equal, however, hospitalists should focus on practices that will improve value beyond the four walls of the hospital.
Here is my shortlist of these practices. While there is crossover between the categories, I divide the practices into those that improve value during the DRG period and also post-DRG and those that improve value primarily post-DRG (thanks to Choosing Wisely for contributing to the recommendations with an asterisk1):
Thinking outside the DRG box will require an adjustment to the approach taken by hospitalists because the current demands are often more than enough for a day’s work. Hospitalists will be called upon to innovate and fashion better approaches to care. This will require support by other members of the healthcare team so hospitalists can work smarter, not harder, to meet the requirements of a changing healthcare system. A prerequisite is better payment models that align financial incentives so that providing higher-value care is sustainable and appropriately rewarded.

Reference
Clinician lists. Choosing Wisely website. Accessed October 25, 2016.
When choosing quality improvement activities, hospitalists have no shortage of choices. In this column, I offer a strategic guide for hospitalists as they assess where best to spend their energy as the shift to value-based care progresses. This includes the introduction of MACRA, the landmark new payment program for doctors and other clinicians (aka the Medicare Access and CHIP Reauthorization Act of 2015), with its incentives for participation in alternative payment models.
Since 1983, Medicare has reimbursed hospitals using a lump-sum payment known as a diagnosis-related group, or DRG. Since then, hospitals have focused a good deal of their energy on removing needless expenses from the hospitalization to improve their bottom line, recognizing the DRG payment they receive is relatively fixed. To this end, a major strategy has been to use hospitalists to decrease length of stay and “right size” the utilization of in-hospital tests and treatments.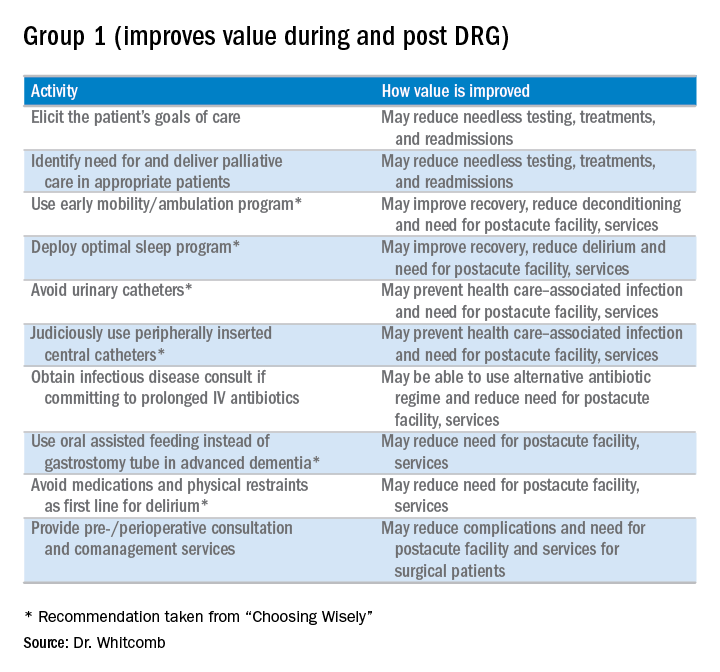
However, things are changing as we enter the era of alternative payment models such as accountable care organizations (ACOs) and bundled payments. The lens Medicare (and, to a great extent, commercial payors) peers through to assess inpatient hospital costs is the DRG payment amount. Beyond that, Medicare has little visibility into the actual costs hospitals incur. Since hospital spending equates to the payment amount for a DRG, it becomes apparent that the incremental opportunity for hospitalists to improve value (quality divided by cost) in alternative payment models stems from payments outside the DRG. Such payments include those related to the post-acute period such as nursing and rehabilitation facilities, readmissions, and part B activity (e.g., consultants and outpatient tests).
What does this mean for hospitalists? MACRA begins in 2019, but initial payments will be based on 2017 performance. The associated advantage of participating in an “advanced alternative payment model” where there is accountability for care beyond the hospitalization is that hospitalists will be rewarded for taking costs out of the post-acute time period.
To be clear, hospitalists should remain agents of in-hospital efficiency and quality. After all, that is how we add value to the hospitals in which we practice. All things being equal, however, hospitalists should focus on practices that will improve value beyond the four walls of the hospital.
Here is my shortlist of these practices. While there is crossover between the categories, I divide the practices into those that improve value during the DRG period and also post-DRG and those that improve value primarily post-DRG (thanks to Choosing Wisely for contributing to the recommendations with an asterisk1):
Thinking outside the DRG box will require an adjustment to the approach taken by hospitalists because the current demands are often more than enough for a day’s work. Hospitalists will be called upon to innovate and fashion better approaches to care. This will require support by other members of the healthcare team so hospitalists can work smarter, not harder, to meet the requirements of a changing healthcare system. A prerequisite is better payment models that align financial incentives so that providing higher-value care is sustainable and appropriately rewarded.

Reference
Clinician lists. Choosing Wisely website. Accessed October 25, 2016.
Strategies for Preventing Patient Falls
Between 700,000 and 1 million people fall each year in U.S. hospitals, and about a third of those result in injuries that add an additional 6.3 days to hospital stays, according to a report from the Joint Commission Center for Transforming Healthcare. Some 11,000 falls are fatal. The Joint Commission Center for Transforming Healthcare has now issued a report on the subject called “Preventing Patient Falls: A Systematic Approach from the Joint Commission Center for Transforming Healthcare Project.”1
“We try to pick those topics that healthcare organizations just haven’t been able to fully tackle even though they’ve put a lot of time and resources into trying to fix them,” says Kelly Barnes, MS, a center project lead in the Center for Transforming Healthcare at The Joint Commission.
The Joint Commission project involved seven hospitals that used Robust Process Improvement, which incorporates tools from Lean Six Sigma and change management methodologies, to reduce falls with injury on inpatient pilot units within their organizations.
During the project, each organization identified the specific factors that led to falls with injury in their environment and developed solutions targeted to those factors. The organizations identified 30 root causes and developed 21 targeted solutions. Because the contributing factors were different at each organization, solution sets were unique to each. Afterward, the organizations saw an aggregate 35% reduction in falls and a 62% reduction in falls with injury.
“One of the takeaways is that you really need support across an organization to have success,” Barnes says. “The more engaged the entire organization is from top down all the way to the bottom, the more successful people are in solving the problems.”
The study resulted in a Targeted Solutions Tool (TST), free to all Joint Commission–accredited customers, to help hospitals.
“You can put your data right into the tool,” Barnes says. “It tells you what your top contributing factors are, and it gives you the solutions that have worked for those contributing factors at other organizations.”
Reference
Health Research & Educational Trust. Preventing patient falls: a systematic approach from the Joint Commission Center for Transforming Healthcare project. Hospitals in Pursuit of Excellence website.
Between 700,000 and 1 million people fall each year in U.S. hospitals, and about a third of those result in injuries that add an additional 6.3 days to hospital stays, according to a report from the Joint Commission Center for Transforming Healthcare. Some 11,000 falls are fatal. The Joint Commission Center for Transforming Healthcare has now issued a report on the subject called “Preventing Patient Falls: A Systematic Approach from the Joint Commission Center for Transforming Healthcare Project.”1
“We try to pick those topics that healthcare organizations just haven’t been able to fully tackle even though they’ve put a lot of time and resources into trying to fix them,” says Kelly Barnes, MS, a center project lead in the Center for Transforming Healthcare at The Joint Commission.
The Joint Commission project involved seven hospitals that used Robust Process Improvement, which incorporates tools from Lean Six Sigma and change management methodologies, to reduce falls with injury on inpatient pilot units within their organizations.
During the project, each organization identified the specific factors that led to falls with injury in their environment and developed solutions targeted to those factors. The organizations identified 30 root causes and developed 21 targeted solutions. Because the contributing factors were different at each organization, solution sets were unique to each. Afterward, the organizations saw an aggregate 35% reduction in falls and a 62% reduction in falls with injury.
“One of the takeaways is that you really need support across an organization to have success,” Barnes says. “The more engaged the entire organization is from top down all the way to the bottom, the more successful people are in solving the problems.”
The study resulted in a Targeted Solutions Tool (TST), free to all Joint Commission–accredited customers, to help hospitals.
“You can put your data right into the tool,” Barnes says. “It tells you what your top contributing factors are, and it gives you the solutions that have worked for those contributing factors at other organizations.”
Reference
Health Research & Educational Trust. Preventing patient falls: a systematic approach from the Joint Commission Center for Transforming Healthcare project. Hospitals in Pursuit of Excellence website.
Between 700,000 and 1 million people fall each year in U.S. hospitals, and about a third of those result in injuries that add an additional 6.3 days to hospital stays, according to a report from the Joint Commission Center for Transforming Healthcare. Some 11,000 falls are fatal. The Joint Commission Center for Transforming Healthcare has now issued a report on the subject called “Preventing Patient Falls: A Systematic Approach from the Joint Commission Center for Transforming Healthcare Project.”1
“We try to pick those topics that healthcare organizations just haven’t been able to fully tackle even though they’ve put a lot of time and resources into trying to fix them,” says Kelly Barnes, MS, a center project lead in the Center for Transforming Healthcare at The Joint Commission.
The Joint Commission project involved seven hospitals that used Robust Process Improvement, which incorporates tools from Lean Six Sigma and change management methodologies, to reduce falls with injury on inpatient pilot units within their organizations.
During the project, each organization identified the specific factors that led to falls with injury in their environment and developed solutions targeted to those factors. The organizations identified 30 root causes and developed 21 targeted solutions. Because the contributing factors were different at each organization, solution sets were unique to each. Afterward, the organizations saw an aggregate 35% reduction in falls and a 62% reduction in falls with injury.
“One of the takeaways is that you really need support across an organization to have success,” Barnes says. “The more engaged the entire organization is from top down all the way to the bottom, the more successful people are in solving the problems.”
The study resulted in a Targeted Solutions Tool (TST), free to all Joint Commission–accredited customers, to help hospitals.
“You can put your data right into the tool,” Barnes says. “It tells you what your top contributing factors are, and it gives you the solutions that have worked for those contributing factors at other organizations.”
Reference
Health Research & Educational Trust. Preventing patient falls: a systematic approach from the Joint Commission Center for Transforming Healthcare project. Hospitals in Pursuit of Excellence website.
Helping Patients Quit Smoking
Inpatient hospitalization can be a key time for patients to quit smoking, according to an abstract called “No More Butts: An Automated System for Inpatient Smoking Cessation Team Consults.”1
“Tobacco smoking continues to be one of the most important public health threats that we face,” says lead author Sujatha Sankaran, MD, assistant clinical professor in the division of hospital medicine and medical director of smoking cessation at the University of California, San Francisco. “Hospitalization is an extremely important moment and provides an excellent opportunity to counsel and provide cessation resources for people who are concerned about their health.”
Inpatients who receive smoking cessation counseling, nicotine replacement, and referral to outpatient resources have increased quit rates six weeks after hospital discharge, their research showed.
However, according to the abstract, in 2014:
- 34.5% of tobacco users admitted to one 600-bed academic hospital were documented as having received and accepted tobacco cessation counseling
- 45.7% of tobacco users received nicotine replacement therapy
- 1.35% of tobacco users received after-discharge consultations to outpatient smoking cessation resources
Researchers piloted a system in which a dedicated respiratory therapist–staffed smoking cessation consult service was trained to provide targeted tobacco cessation services to all inpatients who use tobacco. Of 1944 patients identified as using tobacco, 1545 received and accepted cessation counseling from a trained member of the Smoking Cessation Team, 1526 received nicotine replacement therapy, and 464 received an electronic referral to either a telephone or in-person quit line
“Hospitalists know firsthand the serious harm that tobacco use causes to patients but often are overwhelmed by the acute issues of patients and are unable to fully address tobacco use with hospitalized patients,” Dr. Sankaran says. “An automated cessation service can help lessen this burden by providing automatic cessation resources to all tobacco users.”
Reference
- Sankaran S, Burke R, O’Keefe S. No more butts: an automated system for inpatient smoking cessation team consults [abstract]. J Hosp Med. 2016;11(suppl 1). Accessed November 9, 2016.
Inpatient hospitalization can be a key time for patients to quit smoking, according to an abstract called “No More Butts: An Automated System for Inpatient Smoking Cessation Team Consults.”1
“Tobacco smoking continues to be one of the most important public health threats that we face,” says lead author Sujatha Sankaran, MD, assistant clinical professor in the division of hospital medicine and medical director of smoking cessation at the University of California, San Francisco. “Hospitalization is an extremely important moment and provides an excellent opportunity to counsel and provide cessation resources for people who are concerned about their health.”
Inpatients who receive smoking cessation counseling, nicotine replacement, and referral to outpatient resources have increased quit rates six weeks after hospital discharge, their research showed.
However, according to the abstract, in 2014:
- 34.5% of tobacco users admitted to one 600-bed academic hospital were documented as having received and accepted tobacco cessation counseling
- 45.7% of tobacco users received nicotine replacement therapy
- 1.35% of tobacco users received after-discharge consultations to outpatient smoking cessation resources
Researchers piloted a system in which a dedicated respiratory therapist–staffed smoking cessation consult service was trained to provide targeted tobacco cessation services to all inpatients who use tobacco. Of 1944 patients identified as using tobacco, 1545 received and accepted cessation counseling from a trained member of the Smoking Cessation Team, 1526 received nicotine replacement therapy, and 464 received an electronic referral to either a telephone or in-person quit line
“Hospitalists know firsthand the serious harm that tobacco use causes to patients but often are overwhelmed by the acute issues of patients and are unable to fully address tobacco use with hospitalized patients,” Dr. Sankaran says. “An automated cessation service can help lessen this burden by providing automatic cessation resources to all tobacco users.”
Reference
- Sankaran S, Burke R, O’Keefe S. No more butts: an automated system for inpatient smoking cessation team consults [abstract]. J Hosp Med. 2016;11(suppl 1). Accessed November 9, 2016.
Inpatient hospitalization can be a key time for patients to quit smoking, according to an abstract called “No More Butts: An Automated System for Inpatient Smoking Cessation Team Consults.”1
“Tobacco smoking continues to be one of the most important public health threats that we face,” says lead author Sujatha Sankaran, MD, assistant clinical professor in the division of hospital medicine and medical director of smoking cessation at the University of California, San Francisco. “Hospitalization is an extremely important moment and provides an excellent opportunity to counsel and provide cessation resources for people who are concerned about their health.”
Inpatients who receive smoking cessation counseling, nicotine replacement, and referral to outpatient resources have increased quit rates six weeks after hospital discharge, their research showed.
However, according to the abstract, in 2014:
- 34.5% of tobacco users admitted to one 600-bed academic hospital were documented as having received and accepted tobacco cessation counseling
- 45.7% of tobacco users received nicotine replacement therapy
- 1.35% of tobacco users received after-discharge consultations to outpatient smoking cessation resources
Researchers piloted a system in which a dedicated respiratory therapist–staffed smoking cessation consult service was trained to provide targeted tobacco cessation services to all inpatients who use tobacco. Of 1944 patients identified as using tobacco, 1545 received and accepted cessation counseling from a trained member of the Smoking Cessation Team, 1526 received nicotine replacement therapy, and 464 received an electronic referral to either a telephone or in-person quit line
“Hospitalists know firsthand the serious harm that tobacco use causes to patients but often are overwhelmed by the acute issues of patients and are unable to fully address tobacco use with hospitalized patients,” Dr. Sankaran says. “An automated cessation service can help lessen this burden by providing automatic cessation resources to all tobacco users.”
Reference
- Sankaran S, Burke R, O’Keefe S. No more butts: an automated system for inpatient smoking cessation team consults [abstract]. J Hosp Med. 2016;11(suppl 1). Accessed November 9, 2016.