User login
Los Angeles Inspires With Arts, Culture
Los Angeles has a flare for the dramatic, and we’re not just talking about Hollywood’s fast-paced, larger-than-life movie industry. When you visit Los Angeles, October 22 – 26, for CHEST 2016, be sure to check out the assortment of arts and culture venues located nearby your home base at CHEST 2016.
Los Angeles has more museums and theaters than any other U.S. city, and we’ll highlight a few local favorites below. For more information on L.A.’s thriving arts and culture scene, check out discoverlosangeles.com.
• The Dorothy Chandler Pavilion – (7-minute drive) – This hall is part of the Los Angeles music center. On October 22 – 23, watch three major U.S. ballet companies share the stage in Celebrate Forsythe. Or, take in The Source, a music-theater production about Chelsea (formerly Bradley) Manning and WikiLeaks.
• The Ahmanson Theatre – (7-minute drive) – This theater is also part of the Los Angeles music center. Be captivated by a 2016 Tony Award–winning play, A View from the Bridge.
• Walt Disney Concert Hall – (6-minute drive) – Home to the Los Angeles Philharmonic Orchestra and the Los Angeles Master Chorale, it is also part of the Los Angeles music center. Listen to the beautiful sounds of Mahler’s Ninth or Hilary Hahn on violin.
• MOCA Grand – (5-minute drive) – The Museum of Contemporary Art has three locations in Los Angeles. The main branch, located on Grand Avenue, is the closest to the convention center. Check out the museum’s main galleries at this location.
• The Getty Center – (30-minute drive) – See spectacular art and architecture at the top of Los Angeles.
Note: all estimated times assume you are starting at the Los Angeles Convention Center.
Los Angeles’ arts and culture scene is sure to inspire you, and CHEST 2016 will move you with the latest clinical information in chest medicine. Join us at CHEST 2016, and you won’t miss a beat with cutting-edge sessions and simulation training designed to update you on the latest patient care strategies. You will be part of an international community of innovative problem solvers. Learn more and register today at chestmeeting.chestnet.org.
Los Angeles has a flare for the dramatic, and we’re not just talking about Hollywood’s fast-paced, larger-than-life movie industry. When you visit Los Angeles, October 22 – 26, for CHEST 2016, be sure to check out the assortment of arts and culture venues located nearby your home base at CHEST 2016.
Los Angeles has more museums and theaters than any other U.S. city, and we’ll highlight a few local favorites below. For more information on L.A.’s thriving arts and culture scene, check out discoverlosangeles.com.
• The Dorothy Chandler Pavilion – (7-minute drive) – This hall is part of the Los Angeles music center. On October 22 – 23, watch three major U.S. ballet companies share the stage in Celebrate Forsythe. Or, take in The Source, a music-theater production about Chelsea (formerly Bradley) Manning and WikiLeaks.
• The Ahmanson Theatre – (7-minute drive) – This theater is also part of the Los Angeles music center. Be captivated by a 2016 Tony Award–winning play, A View from the Bridge.
• Walt Disney Concert Hall – (6-minute drive) – Home to the Los Angeles Philharmonic Orchestra and the Los Angeles Master Chorale, it is also part of the Los Angeles music center. Listen to the beautiful sounds of Mahler’s Ninth or Hilary Hahn on violin.
• MOCA Grand – (5-minute drive) – The Museum of Contemporary Art has three locations in Los Angeles. The main branch, located on Grand Avenue, is the closest to the convention center. Check out the museum’s main galleries at this location.
• The Getty Center – (30-minute drive) – See spectacular art and architecture at the top of Los Angeles.
Note: all estimated times assume you are starting at the Los Angeles Convention Center.
Los Angeles’ arts and culture scene is sure to inspire you, and CHEST 2016 will move you with the latest clinical information in chest medicine. Join us at CHEST 2016, and you won’t miss a beat with cutting-edge sessions and simulation training designed to update you on the latest patient care strategies. You will be part of an international community of innovative problem solvers. Learn more and register today at chestmeeting.chestnet.org.
Los Angeles has a flare for the dramatic, and we’re not just talking about Hollywood’s fast-paced, larger-than-life movie industry. When you visit Los Angeles, October 22 – 26, for CHEST 2016, be sure to check out the assortment of arts and culture venues located nearby your home base at CHEST 2016.
Los Angeles has more museums and theaters than any other U.S. city, and we’ll highlight a few local favorites below. For more information on L.A.’s thriving arts and culture scene, check out discoverlosangeles.com.
• The Dorothy Chandler Pavilion – (7-minute drive) – This hall is part of the Los Angeles music center. On October 22 – 23, watch three major U.S. ballet companies share the stage in Celebrate Forsythe. Or, take in The Source, a music-theater production about Chelsea (formerly Bradley) Manning and WikiLeaks.
• The Ahmanson Theatre – (7-minute drive) – This theater is also part of the Los Angeles music center. Be captivated by a 2016 Tony Award–winning play, A View from the Bridge.
• Walt Disney Concert Hall – (6-minute drive) – Home to the Los Angeles Philharmonic Orchestra and the Los Angeles Master Chorale, it is also part of the Los Angeles music center. Listen to the beautiful sounds of Mahler’s Ninth or Hilary Hahn on violin.
• MOCA Grand – (5-minute drive) – The Museum of Contemporary Art has three locations in Los Angeles. The main branch, located on Grand Avenue, is the closest to the convention center. Check out the museum’s main galleries at this location.
• The Getty Center – (30-minute drive) – See spectacular art and architecture at the top of Los Angeles.
Note: all estimated times assume you are starting at the Los Angeles Convention Center.
Los Angeles’ arts and culture scene is sure to inspire you, and CHEST 2016 will move you with the latest clinical information in chest medicine. Join us at CHEST 2016, and you won’t miss a beat with cutting-edge sessions and simulation training designed to update you on the latest patient care strategies. You will be part of an international community of innovative problem solvers. Learn more and register today at chestmeeting.chestnet.org.
Pulmonary Perspectives® New Technology Enhances Electromagnetic Navigation Bronchoscopy
Following the National Lung Screening Trial (NLST), which showed at-risk patients screened with CT scans had reduced lung cancer-specific mortality, many institutions have incorporated lung cancer screening protocols into clinical practice (Aberle et al. N Engl J Med. 2011;365[5]:395). These protocols, along with new generation, high resolution multidetector CT scans, have increased the number of detected peripheral lung nodules, many smaller in size. It is estimated that over 150,000 solitary nodules are diagnosed each year in the United States (Herth et al. Expert Rev Respir Med. 2016; 0[8]:901) and, in keeping with the NLST, greater than 25% of subjects screened have lung nodules suspicious for lung cancer. As a result, many leading health practices have created specific lung nodule programs to handle the volume in an effort to deliver timely care in the evaluation of lung cancer.
Pulmonary specialists managing patients with lung nodules are faced with the difficult challenge of deciding if a patient with a nodule is a candidate for serial surveillance, tissue biopsy (transthoracic needle aspiration [TTNA] vs. bronchoscopic biopsy [TBX]), or surgical resection. Calculation of the probability of a nodule being malignant is most helpful in making these decisions for patients with low and high malignancy risk factors, as surveillance and resection are appropriate steps, respectively. However, for those with an intermediate (5%-65%) probability of having a malignant nodule, the diagnostic procedure risks, yields, and timing have to be considered because delayed sampling or false-negative results may negatively impact survival. Kanashiki et al (Oncol Rep. 2003;10[3]:649) showed that worse survival is associated with patients with imaging-to-diagnosis times of greater than 4 months. Over the past decade, image-guided bronchoscopy has been used to improve the yield for tissue sampling of smaller peripheral nodules in a timely fashion. The most common method of image-guided bronchoscopy today is electromagnetic navigation bronchoscopy (ENB).
Electromagnetic navigation bronchoscopy has shown promise for increasing diagnostic yields for peripheral nodules (PN) over conventional bronchoscopy. Over time, the improved yields have plateaued as ENB use in clinical practice increased and limitations of the early generation technology became apparent. Earlier ENB technology uses a single inspiratory CT scan of the chest to reconstruct a 3D virtual model of the airways and parenchyma. A tracked sensor is then used to navigate through the imaging reconstructed airways toward the targeted lesion, the sensor is then removed, and through a dedicated catheter instruments are used to obtain samples from the lesion. In a meta-analysis using this technology, lesions greater than 2 cm had a diagnostic yield ranging from 66.7% to 94.7%. However, as the PN size decreased to less than or equal to 2 cm, the diagnostic yield range dropped significantly with some yields reported as low as 18.2% (van ‘t Westeinde et al. Chest. 2012;142(2):377). More recently, Ost and colleagues performed a multicenter study of consecutive patients undergoing bronchoscopic sampling of PN (Ost et al. Am J Respir Crit Care Med. 2016;193[1]:68). Although it was not a randomized trial and each bronchoscopist influenced the selection of the sampling technique, the authors reported that the diagnostic yields for navigation-guided bronchoscopy were lower than conventional bronchoscopy, 38.5% and 63.7%, respectively. Taken on face value alone, one might conclude that ENB not be used to biopsy PNs. However, deeper analysis of the data showed that 97% of the ENB procedures were performed using the earlier technology described above, suggesting that the single inspiratory imaging CT scan and navigation procedure technique, which differs significantly from conventional bronchoscopy, may have some influence on the lower than expected yields.
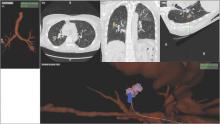
Despite increasing use and experience with ENB, diagnostic yields remain static. Chen and colleagues hypothesized that using a single inspiratory CT scan may not allow the endoscopist to make adjustments for PN movement as the lung moves during the respiratory cycle. Using different imaging protocol, the investigators assessed movement of 85 lung nodules during the respiratory cycle with paired-full inspiration and tidal-volume expiration, thin sliced (0.5-1.0 mm) CT scans. They found that the average motion of all lesions during respiration was 17.6 mm, 12.2 mm in the right-upper lobe, 10.6 mm in the left-upper lobe, and 25.3 mm and 23.8 mm in the right- and left- lower lobes, respectively (Chen et al. Chest. 2015;147[5];1275) (Fig. 1). They concluded that the location of targeted lesions on a single inspiration planning CT scan alone does not accurately represent the position of the lesion during bronchoscopy.
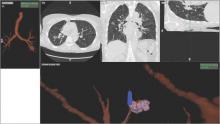
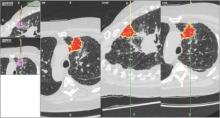
Although being able to correct for nodule movement throughout the respiratory cycle during the procedure is a significant improvement, it doesn’t guarantee that the tissue sample is obtained from the targeted lesion. To accomplish that, the system would have to be able to determine when the instrument being used to sample is in the target. The earlier ENB systems allowed for navigation to the target with a separate sensor through a steerable catheter. However, when the target was reached, the sensor had to be removed so that sampling instruments could be introduced into the catheter. Since the instruments are not tracked and the movement of the nodule is occurring, there is no guarantee that the instrument is in the target at the time of sampling. Advanced technology now allows for the tracking sensor to be placed in the tip of standard bronchoscopy instruments, making them “tip-tracked” and able to be used with standard bronchoscopes and equipment; thus, making the new ENB procedure similar to conventional bronchoscopy that was shown to have higher diagnostic yields (Figs. 2 and 3).
Our institution incorporated this technology (Veran Medical, St. Louis) into our advanced diagnostic and interventional pulmonary program for lung nodules and published our initial experience and results. During the initial 8 months of screening for lung cancer, we performed procedures on 44 patients with PNs suspicious for lung cancer. The rate for successful target sampling was 90.2% with a cancer diagnosis rate of 39%, which is similar to that found in the NLST. Those patients who had nonmalignant but abnormal pathologic findings (inflammation, granuloma, fibrosis, and so on) were monitored for a minimum of 12 months. Most of the lesions either remained stable or disappeared on follow-up imaging (Flenaugh et al. The Internet Journal of Pulmonary Medicine. 2016;18[1]). We concluded that (1) the combination of paired inspiratory and expiratory CT scan imaging accounts for nodule movement and (2) using tip-tracked conventional instruments to enter into the lesion at the time of biopsy contributes to improved yields.
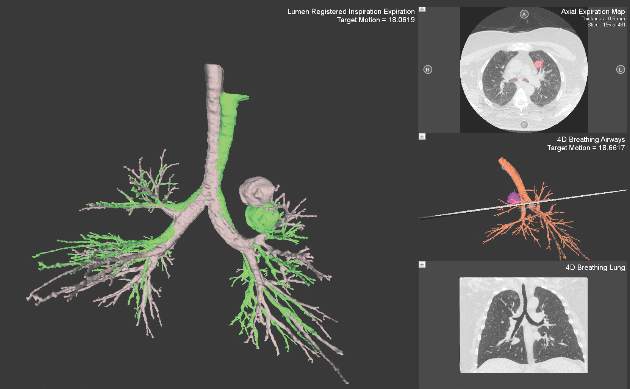
Newer ENB technology is not limited to transbronchial sampling. For PNs less than 2 cm and deep in the lung periphery, current recommendations prefer TTNA over bronchoscopic biopsy because of yield rates of 90% (Chest. 2007; 132(suppl 3):131S). Using the same paired CT scanning and tip-tracking method on transthoracic needles, the new systems allow pulmonologists to perform electromagnetic transthoracic needle aspiration (ETTNA) of PNs using the same basic equipment and during the same procedure visit (Fig. 4). This “one stop shopping” approach of bronchoscopy with the option of converting to ETTNA if the PN is not reachable endoscopically has proven to be cost efficient and allows for timely diagnosis and focused care (Yarmis et al. J Thorac Dis. 2016;8(1):186). In a prospective study designed specifically to assess feasibility, safety, and diagnostic yield of ETTNA in a single procedure, Yarmis and colleagues enrolled 24 patients to undergo endobronchial ultrasound for lung cancer staging followed by ENB and ETTNA. Ninety-six percent of the patients were candidates for ETTNA. The authors reported the yield for ETTNA was 83%, ETTNA plus ENB 87%, and ETTNA plus ENB plus endobronchial ultrasound for complete staging was 92%. Five pneumothoraces were reported; however, only two (8%) required a drainage intervention. This protocol is unique because it makes use of several advanced diagnostic procedures, including tip-tracked navigation technology, to localize, sample, diagnose, and stage during one patient procedure visit.
As lung cancer screening becomes commonplace in clinical practice and imaging technology improves, pulmonary specialists can expect to encounter and manage a greater number of pulmonary nodules. Advancements in technology now offer options for improving diagnostic accuracy while providing timely, safe, and cost effective care. While not all new technology will prove beneficial in disease management, those that improve the deficiencies of earlier technology offer us the best chance to improve practice. This perspective highlights such technology.
Dr. Flenaugh is Associate Professor, Director of Advanced Diagnostic & Interventional Pulmonary Service,Morehouse School of Medicine and Grady Hospital, Atlanta; Dr. Foreman is Professor of Medicine, Associate Chair for Research, Pulmonary & Critical Care Medicine, Morehouse School of Medicine.
Following the National Lung Screening Trial (NLST), which showed at-risk patients screened with CT scans had reduced lung cancer-specific mortality, many institutions have incorporated lung cancer screening protocols into clinical practice (Aberle et al. N Engl J Med. 2011;365[5]:395). These protocols, along with new generation, high resolution multidetector CT scans, have increased the number of detected peripheral lung nodules, many smaller in size. It is estimated that over 150,000 solitary nodules are diagnosed each year in the United States (Herth et al. Expert Rev Respir Med. 2016; 0[8]:901) and, in keeping with the NLST, greater than 25% of subjects screened have lung nodules suspicious for lung cancer. As a result, many leading health practices have created specific lung nodule programs to handle the volume in an effort to deliver timely care in the evaluation of lung cancer.
Pulmonary specialists managing patients with lung nodules are faced with the difficult challenge of deciding if a patient with a nodule is a candidate for serial surveillance, tissue biopsy (transthoracic needle aspiration [TTNA] vs. bronchoscopic biopsy [TBX]), or surgical resection. Calculation of the probability of a nodule being malignant is most helpful in making these decisions for patients with low and high malignancy risk factors, as surveillance and resection are appropriate steps, respectively. However, for those with an intermediate (5%-65%) probability of having a malignant nodule, the diagnostic procedure risks, yields, and timing have to be considered because delayed sampling or false-negative results may negatively impact survival. Kanashiki et al (Oncol Rep. 2003;10[3]:649) showed that worse survival is associated with patients with imaging-to-diagnosis times of greater than 4 months. Over the past decade, image-guided bronchoscopy has been used to improve the yield for tissue sampling of smaller peripheral nodules in a timely fashion. The most common method of image-guided bronchoscopy today is electromagnetic navigation bronchoscopy (ENB).
Electromagnetic navigation bronchoscopy has shown promise for increasing diagnostic yields for peripheral nodules (PN) over conventional bronchoscopy. Over time, the improved yields have plateaued as ENB use in clinical practice increased and limitations of the early generation technology became apparent. Earlier ENB technology uses a single inspiratory CT scan of the chest to reconstruct a 3D virtual model of the airways and parenchyma. A tracked sensor is then used to navigate through the imaging reconstructed airways toward the targeted lesion, the sensor is then removed, and through a dedicated catheter instruments are used to obtain samples from the lesion. In a meta-analysis using this technology, lesions greater than 2 cm had a diagnostic yield ranging from 66.7% to 94.7%. However, as the PN size decreased to less than or equal to 2 cm, the diagnostic yield range dropped significantly with some yields reported as low as 18.2% (van ‘t Westeinde et al. Chest. 2012;142(2):377). More recently, Ost and colleagues performed a multicenter study of consecutive patients undergoing bronchoscopic sampling of PN (Ost et al. Am J Respir Crit Care Med. 2016;193[1]:68). Although it was not a randomized trial and each bronchoscopist influenced the selection of the sampling technique, the authors reported that the diagnostic yields for navigation-guided bronchoscopy were lower than conventional bronchoscopy, 38.5% and 63.7%, respectively. Taken on face value alone, one might conclude that ENB not be used to biopsy PNs. However, deeper analysis of the data showed that 97% of the ENB procedures were performed using the earlier technology described above, suggesting that the single inspiratory imaging CT scan and navigation procedure technique, which differs significantly from conventional bronchoscopy, may have some influence on the lower than expected yields.
Despite increasing use and experience with ENB, diagnostic yields remain static. Chen and colleagues hypothesized that using a single inspiratory CT scan may not allow the endoscopist to make adjustments for PN movement as the lung moves during the respiratory cycle. Using different imaging protocol, the investigators assessed movement of 85 lung nodules during the respiratory cycle with paired-full inspiration and tidal-volume expiration, thin sliced (0.5-1.0 mm) CT scans. They found that the average motion of all lesions during respiration was 17.6 mm, 12.2 mm in the right-upper lobe, 10.6 mm in the left-upper lobe, and 25.3 mm and 23.8 mm in the right- and left- lower lobes, respectively (Chen et al. Chest. 2015;147[5];1275) (Fig. 1). They concluded that the location of targeted lesions on a single inspiration planning CT scan alone does not accurately represent the position of the lesion during bronchoscopy.
Although being able to correct for nodule movement throughout the respiratory cycle during the procedure is a significant improvement, it doesn’t guarantee that the tissue sample is obtained from the targeted lesion. To accomplish that, the system would have to be able to determine when the instrument being used to sample is in the target. The earlier ENB systems allowed for navigation to the target with a separate sensor through a steerable catheter. However, when the target was reached, the sensor had to be removed so that sampling instruments could be introduced into the catheter. Since the instruments are not tracked and the movement of the nodule is occurring, there is no guarantee that the instrument is in the target at the time of sampling. Advanced technology now allows for the tracking sensor to be placed in the tip of standard bronchoscopy instruments, making them “tip-tracked” and able to be used with standard bronchoscopes and equipment; thus, making the new ENB procedure similar to conventional bronchoscopy that was shown to have higher diagnostic yields (Figs. 2 and 3).
Our institution incorporated this technology (Veran Medical, St. Louis) into our advanced diagnostic and interventional pulmonary program for lung nodules and published our initial experience and results. During the initial 8 months of screening for lung cancer, we performed procedures on 44 patients with PNs suspicious for lung cancer. The rate for successful target sampling was 90.2% with a cancer diagnosis rate of 39%, which is similar to that found in the NLST. Those patients who had nonmalignant but abnormal pathologic findings (inflammation, granuloma, fibrosis, and so on) were monitored for a minimum of 12 months. Most of the lesions either remained stable or disappeared on follow-up imaging (Flenaugh et al. The Internet Journal of Pulmonary Medicine. 2016;18[1]). We concluded that (1) the combination of paired inspiratory and expiratory CT scan imaging accounts for nodule movement and (2) using tip-tracked conventional instruments to enter into the lesion at the time of biopsy contributes to improved yields.
Newer ENB technology is not limited to transbronchial sampling. For PNs less than 2 cm and deep in the lung periphery, current recommendations prefer TTNA over bronchoscopic biopsy because of yield rates of 90% (Chest. 2007; 132(suppl 3):131S). Using the same paired CT scanning and tip-tracking method on transthoracic needles, the new systems allow pulmonologists to perform electromagnetic transthoracic needle aspiration (ETTNA) of PNs using the same basic equipment and during the same procedure visit (Fig. 4). This “one stop shopping” approach of bronchoscopy with the option of converting to ETTNA if the PN is not reachable endoscopically has proven to be cost efficient and allows for timely diagnosis and focused care (Yarmis et al. J Thorac Dis. 2016;8(1):186). In a prospective study designed specifically to assess feasibility, safety, and diagnostic yield of ETTNA in a single procedure, Yarmis and colleagues enrolled 24 patients to undergo endobronchial ultrasound for lung cancer staging followed by ENB and ETTNA. Ninety-six percent of the patients were candidates for ETTNA. The authors reported the yield for ETTNA was 83%, ETTNA plus ENB 87%, and ETTNA plus ENB plus endobronchial ultrasound for complete staging was 92%. Five pneumothoraces were reported; however, only two (8%) required a drainage intervention. This protocol is unique because it makes use of several advanced diagnostic procedures, including tip-tracked navigation technology, to localize, sample, diagnose, and stage during one patient procedure visit.
As lung cancer screening becomes commonplace in clinical practice and imaging technology improves, pulmonary specialists can expect to encounter and manage a greater number of pulmonary nodules. Advancements in technology now offer options for improving diagnostic accuracy while providing timely, safe, and cost effective care. While not all new technology will prove beneficial in disease management, those that improve the deficiencies of earlier technology offer us the best chance to improve practice. This perspective highlights such technology.
Dr. Flenaugh is Associate Professor, Director of Advanced Diagnostic & Interventional Pulmonary Service,Morehouse School of Medicine and Grady Hospital, Atlanta; Dr. Foreman is Professor of Medicine, Associate Chair for Research, Pulmonary & Critical Care Medicine, Morehouse School of Medicine.
Following the National Lung Screening Trial (NLST), which showed at-risk patients screened with CT scans had reduced lung cancer-specific mortality, many institutions have incorporated lung cancer screening protocols into clinical practice (Aberle et al. N Engl J Med. 2011;365[5]:395). These protocols, along with new generation, high resolution multidetector CT scans, have increased the number of detected peripheral lung nodules, many smaller in size. It is estimated that over 150,000 solitary nodules are diagnosed each year in the United States (Herth et al. Expert Rev Respir Med. 2016; 0[8]:901) and, in keeping with the NLST, greater than 25% of subjects screened have lung nodules suspicious for lung cancer. As a result, many leading health practices have created specific lung nodule programs to handle the volume in an effort to deliver timely care in the evaluation of lung cancer.
Pulmonary specialists managing patients with lung nodules are faced with the difficult challenge of deciding if a patient with a nodule is a candidate for serial surveillance, tissue biopsy (transthoracic needle aspiration [TTNA] vs. bronchoscopic biopsy [TBX]), or surgical resection. Calculation of the probability of a nodule being malignant is most helpful in making these decisions for patients with low and high malignancy risk factors, as surveillance and resection are appropriate steps, respectively. However, for those with an intermediate (5%-65%) probability of having a malignant nodule, the diagnostic procedure risks, yields, and timing have to be considered because delayed sampling or false-negative results may negatively impact survival. Kanashiki et al (Oncol Rep. 2003;10[3]:649) showed that worse survival is associated with patients with imaging-to-diagnosis times of greater than 4 months. Over the past decade, image-guided bronchoscopy has been used to improve the yield for tissue sampling of smaller peripheral nodules in a timely fashion. The most common method of image-guided bronchoscopy today is electromagnetic navigation bronchoscopy (ENB).
Electromagnetic navigation bronchoscopy has shown promise for increasing diagnostic yields for peripheral nodules (PN) over conventional bronchoscopy. Over time, the improved yields have plateaued as ENB use in clinical practice increased and limitations of the early generation technology became apparent. Earlier ENB technology uses a single inspiratory CT scan of the chest to reconstruct a 3D virtual model of the airways and parenchyma. A tracked sensor is then used to navigate through the imaging reconstructed airways toward the targeted lesion, the sensor is then removed, and through a dedicated catheter instruments are used to obtain samples from the lesion. In a meta-analysis using this technology, lesions greater than 2 cm had a diagnostic yield ranging from 66.7% to 94.7%. However, as the PN size decreased to less than or equal to 2 cm, the diagnostic yield range dropped significantly with some yields reported as low as 18.2% (van ‘t Westeinde et al. Chest. 2012;142(2):377). More recently, Ost and colleagues performed a multicenter study of consecutive patients undergoing bronchoscopic sampling of PN (Ost et al. Am J Respir Crit Care Med. 2016;193[1]:68). Although it was not a randomized trial and each bronchoscopist influenced the selection of the sampling technique, the authors reported that the diagnostic yields for navigation-guided bronchoscopy were lower than conventional bronchoscopy, 38.5% and 63.7%, respectively. Taken on face value alone, one might conclude that ENB not be used to biopsy PNs. However, deeper analysis of the data showed that 97% of the ENB procedures were performed using the earlier technology described above, suggesting that the single inspiratory imaging CT scan and navigation procedure technique, which differs significantly from conventional bronchoscopy, may have some influence on the lower than expected yields.
Despite increasing use and experience with ENB, diagnostic yields remain static. Chen and colleagues hypothesized that using a single inspiratory CT scan may not allow the endoscopist to make adjustments for PN movement as the lung moves during the respiratory cycle. Using different imaging protocol, the investigators assessed movement of 85 lung nodules during the respiratory cycle with paired-full inspiration and tidal-volume expiration, thin sliced (0.5-1.0 mm) CT scans. They found that the average motion of all lesions during respiration was 17.6 mm, 12.2 mm in the right-upper lobe, 10.6 mm in the left-upper lobe, and 25.3 mm and 23.8 mm in the right- and left- lower lobes, respectively (Chen et al. Chest. 2015;147[5];1275) (Fig. 1). They concluded that the location of targeted lesions on a single inspiration planning CT scan alone does not accurately represent the position of the lesion during bronchoscopy.
Although being able to correct for nodule movement throughout the respiratory cycle during the procedure is a significant improvement, it doesn’t guarantee that the tissue sample is obtained from the targeted lesion. To accomplish that, the system would have to be able to determine when the instrument being used to sample is in the target. The earlier ENB systems allowed for navigation to the target with a separate sensor through a steerable catheter. However, when the target was reached, the sensor had to be removed so that sampling instruments could be introduced into the catheter. Since the instruments are not tracked and the movement of the nodule is occurring, there is no guarantee that the instrument is in the target at the time of sampling. Advanced technology now allows for the tracking sensor to be placed in the tip of standard bronchoscopy instruments, making them “tip-tracked” and able to be used with standard bronchoscopes and equipment; thus, making the new ENB procedure similar to conventional bronchoscopy that was shown to have higher diagnostic yields (Figs. 2 and 3).
Our institution incorporated this technology (Veran Medical, St. Louis) into our advanced diagnostic and interventional pulmonary program for lung nodules and published our initial experience and results. During the initial 8 months of screening for lung cancer, we performed procedures on 44 patients with PNs suspicious for lung cancer. The rate for successful target sampling was 90.2% with a cancer diagnosis rate of 39%, which is similar to that found in the NLST. Those patients who had nonmalignant but abnormal pathologic findings (inflammation, granuloma, fibrosis, and so on) were monitored for a minimum of 12 months. Most of the lesions either remained stable or disappeared on follow-up imaging (Flenaugh et al. The Internet Journal of Pulmonary Medicine. 2016;18[1]). We concluded that (1) the combination of paired inspiratory and expiratory CT scan imaging accounts for nodule movement and (2) using tip-tracked conventional instruments to enter into the lesion at the time of biopsy contributes to improved yields.
Newer ENB technology is not limited to transbronchial sampling. For PNs less than 2 cm and deep in the lung periphery, current recommendations prefer TTNA over bronchoscopic biopsy because of yield rates of 90% (Chest. 2007; 132(suppl 3):131S). Using the same paired CT scanning and tip-tracking method on transthoracic needles, the new systems allow pulmonologists to perform electromagnetic transthoracic needle aspiration (ETTNA) of PNs using the same basic equipment and during the same procedure visit (Fig. 4). This “one stop shopping” approach of bronchoscopy with the option of converting to ETTNA if the PN is not reachable endoscopically has proven to be cost efficient and allows for timely diagnosis and focused care (Yarmis et al. J Thorac Dis. 2016;8(1):186). In a prospective study designed specifically to assess feasibility, safety, and diagnostic yield of ETTNA in a single procedure, Yarmis and colleagues enrolled 24 patients to undergo endobronchial ultrasound for lung cancer staging followed by ENB and ETTNA. Ninety-six percent of the patients were candidates for ETTNA. The authors reported the yield for ETTNA was 83%, ETTNA plus ENB 87%, and ETTNA plus ENB plus endobronchial ultrasound for complete staging was 92%. Five pneumothoraces were reported; however, only two (8%) required a drainage intervention. This protocol is unique because it makes use of several advanced diagnostic procedures, including tip-tracked navigation technology, to localize, sample, diagnose, and stage during one patient procedure visit.
As lung cancer screening becomes commonplace in clinical practice and imaging technology improves, pulmonary specialists can expect to encounter and manage a greater number of pulmonary nodules. Advancements in technology now offer options for improving diagnostic accuracy while providing timely, safe, and cost effective care. While not all new technology will prove beneficial in disease management, those that improve the deficiencies of earlier technology offer us the best chance to improve practice. This perspective highlights such technology.
Dr. Flenaugh is Associate Professor, Director of Advanced Diagnostic & Interventional Pulmonary Service,Morehouse School of Medicine and Grady Hospital, Atlanta; Dr. Foreman is Professor of Medicine, Associate Chair for Research, Pulmonary & Critical Care Medicine, Morehouse School of Medicine.
NETWORKS: Disaster preparedness. New acronyms. ECS in transplantation. Electronic cigarettes.
Disaster Response
Lessons from Orlando
The recent nightclub shootings in Orlando have forced my colleagues and I at our Level I Trauma Center to reexamine the way we do business. Our typical approach to injury involves resource-intense therapy with a gang of clinicians, while anticipating no more than one or two patients at a time. While this model is excellent for training, we would struggle with the scale of casualties seen in Orlando.
Several observations may be made internally and have been made in the press. Triage should take place prior to the emergency department so that patients are appropriately prioritized to high-intensity support. Fundamental high-impact interventions requiring simple application, such as tourniquets, should be part of the training for all medical and nonmedical first responders. Perhaps most importantly, we need to reexamine the concept that health care is provided by competing geographic and economic entities. Evolution of trauma care has “followed the money” but not necessarily the need. An approach viewing trauma care as a right and acute response as a community resource may be necessary.
In 2008, the Republican Party held its convention in St. Paul, Minn. Reports indicated that 20,000-50,000 individuals were expected to enter the city, including protesters and anarchist groups. We prepared together for events ranging from vehicular crashes to biologic agents or explosive events (Dries et al. J Trauma. 2012; 73[6]:1614). Since then, however, there has been little community-wide planning.
Orlando reminds us that we dare not leave these plans on the shelf.
David Dries, MD, FCCP
Steering Committee Member
Practice Operations
MACRA, QPP, MIPS, APM: Know these acronyms
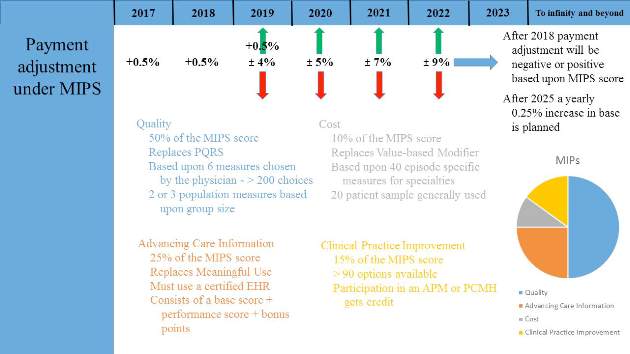
In October 2015, Congress passed the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). A bipartisan legislation, it replaces the flawed Sustainable Growth Rate (SGR) formula that would have forced a 21% cut in Medicare payments to clinicians. MACRA established Quality Payment Program (QPP) that has two paths that link quality to payments: the Merit-Based Incentive Payment System (MIPS) or Advanced Alternative Payment Models (APMs).
MIPS streamlines three currently independent programs – (Physician Quality Reporting Program [PQRS], Value-Based Payment Modifier [VM], and Medicare Electronic Health Records Incentive Program) – into a single program in which eligible professions (EPs) will be measured on quality (50%), resource use/cost (10%), clinical practice improvement activities (15%), and advancing care information (25%). The resulting composite performance score (CPS, scale 0-100) is used to determine and apply a +/- or neutral payment adjustment based on a performance threshold. Payment adjustments will begin in 2019 (based on 2017 performance period). Most physicians will be subject to MIPS, which does not apply to hospitals or facilities.
APMs are new approaches to paying for medical care incentivizing quality and value. As defined by MACRA, APMs include CMS Innovation Center models, the Medicare Shared Saving program, and certain demonstration programs. To qualify for payments, the APMs must also use certified EHR technology, report on certain quality measures, and bear more than nominal financial risk.
Both MIPS and APMs are value-based payment models that incentivize providers on quality, outcomes, and cost containment. Most physicians who see Medicare patients will be required to report either the MIPS or Advanced APM track starting in January 2017.
Editor’s Note – See additional article on MACRA on page in this issue.
Adel Bassily-Marcus, MD, FCCP
Vice-Chair
Transplant
Extracorporeal circulatory support in thoracic medicine and surgery – evolving technology and expanding role
There is growing interest in the use of extracorporeal support (ECS) beyond intraoperative and perioperative utility. This has been driven by improvements in safety and efficacy resulting from corresponding technological advances and enhanced user ability. The paucity of donors, however, remains a significant limiting factor in lung transplantation (LT), and there is a growing number of recipients on the waiting list getting too sick for transplantation. ECS is now commonly used to bridge recipients to LT, and reported outcomes show great promise. Indeed, there is even a growing interest in combining ECS with the ex vivo reconditioning of lungs in a further attempt to broaden the donor pool.
This newly developing paradigm constitutes a confluence of contemporary technologies that should allow more marginal or previously unacceptable donor lungs to be procured and also for the use of cardiopulmonary support to bridge sicker recipients safely. As with most technologies, the prerequisite capital outlay, training, and logistical resources will be required to allow for the acquisition of skill and safety. Furthermore, these trends will likely stimulate development of standards and guidelines to ensure a continuing quest for excellence.
The ongoing use of ECS in transplantation has a ripple effect that may prompt its use in other clinical scenarios, such as a rescue therapy in acute exacerbations of COPD, an alternative to mechanical ventilation following complex thoracic pulmonary or esophageal resections, and in cases of unexpected intraoperative cardiopulmonary collapse. One thing remains likely, however, ECS is here to stay.
Jeremiah Hayanga, MD
Steering Committee Member
Norihisa Shigemura, MD
Steering Committee Member
Women’s Health
Exposure of adolescents to electronic cigarettes: still a cause for alarm despite recent FDA ruling
Developed in 2003, electronic cigarettes (e-cigarettes) have been available in the United States since 2007. Between 2010 and 2013, adult use doubled. By 2013, the major tobacco companies had entered the market, and e-cigarettes were marketed widely (television, Internet, and print) as healthier alternatives to tobacco, useful for quitting smoking, and a way to circumvent smoke-free laws by allowing smokers to “smoke anywhere” (Grana et al. Circulation. 2014;129[19]:1972).
For adolescents, e-cigarette use tripled between 2013 and 2014, from 4.5% (660,000) to 13.4% (2 million) for high school students and from 1.1% (120,000) to 3.9% (450,000) for middle school students (CDC Press Release. http://www.cdc.gov/media/releases/2015/p0416-e-cigarette-use.html). Teenage experimentation, in conjunction with susceptibility to brain-modifying effects of nicotine, places this population at risk for lifelong nicotine addiction. Teenagers who use e-cigarettes are more likely to become regular cigarette smokers than nonusers (Dutra et al. JAMA Pediatr. 2014;168[7]:610; Levanthal et al. JAMA. 2015;314[7]:700). Local and state municipalities have enacted legislation, adding e-cigarettes and other electronic nicotine delivery systems (ENDS) to existing tobacco regulations. On May 5, 2016, a long-anticipated ruling from the FDA extended oversight to include all tobacco products, including e-cigarettes and hookahs, allowing the agency to address public health concerns, such as youth access. However, a key provision of the new tobacco “deeming” rules was subsequently removed less than a month later – one that would have removed flavored e-cigarettes, cigars, hookahs, and other flavored tobacco products from the market in November pending review by the Food and Drug Administration (Boyles. MedPage Today. medpagetoday.com/pulmonology/smoking/58274).
ENDS as a smoking cessation tool, a “safer” alternative to combustible tobacco, is much debated (Green et al. N Engl J Med. 2016;374[14]:1301). There is accumulating evidence of its in vivo and in vitro toxicity (Bhatnagar et al. Circulation. 2014;130[16]:1418; Gibbs et al. Chest. 2016;149[2]:552). Studies have shown that the varied concentration and flavorings used are cytotoxic to human embryonic stem cells as well as mice neural stem cells (Bahl et al. Reprod Toxicol. 2012[4];34:529) and that exposure to propylene glycol and glycerin, main base ingredients in e-liquids, can result in eye and respiratory irritation (Grana et al. Circulation. 2014; 129[19]:1972). Additionally, current evidence does not support e-cigarettes for smoking cessation (Grana et al. Circulation. 2014;129[19]:1972). The accumulating evidence of adverse effects and the increased use in adolescents underscores the need for stricter regulations by the FDA in order to prevent renormalization of the smoking behavior and to protect public health. The rollout of the FDA’s ruling will warrant ongoing evaluation.
Linda S. Efferen, MD, MBA
Consultant
Amanpreet Kaur, MD
Steering Committee Member
Disaster Response
Lessons from Orlando
The recent nightclub shootings in Orlando have forced my colleagues and I at our Level I Trauma Center to reexamine the way we do business. Our typical approach to injury involves resource-intense therapy with a gang of clinicians, while anticipating no more than one or two patients at a time. While this model is excellent for training, we would struggle with the scale of casualties seen in Orlando.
Several observations may be made internally and have been made in the press. Triage should take place prior to the emergency department so that patients are appropriately prioritized to high-intensity support. Fundamental high-impact interventions requiring simple application, such as tourniquets, should be part of the training for all medical and nonmedical first responders. Perhaps most importantly, we need to reexamine the concept that health care is provided by competing geographic and economic entities. Evolution of trauma care has “followed the money” but not necessarily the need. An approach viewing trauma care as a right and acute response as a community resource may be necessary.
In 2008, the Republican Party held its convention in St. Paul, Minn. Reports indicated that 20,000-50,000 individuals were expected to enter the city, including protesters and anarchist groups. We prepared together for events ranging from vehicular crashes to biologic agents or explosive events (Dries et al. J Trauma. 2012; 73[6]:1614). Since then, however, there has been little community-wide planning.
Orlando reminds us that we dare not leave these plans on the shelf.
David Dries, MD, FCCP
Steering Committee Member
Practice Operations
MACRA, QPP, MIPS, APM: Know these acronyms
In October 2015, Congress passed the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). A bipartisan legislation, it replaces the flawed Sustainable Growth Rate (SGR) formula that would have forced a 21% cut in Medicare payments to clinicians. MACRA established Quality Payment Program (QPP) that has two paths that link quality to payments: the Merit-Based Incentive Payment System (MIPS) or Advanced Alternative Payment Models (APMs).
MIPS streamlines three currently independent programs – (Physician Quality Reporting Program [PQRS], Value-Based Payment Modifier [VM], and Medicare Electronic Health Records Incentive Program) – into a single program in which eligible professions (EPs) will be measured on quality (50%), resource use/cost (10%), clinical practice improvement activities (15%), and advancing care information (25%). The resulting composite performance score (CPS, scale 0-100) is used to determine and apply a +/- or neutral payment adjustment based on a performance threshold. Payment adjustments will begin in 2019 (based on 2017 performance period). Most physicians will be subject to MIPS, which does not apply to hospitals or facilities.
APMs are new approaches to paying for medical care incentivizing quality and value. As defined by MACRA, APMs include CMS Innovation Center models, the Medicare Shared Saving program, and certain demonstration programs. To qualify for payments, the APMs must also use certified EHR technology, report on certain quality measures, and bear more than nominal financial risk.
Both MIPS and APMs are value-based payment models that incentivize providers on quality, outcomes, and cost containment. Most physicians who see Medicare patients will be required to report either the MIPS or Advanced APM track starting in January 2017.
Editor’s Note – See additional article on MACRA on page in this issue.
Adel Bassily-Marcus, MD, FCCP
Vice-Chair
Transplant
Extracorporeal circulatory support in thoracic medicine and surgery – evolving technology and expanding role
There is growing interest in the use of extracorporeal support (ECS) beyond intraoperative and perioperative utility. This has been driven by improvements in safety and efficacy resulting from corresponding technological advances and enhanced user ability. The paucity of donors, however, remains a significant limiting factor in lung transplantation (LT), and there is a growing number of recipients on the waiting list getting too sick for transplantation. ECS is now commonly used to bridge recipients to LT, and reported outcomes show great promise. Indeed, there is even a growing interest in combining ECS with the ex vivo reconditioning of lungs in a further attempt to broaden the donor pool.
This newly developing paradigm constitutes a confluence of contemporary technologies that should allow more marginal or previously unacceptable donor lungs to be procured and also for the use of cardiopulmonary support to bridge sicker recipients safely. As with most technologies, the prerequisite capital outlay, training, and logistical resources will be required to allow for the acquisition of skill and safety. Furthermore, these trends will likely stimulate development of standards and guidelines to ensure a continuing quest for excellence.
The ongoing use of ECS in transplantation has a ripple effect that may prompt its use in other clinical scenarios, such as a rescue therapy in acute exacerbations of COPD, an alternative to mechanical ventilation following complex thoracic pulmonary or esophageal resections, and in cases of unexpected intraoperative cardiopulmonary collapse. One thing remains likely, however, ECS is here to stay.
Jeremiah Hayanga, MD
Steering Committee Member
Norihisa Shigemura, MD
Steering Committee Member
Women’s Health
Exposure of adolescents to electronic cigarettes: still a cause for alarm despite recent FDA ruling
Developed in 2003, electronic cigarettes (e-cigarettes) have been available in the United States since 2007. Between 2010 and 2013, adult use doubled. By 2013, the major tobacco companies had entered the market, and e-cigarettes were marketed widely (television, Internet, and print) as healthier alternatives to tobacco, useful for quitting smoking, and a way to circumvent smoke-free laws by allowing smokers to “smoke anywhere” (Grana et al. Circulation. 2014;129[19]:1972).
For adolescents, e-cigarette use tripled between 2013 and 2014, from 4.5% (660,000) to 13.4% (2 million) for high school students and from 1.1% (120,000) to 3.9% (450,000) for middle school students (CDC Press Release. http://www.cdc.gov/media/releases/2015/p0416-e-cigarette-use.html). Teenage experimentation, in conjunction with susceptibility to brain-modifying effects of nicotine, places this population at risk for lifelong nicotine addiction. Teenagers who use e-cigarettes are more likely to become regular cigarette smokers than nonusers (Dutra et al. JAMA Pediatr. 2014;168[7]:610; Levanthal et al. JAMA. 2015;314[7]:700). Local and state municipalities have enacted legislation, adding e-cigarettes and other electronic nicotine delivery systems (ENDS) to existing tobacco regulations. On May 5, 2016, a long-anticipated ruling from the FDA extended oversight to include all tobacco products, including e-cigarettes and hookahs, allowing the agency to address public health concerns, such as youth access. However, a key provision of the new tobacco “deeming” rules was subsequently removed less than a month later – one that would have removed flavored e-cigarettes, cigars, hookahs, and other flavored tobacco products from the market in November pending review by the Food and Drug Administration (Boyles. MedPage Today. medpagetoday.com/pulmonology/smoking/58274).
ENDS as a smoking cessation tool, a “safer” alternative to combustible tobacco, is much debated (Green et al. N Engl J Med. 2016;374[14]:1301). There is accumulating evidence of its in vivo and in vitro toxicity (Bhatnagar et al. Circulation. 2014;130[16]:1418; Gibbs et al. Chest. 2016;149[2]:552). Studies have shown that the varied concentration and flavorings used are cytotoxic to human embryonic stem cells as well as mice neural stem cells (Bahl et al. Reprod Toxicol. 2012[4];34:529) and that exposure to propylene glycol and glycerin, main base ingredients in e-liquids, can result in eye and respiratory irritation (Grana et al. Circulation. 2014; 129[19]:1972). Additionally, current evidence does not support e-cigarettes for smoking cessation (Grana et al. Circulation. 2014;129[19]:1972). The accumulating evidence of adverse effects and the increased use in adolescents underscores the need for stricter regulations by the FDA in order to prevent renormalization of the smoking behavior and to protect public health. The rollout of the FDA’s ruling will warrant ongoing evaluation.
Linda S. Efferen, MD, MBA
Consultant
Amanpreet Kaur, MD
Steering Committee Member
Disaster Response
Lessons from Orlando
The recent nightclub shootings in Orlando have forced my colleagues and I at our Level I Trauma Center to reexamine the way we do business. Our typical approach to injury involves resource-intense therapy with a gang of clinicians, while anticipating no more than one or two patients at a time. While this model is excellent for training, we would struggle with the scale of casualties seen in Orlando.
Several observations may be made internally and have been made in the press. Triage should take place prior to the emergency department so that patients are appropriately prioritized to high-intensity support. Fundamental high-impact interventions requiring simple application, such as tourniquets, should be part of the training for all medical and nonmedical first responders. Perhaps most importantly, we need to reexamine the concept that health care is provided by competing geographic and economic entities. Evolution of trauma care has “followed the money” but not necessarily the need. An approach viewing trauma care as a right and acute response as a community resource may be necessary.
In 2008, the Republican Party held its convention in St. Paul, Minn. Reports indicated that 20,000-50,000 individuals were expected to enter the city, including protesters and anarchist groups. We prepared together for events ranging from vehicular crashes to biologic agents or explosive events (Dries et al. J Trauma. 2012; 73[6]:1614). Since then, however, there has been little community-wide planning.
Orlando reminds us that we dare not leave these plans on the shelf.
David Dries, MD, FCCP
Steering Committee Member
Practice Operations
MACRA, QPP, MIPS, APM: Know these acronyms
In October 2015, Congress passed the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). A bipartisan legislation, it replaces the flawed Sustainable Growth Rate (SGR) formula that would have forced a 21% cut in Medicare payments to clinicians. MACRA established Quality Payment Program (QPP) that has two paths that link quality to payments: the Merit-Based Incentive Payment System (MIPS) or Advanced Alternative Payment Models (APMs).
MIPS streamlines three currently independent programs – (Physician Quality Reporting Program [PQRS], Value-Based Payment Modifier [VM], and Medicare Electronic Health Records Incentive Program) – into a single program in which eligible professions (EPs) will be measured on quality (50%), resource use/cost (10%), clinical practice improvement activities (15%), and advancing care information (25%). The resulting composite performance score (CPS, scale 0-100) is used to determine and apply a +/- or neutral payment adjustment based on a performance threshold. Payment adjustments will begin in 2019 (based on 2017 performance period). Most physicians will be subject to MIPS, which does not apply to hospitals or facilities.
APMs are new approaches to paying for medical care incentivizing quality and value. As defined by MACRA, APMs include CMS Innovation Center models, the Medicare Shared Saving program, and certain demonstration programs. To qualify for payments, the APMs must also use certified EHR technology, report on certain quality measures, and bear more than nominal financial risk.
Both MIPS and APMs are value-based payment models that incentivize providers on quality, outcomes, and cost containment. Most physicians who see Medicare patients will be required to report either the MIPS or Advanced APM track starting in January 2017.
Editor’s Note – See additional article on MACRA on page in this issue.
Adel Bassily-Marcus, MD, FCCP
Vice-Chair
Transplant
Extracorporeal circulatory support in thoracic medicine and surgery – evolving technology and expanding role
There is growing interest in the use of extracorporeal support (ECS) beyond intraoperative and perioperative utility. This has been driven by improvements in safety and efficacy resulting from corresponding technological advances and enhanced user ability. The paucity of donors, however, remains a significant limiting factor in lung transplantation (LT), and there is a growing number of recipients on the waiting list getting too sick for transplantation. ECS is now commonly used to bridge recipients to LT, and reported outcomes show great promise. Indeed, there is even a growing interest in combining ECS with the ex vivo reconditioning of lungs in a further attempt to broaden the donor pool.
This newly developing paradigm constitutes a confluence of contemporary technologies that should allow more marginal or previously unacceptable donor lungs to be procured and also for the use of cardiopulmonary support to bridge sicker recipients safely. As with most technologies, the prerequisite capital outlay, training, and logistical resources will be required to allow for the acquisition of skill and safety. Furthermore, these trends will likely stimulate development of standards and guidelines to ensure a continuing quest for excellence.
The ongoing use of ECS in transplantation has a ripple effect that may prompt its use in other clinical scenarios, such as a rescue therapy in acute exacerbations of COPD, an alternative to mechanical ventilation following complex thoracic pulmonary or esophageal resections, and in cases of unexpected intraoperative cardiopulmonary collapse. One thing remains likely, however, ECS is here to stay.
Jeremiah Hayanga, MD
Steering Committee Member
Norihisa Shigemura, MD
Steering Committee Member
Women’s Health
Exposure of adolescents to electronic cigarettes: still a cause for alarm despite recent FDA ruling
Developed in 2003, electronic cigarettes (e-cigarettes) have been available in the United States since 2007. Between 2010 and 2013, adult use doubled. By 2013, the major tobacco companies had entered the market, and e-cigarettes were marketed widely (television, Internet, and print) as healthier alternatives to tobacco, useful for quitting smoking, and a way to circumvent smoke-free laws by allowing smokers to “smoke anywhere” (Grana et al. Circulation. 2014;129[19]:1972).
For adolescents, e-cigarette use tripled between 2013 and 2014, from 4.5% (660,000) to 13.4% (2 million) for high school students and from 1.1% (120,000) to 3.9% (450,000) for middle school students (CDC Press Release. http://www.cdc.gov/media/releases/2015/p0416-e-cigarette-use.html). Teenage experimentation, in conjunction with susceptibility to brain-modifying effects of nicotine, places this population at risk for lifelong nicotine addiction. Teenagers who use e-cigarettes are more likely to become regular cigarette smokers than nonusers (Dutra et al. JAMA Pediatr. 2014;168[7]:610; Levanthal et al. JAMA. 2015;314[7]:700). Local and state municipalities have enacted legislation, adding e-cigarettes and other electronic nicotine delivery systems (ENDS) to existing tobacco regulations. On May 5, 2016, a long-anticipated ruling from the FDA extended oversight to include all tobacco products, including e-cigarettes and hookahs, allowing the agency to address public health concerns, such as youth access. However, a key provision of the new tobacco “deeming” rules was subsequently removed less than a month later – one that would have removed flavored e-cigarettes, cigars, hookahs, and other flavored tobacco products from the market in November pending review by the Food and Drug Administration (Boyles. MedPage Today. medpagetoday.com/pulmonology/smoking/58274).
ENDS as a smoking cessation tool, a “safer” alternative to combustible tobacco, is much debated (Green et al. N Engl J Med. 2016;374[14]:1301). There is accumulating evidence of its in vivo and in vitro toxicity (Bhatnagar et al. Circulation. 2014;130[16]:1418; Gibbs et al. Chest. 2016;149[2]:552). Studies have shown that the varied concentration and flavorings used are cytotoxic to human embryonic stem cells as well as mice neural stem cells (Bahl et al. Reprod Toxicol. 2012[4];34:529) and that exposure to propylene glycol and glycerin, main base ingredients in e-liquids, can result in eye and respiratory irritation (Grana et al. Circulation. 2014; 129[19]:1972). Additionally, current evidence does not support e-cigarettes for smoking cessation (Grana et al. Circulation. 2014;129[19]:1972). The accumulating evidence of adverse effects and the increased use in adolescents underscores the need for stricter regulations by the FDA in order to prevent renormalization of the smoking behavior and to protect public health. The rollout of the FDA’s ruling will warrant ongoing evaluation.
Linda S. Efferen, MD, MBA
Consultant
Amanpreet Kaur, MD
Steering Committee Member
Catching up with our past presidents
Where are they now? What have they been up to? CHEST’s Past Presidents each forged the way for the many successes of the American College of Chest Physicians (CHEST), leading to enhanced patient care around the globe. Their outstanding leadership and vision are evidenced today in many of CHEST’s current initiatives, and now it is time to check in with these past leaders to give us a look at what’s new.
Alex G. Little, MD, FCCP
President 1990-1991
Being President of the American College of Chest Physicians was a remarkable and exhilarating experience beginning with my inauguration in San Francisco in 1990. Although I had been active with the College for several years, the responsibility of the presidency entailed a much closer relationship with the organization, the excellent staff, the physician leaders, the greater membership, and notably, Dr. Al Soffer. As the Executive Director, Al was my go to advisor and guide for questions and advice. He and his wife Izzy became good personal friends and that relationship is one of the major benefits of my presidency (although it never resulted in him showing any mercy on the tennis courts).
For me, as a surgeon, one of the appealing aspects of the College, and, in particular, its annual meeting, was its interdisciplinary nature with pulmonologists, surgeons, and cardiologists interacting in a way that more narrowly focused specialty societies rarely provide. Learning alternative perspectives and hearing from other disciplines is always interesting and occasionally critically important for progress toward maximal patient care.
During my tenure, there were several noteworthy events. The College continued to exhibit robust growth in membership, strengthening its role in supporting chest physicians. We opened the new (amazingly, now the old) headquarters building in Northbrook, signaling a commitment to remain state of the art and joined the challenge of providing continuing medical education for our members.
I retired from clinical practice and as Chair of Surgery at Wright State in 2010 when my wife Louise and I settled in Tucson. I am involved with teaching and mentoring general and cardiothoracic residents at the University of Arizona and also keep active with ongoing clinical research projects. With my leisure time, I play tennis, read books I should have gotten to in earlier years, look for a publisher for a book I have written on the evolution of thoracic surgery (for the general reader), and admire my wife’s expertise in making glass beads and jewelry.
Where are they now? What have they been up to? CHEST’s Past Presidents each forged the way for the many successes of the American College of Chest Physicians (CHEST), leading to enhanced patient care around the globe. Their outstanding leadership and vision are evidenced today in many of CHEST’s current initiatives, and now it is time to check in with these past leaders to give us a look at what’s new.
Alex G. Little, MD, FCCP
President 1990-1991
Being President of the American College of Chest Physicians was a remarkable and exhilarating experience beginning with my inauguration in San Francisco in 1990. Although I had been active with the College for several years, the responsibility of the presidency entailed a much closer relationship with the organization, the excellent staff, the physician leaders, the greater membership, and notably, Dr. Al Soffer. As the Executive Director, Al was my go to advisor and guide for questions and advice. He and his wife Izzy became good personal friends and that relationship is one of the major benefits of my presidency (although it never resulted in him showing any mercy on the tennis courts).
For me, as a surgeon, one of the appealing aspects of the College, and, in particular, its annual meeting, was its interdisciplinary nature with pulmonologists, surgeons, and cardiologists interacting in a way that more narrowly focused specialty societies rarely provide. Learning alternative perspectives and hearing from other disciplines is always interesting and occasionally critically important for progress toward maximal patient care.
During my tenure, there were several noteworthy events. The College continued to exhibit robust growth in membership, strengthening its role in supporting chest physicians. We opened the new (amazingly, now the old) headquarters building in Northbrook, signaling a commitment to remain state of the art and joined the challenge of providing continuing medical education for our members.
I retired from clinical practice and as Chair of Surgery at Wright State in 2010 when my wife Louise and I settled in Tucson. I am involved with teaching and mentoring general and cardiothoracic residents at the University of Arizona and also keep active with ongoing clinical research projects. With my leisure time, I play tennis, read books I should have gotten to in earlier years, look for a publisher for a book I have written on the evolution of thoracic surgery (for the general reader), and admire my wife’s expertise in making glass beads and jewelry.
Where are they now? What have they been up to? CHEST’s Past Presidents each forged the way for the many successes of the American College of Chest Physicians (CHEST), leading to enhanced patient care around the globe. Their outstanding leadership and vision are evidenced today in many of CHEST’s current initiatives, and now it is time to check in with these past leaders to give us a look at what’s new.
Alex G. Little, MD, FCCP
President 1990-1991
Being President of the American College of Chest Physicians was a remarkable and exhilarating experience beginning with my inauguration in San Francisco in 1990. Although I had been active with the College for several years, the responsibility of the presidency entailed a much closer relationship with the organization, the excellent staff, the physician leaders, the greater membership, and notably, Dr. Al Soffer. As the Executive Director, Al was my go to advisor and guide for questions and advice. He and his wife Izzy became good personal friends and that relationship is one of the major benefits of my presidency (although it never resulted in him showing any mercy on the tennis courts).
For me, as a surgeon, one of the appealing aspects of the College, and, in particular, its annual meeting, was its interdisciplinary nature with pulmonologists, surgeons, and cardiologists interacting in a way that more narrowly focused specialty societies rarely provide. Learning alternative perspectives and hearing from other disciplines is always interesting and occasionally critically important for progress toward maximal patient care.
During my tenure, there were several noteworthy events. The College continued to exhibit robust growth in membership, strengthening its role in supporting chest physicians. We opened the new (amazingly, now the old) headquarters building in Northbrook, signaling a commitment to remain state of the art and joined the challenge of providing continuing medical education for our members.
I retired from clinical practice and as Chair of Surgery at Wright State in 2010 when my wife Louise and I settled in Tucson. I am involved with teaching and mentoring general and cardiothoracic residents at the University of Arizona and also keep active with ongoing clinical research projects. With my leisure time, I play tennis, read books I should have gotten to in earlier years, look for a publisher for a book I have written on the evolution of thoracic surgery (for the general reader), and admire my wife’s expertise in making glass beads and jewelry.
A MACRA primer
Most physicians realize that the specter of the Sustainable Growth Rate (SGR) has been replaced by a “new plan” enacted by Congress under the guise of the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015. A major goal of the programs defined by MACRA is to provide quality care while improving value, the Quality Payment Program (QPP). There are currently two paths for reimbursement from which physicians may choose defined by QPP: the Merit-based Incentive Payment System (MIPS) or the Advanced Alternative Payment Models (APMs). These will be explained in general terms but it would benefit all health-care professionals to visit the CMS website for additional details on the program.
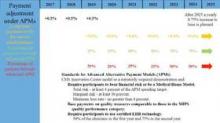
Most physicians will initially choose MIPS by default as most do not currently participate in programs that qualify as APMs. MIPS will eventually result in the demise of the multiple reporting systems presently used by CMS to include the Physician Quality Reporting System (PQRS), the Value-Based Modifier (VBM) Program, and the Medicare Electronic Health Record (EHR) Incentive Program (Meaningful Use). These will be streamlined into a single program, although many of the components are carried through to MIPS (Fig. 1).
Data from health-care providers will be collected through a variety of sources beginning in January 2017 and this will be used to determine the MIPS score as briefly outlined by the colored text in Figure 1. The 2017 data will determine the MIPS Composite Performance Score (CPS). From 2017 through 2019, CMS will provide a 0.5% increase in payment for services. Between 2020 and 2025, no increase is planned, but starting in 2026, a yearly 0.25% increase in reimbursement is planned. In 2019, physician payment will be adjusted positively or negatively by 4% based upon their MIPS CPS and a threshold CPS determined for all participants. This adjustment will be revenue-neutral, so for every winner there will be a corresponding loser based upon one’s MIPS score. However, there is a scaling factor built into the system for years 2019 to 2024, using up to $500 million to reward those whose CPS are at the highest levels. This adjustment will increase to 5% in 2020, 7% in 2021, and 9% from 2022 onward. Eligible providers can participate as an individual or as a group.
The Advanced Alternative Payment Model, as defined by MACRA, may include a CMS Innovation Center model, MSSP (Medicare Shared Savings Program), Demonstration under the Health Care Quality Demonstration Program, or Demonstration required by federal law. To be an eligible APM requires that these entities: require participants to use certified EHR technology; base payment on quality measures comparable to those in the MIPS quality performance category; either require APM entities to bear more than nominal financial risk for monetary losses; or be a Medical Home Model expanded under Center for Medicare and Medicaid Innovation authority.
To become a qualifying participant (QP) one must have either a percentage of payments or a percentage of patients through an eligible APM. CMS will calculate a threshold score using Medicare Part B data for professional services and payments in that APM. The percentage of each is illustrated in Figure 2 and will increase from 2019 to 2024. 2017 will be the first year eligible participants will be assessed to determine whether they qualify. If an eligible participant qualifies, year 2018 base payments will be used to determine year 2019 lump sum payment. This is set at 5%. This cycle will continue each year to determine if the participant qualifies for the lump sum distribution. In addition, qualified APMs will receive a yearly 0.75% increase in base payments starting in year 2026. If one participates in an APM but does not meet the threshold for QP set by CMS, one receives either no payment adjustment or may opt to participate in MIPS. Beginning in 2021, CMS may count data from other non-Medicare payers to determine eligibility as a QP.
The goal of the Quality Payment Program is to change the way Medicare pays clinicians and to offer financial incentives for providing high value care. Physicians will be required to participate in either the MIPS or APM programs unless they are in their first year of Part B participation or have a low volume of patients. The program will almost certainly continue to change as input is received from many stakeholders, most importantly health-care professionals and patients. Physicians are, therefore, encouraged to learn more about the program to maximize your reimbursement.
Most physicians realize that the specter of the Sustainable Growth Rate (SGR) has been replaced by a “new plan” enacted by Congress under the guise of the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015. A major goal of the programs defined by MACRA is to provide quality care while improving value, the Quality Payment Program (QPP). There are currently two paths for reimbursement from which physicians may choose defined by QPP: the Merit-based Incentive Payment System (MIPS) or the Advanced Alternative Payment Models (APMs). These will be explained in general terms but it would benefit all health-care professionals to visit the CMS website for additional details on the program.
Most physicians will initially choose MIPS by default as most do not currently participate in programs that qualify as APMs. MIPS will eventually result in the demise of the multiple reporting systems presently used by CMS to include the Physician Quality Reporting System (PQRS), the Value-Based Modifier (VBM) Program, and the Medicare Electronic Health Record (EHR) Incentive Program (Meaningful Use). These will be streamlined into a single program, although many of the components are carried through to MIPS (Fig. 1).
Data from health-care providers will be collected through a variety of sources beginning in January 2017 and this will be used to determine the MIPS score as briefly outlined by the colored text in Figure 1. The 2017 data will determine the MIPS Composite Performance Score (CPS). From 2017 through 2019, CMS will provide a 0.5% increase in payment for services. Between 2020 and 2025, no increase is planned, but starting in 2026, a yearly 0.25% increase in reimbursement is planned. In 2019, physician payment will be adjusted positively or negatively by 4% based upon their MIPS CPS and a threshold CPS determined for all participants. This adjustment will be revenue-neutral, so for every winner there will be a corresponding loser based upon one’s MIPS score. However, there is a scaling factor built into the system for years 2019 to 2024, using up to $500 million to reward those whose CPS are at the highest levels. This adjustment will increase to 5% in 2020, 7% in 2021, and 9% from 2022 onward. Eligible providers can participate as an individual or as a group.
The Advanced Alternative Payment Model, as defined by MACRA, may include a CMS Innovation Center model, MSSP (Medicare Shared Savings Program), Demonstration under the Health Care Quality Demonstration Program, or Demonstration required by federal law. To be an eligible APM requires that these entities: require participants to use certified EHR technology; base payment on quality measures comparable to those in the MIPS quality performance category; either require APM entities to bear more than nominal financial risk for monetary losses; or be a Medical Home Model expanded under Center for Medicare and Medicaid Innovation authority.
To become a qualifying participant (QP) one must have either a percentage of payments or a percentage of patients through an eligible APM. CMS will calculate a threshold score using Medicare Part B data for professional services and payments in that APM. The percentage of each is illustrated in Figure 2 and will increase from 2019 to 2024. 2017 will be the first year eligible participants will be assessed to determine whether they qualify. If an eligible participant qualifies, year 2018 base payments will be used to determine year 2019 lump sum payment. This is set at 5%. This cycle will continue each year to determine if the participant qualifies for the lump sum distribution. In addition, qualified APMs will receive a yearly 0.75% increase in base payments starting in year 2026. If one participates in an APM but does not meet the threshold for QP set by CMS, one receives either no payment adjustment or may opt to participate in MIPS. Beginning in 2021, CMS may count data from other non-Medicare payers to determine eligibility as a QP.
The goal of the Quality Payment Program is to change the way Medicare pays clinicians and to offer financial incentives for providing high value care. Physicians will be required to participate in either the MIPS or APM programs unless they are in their first year of Part B participation or have a low volume of patients. The program will almost certainly continue to change as input is received from many stakeholders, most importantly health-care professionals and patients. Physicians are, therefore, encouraged to learn more about the program to maximize your reimbursement.
Most physicians realize that the specter of the Sustainable Growth Rate (SGR) has been replaced by a “new plan” enacted by Congress under the guise of the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015. A major goal of the programs defined by MACRA is to provide quality care while improving value, the Quality Payment Program (QPP). There are currently two paths for reimbursement from which physicians may choose defined by QPP: the Merit-based Incentive Payment System (MIPS) or the Advanced Alternative Payment Models (APMs). These will be explained in general terms but it would benefit all health-care professionals to visit the CMS website for additional details on the program.
Most physicians will initially choose MIPS by default as most do not currently participate in programs that qualify as APMs. MIPS will eventually result in the demise of the multiple reporting systems presently used by CMS to include the Physician Quality Reporting System (PQRS), the Value-Based Modifier (VBM) Program, and the Medicare Electronic Health Record (EHR) Incentive Program (Meaningful Use). These will be streamlined into a single program, although many of the components are carried through to MIPS (Fig. 1).
Data from health-care providers will be collected through a variety of sources beginning in January 2017 and this will be used to determine the MIPS score as briefly outlined by the colored text in Figure 1. The 2017 data will determine the MIPS Composite Performance Score (CPS). From 2017 through 2019, CMS will provide a 0.5% increase in payment for services. Between 2020 and 2025, no increase is planned, but starting in 2026, a yearly 0.25% increase in reimbursement is planned. In 2019, physician payment will be adjusted positively or negatively by 4% based upon their MIPS CPS and a threshold CPS determined for all participants. This adjustment will be revenue-neutral, so for every winner there will be a corresponding loser based upon one’s MIPS score. However, there is a scaling factor built into the system for years 2019 to 2024, using up to $500 million to reward those whose CPS are at the highest levels. This adjustment will increase to 5% in 2020, 7% in 2021, and 9% from 2022 onward. Eligible providers can participate as an individual or as a group.
The Advanced Alternative Payment Model, as defined by MACRA, may include a CMS Innovation Center model, MSSP (Medicare Shared Savings Program), Demonstration under the Health Care Quality Demonstration Program, or Demonstration required by federal law. To be an eligible APM requires that these entities: require participants to use certified EHR technology; base payment on quality measures comparable to those in the MIPS quality performance category; either require APM entities to bear more than nominal financial risk for monetary losses; or be a Medical Home Model expanded under Center for Medicare and Medicaid Innovation authority.
To become a qualifying participant (QP) one must have either a percentage of payments or a percentage of patients through an eligible APM. CMS will calculate a threshold score using Medicare Part B data for professional services and payments in that APM. The percentage of each is illustrated in Figure 2 and will increase from 2019 to 2024. 2017 will be the first year eligible participants will be assessed to determine whether they qualify. If an eligible participant qualifies, year 2018 base payments will be used to determine year 2019 lump sum payment. This is set at 5%. This cycle will continue each year to determine if the participant qualifies for the lump sum distribution. In addition, qualified APMs will receive a yearly 0.75% increase in base payments starting in year 2026. If one participates in an APM but does not meet the threshold for QP set by CMS, one receives either no payment adjustment or may opt to participate in MIPS. Beginning in 2021, CMS may count data from other non-Medicare payers to determine eligibility as a QP.
The goal of the Quality Payment Program is to change the way Medicare pays clinicians and to offer financial incentives for providing high value care. Physicians will be required to participate in either the MIPS or APM programs unless they are in their first year of Part B participation or have a low volume of patients. The program will almost certainly continue to change as input is received from many stakeholders, most importantly health-care professionals and patients. Physicians are, therefore, encouraged to learn more about the program to maximize your reimbursement.
Something for everyone: LA cuisine, clinical education at CHEST 2016
Los Angeles is famous for its eclectic mix of palate-pleasing dining options. Chic cafes; international flavors; vegan eateries; and local, coastal cuisine are all readily available. When CHEST 2016 travels to Los Angeles in October, we know you’ll satisfy your taste buds and your educational needs.
With so many options to choose from, here are some recommendations from our favorite Los Angeles locals – CHEST members – to help you plan out your menu:
• LA Prime, 35th floor of the Westin Bonaventure Hotel (6-minute drive): Famous for prime beef steaks, seafood, and panoramic city views. Located at 404 S. Figueroa St, Los Angeles, CA 90071
• Water Grill (6-minute drive): This seafood restaurant is sustainably minded and provides a wide array of delicately prepared seafood in a relaxed, elegant space. Located at 544 S. Grand Ave, Los Angeles, CA 90071
• Pacific Dining Car (7-minute drive): Dine on steak in a railway dining car atmosphere at this iconic restaurant open 24 hours a day every day of the year. Located at 1310 W. 6th St, Los Angeles, CA 90017
• Sticky Rice (7-minute drive): Inside Grand Central Market, enjoy Thai “comfort food” with an emphasis on organic, free-range, and locally sourced seasonal ingredients. Located at 317 S. Broadway, Los Angeles, CA 90013
• Mexicali Taco & Co (9-minute drive): Enjoy mouthwatering Baja style Mexican food, reasonable prices, and a casual dining experience. Located at 702 N. Figueroa St, Los Angeles, CA 90012
• Crossroads Kitchen (22-minute drive): Courtesy of Oprah’s former chef Tal Ronnen, this upscale eatery provides an elegant backdrop for refined vegan dishes paired with wines and cocktails. Located at 8284 Melrose Ave, Los Angeles, CA 90046
• The Sky Room in Long Beach (33-minute drive): This hotel bar/eatery offers New American fare and city views, plus music and dancing on weekends. Located at 40 S. Locust Ave, Long Beach, CA 90802
Looking for a quick bite? Here are some options within walking distance to the convention center:
• Yardhouse (5-minute walk): Find the craft beer you’re looking for while benefiting from a large, diverse menu. Located at 800 W. Olympic Blvd, Los Angeles, CA 90015
• Tom’s Urban (1-minute walk): Enjoy a sprawling gastropub featuring an all-day American menu, large draft beers, and sports on big screens. Located at 1011 S. Figueroa St, Los Angeles, CA 90015
• TASTE Food Hall FIGat7th (4-minute walk): Walk over to Figueroa and 7th, and you’ll find a large food court complete with unique flavor profiles that are shaping the contemporary Los Angeles culinary landscape. Located at 735 S. Figueroa St, Los Angeles, CA 90017
Los Angeles is sure to satisfy your inner foodie with its wide variety of culinary options. From October 22 to 26, CHEST 2016 will also offer you a variety of educational options including postgraduate courses, simulation and interactive learning, interdisciplinary programs, problem-based learning sessions, keynotes and honor lectures, industry supported sessions, and more. CHEST 2016 is dedicated to delivering the latest information in pulmonary, critical care, and sleep medicine to you, ensuring you make the best decisions with your patients. Register by August 31 to pay the lowest fees. Learn more at chestmeeting.chestnet.org.
Los Angeles is famous for its eclectic mix of palate-pleasing dining options. Chic cafes; international flavors; vegan eateries; and local, coastal cuisine are all readily available. When CHEST 2016 travels to Los Angeles in October, we know you’ll satisfy your taste buds and your educational needs.
With so many options to choose from, here are some recommendations from our favorite Los Angeles locals – CHEST members – to help you plan out your menu:
• LA Prime, 35th floor of the Westin Bonaventure Hotel (6-minute drive): Famous for prime beef steaks, seafood, and panoramic city views. Located at 404 S. Figueroa St, Los Angeles, CA 90071
• Water Grill (6-minute drive): This seafood restaurant is sustainably minded and provides a wide array of delicately prepared seafood in a relaxed, elegant space. Located at 544 S. Grand Ave, Los Angeles, CA 90071
• Pacific Dining Car (7-minute drive): Dine on steak in a railway dining car atmosphere at this iconic restaurant open 24 hours a day every day of the year. Located at 1310 W. 6th St, Los Angeles, CA 90017
• Sticky Rice (7-minute drive): Inside Grand Central Market, enjoy Thai “comfort food” with an emphasis on organic, free-range, and locally sourced seasonal ingredients. Located at 317 S. Broadway, Los Angeles, CA 90013
• Mexicali Taco & Co (9-minute drive): Enjoy mouthwatering Baja style Mexican food, reasonable prices, and a casual dining experience. Located at 702 N. Figueroa St, Los Angeles, CA 90012
• Crossroads Kitchen (22-minute drive): Courtesy of Oprah’s former chef Tal Ronnen, this upscale eatery provides an elegant backdrop for refined vegan dishes paired with wines and cocktails. Located at 8284 Melrose Ave, Los Angeles, CA 90046
• The Sky Room in Long Beach (33-minute drive): This hotel bar/eatery offers New American fare and city views, plus music and dancing on weekends. Located at 40 S. Locust Ave, Long Beach, CA 90802
Looking for a quick bite? Here are some options within walking distance to the convention center:
• Yardhouse (5-minute walk): Find the craft beer you’re looking for while benefiting from a large, diverse menu. Located at 800 W. Olympic Blvd, Los Angeles, CA 90015
• Tom’s Urban (1-minute walk): Enjoy a sprawling gastropub featuring an all-day American menu, large draft beers, and sports on big screens. Located at 1011 S. Figueroa St, Los Angeles, CA 90015
• TASTE Food Hall FIGat7th (4-minute walk): Walk over to Figueroa and 7th, and you’ll find a large food court complete with unique flavor profiles that are shaping the contemporary Los Angeles culinary landscape. Located at 735 S. Figueroa St, Los Angeles, CA 90017
Los Angeles is sure to satisfy your inner foodie with its wide variety of culinary options. From October 22 to 26, CHEST 2016 will also offer you a variety of educational options including postgraduate courses, simulation and interactive learning, interdisciplinary programs, problem-based learning sessions, keynotes and honor lectures, industry supported sessions, and more. CHEST 2016 is dedicated to delivering the latest information in pulmonary, critical care, and sleep medicine to you, ensuring you make the best decisions with your patients. Register by August 31 to pay the lowest fees. Learn more at chestmeeting.chestnet.org.
Los Angeles is famous for its eclectic mix of palate-pleasing dining options. Chic cafes; international flavors; vegan eateries; and local, coastal cuisine are all readily available. When CHEST 2016 travels to Los Angeles in October, we know you’ll satisfy your taste buds and your educational needs.
With so many options to choose from, here are some recommendations from our favorite Los Angeles locals – CHEST members – to help you plan out your menu:
• LA Prime, 35th floor of the Westin Bonaventure Hotel (6-minute drive): Famous for prime beef steaks, seafood, and panoramic city views. Located at 404 S. Figueroa St, Los Angeles, CA 90071
• Water Grill (6-minute drive): This seafood restaurant is sustainably minded and provides a wide array of delicately prepared seafood in a relaxed, elegant space. Located at 544 S. Grand Ave, Los Angeles, CA 90071
• Pacific Dining Car (7-minute drive): Dine on steak in a railway dining car atmosphere at this iconic restaurant open 24 hours a day every day of the year. Located at 1310 W. 6th St, Los Angeles, CA 90017
• Sticky Rice (7-minute drive): Inside Grand Central Market, enjoy Thai “comfort food” with an emphasis on organic, free-range, and locally sourced seasonal ingredients. Located at 317 S. Broadway, Los Angeles, CA 90013
• Mexicali Taco & Co (9-minute drive): Enjoy mouthwatering Baja style Mexican food, reasonable prices, and a casual dining experience. Located at 702 N. Figueroa St, Los Angeles, CA 90012
• Crossroads Kitchen (22-minute drive): Courtesy of Oprah’s former chef Tal Ronnen, this upscale eatery provides an elegant backdrop for refined vegan dishes paired with wines and cocktails. Located at 8284 Melrose Ave, Los Angeles, CA 90046
• The Sky Room in Long Beach (33-minute drive): This hotel bar/eatery offers New American fare and city views, plus music and dancing on weekends. Located at 40 S. Locust Ave, Long Beach, CA 90802
Looking for a quick bite? Here are some options within walking distance to the convention center:
• Yardhouse (5-minute walk): Find the craft beer you’re looking for while benefiting from a large, diverse menu. Located at 800 W. Olympic Blvd, Los Angeles, CA 90015
• Tom’s Urban (1-minute walk): Enjoy a sprawling gastropub featuring an all-day American menu, large draft beers, and sports on big screens. Located at 1011 S. Figueroa St, Los Angeles, CA 90015
• TASTE Food Hall FIGat7th (4-minute walk): Walk over to Figueroa and 7th, and you’ll find a large food court complete with unique flavor profiles that are shaping the contemporary Los Angeles culinary landscape. Located at 735 S. Figueroa St, Los Angeles, CA 90017
Los Angeles is sure to satisfy your inner foodie with its wide variety of culinary options. From October 22 to 26, CHEST 2016 will also offer you a variety of educational options including postgraduate courses, simulation and interactive learning, interdisciplinary programs, problem-based learning sessions, keynotes and honor lectures, industry supported sessions, and more. CHEST 2016 is dedicated to delivering the latest information in pulmonary, critical care, and sleep medicine to you, ensuring you make the best decisions with your patients. Register by August 31 to pay the lowest fees. Learn more at chestmeeting.chestnet.org.
MOC 10-year assessment
The American Board of Internal Medicine (ABIM) has responded to physicians’ and other stakeholders’ input regarding the Maintenance of Certification (MOC) 10-year assessment and will begin offering an alternate option in January 2018. The new option will include shorter assessments taken more frequently that will be able to be completed from a physician’s office or home. These shorter assessments will identify knowledge gaps, so physicians can tailor their continuing education in order to stay current in knowledge and practice. Successful performance on the shorter assessments will allow physicians to opt out of the longer 10-year exam. The program will be piloted for Internal Medicine and select subspecialties and, based on feedback, will be extended to additional subspecialties at a later date.
Physicians whose certifications expire prior to the new assessment option becoming available will need to pass the current exam in order to maintain certification but then will not need to take another assessment for 10 years.
ABIM’s full announcement can be viewed at abim.org/news/abim-announces-plans-to-offer-physicians-moc-assessment-options-in-january-2018.aspx.
Any questions regarding this development should be directed to the ABIM by visiting www.abim.org/contact.
The American Board of Internal Medicine (ABIM) has responded to physicians’ and other stakeholders’ input regarding the Maintenance of Certification (MOC) 10-year assessment and will begin offering an alternate option in January 2018. The new option will include shorter assessments taken more frequently that will be able to be completed from a physician’s office or home. These shorter assessments will identify knowledge gaps, so physicians can tailor their continuing education in order to stay current in knowledge and practice. Successful performance on the shorter assessments will allow physicians to opt out of the longer 10-year exam. The program will be piloted for Internal Medicine and select subspecialties and, based on feedback, will be extended to additional subspecialties at a later date.
Physicians whose certifications expire prior to the new assessment option becoming available will need to pass the current exam in order to maintain certification but then will not need to take another assessment for 10 years.
ABIM’s full announcement can be viewed at abim.org/news/abim-announces-plans-to-offer-physicians-moc-assessment-options-in-january-2018.aspx.
Any questions regarding this development should be directed to the ABIM by visiting www.abim.org/contact.
The American Board of Internal Medicine (ABIM) has responded to physicians’ and other stakeholders’ input regarding the Maintenance of Certification (MOC) 10-year assessment and will begin offering an alternate option in January 2018. The new option will include shorter assessments taken more frequently that will be able to be completed from a physician’s office or home. These shorter assessments will identify knowledge gaps, so physicians can tailor their continuing education in order to stay current in knowledge and practice. Successful performance on the shorter assessments will allow physicians to opt out of the longer 10-year exam. The program will be piloted for Internal Medicine and select subspecialties and, based on feedback, will be extended to additional subspecialties at a later date.
Physicians whose certifications expire prior to the new assessment option becoming available will need to pass the current exam in order to maintain certification but then will not need to take another assessment for 10 years.
ABIM’s full announcement can be viewed at abim.org/news/abim-announces-plans-to-offer-physicians-moc-assessment-options-in-january-2018.aspx.
Any questions regarding this development should be directed to the ABIM by visiting www.abim.org/contact.
CHEST Clinical Trials Registry announcement
A new clinical trial is now available in the CHEST Clinical Trials Registry (SENSCISTM, or Safety and Efficacy of Nintedanib in Systemic SClerosIS), a double-blind, randomized, placebo-controlled trial evaluating efficacy and safety of oral nintedanib treatment for at least 52 weeks in patients with Systemic Sclerosis-associated Interstitial Lung Disease (SSc-ILD). The CHEST Clinical Trials Registry is a free service that connects physicians to information about clinical trials in respiratory disease, conducted by participating pharmaceutical companies. To learn more about the registry and how to participate in this clinical trial, please visit www.chestnet.org/Guidelines-and-Resources/Clinical-Trials/Clinical-Trials-Registry.
A new clinical trial is now available in the CHEST Clinical Trials Registry (SENSCISTM, or Safety and Efficacy of Nintedanib in Systemic SClerosIS), a double-blind, randomized, placebo-controlled trial evaluating efficacy and safety of oral nintedanib treatment for at least 52 weeks in patients with Systemic Sclerosis-associated Interstitial Lung Disease (SSc-ILD). The CHEST Clinical Trials Registry is a free service that connects physicians to information about clinical trials in respiratory disease, conducted by participating pharmaceutical companies. To learn more about the registry and how to participate in this clinical trial, please visit www.chestnet.org/Guidelines-and-Resources/Clinical-Trials/Clinical-Trials-Registry.
A new clinical trial is now available in the CHEST Clinical Trials Registry (SENSCISTM, or Safety and Efficacy of Nintedanib in Systemic SClerosIS), a double-blind, randomized, placebo-controlled trial evaluating efficacy and safety of oral nintedanib treatment for at least 52 weeks in patients with Systemic Sclerosis-associated Interstitial Lung Disease (SSc-ILD). The CHEST Clinical Trials Registry is a free service that connects physicians to information about clinical trials in respiratory disease, conducted by participating pharmaceutical companies. To learn more about the registry and how to participate in this clinical trial, please visit www.chestnet.org/Guidelines-and-Resources/Clinical-Trials/Clinical-Trials-Registry.
This Month in CHEST: Editor’s Picks
COMMENTARY
Establishing Pulmonary and Critical Care Medicine in China: 2016 Report on Implementation and Government Recognition: Joint Statement of the Chinese Association of Chest Physicians and the American College of Chest Physicians.
By Dr. Renli Qiao et al, on behalf of the China-CHEST PCCM Program Steering Committee.
CONTEMPORARY REVIEWS IN SLEEP MEDICINE
Cancer and OSA: Current Evidence From Human Studies. By Dr. M. A. Martinez-Garcia et al.
ORIGINAL RESEARCH
Association Between Occupational Exposures and Sarcoidosis: An Analysis From Death Certificates in the United States, 1988-1999. By Dr. H. Liu et al.
Nonlinear Imputation of PaO2/FIO2 From SpO2/FIO2 Among Patients With Acute Respiratory Distress Syndrome. By Dr. S. M. Brown et al.
Blood Eosinophils and Outcomes in Severe Hospitalized Exacerbations of COPD. By Dr. M. Bafadhel et al.
A Randomized Controlled Trial of a Novel Sheath Cryoprobe for Bronchoscopic Lung Biopsy in a Porcine Model. By Dr. L. B. Yarmus et al.
COMMENTARY
Establishing Pulmonary and Critical Care Medicine in China: 2016 Report on Implementation and Government Recognition: Joint Statement of the Chinese Association of Chest Physicians and the American College of Chest Physicians.
By Dr. Renli Qiao et al, on behalf of the China-CHEST PCCM Program Steering Committee.
CONTEMPORARY REVIEWS IN SLEEP MEDICINE
Cancer and OSA: Current Evidence From Human Studies. By Dr. M. A. Martinez-Garcia et al.
ORIGINAL RESEARCH
Association Between Occupational Exposures and Sarcoidosis: An Analysis From Death Certificates in the United States, 1988-1999. By Dr. H. Liu et al.
Nonlinear Imputation of PaO2/FIO2 From SpO2/FIO2 Among Patients With Acute Respiratory Distress Syndrome. By Dr. S. M. Brown et al.
Blood Eosinophils and Outcomes in Severe Hospitalized Exacerbations of COPD. By Dr. M. Bafadhel et al.
A Randomized Controlled Trial of a Novel Sheath Cryoprobe for Bronchoscopic Lung Biopsy in a Porcine Model. By Dr. L. B. Yarmus et al.
COMMENTARY
Establishing Pulmonary and Critical Care Medicine in China: 2016 Report on Implementation and Government Recognition: Joint Statement of the Chinese Association of Chest Physicians and the American College of Chest Physicians.
By Dr. Renli Qiao et al, on behalf of the China-CHEST PCCM Program Steering Committee.
CONTEMPORARY REVIEWS IN SLEEP MEDICINE
Cancer and OSA: Current Evidence From Human Studies. By Dr. M. A. Martinez-Garcia et al.
ORIGINAL RESEARCH
Association Between Occupational Exposures and Sarcoidosis: An Analysis From Death Certificates in the United States, 1988-1999. By Dr. H. Liu et al.
Nonlinear Imputation of PaO2/FIO2 From SpO2/FIO2 Among Patients With Acute Respiratory Distress Syndrome. By Dr. S. M. Brown et al.
Blood Eosinophils and Outcomes in Severe Hospitalized Exacerbations of COPD. By Dr. M. Bafadhel et al.
A Randomized Controlled Trial of a Novel Sheath Cryoprobe for Bronchoscopic Lung Biopsy in a Porcine Model. By Dr. L. B. Yarmus et al.
Updated Patient Education guides available
The CHEST Foundation continues to look for new ways to expand our patient education offerings. With the collaboration of the CHEST Foundation’s Patient Education Work Group, the Allergy & Asthma NetWork, and CHEST’s NetWorks, we have completely revamped Living Well With COPD and Living Well With Asthma (previously titled Controlling Your Asthma). At less than 30 pages each, the guides are more user-friendly, featuring multiple diagrams to supplement instructions, take-away glossaries, easy-to-read infographics, and new FAQs.
The guides are available to order in packs of 25 in the CHEST store. Packs are $50 for members and $62.50 for nonmembers. The new guides are available for viewing online at chestnet.org/asthmainfo and chestnet.org/copdinfo.
The CHEST Foundation continues to look for new ways to expand our patient education offerings. With the collaboration of the CHEST Foundation’s Patient Education Work Group, the Allergy & Asthma NetWork, and CHEST’s NetWorks, we have completely revamped Living Well With COPD and Living Well With Asthma (previously titled Controlling Your Asthma). At less than 30 pages each, the guides are more user-friendly, featuring multiple diagrams to supplement instructions, take-away glossaries, easy-to-read infographics, and new FAQs.
The guides are available to order in packs of 25 in the CHEST store. Packs are $50 for members and $62.50 for nonmembers. The new guides are available for viewing online at chestnet.org/asthmainfo and chestnet.org/copdinfo.
The CHEST Foundation continues to look for new ways to expand our patient education offerings. With the collaboration of the CHEST Foundation’s Patient Education Work Group, the Allergy & Asthma NetWork, and CHEST’s NetWorks, we have completely revamped Living Well With COPD and Living Well With Asthma (previously titled Controlling Your Asthma). At less than 30 pages each, the guides are more user-friendly, featuring multiple diagrams to supplement instructions, take-away glossaries, easy-to-read infographics, and new FAQs.
The guides are available to order in packs of 25 in the CHEST store. Packs are $50 for members and $62.50 for nonmembers. The new guides are available for viewing online at chestnet.org/asthmainfo and chestnet.org/copdinfo.