User login
This Month in the Journal CHEST®
Giants In Chest Medicine
Sonia Buist, MBChB. By Dr. J.A. Krishnan.
Editorial
Is Big Tobacco Still Trying to Deceive the Public? This Is No Time to Rest on Our Laurels. By Drs. D. R. McCaffree and N. R. Desai.
Original Research
Defining the “Frequent Exacerbator” Phenotype in COPD: A Hypothesis-Free Approach. By Dr. O. Le Rouzic, et al.
Trial Duration and Risk Reduction in Combination Therapy Trials for Pulmonary Arterial Hypertension: A Systematic Review. By Dr. A. C. Lajoie, et al.
Tai Chi and Pulmonary Rehabilitation Compared for Treatment-Naive Patients With COPD: A Randomized Controlled Trial. By Dr. M. I. Polkey, et al.
Giants In Chest Medicine
Sonia Buist, MBChB. By Dr. J.A. Krishnan.
Editorial
Is Big Tobacco Still Trying to Deceive the Public? This Is No Time to Rest on Our Laurels. By Drs. D. R. McCaffree and N. R. Desai.
Original Research
Defining the “Frequent Exacerbator” Phenotype in COPD: A Hypothesis-Free Approach. By Dr. O. Le Rouzic, et al.
Trial Duration and Risk Reduction in Combination Therapy Trials for Pulmonary Arterial Hypertension: A Systematic Review. By Dr. A. C. Lajoie, et al.
Tai Chi and Pulmonary Rehabilitation Compared for Treatment-Naive Patients With COPD: A Randomized Controlled Trial. By Dr. M. I. Polkey, et al.
Giants In Chest Medicine
Sonia Buist, MBChB. By Dr. J.A. Krishnan.
Editorial
Is Big Tobacco Still Trying to Deceive the Public? This Is No Time to Rest on Our Laurels. By Drs. D. R. McCaffree and N. R. Desai.
Original Research
Defining the “Frequent Exacerbator” Phenotype in COPD: A Hypothesis-Free Approach. By Dr. O. Le Rouzic, et al.
Trial Duration and Risk Reduction in Combination Therapy Trials for Pulmonary Arterial Hypertension: A Systematic Review. By Dr. A. C. Lajoie, et al.
Tai Chi and Pulmonary Rehabilitation Compared for Treatment-Naive Patients With COPD: A Randomized Controlled Trial. By Dr. M. I. Polkey, et al.
Talc pleurodesis, ICS, cardiopulmonary exercise testing
Interventional Chest/Diagnostic Procedures
Review of The AMPLE Trial: is talc making a comeback?
A proposed advantage of indwelling pleural catheters (IPC) is their purported ability to reduce hospitalization time when compared with the more traditional talc pleurodesis procedure. The recently published AMPLE trial was a multicenter randomized trial comparing the impact of IPCs vs talc pleurodesis on hospitalization days in patients with malignant pleural effusions. One-hundred forty-six patients were randomized for pleurodesis to either IPC vs pleurodesis via talc slurry in nine centers in Australia, New Zealand, Singapore, and Hong Kong. Patients were followed for up to 12 months. Secondary outcomes included need for further pleural intervention, breathlessness, quality of life, and adverse events.
Patients randomized to IPC spent on average 2 days less in the hospital (10 vs 12 days), a difference that was statistically significant, though of questionable clinical relevance, and somewhat disappointing in light of a prior prospective study from the same group suggesting a benefit of 6 to 7 days (Fysh. Chest. 2012;142[2]:394. As in previous studies, additional pleural procedures were more common in the talc group, adverse events occurred more frequently with IPC, but breathlessness and quality of life were identical in both groups.
This study raises interesting questions. Clearly, IPCs have been favored over talc pleurodesis in the US in the last decade, primarily because of a perceived benefit in terms of hospitalization time. In the absence of clear advantage of IPC on time spent in the hospital, impact on breathlessness and quality of life, and considering the inconvenience of frequent drainage, co-pay incurred by patients, and increased adverse events with IPC, the pendulum may swing again toward talc pleurodesis.
Christine Argento, MD, FCCP
Fabien Maldonado, MD, FCCP
Steering Committee Members
Pediatric Chest Medicine
Early escalation of inhaled corticosteroids: does it help prevent asthma exacerbations?
Asthma is one of the most common chronic conditions in children. The importance of effective control of asthma to prevent exacerbations is well accepted. Inhaled corticosteroids (ICS) are a preferred component of treatment to improve asthma control in children with persistent asthma; however, exacerbations can still occur and result in significant morbidity. Most patients receive systemic corticosteroids during acute asthma exacerbations. The most recent Global Initiative for Asthma (GINA) guidelines recommend increasing ICS at the first signs of an asthma exacerbation in an effort to lessen the need for systemic corticosteroids (GINA. Global strategy for asthma management and prevention. 2017. http://www.ginasthma.org/).
In a recent issue of the New England Journal of Medicine, Jackson and colleagues at the National Heart, Lung, and Blood Institute AsthmaNet published the results of a randomized, double-blind 48-week trial, which included 254 children between ages 5 and 11 years with mild-moderate asthma. Their objectives were to compare exacerbation rates, time to first exacerbation, acute care visits, and bronchodilator use in children randomized to treatment with either high (5 x baseline ICS dose x 7 days) or low dose inhaled corticosteroids early in a drop to the “yellow zone” (Jackson, et al. N Engl J Med. 2018;378[10]:891).
Time to asthma exacerbations and exacerbations that required treatment with corticosteroids did not significantly differ between the low dose and high dose groups. Unexpectedly, the rate of exacerbations was higher with the high dose compared with the low dose group (0.48 vs 0.37). The children who were in the high dose group received 16% more ICS compared with the low dose group. Although not significant, there was a lower linear growth rate, ~0.23 cm per year seen in this high-dose group than in the low-dose group. Additionally, the use of bronchodilator, symptoms, and the rates of evaluation by a physician (ie, emergency department or urgent care visits) did not significantly differ between the two groups.
This study was specific to school-age children with mild-moderate persistent asthma treated with low dose ICS with a history of good adherence. Overall, this well-designed study helps address a question that many clinicians have regarding escalating ICS in the “yellow zone.” Escalating ICS did not reduce exacerbations at the cost of a lower linear growth rate. When it comes to escalating ICS for asthma exacerbation, more is not better.
In conclusion, in children with mild-to-moderate persistent asthma treated with daily inhaled glucocorticoids, quintupling the dose at the early signs of loss of asthma control did not reduce the rate of severe asthma exacerbations or improve other asthma outcomes and may be associated with diminished linear growth. (Funded by the National Heart, Lung, and Blood Institute; STICS ClinicalTrials.gov number, NCT02066129).
John Bishara, DO
Fellow-in-Training Member
Pulmonary Physiology, Function, and Rehabilitation
Understanding cardiopulmonary exercise testing
The cardiopulmonary exercise test (CPET) is an underutilized tool for evaluating patients with dyspnea of uncertain etiology. This is often due to the daunting task of trying to make sense of seemingly large amounts of interacting data, along with clinicians not having been taught a systematic approach for interpreting the results. Unlike other typical tests we order that point to a specific laboratory or anatomic radiographic abnormality, narrowing our differential to a few possibilities, one needs a different mindset when interpreting a CPET. This is a study to demonstrate the body’s normal or abnormal physiologic responses to increasing levels of physical stress. Because different conditions can give similar findings, the physiologic abnormalities must be interpreted in the context of the clinical presentation. If the results do not entirely fit the suspected diagnosis, they should be reported in a manner that may help guide the ordering physician down an alternate pathway. This CHEST NetWork has sought ways to reach out to members to promote a better understanding of the utilization of the basics of pulmonary physiology in the management of patients. We created an online two-part video demonstrating a basic systematic approach toward understanding the combinations of findings one often sees when performing a CPET. A comprehensive understanding cannot be shown in a 40-minute video series, but, hopefully, this will give a starting point to make this task easier and more enjoyable.
Zachary Morris, MD, FCCP
Steering Committee Member
Pulmonary Vascular Disease
BMPR2 mutation regulates singular millimetric fibrovascular lesions in bronchial circulation in PAH
Patients with PAH with BMPR2 mutation are younger with worse hemodynamics, ie, higher mean PAP with higher PVR and a lower cardiac index in comparison to the noncarriers. A systematic analysis of pulmonary imaging using CT angiography or magnetic resonance imaging in patients with PAH demonstrated increased bronchial arterial hypertrophy in BMPR2 mutation carriers compared with those without the mutation. Moreover, hemoptysis is more frequently encountered in patients with PAH with BMPR2 mutation and presumably related to bronchial artery remodeling and angiogenesis. French investigators described, in histopathology findings of explanted lungs of 44 patients with PAH (23 carriers of BMPR2 and 21 noncarriers), unusual singular millimetric fibrovascular lesions (SiMFi) in patients with BMPR2 mutations. The SiMFi is a structure of millimetric dimension with fibrovascular characteristics that are extremely rich in collagen and displayed more than one vascular channel. SiMFi did not show a classic glomeruloid pattern with predominant endothelial cell proliferation as seen in plexiform lesions but rather a large conglomerate of hypertrophic vessels. Performing an ink injection experiment in a freshly explanted lung highlighted a patent connection between bronchial/systemic vessels and pulmonary septal veins. SiMFis had an increased amount of bronchial microvessels and showed increased hypertrophy of larger bronchial arteries. SiMFi is directly related to hypertrophy and/or angiogenesis of vasa vasorum/bronchial arteries in the vicinity of the diseased artery. In patients with PAH with BMPR2 mutations, bronchial angiogenesis is more prevalent compared with patients with PAH lacking these mutations. This highlights the role of bronchial arteries in the spectrum of PAH.
Hector Cajigas, MD, FCCP
Sandeep Sahay, MD, FCCP
Steering Committee Members
References
1.Ghigna MR, et al. BMPR2 mutation status influences bronchial vascular changes in pulmonary arterial hypertension. Eur Respir J. 2016;48[6]:1668. Epub 2016 Nov 3.
2. Tio D, et al. Risk factors for hemoptysis in idiopathic and hereditary pulmonary arterial hypertension. PLoS One. 2013;8:e78132.
3. Elliott CG, et al. Relationship of BMPR2 mutations to vasoreactivity in pulmonary arterial hypertension. Circulation. 2006;113[21]:2509.
Thoracic Oncology
We have a lung cancer screening test but we could use it better
The American Lung Association recently demonstrated the majority of current and former smokers don’t know about lung cancer screening (LCS) with low-dose CT scanning.1 Researchers estimate less than 5% of eligible persons received LCS.2 Awareness campaigns targeting patients and health care providers at the local level can improve LCS uptake.3,4 While any new clinical practice has an expected implementation delay, LCS has another implementation barrier: complex eligibility criteria (age 55 – 80 years PLUS 30+ pack-year smoking history PLUS quit time less than 15 years). Electronic health record (EHR) tools might accelerate the adoption curve to identify eligible persons.5 Moreover, assessing and recording a qualitative smoking history is challenging, at best. One center showed 96.2% discordance between EHR smoking history and that obtained during shared decision-making visit for LCS.6 Mostly, the EHR underreported quantitative pack-year history; meaning LCS-eligible patients might fail to be identified by EHR review alone. Another small pilot showed that some patients age 55 – 79 years will update their EHR smoking history using patient portal, but this will not be effective for all patients.7 For current smokers, age alone may be an effective identification strategy, given the average start time for most smokers.8
Even though current LCS guidelines leave out some individuals at high risk for lung cancer, we must continue efforts to offer this potentially life-saving service to patients now eligible. Using EHR tools may help proactively identify those who are eligible for lung cancer screening.
A bbie Begnaud, MD
NetWork Member
References
1. New Study from American Lung Association’s LUNG FORCE Reveals Low Awareness of Lifesaving Lung Cancer Screening Among Those at Greatest Risk. (2017). http://www.lung.org/about-us/media/press-releases/new-study-lung-cancer-screening.html. Accessed April 19, 2018.
2. Soneji S, et al. Underuse of Chest Radiography Versus Computed Tomography for Lung Cancer Screening. Am J Public Health. 2017;107(8):1248.
3. Cardarelli R, et al. Terminate lung cancer (TLC) study-A mixed-methods population approach to increase lung cancer screening awareness and low-dose computed tomography in Eastern Kentucky. Cancer Epidemiol. 2017;46:1.
4. Jessup, DL, et al. Implementation of digital awareness strategies to engage patients and providers in a lung cancer screening program: retrospective study. J Med Internet Res. 2018;20(2):e52.
5. Comparison of the Electronic Medical Record versus a Shared Decision Making Conversation. Ann Am Thorac Soc. 2018. In press.
6. Modin HE, et al. Pack-year cigarette smoking history for determination of lung cancer screening eligibility. Ann Am Thorac Soc. 2017 Aug;14(8):1320-1325.
7. Begnaud AL, et al. Randomized electronic promotion of lung cancer screening: a pilot. JCO Clinical Cancer Informatics(1), 1-6. doi:10.1200/cci.17.00033
8. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. (2014). Atlanta, GA.
Interventional Chest/Diagnostic Procedures
Review of The AMPLE Trial: is talc making a comeback?
A proposed advantage of indwelling pleural catheters (IPC) is their purported ability to reduce hospitalization time when compared with the more traditional talc pleurodesis procedure. The recently published AMPLE trial was a multicenter randomized trial comparing the impact of IPCs vs talc pleurodesis on hospitalization days in patients with malignant pleural effusions. One-hundred forty-six patients were randomized for pleurodesis to either IPC vs pleurodesis via talc slurry in nine centers in Australia, New Zealand, Singapore, and Hong Kong. Patients were followed for up to 12 months. Secondary outcomes included need for further pleural intervention, breathlessness, quality of life, and adverse events.
Patients randomized to IPC spent on average 2 days less in the hospital (10 vs 12 days), a difference that was statistically significant, though of questionable clinical relevance, and somewhat disappointing in light of a prior prospective study from the same group suggesting a benefit of 6 to 7 days (Fysh. Chest. 2012;142[2]:394. As in previous studies, additional pleural procedures were more common in the talc group, adverse events occurred more frequently with IPC, but breathlessness and quality of life were identical in both groups.
This study raises interesting questions. Clearly, IPCs have been favored over talc pleurodesis in the US in the last decade, primarily because of a perceived benefit in terms of hospitalization time. In the absence of clear advantage of IPC on time spent in the hospital, impact on breathlessness and quality of life, and considering the inconvenience of frequent drainage, co-pay incurred by patients, and increased adverse events with IPC, the pendulum may swing again toward talc pleurodesis.
Christine Argento, MD, FCCP
Fabien Maldonado, MD, FCCP
Steering Committee Members
Pediatric Chest Medicine
Early escalation of inhaled corticosteroids: does it help prevent asthma exacerbations?
Asthma is one of the most common chronic conditions in children. The importance of effective control of asthma to prevent exacerbations is well accepted. Inhaled corticosteroids (ICS) are a preferred component of treatment to improve asthma control in children with persistent asthma; however, exacerbations can still occur and result in significant morbidity. Most patients receive systemic corticosteroids during acute asthma exacerbations. The most recent Global Initiative for Asthma (GINA) guidelines recommend increasing ICS at the first signs of an asthma exacerbation in an effort to lessen the need for systemic corticosteroids (GINA. Global strategy for asthma management and prevention. 2017. http://www.ginasthma.org/).
In a recent issue of the New England Journal of Medicine, Jackson and colleagues at the National Heart, Lung, and Blood Institute AsthmaNet published the results of a randomized, double-blind 48-week trial, which included 254 children between ages 5 and 11 years with mild-moderate asthma. Their objectives were to compare exacerbation rates, time to first exacerbation, acute care visits, and bronchodilator use in children randomized to treatment with either high (5 x baseline ICS dose x 7 days) or low dose inhaled corticosteroids early in a drop to the “yellow zone” (Jackson, et al. N Engl J Med. 2018;378[10]:891).
Time to asthma exacerbations and exacerbations that required treatment with corticosteroids did not significantly differ between the low dose and high dose groups. Unexpectedly, the rate of exacerbations was higher with the high dose compared with the low dose group (0.48 vs 0.37). The children who were in the high dose group received 16% more ICS compared with the low dose group. Although not significant, there was a lower linear growth rate, ~0.23 cm per year seen in this high-dose group than in the low-dose group. Additionally, the use of bronchodilator, symptoms, and the rates of evaluation by a physician (ie, emergency department or urgent care visits) did not significantly differ between the two groups.
This study was specific to school-age children with mild-moderate persistent asthma treated with low dose ICS with a history of good adherence. Overall, this well-designed study helps address a question that many clinicians have regarding escalating ICS in the “yellow zone.” Escalating ICS did not reduce exacerbations at the cost of a lower linear growth rate. When it comes to escalating ICS for asthma exacerbation, more is not better.
In conclusion, in children with mild-to-moderate persistent asthma treated with daily inhaled glucocorticoids, quintupling the dose at the early signs of loss of asthma control did not reduce the rate of severe asthma exacerbations or improve other asthma outcomes and may be associated with diminished linear growth. (Funded by the National Heart, Lung, and Blood Institute; STICS ClinicalTrials.gov number, NCT02066129).
John Bishara, DO
Fellow-in-Training Member
Pulmonary Physiology, Function, and Rehabilitation
Understanding cardiopulmonary exercise testing
The cardiopulmonary exercise test (CPET) is an underutilized tool for evaluating patients with dyspnea of uncertain etiology. This is often due to the daunting task of trying to make sense of seemingly large amounts of interacting data, along with clinicians not having been taught a systematic approach for interpreting the results. Unlike other typical tests we order that point to a specific laboratory or anatomic radiographic abnormality, narrowing our differential to a few possibilities, one needs a different mindset when interpreting a CPET. This is a study to demonstrate the body’s normal or abnormal physiologic responses to increasing levels of physical stress. Because different conditions can give similar findings, the physiologic abnormalities must be interpreted in the context of the clinical presentation. If the results do not entirely fit the suspected diagnosis, they should be reported in a manner that may help guide the ordering physician down an alternate pathway. This CHEST NetWork has sought ways to reach out to members to promote a better understanding of the utilization of the basics of pulmonary physiology in the management of patients. We created an online two-part video demonstrating a basic systematic approach toward understanding the combinations of findings one often sees when performing a CPET. A comprehensive understanding cannot be shown in a 40-minute video series, but, hopefully, this will give a starting point to make this task easier and more enjoyable.
Zachary Morris, MD, FCCP
Steering Committee Member
Pulmonary Vascular Disease
BMPR2 mutation regulates singular millimetric fibrovascular lesions in bronchial circulation in PAH
Patients with PAH with BMPR2 mutation are younger with worse hemodynamics, ie, higher mean PAP with higher PVR and a lower cardiac index in comparison to the noncarriers. A systematic analysis of pulmonary imaging using CT angiography or magnetic resonance imaging in patients with PAH demonstrated increased bronchial arterial hypertrophy in BMPR2 mutation carriers compared with those without the mutation. Moreover, hemoptysis is more frequently encountered in patients with PAH with BMPR2 mutation and presumably related to bronchial artery remodeling and angiogenesis. French investigators described, in histopathology findings of explanted lungs of 44 patients with PAH (23 carriers of BMPR2 and 21 noncarriers), unusual singular millimetric fibrovascular lesions (SiMFi) in patients with BMPR2 mutations. The SiMFi is a structure of millimetric dimension with fibrovascular characteristics that are extremely rich in collagen and displayed more than one vascular channel. SiMFi did not show a classic glomeruloid pattern with predominant endothelial cell proliferation as seen in plexiform lesions but rather a large conglomerate of hypertrophic vessels. Performing an ink injection experiment in a freshly explanted lung highlighted a patent connection between bronchial/systemic vessels and pulmonary septal veins. SiMFis had an increased amount of bronchial microvessels and showed increased hypertrophy of larger bronchial arteries. SiMFi is directly related to hypertrophy and/or angiogenesis of vasa vasorum/bronchial arteries in the vicinity of the diseased artery. In patients with PAH with BMPR2 mutations, bronchial angiogenesis is more prevalent compared with patients with PAH lacking these mutations. This highlights the role of bronchial arteries in the spectrum of PAH.
Hector Cajigas, MD, FCCP
Sandeep Sahay, MD, FCCP
Steering Committee Members
References
1.Ghigna MR, et al. BMPR2 mutation status influences bronchial vascular changes in pulmonary arterial hypertension. Eur Respir J. 2016;48[6]:1668. Epub 2016 Nov 3.
2. Tio D, et al. Risk factors for hemoptysis in idiopathic and hereditary pulmonary arterial hypertension. PLoS One. 2013;8:e78132.
3. Elliott CG, et al. Relationship of BMPR2 mutations to vasoreactivity in pulmonary arterial hypertension. Circulation. 2006;113[21]:2509.
Thoracic Oncology
We have a lung cancer screening test but we could use it better
The American Lung Association recently demonstrated the majority of current and former smokers don’t know about lung cancer screening (LCS) with low-dose CT scanning.1 Researchers estimate less than 5% of eligible persons received LCS.2 Awareness campaigns targeting patients and health care providers at the local level can improve LCS uptake.3,4 While any new clinical practice has an expected implementation delay, LCS has another implementation barrier: complex eligibility criteria (age 55 – 80 years PLUS 30+ pack-year smoking history PLUS quit time less than 15 years). Electronic health record (EHR) tools might accelerate the adoption curve to identify eligible persons.5 Moreover, assessing and recording a qualitative smoking history is challenging, at best. One center showed 96.2% discordance between EHR smoking history and that obtained during shared decision-making visit for LCS.6 Mostly, the EHR underreported quantitative pack-year history; meaning LCS-eligible patients might fail to be identified by EHR review alone. Another small pilot showed that some patients age 55 – 79 years will update their EHR smoking history using patient portal, but this will not be effective for all patients.7 For current smokers, age alone may be an effective identification strategy, given the average start time for most smokers.8
Even though current LCS guidelines leave out some individuals at high risk for lung cancer, we must continue efforts to offer this potentially life-saving service to patients now eligible. Using EHR tools may help proactively identify those who are eligible for lung cancer screening.
A bbie Begnaud, MD
NetWork Member
References
1. New Study from American Lung Association’s LUNG FORCE Reveals Low Awareness of Lifesaving Lung Cancer Screening Among Those at Greatest Risk. (2017). http://www.lung.org/about-us/media/press-releases/new-study-lung-cancer-screening.html. Accessed April 19, 2018.
2. Soneji S, et al. Underuse of Chest Radiography Versus Computed Tomography for Lung Cancer Screening. Am J Public Health. 2017;107(8):1248.
3. Cardarelli R, et al. Terminate lung cancer (TLC) study-A mixed-methods population approach to increase lung cancer screening awareness and low-dose computed tomography in Eastern Kentucky. Cancer Epidemiol. 2017;46:1.
4. Jessup, DL, et al. Implementation of digital awareness strategies to engage patients and providers in a lung cancer screening program: retrospective study. J Med Internet Res. 2018;20(2):e52.
5. Comparison of the Electronic Medical Record versus a Shared Decision Making Conversation. Ann Am Thorac Soc. 2018. In press.
6. Modin HE, et al. Pack-year cigarette smoking history for determination of lung cancer screening eligibility. Ann Am Thorac Soc. 2017 Aug;14(8):1320-1325.
7. Begnaud AL, et al. Randomized electronic promotion of lung cancer screening: a pilot. JCO Clinical Cancer Informatics(1), 1-6. doi:10.1200/cci.17.00033
8. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. (2014). Atlanta, GA.
Interventional Chest/Diagnostic Procedures
Review of The AMPLE Trial: is talc making a comeback?
A proposed advantage of indwelling pleural catheters (IPC) is their purported ability to reduce hospitalization time when compared with the more traditional talc pleurodesis procedure. The recently published AMPLE trial was a multicenter randomized trial comparing the impact of IPCs vs talc pleurodesis on hospitalization days in patients with malignant pleural effusions. One-hundred forty-six patients were randomized for pleurodesis to either IPC vs pleurodesis via talc slurry in nine centers in Australia, New Zealand, Singapore, and Hong Kong. Patients were followed for up to 12 months. Secondary outcomes included need for further pleural intervention, breathlessness, quality of life, and adverse events.
Patients randomized to IPC spent on average 2 days less in the hospital (10 vs 12 days), a difference that was statistically significant, though of questionable clinical relevance, and somewhat disappointing in light of a prior prospective study from the same group suggesting a benefit of 6 to 7 days (Fysh. Chest. 2012;142[2]:394. As in previous studies, additional pleural procedures were more common in the talc group, adverse events occurred more frequently with IPC, but breathlessness and quality of life were identical in both groups.
This study raises interesting questions. Clearly, IPCs have been favored over talc pleurodesis in the US in the last decade, primarily because of a perceived benefit in terms of hospitalization time. In the absence of clear advantage of IPC on time spent in the hospital, impact on breathlessness and quality of life, and considering the inconvenience of frequent drainage, co-pay incurred by patients, and increased adverse events with IPC, the pendulum may swing again toward talc pleurodesis.
Christine Argento, MD, FCCP
Fabien Maldonado, MD, FCCP
Steering Committee Members
Pediatric Chest Medicine
Early escalation of inhaled corticosteroids: does it help prevent asthma exacerbations?
Asthma is one of the most common chronic conditions in children. The importance of effective control of asthma to prevent exacerbations is well accepted. Inhaled corticosteroids (ICS) are a preferred component of treatment to improve asthma control in children with persistent asthma; however, exacerbations can still occur and result in significant morbidity. Most patients receive systemic corticosteroids during acute asthma exacerbations. The most recent Global Initiative for Asthma (GINA) guidelines recommend increasing ICS at the first signs of an asthma exacerbation in an effort to lessen the need for systemic corticosteroids (GINA. Global strategy for asthma management and prevention. 2017. http://www.ginasthma.org/).
In a recent issue of the New England Journal of Medicine, Jackson and colleagues at the National Heart, Lung, and Blood Institute AsthmaNet published the results of a randomized, double-blind 48-week trial, which included 254 children between ages 5 and 11 years with mild-moderate asthma. Their objectives were to compare exacerbation rates, time to first exacerbation, acute care visits, and bronchodilator use in children randomized to treatment with either high (5 x baseline ICS dose x 7 days) or low dose inhaled corticosteroids early in a drop to the “yellow zone” (Jackson, et al. N Engl J Med. 2018;378[10]:891).
Time to asthma exacerbations and exacerbations that required treatment with corticosteroids did not significantly differ between the low dose and high dose groups. Unexpectedly, the rate of exacerbations was higher with the high dose compared with the low dose group (0.48 vs 0.37). The children who were in the high dose group received 16% more ICS compared with the low dose group. Although not significant, there was a lower linear growth rate, ~0.23 cm per year seen in this high-dose group than in the low-dose group. Additionally, the use of bronchodilator, symptoms, and the rates of evaluation by a physician (ie, emergency department or urgent care visits) did not significantly differ between the two groups.
This study was specific to school-age children with mild-moderate persistent asthma treated with low dose ICS with a history of good adherence. Overall, this well-designed study helps address a question that many clinicians have regarding escalating ICS in the “yellow zone.” Escalating ICS did not reduce exacerbations at the cost of a lower linear growth rate. When it comes to escalating ICS for asthma exacerbation, more is not better.
In conclusion, in children with mild-to-moderate persistent asthma treated with daily inhaled glucocorticoids, quintupling the dose at the early signs of loss of asthma control did not reduce the rate of severe asthma exacerbations or improve other asthma outcomes and may be associated with diminished linear growth. (Funded by the National Heart, Lung, and Blood Institute; STICS ClinicalTrials.gov number, NCT02066129).
John Bishara, DO
Fellow-in-Training Member
Pulmonary Physiology, Function, and Rehabilitation
Understanding cardiopulmonary exercise testing
The cardiopulmonary exercise test (CPET) is an underutilized tool for evaluating patients with dyspnea of uncertain etiology. This is often due to the daunting task of trying to make sense of seemingly large amounts of interacting data, along with clinicians not having been taught a systematic approach for interpreting the results. Unlike other typical tests we order that point to a specific laboratory or anatomic radiographic abnormality, narrowing our differential to a few possibilities, one needs a different mindset when interpreting a CPET. This is a study to demonstrate the body’s normal or abnormal physiologic responses to increasing levels of physical stress. Because different conditions can give similar findings, the physiologic abnormalities must be interpreted in the context of the clinical presentation. If the results do not entirely fit the suspected diagnosis, they should be reported in a manner that may help guide the ordering physician down an alternate pathway. This CHEST NetWork has sought ways to reach out to members to promote a better understanding of the utilization of the basics of pulmonary physiology in the management of patients. We created an online two-part video demonstrating a basic systematic approach toward understanding the combinations of findings one often sees when performing a CPET. A comprehensive understanding cannot be shown in a 40-minute video series, but, hopefully, this will give a starting point to make this task easier and more enjoyable.
Zachary Morris, MD, FCCP
Steering Committee Member
Pulmonary Vascular Disease
BMPR2 mutation regulates singular millimetric fibrovascular lesions in bronchial circulation in PAH
Patients with PAH with BMPR2 mutation are younger with worse hemodynamics, ie, higher mean PAP with higher PVR and a lower cardiac index in comparison to the noncarriers. A systematic analysis of pulmonary imaging using CT angiography or magnetic resonance imaging in patients with PAH demonstrated increased bronchial arterial hypertrophy in BMPR2 mutation carriers compared with those without the mutation. Moreover, hemoptysis is more frequently encountered in patients with PAH with BMPR2 mutation and presumably related to bronchial artery remodeling and angiogenesis. French investigators described, in histopathology findings of explanted lungs of 44 patients with PAH (23 carriers of BMPR2 and 21 noncarriers), unusual singular millimetric fibrovascular lesions (SiMFi) in patients with BMPR2 mutations. The SiMFi is a structure of millimetric dimension with fibrovascular characteristics that are extremely rich in collagen and displayed more than one vascular channel. SiMFi did not show a classic glomeruloid pattern with predominant endothelial cell proliferation as seen in plexiform lesions but rather a large conglomerate of hypertrophic vessels. Performing an ink injection experiment in a freshly explanted lung highlighted a patent connection between bronchial/systemic vessels and pulmonary septal veins. SiMFis had an increased amount of bronchial microvessels and showed increased hypertrophy of larger bronchial arteries. SiMFi is directly related to hypertrophy and/or angiogenesis of vasa vasorum/bronchial arteries in the vicinity of the diseased artery. In patients with PAH with BMPR2 mutations, bronchial angiogenesis is more prevalent compared with patients with PAH lacking these mutations. This highlights the role of bronchial arteries in the spectrum of PAH.
Hector Cajigas, MD, FCCP
Sandeep Sahay, MD, FCCP
Steering Committee Members
References
1.Ghigna MR, et al. BMPR2 mutation status influences bronchial vascular changes in pulmonary arterial hypertension. Eur Respir J. 2016;48[6]:1668. Epub 2016 Nov 3.
2. Tio D, et al. Risk factors for hemoptysis in idiopathic and hereditary pulmonary arterial hypertension. PLoS One. 2013;8:e78132.
3. Elliott CG, et al. Relationship of BMPR2 mutations to vasoreactivity in pulmonary arterial hypertension. Circulation. 2006;113[21]:2509.
Thoracic Oncology
We have a lung cancer screening test but we could use it better
The American Lung Association recently demonstrated the majority of current and former smokers don’t know about lung cancer screening (LCS) with low-dose CT scanning.1 Researchers estimate less than 5% of eligible persons received LCS.2 Awareness campaigns targeting patients and health care providers at the local level can improve LCS uptake.3,4 While any new clinical practice has an expected implementation delay, LCS has another implementation barrier: complex eligibility criteria (age 55 – 80 years PLUS 30+ pack-year smoking history PLUS quit time less than 15 years). Electronic health record (EHR) tools might accelerate the adoption curve to identify eligible persons.5 Moreover, assessing and recording a qualitative smoking history is challenging, at best. One center showed 96.2% discordance between EHR smoking history and that obtained during shared decision-making visit for LCS.6 Mostly, the EHR underreported quantitative pack-year history; meaning LCS-eligible patients might fail to be identified by EHR review alone. Another small pilot showed that some patients age 55 – 79 years will update their EHR smoking history using patient portal, but this will not be effective for all patients.7 For current smokers, age alone may be an effective identification strategy, given the average start time for most smokers.8
Even though current LCS guidelines leave out some individuals at high risk for lung cancer, we must continue efforts to offer this potentially life-saving service to patients now eligible. Using EHR tools may help proactively identify those who are eligible for lung cancer screening.
A bbie Begnaud, MD
NetWork Member
References
1. New Study from American Lung Association’s LUNG FORCE Reveals Low Awareness of Lifesaving Lung Cancer Screening Among Those at Greatest Risk. (2017). http://www.lung.org/about-us/media/press-releases/new-study-lung-cancer-screening.html. Accessed April 19, 2018.
2. Soneji S, et al. Underuse of Chest Radiography Versus Computed Tomography for Lung Cancer Screening. Am J Public Health. 2017;107(8):1248.
3. Cardarelli R, et al. Terminate lung cancer (TLC) study-A mixed-methods population approach to increase lung cancer screening awareness and low-dose computed tomography in Eastern Kentucky. Cancer Epidemiol. 2017;46:1.
4. Jessup, DL, et al. Implementation of digital awareness strategies to engage patients and providers in a lung cancer screening program: retrospective study. J Med Internet Res. 2018;20(2):e52.
5. Comparison of the Electronic Medical Record versus a Shared Decision Making Conversation. Ann Am Thorac Soc. 2018. In press.
6. Modin HE, et al. Pack-year cigarette smoking history for determination of lung cancer screening eligibility. Ann Am Thorac Soc. 2017 Aug;14(8):1320-1325.
7. Begnaud AL, et al. Randomized electronic promotion of lung cancer screening: a pilot. JCO Clinical Cancer Informatics(1), 1-6. doi:10.1200/cci.17.00033
8. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. (2014). Atlanta, GA.
Expanding CHEST’s ‘Women in Pulmonary’ Program
The gender gap exists for women in pulmonary medicine. According to the Medscape Pulmonologist Compensation Report 2017, women pulmonologists earned 23% less than their male counterparts even though:
- 2% of women pulmonologists work part time vs 8% of men;
- more women (66%) than men (48%) reported seeking promotion. (Grisham, 2017)
If we take a look at a recent report done by Doximity that analyzed responses on more than 65,000 licensed US doctors across the country, the report reveals that the gap between female and male physicians across the nation, women on average make about $91,000 less annually (Doximity, 2018).
Despite ever-growing enrollment rates for women in medical schools, female physicians are often underrepresented in academic and research settings. According to a study published in the Journal of National Medical Association, “between 80 and 90 percent of leadership roles in medicine, like medical school deans, are filled by men.” (Morton & Sonnad, 2007)
These astounding gaps do not stop at the clinician’s door. This gender inequality is evident in the women who are receiving medical treatment, as well. There are two major issues that exist for women seeking treatment:
1. Not being taken as seriously as male patients:
- Women are more likely to be prescribed sedatives for their pain, and men are more likely to be prescribed pain medication. (L. Calderone, 1990)
- Women are more likely to be treated less aggressively in their initial encounters with the health-care system until they prove that they are as sick as male patients with similar symptoms. (Hoffmann & Tarzian, 2001)
- Nationwide, men wait an average of 49 minutes before receiving an analgesic for acute abdominal pain. Women wait an average of 65 minutes for the same thing. (Chen, et al., 2008)
- Multiple studies have shown that female patients’ symptoms are less likely to be taken seriously by doctors, and women are more likely to be misdiagnosed, have their symptoms go unrecognized, or be told what they’re experiencing is psychosomatic. (Hoffmann & Tarzian, 2001) (Carnlöf, Iwarzon, Jensen-Urstad, Gadler, & Insulander, 2017)
2. Being diagnosed and treated the same as male patients
- Up until 1993 when the National Institutes of Health Revitalization Act mandated that all women and minorities be included in clinical trials funded by the NIH, the guidelines and diagnosis for treatment have historically been based off the archetypal patient: a 154-pound white male. Because of this, women are often misdiagnosed or receive treatments that are ineffective or potentially harmful to their health. Even still, researchers frequently do not enroll an adequate number of women or fail to analyze or report data separately by sex. (MHC Center, 2014)
- Women and men metabolize drugs differently, yet dosages are rarely broken down by sex. Women also experience different side effects and derive different benefits from the same treatments. (Soldin & Mattison, 2009)
- Female patients have a 1.5 to 1.7 times higher chance of having an adverse drug reaction. (Rademaker, 2001)
- There are many diseases and conditions that are alarmingly more prevalent among women. Nonsmoking women are three times more likely to get lung cancer than nonsmoking men, according to a comprehensive 2014 report by Brigham and Women’s Hospital in Boston, called “Women’s Health Can’t Wait.” (MHC Center, 2014)
“While the number of women participating in lung cancer clinical trials has risen, women—particularly those from racial and ethnic minorities—are still less likely to enroll in these trials than men. Even when studies include women, researchers often fail to analyze data by sex or include hormone status or other gender-specific factors, making it difficult to uncover differences in incidence, prevalence, and survivability between men and women and to replicate the studies.” (MHC Center, 2014)In the pulmonary space, there is growing evidence that a number of pulmonary diseases affect women differently and with a greater degree of severity than men. Respiratory conditions that impact women nearly exclusively include pulmonary hypertension, catamenial diseases, and pregnancy-associated asthma exacerbation. (Pinkerton, et al., 2015) According to the CDC, cancer is the number one cause of death for women ages 35-64, and the number one cancer killer in women is lung cancer. Women have been taught to care and take notice of the symptoms of breast cancer, HPV, ovarian cancer, and other “women’s diseases,” and, yet, more women die every day from lung cancer than from breast, ovarian, and uterine cancers combined.
Why CHEST?
Now, why does this matter to us at CHEST? What can we do about it? How do we begin to tackle such a large issue that permeates nearly every facet of society?
CHEST is in a unique position to not only address the professional development needs of our female membership, but with the help and leadership of the CHEST Foundation and a new partnership with HealthyWomen, we are poised to address the gaps in education for our clinicians, patients, and the public.
To address these needs, the Women in Pulmonary program was created. Women in Pulmonary started as a yearly luncheon and has expanded into a yearlong program that will work to fill these gaps by not only elevating the wants and needs of women in pulmonary medicine, but also by bringing awareness to clinicians, patients, and the public on diseases that are not typically considered “women’s issues.”
CHEST and HealthyWomen are working to provide education, in the form of free webinars, multimedia resources, and live events to achieve the following outcomes:
Women in Pulmonary Medicine: CHEST and HealthyWomen aim to create the tools and educational opportunities that will empower our female clinicians to elevate their voices and become advocates for their career advancement, as well as improved diagnosis and treatment of women with pulmonary diseases.
Patients, Caregivers, and the Public: With this initiative, CHEST and HealthyWomen strive to empower women with the knowledge they need to become champions of their lung health. We will provide them with talking points, questions and awareness of symptoms of pulmonary conditions and diseases, such as: lung cancer, ILD/IPF, COPD, pulmonary hypertension, and asthma so that they are better able to go to their doctor appointments ready to advocate for the care they need.
Clinicians: CHEST and HealthyWomen will aim to equip all clinicians, not just women, with exposure and education that address gender differences in treatment and diagnosis of diseases like lung cancer, asthma, COPD, PH, and ILD/IPF.
Women in Pulmonary aims to provide essential education to every clinician treating women, promote awareness among patients and the public on key information to improve conversations with their health-care providers, and create opportunities for women in chest medicine to advance their careers through professional development, engagement, networking, and mentorship connections. This program will be one step in the direction of changing how women are viewed in medicine and how diseases are perceived across genders.
Bibliography
Calderone K. The influence of gender on the frequency of pain and sedative medication administered to postoperative patients. Sex Roles. 1990;23(11-12): 713-725.
Carnlöf C, et al. Women with PSVY are often misdiagnosed, referred later than men, and have more symptoms after ablation. Scand Cardiovasc J. 2017; 51(6): 299-307.
Chen EH, et al. Gender disparity in analgesic treatment of emergency departmetn patietns with acute abdominal pain. Acad Emerg Med. 2008;15(5):414-418.
Doximity. 2018 Physician Compensation Report. Doximity.
Grisham S. Medscape Pulmonologist Compensation Report 2017. https://www.medscape.com/slideshow/compensation-2017-pulmonary-medicine-6008586. Accessed Jan 16, 2018.
Hoffmann DE, Tarzian AJ. The girl who cried pain: a bias against women in the treatment of pain. J Law Med Ethics. 2001;29(1):13-27.
MHC Center. Sex-Specific Medical Research: Why Women’s Health Can’t Wait. Brigham and Women’s Hospital, Mary Horrigan Connors Center for Women’s Health & Gender Biology. Brigham and Women’s Hospital;2014.
Morton MJ, Sonnad SS. Women on professional society and journal editorial boards. J National Med Assoc. 2007;99(7):764-771.
Pinkerton K, et al. Women and lung disease. sex differences and global health disparities. Am J Respir Crit Care Med. 2015;192(1):11-16.
Rademaker M. (2001). Do women have more adverse drug reactions? Am J Clin Dermatol. 2001;2(6): 349-351.
Soldin O, Mattison M. Sex differences in pharmacokinetics and pharmacodynamics. Clin Pharmacokinetics. 2009;48(3):143-157.
The gender gap exists for women in pulmonary medicine. According to the Medscape Pulmonologist Compensation Report 2017, women pulmonologists earned 23% less than their male counterparts even though:
- 2% of women pulmonologists work part time vs 8% of men;
- more women (66%) than men (48%) reported seeking promotion. (Grisham, 2017)
If we take a look at a recent report done by Doximity that analyzed responses on more than 65,000 licensed US doctors across the country, the report reveals that the gap between female and male physicians across the nation, women on average make about $91,000 less annually (Doximity, 2018).
Despite ever-growing enrollment rates for women in medical schools, female physicians are often underrepresented in academic and research settings. According to a study published in the Journal of National Medical Association, “between 80 and 90 percent of leadership roles in medicine, like medical school deans, are filled by men.” (Morton & Sonnad, 2007)
These astounding gaps do not stop at the clinician’s door. This gender inequality is evident in the women who are receiving medical treatment, as well. There are two major issues that exist for women seeking treatment:
1. Not being taken as seriously as male patients:
- Women are more likely to be prescribed sedatives for their pain, and men are more likely to be prescribed pain medication. (L. Calderone, 1990)
- Women are more likely to be treated less aggressively in their initial encounters with the health-care system until they prove that they are as sick as male patients with similar symptoms. (Hoffmann & Tarzian, 2001)
- Nationwide, men wait an average of 49 minutes before receiving an analgesic for acute abdominal pain. Women wait an average of 65 minutes for the same thing. (Chen, et al., 2008)
- Multiple studies have shown that female patients’ symptoms are less likely to be taken seriously by doctors, and women are more likely to be misdiagnosed, have their symptoms go unrecognized, or be told what they’re experiencing is psychosomatic. (Hoffmann & Tarzian, 2001) (Carnlöf, Iwarzon, Jensen-Urstad, Gadler, & Insulander, 2017)
2. Being diagnosed and treated the same as male patients
- Up until 1993 when the National Institutes of Health Revitalization Act mandated that all women and minorities be included in clinical trials funded by the NIH, the guidelines and diagnosis for treatment have historically been based off the archetypal patient: a 154-pound white male. Because of this, women are often misdiagnosed or receive treatments that are ineffective or potentially harmful to their health. Even still, researchers frequently do not enroll an adequate number of women or fail to analyze or report data separately by sex. (MHC Center, 2014)
- Women and men metabolize drugs differently, yet dosages are rarely broken down by sex. Women also experience different side effects and derive different benefits from the same treatments. (Soldin & Mattison, 2009)
- Female patients have a 1.5 to 1.7 times higher chance of having an adverse drug reaction. (Rademaker, 2001)
- There are many diseases and conditions that are alarmingly more prevalent among women. Nonsmoking women are three times more likely to get lung cancer than nonsmoking men, according to a comprehensive 2014 report by Brigham and Women’s Hospital in Boston, called “Women’s Health Can’t Wait.” (MHC Center, 2014)
“While the number of women participating in lung cancer clinical trials has risen, women—particularly those from racial and ethnic minorities—are still less likely to enroll in these trials than men. Even when studies include women, researchers often fail to analyze data by sex or include hormone status or other gender-specific factors, making it difficult to uncover differences in incidence, prevalence, and survivability between men and women and to replicate the studies.” (MHC Center, 2014)In the pulmonary space, there is growing evidence that a number of pulmonary diseases affect women differently and with a greater degree of severity than men. Respiratory conditions that impact women nearly exclusively include pulmonary hypertension, catamenial diseases, and pregnancy-associated asthma exacerbation. (Pinkerton, et al., 2015) According to the CDC, cancer is the number one cause of death for women ages 35-64, and the number one cancer killer in women is lung cancer. Women have been taught to care and take notice of the symptoms of breast cancer, HPV, ovarian cancer, and other “women’s diseases,” and, yet, more women die every day from lung cancer than from breast, ovarian, and uterine cancers combined.
Why CHEST?
Now, why does this matter to us at CHEST? What can we do about it? How do we begin to tackle such a large issue that permeates nearly every facet of society?
CHEST is in a unique position to not only address the professional development needs of our female membership, but with the help and leadership of the CHEST Foundation and a new partnership with HealthyWomen, we are poised to address the gaps in education for our clinicians, patients, and the public.
To address these needs, the Women in Pulmonary program was created. Women in Pulmonary started as a yearly luncheon and has expanded into a yearlong program that will work to fill these gaps by not only elevating the wants and needs of women in pulmonary medicine, but also by bringing awareness to clinicians, patients, and the public on diseases that are not typically considered “women’s issues.”
CHEST and HealthyWomen are working to provide education, in the form of free webinars, multimedia resources, and live events to achieve the following outcomes:
Women in Pulmonary Medicine: CHEST and HealthyWomen aim to create the tools and educational opportunities that will empower our female clinicians to elevate their voices and become advocates for their career advancement, as well as improved diagnosis and treatment of women with pulmonary diseases.
Patients, Caregivers, and the Public: With this initiative, CHEST and HealthyWomen strive to empower women with the knowledge they need to become champions of their lung health. We will provide them with talking points, questions and awareness of symptoms of pulmonary conditions and diseases, such as: lung cancer, ILD/IPF, COPD, pulmonary hypertension, and asthma so that they are better able to go to their doctor appointments ready to advocate for the care they need.
Clinicians: CHEST and HealthyWomen will aim to equip all clinicians, not just women, with exposure and education that address gender differences in treatment and diagnosis of diseases like lung cancer, asthma, COPD, PH, and ILD/IPF.
Women in Pulmonary aims to provide essential education to every clinician treating women, promote awareness among patients and the public on key information to improve conversations with their health-care providers, and create opportunities for women in chest medicine to advance their careers through professional development, engagement, networking, and mentorship connections. This program will be one step in the direction of changing how women are viewed in medicine and how diseases are perceived across genders.
Bibliography
Calderone K. The influence of gender on the frequency of pain and sedative medication administered to postoperative patients. Sex Roles. 1990;23(11-12): 713-725.
Carnlöf C, et al. Women with PSVY are often misdiagnosed, referred later than men, and have more symptoms after ablation. Scand Cardiovasc J. 2017; 51(6): 299-307.
Chen EH, et al. Gender disparity in analgesic treatment of emergency departmetn patietns with acute abdominal pain. Acad Emerg Med. 2008;15(5):414-418.
Doximity. 2018 Physician Compensation Report. Doximity.
Grisham S. Medscape Pulmonologist Compensation Report 2017. https://www.medscape.com/slideshow/compensation-2017-pulmonary-medicine-6008586. Accessed Jan 16, 2018.
Hoffmann DE, Tarzian AJ. The girl who cried pain: a bias against women in the treatment of pain. J Law Med Ethics. 2001;29(1):13-27.
MHC Center. Sex-Specific Medical Research: Why Women’s Health Can’t Wait. Brigham and Women’s Hospital, Mary Horrigan Connors Center for Women’s Health & Gender Biology. Brigham and Women’s Hospital;2014.
Morton MJ, Sonnad SS. Women on professional society and journal editorial boards. J National Med Assoc. 2007;99(7):764-771.
Pinkerton K, et al. Women and lung disease. sex differences and global health disparities. Am J Respir Crit Care Med. 2015;192(1):11-16.
Rademaker M. (2001). Do women have more adverse drug reactions? Am J Clin Dermatol. 2001;2(6): 349-351.
Soldin O, Mattison M. Sex differences in pharmacokinetics and pharmacodynamics. Clin Pharmacokinetics. 2009;48(3):143-157.
The gender gap exists for women in pulmonary medicine. According to the Medscape Pulmonologist Compensation Report 2017, women pulmonologists earned 23% less than their male counterparts even though:
- 2% of women pulmonologists work part time vs 8% of men;
- more women (66%) than men (48%) reported seeking promotion. (Grisham, 2017)
If we take a look at a recent report done by Doximity that analyzed responses on more than 65,000 licensed US doctors across the country, the report reveals that the gap between female and male physicians across the nation, women on average make about $91,000 less annually (Doximity, 2018).
Despite ever-growing enrollment rates for women in medical schools, female physicians are often underrepresented in academic and research settings. According to a study published in the Journal of National Medical Association, “between 80 and 90 percent of leadership roles in medicine, like medical school deans, are filled by men.” (Morton & Sonnad, 2007)
These astounding gaps do not stop at the clinician’s door. This gender inequality is evident in the women who are receiving medical treatment, as well. There are two major issues that exist for women seeking treatment:
1. Not being taken as seriously as male patients:
- Women are more likely to be prescribed sedatives for their pain, and men are more likely to be prescribed pain medication. (L. Calderone, 1990)
- Women are more likely to be treated less aggressively in their initial encounters with the health-care system until they prove that they are as sick as male patients with similar symptoms. (Hoffmann & Tarzian, 2001)
- Nationwide, men wait an average of 49 minutes before receiving an analgesic for acute abdominal pain. Women wait an average of 65 minutes for the same thing. (Chen, et al., 2008)
- Multiple studies have shown that female patients’ symptoms are less likely to be taken seriously by doctors, and women are more likely to be misdiagnosed, have their symptoms go unrecognized, or be told what they’re experiencing is psychosomatic. (Hoffmann & Tarzian, 2001) (Carnlöf, Iwarzon, Jensen-Urstad, Gadler, & Insulander, 2017)
2. Being diagnosed and treated the same as male patients
- Up until 1993 when the National Institutes of Health Revitalization Act mandated that all women and minorities be included in clinical trials funded by the NIH, the guidelines and diagnosis for treatment have historically been based off the archetypal patient: a 154-pound white male. Because of this, women are often misdiagnosed or receive treatments that are ineffective or potentially harmful to their health. Even still, researchers frequently do not enroll an adequate number of women or fail to analyze or report data separately by sex. (MHC Center, 2014)
- Women and men metabolize drugs differently, yet dosages are rarely broken down by sex. Women also experience different side effects and derive different benefits from the same treatments. (Soldin & Mattison, 2009)
- Female patients have a 1.5 to 1.7 times higher chance of having an adverse drug reaction. (Rademaker, 2001)
- There are many diseases and conditions that are alarmingly more prevalent among women. Nonsmoking women are three times more likely to get lung cancer than nonsmoking men, according to a comprehensive 2014 report by Brigham and Women’s Hospital in Boston, called “Women’s Health Can’t Wait.” (MHC Center, 2014)
“While the number of women participating in lung cancer clinical trials has risen, women—particularly those from racial and ethnic minorities—are still less likely to enroll in these trials than men. Even when studies include women, researchers often fail to analyze data by sex or include hormone status or other gender-specific factors, making it difficult to uncover differences in incidence, prevalence, and survivability between men and women and to replicate the studies.” (MHC Center, 2014)In the pulmonary space, there is growing evidence that a number of pulmonary diseases affect women differently and with a greater degree of severity than men. Respiratory conditions that impact women nearly exclusively include pulmonary hypertension, catamenial diseases, and pregnancy-associated asthma exacerbation. (Pinkerton, et al., 2015) According to the CDC, cancer is the number one cause of death for women ages 35-64, and the number one cancer killer in women is lung cancer. Women have been taught to care and take notice of the symptoms of breast cancer, HPV, ovarian cancer, and other “women’s diseases,” and, yet, more women die every day from lung cancer than from breast, ovarian, and uterine cancers combined.
Why CHEST?
Now, why does this matter to us at CHEST? What can we do about it? How do we begin to tackle such a large issue that permeates nearly every facet of society?
CHEST is in a unique position to not only address the professional development needs of our female membership, but with the help and leadership of the CHEST Foundation and a new partnership with HealthyWomen, we are poised to address the gaps in education for our clinicians, patients, and the public.
To address these needs, the Women in Pulmonary program was created. Women in Pulmonary started as a yearly luncheon and has expanded into a yearlong program that will work to fill these gaps by not only elevating the wants and needs of women in pulmonary medicine, but also by bringing awareness to clinicians, patients, and the public on diseases that are not typically considered “women’s issues.”
CHEST and HealthyWomen are working to provide education, in the form of free webinars, multimedia resources, and live events to achieve the following outcomes:
Women in Pulmonary Medicine: CHEST and HealthyWomen aim to create the tools and educational opportunities that will empower our female clinicians to elevate their voices and become advocates for their career advancement, as well as improved diagnosis and treatment of women with pulmonary diseases.
Patients, Caregivers, and the Public: With this initiative, CHEST and HealthyWomen strive to empower women with the knowledge they need to become champions of their lung health. We will provide them with talking points, questions and awareness of symptoms of pulmonary conditions and diseases, such as: lung cancer, ILD/IPF, COPD, pulmonary hypertension, and asthma so that they are better able to go to their doctor appointments ready to advocate for the care they need.
Clinicians: CHEST and HealthyWomen will aim to equip all clinicians, not just women, with exposure and education that address gender differences in treatment and diagnosis of diseases like lung cancer, asthma, COPD, PH, and ILD/IPF.
Women in Pulmonary aims to provide essential education to every clinician treating women, promote awareness among patients and the public on key information to improve conversations with their health-care providers, and create opportunities for women in chest medicine to advance their careers through professional development, engagement, networking, and mentorship connections. This program will be one step in the direction of changing how women are viewed in medicine and how diseases are perceived across genders.
Bibliography
Calderone K. The influence of gender on the frequency of pain and sedative medication administered to postoperative patients. Sex Roles. 1990;23(11-12): 713-725.
Carnlöf C, et al. Women with PSVY are often misdiagnosed, referred later than men, and have more symptoms after ablation. Scand Cardiovasc J. 2017; 51(6): 299-307.
Chen EH, et al. Gender disparity in analgesic treatment of emergency departmetn patietns with acute abdominal pain. Acad Emerg Med. 2008;15(5):414-418.
Doximity. 2018 Physician Compensation Report. Doximity.
Grisham S. Medscape Pulmonologist Compensation Report 2017. https://www.medscape.com/slideshow/compensation-2017-pulmonary-medicine-6008586. Accessed Jan 16, 2018.
Hoffmann DE, Tarzian AJ. The girl who cried pain: a bias against women in the treatment of pain. J Law Med Ethics. 2001;29(1):13-27.
MHC Center. Sex-Specific Medical Research: Why Women’s Health Can’t Wait. Brigham and Women’s Hospital, Mary Horrigan Connors Center for Women’s Health & Gender Biology. Brigham and Women’s Hospital;2014.
Morton MJ, Sonnad SS. Women on professional society and journal editorial boards. J National Med Assoc. 2007;99(7):764-771.
Pinkerton K, et al. Women and lung disease. sex differences and global health disparities. Am J Respir Crit Care Med. 2015;192(1):11-16.
Rademaker M. (2001). Do women have more adverse drug reactions? Am J Clin Dermatol. 2001;2(6): 349-351.
Soldin O, Mattison M. Sex differences in pharmacokinetics and pharmacodynamics. Clin Pharmacokinetics. 2009;48(3):143-157.
In Memoriam
CHEST has been informed of the following members’ deaths. We extend our sincere condolences to friends and family.
Nagesh V Salian, MD, FCCP (2016)
Ted A Calinog, MD, FCCP (2017)
Azam Ansari, MD
(2017)
Arthur E. Schmidt, MD, FCCP (2017)
W. Gerald Rainer, MD, FCCP (2017)
CHEST has been informed of the following members’ deaths. We extend our sincere condolences to friends and family.
Nagesh V Salian, MD, FCCP (2016)
Ted A Calinog, MD, FCCP (2017)
Azam Ansari, MD
(2017)
Arthur E. Schmidt, MD, FCCP (2017)
W. Gerald Rainer, MD, FCCP (2017)
CHEST has been informed of the following members’ deaths. We extend our sincere condolences to friends and family.
Nagesh V Salian, MD, FCCP (2016)
Ted A Calinog, MD, FCCP (2017)
Azam Ansari, MD
(2017)
Arthur E. Schmidt, MD, FCCP (2017)
W. Gerald Rainer, MD, FCCP (2017)
Five things to do around the convention center at CHEST 2018
Planning to attend CHEST 2018? We know you’re always on the go, so we’ve come up with a few quick things to do in San Antonio without having to go more than a few blocks outside of the convention center.
Whataburger
While some may be hardcore In-N-Out fans, there’s another well known burger joint in Texas with a location that happens to be next to the convention center on E Commerce St. Head on over to Whataburger and experience what the company calls a “bigger, better burger.”
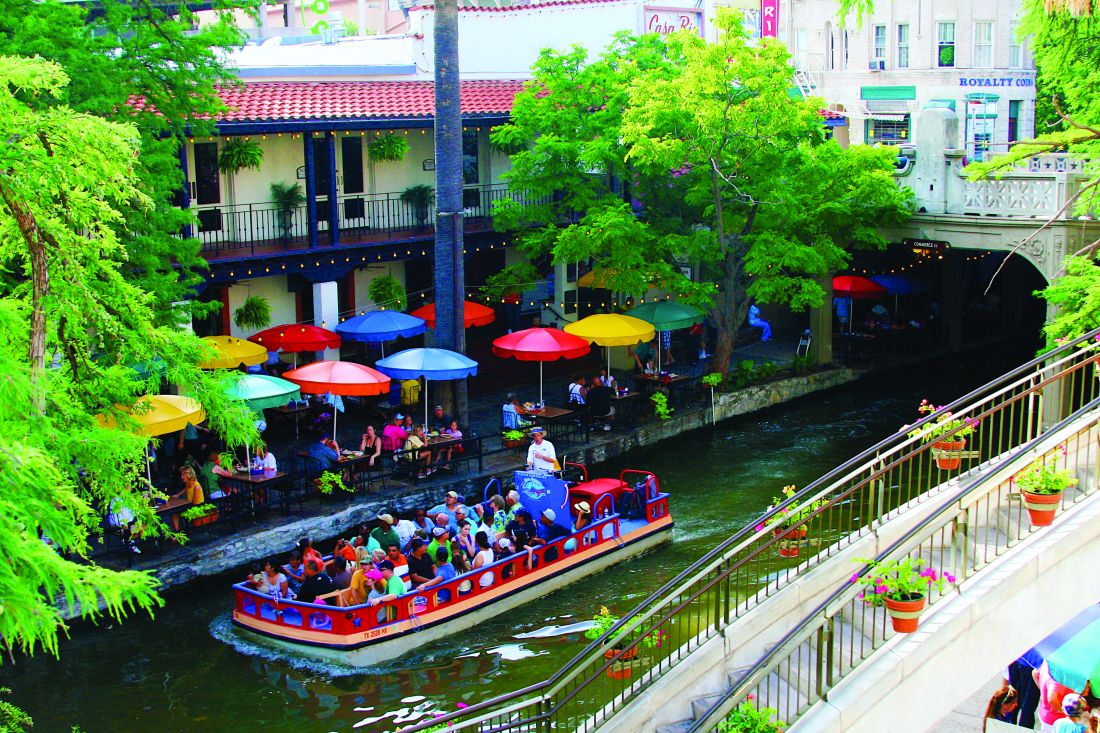
San Antonio Riverwalk
Want to experience the San Antonio, Texas atmosphere but don’t have time for a long excursion? The Henry B. Gonzalez Convention Center is a few steps away from the Riverwalk, which winds throughout the city. Off of the northwest corner of the convention center, take a stroll and experience the picturesque beauty of the San Antonio river, the restaurants, and the bright colorful surroundings.
La Villita Historic Arts Village
Interested in art? Interested in architecture? La Villita, located on the west side of the convention center on S Alamo St, is on the US government’s National Register of Historic Places as a Historic District. Take a look at different architectural styles, like adobe, early Victorian, and Texas vernacular limestone buildings. You’ll find markers throughout La Villita with information about each building’s history. You’ll also find local artists, custom art, and unique dining options.
Tower of the Americas
Exit the south end of the convention center to go to the Tower of the Americas for a spectacular view of the city. This 750-foot tall tower has an observation deck, revolving restaurant with panoramic views, a stationary bar, and a 4D theater adventure ride great for the whole family. This is a great stop for lunch, dinner, or a nice afternoon activity.
The Alamo
Lastly, if you have an hour to spare, take a tour of the Alamo that commemorates the 1836 siege and battle. There are free and ticketed activities, including audio or guided tours (ticketed) or history talks, visiting the Alamo Church, exhibitions, and more! Don’t forget to stop at the gift shop for a souvenir or two to take home.
Planning to attend CHEST 2018? We know you’re always on the go, so we’ve come up with a few quick things to do in San Antonio without having to go more than a few blocks outside of the convention center.
Whataburger
While some may be hardcore In-N-Out fans, there’s another well known burger joint in Texas with a location that happens to be next to the convention center on E Commerce St. Head on over to Whataburger and experience what the company calls a “bigger, better burger.”
San Antonio Riverwalk
Want to experience the San Antonio, Texas atmosphere but don’t have time for a long excursion? The Henry B. Gonzalez Convention Center is a few steps away from the Riverwalk, which winds throughout the city. Off of the northwest corner of the convention center, take a stroll and experience the picturesque beauty of the San Antonio river, the restaurants, and the bright colorful surroundings.
La Villita Historic Arts Village
Interested in art? Interested in architecture? La Villita, located on the west side of the convention center on S Alamo St, is on the US government’s National Register of Historic Places as a Historic District. Take a look at different architectural styles, like adobe, early Victorian, and Texas vernacular limestone buildings. You’ll find markers throughout La Villita with information about each building’s history. You’ll also find local artists, custom art, and unique dining options.
Tower of the Americas
Exit the south end of the convention center to go to the Tower of the Americas for a spectacular view of the city. This 750-foot tall tower has an observation deck, revolving restaurant with panoramic views, a stationary bar, and a 4D theater adventure ride great for the whole family. This is a great stop for lunch, dinner, or a nice afternoon activity.
The Alamo
Lastly, if you have an hour to spare, take a tour of the Alamo that commemorates the 1836 siege and battle. There are free and ticketed activities, including audio or guided tours (ticketed) or history talks, visiting the Alamo Church, exhibitions, and more! Don’t forget to stop at the gift shop for a souvenir or two to take home.
Planning to attend CHEST 2018? We know you’re always on the go, so we’ve come up with a few quick things to do in San Antonio without having to go more than a few blocks outside of the convention center.
Whataburger
While some may be hardcore In-N-Out fans, there’s another well known burger joint in Texas with a location that happens to be next to the convention center on E Commerce St. Head on over to Whataburger and experience what the company calls a “bigger, better burger.”
San Antonio Riverwalk
Want to experience the San Antonio, Texas atmosphere but don’t have time for a long excursion? The Henry B. Gonzalez Convention Center is a few steps away from the Riverwalk, which winds throughout the city. Off of the northwest corner of the convention center, take a stroll and experience the picturesque beauty of the San Antonio river, the restaurants, and the bright colorful surroundings.
La Villita Historic Arts Village
Interested in art? Interested in architecture? La Villita, located on the west side of the convention center on S Alamo St, is on the US government’s National Register of Historic Places as a Historic District. Take a look at different architectural styles, like adobe, early Victorian, and Texas vernacular limestone buildings. You’ll find markers throughout La Villita with information about each building’s history. You’ll also find local artists, custom art, and unique dining options.
Tower of the Americas
Exit the south end of the convention center to go to the Tower of the Americas for a spectacular view of the city. This 750-foot tall tower has an observation deck, revolving restaurant with panoramic views, a stationary bar, and a 4D theater adventure ride great for the whole family. This is a great stop for lunch, dinner, or a nice afternoon activity.
The Alamo
Lastly, if you have an hour to spare, take a tour of the Alamo that commemorates the 1836 siege and battle. There are free and ticketed activities, including audio or guided tours (ticketed) or history talks, visiting the Alamo Church, exhibitions, and more! Don’t forget to stop at the gift shop for a souvenir or two to take home.
New lung cancer screening guideline from CHEST
An update to CHEST’s lung cancer screening guideline, Screening for Lung Cancer: CHEST Guideline and Expert Panel Report, has just been published online in the journal CHEST®. This update was made possible by the hard work of my co-authors and the amazing support of the CHEST staff.
Our goal was to update the evidence base for the benefit, harms, and implementation of low-radiation dose chest CT screening, then use this evidence base to produce meaningful and usable recommendations. The process for developing the guideline followed the rigorous methodological standards of CHEST in which the evidence was gathered from a systematic literature review, and the overall quality of the body of evidence was assessed using the GRADE approach. Recommendations were developed and graded based on this assessment.
There are a few aspects of the new guidelines to highlight. First, we have updated some of the core recommendations; second, we have developed new recommendations related to the implementation of high-quality screening; and third, the CHEST approach to guideline development has evolved to allow us to provide recommendations in which the evidence allows and statements based on experience and expert consensus in which it does not. Through this process, we developed six graded recommendations and nine ungraded consensus-based statements.
In this update, a few changes to the core recommendations about who should be screened are worthy to note:
- We have recommended an increase to the upper age of the screen-eligible cohort from 74 to 77, in line with CMS coverage and reflecting the oldest age of participants in the National Lung Screening Trial at the end of the screening period.
- We have directly addressed the cohort of individuals who are at high risk for having/developing lung cancer based on clinical risk prediction calculators but do not meet the current eligibility criteria. We recommended that this cohort should not be routinely screened given the greater potential for this cohort to have comorbid conditions that would influence morbidity from the evaluation and treatment of screen-detected findings and death from any cause. We did, however, state that there will be individuals within the cohort deemed to be at high risk for lung cancer from a clinical risk prediction calculator who are healthy enough to benefit from lung cancer screening and that low-radiation dose CT screening could be considered in these individuals.
- We recommended against low-radiation dose CT screening in cohorts at low risk of developing lung cancer and in individuals with comorbidities that adversely influence their ability to tolerate the evaluation of screen-detected findings, tolerate treatment of an early stage screen-detected lung cancer, or that substantially limit their life expectancy.
- We also highlighted that screening is reserved for patients without symptoms that could be caused by the presence of lung cancer, stressing that all symptomatic patients should receive an appropriate diagnostic evaluation.
Our remaining recommendation and statements are focused on aspects of screening implementation that influence the balance of benefit and harms of screening and lend to an approach to screening that respects patient values. An extensive literature review, followed by a recommendation or statement, is provided to guide programs in the following areas:
- the choice of nodule size to define what constitutes a positive test;
- maximizing compliance with annual screening exams;
- developing a comprehensive approach to lung nodule management;
- minimizing overtreatment of potentially indolent lung cancers;
- the provision of evidence-based tobacco cessation treatment;
- providing effective counseling and shared decision-making visits prior to the low-radiation dose CT scan;
- how to perform the low-radiation dose CT scan;
- structured reporting of the exam results, management of non-nodule findings on the low radiation dose CT; and
- the development of data collection and reporting tools that are capable of assisting with quality improvement initiatives.
Throughout the recommendations and statements, we have tried to be sensitive to the variety of acceptable approaches to screening program organization, ranging from program structures that are entirely decentralized (test ordering, counseling, and management of the findings by the referring provider) to those that are entirely centralized (test ordering, counseling, and management of the findings by the screening program).
Though we have attempted to comprehensively evaluate the literature and balance available evidence with pragmatism and the needs of our patients, we recognize that well-intentioned and informed experts can have different opinions about aspects of our guidelines. This highlights the need for further research to guide the screening community. Most will agree that it is time to increase access to high- quality lung cancer screening programs across the country. We hope that the updated CHEST lung cancer screening guidelines can help catalyze this.
Coinciding with the publication of the guideline, CHEST has developed new e-learning modules on the benefits and harms of CT screening for lung cancer. The modules are based on the CHEST 2018 educational session on the Screening for Lung Cancer Guidelines. The modules are available at chestnet.org/lungcancerscreening.
An update to CHEST’s lung cancer screening guideline, Screening for Lung Cancer: CHEST Guideline and Expert Panel Report, has just been published online in the journal CHEST®. This update was made possible by the hard work of my co-authors and the amazing support of the CHEST staff.
Our goal was to update the evidence base for the benefit, harms, and implementation of low-radiation dose chest CT screening, then use this evidence base to produce meaningful and usable recommendations. The process for developing the guideline followed the rigorous methodological standards of CHEST in which the evidence was gathered from a systematic literature review, and the overall quality of the body of evidence was assessed using the GRADE approach. Recommendations were developed and graded based on this assessment.
There are a few aspects of the new guidelines to highlight. First, we have updated some of the core recommendations; second, we have developed new recommendations related to the implementation of high-quality screening; and third, the CHEST approach to guideline development has evolved to allow us to provide recommendations in which the evidence allows and statements based on experience and expert consensus in which it does not. Through this process, we developed six graded recommendations and nine ungraded consensus-based statements.
In this update, a few changes to the core recommendations about who should be screened are worthy to note:
- We have recommended an increase to the upper age of the screen-eligible cohort from 74 to 77, in line with CMS coverage and reflecting the oldest age of participants in the National Lung Screening Trial at the end of the screening period.
- We have directly addressed the cohort of individuals who are at high risk for having/developing lung cancer based on clinical risk prediction calculators but do not meet the current eligibility criteria. We recommended that this cohort should not be routinely screened given the greater potential for this cohort to have comorbid conditions that would influence morbidity from the evaluation and treatment of screen-detected findings and death from any cause. We did, however, state that there will be individuals within the cohort deemed to be at high risk for lung cancer from a clinical risk prediction calculator who are healthy enough to benefit from lung cancer screening and that low-radiation dose CT screening could be considered in these individuals.
- We recommended against low-radiation dose CT screening in cohorts at low risk of developing lung cancer and in individuals with comorbidities that adversely influence their ability to tolerate the evaluation of screen-detected findings, tolerate treatment of an early stage screen-detected lung cancer, or that substantially limit their life expectancy.
- We also highlighted that screening is reserved for patients without symptoms that could be caused by the presence of lung cancer, stressing that all symptomatic patients should receive an appropriate diagnostic evaluation.
Our remaining recommendation and statements are focused on aspects of screening implementation that influence the balance of benefit and harms of screening and lend to an approach to screening that respects patient values. An extensive literature review, followed by a recommendation or statement, is provided to guide programs in the following areas:
- the choice of nodule size to define what constitutes a positive test;
- maximizing compliance with annual screening exams;
- developing a comprehensive approach to lung nodule management;
- minimizing overtreatment of potentially indolent lung cancers;
- the provision of evidence-based tobacco cessation treatment;
- providing effective counseling and shared decision-making visits prior to the low-radiation dose CT scan;
- how to perform the low-radiation dose CT scan;
- structured reporting of the exam results, management of non-nodule findings on the low radiation dose CT; and
- the development of data collection and reporting tools that are capable of assisting with quality improvement initiatives.
Throughout the recommendations and statements, we have tried to be sensitive to the variety of acceptable approaches to screening program organization, ranging from program structures that are entirely decentralized (test ordering, counseling, and management of the findings by the referring provider) to those that are entirely centralized (test ordering, counseling, and management of the findings by the screening program).
Though we have attempted to comprehensively evaluate the literature and balance available evidence with pragmatism and the needs of our patients, we recognize that well-intentioned and informed experts can have different opinions about aspects of our guidelines. This highlights the need for further research to guide the screening community. Most will agree that it is time to increase access to high- quality lung cancer screening programs across the country. We hope that the updated CHEST lung cancer screening guidelines can help catalyze this.
Coinciding with the publication of the guideline, CHEST has developed new e-learning modules on the benefits and harms of CT screening for lung cancer. The modules are based on the CHEST 2018 educational session on the Screening for Lung Cancer Guidelines. The modules are available at chestnet.org/lungcancerscreening.
An update to CHEST’s lung cancer screening guideline, Screening for Lung Cancer: CHEST Guideline and Expert Panel Report, has just been published online in the journal CHEST®. This update was made possible by the hard work of my co-authors and the amazing support of the CHEST staff.
Our goal was to update the evidence base for the benefit, harms, and implementation of low-radiation dose chest CT screening, then use this evidence base to produce meaningful and usable recommendations. The process for developing the guideline followed the rigorous methodological standards of CHEST in which the evidence was gathered from a systematic literature review, and the overall quality of the body of evidence was assessed using the GRADE approach. Recommendations were developed and graded based on this assessment.
There are a few aspects of the new guidelines to highlight. First, we have updated some of the core recommendations; second, we have developed new recommendations related to the implementation of high-quality screening; and third, the CHEST approach to guideline development has evolved to allow us to provide recommendations in which the evidence allows and statements based on experience and expert consensus in which it does not. Through this process, we developed six graded recommendations and nine ungraded consensus-based statements.
In this update, a few changes to the core recommendations about who should be screened are worthy to note:
- We have recommended an increase to the upper age of the screen-eligible cohort from 74 to 77, in line with CMS coverage and reflecting the oldest age of participants in the National Lung Screening Trial at the end of the screening period.
- We have directly addressed the cohort of individuals who are at high risk for having/developing lung cancer based on clinical risk prediction calculators but do not meet the current eligibility criteria. We recommended that this cohort should not be routinely screened given the greater potential for this cohort to have comorbid conditions that would influence morbidity from the evaluation and treatment of screen-detected findings and death from any cause. We did, however, state that there will be individuals within the cohort deemed to be at high risk for lung cancer from a clinical risk prediction calculator who are healthy enough to benefit from lung cancer screening and that low-radiation dose CT screening could be considered in these individuals.
- We recommended against low-radiation dose CT screening in cohorts at low risk of developing lung cancer and in individuals with comorbidities that adversely influence their ability to tolerate the evaluation of screen-detected findings, tolerate treatment of an early stage screen-detected lung cancer, or that substantially limit their life expectancy.
- We also highlighted that screening is reserved for patients without symptoms that could be caused by the presence of lung cancer, stressing that all symptomatic patients should receive an appropriate diagnostic evaluation.
Our remaining recommendation and statements are focused on aspects of screening implementation that influence the balance of benefit and harms of screening and lend to an approach to screening that respects patient values. An extensive literature review, followed by a recommendation or statement, is provided to guide programs in the following areas:
- the choice of nodule size to define what constitutes a positive test;
- maximizing compliance with annual screening exams;
- developing a comprehensive approach to lung nodule management;
- minimizing overtreatment of potentially indolent lung cancers;
- the provision of evidence-based tobacco cessation treatment;
- providing effective counseling and shared decision-making visits prior to the low-radiation dose CT scan;
- how to perform the low-radiation dose CT scan;
- structured reporting of the exam results, management of non-nodule findings on the low radiation dose CT; and
- the development of data collection and reporting tools that are capable of assisting with quality improvement initiatives.
Throughout the recommendations and statements, we have tried to be sensitive to the variety of acceptable approaches to screening program organization, ranging from program structures that are entirely decentralized (test ordering, counseling, and management of the findings by the referring provider) to those that are entirely centralized (test ordering, counseling, and management of the findings by the screening program).
Though we have attempted to comprehensively evaluate the literature and balance available evidence with pragmatism and the needs of our patients, we recognize that well-intentioned and informed experts can have different opinions about aspects of our guidelines. This highlights the need for further research to guide the screening community. Most will agree that it is time to increase access to high- quality lung cancer screening programs across the country. We hope that the updated CHEST lung cancer screening guidelines can help catalyze this.
Coinciding with the publication of the guideline, CHEST has developed new e-learning modules on the benefits and harms of CT screening for lung cancer. The modules are based on the CHEST 2018 educational session on the Screening for Lung Cancer Guidelines. The modules are available at chestnet.org/lungcancerscreening.
Bringing respiratory care to asthma clinics in Guyana
How it all started
The study abroad project was truly a goal and vision that came about after returning to Guyana after approximately 46 years. I was born in Guyana but left as a child and returned later and joined a mission group. In 2015, I began a personal journey of missionary service with the team of Bridge Global Medical Missions (BGMM) in Georgetown, Guyana. I was the first respiratory therapist to join the team.
I remember during the first few days in the hospitals I was told that there was “a lot of wheezing” in the EDs. Treating patients consisted of just administrating short-acting nebulizer treatments, but I remember being very impressed with the ICU at the main public hospital, Georgetown Public Hospital Corporation (GPHC), because they had the ventilators I could use. However, physicians only managed the patients while the nurses were left to monitor the ventilators and equipment, which they did not understand.
At the Linden Hospital in Guyana, the ED was constantly full of the “wheezers,” and the ICU only had ventilators that were basically nonfunctioning due to language barriers or a lack of biomed professionals. One of my fondest memories was fixing two ventilators from China. I could get the ventilators to work and explain the basic modes because in my mind, it was just a ventilator, and they could see the modes. The problem was the language was all in Chinese! So, we all got together: a Cuban doctor, a Cuban biomed, and a nurse with a translation program and, finally, changed the language to English. It was an interesting day!
When we were on our study abroad trip this past January, I was able to place an intubated patient on that same ventilator. After my first visit to Linden Hospital, I addressed a few of my observations with the medical director, and I will never forget his comment. He said, “I thought respiratory would just come do some nebulizer treatments and show us oxygen.”
Study abroad and respiratory care
Then the vision of my project began, because I needed to show him the scope of the practice of a respiratory therapist. I asked Dr. Heyliger-Thomas of BGMM if she could assist me in promoting a study abroad program in Guyana with the Ministry of Health. It was very important for me to bring my students to Guyana for many reasons, the most important being the profession was needed there, and our students would be excellent representatives.
In 2015, the study “Introduction of spirometry into clinical practice in Georgetown, Guyana: quality and diagnostic outcomes” highlighted increased physician referral to the country’s only COPD/asthma clinic. I wanted to promote the importance of study abroad and international mission work, especially when promoting the care of asthma and the pulmonary patient, which I believe we did. The main project during study abroad was to test the school-aged children in Linden, thereby showing that there was undiagnosed asthma.
The 2 days that we were in Linden brought the largest sign-up for their clinic. When we did our screening at Mackenzie High School, we were able to utilize the portable spirometers and printer purchased by the CHEST Foundation community service grant. We are still collecting data, but the one thing that was revealed was the difficulty in obtaining medication for the treatment of asthma and COPD in some areas.
This project was also a learning experience for our students in many ways: in how they performed their interviews, how the culture affected the way their patients answered their questionnaires, and even how they performed on the tests. The value to the student and the individual of working within a different culture, far away from the norms of North America, allows them to appreciate their patients, the work they do, and their interprofessional team in a whole new light.
I want this experience to have an impact on each student’s life. You are a teacher, an instructor, a mentor, professor, and much more when traveling with 10 students. The most satisfying moment is the transformation you see in them. They are no longer timid and unsure of themselves; they have greater confidence in their abilities and a deeper understanding of the needs of a patient. They finally understand the importance of culture as it pertains to health care.
The effect of the CHEST Foundation grant
Applying for the CHEST Foundation community service grant was the largest grant I had ever attempted. Having a support system behind you is the most important piece of advice I can give to future grant applicants. I could not have completed my grant without our grant team at Texas State University. They truly had my back; and close to the deadline when it seemed insurmountable, they helped push me through it. The other piece of advice is to have a true vision and stick to that vision. The most difficult part of my project was the budget, prioritizing the things or people that I needed. Honestly, I needed help here, because for me, I needed everything. I had to make choices and leave some things out. I focused on what the actual need was for the many.
My ultimate goal for Guyana is to promote and show the need for respiratory care professionals to have that education offered at the University of Guyana as part of its allied health program and assist those in the application to the International Fellowship Program of the American Association of Respiratory Care—there has never been a fellow from Guyana. I believe that Guyana will have the resources, and with assistance, could achieve the goal. My vision and goal started in 2016, and I want to achieve it in the next 10 years.
I would like to thank all the CHEST Foundation donors from the bottom of my heart. This project was real and, as a CHEST member myself, it encourages me to be a better donor. Thank you—for it was and is much appreciated. Finally, I would like to express my thanks to my Co-Assistant Program Director, Holly Wise (Mass Communications) and Amber Hazelett, RRT (RC assistant), and the BGMM team for their entire support throughout the study abroad journey.
(This article was previous published in CHEST Thought Leaders.)
This grant is supported in full by the CHEST Foundation. Donors like you make grants like this possible. Thank you for your generosity and passion for community service and moving the needle forward on improving patient outcomes. To support community service initiatives, and the next generation of lung health champions, please go to foundation.chestnet.org/donate
How it all started
The study abroad project was truly a goal and vision that came about after returning to Guyana after approximately 46 years. I was born in Guyana but left as a child and returned later and joined a mission group. In 2015, I began a personal journey of missionary service with the team of Bridge Global Medical Missions (BGMM) in Georgetown, Guyana. I was the first respiratory therapist to join the team.
I remember during the first few days in the hospitals I was told that there was “a lot of wheezing” in the EDs. Treating patients consisted of just administrating short-acting nebulizer treatments, but I remember being very impressed with the ICU at the main public hospital, Georgetown Public Hospital Corporation (GPHC), because they had the ventilators I could use. However, physicians only managed the patients while the nurses were left to monitor the ventilators and equipment, which they did not understand.
At the Linden Hospital in Guyana, the ED was constantly full of the “wheezers,” and the ICU only had ventilators that were basically nonfunctioning due to language barriers or a lack of biomed professionals. One of my fondest memories was fixing two ventilators from China. I could get the ventilators to work and explain the basic modes because in my mind, it was just a ventilator, and they could see the modes. The problem was the language was all in Chinese! So, we all got together: a Cuban doctor, a Cuban biomed, and a nurse with a translation program and, finally, changed the language to English. It was an interesting day!
When we were on our study abroad trip this past January, I was able to place an intubated patient on that same ventilator. After my first visit to Linden Hospital, I addressed a few of my observations with the medical director, and I will never forget his comment. He said, “I thought respiratory would just come do some nebulizer treatments and show us oxygen.”
Study abroad and respiratory care
Then the vision of my project began, because I needed to show him the scope of the practice of a respiratory therapist. I asked Dr. Heyliger-Thomas of BGMM if she could assist me in promoting a study abroad program in Guyana with the Ministry of Health. It was very important for me to bring my students to Guyana for many reasons, the most important being the profession was needed there, and our students would be excellent representatives.
In 2015, the study “Introduction of spirometry into clinical practice in Georgetown, Guyana: quality and diagnostic outcomes” highlighted increased physician referral to the country’s only COPD/asthma clinic. I wanted to promote the importance of study abroad and international mission work, especially when promoting the care of asthma and the pulmonary patient, which I believe we did. The main project during study abroad was to test the school-aged children in Linden, thereby showing that there was undiagnosed asthma.
The 2 days that we were in Linden brought the largest sign-up for their clinic. When we did our screening at Mackenzie High School, we were able to utilize the portable spirometers and printer purchased by the CHEST Foundation community service grant. We are still collecting data, but the one thing that was revealed was the difficulty in obtaining medication for the treatment of asthma and COPD in some areas.
This project was also a learning experience for our students in many ways: in how they performed their interviews, how the culture affected the way their patients answered their questionnaires, and even how they performed on the tests. The value to the student and the individual of working within a different culture, far away from the norms of North America, allows them to appreciate their patients, the work they do, and their interprofessional team in a whole new light.
I want this experience to have an impact on each student’s life. You are a teacher, an instructor, a mentor, professor, and much more when traveling with 10 students. The most satisfying moment is the transformation you see in them. They are no longer timid and unsure of themselves; they have greater confidence in their abilities and a deeper understanding of the needs of a patient. They finally understand the importance of culture as it pertains to health care.
The effect of the CHEST Foundation grant
Applying for the CHEST Foundation community service grant was the largest grant I had ever attempted. Having a support system behind you is the most important piece of advice I can give to future grant applicants. I could not have completed my grant without our grant team at Texas State University. They truly had my back; and close to the deadline when it seemed insurmountable, they helped push me through it. The other piece of advice is to have a true vision and stick to that vision. The most difficult part of my project was the budget, prioritizing the things or people that I needed. Honestly, I needed help here, because for me, I needed everything. I had to make choices and leave some things out. I focused on what the actual need was for the many.
My ultimate goal for Guyana is to promote and show the need for respiratory care professionals to have that education offered at the University of Guyana as part of its allied health program and assist those in the application to the International Fellowship Program of the American Association of Respiratory Care—there has never been a fellow from Guyana. I believe that Guyana will have the resources, and with assistance, could achieve the goal. My vision and goal started in 2016, and I want to achieve it in the next 10 years.
I would like to thank all the CHEST Foundation donors from the bottom of my heart. This project was real and, as a CHEST member myself, it encourages me to be a better donor. Thank you—for it was and is much appreciated. Finally, I would like to express my thanks to my Co-Assistant Program Director, Holly Wise (Mass Communications) and Amber Hazelett, RRT (RC assistant), and the BGMM team for their entire support throughout the study abroad journey.
(This article was previous published in CHEST Thought Leaders.)
This grant is supported in full by the CHEST Foundation. Donors like you make grants like this possible. Thank you for your generosity and passion for community service and moving the needle forward on improving patient outcomes. To support community service initiatives, and the next generation of lung health champions, please go to foundation.chestnet.org/donate
How it all started
The study abroad project was truly a goal and vision that came about after returning to Guyana after approximately 46 years. I was born in Guyana but left as a child and returned later and joined a mission group. In 2015, I began a personal journey of missionary service with the team of Bridge Global Medical Missions (BGMM) in Georgetown, Guyana. I was the first respiratory therapist to join the team.
I remember during the first few days in the hospitals I was told that there was “a lot of wheezing” in the EDs. Treating patients consisted of just administrating short-acting nebulizer treatments, but I remember being very impressed with the ICU at the main public hospital, Georgetown Public Hospital Corporation (GPHC), because they had the ventilators I could use. However, physicians only managed the patients while the nurses were left to monitor the ventilators and equipment, which they did not understand.
At the Linden Hospital in Guyana, the ED was constantly full of the “wheezers,” and the ICU only had ventilators that were basically nonfunctioning due to language barriers or a lack of biomed professionals. One of my fondest memories was fixing two ventilators from China. I could get the ventilators to work and explain the basic modes because in my mind, it was just a ventilator, and they could see the modes. The problem was the language was all in Chinese! So, we all got together: a Cuban doctor, a Cuban biomed, and a nurse with a translation program and, finally, changed the language to English. It was an interesting day!
When we were on our study abroad trip this past January, I was able to place an intubated patient on that same ventilator. After my first visit to Linden Hospital, I addressed a few of my observations with the medical director, and I will never forget his comment. He said, “I thought respiratory would just come do some nebulizer treatments and show us oxygen.”
Study abroad and respiratory care
Then the vision of my project began, because I needed to show him the scope of the practice of a respiratory therapist. I asked Dr. Heyliger-Thomas of BGMM if she could assist me in promoting a study abroad program in Guyana with the Ministry of Health. It was very important for me to bring my students to Guyana for many reasons, the most important being the profession was needed there, and our students would be excellent representatives.
In 2015, the study “Introduction of spirometry into clinical practice in Georgetown, Guyana: quality and diagnostic outcomes” highlighted increased physician referral to the country’s only COPD/asthma clinic. I wanted to promote the importance of study abroad and international mission work, especially when promoting the care of asthma and the pulmonary patient, which I believe we did. The main project during study abroad was to test the school-aged children in Linden, thereby showing that there was undiagnosed asthma.
The 2 days that we were in Linden brought the largest sign-up for their clinic. When we did our screening at Mackenzie High School, we were able to utilize the portable spirometers and printer purchased by the CHEST Foundation community service grant. We are still collecting data, but the one thing that was revealed was the difficulty in obtaining medication for the treatment of asthma and COPD in some areas.
This project was also a learning experience for our students in many ways: in how they performed their interviews, how the culture affected the way their patients answered their questionnaires, and even how they performed on the tests. The value to the student and the individual of working within a different culture, far away from the norms of North America, allows them to appreciate their patients, the work they do, and their interprofessional team in a whole new light.
I want this experience to have an impact on each student’s life. You are a teacher, an instructor, a mentor, professor, and much more when traveling with 10 students. The most satisfying moment is the transformation you see in them. They are no longer timid and unsure of themselves; they have greater confidence in their abilities and a deeper understanding of the needs of a patient. They finally understand the importance of culture as it pertains to health care.
The effect of the CHEST Foundation grant
Applying for the CHEST Foundation community service grant was the largest grant I had ever attempted. Having a support system behind you is the most important piece of advice I can give to future grant applicants. I could not have completed my grant without our grant team at Texas State University. They truly had my back; and close to the deadline when it seemed insurmountable, they helped push me through it. The other piece of advice is to have a true vision and stick to that vision. The most difficult part of my project was the budget, prioritizing the things or people that I needed. Honestly, I needed help here, because for me, I needed everything. I had to make choices and leave some things out. I focused on what the actual need was for the many.
My ultimate goal for Guyana is to promote and show the need for respiratory care professionals to have that education offered at the University of Guyana as part of its allied health program and assist those in the application to the International Fellowship Program of the American Association of Respiratory Care—there has never been a fellow from Guyana. I believe that Guyana will have the resources, and with assistance, could achieve the goal. My vision and goal started in 2016, and I want to achieve it in the next 10 years.
I would like to thank all the CHEST Foundation donors from the bottom of my heart. This project was real and, as a CHEST member myself, it encourages me to be a better donor. Thank you—for it was and is much appreciated. Finally, I would like to express my thanks to my Co-Assistant Program Director, Holly Wise (Mass Communications) and Amber Hazelett, RRT (RC assistant), and the BGMM team for their entire support throughout the study abroad journey.
(This article was previous published in CHEST Thought Leaders.)
This grant is supported in full by the CHEST Foundation. Donors like you make grants like this possible. Thank you for your generosity and passion for community service and moving the needle forward on improving patient outcomes. To support community service initiatives, and the next generation of lung health champions, please go to foundation.chestnet.org/donate
FDA to host meeting about sleep apnea devices
You are invited to attend this open meeting on April 16, held at the FDA White Oak Campus in Silver Spring, Md. (https://www.fda.gov/MedicalDevices/NewsEvents/WorkshopsConferences/ucm596147.htm). The FDA is soliciting ideas or opinions about criteria or processes for FDA review of medical devices to diagnose or treat sleep apnea. CHEST is represented by Dr. Neil Freedman ([email protected]) and Dr. Barbara Phillips ([email protected]) who also welcome your input by email prior to the meeting. Home testing, “apps,” and the criteria to diagnose sleep apnea and/or its resolution are among the topics to be discussed.
You are invited to attend this open meeting on April 16, held at the FDA White Oak Campus in Silver Spring, Md. (https://www.fda.gov/MedicalDevices/NewsEvents/WorkshopsConferences/ucm596147.htm). The FDA is soliciting ideas or opinions about criteria or processes for FDA review of medical devices to diagnose or treat sleep apnea. CHEST is represented by Dr. Neil Freedman ([email protected]) and Dr. Barbara Phillips ([email protected]) who also welcome your input by email prior to the meeting. Home testing, “apps,” and the criteria to diagnose sleep apnea and/or its resolution are among the topics to be discussed.
You are invited to attend this open meeting on April 16, held at the FDA White Oak Campus in Silver Spring, Md. (https://www.fda.gov/MedicalDevices/NewsEvents/WorkshopsConferences/ucm596147.htm). The FDA is soliciting ideas or opinions about criteria or processes for FDA review of medical devices to diagnose or treat sleep apnea. CHEST is represented by Dr. Neil Freedman ([email protected]) and Dr. Barbara Phillips ([email protected]) who also welcome your input by email prior to the meeting. Home testing, “apps,” and the criteria to diagnose sleep apnea and/or its resolution are among the topics to be discussed.
“No consequence” Knowledge Check-In expands
In 2018, ABIM is introducing the new Knowledge Check-In assessment option, an every-2-year assessment option serving as an alternative to the 10-year assessment model. Initially, for 2018, this option will be piloted for both Internal Medicine and Nephrology. In 2019, the Knowledge Check-In will expand to several additional specialties, including Pulmonary Disease. The remaining specialties, including Critical Care Medicine, will become available in 2020.
Previously, ABIM announced that physicians taking the Knowledge Check-In in 2018—the initial year it is offered in Internal Medicine or Nephrology—would have another chance to take it again 2 years later if they were unsuccessful, even if they were due to pass the exam that year. Based on feedback ABIM received from the physician community, this feature is now being extended to include all other Internal Medicine subspecialties in the future. Therefore, if a physician opts to take the Knowledge Check-In the first year it is offered in their subspecialty and is unsuccessful, they will get at least one additional opportunity to take it 2 years later.
For more information visit www.abim.org/checkin.
In 2018, ABIM is introducing the new Knowledge Check-In assessment option, an every-2-year assessment option serving as an alternative to the 10-year assessment model. Initially, for 2018, this option will be piloted for both Internal Medicine and Nephrology. In 2019, the Knowledge Check-In will expand to several additional specialties, including Pulmonary Disease. The remaining specialties, including Critical Care Medicine, will become available in 2020.
Previously, ABIM announced that physicians taking the Knowledge Check-In in 2018—the initial year it is offered in Internal Medicine or Nephrology—would have another chance to take it again 2 years later if they were unsuccessful, even if they were due to pass the exam that year. Based on feedback ABIM received from the physician community, this feature is now being extended to include all other Internal Medicine subspecialties in the future. Therefore, if a physician opts to take the Knowledge Check-In the first year it is offered in their subspecialty and is unsuccessful, they will get at least one additional opportunity to take it 2 years later.
For more information visit www.abim.org/checkin.
In 2018, ABIM is introducing the new Knowledge Check-In assessment option, an every-2-year assessment option serving as an alternative to the 10-year assessment model. Initially, for 2018, this option will be piloted for both Internal Medicine and Nephrology. In 2019, the Knowledge Check-In will expand to several additional specialties, including Pulmonary Disease. The remaining specialties, including Critical Care Medicine, will become available in 2020.
Previously, ABIM announced that physicians taking the Knowledge Check-In in 2018—the initial year it is offered in Internal Medicine or Nephrology—would have another chance to take it again 2 years later if they were unsuccessful, even if they were due to pass the exam that year. Based on feedback ABIM received from the physician community, this feature is now being extended to include all other Internal Medicine subspecialties in the future. Therefore, if a physician opts to take the Knowledge Check-In the first year it is offered in their subspecialty and is unsuccessful, they will get at least one additional opportunity to take it 2 years later.
For more information visit www.abim.org/checkin.
New strategic plan for CHEST
We are pleased to announce the completion of a new, multiyear strategic plan for CHEST. Over the past few years, key stakeholders have provided essential input, resulting in a plan that identifies a very focused set of priorities we’ll pursue to help achieve our overarching strategy. Having selected these priorities, which leverage our strengths and strategic advantages, we are committed to dedicating sufficient resources toward their accomplishment over the next several years.
Each year, the plan will be reviewed and modified to reflect changes to CHEST priorities.
A strategic plan is an important tool for our organization because it truly does focus and direct our efforts and resources. Guided by our 2013-2017 strategic plan, we were able to accomplish the following:
- Developed events, products, and services that produced meaningful education for the CHEST community and generated positive financial margins;
- Optimized our membership model to increase engagement of all clinicians on the health-care team;
- Enhanced our global presence through guideline development and increased educational offerings;
- Launched a new Association Management System (AMS) and made strides to becoming a data-driven organization;
- Built and moved into a new building that enhanced our ability to develop and host courses in the CHEST Innovation, Simulation, and Training Center;
- Increased our visibility through our rebrand as “CHEST”;
- Fostered relationships and collaborated with other organizations to promote lung health through the CHEST Foundation; and
- Met our budget goals and financial covenants with our bank, and increased the CHEST Foundation’s corpus for grants and awards.
This new strategic plan can be found on chestnet.org under the “About” section. As members of CHEST, we invite you to review what’s outlined and become familiar with what the plan encompasses. This plan provides details to help you understand the future direction of CHEST, and we know you’ll support us in these important endeavors.
We are pleased to announce the completion of a new, multiyear strategic plan for CHEST. Over the past few years, key stakeholders have provided essential input, resulting in a plan that identifies a very focused set of priorities we’ll pursue to help achieve our overarching strategy. Having selected these priorities, which leverage our strengths and strategic advantages, we are committed to dedicating sufficient resources toward their accomplishment over the next several years.
Each year, the plan will be reviewed and modified to reflect changes to CHEST priorities.
A strategic plan is an important tool for our organization because it truly does focus and direct our efforts and resources. Guided by our 2013-2017 strategic plan, we were able to accomplish the following:
- Developed events, products, and services that produced meaningful education for the CHEST community and generated positive financial margins;
- Optimized our membership model to increase engagement of all clinicians on the health-care team;
- Enhanced our global presence through guideline development and increased educational offerings;
- Launched a new Association Management System (AMS) and made strides to becoming a data-driven organization;
- Built and moved into a new building that enhanced our ability to develop and host courses in the CHEST Innovation, Simulation, and Training Center;
- Increased our visibility through our rebrand as “CHEST”;
- Fostered relationships and collaborated with other organizations to promote lung health through the CHEST Foundation; and
- Met our budget goals and financial covenants with our bank, and increased the CHEST Foundation’s corpus for grants and awards.
This new strategic plan can be found on chestnet.org under the “About” section. As members of CHEST, we invite you to review what’s outlined and become familiar with what the plan encompasses. This plan provides details to help you understand the future direction of CHEST, and we know you’ll support us in these important endeavors.
We are pleased to announce the completion of a new, multiyear strategic plan for CHEST. Over the past few years, key stakeholders have provided essential input, resulting in a plan that identifies a very focused set of priorities we’ll pursue to help achieve our overarching strategy. Having selected these priorities, which leverage our strengths and strategic advantages, we are committed to dedicating sufficient resources toward their accomplishment over the next several years.
Each year, the plan will be reviewed and modified to reflect changes to CHEST priorities.
A strategic plan is an important tool for our organization because it truly does focus and direct our efforts and resources. Guided by our 2013-2017 strategic plan, we were able to accomplish the following:
- Developed events, products, and services that produced meaningful education for the CHEST community and generated positive financial margins;
- Optimized our membership model to increase engagement of all clinicians on the health-care team;
- Enhanced our global presence through guideline development and increased educational offerings;
- Launched a new Association Management System (AMS) and made strides to becoming a data-driven organization;
- Built and moved into a new building that enhanced our ability to develop and host courses in the CHEST Innovation, Simulation, and Training Center;
- Increased our visibility through our rebrand as “CHEST”;
- Fostered relationships and collaborated with other organizations to promote lung health through the CHEST Foundation; and
- Met our budget goals and financial covenants with our bank, and increased the CHEST Foundation’s corpus for grants and awards.
This new strategic plan can be found on chestnet.org under the “About” section. As members of CHEST, we invite you to review what’s outlined and become familiar with what the plan encompasses. This plan provides details to help you understand the future direction of CHEST, and we know you’ll support us in these important endeavors.