User login
About ABIM’s Longitudinal Knowledge Assessment
Physicians from every specialty have stepped up in extraordinary ways during the pandemic; however, ABIM recognizes that pulmonary disease and critical care physicians, along with hospitalists and infectious disease specialists, have been especially burdened. ABIM has heard from many pulmonary disease and critical care medicine physicians asking for greater flexibility and choice in how they can maintain their board certifications.
For that reason, ABIM has extended deadlines for all Maintenance of Certification (MOC) requirements to 12/31/22 and to 2023 for Critical Care Medicine, Hospital Medicine, Infectious Disease, and Pulmonary Disease.
What assessment options does ABIM offer?
If you haven’t needed to take an MOC exam for a while, you might not be aware of ABIM’s current options and how they might work for you:
- The traditional, 10-year MOC assessment (a point-in-time exam taken at a test center)
- The new Longitudinal Knowledge Assessment (LKATM) (available in 12 specialties including Internal Medicine and Sleep Medicine now, and in Critical Care Medicine and Pulmonary Disease in 2023)
The 2-year Knowledge Check-In was retired at the end of 2021 with the introduction of the LKA.
How the new LKA works
As a longitudinal assessment, the LKA is designed to help you measure your medical knowledge over time and better melds assessment and learning. It consists of a 5-year cycle, during which you’ll be offered 30 questions each quarter, and need to open at least 500 out of 600 questions to meet the LKA Participation Requirement. You can choose not to open up to 100 questions over 5 years, allowing you to take breaks when you need them.
Once enrolled, you can take questions on your laptop, desktop, or smartphone. You’ll also be able to answer questions where and when it’s convenient for you, such as at your home or office – with no need to schedule an appointment or go to a test center. You can use all the same resources you use in practice – journals, apps, and your own personal notes—anything except another person. For most questions, you’ll find out immediately if your answer was correct or not, and you’ll receive a rationale explaining why, along with one or more references.
You’ll have 4 minutes to answer each question and can add extra time if needed by drawing from an annual 30-minute time bank. For each correct answer, you’ll earn 0.2 MOC points, and if you choose to participate in LKA for more than one of your certificates, you’ll have even more opportunities to earn points. In addition, beginning in your second year of participation, interim score reports will give you helpful information to let you know how you’re doing, so you can re-adjust your approach and focus your studies as needed. A pass/fail decision is made at the end of the 5-year cycle.
About eligibility
If you are currently certified in Critical Care Medicine or Pulmonary Disease and had an assessment due in 2020, 2021 or 2022, you don’t need to take an assessment this year and will be eligible to enroll in the LKA in 2023, or you can choose to take the traditional 10-year MOC exam.
Upon enrolling, you will continue to be reported as “Certified” as long as you are meeting the LKA Participation Requirement. If your next assessment isn’t due for a while, you will be able to enroll in the LKA in your assessment due year—not before then.
More information about eligibility can be found in a special section of ABIM’s website.
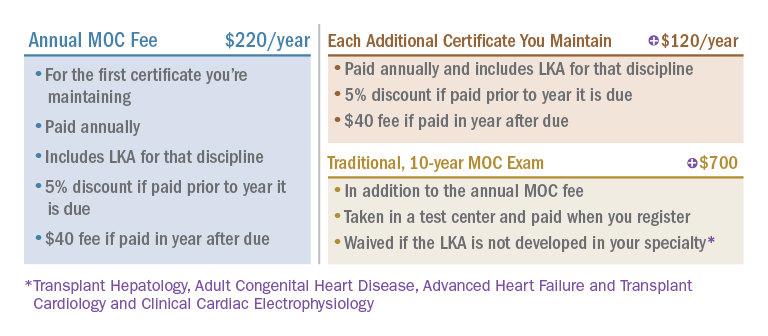
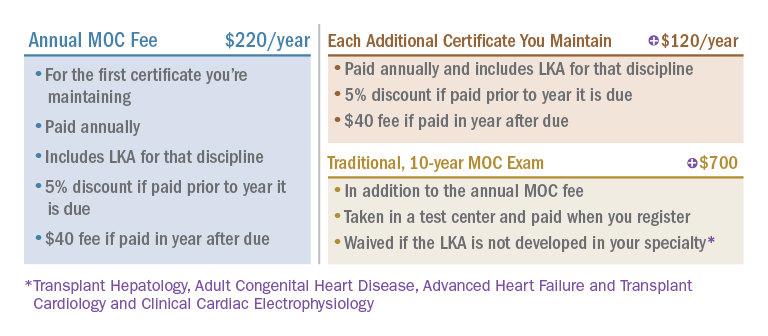
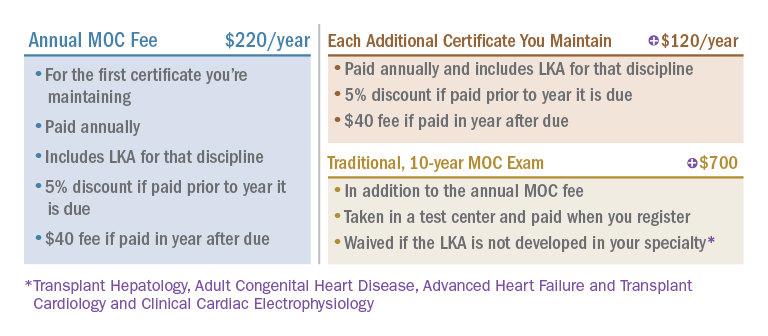
How much does it cost?
ABIM revised its MOC fees in 2022 to provide an option to pay less over time than previously, and the LKA will be included in your annual MOC fee at no additional cost. Here’s how it works:
In closing
Thousands of physicians have already started taking the LKA in 2022 and are reporting positive experiences with it. The ABIM is excited that physicians in additional disciplines, including Critical Care Medicine and Pulmonary Disease, will get to experience it themselves in 2023.
Physicians from every specialty have stepped up in extraordinary ways during the pandemic; however, ABIM recognizes that pulmonary disease and critical care physicians, along with hospitalists and infectious disease specialists, have been especially burdened. ABIM has heard from many pulmonary disease and critical care medicine physicians asking for greater flexibility and choice in how they can maintain their board certifications.
For that reason, ABIM has extended deadlines for all Maintenance of Certification (MOC) requirements to 12/31/22 and to 2023 for Critical Care Medicine, Hospital Medicine, Infectious Disease, and Pulmonary Disease.
What assessment options does ABIM offer?
If you haven’t needed to take an MOC exam for a while, you might not be aware of ABIM’s current options and how they might work for you:
- The traditional, 10-year MOC assessment (a point-in-time exam taken at a test center)
- The new Longitudinal Knowledge Assessment (LKATM) (available in 12 specialties including Internal Medicine and Sleep Medicine now, and in Critical Care Medicine and Pulmonary Disease in 2023)
The 2-year Knowledge Check-In was retired at the end of 2021 with the introduction of the LKA.
How the new LKA works
As a longitudinal assessment, the LKA is designed to help you measure your medical knowledge over time and better melds assessment and learning. It consists of a 5-year cycle, during which you’ll be offered 30 questions each quarter, and need to open at least 500 out of 600 questions to meet the LKA Participation Requirement. You can choose not to open up to 100 questions over 5 years, allowing you to take breaks when you need them.
Once enrolled, you can take questions on your laptop, desktop, or smartphone. You’ll also be able to answer questions where and when it’s convenient for you, such as at your home or office – with no need to schedule an appointment or go to a test center. You can use all the same resources you use in practice – journals, apps, and your own personal notes—anything except another person. For most questions, you’ll find out immediately if your answer was correct or not, and you’ll receive a rationale explaining why, along with one or more references.
You’ll have 4 minutes to answer each question and can add extra time if needed by drawing from an annual 30-minute time bank. For each correct answer, you’ll earn 0.2 MOC points, and if you choose to participate in LKA for more than one of your certificates, you’ll have even more opportunities to earn points. In addition, beginning in your second year of participation, interim score reports will give you helpful information to let you know how you’re doing, so you can re-adjust your approach and focus your studies as needed. A pass/fail decision is made at the end of the 5-year cycle.
About eligibility
If you are currently certified in Critical Care Medicine or Pulmonary Disease and had an assessment due in 2020, 2021 or 2022, you don’t need to take an assessment this year and will be eligible to enroll in the LKA in 2023, or you can choose to take the traditional 10-year MOC exam.
Upon enrolling, you will continue to be reported as “Certified” as long as you are meeting the LKA Participation Requirement. If your next assessment isn’t due for a while, you will be able to enroll in the LKA in your assessment due year—not before then.
More information about eligibility can be found in a special section of ABIM’s website.
How much does it cost?
ABIM revised its MOC fees in 2022 to provide an option to pay less over time than previously, and the LKA will be included in your annual MOC fee at no additional cost. Here’s how it works:
In closing
Thousands of physicians have already started taking the LKA in 2022 and are reporting positive experiences with it. The ABIM is excited that physicians in additional disciplines, including Critical Care Medicine and Pulmonary Disease, will get to experience it themselves in 2023.
Physicians from every specialty have stepped up in extraordinary ways during the pandemic; however, ABIM recognizes that pulmonary disease and critical care physicians, along with hospitalists and infectious disease specialists, have been especially burdened. ABIM has heard from many pulmonary disease and critical care medicine physicians asking for greater flexibility and choice in how they can maintain their board certifications.
For that reason, ABIM has extended deadlines for all Maintenance of Certification (MOC) requirements to 12/31/22 and to 2023 for Critical Care Medicine, Hospital Medicine, Infectious Disease, and Pulmonary Disease.
What assessment options does ABIM offer?
If you haven’t needed to take an MOC exam for a while, you might not be aware of ABIM’s current options and how they might work for you:
- The traditional, 10-year MOC assessment (a point-in-time exam taken at a test center)
- The new Longitudinal Knowledge Assessment (LKATM) (available in 12 specialties including Internal Medicine and Sleep Medicine now, and in Critical Care Medicine and Pulmonary Disease in 2023)
The 2-year Knowledge Check-In was retired at the end of 2021 with the introduction of the LKA.
How the new LKA works
As a longitudinal assessment, the LKA is designed to help you measure your medical knowledge over time and better melds assessment and learning. It consists of a 5-year cycle, during which you’ll be offered 30 questions each quarter, and need to open at least 500 out of 600 questions to meet the LKA Participation Requirement. You can choose not to open up to 100 questions over 5 years, allowing you to take breaks when you need them.
Once enrolled, you can take questions on your laptop, desktop, or smartphone. You’ll also be able to answer questions where and when it’s convenient for you, such as at your home or office – with no need to schedule an appointment or go to a test center. You can use all the same resources you use in practice – journals, apps, and your own personal notes—anything except another person. For most questions, you’ll find out immediately if your answer was correct or not, and you’ll receive a rationale explaining why, along with one or more references.
You’ll have 4 minutes to answer each question and can add extra time if needed by drawing from an annual 30-minute time bank. For each correct answer, you’ll earn 0.2 MOC points, and if you choose to participate in LKA for more than one of your certificates, you’ll have even more opportunities to earn points. In addition, beginning in your second year of participation, interim score reports will give you helpful information to let you know how you’re doing, so you can re-adjust your approach and focus your studies as needed. A pass/fail decision is made at the end of the 5-year cycle.
About eligibility
If you are currently certified in Critical Care Medicine or Pulmonary Disease and had an assessment due in 2020, 2021 or 2022, you don’t need to take an assessment this year and will be eligible to enroll in the LKA in 2023, or you can choose to take the traditional 10-year MOC exam.
Upon enrolling, you will continue to be reported as “Certified” as long as you are meeting the LKA Participation Requirement. If your next assessment isn’t due for a while, you will be able to enroll in the LKA in your assessment due year—not before then.
More information about eligibility can be found in a special section of ABIM’s website.
How much does it cost?
ABIM revised its MOC fees in 2022 to provide an option to pay less over time than previously, and the LKA will be included in your annual MOC fee at no additional cost. Here’s how it works:
In closing
Thousands of physicians have already started taking the LKA in 2022 and are reporting positive experiences with it. The ABIM is excited that physicians in additional disciplines, including Critical Care Medicine and Pulmonary Disease, will get to experience it themselves in 2023.
Patients need Sep-1: Why don’t some doctors like it?
Since its inception, the CMS Sep-1 Core Quality Measure has been unpopular in some circles. It is now under official attack by the American College of Emergency Physicians (ACEP) and the Infectious Diseases Society of America (IDSA), along with a handful of smaller professional societies. These societies appealed the National Quality Forum’s (NQF) 2021 recommendation that the measure be renewed. The NQF is the multidisciplinary and broadly representative group of evaluators who evaluate proposals for CMS-sponsored quality improvement on behalf of the American people and of the Centers for Medicare & Medicaid Services (CMS). Readers of CHEST Physician are likely familiar with core measures, in general, and with Sep-1, in particular. CMS requires hospitals to publicly report their compliance with several Core Quality Measures, and the failure to do so results in across the board reductions in Medicare payments. As of now, no penalties are levied for the degree of compliance but only for failure to report the degree of compliance.
The measure asks, in the main, for hospitals to perform what most physicians can agree should be standard care for patients with sepsis. Depending on whether shock is present, the measure requires:
1. Blood cultures before antibiotics
2. Antibiotics within 3 hours of recognition of sepsis
3. Serum lactate measurement in the first 3 hours and, if increased, a repeat measurement by 6 hours
4. If the patient is hypotensive, 30 mL/kg IV crystalloid within 3 hours, or documentation of why that is not appropriate for the patient
5. If hypotension persists, vasopressors within 6 hours
6. Repeat cardiovascular assessment within 6 hours for patients with shock
If I evaluate these criteria as a patient who has been hospitalized for a serious infection, which I am, they do not seem particularly stringent. In fact, as a patient, I would want my doctors and nurses to act substantially faster than this if I had sepsis or septic shock. If my doctor did not come back in less than 6 hours to check on my shock status, I would be disappointed, to say the least. Nevertheless, some physicians and professional societies see no reason why these should be standards and state that the data underlying them are of low quality. Meanwhile, according to CMS’ own careful evaluation, national compliance with the measures is less than 50%, while being compliant with the measures reduces absolute overall mortality by approximately 4%, from 26.3% to 22.2% (Townsend SR et al. Chest. 2022;161[2]:392-406). This would translate to between 14,000 and 15,000 fewer patients dying from sepsis per year, if all patients received bundled, measure-compliant care. These are patients I don’t care to ignore.
ACEP and IDSA point specifically to the new Surviving Sepsis Campaign Guidelines (SSC) recommendations as evidence that the antibiotic measure is based on low quality evidence (Evans L et al. Crit Care Med. 2021;49[11]:1974-82). In this regard, they are technically correct; the system of evidence review that the SSC panel uses, Grading of Assessment, Recommendations, and Evaluation (GRADE), considers that retrospective analyses, which nearly all of these studies are, can be graded no higher than low quality. Clearly, retrospective studies will never achieve the level of certainty that we achieve with randomized controlled trials, but the NQF, itself, typically views that when a number of well-performed retrospective studies point in the same direction, the level of evidence is at least moderate. After all, just as it would be inappropriate to randomize participants to decades of smoking vs nonsmoking in order prove that smoking causes lung cancer, it is not appropriate to randomize patients with sepsis to receive delayed antibiotics before we accept that such delays are harmful to them.
ACEP and IDSA also assert that the association of early antibiotics with survival is “stronger” for septic shock than for sepsis. In fact, the association is quite strong for both severities of illness. Until it progresses to septic shock, the expected mortality of sepsis is lower, and the percent reduction in mortality is less than for septic shock. However, the opportunity for lives preserved is quite large, because the number of patients with sepsis at presentation is approximately 10 times higher than the number with septic shock at presentation. Antibiotic delays are also associated with progression from infection or sepsis to septic shock (Whiles BB et al. Crit Care Med. 2017;45[4]:623-29; Bisarya R et al. Chest. 2022;161[1]:112-20). Importantly, SSC gave a strong recommendation for all patients with suspected sepsis to receive antibiotics within 3 hours of suspecting sepsis and within 1 hour of suspecting septic shock, a recommendation even stronger than that of Sep-1.
Critics opine that CMS should stop looking at the process measures and focus only on the outcomes of sepsis care. There is a certain attractiveness to this proposition. One could say that it does not matter so much how a hospital achieves lower mortality as long as they do achieve it. However, the question would then become – how low should the mortality rate be? I have a notion that whatever the number, the Sep-1 critics would find it unbearable.
There is a core principle embedded in the Sep-1 process measures, in SSC guidelines, and in the concept of early goal-directed therapy that preceded them: success is not dependent only on what we do but on when we do it. All of you have experienced this. Each of you has attended a professional school, whether medical, nursing, respiratory therapy, etc. None of you showed up unannounced on opening day of the semester and was admitted to that school. All of you garnered the grades, solicited the letters of recommendation, took the entrance exams, and submitted an application. Some of you went to an interview. All of these things were done in a timely fashion; professional schools do not accept incomplete applications or late applications. Doing the right things at the wrong time would have left us all pursuing different careers.
Very early in my career as an attending physician in the ICU, I found myself exasperated by the circumstances of many patients who we received in the ICU with sepsis. I would peruse their medical records and find that they had been septic, ie, had met criteria for severe sepsis, 1 to 2 days before their deterioration to septic shock, yet they had not been diagnosed with sepsis until shock developed. In the ICU, we began resuscitative fluids, ensured appropriate antibiotics, and started vasopressors, but it was often to no avail. The treatments we gave made no difference for many patients, because they were given too late. For me, this was career altering; much of my career since that time has focused on teaching medical personnel how to recognize sepsis, how to give timely and appropriate treatments, and how to keep the data to show when they have done that and when they have not.
Before Sep-1 many, if not most, of the hospitals in the United States had no particular strategy in place to recognize and treat patients with sepsis, even though it was and is the most common cause of death and the costliest condition in American hospitals. Now, most hospitals do have such strategies. Assertions by professional societies that it is difficult to collect the data for Sep-1 reporting are likely true. However, keeping patients safe and alive is a hospital’s primary reason for existing. As long as hospitals are tracking each antibiotic and every liter of fluid so that they can bill for them, my own ears are deaf to hearing that it is too difficult to make sure that we are doing our job. Modifying or eliminating Sep-1 for any reason except data that show we can clearly further improve the outcome for all patients with sepsis is the wrong move to make. So far, other professional societies want to remove elements of Sep-1 without evidence that it would improve our care for patients with sepsis or their outcomes. Thankfully, from the time we proposed the first criteria for diagnosing sepsis, CHEST has promoted what is best for patients, whether it is difficult or not.
Dr. Simpson is a pulmonologist and intensivist with an extensive background in sepsis and in critical care quality improvement, including by serving as a senior adviser to the Solving Sepsis initiative of the Biomedical Advanced Research and Development Authority (BARDA) of the U.S. Department of Health and Human Services and an author of the 2016 and 2020 updates of the Surviving Sepsis Campaign Guidelines. Dr. Simpson is the senior medical adviser for Sepsis Alliance, a nationwide patient information and advocacy organization. He is the immediate past president of CHEST.
Since its inception, the CMS Sep-1 Core Quality Measure has been unpopular in some circles. It is now under official attack by the American College of Emergency Physicians (ACEP) and the Infectious Diseases Society of America (IDSA), along with a handful of smaller professional societies. These societies appealed the National Quality Forum’s (NQF) 2021 recommendation that the measure be renewed. The NQF is the multidisciplinary and broadly representative group of evaluators who evaluate proposals for CMS-sponsored quality improvement on behalf of the American people and of the Centers for Medicare & Medicaid Services (CMS). Readers of CHEST Physician are likely familiar with core measures, in general, and with Sep-1, in particular. CMS requires hospitals to publicly report their compliance with several Core Quality Measures, and the failure to do so results in across the board reductions in Medicare payments. As of now, no penalties are levied for the degree of compliance but only for failure to report the degree of compliance.
The measure asks, in the main, for hospitals to perform what most physicians can agree should be standard care for patients with sepsis. Depending on whether shock is present, the measure requires:
1. Blood cultures before antibiotics
2. Antibiotics within 3 hours of recognition of sepsis
3. Serum lactate measurement in the first 3 hours and, if increased, a repeat measurement by 6 hours
4. If the patient is hypotensive, 30 mL/kg IV crystalloid within 3 hours, or documentation of why that is not appropriate for the patient
5. If hypotension persists, vasopressors within 6 hours
6. Repeat cardiovascular assessment within 6 hours for patients with shock
If I evaluate these criteria as a patient who has been hospitalized for a serious infection, which I am, they do not seem particularly stringent. In fact, as a patient, I would want my doctors and nurses to act substantially faster than this if I had sepsis or septic shock. If my doctor did not come back in less than 6 hours to check on my shock status, I would be disappointed, to say the least. Nevertheless, some physicians and professional societies see no reason why these should be standards and state that the data underlying them are of low quality. Meanwhile, according to CMS’ own careful evaluation, national compliance with the measures is less than 50%, while being compliant with the measures reduces absolute overall mortality by approximately 4%, from 26.3% to 22.2% (Townsend SR et al. Chest. 2022;161[2]:392-406). This would translate to between 14,000 and 15,000 fewer patients dying from sepsis per year, if all patients received bundled, measure-compliant care. These are patients I don’t care to ignore.
ACEP and IDSA point specifically to the new Surviving Sepsis Campaign Guidelines (SSC) recommendations as evidence that the antibiotic measure is based on low quality evidence (Evans L et al. Crit Care Med. 2021;49[11]:1974-82). In this regard, they are technically correct; the system of evidence review that the SSC panel uses, Grading of Assessment, Recommendations, and Evaluation (GRADE), considers that retrospective analyses, which nearly all of these studies are, can be graded no higher than low quality. Clearly, retrospective studies will never achieve the level of certainty that we achieve with randomized controlled trials, but the NQF, itself, typically views that when a number of well-performed retrospective studies point in the same direction, the level of evidence is at least moderate. After all, just as it would be inappropriate to randomize participants to decades of smoking vs nonsmoking in order prove that smoking causes lung cancer, it is not appropriate to randomize patients with sepsis to receive delayed antibiotics before we accept that such delays are harmful to them.
ACEP and IDSA also assert that the association of early antibiotics with survival is “stronger” for septic shock than for sepsis. In fact, the association is quite strong for both severities of illness. Until it progresses to septic shock, the expected mortality of sepsis is lower, and the percent reduction in mortality is less than for septic shock. However, the opportunity for lives preserved is quite large, because the number of patients with sepsis at presentation is approximately 10 times higher than the number with septic shock at presentation. Antibiotic delays are also associated with progression from infection or sepsis to septic shock (Whiles BB et al. Crit Care Med. 2017;45[4]:623-29; Bisarya R et al. Chest. 2022;161[1]:112-20). Importantly, SSC gave a strong recommendation for all patients with suspected sepsis to receive antibiotics within 3 hours of suspecting sepsis and within 1 hour of suspecting septic shock, a recommendation even stronger than that of Sep-1.
Critics opine that CMS should stop looking at the process measures and focus only on the outcomes of sepsis care. There is a certain attractiveness to this proposition. One could say that it does not matter so much how a hospital achieves lower mortality as long as they do achieve it. However, the question would then become – how low should the mortality rate be? I have a notion that whatever the number, the Sep-1 critics would find it unbearable.
There is a core principle embedded in the Sep-1 process measures, in SSC guidelines, and in the concept of early goal-directed therapy that preceded them: success is not dependent only on what we do but on when we do it. All of you have experienced this. Each of you has attended a professional school, whether medical, nursing, respiratory therapy, etc. None of you showed up unannounced on opening day of the semester and was admitted to that school. All of you garnered the grades, solicited the letters of recommendation, took the entrance exams, and submitted an application. Some of you went to an interview. All of these things were done in a timely fashion; professional schools do not accept incomplete applications or late applications. Doing the right things at the wrong time would have left us all pursuing different careers.
Very early in my career as an attending physician in the ICU, I found myself exasperated by the circumstances of many patients who we received in the ICU with sepsis. I would peruse their medical records and find that they had been septic, ie, had met criteria for severe sepsis, 1 to 2 days before their deterioration to septic shock, yet they had not been diagnosed with sepsis until shock developed. In the ICU, we began resuscitative fluids, ensured appropriate antibiotics, and started vasopressors, but it was often to no avail. The treatments we gave made no difference for many patients, because they were given too late. For me, this was career altering; much of my career since that time has focused on teaching medical personnel how to recognize sepsis, how to give timely and appropriate treatments, and how to keep the data to show when they have done that and when they have not.
Before Sep-1 many, if not most, of the hospitals in the United States had no particular strategy in place to recognize and treat patients with sepsis, even though it was and is the most common cause of death and the costliest condition in American hospitals. Now, most hospitals do have such strategies. Assertions by professional societies that it is difficult to collect the data for Sep-1 reporting are likely true. However, keeping patients safe and alive is a hospital’s primary reason for existing. As long as hospitals are tracking each antibiotic and every liter of fluid so that they can bill for them, my own ears are deaf to hearing that it is too difficult to make sure that we are doing our job. Modifying or eliminating Sep-1 for any reason except data that show we can clearly further improve the outcome for all patients with sepsis is the wrong move to make. So far, other professional societies want to remove elements of Sep-1 without evidence that it would improve our care for patients with sepsis or their outcomes. Thankfully, from the time we proposed the first criteria for diagnosing sepsis, CHEST has promoted what is best for patients, whether it is difficult or not.
Dr. Simpson is a pulmonologist and intensivist with an extensive background in sepsis and in critical care quality improvement, including by serving as a senior adviser to the Solving Sepsis initiative of the Biomedical Advanced Research and Development Authority (BARDA) of the U.S. Department of Health and Human Services and an author of the 2016 and 2020 updates of the Surviving Sepsis Campaign Guidelines. Dr. Simpson is the senior medical adviser for Sepsis Alliance, a nationwide patient information and advocacy organization. He is the immediate past president of CHEST.
Since its inception, the CMS Sep-1 Core Quality Measure has been unpopular in some circles. It is now under official attack by the American College of Emergency Physicians (ACEP) and the Infectious Diseases Society of America (IDSA), along with a handful of smaller professional societies. These societies appealed the National Quality Forum’s (NQF) 2021 recommendation that the measure be renewed. The NQF is the multidisciplinary and broadly representative group of evaluators who evaluate proposals for CMS-sponsored quality improvement on behalf of the American people and of the Centers for Medicare & Medicaid Services (CMS). Readers of CHEST Physician are likely familiar with core measures, in general, and with Sep-1, in particular. CMS requires hospitals to publicly report their compliance with several Core Quality Measures, and the failure to do so results in across the board reductions in Medicare payments. As of now, no penalties are levied for the degree of compliance but only for failure to report the degree of compliance.
The measure asks, in the main, for hospitals to perform what most physicians can agree should be standard care for patients with sepsis. Depending on whether shock is present, the measure requires:
1. Blood cultures before antibiotics
2. Antibiotics within 3 hours of recognition of sepsis
3. Serum lactate measurement in the first 3 hours and, if increased, a repeat measurement by 6 hours
4. If the patient is hypotensive, 30 mL/kg IV crystalloid within 3 hours, or documentation of why that is not appropriate for the patient
5. If hypotension persists, vasopressors within 6 hours
6. Repeat cardiovascular assessment within 6 hours for patients with shock
If I evaluate these criteria as a patient who has been hospitalized for a serious infection, which I am, they do not seem particularly stringent. In fact, as a patient, I would want my doctors and nurses to act substantially faster than this if I had sepsis or septic shock. If my doctor did not come back in less than 6 hours to check on my shock status, I would be disappointed, to say the least. Nevertheless, some physicians and professional societies see no reason why these should be standards and state that the data underlying them are of low quality. Meanwhile, according to CMS’ own careful evaluation, national compliance with the measures is less than 50%, while being compliant with the measures reduces absolute overall mortality by approximately 4%, from 26.3% to 22.2% (Townsend SR et al. Chest. 2022;161[2]:392-406). This would translate to between 14,000 and 15,000 fewer patients dying from sepsis per year, if all patients received bundled, measure-compliant care. These are patients I don’t care to ignore.
ACEP and IDSA point specifically to the new Surviving Sepsis Campaign Guidelines (SSC) recommendations as evidence that the antibiotic measure is based on low quality evidence (Evans L et al. Crit Care Med. 2021;49[11]:1974-82). In this regard, they are technically correct; the system of evidence review that the SSC panel uses, Grading of Assessment, Recommendations, and Evaluation (GRADE), considers that retrospective analyses, which nearly all of these studies are, can be graded no higher than low quality. Clearly, retrospective studies will never achieve the level of certainty that we achieve with randomized controlled trials, but the NQF, itself, typically views that when a number of well-performed retrospective studies point in the same direction, the level of evidence is at least moderate. After all, just as it would be inappropriate to randomize participants to decades of smoking vs nonsmoking in order prove that smoking causes lung cancer, it is not appropriate to randomize patients with sepsis to receive delayed antibiotics before we accept that such delays are harmful to them.
ACEP and IDSA also assert that the association of early antibiotics with survival is “stronger” for septic shock than for sepsis. In fact, the association is quite strong for both severities of illness. Until it progresses to septic shock, the expected mortality of sepsis is lower, and the percent reduction in mortality is less than for septic shock. However, the opportunity for lives preserved is quite large, because the number of patients with sepsis at presentation is approximately 10 times higher than the number with septic shock at presentation. Antibiotic delays are also associated with progression from infection or sepsis to septic shock (Whiles BB et al. Crit Care Med. 2017;45[4]:623-29; Bisarya R et al. Chest. 2022;161[1]:112-20). Importantly, SSC gave a strong recommendation for all patients with suspected sepsis to receive antibiotics within 3 hours of suspecting sepsis and within 1 hour of suspecting septic shock, a recommendation even stronger than that of Sep-1.
Critics opine that CMS should stop looking at the process measures and focus only on the outcomes of sepsis care. There is a certain attractiveness to this proposition. One could say that it does not matter so much how a hospital achieves lower mortality as long as they do achieve it. However, the question would then become – how low should the mortality rate be? I have a notion that whatever the number, the Sep-1 critics would find it unbearable.
There is a core principle embedded in the Sep-1 process measures, in SSC guidelines, and in the concept of early goal-directed therapy that preceded them: success is not dependent only on what we do but on when we do it. All of you have experienced this. Each of you has attended a professional school, whether medical, nursing, respiratory therapy, etc. None of you showed up unannounced on opening day of the semester and was admitted to that school. All of you garnered the grades, solicited the letters of recommendation, took the entrance exams, and submitted an application. Some of you went to an interview. All of these things were done in a timely fashion; professional schools do not accept incomplete applications or late applications. Doing the right things at the wrong time would have left us all pursuing different careers.
Very early in my career as an attending physician in the ICU, I found myself exasperated by the circumstances of many patients who we received in the ICU with sepsis. I would peruse their medical records and find that they had been septic, ie, had met criteria for severe sepsis, 1 to 2 days before their deterioration to septic shock, yet they had not been diagnosed with sepsis until shock developed. In the ICU, we began resuscitative fluids, ensured appropriate antibiotics, and started vasopressors, but it was often to no avail. The treatments we gave made no difference for many patients, because they were given too late. For me, this was career altering; much of my career since that time has focused on teaching medical personnel how to recognize sepsis, how to give timely and appropriate treatments, and how to keep the data to show when they have done that and when they have not.
Before Sep-1 many, if not most, of the hospitals in the United States had no particular strategy in place to recognize and treat patients with sepsis, even though it was and is the most common cause of death and the costliest condition in American hospitals. Now, most hospitals do have such strategies. Assertions by professional societies that it is difficult to collect the data for Sep-1 reporting are likely true. However, keeping patients safe and alive is a hospital’s primary reason for existing. As long as hospitals are tracking each antibiotic and every liter of fluid so that they can bill for them, my own ears are deaf to hearing that it is too difficult to make sure that we are doing our job. Modifying or eliminating Sep-1 for any reason except data that show we can clearly further improve the outcome for all patients with sepsis is the wrong move to make. So far, other professional societies want to remove elements of Sep-1 without evidence that it would improve our care for patients with sepsis or their outcomes. Thankfully, from the time we proposed the first criteria for diagnosing sepsis, CHEST has promoted what is best for patients, whether it is difficult or not.
Dr. Simpson is a pulmonologist and intensivist with an extensive background in sepsis and in critical care quality improvement, including by serving as a senior adviser to the Solving Sepsis initiative of the Biomedical Advanced Research and Development Authority (BARDA) of the U.S. Department of Health and Human Services and an author of the 2016 and 2020 updates of the Surviving Sepsis Campaign Guidelines. Dr. Simpson is the senior medical adviser for Sepsis Alliance, a nationwide patient information and advocacy organization. He is the immediate past president of CHEST.
CHEST in the news
CHEST works to provide opportunities for members to serve as expert sources for both mainstream and trade media to create a stronger voice for members in pulmonary, critical care, and sleep medicine.
Below are media coverage highlights from the past few months that work to expand awareness of CHEST and to promote the expertise of CHEST members in the media.
Improving NIV access for patients with COPD
In December, Pulmonology Advisor covered recommendations from the noninvasive ventilation Technical Expert Panel report published in the journal CHEST® by The American College of Chest Physicians, the American Association for Respiratory Care, the American Academy of Sleep Medicine, and the American Thoracic Society.
The article shares that, in the United States, patients with COPD are often prescribed home mechanical ventilators rather than more appropriate devices, due largely to current Centers for Medicare & Medicaid Services (CMS) policies that do not always take into account unique complexities of patients’ conditions.
In addition to the recommendations covered in Optimal NIV Medicare Access Promotion: Patients With COPD, the Technical Expert Panel also published reports on patients with Obstructive Sleep Apnea, patients with Central Sleep Apnea, patients with Hypoventilation Syndromes, and patients with Thoracic Restrictive Disorders in the journal CHEST.
The full article, Expert Panel Guidelines Promote Access to In-Home NIV for Patients With COPD, can be found on the Pulmonology Advisor website.
OSA and cardiovascular mortality
A journal CHEST® article, “A Validation Study of Four Different Cluster Analyses of OSA and the Incidence of Cardiovascular Mortality in a Hispanic Population,” by Gonzalo Labarca, MD, et al. was featured in a Healio Pulmonology article.
The research showed an association between excessive sleepiness and increased risk for cardiovascular mortality in Hispanic adults with moderate to severe Obstructive Sleep Apnea and, in the article, Dr. Labarca says, “The Latino population is underrepresented in the scientific literature. Therefore, validation data regarding novel approaches to better identify a subtype of OSA patients at high risk of CV mortality is strongly needed.”
The full article, Risk for CV Mortality Elevated in Hispanic Adults with OSA, Excessive Sleepiness, can be found on the Healio website.
Member in the news:
Chair of the CHEST COVID-19 Task Force, Ryan Maves, MD , joined New York Times podcast, “The Daily” to discuss how the omicron COVID-19 surge was different than previous surges because unvaccinated deaths are skewing younger. During the podcast, Dr. Maves said, “You know, many more [unvaccinated] people in their 40s and 50s are dying. And it’s a grim feeling, watching people who are your own age and maybe not that much older than you die of an entirely preventable illness.” The full podcast, This COVID Surge Feels Different can be found on the New York Times website.
CHEST news
CHEST regularly issues statements and press releases on a variety of topics, including closing the synthetic nicotine loophole and requests for Congress to extend telehealth services.
For all recent CHEST News, including these statements, visit the CHEST Newsroom at chestnet.org, and follow the hashtag #CHESTNews on Twitter.
If you have been included in a recent news article and would like it to be featured, send the coverage to [email protected].
CHEST works to provide opportunities for members to serve as expert sources for both mainstream and trade media to create a stronger voice for members in pulmonary, critical care, and sleep medicine.
Below are media coverage highlights from the past few months that work to expand awareness of CHEST and to promote the expertise of CHEST members in the media.
Improving NIV access for patients with COPD
In December, Pulmonology Advisor covered recommendations from the noninvasive ventilation Technical Expert Panel report published in the journal CHEST® by The American College of Chest Physicians, the American Association for Respiratory Care, the American Academy of Sleep Medicine, and the American Thoracic Society.
The article shares that, in the United States, patients with COPD are often prescribed home mechanical ventilators rather than more appropriate devices, due largely to current Centers for Medicare & Medicaid Services (CMS) policies that do not always take into account unique complexities of patients’ conditions.
In addition to the recommendations covered in Optimal NIV Medicare Access Promotion: Patients With COPD, the Technical Expert Panel also published reports on patients with Obstructive Sleep Apnea, patients with Central Sleep Apnea, patients with Hypoventilation Syndromes, and patients with Thoracic Restrictive Disorders in the journal CHEST.
The full article, Expert Panel Guidelines Promote Access to In-Home NIV for Patients With COPD, can be found on the Pulmonology Advisor website.
OSA and cardiovascular mortality
A journal CHEST® article, “A Validation Study of Four Different Cluster Analyses of OSA and the Incidence of Cardiovascular Mortality in a Hispanic Population,” by Gonzalo Labarca, MD, et al. was featured in a Healio Pulmonology article.
The research showed an association between excessive sleepiness and increased risk for cardiovascular mortality in Hispanic adults with moderate to severe Obstructive Sleep Apnea and, in the article, Dr. Labarca says, “The Latino population is underrepresented in the scientific literature. Therefore, validation data regarding novel approaches to better identify a subtype of OSA patients at high risk of CV mortality is strongly needed.”
The full article, Risk for CV Mortality Elevated in Hispanic Adults with OSA, Excessive Sleepiness, can be found on the Healio website.
Member in the news:
Chair of the CHEST COVID-19 Task Force, Ryan Maves, MD , joined New York Times podcast, “The Daily” to discuss how the omicron COVID-19 surge was different than previous surges because unvaccinated deaths are skewing younger. During the podcast, Dr. Maves said, “You know, many more [unvaccinated] people in their 40s and 50s are dying. And it’s a grim feeling, watching people who are your own age and maybe not that much older than you die of an entirely preventable illness.” The full podcast, This COVID Surge Feels Different can be found on the New York Times website.
CHEST news
CHEST regularly issues statements and press releases on a variety of topics, including closing the synthetic nicotine loophole and requests for Congress to extend telehealth services.
For all recent CHEST News, including these statements, visit the CHEST Newsroom at chestnet.org, and follow the hashtag #CHESTNews on Twitter.
If you have been included in a recent news article and would like it to be featured, send the coverage to [email protected].
CHEST works to provide opportunities for members to serve as expert sources for both mainstream and trade media to create a stronger voice for members in pulmonary, critical care, and sleep medicine.
Below are media coverage highlights from the past few months that work to expand awareness of CHEST and to promote the expertise of CHEST members in the media.
Improving NIV access for patients with COPD
In December, Pulmonology Advisor covered recommendations from the noninvasive ventilation Technical Expert Panel report published in the journal CHEST® by The American College of Chest Physicians, the American Association for Respiratory Care, the American Academy of Sleep Medicine, and the American Thoracic Society.
The article shares that, in the United States, patients with COPD are often prescribed home mechanical ventilators rather than more appropriate devices, due largely to current Centers for Medicare & Medicaid Services (CMS) policies that do not always take into account unique complexities of patients’ conditions.
In addition to the recommendations covered in Optimal NIV Medicare Access Promotion: Patients With COPD, the Technical Expert Panel also published reports on patients with Obstructive Sleep Apnea, patients with Central Sleep Apnea, patients with Hypoventilation Syndromes, and patients with Thoracic Restrictive Disorders in the journal CHEST.
The full article, Expert Panel Guidelines Promote Access to In-Home NIV for Patients With COPD, can be found on the Pulmonology Advisor website.
OSA and cardiovascular mortality
A journal CHEST® article, “A Validation Study of Four Different Cluster Analyses of OSA and the Incidence of Cardiovascular Mortality in a Hispanic Population,” by Gonzalo Labarca, MD, et al. was featured in a Healio Pulmonology article.
The research showed an association between excessive sleepiness and increased risk for cardiovascular mortality in Hispanic adults with moderate to severe Obstructive Sleep Apnea and, in the article, Dr. Labarca says, “The Latino population is underrepresented in the scientific literature. Therefore, validation data regarding novel approaches to better identify a subtype of OSA patients at high risk of CV mortality is strongly needed.”
The full article, Risk for CV Mortality Elevated in Hispanic Adults with OSA, Excessive Sleepiness, can be found on the Healio website.
Member in the news:
Chair of the CHEST COVID-19 Task Force, Ryan Maves, MD , joined New York Times podcast, “The Daily” to discuss how the omicron COVID-19 surge was different than previous surges because unvaccinated deaths are skewing younger. During the podcast, Dr. Maves said, “You know, many more [unvaccinated] people in their 40s and 50s are dying. And it’s a grim feeling, watching people who are your own age and maybe not that much older than you die of an entirely preventable illness.” The full podcast, This COVID Surge Feels Different can be found on the New York Times website.
CHEST news
CHEST regularly issues statements and press releases on a variety of topics, including closing the synthetic nicotine loophole and requests for Congress to extend telehealth services.
For all recent CHEST News, including these statements, visit the CHEST Newsroom at chestnet.org, and follow the hashtag #CHESTNews on Twitter.
If you have been included in a recent news article and would like it to be featured, send the coverage to [email protected].
Building trust together
During the fall of 2020, the CHEST Foundation launched a Listening Tour in areas of the United States that were experiencing disproportionate incidents and mortality from COVID-19. This program was initiated to gain insights in order toand identify solutions to combat lung health inequities among marginalized communities. The COVID-19 pandemic has exacerbated health disparities in America. Underserved communities, communities with higher rates of poverty, and communities of color have suffered disproportionate rates of illness and mortality due to COVID-19.
Even before the COVID-19 pandemic, underserved communities were impacted disproportionately by four of the most common lung diseases: asthma, chronic obstructive pulmonary diseaseCOPD, interstitial lung disease, and lung cancer. Inequities in care and health outcomes are well documented. Inequities are due to a multitude of factors, including socioeconomic status, environmental issues such as air populationpollution, and issues that impact access to care, such as individuals being uninsured or under insured, and a lack of specialists in underserved communities.
The CHEST Foundation selected Listening Tour cities based on a number of criteria, including documented inequities in lung health and prevalence of the predominant lung diseases. Listening Tour events were held virtually in Jackson, MS; New York, NY; Chicago, IL; South Texas; and the US Southwest. In each location, the CHEST Foundation approached community leaders, clinicians, patients, and families to participate. Individual interviews focused on lung health experiences, positive and negative; needs from clinicians, patients, families, and community leaders; and help actually received (or not) based on these needs.
A theme that emerged centered on the importance trust plays in the patient/clinician relationship. Barriers to the establishment of trust as expressed by patients related to:
- Perceived dismissive attitudes among physicians
- Lack of understanding and/or appreciation about social determinants of health
- Overuse of highly technical/medical terminology that can be intimidating to patients
- General cultural and philosophical differences that may contribute to implicit biases
Gaining trust and building rapport among patients is not only limited to key findings from the Listening Tour but also corroborated through peer- reviewed studies. Many studies have documented that trust is the foundation on which patient/clinician relationshipss are built and without it, patients are less likely to maintain adherence to treatment plans, miss appointments, minimize sharing information about their symptoms, and suffer from poorer health and overall quality of life.
In response, the CHEST Foundation is proposing a project with the aim of broader replication based upon key findings. Building trust and developing rapport with patients areis key in creating an environment where they are active participants in their care. An empathetic care training model will provide clinicians with an understanding of the barriers that exist and the tools needed to establish trust with their patients.
The major components of the project include:
1. Development and standardization of a culturally competent toolkit for use during the first five 5 minutes of clinician/patient encounters
2. Creating Creation of education on the tool and training clinicians that who will pilot the tool in health care clinics/medical institutions and collect data on its impact
3. Implementation of the tool use during clinician/patient visits and data collection
4. Data analysis and synthesis of findings for use in refinement and scalability for broader impact
Future plans include scaling the project to additional sites and health care settings; disseminating the culturally competent tool along with education for its utilization to CHEST’s membership and to a larger audience of health care providers; and sharing results and lessons learned. The CHEST Foundation is hoping to build a national, sustainable program that helps achieve health equity, but in order to achieve this, we need your help. Make a donation, and join the CHEST Foundation as we embark on a bold new initiative to build trust, identify and remove barriers, and promote health care access for all in order to help fight lung disease. Together, we will build trust and understanding within communities, specifically between patients, their families, their caregivers, and their clinicians.
During the fall of 2020, the CHEST Foundation launched a Listening Tour in areas of the United States that were experiencing disproportionate incidents and mortality from COVID-19. This program was initiated to gain insights in order toand identify solutions to combat lung health inequities among marginalized communities. The COVID-19 pandemic has exacerbated health disparities in America. Underserved communities, communities with higher rates of poverty, and communities of color have suffered disproportionate rates of illness and mortality due to COVID-19.
Even before the COVID-19 pandemic, underserved communities were impacted disproportionately by four of the most common lung diseases: asthma, chronic obstructive pulmonary diseaseCOPD, interstitial lung disease, and lung cancer. Inequities in care and health outcomes are well documented. Inequities are due to a multitude of factors, including socioeconomic status, environmental issues such as air populationpollution, and issues that impact access to care, such as individuals being uninsured or under insured, and a lack of specialists in underserved communities.
The CHEST Foundation selected Listening Tour cities based on a number of criteria, including documented inequities in lung health and prevalence of the predominant lung diseases. Listening Tour events were held virtually in Jackson, MS; New York, NY; Chicago, IL; South Texas; and the US Southwest. In each location, the CHEST Foundation approached community leaders, clinicians, patients, and families to participate. Individual interviews focused on lung health experiences, positive and negative; needs from clinicians, patients, families, and community leaders; and help actually received (or not) based on these needs.
A theme that emerged centered on the importance trust plays in the patient/clinician relationship. Barriers to the establishment of trust as expressed by patients related to:
- Perceived dismissive attitudes among physicians
- Lack of understanding and/or appreciation about social determinants of health
- Overuse of highly technical/medical terminology that can be intimidating to patients
- General cultural and philosophical differences that may contribute to implicit biases
Gaining trust and building rapport among patients is not only limited to key findings from the Listening Tour but also corroborated through peer- reviewed studies. Many studies have documented that trust is the foundation on which patient/clinician relationshipss are built and without it, patients are less likely to maintain adherence to treatment plans, miss appointments, minimize sharing information about their symptoms, and suffer from poorer health and overall quality of life.
In response, the CHEST Foundation is proposing a project with the aim of broader replication based upon key findings. Building trust and developing rapport with patients areis key in creating an environment where they are active participants in their care. An empathetic care training model will provide clinicians with an understanding of the barriers that exist and the tools needed to establish trust with their patients.
The major components of the project include:
1. Development and standardization of a culturally competent toolkit for use during the first five 5 minutes of clinician/patient encounters
2. Creating Creation of education on the tool and training clinicians that who will pilot the tool in health care clinics/medical institutions and collect data on its impact
3. Implementation of the tool use during clinician/patient visits and data collection
4. Data analysis and synthesis of findings for use in refinement and scalability for broader impact
Future plans include scaling the project to additional sites and health care settings; disseminating the culturally competent tool along with education for its utilization to CHEST’s membership and to a larger audience of health care providers; and sharing results and lessons learned. The CHEST Foundation is hoping to build a national, sustainable program that helps achieve health equity, but in order to achieve this, we need your help. Make a donation, and join the CHEST Foundation as we embark on a bold new initiative to build trust, identify and remove barriers, and promote health care access for all in order to help fight lung disease. Together, we will build trust and understanding within communities, specifically between patients, their families, their caregivers, and their clinicians.
During the fall of 2020, the CHEST Foundation launched a Listening Tour in areas of the United States that were experiencing disproportionate incidents and mortality from COVID-19. This program was initiated to gain insights in order toand identify solutions to combat lung health inequities among marginalized communities. The COVID-19 pandemic has exacerbated health disparities in America. Underserved communities, communities with higher rates of poverty, and communities of color have suffered disproportionate rates of illness and mortality due to COVID-19.
Even before the COVID-19 pandemic, underserved communities were impacted disproportionately by four of the most common lung diseases: asthma, chronic obstructive pulmonary diseaseCOPD, interstitial lung disease, and lung cancer. Inequities in care and health outcomes are well documented. Inequities are due to a multitude of factors, including socioeconomic status, environmental issues such as air populationpollution, and issues that impact access to care, such as individuals being uninsured or under insured, and a lack of specialists in underserved communities.
The CHEST Foundation selected Listening Tour cities based on a number of criteria, including documented inequities in lung health and prevalence of the predominant lung diseases. Listening Tour events were held virtually in Jackson, MS; New York, NY; Chicago, IL; South Texas; and the US Southwest. In each location, the CHEST Foundation approached community leaders, clinicians, patients, and families to participate. Individual interviews focused on lung health experiences, positive and negative; needs from clinicians, patients, families, and community leaders; and help actually received (or not) based on these needs.
A theme that emerged centered on the importance trust plays in the patient/clinician relationship. Barriers to the establishment of trust as expressed by patients related to:
- Perceived dismissive attitudes among physicians
- Lack of understanding and/or appreciation about social determinants of health
- Overuse of highly technical/medical terminology that can be intimidating to patients
- General cultural and philosophical differences that may contribute to implicit biases
Gaining trust and building rapport among patients is not only limited to key findings from the Listening Tour but also corroborated through peer- reviewed studies. Many studies have documented that trust is the foundation on which patient/clinician relationshipss are built and without it, patients are less likely to maintain adherence to treatment plans, miss appointments, minimize sharing information about their symptoms, and suffer from poorer health and overall quality of life.
In response, the CHEST Foundation is proposing a project with the aim of broader replication based upon key findings. Building trust and developing rapport with patients areis key in creating an environment where they are active participants in their care. An empathetic care training model will provide clinicians with an understanding of the barriers that exist and the tools needed to establish trust with their patients.
The major components of the project include:
1. Development and standardization of a culturally competent toolkit for use during the first five 5 minutes of clinician/patient encounters
2. Creating Creation of education on the tool and training clinicians that who will pilot the tool in health care clinics/medical institutions and collect data on its impact
3. Implementation of the tool use during clinician/patient visits and data collection
4. Data analysis and synthesis of findings for use in refinement and scalability for broader impact
Future plans include scaling the project to additional sites and health care settings; disseminating the culturally competent tool along with education for its utilization to CHEST’s membership and to a larger audience of health care providers; and sharing results and lessons learned. The CHEST Foundation is hoping to build a national, sustainable program that helps achieve health equity, but in order to achieve this, we need your help. Make a donation, and join the CHEST Foundation as we embark on a bold new initiative to build trust, identify and remove barriers, and promote health care access for all in order to help fight lung disease. Together, we will build trust and understanding within communities, specifically between patients, their families, their caregivers, and their clinicians.
Asthma, IPF, mechanical ventilation and more...
Airway disorders network: Asthma and COPD section
Betting on asthma: The over and under of diagnosis
Asthma is one of the major chronic respiratory diseases worldwide (WHO 2020), yet it is a clinical syndrome that lacks a consensus on its definition, is comprised of nonspecific respiratory symptoms, and is without a gold standard diagnostic test or a set guideline on confirmation of bronchial hyperresponsiveness (Sá-Sousa A et al. Clin Transl Allergy. 2014 Aug 4;4:24). In addition, once adequately treated, there is an absence of an algorithm to diagnose disease remission (Aaron SD et al. Am J Respir Crit Care Med. 2018 Oct 15;198[8]:1012-20). It is estimated that 20%-70% of people with asthma worldwide across the spectrum of all ages remain undiagnosed.
Spirometry and bronchoprovocation challenges with fixed cut-off values demonstrate reduced sensitivity with day-to-day, diurnal, and long-term variation in airflow obstruction, inflammation, and bronchial hyperresponsiveness (Wang R et al. Thorax. 2021 Jun;76[6]:624-31). Inflammatory biomarkers like fractional exhaled nitric oxide (FeNO) have higher specificity but are subject to diurnal variation and confounding diagnoses.
Overdiagnosis of asthma can result in lost opportunity to diagnose significant cardiopulmonary diseases, unnecessary escalation of the asthma treatment regimen for poorly controlled respiratory symptoms, potential for medication adverse effects, and, increased cost burden to the patient and to the health care system (Aaron SD et al. JAMA. 2017;317:269-79; Shaw D et al. Prim Care Respir J. 2012;21:283-7). Among the newly physician-diagnosed asthmatics, <50% have spirometry performed within 1 year of diagnosis (Sokol KC et al. Am J Med. 2015 May;128[5]:502-8). Spirometry was further underutilized with limit on aerosol-generating procedures during COVID-19 pandemic (Kankaanranta H et al. J Allergy Clin Immunol Pract. 2021 Dec;9[12]:4252-3); 30%-35% obese and nonobese patients with physician-diagnosed asthma did not have current asthma when objectively assessed for airflow limitation (Aaron SD et al. JAMA. 2017;317:269-79; van Huisstede A, et al. Respir Med. 2013;107:1356-64).
Clinical remission is greater in early-onset asthma as compared with late-onset asthma (De Marco R et al. J Allergy Clin Immunol. 2002;110:228-35). If asthma is well controlled, a stepping down treatment regimen is suggested (Global Initiative for Asthma 2021;Usmani et al. J Allergy Clin Immunol Pract. 2017 Sep-Oct;5[5]:1378-87.e5; Hagan JB et al. Allergy. 2014 Apr;69[4]:510-6), and although a randomized trial is lacking, it may be feasible to “undiagnose” patients who don’t experience clinical worsening, airflow obstruction, or bronchial hyperresponsiveness after being tapered off all asthma medications with a low relapse rate (Aaron SD et al. JAMA. 2017;317:269-79; J Fam Pract. 2018;67(11):704-7).
Asthma over- and underdiagnosis is prevalent and has clinical and global health consequences. New standardized algorithms with improved biomarkers may help alter this oversight.
Richa Nahar, MD
Network Member-at-Large
Allen J. Blaivas, DO, FCCP
Network Steering Committee Chair
Diffuse lung disease and lung transplant network: Interstitial lung disease section
Future therapies for IPF
Idiopathic pulmonary fibrosis (IPF) is a chronic lung disease characterized by progressive fibrosis, respiratory failure, and a mortality rate of 80% at 5 years. Only two drugs are currently FDA-approved for IPF treatment.
The antifibrotics pirfenidone and nintedanib reduce the rate of forced vital capacity (FVC) decline and improve progression free survival (King TE et al. N Engl J Med. 2014;370:2083-92; King TE et al. N Engl J Med. 2014;370:2071-82). While considered revolutionary when introduced, these medications neither reverse disease progression nor improve symptoms. More recently, the Galapagos ISABELA Phase III clinical trial of ziritaxestat in IPF was discontinued due to an unfavorable risk-benefit profile. Despite this, several prospects for IPF therapy exist.
Post hoc analysis of the INCREASE Trial demonstrated a positive effect of inhaled treprostinil on FVC in patients with IPF and group 3 pulmonary hypertension (Waxman A et al. N Engl J Med. 2021;384:325-34). Consequently, a phase 3 randomized trial investigating its safety and efficacy in patients with IPF alone is ongoing. Additional targeted therapies for IPF are also emerging. Recombinant human pentraxin-2, an inhibitor of monocyte differentiation into proinflammatory macrophages, and pamrevlumab, a recombinant human monoclonal antibody against connective tissue growth factor, both demonstrated attenuation of FVC decline compared with placebo in phase 2 trials. Both are currently in phase 3 studies (Raghu G et al. JAMA. 2018 Jun 12;319[22]:2299-307; Sgalla G et al. Expert Opin Investig Drugs. 2020 Aug;29[8]:771-7) Lastly, in February the Food and Drug Administration granted breakthrough therapy designation to BI 1015550 for treatment of IPF based on a 12-week phase 2 randomized, double-blind, placebo-controlled trial. (Data will be presented at ATS). BI 1015550 is an oral, phosphodiesterase 4B (PDE4B) inhibitor with both antifibrotic and anti-inflammatory properties. These advances in drug development provide hope for a future where IPF is transformed from a fatal disease to one manageable over many years.
Adrian Shifren, MD
Network Member-at-Large
Gabriel Schroeder, MD
Network Member-at-Large
Sleep medicine network: Home-based mechanical ventilation and neuromuscular section
Role of airway clearance therapies in neuromuscular disease
Individuals with neuromuscular weakness have an impaired ability to cough and clear secretions from the airway, which can result in atelectasis and pneumonia. Proximal airway clearance therapies (ACT), including manual lung volume recruitment (LVR) and mechanical in-exsufflation (MI-E), mobilize secretions, improve cough efficacy, maintain chest wall compliance, and slow progression of restrictive lung impairment (Chatwin et al. Respir Med. 2018;136:98-110; Sheers et al. Respirology. 2019;24:512-520).
ACT are recommended in international care guidelines for respiratory management of individuals with neuromuscular disease. At a recent Home-based Mechanical Ventilation and Neuromuscular Disease Section “PEEPS Talking PAP” rounds, participants discussed their approach to ACT. Practices varied by country and between adult/pediatric care providers. MI-E is most often used in the United States, but elsewhere in the world, LVR with a self-inflating bag and one-way valve is first-line therapy. Clinical care guidelines suggest initiation of regular ACT when cough peak flow is < 270 L/minute, forced vital capacity < 40%-60% predicted, or with subjectively weak cough (Hull et al. Thorax. 2012;67(7):654-655; Amin et al. Can J Resp Crit Care Sleep Med. 2017;1(1):7-36; McKim et al. Can Resp J. 2011;18(4):197-215; Birnkrant et al. Lancet Neurol. 2018;17(4):347-361; Sheehan et al. Pediatrics. 2018;142(Suppl 2):S62-s71).
Optimal timing for initiation of routine ACT, however, is not clear. A newly published randomized controlled trial of twice daily LVR in boys with Duchenne muscular dystrophy with relatively normal baseline lung function did not demonstrate a significant slowing of decline in forced vital capacity over 2 years. In individuals with preserved lung function, the burden of regular therapy may outweigh benefit (Katz et al. Thorax. 2022; doi: 10.1136/thoraxjnl-2021-218196). (While we are still learning about how best to apply this therapy in less advanced neuromuscular disease, ACT has demonstrated benefits during respiratory exacerbations, and routine use plays a role in preservation of lung function in more advanced disease (Katz et al. Ann Am Thorac Soc. 2016;13(2):217-222; McKim et al. Arch Phys Med Rehab. 2012;93(7):1117-1122; O’Sullivan et al. Arch Phys Med Rehabil. 2021;102(5):976-983; Bach et al. Am J Phys Med Rehab. 2008;87(9):720-725).
Sherri Katz, MD, FCCP
Section Steering Committee Chair
Critical care network: Mechanical ventilation and airways management section
NIV following extubation: Which devices and which patients?
For those of us interested in studying mechanical ventilation, an interesting paradox exists: despite our interest and enthusiasm in studying it, our patients benefit from avoiding it! Patients who require re-intubation are at high risk of in-hospital mortality (Frutos-Vivar et al. J Crit Care. 2011;26:502-9).
Studies in high-risk patients receiving mechanical ventilation have demonstrated that patients treated with immediate noninvasive ventilation (NIV) following extubation had reduced risk of re-intubation. CHEST guidelines focused on ventilator liberation considered these studies in a metanalysis which led to recommendations to employ NIV immediately after extubation in high-risk patients to reduce re-intubation rates (Ouellette D et al. Chest. 2017;151:166-80).
In the years since the publication of the CHEST guidelines, more information has been forthcoming. Evidence has emerged that treatment with high-flow nasal cannula devices following extubation may mitigate against re-intubation. An interesting strategy from the High-Wean Study Group suggested that postextubation combination therapy with both a high-flow cannula and NIV leads to improved outcomes compared with high-flow alone (Thille AW et al. JAMA. 2019;322:1465-75).
Thille and coworkers recently broadened our concept of patients who may benefit from NIV post extubation. They examined a cohort of obese patients requiring mechanical ventilation, finding that when patients were treated with NIV and high-flow nasal cannula post extubation, that they had a reduced risk of re-intubation compared with a group receiving high flow alone (Thille AW, et al. Am J Respir Crit Care Med. 2022;205:440-9).
As the incoming chair of the Mechanical Ventilation and Airways Management Section of the CHEST Critical Care Network, I look forward during the next 2 years to having interesting conversations about topics like this one and working with section members to develop exciting new projects concerning mechanical ventilation.
Daniel Ouellette, MD, MS, FCCP
Section Steering Committee Chair
Thoracic oncology and chest procedures network: Pleural disease section
Management of recurrent transudative pleural effusions (REDUCE trial)
Nonmalignant pleural effusions contribute significantly to health care costs and mortality (Mummadi SR et al. CHEST. 2021 Oct;160[4]:1534-51; Walker SP et al. CHEST. 2017 May;151[5]:1099-105). Management of transudative effusions has traditionally been to treat the underlying etiology. However, despite maximal medical therapies, these recurrent effusions may add to patients’ symptom burden and often create a challenge for the clinician. In 2017, the FDA approved the use of indwelling pleural catheters (IPC) in patients with recurrent transudative effusions, but data are limited.
In a recent prospective multicenter randomized control trial, Walker and colleagues (Eur Respir J. 2022 Feb;59:2101362) aimed to compare IPCs to repeated therapeutic thoracentesis (TT) in the management of transudative effusions. Pleural fluid etiologies included heart (68%), liver (24%), and renal failure (8%). The primary outcome was mean dyspnea score (daily visual analog scales) over 12 weeks, and there was no significant difference noted (39.7 vs. 45.0, mean difference –2.9 mm, 95% confidence interval [CI] –16.1 to 10.3; P = .67). Secondary outcomes demonstrated increased overall drainage in the IPC vs. TT group (17,412 mL vs. 2,901 mL, difference 13,892 mL, 95% CI, 7,669-20,116 mL; P < .001) and fewer invasive procedures required in the IPC group. Adverse events were noted in 59% of the IPC group compared with 37% managed with TT (OR, 3.13, 95% CI, 1.07-9.13, P = .04).
The REDUCE trial offers valuable data, but failure to meet primary outcome, study size, and adverse events highlight limitations to a definitive change in practice. Further study with specific-disease processes (ie, cardiac) may be helpful in the future. As in malignant pleural effusions, the selection of definitive pleural intervention should be tailored for each patient.
Maria Azhar, MD
Network Member-at-Large
Saadia A. Faiz, MD FCCP
Section Steering Committee Chair
Airway disorders network: Asthma and COPD section
Betting on asthma: The over and under of diagnosis
Asthma is one of the major chronic respiratory diseases worldwide (WHO 2020), yet it is a clinical syndrome that lacks a consensus on its definition, is comprised of nonspecific respiratory symptoms, and is without a gold standard diagnostic test or a set guideline on confirmation of bronchial hyperresponsiveness (Sá-Sousa A et al. Clin Transl Allergy. 2014 Aug 4;4:24). In addition, once adequately treated, there is an absence of an algorithm to diagnose disease remission (Aaron SD et al. Am J Respir Crit Care Med. 2018 Oct 15;198[8]:1012-20). It is estimated that 20%-70% of people with asthma worldwide across the spectrum of all ages remain undiagnosed.
Spirometry and bronchoprovocation challenges with fixed cut-off values demonstrate reduced sensitivity with day-to-day, diurnal, and long-term variation in airflow obstruction, inflammation, and bronchial hyperresponsiveness (Wang R et al. Thorax. 2021 Jun;76[6]:624-31). Inflammatory biomarkers like fractional exhaled nitric oxide (FeNO) have higher specificity but are subject to diurnal variation and confounding diagnoses.
Overdiagnosis of asthma can result in lost opportunity to diagnose significant cardiopulmonary diseases, unnecessary escalation of the asthma treatment regimen for poorly controlled respiratory symptoms, potential for medication adverse effects, and, increased cost burden to the patient and to the health care system (Aaron SD et al. JAMA. 2017;317:269-79; Shaw D et al. Prim Care Respir J. 2012;21:283-7). Among the newly physician-diagnosed asthmatics, <50% have spirometry performed within 1 year of diagnosis (Sokol KC et al. Am J Med. 2015 May;128[5]:502-8). Spirometry was further underutilized with limit on aerosol-generating procedures during COVID-19 pandemic (Kankaanranta H et al. J Allergy Clin Immunol Pract. 2021 Dec;9[12]:4252-3); 30%-35% obese and nonobese patients with physician-diagnosed asthma did not have current asthma when objectively assessed for airflow limitation (Aaron SD et al. JAMA. 2017;317:269-79; van Huisstede A, et al. Respir Med. 2013;107:1356-64).
Clinical remission is greater in early-onset asthma as compared with late-onset asthma (De Marco R et al. J Allergy Clin Immunol. 2002;110:228-35). If asthma is well controlled, a stepping down treatment regimen is suggested (Global Initiative for Asthma 2021;Usmani et al. J Allergy Clin Immunol Pract. 2017 Sep-Oct;5[5]:1378-87.e5; Hagan JB et al. Allergy. 2014 Apr;69[4]:510-6), and although a randomized trial is lacking, it may be feasible to “undiagnose” patients who don’t experience clinical worsening, airflow obstruction, or bronchial hyperresponsiveness after being tapered off all asthma medications with a low relapse rate (Aaron SD et al. JAMA. 2017;317:269-79; J Fam Pract. 2018;67(11):704-7).
Asthma over- and underdiagnosis is prevalent and has clinical and global health consequences. New standardized algorithms with improved biomarkers may help alter this oversight.
Richa Nahar, MD
Network Member-at-Large
Allen J. Blaivas, DO, FCCP
Network Steering Committee Chair
Diffuse lung disease and lung transplant network: Interstitial lung disease section
Future therapies for IPF
Idiopathic pulmonary fibrosis (IPF) is a chronic lung disease characterized by progressive fibrosis, respiratory failure, and a mortality rate of 80% at 5 years. Only two drugs are currently FDA-approved for IPF treatment.
The antifibrotics pirfenidone and nintedanib reduce the rate of forced vital capacity (FVC) decline and improve progression free survival (King TE et al. N Engl J Med. 2014;370:2083-92; King TE et al. N Engl J Med. 2014;370:2071-82). While considered revolutionary when introduced, these medications neither reverse disease progression nor improve symptoms. More recently, the Galapagos ISABELA Phase III clinical trial of ziritaxestat in IPF was discontinued due to an unfavorable risk-benefit profile. Despite this, several prospects for IPF therapy exist.
Post hoc analysis of the INCREASE Trial demonstrated a positive effect of inhaled treprostinil on FVC in patients with IPF and group 3 pulmonary hypertension (Waxman A et al. N Engl J Med. 2021;384:325-34). Consequently, a phase 3 randomized trial investigating its safety and efficacy in patients with IPF alone is ongoing. Additional targeted therapies for IPF are also emerging. Recombinant human pentraxin-2, an inhibitor of monocyte differentiation into proinflammatory macrophages, and pamrevlumab, a recombinant human monoclonal antibody against connective tissue growth factor, both demonstrated attenuation of FVC decline compared with placebo in phase 2 trials. Both are currently in phase 3 studies (Raghu G et al. JAMA. 2018 Jun 12;319[22]:2299-307; Sgalla G et al. Expert Opin Investig Drugs. 2020 Aug;29[8]:771-7) Lastly, in February the Food and Drug Administration granted breakthrough therapy designation to BI 1015550 for treatment of IPF based on a 12-week phase 2 randomized, double-blind, placebo-controlled trial. (Data will be presented at ATS). BI 1015550 is an oral, phosphodiesterase 4B (PDE4B) inhibitor with both antifibrotic and anti-inflammatory properties. These advances in drug development provide hope for a future where IPF is transformed from a fatal disease to one manageable over many years.
Adrian Shifren, MD
Network Member-at-Large
Gabriel Schroeder, MD
Network Member-at-Large
Sleep medicine network: Home-based mechanical ventilation and neuromuscular section
Role of airway clearance therapies in neuromuscular disease
Individuals with neuromuscular weakness have an impaired ability to cough and clear secretions from the airway, which can result in atelectasis and pneumonia. Proximal airway clearance therapies (ACT), including manual lung volume recruitment (LVR) and mechanical in-exsufflation (MI-E), mobilize secretions, improve cough efficacy, maintain chest wall compliance, and slow progression of restrictive lung impairment (Chatwin et al. Respir Med. 2018;136:98-110; Sheers et al. Respirology. 2019;24:512-520).
ACT are recommended in international care guidelines for respiratory management of individuals with neuromuscular disease. At a recent Home-based Mechanical Ventilation and Neuromuscular Disease Section “PEEPS Talking PAP” rounds, participants discussed their approach to ACT. Practices varied by country and between adult/pediatric care providers. MI-E is most often used in the United States, but elsewhere in the world, LVR with a self-inflating bag and one-way valve is first-line therapy. Clinical care guidelines suggest initiation of regular ACT when cough peak flow is < 270 L/minute, forced vital capacity < 40%-60% predicted, or with subjectively weak cough (Hull et al. Thorax. 2012;67(7):654-655; Amin et al. Can J Resp Crit Care Sleep Med. 2017;1(1):7-36; McKim et al. Can Resp J. 2011;18(4):197-215; Birnkrant et al. Lancet Neurol. 2018;17(4):347-361; Sheehan et al. Pediatrics. 2018;142(Suppl 2):S62-s71).
Optimal timing for initiation of routine ACT, however, is not clear. A newly published randomized controlled trial of twice daily LVR in boys with Duchenne muscular dystrophy with relatively normal baseline lung function did not demonstrate a significant slowing of decline in forced vital capacity over 2 years. In individuals with preserved lung function, the burden of regular therapy may outweigh benefit (Katz et al. Thorax. 2022; doi: 10.1136/thoraxjnl-2021-218196). (While we are still learning about how best to apply this therapy in less advanced neuromuscular disease, ACT has demonstrated benefits during respiratory exacerbations, and routine use plays a role in preservation of lung function in more advanced disease (Katz et al. Ann Am Thorac Soc. 2016;13(2):217-222; McKim et al. Arch Phys Med Rehab. 2012;93(7):1117-1122; O’Sullivan et al. Arch Phys Med Rehabil. 2021;102(5):976-983; Bach et al. Am J Phys Med Rehab. 2008;87(9):720-725).
Sherri Katz, MD, FCCP
Section Steering Committee Chair
Critical care network: Mechanical ventilation and airways management section
NIV following extubation: Which devices and which patients?
For those of us interested in studying mechanical ventilation, an interesting paradox exists: despite our interest and enthusiasm in studying it, our patients benefit from avoiding it! Patients who require re-intubation are at high risk of in-hospital mortality (Frutos-Vivar et al. J Crit Care. 2011;26:502-9).
Studies in high-risk patients receiving mechanical ventilation have demonstrated that patients treated with immediate noninvasive ventilation (NIV) following extubation had reduced risk of re-intubation. CHEST guidelines focused on ventilator liberation considered these studies in a metanalysis which led to recommendations to employ NIV immediately after extubation in high-risk patients to reduce re-intubation rates (Ouellette D et al. Chest. 2017;151:166-80).
In the years since the publication of the CHEST guidelines, more information has been forthcoming. Evidence has emerged that treatment with high-flow nasal cannula devices following extubation may mitigate against re-intubation. An interesting strategy from the High-Wean Study Group suggested that postextubation combination therapy with both a high-flow cannula and NIV leads to improved outcomes compared with high-flow alone (Thille AW et al. JAMA. 2019;322:1465-75).
Thille and coworkers recently broadened our concept of patients who may benefit from NIV post extubation. They examined a cohort of obese patients requiring mechanical ventilation, finding that when patients were treated with NIV and high-flow nasal cannula post extubation, that they had a reduced risk of re-intubation compared with a group receiving high flow alone (Thille AW, et al. Am J Respir Crit Care Med. 2022;205:440-9).
As the incoming chair of the Mechanical Ventilation and Airways Management Section of the CHEST Critical Care Network, I look forward during the next 2 years to having interesting conversations about topics like this one and working with section members to develop exciting new projects concerning mechanical ventilation.
Daniel Ouellette, MD, MS, FCCP
Section Steering Committee Chair
Thoracic oncology and chest procedures network: Pleural disease section
Management of recurrent transudative pleural effusions (REDUCE trial)
Nonmalignant pleural effusions contribute significantly to health care costs and mortality (Mummadi SR et al. CHEST. 2021 Oct;160[4]:1534-51; Walker SP et al. CHEST. 2017 May;151[5]:1099-105). Management of transudative effusions has traditionally been to treat the underlying etiology. However, despite maximal medical therapies, these recurrent effusions may add to patients’ symptom burden and often create a challenge for the clinician. In 2017, the FDA approved the use of indwelling pleural catheters (IPC) in patients with recurrent transudative effusions, but data are limited.
In a recent prospective multicenter randomized control trial, Walker and colleagues (Eur Respir J. 2022 Feb;59:2101362) aimed to compare IPCs to repeated therapeutic thoracentesis (TT) in the management of transudative effusions. Pleural fluid etiologies included heart (68%), liver (24%), and renal failure (8%). The primary outcome was mean dyspnea score (daily visual analog scales) over 12 weeks, and there was no significant difference noted (39.7 vs. 45.0, mean difference –2.9 mm, 95% confidence interval [CI] –16.1 to 10.3; P = .67). Secondary outcomes demonstrated increased overall drainage in the IPC vs. TT group (17,412 mL vs. 2,901 mL, difference 13,892 mL, 95% CI, 7,669-20,116 mL; P < .001) and fewer invasive procedures required in the IPC group. Adverse events were noted in 59% of the IPC group compared with 37% managed with TT (OR, 3.13, 95% CI, 1.07-9.13, P = .04).
The REDUCE trial offers valuable data, but failure to meet primary outcome, study size, and adverse events highlight limitations to a definitive change in practice. Further study with specific-disease processes (ie, cardiac) may be helpful in the future. As in malignant pleural effusions, the selection of definitive pleural intervention should be tailored for each patient.
Maria Azhar, MD
Network Member-at-Large
Saadia A. Faiz, MD FCCP
Section Steering Committee Chair
Airway disorders network: Asthma and COPD section
Betting on asthma: The over and under of diagnosis
Asthma is one of the major chronic respiratory diseases worldwide (WHO 2020), yet it is a clinical syndrome that lacks a consensus on its definition, is comprised of nonspecific respiratory symptoms, and is without a gold standard diagnostic test or a set guideline on confirmation of bronchial hyperresponsiveness (Sá-Sousa A et al. Clin Transl Allergy. 2014 Aug 4;4:24). In addition, once adequately treated, there is an absence of an algorithm to diagnose disease remission (Aaron SD et al. Am J Respir Crit Care Med. 2018 Oct 15;198[8]:1012-20). It is estimated that 20%-70% of people with asthma worldwide across the spectrum of all ages remain undiagnosed.
Spirometry and bronchoprovocation challenges with fixed cut-off values demonstrate reduced sensitivity with day-to-day, diurnal, and long-term variation in airflow obstruction, inflammation, and bronchial hyperresponsiveness (Wang R et al. Thorax. 2021 Jun;76[6]:624-31). Inflammatory biomarkers like fractional exhaled nitric oxide (FeNO) have higher specificity but are subject to diurnal variation and confounding diagnoses.
Overdiagnosis of asthma can result in lost opportunity to diagnose significant cardiopulmonary diseases, unnecessary escalation of the asthma treatment regimen for poorly controlled respiratory symptoms, potential for medication adverse effects, and, increased cost burden to the patient and to the health care system (Aaron SD et al. JAMA. 2017;317:269-79; Shaw D et al. Prim Care Respir J. 2012;21:283-7). Among the newly physician-diagnosed asthmatics, <50% have spirometry performed within 1 year of diagnosis (Sokol KC et al. Am J Med. 2015 May;128[5]:502-8). Spirometry was further underutilized with limit on aerosol-generating procedures during COVID-19 pandemic (Kankaanranta H et al. J Allergy Clin Immunol Pract. 2021 Dec;9[12]:4252-3); 30%-35% obese and nonobese patients with physician-diagnosed asthma did not have current asthma when objectively assessed for airflow limitation (Aaron SD et al. JAMA. 2017;317:269-79; van Huisstede A, et al. Respir Med. 2013;107:1356-64).
Clinical remission is greater in early-onset asthma as compared with late-onset asthma (De Marco R et al. J Allergy Clin Immunol. 2002;110:228-35). If asthma is well controlled, a stepping down treatment regimen is suggested (Global Initiative for Asthma 2021;Usmani et al. J Allergy Clin Immunol Pract. 2017 Sep-Oct;5[5]:1378-87.e5; Hagan JB et al. Allergy. 2014 Apr;69[4]:510-6), and although a randomized trial is lacking, it may be feasible to “undiagnose” patients who don’t experience clinical worsening, airflow obstruction, or bronchial hyperresponsiveness after being tapered off all asthma medications with a low relapse rate (Aaron SD et al. JAMA. 2017;317:269-79; J Fam Pract. 2018;67(11):704-7).
Asthma over- and underdiagnosis is prevalent and has clinical and global health consequences. New standardized algorithms with improved biomarkers may help alter this oversight.
Richa Nahar, MD
Network Member-at-Large
Allen J. Blaivas, DO, FCCP
Network Steering Committee Chair
Diffuse lung disease and lung transplant network: Interstitial lung disease section
Future therapies for IPF
Idiopathic pulmonary fibrosis (IPF) is a chronic lung disease characterized by progressive fibrosis, respiratory failure, and a mortality rate of 80% at 5 years. Only two drugs are currently FDA-approved for IPF treatment.
The antifibrotics pirfenidone and nintedanib reduce the rate of forced vital capacity (FVC) decline and improve progression free survival (King TE et al. N Engl J Med. 2014;370:2083-92; King TE et al. N Engl J Med. 2014;370:2071-82). While considered revolutionary when introduced, these medications neither reverse disease progression nor improve symptoms. More recently, the Galapagos ISABELA Phase III clinical trial of ziritaxestat in IPF was discontinued due to an unfavorable risk-benefit profile. Despite this, several prospects for IPF therapy exist.
Post hoc analysis of the INCREASE Trial demonstrated a positive effect of inhaled treprostinil on FVC in patients with IPF and group 3 pulmonary hypertension (Waxman A et al. N Engl J Med. 2021;384:325-34). Consequently, a phase 3 randomized trial investigating its safety and efficacy in patients with IPF alone is ongoing. Additional targeted therapies for IPF are also emerging. Recombinant human pentraxin-2, an inhibitor of monocyte differentiation into proinflammatory macrophages, and pamrevlumab, a recombinant human monoclonal antibody against connective tissue growth factor, both demonstrated attenuation of FVC decline compared with placebo in phase 2 trials. Both are currently in phase 3 studies (Raghu G et al. JAMA. 2018 Jun 12;319[22]:2299-307; Sgalla G et al. Expert Opin Investig Drugs. 2020 Aug;29[8]:771-7) Lastly, in February the Food and Drug Administration granted breakthrough therapy designation to BI 1015550 for treatment of IPF based on a 12-week phase 2 randomized, double-blind, placebo-controlled trial. (Data will be presented at ATS). BI 1015550 is an oral, phosphodiesterase 4B (PDE4B) inhibitor with both antifibrotic and anti-inflammatory properties. These advances in drug development provide hope for a future where IPF is transformed from a fatal disease to one manageable over many years.
Adrian Shifren, MD
Network Member-at-Large
Gabriel Schroeder, MD
Network Member-at-Large
Sleep medicine network: Home-based mechanical ventilation and neuromuscular section
Role of airway clearance therapies in neuromuscular disease
Individuals with neuromuscular weakness have an impaired ability to cough and clear secretions from the airway, which can result in atelectasis and pneumonia. Proximal airway clearance therapies (ACT), including manual lung volume recruitment (LVR) and mechanical in-exsufflation (MI-E), mobilize secretions, improve cough efficacy, maintain chest wall compliance, and slow progression of restrictive lung impairment (Chatwin et al. Respir Med. 2018;136:98-110; Sheers et al. Respirology. 2019;24:512-520).
ACT are recommended in international care guidelines for respiratory management of individuals with neuromuscular disease. At a recent Home-based Mechanical Ventilation and Neuromuscular Disease Section “PEEPS Talking PAP” rounds, participants discussed their approach to ACT. Practices varied by country and between adult/pediatric care providers. MI-E is most often used in the United States, but elsewhere in the world, LVR with a self-inflating bag and one-way valve is first-line therapy. Clinical care guidelines suggest initiation of regular ACT when cough peak flow is < 270 L/minute, forced vital capacity < 40%-60% predicted, or with subjectively weak cough (Hull et al. Thorax. 2012;67(7):654-655; Amin et al. Can J Resp Crit Care Sleep Med. 2017;1(1):7-36; McKim et al. Can Resp J. 2011;18(4):197-215; Birnkrant et al. Lancet Neurol. 2018;17(4):347-361; Sheehan et al. Pediatrics. 2018;142(Suppl 2):S62-s71).
Optimal timing for initiation of routine ACT, however, is not clear. A newly published randomized controlled trial of twice daily LVR in boys with Duchenne muscular dystrophy with relatively normal baseline lung function did not demonstrate a significant slowing of decline in forced vital capacity over 2 years. In individuals with preserved lung function, the burden of regular therapy may outweigh benefit (Katz et al. Thorax. 2022; doi: 10.1136/thoraxjnl-2021-218196). (While we are still learning about how best to apply this therapy in less advanced neuromuscular disease, ACT has demonstrated benefits during respiratory exacerbations, and routine use plays a role in preservation of lung function in more advanced disease (Katz et al. Ann Am Thorac Soc. 2016;13(2):217-222; McKim et al. Arch Phys Med Rehab. 2012;93(7):1117-1122; O’Sullivan et al. Arch Phys Med Rehabil. 2021;102(5):976-983; Bach et al. Am J Phys Med Rehab. 2008;87(9):720-725).
Sherri Katz, MD, FCCP
Section Steering Committee Chair
Critical care network: Mechanical ventilation and airways management section
NIV following extubation: Which devices and which patients?
For those of us interested in studying mechanical ventilation, an interesting paradox exists: despite our interest and enthusiasm in studying it, our patients benefit from avoiding it! Patients who require re-intubation are at high risk of in-hospital mortality (Frutos-Vivar et al. J Crit Care. 2011;26:502-9).
Studies in high-risk patients receiving mechanical ventilation have demonstrated that patients treated with immediate noninvasive ventilation (NIV) following extubation had reduced risk of re-intubation. CHEST guidelines focused on ventilator liberation considered these studies in a metanalysis which led to recommendations to employ NIV immediately after extubation in high-risk patients to reduce re-intubation rates (Ouellette D et al. Chest. 2017;151:166-80).
In the years since the publication of the CHEST guidelines, more information has been forthcoming. Evidence has emerged that treatment with high-flow nasal cannula devices following extubation may mitigate against re-intubation. An interesting strategy from the High-Wean Study Group suggested that postextubation combination therapy with both a high-flow cannula and NIV leads to improved outcomes compared with high-flow alone (Thille AW et al. JAMA. 2019;322:1465-75).
Thille and coworkers recently broadened our concept of patients who may benefit from NIV post extubation. They examined a cohort of obese patients requiring mechanical ventilation, finding that when patients were treated with NIV and high-flow nasal cannula post extubation, that they had a reduced risk of re-intubation compared with a group receiving high flow alone (Thille AW, et al. Am J Respir Crit Care Med. 2022;205:440-9).
As the incoming chair of the Mechanical Ventilation and Airways Management Section of the CHEST Critical Care Network, I look forward during the next 2 years to having interesting conversations about topics like this one and working with section members to develop exciting new projects concerning mechanical ventilation.
Daniel Ouellette, MD, MS, FCCP
Section Steering Committee Chair
Thoracic oncology and chest procedures network: Pleural disease section
Management of recurrent transudative pleural effusions (REDUCE trial)
Nonmalignant pleural effusions contribute significantly to health care costs and mortality (Mummadi SR et al. CHEST. 2021 Oct;160[4]:1534-51; Walker SP et al. CHEST. 2017 May;151[5]:1099-105). Management of transudative effusions has traditionally been to treat the underlying etiology. However, despite maximal medical therapies, these recurrent effusions may add to patients’ symptom burden and often create a challenge for the clinician. In 2017, the FDA approved the use of indwelling pleural catheters (IPC) in patients with recurrent transudative effusions, but data are limited.
In a recent prospective multicenter randomized control trial, Walker and colleagues (Eur Respir J. 2022 Feb;59:2101362) aimed to compare IPCs to repeated therapeutic thoracentesis (TT) in the management of transudative effusions. Pleural fluid etiologies included heart (68%), liver (24%), and renal failure (8%). The primary outcome was mean dyspnea score (daily visual analog scales) over 12 weeks, and there was no significant difference noted (39.7 vs. 45.0, mean difference –2.9 mm, 95% confidence interval [CI] –16.1 to 10.3; P = .67). Secondary outcomes demonstrated increased overall drainage in the IPC vs. TT group (17,412 mL vs. 2,901 mL, difference 13,892 mL, 95% CI, 7,669-20,116 mL; P < .001) and fewer invasive procedures required in the IPC group. Adverse events were noted in 59% of the IPC group compared with 37% managed with TT (OR, 3.13, 95% CI, 1.07-9.13, P = .04).
The REDUCE trial offers valuable data, but failure to meet primary outcome, study size, and adverse events highlight limitations to a definitive change in practice. Further study with specific-disease processes (ie, cardiac) may be helpful in the future. As in malignant pleural effusions, the selection of definitive pleural intervention should be tailored for each patient.
Maria Azhar, MD
Network Member-at-Large
Saadia A. Faiz, MD FCCP
Section Steering Committee Chair
This month in the journal CHEST®
Editor’s picks
Barriers and Enablers to Objective Testing for Asthma and COPD in Primary Care: A Systematic Review Using the Theoretical Domains Framework
By Dr. Janet Yamada et al.
COVID Complications: Diagnostic and Therapeutic Considerations for Critical Covid
By Dr. David M. Maslove et al.
Interstitial Lung Abnormalities, Emphysema, and Spirometry in Smokers
By Dr. Aravind A. Menon et al.
Sleep-Disordered Breathing in Hospitalized Patients: A Game Changer?
By Dr. Sunil Sharma and Dr. Robert Stansbury.
Distribution, Risk Factors, and Temporal Trends for Lung Cancer Incidence and Mortality: A Global Analysis
By Dr. Junjie Huang et al.
Editor’s picks
Editor’s picks
Barriers and Enablers to Objective Testing for Asthma and COPD in Primary Care: A Systematic Review Using the Theoretical Domains Framework
By Dr. Janet Yamada et al.
COVID Complications: Diagnostic and Therapeutic Considerations for Critical Covid
By Dr. David M. Maslove et al.
Interstitial Lung Abnormalities, Emphysema, and Spirometry in Smokers
By Dr. Aravind A. Menon et al.
Sleep-Disordered Breathing in Hospitalized Patients: A Game Changer?
By Dr. Sunil Sharma and Dr. Robert Stansbury.
Distribution, Risk Factors, and Temporal Trends for Lung Cancer Incidence and Mortality: A Global Analysis
By Dr. Junjie Huang et al.
Barriers and Enablers to Objective Testing for Asthma and COPD in Primary Care: A Systematic Review Using the Theoretical Domains Framework
By Dr. Janet Yamada et al.
COVID Complications: Diagnostic and Therapeutic Considerations for Critical Covid
By Dr. David M. Maslove et al.
Interstitial Lung Abnormalities, Emphysema, and Spirometry in Smokers
By Dr. Aravind A. Menon et al.
Sleep-Disordered Breathing in Hospitalized Patients: A Game Changer?
By Dr. Sunil Sharma and Dr. Robert Stansbury.
Distribution, Risk Factors, and Temporal Trends for Lung Cancer Incidence and Mortality: A Global Analysis
By Dr. Junjie Huang et al.
Victor Test, MD, FCCP, receives Medal of Valor from AMA
The American Medical Association (AMA) honored CHEST Board Member Victor J. Test, MD, FCCP, with the AMA Medal of Valor for his work on behalf of patients and his community during the COVID-19 pandemic.
The award, which recognizes physicians who demonstrate courage under extraordinary circumstances, was presented to Dr. Test because of his quick decisive actions during the onset of the pandemic, including personally securing personal protective equipment to supply the critical care faculty and fellows at the Texas Tech University hospital in Lubbock and building plexiglass and PVC chambers for the physicians and nursing staff caring for patients with COVID-19.
Read more here.
The American Medical Association (AMA) honored CHEST Board Member Victor J. Test, MD, FCCP, with the AMA Medal of Valor for his work on behalf of patients and his community during the COVID-19 pandemic.
The award, which recognizes physicians who demonstrate courage under extraordinary circumstances, was presented to Dr. Test because of his quick decisive actions during the onset of the pandemic, including personally securing personal protective equipment to supply the critical care faculty and fellows at the Texas Tech University hospital in Lubbock and building plexiglass and PVC chambers for the physicians and nursing staff caring for patients with COVID-19.
Read more here.
The American Medical Association (AMA) honored CHEST Board Member Victor J. Test, MD, FCCP, with the AMA Medal of Valor for his work on behalf of patients and his community during the COVID-19 pandemic.
The award, which recognizes physicians who demonstrate courage under extraordinary circumstances, was presented to Dr. Test because of his quick decisive actions during the onset of the pandemic, including personally securing personal protective equipment to supply the critical care faculty and fellows at the Texas Tech University hospital in Lubbock and building plexiglass and PVC chambers for the physicians and nursing staff caring for patients with COVID-19.
Read more here.
Off to the races with The CHEST Foundation
The CHEST Foundation cordially invites CHEST members and colleagues, health care professionals, and others to champion lung health and attend the annual Belmont Stakes Dinner and Auction, Saturday, June 11, in New York at the beautiful Water Club overlooking the East River.
Hosted by CHEST President-Elect Doreen Addrizzo-Harris, MD, FCCP, this year’s celebration will include a lively cocktail reception, a silent and live auction, dinner, and a rooftop after-party for young professionals to network with colleagues and CHEST leadership and take the challenge for a chance to win great prizes, including a Peloton, ultrasound machine, and access to CHEST courses and events. Fully immerse yourself in the event, and wear your race-day best!
This year, we are honoring two outstanding patients and advocates, Betsy Glaeser and Fred Schick, for their remarkable achievements in patient empowerment and access. Glaeser, who was diagnosed with nontuberculous mycobacteria (disease NTM) more than 20 years ago, pioneered opportunities for NTM-specific research funding and runs a hundreds-strong support group for people with NTM and bronchiectasis. Schick, who has pulmonary fibrosis, is an active ambassador in the patient community in Chicago and also leads local support groups for others with the disease.
All proceeds from the evening’s events will benefit the CHEST Foundation’s continued work toward bringing impactful, informative resources to patients.
As the patient-focused philanthropic arm of the American College of Chest Physicians, the CHEST Foundation is on a mission to champion lung health and strives to give health care professionals, patients, and caregivers opportunities to come together, give back, and advocate for change.
Since its inception, the Foundation has provided more than $8 million in research grants and $3 million in community grants, created free patient education resources for more than 80 disease states, and provided thousands of units of personal protective equipment and $1 million for pandemic relief efforts through COVID-19 Reaction Microgrants.
Support the continued work of the Foundation – and watch some of the most exciting few minutes in sports among colleagues and friends – at this year’s Belmont Stakes Dinner and Auction. To purchase a ticket, or to learn more about sponsorship benefits or underwriting opportunities, contact Angela Perillo at [email protected] or +1 (224) 521-9520.
The CHEST Foundation cordially invites CHEST members and colleagues, health care professionals, and others to champion lung health and attend the annual Belmont Stakes Dinner and Auction, Saturday, June 11, in New York at the beautiful Water Club overlooking the East River.
Hosted by CHEST President-Elect Doreen Addrizzo-Harris, MD, FCCP, this year’s celebration will include a lively cocktail reception, a silent and live auction, dinner, and a rooftop after-party for young professionals to network with colleagues and CHEST leadership and take the challenge for a chance to win great prizes, including a Peloton, ultrasound machine, and access to CHEST courses and events. Fully immerse yourself in the event, and wear your race-day best!
This year, we are honoring two outstanding patients and advocates, Betsy Glaeser and Fred Schick, for their remarkable achievements in patient empowerment and access. Glaeser, who was diagnosed with nontuberculous mycobacteria (disease NTM) more than 20 years ago, pioneered opportunities for NTM-specific research funding and runs a hundreds-strong support group for people with NTM and bronchiectasis. Schick, who has pulmonary fibrosis, is an active ambassador in the patient community in Chicago and also leads local support groups for others with the disease.
All proceeds from the evening’s events will benefit the CHEST Foundation’s continued work toward bringing impactful, informative resources to patients.
As the patient-focused philanthropic arm of the American College of Chest Physicians, the CHEST Foundation is on a mission to champion lung health and strives to give health care professionals, patients, and caregivers opportunities to come together, give back, and advocate for change.
Since its inception, the Foundation has provided more than $8 million in research grants and $3 million in community grants, created free patient education resources for more than 80 disease states, and provided thousands of units of personal protective equipment and $1 million for pandemic relief efforts through COVID-19 Reaction Microgrants.
Support the continued work of the Foundation – and watch some of the most exciting few minutes in sports among colleagues and friends – at this year’s Belmont Stakes Dinner and Auction. To purchase a ticket, or to learn more about sponsorship benefits or underwriting opportunities, contact Angela Perillo at [email protected] or +1 (224) 521-9520.
The CHEST Foundation cordially invites CHEST members and colleagues, health care professionals, and others to champion lung health and attend the annual Belmont Stakes Dinner and Auction, Saturday, June 11, in New York at the beautiful Water Club overlooking the East River.
Hosted by CHEST President-Elect Doreen Addrizzo-Harris, MD, FCCP, this year’s celebration will include a lively cocktail reception, a silent and live auction, dinner, and a rooftop after-party for young professionals to network with colleagues and CHEST leadership and take the challenge for a chance to win great prizes, including a Peloton, ultrasound machine, and access to CHEST courses and events. Fully immerse yourself in the event, and wear your race-day best!
This year, we are honoring two outstanding patients and advocates, Betsy Glaeser and Fred Schick, for their remarkable achievements in patient empowerment and access. Glaeser, who was diagnosed with nontuberculous mycobacteria (disease NTM) more than 20 years ago, pioneered opportunities for NTM-specific research funding and runs a hundreds-strong support group for people with NTM and bronchiectasis. Schick, who has pulmonary fibrosis, is an active ambassador in the patient community in Chicago and also leads local support groups for others with the disease.
All proceeds from the evening’s events will benefit the CHEST Foundation’s continued work toward bringing impactful, informative resources to patients.
As the patient-focused philanthropic arm of the American College of Chest Physicians, the CHEST Foundation is on a mission to champion lung health and strives to give health care professionals, patients, and caregivers opportunities to come together, give back, and advocate for change.
Since its inception, the Foundation has provided more than $8 million in research grants and $3 million in community grants, created free patient education resources for more than 80 disease states, and provided thousands of units of personal protective equipment and $1 million for pandemic relief efforts through COVID-19 Reaction Microgrants.
Support the continued work of the Foundation – and watch some of the most exciting few minutes in sports among colleagues and friends – at this year’s Belmont Stakes Dinner and Auction. To purchase a ticket, or to learn more about sponsorship benefits or underwriting opportunities, contact Angela Perillo at [email protected] or +1 (224) 521-9520.
Chest Infections and Disaster Response
Addressing disparities of socioeconomic status, race, and education in vaccine hesitancy and uptake
Vaccine hesitancy is described by the World Health Organization (WHO) as a “delay in acceptance or refusal of vaccination, despite availability of vaccine services.”1 Disparities in COVID-19 vaccine uptake, in addition to preexisting views of vaccine hesitancy, are consistently in the mainstream news.
The United States has a high rate of vaccine hesitancy, with a third of the country surveyed in 2021 stating they were unlikely to become vaccinated against COVID-19.2 This is in contrast to over 90% of people in Australia, China, and Norway saying they were highly likely to become vaccinated. Prepandemic, however, vaccination rates for preventable respiratory illness were already suboptimal. In fact, in 2019, the WHO declared vaccine hesitancy a top 10 priority due to the threat low vaccination causes on a global level.1
U.S. health care systems’ cost to patients may serve as a disincentive for health care utilization, decreasing health care contacts. Further, changes in insurance can lead to provider discontinuity, which may erode the trusted patient-physician relationship. These realities may contribute to vaccine hesitancy that has been inversely correlated to both number of health care visits and trust in health care providers. Vaccine hesitancy exacerbates health disparities.1 Health literacy (understanding of health), education level, and general vaccine knowledge contribute to vaccine hesitancy also. Additionally, high social vulnerability (a score calculated from factors related to socioeconomic status, race, household makeup, housing type, and transportation) is strongly inversely correlated with vaccination rates. In places with both high social vulnerability and vaccine hesitancy, the vaccine-hesitant individuals have far fewer vaccinations.3
Providers can impact vaccine uptake. Broadly, efforts to understand and address issues of trust in health care are needed. Educational materials should be disseminated to high-risk and medically underserved communities. At medical appointments, assessment of vaccination status, followed by providing individualized information regarding vaccine benefits and specific concerns may help increase uptake. In a survey of high-risk adults, only 14.8 and 18.5% of patients stated that the pneumococcal vaccine was offered to them in the last year and 5 years, respectively.1 Providers can have a strong impact on people obtaining vaccines; over half of patients receive vaccines when their provider recommends it.1,4 As a medical community focused on respiratory health, we need to prioritize offering vaccinations during inpatient and outpatient encounters.
By Jamie R. Felzer, MD, MPH
Network Member
Cassie C. Kennedy, MD, FCCP
Vice Chair, Council of Networks
Dr. Felzer is a Fellow and Dr. Kennedy is Associate Professor of Medicine, Division of Pulmonary and Critical Care Medicine, Mayo Clinic, Rochester, MN.
References
1. Gatwood J et al. Am J Health Promot. 2021;35:908.
2. Wong LP et al. Infect Dis Poverty. 2021;10:122.
3. Crane MA et al. Health Aff (Millwood). 2021;40:1792.
4. Strully KW et al. Front Public Health. 2021;9:645268.
Addressing disparities of socioeconomic status, race, and education in vaccine hesitancy and uptake
Vaccine hesitancy is described by the World Health Organization (WHO) as a “delay in acceptance or refusal of vaccination, despite availability of vaccine services.”1 Disparities in COVID-19 vaccine uptake, in addition to preexisting views of vaccine hesitancy, are consistently in the mainstream news.
The United States has a high rate of vaccine hesitancy, with a third of the country surveyed in 2021 stating they were unlikely to become vaccinated against COVID-19.2 This is in contrast to over 90% of people in Australia, China, and Norway saying they were highly likely to become vaccinated. Prepandemic, however, vaccination rates for preventable respiratory illness were already suboptimal. In fact, in 2019, the WHO declared vaccine hesitancy a top 10 priority due to the threat low vaccination causes on a global level.1
U.S. health care systems’ cost to patients may serve as a disincentive for health care utilization, decreasing health care contacts. Further, changes in insurance can lead to provider discontinuity, which may erode the trusted patient-physician relationship. These realities may contribute to vaccine hesitancy that has been inversely correlated to both number of health care visits and trust in health care providers. Vaccine hesitancy exacerbates health disparities.1 Health literacy (understanding of health), education level, and general vaccine knowledge contribute to vaccine hesitancy also. Additionally, high social vulnerability (a score calculated from factors related to socioeconomic status, race, household makeup, housing type, and transportation) is strongly inversely correlated with vaccination rates. In places with both high social vulnerability and vaccine hesitancy, the vaccine-hesitant individuals have far fewer vaccinations.3
Providers can impact vaccine uptake. Broadly, efforts to understand and address issues of trust in health care are needed. Educational materials should be disseminated to high-risk and medically underserved communities. At medical appointments, assessment of vaccination status, followed by providing individualized information regarding vaccine benefits and specific concerns may help increase uptake. In a survey of high-risk adults, only 14.8 and 18.5% of patients stated that the pneumococcal vaccine was offered to them in the last year and 5 years, respectively.1 Providers can have a strong impact on people obtaining vaccines; over half of patients receive vaccines when their provider recommends it.1,4 As a medical community focused on respiratory health, we need to prioritize offering vaccinations during inpatient and outpatient encounters.
By Jamie R. Felzer, MD, MPH
Network Member
Cassie C. Kennedy, MD, FCCP
Vice Chair, Council of Networks
Dr. Felzer is a Fellow and Dr. Kennedy is Associate Professor of Medicine, Division of Pulmonary and Critical Care Medicine, Mayo Clinic, Rochester, MN.
References
1. Gatwood J et al. Am J Health Promot. 2021;35:908.
2. Wong LP et al. Infect Dis Poverty. 2021;10:122.
3. Crane MA et al. Health Aff (Millwood). 2021;40:1792.
4. Strully KW et al. Front Public Health. 2021;9:645268.
Addressing disparities of socioeconomic status, race, and education in vaccine hesitancy and uptake
Vaccine hesitancy is described by the World Health Organization (WHO) as a “delay in acceptance or refusal of vaccination, despite availability of vaccine services.”1 Disparities in COVID-19 vaccine uptake, in addition to preexisting views of vaccine hesitancy, are consistently in the mainstream news.
The United States has a high rate of vaccine hesitancy, with a third of the country surveyed in 2021 stating they were unlikely to become vaccinated against COVID-19.2 This is in contrast to over 90% of people in Australia, China, and Norway saying they were highly likely to become vaccinated. Prepandemic, however, vaccination rates for preventable respiratory illness were already suboptimal. In fact, in 2019, the WHO declared vaccine hesitancy a top 10 priority due to the threat low vaccination causes on a global level.1
U.S. health care systems’ cost to patients may serve as a disincentive for health care utilization, decreasing health care contacts. Further, changes in insurance can lead to provider discontinuity, which may erode the trusted patient-physician relationship. These realities may contribute to vaccine hesitancy that has been inversely correlated to both number of health care visits and trust in health care providers. Vaccine hesitancy exacerbates health disparities.1 Health literacy (understanding of health), education level, and general vaccine knowledge contribute to vaccine hesitancy also. Additionally, high social vulnerability (a score calculated from factors related to socioeconomic status, race, household makeup, housing type, and transportation) is strongly inversely correlated with vaccination rates. In places with both high social vulnerability and vaccine hesitancy, the vaccine-hesitant individuals have far fewer vaccinations.3
Providers can impact vaccine uptake. Broadly, efforts to understand and address issues of trust in health care are needed. Educational materials should be disseminated to high-risk and medically underserved communities. At medical appointments, assessment of vaccination status, followed by providing individualized information regarding vaccine benefits and specific concerns may help increase uptake. In a survey of high-risk adults, only 14.8 and 18.5% of patients stated that the pneumococcal vaccine was offered to them in the last year and 5 years, respectively.1 Providers can have a strong impact on people obtaining vaccines; over half of patients receive vaccines when their provider recommends it.1,4 As a medical community focused on respiratory health, we need to prioritize offering vaccinations during inpatient and outpatient encounters.
By Jamie R. Felzer, MD, MPH
Network Member
Cassie C. Kennedy, MD, FCCP
Vice Chair, Council of Networks
Dr. Felzer is a Fellow and Dr. Kennedy is Associate Professor of Medicine, Division of Pulmonary and Critical Care Medicine, Mayo Clinic, Rochester, MN.
References
1. Gatwood J et al. Am J Health Promot. 2021;35:908.
2. Wong LP et al. Infect Dis Poverty. 2021;10:122.
3. Crane MA et al. Health Aff (Millwood). 2021;40:1792.
4. Strully KW et al. Front Public Health. 2021;9:645268.
FeNO guidelines. Marijuana use in pregnancy.
Airway disorders
FeNO guidelines and the art of clinical medicine
The American Thoracic Society (ATS) recently published new guidelines on the use of fractional exhaled nitric oxide (FeNO) in the management of asthma (Khatri S. Am J Respir Crit Care Med. 2021;204[10]:e97-e109). The previous iteration dealt with questions about the interpretation of FeNO levels. However, the updated guidelines address a single question: Should patients with asthma in whom treatment is being contemplated undergo FeNO testing?
Several roles of nitric oxide (NO) have been discovered, including as a marker of eosinophilic airway inflammation or T2-inflammation. The fraction of NO during steady-state exhalation, easily measured by a handheld device, is a standardized quantitative noninvasive method to assess severity of airway eosinophilic inflammation. However, factors like concomitant sinusitis, bronchoconstriction, obesity, and smoking can also affect FeNO levels, and interpretation is context-dependent. Moreover, some biologic agents have variable effects on FeNO while still being effective in controlling T2 inflammation. Therefore, FeNO is neither the broadest nor the most sensitive signal of T2 inflammation, and there is much unknown about using FeNO to guide asthma treatment. Heterogeneity is one of the many challenges, as different endotypes and clinical subsets vary in the inflammatory pathways leading to airway hyperresponsiveness and remodeling.
The panel assessed the value of FeNO testing in improving asthma control questionnaire scores (ACT, ACQ-7), oral corticosteroid use, asthma exacerbations, lung function, health care utilization, and cost-effectiveness. FeNO-guided therapy compared with therapy without FeNO reduced exacerbations and oral corticosteroid use, though effect size was modest. Among other outcomes, while the trend favored FeNO, it did not reach statistical significance. Adverse effects of FeNO testing were trivial, and the cost is moderate though dependent on the institution size and testing frequency. Thus, for clinicians who manage adults and children 4 years of age and older, in whom treatment for asthma is being considered, it is suggested that FeNO testing be done in addition to usual care. The guidelines do not recommend specific steps to modify treatment based on FeNO results but suggest a decision framework, reminding us that clinical context is key and FeNO is merely one signal. In recognizing its own fallibility, this document suggests that in the continually evolving world of asthma, the art of clinical medicine still reigns supreme.
Uddalak Majumdar, MDDr. Majumdar is a Fellow, Pulmonary & Critical Care Medicine, Respiratory Institute, Cleveland Clinic, Cleveland, Ohio.
Sleep medicine
Marijuana use in pregnancy
Marijuana is the most commonly used illegal drug in the United States. According to the CDC, about 1 in 20 women report using marijuana while pregnant (https://www.cdc.gov/marijuana/health-effects/pregnancy.html). As states legalize marijuana for medicinal or recreational purposes, its use by pregnant women could increase even further. While some use it to ease morning sickness and anxiety, they may not be aware that it can pose risks.
Research has been raising concerns about the effects of marijuana use during pregnancy for years. A study from 1978 linked maternal cannabis use with children’s behavioral problems and deficits in language comprehension, visual perception, attention, and memory (Life Sci. 1995;56[23-24]:2159-68). ). More recent research has linked use to low birth weight, reduced IQ, autism, delusional thoughts, and attention problems, although some other studies have not identified such associations.
A new study shows that children of women who use marijuana during or soon after pregnancy were twice as likely to become anxious, aggressive, or hyperactive. This corresponded with widespread reductions in immune-related gene expression in the placenta, which correlated with anxiety and hyperactivity (Proc National Acad Sci. 2021;118[47]e2106115118).
Chemicals from marijuana can be passed to the baby through breast milk. THC is stored in body fat and slowly released over time. Exposure could still occur even after stopping use (Marijuana use during pregnancy and lactation. ACOG Committee Opinion, Number 722, October 2017).
Studies have shown that THC can pass through the mother’s bloodstream to the placenta and the fetus. This occurs independent of how cannabis is consumed (smoking, vaping, eating, or oils/creams). Patients should be educated that no amount has been proven safe to use during pregnancy or breastfeeding.
Anita Rajagopal, MD, FCCP, Respiratory-Related Sleep Disorders Section, Member-at-Large
Dr. Rajagopal is Network Medical Director, Community Physician Network, Sleep Medicine/Medical Director, Community Health Network Sleep-Wake Disorders Center, Community Health Network, Indianapolis, Indiana.
Airway disorders
FeNO guidelines and the art of clinical medicine
The American Thoracic Society (ATS) recently published new guidelines on the use of fractional exhaled nitric oxide (FeNO) in the management of asthma (Khatri S. Am J Respir Crit Care Med. 2021;204[10]:e97-e109). The previous iteration dealt with questions about the interpretation of FeNO levels. However, the updated guidelines address a single question: Should patients with asthma in whom treatment is being contemplated undergo FeNO testing?
Several roles of nitric oxide (NO) have been discovered, including as a marker of eosinophilic airway inflammation or T2-inflammation. The fraction of NO during steady-state exhalation, easily measured by a handheld device, is a standardized quantitative noninvasive method to assess severity of airway eosinophilic inflammation. However, factors like concomitant sinusitis, bronchoconstriction, obesity, and smoking can also affect FeNO levels, and interpretation is context-dependent. Moreover, some biologic agents have variable effects on FeNO while still being effective in controlling T2 inflammation. Therefore, FeNO is neither the broadest nor the most sensitive signal of T2 inflammation, and there is much unknown about using FeNO to guide asthma treatment. Heterogeneity is one of the many challenges, as different endotypes and clinical subsets vary in the inflammatory pathways leading to airway hyperresponsiveness and remodeling.
The panel assessed the value of FeNO testing in improving asthma control questionnaire scores (ACT, ACQ-7), oral corticosteroid use, asthma exacerbations, lung function, health care utilization, and cost-effectiveness. FeNO-guided therapy compared with therapy without FeNO reduced exacerbations and oral corticosteroid use, though effect size was modest. Among other outcomes, while the trend favored FeNO, it did not reach statistical significance. Adverse effects of FeNO testing were trivial, and the cost is moderate though dependent on the institution size and testing frequency. Thus, for clinicians who manage adults and children 4 years of age and older, in whom treatment for asthma is being considered, it is suggested that FeNO testing be done in addition to usual care. The guidelines do not recommend specific steps to modify treatment based on FeNO results but suggest a decision framework, reminding us that clinical context is key and FeNO is merely one signal. In recognizing its own fallibility, this document suggests that in the continually evolving world of asthma, the art of clinical medicine still reigns supreme.
Uddalak Majumdar, MDDr. Majumdar is a Fellow, Pulmonary & Critical Care Medicine, Respiratory Institute, Cleveland Clinic, Cleveland, Ohio.
Sleep medicine
Marijuana use in pregnancy
Marijuana is the most commonly used illegal drug in the United States. According to the CDC, about 1 in 20 women report using marijuana while pregnant (https://www.cdc.gov/marijuana/health-effects/pregnancy.html). As states legalize marijuana for medicinal or recreational purposes, its use by pregnant women could increase even further. While some use it to ease morning sickness and anxiety, they may not be aware that it can pose risks.
Research has been raising concerns about the effects of marijuana use during pregnancy for years. A study from 1978 linked maternal cannabis use with children’s behavioral problems and deficits in language comprehension, visual perception, attention, and memory (Life Sci. 1995;56[23-24]:2159-68). ). More recent research has linked use to low birth weight, reduced IQ, autism, delusional thoughts, and attention problems, although some other studies have not identified such associations.
A new study shows that children of women who use marijuana during or soon after pregnancy were twice as likely to become anxious, aggressive, or hyperactive. This corresponded with widespread reductions in immune-related gene expression in the placenta, which correlated with anxiety and hyperactivity (Proc National Acad Sci. 2021;118[47]e2106115118).
Chemicals from marijuana can be passed to the baby through breast milk. THC is stored in body fat and slowly released over time. Exposure could still occur even after stopping use (Marijuana use during pregnancy and lactation. ACOG Committee Opinion, Number 722, October 2017).
Studies have shown that THC can pass through the mother’s bloodstream to the placenta and the fetus. This occurs independent of how cannabis is consumed (smoking, vaping, eating, or oils/creams). Patients should be educated that no amount has been proven safe to use during pregnancy or breastfeeding.
Anita Rajagopal, MD, FCCP, Respiratory-Related Sleep Disorders Section, Member-at-Large
Dr. Rajagopal is Network Medical Director, Community Physician Network, Sleep Medicine/Medical Director, Community Health Network Sleep-Wake Disorders Center, Community Health Network, Indianapolis, Indiana.
Airway disorders
FeNO guidelines and the art of clinical medicine
The American Thoracic Society (ATS) recently published new guidelines on the use of fractional exhaled nitric oxide (FeNO) in the management of asthma (Khatri S. Am J Respir Crit Care Med. 2021;204[10]:e97-e109). The previous iteration dealt with questions about the interpretation of FeNO levels. However, the updated guidelines address a single question: Should patients with asthma in whom treatment is being contemplated undergo FeNO testing?
Several roles of nitric oxide (NO) have been discovered, including as a marker of eosinophilic airway inflammation or T2-inflammation. The fraction of NO during steady-state exhalation, easily measured by a handheld device, is a standardized quantitative noninvasive method to assess severity of airway eosinophilic inflammation. However, factors like concomitant sinusitis, bronchoconstriction, obesity, and smoking can also affect FeNO levels, and interpretation is context-dependent. Moreover, some biologic agents have variable effects on FeNO while still being effective in controlling T2 inflammation. Therefore, FeNO is neither the broadest nor the most sensitive signal of T2 inflammation, and there is much unknown about using FeNO to guide asthma treatment. Heterogeneity is one of the many challenges, as different endotypes and clinical subsets vary in the inflammatory pathways leading to airway hyperresponsiveness and remodeling.
The panel assessed the value of FeNO testing in improving asthma control questionnaire scores (ACT, ACQ-7), oral corticosteroid use, asthma exacerbations, lung function, health care utilization, and cost-effectiveness. FeNO-guided therapy compared with therapy without FeNO reduced exacerbations and oral corticosteroid use, though effect size was modest. Among other outcomes, while the trend favored FeNO, it did not reach statistical significance. Adverse effects of FeNO testing were trivial, and the cost is moderate though dependent on the institution size and testing frequency. Thus, for clinicians who manage adults and children 4 years of age and older, in whom treatment for asthma is being considered, it is suggested that FeNO testing be done in addition to usual care. The guidelines do not recommend specific steps to modify treatment based on FeNO results but suggest a decision framework, reminding us that clinical context is key and FeNO is merely one signal. In recognizing its own fallibility, this document suggests that in the continually evolving world of asthma, the art of clinical medicine still reigns supreme.
Uddalak Majumdar, MDDr. Majumdar is a Fellow, Pulmonary & Critical Care Medicine, Respiratory Institute, Cleveland Clinic, Cleveland, Ohio.
Sleep medicine
Marijuana use in pregnancy
Marijuana is the most commonly used illegal drug in the United States. According to the CDC, about 1 in 20 women report using marijuana while pregnant (https://www.cdc.gov/marijuana/health-effects/pregnancy.html). As states legalize marijuana for medicinal or recreational purposes, its use by pregnant women could increase even further. While some use it to ease morning sickness and anxiety, they may not be aware that it can pose risks.
Research has been raising concerns about the effects of marijuana use during pregnancy for years. A study from 1978 linked maternal cannabis use with children’s behavioral problems and deficits in language comprehension, visual perception, attention, and memory (Life Sci. 1995;56[23-24]:2159-68). ). More recent research has linked use to low birth weight, reduced IQ, autism, delusional thoughts, and attention problems, although some other studies have not identified such associations.
A new study shows that children of women who use marijuana during or soon after pregnancy were twice as likely to become anxious, aggressive, or hyperactive. This corresponded with widespread reductions in immune-related gene expression in the placenta, which correlated with anxiety and hyperactivity (Proc National Acad Sci. 2021;118[47]e2106115118).
Chemicals from marijuana can be passed to the baby through breast milk. THC is stored in body fat and slowly released over time. Exposure could still occur even after stopping use (Marijuana use during pregnancy and lactation. ACOG Committee Opinion, Number 722, October 2017).
Studies have shown that THC can pass through the mother’s bloodstream to the placenta and the fetus. This occurs independent of how cannabis is consumed (smoking, vaping, eating, or oils/creams). Patients should be educated that no amount has been proven safe to use during pregnancy or breastfeeding.
Anita Rajagopal, MD, FCCP, Respiratory-Related Sleep Disorders Section, Member-at-Large
Dr. Rajagopal is Network Medical Director, Community Physician Network, Sleep Medicine/Medical Director, Community Health Network Sleep-Wake Disorders Center, Community Health Network, Indianapolis, Indiana.