User login
Take action: Turn up the heat on prior auth
In our recent member survey, 99% of respondents expressed that prior authorization has a negative impact on patients’ access to clinically appropriate treatments. We need to continue to put pressure on legislators to eliminate prior authorization burdens.
AGA endorses the Improving Seniors Timely Access to Care Act, which would streamline the prior authorization process in Medicare Advantage by approving in real-time commonly approved services and implementing a standardized electronic prior authorization process.
Despite large bipartisan support, we need your help getting this bill across the finish line! Please take five minutes to ask your Representative to cosponsor this necessary bill by participating in our campaign.
Go to the AGA action center to contact your lawmakers!
In our recent member survey, 99% of respondents expressed that prior authorization has a negative impact on patients’ access to clinically appropriate treatments. We need to continue to put pressure on legislators to eliminate prior authorization burdens.
AGA endorses the Improving Seniors Timely Access to Care Act, which would streamline the prior authorization process in Medicare Advantage by approving in real-time commonly approved services and implementing a standardized electronic prior authorization process.
Despite large bipartisan support, we need your help getting this bill across the finish line! Please take five minutes to ask your Representative to cosponsor this necessary bill by participating in our campaign.
Go to the AGA action center to contact your lawmakers!
In our recent member survey, 99% of respondents expressed that prior authorization has a negative impact on patients’ access to clinically appropriate treatments. We need to continue to put pressure on legislators to eliminate prior authorization burdens.
AGA endorses the Improving Seniors Timely Access to Care Act, which would streamline the prior authorization process in Medicare Advantage by approving in real-time commonly approved services and implementing a standardized electronic prior authorization process.
Despite large bipartisan support, we need your help getting this bill across the finish line! Please take five minutes to ask your Representative to cosponsor this necessary bill by participating in our campaign.
Go to the AGA action center to contact your lawmakers!
2022 AGA recognition prize award recipients

“AGA is proud to officially announce the exceptional individuals selected for 2022 AGA Recognition Prizes. I wish to thank all the nominators and those who provided nomination letters, and the selection committees for the tough task they had to select among the many superb nominees,” said Bishr Omary, MD, PhD, AGAF, chair of the AGA. “Please join us in congratulating this year’s distinguished awardees and applauding their contributions to the field of gastroenterology that advance our profession and the patients we serve.”
AGA looks forward to celebrating the recipients during Digestive Disease Week® 2022, May 21-24, in San Diego, Calif.
Meet and learn more about our award recipients here.

“AGA is proud to officially announce the exceptional individuals selected for 2022 AGA Recognition Prizes. I wish to thank all the nominators and those who provided nomination letters, and the selection committees for the tough task they had to select among the many superb nominees,” said Bishr Omary, MD, PhD, AGAF, chair of the AGA. “Please join us in congratulating this year’s distinguished awardees and applauding their contributions to the field of gastroenterology that advance our profession and the patients we serve.”
AGA looks forward to celebrating the recipients during Digestive Disease Week® 2022, May 21-24, in San Diego, Calif.
Meet and learn more about our award recipients here.

“AGA is proud to officially announce the exceptional individuals selected for 2022 AGA Recognition Prizes. I wish to thank all the nominators and those who provided nomination letters, and the selection committees for the tough task they had to select among the many superb nominees,” said Bishr Omary, MD, PhD, AGAF, chair of the AGA. “Please join us in congratulating this year’s distinguished awardees and applauding their contributions to the field of gastroenterology that advance our profession and the patients we serve.”
AGA looks forward to celebrating the recipients during Digestive Disease Week® 2022, May 21-24, in San Diego, Calif.
Meet and learn more about our award recipients here.
New governing board members
M. Bishr Omary, MD, PhD, AGAF, chair of the AGA Nominating Committee, is pleased to announce that Maria T. Abreu, MD, AGAF, joins the presidential line-up for AGA.
Vice President
Maria T. Abreu, MD, AGAF
Director, Crohn’s and Colitis Center
University of Miami
Maria T. Abreu, MD, AGAF, has more than 20 years of leadership experience in basic, translational, and clinical research and mentoring. She is AGA’s current councillor at-large, past chair of the AGA Institute Council, and an AGA Institute Council Section Research Mentor Award recipient (2020) for the IMIBD section. Dr. Abreu is also a recipient of the 2019 Sherman Prize by The Bruce and Cynthia Sherman Charitable Foundation that recognizes outstanding achievements in intestinal bowel disease.
Read her bio from the University of Miami.
The nominating committee also appointed the following slate of councillors which is subject to membership vote.
At-Large Councillor
Kim Barrett, PhD, AGAF
Vice dean for research
University of California, Davis
Kim Barrett, PhD, AGAF, is the current chair of the AGA Publications Committee, former chair of the AGA Ethics And Audit Committees, and served twice as director of the Academic Skills Workshop. She was recognized with AGA’s top research award, the AGA Distinguished Achievement Award in Basic Science (2021).
Her research interests have centered on the physiology and pathophysiology of the intestinal epithelium and their relevance to inflammatory bowel diseases and diarrheal diseases and have resulted in more than 300 publications.
Read her bio from UC Davis.
Councillor For Development And Growth
Lawrence Kosinski, MD, MBA, AGAF
Chief medical officer
SonarMD
A serial entrepreneur and thought leader in the world of value-based payment, Larry Kosinski, MD, MBA, AGAF, currently serves as chief medical officer of SonarMD, the leading value-based care coordination solution for complex chronic diseases. He founded SonarMD in 2014 to make it easier for specialists and patients to work together to manage symptomatic chronic illness and prevent clinical deterioration, improving health outcomes, and lowering the cost of care.
In 2021, Dr. Kosinski was selected for his expertise in value-based payment to serve on the Centers for Medicare & Medicaid Services’ Physician-Focused Payment Model Technical Advisory Committee and help develop bold, new Medicare payment models.
Read his bio from the SonarMD website.
Education & Training Councillor
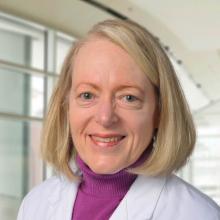
Sheryl Pfeil, MD, AGAF
Medical director and professor of clinical medicine, Clinical Skills Education and Assessment Center
The Ohio State University Wexner Medical Center
Sheryl Pfeil, MD, AGAF, has been an AGA member for 30 years, serving on the Education And Training Committee, as past chair of the Academy of Educators, as cochair of the AGA future leaders program, and on the editorial board for Gastro Hep Advances. Dr. Pfeil has 30 years of experience in medical education, leading medical students, residents, and fellow education.
Her educational research interests include professional development, training and assessment methods, and virtual education.
Read her bio from The Ohio State University.
Pending approval by the voting membership, all board members begin their terms after DDW 2022. The voting membership will be sent a ballot to approve the slate of councillors on or before March 28, 2022, with a response date of no later than April 29, 2022. Results will be announced at the AGA Annual Business Meeting on June 1, 2022.
M. Bishr Omary, MD, PhD, AGAF, chair of the AGA Nominating Committee, is pleased to announce that Maria T. Abreu, MD, AGAF, joins the presidential line-up for AGA.
Vice President
Maria T. Abreu, MD, AGAF
Director, Crohn’s and Colitis Center
University of Miami
Maria T. Abreu, MD, AGAF, has more than 20 years of leadership experience in basic, translational, and clinical research and mentoring. She is AGA’s current councillor at-large, past chair of the AGA Institute Council, and an AGA Institute Council Section Research Mentor Award recipient (2020) for the IMIBD section. Dr. Abreu is also a recipient of the 2019 Sherman Prize by The Bruce and Cynthia Sherman Charitable Foundation that recognizes outstanding achievements in intestinal bowel disease.
Read her bio from the University of Miami.
The nominating committee also appointed the following slate of councillors which is subject to membership vote.
At-Large Councillor
Kim Barrett, PhD, AGAF
Vice dean for research
University of California, Davis
Kim Barrett, PhD, AGAF, is the current chair of the AGA Publications Committee, former chair of the AGA Ethics And Audit Committees, and served twice as director of the Academic Skills Workshop. She was recognized with AGA’s top research award, the AGA Distinguished Achievement Award in Basic Science (2021).
Her research interests have centered on the physiology and pathophysiology of the intestinal epithelium and their relevance to inflammatory bowel diseases and diarrheal diseases and have resulted in more than 300 publications.
Read her bio from UC Davis.
Councillor For Development And Growth
Lawrence Kosinski, MD, MBA, AGAF
Chief medical officer
SonarMD
A serial entrepreneur and thought leader in the world of value-based payment, Larry Kosinski, MD, MBA, AGAF, currently serves as chief medical officer of SonarMD, the leading value-based care coordination solution for complex chronic diseases. He founded SonarMD in 2014 to make it easier for specialists and patients to work together to manage symptomatic chronic illness and prevent clinical deterioration, improving health outcomes, and lowering the cost of care.
In 2021, Dr. Kosinski was selected for his expertise in value-based payment to serve on the Centers for Medicare & Medicaid Services’ Physician-Focused Payment Model Technical Advisory Committee and help develop bold, new Medicare payment models.
Read his bio from the SonarMD website.
Education & Training Councillor
Sheryl Pfeil, MD, AGAF
Medical director and professor of clinical medicine, Clinical Skills Education and Assessment Center
The Ohio State University Wexner Medical Center
Sheryl Pfeil, MD, AGAF, has been an AGA member for 30 years, serving on the Education And Training Committee, as past chair of the Academy of Educators, as cochair of the AGA future leaders program, and on the editorial board for Gastro Hep Advances. Dr. Pfeil has 30 years of experience in medical education, leading medical students, residents, and fellow education.
Her educational research interests include professional development, training and assessment methods, and virtual education.
Read her bio from The Ohio State University.
Pending approval by the voting membership, all board members begin their terms after DDW 2022. The voting membership will be sent a ballot to approve the slate of councillors on or before March 28, 2022, with a response date of no later than April 29, 2022. Results will be announced at the AGA Annual Business Meeting on June 1, 2022.
M. Bishr Omary, MD, PhD, AGAF, chair of the AGA Nominating Committee, is pleased to announce that Maria T. Abreu, MD, AGAF, joins the presidential line-up for AGA.
Vice President
Maria T. Abreu, MD, AGAF
Director, Crohn’s and Colitis Center
University of Miami
Maria T. Abreu, MD, AGAF, has more than 20 years of leadership experience in basic, translational, and clinical research and mentoring. She is AGA’s current councillor at-large, past chair of the AGA Institute Council, and an AGA Institute Council Section Research Mentor Award recipient (2020) for the IMIBD section. Dr. Abreu is also a recipient of the 2019 Sherman Prize by The Bruce and Cynthia Sherman Charitable Foundation that recognizes outstanding achievements in intestinal bowel disease.
Read her bio from the University of Miami.
The nominating committee also appointed the following slate of councillors which is subject to membership vote.
At-Large Councillor
Kim Barrett, PhD, AGAF
Vice dean for research
University of California, Davis
Kim Barrett, PhD, AGAF, is the current chair of the AGA Publications Committee, former chair of the AGA Ethics And Audit Committees, and served twice as director of the Academic Skills Workshop. She was recognized with AGA’s top research award, the AGA Distinguished Achievement Award in Basic Science (2021).
Her research interests have centered on the physiology and pathophysiology of the intestinal epithelium and their relevance to inflammatory bowel diseases and diarrheal diseases and have resulted in more than 300 publications.
Read her bio from UC Davis.
Councillor For Development And Growth
Lawrence Kosinski, MD, MBA, AGAF
Chief medical officer
SonarMD
A serial entrepreneur and thought leader in the world of value-based payment, Larry Kosinski, MD, MBA, AGAF, currently serves as chief medical officer of SonarMD, the leading value-based care coordination solution for complex chronic diseases. He founded SonarMD in 2014 to make it easier for specialists and patients to work together to manage symptomatic chronic illness and prevent clinical deterioration, improving health outcomes, and lowering the cost of care.
In 2021, Dr. Kosinski was selected for his expertise in value-based payment to serve on the Centers for Medicare & Medicaid Services’ Physician-Focused Payment Model Technical Advisory Committee and help develop bold, new Medicare payment models.
Read his bio from the SonarMD website.
Education & Training Councillor
Sheryl Pfeil, MD, AGAF
Medical director and professor of clinical medicine, Clinical Skills Education and Assessment Center
The Ohio State University Wexner Medical Center
Sheryl Pfeil, MD, AGAF, has been an AGA member for 30 years, serving on the Education And Training Committee, as past chair of the Academy of Educators, as cochair of the AGA future leaders program, and on the editorial board for Gastro Hep Advances. Dr. Pfeil has 30 years of experience in medical education, leading medical students, residents, and fellow education.
Her educational research interests include professional development, training and assessment methods, and virtual education.
Read her bio from The Ohio State University.
Pending approval by the voting membership, all board members begin their terms after DDW 2022. The voting membership will be sent a ballot to approve the slate of councillors on or before March 28, 2022, with a response date of no later than April 29, 2022. Results will be announced at the AGA Annual Business Meeting on June 1, 2022.
Five reasons to update your will
You have a will, so you can rest easy, right? Not necessarily. Even though it can provide for some contingencies, an old will can’t cover every change that may have occurred since it was first drawn. Professionals advise that you review your will every few years and more often if situations such as the following five have occurred since you last updated your will.
#1. Family changes
If you’ve had any changes in your family situation, you will probably need to update your will. Events such as marriage, divorce, death, birth, adoption, or a falling out with a loved one may affect how your estate will be distributed, who should act as guardian for your dependents, and who should be named as executor of your estate.
#2. Relocating to a new state
The laws among the states vary. Moving to a new state or purchasing property in another state can affect your estate plan and how property in that state will be taxed and distributed.
#3. Tax law changes
Federal and state legislatures are continually tinkering with federal estate and state inheritance tax laws. An old will may fail to take advantage of strategies that will minimize estate taxes.
#4. You want to support a favorite cause
If you have developed a connection to a cause, you may want to benefit a particular charity with a gift in your estate. Contact us for sample language you can share with your attorney to include a gift to us in your will.
#5. Changes in your estate’s value
When you made your will, your assets may have been relatively modest. Now the value may be larger and your will no longer reflects how you would like your estate divided.
Consider including a gift to the AGA Research Foundation in your will. You will help spark future discoveries in GI. Visit our website at https://gastro.planmylegacy.org or contact us at [email protected].
You have a will, so you can rest easy, right? Not necessarily. Even though it can provide for some contingencies, an old will can’t cover every change that may have occurred since it was first drawn. Professionals advise that you review your will every few years and more often if situations such as the following five have occurred since you last updated your will.
#1. Family changes
If you’ve had any changes in your family situation, you will probably need to update your will. Events such as marriage, divorce, death, birth, adoption, or a falling out with a loved one may affect how your estate will be distributed, who should act as guardian for your dependents, and who should be named as executor of your estate.
#2. Relocating to a new state
The laws among the states vary. Moving to a new state or purchasing property in another state can affect your estate plan and how property in that state will be taxed and distributed.
#3. Tax law changes
Federal and state legislatures are continually tinkering with federal estate and state inheritance tax laws. An old will may fail to take advantage of strategies that will minimize estate taxes.
#4. You want to support a favorite cause
If you have developed a connection to a cause, you may want to benefit a particular charity with a gift in your estate. Contact us for sample language you can share with your attorney to include a gift to us in your will.
#5. Changes in your estate’s value
When you made your will, your assets may have been relatively modest. Now the value may be larger and your will no longer reflects how you would like your estate divided.
Consider including a gift to the AGA Research Foundation in your will. You will help spark future discoveries in GI. Visit our website at https://gastro.planmylegacy.org or contact us at [email protected].
You have a will, so you can rest easy, right? Not necessarily. Even though it can provide for some contingencies, an old will can’t cover every change that may have occurred since it was first drawn. Professionals advise that you review your will every few years and more often if situations such as the following five have occurred since you last updated your will.
#1. Family changes
If you’ve had any changes in your family situation, you will probably need to update your will. Events such as marriage, divorce, death, birth, adoption, or a falling out with a loved one may affect how your estate will be distributed, who should act as guardian for your dependents, and who should be named as executor of your estate.
#2. Relocating to a new state
The laws among the states vary. Moving to a new state or purchasing property in another state can affect your estate plan and how property in that state will be taxed and distributed.
#3. Tax law changes
Federal and state legislatures are continually tinkering with federal estate and state inheritance tax laws. An old will may fail to take advantage of strategies that will minimize estate taxes.
#4. You want to support a favorite cause
If you have developed a connection to a cause, you may want to benefit a particular charity with a gift in your estate. Contact us for sample language you can share with your attorney to include a gift to us in your will.
#5. Changes in your estate’s value
When you made your will, your assets may have been relatively modest. Now the value may be larger and your will no longer reflects how you would like your estate divided.
Consider including a gift to the AGA Research Foundation in your will. You will help spark future discoveries in GI. Visit our website at https://gastro.planmylegacy.org or contact us at [email protected].
The New Gastroenterologist seeks its next editor-in-chief
AGA’s cutting-edge, trainee and early-career focused e-newsletter The New Gastroenterologist (TNG) is seeking applications for the position of editor-in-chief (EIC). The role will facilitate the communication of the latest clinical advances among peers and build strong leadership skills managing editorial responsibilities as well as working with reviewers and fellow editors at AGA’s journals.
The term is from Oct. 1, 2022 – Sept. 30, 2027, with a transition period starting July 2022.
About TNG
TNG content covers highly relevant clinical topics, such as diverticular hemorrhage as well as microscopic colitis and diarrhea. Also included in each issue are articles that focus on career pathways, financial and legal matters, perspectives from private practice, brief reviews on clinically-relevant topics, issues in clinical medical ethics, and other topics that are relevant to early career GIs. Each issue also contains an introductory letter from the editor as well as a curated list of relevant articles from the AGA Journals.
Honorarium
The EIC will receive an annual honorarium of $5,000.
Qualifications
- AGA member, between second year of fellowship and five years post-fellowship.
- Experience identifying and promoting newsworthy content that is relevant to the trainee and early-career GI community, as well as excellent judgment that expands the outstanding reputation of TNG and AGA.
- Experience in medical, scientific or news-related publishing is preferred, but not required.
- Familiarity with AGA and its priorities, activities and stances on important issues is ideal, preferably via past volunteer member experience with the association.
- The EIC must be able to devote sufficient time to TNG matters and may not accept editorial appointments to competing publications during their tenure as EIC.
For more information or to apply view the full request for applications. If you have questions, please contact Ryan Farrell, managing editor, The New Gastroenterologist, at [email protected].
AGA’s cutting-edge, trainee and early-career focused e-newsletter The New Gastroenterologist (TNG) is seeking applications for the position of editor-in-chief (EIC). The role will facilitate the communication of the latest clinical advances among peers and build strong leadership skills managing editorial responsibilities as well as working with reviewers and fellow editors at AGA’s journals.
The term is from Oct. 1, 2022 – Sept. 30, 2027, with a transition period starting July 2022.
About TNG
TNG content covers highly relevant clinical topics, such as diverticular hemorrhage as well as microscopic colitis and diarrhea. Also included in each issue are articles that focus on career pathways, financial and legal matters, perspectives from private practice, brief reviews on clinically-relevant topics, issues in clinical medical ethics, and other topics that are relevant to early career GIs. Each issue also contains an introductory letter from the editor as well as a curated list of relevant articles from the AGA Journals.
Honorarium
The EIC will receive an annual honorarium of $5,000.
Qualifications
- AGA member, between second year of fellowship and five years post-fellowship.
- Experience identifying and promoting newsworthy content that is relevant to the trainee and early-career GI community, as well as excellent judgment that expands the outstanding reputation of TNG and AGA.
- Experience in medical, scientific or news-related publishing is preferred, but not required.
- Familiarity with AGA and its priorities, activities and stances on important issues is ideal, preferably via past volunteer member experience with the association.
- The EIC must be able to devote sufficient time to TNG matters and may not accept editorial appointments to competing publications during their tenure as EIC.
For more information or to apply view the full request for applications. If you have questions, please contact Ryan Farrell, managing editor, The New Gastroenterologist, at [email protected].
AGA’s cutting-edge, trainee and early-career focused e-newsletter The New Gastroenterologist (TNG) is seeking applications for the position of editor-in-chief (EIC). The role will facilitate the communication of the latest clinical advances among peers and build strong leadership skills managing editorial responsibilities as well as working with reviewers and fellow editors at AGA’s journals.
The term is from Oct. 1, 2022 – Sept. 30, 2027, with a transition period starting July 2022.
About TNG
TNG content covers highly relevant clinical topics, such as diverticular hemorrhage as well as microscopic colitis and diarrhea. Also included in each issue are articles that focus on career pathways, financial and legal matters, perspectives from private practice, brief reviews on clinically-relevant topics, issues in clinical medical ethics, and other topics that are relevant to early career GIs. Each issue also contains an introductory letter from the editor as well as a curated list of relevant articles from the AGA Journals.
Honorarium
The EIC will receive an annual honorarium of $5,000.
Qualifications
- AGA member, between second year of fellowship and five years post-fellowship.
- Experience identifying and promoting newsworthy content that is relevant to the trainee and early-career GI community, as well as excellent judgment that expands the outstanding reputation of TNG and AGA.
- Experience in medical, scientific or news-related publishing is preferred, but not required.
- Familiarity with AGA and its priorities, activities and stances on important issues is ideal, preferably via past volunteer member experience with the association.
- The EIC must be able to devote sufficient time to TNG matters and may not accept editorial appointments to competing publications during their tenure as EIC.
For more information or to apply view the full request for applications. If you have questions, please contact Ryan Farrell, managing editor, The New Gastroenterologist, at [email protected].
Register for the 2022 AGA Tech Summit
Innovative technologies for obesity management, emerging noninvasive diagnostic tools, and the AI revolution in health care are just some of the topics featured at the 2022 AGA Tech Summit, April 14-15, in San Francisco. Registration is now open.
This year’s Summit features a keynote lecture from Rajni Natesan, MD, MBA, chief medical officer for Braid Health, on how the power of data connectivity is being used in the transformation of health care.
The 2022 Summit continues to feature ancillary programs for physician innovators and trainees interested in innovation.
See the next big idea in gastroenterology. The Shark Tank competition is where GI innovators pitch their concepts to a panel of judges. Have an idea you think has potential
Get an exclusive behind-the-scenes tour of the MedTech world through the AGA Innovation Fellows Program. The program connects GI fellows in their third and fourth year, as well as those in advanced endoscopy fellowship programs, with successful physician innovators and industry thought leaders with the goals of sharpening their entrepreneurial talents and introducing careers in GI innovation.
Join the GI innovation community at the AGA Tech Summit and be part of it yourself.
Innovative technologies for obesity management, emerging noninvasive diagnostic tools, and the AI revolution in health care are just some of the topics featured at the 2022 AGA Tech Summit, April 14-15, in San Francisco. Registration is now open.
This year’s Summit features a keynote lecture from Rajni Natesan, MD, MBA, chief medical officer for Braid Health, on how the power of data connectivity is being used in the transformation of health care.
The 2022 Summit continues to feature ancillary programs for physician innovators and trainees interested in innovation.
See the next big idea in gastroenterology. The Shark Tank competition is where GI innovators pitch their concepts to a panel of judges. Have an idea you think has potential
Get an exclusive behind-the-scenes tour of the MedTech world through the AGA Innovation Fellows Program. The program connects GI fellows in their third and fourth year, as well as those in advanced endoscopy fellowship programs, with successful physician innovators and industry thought leaders with the goals of sharpening their entrepreneurial talents and introducing careers in GI innovation.
Join the GI innovation community at the AGA Tech Summit and be part of it yourself.
Innovative technologies for obesity management, emerging noninvasive diagnostic tools, and the AI revolution in health care are just some of the topics featured at the 2022 AGA Tech Summit, April 14-15, in San Francisco. Registration is now open.
This year’s Summit features a keynote lecture from Rajni Natesan, MD, MBA, chief medical officer for Braid Health, on how the power of data connectivity is being used in the transformation of health care.
The 2022 Summit continues to feature ancillary programs for physician innovators and trainees interested in innovation.
See the next big idea in gastroenterology. The Shark Tank competition is where GI innovators pitch their concepts to a panel of judges. Have an idea you think has potential
Get an exclusive behind-the-scenes tour of the MedTech world through the AGA Innovation Fellows Program. The program connects GI fellows in their third and fourth year, as well as those in advanced endoscopy fellowship programs, with successful physician innovators and industry thought leaders with the goals of sharpening their entrepreneurial talents and introducing careers in GI innovation.
Join the GI innovation community at the AGA Tech Summit and be part of it yourself.
Simple ways to create your legacy
Creating a legacy of giving is easier than you think. Take some time to start creating your legacy while supporting the AGA Research Foundation. Gifts to charitable organizations, such as the AGA Research Foundation, in your plans ensure your support for our mission continues for years to come.
Here are two ideas to help you get started.
- Name the AGA Research Foundation as a beneficiary. This arrangement is one of the most tax-smart ways to support the AGA Research Foundation after your lifetime. When you leave retirement plan assets to us, we bypass any taxes and receive the full amount.
- Include the AGA Research Foundation in your will or living trust. This gift can be made by including as little as one sentence in your will or living trust. Plus, your gift can be modified throughout your lifetime as circumstances change.
Want to learn more about including a gift to the AGA Research Foundation in your plans? Visit our website at https://gastro.planmylegacy.org.
Creating a legacy of giving is easier than you think. Take some time to start creating your legacy while supporting the AGA Research Foundation. Gifts to charitable organizations, such as the AGA Research Foundation, in your plans ensure your support for our mission continues for years to come.
Here are two ideas to help you get started.
- Name the AGA Research Foundation as a beneficiary. This arrangement is one of the most tax-smart ways to support the AGA Research Foundation after your lifetime. When you leave retirement plan assets to us, we bypass any taxes and receive the full amount.
- Include the AGA Research Foundation in your will or living trust. This gift can be made by including as little as one sentence in your will or living trust. Plus, your gift can be modified throughout your lifetime as circumstances change.
Want to learn more about including a gift to the AGA Research Foundation in your plans? Visit our website at https://gastro.planmylegacy.org.
Creating a legacy of giving is easier than you think. Take some time to start creating your legacy while supporting the AGA Research Foundation. Gifts to charitable organizations, such as the AGA Research Foundation, in your plans ensure your support for our mission continues for years to come.
Here are two ideas to help you get started.
- Name the AGA Research Foundation as a beneficiary. This arrangement is one of the most tax-smart ways to support the AGA Research Foundation after your lifetime. When you leave retirement plan assets to us, we bypass any taxes and receive the full amount.
- Include the AGA Research Foundation in your will or living trust. This gift can be made by including as little as one sentence in your will or living trust. Plus, your gift can be modified throughout your lifetime as circumstances change.
Want to learn more about including a gift to the AGA Research Foundation in your plans? Visit our website at https://gastro.planmylegacy.org.
Introducing the new AGA FORWARD Scholars
We’re proud to announce the 10 early-career physician-scientists selected as “Scholars” for the 2021-2023 AGA FORWARD Program: Fostering Opportunities Resulting in Workforce and Research Diversity, supported by NIH (1R25DK118761-01). This new cohort of Scholars will participate in a training and mentorship program designed to provide concrete and applicable skills to promote physician-scientists from underrepresented populations in the pursuit of successful careers.
“AGA is excited to announce our second cohort of FORWARD Program Scholars as we continue in our promise to inspire and cultivate the next generation of prominent, diverse leaders in gastroenterology and hepatology,” said Byron Cryer, MD, FORWARD Program cochair, AGA Equity Project cochair, and associate dean for the Office of Faculty Diversity & Development at UT Southwestern Medical Center, Dallas. “This class includes gastroenterology and hepatology’s most gifted leaders who are trailblazers for the future of academic medicine.”
- Muyiwa Awoniyi, MD, PhD
- Bubu Banini, MD, PhD
- Manuel Braga Neto, MD, PhD
- Jihane Benhammou, MD, PhD
- Cassandra Fritz, MD
- Joel Gabre, MD
- Rachel Issaka, MD, MAS
- Jeremy Louissaint, MD
- Vivian Ortiz, MD
- Nicolette Rodriguez, MD, MPH
Each Scholar has been paired with a top GI investigator for the duration of the program who will provide mentorship and help in developing the Scholar’s leadership skills and strengthening their research and management skills to ensure continued success in their careers. In addition to the GI mentors, the program will be introducing five “near-peer” mentors from the inaugural FORWARD cohort who will each serve as program guides for the current cohort Scholars.
Learn more about this program at https://www.gastro.org/aga-leadership/initiatives-and-programs/forward-program.
We’re proud to announce the 10 early-career physician-scientists selected as “Scholars” for the 2021-2023 AGA FORWARD Program: Fostering Opportunities Resulting in Workforce and Research Diversity, supported by NIH (1R25DK118761-01). This new cohort of Scholars will participate in a training and mentorship program designed to provide concrete and applicable skills to promote physician-scientists from underrepresented populations in the pursuit of successful careers.
“AGA is excited to announce our second cohort of FORWARD Program Scholars as we continue in our promise to inspire and cultivate the next generation of prominent, diverse leaders in gastroenterology and hepatology,” said Byron Cryer, MD, FORWARD Program cochair, AGA Equity Project cochair, and associate dean for the Office of Faculty Diversity & Development at UT Southwestern Medical Center, Dallas. “This class includes gastroenterology and hepatology’s most gifted leaders who are trailblazers for the future of academic medicine.”
- Muyiwa Awoniyi, MD, PhD
- Bubu Banini, MD, PhD
- Manuel Braga Neto, MD, PhD
- Jihane Benhammou, MD, PhD
- Cassandra Fritz, MD
- Joel Gabre, MD
- Rachel Issaka, MD, MAS
- Jeremy Louissaint, MD
- Vivian Ortiz, MD
- Nicolette Rodriguez, MD, MPH
Each Scholar has been paired with a top GI investigator for the duration of the program who will provide mentorship and help in developing the Scholar’s leadership skills and strengthening their research and management skills to ensure continued success in their careers. In addition to the GI mentors, the program will be introducing five “near-peer” mentors from the inaugural FORWARD cohort who will each serve as program guides for the current cohort Scholars.
Learn more about this program at https://www.gastro.org/aga-leadership/initiatives-and-programs/forward-program.
We’re proud to announce the 10 early-career physician-scientists selected as “Scholars” for the 2021-2023 AGA FORWARD Program: Fostering Opportunities Resulting in Workforce and Research Diversity, supported by NIH (1R25DK118761-01). This new cohort of Scholars will participate in a training and mentorship program designed to provide concrete and applicable skills to promote physician-scientists from underrepresented populations in the pursuit of successful careers.
“AGA is excited to announce our second cohort of FORWARD Program Scholars as we continue in our promise to inspire and cultivate the next generation of prominent, diverse leaders in gastroenterology and hepatology,” said Byron Cryer, MD, FORWARD Program cochair, AGA Equity Project cochair, and associate dean for the Office of Faculty Diversity & Development at UT Southwestern Medical Center, Dallas. “This class includes gastroenterology and hepatology’s most gifted leaders who are trailblazers for the future of academic medicine.”
- Muyiwa Awoniyi, MD, PhD
- Bubu Banini, MD, PhD
- Manuel Braga Neto, MD, PhD
- Jihane Benhammou, MD, PhD
- Cassandra Fritz, MD
- Joel Gabre, MD
- Rachel Issaka, MD, MAS
- Jeremy Louissaint, MD
- Vivian Ortiz, MD
- Nicolette Rodriguez, MD, MPH
Each Scholar has been paired with a top GI investigator for the duration of the program who will provide mentorship and help in developing the Scholar’s leadership skills and strengthening their research and management skills to ensure continued success in their careers. In addition to the GI mentors, the program will be introducing five “near-peer” mentors from the inaugural FORWARD cohort who will each serve as program guides for the current cohort Scholars.
Learn more about this program at https://www.gastro.org/aga-leadership/initiatives-and-programs/forward-program.
Gut Microbiota for Health World Summit 2022
Registration is now open for the Gut Microbiota for Health (GMFH) World Summit 2022, taking place March 12-13 in Washington, D.C., and virtually.
Organized by AGA and the European Society of Neurogastroenterology and Motility (ESNM), the GMFH World Summit is the preeminent international meeting on the gut microbiome for clinicians, dietitians and researchers.
Now in its 10th year, the program for this year’s conference will focus on “The Gut Microbiome in Precision Nutrition and Medicine.” Join us to gain a deeper understanding of the role of the gut microbiome in precision medicine and discover personalized approaches to modulating the gut microbiome that may promote health and improve patient outcomes for a variety of disorders and diseases.
Registration is now open for the Gut Microbiota for Health (GMFH) World Summit 2022, taking place March 12-13 in Washington, D.C., and virtually.
Organized by AGA and the European Society of Neurogastroenterology and Motility (ESNM), the GMFH World Summit is the preeminent international meeting on the gut microbiome for clinicians, dietitians and researchers.
Now in its 10th year, the program for this year’s conference will focus on “The Gut Microbiome in Precision Nutrition and Medicine.” Join us to gain a deeper understanding of the role of the gut microbiome in precision medicine and discover personalized approaches to modulating the gut microbiome that may promote health and improve patient outcomes for a variety of disorders and diseases.
Registration is now open for the Gut Microbiota for Health (GMFH) World Summit 2022, taking place March 12-13 in Washington, D.C., and virtually.
Organized by AGA and the European Society of Neurogastroenterology and Motility (ESNM), the GMFH World Summit is the preeminent international meeting on the gut microbiome for clinicians, dietitians and researchers.
Now in its 10th year, the program for this year’s conference will focus on “The Gut Microbiome in Precision Nutrition and Medicine.” Join us to gain a deeper understanding of the role of the gut microbiome in precision medicine and discover personalized approaches to modulating the gut microbiome that may promote health and improve patient outcomes for a variety of disorders and diseases.
See Gastroenterology’s curated ‘Equity in GI’ journal collection
Gastroenterology, an AGA journal, is proud to announce the release of a special collection of articles focused on the intersection of diversity, equity, and inclusion (DEI) within gastroenterology and hepatology. This curated collection, under the guidance of the journal’s new DEI section editor Chyke Doubeni, MBBS, MPH, includes original research, reviews, commentaries, and editorials on matters of health disparities, socioeconomic determinants of health outcomes, and population-based studies on disease incidence among races and ethnicities, among others. New articles are added to the collection as they are published.
View the special collection on Gastroenterology’s website, which is designed to help you quickly and easily look over the latest DEI articles and content of interest. Recent articles include the following:
- “How to incorporate health equity training into GI/hepatology fellowships,” by Jannel Lee-Allen, MD, and Brijen J. Shah, MD.
- “Disparities in preventable mortality from colorectal cancer: Are they the result of structural racism?” by Chyke A. Doubeni, MBBS, MPH; Kevin Selby, MD; and Theodore R. Levin, MD.
- “COVID-19 pediatric patients: GI symptoms, presentations and disparities by race/ethnicity in a large, multicenter U.S. study,” by Yusuf Ashktorab, MD; Anas Brim, MD; Antonio Pizuorno, MD; Vijay Gayam, MD; Sahar Nikdel, MD; and Hassan Brim, PhD.
View all of Gastroenterology’s curated article collections.
Gastroenterology, an AGA journal, is proud to announce the release of a special collection of articles focused on the intersection of diversity, equity, and inclusion (DEI) within gastroenterology and hepatology. This curated collection, under the guidance of the journal’s new DEI section editor Chyke Doubeni, MBBS, MPH, includes original research, reviews, commentaries, and editorials on matters of health disparities, socioeconomic determinants of health outcomes, and population-based studies on disease incidence among races and ethnicities, among others. New articles are added to the collection as they are published.
View the special collection on Gastroenterology’s website, which is designed to help you quickly and easily look over the latest DEI articles and content of interest. Recent articles include the following:
- “How to incorporate health equity training into GI/hepatology fellowships,” by Jannel Lee-Allen, MD, and Brijen J. Shah, MD.
- “Disparities in preventable mortality from colorectal cancer: Are they the result of structural racism?” by Chyke A. Doubeni, MBBS, MPH; Kevin Selby, MD; and Theodore R. Levin, MD.
- “COVID-19 pediatric patients: GI symptoms, presentations and disparities by race/ethnicity in a large, multicenter U.S. study,” by Yusuf Ashktorab, MD; Anas Brim, MD; Antonio Pizuorno, MD; Vijay Gayam, MD; Sahar Nikdel, MD; and Hassan Brim, PhD.
View all of Gastroenterology’s curated article collections.
Gastroenterology, an AGA journal, is proud to announce the release of a special collection of articles focused on the intersection of diversity, equity, and inclusion (DEI) within gastroenterology and hepatology. This curated collection, under the guidance of the journal’s new DEI section editor Chyke Doubeni, MBBS, MPH, includes original research, reviews, commentaries, and editorials on matters of health disparities, socioeconomic determinants of health outcomes, and population-based studies on disease incidence among races and ethnicities, among others. New articles are added to the collection as they are published.
View the special collection on Gastroenterology’s website, which is designed to help you quickly and easily look over the latest DEI articles and content of interest. Recent articles include the following:
- “How to incorporate health equity training into GI/hepatology fellowships,” by Jannel Lee-Allen, MD, and Brijen J. Shah, MD.
- “Disparities in preventable mortality from colorectal cancer: Are they the result of structural racism?” by Chyke A. Doubeni, MBBS, MPH; Kevin Selby, MD; and Theodore R. Levin, MD.
- “COVID-19 pediatric patients: GI symptoms, presentations and disparities by race/ethnicity in a large, multicenter U.S. study,” by Yusuf Ashktorab, MD; Anas Brim, MD; Antonio Pizuorno, MD; Vijay Gayam, MD; Sahar Nikdel, MD; and Hassan Brim, PhD.
View all of Gastroenterology’s curated article collections.