User login
Wells Score Can't Rule Out Deep Vein Thrombosis in Inpatient Setting
Clinical question: Should the Wells score be used for DVT risk stratification in the hospital?
Background: The Wells score was derived to reduce lower extremity ultrasounds (LEUS) in the outpatient evaluation of DVTs. There has never been a large prospective trial to validate its use in hospitalized patients.
Study design: Single-center, prospective cohort study.
Setting: Quaternary care, academic hospital.
Synopsis: Between November 2012 and December 2013, all inpatients at a single medical center who underwent a LEUS for suspected DVT, including 1,135 inpatients 16 years or older, had Wells risk factors recorded. The incidence of proximal DVTs noted for low, moderate, and high pretest probability groups were 5.9%, 9.5%, and 16.4%, respectively. Compared to the outpatient incidence of 3.0%, 16.6%, and 74.6% reported by Wells and colleagues, there were nonsignificant differences among inpatient groups. The difference between low and moderate pretest probability groups was not significant.
Discrimination of risk for DVT in hospitalized patients performed only slightly better than chance (AUC, 0.60) and the failure rate was double that of the original outpatient study (5.9% vs. 3.0%).
A possible explanation for these findings is the increased prevalence of immobilization (6x), cancer (3x), and risk factors not included in the Wells score (COPD, heart failure, and infection) in hospitalized patients.
Bottom line: The Wells score may not be sufficient to rule out DVT or influence management in the inpatient setting.
Citation: Silveira PC, Ip IK, Goldhaber SZ, Piazza G, Benson CB, Khorasani R. Performance of Wells score for deep vein thrombosis in the inpatient setting. JAMA Intern Med. 2015;175(7):1112-1117.
Clinical question: Should the Wells score be used for DVT risk stratification in the hospital?
Background: The Wells score was derived to reduce lower extremity ultrasounds (LEUS) in the outpatient evaluation of DVTs. There has never been a large prospective trial to validate its use in hospitalized patients.
Study design: Single-center, prospective cohort study.
Setting: Quaternary care, academic hospital.
Synopsis: Between November 2012 and December 2013, all inpatients at a single medical center who underwent a LEUS for suspected DVT, including 1,135 inpatients 16 years or older, had Wells risk factors recorded. The incidence of proximal DVTs noted for low, moderate, and high pretest probability groups were 5.9%, 9.5%, and 16.4%, respectively. Compared to the outpatient incidence of 3.0%, 16.6%, and 74.6% reported by Wells and colleagues, there were nonsignificant differences among inpatient groups. The difference between low and moderate pretest probability groups was not significant.
Discrimination of risk for DVT in hospitalized patients performed only slightly better than chance (AUC, 0.60) and the failure rate was double that of the original outpatient study (5.9% vs. 3.0%).
A possible explanation for these findings is the increased prevalence of immobilization (6x), cancer (3x), and risk factors not included in the Wells score (COPD, heart failure, and infection) in hospitalized patients.
Bottom line: The Wells score may not be sufficient to rule out DVT or influence management in the inpatient setting.
Citation: Silveira PC, Ip IK, Goldhaber SZ, Piazza G, Benson CB, Khorasani R. Performance of Wells score for deep vein thrombosis in the inpatient setting. JAMA Intern Med. 2015;175(7):1112-1117.
Clinical question: Should the Wells score be used for DVT risk stratification in the hospital?
Background: The Wells score was derived to reduce lower extremity ultrasounds (LEUS) in the outpatient evaluation of DVTs. There has never been a large prospective trial to validate its use in hospitalized patients.
Study design: Single-center, prospective cohort study.
Setting: Quaternary care, academic hospital.
Synopsis: Between November 2012 and December 2013, all inpatients at a single medical center who underwent a LEUS for suspected DVT, including 1,135 inpatients 16 years or older, had Wells risk factors recorded. The incidence of proximal DVTs noted for low, moderate, and high pretest probability groups were 5.9%, 9.5%, and 16.4%, respectively. Compared to the outpatient incidence of 3.0%, 16.6%, and 74.6% reported by Wells and colleagues, there were nonsignificant differences among inpatient groups. The difference between low and moderate pretest probability groups was not significant.
Discrimination of risk for DVT in hospitalized patients performed only slightly better than chance (AUC, 0.60) and the failure rate was double that of the original outpatient study (5.9% vs. 3.0%).
A possible explanation for these findings is the increased prevalence of immobilization (6x), cancer (3x), and risk factors not included in the Wells score (COPD, heart failure, and infection) in hospitalized patients.
Bottom line: The Wells score may not be sufficient to rule out DVT or influence management in the inpatient setting.
Citation: Silveira PC, Ip IK, Goldhaber SZ, Piazza G, Benson CB, Khorasani R. Performance of Wells score for deep vein thrombosis in the inpatient setting. JAMA Intern Med. 2015;175(7):1112-1117.
Antibiotic Therapy, Appendectomy for Uncomplicated Acute Appendicitis
Clinical question: Is antibiotic therapy noninferior to appendectomy for treatment of uncomplicated acute appendicitis?
Background: Previous randomized clinical trials have compared antibiotic therapy versus appendectomy for the treatment of uncomplicated, acute appendicitis. Each of these studies had significant limitations, and appendectomy has remained the standard of care.
Study design: Noninferiority, randomized clinical trial.
Setting: Six hospitals in Finland.
Synopsis: Investigators randomized 530 patients with uncomplicated appendicitis confirmed on CT to appendectomy or antibiotic therapy, with a noninferiority margin of 24%. Of the 256 patients randomized to antibiotics who were available for follow-up, 70 received surgical intervention within one year. This resulted in a difference between treatment groups of -27%. Further analysis revealed that five of those patients had normal appendices and did not actually require appendectomy. Secondary outcome analysis demonstrated a significantly lower complication rate among patients in the antibiotic group (2.8%) compared with the surgical group (20.5%); however, the open operative approach used on most patients may have resulted in increased wound complications.
Although noninferiority of antibiotic treatment was not demonstrated, the majority of patients in the antibiotic group (73%) were found to have successful treatment with antibiotics alone. None of these patients, including those eventually undergoing appendectomy, suffered major complications. Although the overall approach to uncomplicated appendicitis may not change, physicians and patients should utilize this data to make an informed decision between antibiotic treatment and appendectomy.
Bottom line: In patients with CT-proven, uncomplicated acute appendicitis, antibiotic treatment did not meet the pre-specified threshold for noninferiority compared with appendectomy, yet a significant majority of patients in the antibiotic arm had successful recovery.
Citation: Salminen P, Paajanen H, Rautio T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: The APPAC randomized clinical trial. JAMA. 2015;313(23):2340-2348
Clinical question: Is antibiotic therapy noninferior to appendectomy for treatment of uncomplicated acute appendicitis?
Background: Previous randomized clinical trials have compared antibiotic therapy versus appendectomy for the treatment of uncomplicated, acute appendicitis. Each of these studies had significant limitations, and appendectomy has remained the standard of care.
Study design: Noninferiority, randomized clinical trial.
Setting: Six hospitals in Finland.
Synopsis: Investigators randomized 530 patients with uncomplicated appendicitis confirmed on CT to appendectomy or antibiotic therapy, with a noninferiority margin of 24%. Of the 256 patients randomized to antibiotics who were available for follow-up, 70 received surgical intervention within one year. This resulted in a difference between treatment groups of -27%. Further analysis revealed that five of those patients had normal appendices and did not actually require appendectomy. Secondary outcome analysis demonstrated a significantly lower complication rate among patients in the antibiotic group (2.8%) compared with the surgical group (20.5%); however, the open operative approach used on most patients may have resulted in increased wound complications.
Although noninferiority of antibiotic treatment was not demonstrated, the majority of patients in the antibiotic group (73%) were found to have successful treatment with antibiotics alone. None of these patients, including those eventually undergoing appendectomy, suffered major complications. Although the overall approach to uncomplicated appendicitis may not change, physicians and patients should utilize this data to make an informed decision between antibiotic treatment and appendectomy.
Bottom line: In patients with CT-proven, uncomplicated acute appendicitis, antibiotic treatment did not meet the pre-specified threshold for noninferiority compared with appendectomy, yet a significant majority of patients in the antibiotic arm had successful recovery.
Citation: Salminen P, Paajanen H, Rautio T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: The APPAC randomized clinical trial. JAMA. 2015;313(23):2340-2348
Clinical question: Is antibiotic therapy noninferior to appendectomy for treatment of uncomplicated acute appendicitis?
Background: Previous randomized clinical trials have compared antibiotic therapy versus appendectomy for the treatment of uncomplicated, acute appendicitis. Each of these studies had significant limitations, and appendectomy has remained the standard of care.
Study design: Noninferiority, randomized clinical trial.
Setting: Six hospitals in Finland.
Synopsis: Investigators randomized 530 patients with uncomplicated appendicitis confirmed on CT to appendectomy or antibiotic therapy, with a noninferiority margin of 24%. Of the 256 patients randomized to antibiotics who were available for follow-up, 70 received surgical intervention within one year. This resulted in a difference between treatment groups of -27%. Further analysis revealed that five of those patients had normal appendices and did not actually require appendectomy. Secondary outcome analysis demonstrated a significantly lower complication rate among patients in the antibiotic group (2.8%) compared with the surgical group (20.5%); however, the open operative approach used on most patients may have resulted in increased wound complications.
Although noninferiority of antibiotic treatment was not demonstrated, the majority of patients in the antibiotic group (73%) were found to have successful treatment with antibiotics alone. None of these patients, including those eventually undergoing appendectomy, suffered major complications. Although the overall approach to uncomplicated appendicitis may not change, physicians and patients should utilize this data to make an informed decision between antibiotic treatment and appendectomy.
Bottom line: In patients with CT-proven, uncomplicated acute appendicitis, antibiotic treatment did not meet the pre-specified threshold for noninferiority compared with appendectomy, yet a significant majority of patients in the antibiotic arm had successful recovery.
Citation: Salminen P, Paajanen H, Rautio T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: The APPAC randomized clinical trial. JAMA. 2015;313(23):2340-2348
Social, System Factors Can Influence Decisions to Continue Patient Care
Clinical question: Why do healthcare providers work while sick?
Background: Healthcare providers generally are aware of the risks of infection to hospitalized patients; however, despite this knowledge, several studies have revealed providers continue to work while ill.
Study design: Mixed-method analysis of a cross-sectional survey.
Setting: Large academic children’s hospital.
Synopsis: Investigators completed 538 of 929 surveys of attending physicians and advanced practice clinicians (APCs), a response rate of 58%. Of the respondents, 95% agreed that sick providers continuing patient care increased their patients’ risk for infection; however, 83% admitted to caring for patients while sick, with physicians being more likely to do so.
Several factors contributed to this behavior, including fear of letting colleagues or patients down, fear of ostracism by colleagues, and concerns for understaffing or discontinuity of care. Qualitative analysis of free-text responses revealed additional factors, including the difficulty of finding sick coverage, the strong cultural norms to continue working unless severely ill, and the ambiguity of defining “too sick to work.”
Limitations of this study included possible response bias, lack of a validated survey, and inclusion of only a single center; however, results confirm prior studies and reveal additional systems factors that hospital leadership could address, supporting providers and improving patient care.
Bottom line: Sick healthcare providers face several challenges that drive them to put their patients at risk by continuing patient care, and these factors could be addressed by healthcare systems as a means of improving overall quality of care.
Citation: Szymczak JE, Smathers S, Hoegg C, Klieger S, Coffin SE, Sammons JS. Reasons why physicians and advanced practice clinicians work while sick: a mixed-methods analysis. JAMA Pediatr. 2015;169(9):815-821. doi:10.1001/jamapediatrics.2015.0684.
Clinical question: Why do healthcare providers work while sick?
Background: Healthcare providers generally are aware of the risks of infection to hospitalized patients; however, despite this knowledge, several studies have revealed providers continue to work while ill.
Study design: Mixed-method analysis of a cross-sectional survey.
Setting: Large academic children’s hospital.
Synopsis: Investigators completed 538 of 929 surveys of attending physicians and advanced practice clinicians (APCs), a response rate of 58%. Of the respondents, 95% agreed that sick providers continuing patient care increased their patients’ risk for infection; however, 83% admitted to caring for patients while sick, with physicians being more likely to do so.
Several factors contributed to this behavior, including fear of letting colleagues or patients down, fear of ostracism by colleagues, and concerns for understaffing or discontinuity of care. Qualitative analysis of free-text responses revealed additional factors, including the difficulty of finding sick coverage, the strong cultural norms to continue working unless severely ill, and the ambiguity of defining “too sick to work.”
Limitations of this study included possible response bias, lack of a validated survey, and inclusion of only a single center; however, results confirm prior studies and reveal additional systems factors that hospital leadership could address, supporting providers and improving patient care.
Bottom line: Sick healthcare providers face several challenges that drive them to put their patients at risk by continuing patient care, and these factors could be addressed by healthcare systems as a means of improving overall quality of care.
Citation: Szymczak JE, Smathers S, Hoegg C, Klieger S, Coffin SE, Sammons JS. Reasons why physicians and advanced practice clinicians work while sick: a mixed-methods analysis. JAMA Pediatr. 2015;169(9):815-821. doi:10.1001/jamapediatrics.2015.0684.
Clinical question: Why do healthcare providers work while sick?
Background: Healthcare providers generally are aware of the risks of infection to hospitalized patients; however, despite this knowledge, several studies have revealed providers continue to work while ill.
Study design: Mixed-method analysis of a cross-sectional survey.
Setting: Large academic children’s hospital.
Synopsis: Investigators completed 538 of 929 surveys of attending physicians and advanced practice clinicians (APCs), a response rate of 58%. Of the respondents, 95% agreed that sick providers continuing patient care increased their patients’ risk for infection; however, 83% admitted to caring for patients while sick, with physicians being more likely to do so.
Several factors contributed to this behavior, including fear of letting colleagues or patients down, fear of ostracism by colleagues, and concerns for understaffing or discontinuity of care. Qualitative analysis of free-text responses revealed additional factors, including the difficulty of finding sick coverage, the strong cultural norms to continue working unless severely ill, and the ambiguity of defining “too sick to work.”
Limitations of this study included possible response bias, lack of a validated survey, and inclusion of only a single center; however, results confirm prior studies and reveal additional systems factors that hospital leadership could address, supporting providers and improving patient care.
Bottom line: Sick healthcare providers face several challenges that drive them to put their patients at risk by continuing patient care, and these factors could be addressed by healthcare systems as a means of improving overall quality of care.
Citation: Szymczak JE, Smathers S, Hoegg C, Klieger S, Coffin SE, Sammons JS. Reasons why physicians and advanced practice clinicians work while sick: a mixed-methods analysis. JAMA Pediatr. 2015;169(9):815-821. doi:10.1001/jamapediatrics.2015.0684.
COPD Exacerbation Prevention: April 2015 CHEST Guidelines
Background
The CHEST guidelines for the prevention of acute exacerbations of chronic obstructive pulmonary disease (AECOPD) were developed through a collaboration between the American College of Chest Physicians (CHEST) and the Canadian Thoracic Society (CTS). They are the first evidence-based guidelines dedicated entirely to the prevention of AECOPD and largely exclude material related to the treatment of symptomatic disease.1
Patients with AECOPD are commonly cared for by hospitalists, so we fill an important role in the longitudinal treatment of this disease. Acute exacerbations and hospitalizations for COPD account for 50% of all COPD-related expenses.2,3 Further, the Agency for Healthcare Research and Quality showed a 20% readmission rate nationally for AECOPD, far higher than the rate for most other diagnoses.4 Consequently, COPD readmission has been added to Medicare’s Hospital Readmissions Reduction Program for fiscal year 2015.5
Hospitalization, when the patient is a captive audience and many of the necessary resources are available, may be a time to initiate preventative strategies.
Guideline Updates
The guidelines for non-pharmacologic interventions start with vaccination and continue with behavioral modification. They support the use of the 23-valent polysaccharide pneumococcal vaccine and annual influenza vaccination, noting that only influenza vaccination has been shown to decrease AECOPD.
Pulmonary rehabilitation is recommended for patients with a recent (fewer than four weeks) exacerbation. Several recommendations favor combining social work interventions with education, adding that face-to-face verbal education is superior to written educational materials. Interestingly, smoking cessation interventions received a weak recommendation, based upon lack of literature specifically focusing on the prevention of AECOPD. Despite this recommendation, smoking cessation intervention is strongly encouraged by the authors, given evidence of a marked reduction in morbidity, mortality, and healthcare utilization among smokers with COPD who quit.6 Finally, telemonitoring is not considered to be superior to usual care.
The guidelines concerning inhaled therapies fall into three major drug classes, including short- and long-acting inhaled muscarinic antagonists (anticholinergic agents), short- and long-acting inhaled beta-agonists, and inhaled corticosteroids.
Long-acting medications are generally considered more effective in preventing exacerbations than those that are short acting. Long-acting muscarinic antagonists (LAMAs) are highlighted for their efficacy, and combination inhaled long-acting beta-agonists (LABAs) and inhaled corticosteroids are preferred over monotherapy with either agent alone. LAMAs are preferred to inhaled corticosteroids or LABAs when given as monotherapy.
Short-acting agents are rated as inferior at preventing exacerbations compared to their long-acting analogs, but short-acting medications are better than placebo when combined with long-acting agents from other drug classes. Triple drug therapy (inhaled LAMAs, LABAs, and corticosteroids) can be considered based on current evidence.
The final recommendations address the use of oral medications. A potentially practice-changing guideline is the recommendation for long-term use of N-acetylcysteine tablets twice daily for patients who have experienced more than two exacerbations within two years. A more intuitive recommendation in this group is that treating an AECOPD with oral or IV steroids decreases the chance of recurrent exacerbations in the future.
The remaining recommendations include daily macrolide therapy, the phosphodiesterate-4 inhibitor roflumilast for those with chronic bronchitis and a recent exacerbation, and slow-release theophylline for stable disease. These guidelines also point out that statins do not have a role in AECOPD prevention. An expert consensus also recommends carbocysteine for patients who have failed “maximal” therapy.1
Established Guideline Analysis
Prior guidelines that address stable COPD do exist, most notably from Quaseem and colleagues in the 2011 Annals of Internal Medicine (AIM) and the 2015 GOLD guidelines.7,8 The prior guidelines published in AIM offered limited recommendations on the preventative interventions of bronchodilator use, pulmonary rehabilitation, and oxygen use.
The recommendations made in AIM are similar to those in the CHEST guidelines; the lack of breadth in the AIM report reflects new data generated over the last half decade. They include preventing causative exposures (e.g. tobacco, occupational), recommending bronchodilator use (with or without inhaled corticosteroids), possibly using phosphodiesterase-4 inhibitors (PD-4 inhibitors), administering appropriate vaccines, and providing education; however, GOLD does not actually present or rate the evidence associated with those recommendations. GOLD does specifically state that statins have no role in AECOPD prevention, a position that is updated from more recent literature.8,9
The National Guideline Clearinghouse (NGC) also includes some references to prevention of AECOPD but has no sections explicitly dedicated to prevention. Of note, the NGC still endorses statin use and does not appear to have incorporated data from newer studies.8,10
Hospitalist Takeaways
Given the high rate of COPD readmissions and its broad impact on morbidity and healthcare costs, measures to prevent COPD exacerbations cannot remain out of scope of care for inpatient physicians. It is important to initiate pulmonary rehab within four weeks of an exacerbation of COPD to prevent future exacerbations. Systems should be put in place to assure that all patients who qualify are vaccinated for influenza and patients who continue to smoke receive cessation counseling.
Today, hospitalists are comfortable with these non-pharmacologic interventions, as well as medications that include inhaled bronchodilators, nebulized medications, macrolide maintenance therapy, and oral steroids; however, other oral medications, such as phosphodiesterase inhibitors, theophylline, and N-acetylcysteine, may be appropriate for select patients, and hospitalists should become more familiar with their utility.11,12,13,14
Finally, it is important to note that both short- and long-acting inhaled muscarinic antagonists have come to the forefront of pharmacologic interventions for COPD exacerbation prevention.
Dr. Lampman, MD, is a hospitalist, consulting provider, and physician leader of the physician advisor program at Duke Regional Hospital in Durham, N.C. Dr. Lovins is a hospitalist, associate chief medical informatics officer, and assistant professor of medicine at Duke University and Duke Regional Hospital.
References
- Criner GJ, Bourbeau J, Diekemper RL, et al. Prevention of acute exacerbations of COPD: American College of Chest Physicians and Canadian Thoracic Society Guideline. Chest. 2015;147(4):894-942.
- Miravitlles M, Garcia-Polo C, Domenech A, Villegas G, Conget F, de la Roza C. Clinical outcomes and cost analysis of exacerbations in chronic obstructive pulmonary disease. Lung. 2013;191(5):523-530.
- Miravitlles M, Murio C, Guerrero T, Gisbert R; DAFNE Study Group. Pharmacoeconomic evaluation of acute exacerbations of chronic bronchitis and COPD. Chest. 2002;121(5):1449-1455.
- Elixhauser A, Au DH, Podulka J. Readmissions for Chronic Obstructive Pulmonary Disease, 2008: Statistical Brief #121.In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, Md.: Agency for Health Care Policy and Research: 2006.
- Readmissions Reduction Program. Centers for Medicare and Medicaid Services website. Accessed September 8, 2015.
- Sicras-Mainar A, Rejas-Gutiérrez J, Navarro-Artieda R, Ibáñez-Nolla J. The effect of quitting smoking on costs and healthcare utilization in patients with chronic obstructive pulmonary disease: a comparison of current smokers versus ex-smokers in routine clinical practice. Lung. 2014;192(4):505-518.
- Qaseem A, Wilt TJ, Weinberger SE, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179-191.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2015. Global Strategy for the Diagnosis, Management, and Prevention of COPD. Accessed September 8, 2015.
- Criner GJ, Connett JE, Aaron SK, et al. Simvastatin for the prevention of exacerbations in moderate-to-severe COPD. N Engl J Med. 2014;370(23):2201-2210.
- Agency for Healthcare Research and Quality. National Guideline Clearinghouse. COPD – chronic obstructive pulmonary disease. In: Pulmonary (acute & chronic). Accessed September 8, 2015.
- Cazzola M, Matera MG. N-acetylcysteine in COPD may be beneficial, but for whom? Lancet Respir Med. 2014;2(3):166-167.
- Turner RD Bothamley. N-acetylcysteine for COPD: the evidence remains inconclusive. Lancet Respir Med. 2014;2(4):e3.
- Zheng JP, Wen FQ, Bai CX, et al. Twice daily N-acetylcysteine 600 mg for exacerbations of chronic obstructive pulmonary disease (PANTHEON): a randomised, double-blind placebo-controlled trial. Lancet Respir Med. 2014;2(3):187-194.
- Amazon.com. Amazon Search. 2015 06/1/2015].
Background
The CHEST guidelines for the prevention of acute exacerbations of chronic obstructive pulmonary disease (AECOPD) were developed through a collaboration between the American College of Chest Physicians (CHEST) and the Canadian Thoracic Society (CTS). They are the first evidence-based guidelines dedicated entirely to the prevention of AECOPD and largely exclude material related to the treatment of symptomatic disease.1
Patients with AECOPD are commonly cared for by hospitalists, so we fill an important role in the longitudinal treatment of this disease. Acute exacerbations and hospitalizations for COPD account for 50% of all COPD-related expenses.2,3 Further, the Agency for Healthcare Research and Quality showed a 20% readmission rate nationally for AECOPD, far higher than the rate for most other diagnoses.4 Consequently, COPD readmission has been added to Medicare’s Hospital Readmissions Reduction Program for fiscal year 2015.5
Hospitalization, when the patient is a captive audience and many of the necessary resources are available, may be a time to initiate preventative strategies.
Guideline Updates
The guidelines for non-pharmacologic interventions start with vaccination and continue with behavioral modification. They support the use of the 23-valent polysaccharide pneumococcal vaccine and annual influenza vaccination, noting that only influenza vaccination has been shown to decrease AECOPD.
Pulmonary rehabilitation is recommended for patients with a recent (fewer than four weeks) exacerbation. Several recommendations favor combining social work interventions with education, adding that face-to-face verbal education is superior to written educational materials. Interestingly, smoking cessation interventions received a weak recommendation, based upon lack of literature specifically focusing on the prevention of AECOPD. Despite this recommendation, smoking cessation intervention is strongly encouraged by the authors, given evidence of a marked reduction in morbidity, mortality, and healthcare utilization among smokers with COPD who quit.6 Finally, telemonitoring is not considered to be superior to usual care.
The guidelines concerning inhaled therapies fall into three major drug classes, including short- and long-acting inhaled muscarinic antagonists (anticholinergic agents), short- and long-acting inhaled beta-agonists, and inhaled corticosteroids.
Long-acting medications are generally considered more effective in preventing exacerbations than those that are short acting. Long-acting muscarinic antagonists (LAMAs) are highlighted for their efficacy, and combination inhaled long-acting beta-agonists (LABAs) and inhaled corticosteroids are preferred over monotherapy with either agent alone. LAMAs are preferred to inhaled corticosteroids or LABAs when given as monotherapy.
Short-acting agents are rated as inferior at preventing exacerbations compared to their long-acting analogs, but short-acting medications are better than placebo when combined with long-acting agents from other drug classes. Triple drug therapy (inhaled LAMAs, LABAs, and corticosteroids) can be considered based on current evidence.
The final recommendations address the use of oral medications. A potentially practice-changing guideline is the recommendation for long-term use of N-acetylcysteine tablets twice daily for patients who have experienced more than two exacerbations within two years. A more intuitive recommendation in this group is that treating an AECOPD with oral or IV steroids decreases the chance of recurrent exacerbations in the future.
The remaining recommendations include daily macrolide therapy, the phosphodiesterate-4 inhibitor roflumilast for those with chronic bronchitis and a recent exacerbation, and slow-release theophylline for stable disease. These guidelines also point out that statins do not have a role in AECOPD prevention. An expert consensus also recommends carbocysteine for patients who have failed “maximal” therapy.1
Established Guideline Analysis
Prior guidelines that address stable COPD do exist, most notably from Quaseem and colleagues in the 2011 Annals of Internal Medicine (AIM) and the 2015 GOLD guidelines.7,8 The prior guidelines published in AIM offered limited recommendations on the preventative interventions of bronchodilator use, pulmonary rehabilitation, and oxygen use.
The recommendations made in AIM are similar to those in the CHEST guidelines; the lack of breadth in the AIM report reflects new data generated over the last half decade. They include preventing causative exposures (e.g. tobacco, occupational), recommending bronchodilator use (with or without inhaled corticosteroids), possibly using phosphodiesterase-4 inhibitors (PD-4 inhibitors), administering appropriate vaccines, and providing education; however, GOLD does not actually present or rate the evidence associated with those recommendations. GOLD does specifically state that statins have no role in AECOPD prevention, a position that is updated from more recent literature.8,9
The National Guideline Clearinghouse (NGC) also includes some references to prevention of AECOPD but has no sections explicitly dedicated to prevention. Of note, the NGC still endorses statin use and does not appear to have incorporated data from newer studies.8,10
Hospitalist Takeaways
Given the high rate of COPD readmissions and its broad impact on morbidity and healthcare costs, measures to prevent COPD exacerbations cannot remain out of scope of care for inpatient physicians. It is important to initiate pulmonary rehab within four weeks of an exacerbation of COPD to prevent future exacerbations. Systems should be put in place to assure that all patients who qualify are vaccinated for influenza and patients who continue to smoke receive cessation counseling.
Today, hospitalists are comfortable with these non-pharmacologic interventions, as well as medications that include inhaled bronchodilators, nebulized medications, macrolide maintenance therapy, and oral steroids; however, other oral medications, such as phosphodiesterase inhibitors, theophylline, and N-acetylcysteine, may be appropriate for select patients, and hospitalists should become more familiar with their utility.11,12,13,14
Finally, it is important to note that both short- and long-acting inhaled muscarinic antagonists have come to the forefront of pharmacologic interventions for COPD exacerbation prevention.
Dr. Lampman, MD, is a hospitalist, consulting provider, and physician leader of the physician advisor program at Duke Regional Hospital in Durham, N.C. Dr. Lovins is a hospitalist, associate chief medical informatics officer, and assistant professor of medicine at Duke University and Duke Regional Hospital.
References
- Criner GJ, Bourbeau J, Diekemper RL, et al. Prevention of acute exacerbations of COPD: American College of Chest Physicians and Canadian Thoracic Society Guideline. Chest. 2015;147(4):894-942.
- Miravitlles M, Garcia-Polo C, Domenech A, Villegas G, Conget F, de la Roza C. Clinical outcomes and cost analysis of exacerbations in chronic obstructive pulmonary disease. Lung. 2013;191(5):523-530.
- Miravitlles M, Murio C, Guerrero T, Gisbert R; DAFNE Study Group. Pharmacoeconomic evaluation of acute exacerbations of chronic bronchitis and COPD. Chest. 2002;121(5):1449-1455.
- Elixhauser A, Au DH, Podulka J. Readmissions for Chronic Obstructive Pulmonary Disease, 2008: Statistical Brief #121.In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, Md.: Agency for Health Care Policy and Research: 2006.
- Readmissions Reduction Program. Centers for Medicare and Medicaid Services website. Accessed September 8, 2015.
- Sicras-Mainar A, Rejas-Gutiérrez J, Navarro-Artieda R, Ibáñez-Nolla J. The effect of quitting smoking on costs and healthcare utilization in patients with chronic obstructive pulmonary disease: a comparison of current smokers versus ex-smokers in routine clinical practice. Lung. 2014;192(4):505-518.
- Qaseem A, Wilt TJ, Weinberger SE, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179-191.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2015. Global Strategy for the Diagnosis, Management, and Prevention of COPD. Accessed September 8, 2015.
- Criner GJ, Connett JE, Aaron SK, et al. Simvastatin for the prevention of exacerbations in moderate-to-severe COPD. N Engl J Med. 2014;370(23):2201-2210.
- Agency for Healthcare Research and Quality. National Guideline Clearinghouse. COPD – chronic obstructive pulmonary disease. In: Pulmonary (acute & chronic). Accessed September 8, 2015.
- Cazzola M, Matera MG. N-acetylcysteine in COPD may be beneficial, but for whom? Lancet Respir Med. 2014;2(3):166-167.
- Turner RD Bothamley. N-acetylcysteine for COPD: the evidence remains inconclusive. Lancet Respir Med. 2014;2(4):e3.
- Zheng JP, Wen FQ, Bai CX, et al. Twice daily N-acetylcysteine 600 mg for exacerbations of chronic obstructive pulmonary disease (PANTHEON): a randomised, double-blind placebo-controlled trial. Lancet Respir Med. 2014;2(3):187-194.
- Amazon.com. Amazon Search. 2015 06/1/2015].
Background
The CHEST guidelines for the prevention of acute exacerbations of chronic obstructive pulmonary disease (AECOPD) were developed through a collaboration between the American College of Chest Physicians (CHEST) and the Canadian Thoracic Society (CTS). They are the first evidence-based guidelines dedicated entirely to the prevention of AECOPD and largely exclude material related to the treatment of symptomatic disease.1
Patients with AECOPD are commonly cared for by hospitalists, so we fill an important role in the longitudinal treatment of this disease. Acute exacerbations and hospitalizations for COPD account for 50% of all COPD-related expenses.2,3 Further, the Agency for Healthcare Research and Quality showed a 20% readmission rate nationally for AECOPD, far higher than the rate for most other diagnoses.4 Consequently, COPD readmission has been added to Medicare’s Hospital Readmissions Reduction Program for fiscal year 2015.5
Hospitalization, when the patient is a captive audience and many of the necessary resources are available, may be a time to initiate preventative strategies.
Guideline Updates
The guidelines for non-pharmacologic interventions start with vaccination and continue with behavioral modification. They support the use of the 23-valent polysaccharide pneumococcal vaccine and annual influenza vaccination, noting that only influenza vaccination has been shown to decrease AECOPD.
Pulmonary rehabilitation is recommended for patients with a recent (fewer than four weeks) exacerbation. Several recommendations favor combining social work interventions with education, adding that face-to-face verbal education is superior to written educational materials. Interestingly, smoking cessation interventions received a weak recommendation, based upon lack of literature specifically focusing on the prevention of AECOPD. Despite this recommendation, smoking cessation intervention is strongly encouraged by the authors, given evidence of a marked reduction in morbidity, mortality, and healthcare utilization among smokers with COPD who quit.6 Finally, telemonitoring is not considered to be superior to usual care.
The guidelines concerning inhaled therapies fall into three major drug classes, including short- and long-acting inhaled muscarinic antagonists (anticholinergic agents), short- and long-acting inhaled beta-agonists, and inhaled corticosteroids.
Long-acting medications are generally considered more effective in preventing exacerbations than those that are short acting. Long-acting muscarinic antagonists (LAMAs) are highlighted for their efficacy, and combination inhaled long-acting beta-agonists (LABAs) and inhaled corticosteroids are preferred over monotherapy with either agent alone. LAMAs are preferred to inhaled corticosteroids or LABAs when given as monotherapy.
Short-acting agents are rated as inferior at preventing exacerbations compared to their long-acting analogs, but short-acting medications are better than placebo when combined with long-acting agents from other drug classes. Triple drug therapy (inhaled LAMAs, LABAs, and corticosteroids) can be considered based on current evidence.
The final recommendations address the use of oral medications. A potentially practice-changing guideline is the recommendation for long-term use of N-acetylcysteine tablets twice daily for patients who have experienced more than two exacerbations within two years. A more intuitive recommendation in this group is that treating an AECOPD with oral or IV steroids decreases the chance of recurrent exacerbations in the future.
The remaining recommendations include daily macrolide therapy, the phosphodiesterate-4 inhibitor roflumilast for those with chronic bronchitis and a recent exacerbation, and slow-release theophylline for stable disease. These guidelines also point out that statins do not have a role in AECOPD prevention. An expert consensus also recommends carbocysteine for patients who have failed “maximal” therapy.1
Established Guideline Analysis
Prior guidelines that address stable COPD do exist, most notably from Quaseem and colleagues in the 2011 Annals of Internal Medicine (AIM) and the 2015 GOLD guidelines.7,8 The prior guidelines published in AIM offered limited recommendations on the preventative interventions of bronchodilator use, pulmonary rehabilitation, and oxygen use.
The recommendations made in AIM are similar to those in the CHEST guidelines; the lack of breadth in the AIM report reflects new data generated over the last half decade. They include preventing causative exposures (e.g. tobacco, occupational), recommending bronchodilator use (with or without inhaled corticosteroids), possibly using phosphodiesterase-4 inhibitors (PD-4 inhibitors), administering appropriate vaccines, and providing education; however, GOLD does not actually present or rate the evidence associated with those recommendations. GOLD does specifically state that statins have no role in AECOPD prevention, a position that is updated from more recent literature.8,9
The National Guideline Clearinghouse (NGC) also includes some references to prevention of AECOPD but has no sections explicitly dedicated to prevention. Of note, the NGC still endorses statin use and does not appear to have incorporated data from newer studies.8,10
Hospitalist Takeaways
Given the high rate of COPD readmissions and its broad impact on morbidity and healthcare costs, measures to prevent COPD exacerbations cannot remain out of scope of care for inpatient physicians. It is important to initiate pulmonary rehab within four weeks of an exacerbation of COPD to prevent future exacerbations. Systems should be put in place to assure that all patients who qualify are vaccinated for influenza and patients who continue to smoke receive cessation counseling.
Today, hospitalists are comfortable with these non-pharmacologic interventions, as well as medications that include inhaled bronchodilators, nebulized medications, macrolide maintenance therapy, and oral steroids; however, other oral medications, such as phosphodiesterase inhibitors, theophylline, and N-acetylcysteine, may be appropriate for select patients, and hospitalists should become more familiar with their utility.11,12,13,14
Finally, it is important to note that both short- and long-acting inhaled muscarinic antagonists have come to the forefront of pharmacologic interventions for COPD exacerbation prevention.
Dr. Lampman, MD, is a hospitalist, consulting provider, and physician leader of the physician advisor program at Duke Regional Hospital in Durham, N.C. Dr. Lovins is a hospitalist, associate chief medical informatics officer, and assistant professor of medicine at Duke University and Duke Regional Hospital.
References
- Criner GJ, Bourbeau J, Diekemper RL, et al. Prevention of acute exacerbations of COPD: American College of Chest Physicians and Canadian Thoracic Society Guideline. Chest. 2015;147(4):894-942.
- Miravitlles M, Garcia-Polo C, Domenech A, Villegas G, Conget F, de la Roza C. Clinical outcomes and cost analysis of exacerbations in chronic obstructive pulmonary disease. Lung. 2013;191(5):523-530.
- Miravitlles M, Murio C, Guerrero T, Gisbert R; DAFNE Study Group. Pharmacoeconomic evaluation of acute exacerbations of chronic bronchitis and COPD. Chest. 2002;121(5):1449-1455.
- Elixhauser A, Au DH, Podulka J. Readmissions for Chronic Obstructive Pulmonary Disease, 2008: Statistical Brief #121.In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, Md.: Agency for Health Care Policy and Research: 2006.
- Readmissions Reduction Program. Centers for Medicare and Medicaid Services website. Accessed September 8, 2015.
- Sicras-Mainar A, Rejas-Gutiérrez J, Navarro-Artieda R, Ibáñez-Nolla J. The effect of quitting smoking on costs and healthcare utilization in patients with chronic obstructive pulmonary disease: a comparison of current smokers versus ex-smokers in routine clinical practice. Lung. 2014;192(4):505-518.
- Qaseem A, Wilt TJ, Weinberger SE, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179-191.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2015. Global Strategy for the Diagnosis, Management, and Prevention of COPD. Accessed September 8, 2015.
- Criner GJ, Connett JE, Aaron SK, et al. Simvastatin for the prevention of exacerbations in moderate-to-severe COPD. N Engl J Med. 2014;370(23):2201-2210.
- Agency for Healthcare Research and Quality. National Guideline Clearinghouse. COPD – chronic obstructive pulmonary disease. In: Pulmonary (acute & chronic). Accessed September 8, 2015.
- Cazzola M, Matera MG. N-acetylcysteine in COPD may be beneficial, but for whom? Lancet Respir Med. 2014;2(3):166-167.
- Turner RD Bothamley. N-acetylcysteine for COPD: the evidence remains inconclusive. Lancet Respir Med. 2014;2(4):e3.
- Zheng JP, Wen FQ, Bai CX, et al. Twice daily N-acetylcysteine 600 mg for exacerbations of chronic obstructive pulmonary disease (PANTHEON): a randomised, double-blind placebo-controlled trial. Lancet Respir Med. 2014;2(3):187-194.
- Amazon.com. Amazon Search. 2015 06/1/2015].
Consumer Reports Rates Hospitals on Infection Control, Prevention
Consumer Reports included for the first time in its national hospital quality ratings a ranking of how well 3,000 hospitals are controlling common deadly infections such as methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile.
The How Your Hospital Can Make You Sick report is based on information provided to the CDC between October 2013 and September 2014. The CDC found that 105 hospitals distinguished themselves by earning high ratings against both infections. Nine hospitals received top ratings for having no infections from MRSA, C. diff, or other measured infections, although none of the country’s highest-profile hospitals are on that list. Only 6% of hospitals scored well against both infections in the new ratings. The CDC estimates that 648,000 people develop infections during their hospital stay, with 75,000 dying from them; many of the deaths can be traced back to widespread, inappropriate use of antibiotics.
“High rates for MRSA and C. diff can be a red flag that a hospital isn’t following the best practices in preventing infections and prescribing antibiotics,” notes Doris Peter, PhD, director of Consumer Reports’ Health Ratings Center, in a prepared statement. “The data show that it is possible to keep infection rates down and in some cases avoid them altogether.”
Among Consumer Reports’ recommendations for hospitals:
- Consistently follow established protocols for managing superbug infections;
- Accurately track how many infections patients get; and
- Promptly report outbreaks to patients and health authorities.
Reference
- Consumer Reports. America’s antibiotic crisis: how your hospital can make you sick. July 29, 2015. Accessed September 12, 2015.
Consumer Reports included for the first time in its national hospital quality ratings a ranking of how well 3,000 hospitals are controlling common deadly infections such as methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile.
The How Your Hospital Can Make You Sick report is based on information provided to the CDC between October 2013 and September 2014. The CDC found that 105 hospitals distinguished themselves by earning high ratings against both infections. Nine hospitals received top ratings for having no infections from MRSA, C. diff, or other measured infections, although none of the country’s highest-profile hospitals are on that list. Only 6% of hospitals scored well against both infections in the new ratings. The CDC estimates that 648,000 people develop infections during their hospital stay, with 75,000 dying from them; many of the deaths can be traced back to widespread, inappropriate use of antibiotics.
“High rates for MRSA and C. diff can be a red flag that a hospital isn’t following the best practices in preventing infections and prescribing antibiotics,” notes Doris Peter, PhD, director of Consumer Reports’ Health Ratings Center, in a prepared statement. “The data show that it is possible to keep infection rates down and in some cases avoid them altogether.”
Among Consumer Reports’ recommendations for hospitals:
- Consistently follow established protocols for managing superbug infections;
- Accurately track how many infections patients get; and
- Promptly report outbreaks to patients and health authorities.
Reference
- Consumer Reports. America’s antibiotic crisis: how your hospital can make you sick. July 29, 2015. Accessed September 12, 2015.
Consumer Reports included for the first time in its national hospital quality ratings a ranking of how well 3,000 hospitals are controlling common deadly infections such as methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile.
The How Your Hospital Can Make You Sick report is based on information provided to the CDC between October 2013 and September 2014. The CDC found that 105 hospitals distinguished themselves by earning high ratings against both infections. Nine hospitals received top ratings for having no infections from MRSA, C. diff, or other measured infections, although none of the country’s highest-profile hospitals are on that list. Only 6% of hospitals scored well against both infections in the new ratings. The CDC estimates that 648,000 people develop infections during their hospital stay, with 75,000 dying from them; many of the deaths can be traced back to widespread, inappropriate use of antibiotics.
“High rates for MRSA and C. diff can be a red flag that a hospital isn’t following the best practices in preventing infections and prescribing antibiotics,” notes Doris Peter, PhD, director of Consumer Reports’ Health Ratings Center, in a prepared statement. “The data show that it is possible to keep infection rates down and in some cases avoid them altogether.”
Among Consumer Reports’ recommendations for hospitals:
- Consistently follow established protocols for managing superbug infections;
- Accurately track how many infections patients get; and
- Promptly report outbreaks to patients and health authorities.
Reference
- Consumer Reports. America’s antibiotic crisis: how your hospital can make you sick. July 29, 2015. Accessed September 12, 2015.
LISTEN NOW: Pediatric Hospital Medicine and the “Right Care” Movement
Three pediatric hospitalists – Dr. Ricardo Quiñonez of San Antonio Children’s Hospital, Dr. Shawn Ralston of Dartmouth-Hitchcock, and Dr. Alan Schroeder of Santa Clara Valley Medical Center – talk about the concept of “right care” in hospital medicine, and their participation in the Lown Institute’s Right Care movement.
Three pediatric hospitalists – Dr. Ricardo Quiñonez of San Antonio Children’s Hospital, Dr. Shawn Ralston of Dartmouth-Hitchcock, and Dr. Alan Schroeder of Santa Clara Valley Medical Center – talk about the concept of “right care” in hospital medicine, and their participation in the Lown Institute’s Right Care movement.
Three pediatric hospitalists – Dr. Ricardo Quiñonez of San Antonio Children’s Hospital, Dr. Shawn Ralston of Dartmouth-Hitchcock, and Dr. Alan Schroeder of Santa Clara Valley Medical Center – talk about the concept of “right care” in hospital medicine, and their participation in the Lown Institute’s Right Care movement.
Prevalence of Undiagnosed Diabetes in US
Diabetes affects up to 14 percent of the U.S. population - an increase from nearly 10 percent in the early 1990s - yet over a third of cases still go undiagnosed, according to a new analysis.
Screening seems to be catching more cases, accounting for the general rise over two decades, the study authors say, but mainly whites have benefited; for Hispanic and Asian people in particular, more than half of cases go undetected.
"We need to better educate people on the risk factors for diabetes - including older age, family history and obesity - and improve screening for those at high risk," lead study author Andy Menke, an epidemiologist at Social and Scientific Systems in Silver Spring, Maryland, said by email.
Globally, about one in nine adults has diagnosed diabetes, and the disease will be the seventh leading cause of death by 2030, according to the World Health Organization.
Most of these people have Type 2, or adult-onset, diabetes, which happens when the body can't properly use or make enough of the hormone insulin to convert blood sugar into energy. Left untreated, diabetes can lead to nerve damage, amputations, blindness, heart disease and strokes.
Average blood sugar levels over the course of several months can be estimated by measuring changes to the hemoglobin molecule in red blood cells. The hemoglobin A1c test measures the percentage of hemoglobin - the protein in red blood cells that
carries oxygen - that is coated with sugar, with readings of 6.5 percent or above signaling diabetes.
People with A1c levels between 5.7 percent and 6.4 percent aren't diabetic, but because this is considered elevated it is sometimes called "pre-diabetes" and considered a risk factor for going on to develop full-blown diabetes.
Menke and colleagues estimated the prevalence of diabetes and pre-diabetes using data from the National Health and Nutrition Examination Survey (NHANES) collected on 2,781 adults in 2011 to 2012 and an additional 23,634 adults from 1988 to 2010.
While the prevalence of diabetes increased over time in the overall population, gains were more pronounced among racial and ethnic minorities, the study found.
About 11 percent of white people have diabetes, the researchers calculated, compared with 22 percent of non-Hispanic black participants, 21 percent of Asians and 23 percent of Hispanics.
Among Asians, 51 percent of those with diabetes were unaware of it, and the same was true for 49 percent of Hispanic people with the condition.
An additional 38 percent of adults fell into the pre-diabetes category. Added to the prevalence of diabetes, that means more than half of the U.S. population has diabetes or is at increased risk for it, the authors point out.
The good news, however, is fewer people are undiagnosed than in the past, Dr. William Herman and Dr. Amy Rothberg of the University of Michigan in Ann Arbor note in commentary accompanying the study in JAMA.
In it, they note that the increase in diabetes prevalence between 1988 and 2012 seen in the study was due to an increase in diagnosed cases, and that overall undiagnosed cases fell from 40 percent in 1988-1994 to 31 percent in 2008-2012.
This "likely reflects increased awareness of the problem of undiagnosed diabetes and increased testing," they said by email.
The drop in undiagnosed cases, they added, may be due in part to the newer, simpler A1c test, which doesn't require fasting or any advance preparation.
It's also possible that new cases of diabetes are starting to fall for the first time in decades because more people are getting the message about lifestyle choices that can contribute to diabetes, noted Dr. David Nathan, director of the diabetes center at Massachusetts General Hospital in Boston and a professor at Harvard Medical School.
In particular, more patients now understand that being overweight or obese increases the risk for diabetes, Nathan, author of a separate report in JAMA on advances in diagnosis and treatment, said by email.
"Behavioral changes, including healthy eating and more activity can prevent, or at least ameliorate, the diabetes epidemic," Nathan said.
Diabetes affects up to 14 percent of the U.S. population - an increase from nearly 10 percent in the early 1990s - yet over a third of cases still go undiagnosed, according to a new analysis.
Screening seems to be catching more cases, accounting for the general rise over two decades, the study authors say, but mainly whites have benefited; for Hispanic and Asian people in particular, more than half of cases go undetected.
"We need to better educate people on the risk factors for diabetes - including older age, family history and obesity - and improve screening for those at high risk," lead study author Andy Menke, an epidemiologist at Social and Scientific Systems in Silver Spring, Maryland, said by email.
Globally, about one in nine adults has diagnosed diabetes, and the disease will be the seventh leading cause of death by 2030, according to the World Health Organization.
Most of these people have Type 2, or adult-onset, diabetes, which happens when the body can't properly use or make enough of the hormone insulin to convert blood sugar into energy. Left untreated, diabetes can lead to nerve damage, amputations, blindness, heart disease and strokes.
Average blood sugar levels over the course of several months can be estimated by measuring changes to the hemoglobin molecule in red blood cells. The hemoglobin A1c test measures the percentage of hemoglobin - the protein in red blood cells that
carries oxygen - that is coated with sugar, with readings of 6.5 percent or above signaling diabetes.
People with A1c levels between 5.7 percent and 6.4 percent aren't diabetic, but because this is considered elevated it is sometimes called "pre-diabetes" and considered a risk factor for going on to develop full-blown diabetes.
Menke and colleagues estimated the prevalence of diabetes and pre-diabetes using data from the National Health and Nutrition Examination Survey (NHANES) collected on 2,781 adults in 2011 to 2012 and an additional 23,634 adults from 1988 to 2010.
While the prevalence of diabetes increased over time in the overall population, gains were more pronounced among racial and ethnic minorities, the study found.
About 11 percent of white people have diabetes, the researchers calculated, compared with 22 percent of non-Hispanic black participants, 21 percent of Asians and 23 percent of Hispanics.
Among Asians, 51 percent of those with diabetes were unaware of it, and the same was true for 49 percent of Hispanic people with the condition.
An additional 38 percent of adults fell into the pre-diabetes category. Added to the prevalence of diabetes, that means more than half of the U.S. population has diabetes or is at increased risk for it, the authors point out.
The good news, however, is fewer people are undiagnosed than in the past, Dr. William Herman and Dr. Amy Rothberg of the University of Michigan in Ann Arbor note in commentary accompanying the study in JAMA.
In it, they note that the increase in diabetes prevalence between 1988 and 2012 seen in the study was due to an increase in diagnosed cases, and that overall undiagnosed cases fell from 40 percent in 1988-1994 to 31 percent in 2008-2012.
This "likely reflects increased awareness of the problem of undiagnosed diabetes and increased testing," they said by email.
The drop in undiagnosed cases, they added, may be due in part to the newer, simpler A1c test, which doesn't require fasting or any advance preparation.
It's also possible that new cases of diabetes are starting to fall for the first time in decades because more people are getting the message about lifestyle choices that can contribute to diabetes, noted Dr. David Nathan, director of the diabetes center at Massachusetts General Hospital in Boston and a professor at Harvard Medical School.
In particular, more patients now understand that being overweight or obese increases the risk for diabetes, Nathan, author of a separate report in JAMA on advances in diagnosis and treatment, said by email.
"Behavioral changes, including healthy eating and more activity can prevent, or at least ameliorate, the diabetes epidemic," Nathan said.
Diabetes affects up to 14 percent of the U.S. population - an increase from nearly 10 percent in the early 1990s - yet over a third of cases still go undiagnosed, according to a new analysis.
Screening seems to be catching more cases, accounting for the general rise over two decades, the study authors say, but mainly whites have benefited; for Hispanic and Asian people in particular, more than half of cases go undetected.
"We need to better educate people on the risk factors for diabetes - including older age, family history and obesity - and improve screening for those at high risk," lead study author Andy Menke, an epidemiologist at Social and Scientific Systems in Silver Spring, Maryland, said by email.
Globally, about one in nine adults has diagnosed diabetes, and the disease will be the seventh leading cause of death by 2030, according to the World Health Organization.
Most of these people have Type 2, or adult-onset, diabetes, which happens when the body can't properly use or make enough of the hormone insulin to convert blood sugar into energy. Left untreated, diabetes can lead to nerve damage, amputations, blindness, heart disease and strokes.
Average blood sugar levels over the course of several months can be estimated by measuring changes to the hemoglobin molecule in red blood cells. The hemoglobin A1c test measures the percentage of hemoglobin - the protein in red blood cells that
carries oxygen - that is coated with sugar, with readings of 6.5 percent or above signaling diabetes.
People with A1c levels between 5.7 percent and 6.4 percent aren't diabetic, but because this is considered elevated it is sometimes called "pre-diabetes" and considered a risk factor for going on to develop full-blown diabetes.
Menke and colleagues estimated the prevalence of diabetes and pre-diabetes using data from the National Health and Nutrition Examination Survey (NHANES) collected on 2,781 adults in 2011 to 2012 and an additional 23,634 adults from 1988 to 2010.
While the prevalence of diabetes increased over time in the overall population, gains were more pronounced among racial and ethnic minorities, the study found.
About 11 percent of white people have diabetes, the researchers calculated, compared with 22 percent of non-Hispanic black participants, 21 percent of Asians and 23 percent of Hispanics.
Among Asians, 51 percent of those with diabetes were unaware of it, and the same was true for 49 percent of Hispanic people with the condition.
An additional 38 percent of adults fell into the pre-diabetes category. Added to the prevalence of diabetes, that means more than half of the U.S. population has diabetes or is at increased risk for it, the authors point out.
The good news, however, is fewer people are undiagnosed than in the past, Dr. William Herman and Dr. Amy Rothberg of the University of Michigan in Ann Arbor note in commentary accompanying the study in JAMA.
In it, they note that the increase in diabetes prevalence between 1988 and 2012 seen in the study was due to an increase in diagnosed cases, and that overall undiagnosed cases fell from 40 percent in 1988-1994 to 31 percent in 2008-2012.
This "likely reflects increased awareness of the problem of undiagnosed diabetes and increased testing," they said by email.
The drop in undiagnosed cases, they added, may be due in part to the newer, simpler A1c test, which doesn't require fasting or any advance preparation.
It's also possible that new cases of diabetes are starting to fall for the first time in decades because more people are getting the message about lifestyle choices that can contribute to diabetes, noted Dr. David Nathan, director of the diabetes center at Massachusetts General Hospital in Boston and a professor at Harvard Medical School.
In particular, more patients now understand that being overweight or obese increases the risk for diabetes, Nathan, author of a separate report in JAMA on advances in diagnosis and treatment, said by email.
"Behavioral changes, including healthy eating and more activity can prevent, or at least ameliorate, the diabetes epidemic," Nathan said.
Hospitalists' Role in Improving Patient Experience: A Baldridge Winner's Perspective
Understanding and improving the patient care experience has become a vital component of delivering high quality care. According to a new survey of American Society for Quality (ASQ) healthcare quality experts, more than 80% of respondents said improving communications between caregivers and patients and easing access to treatment across the entire continuum of care should be top priorities for improving patient experience. For Hill Country Memorial (HCM) in Fredericksburg, Texas, winner of the Malcolm Baldrige National Quality Award, accomplishing this kind of top-level patient experience performance involved engaging physicians—particularly hospitalists—using voice of the customer (VOC) input.
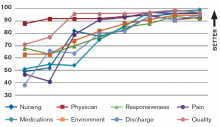
HCM did not achieve overnight success, however; instead, the facility achieved year-over-year improvement in finance and growth, patient experience, quality of care, and workforce environment and engagement (see Figure 1).
HCM developed a systematic VOC input-to-action process in which listening and learning methods during annual planning led them to institute a hospitalist program. Results included:
- Improved access to primary care, achieved by increasing the physicians’ hours of availability in their clinics, and improved work-life balance, enhancing engagement and alignment of the medical staff and HCM;
- Reductions in delays in admissions, discharges, and length of stay; and
- Real-time review and management of clinical data, not just during the daily rounding as had been done previously.
One of the major hurdles in the way of achieving patient satisfaction, according to the ASQ patient experience survey, is care that is fragmented and uncoordinated because of communication issues. HCM has overcome those hurdles using strategies such as a daily afternoon huddle in which hospitalists meet with a multidisciplinary team so that everyone understands patient action plans and current concerns. The process of discharge planning begins in these huddles so that more complex issues are initiated on day one of the hospital stay.
A new rounding communication process, called GIFT for greet, inform, find out, and time, has dramatically improved patient satisfaction and engagement. GIFT enables hospitalists to greet a patient with a personal introduction and an explanation of their position and responsibilities. Hospitalists always sit while engaging the patient, and they make it a point to acknowledge not only the patient but everyone present in the room. Personalized “baseball cards” featuring the hospitalist’s background, including personal interests and hobbies, are handed out to patients or family members. Hospitalists take time to inform the patient and appropriate family members and caregivers of all diagnostic test results and the clinical response of treatment to date. Treatment plans and further diagnostic tests or procedures are discussed. A report of all consultants who have joined or will be joining in the care, along with their roles in the treatment planned, is fully vetted.
One key to a successful patient experience is discovering the concerns of the patient, family members, friends, and caregivers. Emotional issues become as important as the physical needs of the patient; these are openly addressed. Ask not “What’s the matter?” but instead “What matters to you?”
Timing the hospitalist’s return to see the patient and the anticipated date of transition of care is the last item in the rounding interaction. The date should be as accurate as possible to reduce patient anxiety and help the patient understand that the hospitalist really cares.
The hospitalist program has also strengthened the relationship between nurses and physicians. Nurses know the hospitalists’ practice patterns well, which allows them to help manage patient interactions and minimize patient anxiety and frustration. The physician-patient relationship is reinforced when nurse leaders include hospitalist satisfaction questions during daily rounding to identify concerns that can be clarified or resolved in real time.
The systematic VOC approach has enabled HCM to design, manage, and improve its key work process at multiple levels of the organization. These processes are reviewed and refined periodically to respond to the changing healthcare environment and stay focused on creating value for customers.
Chip Caldwell is chairman of Caldwell Butler, a firm specializing in coaching organizations to achieve world class performance in margin improvement, patient experience, physician/clinical enterprise, and capacity optimization. Jayne Pope, MBA, RN, is CEO of Hill Country Memorial Hospital in Fredericksburg, Texas. James Partin, MD, is CMO at Hill Country Memorial.
Understanding and improving the patient care experience has become a vital component of delivering high quality care. According to a new survey of American Society for Quality (ASQ) healthcare quality experts, more than 80% of respondents said improving communications between caregivers and patients and easing access to treatment across the entire continuum of care should be top priorities for improving patient experience. For Hill Country Memorial (HCM) in Fredericksburg, Texas, winner of the Malcolm Baldrige National Quality Award, accomplishing this kind of top-level patient experience performance involved engaging physicians—particularly hospitalists—using voice of the customer (VOC) input.
HCM did not achieve overnight success, however; instead, the facility achieved year-over-year improvement in finance and growth, patient experience, quality of care, and workforce environment and engagement (see Figure 1).
HCM developed a systematic VOC input-to-action process in which listening and learning methods during annual planning led them to institute a hospitalist program. Results included:
- Improved access to primary care, achieved by increasing the physicians’ hours of availability in their clinics, and improved work-life balance, enhancing engagement and alignment of the medical staff and HCM;
- Reductions in delays in admissions, discharges, and length of stay; and
- Real-time review and management of clinical data, not just during the daily rounding as had been done previously.
One of the major hurdles in the way of achieving patient satisfaction, according to the ASQ patient experience survey, is care that is fragmented and uncoordinated because of communication issues. HCM has overcome those hurdles using strategies such as a daily afternoon huddle in which hospitalists meet with a multidisciplinary team so that everyone understands patient action plans and current concerns. The process of discharge planning begins in these huddles so that more complex issues are initiated on day one of the hospital stay.
A new rounding communication process, called GIFT for greet, inform, find out, and time, has dramatically improved patient satisfaction and engagement. GIFT enables hospitalists to greet a patient with a personal introduction and an explanation of their position and responsibilities. Hospitalists always sit while engaging the patient, and they make it a point to acknowledge not only the patient but everyone present in the room. Personalized “baseball cards” featuring the hospitalist’s background, including personal interests and hobbies, are handed out to patients or family members. Hospitalists take time to inform the patient and appropriate family members and caregivers of all diagnostic test results and the clinical response of treatment to date. Treatment plans and further diagnostic tests or procedures are discussed. A report of all consultants who have joined or will be joining in the care, along with their roles in the treatment planned, is fully vetted.
One key to a successful patient experience is discovering the concerns of the patient, family members, friends, and caregivers. Emotional issues become as important as the physical needs of the patient; these are openly addressed. Ask not “What’s the matter?” but instead “What matters to you?”
Timing the hospitalist’s return to see the patient and the anticipated date of transition of care is the last item in the rounding interaction. The date should be as accurate as possible to reduce patient anxiety and help the patient understand that the hospitalist really cares.
The hospitalist program has also strengthened the relationship between nurses and physicians. Nurses know the hospitalists’ practice patterns well, which allows them to help manage patient interactions and minimize patient anxiety and frustration. The physician-patient relationship is reinforced when nurse leaders include hospitalist satisfaction questions during daily rounding to identify concerns that can be clarified or resolved in real time.
The systematic VOC approach has enabled HCM to design, manage, and improve its key work process at multiple levels of the organization. These processes are reviewed and refined periodically to respond to the changing healthcare environment and stay focused on creating value for customers.
Chip Caldwell is chairman of Caldwell Butler, a firm specializing in coaching organizations to achieve world class performance in margin improvement, patient experience, physician/clinical enterprise, and capacity optimization. Jayne Pope, MBA, RN, is CEO of Hill Country Memorial Hospital in Fredericksburg, Texas. James Partin, MD, is CMO at Hill Country Memorial.
Understanding and improving the patient care experience has become a vital component of delivering high quality care. According to a new survey of American Society for Quality (ASQ) healthcare quality experts, more than 80% of respondents said improving communications between caregivers and patients and easing access to treatment across the entire continuum of care should be top priorities for improving patient experience. For Hill Country Memorial (HCM) in Fredericksburg, Texas, winner of the Malcolm Baldrige National Quality Award, accomplishing this kind of top-level patient experience performance involved engaging physicians—particularly hospitalists—using voice of the customer (VOC) input.
HCM did not achieve overnight success, however; instead, the facility achieved year-over-year improvement in finance and growth, patient experience, quality of care, and workforce environment and engagement (see Figure 1).
HCM developed a systematic VOC input-to-action process in which listening and learning methods during annual planning led them to institute a hospitalist program. Results included:
- Improved access to primary care, achieved by increasing the physicians’ hours of availability in their clinics, and improved work-life balance, enhancing engagement and alignment of the medical staff and HCM;
- Reductions in delays in admissions, discharges, and length of stay; and
- Real-time review and management of clinical data, not just during the daily rounding as had been done previously.
One of the major hurdles in the way of achieving patient satisfaction, according to the ASQ patient experience survey, is care that is fragmented and uncoordinated because of communication issues. HCM has overcome those hurdles using strategies such as a daily afternoon huddle in which hospitalists meet with a multidisciplinary team so that everyone understands patient action plans and current concerns. The process of discharge planning begins in these huddles so that more complex issues are initiated on day one of the hospital stay.
A new rounding communication process, called GIFT for greet, inform, find out, and time, has dramatically improved patient satisfaction and engagement. GIFT enables hospitalists to greet a patient with a personal introduction and an explanation of their position and responsibilities. Hospitalists always sit while engaging the patient, and they make it a point to acknowledge not only the patient but everyone present in the room. Personalized “baseball cards” featuring the hospitalist’s background, including personal interests and hobbies, are handed out to patients or family members. Hospitalists take time to inform the patient and appropriate family members and caregivers of all diagnostic test results and the clinical response of treatment to date. Treatment plans and further diagnostic tests or procedures are discussed. A report of all consultants who have joined or will be joining in the care, along with their roles in the treatment planned, is fully vetted.
One key to a successful patient experience is discovering the concerns of the patient, family members, friends, and caregivers. Emotional issues become as important as the physical needs of the patient; these are openly addressed. Ask not “What’s the matter?” but instead “What matters to you?”
Timing the hospitalist’s return to see the patient and the anticipated date of transition of care is the last item in the rounding interaction. The date should be as accurate as possible to reduce patient anxiety and help the patient understand that the hospitalist really cares.
The hospitalist program has also strengthened the relationship between nurses and physicians. Nurses know the hospitalists’ practice patterns well, which allows them to help manage patient interactions and minimize patient anxiety and frustration. The physician-patient relationship is reinforced when nurse leaders include hospitalist satisfaction questions during daily rounding to identify concerns that can be clarified or resolved in real time.
The systematic VOC approach has enabled HCM to design, manage, and improve its key work process at multiple levels of the organization. These processes are reviewed and refined periodically to respond to the changing healthcare environment and stay focused on creating value for customers.
Chip Caldwell is chairman of Caldwell Butler, a firm specializing in coaching organizations to achieve world class performance in margin improvement, patient experience, physician/clinical enterprise, and capacity optimization. Jayne Pope, MBA, RN, is CEO of Hill Country Memorial Hospital in Fredericksburg, Texas. James Partin, MD, is CMO at Hill Country Memorial.
Post-Procedural Bridging Therapy for Secondary Prevention of VTE Increases Rate of Bleeding
Clinical question: Is post-procedural bridging therapy necessary for secondary prevention of VTE?
Background: Bridging therapy has been studied to stratify peri-procedural risk for patients with atrial fibrillation and mechanical heart valves. Data examining the necessity of post-procedural bridging for secondary prevention of VTE are lacking.
Study design: Retrospective, cohort study.
Setting: Single-state, integrated, healthcare delivery system.
Synopsis: A retrospective analysis of patients treated with warfarin for VTE prior to undergoing an invasive procedure was conducted from January 2006 through March 2012 to evaluate the occurrence of post-procedural bleeding secondary to bridging therapy, as well as the occurrence of VTE if bridging therapy was withheld.
Nearly 19,000 procedures were evaluated, of which 1,812 were included in the study. Of note, 11,710 procedures were excluded because the indication for anticoagulation was not VTE. The primary outcome was post-procedure bleeding events at 30 days, while secondary outcomes included severe bleeding events, recurrent VTE, and 30-day mortality. Patient risk of recurrent VTE was stratified into low-, medium-, and high-risk categories based on AT9 current guidelines.
Clinically relevant bleeding events occurred in 2.7% (15/555) of bridged patients and in 0.2% (2/1257) of non-bridged patients (hazard ratio of 17.2). With respect to VTE recurrence, there were three events in the non-bridged group and zero in the bridged group, which was not statistically significant (P=0.56). No VTE events were seen in the high-risk group, and there was no mortality at 30 days across any group.
Bottom line: Peri-procedural bridging therapy for VTE is associated with higher risk of bleeding, but there is not a significant risk of recurrent VTE if bridging therapy is withheld.
Citation: Clark NP, Witt DM, Davies LE, et al. Bleeding, recurrent venous thromboembolism, and mortality risks during warfarin interruption for invasive procedures. JAMA Intern Med. 2015;175(7):1163-1168. doi:10.1001/jamainternmed.2015.1843.
Clinical question: Is post-procedural bridging therapy necessary for secondary prevention of VTE?
Background: Bridging therapy has been studied to stratify peri-procedural risk for patients with atrial fibrillation and mechanical heart valves. Data examining the necessity of post-procedural bridging for secondary prevention of VTE are lacking.
Study design: Retrospective, cohort study.
Setting: Single-state, integrated, healthcare delivery system.
Synopsis: A retrospective analysis of patients treated with warfarin for VTE prior to undergoing an invasive procedure was conducted from January 2006 through March 2012 to evaluate the occurrence of post-procedural bleeding secondary to bridging therapy, as well as the occurrence of VTE if bridging therapy was withheld.
Nearly 19,000 procedures were evaluated, of which 1,812 were included in the study. Of note, 11,710 procedures were excluded because the indication for anticoagulation was not VTE. The primary outcome was post-procedure bleeding events at 30 days, while secondary outcomes included severe bleeding events, recurrent VTE, and 30-day mortality. Patient risk of recurrent VTE was stratified into low-, medium-, and high-risk categories based on AT9 current guidelines.
Clinically relevant bleeding events occurred in 2.7% (15/555) of bridged patients and in 0.2% (2/1257) of non-bridged patients (hazard ratio of 17.2). With respect to VTE recurrence, there were three events in the non-bridged group and zero in the bridged group, which was not statistically significant (P=0.56). No VTE events were seen in the high-risk group, and there was no mortality at 30 days across any group.
Bottom line: Peri-procedural bridging therapy for VTE is associated with higher risk of bleeding, but there is not a significant risk of recurrent VTE if bridging therapy is withheld.
Citation: Clark NP, Witt DM, Davies LE, et al. Bleeding, recurrent venous thromboembolism, and mortality risks during warfarin interruption for invasive procedures. JAMA Intern Med. 2015;175(7):1163-1168. doi:10.1001/jamainternmed.2015.1843.
Clinical question: Is post-procedural bridging therapy necessary for secondary prevention of VTE?
Background: Bridging therapy has been studied to stratify peri-procedural risk for patients with atrial fibrillation and mechanical heart valves. Data examining the necessity of post-procedural bridging for secondary prevention of VTE are lacking.
Study design: Retrospective, cohort study.
Setting: Single-state, integrated, healthcare delivery system.
Synopsis: A retrospective analysis of patients treated with warfarin for VTE prior to undergoing an invasive procedure was conducted from January 2006 through March 2012 to evaluate the occurrence of post-procedural bleeding secondary to bridging therapy, as well as the occurrence of VTE if bridging therapy was withheld.
Nearly 19,000 procedures were evaluated, of which 1,812 were included in the study. Of note, 11,710 procedures were excluded because the indication for anticoagulation was not VTE. The primary outcome was post-procedure bleeding events at 30 days, while secondary outcomes included severe bleeding events, recurrent VTE, and 30-day mortality. Patient risk of recurrent VTE was stratified into low-, medium-, and high-risk categories based on AT9 current guidelines.
Clinically relevant bleeding events occurred in 2.7% (15/555) of bridged patients and in 0.2% (2/1257) of non-bridged patients (hazard ratio of 17.2). With respect to VTE recurrence, there were three events in the non-bridged group and zero in the bridged group, which was not statistically significant (P=0.56). No VTE events were seen in the high-risk group, and there was no mortality at 30 days across any group.
Bottom line: Peri-procedural bridging therapy for VTE is associated with higher risk of bleeding, but there is not a significant risk of recurrent VTE if bridging therapy is withheld.
Citation: Clark NP, Witt DM, Davies LE, et al. Bleeding, recurrent venous thromboembolism, and mortality risks during warfarin interruption for invasive procedures. JAMA Intern Med. 2015;175(7):1163-1168. doi:10.1001/jamainternmed.2015.1843.
Short-Course Antimicrobial Therapy Outcomes for Intraabdominal Infection
Clinical question: Does a short, fixed duration of antibiotic therapy for complicated intraabdominal infections lead to equivalent outcomes and less antibiotic exposure than the traditional approach?
Background: Published guidelines recommend appropriate antimicrobial agents for intraabdominal infections, but the optimal duration of therapy remains unclear. Most practitioners continue to treat for 10-14 days and until all physiologic evidence of the systemic inflammatory response syndrome (SIRS) has resolved. More recently, small studies have suggested that a shorter course may lead to equivalent outcomes with decreased antibiotic exposure.
Study design: Open-label, multicenter, randomized control trial.
Setting: Twenty-three sites throughout the U.S. and Canada.
Synopsis: In the short-course group, 257 patients were randomized to receive antimicrobial therapy for four full days after their index source-control procedure; 260 patients in the control group received antimicrobial therapy until two days after resolution of the physiological abnormalities related to SIRS. The median duration of therapy was 4.0 days (interquartile range [IQR], 4.0-5.0) for the experimental group and 8.0 days (IQR 5.0-10.0) in the control group (95% CI, -4.7 to -3.3; P<0.001).
There was no significant difference in surgical site infection, recurrent intraabdominal infection, or death between the experimental and control groups (21.8% vs. 22.3%, 95% CI -7.0 to 8.0; P=0.92). In the experimental group, 47 patients did not adhere to the protocol, all of whom received a longer antimicrobial treatment course than specified in the protocol.
This trial excluded patients without adequate source control and included a small number of immunocompromised hosts. The rate of nonadherence to the protocol was high, at 18% of patients in the experimental group. The calculated sample size to assert equivalence between groups was not achieved, although the results are suggestive of equivalence.
Bottom line: A shorter course of antimicrobial therapy for complicated intraabdominal infections might lead to equivalent outcomes with less antibiotic exposure compared with current practice; however, it is challenging for providers to stop antimicrobial therapy while patients continue to show physiologic evidence of SIRS.
Citation: Sawyer RG, Claridge JA, Nathens AB, et al. Trial of short-course antimicrobial therapy for intraabdominal infection. NEJM. 2015;372(21):1996-2005.
Clinical question: Does a short, fixed duration of antibiotic therapy for complicated intraabdominal infections lead to equivalent outcomes and less antibiotic exposure than the traditional approach?
Background: Published guidelines recommend appropriate antimicrobial agents for intraabdominal infections, but the optimal duration of therapy remains unclear. Most practitioners continue to treat for 10-14 days and until all physiologic evidence of the systemic inflammatory response syndrome (SIRS) has resolved. More recently, small studies have suggested that a shorter course may lead to equivalent outcomes with decreased antibiotic exposure.
Study design: Open-label, multicenter, randomized control trial.
Setting: Twenty-three sites throughout the U.S. and Canada.
Synopsis: In the short-course group, 257 patients were randomized to receive antimicrobial therapy for four full days after their index source-control procedure; 260 patients in the control group received antimicrobial therapy until two days after resolution of the physiological abnormalities related to SIRS. The median duration of therapy was 4.0 days (interquartile range [IQR], 4.0-5.0) for the experimental group and 8.0 days (IQR 5.0-10.0) in the control group (95% CI, -4.7 to -3.3; P<0.001).
There was no significant difference in surgical site infection, recurrent intraabdominal infection, or death between the experimental and control groups (21.8% vs. 22.3%, 95% CI -7.0 to 8.0; P=0.92). In the experimental group, 47 patients did not adhere to the protocol, all of whom received a longer antimicrobial treatment course than specified in the protocol.
This trial excluded patients without adequate source control and included a small number of immunocompromised hosts. The rate of nonadherence to the protocol was high, at 18% of patients in the experimental group. The calculated sample size to assert equivalence between groups was not achieved, although the results are suggestive of equivalence.
Bottom line: A shorter course of antimicrobial therapy for complicated intraabdominal infections might lead to equivalent outcomes with less antibiotic exposure compared with current practice; however, it is challenging for providers to stop antimicrobial therapy while patients continue to show physiologic evidence of SIRS.
Citation: Sawyer RG, Claridge JA, Nathens AB, et al. Trial of short-course antimicrobial therapy for intraabdominal infection. NEJM. 2015;372(21):1996-2005.
Clinical question: Does a short, fixed duration of antibiotic therapy for complicated intraabdominal infections lead to equivalent outcomes and less antibiotic exposure than the traditional approach?
Background: Published guidelines recommend appropriate antimicrobial agents for intraabdominal infections, but the optimal duration of therapy remains unclear. Most practitioners continue to treat for 10-14 days and until all physiologic evidence of the systemic inflammatory response syndrome (SIRS) has resolved. More recently, small studies have suggested that a shorter course may lead to equivalent outcomes with decreased antibiotic exposure.
Study design: Open-label, multicenter, randomized control trial.
Setting: Twenty-three sites throughout the U.S. and Canada.
Synopsis: In the short-course group, 257 patients were randomized to receive antimicrobial therapy for four full days after their index source-control procedure; 260 patients in the control group received antimicrobial therapy until two days after resolution of the physiological abnormalities related to SIRS. The median duration of therapy was 4.0 days (interquartile range [IQR], 4.0-5.0) for the experimental group and 8.0 days (IQR 5.0-10.0) in the control group (95% CI, -4.7 to -3.3; P<0.001).
There was no significant difference in surgical site infection, recurrent intraabdominal infection, or death between the experimental and control groups (21.8% vs. 22.3%, 95% CI -7.0 to 8.0; P=0.92). In the experimental group, 47 patients did not adhere to the protocol, all of whom received a longer antimicrobial treatment course than specified in the protocol.
This trial excluded patients without adequate source control and included a small number of immunocompromised hosts. The rate of nonadherence to the protocol was high, at 18% of patients in the experimental group. The calculated sample size to assert equivalence between groups was not achieved, although the results are suggestive of equivalence.
Bottom line: A shorter course of antimicrobial therapy for complicated intraabdominal infections might lead to equivalent outcomes with less antibiotic exposure compared with current practice; however, it is challenging for providers to stop antimicrobial therapy while patients continue to show physiologic evidence of SIRS.
Citation: Sawyer RG, Claridge JA, Nathens AB, et al. Trial of short-course antimicrobial therapy for intraabdominal infection. NEJM. 2015;372(21):1996-2005.