User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Clonidine: Off-label uses in pediatric patients
Clonidine is a centrally acting alpha-2 agonist originally developed for treating hypertension. It is believed to work by stimulating alpha-2 receptors in various areas of the brain. It is nonselective, binding alpha-2A, -2B, and -2C receptors, and mediates inattentiveness, hyperactivity, impulsivity, sedation, and hypotension.1 Clonidine is available as immediate-release (IR), extended-release, and patch formulations, with typical doses ranging from 0.1 to 0.4 mg/d. The most common adverse effects are anticholinergic, such as sedation, dry mouth, and constipation. Since clonidine is effective at lowering blood pressure, the main safety concern is the possibility of rebound hypertension if abruptly stopped, which necessitates a short taper period.1
In child and adolescent psychiatry, the only FDA-approved use of clonidine is for treating attention-deficit/hyperactivity disorder (ADHD). Yet this medication has been increasingly used off-label for several common psychiatric ailments in pediatric patients. In this article, we discuss potential uses of clonidine in child and adolescent psychiatry; except for ADHD, all uses we describe are off-label.
ADHD. Clonidine is effective both as a monotherapy and as an adjunctive therapy to stimulants for pediatric ADHD. When used alone, clonidine is better suited for patients who have hyperactivity as their primary concern, whereas stimulants may be better suited for patients with inattentive subtypes. It also can help reduce sleep disturbances associated with the use of stimulants, especially insomnia.1
Tics/Tourette syndrome. Clonidine is a first-line treatment for tics in Tourette syndrome, demonstrating high efficacy with limited or no adverse effects. Furthermore, ADHD is the most common comorbid condition in patients with dystonic tics, which makes clonidine useful for simultaneously treating both conditions.2
Insomnia. Currently, there are no FDA-approved medications for treating sleep disorders in children and adolescents. However, clonidine is among the most used medications for childhood sleep difficulties, second only to antihistamines. The IR formulation is often preferred for this indication due to increased sedation.3
Posttraumatic stress disorder (PTSD). Research has shown clonidine can help reduce hyperarousal symptoms, address sleep difficulties, and reduce PTSD trauma nightmares, anxiety, and irritability.4
Substance detoxification. Clonidine successfully suppresses opiate withdrawal signs and symptoms by reducing sympathetic overactivity. It can help with alcohol withdrawal and smoking cessation.2
Antipsychotic-induced akathisia. Controlled trials have shown that clonidine significantly reduces akathisia associated with the use of antipsychotics.2
Sialorrhea. Due to its anticholinergic effects, clonidine can effectively reduce antipsychotic-induced hypersalivation.2
Behavioral disturbances. Due to its sedative and anti-impulsive properties, clonidine can be used to address broadly defined behavioral issues, including anxiety-related behaviors, aggression, and agitation, although there is a lack of proven efficacy.1,2,4
1. Stahl SM, Grady MM, Muntner N. Stahl’s Essential Psychopharmacology: Prescriber’s Guide: Children and Adolescents. Cambridge University Press; 2019.
2. Naguy A. Clonidine use in psychiatry: panacea or panache. Pharmacology. 2016;98(1-2):87-92. doi:10.1159/000446441
3. Jang YJ, Choi H, Han TS, et al. Effectiveness of clonidine in child and adolescent sleep disorders. Psychiatry Investig. 2022;19(9):738-747. doi:10.30773/pi.2022.0117
4. Bajor LA, Balsara C, Osser DN. An evidence-based approach to psychopharmacology for posttraumatic stress disorder (PTSD) - 2022 update. Psychiatry Res. 2022;317:114840. doi:10.1016/j.psychres.2022.114840
Clonidine is a centrally acting alpha-2 agonist originally developed for treating hypertension. It is believed to work by stimulating alpha-2 receptors in various areas of the brain. It is nonselective, binding alpha-2A, -2B, and -2C receptors, and mediates inattentiveness, hyperactivity, impulsivity, sedation, and hypotension.1 Clonidine is available as immediate-release (IR), extended-release, and patch formulations, with typical doses ranging from 0.1 to 0.4 mg/d. The most common adverse effects are anticholinergic, such as sedation, dry mouth, and constipation. Since clonidine is effective at lowering blood pressure, the main safety concern is the possibility of rebound hypertension if abruptly stopped, which necessitates a short taper period.1
In child and adolescent psychiatry, the only FDA-approved use of clonidine is for treating attention-deficit/hyperactivity disorder (ADHD). Yet this medication has been increasingly used off-label for several common psychiatric ailments in pediatric patients. In this article, we discuss potential uses of clonidine in child and adolescent psychiatry; except for ADHD, all uses we describe are off-label.
ADHD. Clonidine is effective both as a monotherapy and as an adjunctive therapy to stimulants for pediatric ADHD. When used alone, clonidine is better suited for patients who have hyperactivity as their primary concern, whereas stimulants may be better suited for patients with inattentive subtypes. It also can help reduce sleep disturbances associated with the use of stimulants, especially insomnia.1
Tics/Tourette syndrome. Clonidine is a first-line treatment for tics in Tourette syndrome, demonstrating high efficacy with limited or no adverse effects. Furthermore, ADHD is the most common comorbid condition in patients with dystonic tics, which makes clonidine useful for simultaneously treating both conditions.2
Insomnia. Currently, there are no FDA-approved medications for treating sleep disorders in children and adolescents. However, clonidine is among the most used medications for childhood sleep difficulties, second only to antihistamines. The IR formulation is often preferred for this indication due to increased sedation.3
Posttraumatic stress disorder (PTSD). Research has shown clonidine can help reduce hyperarousal symptoms, address sleep difficulties, and reduce PTSD trauma nightmares, anxiety, and irritability.4
Substance detoxification. Clonidine successfully suppresses opiate withdrawal signs and symptoms by reducing sympathetic overactivity. It can help with alcohol withdrawal and smoking cessation.2
Antipsychotic-induced akathisia. Controlled trials have shown that clonidine significantly reduces akathisia associated with the use of antipsychotics.2
Sialorrhea. Due to its anticholinergic effects, clonidine can effectively reduce antipsychotic-induced hypersalivation.2
Behavioral disturbances. Due to its sedative and anti-impulsive properties, clonidine can be used to address broadly defined behavioral issues, including anxiety-related behaviors, aggression, and agitation, although there is a lack of proven efficacy.1,2,4
Clonidine is a centrally acting alpha-2 agonist originally developed for treating hypertension. It is believed to work by stimulating alpha-2 receptors in various areas of the brain. It is nonselective, binding alpha-2A, -2B, and -2C receptors, and mediates inattentiveness, hyperactivity, impulsivity, sedation, and hypotension.1 Clonidine is available as immediate-release (IR), extended-release, and patch formulations, with typical doses ranging from 0.1 to 0.4 mg/d. The most common adverse effects are anticholinergic, such as sedation, dry mouth, and constipation. Since clonidine is effective at lowering blood pressure, the main safety concern is the possibility of rebound hypertension if abruptly stopped, which necessitates a short taper period.1
In child and adolescent psychiatry, the only FDA-approved use of clonidine is for treating attention-deficit/hyperactivity disorder (ADHD). Yet this medication has been increasingly used off-label for several common psychiatric ailments in pediatric patients. In this article, we discuss potential uses of clonidine in child and adolescent psychiatry; except for ADHD, all uses we describe are off-label.
ADHD. Clonidine is effective both as a monotherapy and as an adjunctive therapy to stimulants for pediatric ADHD. When used alone, clonidine is better suited for patients who have hyperactivity as their primary concern, whereas stimulants may be better suited for patients with inattentive subtypes. It also can help reduce sleep disturbances associated with the use of stimulants, especially insomnia.1
Tics/Tourette syndrome. Clonidine is a first-line treatment for tics in Tourette syndrome, demonstrating high efficacy with limited or no adverse effects. Furthermore, ADHD is the most common comorbid condition in patients with dystonic tics, which makes clonidine useful for simultaneously treating both conditions.2
Insomnia. Currently, there are no FDA-approved medications for treating sleep disorders in children and adolescents. However, clonidine is among the most used medications for childhood sleep difficulties, second only to antihistamines. The IR formulation is often preferred for this indication due to increased sedation.3
Posttraumatic stress disorder (PTSD). Research has shown clonidine can help reduce hyperarousal symptoms, address sleep difficulties, and reduce PTSD trauma nightmares, anxiety, and irritability.4
Substance detoxification. Clonidine successfully suppresses opiate withdrawal signs and symptoms by reducing sympathetic overactivity. It can help with alcohol withdrawal and smoking cessation.2
Antipsychotic-induced akathisia. Controlled trials have shown that clonidine significantly reduces akathisia associated with the use of antipsychotics.2
Sialorrhea. Due to its anticholinergic effects, clonidine can effectively reduce antipsychotic-induced hypersalivation.2
Behavioral disturbances. Due to its sedative and anti-impulsive properties, clonidine can be used to address broadly defined behavioral issues, including anxiety-related behaviors, aggression, and agitation, although there is a lack of proven efficacy.1,2,4
1. Stahl SM, Grady MM, Muntner N. Stahl’s Essential Psychopharmacology: Prescriber’s Guide: Children and Adolescents. Cambridge University Press; 2019.
2. Naguy A. Clonidine use in psychiatry: panacea or panache. Pharmacology. 2016;98(1-2):87-92. doi:10.1159/000446441
3. Jang YJ, Choi H, Han TS, et al. Effectiveness of clonidine in child and adolescent sleep disorders. Psychiatry Investig. 2022;19(9):738-747. doi:10.30773/pi.2022.0117
4. Bajor LA, Balsara C, Osser DN. An evidence-based approach to psychopharmacology for posttraumatic stress disorder (PTSD) - 2022 update. Psychiatry Res. 2022;317:114840. doi:10.1016/j.psychres.2022.114840
1. Stahl SM, Grady MM, Muntner N. Stahl’s Essential Psychopharmacology: Prescriber’s Guide: Children and Adolescents. Cambridge University Press; 2019.
2. Naguy A. Clonidine use in psychiatry: panacea or panache. Pharmacology. 2016;98(1-2):87-92. doi:10.1159/000446441
3. Jang YJ, Choi H, Han TS, et al. Effectiveness of clonidine in child and adolescent sleep disorders. Psychiatry Investig. 2022;19(9):738-747. doi:10.30773/pi.2022.0117
4. Bajor LA, Balsara C, Osser DN. An evidence-based approach to psychopharmacology for posttraumatic stress disorder (PTSD) - 2022 update. Psychiatry Res. 2022;317:114840. doi:10.1016/j.psychres.2022.114840
Intranasal esketamine: A primer
Intranasal esketamine is an FDA-approved ketamine molecule indicated for use together with an oral antidepressant for treatment-resistant depression (TRD) in patients age ≥18 who have had an inadequate response to ≥2 antidepressants, and for depressive symptoms in adults with major depressive disorder with suicidal thoughts or actions.¹ Since March 2019, we’ve been treating patients with intranasal esketamine. Based on our experiences, here is a summary of what we have learned.
REMS is required. Due to the potential risks resulting from sedation and dissociation caused by esketamine and the risk of abuse and misuse, esketamine is available only through a Risk Evaluation and Mitigation Strategy (REMS) program. The program links your office Drug Enforcement Administration number to the address where this schedule III medication will be stored and given to the patient for self-administration. Requirements and other details about the REMS are available at www.spravatorems.com.
Treatment. Start with the online REMS patient enrollment/consent form. Contraindications include having a history of aneurysmal vascular disease, intracerebral hemorrhage, or allergy to ketamine/esketamine. Adjunctive treatment with esketamine plus sertraline, escitalopram, venlafaxine, or duloxetine are comparably effective.¹ We have found that adding magnesium to block glutamate action at N-methyl-
Iatrogenic effects rarely lead to dropout. The first session is critical to allay anticipatory anxiety. Sedation, blood pressure increase, and dissociation are common but transient adverse effects that typically peak at 40 minutes and resolve by 90 minutes. Record blood pressure on a REMS monitoring form before treatment, at 40 minutes, and at 2 hours. Avoid administering sedative or prohypertensive medications together with esketamine.¹ Dissociation is more common in patients with a history of trauma. Combine music, guided imagery, or psychotherapy to harness this for therapeutic benefit. Sleepiness can last 4 hours; make sure the patient has arranged for a ride home, as they cannot drive until the next day. Verify normal blood pressure before starting treatment. Clonidine or labetalol for hypertension/severe dissociation and ondansetron or prochlorperazine for nausea are rarely needed. Advise patients to use the bathroom before treatment and keep a trash can nearby for vomiting. Other transient adverse effects found in TRD clinical trials that occurred >5% and twice that of placebo were dizziness, vertigo, numbness, and feeling drunk.¹
Reimbursement for treatment with esketamine is available through most insurances, including copay cards, rebates, deductible support, and free assistance programs. Coverage is either through pharmacy benefit, assignment of medical benefit (pharmacy handles the medical benefit), or medical benefit with remuneration above wholesale price.
Zeitgeist shift. Emergency departments are backlogged and patients languish waiting to feel the effects of oral antidepressants. Intranasal esketamine could help alleviate this situation by producing a more immediate response. We also have observed improvements in comorbid posttraumatic stress disorder and in cognitive deficits of dementia, possibly due to rapidly enhanced neuroplasticity, neurogenesis, and astrocyte functioning, which NMDA receptor antagonism, AMPA activation, and downstream mediators (eg, brain-derived neurotrophic factor) may promote.4
1. Spravato (esketamine nasal spray) medication guide. Accessed November 22, 2022. https://www.janssenlabels.com/package-insert/product-patient-information/SPRAVATO-medication-guide.pdf
2. Spravato Healthcare Professional Website. TRD safety & efficacy. Accessed November 22, 2022. https://www.spravatohcp.com/trd-long-term/efficacy
3. Popova V, Daly EJ, Trivedi M, et al. Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: a randomized double-blind active-controlled study. Am J Psychiatry. 2019;176(6):428-438. doi:10.1176/appi.ajp.2019.19020172
4. Matveychuk D, Thomas RK, Swainson J, et al. Ketamine as an antidepressant: overview of its mechanisms of action and potential predictive biomarkers. Ther Adv Psychopharmacol. 2020;10:2045125320916657. doi:10.1177/2045125320916657
Intranasal esketamine is an FDA-approved ketamine molecule indicated for use together with an oral antidepressant for treatment-resistant depression (TRD) in patients age ≥18 who have had an inadequate response to ≥2 antidepressants, and for depressive symptoms in adults with major depressive disorder with suicidal thoughts or actions.¹ Since March 2019, we’ve been treating patients with intranasal esketamine. Based on our experiences, here is a summary of what we have learned.
REMS is required. Due to the potential risks resulting from sedation and dissociation caused by esketamine and the risk of abuse and misuse, esketamine is available only through a Risk Evaluation and Mitigation Strategy (REMS) program. The program links your office Drug Enforcement Administration number to the address where this schedule III medication will be stored and given to the patient for self-administration. Requirements and other details about the REMS are available at www.spravatorems.com.
Treatment. Start with the online REMS patient enrollment/consent form. Contraindications include having a history of aneurysmal vascular disease, intracerebral hemorrhage, or allergy to ketamine/esketamine. Adjunctive treatment with esketamine plus sertraline, escitalopram, venlafaxine, or duloxetine are comparably effective.¹ We have found that adding magnesium to block glutamate action at N-methyl-
Iatrogenic effects rarely lead to dropout. The first session is critical to allay anticipatory anxiety. Sedation, blood pressure increase, and dissociation are common but transient adverse effects that typically peak at 40 minutes and resolve by 90 minutes. Record blood pressure on a REMS monitoring form before treatment, at 40 minutes, and at 2 hours. Avoid administering sedative or prohypertensive medications together with esketamine.¹ Dissociation is more common in patients with a history of trauma. Combine music, guided imagery, or psychotherapy to harness this for therapeutic benefit. Sleepiness can last 4 hours; make sure the patient has arranged for a ride home, as they cannot drive until the next day. Verify normal blood pressure before starting treatment. Clonidine or labetalol for hypertension/severe dissociation and ondansetron or prochlorperazine for nausea are rarely needed. Advise patients to use the bathroom before treatment and keep a trash can nearby for vomiting. Other transient adverse effects found in TRD clinical trials that occurred >5% and twice that of placebo were dizziness, vertigo, numbness, and feeling drunk.¹
Reimbursement for treatment with esketamine is available through most insurances, including copay cards, rebates, deductible support, and free assistance programs. Coverage is either through pharmacy benefit, assignment of medical benefit (pharmacy handles the medical benefit), or medical benefit with remuneration above wholesale price.
Zeitgeist shift. Emergency departments are backlogged and patients languish waiting to feel the effects of oral antidepressants. Intranasal esketamine could help alleviate this situation by producing a more immediate response. We also have observed improvements in comorbid posttraumatic stress disorder and in cognitive deficits of dementia, possibly due to rapidly enhanced neuroplasticity, neurogenesis, and astrocyte functioning, which NMDA receptor antagonism, AMPA activation, and downstream mediators (eg, brain-derived neurotrophic factor) may promote.4
Intranasal esketamine is an FDA-approved ketamine molecule indicated for use together with an oral antidepressant for treatment-resistant depression (TRD) in patients age ≥18 who have had an inadequate response to ≥2 antidepressants, and for depressive symptoms in adults with major depressive disorder with suicidal thoughts or actions.¹ Since March 2019, we’ve been treating patients with intranasal esketamine. Based on our experiences, here is a summary of what we have learned.
REMS is required. Due to the potential risks resulting from sedation and dissociation caused by esketamine and the risk of abuse and misuse, esketamine is available only through a Risk Evaluation and Mitigation Strategy (REMS) program. The program links your office Drug Enforcement Administration number to the address where this schedule III medication will be stored and given to the patient for self-administration. Requirements and other details about the REMS are available at www.spravatorems.com.
Treatment. Start with the online REMS patient enrollment/consent form. Contraindications include having a history of aneurysmal vascular disease, intracerebral hemorrhage, or allergy to ketamine/esketamine. Adjunctive treatment with esketamine plus sertraline, escitalopram, venlafaxine, or duloxetine are comparably effective.¹ We have found that adding magnesium to block glutamate action at N-methyl-
Iatrogenic effects rarely lead to dropout. The first session is critical to allay anticipatory anxiety. Sedation, blood pressure increase, and dissociation are common but transient adverse effects that typically peak at 40 minutes and resolve by 90 minutes. Record blood pressure on a REMS monitoring form before treatment, at 40 minutes, and at 2 hours. Avoid administering sedative or prohypertensive medications together with esketamine.¹ Dissociation is more common in patients with a history of trauma. Combine music, guided imagery, or psychotherapy to harness this for therapeutic benefit. Sleepiness can last 4 hours; make sure the patient has arranged for a ride home, as they cannot drive until the next day. Verify normal blood pressure before starting treatment. Clonidine or labetalol for hypertension/severe dissociation and ondansetron or prochlorperazine for nausea are rarely needed. Advise patients to use the bathroom before treatment and keep a trash can nearby for vomiting. Other transient adverse effects found in TRD clinical trials that occurred >5% and twice that of placebo were dizziness, vertigo, numbness, and feeling drunk.¹
Reimbursement for treatment with esketamine is available through most insurances, including copay cards, rebates, deductible support, and free assistance programs. Coverage is either through pharmacy benefit, assignment of medical benefit (pharmacy handles the medical benefit), or medical benefit with remuneration above wholesale price.
Zeitgeist shift. Emergency departments are backlogged and patients languish waiting to feel the effects of oral antidepressants. Intranasal esketamine could help alleviate this situation by producing a more immediate response. We also have observed improvements in comorbid posttraumatic stress disorder and in cognitive deficits of dementia, possibly due to rapidly enhanced neuroplasticity, neurogenesis, and astrocyte functioning, which NMDA receptor antagonism, AMPA activation, and downstream mediators (eg, brain-derived neurotrophic factor) may promote.4
1. Spravato (esketamine nasal spray) medication guide. Accessed November 22, 2022. https://www.janssenlabels.com/package-insert/product-patient-information/SPRAVATO-medication-guide.pdf
2. Spravato Healthcare Professional Website. TRD safety & efficacy. Accessed November 22, 2022. https://www.spravatohcp.com/trd-long-term/efficacy
3. Popova V, Daly EJ, Trivedi M, et al. Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: a randomized double-blind active-controlled study. Am J Psychiatry. 2019;176(6):428-438. doi:10.1176/appi.ajp.2019.19020172
4. Matveychuk D, Thomas RK, Swainson J, et al. Ketamine as an antidepressant: overview of its mechanisms of action and potential predictive biomarkers. Ther Adv Psychopharmacol. 2020;10:2045125320916657. doi:10.1177/2045125320916657
1. Spravato (esketamine nasal spray) medication guide. Accessed November 22, 2022. https://www.janssenlabels.com/package-insert/product-patient-information/SPRAVATO-medication-guide.pdf
2. Spravato Healthcare Professional Website. TRD safety & efficacy. Accessed November 22, 2022. https://www.spravatohcp.com/trd-long-term/efficacy
3. Popova V, Daly EJ, Trivedi M, et al. Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: a randomized double-blind active-controlled study. Am J Psychiatry. 2019;176(6):428-438. doi:10.1176/appi.ajp.2019.19020172
4. Matveychuk D, Thomas RK, Swainson J, et al. Ketamine as an antidepressant: overview of its mechanisms of action and potential predictive biomarkers. Ther Adv Psychopharmacol. 2020;10:2045125320916657. doi:10.1177/2045125320916657
More on SWOT analysis, more
I enjoyed reading the optimistic outlook for psychiatry outlined in your SWOT analysis (“Contemporary psychiatry: A SWOT analysis,”
I think, though, you misplaced an opportunity as a threat in your assessment that the increase in the amount of advanced practice psychiatric nurses (PMHAPRNs) presents a threat to psychiatry. The presence of an increased number of PMHAPRNs provides access to a larger number of people needing treatment by qualified, skilled mental health professionals and an opportunity for psychiatrists to participate in highly effective teams of psychiatric clinicians. This workforce-building is of particular importance during our current clinician shortage, especially within psychiatry. Most research has shown that advanced practice nurses’ quality of care is competitive with that of physicians with similar experience, and that patient satisfaction is high. Advanced practice nurses are more likely than physicians to provide care in underserved populations and in rural communities. We are educated to practice independently within our scope, to standards established by our professional organizations as well as American Psychiatric Association (APA) clinical guidelines. I hope you will reconsider your view of your PMHAPRN colleagues as a threat and see them as a positive contribution to your chosen field of psychiatry, like the APA has shown in their choice of including a PMHAPRN as a clinical expert team member on the SMI Adviser initiative.
Stella Logan, APRN, PMHCNS-BC, PMHNP-BC
Austin, Texas
Dr. Nasrallah responds
Thank you for your letter regarding my SWOT article. It was originally written for the newsletter of the Ohio Psychiatric Physicians Association, comprised of 1,000 psychiatrists. To them, nurse practitioners (NPs) are regarded as a threat because some mental health care systems have been laying off psychiatrists and hiring NPs to lower costs. This obviously is perceived as a threat. I do agree with you that well-qualified NPs are providing needed mental health services in underserved areas (eg, inner cities and rural areas), where it is very difficult to recruit psychiatrists due to the severe shortage nationally.
Henry A. Nasrallah, MD, DLFAPA
Editor-in-Chief
Continue to: More on the transdiagnostic model
More on the transdiagnostic model
I just had the pleasure of reading your February 2023 editorial (“Depression and schizophrenia: Many biological and clinical similarities,”
David Krassner, MD
Phoenix, Arizona
I completely agree with your promotion of a unified transdiagnostic model. All of this makes sense on the continuum of consciousness—restricted consciousness represents fear, whereas wide consciousness represents complete connectivity (love in the spiritual sense). Therefore, a threat not resolved can lead to defeat and an unresolved painful defeat can lead to a psychotic projection. Is it no surprise, then, that a medication such as quetiapine can treat the whole continuum from anxiety at low doses to psychosis at high doses?
Mike Primc, MD
Chardon, Ohio
I enjoyed reading the optimistic outlook for psychiatry outlined in your SWOT analysis (“Contemporary psychiatry: A SWOT analysis,”
I think, though, you misplaced an opportunity as a threat in your assessment that the increase in the amount of advanced practice psychiatric nurses (PMHAPRNs) presents a threat to psychiatry. The presence of an increased number of PMHAPRNs provides access to a larger number of people needing treatment by qualified, skilled mental health professionals and an opportunity for psychiatrists to participate in highly effective teams of psychiatric clinicians. This workforce-building is of particular importance during our current clinician shortage, especially within psychiatry. Most research has shown that advanced practice nurses’ quality of care is competitive with that of physicians with similar experience, and that patient satisfaction is high. Advanced practice nurses are more likely than physicians to provide care in underserved populations and in rural communities. We are educated to practice independently within our scope, to standards established by our professional organizations as well as American Psychiatric Association (APA) clinical guidelines. I hope you will reconsider your view of your PMHAPRN colleagues as a threat and see them as a positive contribution to your chosen field of psychiatry, like the APA has shown in their choice of including a PMHAPRN as a clinical expert team member on the SMI Adviser initiative.
Stella Logan, APRN, PMHCNS-BC, PMHNP-BC
Austin, Texas
Dr. Nasrallah responds
Thank you for your letter regarding my SWOT article. It was originally written for the newsletter of the Ohio Psychiatric Physicians Association, comprised of 1,000 psychiatrists. To them, nurse practitioners (NPs) are regarded as a threat because some mental health care systems have been laying off psychiatrists and hiring NPs to lower costs. This obviously is perceived as a threat. I do agree with you that well-qualified NPs are providing needed mental health services in underserved areas (eg, inner cities and rural areas), where it is very difficult to recruit psychiatrists due to the severe shortage nationally.
Henry A. Nasrallah, MD, DLFAPA
Editor-in-Chief
Continue to: More on the transdiagnostic model
More on the transdiagnostic model
I just had the pleasure of reading your February 2023 editorial (“Depression and schizophrenia: Many biological and clinical similarities,”
David Krassner, MD
Phoenix, Arizona
I completely agree with your promotion of a unified transdiagnostic model. All of this makes sense on the continuum of consciousness—restricted consciousness represents fear, whereas wide consciousness represents complete connectivity (love in the spiritual sense). Therefore, a threat not resolved can lead to defeat and an unresolved painful defeat can lead to a psychotic projection. Is it no surprise, then, that a medication such as quetiapine can treat the whole continuum from anxiety at low doses to psychosis at high doses?
Mike Primc, MD
Chardon, Ohio
I enjoyed reading the optimistic outlook for psychiatry outlined in your SWOT analysis (“Contemporary psychiatry: A SWOT analysis,”
I think, though, you misplaced an opportunity as a threat in your assessment that the increase in the amount of advanced practice psychiatric nurses (PMHAPRNs) presents a threat to psychiatry. The presence of an increased number of PMHAPRNs provides access to a larger number of people needing treatment by qualified, skilled mental health professionals and an opportunity for psychiatrists to participate in highly effective teams of psychiatric clinicians. This workforce-building is of particular importance during our current clinician shortage, especially within psychiatry. Most research has shown that advanced practice nurses’ quality of care is competitive with that of physicians with similar experience, and that patient satisfaction is high. Advanced practice nurses are more likely than physicians to provide care in underserved populations and in rural communities. We are educated to practice independently within our scope, to standards established by our professional organizations as well as American Psychiatric Association (APA) clinical guidelines. I hope you will reconsider your view of your PMHAPRN colleagues as a threat and see them as a positive contribution to your chosen field of psychiatry, like the APA has shown in their choice of including a PMHAPRN as a clinical expert team member on the SMI Adviser initiative.
Stella Logan, APRN, PMHCNS-BC, PMHNP-BC
Austin, Texas
Dr. Nasrallah responds
Thank you for your letter regarding my SWOT article. It was originally written for the newsletter of the Ohio Psychiatric Physicians Association, comprised of 1,000 psychiatrists. To them, nurse practitioners (NPs) are regarded as a threat because some mental health care systems have been laying off psychiatrists and hiring NPs to lower costs. This obviously is perceived as a threat. I do agree with you that well-qualified NPs are providing needed mental health services in underserved areas (eg, inner cities and rural areas), where it is very difficult to recruit psychiatrists due to the severe shortage nationally.
Henry A. Nasrallah, MD, DLFAPA
Editor-in-Chief
Continue to: More on the transdiagnostic model
More on the transdiagnostic model
I just had the pleasure of reading your February 2023 editorial (“Depression and schizophrenia: Many biological and clinical similarities,”
David Krassner, MD
Phoenix, Arizona
I completely agree with your promotion of a unified transdiagnostic model. All of this makes sense on the continuum of consciousness—restricted consciousness represents fear, whereas wide consciousness represents complete connectivity (love in the spiritual sense). Therefore, a threat not resolved can lead to defeat and an unresolved painful defeat can lead to a psychotic projection. Is it no surprise, then, that a medication such as quetiapine can treat the whole continuum from anxiety at low doses to psychosis at high doses?
Mike Primc, MD
Chardon, Ohio
Psychiatric comorbidities predict complex polypharmacy in bipolar disorder
Patients with bipolar disorder (BD) often receive prescriptions for multiple medications to manage a range of medical and psychiatric symptoms, but the definition of polypharmacy in these patients is inconsistent, and characteristics associated with complex polypharmacy have not been well studied, wrote Andrea Aguglia, MD, of the University of Genoa, Italy, and colleagues.
Previous studies have shown an increased risk for comorbid medical and psychiatric illnesses in BD patients, the researchers noted, and changes in prescribing trends have prompted greater use of combination therapies such as mood stabilizers with or without antipsychotics.
In a study published in Psychiatry Research, the investigators reviewed data from 556 adults with BD. Participants were aged 18 and older with a primary diagnosis of BD type I or II based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, criteria. The mean age of the participants was 49.17 years, 43.7% were male, and 34.2% were employed. A total of 327 patients (58.8%) had a medical comorbidity, and 193 (34.7%) used an illicit substance.
A total of 225 patients (40.5%) met the criteria for complex polypharmacy by taking at least 4 medications.
BD patients with complex polypharmacy were significantly more likely than those without complex polypharmacy to be single (50.7% vs. 37.8%, P = .025) and unemployed (25.3% vs. 40.2%, P < .001).
On the clinical side, complex polypharmacy in BD patients was significantly associated with a higher prevalence of both medical and psychiatric comorbidities (65.3% vs. 54.4%, P = .010; and 50.7% vs. 34.1%, P < .001, respectively). The association with medical comorbidities and complex polypharmacy in BD was unexpected, the researchers said, “as psychotropic medications should be used with cautiousness in patients suffering from medical conditions.”
BD patients with complex polypharmacy also had a significantly earlier age of onset, longer duration of illness, and increased number of hospitalizations than those without complex polypharmacy.
Rates of at least one substance including alcohol, cannabinoids, and cocaine/amphetamines were significantly higher among BD patients with complex polypharmacy, compared with those without, but no differences in heroin use were noted between the groups.
In a logistic regression analysis, single status, older age, number of hospitalizations, and the presence of psychiatric comorbidities were significantly associated with complex polypharmacy.
The study findings were limited by several factors including the focus on an inpatient population, inability to consider clinical factors such as type of mood episode and bipolar cycle, and the cross-sectional design that prevented conclusions of causality, the researchers noted.
However, the study is the first known to focus on both sociodemographic and clinical factors associated with polypharmacy in BD, and the results suggest that implementing complementary psychosocial strategies might help reduce medication use in these patients, they concluded. Data from further longitudinal studies may help guide long-term management of BD, “especially when pharmacological discontinuation is needed,” they said.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Patients with bipolar disorder (BD) often receive prescriptions for multiple medications to manage a range of medical and psychiatric symptoms, but the definition of polypharmacy in these patients is inconsistent, and characteristics associated with complex polypharmacy have not been well studied, wrote Andrea Aguglia, MD, of the University of Genoa, Italy, and colleagues.
Previous studies have shown an increased risk for comorbid medical and psychiatric illnesses in BD patients, the researchers noted, and changes in prescribing trends have prompted greater use of combination therapies such as mood stabilizers with or without antipsychotics.
In a study published in Psychiatry Research, the investigators reviewed data from 556 adults with BD. Participants were aged 18 and older with a primary diagnosis of BD type I or II based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, criteria. The mean age of the participants was 49.17 years, 43.7% were male, and 34.2% were employed. A total of 327 patients (58.8%) had a medical comorbidity, and 193 (34.7%) used an illicit substance.
A total of 225 patients (40.5%) met the criteria for complex polypharmacy by taking at least 4 medications.
BD patients with complex polypharmacy were significantly more likely than those without complex polypharmacy to be single (50.7% vs. 37.8%, P = .025) and unemployed (25.3% vs. 40.2%, P < .001).
On the clinical side, complex polypharmacy in BD patients was significantly associated with a higher prevalence of both medical and psychiatric comorbidities (65.3% vs. 54.4%, P = .010; and 50.7% vs. 34.1%, P < .001, respectively). The association with medical comorbidities and complex polypharmacy in BD was unexpected, the researchers said, “as psychotropic medications should be used with cautiousness in patients suffering from medical conditions.”
BD patients with complex polypharmacy also had a significantly earlier age of onset, longer duration of illness, and increased number of hospitalizations than those without complex polypharmacy.
Rates of at least one substance including alcohol, cannabinoids, and cocaine/amphetamines were significantly higher among BD patients with complex polypharmacy, compared with those without, but no differences in heroin use were noted between the groups.
In a logistic regression analysis, single status, older age, number of hospitalizations, and the presence of psychiatric comorbidities were significantly associated with complex polypharmacy.
The study findings were limited by several factors including the focus on an inpatient population, inability to consider clinical factors such as type of mood episode and bipolar cycle, and the cross-sectional design that prevented conclusions of causality, the researchers noted.
However, the study is the first known to focus on both sociodemographic and clinical factors associated with polypharmacy in BD, and the results suggest that implementing complementary psychosocial strategies might help reduce medication use in these patients, they concluded. Data from further longitudinal studies may help guide long-term management of BD, “especially when pharmacological discontinuation is needed,” they said.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Patients with bipolar disorder (BD) often receive prescriptions for multiple medications to manage a range of medical and psychiatric symptoms, but the definition of polypharmacy in these patients is inconsistent, and characteristics associated with complex polypharmacy have not been well studied, wrote Andrea Aguglia, MD, of the University of Genoa, Italy, and colleagues.
Previous studies have shown an increased risk for comorbid medical and psychiatric illnesses in BD patients, the researchers noted, and changes in prescribing trends have prompted greater use of combination therapies such as mood stabilizers with or without antipsychotics.
In a study published in Psychiatry Research, the investigators reviewed data from 556 adults with BD. Participants were aged 18 and older with a primary diagnosis of BD type I or II based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, criteria. The mean age of the participants was 49.17 years, 43.7% were male, and 34.2% were employed. A total of 327 patients (58.8%) had a medical comorbidity, and 193 (34.7%) used an illicit substance.
A total of 225 patients (40.5%) met the criteria for complex polypharmacy by taking at least 4 medications.
BD patients with complex polypharmacy were significantly more likely than those without complex polypharmacy to be single (50.7% vs. 37.8%, P = .025) and unemployed (25.3% vs. 40.2%, P < .001).
On the clinical side, complex polypharmacy in BD patients was significantly associated with a higher prevalence of both medical and psychiatric comorbidities (65.3% vs. 54.4%, P = .010; and 50.7% vs. 34.1%, P < .001, respectively). The association with medical comorbidities and complex polypharmacy in BD was unexpected, the researchers said, “as psychotropic medications should be used with cautiousness in patients suffering from medical conditions.”
BD patients with complex polypharmacy also had a significantly earlier age of onset, longer duration of illness, and increased number of hospitalizations than those without complex polypharmacy.
Rates of at least one substance including alcohol, cannabinoids, and cocaine/amphetamines were significantly higher among BD patients with complex polypharmacy, compared with those without, but no differences in heroin use were noted between the groups.
In a logistic regression analysis, single status, older age, number of hospitalizations, and the presence of psychiatric comorbidities were significantly associated with complex polypharmacy.
The study findings were limited by several factors including the focus on an inpatient population, inability to consider clinical factors such as type of mood episode and bipolar cycle, and the cross-sectional design that prevented conclusions of causality, the researchers noted.
However, the study is the first known to focus on both sociodemographic and clinical factors associated with polypharmacy in BD, and the results suggest that implementing complementary psychosocial strategies might help reduce medication use in these patients, they concluded. Data from further longitudinal studies may help guide long-term management of BD, “especially when pharmacological discontinuation is needed,” they said.
The study received no outside funding. The researchers had no financial conflicts to disclose.
FROM PSYCHIATRY RESEARCH
Are parents infecting their children with contagious negativity?
A couple of weeks ago I stumbled across a report of a Pew Research Center’s survey titled “Parenting in America today” (Pew Research Center. Jan. 24, 2023), which found that 40% of parents in the United States with children younger than 18 are “extremely or very worried” that at some point their children might struggle with anxiety or depression. Thirty-six percent replied that they were “somewhat” worried. This total of more than 75% represents a significant change from the 2015 Pew Center survey in which only 54% of parents were “somewhat” worried about their children’s mental health.
Prompted by these findings I began work on a column in which I planned to encourage pediatricians to think more like family physicians when we were working with children who were experiencing serious mental health problems. My primary message was going to be that we should turn more of our attention to the mental health of the anxious parents who must endure the often long and frustrating path toward effective psychiatric care for their children. This might come in the form of some simple suggestions about nonpharmacologic self-help strategies. Or, it could mean encouraging parents to seek psychiatric care or counseling for themselves as they wait for help for their child.
However, as I began that column, my thoughts kept drifting toward a broader consideration of the relationship between parents and pediatric mental health. If mental health of children is causing their parents to be anxious and depressed isn’t it just as likely that this is a bidirectional connection? This was not exactly an “aha” moment for me because it is a relationship I have considered for sometime. However, it is a concept that I have come to realize is receiving far too little attention.
There are exceptions. For example, a recent opinion piece in the New York Times by David French, “What if Kids Are Sad and Stressed Because Their Parents Are?” (March 19, 2023) echoes many of my concerns. Drawing on his experiences traveling around college campuses, Mr. French observes, “Just as parents are upset about their children’s anxiety and depression, children are anxious about their parent’s mental health.”
He notes that an August 2022 NBC News poll found that 58% of registered voters feel this country’s best days are behind it and joins me in imagining that this negative mind set is filtering down to the pediatric population. He acknowledges that there are other likely contributors to teen unhappiness including the ubiquity of smart phones, the secularization of society, and the media’s focus on the political divide. However, Mr. French wonders if the parenting style that results in childhood experiences that are dominated by adult supervision and protection may also be playing a large role.
In his conclusion, Mr. French asks us to consider “How much fear and anxiety should we import to our lives and homes?” as we adults search for an answer.
As I continued to drill down for other possible solutions, I encountered an avenue of psychological research that suggests that instead of, or in addition to, filtering out the anxiety-generating deluge of information, we begin to give some thought to how our beliefs may be coloring our perception of reality.
Jeremy D.W. Clifton, PhD, a psychologist at the University of Pennsylvania Positive Psychology Center has done extensive research on the relationship between our basic beliefs about the world (known as primal beliefs or simply primals in psychologist lingo) and how we interpret reality. For example, one of your primal beliefs may be that the world is a dangerous place. I, on the other hand, may see the world as a stimulating environment offering me endless opportunities to explore. I may see the world as an abundant resource limited only by my creativity. You, however, see it as a barren wasteland.
Dr. Clifton’s research has shown that our primals (at least those of adults) are relatively immutable through one’s lifetime and “do not appear to be the consequence of our experiences.” For example, living in a ZIP code with a high crime rate does not predict that you will see the world as a dangerous place. Nor does being affluent guarantee that an adult sees the world rich with opportunities.
It is unclear exactly when and by what process we develop our primal beliefs, but it is safe to say our parents probably play a large role. Exactly to what degree the tsunami of bad news we are allowing to inundate our children’s lives plays a role is unclear. However, it is reasonable to assume that news about climate change, school shootings, and the pandemic must be a contributor.
According to Dr. Clifton, there is some evidence that certain mind exercises, when applied diligently, can occasionally modify the primal beliefs of an individual who sees the world as dangerous and barren. Until such strategies become more readily accessible, the best we can do is acknowledge that our children are like canaries in a coal mine full of negative perceptions, then do our best to clear the air.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
A couple of weeks ago I stumbled across a report of a Pew Research Center’s survey titled “Parenting in America today” (Pew Research Center. Jan. 24, 2023), which found that 40% of parents in the United States with children younger than 18 are “extremely or very worried” that at some point their children might struggle with anxiety or depression. Thirty-six percent replied that they were “somewhat” worried. This total of more than 75% represents a significant change from the 2015 Pew Center survey in which only 54% of parents were “somewhat” worried about their children’s mental health.
Prompted by these findings I began work on a column in which I planned to encourage pediatricians to think more like family physicians when we were working with children who were experiencing serious mental health problems. My primary message was going to be that we should turn more of our attention to the mental health of the anxious parents who must endure the often long and frustrating path toward effective psychiatric care for their children. This might come in the form of some simple suggestions about nonpharmacologic self-help strategies. Or, it could mean encouraging parents to seek psychiatric care or counseling for themselves as they wait for help for their child.
However, as I began that column, my thoughts kept drifting toward a broader consideration of the relationship between parents and pediatric mental health. If mental health of children is causing their parents to be anxious and depressed isn’t it just as likely that this is a bidirectional connection? This was not exactly an “aha” moment for me because it is a relationship I have considered for sometime. However, it is a concept that I have come to realize is receiving far too little attention.
There are exceptions. For example, a recent opinion piece in the New York Times by David French, “What if Kids Are Sad and Stressed Because Their Parents Are?” (March 19, 2023) echoes many of my concerns. Drawing on his experiences traveling around college campuses, Mr. French observes, “Just as parents are upset about their children’s anxiety and depression, children are anxious about their parent’s mental health.”
He notes that an August 2022 NBC News poll found that 58% of registered voters feel this country’s best days are behind it and joins me in imagining that this negative mind set is filtering down to the pediatric population. He acknowledges that there are other likely contributors to teen unhappiness including the ubiquity of smart phones, the secularization of society, and the media’s focus on the political divide. However, Mr. French wonders if the parenting style that results in childhood experiences that are dominated by adult supervision and protection may also be playing a large role.
In his conclusion, Mr. French asks us to consider “How much fear and anxiety should we import to our lives and homes?” as we adults search for an answer.
As I continued to drill down for other possible solutions, I encountered an avenue of psychological research that suggests that instead of, or in addition to, filtering out the anxiety-generating deluge of information, we begin to give some thought to how our beliefs may be coloring our perception of reality.
Jeremy D.W. Clifton, PhD, a psychologist at the University of Pennsylvania Positive Psychology Center has done extensive research on the relationship between our basic beliefs about the world (known as primal beliefs or simply primals in psychologist lingo) and how we interpret reality. For example, one of your primal beliefs may be that the world is a dangerous place. I, on the other hand, may see the world as a stimulating environment offering me endless opportunities to explore. I may see the world as an abundant resource limited only by my creativity. You, however, see it as a barren wasteland.
Dr. Clifton’s research has shown that our primals (at least those of adults) are relatively immutable through one’s lifetime and “do not appear to be the consequence of our experiences.” For example, living in a ZIP code with a high crime rate does not predict that you will see the world as a dangerous place. Nor does being affluent guarantee that an adult sees the world rich with opportunities.
It is unclear exactly when and by what process we develop our primal beliefs, but it is safe to say our parents probably play a large role. Exactly to what degree the tsunami of bad news we are allowing to inundate our children’s lives plays a role is unclear. However, it is reasonable to assume that news about climate change, school shootings, and the pandemic must be a contributor.
According to Dr. Clifton, there is some evidence that certain mind exercises, when applied diligently, can occasionally modify the primal beliefs of an individual who sees the world as dangerous and barren. Until such strategies become more readily accessible, the best we can do is acknowledge that our children are like canaries in a coal mine full of negative perceptions, then do our best to clear the air.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
A couple of weeks ago I stumbled across a report of a Pew Research Center’s survey titled “Parenting in America today” (Pew Research Center. Jan. 24, 2023), which found that 40% of parents in the United States with children younger than 18 are “extremely or very worried” that at some point their children might struggle with anxiety or depression. Thirty-six percent replied that they were “somewhat” worried. This total of more than 75% represents a significant change from the 2015 Pew Center survey in which only 54% of parents were “somewhat” worried about their children’s mental health.
Prompted by these findings I began work on a column in which I planned to encourage pediatricians to think more like family physicians when we were working with children who were experiencing serious mental health problems. My primary message was going to be that we should turn more of our attention to the mental health of the anxious parents who must endure the often long and frustrating path toward effective psychiatric care for their children. This might come in the form of some simple suggestions about nonpharmacologic self-help strategies. Or, it could mean encouraging parents to seek psychiatric care or counseling for themselves as they wait for help for their child.
However, as I began that column, my thoughts kept drifting toward a broader consideration of the relationship between parents and pediatric mental health. If mental health of children is causing their parents to be anxious and depressed isn’t it just as likely that this is a bidirectional connection? This was not exactly an “aha” moment for me because it is a relationship I have considered for sometime. However, it is a concept that I have come to realize is receiving far too little attention.
There are exceptions. For example, a recent opinion piece in the New York Times by David French, “What if Kids Are Sad and Stressed Because Their Parents Are?” (March 19, 2023) echoes many of my concerns. Drawing on his experiences traveling around college campuses, Mr. French observes, “Just as parents are upset about their children’s anxiety and depression, children are anxious about their parent’s mental health.”
He notes that an August 2022 NBC News poll found that 58% of registered voters feel this country’s best days are behind it and joins me in imagining that this negative mind set is filtering down to the pediatric population. He acknowledges that there are other likely contributors to teen unhappiness including the ubiquity of smart phones, the secularization of society, and the media’s focus on the political divide. However, Mr. French wonders if the parenting style that results in childhood experiences that are dominated by adult supervision and protection may also be playing a large role.
In his conclusion, Mr. French asks us to consider “How much fear and anxiety should we import to our lives and homes?” as we adults search for an answer.
As I continued to drill down for other possible solutions, I encountered an avenue of psychological research that suggests that instead of, or in addition to, filtering out the anxiety-generating deluge of information, we begin to give some thought to how our beliefs may be coloring our perception of reality.
Jeremy D.W. Clifton, PhD, a psychologist at the University of Pennsylvania Positive Psychology Center has done extensive research on the relationship between our basic beliefs about the world (known as primal beliefs or simply primals in psychologist lingo) and how we interpret reality. For example, one of your primal beliefs may be that the world is a dangerous place. I, on the other hand, may see the world as a stimulating environment offering me endless opportunities to explore. I may see the world as an abundant resource limited only by my creativity. You, however, see it as a barren wasteland.
Dr. Clifton’s research has shown that our primals (at least those of adults) are relatively immutable through one’s lifetime and “do not appear to be the consequence of our experiences.” For example, living in a ZIP code with a high crime rate does not predict that you will see the world as a dangerous place. Nor does being affluent guarantee that an adult sees the world rich with opportunities.
It is unclear exactly when and by what process we develop our primal beliefs, but it is safe to say our parents probably play a large role. Exactly to what degree the tsunami of bad news we are allowing to inundate our children’s lives plays a role is unclear. However, it is reasonable to assume that news about climate change, school shootings, and the pandemic must be a contributor.
According to Dr. Clifton, there is some evidence that certain mind exercises, when applied diligently, can occasionally modify the primal beliefs of an individual who sees the world as dangerous and barren. Until such strategies become more readily accessible, the best we can do is acknowledge that our children are like canaries in a coal mine full of negative perceptions, then do our best to clear the air.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Impact of child abuse differs by gender
PARIS – , new research shows.
Investigators found childhood emotional and sexual abuse had a greater effect on women than men, whereas men were more adversely affected by emotional and physical neglect.
“Our findings indicate that exposure to childhood maltreatment increases the risk of having psychiatric symptoms in both men and women,” lead researcher Thanavadee Prachason, PhD, department of psychiatry and neuropsychology, Maastricht (the Netherlands) University Medical Center, said in a press release.
“Exposure to emotionally or sexually abusive experiences during childhood increases the risk of a variety of psychiatric symptoms, particularly in women. In contrast, a history of emotional or physical neglect in childhood increases the risk of having psychiatric symptoms more in men,” Dr. Prachason added.
The findings were presented at the European Psychiatric Association 2023 Congress.
A leading mental illness risk factor
Study presenter Laura Fusar-Poli, MD, PhD, from the department of brain and behavioral sciences, University of Pavia (Italy), said that the differential impact of trauma subtypes in men and women indicate that both gender and the type of childhood adversity experienced need to be taken into account in future studies.
Dr. Fusar-Poli began by highlighting that 13%-36% of individuals have experienced some kind of childhood trauma, with 30% exposed to at least two types of trauma.
Trauma has been identified as a risk factor for a range of mental health problems.
“It is estimated that, worldwide, around one third of all psychiatric disorders are related to childhood trauma,” senior researcher Sinan Gül
Consequently, “childhood trauma is a leading preventable risk factor for mental illness,” he added.
Previous research suggests the subtype of trauma has an impact on subsequent biological changes and clinical outcomes, and that there are gender differences in the effects of childhood trauma.
To investigate, the researchers examined data from TwinssCan, a Belgian cohort of twins and siblings aged 15-35 years without a diagnosis of pervasive mental disorders.
The study included 477 females and 314 males who had completed the Childhood Trauma Questionnaire–Short Form (CTQ) and the Symptom Checklist-90 SR (SCL-90) to determine exposure to childhood adversity and levels of psychopathology, respectively.
Results showed that total CTQ scores were significantly associated with total SCL-90 scores in both men and women, as well as with each of the nine symptom domains of the SCL-90 (P < .001 for all assessments). These included psychoticism, paranoid ideation, anxiety, depression, somatization, obsessive-compulsive, interpersonal sensitivity, hostility, and phobic anxiety.
There were no significant differences in the associations with total CTQ scores between men and women.
However, when the researchers examined trauma subtypes and psychopathology, clear gender differences emerged.
Investigators found a significant association between emotional abuse on the CTQ and total SCL-90 scores in both men (P < .023) and women (P < .001), but that the association was significantly stronger in women (P = .043).
Sexual abuse was significantly associated with total SCL-90 scores in women (P < .001), while emotional neglect and physical neglect were significantly associated with psychopathology scores in men (P = .026 and P < .001, respectively).
“Physical neglect may include experiences of not having enough to eat, wearing dirty clothes, not being taken care of, and not getting taken to the doctor when the person was growing up,” said Dr. Prachason.
“Emotional neglect may include childhood experiences like not feeling loved or important, and not feeling close to the family.”
In women, emotional abuse was significantly associated with all nine symptom domains of the SCL-90, while sexual abuse was associated with seven: psychoticism, paranoid ideation, anxiety, depression, somatization, obsessive-compulsive, and hostility.
Physical neglect, in men, was significantly associated with eight of the symptom domains (all but somatization), but emotional neglect was linked only to depression, Dr. Fusar-Poli reported.
“This study showed a very important consequence of childhood trauma, and not only in people with mental disorders. I would like to underline that this is a general population, composed of adolescents and young adults, which is the age in which the majority of mental disorders starts, Dr. Fusar-Poli said in an interview.
She emphasized that psychotic disorders are only a part of the “broad range” of conditions that may be related to childhood trauma, which “can have an impact on sub-threshold symptoms that can affect functioning and quality of life in the general population.”
Addressing the differential findings in men and women, Dr. Gül
However, he said, this is “something that we really need understand,” as there is likely an underlying mechanism, “and not only a biological mechanism but probably a societal one.”
Dr. Gül
Compromised cognitive, emotional function
Commenting on the findings for this news organization, Elaine F. Walker, PhD, professor of psychology and neuroscience at Emory University in Atlanta, said stress exposure in general, including childhood trauma, “has transdiagnostic effects on vulnerability to mental disorders.”
“The effects are primarily mediated by the hypothalamic-pituitary-adrenal axis, which triggers the release of cortisol. When persistently elevated, this can result in neurobiological processes that have adverse effects on brain structure and circuitry which, in turn, compromises cognitive and emotional functioning,” said Dr. Walker, who was not associated with the study.
She noted that, “while it is possible that there are sex differences in biological sensitivity to certain subtypes of childhood trauma, it may also be the case that sex differences in the likelihood of exposure to trauma subtypes is actually the key factor.”
“At the present time, there are not specific treatment protocols aimed at addressing childhood trauma subtypes, but most experienced therapists will incorporate information about the individual’s trauma history in their treatment,” Dr. Walker added.
Also commenting on the research, Philip Gorwood, MD, PhD, head of the Clinique des Maladies Mentales et de l’Encéphale at Centre Hospitalier Sainte Anne in Paris, said the results are “important … as childhood trauma has been clearly recognized as a major risk factor for the vast majority of psychiatric disorders, but with poor knowledge of gender specificities.”
“Understanding which aspects of trauma are more damaging according to gender will facilitate research on the resilience process. Many intervention strategies will indeed benefit from a more personalized approach,” he said in a statement. Dr. Gorwood was not involved with this study.
The study authors, Dr. Gorwood, and Dr. Walker report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
PARIS – , new research shows.
Investigators found childhood emotional and sexual abuse had a greater effect on women than men, whereas men were more adversely affected by emotional and physical neglect.
“Our findings indicate that exposure to childhood maltreatment increases the risk of having psychiatric symptoms in both men and women,” lead researcher Thanavadee Prachason, PhD, department of psychiatry and neuropsychology, Maastricht (the Netherlands) University Medical Center, said in a press release.
“Exposure to emotionally or sexually abusive experiences during childhood increases the risk of a variety of psychiatric symptoms, particularly in women. In contrast, a history of emotional or physical neglect in childhood increases the risk of having psychiatric symptoms more in men,” Dr. Prachason added.
The findings were presented at the European Psychiatric Association 2023 Congress.
A leading mental illness risk factor
Study presenter Laura Fusar-Poli, MD, PhD, from the department of brain and behavioral sciences, University of Pavia (Italy), said that the differential impact of trauma subtypes in men and women indicate that both gender and the type of childhood adversity experienced need to be taken into account in future studies.
Dr. Fusar-Poli began by highlighting that 13%-36% of individuals have experienced some kind of childhood trauma, with 30% exposed to at least two types of trauma.
Trauma has been identified as a risk factor for a range of mental health problems.
“It is estimated that, worldwide, around one third of all psychiatric disorders are related to childhood trauma,” senior researcher Sinan Gül
Consequently, “childhood trauma is a leading preventable risk factor for mental illness,” he added.
Previous research suggests the subtype of trauma has an impact on subsequent biological changes and clinical outcomes, and that there are gender differences in the effects of childhood trauma.
To investigate, the researchers examined data from TwinssCan, a Belgian cohort of twins and siblings aged 15-35 years without a diagnosis of pervasive mental disorders.
The study included 477 females and 314 males who had completed the Childhood Trauma Questionnaire–Short Form (CTQ) and the Symptom Checklist-90 SR (SCL-90) to determine exposure to childhood adversity and levels of psychopathology, respectively.
Results showed that total CTQ scores were significantly associated with total SCL-90 scores in both men and women, as well as with each of the nine symptom domains of the SCL-90 (P < .001 for all assessments). These included psychoticism, paranoid ideation, anxiety, depression, somatization, obsessive-compulsive, interpersonal sensitivity, hostility, and phobic anxiety.
There were no significant differences in the associations with total CTQ scores between men and women.
However, when the researchers examined trauma subtypes and psychopathology, clear gender differences emerged.
Investigators found a significant association between emotional abuse on the CTQ and total SCL-90 scores in both men (P < .023) and women (P < .001), but that the association was significantly stronger in women (P = .043).
Sexual abuse was significantly associated with total SCL-90 scores in women (P < .001), while emotional neglect and physical neglect were significantly associated with psychopathology scores in men (P = .026 and P < .001, respectively).
“Physical neglect may include experiences of not having enough to eat, wearing dirty clothes, not being taken care of, and not getting taken to the doctor when the person was growing up,” said Dr. Prachason.
“Emotional neglect may include childhood experiences like not feeling loved or important, and not feeling close to the family.”
In women, emotional abuse was significantly associated with all nine symptom domains of the SCL-90, while sexual abuse was associated with seven: psychoticism, paranoid ideation, anxiety, depression, somatization, obsessive-compulsive, and hostility.
Physical neglect, in men, was significantly associated with eight of the symptom domains (all but somatization), but emotional neglect was linked only to depression, Dr. Fusar-Poli reported.
“This study showed a very important consequence of childhood trauma, and not only in people with mental disorders. I would like to underline that this is a general population, composed of adolescents and young adults, which is the age in which the majority of mental disorders starts, Dr. Fusar-Poli said in an interview.
She emphasized that psychotic disorders are only a part of the “broad range” of conditions that may be related to childhood trauma, which “can have an impact on sub-threshold symptoms that can affect functioning and quality of life in the general population.”
Addressing the differential findings in men and women, Dr. Gül
However, he said, this is “something that we really need understand,” as there is likely an underlying mechanism, “and not only a biological mechanism but probably a societal one.”
Dr. Gül
Compromised cognitive, emotional function
Commenting on the findings for this news organization, Elaine F. Walker, PhD, professor of psychology and neuroscience at Emory University in Atlanta, said stress exposure in general, including childhood trauma, “has transdiagnostic effects on vulnerability to mental disorders.”
“The effects are primarily mediated by the hypothalamic-pituitary-adrenal axis, which triggers the release of cortisol. When persistently elevated, this can result in neurobiological processes that have adverse effects on brain structure and circuitry which, in turn, compromises cognitive and emotional functioning,” said Dr. Walker, who was not associated with the study.
She noted that, “while it is possible that there are sex differences in biological sensitivity to certain subtypes of childhood trauma, it may also be the case that sex differences in the likelihood of exposure to trauma subtypes is actually the key factor.”
“At the present time, there are not specific treatment protocols aimed at addressing childhood trauma subtypes, but most experienced therapists will incorporate information about the individual’s trauma history in their treatment,” Dr. Walker added.
Also commenting on the research, Philip Gorwood, MD, PhD, head of the Clinique des Maladies Mentales et de l’Encéphale at Centre Hospitalier Sainte Anne in Paris, said the results are “important … as childhood trauma has been clearly recognized as a major risk factor for the vast majority of psychiatric disorders, but with poor knowledge of gender specificities.”
“Understanding which aspects of trauma are more damaging according to gender will facilitate research on the resilience process. Many intervention strategies will indeed benefit from a more personalized approach,” he said in a statement. Dr. Gorwood was not involved with this study.
The study authors, Dr. Gorwood, and Dr. Walker report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
PARIS – , new research shows.
Investigators found childhood emotional and sexual abuse had a greater effect on women than men, whereas men were more adversely affected by emotional and physical neglect.
“Our findings indicate that exposure to childhood maltreatment increases the risk of having psychiatric symptoms in both men and women,” lead researcher Thanavadee Prachason, PhD, department of psychiatry and neuropsychology, Maastricht (the Netherlands) University Medical Center, said in a press release.
“Exposure to emotionally or sexually abusive experiences during childhood increases the risk of a variety of psychiatric symptoms, particularly in women. In contrast, a history of emotional or physical neglect in childhood increases the risk of having psychiatric symptoms more in men,” Dr. Prachason added.
The findings were presented at the European Psychiatric Association 2023 Congress.
A leading mental illness risk factor
Study presenter Laura Fusar-Poli, MD, PhD, from the department of brain and behavioral sciences, University of Pavia (Italy), said that the differential impact of trauma subtypes in men and women indicate that both gender and the type of childhood adversity experienced need to be taken into account in future studies.
Dr. Fusar-Poli began by highlighting that 13%-36% of individuals have experienced some kind of childhood trauma, with 30% exposed to at least two types of trauma.
Trauma has been identified as a risk factor for a range of mental health problems.
“It is estimated that, worldwide, around one third of all psychiatric disorders are related to childhood trauma,” senior researcher Sinan Gül
Consequently, “childhood trauma is a leading preventable risk factor for mental illness,” he added.
Previous research suggests the subtype of trauma has an impact on subsequent biological changes and clinical outcomes, and that there are gender differences in the effects of childhood trauma.
To investigate, the researchers examined data from TwinssCan, a Belgian cohort of twins and siblings aged 15-35 years without a diagnosis of pervasive mental disorders.
The study included 477 females and 314 males who had completed the Childhood Trauma Questionnaire–Short Form (CTQ) and the Symptom Checklist-90 SR (SCL-90) to determine exposure to childhood adversity and levels of psychopathology, respectively.
Results showed that total CTQ scores were significantly associated with total SCL-90 scores in both men and women, as well as with each of the nine symptom domains of the SCL-90 (P < .001 for all assessments). These included psychoticism, paranoid ideation, anxiety, depression, somatization, obsessive-compulsive, interpersonal sensitivity, hostility, and phobic anxiety.
There were no significant differences in the associations with total CTQ scores between men and women.
However, when the researchers examined trauma subtypes and psychopathology, clear gender differences emerged.
Investigators found a significant association between emotional abuse on the CTQ and total SCL-90 scores in both men (P < .023) and women (P < .001), but that the association was significantly stronger in women (P = .043).
Sexual abuse was significantly associated with total SCL-90 scores in women (P < .001), while emotional neglect and physical neglect were significantly associated with psychopathology scores in men (P = .026 and P < .001, respectively).
“Physical neglect may include experiences of not having enough to eat, wearing dirty clothes, not being taken care of, and not getting taken to the doctor when the person was growing up,” said Dr. Prachason.
“Emotional neglect may include childhood experiences like not feeling loved or important, and not feeling close to the family.”
In women, emotional abuse was significantly associated with all nine symptom domains of the SCL-90, while sexual abuse was associated with seven: psychoticism, paranoid ideation, anxiety, depression, somatization, obsessive-compulsive, and hostility.
Physical neglect, in men, was significantly associated with eight of the symptom domains (all but somatization), but emotional neglect was linked only to depression, Dr. Fusar-Poli reported.
“This study showed a very important consequence of childhood trauma, and not only in people with mental disorders. I would like to underline that this is a general population, composed of adolescents and young adults, which is the age in which the majority of mental disorders starts, Dr. Fusar-Poli said in an interview.
She emphasized that psychotic disorders are only a part of the “broad range” of conditions that may be related to childhood trauma, which “can have an impact on sub-threshold symptoms that can affect functioning and quality of life in the general population.”
Addressing the differential findings in men and women, Dr. Gül
However, he said, this is “something that we really need understand,” as there is likely an underlying mechanism, “and not only a biological mechanism but probably a societal one.”
Dr. Gül
Compromised cognitive, emotional function
Commenting on the findings for this news organization, Elaine F. Walker, PhD, professor of psychology and neuroscience at Emory University in Atlanta, said stress exposure in general, including childhood trauma, “has transdiagnostic effects on vulnerability to mental disorders.”
“The effects are primarily mediated by the hypothalamic-pituitary-adrenal axis, which triggers the release of cortisol. When persistently elevated, this can result in neurobiological processes that have adverse effects on brain structure and circuitry which, in turn, compromises cognitive and emotional functioning,” said Dr. Walker, who was not associated with the study.
She noted that, “while it is possible that there are sex differences in biological sensitivity to certain subtypes of childhood trauma, it may also be the case that sex differences in the likelihood of exposure to trauma subtypes is actually the key factor.”
“At the present time, there are not specific treatment protocols aimed at addressing childhood trauma subtypes, but most experienced therapists will incorporate information about the individual’s trauma history in their treatment,” Dr. Walker added.
Also commenting on the research, Philip Gorwood, MD, PhD, head of the Clinique des Maladies Mentales et de l’Encéphale at Centre Hospitalier Sainte Anne in Paris, said the results are “important … as childhood trauma has been clearly recognized as a major risk factor for the vast majority of psychiatric disorders, but with poor knowledge of gender specificities.”
“Understanding which aspects of trauma are more damaging according to gender will facilitate research on the resilience process. Many intervention strategies will indeed benefit from a more personalized approach,” he said in a statement. Dr. Gorwood was not involved with this study.
The study authors, Dr. Gorwood, and Dr. Walker report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT EPA 2023
‘Excess’ deaths surging, but why?
This transcript has been edited for clarity.
“Excess deaths.” You’ve heard the phrase countless times by now. It is one of the myriad of previously esoteric epidemiology terms that the pandemic brought squarely into the zeitgeist.
As a sort of standard candle of the performance of a state or a region or a country in terms of health care, it has a lot of utility – if for nothing more than Monday-morning quarterbacking. But this week, I want to dig in on the concept a bit because, according to a new study, the excess death gap between the United States and Western Europe has never been higher.
You might imagine that the best way to figure this out is for some group of intelligent people to review each death and decide, somehow, whether it was expected or not. But aside from being impractical, this would end up being somewhat subjective. That older person who died from pneumonia – was that an expected death? Could it have been avoided?
Rather, the calculation of excess mortality relies on large numbers and statistical inference to compare an expected number of deaths with those that are observed.
The difference is excess mortality, even if you can never be sure whether any particular death was expected or not.
As always, however, the devil is in the details. What data do you use to define the expected number of deaths?
There are options here. Probably the most straightforward analysis uses past data from the country of interest. You look at annual deaths over some historical period of time and compare those numbers with the rates today. Two issues need to be accounted for here: population growth – a larger population will have more deaths, so you need to adjust the historical population with current levels, and demographic shifts – an older or more male population will have more deaths, so you need to adjust for that as well.
But provided you take care of those factors, you can estimate fairly well how many deaths you can expect to see in any given period of time.
Still, you should see right away that excess mortality is a relative concept. If you think that, just perhaps, the United States has some systematic failure to deliver care that has been stable and persistent over time, you wouldn’t capture that failing in an excess mortality calculation that uses U.S. historical data as the baseline.
The best way to get around that is to use data from other countries, and that’s just what this article – a rare single-author piece by Patrick Heuveline – does, calculating excess deaths in the United States by standardizing our mortality rates to the five largest Western European countries: the United Kingdom, France, Germany, Italy, and Spain.
Controlling for the differences in the demographics of that European population, here is the expected number of deaths in the United States over the past 5 years.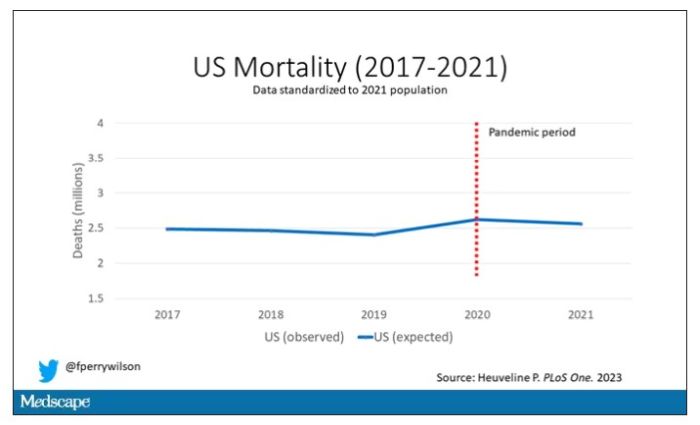
Note that there is a small uptick in expected deaths in 2020, reflecting the pandemic, which returns to baseline levels by 2021. This is because that’s what happened in Europe; by 2021, the excess mortality due to COVID-19 was quite low.
Here are the actual deaths in the US during that time.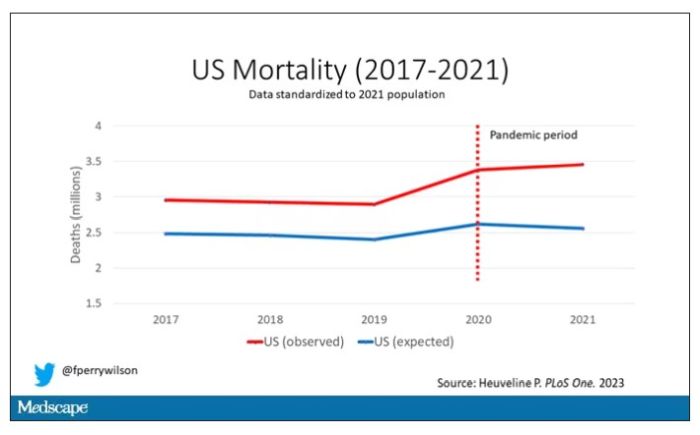
Highlighted here in green, then, is the excess mortality over time in the United States.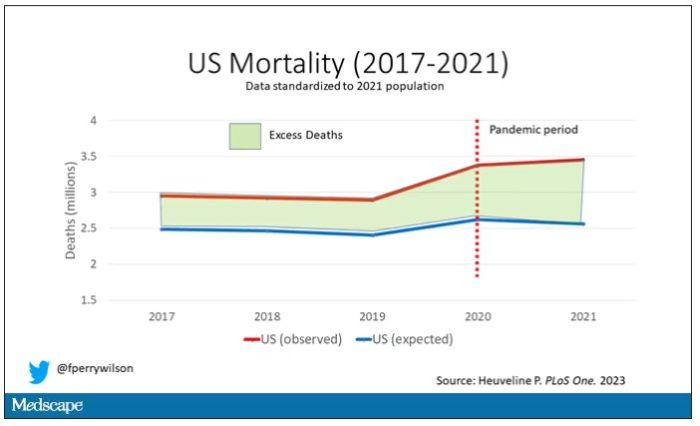
There are some fascinating and concerning findings here.
First of all, you can see that even before the pandemic, the United States has an excess mortality problem. This is not entirely a surprise; we’ve known that so-called “deaths of despair,” those due to alcohol abuse, drug overdoses, and suicide, are at an all-time high and tend to affect a “prime of life” population that would not otherwise be expected to die. In fact, fully 50% of the excess deaths in the United States occur in those between ages 15 and 64.
Excess deaths are also a concerning percentage of total deaths. In 2017, 17% of total deaths in the United States could be considered “excess.” In 2021, that number had doubled to 35%. Nearly 900,000 individuals in the United States died in 2021 who perhaps didn’t need to.
The obvious culprit to blame here is COVID, but COVID-associated excess deaths only explain about 50% of the excess we see in 2021. The rest reflect something even more concerning: a worsening of the failures of the past, perhaps exacerbated by the pandemic but not due to the virus itself.
Of course, we started this discussion acknowledging that the calculation of excess mortality is exquisitely dependent on how you model the expected number of deaths, and I’m sure some will take issue with the use of European numbers when applied to Americans. After all, Europe has, by and large, a robust public health service, socialized medicine, and healthcare that does not run the risk of bankrupting its citizens. How can we compare our outcomes to a place like that?
How indeed.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven,Conn. He reported no relevant conflicts of interest.
A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
“Excess deaths.” You’ve heard the phrase countless times by now. It is one of the myriad of previously esoteric epidemiology terms that the pandemic brought squarely into the zeitgeist.
As a sort of standard candle of the performance of a state or a region or a country in terms of health care, it has a lot of utility – if for nothing more than Monday-morning quarterbacking. But this week, I want to dig in on the concept a bit because, according to a new study, the excess death gap between the United States and Western Europe has never been higher.
You might imagine that the best way to figure this out is for some group of intelligent people to review each death and decide, somehow, whether it was expected or not. But aside from being impractical, this would end up being somewhat subjective. That older person who died from pneumonia – was that an expected death? Could it have been avoided?
Rather, the calculation of excess mortality relies on large numbers and statistical inference to compare an expected number of deaths with those that are observed.
The difference is excess mortality, even if you can never be sure whether any particular death was expected or not.
As always, however, the devil is in the details. What data do you use to define the expected number of deaths?
There are options here. Probably the most straightforward analysis uses past data from the country of interest. You look at annual deaths over some historical period of time and compare those numbers with the rates today. Two issues need to be accounted for here: population growth – a larger population will have more deaths, so you need to adjust the historical population with current levels, and demographic shifts – an older or more male population will have more deaths, so you need to adjust for that as well.
But provided you take care of those factors, you can estimate fairly well how many deaths you can expect to see in any given period of time.
Still, you should see right away that excess mortality is a relative concept. If you think that, just perhaps, the United States has some systematic failure to deliver care that has been stable and persistent over time, you wouldn’t capture that failing in an excess mortality calculation that uses U.S. historical data as the baseline.
The best way to get around that is to use data from other countries, and that’s just what this article – a rare single-author piece by Patrick Heuveline – does, calculating excess deaths in the United States by standardizing our mortality rates to the five largest Western European countries: the United Kingdom, France, Germany, Italy, and Spain.
Controlling for the differences in the demographics of that European population, here is the expected number of deaths in the United States over the past 5 years.
Note that there is a small uptick in expected deaths in 2020, reflecting the pandemic, which returns to baseline levels by 2021. This is because that’s what happened in Europe; by 2021, the excess mortality due to COVID-19 was quite low.
Here are the actual deaths in the US during that time.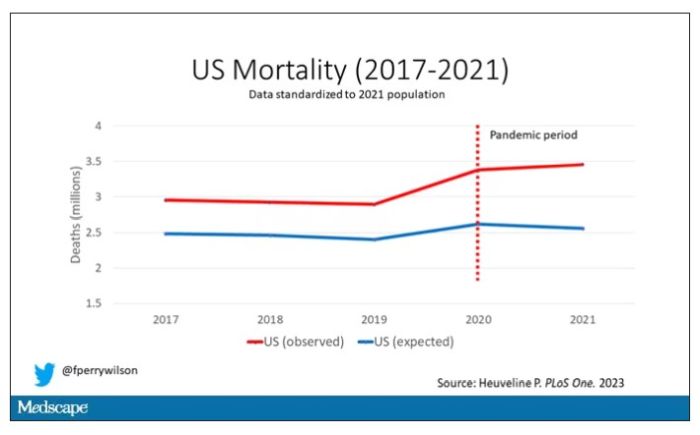
Highlighted here in green, then, is the excess mortality over time in the United States.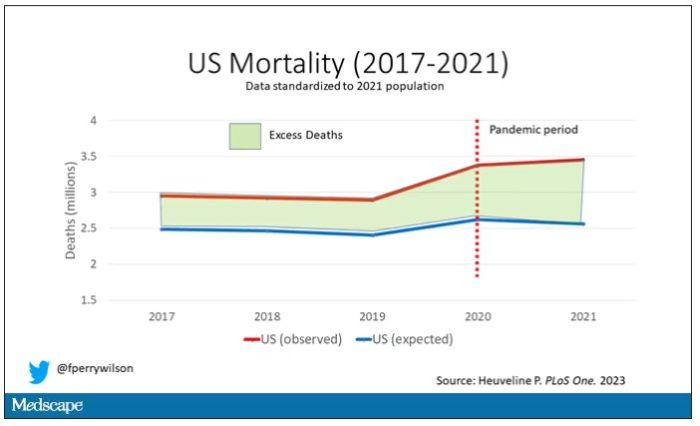
There are some fascinating and concerning findings here.
First of all, you can see that even before the pandemic, the United States has an excess mortality problem. This is not entirely a surprise; we’ve known that so-called “deaths of despair,” those due to alcohol abuse, drug overdoses, and suicide, are at an all-time high and tend to affect a “prime of life” population that would not otherwise be expected to die. In fact, fully 50% of the excess deaths in the United States occur in those between ages 15 and 64.
Excess deaths are also a concerning percentage of total deaths. In 2017, 17% of total deaths in the United States could be considered “excess.” In 2021, that number had doubled to 35%. Nearly 900,000 individuals in the United States died in 2021 who perhaps didn’t need to.
The obvious culprit to blame here is COVID, but COVID-associated excess deaths only explain about 50% of the excess we see in 2021. The rest reflect something even more concerning: a worsening of the failures of the past, perhaps exacerbated by the pandemic but not due to the virus itself.
Of course, we started this discussion acknowledging that the calculation of excess mortality is exquisitely dependent on how you model the expected number of deaths, and I’m sure some will take issue with the use of European numbers when applied to Americans. After all, Europe has, by and large, a robust public health service, socialized medicine, and healthcare that does not run the risk of bankrupting its citizens. How can we compare our outcomes to a place like that?
How indeed.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven,Conn. He reported no relevant conflicts of interest.
A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
“Excess deaths.” You’ve heard the phrase countless times by now. It is one of the myriad of previously esoteric epidemiology terms that the pandemic brought squarely into the zeitgeist.
As a sort of standard candle of the performance of a state or a region or a country in terms of health care, it has a lot of utility – if for nothing more than Monday-morning quarterbacking. But this week, I want to dig in on the concept a bit because, according to a new study, the excess death gap between the United States and Western Europe has never been higher.
You might imagine that the best way to figure this out is for some group of intelligent people to review each death and decide, somehow, whether it was expected or not. But aside from being impractical, this would end up being somewhat subjective. That older person who died from pneumonia – was that an expected death? Could it have been avoided?
Rather, the calculation of excess mortality relies on large numbers and statistical inference to compare an expected number of deaths with those that are observed.
The difference is excess mortality, even if you can never be sure whether any particular death was expected or not.
As always, however, the devil is in the details. What data do you use to define the expected number of deaths?
There are options here. Probably the most straightforward analysis uses past data from the country of interest. You look at annual deaths over some historical period of time and compare those numbers with the rates today. Two issues need to be accounted for here: population growth – a larger population will have more deaths, so you need to adjust the historical population with current levels, and demographic shifts – an older or more male population will have more deaths, so you need to adjust for that as well.
But provided you take care of those factors, you can estimate fairly well how many deaths you can expect to see in any given period of time.
Still, you should see right away that excess mortality is a relative concept. If you think that, just perhaps, the United States has some systematic failure to deliver care that has been stable and persistent over time, you wouldn’t capture that failing in an excess mortality calculation that uses U.S. historical data as the baseline.
The best way to get around that is to use data from other countries, and that’s just what this article – a rare single-author piece by Patrick Heuveline – does, calculating excess deaths in the United States by standardizing our mortality rates to the five largest Western European countries: the United Kingdom, France, Germany, Italy, and Spain.
Controlling for the differences in the demographics of that European population, here is the expected number of deaths in the United States over the past 5 years.
Note that there is a small uptick in expected deaths in 2020, reflecting the pandemic, which returns to baseline levels by 2021. This is because that’s what happened in Europe; by 2021, the excess mortality due to COVID-19 was quite low.
Here are the actual deaths in the US during that time.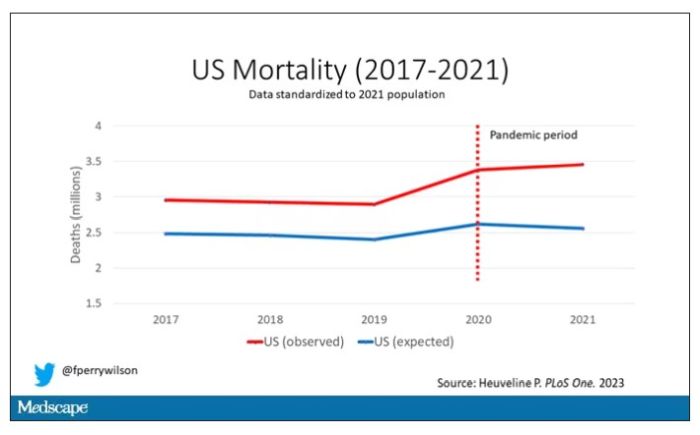
Highlighted here in green, then, is the excess mortality over time in the United States.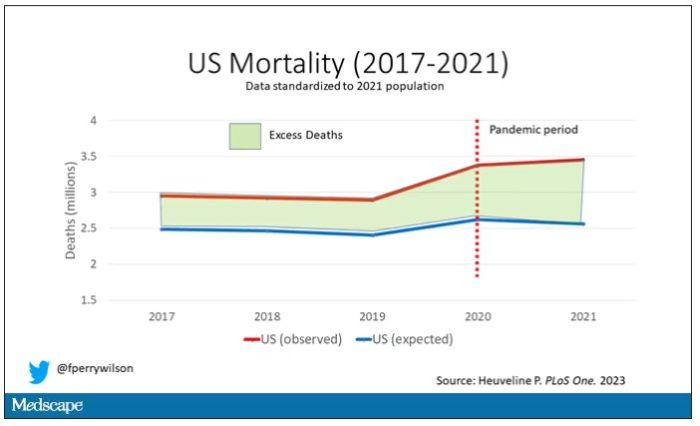
There are some fascinating and concerning findings here.
First of all, you can see that even before the pandemic, the United States has an excess mortality problem. This is not entirely a surprise; we’ve known that so-called “deaths of despair,” those due to alcohol abuse, drug overdoses, and suicide, are at an all-time high and tend to affect a “prime of life” population that would not otherwise be expected to die. In fact, fully 50% of the excess deaths in the United States occur in those between ages 15 and 64.
Excess deaths are also a concerning percentage of total deaths. In 2017, 17% of total deaths in the United States could be considered “excess.” In 2021, that number had doubled to 35%. Nearly 900,000 individuals in the United States died in 2021 who perhaps didn’t need to.
The obvious culprit to blame here is COVID, but COVID-associated excess deaths only explain about 50% of the excess we see in 2021. The rest reflect something even more concerning: a worsening of the failures of the past, perhaps exacerbated by the pandemic but not due to the virus itself.
Of course, we started this discussion acknowledging that the calculation of excess mortality is exquisitely dependent on how you model the expected number of deaths, and I’m sure some will take issue with the use of European numbers when applied to Americans. After all, Europe has, by and large, a robust public health service, socialized medicine, and healthcare that does not run the risk of bankrupting its citizens. How can we compare our outcomes to a place like that?
How indeed.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven,Conn. He reported no relevant conflicts of interest.
A version of this article originally appeared on Medscape.com.
A new way to gauge suicide risk?
Researchers found SDOH are risk factors for suicide among U.S. veterans and NLP can be leveraged to extract SDOH information from unstructured data in the EHR.
“Since SDOH is overwhelmingly described in EHR notes, the importance of NLP-extracted SDOH can be very significant, meaning that NLP can be used as an effective method for epidemiological and public health study,” senior investigator Hong Yu, PhD, from Miner School of Information and Computer Sciences, University of Massachusetts Lowell, told this news organization.
Although the study was conducted among U.S. veterans, the results likely hold for the general population as well.
“The NLP methods are generalizable. The SDOH categories are generalizable. There may be some variations in terms of the strength of associations in NLP-extracted SDOH and suicide death, but the overall findings are generalizable,” Dr. Yu said.
The study was published online JAMA Network Open.
Improved risk assessment
SDOH, which include factors such as socioeconomic status, access to healthy food, education, housing, and physical environment, are strong predictors of suicidal behaviors.
Several studies have identified a range of common risk factors for suicide using International Classification of Diseases (ICD) codes and other “structured” data from the EHR. However, the use of unstructured EHR data from clinician notes has received little attention in investigating potential associations between suicide and SDOH.
Using the large Veterans Health Administration EHR system, the researchers determined associations between veterans’ death by suicide and recent SDOH, identified using both structured data (ICD-10 codes and Veterans Health Administration stop codes) and unstructured data (NLP-processed clinical notes).
Participants included 8,821 veterans who committed suicide and 35,284 matched controls. The cohort was mostly male (96%) and White (79%). The mean age was 58 years.
The NLP-extracted SDOH were social isolation, job or financial insecurity, housing instability, legal problems, violence, barriers to care, transition of care, and food insecurity.
All of these unstructured clinical notes on SDOH were significantly associated with increased risk for death by suicide.
Legal problems had the largest estimated effect size, more than twice the risk of those with no exposure (adjusted odds ratio 2.62; 95% confidence interval, 2.38-2.89), followed by violence (aOR, 2.34; 95% CI, 2.17-2.52) and social isolation (aOR, 1.94; 95% CI, 1.83-2.06).
Similarly, all of the structured SDOH – social or family problems, employment or financial problems, housing instability, legal problems, violence, and nonspecific psychosocial needs – also showed significant associations with increased risk for suicide death, once again, with legal problems linked to the highest risk (aOR, 2.63; 95% CI, 2.37-2.91).
When combining the structured and NLP-extracted unstructured data, the top three risk factors for death by suicide were legal problems (aOR, 2.66; 95% CI 2.46-2.89), violence (aOR, 2.12; 95% CI, 1.98-2.27), and nonspecific psychosocial needs (aOR, 2.07; 95% CI, 1.92-2.23).
“To our knowledge, this the first large-scale study to implement and use an NLP system to extract SDOH information from unstructured EHR data,” the researchers write.
“We strongly believe that analyzing all available SDOH information, including those contained in clinical notes, can help develop a better system for risk assessment and suicide prevention. However, more studies are required to investigate ways of seamlessly incorporating SDOHs into existing health care systems,” they conclude.
Dr. Yu said it’s also important to note that their NLP system is built upon “the most advanced deep-learning technologies and therefore is more generalizable than most existing work that mainly used rule-based approaches or traditional machine learning for identifying social determinants of health.”
In an accompanying editorial, Ishanu Chattopadhyay, PhD, of the University of Chicago, said this suggests that unstructured clinical notes “may efficiently identify at-risk individuals even when structured data on the relevant variables are missing or incomplete.”
This work may provide “the foundation for addressing the key hurdles in enacting efficient universal assessment for suicide risk among the veterans and perhaps in the general population,” Dr. Chattopadhyay added.
This research was funded by a grant from the National Institute of Mental Health. The study authors and editorialist report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Researchers found SDOH are risk factors for suicide among U.S. veterans and NLP can be leveraged to extract SDOH information from unstructured data in the EHR.
“Since SDOH is overwhelmingly described in EHR notes, the importance of NLP-extracted SDOH can be very significant, meaning that NLP can be used as an effective method for epidemiological and public health study,” senior investigator Hong Yu, PhD, from Miner School of Information and Computer Sciences, University of Massachusetts Lowell, told this news organization.
Although the study was conducted among U.S. veterans, the results likely hold for the general population as well.
“The NLP methods are generalizable. The SDOH categories are generalizable. There may be some variations in terms of the strength of associations in NLP-extracted SDOH and suicide death, but the overall findings are generalizable,” Dr. Yu said.
The study was published online JAMA Network Open.
Improved risk assessment
SDOH, which include factors such as socioeconomic status, access to healthy food, education, housing, and physical environment, are strong predictors of suicidal behaviors.
Several studies have identified a range of common risk factors for suicide using International Classification of Diseases (ICD) codes and other “structured” data from the EHR. However, the use of unstructured EHR data from clinician notes has received little attention in investigating potential associations between suicide and SDOH.
Using the large Veterans Health Administration EHR system, the researchers determined associations between veterans’ death by suicide and recent SDOH, identified using both structured data (ICD-10 codes and Veterans Health Administration stop codes) and unstructured data (NLP-processed clinical notes).
Participants included 8,821 veterans who committed suicide and 35,284 matched controls. The cohort was mostly male (96%) and White (79%). The mean age was 58 years.
The NLP-extracted SDOH were social isolation, job or financial insecurity, housing instability, legal problems, violence, barriers to care, transition of care, and food insecurity.
All of these unstructured clinical notes on SDOH were significantly associated with increased risk for death by suicide.
Legal problems had the largest estimated effect size, more than twice the risk of those with no exposure (adjusted odds ratio 2.62; 95% confidence interval, 2.38-2.89), followed by violence (aOR, 2.34; 95% CI, 2.17-2.52) and social isolation (aOR, 1.94; 95% CI, 1.83-2.06).
Similarly, all of the structured SDOH – social or family problems, employment or financial problems, housing instability, legal problems, violence, and nonspecific psychosocial needs – also showed significant associations with increased risk for suicide death, once again, with legal problems linked to the highest risk (aOR, 2.63; 95% CI, 2.37-2.91).
When combining the structured and NLP-extracted unstructured data, the top three risk factors for death by suicide were legal problems (aOR, 2.66; 95% CI 2.46-2.89), violence (aOR, 2.12; 95% CI, 1.98-2.27), and nonspecific psychosocial needs (aOR, 2.07; 95% CI, 1.92-2.23).
“To our knowledge, this the first large-scale study to implement and use an NLP system to extract SDOH information from unstructured EHR data,” the researchers write.
“We strongly believe that analyzing all available SDOH information, including those contained in clinical notes, can help develop a better system for risk assessment and suicide prevention. However, more studies are required to investigate ways of seamlessly incorporating SDOHs into existing health care systems,” they conclude.
Dr. Yu said it’s also important to note that their NLP system is built upon “the most advanced deep-learning technologies and therefore is more generalizable than most existing work that mainly used rule-based approaches or traditional machine learning for identifying social determinants of health.”
In an accompanying editorial, Ishanu Chattopadhyay, PhD, of the University of Chicago, said this suggests that unstructured clinical notes “may efficiently identify at-risk individuals even when structured data on the relevant variables are missing or incomplete.”
This work may provide “the foundation for addressing the key hurdles in enacting efficient universal assessment for suicide risk among the veterans and perhaps in the general population,” Dr. Chattopadhyay added.
This research was funded by a grant from the National Institute of Mental Health. The study authors and editorialist report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Researchers found SDOH are risk factors for suicide among U.S. veterans and NLP can be leveraged to extract SDOH information from unstructured data in the EHR.
“Since SDOH is overwhelmingly described in EHR notes, the importance of NLP-extracted SDOH can be very significant, meaning that NLP can be used as an effective method for epidemiological and public health study,” senior investigator Hong Yu, PhD, from Miner School of Information and Computer Sciences, University of Massachusetts Lowell, told this news organization.
Although the study was conducted among U.S. veterans, the results likely hold for the general population as well.
“The NLP methods are generalizable. The SDOH categories are generalizable. There may be some variations in terms of the strength of associations in NLP-extracted SDOH and suicide death, but the overall findings are generalizable,” Dr. Yu said.
The study was published online JAMA Network Open.
Improved risk assessment
SDOH, which include factors such as socioeconomic status, access to healthy food, education, housing, and physical environment, are strong predictors of suicidal behaviors.
Several studies have identified a range of common risk factors for suicide using International Classification of Diseases (ICD) codes and other “structured” data from the EHR. However, the use of unstructured EHR data from clinician notes has received little attention in investigating potential associations between suicide and SDOH.
Using the large Veterans Health Administration EHR system, the researchers determined associations between veterans’ death by suicide and recent SDOH, identified using both structured data (ICD-10 codes and Veterans Health Administration stop codes) and unstructured data (NLP-processed clinical notes).
Participants included 8,821 veterans who committed suicide and 35,284 matched controls. The cohort was mostly male (96%) and White (79%). The mean age was 58 years.
The NLP-extracted SDOH were social isolation, job or financial insecurity, housing instability, legal problems, violence, barriers to care, transition of care, and food insecurity.
All of these unstructured clinical notes on SDOH were significantly associated with increased risk for death by suicide.
Legal problems had the largest estimated effect size, more than twice the risk of those with no exposure (adjusted odds ratio 2.62; 95% confidence interval, 2.38-2.89), followed by violence (aOR, 2.34; 95% CI, 2.17-2.52) and social isolation (aOR, 1.94; 95% CI, 1.83-2.06).
Similarly, all of the structured SDOH – social or family problems, employment or financial problems, housing instability, legal problems, violence, and nonspecific psychosocial needs – also showed significant associations with increased risk for suicide death, once again, with legal problems linked to the highest risk (aOR, 2.63; 95% CI, 2.37-2.91).
When combining the structured and NLP-extracted unstructured data, the top three risk factors for death by suicide were legal problems (aOR, 2.66; 95% CI 2.46-2.89), violence (aOR, 2.12; 95% CI, 1.98-2.27), and nonspecific psychosocial needs (aOR, 2.07; 95% CI, 1.92-2.23).
“To our knowledge, this the first large-scale study to implement and use an NLP system to extract SDOH information from unstructured EHR data,” the researchers write.
“We strongly believe that analyzing all available SDOH information, including those contained in clinical notes, can help develop a better system for risk assessment and suicide prevention. However, more studies are required to investigate ways of seamlessly incorporating SDOHs into existing health care systems,” they conclude.
Dr. Yu said it’s also important to note that their NLP system is built upon “the most advanced deep-learning technologies and therefore is more generalizable than most existing work that mainly used rule-based approaches or traditional machine learning for identifying social determinants of health.”
In an accompanying editorial, Ishanu Chattopadhyay, PhD, of the University of Chicago, said this suggests that unstructured clinical notes “may efficiently identify at-risk individuals even when structured data on the relevant variables are missing or incomplete.”
This work may provide “the foundation for addressing the key hurdles in enacting efficient universal assessment for suicide risk among the veterans and perhaps in the general population,” Dr. Chattopadhyay added.
This research was funded by a grant from the National Institute of Mental Health. The study authors and editorialist report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Telehealth services tied to a major reduction in opioid overdose deaths
, a new study of Medicare beneficiaries shows.
Telehealth services for opioid use disorder (OUD) were used far more often during the pandemic than before COVID-19, and those who used them were 33% less likely to die of a drug overdose.
Investigators also found a significant increase in MOUD use during the pandemic. Fatal drug overdoses were 59% less likely among individuals who received MOUD from an opioid treatment program and 38% less likely among those treated with buprenorphine in an office-based setting.
The results come as policymakers are preparing for the end of the public health emergency that prompted the expansion of OUD-related telehealth and MOUD prescribing and are deciding whether to make those expansions permanent.
“The expansion of telehealth during the COVID-19 pandemic appears to have had positive effects on patients receiving MOUD, improved retention among patients who received MOUD, and lowered risks for both nonfatal and fatal overdose,” lead investigator Christopher M. Jones, PharmD, DrPH, director of the National Center for Injury Prevention and Control at the Centers for Disease Control and Prevention, Atlanta, Georgia, told this news organization. “Our results suggest that telehealth is a valuable tool in the toolbox for expanding access to and improving retention on MOUD.”
The findings were published online in JAMA Psychiatry.
Increase in treatment
The study included 105,162 Medicare beneficiaries who began OUD treatment between March and August in 2019 (prepandemic cohort; 67.6%
aged 45-74 years), and 70,479 who began treatment between March and August of 2020 (pandemic cohort; 66.3% aged 45-74 years).
Participants had not received OUD treatment in the 6 months leading up to study enrollment and were followed for 6 months after treatment began.
Significantly more study participants received OUD-related telehealth services during the pandemic than prior to 2019 (19.6% vs. 0.6%; P < .001). Receipt of MOUD was also significantly higher in the pandemic cohort (12.6% vs. 10.8%; P < .001).
The rate of drug overdose deaths was higher in the pandemic cohort (5.1 deaths vs. 3.7 deaths per 1,000 beneficiaries; P < .001). But the percentage of deaths from drug overdoses did not differ between groups (4.8% in the prepandemic cohort vs. 5.1% in the pandemic cohort; P = .49).
In the pandemic cohort, fatal drug overdoses were 33% less likely among those who received OUD-related telehealth services (adjusted odds ratio, 0.67; 95% confidence interval, 0.48-0.92); 59% less likely among those who received MOUD from opioid treatment programs (aOR, 0.41; 95% CI, 0.25-0.68), and 38% less likely among those who received buprenorphine in office-based settings (aOR, 0.62; 95% CI, 0.43-0.91).
Risk of fatal overdose was significantly lower among women and those aged 65 years and older. There were no significant differences in risk based on urban or rural residency or on ethnicity.
“Against the backdrop of a highly potent illicit drug supply driven by illicit fentanyl and fentanyl analogues and historically large increases in overdose deaths during the COVID-19 pandemic, MOUD was still highly effective at reducing risk for fatal overdose,” Dr. Jones said.
While the use of buprenorphine in office-based settings was associated with a decreased risk of overdose death, use of extended-release naltrexone was not.
“Prior research has demonstrated the effectiveness of extended-release naltrexone in the treatment of opioid use disorder,” Dr. Jones said. “However, research has also shown that patients have challenges getting started, or inducted, on extended-release naltrexone.”
An earlier study by Dr. Jones and colleagues showed that rates of retention were lower with extended-release naltrexone, compared with buprenorphine in office-based settings or MOUD from opioid treatment programs.
The new study included only a small number of individuals who were receiving extended-release naltrexone, which may have influenced the findings. In addition, challenges with induction and retention may be driving the results, Dr. Jones noted.
“Efforts to improve induction and retention with extended-release naltrexone are important areas for future research and clinical practice,” he added.
An important engagement tool
A number of questions about telehealth care for OUD remain, including whether increased access to care accounts for the reduction in drug overdose risk that the investigators found or whether other factors are at play.
“There is still more we need to understand about telehealth, such as the quality of care provided and the particular aspects of care provided by telehealth and how this influences health outcomes,” Dr. Jones said.
The results also suggest treatments for OUD are still not finding their way to patients who might benefit, he added.
“Despite the positive findings and the prior research showing that MOUD is highly effective, we found that only one in five patients received telehealth services and only one in eight received any MOUD. This really underscores the need to expand these services across clinical settings,” he added.
These and earlier findings demonstrate the potential benefits of continuing pandemic-era expansion of OUD-related telehealth services and MOUD access, Dr. Jones said.
In preparation for the end of the public health emergency on May 1, the Drug Enforcement Agency recently released a proposal that would allow providers to prescribe a 30-day supply of buprenorphine, but for patients to receive additional prescriptions, a face-to-face meeting would be required. The proposal has drawn criticism from addiction medicine specialists.
The current study didn’t explore if or how the proposal might affect patients with OUD or whether it could blunt the positive effects of the findings.
“Prior research shows that keeping individuals engaged in treatment, including on medications, is a critical part of reducing the negative health and social impacts of opioid use disorder. Our results suggest that telehealth can be an important tool in helping patients engage in and stay connected in care,” said Dr. Jones.
The study was funded by the Centers for Disease Control and Prevention, the Centers for Medicare & Medicaid Services, and the National Institutes of Health. Dr. Johnson reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
, a new study of Medicare beneficiaries shows.
Telehealth services for opioid use disorder (OUD) were used far more often during the pandemic than before COVID-19, and those who used them were 33% less likely to die of a drug overdose.
Investigators also found a significant increase in MOUD use during the pandemic. Fatal drug overdoses were 59% less likely among individuals who received MOUD from an opioid treatment program and 38% less likely among those treated with buprenorphine in an office-based setting.
The results come as policymakers are preparing for the end of the public health emergency that prompted the expansion of OUD-related telehealth and MOUD prescribing and are deciding whether to make those expansions permanent.
“The expansion of telehealth during the COVID-19 pandemic appears to have had positive effects on patients receiving MOUD, improved retention among patients who received MOUD, and lowered risks for both nonfatal and fatal overdose,” lead investigator Christopher M. Jones, PharmD, DrPH, director of the National Center for Injury Prevention and Control at the Centers for Disease Control and Prevention, Atlanta, Georgia, told this news organization. “Our results suggest that telehealth is a valuable tool in the toolbox for expanding access to and improving retention on MOUD.”
The findings were published online in JAMA Psychiatry.
Increase in treatment
The study included 105,162 Medicare beneficiaries who began OUD treatment between March and August in 2019 (prepandemic cohort; 67.6%
aged 45-74 years), and 70,479 who began treatment between March and August of 2020 (pandemic cohort; 66.3% aged 45-74 years).
Participants had not received OUD treatment in the 6 months leading up to study enrollment and were followed for 6 months after treatment began.
Significantly more study participants received OUD-related telehealth services during the pandemic than prior to 2019 (19.6% vs. 0.6%; P < .001). Receipt of MOUD was also significantly higher in the pandemic cohort (12.6% vs. 10.8%; P < .001).
The rate of drug overdose deaths was higher in the pandemic cohort (5.1 deaths vs. 3.7 deaths per 1,000 beneficiaries; P < .001). But the percentage of deaths from drug overdoses did not differ between groups (4.8% in the prepandemic cohort vs. 5.1% in the pandemic cohort; P = .49).
In the pandemic cohort, fatal drug overdoses were 33% less likely among those who received OUD-related telehealth services (adjusted odds ratio, 0.67; 95% confidence interval, 0.48-0.92); 59% less likely among those who received MOUD from opioid treatment programs (aOR, 0.41; 95% CI, 0.25-0.68), and 38% less likely among those who received buprenorphine in office-based settings (aOR, 0.62; 95% CI, 0.43-0.91).
Risk of fatal overdose was significantly lower among women and those aged 65 years and older. There were no significant differences in risk based on urban or rural residency or on ethnicity.
“Against the backdrop of a highly potent illicit drug supply driven by illicit fentanyl and fentanyl analogues and historically large increases in overdose deaths during the COVID-19 pandemic, MOUD was still highly effective at reducing risk for fatal overdose,” Dr. Jones said.
While the use of buprenorphine in office-based settings was associated with a decreased risk of overdose death, use of extended-release naltrexone was not.
“Prior research has demonstrated the effectiveness of extended-release naltrexone in the treatment of opioid use disorder,” Dr. Jones said. “However, research has also shown that patients have challenges getting started, or inducted, on extended-release naltrexone.”
An earlier study by Dr. Jones and colleagues showed that rates of retention were lower with extended-release naltrexone, compared with buprenorphine in office-based settings or MOUD from opioid treatment programs.
The new study included only a small number of individuals who were receiving extended-release naltrexone, which may have influenced the findings. In addition, challenges with induction and retention may be driving the results, Dr. Jones noted.
“Efforts to improve induction and retention with extended-release naltrexone are important areas for future research and clinical practice,” he added.
An important engagement tool
A number of questions about telehealth care for OUD remain, including whether increased access to care accounts for the reduction in drug overdose risk that the investigators found or whether other factors are at play.
“There is still more we need to understand about telehealth, such as the quality of care provided and the particular aspects of care provided by telehealth and how this influences health outcomes,” Dr. Jones said.
The results also suggest treatments for OUD are still not finding their way to patients who might benefit, he added.
“Despite the positive findings and the prior research showing that MOUD is highly effective, we found that only one in five patients received telehealth services and only one in eight received any MOUD. This really underscores the need to expand these services across clinical settings,” he added.
These and earlier findings demonstrate the potential benefits of continuing pandemic-era expansion of OUD-related telehealth services and MOUD access, Dr. Jones said.
In preparation for the end of the public health emergency on May 1, the Drug Enforcement Agency recently released a proposal that would allow providers to prescribe a 30-day supply of buprenorphine, but for patients to receive additional prescriptions, a face-to-face meeting would be required. The proposal has drawn criticism from addiction medicine specialists.
The current study didn’t explore if or how the proposal might affect patients with OUD or whether it could blunt the positive effects of the findings.
“Prior research shows that keeping individuals engaged in treatment, including on medications, is a critical part of reducing the negative health and social impacts of opioid use disorder. Our results suggest that telehealth can be an important tool in helping patients engage in and stay connected in care,” said Dr. Jones.
The study was funded by the Centers for Disease Control and Prevention, the Centers for Medicare & Medicaid Services, and the National Institutes of Health. Dr. Johnson reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
, a new study of Medicare beneficiaries shows.
Telehealth services for opioid use disorder (OUD) were used far more often during the pandemic than before COVID-19, and those who used them were 33% less likely to die of a drug overdose.
Investigators also found a significant increase in MOUD use during the pandemic. Fatal drug overdoses were 59% less likely among individuals who received MOUD from an opioid treatment program and 38% less likely among those treated with buprenorphine in an office-based setting.
The results come as policymakers are preparing for the end of the public health emergency that prompted the expansion of OUD-related telehealth and MOUD prescribing and are deciding whether to make those expansions permanent.
“The expansion of telehealth during the COVID-19 pandemic appears to have had positive effects on patients receiving MOUD, improved retention among patients who received MOUD, and lowered risks for both nonfatal and fatal overdose,” lead investigator Christopher M. Jones, PharmD, DrPH, director of the National Center for Injury Prevention and Control at the Centers for Disease Control and Prevention, Atlanta, Georgia, told this news organization. “Our results suggest that telehealth is a valuable tool in the toolbox for expanding access to and improving retention on MOUD.”
The findings were published online in JAMA Psychiatry.
Increase in treatment
The study included 105,162 Medicare beneficiaries who began OUD treatment between March and August in 2019 (prepandemic cohort; 67.6%
aged 45-74 years), and 70,479 who began treatment between March and August of 2020 (pandemic cohort; 66.3% aged 45-74 years).
Participants had not received OUD treatment in the 6 months leading up to study enrollment and were followed for 6 months after treatment began.
Significantly more study participants received OUD-related telehealth services during the pandemic than prior to 2019 (19.6% vs. 0.6%; P < .001). Receipt of MOUD was also significantly higher in the pandemic cohort (12.6% vs. 10.8%; P < .001).
The rate of drug overdose deaths was higher in the pandemic cohort (5.1 deaths vs. 3.7 deaths per 1,000 beneficiaries; P < .001). But the percentage of deaths from drug overdoses did not differ between groups (4.8% in the prepandemic cohort vs. 5.1% in the pandemic cohort; P = .49).
In the pandemic cohort, fatal drug overdoses were 33% less likely among those who received OUD-related telehealth services (adjusted odds ratio, 0.67; 95% confidence interval, 0.48-0.92); 59% less likely among those who received MOUD from opioid treatment programs (aOR, 0.41; 95% CI, 0.25-0.68), and 38% less likely among those who received buprenorphine in office-based settings (aOR, 0.62; 95% CI, 0.43-0.91).
Risk of fatal overdose was significantly lower among women and those aged 65 years and older. There were no significant differences in risk based on urban or rural residency or on ethnicity.
“Against the backdrop of a highly potent illicit drug supply driven by illicit fentanyl and fentanyl analogues and historically large increases in overdose deaths during the COVID-19 pandemic, MOUD was still highly effective at reducing risk for fatal overdose,” Dr. Jones said.
While the use of buprenorphine in office-based settings was associated with a decreased risk of overdose death, use of extended-release naltrexone was not.
“Prior research has demonstrated the effectiveness of extended-release naltrexone in the treatment of opioid use disorder,” Dr. Jones said. “However, research has also shown that patients have challenges getting started, or inducted, on extended-release naltrexone.”
An earlier study by Dr. Jones and colleagues showed that rates of retention were lower with extended-release naltrexone, compared with buprenorphine in office-based settings or MOUD from opioid treatment programs.
The new study included only a small number of individuals who were receiving extended-release naltrexone, which may have influenced the findings. In addition, challenges with induction and retention may be driving the results, Dr. Jones noted.
“Efforts to improve induction and retention with extended-release naltrexone are important areas for future research and clinical practice,” he added.
An important engagement tool
A number of questions about telehealth care for OUD remain, including whether increased access to care accounts for the reduction in drug overdose risk that the investigators found or whether other factors are at play.
“There is still more we need to understand about telehealth, such as the quality of care provided and the particular aspects of care provided by telehealth and how this influences health outcomes,” Dr. Jones said.
The results also suggest treatments for OUD are still not finding their way to patients who might benefit, he added.
“Despite the positive findings and the prior research showing that MOUD is highly effective, we found that only one in five patients received telehealth services and only one in eight received any MOUD. This really underscores the need to expand these services across clinical settings,” he added.
These and earlier findings demonstrate the potential benefits of continuing pandemic-era expansion of OUD-related telehealth services and MOUD access, Dr. Jones said.
In preparation for the end of the public health emergency on May 1, the Drug Enforcement Agency recently released a proposal that would allow providers to prescribe a 30-day supply of buprenorphine, but for patients to receive additional prescriptions, a face-to-face meeting would be required. The proposal has drawn criticism from addiction medicine specialists.
The current study didn’t explore if or how the proposal might affect patients with OUD or whether it could blunt the positive effects of the findings.
“Prior research shows that keeping individuals engaged in treatment, including on medications, is a critical part of reducing the negative health and social impacts of opioid use disorder. Our results suggest that telehealth can be an important tool in helping patients engage in and stay connected in care,” said Dr. Jones.
The study was funded by the Centers for Disease Control and Prevention, the Centers for Medicare & Medicaid Services, and the National Institutes of Health. Dr. Johnson reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM JAMA PSYCHIATRY