User login
THE CASE
A 28-year-old woman with an unremarkable medical history presented with an enlarging nodule that had been growing under her left great toenail for 6 months. The patient monitored the nodule, hoping that it would resolve on its own, but found that it steadily increased in size and began to displace the nail, causing pain. At the time of presentation, the nodule measured approximately 10 mm in diameter, and there was significant (~80°) superior displacement of the nail (FIGURE 1).
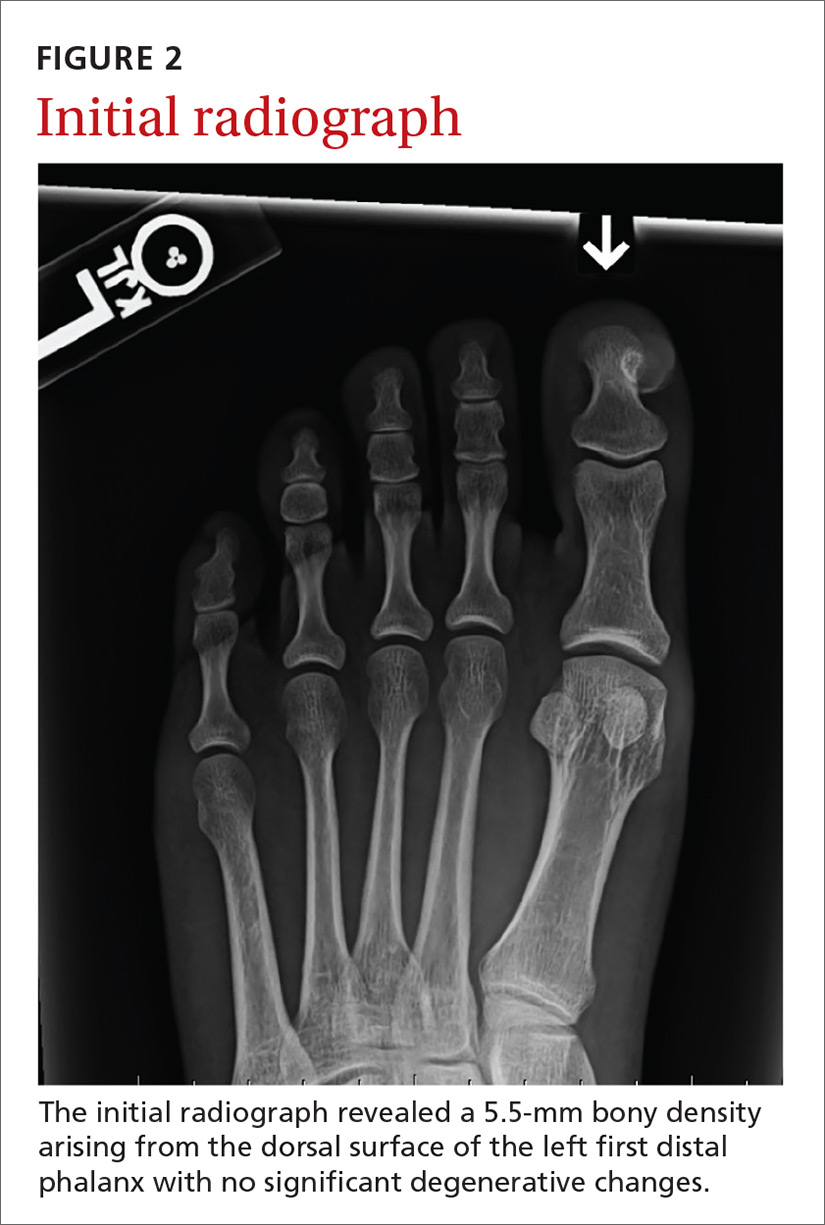
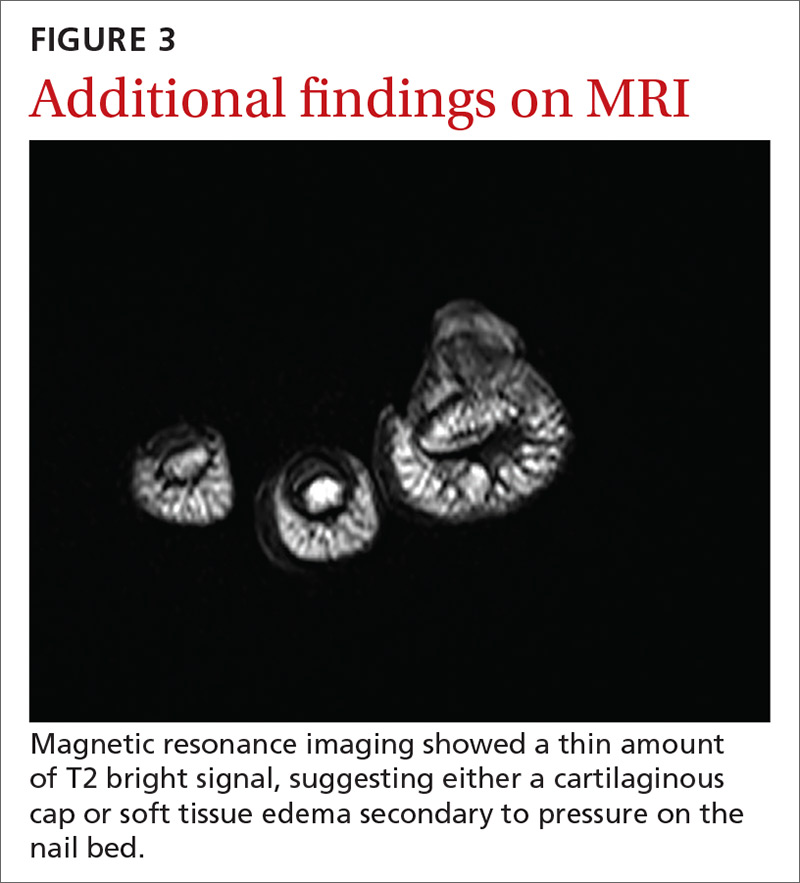
An initial radiograph identified a 5.5-mm bony density arising from the dorsal surface of the left first distal phalanx with no significant degenerative changes (FIGURE 2). A subsequent magnetic resonance image confirmed the bony excrescence and noted marrow continuity. A thin amount of T2 bright signal was also observed, suggesting either a cartilaginous cap or soft tissue edema secondary to pressure on the nail bed (FIGURE 3).
THE DIAGNOSIS
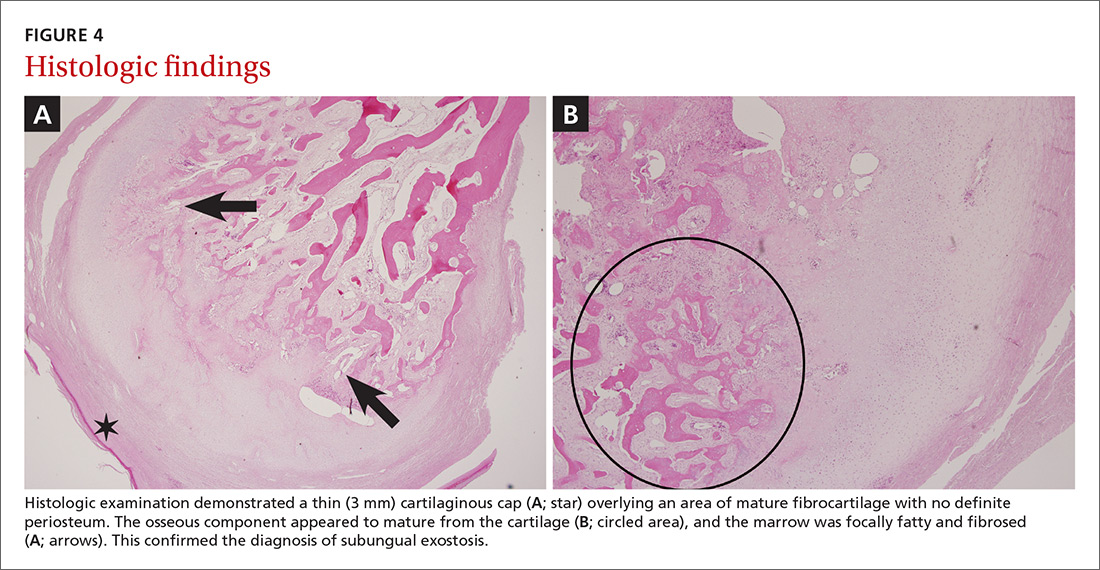
Histologic examination demonstrated a thin (3 mm) cartilaginous cap overlying an area of mature fibrocartilage with no definite periosteum. The osseous component appeared to mature from the cartilage, and the marrow was focally fatty and fibrosed (FIGURES 4A and 4B). Expert consultation with the Joint Pathology Center confirmed a benign osteochondromatous lesion.
The histologic differential diagnosis of this patient’s lesion included subungual exostosis and osteochondroma. Based on the patient’s age, location of the lesion, and histologic findings, the final diagnosis was subungual exostosis.
DISCUSSION
Subungual exostoses are benign osteocartilaginous tumors that most commonly affect children and young adults. They predominantly manifest on the dorsomedial aspect of the tip of the great toe (~80%), but can occur on other digits of the foot or hand.1 They are caused by a proliferation of fibrous tissue under the nail bed. The fibrocartilage cap then undergoes endochondral ossification to woven bone and lamellar bone trabeculae. As these lesions mature, they establish continuity with the underlying bone in the phalanx.2 Subungual exostoses were once thought to represent a proliferative response to trauma, but further research has identified a recurrent t(X;6) (q22;q13-14) translocation, suggesting a neoplastic origin.3
Osteochondromas are also common benign tumors formed by endochondral ossification, although secondary transformation into low-grade chondrosarcomas is well-documented.1 Osteochondromas commonly affect younger patients. They occur at epiphyseal areas of developing bone and have a hyaline matrix and chondrocyte pattern similar to that of a normal epiphyseal area, with confluence to the underlying trabecular and cortical bone. They are not caused by previous trauma and generally only become symptomatic after they have grown large enough to cause mechanical problems.1
Continue to: More diagnoses to consider
More diagnoses to consider
Other potential diagnoses for benign osteochondromatous lesions include bizarre parosteal osteochondromatous proliferations (BPOP) and digital mucous cysts.
BPOPs, also known as Nora’s lesions (crediting preliminary research performed by Nora and colleagues in 19834), are irregular formations of hypercellular cartilage, bone, and large chondrocytes. They predominantly occur in the small bones of the hands and feet, but may involve the skull and long bones.3 Unlike subungual exostoses and osteochondromas, BPOPs tend to occur in the third and fourth decades of life and generally do not alter, or have continuity with, the underlying bone.4
Histologically, BPOPs undergo irregular maturation, leaving a characteristic blue tint at the border of the newly formed trabecular bone. As with subungual exostoses, these lesions were traditionally believed to be reactive in nature. However, cytogenetic studies have identified variant translocations involving 1q32 (most commonly t[1;17] [q32;q21]) that are unique and common to these lesions.5
Digital mucous cysts are benign ganglion cysts that typically appear in the distal interphalangeal joints or at the proximal nail fold. They are believed to result from mucoid degeneration of connective tissue. Although generally associated with the hands, these cysts can also occur on the feet.6
Continue to: Our patient's outcome
Our patient’s outcome
After orthopedic consultation, the lesion and a 5 × 5-mm portion of the adherent germinal nail matrix were resected operatively through a medial excision. A small flap of the lateral nail matrix was rotated to cover the matrix defect, and the wound was closed. Postoperatively, the patient experienced slow wound healing (a total of 3 weeks), but there was no recurrence of the lesion at the 2-month follow-up.
THE TAKEAWAY
Osteocartilaginous tumors present as rapidly growing lesions on the distal tips of fingers and toes, but they may also occur on long bones and on the skull. Rarely malignant in nature, most of these lesions can be differentiated by location, histopathologic features, and patient age at onset. Consider surgical consultation and excision for relief of pain and/or cosmetic reasons. Recurrence is rare.
CORRESPONDENCE
Michael Barna, MD, Naval Hospital Camp Lejeune, Department of Family Medicine, 100 Brewster Blvd, Camp Lejeune, NC 28547; [email protected].
1. Miller-Breslow A, Dorfman HD. Dupuytren’s (subungual) exostosis. Am J Surg Pathol. 1988;12:368-378.
2. DaCambra MP, Gupta SK, Ferri-de-Barros F. Subungual exostosis of the toes: a systematic review. Clin Orthop Relat Res. 2014;472:1251-1259.
3. Meneses MF, Unni KK, Swee RG. Bizarre parosteal osteochondromatous proliferation of bone (Nora’s lesion). Am J Surg Pathol. 1993;17:691-697.
4. Nora FE, Dahlin DC, Beabout JW. Bizarre parosteal osteochondromatous proliferations of the hand and feet. Am J Surg Pathol. 1983;7:245-250.
5. Zambrano E, Nosé V, Perez-Atayde AR, et al. Distinct chromosomal rearrangements in subungual (Dupuytren) exostosis and bizarre parosteal osteochondromatous proliferation (Nora lesion). Am J Surg Pathol. 2004;28:1033-1039.
6. Salerni G, Alonso C. Images in clinical medicine. Digital mucous cyst. N Engl J Med. 2012;366:1335.
THE CASE
A 28-year-old woman with an unremarkable medical history presented with an enlarging nodule that had been growing under her left great toenail for 6 months. The patient monitored the nodule, hoping that it would resolve on its own, but found that it steadily increased in size and began to displace the nail, causing pain. At the time of presentation, the nodule measured approximately 10 mm in diameter, and there was significant (~80°) superior displacement of the nail (FIGURE 1).
An initial radiograph identified a 5.5-mm bony density arising from the dorsal surface of the left first distal phalanx with no significant degenerative changes (FIGURE 2). A subsequent magnetic resonance image confirmed the bony excrescence and noted marrow continuity. A thin amount of T2 bright signal was also observed, suggesting either a cartilaginous cap or soft tissue edema secondary to pressure on the nail bed (FIGURE 3).
THE DIAGNOSIS
Histologic examination demonstrated a thin (3 mm) cartilaginous cap overlying an area of mature fibrocartilage with no definite periosteum. The osseous component appeared to mature from the cartilage, and the marrow was focally fatty and fibrosed (FIGURES 4A and 4B). Expert consultation with the Joint Pathology Center confirmed a benign osteochondromatous lesion.
The histologic differential diagnosis of this patient’s lesion included subungual exostosis and osteochondroma. Based on the patient’s age, location of the lesion, and histologic findings, the final diagnosis was subungual exostosis.
DISCUSSION
Subungual exostoses are benign osteocartilaginous tumors that most commonly affect children and young adults. They predominantly manifest on the dorsomedial aspect of the tip of the great toe (~80%), but can occur on other digits of the foot or hand.1 They are caused by a proliferation of fibrous tissue under the nail bed. The fibrocartilage cap then undergoes endochondral ossification to woven bone and lamellar bone trabeculae. As these lesions mature, they establish continuity with the underlying bone in the phalanx.2 Subungual exostoses were once thought to represent a proliferative response to trauma, but further research has identified a recurrent t(X;6) (q22;q13-14) translocation, suggesting a neoplastic origin.3
Osteochondromas are also common benign tumors formed by endochondral ossification, although secondary transformation into low-grade chondrosarcomas is well-documented.1 Osteochondromas commonly affect younger patients. They occur at epiphyseal areas of developing bone and have a hyaline matrix and chondrocyte pattern similar to that of a normal epiphyseal area, with confluence to the underlying trabecular and cortical bone. They are not caused by previous trauma and generally only become symptomatic after they have grown large enough to cause mechanical problems.1
Continue to: More diagnoses to consider
More diagnoses to consider
Other potential diagnoses for benign osteochondromatous lesions include bizarre parosteal osteochondromatous proliferations (BPOP) and digital mucous cysts.
BPOPs, also known as Nora’s lesions (crediting preliminary research performed by Nora and colleagues in 19834), are irregular formations of hypercellular cartilage, bone, and large chondrocytes. They predominantly occur in the small bones of the hands and feet, but may involve the skull and long bones.3 Unlike subungual exostoses and osteochondromas, BPOPs tend to occur in the third and fourth decades of life and generally do not alter, or have continuity with, the underlying bone.4
Histologically, BPOPs undergo irregular maturation, leaving a characteristic blue tint at the border of the newly formed trabecular bone. As with subungual exostoses, these lesions were traditionally believed to be reactive in nature. However, cytogenetic studies have identified variant translocations involving 1q32 (most commonly t[1;17] [q32;q21]) that are unique and common to these lesions.5
Digital mucous cysts are benign ganglion cysts that typically appear in the distal interphalangeal joints or at the proximal nail fold. They are believed to result from mucoid degeneration of connective tissue. Although generally associated with the hands, these cysts can also occur on the feet.6
Continue to: Our patient's outcome
Our patient’s outcome
After orthopedic consultation, the lesion and a 5 × 5-mm portion of the adherent germinal nail matrix were resected operatively through a medial excision. A small flap of the lateral nail matrix was rotated to cover the matrix defect, and the wound was closed. Postoperatively, the patient experienced slow wound healing (a total of 3 weeks), but there was no recurrence of the lesion at the 2-month follow-up.
THE TAKEAWAY
Osteocartilaginous tumors present as rapidly growing lesions on the distal tips of fingers and toes, but they may also occur on long bones and on the skull. Rarely malignant in nature, most of these lesions can be differentiated by location, histopathologic features, and patient age at onset. Consider surgical consultation and excision for relief of pain and/or cosmetic reasons. Recurrence is rare.
CORRESPONDENCE
Michael Barna, MD, Naval Hospital Camp Lejeune, Department of Family Medicine, 100 Brewster Blvd, Camp Lejeune, NC 28547; [email protected].
THE CASE
A 28-year-old woman with an unremarkable medical history presented with an enlarging nodule that had been growing under her left great toenail for 6 months. The patient monitored the nodule, hoping that it would resolve on its own, but found that it steadily increased in size and began to displace the nail, causing pain. At the time of presentation, the nodule measured approximately 10 mm in diameter, and there was significant (~80°) superior displacement of the nail (FIGURE 1).
An initial radiograph identified a 5.5-mm bony density arising from the dorsal surface of the left first distal phalanx with no significant degenerative changes (FIGURE 2). A subsequent magnetic resonance image confirmed the bony excrescence and noted marrow continuity. A thin amount of T2 bright signal was also observed, suggesting either a cartilaginous cap or soft tissue edema secondary to pressure on the nail bed (FIGURE 3).
THE DIAGNOSIS
Histologic examination demonstrated a thin (3 mm) cartilaginous cap overlying an area of mature fibrocartilage with no definite periosteum. The osseous component appeared to mature from the cartilage, and the marrow was focally fatty and fibrosed (FIGURES 4A and 4B). Expert consultation with the Joint Pathology Center confirmed a benign osteochondromatous lesion.
The histologic differential diagnosis of this patient’s lesion included subungual exostosis and osteochondroma. Based on the patient’s age, location of the lesion, and histologic findings, the final diagnosis was subungual exostosis.
DISCUSSION
Subungual exostoses are benign osteocartilaginous tumors that most commonly affect children and young adults. They predominantly manifest on the dorsomedial aspect of the tip of the great toe (~80%), but can occur on other digits of the foot or hand.1 They are caused by a proliferation of fibrous tissue under the nail bed. The fibrocartilage cap then undergoes endochondral ossification to woven bone and lamellar bone trabeculae. As these lesions mature, they establish continuity with the underlying bone in the phalanx.2 Subungual exostoses were once thought to represent a proliferative response to trauma, but further research has identified a recurrent t(X;6) (q22;q13-14) translocation, suggesting a neoplastic origin.3
Osteochondromas are also common benign tumors formed by endochondral ossification, although secondary transformation into low-grade chondrosarcomas is well-documented.1 Osteochondromas commonly affect younger patients. They occur at epiphyseal areas of developing bone and have a hyaline matrix and chondrocyte pattern similar to that of a normal epiphyseal area, with confluence to the underlying trabecular and cortical bone. They are not caused by previous trauma and generally only become symptomatic after they have grown large enough to cause mechanical problems.1
Continue to: More diagnoses to consider
More diagnoses to consider
Other potential diagnoses for benign osteochondromatous lesions include bizarre parosteal osteochondromatous proliferations (BPOP) and digital mucous cysts.
BPOPs, also known as Nora’s lesions (crediting preliminary research performed by Nora and colleagues in 19834), are irregular formations of hypercellular cartilage, bone, and large chondrocytes. They predominantly occur in the small bones of the hands and feet, but may involve the skull and long bones.3 Unlike subungual exostoses and osteochondromas, BPOPs tend to occur in the third and fourth decades of life and generally do not alter, or have continuity with, the underlying bone.4
Histologically, BPOPs undergo irregular maturation, leaving a characteristic blue tint at the border of the newly formed trabecular bone. As with subungual exostoses, these lesions were traditionally believed to be reactive in nature. However, cytogenetic studies have identified variant translocations involving 1q32 (most commonly t[1;17] [q32;q21]) that are unique and common to these lesions.5
Digital mucous cysts are benign ganglion cysts that typically appear in the distal interphalangeal joints or at the proximal nail fold. They are believed to result from mucoid degeneration of connective tissue. Although generally associated with the hands, these cysts can also occur on the feet.6
Continue to: Our patient's outcome
Our patient’s outcome
After orthopedic consultation, the lesion and a 5 × 5-mm portion of the adherent germinal nail matrix were resected operatively through a medial excision. A small flap of the lateral nail matrix was rotated to cover the matrix defect, and the wound was closed. Postoperatively, the patient experienced slow wound healing (a total of 3 weeks), but there was no recurrence of the lesion at the 2-month follow-up.
THE TAKEAWAY
Osteocartilaginous tumors present as rapidly growing lesions on the distal tips of fingers and toes, but they may also occur on long bones and on the skull. Rarely malignant in nature, most of these lesions can be differentiated by location, histopathologic features, and patient age at onset. Consider surgical consultation and excision for relief of pain and/or cosmetic reasons. Recurrence is rare.
CORRESPONDENCE
Michael Barna, MD, Naval Hospital Camp Lejeune, Department of Family Medicine, 100 Brewster Blvd, Camp Lejeune, NC 28547; [email protected].
1. Miller-Breslow A, Dorfman HD. Dupuytren’s (subungual) exostosis. Am J Surg Pathol. 1988;12:368-378.
2. DaCambra MP, Gupta SK, Ferri-de-Barros F. Subungual exostosis of the toes: a systematic review. Clin Orthop Relat Res. 2014;472:1251-1259.
3. Meneses MF, Unni KK, Swee RG. Bizarre parosteal osteochondromatous proliferation of bone (Nora’s lesion). Am J Surg Pathol. 1993;17:691-697.
4. Nora FE, Dahlin DC, Beabout JW. Bizarre parosteal osteochondromatous proliferations of the hand and feet. Am J Surg Pathol. 1983;7:245-250.
5. Zambrano E, Nosé V, Perez-Atayde AR, et al. Distinct chromosomal rearrangements in subungual (Dupuytren) exostosis and bizarre parosteal osteochondromatous proliferation (Nora lesion). Am J Surg Pathol. 2004;28:1033-1039.
6. Salerni G, Alonso C. Images in clinical medicine. Digital mucous cyst. N Engl J Med. 2012;366:1335.
1. Miller-Breslow A, Dorfman HD. Dupuytren’s (subungual) exostosis. Am J Surg Pathol. 1988;12:368-378.
2. DaCambra MP, Gupta SK, Ferri-de-Barros F. Subungual exostosis of the toes: a systematic review. Clin Orthop Relat Res. 2014;472:1251-1259.
3. Meneses MF, Unni KK, Swee RG. Bizarre parosteal osteochondromatous proliferation of bone (Nora’s lesion). Am J Surg Pathol. 1993;17:691-697.
4. Nora FE, Dahlin DC, Beabout JW. Bizarre parosteal osteochondromatous proliferations of the hand and feet. Am J Surg Pathol. 1983;7:245-250.
5. Zambrano E, Nosé V, Perez-Atayde AR, et al. Distinct chromosomal rearrangements in subungual (Dupuytren) exostosis and bizarre parosteal osteochondromatous proliferation (Nora lesion). Am J Surg Pathol. 2004;28:1033-1039.
6. Salerni G, Alonso C. Images in clinical medicine. Digital mucous cyst. N Engl J Med. 2012;366:1335.