User login
Study IDs factors contributing to sleep clinic no-show rates
SAN ANTONIO – results from a single-center study showed.
“There are lots of people with sleep problems,” one of the study’s authors, Alvan Nzewuihe, MD, said in an interview at the annual meeting of the Associated Professional Sleep Societies. “However, we have to identify these patients to be able to help them. If they don’t come to the sleep clinic [for assessment], we are going nowhere.”
In an effort to better understand determinants of no-show rates among sleep clinics, Dr. Nzewuihe and colleagues performed a 10-month, retrospective chart review of 2,532 patients scheduled at Saint Louis University’s SLUCare Sleep Disorders Center during the months of July and October 2017 and April 2018. A no-show was determined if the patient failed to show up at their scheduled appointment on time or if they canceled their appointment. The researchers used multivariable logistic regression to determine which factors were independently associated with no-show rates.
Dr. Nzewuihe, a sleep medicine physician at the university, reported that the overall no-show rate during the study period was 21.2% and did not change with age, sex, or appointment factors such as time of day, day of week, or season of the year. Significant determinants of no-show rates included being a new patient (39.1% vs. 28.8% among established patients; P less than .0001) and having no health insurance (47.5% vs. public 28.3% vs private 24.2%; P less than .0001). Multivariate logistic regression confirmed the associations. New patients were 1.96 times more likely to not show up to the sleep clinic, compared with established patients, while patients with no health insurance coverage were 1.55 times more likely to not show up, compared with those with public health insurance.
The researchers wrote in their poster abstract, “Patients who are new to the clinic or have no insurance coverage have a higher odds of not showing up to their appointment and delaying their care. Efforts to prioritize high-risk patients of nonadherence will help contribute to better care and outcomes. Further studies are needed to develop methods to decrease no-show rates once high-risk appointments have been identified.”
Dr. Nzewuihe acknowledged certain limitations of the study, including its retrospective design and the fact that other possible contributing factors were not evaluated such as literacy level, employment status, and length of time between appointment booking and appointment date. The study’s first author was Julie Sahrmann, DO. The researchers reported having no financial disclosures.
SOURCE: Sahrmann J et al. Sleep 2019, Abstract 0965.
SAN ANTONIO – results from a single-center study showed.
“There are lots of people with sleep problems,” one of the study’s authors, Alvan Nzewuihe, MD, said in an interview at the annual meeting of the Associated Professional Sleep Societies. “However, we have to identify these patients to be able to help them. If they don’t come to the sleep clinic [for assessment], we are going nowhere.”
In an effort to better understand determinants of no-show rates among sleep clinics, Dr. Nzewuihe and colleagues performed a 10-month, retrospective chart review of 2,532 patients scheduled at Saint Louis University’s SLUCare Sleep Disorders Center during the months of July and October 2017 and April 2018. A no-show was determined if the patient failed to show up at their scheduled appointment on time or if they canceled their appointment. The researchers used multivariable logistic regression to determine which factors were independently associated with no-show rates.
Dr. Nzewuihe, a sleep medicine physician at the university, reported that the overall no-show rate during the study period was 21.2% and did not change with age, sex, or appointment factors such as time of day, day of week, or season of the year. Significant determinants of no-show rates included being a new patient (39.1% vs. 28.8% among established patients; P less than .0001) and having no health insurance (47.5% vs. public 28.3% vs private 24.2%; P less than .0001). Multivariate logistic regression confirmed the associations. New patients were 1.96 times more likely to not show up to the sleep clinic, compared with established patients, while patients with no health insurance coverage were 1.55 times more likely to not show up, compared with those with public health insurance.
The researchers wrote in their poster abstract, “Patients who are new to the clinic or have no insurance coverage have a higher odds of not showing up to their appointment and delaying their care. Efforts to prioritize high-risk patients of nonadherence will help contribute to better care and outcomes. Further studies are needed to develop methods to decrease no-show rates once high-risk appointments have been identified.”
Dr. Nzewuihe acknowledged certain limitations of the study, including its retrospective design and the fact that other possible contributing factors were not evaluated such as literacy level, employment status, and length of time between appointment booking and appointment date. The study’s first author was Julie Sahrmann, DO. The researchers reported having no financial disclosures.
SOURCE: Sahrmann J et al. Sleep 2019, Abstract 0965.
SAN ANTONIO – results from a single-center study showed.
“There are lots of people with sleep problems,” one of the study’s authors, Alvan Nzewuihe, MD, said in an interview at the annual meeting of the Associated Professional Sleep Societies. “However, we have to identify these patients to be able to help them. If they don’t come to the sleep clinic [for assessment], we are going nowhere.”
In an effort to better understand determinants of no-show rates among sleep clinics, Dr. Nzewuihe and colleagues performed a 10-month, retrospective chart review of 2,532 patients scheduled at Saint Louis University’s SLUCare Sleep Disorders Center during the months of July and October 2017 and April 2018. A no-show was determined if the patient failed to show up at their scheduled appointment on time or if they canceled their appointment. The researchers used multivariable logistic regression to determine which factors were independently associated with no-show rates.
Dr. Nzewuihe, a sleep medicine physician at the university, reported that the overall no-show rate during the study period was 21.2% and did not change with age, sex, or appointment factors such as time of day, day of week, or season of the year. Significant determinants of no-show rates included being a new patient (39.1% vs. 28.8% among established patients; P less than .0001) and having no health insurance (47.5% vs. public 28.3% vs private 24.2%; P less than .0001). Multivariate logistic regression confirmed the associations. New patients were 1.96 times more likely to not show up to the sleep clinic, compared with established patients, while patients with no health insurance coverage were 1.55 times more likely to not show up, compared with those with public health insurance.
The researchers wrote in their poster abstract, “Patients who are new to the clinic or have no insurance coverage have a higher odds of not showing up to their appointment and delaying their care. Efforts to prioritize high-risk patients of nonadherence will help contribute to better care and outcomes. Further studies are needed to develop methods to decrease no-show rates once high-risk appointments have been identified.”
Dr. Nzewuihe acknowledged certain limitations of the study, including its retrospective design and the fact that other possible contributing factors were not evaluated such as literacy level, employment status, and length of time between appointment booking and appointment date. The study’s first author was Julie Sahrmann, DO. The researchers reported having no financial disclosures.
SOURCE: Sahrmann J et al. Sleep 2019, Abstract 0965.
REPORTING FROM SLEEP 2019
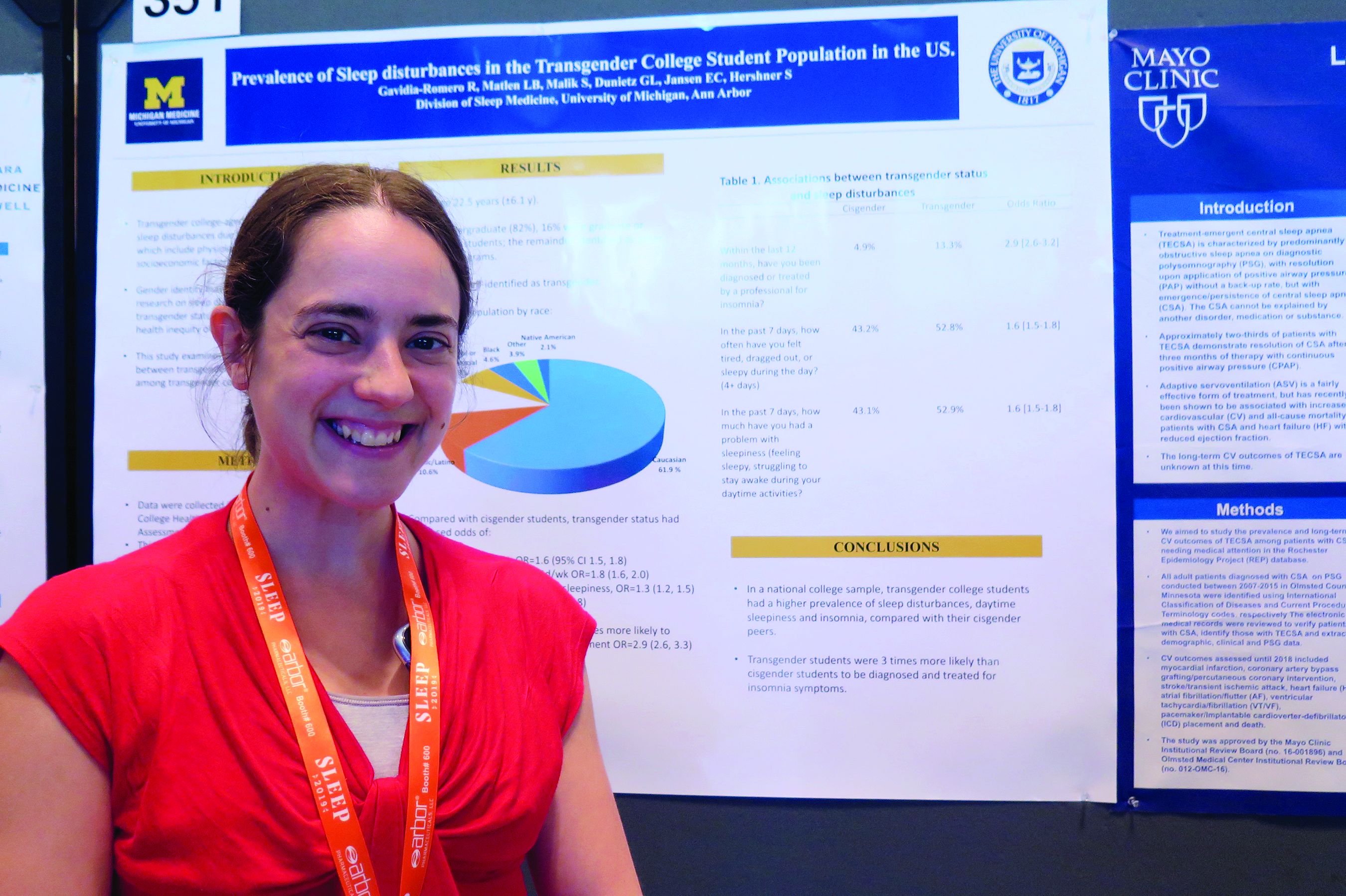
Insomnia common among transgender college students
SAN ANTONIO – Compared with their cisgender counterparts, , results from a large national population-based survey showed.
“That was a stronger association than we expected,” one of the study’s researchers, Lisa B. Matlen, MD, said during an interview at the annual meeting of the Associated Professional Sleep Societies.
According to Dr. Matlen, a fellow in the division of sleep medicine at the University of Michigan, Ann Arbor, the transgender population is “extremely understudied” when it comes to research on sleep disturbances. In an effort to examine the prevalence of sleep disturbances and the association between transgender identity and sleep disturbances among transgender college students in the United States, she and her colleagues drew from the 2016 and 2017 American College Health Association National College Health Assessment II, a confidential, voluntary, electronically administered survey of college and university students. In all, 224,233 students were polled, and the researchers analyzed their responses to questions about gender identity, sleep symptoms, and diagnoses.
The mean age of the respondents was 23 years, and most (82%) were undergraduate students. Of the 224,233 students, 3,471 (1.6%) self-identified as transgender. More than half of the transgender population (61.9%) was white, 10.6% were Hispanic/Latino, 10.5% were Asian or Pacific Islander, 6.3% were biracial or multiracial, 4.6% were black, and the rest were from other ethnicities. Compared with cisgender students, transgender students had increased odds of sleep disturbances (odds ratio, 1.6), not feeling well rested on 4 or more days per week (OR, 1.8), going to bed early on 3 or more days per week due to sleepiness (OR, 1.3), and having insomnia 3 or more days per week (OR, 1.7). In addition, transgender students were nearly three times more likely to have an insomnia diagnosis and treatment, compared with their cisgender counterparts (OR, 2.9).
Dr. Matlen acknowledged certain limitations of the study, including the fact that it drew from a population-based sample and that the survey was based on self-reported information. The study’s first author was Ronald R. Gavidia Romero, MD. The researchers reported having no financial disclosures.
SAN ANTONIO – Compared with their cisgender counterparts, , results from a large national population-based survey showed.
“That was a stronger association than we expected,” one of the study’s researchers, Lisa B. Matlen, MD, said during an interview at the annual meeting of the Associated Professional Sleep Societies.
According to Dr. Matlen, a fellow in the division of sleep medicine at the University of Michigan, Ann Arbor, the transgender population is “extremely understudied” when it comes to research on sleep disturbances. In an effort to examine the prevalence of sleep disturbances and the association between transgender identity and sleep disturbances among transgender college students in the United States, she and her colleagues drew from the 2016 and 2017 American College Health Association National College Health Assessment II, a confidential, voluntary, electronically administered survey of college and university students. In all, 224,233 students were polled, and the researchers analyzed their responses to questions about gender identity, sleep symptoms, and diagnoses.
The mean age of the respondents was 23 years, and most (82%) were undergraduate students. Of the 224,233 students, 3,471 (1.6%) self-identified as transgender. More than half of the transgender population (61.9%) was white, 10.6% were Hispanic/Latino, 10.5% were Asian or Pacific Islander, 6.3% were biracial or multiracial, 4.6% were black, and the rest were from other ethnicities. Compared with cisgender students, transgender students had increased odds of sleep disturbances (odds ratio, 1.6), not feeling well rested on 4 or more days per week (OR, 1.8), going to bed early on 3 or more days per week due to sleepiness (OR, 1.3), and having insomnia 3 or more days per week (OR, 1.7). In addition, transgender students were nearly three times more likely to have an insomnia diagnosis and treatment, compared with their cisgender counterparts (OR, 2.9).
Dr. Matlen acknowledged certain limitations of the study, including the fact that it drew from a population-based sample and that the survey was based on self-reported information. The study’s first author was Ronald R. Gavidia Romero, MD. The researchers reported having no financial disclosures.
SAN ANTONIO – Compared with their cisgender counterparts, , results from a large national population-based survey showed.
“That was a stronger association than we expected,” one of the study’s researchers, Lisa B. Matlen, MD, said during an interview at the annual meeting of the Associated Professional Sleep Societies.
According to Dr. Matlen, a fellow in the division of sleep medicine at the University of Michigan, Ann Arbor, the transgender population is “extremely understudied” when it comes to research on sleep disturbances. In an effort to examine the prevalence of sleep disturbances and the association between transgender identity and sleep disturbances among transgender college students in the United States, she and her colleagues drew from the 2016 and 2017 American College Health Association National College Health Assessment II, a confidential, voluntary, electronically administered survey of college and university students. In all, 224,233 students were polled, and the researchers analyzed their responses to questions about gender identity, sleep symptoms, and diagnoses.
The mean age of the respondents was 23 years, and most (82%) were undergraduate students. Of the 224,233 students, 3,471 (1.6%) self-identified as transgender. More than half of the transgender population (61.9%) was white, 10.6% were Hispanic/Latino, 10.5% were Asian or Pacific Islander, 6.3% were biracial or multiracial, 4.6% were black, and the rest were from other ethnicities. Compared with cisgender students, transgender students had increased odds of sleep disturbances (odds ratio, 1.6), not feeling well rested on 4 or more days per week (OR, 1.8), going to bed early on 3 or more days per week due to sleepiness (OR, 1.3), and having insomnia 3 or more days per week (OR, 1.7). In addition, transgender students were nearly three times more likely to have an insomnia diagnosis and treatment, compared with their cisgender counterparts (OR, 2.9).
Dr. Matlen acknowledged certain limitations of the study, including the fact that it drew from a population-based sample and that the survey was based on self-reported information. The study’s first author was Ronald R. Gavidia Romero, MD. The researchers reported having no financial disclosures.
REPORTING FROM SLEEP 2019
Estimated prevalence of OSA in the Americas stands at 170 million
, results from a novel epidemiologic analysis showed.
“I would not have thought that there are 170 million people in the Americas with clinically important sleep apnea based on our conservative estimates,” the study’s first author, Atul Malhotra, MD, said in an interview in advance of the annual meeting of the Associated Professional Sleep Societies. “Even if we restrict the conversation to moderate to severe sleep apnea, we still see 81 million people afflicted in the Americas alone. We have recently estimated almost 1 billion patients afflicted with OSA worldwide.”
In an effort to estimate the Americas’ prevalence of adult OSA using existing data from epidemiologic studies, Dr. Malhotra, director of sleep medicine at the University of California, San Diego, senior author Adam V. Benjafield, PhD, and their colleagues contacted authors of important analyses on the topic following an exhaustive review of the literature. For countries where no measurement had been made, they used publicly available data to obtain estimates of age, sex, race, and body mass index. Next, they developed an algorithm to match countries without prevalence estimates with countries from which OSA epidemiologic studies exist. “The situation was complicated given the variable age of the existing studies, the differences in technology used (e.g., nasal pressure vs. thermistor), the changing scoring criteria, and other sources of variability,” the researchers wrote in their abstract.
Dr. Malhotra reported on data from 38 of 40 countries in the Americas. Drawing from American Academy of Sleep Medicine 2012 criteria and using what they characterized as a “somewhat conservative” approach, the researchers estimated the prevalence of adult OSA in the Americas to be 170 million, or 37% of the population. In addition, they estimate that 81 million adults, or 18% of the population, suffer from moderate to severe OSA based on an apnea hypopnea index of 15 or more per hour. The countries with the greatest burden of OSA are the United States (54 million), Brazil (49 million), and Colombia (11 million).
“The findings will hopefully help to raise awareness about the disease but also encourage a strategic conversation regarding how best to address this large burden,” Dr. Malhotra said. “We are unaware of prior efforts to estimate OSA prevalence on a large scale.”
He acknowledged certain limitations of the study, including that the methods, equipment, definitions, and criteria used in existing studies in the medial literature varied widely. “We did our best to harmonize these methods across studies but obviously we can’t change the equipment that was used in previous studies,” he said. “Thus, we view our findings as an estimate requiring further efforts to corroborate.”
The research stemmed from an academic/industry partnership with ResMed, which provided a donation the UCSD Sleep Medicine Center. Dr. Malhotra reported having no financial disclosures. Dr. Benjafield is an employee of ResMed, a medical equipment company that specializes in sleep-related breathing devices.
SOURCE: Malhotra A et al. SLEEP 2019, Abstract 0477.
, results from a novel epidemiologic analysis showed.
“I would not have thought that there are 170 million people in the Americas with clinically important sleep apnea based on our conservative estimates,” the study’s first author, Atul Malhotra, MD, said in an interview in advance of the annual meeting of the Associated Professional Sleep Societies. “Even if we restrict the conversation to moderate to severe sleep apnea, we still see 81 million people afflicted in the Americas alone. We have recently estimated almost 1 billion patients afflicted with OSA worldwide.”
In an effort to estimate the Americas’ prevalence of adult OSA using existing data from epidemiologic studies, Dr. Malhotra, director of sleep medicine at the University of California, San Diego, senior author Adam V. Benjafield, PhD, and their colleagues contacted authors of important analyses on the topic following an exhaustive review of the literature. For countries where no measurement had been made, they used publicly available data to obtain estimates of age, sex, race, and body mass index. Next, they developed an algorithm to match countries without prevalence estimates with countries from which OSA epidemiologic studies exist. “The situation was complicated given the variable age of the existing studies, the differences in technology used (e.g., nasal pressure vs. thermistor), the changing scoring criteria, and other sources of variability,” the researchers wrote in their abstract.
Dr. Malhotra reported on data from 38 of 40 countries in the Americas. Drawing from American Academy of Sleep Medicine 2012 criteria and using what they characterized as a “somewhat conservative” approach, the researchers estimated the prevalence of adult OSA in the Americas to be 170 million, or 37% of the population. In addition, they estimate that 81 million adults, or 18% of the population, suffer from moderate to severe OSA based on an apnea hypopnea index of 15 or more per hour. The countries with the greatest burden of OSA are the United States (54 million), Brazil (49 million), and Colombia (11 million).
“The findings will hopefully help to raise awareness about the disease but also encourage a strategic conversation regarding how best to address this large burden,” Dr. Malhotra said. “We are unaware of prior efforts to estimate OSA prevalence on a large scale.”
He acknowledged certain limitations of the study, including that the methods, equipment, definitions, and criteria used in existing studies in the medial literature varied widely. “We did our best to harmonize these methods across studies but obviously we can’t change the equipment that was used in previous studies,” he said. “Thus, we view our findings as an estimate requiring further efforts to corroborate.”
The research stemmed from an academic/industry partnership with ResMed, which provided a donation the UCSD Sleep Medicine Center. Dr. Malhotra reported having no financial disclosures. Dr. Benjafield is an employee of ResMed, a medical equipment company that specializes in sleep-related breathing devices.
SOURCE: Malhotra A et al. SLEEP 2019, Abstract 0477.
, results from a novel epidemiologic analysis showed.
“I would not have thought that there are 170 million people in the Americas with clinically important sleep apnea based on our conservative estimates,” the study’s first author, Atul Malhotra, MD, said in an interview in advance of the annual meeting of the Associated Professional Sleep Societies. “Even if we restrict the conversation to moderate to severe sleep apnea, we still see 81 million people afflicted in the Americas alone. We have recently estimated almost 1 billion patients afflicted with OSA worldwide.”
In an effort to estimate the Americas’ prevalence of adult OSA using existing data from epidemiologic studies, Dr. Malhotra, director of sleep medicine at the University of California, San Diego, senior author Adam V. Benjafield, PhD, and their colleagues contacted authors of important analyses on the topic following an exhaustive review of the literature. For countries where no measurement had been made, they used publicly available data to obtain estimates of age, sex, race, and body mass index. Next, they developed an algorithm to match countries without prevalence estimates with countries from which OSA epidemiologic studies exist. “The situation was complicated given the variable age of the existing studies, the differences in technology used (e.g., nasal pressure vs. thermistor), the changing scoring criteria, and other sources of variability,” the researchers wrote in their abstract.
Dr. Malhotra reported on data from 38 of 40 countries in the Americas. Drawing from American Academy of Sleep Medicine 2012 criteria and using what they characterized as a “somewhat conservative” approach, the researchers estimated the prevalence of adult OSA in the Americas to be 170 million, or 37% of the population. In addition, they estimate that 81 million adults, or 18% of the population, suffer from moderate to severe OSA based on an apnea hypopnea index of 15 or more per hour. The countries with the greatest burden of OSA are the United States (54 million), Brazil (49 million), and Colombia (11 million).
“The findings will hopefully help to raise awareness about the disease but also encourage a strategic conversation regarding how best to address this large burden,” Dr. Malhotra said. “We are unaware of prior efforts to estimate OSA prevalence on a large scale.”
He acknowledged certain limitations of the study, including that the methods, equipment, definitions, and criteria used in existing studies in the medial literature varied widely. “We did our best to harmonize these methods across studies but obviously we can’t change the equipment that was used in previous studies,” he said. “Thus, we view our findings as an estimate requiring further efforts to corroborate.”
The research stemmed from an academic/industry partnership with ResMed, which provided a donation the UCSD Sleep Medicine Center. Dr. Malhotra reported having no financial disclosures. Dr. Benjafield is an employee of ResMed, a medical equipment company that specializes in sleep-related breathing devices.
SOURCE: Malhotra A et al. SLEEP 2019, Abstract 0477.
REPORTING FROM SLEEP 2019
Key clinical point: The large burden of OSA in the Americas has not been widely appreciated.
Major finding: The estimated prevalence of adult OSA in the Americas is 170 million, or 37% of the population.
Study details: An analysis of epidemiologic studies that included data on 38 countries in the Americas.
Disclosures: The research stemmed from an academic/industry partnership with ResMed, a medical equipment company that specializes in sleep-related breathing devices, which provided a donation the UCSD Sleep Medicine Center. Dr. Malhotra reported having no financial disclosures. Dr. Benjafield is an employee of ResMed.
Source: Malhotra A et al. SLEEP 2019, Abstract 0477.