User login
RIV poster contest a meeting highlight
Look back at the history of SHM’s annual Research, Innovations and Clinical Vignettes poster competition – better known as the RIV – and it may seem inevitable that it’s grown into one of the main highlights of the conference. The RIV has become so popular that the number of submissions has nearly tripled from 634 in 2010 to 1,712 this year.
“Certainly, there is some natural evolution,” said Dr. Fang, a hospitalist, researcher, and anticoagulation clinic director at the University of California San Francisco. “But not all specialty societies embrace research or encourage its growth, so I would give a lot of credit to the Society of Hospital Medicine for being very deliberate in trying to strengthen its research program, highlight the research that hospitalists do, and make research a core pillar of what SHM stands for.”
The efforts have clearly worked, as RIV is a major driver for annual meeting attendance. The poster competition draws massive crowds that snake their way through the accepted posters.
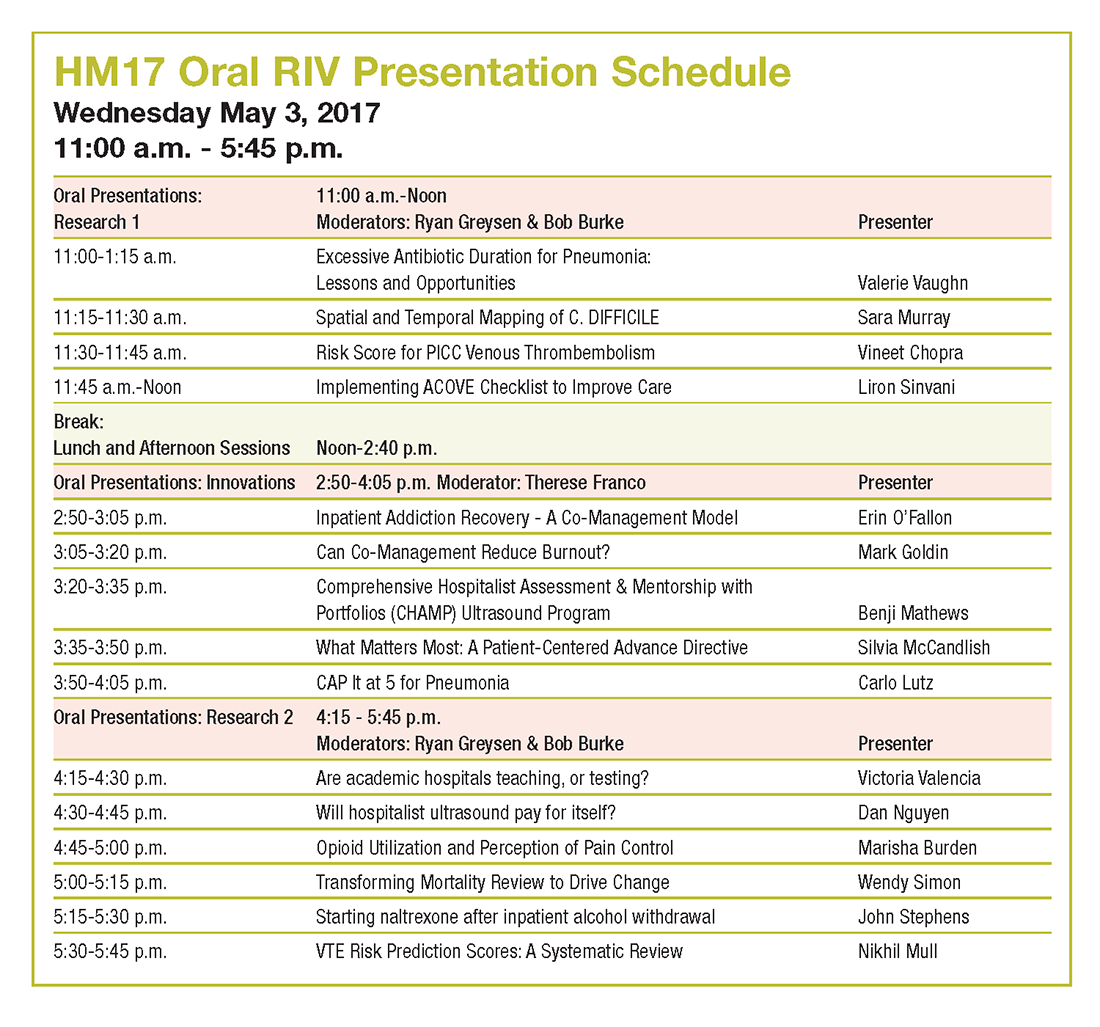
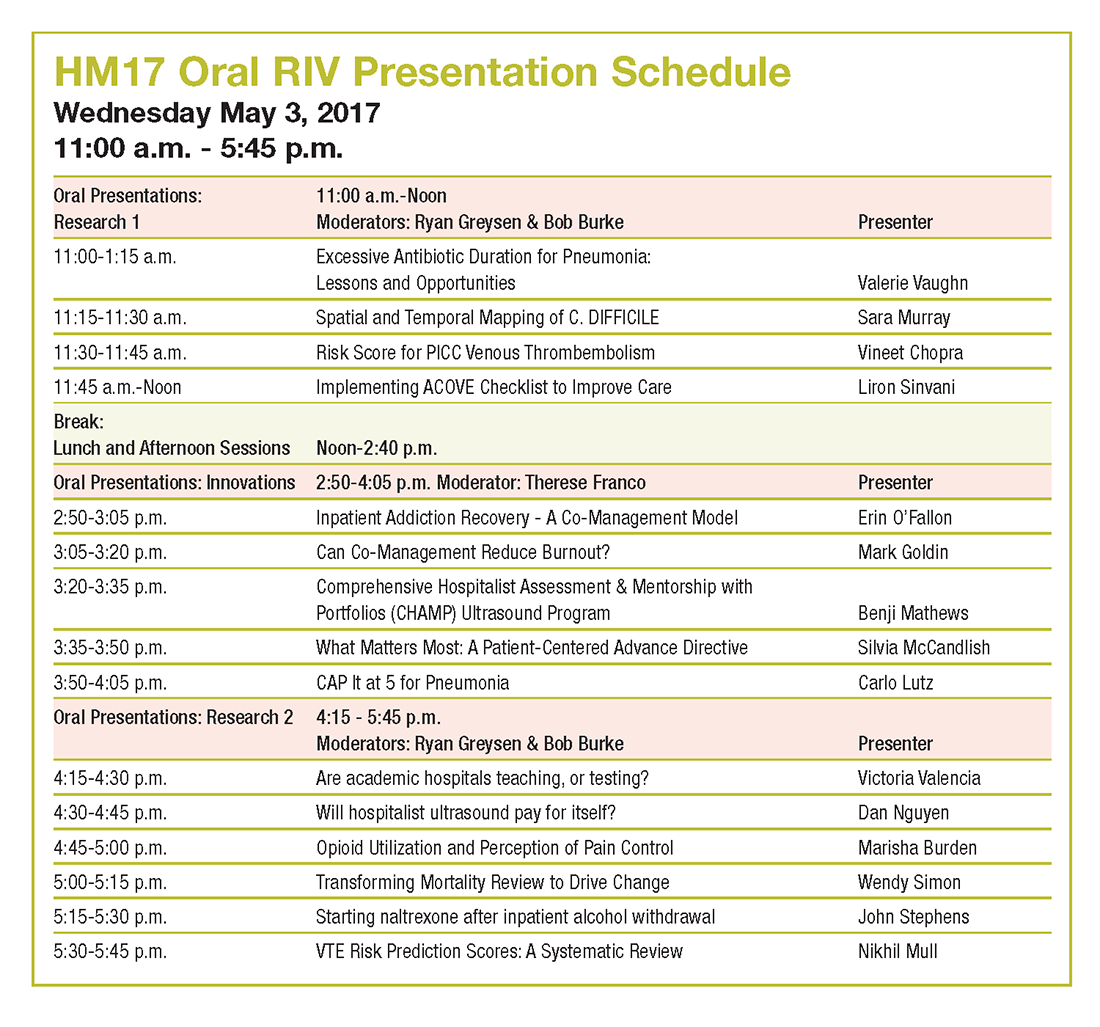
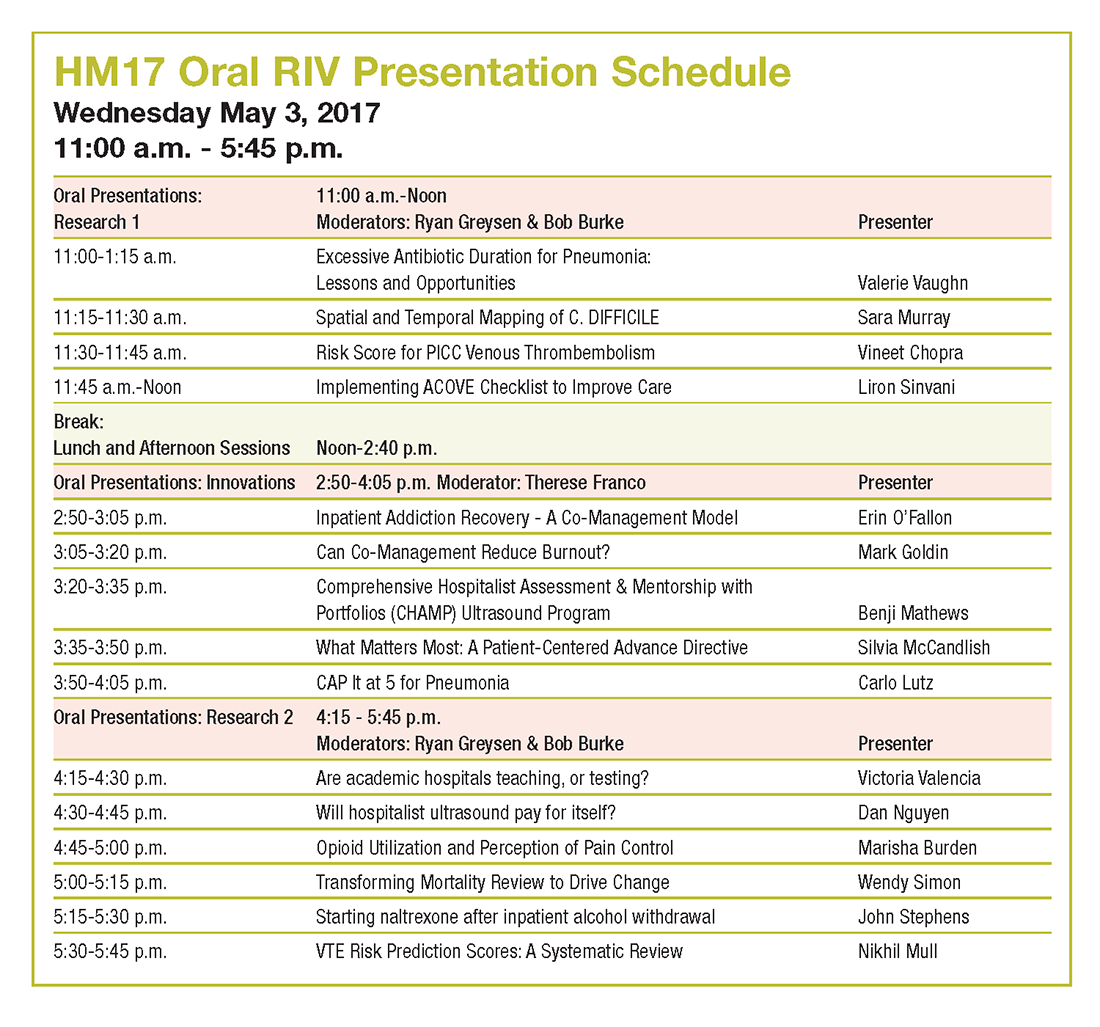
For those interested in a deeper dive, SHM chooses a dozen or so top abstracts for oral presentations that are, in Dr. Fang’s words, “the creme de la creme of all the research and innovations for the given year.”
The growth of the abstracts competition comes, of course, as the specialty itself has seen its ranks skyrocket. Hospitalists now number an estimated 52,000 nationally, and in addition to providing direct clinical care, have taken ownership of key health care drivers like patient safety, quality improvement, and systems change.
“We do what we do for the good of health care and, ultimately, for the good of our patients,” Dr. Fang said. “Sometimes that’s rounding and taking care of patients in a clinical fashion, and sometimes it’s contributing to the medical literature. It could have been really easy for a specialty to say, ‘Not our problem,’ or ‘No, we’re just rounding.’ ”
HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM, believes that the commitment of SHM’s founding generation to do research for the past decade has created a group of mentors that push younger hospitalists to do more of the same.
“If we didn’t have the research engine part of hospital medicine, if we didn’t have the folks who are getting into administration and other important leadership areas, we wouldn’t see the maturation of this specialty and we would, in many ways, be stuck at the point at which we started,” Dr. Feldman said. “The only way for us to move forward is to do the research, to be in position to make sure that hospital medicine continues to grow in a direction that is good for our patients, for us, and for the entire system.”
That perspective is what motivates hospitalists to make the RIV bigger each year, said Dr. Fang.
“Having your abstract accepted as a poster or an oral presentation showcases all the work that you’ve put into it,” Dr. Fang said. “There’s a huge amount of pride in showing what you’ve been able to achieve. The driving force is the desire to see what other people are doing, and network to share ideas. That’s the really wonderful part of the RIV competition.”
Look back at the history of SHM’s annual Research, Innovations and Clinical Vignettes poster competition – better known as the RIV – and it may seem inevitable that it’s grown into one of the main highlights of the conference. The RIV has become so popular that the number of submissions has nearly tripled from 634 in 2010 to 1,712 this year.
“Certainly, there is some natural evolution,” said Dr. Fang, a hospitalist, researcher, and anticoagulation clinic director at the University of California San Francisco. “But not all specialty societies embrace research or encourage its growth, so I would give a lot of credit to the Society of Hospital Medicine for being very deliberate in trying to strengthen its research program, highlight the research that hospitalists do, and make research a core pillar of what SHM stands for.”
The efforts have clearly worked, as RIV is a major driver for annual meeting attendance. The poster competition draws massive crowds that snake their way through the accepted posters.
For those interested in a deeper dive, SHM chooses a dozen or so top abstracts for oral presentations that are, in Dr. Fang’s words, “the creme de la creme of all the research and innovations for the given year.”
The growth of the abstracts competition comes, of course, as the specialty itself has seen its ranks skyrocket. Hospitalists now number an estimated 52,000 nationally, and in addition to providing direct clinical care, have taken ownership of key health care drivers like patient safety, quality improvement, and systems change.
“We do what we do for the good of health care and, ultimately, for the good of our patients,” Dr. Fang said. “Sometimes that’s rounding and taking care of patients in a clinical fashion, and sometimes it’s contributing to the medical literature. It could have been really easy for a specialty to say, ‘Not our problem,’ or ‘No, we’re just rounding.’ ”
HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM, believes that the commitment of SHM’s founding generation to do research for the past decade has created a group of mentors that push younger hospitalists to do more of the same.
“If we didn’t have the research engine part of hospital medicine, if we didn’t have the folks who are getting into administration and other important leadership areas, we wouldn’t see the maturation of this specialty and we would, in many ways, be stuck at the point at which we started,” Dr. Feldman said. “The only way for us to move forward is to do the research, to be in position to make sure that hospital medicine continues to grow in a direction that is good for our patients, for us, and for the entire system.”
That perspective is what motivates hospitalists to make the RIV bigger each year, said Dr. Fang.
“Having your abstract accepted as a poster or an oral presentation showcases all the work that you’ve put into it,” Dr. Fang said. “There’s a huge amount of pride in showing what you’ve been able to achieve. The driving force is the desire to see what other people are doing, and network to share ideas. That’s the really wonderful part of the RIV competition.”
Look back at the history of SHM’s annual Research, Innovations and Clinical Vignettes poster competition – better known as the RIV – and it may seem inevitable that it’s grown into one of the main highlights of the conference. The RIV has become so popular that the number of submissions has nearly tripled from 634 in 2010 to 1,712 this year.
“Certainly, there is some natural evolution,” said Dr. Fang, a hospitalist, researcher, and anticoagulation clinic director at the University of California San Francisco. “But not all specialty societies embrace research or encourage its growth, so I would give a lot of credit to the Society of Hospital Medicine for being very deliberate in trying to strengthen its research program, highlight the research that hospitalists do, and make research a core pillar of what SHM stands for.”
The efforts have clearly worked, as RIV is a major driver for annual meeting attendance. The poster competition draws massive crowds that snake their way through the accepted posters.
For those interested in a deeper dive, SHM chooses a dozen or so top abstracts for oral presentations that are, in Dr. Fang’s words, “the creme de la creme of all the research and innovations for the given year.”
The growth of the abstracts competition comes, of course, as the specialty itself has seen its ranks skyrocket. Hospitalists now number an estimated 52,000 nationally, and in addition to providing direct clinical care, have taken ownership of key health care drivers like patient safety, quality improvement, and systems change.
“We do what we do for the good of health care and, ultimately, for the good of our patients,” Dr. Fang said. “Sometimes that’s rounding and taking care of patients in a clinical fashion, and sometimes it’s contributing to the medical literature. It could have been really easy for a specialty to say, ‘Not our problem,’ or ‘No, we’re just rounding.’ ”
HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM, believes that the commitment of SHM’s founding generation to do research for the past decade has created a group of mentors that push younger hospitalists to do more of the same.
“If we didn’t have the research engine part of hospital medicine, if we didn’t have the folks who are getting into administration and other important leadership areas, we wouldn’t see the maturation of this specialty and we would, in many ways, be stuck at the point at which we started,” Dr. Feldman said. “The only way for us to move forward is to do the research, to be in position to make sure that hospital medicine continues to grow in a direction that is good for our patients, for us, and for the entire system.”
That perspective is what motivates hospitalists to make the RIV bigger each year, said Dr. Fang.
“Having your abstract accepted as a poster or an oral presentation showcases all the work that you’ve put into it,” Dr. Fang said. “There’s a huge amount of pride in showing what you’ve been able to achieve. The driving force is the desire to see what other people are doing, and network to share ideas. That’s the really wonderful part of the RIV competition.”
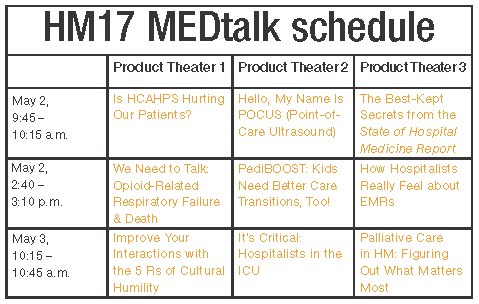
MEDtalk presentations
Is HCAHPS Hurting Our Patients?
Speakers: Suparna Dutta, MD, MS, MPH, and John Biebelhausen, MD, MBA
Explore the unintended consequences of assessing patient satisfaction and labeling pain as “the fifth vital sign” in the midst of a national opioid epidemic. The Hospital Consumer Assessment of Healthcare Providers and Systems, which was developed by the Centers for Medicare & Medicaid Services to assess the inpatient experience and impacts hospital reimbursement, includes directed questions about pain management.
Join us as we review the background of HCAHPS, its potential unintended impacts over the years, as well as current and future efforts of SHM toward improving health policy in this domain.
Hello, My Name Is POCUS (Point-of-Care Ultrasound)
Speaker: Nilam Soni, MD, MS, FHM
Point-of-care ultrasound is being used by more hospitalists to perform bedside diagnostics and to guide invasive procedures. However, most practicing hospitalists completed their training before point-of-care ultrasound education was common in medical school and residency curricula. This interactive session will:
- Explain what point-of-care ultrasonography is and how hospitalists are currently using it.
- Highlight some of the unique point-of-care ultrasound activities at HM17.
- Describe the launch of a new point-of-care ultrasound certification program offered by SHM & ACCP.
The Best-Kept Secrets from the State of Hospital Medicine Report
Speaker: Johnbuck Creamer, MD, SFHM
The State of Hospital Medicine Report is powered by SHM’s biannual survey that recently captured data from nearly 600 HM groups, augmented by additional hospitalist data licensed from MGMA. We’ll explore trends and difference among groups, including:
- Compensation per wRVU and use of nocturnists are increasing.
- Turnover rates are decreasing.
- Compensation for quality performance varies greatly among academic, nonacademic, and pediatric practice groups.
- NP/PA utilization rates are very different between East and West U.S. regions.
- Family Practice presence is increasing in adult-only practice groups.
- Academic groups are falling further behind in CPT coding levels.
We Need to Talk: Opioid-Related Respiratory Failure & Death
Speaker: Thomas Frederickson, MD, SFHM
Discussion topics:
- The opioid epidemic – not just an outpatient issue.
- How opioids can cause respiratory arrest and death, and why current screening and monitoring strategies can fail.
- What works – examples of successful strategies that have been implemented and have saved lives.
PediBOOST®: Kids Need Better Care Transitions, Too!
Speaker: James O’Callaghan, MD, SFHM
PediBOOST is a pediatric-specific adaption of the SHM Project BOOST® (Better Outcomes by Optimizing Safe Transitions) quality initiative. The goal is to improve poor discharge processes (demonstrated by low patient satisfaction and worse clinical outcomes, not just higher hospital readmission rates).
It considers unique problems for hospitalized children, including:
- Medication issues – palatability and adherence concerns, need for compounding.
- Equipment issues – portability use for home and school.
- Education issues – engagement of patient, as developmentally appropriate, along with training of all providers who might care for the patient (parents, teachers).
How Hospitalists Really Feel about EMRs
Speaker: Rupesh Prasad, MD, MPH, SFHM
Electronic medical record use has tremendously increased in the last few years.
- What are the potential benefits of use – have they been realized?
- What do the hospitalists think:
- How have EMRs impacted patient safety?
- How have EMRs impacted patient face to face time?
- What are hospitalists’ frustrations about EMRs?
Improve Your Interactions with the 5 Rs of Cultural Humility
Speaker: O’Neil Pyke, MD, SFHM
As the proverbial stranger at the bedside, HM providers are tasked with a very challenging proposition: meet a new patient in their most vulnerable state and quickly establish effective lines of communication and trust and provide patient-centric care, ultimately yielding a satisfied patient (and family) irrespective of the clinical outcome. With increased focus on patient experience and satisfaction, it is imperative that hospitals and health systems equip all hospitalists with the tools needed to deliver culturally competent care to all patients served.
The goal of the 5 Rs is to equip HM providers with tangible resources and easy to understand reminders that focus on encouraging awareness and, ultimately, deliver culturally “humble” care to all patients (and family members).
- Respect: Hospitalists will treat every person with the utmost respect and strive to preserve patient dignity.
- Regard: Hospitalists will hold every person in their highest regard and not allow unconscious biases to manifest, exercising utmost sensitivity to anticipated differences in beliefs, value systems, and preferences.
- Relevance: Hospitalists will expect cultural humility to be relevant and apply this practice to every encounter.
- Reflection: Hospitalists will approach every encounter with humility and understanding that there is always something to learn from everyone.
- Resiliency: In order to provide better care for hospitalized patients, hospitalists will embody the practice of cultural humility to enhance personal resiliency and compassion for all.
It’s Critical: Hospitalists in the ICU
Speaker: Joseph Sweigart, MD
We hope to:
- Describe formation of purpose of the critical care task force within the Education Committee.
- Discuss the creation and execution of the SHM critical care survey.
- Present selected results including:
- Introduce strategies to address the practice gaps identified including:
Palliative Care in Hospital Medicine: Figuring Out What Matters Most
Speaker: Rab Razzak, MBBS, MD
We aim to:
- Discuss the overall definition of palliative care. It is for all seriously ill patients and focuses on human-centered care and quality of life, best provided early in an illness.
- Idea of primary palliative care and role of hospitalists. Most palliative care is provided by frontline clinicians, and hospitalists are optimally positioned to support seriously ill patients and their families. It is crucial for HM to involve palliative care specialists when needed.
- Effective communication about serious illness – words that work and how to operationalize human-centered care while honestly discussing serious illness.
Is HCAHPS Hurting Our Patients?
Speakers: Suparna Dutta, MD, MS, MPH, and John Biebelhausen, MD, MBA
Explore the unintended consequences of assessing patient satisfaction and labeling pain as “the fifth vital sign” in the midst of a national opioid epidemic. The Hospital Consumer Assessment of Healthcare Providers and Systems, which was developed by the Centers for Medicare & Medicaid Services to assess the inpatient experience and impacts hospital reimbursement, includes directed questions about pain management.
Join us as we review the background of HCAHPS, its potential unintended impacts over the years, as well as current and future efforts of SHM toward improving health policy in this domain.
Hello, My Name Is POCUS (Point-of-Care Ultrasound)
Speaker: Nilam Soni, MD, MS, FHM
Point-of-care ultrasound is being used by more hospitalists to perform bedside diagnostics and to guide invasive procedures. However, most practicing hospitalists completed their training before point-of-care ultrasound education was common in medical school and residency curricula. This interactive session will:
- Explain what point-of-care ultrasonography is and how hospitalists are currently using it.
- Highlight some of the unique point-of-care ultrasound activities at HM17.
- Describe the launch of a new point-of-care ultrasound certification program offered by SHM & ACCP.
The Best-Kept Secrets from the State of Hospital Medicine Report
Speaker: Johnbuck Creamer, MD, SFHM
The State of Hospital Medicine Report is powered by SHM’s biannual survey that recently captured data from nearly 600 HM groups, augmented by additional hospitalist data licensed from MGMA. We’ll explore trends and difference among groups, including:
- Compensation per wRVU and use of nocturnists are increasing.
- Turnover rates are decreasing.
- Compensation for quality performance varies greatly among academic, nonacademic, and pediatric practice groups.
- NP/PA utilization rates are very different between East and West U.S. regions.
- Family Practice presence is increasing in adult-only practice groups.
- Academic groups are falling further behind in CPT coding levels.
We Need to Talk: Opioid-Related Respiratory Failure & Death
Speaker: Thomas Frederickson, MD, SFHM
Discussion topics:
- The opioid epidemic – not just an outpatient issue.
- How opioids can cause respiratory arrest and death, and why current screening and monitoring strategies can fail.
- What works – examples of successful strategies that have been implemented and have saved lives.
PediBOOST®: Kids Need Better Care Transitions, Too!
Speaker: James O’Callaghan, MD, SFHM
PediBOOST is a pediatric-specific adaption of the SHM Project BOOST® (Better Outcomes by Optimizing Safe Transitions) quality initiative. The goal is to improve poor discharge processes (demonstrated by low patient satisfaction and worse clinical outcomes, not just higher hospital readmission rates).
It considers unique problems for hospitalized children, including:
- Medication issues – palatability and adherence concerns, need for compounding.
- Equipment issues – portability use for home and school.
- Education issues – engagement of patient, as developmentally appropriate, along with training of all providers who might care for the patient (parents, teachers).
How Hospitalists Really Feel about EMRs
Speaker: Rupesh Prasad, MD, MPH, SFHM
Electronic medical record use has tremendously increased in the last few years.
- What are the potential benefits of use – have they been realized?
- What do the hospitalists think:
- How have EMRs impacted patient safety?
- How have EMRs impacted patient face to face time?
- What are hospitalists’ frustrations about EMRs?
Improve Your Interactions with the 5 Rs of Cultural Humility
Speaker: O’Neil Pyke, MD, SFHM
As the proverbial stranger at the bedside, HM providers are tasked with a very challenging proposition: meet a new patient in their most vulnerable state and quickly establish effective lines of communication and trust and provide patient-centric care, ultimately yielding a satisfied patient (and family) irrespective of the clinical outcome. With increased focus on patient experience and satisfaction, it is imperative that hospitals and health systems equip all hospitalists with the tools needed to deliver culturally competent care to all patients served.
The goal of the 5 Rs is to equip HM providers with tangible resources and easy to understand reminders that focus on encouraging awareness and, ultimately, deliver culturally “humble” care to all patients (and family members).
- Respect: Hospitalists will treat every person with the utmost respect and strive to preserve patient dignity.
- Regard: Hospitalists will hold every person in their highest regard and not allow unconscious biases to manifest, exercising utmost sensitivity to anticipated differences in beliefs, value systems, and preferences.
- Relevance: Hospitalists will expect cultural humility to be relevant and apply this practice to every encounter.
- Reflection: Hospitalists will approach every encounter with humility and understanding that there is always something to learn from everyone.
- Resiliency: In order to provide better care for hospitalized patients, hospitalists will embody the practice of cultural humility to enhance personal resiliency and compassion for all.
It’s Critical: Hospitalists in the ICU
Speaker: Joseph Sweigart, MD
We hope to:
- Describe formation of purpose of the critical care task force within the Education Committee.
- Discuss the creation and execution of the SHM critical care survey.
- Present selected results including:
- Introduce strategies to address the practice gaps identified including:
Palliative Care in Hospital Medicine: Figuring Out What Matters Most
Speaker: Rab Razzak, MBBS, MD
We aim to:
- Discuss the overall definition of palliative care. It is for all seriously ill patients and focuses on human-centered care and quality of life, best provided early in an illness.
- Idea of primary palliative care and role of hospitalists. Most palliative care is provided by frontline clinicians, and hospitalists are optimally positioned to support seriously ill patients and their families. It is crucial for HM to involve palliative care specialists when needed.
- Effective communication about serious illness – words that work and how to operationalize human-centered care while honestly discussing serious illness.
Is HCAHPS Hurting Our Patients?
Speakers: Suparna Dutta, MD, MS, MPH, and John Biebelhausen, MD, MBA
Explore the unintended consequences of assessing patient satisfaction and labeling pain as “the fifth vital sign” in the midst of a national opioid epidemic. The Hospital Consumer Assessment of Healthcare Providers and Systems, which was developed by the Centers for Medicare & Medicaid Services to assess the inpatient experience and impacts hospital reimbursement, includes directed questions about pain management.
Join us as we review the background of HCAHPS, its potential unintended impacts over the years, as well as current and future efforts of SHM toward improving health policy in this domain.
Hello, My Name Is POCUS (Point-of-Care Ultrasound)
Speaker: Nilam Soni, MD, MS, FHM
Point-of-care ultrasound is being used by more hospitalists to perform bedside diagnostics and to guide invasive procedures. However, most practicing hospitalists completed their training before point-of-care ultrasound education was common in medical school and residency curricula. This interactive session will:
- Explain what point-of-care ultrasonography is and how hospitalists are currently using it.
- Highlight some of the unique point-of-care ultrasound activities at HM17.
- Describe the launch of a new point-of-care ultrasound certification program offered by SHM & ACCP.
The Best-Kept Secrets from the State of Hospital Medicine Report
Speaker: Johnbuck Creamer, MD, SFHM
The State of Hospital Medicine Report is powered by SHM’s biannual survey that recently captured data from nearly 600 HM groups, augmented by additional hospitalist data licensed from MGMA. We’ll explore trends and difference among groups, including:
- Compensation per wRVU and use of nocturnists are increasing.
- Turnover rates are decreasing.
- Compensation for quality performance varies greatly among academic, nonacademic, and pediatric practice groups.
- NP/PA utilization rates are very different between East and West U.S. regions.
- Family Practice presence is increasing in adult-only practice groups.
- Academic groups are falling further behind in CPT coding levels.
We Need to Talk: Opioid-Related Respiratory Failure & Death
Speaker: Thomas Frederickson, MD, SFHM
Discussion topics:
- The opioid epidemic – not just an outpatient issue.
- How opioids can cause respiratory arrest and death, and why current screening and monitoring strategies can fail.
- What works – examples of successful strategies that have been implemented and have saved lives.
PediBOOST®: Kids Need Better Care Transitions, Too!
Speaker: James O’Callaghan, MD, SFHM
PediBOOST is a pediatric-specific adaption of the SHM Project BOOST® (Better Outcomes by Optimizing Safe Transitions) quality initiative. The goal is to improve poor discharge processes (demonstrated by low patient satisfaction and worse clinical outcomes, not just higher hospital readmission rates).
It considers unique problems for hospitalized children, including:
- Medication issues – palatability and adherence concerns, need for compounding.
- Equipment issues – portability use for home and school.
- Education issues – engagement of patient, as developmentally appropriate, along with training of all providers who might care for the patient (parents, teachers).
How Hospitalists Really Feel about EMRs
Speaker: Rupesh Prasad, MD, MPH, SFHM
Electronic medical record use has tremendously increased in the last few years.
- What are the potential benefits of use – have they been realized?
- What do the hospitalists think:
- How have EMRs impacted patient safety?
- How have EMRs impacted patient face to face time?
- What are hospitalists’ frustrations about EMRs?
Improve Your Interactions with the 5 Rs of Cultural Humility
Speaker: O’Neil Pyke, MD, SFHM
As the proverbial stranger at the bedside, HM providers are tasked with a very challenging proposition: meet a new patient in their most vulnerable state and quickly establish effective lines of communication and trust and provide patient-centric care, ultimately yielding a satisfied patient (and family) irrespective of the clinical outcome. With increased focus on patient experience and satisfaction, it is imperative that hospitals and health systems equip all hospitalists with the tools needed to deliver culturally competent care to all patients served.
The goal of the 5 Rs is to equip HM providers with tangible resources and easy to understand reminders that focus on encouraging awareness and, ultimately, deliver culturally “humble” care to all patients (and family members).
- Respect: Hospitalists will treat every person with the utmost respect and strive to preserve patient dignity.
- Regard: Hospitalists will hold every person in their highest regard and not allow unconscious biases to manifest, exercising utmost sensitivity to anticipated differences in beliefs, value systems, and preferences.
- Relevance: Hospitalists will expect cultural humility to be relevant and apply this practice to every encounter.
- Reflection: Hospitalists will approach every encounter with humility and understanding that there is always something to learn from everyone.
- Resiliency: In order to provide better care for hospitalized patients, hospitalists will embody the practice of cultural humility to enhance personal resiliency and compassion for all.
It’s Critical: Hospitalists in the ICU
Speaker: Joseph Sweigart, MD
We hope to:
- Describe formation of purpose of the critical care task force within the Education Committee.
- Discuss the creation and execution of the SHM critical care survey.
- Present selected results including:
- Introduce strategies to address the practice gaps identified including:
Palliative Care in Hospital Medicine: Figuring Out What Matters Most
Speaker: Rab Razzak, MBBS, MD
We aim to:
- Discuss the overall definition of palliative care. It is for all seriously ill patients and focuses on human-centered care and quality of life, best provided early in an illness.
- Idea of primary palliative care and role of hospitalists. Most palliative care is provided by frontline clinicians, and hospitalists are optimally positioned to support seriously ill patients and their families. It is crucial for HM to involve palliative care specialists when needed.
- Effective communication about serious illness – words that work and how to operationalize human-centered care while honestly discussing serious illness.
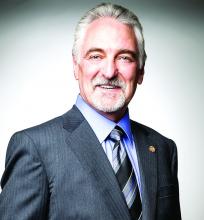
Tips from 'the father of modern networking'
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
What’s new at HM17
There is only one annual meeting dedicated to hospitalists, designed by hospitalists, and focusing purely on issues important to hospitalists. But even that isn’t enough to make sure more hospitalists show up every year.
That’s because a yearly conference can’t just be a rehash of the last one.
A valuable conference, certainly one worth spending the bulk of a continuing medical budget on, offers something new every year. Or, to look at the schedule for HM17, a lot of new every year.
That’s an unlikely complaint this year. The annual meeting schedule for May 1-4 at Mandalay Bay Resort and Casino includes five new educational tracks: High Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
“We’re really excited to be able to offer more clinical content,” said HM17 course director Lenny Feldman, MD, FAAP, FACP, SFHM.
Dr. Feldman sees each of the new tracks as filling separate and specific needs of HM attendees who vary from nonphysician providers to hospitalists to medical students.
Take, for instance, the High Value Care, Clinical Updates, and Diagnostic Reasoning sessions that are debuting.
“We wanted to make sure that we had as many clinically oriented sessions as possible,” Dr. Feldman said. “Which meant we needed to increase the amount of clinical content we have offered compared to the past few years. The new clinical track allows us to add probably 12 or so different sessions that will fill the needs of our attendees.”
The Diagnostic Reasoning and High Value Care tracks, in particular, highlight the annual meeting’s continued evolution toward a focus on evidence-based care, as that mantra becomes a bedrock of clinical treatment.
“Training our hospitalists to use the best dialogistic reasoning in their approach to their patients is a big push in hospital medicine right now,” Dr. Feldman said, “Hopefully, a track on that topic will excite people who love thinking about medicine, who got into medicine because of the mystery and want a renewed focus on how to be a great diagnostician.”
Dr. Feldman also noted that the High Value Care track should be a hot topic, as hospitalists want to learn how to provide high quality and high value care to patients at the same time. The new tracks should appeal to different groups and make the annual meeting more appealing to a variety of attendees, not just rank-and-file doctors.
The mini Medical Education track, for instance, is a subset of a half-dozen sessions tailored directly to medical educators in academic settings who face different challenges than their counterparts in community settings. The same goes for the Health Policy track, which will offer a handful of sessions suitable for novices looking to learn more in an age of reform, or policy wonks hoping to expand their knowledge.
Meeting evolving needs
New offerings aren’t limited to the main conference schedule. The 2017 roster of pre-courses includes one titled, “Bugs, Drugs and You: Infectious Diseases ‘Boot Camp’ for Hospitalists.” This daylong session hasn’t been held since 2013, and copresenter Jennifer Hanrahan, DO, associate professor of medicine at Case Western Reserve University in Cleveland, says the timing is good.
“I don’t know that the percentage of people hospitalized for infection has increased,” she said. “Because we are doing things more quickly than we did in the past, length of stays are shorter and there is a lot of pressure to get patients out of the hospital. There is a lot of consultation with Infectious Disease.”
Dr. Hanrahan, who also serves as medical director of infection prevention at Cleveland’s MetroHealth Medical Center, says that with so many patients hospitalized for infections, the value of updating one’s knowledge every few years is critical.
“I’ve been an infectious disease physician for 18 years and I’m also a hospitalist,” she said. “The types of questions I get vary a great deal depending on the experience of the hospitalist. My hope would be that we would be able to provide a basic level of understanding so that people would be more confident in approaching these problems.”
Another new feature this year is offer some of the most popular sessions at multiple times. In years past, popular sessions – such as “Update and Pearls in Infectious Diseases” and “Non–Evidence-Based Medicine: Things We Do for No Reason” – are standing room only events with attendees sitting on floors or gathered to eavesdrop from doorways.
“That says something about the content that’s being delivered, but that’s not very comfortable for folks who want to sit through a session,” Dr. Feldman said. “We’ve decided to add repeat sessions of popular presentations. We want everyone to be comfortable while they’re learning the important clinical content that’s being delivered at these sessions.”
The 2017 focus on healthcare policy is also new. Educational sessions on the policy landscape will be formally buttressed by plenary presentations from Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation, and Karen DeSalvo, MD, MPH, MSc, a former acting assistant secretary for health at the U.S. Department of Health and Human Services and national coordinator for health information technology.
“There’s a thirst for (policy news) among members of the Society of Hospital Medicine,” Dr. Feldman said. “It is easy to get lost in the day-to-day work that we do, but I think most of us really enjoy hearing about the bigger picture, especially when the bigger picture is in flux.”
“Right now, this is critical,” added Dr. Finn. “Health insurance coverage has a huge impact on hospitals. I think all practicing hospitalists will need to engage with the hospital C-suite if insurance and coverage changes. Since we are hospital based, we are directly tied to anything that the federal government does in terms of health care changes. It’s important for hospitalists to be knowledgeable about health policy.”
One major highlight of the meeting calendar – less new and more historically under-appreciated, in Dr. Feldman’s view – should be the 18 workshop presentations, which are essentially 90-minute dissertations, whittled down from roughly 150 submissions.
“These are the best submissions that we received,” Dr. Feldman said. “We worked hard to make sure that the workshops encompass the breadth and depth of hospital medicine. It is not just one area that’s covered in every workshop. We’ll have workshops ranging from clinical reasoning and communication with patients, to quality improvement issues and high value care discussions, as well as a case-based approach to inpatient dermatology.”
While annual meetings’ new offerings are always an important draw, Dr. Feldman says that the annual “standbys,” such as practice management and pediatrics, are necessary to keep attendees up to date on best practices in changing times.
“It’s pretty self-evident that if we’re going to be an important specialty, we need to serve those who are caring for patients day in and day out, as well as folks who are researching how we can do it better,” he said. “Then we must make sure that data is disseminated to all of us who are taking care of patients. That’s one of the really important parts of this meeting: dissemination of the important work.”
There is only one annual meeting dedicated to hospitalists, designed by hospitalists, and focusing purely on issues important to hospitalists. But even that isn’t enough to make sure more hospitalists show up every year.
That’s because a yearly conference can’t just be a rehash of the last one.
A valuable conference, certainly one worth spending the bulk of a continuing medical budget on, offers something new every year. Or, to look at the schedule for HM17, a lot of new every year.
That’s an unlikely complaint this year. The annual meeting schedule for May 1-4 at Mandalay Bay Resort and Casino includes five new educational tracks: High Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
“We’re really excited to be able to offer more clinical content,” said HM17 course director Lenny Feldman, MD, FAAP, FACP, SFHM.
Dr. Feldman sees each of the new tracks as filling separate and specific needs of HM attendees who vary from nonphysician providers to hospitalists to medical students.
Take, for instance, the High Value Care, Clinical Updates, and Diagnostic Reasoning sessions that are debuting.
“We wanted to make sure that we had as many clinically oriented sessions as possible,” Dr. Feldman said. “Which meant we needed to increase the amount of clinical content we have offered compared to the past few years. The new clinical track allows us to add probably 12 or so different sessions that will fill the needs of our attendees.”
The Diagnostic Reasoning and High Value Care tracks, in particular, highlight the annual meeting’s continued evolution toward a focus on evidence-based care, as that mantra becomes a bedrock of clinical treatment.
“Training our hospitalists to use the best dialogistic reasoning in their approach to their patients is a big push in hospital medicine right now,” Dr. Feldman said, “Hopefully, a track on that topic will excite people who love thinking about medicine, who got into medicine because of the mystery and want a renewed focus on how to be a great diagnostician.”
Dr. Feldman also noted that the High Value Care track should be a hot topic, as hospitalists want to learn how to provide high quality and high value care to patients at the same time. The new tracks should appeal to different groups and make the annual meeting more appealing to a variety of attendees, not just rank-and-file doctors.
The mini Medical Education track, for instance, is a subset of a half-dozen sessions tailored directly to medical educators in academic settings who face different challenges than their counterparts in community settings. The same goes for the Health Policy track, which will offer a handful of sessions suitable for novices looking to learn more in an age of reform, or policy wonks hoping to expand their knowledge.
Meeting evolving needs
New offerings aren’t limited to the main conference schedule. The 2017 roster of pre-courses includes one titled, “Bugs, Drugs and You: Infectious Diseases ‘Boot Camp’ for Hospitalists.” This daylong session hasn’t been held since 2013, and copresenter Jennifer Hanrahan, DO, associate professor of medicine at Case Western Reserve University in Cleveland, says the timing is good.
“I don’t know that the percentage of people hospitalized for infection has increased,” she said. “Because we are doing things more quickly than we did in the past, length of stays are shorter and there is a lot of pressure to get patients out of the hospital. There is a lot of consultation with Infectious Disease.”
Dr. Hanrahan, who also serves as medical director of infection prevention at Cleveland’s MetroHealth Medical Center, says that with so many patients hospitalized for infections, the value of updating one’s knowledge every few years is critical.
“I’ve been an infectious disease physician for 18 years and I’m also a hospitalist,” she said. “The types of questions I get vary a great deal depending on the experience of the hospitalist. My hope would be that we would be able to provide a basic level of understanding so that people would be more confident in approaching these problems.”
Another new feature this year is offer some of the most popular sessions at multiple times. In years past, popular sessions – such as “Update and Pearls in Infectious Diseases” and “Non–Evidence-Based Medicine: Things We Do for No Reason” – are standing room only events with attendees sitting on floors or gathered to eavesdrop from doorways.
“That says something about the content that’s being delivered, but that’s not very comfortable for folks who want to sit through a session,” Dr. Feldman said. “We’ve decided to add repeat sessions of popular presentations. We want everyone to be comfortable while they’re learning the important clinical content that’s being delivered at these sessions.”
The 2017 focus on healthcare policy is also new. Educational sessions on the policy landscape will be formally buttressed by plenary presentations from Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation, and Karen DeSalvo, MD, MPH, MSc, a former acting assistant secretary for health at the U.S. Department of Health and Human Services and national coordinator for health information technology.
“There’s a thirst for (policy news) among members of the Society of Hospital Medicine,” Dr. Feldman said. “It is easy to get lost in the day-to-day work that we do, but I think most of us really enjoy hearing about the bigger picture, especially when the bigger picture is in flux.”
“Right now, this is critical,” added Dr. Finn. “Health insurance coverage has a huge impact on hospitals. I think all practicing hospitalists will need to engage with the hospital C-suite if insurance and coverage changes. Since we are hospital based, we are directly tied to anything that the federal government does in terms of health care changes. It’s important for hospitalists to be knowledgeable about health policy.”
One major highlight of the meeting calendar – less new and more historically under-appreciated, in Dr. Feldman’s view – should be the 18 workshop presentations, which are essentially 90-minute dissertations, whittled down from roughly 150 submissions.
“These are the best submissions that we received,” Dr. Feldman said. “We worked hard to make sure that the workshops encompass the breadth and depth of hospital medicine. It is not just one area that’s covered in every workshop. We’ll have workshops ranging from clinical reasoning and communication with patients, to quality improvement issues and high value care discussions, as well as a case-based approach to inpatient dermatology.”
While annual meetings’ new offerings are always an important draw, Dr. Feldman says that the annual “standbys,” such as practice management and pediatrics, are necessary to keep attendees up to date on best practices in changing times.
“It’s pretty self-evident that if we’re going to be an important specialty, we need to serve those who are caring for patients day in and day out, as well as folks who are researching how we can do it better,” he said. “Then we must make sure that data is disseminated to all of us who are taking care of patients. That’s one of the really important parts of this meeting: dissemination of the important work.”
There is only one annual meeting dedicated to hospitalists, designed by hospitalists, and focusing purely on issues important to hospitalists. But even that isn’t enough to make sure more hospitalists show up every year.
That’s because a yearly conference can’t just be a rehash of the last one.
A valuable conference, certainly one worth spending the bulk of a continuing medical budget on, offers something new every year. Or, to look at the schedule for HM17, a lot of new every year.
That’s an unlikely complaint this year. The annual meeting schedule for May 1-4 at Mandalay Bay Resort and Casino includes five new educational tracks: High Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
“We’re really excited to be able to offer more clinical content,” said HM17 course director Lenny Feldman, MD, FAAP, FACP, SFHM.
Dr. Feldman sees each of the new tracks as filling separate and specific needs of HM attendees who vary from nonphysician providers to hospitalists to medical students.
Take, for instance, the High Value Care, Clinical Updates, and Diagnostic Reasoning sessions that are debuting.
“We wanted to make sure that we had as many clinically oriented sessions as possible,” Dr. Feldman said. “Which meant we needed to increase the amount of clinical content we have offered compared to the past few years. The new clinical track allows us to add probably 12 or so different sessions that will fill the needs of our attendees.”
The Diagnostic Reasoning and High Value Care tracks, in particular, highlight the annual meeting’s continued evolution toward a focus on evidence-based care, as that mantra becomes a bedrock of clinical treatment.
“Training our hospitalists to use the best dialogistic reasoning in their approach to their patients is a big push in hospital medicine right now,” Dr. Feldman said, “Hopefully, a track on that topic will excite people who love thinking about medicine, who got into medicine because of the mystery and want a renewed focus on how to be a great diagnostician.”
Dr. Feldman also noted that the High Value Care track should be a hot topic, as hospitalists want to learn how to provide high quality and high value care to patients at the same time. The new tracks should appeal to different groups and make the annual meeting more appealing to a variety of attendees, not just rank-and-file doctors.
The mini Medical Education track, for instance, is a subset of a half-dozen sessions tailored directly to medical educators in academic settings who face different challenges than their counterparts in community settings. The same goes for the Health Policy track, which will offer a handful of sessions suitable for novices looking to learn more in an age of reform, or policy wonks hoping to expand their knowledge.
Meeting evolving needs
New offerings aren’t limited to the main conference schedule. The 2017 roster of pre-courses includes one titled, “Bugs, Drugs and You: Infectious Diseases ‘Boot Camp’ for Hospitalists.” This daylong session hasn’t been held since 2013, and copresenter Jennifer Hanrahan, DO, associate professor of medicine at Case Western Reserve University in Cleveland, says the timing is good.
“I don’t know that the percentage of people hospitalized for infection has increased,” she said. “Because we are doing things more quickly than we did in the past, length of stays are shorter and there is a lot of pressure to get patients out of the hospital. There is a lot of consultation with Infectious Disease.”
Dr. Hanrahan, who also serves as medical director of infection prevention at Cleveland’s MetroHealth Medical Center, says that with so many patients hospitalized for infections, the value of updating one’s knowledge every few years is critical.
“I’ve been an infectious disease physician for 18 years and I’m also a hospitalist,” she said. “The types of questions I get vary a great deal depending on the experience of the hospitalist. My hope would be that we would be able to provide a basic level of understanding so that people would be more confident in approaching these problems.”
Another new feature this year is offer some of the most popular sessions at multiple times. In years past, popular sessions – such as “Update and Pearls in Infectious Diseases” and “Non–Evidence-Based Medicine: Things We Do for No Reason” – are standing room only events with attendees sitting on floors or gathered to eavesdrop from doorways.
“That says something about the content that’s being delivered, but that’s not very comfortable for folks who want to sit through a session,” Dr. Feldman said. “We’ve decided to add repeat sessions of popular presentations. We want everyone to be comfortable while they’re learning the important clinical content that’s being delivered at these sessions.”
The 2017 focus on healthcare policy is also new. Educational sessions on the policy landscape will be formally buttressed by plenary presentations from Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation, and Karen DeSalvo, MD, MPH, MSc, a former acting assistant secretary for health at the U.S. Department of Health and Human Services and national coordinator for health information technology.
“There’s a thirst for (policy news) among members of the Society of Hospital Medicine,” Dr. Feldman said. “It is easy to get lost in the day-to-day work that we do, but I think most of us really enjoy hearing about the bigger picture, especially when the bigger picture is in flux.”
“Right now, this is critical,” added Dr. Finn. “Health insurance coverage has a huge impact on hospitals. I think all practicing hospitalists will need to engage with the hospital C-suite if insurance and coverage changes. Since we are hospital based, we are directly tied to anything that the federal government does in terms of health care changes. It’s important for hospitalists to be knowledgeable about health policy.”
One major highlight of the meeting calendar – less new and more historically under-appreciated, in Dr. Feldman’s view – should be the 18 workshop presentations, which are essentially 90-minute dissertations, whittled down from roughly 150 submissions.
“These are the best submissions that we received,” Dr. Feldman said. “We worked hard to make sure that the workshops encompass the breadth and depth of hospital medicine. It is not just one area that’s covered in every workshop. We’ll have workshops ranging from clinical reasoning and communication with patients, to quality improvement issues and high value care discussions, as well as a case-based approach to inpatient dermatology.”
While annual meetings’ new offerings are always an important draw, Dr. Feldman says that the annual “standbys,” such as practice management and pediatrics, are necessary to keep attendees up to date on best practices in changing times.
“It’s pretty self-evident that if we’re going to be an important specialty, we need to serve those who are caring for patients day in and day out, as well as folks who are researching how we can do it better,” he said. “Then we must make sure that data is disseminated to all of us who are taking care of patients. That’s one of the really important parts of this meeting: dissemination of the important work.”
HM17’s ‘must-see sessions’
LAS VEGAS — Not to sound like a Sin City come on, but pick a course, any course.
No, seriously.
Hospitalists and other attendees at the Hospitalist Medicine 2017 meeting next month will do well to figure out what sessions they want to attend before arriving at the Mandalay Bay Resort and Casino. This 4-day Super Bowl of hospital medicine prides itself on offering more than any attendee can find time for. This year is no exception, as the annual meeting has added five new educational tracks: High-Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
The committee does its job to fill the meeting with best-in-class educational sessions. Here are some of the group’s recommendations for this year’s meeting:
1. “The Hospitalist’s Role in the Opioid Epidemic” – Tuesday, May 2; 1:35 p.m.–2:35 p.m.
2. “Opioids for Acute Pain Management in the Seriously Ill – How to Safely Prescribe” – Wednesday, May 3; 2:50 p.m.–3:30 p.m.
3. “Non-opiate Pain Management for the Hospitalist” – Wednesday, May 3; 4:20 p.m.–5:00 p.m.
Elizabeth Cook, MD, medical director of the hospitalist division of Medical Associates of Central Virginia in Lynchburg, said, “The historical emphasis on pain control has helped contributed to the current epidemic of opioid abuse, overdoses, and deaths. Hospitalists have a need to use these medications for care of the hospitalized patient but have an important part to play in leading the way to appropriate use and patient education regarding the dangers of these medications. These sessions will provide hospitalists with some tools to use in beginning to effect a shift in pain management strategies and responsible use of narcotic pain medications.”
Miguel Angel Villagra, MD, FACP, FHM, hospitalist department program medical director at White River Medical Center in Batesville, Ark., said, “As primary front-line providers in the acute care setting, we face the everyday struggles in the management of chronic opioid users. Acquiring some general guidelines can help us tailor our approach within an ethical focus to improve the care of this population.”
Sarah Stella, MD, an academic hospitalist at Denver Health, said, “This is a crucial and timely topic. Hospitalists have had a hand in perpetuating the opioid epidemic and can play an important role in helping to end it. In this regard, there are many opportunities to do good, such as judicious prescribing and tapering medications for acute pain, starting eligible patients on Suboxone [buprenorphine] in-house, and arranging substance abuse treatment follow-up.”
4. “Focus on POCUS - Introduction to Point-of-Care Ultrasound for Pediatric Hospitalists” – Tuesday, May 2; 10:35 a.m.–11:35 a.m.
Weijen Chang, MD, SFHM, FAAP, chief of the division of pediatric hospital medicine, Baystate Medical Center/Baystate Children’s Hospital, Springfield, Mass., said, “This is the first pediatric POCUS session offered at SHM ever. And it does not require an additional cost ... the pediatric track is critically important, as a substantial number of athlete attendees are either Peds or MedPeds. I think SHM aims to create a pediatric track that discusses topics that are less covered in other meetings, such as the value equation and issues facing women leaders in HM.”
6. “Foundations of a Hospital Medicine Telemedicine Program” – Wednesday, May 3; 415 p.m.–5:20 p.m.
Dr. Villagra added, “Telemedicine is a new innovative technology with the promise of overcoming geographical barriers to health care providers. A lot of new companies and software development has made this technology more user/patient friendly.”
7. “Hot Topics in Health Policy for Hospitalists” – Thursday, May 4; 7:40 a.m.–8:35 a.m.
8. “The Impact of the New Administration on Health Care Reform” – Thursday, May 4; 8:45 a.m.–9:40 a.m.
9. “Health Care Payment Reform for Hospitalist 2017: Tips for MIPS and Beyond” – Thursday, May 4; 9:50 a.m.–10:45 a.m.
Dr. Stella said, “As a safety-net hospitalist in Colorado, a state which largely expanded Medicare under the Affordable Care Act (ACA), I am concerned about the impact repealing the ACA would have on my patients as well as on safety-net hospitals such as my own. I hope that these sessions will increase my understanding of the issues and my ability to advocate for my patients.”
Dr. Cook said, “The U.S. government is functioning in historically unprecedented ways with major shifts in health care policy expected to occur over the next 4 years. It is essential that physician leaders play an active role in shaping the discussion around these important topics ... hospitalists have an opportunity to provide leadership in this arena, and these sessions will help participants to build the knowledge about these complex issues that is crucial to being an active part of the dialogue.”
10. “Workshop: Hospitalists as Leaders in Patient Flow and Hospital Throughput” – Thursday, May 4; 10 a.m.–11:30 a.m.
Dr. Stella said, “Recently, I was appointed to a leadership role on a major initiative to improve hospital patient flow at my institution. We are concentrating on several different areas, including avoidable hospitalizations, preventable excess days, delayed discharges, and variable access to services. I was excited to see a workshop this year dedicated to how hospitalists can successfully lead such initiatives. I will definitely be attending this session as I am interested in what others are doing in their institutions to creatively overcome patient flow challenges.”
11. “Hospitalist Careers: So Many Options” – Tuesday, May 2; 10:35 a.m.–11:15 a.m.
Dr. Villagra said, “Hospital medicine has so many pathways for a full career development and is not a pit stop before fellowship. Early- and mid-career hospitalists can benefit from interactions with senior hospitalists for the understanding of what hospital medicine has to offer for their professional growth.”
Richard Quinn is a freelance writer in New Jersey.
LAS VEGAS — Not to sound like a Sin City come on, but pick a course, any course.
No, seriously.
Hospitalists and other attendees at the Hospitalist Medicine 2017 meeting next month will do well to figure out what sessions they want to attend before arriving at the Mandalay Bay Resort and Casino. This 4-day Super Bowl of hospital medicine prides itself on offering more than any attendee can find time for. This year is no exception, as the annual meeting has added five new educational tracks: High-Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
The committee does its job to fill the meeting with best-in-class educational sessions. Here are some of the group’s recommendations for this year’s meeting:
1. “The Hospitalist’s Role in the Opioid Epidemic” – Tuesday, May 2; 1:35 p.m.–2:35 p.m.
2. “Opioids for Acute Pain Management in the Seriously Ill – How to Safely Prescribe” – Wednesday, May 3; 2:50 p.m.–3:30 p.m.
3. “Non-opiate Pain Management for the Hospitalist” – Wednesday, May 3; 4:20 p.m.–5:00 p.m.
Elizabeth Cook, MD, medical director of the hospitalist division of Medical Associates of Central Virginia in Lynchburg, said, “The historical emphasis on pain control has helped contributed to the current epidemic of opioid abuse, overdoses, and deaths. Hospitalists have a need to use these medications for care of the hospitalized patient but have an important part to play in leading the way to appropriate use and patient education regarding the dangers of these medications. These sessions will provide hospitalists with some tools to use in beginning to effect a shift in pain management strategies and responsible use of narcotic pain medications.”
Miguel Angel Villagra, MD, FACP, FHM, hospitalist department program medical director at White River Medical Center in Batesville, Ark., said, “As primary front-line providers in the acute care setting, we face the everyday struggles in the management of chronic opioid users. Acquiring some general guidelines can help us tailor our approach within an ethical focus to improve the care of this population.”
Sarah Stella, MD, an academic hospitalist at Denver Health, said, “This is a crucial and timely topic. Hospitalists have had a hand in perpetuating the opioid epidemic and can play an important role in helping to end it. In this regard, there are many opportunities to do good, such as judicious prescribing and tapering medications for acute pain, starting eligible patients on Suboxone [buprenorphine] in-house, and arranging substance abuse treatment follow-up.”
4. “Focus on POCUS - Introduction to Point-of-Care Ultrasound for Pediatric Hospitalists” – Tuesday, May 2; 10:35 a.m.–11:35 a.m.
Weijen Chang, MD, SFHM, FAAP, chief of the division of pediatric hospital medicine, Baystate Medical Center/Baystate Children’s Hospital, Springfield, Mass., said, “This is the first pediatric POCUS session offered at SHM ever. And it does not require an additional cost ... the pediatric track is critically important, as a substantial number of athlete attendees are either Peds or MedPeds. I think SHM aims to create a pediatric track that discusses topics that are less covered in other meetings, such as the value equation and issues facing women leaders in HM.”
6. “Foundations of a Hospital Medicine Telemedicine Program” – Wednesday, May 3; 415 p.m.–5:20 p.m.
Dr. Villagra added, “Telemedicine is a new innovative technology with the promise of overcoming geographical barriers to health care providers. A lot of new companies and software development has made this technology more user/patient friendly.”
7. “Hot Topics in Health Policy for Hospitalists” – Thursday, May 4; 7:40 a.m.–8:35 a.m.
8. “The Impact of the New Administration on Health Care Reform” – Thursday, May 4; 8:45 a.m.–9:40 a.m.
9. “Health Care Payment Reform for Hospitalist 2017: Tips for MIPS and Beyond” – Thursday, May 4; 9:50 a.m.–10:45 a.m.
Dr. Stella said, “As a safety-net hospitalist in Colorado, a state which largely expanded Medicare under the Affordable Care Act (ACA), I am concerned about the impact repealing the ACA would have on my patients as well as on safety-net hospitals such as my own. I hope that these sessions will increase my understanding of the issues and my ability to advocate for my patients.”
Dr. Cook said, “The U.S. government is functioning in historically unprecedented ways with major shifts in health care policy expected to occur over the next 4 years. It is essential that physician leaders play an active role in shaping the discussion around these important topics ... hospitalists have an opportunity to provide leadership in this arena, and these sessions will help participants to build the knowledge about these complex issues that is crucial to being an active part of the dialogue.”
10. “Workshop: Hospitalists as Leaders in Patient Flow and Hospital Throughput” – Thursday, May 4; 10 a.m.–11:30 a.m.
Dr. Stella said, “Recently, I was appointed to a leadership role on a major initiative to improve hospital patient flow at my institution. We are concentrating on several different areas, including avoidable hospitalizations, preventable excess days, delayed discharges, and variable access to services. I was excited to see a workshop this year dedicated to how hospitalists can successfully lead such initiatives. I will definitely be attending this session as I am interested in what others are doing in their institutions to creatively overcome patient flow challenges.”
11. “Hospitalist Careers: So Many Options” – Tuesday, May 2; 10:35 a.m.–11:15 a.m.
Dr. Villagra said, “Hospital medicine has so many pathways for a full career development and is not a pit stop before fellowship. Early- and mid-career hospitalists can benefit from interactions with senior hospitalists for the understanding of what hospital medicine has to offer for their professional growth.”
Richard Quinn is a freelance writer in New Jersey.
LAS VEGAS — Not to sound like a Sin City come on, but pick a course, any course.
No, seriously.
Hospitalists and other attendees at the Hospitalist Medicine 2017 meeting next month will do well to figure out what sessions they want to attend before arriving at the Mandalay Bay Resort and Casino. This 4-day Super Bowl of hospital medicine prides itself on offering more than any attendee can find time for. This year is no exception, as the annual meeting has added five new educational tracks: High-Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
The committee does its job to fill the meeting with best-in-class educational sessions. Here are some of the group’s recommendations for this year’s meeting:
1. “The Hospitalist’s Role in the Opioid Epidemic” – Tuesday, May 2; 1:35 p.m.–2:35 p.m.
2. “Opioids for Acute Pain Management in the Seriously Ill – How to Safely Prescribe” – Wednesday, May 3; 2:50 p.m.–3:30 p.m.
3. “Non-opiate Pain Management for the Hospitalist” – Wednesday, May 3; 4:20 p.m.–5:00 p.m.
Elizabeth Cook, MD, medical director of the hospitalist division of Medical Associates of Central Virginia in Lynchburg, said, “The historical emphasis on pain control has helped contributed to the current epidemic of opioid abuse, overdoses, and deaths. Hospitalists have a need to use these medications for care of the hospitalized patient but have an important part to play in leading the way to appropriate use and patient education regarding the dangers of these medications. These sessions will provide hospitalists with some tools to use in beginning to effect a shift in pain management strategies and responsible use of narcotic pain medications.”
Miguel Angel Villagra, MD, FACP, FHM, hospitalist department program medical director at White River Medical Center in Batesville, Ark., said, “As primary front-line providers in the acute care setting, we face the everyday struggles in the management of chronic opioid users. Acquiring some general guidelines can help us tailor our approach within an ethical focus to improve the care of this population.”
Sarah Stella, MD, an academic hospitalist at Denver Health, said, “This is a crucial and timely topic. Hospitalists have had a hand in perpetuating the opioid epidemic and can play an important role in helping to end it. In this regard, there are many opportunities to do good, such as judicious prescribing and tapering medications for acute pain, starting eligible patients on Suboxone [buprenorphine] in-house, and arranging substance abuse treatment follow-up.”
4. “Focus on POCUS - Introduction to Point-of-Care Ultrasound for Pediatric Hospitalists” – Tuesday, May 2; 10:35 a.m.–11:35 a.m.
Weijen Chang, MD, SFHM, FAAP, chief of the division of pediatric hospital medicine, Baystate Medical Center/Baystate Children’s Hospital, Springfield, Mass., said, “This is the first pediatric POCUS session offered at SHM ever. And it does not require an additional cost ... the pediatric track is critically important, as a substantial number of athlete attendees are either Peds or MedPeds. I think SHM aims to create a pediatric track that discusses topics that are less covered in other meetings, such as the value equation and issues facing women leaders in HM.”
6. “Foundations of a Hospital Medicine Telemedicine Program” – Wednesday, May 3; 415 p.m.–5:20 p.m.
Dr. Villagra added, “Telemedicine is a new innovative technology with the promise of overcoming geographical barriers to health care providers. A lot of new companies and software development has made this technology more user/patient friendly.”
7. “Hot Topics in Health Policy for Hospitalists” – Thursday, May 4; 7:40 a.m.–8:35 a.m.
8. “The Impact of the New Administration on Health Care Reform” – Thursday, May 4; 8:45 a.m.–9:40 a.m.
9. “Health Care Payment Reform for Hospitalist 2017: Tips for MIPS and Beyond” – Thursday, May 4; 9:50 a.m.–10:45 a.m.
Dr. Stella said, “As a safety-net hospitalist in Colorado, a state which largely expanded Medicare under the Affordable Care Act (ACA), I am concerned about the impact repealing the ACA would have on my patients as well as on safety-net hospitals such as my own. I hope that these sessions will increase my understanding of the issues and my ability to advocate for my patients.”
Dr. Cook said, “The U.S. government is functioning in historically unprecedented ways with major shifts in health care policy expected to occur over the next 4 years. It is essential that physician leaders play an active role in shaping the discussion around these important topics ... hospitalists have an opportunity to provide leadership in this arena, and these sessions will help participants to build the knowledge about these complex issues that is crucial to being an active part of the dialogue.”
10. “Workshop: Hospitalists as Leaders in Patient Flow and Hospital Throughput” – Thursday, May 4; 10 a.m.–11:30 a.m.
Dr. Stella said, “Recently, I was appointed to a leadership role on a major initiative to improve hospital patient flow at my institution. We are concentrating on several different areas, including avoidable hospitalizations, preventable excess days, delayed discharges, and variable access to services. I was excited to see a workshop this year dedicated to how hospitalists can successfully lead such initiatives. I will definitely be attending this session as I am interested in what others are doing in their institutions to creatively overcome patient flow challenges.”
11. “Hospitalist Careers: So Many Options” – Tuesday, May 2; 10:35 a.m.–11:15 a.m.
Dr. Villagra said, “Hospital medicine has so many pathways for a full career development and is not a pit stop before fellowship. Early- and mid-career hospitalists can benefit from interactions with senior hospitalists for the understanding of what hospital medicine has to offer for their professional growth.”
Richard Quinn is a freelance writer in New Jersey.
Fellows and Awards of Excellence
Vineet Arora, MD, understands the unique value of being named one of this year’s three Masters in Hospital Medicine. It’s an honor bestowed for hospitalists, by hospitalists.
“I take a lot of pride in an honor determined by peers,” said Dr. Arora, an academic hospitalist at University of Chicago Medicine. “While peers are often the biggest support you receive in your professional career, because they are in the trenches with you, they can also be your best critics. That is especially true of the type of work that I do, which relies on the buy-in of frontline clinicians – including hospitalists and trainees – to achieve better patient care and education.”
The designation of new Masters in Hospital Medicine is a major moment at SHM’s annual meeting. The 2017 list of awardees is headlined by Dr. Arora and the other MHM designees: former SHM President Burke Kealey, MD, and Richard Slataper, MD, who was heavily involved with the National Association of Inpatient Physicians, a predecessor to SHM. The three new masters bring to 24 the number of MHMs the society has named since unveiling the honor in 2010.
Dr. Arora understands that after 20 years as a specialty, just two dozen practitioners have reached hospital medicine’s highest professional distinction.
“I think of ‘mastery’ as someone who has achieved the highest level of expertise in a field, so an honor like Master in Hospital Medicine definitely means a lot to me,” she said. “Especially given the prior recipients of this honor, and the importance of SHM in my own professional growth and development since I was a trainee.”
In addition to the top honor, HM17 will see the induction of 159 Fellows in Hospital Medicine (FHM) and 58 Senior Fellows in Hospital Medicine (SFHM). This year’s fellows join the thousands of physicians and nonphysician providers (NPPs) that have attained the distinction.
SHM also bestows its annual Awards of Excellence (past winners listed here include Dr. Arora and Dr. Kealey) that recognize practitioners across skill sets. The awards are meant to honor SHM members “whose exemplary contributions to the hospital medicine movement deserve acknowledgment and respect,” according to the society’s website.
The 2017 Award winners include:
• Excellence in Teamwork in Quality Improvement: Johnston Memorial Hospital in Abingdon, Va.
• Excellence in Research: Jeffrey Barsuk, MD, MS, SFHM.
• Excellence in Teaching: Steven Cohn, MD, FACP, SFHM.
• Excellence in Hospital Medicine for Non-Physicians: Michael McFall.
• Outstanding Service in Hospital Medicine: Jeffrey Greenwald, MD, SFHM.
• Clinical Excellence: Barbara Slawski, MD.
• Excellence in Humanitarian Services: Jonathan Crocker, MD, FHM.
Dr. Arora, who has served on the SHM committee that analyzes all nominees for the annual awards, recognizes the value of honoring these high-achieving clinicians.
“There is great value to having our specialty society recognize members in different ways,” she said “The awards of excellence serve as a wonderful reminder of the incredible impact that hospitalists have in many diverse ways … while having the distinction of a fellow or senior fellow serves as a nice benchmark to which new hospitalists can aspire and gain recognition as they emerge as leaders in the field.”
Vineet Arora, MD, understands the unique value of being named one of this year’s three Masters in Hospital Medicine. It’s an honor bestowed for hospitalists, by hospitalists.
“I take a lot of pride in an honor determined by peers,” said Dr. Arora, an academic hospitalist at University of Chicago Medicine. “While peers are often the biggest support you receive in your professional career, because they are in the trenches with you, they can also be your best critics. That is especially true of the type of work that I do, which relies on the buy-in of frontline clinicians – including hospitalists and trainees – to achieve better patient care and education.”
The designation of new Masters in Hospital Medicine is a major moment at SHM’s annual meeting. The 2017 list of awardees is headlined by Dr. Arora and the other MHM designees: former SHM President Burke Kealey, MD, and Richard Slataper, MD, who was heavily involved with the National Association of Inpatient Physicians, a predecessor to SHM. The three new masters bring to 24 the number of MHMs the society has named since unveiling the honor in 2010.
Dr. Arora understands that after 20 years as a specialty, just two dozen practitioners have reached hospital medicine’s highest professional distinction.
“I think of ‘mastery’ as someone who has achieved the highest level of expertise in a field, so an honor like Master in Hospital Medicine definitely means a lot to me,” she said. “Especially given the prior recipients of this honor, and the importance of SHM in my own professional growth and development since I was a trainee.”
In addition to the top honor, HM17 will see the induction of 159 Fellows in Hospital Medicine (FHM) and 58 Senior Fellows in Hospital Medicine (SFHM). This year’s fellows join the thousands of physicians and nonphysician providers (NPPs) that have attained the distinction.
SHM also bestows its annual Awards of Excellence (past winners listed here include Dr. Arora and Dr. Kealey) that recognize practitioners across skill sets. The awards are meant to honor SHM members “whose exemplary contributions to the hospital medicine movement deserve acknowledgment and respect,” according to the society’s website.
The 2017 Award winners include:
• Excellence in Teamwork in Quality Improvement: Johnston Memorial Hospital in Abingdon, Va.
• Excellence in Research: Jeffrey Barsuk, MD, MS, SFHM.
• Excellence in Teaching: Steven Cohn, MD, FACP, SFHM.
• Excellence in Hospital Medicine for Non-Physicians: Michael McFall.
• Outstanding Service in Hospital Medicine: Jeffrey Greenwald, MD, SFHM.
• Clinical Excellence: Barbara Slawski, MD.
• Excellence in Humanitarian Services: Jonathan Crocker, MD, FHM.
Dr. Arora, who has served on the SHM committee that analyzes all nominees for the annual awards, recognizes the value of honoring these high-achieving clinicians.
“There is great value to having our specialty society recognize members in different ways,” she said “The awards of excellence serve as a wonderful reminder of the incredible impact that hospitalists have in many diverse ways … while having the distinction of a fellow or senior fellow serves as a nice benchmark to which new hospitalists can aspire and gain recognition as they emerge as leaders in the field.”
Vineet Arora, MD, understands the unique value of being named one of this year’s three Masters in Hospital Medicine. It’s an honor bestowed for hospitalists, by hospitalists.
“I take a lot of pride in an honor determined by peers,” said Dr. Arora, an academic hospitalist at University of Chicago Medicine. “While peers are often the biggest support you receive in your professional career, because they are in the trenches with you, they can also be your best critics. That is especially true of the type of work that I do, which relies on the buy-in of frontline clinicians – including hospitalists and trainees – to achieve better patient care and education.”
The designation of new Masters in Hospital Medicine is a major moment at SHM’s annual meeting. The 2017 list of awardees is headlined by Dr. Arora and the other MHM designees: former SHM President Burke Kealey, MD, and Richard Slataper, MD, who was heavily involved with the National Association of Inpatient Physicians, a predecessor to SHM. The three new masters bring to 24 the number of MHMs the society has named since unveiling the honor in 2010.
Dr. Arora understands that after 20 years as a specialty, just two dozen practitioners have reached hospital medicine’s highest professional distinction.
“I think of ‘mastery’ as someone who has achieved the highest level of expertise in a field, so an honor like Master in Hospital Medicine definitely means a lot to me,” she said. “Especially given the prior recipients of this honor, and the importance of SHM in my own professional growth and development since I was a trainee.”
In addition to the top honor, HM17 will see the induction of 159 Fellows in Hospital Medicine (FHM) and 58 Senior Fellows in Hospital Medicine (SFHM). This year’s fellows join the thousands of physicians and nonphysician providers (NPPs) that have attained the distinction.
SHM also bestows its annual Awards of Excellence (past winners listed here include Dr. Arora and Dr. Kealey) that recognize practitioners across skill sets. The awards are meant to honor SHM members “whose exemplary contributions to the hospital medicine movement deserve acknowledgment and respect,” according to the society’s website.
The 2017 Award winners include:
• Excellence in Teamwork in Quality Improvement: Johnston Memorial Hospital in Abingdon, Va.
• Excellence in Research: Jeffrey Barsuk, MD, MS, SFHM.
• Excellence in Teaching: Steven Cohn, MD, FACP, SFHM.
• Excellence in Hospital Medicine for Non-Physicians: Michael McFall.
• Outstanding Service in Hospital Medicine: Jeffrey Greenwald, MD, SFHM.
• Clinical Excellence: Barbara Slawski, MD.
• Excellence in Humanitarian Services: Jonathan Crocker, MD, FHM.
Dr. Arora, who has served on the SHM committee that analyzes all nominees for the annual awards, recognizes the value of honoring these high-achieving clinicians.
“There is great value to having our specialty society recognize members in different ways,” she said “The awards of excellence serve as a wonderful reminder of the incredible impact that hospitalists have in many diverse ways … while having the distinction of a fellow or senior fellow serves as a nice benchmark to which new hospitalists can aspire and gain recognition as they emerge as leaders in the field.”
Networking: A skill worth learning
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
Tips for significant others
Heather Howell has gotten pretty good at making the most out of SHM’s annual meeting. It’s not that she has a system for wending through scores of educational offerings, a knack for interpersonal networking or award-winning research.
It’s that she’s the spouse of former SHM President Eric Howell, MD, MHM, and a long-time annual meeting attendee with her husband.
Welcome to HM17, family style. While thousands of hospitalists, nonphysician practitioners, and other attendees swarm the Mandalay Bay Resort and Casino for a four-day crash course on all things hospital medicine, thousands more family members tag along. Husbands and wives, like Mrs. Howell, and, in years past, children like the Howells’ 14-year-old son Mason and 12-year-old daughter Anna. The kids aren’t traveling this year, which is tip No. 1.
“It gets harder as they’re older to drag them to San Diego or Vegas in the middle of a school year, which is when [the annual meeting] is usually held,” said Mrs. Howell, whose day job is as a real estate agent.
Tip No. 2? Make friends the first time around. Maybe it’s with spouses of other physicians from your significant other’s practice. Or maybe it’s with your spouse’s old friends from past jobs. For Mrs. Howell, it’s SHM staff and the families of board members her husband has worked with for years.
“I’ve been doing it for so long that I’ve met a lot of the other [spouses] that do go,” she said. “Usually, if Eric is in meetings all day, I will connect with some of the other spouses and we will go on excursions that are in that town. There is usually so much going on.”
Las Vegas is certainly no exception. In fact, SHM has a dedicated web page recommending family activities. Recommendations include hanging out at the 11-acre Mandalay Beach, which encompasses 2,700 tons of sand, three pools and a lazy river. There’s also the popular Shark Reef Aquarium, a 1.6 million-gallon saltwater habitat with some 2,000 creatures.
Mrs. Howell says excursions further afield could include Red Rock Canyon National Conservation Area, which lies a 25-minute drive from the convention, or the Grand Canyon, which is about two hours east. But planning too much, especially with children, can become a challenge.
“When I arrive, there always seems to be a group of people that are going to do things,” Mrs. Howell said. “It’s very easy to hook up with the other spouses that aren’t involved in the meeting. We always tend to find each other.”
Heather Howell has gotten pretty good at making the most out of SHM’s annual meeting. It’s not that she has a system for wending through scores of educational offerings, a knack for interpersonal networking or award-winning research.
It’s that she’s the spouse of former SHM President Eric Howell, MD, MHM, and a long-time annual meeting attendee with her husband.
Welcome to HM17, family style. While thousands of hospitalists, nonphysician practitioners, and other attendees swarm the Mandalay Bay Resort and Casino for a four-day crash course on all things hospital medicine, thousands more family members tag along. Husbands and wives, like Mrs. Howell, and, in years past, children like the Howells’ 14-year-old son Mason and 12-year-old daughter Anna. The kids aren’t traveling this year, which is tip No. 1.
“It gets harder as they’re older to drag them to San Diego or Vegas in the middle of a school year, which is when [the annual meeting] is usually held,” said Mrs. Howell, whose day job is as a real estate agent.
Tip No. 2? Make friends the first time around. Maybe it’s with spouses of other physicians from your significant other’s practice. Or maybe it’s with your spouse’s old friends from past jobs. For Mrs. Howell, it’s SHM staff and the families of board members her husband has worked with for years.
“I’ve been doing it for so long that I’ve met a lot of the other [spouses] that do go,” she said. “Usually, if Eric is in meetings all day, I will connect with some of the other spouses and we will go on excursions that are in that town. There is usually so much going on.”
Las Vegas is certainly no exception. In fact, SHM has a dedicated web page recommending family activities. Recommendations include hanging out at the 11-acre Mandalay Beach, which encompasses 2,700 tons of sand, three pools and a lazy river. There’s also the popular Shark Reef Aquarium, a 1.6 million-gallon saltwater habitat with some 2,000 creatures.
Mrs. Howell says excursions further afield could include Red Rock Canyon National Conservation Area, which lies a 25-minute drive from the convention, or the Grand Canyon, which is about two hours east. But planning too much, especially with children, can become a challenge.
“When I arrive, there always seems to be a group of people that are going to do things,” Mrs. Howell said. “It’s very easy to hook up with the other spouses that aren’t involved in the meeting. We always tend to find each other.”
Heather Howell has gotten pretty good at making the most out of SHM’s annual meeting. It’s not that she has a system for wending through scores of educational offerings, a knack for interpersonal networking or award-winning research.
It’s that she’s the spouse of former SHM President Eric Howell, MD, MHM, and a long-time annual meeting attendee with her husband.
Welcome to HM17, family style. While thousands of hospitalists, nonphysician practitioners, and other attendees swarm the Mandalay Bay Resort and Casino for a four-day crash course on all things hospital medicine, thousands more family members tag along. Husbands and wives, like Mrs. Howell, and, in years past, children like the Howells’ 14-year-old son Mason and 12-year-old daughter Anna. The kids aren’t traveling this year, which is tip No. 1.
“It gets harder as they’re older to drag them to San Diego or Vegas in the middle of a school year, which is when [the annual meeting] is usually held,” said Mrs. Howell, whose day job is as a real estate agent.
Tip No. 2? Make friends the first time around. Maybe it’s with spouses of other physicians from your significant other’s practice. Or maybe it’s with your spouse’s old friends from past jobs. For Mrs. Howell, it’s SHM staff and the families of board members her husband has worked with for years.
“I’ve been doing it for so long that I’ve met a lot of the other [spouses] that do go,” she said. “Usually, if Eric is in meetings all day, I will connect with some of the other spouses and we will go on excursions that are in that town. There is usually so much going on.”
Las Vegas is certainly no exception. In fact, SHM has a dedicated web page recommending family activities. Recommendations include hanging out at the 11-acre Mandalay Beach, which encompasses 2,700 tons of sand, three pools and a lazy river. There’s also the popular Shark Reef Aquarium, a 1.6 million-gallon saltwater habitat with some 2,000 creatures.
Mrs. Howell says excursions further afield could include Red Rock Canyon National Conservation Area, which lies a 25-minute drive from the convention, or the Grand Canyon, which is about two hours east. But planning too much, especially with children, can become a challenge.
“When I arrive, there always seems to be a group of people that are going to do things,” Mrs. Howell said. “It’s very easy to hook up with the other spouses that aren’t involved in the meeting. We always tend to find each other.”
HM17: Plenaries – Conway and DeSalvo
The first two plenary addresses at HM17 are focused on policy at a time when the dynamically evolving U.S. health care delivery system may seem daunting, opaque, and labyrinthine.
Some might view the health care landscape as hopelessly confusing. Yet both of the keynote speakers use the same word for what they hope to leave their listeners with: optimism.
“Though it feels uncertain in the headlines, the reality is that the health care world feels pretty united in that we need to continue the progress we’ve made on moving away from the fee-for-service model and to let people practice medicine the way they want – to work better as teams and focus on patients and outcomes,” said Karen DeSalvo, MD, MPH, MSc, former acting assistant secretary for health in the U.S. Department of Health and Human Services (HHS) and former national coordinator for health information technology.
“I would view it as an opportunity as well,” said Dr. Conway, who still moonlights as a pediatric academic hospitalist on weekends in greater Washington, D.C. “I think the pieces are coming together. Everything from data, to new payment models, to the MACRA Medicare Physician payment legislation, really suggests a time of positive change.”
Dr. DeSalvo, a former political appointee, joined HHS as the national coordinator for health information technology in 2014 and soon thereafter assumed the acting assistant secretary role. Dr. Conway has attained one of the country’s highest-ranking public health care jobs since joining CMS in 2011. He retained the top post at CMS while President Donald Trump’s nominee to lead the agency, Seema Verma, awaited a confirmation hearing before the U.S. Senate. Dr. Conway’s prior title was principal deputy administrator and CMS chief medical officer.
“I don’t want people to lose sight of the fact that there’s this entire care system that everybody’s working and innovating in every day, trying to find more efficient, effective ways to get better outcomes,” she said. “Hospitalists, quite frankly, have been leading that for their entire existence. They really understand in great granular detail what it takes.”
Dr. DeSalvo believes that the progress of the past 5 years has established a path that must be followed. The public sector move away from fee-for-service has combined with emerging technology platforms to create a new age where physicians and insurers can judge, in real time, how well care is working.
“We’re now in a feedback loop where we can say – ‘When we’ve built a care system like this or when we pay this way, we are actually seeing improved outcomes’ – and change doesn’t take as long,” Dr. DeSalvo said.
Dr. Conway, whose working title for his speech is “Health care System Transformation,” said hospitalists should be encouraged by how well the field has already adapted to the proliferation of accountable care organizations (ACOs), value-based purchasing (VBP), alternative payment models (APM), and the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015. He noted that, as innovations lead to better and more coordinated patient care, hospitalists, patients, and hospitals would all benefit.
“I want to leave people with the idea that value-based payment innovation and delivery system reform will continue to be critical aspects of improving our health system,” he said. “I also want hospitalists to continue to stay engaged with these new payment models, help lead them, and provide better patient care as a part of them.”
The first two plenary addresses at HM17 are focused on policy at a time when the dynamically evolving U.S. health care delivery system may seem daunting, opaque, and labyrinthine.
Some might view the health care landscape as hopelessly confusing. Yet both of the keynote speakers use the same word for what they hope to leave their listeners with: optimism.
“Though it feels uncertain in the headlines, the reality is that the health care world feels pretty united in that we need to continue the progress we’ve made on moving away from the fee-for-service model and to let people practice medicine the way they want – to work better as teams and focus on patients and outcomes,” said Karen DeSalvo, MD, MPH, MSc, former acting assistant secretary for health in the U.S. Department of Health and Human Services (HHS) and former national coordinator for health information technology.
“I would view it as an opportunity as well,” said Dr. Conway, who still moonlights as a pediatric academic hospitalist on weekends in greater Washington, D.C. “I think the pieces are coming together. Everything from data, to new payment models, to the MACRA Medicare Physician payment legislation, really suggests a time of positive change.”
Dr. DeSalvo, a former political appointee, joined HHS as the national coordinator for health information technology in 2014 and soon thereafter assumed the acting assistant secretary role. Dr. Conway has attained one of the country’s highest-ranking public health care jobs since joining CMS in 2011. He retained the top post at CMS while President Donald Trump’s nominee to lead the agency, Seema Verma, awaited a confirmation hearing before the U.S. Senate. Dr. Conway’s prior title was principal deputy administrator and CMS chief medical officer.
“I don’t want people to lose sight of the fact that there’s this entire care system that everybody’s working and innovating in every day, trying to find more efficient, effective ways to get better outcomes,” she said. “Hospitalists, quite frankly, have been leading that for their entire existence. They really understand in great granular detail what it takes.”
Dr. DeSalvo believes that the progress of the past 5 years has established a path that must be followed. The public sector move away from fee-for-service has combined with emerging technology platforms to create a new age where physicians and insurers can judge, in real time, how well care is working.
“We’re now in a feedback loop where we can say – ‘When we’ve built a care system like this or when we pay this way, we are actually seeing improved outcomes’ – and change doesn’t take as long,” Dr. DeSalvo said.
Dr. Conway, whose working title for his speech is “Health care System Transformation,” said hospitalists should be encouraged by how well the field has already adapted to the proliferation of accountable care organizations (ACOs), value-based purchasing (VBP), alternative payment models (APM), and the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015. He noted that, as innovations lead to better and more coordinated patient care, hospitalists, patients, and hospitals would all benefit.
“I want to leave people with the idea that value-based payment innovation and delivery system reform will continue to be critical aspects of improving our health system,” he said. “I also want hospitalists to continue to stay engaged with these new payment models, help lead them, and provide better patient care as a part of them.”
The first two plenary addresses at HM17 are focused on policy at a time when the dynamically evolving U.S. health care delivery system may seem daunting, opaque, and labyrinthine.
Some might view the health care landscape as hopelessly confusing. Yet both of the keynote speakers use the same word for what they hope to leave their listeners with: optimism.
“Though it feels uncertain in the headlines, the reality is that the health care world feels pretty united in that we need to continue the progress we’ve made on moving away from the fee-for-service model and to let people practice medicine the way they want – to work better as teams and focus on patients and outcomes,” said Karen DeSalvo, MD, MPH, MSc, former acting assistant secretary for health in the U.S. Department of Health and Human Services (HHS) and former national coordinator for health information technology.
“I would view it as an opportunity as well,” said Dr. Conway, who still moonlights as a pediatric academic hospitalist on weekends in greater Washington, D.C. “I think the pieces are coming together. Everything from data, to new payment models, to the MACRA Medicare Physician payment legislation, really suggests a time of positive change.”
Dr. DeSalvo, a former political appointee, joined HHS as the national coordinator for health information technology in 2014 and soon thereafter assumed the acting assistant secretary role. Dr. Conway has attained one of the country’s highest-ranking public health care jobs since joining CMS in 2011. He retained the top post at CMS while President Donald Trump’s nominee to lead the agency, Seema Verma, awaited a confirmation hearing before the U.S. Senate. Dr. Conway’s prior title was principal deputy administrator and CMS chief medical officer.
“I don’t want people to lose sight of the fact that there’s this entire care system that everybody’s working and innovating in every day, trying to find more efficient, effective ways to get better outcomes,” she said. “Hospitalists, quite frankly, have been leading that for their entire existence. They really understand in great granular detail what it takes.”
Dr. DeSalvo believes that the progress of the past 5 years has established a path that must be followed. The public sector move away from fee-for-service has combined with emerging technology platforms to create a new age where physicians and insurers can judge, in real time, how well care is working.
“We’re now in a feedback loop where we can say – ‘When we’ve built a care system like this or when we pay this way, we are actually seeing improved outcomes’ – and change doesn’t take as long,” Dr. DeSalvo said.
Dr. Conway, whose working title for his speech is “Health care System Transformation,” said hospitalists should be encouraged by how well the field has already adapted to the proliferation of accountable care organizations (ACOs), value-based purchasing (VBP), alternative payment models (APM), and the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015. He noted that, as innovations lead to better and more coordinated patient care, hospitalists, patients, and hospitals would all benefit.
“I want to leave people with the idea that value-based payment innovation and delivery system reform will continue to be critical aspects of improving our health system,” he said. “I also want hospitalists to continue to stay engaged with these new payment models, help lead them, and provide better patient care as a part of them.”