User login
Dispensing with expert testimony
Question: When a doctor could not find a dislodged biopsy guide wire, he abandoned his search after informing the patient of his intention to retrieve it at a later date. Two months later, he was successful in locating and removing the foreign body, but the patient alleged she suffered pain and anxiety in the interim. She filed a negligence lawsuit and, based on the “obvious” nature of her injuries, called no expert witness to testify on her behalf.
Which of the following choices is best?
A. Expert testimony is always needed to establish the applicable standard of care in medical negligence lawsuits.
B. Although a plaintiff is not qualified to expound on medical matters, he/she can offer evidence from learned treatises and medical texts.
C. The jury is the one who determines whether a plaintiff can invoke either the res ipsa loquitur doctrine or the “common knowledge” rule to obviate the need for an expert witness.
D. This patient will likely win her case.
E. All are incorrect.
Answer: E. It is well-established law that the question of negligence must be decided by reference to relevant medical standards of care for which the plaintiff carries the burden of proving through expert medical testimony. Only a professional, duly qualified by the court as an expert witness, is allowed to offer medical testimony – whereas the plaintiff typically will be disqualified from playing this role because of the complexity of issues involved.
However, under either the doctrine of res ipsa loquitur (“the thing speaks for itself”) or the “common knowledge” rule, a court (i.e., the judge) may allow the jury to infer negligence in the absence of expert testimony.
The res doctrine is invoked where there is only circumstantial but no direct evidence, and three conditions are met: 1) The injury would not have occurred in the absence of someone’s negligence; 2) the plaintiff was not at fault; and 3) the defendant had total control of the instrumentality that led to the injury.
The closely related “common knowledge” rule relies on the everyday knowledge and experience of the layperson to identify plain and obvious negligent conduct, which then allows the judge to waive the expert requirement.
The two principles are frequently used interchangeably, ultimately favoring the plaintiff by dispensing with the difficult and expensive task of securing a qualified expert willing to testify against a doctor defendant.
The best example of res in action is the surgeon who inadvertently leaves behind a sponge or instrument inside a body cavity. Other successfully litigated examples include a cardiac arrest in the operating room, hypoxia in the recovery room, burns to the buttock, gangrene after the accidental injection of penicillin into an artery, air trapped subcutaneously from a displaced needle, and a pierced eyeball during a procedure.
A particularly well-known example is Ybarra v. Spangard, in which the patient developed shoulder injuries during an appendectomy.1 The Supreme Court of California felt it was appropriate to place the burden on the operating room defendants to explain how the patient, unconscious under general anesthesia throughout the procedure, sustained the shoulder injury.
The scenario provided in the opening question is taken from a 2013 New York case, James v. Wormuth, in which the plaintiff relied on the res doctrine.2 The defendant doctor had left a guide wire in the plaintiff’s chest following a biopsy and was unable to locate it after a 20-minute search. However, he was able to retrieve the wire 2 months later under C-arm imaging.
The plaintiff sued the doctor for pain and anxiety, but did not call any expert witness, relying instead on the “foreign object” basis for invoking the res doctrine. The lower court ruled for the doctor, and the court of appeals affirmed.
It reasoned that the object was left behind deliberately, not unintentionally, and that under the circumstances of the case, an expert witness was needed to set out the applicable standard of care, without which a jury could not determine whether the doctor’s professional judgment breached the requisite standard. The court also ruled that the plaintiff failed to satisfy the “exclusive control” requirement of the res doctrine, because several other individuals participated to an extent in the medical procedure.
Hawaii’s case of Barbee v. Queen’s Medical Center is illustrative of the “common knowledge” rule.3 Mr. Barbee, age 75 years, underwent laparoscopic nephrectomy for a malignancy. Massive bleeding complicated his postoperative course, the hemoglobin falling into the 3 range, and he required emergent reoperation. Over the next 18 months, the patient progressively deteriorated, eventually requiring dialysis and dying from a stroke and intestinal volvulus.
Notwithstanding an initial jury verdict in favor of the plaintiff’s children, awarding each of the three children $365,000, the defendants filed a so-called JNOV motion (current term is “judgment as a matter of law”) to negate the jury verdict, on the basis that the plaintiffs failed to present competent expert testimony at trial to prove causation.
The plaintiffs countered that the cause of death was within the realm of common knowledge, thus no expert was necessary. They asserted that “any lay person can easily grasp the concept that a person dies from losing so much blood that multiple organs fail to perform their functions.” Mr. Barbee’s death thus was not “of such a technical nature that lay persons are incompetent to draw their own conclusions from facts presented without aid.”
Hawaii’s Intermediate Court of Appeals disagreed with the plaintiffs, holding that although “Hawaii does recognize a ‘common knowledge’ exception to the requirement that a plaintiff must introduce expert medical testimony on causation … this exception is rare in application.” The court asserted that the causal link between any alleged negligence and Mr. Barbee’s death 17 months later is not within the realm of common knowledge.
It reasoned that the long-term effects of internal bleeding are not so widely known as to be analogous to leaving a sponge within a patient or removing the wrong limb during an amputation. Moreover, Mr. Barbee had a long history of preexisting conditions, including hypertension, diabetes, and cancer. He also suffered numerous and serious postoperative medical conditions, including a stroke and surgery to remove part of his intestine, which had become gangrenous.
Thus, the role that preexisting conditions and/or the subsequent complications of this type played in Mr. Barbee’s death was not within the knowledge of the average layperson.
The “common knowledge” rule is aligned with, though not identical to, the res doctrine, but courts are known to conflate the two legal principles, often using them interchangeably.4
Strictly speaking, the “common knowledge” waiver comes into play where direct evidence of negligent conduct lies within the realm of everyday lay knowledge that the physician had deviated from common practice. It may or may not address the causation issue.
On the other hand, res is successfully invoked when, despite no direct evidence of negligence and causation, the circumstances surrounding the injury are such that the plaintiff’s case can go to the jury without expert testimony.
References
1. Ybarra v. Spangard, 154 P.2d 687 (Cal. 1944).
2. James v. Wormuth, 997 N.E.2d 133 (N.Y. 2013).
3. Barbee v. Queen’s Medical Center, 119 Haw 136 (2008).
4. Spinner, Amanda E. Common Ignorance: Medical Malpractice Law and the Misconceived Application of the “Common Knowledge” and “Res Ipsa Loquitur” Doctrines.” Touro Law Review: Vol. 31: No. 3, Article 15. Available at http://digitalcommons.tourolaw.edu/lawreview/vol31/iss3/15.
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: When a doctor could not find a dislodged biopsy guide wire, he abandoned his search after informing the patient of his intention to retrieve it at a later date. Two months later, he was successful in locating and removing the foreign body, but the patient alleged she suffered pain and anxiety in the interim. She filed a negligence lawsuit and, based on the “obvious” nature of her injuries, called no expert witness to testify on her behalf.
Which of the following choices is best?
A. Expert testimony is always needed to establish the applicable standard of care in medical negligence lawsuits.
B. Although a plaintiff is not qualified to expound on medical matters, he/she can offer evidence from learned treatises and medical texts.
C. The jury is the one who determines whether a plaintiff can invoke either the res ipsa loquitur doctrine or the “common knowledge” rule to obviate the need for an expert witness.
D. This patient will likely win her case.
E. All are incorrect.
Answer: E. It is well-established law that the question of negligence must be decided by reference to relevant medical standards of care for which the plaintiff carries the burden of proving through expert medical testimony. Only a professional, duly qualified by the court as an expert witness, is allowed to offer medical testimony – whereas the plaintiff typically will be disqualified from playing this role because of the complexity of issues involved.
However, under either the doctrine of res ipsa loquitur (“the thing speaks for itself”) or the “common knowledge” rule, a court (i.e., the judge) may allow the jury to infer negligence in the absence of expert testimony.
The res doctrine is invoked where there is only circumstantial but no direct evidence, and three conditions are met: 1) The injury would not have occurred in the absence of someone’s negligence; 2) the plaintiff was not at fault; and 3) the defendant had total control of the instrumentality that led to the injury.
The closely related “common knowledge” rule relies on the everyday knowledge and experience of the layperson to identify plain and obvious negligent conduct, which then allows the judge to waive the expert requirement.
The two principles are frequently used interchangeably, ultimately favoring the plaintiff by dispensing with the difficult and expensive task of securing a qualified expert willing to testify against a doctor defendant.
The best example of res in action is the surgeon who inadvertently leaves behind a sponge or instrument inside a body cavity. Other successfully litigated examples include a cardiac arrest in the operating room, hypoxia in the recovery room, burns to the buttock, gangrene after the accidental injection of penicillin into an artery, air trapped subcutaneously from a displaced needle, and a pierced eyeball during a procedure.
A particularly well-known example is Ybarra v. Spangard, in which the patient developed shoulder injuries during an appendectomy.1 The Supreme Court of California felt it was appropriate to place the burden on the operating room defendants to explain how the patient, unconscious under general anesthesia throughout the procedure, sustained the shoulder injury.
The scenario provided in the opening question is taken from a 2013 New York case, James v. Wormuth, in which the plaintiff relied on the res doctrine.2 The defendant doctor had left a guide wire in the plaintiff’s chest following a biopsy and was unable to locate it after a 20-minute search. However, he was able to retrieve the wire 2 months later under C-arm imaging.
The plaintiff sued the doctor for pain and anxiety, but did not call any expert witness, relying instead on the “foreign object” basis for invoking the res doctrine. The lower court ruled for the doctor, and the court of appeals affirmed.
It reasoned that the object was left behind deliberately, not unintentionally, and that under the circumstances of the case, an expert witness was needed to set out the applicable standard of care, without which a jury could not determine whether the doctor’s professional judgment breached the requisite standard. The court also ruled that the plaintiff failed to satisfy the “exclusive control” requirement of the res doctrine, because several other individuals participated to an extent in the medical procedure.
Hawaii’s case of Barbee v. Queen’s Medical Center is illustrative of the “common knowledge” rule.3 Mr. Barbee, age 75 years, underwent laparoscopic nephrectomy for a malignancy. Massive bleeding complicated his postoperative course, the hemoglobin falling into the 3 range, and he required emergent reoperation. Over the next 18 months, the patient progressively deteriorated, eventually requiring dialysis and dying from a stroke and intestinal volvulus.
Notwithstanding an initial jury verdict in favor of the plaintiff’s children, awarding each of the three children $365,000, the defendants filed a so-called JNOV motion (current term is “judgment as a matter of law”) to negate the jury verdict, on the basis that the plaintiffs failed to present competent expert testimony at trial to prove causation.
The plaintiffs countered that the cause of death was within the realm of common knowledge, thus no expert was necessary. They asserted that “any lay person can easily grasp the concept that a person dies from losing so much blood that multiple organs fail to perform their functions.” Mr. Barbee’s death thus was not “of such a technical nature that lay persons are incompetent to draw their own conclusions from facts presented without aid.”
Hawaii’s Intermediate Court of Appeals disagreed with the plaintiffs, holding that although “Hawaii does recognize a ‘common knowledge’ exception to the requirement that a plaintiff must introduce expert medical testimony on causation … this exception is rare in application.” The court asserted that the causal link between any alleged negligence and Mr. Barbee’s death 17 months later is not within the realm of common knowledge.
It reasoned that the long-term effects of internal bleeding are not so widely known as to be analogous to leaving a sponge within a patient or removing the wrong limb during an amputation. Moreover, Mr. Barbee had a long history of preexisting conditions, including hypertension, diabetes, and cancer. He also suffered numerous and serious postoperative medical conditions, including a stroke and surgery to remove part of his intestine, which had become gangrenous.
Thus, the role that preexisting conditions and/or the subsequent complications of this type played in Mr. Barbee’s death was not within the knowledge of the average layperson.
The “common knowledge” rule is aligned with, though not identical to, the res doctrine, but courts are known to conflate the two legal principles, often using them interchangeably.4
Strictly speaking, the “common knowledge” waiver comes into play where direct evidence of negligent conduct lies within the realm of everyday lay knowledge that the physician had deviated from common practice. It may or may not address the causation issue.
On the other hand, res is successfully invoked when, despite no direct evidence of negligence and causation, the circumstances surrounding the injury are such that the plaintiff’s case can go to the jury without expert testimony.
References
1. Ybarra v. Spangard, 154 P.2d 687 (Cal. 1944).
2. James v. Wormuth, 997 N.E.2d 133 (N.Y. 2013).
3. Barbee v. Queen’s Medical Center, 119 Haw 136 (2008).
4. Spinner, Amanda E. Common Ignorance: Medical Malpractice Law and the Misconceived Application of the “Common Knowledge” and “Res Ipsa Loquitur” Doctrines.” Touro Law Review: Vol. 31: No. 3, Article 15. Available at http://digitalcommons.tourolaw.edu/lawreview/vol31/iss3/15.
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: When a doctor could not find a dislodged biopsy guide wire, he abandoned his search after informing the patient of his intention to retrieve it at a later date. Two months later, he was successful in locating and removing the foreign body, but the patient alleged she suffered pain and anxiety in the interim. She filed a negligence lawsuit and, based on the “obvious” nature of her injuries, called no expert witness to testify on her behalf.
Which of the following choices is best?
A. Expert testimony is always needed to establish the applicable standard of care in medical negligence lawsuits.
B. Although a plaintiff is not qualified to expound on medical matters, he/she can offer evidence from learned treatises and medical texts.
C. The jury is the one who determines whether a plaintiff can invoke either the res ipsa loquitur doctrine or the “common knowledge” rule to obviate the need for an expert witness.
D. This patient will likely win her case.
E. All are incorrect.
Answer: E. It is well-established law that the question of negligence must be decided by reference to relevant medical standards of care for which the plaintiff carries the burden of proving through expert medical testimony. Only a professional, duly qualified by the court as an expert witness, is allowed to offer medical testimony – whereas the plaintiff typically will be disqualified from playing this role because of the complexity of issues involved.
However, under either the doctrine of res ipsa loquitur (“the thing speaks for itself”) or the “common knowledge” rule, a court (i.e., the judge) may allow the jury to infer negligence in the absence of expert testimony.
The res doctrine is invoked where there is only circumstantial but no direct evidence, and three conditions are met: 1) The injury would not have occurred in the absence of someone’s negligence; 2) the plaintiff was not at fault; and 3) the defendant had total control of the instrumentality that led to the injury.
The closely related “common knowledge” rule relies on the everyday knowledge and experience of the layperson to identify plain and obvious negligent conduct, which then allows the judge to waive the expert requirement.
The two principles are frequently used interchangeably, ultimately favoring the plaintiff by dispensing with the difficult and expensive task of securing a qualified expert willing to testify against a doctor defendant.
The best example of res in action is the surgeon who inadvertently leaves behind a sponge or instrument inside a body cavity. Other successfully litigated examples include a cardiac arrest in the operating room, hypoxia in the recovery room, burns to the buttock, gangrene after the accidental injection of penicillin into an artery, air trapped subcutaneously from a displaced needle, and a pierced eyeball during a procedure.
A particularly well-known example is Ybarra v. Spangard, in which the patient developed shoulder injuries during an appendectomy.1 The Supreme Court of California felt it was appropriate to place the burden on the operating room defendants to explain how the patient, unconscious under general anesthesia throughout the procedure, sustained the shoulder injury.
The scenario provided in the opening question is taken from a 2013 New York case, James v. Wormuth, in which the plaintiff relied on the res doctrine.2 The defendant doctor had left a guide wire in the plaintiff’s chest following a biopsy and was unable to locate it after a 20-minute search. However, he was able to retrieve the wire 2 months later under C-arm imaging.
The plaintiff sued the doctor for pain and anxiety, but did not call any expert witness, relying instead on the “foreign object” basis for invoking the res doctrine. The lower court ruled for the doctor, and the court of appeals affirmed.
It reasoned that the object was left behind deliberately, not unintentionally, and that under the circumstances of the case, an expert witness was needed to set out the applicable standard of care, without which a jury could not determine whether the doctor’s professional judgment breached the requisite standard. The court also ruled that the plaintiff failed to satisfy the “exclusive control” requirement of the res doctrine, because several other individuals participated to an extent in the medical procedure.
Hawaii’s case of Barbee v. Queen’s Medical Center is illustrative of the “common knowledge” rule.3 Mr. Barbee, age 75 years, underwent laparoscopic nephrectomy for a malignancy. Massive bleeding complicated his postoperative course, the hemoglobin falling into the 3 range, and he required emergent reoperation. Over the next 18 months, the patient progressively deteriorated, eventually requiring dialysis and dying from a stroke and intestinal volvulus.
Notwithstanding an initial jury verdict in favor of the plaintiff’s children, awarding each of the three children $365,000, the defendants filed a so-called JNOV motion (current term is “judgment as a matter of law”) to negate the jury verdict, on the basis that the plaintiffs failed to present competent expert testimony at trial to prove causation.
The plaintiffs countered that the cause of death was within the realm of common knowledge, thus no expert was necessary. They asserted that “any lay person can easily grasp the concept that a person dies from losing so much blood that multiple organs fail to perform their functions.” Mr. Barbee’s death thus was not “of such a technical nature that lay persons are incompetent to draw their own conclusions from facts presented without aid.”
Hawaii’s Intermediate Court of Appeals disagreed with the plaintiffs, holding that although “Hawaii does recognize a ‘common knowledge’ exception to the requirement that a plaintiff must introduce expert medical testimony on causation … this exception is rare in application.” The court asserted that the causal link between any alleged negligence and Mr. Barbee’s death 17 months later is not within the realm of common knowledge.
It reasoned that the long-term effects of internal bleeding are not so widely known as to be analogous to leaving a sponge within a patient or removing the wrong limb during an amputation. Moreover, Mr. Barbee had a long history of preexisting conditions, including hypertension, diabetes, and cancer. He also suffered numerous and serious postoperative medical conditions, including a stroke and surgery to remove part of his intestine, which had become gangrenous.
Thus, the role that preexisting conditions and/or the subsequent complications of this type played in Mr. Barbee’s death was not within the knowledge of the average layperson.
The “common knowledge” rule is aligned with, though not identical to, the res doctrine, but courts are known to conflate the two legal principles, often using them interchangeably.4
Strictly speaking, the “common knowledge” waiver comes into play where direct evidence of negligent conduct lies within the realm of everyday lay knowledge that the physician had deviated from common practice. It may or may not address the causation issue.
On the other hand, res is successfully invoked when, despite no direct evidence of negligence and causation, the circumstances surrounding the injury are such that the plaintiff’s case can go to the jury without expert testimony.
References
1. Ybarra v. Spangard, 154 P.2d 687 (Cal. 1944).
2. James v. Wormuth, 997 N.E.2d 133 (N.Y. 2013).
3. Barbee v. Queen’s Medical Center, 119 Haw 136 (2008).
4. Spinner, Amanda E. Common Ignorance: Medical Malpractice Law and the Misconceived Application of the “Common Knowledge” and “Res Ipsa Loquitur” Doctrines.” Touro Law Review: Vol. 31: No. 3, Article 15. Available at http://digitalcommons.tourolaw.edu/lawreview/vol31/iss3/15.
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Allegations: Current Trends in Medical Malpractice, Part 2
Most medical malpractice cases are still resolved in a courtroom—typically after years of preparation and personal torment. Yet, overall rates of paid medical malpractice claims among all physicians have been steadily decreasing over the past two decades, with reports showing decreases of 30% to 50% in paid claims since 2000.1-3 At the same time, while median payments and insurance premiums continued to increase until the mid-2000s, they now appear to have plateaued.1
None of these changes occurred in isolation. More than 30 states now have caps on noneconomic or total damages.2 As noted in part 1, since 2000, some states have enacted comprehensive tort reform.4 However, whether these changes in malpractice patterns can be attributed directly to specific policy changes remains a hotly contested issue.
Malpractice Risk in Emergency Medicine
To what extent do the trends in medical malpractice apply to emergency medicine (EM)? While emergency physicians’ (EPs’) perception of malpractice risk ranks higher than any other medical specialty,5 in a review of a large sample of malpractice claims from 1991 through 2005, EPs ranked in the middle among specialties with respect to annual risk of a malpractice claim.6 Moreover, the annual risk of a claim for EPs is just under 8%, compared to 7.4% for all physicians. Yet, for neurosurgery and cardiothoracic surgery—the specialties with the highest overall risk of malpractice claims—the annual risk approaches 20%.6 Regarding payout statistics, less than one-fifth of the claims against EPs resulted in payment.6 In a review of a separate insurance database of closed claims, EPs were named as the primary defendant in only 19% of cases.7
Despite the discrepancies between perceived risk and absolute risk of malpractice claims among EPs, malpractice lawsuits continue to affect the practice of EM. This is evidenced in several surveys, in which the majority of EP participants admitted to practicing “defensive medicine” by ordering tests that were felt to be unnecessary and did so in response to perceived malpractice risk.8-10 Perceived risk also accounts for the significant variation in decision-making in the ED with respect to diagnostic testing and hospitalization of patients.11 One would expect that lowering malpractice risk would result in less so-called unnecessary testing, but whether or not this is truly the case remains to be seen.
Effects of Malpractice Reform
A study by Waxman et al12 on the effects of significant malpractice tort reform in ED care in Texas, Georgia, and South Carolina found no difference in rates of imaging studies, charges, or patient admissions. Furthermore, legislation reform did not increase plaintiff onus to prove proximate “gross negligence” rather than simply a breach from “reasonably skillful and careful” medicine.12 These findings suggest that perception of malpractice risk might simply be serving as a proxy for physicians’ underlying risk tolerance, and be less subject to influence by external forces.
Areas Associated With Malpractice Risk
A number of closed-claim databases attempted to identify the characteristics of patient encounters that can lead to malpractice claims, including patient conditions and sources of error. Diagnostic errors have consistently been found to be the leading cause of malpractice claims, accounting for 28% to 65% of claims, followed by inappropriate management of medical treatment and improper performance of a procedure.7,13-16 A January 2016 benchmarking system report by CRICO Strategies found that 30% of 23,658 medical malpractice claims filed between 2009 through 2013 cited failures in communication as a factor.17 The report also revealed that among these failed communications, those that occurred between health care providers are more likely to result in payout compared to miscommunications between providers and patients.17 This report further noted 70% to 80% of claims closed without payment.7,16 Closed claims were significantly more likely to involve serious injuries or death.7,18 Leading conditions that resulted in claims include myocardial infarction, nonspecific chest pain, symptoms involving the abdomen or pelvis, appendicitis, and orthopedic injuries.7,13,16
Diagnostic Errors
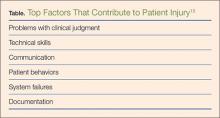
Errors in diagnosis have been attributed to multiple factors in the ED. The two most common factors were failure to order tests and failure to perform an adequate history and physical examination, both of which contribute to rationalization of the practice of defensive medicine under the current tort system.13 Other significant factors associated with errors in diagnosis include misinterpretation of test results or imaging studies and failure to obtain an appropriate consultation. Processes contributing to each of these potential errors include mistakes in judgment, lack of knowledge, miscommunication, and insufficient documentation (Table).15
Strategies for Reducing Malpractice Risk
In part 1, we listed several strategies EPs could adopt to help reduce malpractice risk. In this section, we will discuss in further detail how these strategies help mitigate malpractice claims.
Patient Communication
Open communication with patients is paramount in reducing the risk of a malpractice allegation. Patients are more likely to become angry or frustrated if they sense a physician is not listening to or addressing their concerns. These patients are in turn more likely to file a complaint if they are harmed or experience a bad outcome during their stay in the ED.
Situations in which patients are unable to provide pertinent information also place the EP at significant risk, as the provider must make decisions without full knowledge of the case. Communication with potential resources such as nursing home staff, the patient’s family, and emergency medical service providers to obtain additional information can help reduce risk.
Of course, when evaluating and treating patients, the EP should always take the time to listen to the patient’s concerns during the encounter to ensure his or her needs have been addressed. In the event of a patient allegation or complaint, the EP should make the effort to explore and de-escalate the situation before the patient is discharged.
Discharge Care and Instructions
According to CRICO, premature discharge as a factor in medical malpractice liability results from inadequate assessment and missed opportunities in 41% of diagnosis-related ED cases.16 The following situation illustrates a brief example of such a missed opportunity: A provider makes a diagnosis of urinary tract infection (UTI) in a patient presenting with fever and abdominal pain but whose urinalysis is suspect for contamination and in whom no pelvic examination was performed to rule out other etiologies. When the same patient later returns to the ED with worse abdominal pain, a sterile urine culture invalidates the diagnosis of UTI, and further evaluation leads to a final diagnosis of ruptured appendix.
Prior to discharging any patient, the EP should provide clear and concise at-home care instructions in a manner in which the patient can understand. Clear instructions on how the patient is to manage his or her care after discharge are vital, and failure to do so in terms the patient can understand can create problems if a harmful result occurs. This is especially important in patients with whom there is a communication barrier—eg, language barrier, hearing impairment, cognitive deficit, intoxication, or violent or irrational behavior. In these situations, the EP should always take advantage of available resources and tools such as language lines, interpreters, discharge planners, psychiatric staff, and supportive family members to help reconcile any communication barriers. These measures will in turn optimize patient outcome and reduce the risk of a later malpractice allegation.
Board Certification
All physicians should maintain their respective board certification and specialty training requirements. Efforts in this area help providers to stay up to date in current practice standards and new developments, thus reducing one’s risk of incurring a malpractice claim.
Patient Safety
All members of the care team should engender an environment that is focused on patient safety, including open communication between providers and with nursing staff and technical support teams. Although interruptions can be detrimental to patient care, simply having an understanding of this phenomenon among all staff members can alleviate some of the working stressors in the ED. Effort must be made to create an environment that allows for clarification between nursing staff and physicians without causing undue antagonism. Fostering supportive communication, having a questioning attitude, and seeking clarification can only enhance patient safety.
The importance of the supervisory role of attending physicians to trainees, physician extenders, and nursing staff must be emphasized, and appropriate guidance from the ED attending is germane in keeping patients safe in teaching environments. Additionally, in departments that suffer the burden of high numbers of admitted patient boarders in the ED, attention must be given to the transitional period between decision to admit and termination of ED care and the acquisition of care of the admitting physician. A clear plan of responsibility must be in place for these high-risk situations.
Policies and Procedures
Departmental policies and procedures should be designed to identify and address all late laboratory results data, radiological discrepancies, and culture results in a timely and uniform manner. Since unaddressed results and discrepancies can result in patient harm, patient-callback processes should be designed to reduce risk by addressing these hazards regularly, thoroughly, and in a timely fashion.
Cognitive Biases
An awareness of inherent biases in the medical decision-making process is also helpful to maintain mindfulness in the routine practice of EM and avoid medical errors. The EP should take care not to be influenced by recent events and diagnostic information that is easy to recall or common, and to ensure the differential addresses possibilities beyond the readily available diagnoses. Further, reliance on an existing opinion may be misleading if subsequent judgments are based on this “anchor,” whether it is true or false.
If the data points of the case do not line up as expected, or if there are unexplained outliers, the EP should expand the frame of reference to seek more appropriate possibilities, and avoid attempts to make the data fit a preferred or favored conclusion.
When one fails to recognize that data do not fit the diagnostic presumption, the true diagnosis can be undermined. Such confirmation bias in turn challenges diagnostic success. Hasty judgment without considering and seeking out relevant information can set up diagnostic failure and premature closure.
Remembering the Basics
Finally, providers should follow the basic principles for every patient. Vital signs are vital for a reason, and all abnormal data must be accounted for prior to patient hand off or discharge. Patient turnover is a high-risk occasion, and demands careful attention to case details between the off-going physician, the accepting physician, and the patient.
All patients presenting to the ED for care should leave the ED at their baseline functional level (ie, if they walk independently, they should still walk independently at discharge). If not, the reason should be sought out and clarified with appropriate recommendations for treatment and follow-up.
Patients and staff should always be treated with respect, which in turn will encourage effective communication. Providers should be honest with patients, document truthfully, respect privacy and confidentiality, practice within one’s competence, confirm information, and avoid assumptions. Compassion goes hand in hand with respectful and open communication. Physicians perceived as compassionate and trustworthy are less likely to be the target of a malpractice suit, even when harm has occurred.
Conclusion
Even though the number of paid medical malpractice claims has continued to decrease over the past 20 years, a discrepancy between perceived and absolute risk persists among EPs—one that perpetuates the practice of defensive medicine and continues to affect EM. Despite the current perceptions and climate, EPs can allay their risk of incurring a malpractice claim by employing the strategies outlined above.
1. Mello MM, Studdert DM, Kachalia A. The medical liability climate and prospects for reform. JAMA. 2014;312(20):2146-2155.
2. Paik M, Black B, Hyman DA. The receding tide of medical malpractice: part 1 - national trends. J Empirical Leg Stud. 2013;10(4):612-638.
3. Bishop TF, Ryan AM, Caslino LP. Paid malpractice claims for adverse events in inpatient and outpatient settings. JAMA. 2011;305(23):2427-2431.
4. Kachalia A, Mello MM. New directions in medical liability reform. N Engl J Med. 2011;364(16):
1564-1572.
5. Carrier ER, Reschovsky JD, Mello MM, Mayrell RC, Katz D. Physicians’ fears of malpractice lawsuits are not assured by tort reforms. Health Aff. 2010;29(9):1585-1592.
6. Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011;365(7):629-636.
7. Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010;17(5):553-560.
8. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293(21):2609-2617.
9. Bishop TF, Federman AD, Keyhani S. Physicians’ views on defensive medicine: a national survey. Arch Intern Med. 2010;170(12):1081-1083.
10. Massachusetts Medical Society. Investigation of defensive medicine in Massachusetts. November 2008. Available at http://www.massmed.org/defensivemedicine. Accessed March 16, 2016.
11. Katz DA, Williams GC, Brown RL, et al. Emergency physicians’ fear of malpractice in evaluating patient with possible acute cardiac ischemia. Ann Emerg Med. 2005;46(6):525-533.
12. Waxman DA, Greenberg MD, Ridgely MS, Kellermann AL, Heaton P. The effect of malpractice reform on emergency department care. N Engl J Med. 2014;371(16):1518-1525.
13. Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
14. Saber Tehrani AS, Lee H, Mathews SC, et al. 25-Year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672-680.
15. Ross J, Ranum D, Troxel DB. Emergency medicine closed claims study. The Doctors Company. Available at http://www.thedoctors.com/ecm/groups/public/@tdc/@web/@kc/@patientsafety/documents/article/con_id_004776.pdf. Accessed March 16, 2016.
16. Ruoff G, ed. 2011 Annual benchmarking report: malpractice risks in emergency medicine. CRICO strategies. 2012. Available at https://www.rmf.harvard.edu/Strategies/Home/Products-and-Services/Comparative-Data/Annual-Benchmark-Reports. Accessed March 16, 2016.
17. Failures in communication contribute to medical malpractice. January 31, 2016. https://www.rmf.harvard.edu/About-CRICO/Media/Press-Releases/News/2016/February/Failures-in-Communication-Contribute-to-Medical-Malpractice.
18. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024-2033. Accessed March 16, 2016.
Most medical malpractice cases are still resolved in a courtroom—typically after years of preparation and personal torment. Yet, overall rates of paid medical malpractice claims among all physicians have been steadily decreasing over the past two decades, with reports showing decreases of 30% to 50% in paid claims since 2000.1-3 At the same time, while median payments and insurance premiums continued to increase until the mid-2000s, they now appear to have plateaued.1
None of these changes occurred in isolation. More than 30 states now have caps on noneconomic or total damages.2 As noted in part 1, since 2000, some states have enacted comprehensive tort reform.4 However, whether these changes in malpractice patterns can be attributed directly to specific policy changes remains a hotly contested issue.
Malpractice Risk in Emergency Medicine
To what extent do the trends in medical malpractice apply to emergency medicine (EM)? While emergency physicians’ (EPs’) perception of malpractice risk ranks higher than any other medical specialty,5 in a review of a large sample of malpractice claims from 1991 through 2005, EPs ranked in the middle among specialties with respect to annual risk of a malpractice claim.6 Moreover, the annual risk of a claim for EPs is just under 8%, compared to 7.4% for all physicians. Yet, for neurosurgery and cardiothoracic surgery—the specialties with the highest overall risk of malpractice claims—the annual risk approaches 20%.6 Regarding payout statistics, less than one-fifth of the claims against EPs resulted in payment.6 In a review of a separate insurance database of closed claims, EPs were named as the primary defendant in only 19% of cases.7
Despite the discrepancies between perceived risk and absolute risk of malpractice claims among EPs, malpractice lawsuits continue to affect the practice of EM. This is evidenced in several surveys, in which the majority of EP participants admitted to practicing “defensive medicine” by ordering tests that were felt to be unnecessary and did so in response to perceived malpractice risk.8-10 Perceived risk also accounts for the significant variation in decision-making in the ED with respect to diagnostic testing and hospitalization of patients.11 One would expect that lowering malpractice risk would result in less so-called unnecessary testing, but whether or not this is truly the case remains to be seen.
Effects of Malpractice Reform
A study by Waxman et al12 on the effects of significant malpractice tort reform in ED care in Texas, Georgia, and South Carolina found no difference in rates of imaging studies, charges, or patient admissions. Furthermore, legislation reform did not increase plaintiff onus to prove proximate “gross negligence” rather than simply a breach from “reasonably skillful and careful” medicine.12 These findings suggest that perception of malpractice risk might simply be serving as a proxy for physicians’ underlying risk tolerance, and be less subject to influence by external forces.
Areas Associated With Malpractice Risk
A number of closed-claim databases attempted to identify the characteristics of patient encounters that can lead to malpractice claims, including patient conditions and sources of error. Diagnostic errors have consistently been found to be the leading cause of malpractice claims, accounting for 28% to 65% of claims, followed by inappropriate management of medical treatment and improper performance of a procedure.7,13-16 A January 2016 benchmarking system report by CRICO Strategies found that 30% of 23,658 medical malpractice claims filed between 2009 through 2013 cited failures in communication as a factor.17 The report also revealed that among these failed communications, those that occurred between health care providers are more likely to result in payout compared to miscommunications between providers and patients.17 This report further noted 70% to 80% of claims closed without payment.7,16 Closed claims were significantly more likely to involve serious injuries or death.7,18 Leading conditions that resulted in claims include myocardial infarction, nonspecific chest pain, symptoms involving the abdomen or pelvis, appendicitis, and orthopedic injuries.7,13,16
Diagnostic Errors
Errors in diagnosis have been attributed to multiple factors in the ED. The two most common factors were failure to order tests and failure to perform an adequate history and physical examination, both of which contribute to rationalization of the practice of defensive medicine under the current tort system.13 Other significant factors associated with errors in diagnosis include misinterpretation of test results or imaging studies and failure to obtain an appropriate consultation. Processes contributing to each of these potential errors include mistakes in judgment, lack of knowledge, miscommunication, and insufficient documentation (Table).15
Strategies for Reducing Malpractice Risk
In part 1, we listed several strategies EPs could adopt to help reduce malpractice risk. In this section, we will discuss in further detail how these strategies help mitigate malpractice claims.
Patient Communication
Open communication with patients is paramount in reducing the risk of a malpractice allegation. Patients are more likely to become angry or frustrated if they sense a physician is not listening to or addressing their concerns. These patients are in turn more likely to file a complaint if they are harmed or experience a bad outcome during their stay in the ED.
Situations in which patients are unable to provide pertinent information also place the EP at significant risk, as the provider must make decisions without full knowledge of the case. Communication with potential resources such as nursing home staff, the patient’s family, and emergency medical service providers to obtain additional information can help reduce risk.
Of course, when evaluating and treating patients, the EP should always take the time to listen to the patient’s concerns during the encounter to ensure his or her needs have been addressed. In the event of a patient allegation or complaint, the EP should make the effort to explore and de-escalate the situation before the patient is discharged.
Discharge Care and Instructions
According to CRICO, premature discharge as a factor in medical malpractice liability results from inadequate assessment and missed opportunities in 41% of diagnosis-related ED cases.16 The following situation illustrates a brief example of such a missed opportunity: A provider makes a diagnosis of urinary tract infection (UTI) in a patient presenting with fever and abdominal pain but whose urinalysis is suspect for contamination and in whom no pelvic examination was performed to rule out other etiologies. When the same patient later returns to the ED with worse abdominal pain, a sterile urine culture invalidates the diagnosis of UTI, and further evaluation leads to a final diagnosis of ruptured appendix.
Prior to discharging any patient, the EP should provide clear and concise at-home care instructions in a manner in which the patient can understand. Clear instructions on how the patient is to manage his or her care after discharge are vital, and failure to do so in terms the patient can understand can create problems if a harmful result occurs. This is especially important in patients with whom there is a communication barrier—eg, language barrier, hearing impairment, cognitive deficit, intoxication, or violent or irrational behavior. In these situations, the EP should always take advantage of available resources and tools such as language lines, interpreters, discharge planners, psychiatric staff, and supportive family members to help reconcile any communication barriers. These measures will in turn optimize patient outcome and reduce the risk of a later malpractice allegation.
Board Certification
All physicians should maintain their respective board certification and specialty training requirements. Efforts in this area help providers to stay up to date in current practice standards and new developments, thus reducing one’s risk of incurring a malpractice claim.
Patient Safety
All members of the care team should engender an environment that is focused on patient safety, including open communication between providers and with nursing staff and technical support teams. Although interruptions can be detrimental to patient care, simply having an understanding of this phenomenon among all staff members can alleviate some of the working stressors in the ED. Effort must be made to create an environment that allows for clarification between nursing staff and physicians without causing undue antagonism. Fostering supportive communication, having a questioning attitude, and seeking clarification can only enhance patient safety.
The importance of the supervisory role of attending physicians to trainees, physician extenders, and nursing staff must be emphasized, and appropriate guidance from the ED attending is germane in keeping patients safe in teaching environments. Additionally, in departments that suffer the burden of high numbers of admitted patient boarders in the ED, attention must be given to the transitional period between decision to admit and termination of ED care and the acquisition of care of the admitting physician. A clear plan of responsibility must be in place for these high-risk situations.
Policies and Procedures
Departmental policies and procedures should be designed to identify and address all late laboratory results data, radiological discrepancies, and culture results in a timely and uniform manner. Since unaddressed results and discrepancies can result in patient harm, patient-callback processes should be designed to reduce risk by addressing these hazards regularly, thoroughly, and in a timely fashion.
Cognitive Biases
An awareness of inherent biases in the medical decision-making process is also helpful to maintain mindfulness in the routine practice of EM and avoid medical errors. The EP should take care not to be influenced by recent events and diagnostic information that is easy to recall or common, and to ensure the differential addresses possibilities beyond the readily available diagnoses. Further, reliance on an existing opinion may be misleading if subsequent judgments are based on this “anchor,” whether it is true or false.
If the data points of the case do not line up as expected, or if there are unexplained outliers, the EP should expand the frame of reference to seek more appropriate possibilities, and avoid attempts to make the data fit a preferred or favored conclusion.
When one fails to recognize that data do not fit the diagnostic presumption, the true diagnosis can be undermined. Such confirmation bias in turn challenges diagnostic success. Hasty judgment without considering and seeking out relevant information can set up diagnostic failure and premature closure.
Remembering the Basics
Finally, providers should follow the basic principles for every patient. Vital signs are vital for a reason, and all abnormal data must be accounted for prior to patient hand off or discharge. Patient turnover is a high-risk occasion, and demands careful attention to case details between the off-going physician, the accepting physician, and the patient.
All patients presenting to the ED for care should leave the ED at their baseline functional level (ie, if they walk independently, they should still walk independently at discharge). If not, the reason should be sought out and clarified with appropriate recommendations for treatment and follow-up.
Patients and staff should always be treated with respect, which in turn will encourage effective communication. Providers should be honest with patients, document truthfully, respect privacy and confidentiality, practice within one’s competence, confirm information, and avoid assumptions. Compassion goes hand in hand with respectful and open communication. Physicians perceived as compassionate and trustworthy are less likely to be the target of a malpractice suit, even when harm has occurred.
Conclusion
Even though the number of paid medical malpractice claims has continued to decrease over the past 20 years, a discrepancy between perceived and absolute risk persists among EPs—one that perpetuates the practice of defensive medicine and continues to affect EM. Despite the current perceptions and climate, EPs can allay their risk of incurring a malpractice claim by employing the strategies outlined above.
Most medical malpractice cases are still resolved in a courtroom—typically after years of preparation and personal torment. Yet, overall rates of paid medical malpractice claims among all physicians have been steadily decreasing over the past two decades, with reports showing decreases of 30% to 50% in paid claims since 2000.1-3 At the same time, while median payments and insurance premiums continued to increase until the mid-2000s, they now appear to have plateaued.1
None of these changes occurred in isolation. More than 30 states now have caps on noneconomic or total damages.2 As noted in part 1, since 2000, some states have enacted comprehensive tort reform.4 However, whether these changes in malpractice patterns can be attributed directly to specific policy changes remains a hotly contested issue.
Malpractice Risk in Emergency Medicine
To what extent do the trends in medical malpractice apply to emergency medicine (EM)? While emergency physicians’ (EPs’) perception of malpractice risk ranks higher than any other medical specialty,5 in a review of a large sample of malpractice claims from 1991 through 2005, EPs ranked in the middle among specialties with respect to annual risk of a malpractice claim.6 Moreover, the annual risk of a claim for EPs is just under 8%, compared to 7.4% for all physicians. Yet, for neurosurgery and cardiothoracic surgery—the specialties with the highest overall risk of malpractice claims—the annual risk approaches 20%.6 Regarding payout statistics, less than one-fifth of the claims against EPs resulted in payment.6 In a review of a separate insurance database of closed claims, EPs were named as the primary defendant in only 19% of cases.7
Despite the discrepancies between perceived risk and absolute risk of malpractice claims among EPs, malpractice lawsuits continue to affect the practice of EM. This is evidenced in several surveys, in which the majority of EP participants admitted to practicing “defensive medicine” by ordering tests that were felt to be unnecessary and did so in response to perceived malpractice risk.8-10 Perceived risk also accounts for the significant variation in decision-making in the ED with respect to diagnostic testing and hospitalization of patients.11 One would expect that lowering malpractice risk would result in less so-called unnecessary testing, but whether or not this is truly the case remains to be seen.
Effects of Malpractice Reform
A study by Waxman et al12 on the effects of significant malpractice tort reform in ED care in Texas, Georgia, and South Carolina found no difference in rates of imaging studies, charges, or patient admissions. Furthermore, legislation reform did not increase plaintiff onus to prove proximate “gross negligence” rather than simply a breach from “reasonably skillful and careful” medicine.12 These findings suggest that perception of malpractice risk might simply be serving as a proxy for physicians’ underlying risk tolerance, and be less subject to influence by external forces.
Areas Associated With Malpractice Risk
A number of closed-claim databases attempted to identify the characteristics of patient encounters that can lead to malpractice claims, including patient conditions and sources of error. Diagnostic errors have consistently been found to be the leading cause of malpractice claims, accounting for 28% to 65% of claims, followed by inappropriate management of medical treatment and improper performance of a procedure.7,13-16 A January 2016 benchmarking system report by CRICO Strategies found that 30% of 23,658 medical malpractice claims filed between 2009 through 2013 cited failures in communication as a factor.17 The report also revealed that among these failed communications, those that occurred between health care providers are more likely to result in payout compared to miscommunications between providers and patients.17 This report further noted 70% to 80% of claims closed without payment.7,16 Closed claims were significantly more likely to involve serious injuries or death.7,18 Leading conditions that resulted in claims include myocardial infarction, nonspecific chest pain, symptoms involving the abdomen or pelvis, appendicitis, and orthopedic injuries.7,13,16
Diagnostic Errors
Errors in diagnosis have been attributed to multiple factors in the ED. The two most common factors were failure to order tests and failure to perform an adequate history and physical examination, both of which contribute to rationalization of the practice of defensive medicine under the current tort system.13 Other significant factors associated with errors in diagnosis include misinterpretation of test results or imaging studies and failure to obtain an appropriate consultation. Processes contributing to each of these potential errors include mistakes in judgment, lack of knowledge, miscommunication, and insufficient documentation (Table).15
Strategies for Reducing Malpractice Risk
In part 1, we listed several strategies EPs could adopt to help reduce malpractice risk. In this section, we will discuss in further detail how these strategies help mitigate malpractice claims.
Patient Communication
Open communication with patients is paramount in reducing the risk of a malpractice allegation. Patients are more likely to become angry or frustrated if they sense a physician is not listening to or addressing their concerns. These patients are in turn more likely to file a complaint if they are harmed or experience a bad outcome during their stay in the ED.
Situations in which patients are unable to provide pertinent information also place the EP at significant risk, as the provider must make decisions without full knowledge of the case. Communication with potential resources such as nursing home staff, the patient’s family, and emergency medical service providers to obtain additional information can help reduce risk.
Of course, when evaluating and treating patients, the EP should always take the time to listen to the patient’s concerns during the encounter to ensure his or her needs have been addressed. In the event of a patient allegation or complaint, the EP should make the effort to explore and de-escalate the situation before the patient is discharged.
Discharge Care and Instructions
According to CRICO, premature discharge as a factor in medical malpractice liability results from inadequate assessment and missed opportunities in 41% of diagnosis-related ED cases.16 The following situation illustrates a brief example of such a missed opportunity: A provider makes a diagnosis of urinary tract infection (UTI) in a patient presenting with fever and abdominal pain but whose urinalysis is suspect for contamination and in whom no pelvic examination was performed to rule out other etiologies. When the same patient later returns to the ED with worse abdominal pain, a sterile urine culture invalidates the diagnosis of UTI, and further evaluation leads to a final diagnosis of ruptured appendix.
Prior to discharging any patient, the EP should provide clear and concise at-home care instructions in a manner in which the patient can understand. Clear instructions on how the patient is to manage his or her care after discharge are vital, and failure to do so in terms the patient can understand can create problems if a harmful result occurs. This is especially important in patients with whom there is a communication barrier—eg, language barrier, hearing impairment, cognitive deficit, intoxication, or violent or irrational behavior. In these situations, the EP should always take advantage of available resources and tools such as language lines, interpreters, discharge planners, psychiatric staff, and supportive family members to help reconcile any communication barriers. These measures will in turn optimize patient outcome and reduce the risk of a later malpractice allegation.
Board Certification
All physicians should maintain their respective board certification and specialty training requirements. Efforts in this area help providers to stay up to date in current practice standards and new developments, thus reducing one’s risk of incurring a malpractice claim.
Patient Safety
All members of the care team should engender an environment that is focused on patient safety, including open communication between providers and with nursing staff and technical support teams. Although interruptions can be detrimental to patient care, simply having an understanding of this phenomenon among all staff members can alleviate some of the working stressors in the ED. Effort must be made to create an environment that allows for clarification between nursing staff and physicians without causing undue antagonism. Fostering supportive communication, having a questioning attitude, and seeking clarification can only enhance patient safety.
The importance of the supervisory role of attending physicians to trainees, physician extenders, and nursing staff must be emphasized, and appropriate guidance from the ED attending is germane in keeping patients safe in teaching environments. Additionally, in departments that suffer the burden of high numbers of admitted patient boarders in the ED, attention must be given to the transitional period between decision to admit and termination of ED care and the acquisition of care of the admitting physician. A clear plan of responsibility must be in place for these high-risk situations.
Policies and Procedures
Departmental policies and procedures should be designed to identify and address all late laboratory results data, radiological discrepancies, and culture results in a timely and uniform manner. Since unaddressed results and discrepancies can result in patient harm, patient-callback processes should be designed to reduce risk by addressing these hazards regularly, thoroughly, and in a timely fashion.
Cognitive Biases
An awareness of inherent biases in the medical decision-making process is also helpful to maintain mindfulness in the routine practice of EM and avoid medical errors. The EP should take care not to be influenced by recent events and diagnostic information that is easy to recall or common, and to ensure the differential addresses possibilities beyond the readily available diagnoses. Further, reliance on an existing opinion may be misleading if subsequent judgments are based on this “anchor,” whether it is true or false.
If the data points of the case do not line up as expected, or if there are unexplained outliers, the EP should expand the frame of reference to seek more appropriate possibilities, and avoid attempts to make the data fit a preferred or favored conclusion.
When one fails to recognize that data do not fit the diagnostic presumption, the true diagnosis can be undermined. Such confirmation bias in turn challenges diagnostic success. Hasty judgment without considering and seeking out relevant information can set up diagnostic failure and premature closure.
Remembering the Basics
Finally, providers should follow the basic principles for every patient. Vital signs are vital for a reason, and all abnormal data must be accounted for prior to patient hand off or discharge. Patient turnover is a high-risk occasion, and demands careful attention to case details between the off-going physician, the accepting physician, and the patient.
All patients presenting to the ED for care should leave the ED at their baseline functional level (ie, if they walk independently, they should still walk independently at discharge). If not, the reason should be sought out and clarified with appropriate recommendations for treatment and follow-up.
Patients and staff should always be treated with respect, which in turn will encourage effective communication. Providers should be honest with patients, document truthfully, respect privacy and confidentiality, practice within one’s competence, confirm information, and avoid assumptions. Compassion goes hand in hand with respectful and open communication. Physicians perceived as compassionate and trustworthy are less likely to be the target of a malpractice suit, even when harm has occurred.
Conclusion
Even though the number of paid medical malpractice claims has continued to decrease over the past 20 years, a discrepancy between perceived and absolute risk persists among EPs—one that perpetuates the practice of defensive medicine and continues to affect EM. Despite the current perceptions and climate, EPs can allay their risk of incurring a malpractice claim by employing the strategies outlined above.
1. Mello MM, Studdert DM, Kachalia A. The medical liability climate and prospects for reform. JAMA. 2014;312(20):2146-2155.
2. Paik M, Black B, Hyman DA. The receding tide of medical malpractice: part 1 - national trends. J Empirical Leg Stud. 2013;10(4):612-638.
3. Bishop TF, Ryan AM, Caslino LP. Paid malpractice claims for adverse events in inpatient and outpatient settings. JAMA. 2011;305(23):2427-2431.
4. Kachalia A, Mello MM. New directions in medical liability reform. N Engl J Med. 2011;364(16):
1564-1572.
5. Carrier ER, Reschovsky JD, Mello MM, Mayrell RC, Katz D. Physicians’ fears of malpractice lawsuits are not assured by tort reforms. Health Aff. 2010;29(9):1585-1592.
6. Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011;365(7):629-636.
7. Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010;17(5):553-560.
8. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293(21):2609-2617.
9. Bishop TF, Federman AD, Keyhani S. Physicians’ views on defensive medicine: a national survey. Arch Intern Med. 2010;170(12):1081-1083.
10. Massachusetts Medical Society. Investigation of defensive medicine in Massachusetts. November 2008. Available at http://www.massmed.org/defensivemedicine. Accessed March 16, 2016.
11. Katz DA, Williams GC, Brown RL, et al. Emergency physicians’ fear of malpractice in evaluating patient with possible acute cardiac ischemia. Ann Emerg Med. 2005;46(6):525-533.
12. Waxman DA, Greenberg MD, Ridgely MS, Kellermann AL, Heaton P. The effect of malpractice reform on emergency department care. N Engl J Med. 2014;371(16):1518-1525.
13. Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
14. Saber Tehrani AS, Lee H, Mathews SC, et al. 25-Year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672-680.
15. Ross J, Ranum D, Troxel DB. Emergency medicine closed claims study. The Doctors Company. Available at http://www.thedoctors.com/ecm/groups/public/@tdc/@web/@kc/@patientsafety/documents/article/con_id_004776.pdf. Accessed March 16, 2016.
16. Ruoff G, ed. 2011 Annual benchmarking report: malpractice risks in emergency medicine. CRICO strategies. 2012. Available at https://www.rmf.harvard.edu/Strategies/Home/Products-and-Services/Comparative-Data/Annual-Benchmark-Reports. Accessed March 16, 2016.
17. Failures in communication contribute to medical malpractice. January 31, 2016. https://www.rmf.harvard.edu/About-CRICO/Media/Press-Releases/News/2016/February/Failures-in-Communication-Contribute-to-Medical-Malpractice.
18. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024-2033. Accessed March 16, 2016.
1. Mello MM, Studdert DM, Kachalia A. The medical liability climate and prospects for reform. JAMA. 2014;312(20):2146-2155.
2. Paik M, Black B, Hyman DA. The receding tide of medical malpractice: part 1 - national trends. J Empirical Leg Stud. 2013;10(4):612-638.
3. Bishop TF, Ryan AM, Caslino LP. Paid malpractice claims for adverse events in inpatient and outpatient settings. JAMA. 2011;305(23):2427-2431.
4. Kachalia A, Mello MM. New directions in medical liability reform. N Engl J Med. 2011;364(16):
1564-1572.
5. Carrier ER, Reschovsky JD, Mello MM, Mayrell RC, Katz D. Physicians’ fears of malpractice lawsuits are not assured by tort reforms. Health Aff. 2010;29(9):1585-1592.
6. Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011;365(7):629-636.
7. Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010;17(5):553-560.
8. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293(21):2609-2617.
9. Bishop TF, Federman AD, Keyhani S. Physicians’ views on defensive medicine: a national survey. Arch Intern Med. 2010;170(12):1081-1083.
10. Massachusetts Medical Society. Investigation of defensive medicine in Massachusetts. November 2008. Available at http://www.massmed.org/defensivemedicine. Accessed March 16, 2016.
11. Katz DA, Williams GC, Brown RL, et al. Emergency physicians’ fear of malpractice in evaluating patient with possible acute cardiac ischemia. Ann Emerg Med. 2005;46(6):525-533.
12. Waxman DA, Greenberg MD, Ridgely MS, Kellermann AL, Heaton P. The effect of malpractice reform on emergency department care. N Engl J Med. 2014;371(16):1518-1525.
13. Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
14. Saber Tehrani AS, Lee H, Mathews SC, et al. 25-Year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672-680.
15. Ross J, Ranum D, Troxel DB. Emergency medicine closed claims study. The Doctors Company. Available at http://www.thedoctors.com/ecm/groups/public/@tdc/@web/@kc/@patientsafety/documents/article/con_id_004776.pdf. Accessed March 16, 2016.
16. Ruoff G, ed. 2011 Annual benchmarking report: malpractice risks in emergency medicine. CRICO strategies. 2012. Available at https://www.rmf.harvard.edu/Strategies/Home/Products-and-Services/Comparative-Data/Annual-Benchmark-Reports. Accessed March 16, 2016.
17. Failures in communication contribute to medical malpractice. January 31, 2016. https://www.rmf.harvard.edu/About-CRICO/Media/Press-Releases/News/2016/February/Failures-in-Communication-Contribute-to-Medical-Malpractice.
18. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024-2033. Accessed March 16, 2016.
Echocardiogram goes unread ... Call to help line is too late
Echocardiograms were done, but who was reading them?
A 67-YEAR-OLD MAN had been under the care of his primary care physician for aortic stenosis. The physician was aware of this diagnosis and did periodic echocardiograms to monitor the patient’s heart. The patient was sent to a cardiologist for additional care. Over the next year and a half, the decedent’s condition worsened, and he died of heart failure.
PLAINTIFF’S CLAIM The defendants deviated from the standard of care in not reading the echocardiograms. If they had, they could have treated him and extended his life.
THE DEFENSE The cardiologist said it was not up to him to read the echocardiogram. The primary care physician acknowledged that he deviated from the standard of care.
VERDICT $3 million Connecticut verdict.
COMMENT This is a clear case of failure to take responsibility. I suspect the failure was based on the assumption by both physicians that the other physician was monitoring the patient’s status.
This happened to me with a patient who gradually drifted into acute heart failure while I assumed the nephrologist was managing his diuretics. A phone call and more furosemide would have prevented that hospital admission. (Luckily, my patient recovered uneventfully.)
Don’t assume the specialist has taken charge; verify or manage the patient yourself.
Third call to help line finally leads to office visit, but it’s too late
A 42-YEAR-OLD WOMAN called a phone help line and told a nurse that she had a fever, chills, sore throat, and severe chest pain. The next day she called again and spoke with a nurse who routed her call to a physician. The physician diagnosed the woman with influenza during their 4-minute conversation. She called again the next day and was told to come in for examination. The woman did so and was admitted. One day later, she died of sepsis secondary to pneumonia.
PLAINTIFF’S CLAIM The standard of care required immediate examination by the time of the second call.
THE DEFENSE The plaintiff did not actually report chest pain until the second call, and she contracted an unusually fast-acting strain of pneumonia.
VERDICT $3.5 million California arbitration award.
COMMENT Delayed diagnosis is one of the main reasons family physicians are successfully sued. Management of this patient may have been reasonable the first day. The second call should have prompted a same day visit or instructions to go to the emergency department or at least an urgent care facility. The third call was too late.
Echocardiograms were done, but who was reading them?
A 67-YEAR-OLD MAN had been under the care of his primary care physician for aortic stenosis. The physician was aware of this diagnosis and did periodic echocardiograms to monitor the patient’s heart. The patient was sent to a cardiologist for additional care. Over the next year and a half, the decedent’s condition worsened, and he died of heart failure.
PLAINTIFF’S CLAIM The defendants deviated from the standard of care in not reading the echocardiograms. If they had, they could have treated him and extended his life.
THE DEFENSE The cardiologist said it was not up to him to read the echocardiogram. The primary care physician acknowledged that he deviated from the standard of care.
VERDICT $3 million Connecticut verdict.
COMMENT This is a clear case of failure to take responsibility. I suspect the failure was based on the assumption by both physicians that the other physician was monitoring the patient’s status.
This happened to me with a patient who gradually drifted into acute heart failure while I assumed the nephrologist was managing his diuretics. A phone call and more furosemide would have prevented that hospital admission. (Luckily, my patient recovered uneventfully.)
Don’t assume the specialist has taken charge; verify or manage the patient yourself.
Third call to help line finally leads to office visit, but it’s too late
A 42-YEAR-OLD WOMAN called a phone help line and told a nurse that she had a fever, chills, sore throat, and severe chest pain. The next day she called again and spoke with a nurse who routed her call to a physician. The physician diagnosed the woman with influenza during their 4-minute conversation. She called again the next day and was told to come in for examination. The woman did so and was admitted. One day later, she died of sepsis secondary to pneumonia.
PLAINTIFF’S CLAIM The standard of care required immediate examination by the time of the second call.
THE DEFENSE The plaintiff did not actually report chest pain until the second call, and she contracted an unusually fast-acting strain of pneumonia.
VERDICT $3.5 million California arbitration award.
COMMENT Delayed diagnosis is one of the main reasons family physicians are successfully sued. Management of this patient may have been reasonable the first day. The second call should have prompted a same day visit or instructions to go to the emergency department or at least an urgent care facility. The third call was too late.
Echocardiograms were done, but who was reading them?
A 67-YEAR-OLD MAN had been under the care of his primary care physician for aortic stenosis. The physician was aware of this diagnosis and did periodic echocardiograms to monitor the patient’s heart. The patient was sent to a cardiologist for additional care. Over the next year and a half, the decedent’s condition worsened, and he died of heart failure.
PLAINTIFF’S CLAIM The defendants deviated from the standard of care in not reading the echocardiograms. If they had, they could have treated him and extended his life.
THE DEFENSE The cardiologist said it was not up to him to read the echocardiogram. The primary care physician acknowledged that he deviated from the standard of care.
VERDICT $3 million Connecticut verdict.
COMMENT This is a clear case of failure to take responsibility. I suspect the failure was based on the assumption by both physicians that the other physician was monitoring the patient’s status.
This happened to me with a patient who gradually drifted into acute heart failure while I assumed the nephrologist was managing his diuretics. A phone call and more furosemide would have prevented that hospital admission. (Luckily, my patient recovered uneventfully.)
Don’t assume the specialist has taken charge; verify or manage the patient yourself.
Third call to help line finally leads to office visit, but it’s too late
A 42-YEAR-OLD WOMAN called a phone help line and told a nurse that she had a fever, chills, sore throat, and severe chest pain. The next day she called again and spoke with a nurse who routed her call to a physician. The physician diagnosed the woman with influenza during their 4-minute conversation. She called again the next day and was told to come in for examination. The woman did so and was admitted. One day later, she died of sepsis secondary to pneumonia.
PLAINTIFF’S CLAIM The standard of care required immediate examination by the time of the second call.
THE DEFENSE The plaintiff did not actually report chest pain until the second call, and she contracted an unusually fast-acting strain of pneumonia.
VERDICT $3.5 million California arbitration award.
COMMENT Delayed diagnosis is one of the main reasons family physicians are successfully sued. Management of this patient may have been reasonable the first day. The second call should have prompted a same day visit or instructions to go to the emergency department or at least an urgent care facility. The third call was too late.
Forgoing artificial nutrition and hydration
Question: Which of the following statements regarding artificial nutrition and hydration (ANH) is least supported in ethics and/or law?
A. One may invoke medical futility and discontinue ANH in noncognitive, terminally ill patients.
B. Forgoing ANH at the end of life is part of good palliative care.
C. Tube feeding is a way to provide food and sustenance and does not constitute medical treatment.
D. Many state statutes allow for the discontinuation of ANH under specified conditions.
E. Discontinuing ANH is most contentious when it affects a young, otherwise healthy person in a persistent vegetative state.
Answer: C.
Only a few decades ago, litigation over end-of-life care took the form of surrogates demanding to stop treatment, e.g., mechanical ventilation, against the orders of the hospital and doctors.1 The parties now tend to reverse their positions, with some families insisting on continuing all treatment modalities, especially artificial nutrition and hydration (ANH) such as tube feedings. Medical futility has been variously defined as an intervention that has no pathophysiologic rationale, where such intervention had already failed in the patient, where maximal treatment is already failing, or where the intervention will not achieve the goals of care. The AMA Code of Medical Ethics advises: “Physicians are not ethically obligated to deliver care that, in their best professional judgment, will not have a reasonable chance of benefiting their patients. Patients should not be given treatments simply because they demand them.”2 The AMA Code also clarifies that “life-sustaining treatment is any treatment that serves to prolong life without reversing the underlying medical condition” and “may include … artificial nutrition and hydration.”3
Although many palliative care specialists have deemed ANH to be of dubious medical benefit at the end of life,4 forgoing ANH nonetheless poses a particularly contentious dilemma. Opponents assert that ANH is a form of feeding rather than medical treatment, denial of which amounts to “starving” the patient to death. However in 1990, the U.S. Supreme Court in Cruzan v. Director5 declared that ANH could not be readily distinguished from other forms of medical treatment. The case involved a 25-year-old woman who lapsed into a persistent vegetative state (PVS) following an automobile accident. Her parents sought a court order to withdraw ANH when it became apparent that she had virtually no chance of recovering her cognitive faculties. Writing for a unanimous Supreme Court, Justice O’Connor opined: “Whether or not the techniques used to pass food and water into the patient’s alimentary tract are termed ‘medical treatment,’ it is clear they all involve some degree of intrusion and restraint. … Feeding a patient by means of a nasogastric tube requires a physician to pass a long flexible tube through the patient’s nose, throat, and esophagus and into the stomach. Because of the discomfort such a tube causes, ‘many patients need to be restrained forcibly and their hands put into large mittens to prevent them from removing the tube.’ A gastrostomy tube … or jejunostomy tube must be surgically implanted into the stomach or small intestine. … Requiring a competent adult to endure such procedures against her will burdens the patient’s liberty, dignity, and freedom to determine the course of her own treatment.”
The English High Court has likewise adopted this position in Airedale NHS Trust v. Bland.6 Tony Bland, a young man, was crushed in a Hillsborough football melee in 1989, which caused him to develop PVS. The court wrote: “The question is not whether it is in the best interests of the patient that he should die. The question is whether it is in the best interests of the patient that his life should be prolonged by the continuance of this form of medical treatment or care. The correct formulation of the question is of particular importance in a case such as the present, where the patient is totally unconscious or where there is no hope whatsoever of any amelioration of his condition.”
In 2005, the United States witnessed its most public and highly politicized case regarding the withdrawal of ANH.7 In 1990, Terri Schiavo, then age 26, sustained a cardiac arrest, possibly caused by an eating disorder and hypokalemia. Her husband, Michael, filed a malpractice suit and won damages of $1.5 million, but the arrest left her in a PVS. Terri had left no advance directive, and her husband said she would rather die than be kept alive artificially, and therefore directed that her tube feeding be stopped. On the other hand, her parents Bob and Mary Schindler wished to keep her alive, and volunteered to take care of her. After a long and bitter legal battle, an appellate court finally agreed to stop Terri’s tube feeding, as it found clear and convincing evidence that she would not have wanted to live in that manner. The U.S. Supreme Court refused to review the case. On Oct. 15, 2003, with the discontinuation of her tube feeding, Terri’s parents appealed to then Florida Gov. Jeb Bush, calling into question the diagnosis of PVS. They insisted Terri’s eyes were open, and she appeared to respond with smiles to the sound of her mother’s voice. Despite contrary expert opinion, 15 doctors testified she could and would improve. Both the Florida legislature and the U.S. Congress intervened but to no avail. Terri died at 10 a.m. on March 31, 2005, 13 days after tube withdrawal. An autopsy revealed severe brain atrophy.
In Cruzan, the U.S. Supreme Court had held that the liberty guaranteed by the Due Process Clause must protect an individual’s deeply personal decision to reject medical treatment, including the artificial delivery of food and water. However, where a patient’s wishes are not clear and convincing, a court will be reluctant to order cessation of treatment. In a 6-0 decision, the California Supreme Court ruled that a patient’s tube feedings could not be discontinued under the circumstances of the Wendland case.8 Robert Wendland regained consciousness after 14 months in a coma, but was left hemiparetic and incontinent, and could not feed by mouth or dress, bathe, and communicate consistently. His wife, Rose, refused to authorize reinsertion of his dislodged feeding tube, believing that Robert would not have wanted it replaced. The patient’s daughter and brother, as well as the hospital’s ethics committee, the county ombudsman, and a court-appointed counsel all agreed with the decision. Robert did not have an advance directive, but had made statements to the effect he would not want to live in a vegetative state. But the patient’s mother, Florence, went to court to block the action. The court determined that Robert’s statements were not clear and convincing because they did not address his current condition, were not sufficiently specific, and were not necessarily intended to direct his medical care. Further, the patient’s spouse had failed to provide sufficient evidence that her decision was in her husband’s best interests.
In some jurisdictions, a patient’s advance medical directive to discontinue ANH may require a specific opt-in or opt-out choice. And although medical directives typically spring into effect when a patient is terminally ill, many jurisdictions allow their applicability in nonterminal conditions such as irreversible unconscious states or where the likely risks and burdens of treatment would outweigh any expected benefits (Hawaii is such a state under HRS §327E-16). Physicians are legally bound to respect a patient’s wish regarding forgoing or continuing therapy including ANH. Given the wide variations in legal requirements governing this emotional matter, physicians must look closely at their individual state statute to determine the proper course of action under the circumstances.
References
1. In re Quinlan, 70 N.J. 10 (1976).
2. Code of Medical Ethics of the AMA, 2014-5 ed., section 2.035.
3. Code of Medical Ethics of the AMA, 2014-5 ed., section 2.20.
4. Danis M. Stopping artificial nutrition and hydration at the end of life. UpToDate, Nov 2, 2015.
5. Cruzan v. Director, Missouri Department of Health, 110 S. Ct. 2841 (1990).
6. Airedale NHS Trust v. Bland (1993) A.C. 789.
7. Available at https://en.wikipedia.org/wiki/Terri_Schiavo_case.
8. Wendland v. Wendland, 28 P.3d 151 (Cal., 2001).
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: Which of the following statements regarding artificial nutrition and hydration (ANH) is least supported in ethics and/or law?
A. One may invoke medical futility and discontinue ANH in noncognitive, terminally ill patients.
B. Forgoing ANH at the end of life is part of good palliative care.
C. Tube feeding is a way to provide food and sustenance and does not constitute medical treatment.
D. Many state statutes allow for the discontinuation of ANH under specified conditions.
E. Discontinuing ANH is most contentious when it affects a young, otherwise healthy person in a persistent vegetative state.
Answer: C.
Only a few decades ago, litigation over end-of-life care took the form of surrogates demanding to stop treatment, e.g., mechanical ventilation, against the orders of the hospital and doctors.1 The parties now tend to reverse their positions, with some families insisting on continuing all treatment modalities, especially artificial nutrition and hydration (ANH) such as tube feedings. Medical futility has been variously defined as an intervention that has no pathophysiologic rationale, where such intervention had already failed in the patient, where maximal treatment is already failing, or where the intervention will not achieve the goals of care. The AMA Code of Medical Ethics advises: “Physicians are not ethically obligated to deliver care that, in their best professional judgment, will not have a reasonable chance of benefiting their patients. Patients should not be given treatments simply because they demand them.”2 The AMA Code also clarifies that “life-sustaining treatment is any treatment that serves to prolong life without reversing the underlying medical condition” and “may include … artificial nutrition and hydration.”3
Although many palliative care specialists have deemed ANH to be of dubious medical benefit at the end of life,4 forgoing ANH nonetheless poses a particularly contentious dilemma. Opponents assert that ANH is a form of feeding rather than medical treatment, denial of which amounts to “starving” the patient to death. However in 1990, the U.S. Supreme Court in Cruzan v. Director5 declared that ANH could not be readily distinguished from other forms of medical treatment. The case involved a 25-year-old woman who lapsed into a persistent vegetative state (PVS) following an automobile accident. Her parents sought a court order to withdraw ANH when it became apparent that she had virtually no chance of recovering her cognitive faculties. Writing for a unanimous Supreme Court, Justice O’Connor opined: “Whether or not the techniques used to pass food and water into the patient’s alimentary tract are termed ‘medical treatment,’ it is clear they all involve some degree of intrusion and restraint. … Feeding a patient by means of a nasogastric tube requires a physician to pass a long flexible tube through the patient’s nose, throat, and esophagus and into the stomach. Because of the discomfort such a tube causes, ‘many patients need to be restrained forcibly and their hands put into large mittens to prevent them from removing the tube.’ A gastrostomy tube … or jejunostomy tube must be surgically implanted into the stomach or small intestine. … Requiring a competent adult to endure such procedures against her will burdens the patient’s liberty, dignity, and freedom to determine the course of her own treatment.”
The English High Court has likewise adopted this position in Airedale NHS Trust v. Bland.6 Tony Bland, a young man, was crushed in a Hillsborough football melee in 1989, which caused him to develop PVS. The court wrote: “The question is not whether it is in the best interests of the patient that he should die. The question is whether it is in the best interests of the patient that his life should be prolonged by the continuance of this form of medical treatment or care. The correct formulation of the question is of particular importance in a case such as the present, where the patient is totally unconscious or where there is no hope whatsoever of any amelioration of his condition.”
In 2005, the United States witnessed its most public and highly politicized case regarding the withdrawal of ANH.7 In 1990, Terri Schiavo, then age 26, sustained a cardiac arrest, possibly caused by an eating disorder and hypokalemia. Her husband, Michael, filed a malpractice suit and won damages of $1.5 million, but the arrest left her in a PVS. Terri had left no advance directive, and her husband said she would rather die than be kept alive artificially, and therefore directed that her tube feeding be stopped. On the other hand, her parents Bob and Mary Schindler wished to keep her alive, and volunteered to take care of her. After a long and bitter legal battle, an appellate court finally agreed to stop Terri’s tube feeding, as it found clear and convincing evidence that she would not have wanted to live in that manner. The U.S. Supreme Court refused to review the case. On Oct. 15, 2003, with the discontinuation of her tube feeding, Terri’s parents appealed to then Florida Gov. Jeb Bush, calling into question the diagnosis of PVS. They insisted Terri’s eyes were open, and she appeared to respond with smiles to the sound of her mother’s voice. Despite contrary expert opinion, 15 doctors testified she could and would improve. Both the Florida legislature and the U.S. Congress intervened but to no avail. Terri died at 10 a.m. on March 31, 2005, 13 days after tube withdrawal. An autopsy revealed severe brain atrophy.
In Cruzan, the U.S. Supreme Court had held that the liberty guaranteed by the Due Process Clause must protect an individual’s deeply personal decision to reject medical treatment, including the artificial delivery of food and water. However, where a patient’s wishes are not clear and convincing, a court will be reluctant to order cessation of treatment. In a 6-0 decision, the California Supreme Court ruled that a patient’s tube feedings could not be discontinued under the circumstances of the Wendland case.8 Robert Wendland regained consciousness after 14 months in a coma, but was left hemiparetic and incontinent, and could not feed by mouth or dress, bathe, and communicate consistently. His wife, Rose, refused to authorize reinsertion of his dislodged feeding tube, believing that Robert would not have wanted it replaced. The patient’s daughter and brother, as well as the hospital’s ethics committee, the county ombudsman, and a court-appointed counsel all agreed with the decision. Robert did not have an advance directive, but had made statements to the effect he would not want to live in a vegetative state. But the patient’s mother, Florence, went to court to block the action. The court determined that Robert’s statements were not clear and convincing because they did not address his current condition, were not sufficiently specific, and were not necessarily intended to direct his medical care. Further, the patient’s spouse had failed to provide sufficient evidence that her decision was in her husband’s best interests.
In some jurisdictions, a patient’s advance medical directive to discontinue ANH may require a specific opt-in or opt-out choice. And although medical directives typically spring into effect when a patient is terminally ill, many jurisdictions allow their applicability in nonterminal conditions such as irreversible unconscious states or where the likely risks and burdens of treatment would outweigh any expected benefits (Hawaii is such a state under HRS §327E-16). Physicians are legally bound to respect a patient’s wish regarding forgoing or continuing therapy including ANH. Given the wide variations in legal requirements governing this emotional matter, physicians must look closely at their individual state statute to determine the proper course of action under the circumstances.
References
1. In re Quinlan, 70 N.J. 10 (1976).
2. Code of Medical Ethics of the AMA, 2014-5 ed., section 2.035.
3. Code of Medical Ethics of the AMA, 2014-5 ed., section 2.20.
4. Danis M. Stopping artificial nutrition and hydration at the end of life. UpToDate, Nov 2, 2015.
5. Cruzan v. Director, Missouri Department of Health, 110 S. Ct. 2841 (1990).
6. Airedale NHS Trust v. Bland (1993) A.C. 789.
7. Available at https://en.wikipedia.org/wiki/Terri_Schiavo_case.
8. Wendland v. Wendland, 28 P.3d 151 (Cal., 2001).
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: Which of the following statements regarding artificial nutrition and hydration (ANH) is least supported in ethics and/or law?
A. One may invoke medical futility and discontinue ANH in noncognitive, terminally ill patients.
B. Forgoing ANH at the end of life is part of good palliative care.
C. Tube feeding is a way to provide food and sustenance and does not constitute medical treatment.
D. Many state statutes allow for the discontinuation of ANH under specified conditions.
E. Discontinuing ANH is most contentious when it affects a young, otherwise healthy person in a persistent vegetative state.
Answer: C.
Only a few decades ago, litigation over end-of-life care took the form of surrogates demanding to stop treatment, e.g., mechanical ventilation, against the orders of the hospital and doctors.1 The parties now tend to reverse their positions, with some families insisting on continuing all treatment modalities, especially artificial nutrition and hydration (ANH) such as tube feedings. Medical futility has been variously defined as an intervention that has no pathophysiologic rationale, where such intervention had already failed in the patient, where maximal treatment is already failing, or where the intervention will not achieve the goals of care. The AMA Code of Medical Ethics advises: “Physicians are not ethically obligated to deliver care that, in their best professional judgment, will not have a reasonable chance of benefiting their patients. Patients should not be given treatments simply because they demand them.”2 The AMA Code also clarifies that “life-sustaining treatment is any treatment that serves to prolong life without reversing the underlying medical condition” and “may include … artificial nutrition and hydration.”3
Although many palliative care specialists have deemed ANH to be of dubious medical benefit at the end of life,4 forgoing ANH nonetheless poses a particularly contentious dilemma. Opponents assert that ANH is a form of feeding rather than medical treatment, denial of which amounts to “starving” the patient to death. However in 1990, the U.S. Supreme Court in Cruzan v. Director5 declared that ANH could not be readily distinguished from other forms of medical treatment. The case involved a 25-year-old woman who lapsed into a persistent vegetative state (PVS) following an automobile accident. Her parents sought a court order to withdraw ANH when it became apparent that she had virtually no chance of recovering her cognitive faculties. Writing for a unanimous Supreme Court, Justice O’Connor opined: “Whether or not the techniques used to pass food and water into the patient’s alimentary tract are termed ‘medical treatment,’ it is clear they all involve some degree of intrusion and restraint. … Feeding a patient by means of a nasogastric tube requires a physician to pass a long flexible tube through the patient’s nose, throat, and esophagus and into the stomach. Because of the discomfort such a tube causes, ‘many patients need to be restrained forcibly and their hands put into large mittens to prevent them from removing the tube.’ A gastrostomy tube … or jejunostomy tube must be surgically implanted into the stomach or small intestine. … Requiring a competent adult to endure such procedures against her will burdens the patient’s liberty, dignity, and freedom to determine the course of her own treatment.”
The English High Court has likewise adopted this position in Airedale NHS Trust v. Bland.6 Tony Bland, a young man, was crushed in a Hillsborough football melee in 1989, which caused him to develop PVS. The court wrote: “The question is not whether it is in the best interests of the patient that he should die. The question is whether it is in the best interests of the patient that his life should be prolonged by the continuance of this form of medical treatment or care. The correct formulation of the question is of particular importance in a case such as the present, where the patient is totally unconscious or where there is no hope whatsoever of any amelioration of his condition.”
In 2005, the United States witnessed its most public and highly politicized case regarding the withdrawal of ANH.7 In 1990, Terri Schiavo, then age 26, sustained a cardiac arrest, possibly caused by an eating disorder and hypokalemia. Her husband, Michael, filed a malpractice suit and won damages of $1.5 million, but the arrest left her in a PVS. Terri had left no advance directive, and her husband said she would rather die than be kept alive artificially, and therefore directed that her tube feeding be stopped. On the other hand, her parents Bob and Mary Schindler wished to keep her alive, and volunteered to take care of her. After a long and bitter legal battle, an appellate court finally agreed to stop Terri’s tube feeding, as it found clear and convincing evidence that she would not have wanted to live in that manner. The U.S. Supreme Court refused to review the case. On Oct. 15, 2003, with the discontinuation of her tube feeding, Terri’s parents appealed to then Florida Gov. Jeb Bush, calling into question the diagnosis of PVS. They insisted Terri’s eyes were open, and she appeared to respond with smiles to the sound of her mother’s voice. Despite contrary expert opinion, 15 doctors testified she could and would improve. Both the Florida legislature and the U.S. Congress intervened but to no avail. Terri died at 10 a.m. on March 31, 2005, 13 days after tube withdrawal. An autopsy revealed severe brain atrophy.
In Cruzan, the U.S. Supreme Court had held that the liberty guaranteed by the Due Process Clause must protect an individual’s deeply personal decision to reject medical treatment, including the artificial delivery of food and water. However, where a patient’s wishes are not clear and convincing, a court will be reluctant to order cessation of treatment. In a 6-0 decision, the California Supreme Court ruled that a patient’s tube feedings could not be discontinued under the circumstances of the Wendland case.8 Robert Wendland regained consciousness after 14 months in a coma, but was left hemiparetic and incontinent, and could not feed by mouth or dress, bathe, and communicate consistently. His wife, Rose, refused to authorize reinsertion of his dislodged feeding tube, believing that Robert would not have wanted it replaced. The patient’s daughter and brother, as well as the hospital’s ethics committee, the county ombudsman, and a court-appointed counsel all agreed with the decision. Robert did not have an advance directive, but had made statements to the effect he would not want to live in a vegetative state. But the patient’s mother, Florence, went to court to block the action. The court determined that Robert’s statements were not clear and convincing because they did not address his current condition, were not sufficiently specific, and were not necessarily intended to direct his medical care. Further, the patient’s spouse had failed to provide sufficient evidence that her decision was in her husband’s best interests.
In some jurisdictions, a patient’s advance medical directive to discontinue ANH may require a specific opt-in or opt-out choice. And although medical directives typically spring into effect when a patient is terminally ill, many jurisdictions allow their applicability in nonterminal conditions such as irreversible unconscious states or where the likely risks and burdens of treatment would outweigh any expected benefits (Hawaii is such a state under HRS §327E-16). Physicians are legally bound to respect a patient’s wish regarding forgoing or continuing therapy including ANH. Given the wide variations in legal requirements governing this emotional matter, physicians must look closely at their individual state statute to determine the proper course of action under the circumstances.
References
1. In re Quinlan, 70 N.J. 10 (1976).
2. Code of Medical Ethics of the AMA, 2014-5 ed., section 2.035.
3. Code of Medical Ethics of the AMA, 2014-5 ed., section 2.20.
4. Danis M. Stopping artificial nutrition and hydration at the end of life. UpToDate, Nov 2, 2015.
5. Cruzan v. Director, Missouri Department of Health, 110 S. Ct. 2841 (1990).
6. Airedale NHS Trust v. Bland (1993) A.C. 789.
7. Available at https://en.wikipedia.org/wiki/Terri_Schiavo_case.
8. Wendland v. Wendland, 28 P.3d 151 (Cal., 2001).
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Law & Medicine: Which doctors get sued?
Question: Doctors are more prone to lawsuits if they:
A. Have been sued before.
B. Spend fewer dollars per hospitalized patient.
C. Show poor communication skills.
D. A and C only.
E. A, B, and C.
Answer: E. Two very recent studies, one by David M. Studdert and the other by Dr. Anupam B. Jena, offer fresh insights into factors linked to the likelihood of a malpractice lawsuit.
The Studdert study concluded that doctors with prior paid claims are at increased risk of incurring yet another lawsuit.1 Instead of simply relying on data from a single insurer or state, the researchers accessed the National Practitioner Data Bank (NPDB) from 2005 through 2014 and identified 66,426 claims paid against 54,099 physicians.
Over that 10-year period, only 1% of physicians accounted for 32% of paid claims. Of all the physicians, 84% incurred only one paid claim during the study period, and 16% had at least two. Four percent of the physicians had at least three. In adjusted analyses, the risk of recurrence increased with the number of previous paid claims.
For example, compared with physicians with a single claim, the 2,160 physicians who had three paid claims had three times the risk of incurring another (hazard ratio, 3.11); this corresponded in absolute terms to a 24% risk within 2 years.
Likelihood of recurrence also varied widely according to specialty. For example, the risk among neurosurgeons was four times greater than that of psychiatrists. As for internists, the risk of recurrence was approximately double that of neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, or obstetrician-gynecologists. The lowest risks of recurrence were seen among psychiatrists (HR, 0.60) and pediatricians (HR, 0.71).
Male physicians had a 38% higher risk of recurrence than did female physicians, and the risk among physicians younger than 35 years was approximately one-third that of their older colleagues (after adjustment for age). Residents had a lower risk of recurrence than did nonresidents, and MDs had a lower risk than did DOs.
Using all 915,564 active physicians in the United States as a denominator, the authors calculated that over the 10-year study period, only 6% of physicians had a paid claim. Note that the 6% figure refers to paid claims reported to the NPDB, which can be expected to be lower than statistics derived from published surveys. These latter studies typically feature self-reported malpractice claims made over a given time period; but it is well known that the majority of such claims are dropped or decided in favor of the doctor, and so will not be reported to the NPDB.
For example, in 2010, the American Medical Association found that 42.2% of 5,825 physicians who responded to its Physician Practice Information survey reported having been sued, with 22.4% sued twice or more.2 The report headlined that by mid career, 61% of doctor have been sued.
Rates varied by specialty, with general surgeons and obstetrician-gynecologists being most likely to be sued (69.2%). Family physicians and general internists had similar rates (38.9% and 34%), and pediatricians and psychiatrists were sued the least.
In that report, male doctors were twice as likely to be sued as were their female counterparts, and physicians in solo and specialty practices were sued more often than those in multispecialty practices. Physicians who had an ownership interest in a practice were also at greater risk, with 47.5% reporting being sued, compared with 33.4% for those with no ownership interest.
The second recent study, reported by Dr. Jena of Harvard Medical School, Boston, and his colleagues, analyzed Florida hospital admissions data covering some 24,000 physicians.3 They found that higher spending by physicians was associated with reduced malpractice claims made the following year.
This pattern held true for physicians in all specialties but one (family practice). For example, among internists, the malpractice risk probability was 1.5% in the bottom spending fifth ($19,725 per admission) and 0.3% in the top fifth ($39,379 per admission). Among obstetricians, the comparable figures were 1.9% and 0.4% respectively.
In addition, a separate subgroup analysis of cesarean-section rates revealed that malpractice claims were approximately halved among obstetricians with rates in the highest fifth, compared with the lowest fifth.
Unfortunately, the Jena study lacked information on illness severity and past malpractice history, and it remains speculative whether increased resource utilization could be attributed entirely to defensive medical practice.4
As interesting as these new reports may be, it is worth remembering that what prompts a lawsuit are poor communication and patient perception that the physician is uncaring and at fault for the bad result.
It is well known that quality of medical care correlates poorly with the filing of malpractice lawsuits, as illustrated in the conclusion of the landmark Harvard study that “medical malpractice litigation infrequently compensates patients injured by medical negligence and rarely identifies, and holds providers accountable for, substandard care.”5 The authors estimated that there was only 1 malpractice claim for every 7.6 adverse events caused by negligence.
In another retrospective chart review study, the quality of treatment as judged by independent peer review was no different in frequently sued versus never-sued obstetricians.6
Communication problems exist in more than 70% of malpractice cases, centering around four themes: 1) deserting the patient; 2) devaluing patient/family views; 3) delivering information poorly; and 4) failing to understand the patient/family perspective.7
Anger, either from the adverse result itself or perceived lack of caring, turns an injured patient into a plaintiff, and lies at the root of all malpractice claims. The patients may not even have a serious injury or a meritorious claim, but they are so frustrated with their physician or the hospital that they contact an attorney to vent their anger.
One experienced attorney volunteered that close to half his malpractice cases could have been avoided through disclosure or apology, noting: “What the patients really wanted was simply an honest explanation of what happened, and, if appropriate, an apology. Unfortunately, when they were not only offered neither, but were rejected as well, they felt doubly wronged and then sought legal counsel.”8
Communicating well begins with active listening. Patients want their doctors to listen to them and to explain their conditions and treatment plans in simple, understandable language. The physician should give them ample opportunity to tell their story and to ask questions.
In one well-publicized study, only 23% of patients were able to complete their opening statement before the doctor interrupted, which occurred, on the average, 18 seconds after the patient began to speak!9
References
1. N Engl J Med. 2016 Jan 28;374(4):354-62.
2. “Medical liability: By late career, 61% of doctors have been sued,” Aug. 16, 2010, American Medical News.
4. “Law & Medicine: Health care costs and defensive medicine,” Jan. 19, 2016, Internal Medicine News.
5. N Engl J Med. 1991 Jul 25;325(4):245-51.
6. JAMA. 1994 Nov 23-30;272(20):1588-91.
7. Arch Intern Med. 1994 Jun 27;154(12):1365-70.
8. Ann Intern Med. 1999 Dec 21;131(12):970-2.
9. Ann Intern Med. 1984 Nov;101(5):692-6.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected]
Question: Doctors are more prone to lawsuits if they:
A. Have been sued before.
B. Spend fewer dollars per hospitalized patient.
C. Show poor communication skills.
D. A and C only.
E. A, B, and C.
Answer: E. Two very recent studies, one by David M. Studdert and the other by Dr. Anupam B. Jena, offer fresh insights into factors linked to the likelihood of a malpractice lawsuit.
The Studdert study concluded that doctors with prior paid claims are at increased risk of incurring yet another lawsuit.1 Instead of simply relying on data from a single insurer or state, the researchers accessed the National Practitioner Data Bank (NPDB) from 2005 through 2014 and identified 66,426 claims paid against 54,099 physicians.
Over that 10-year period, only 1% of physicians accounted for 32% of paid claims. Of all the physicians, 84% incurred only one paid claim during the study period, and 16% had at least two. Four percent of the physicians had at least three. In adjusted analyses, the risk of recurrence increased with the number of previous paid claims.
For example, compared with physicians with a single claim, the 2,160 physicians who had three paid claims had three times the risk of incurring another (hazard ratio, 3.11); this corresponded in absolute terms to a 24% risk within 2 years.
Likelihood of recurrence also varied widely according to specialty. For example, the risk among neurosurgeons was four times greater than that of psychiatrists. As for internists, the risk of recurrence was approximately double that of neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, or obstetrician-gynecologists. The lowest risks of recurrence were seen among psychiatrists (HR, 0.60) and pediatricians (HR, 0.71).
Male physicians had a 38% higher risk of recurrence than did female physicians, and the risk among physicians younger than 35 years was approximately one-third that of their older colleagues (after adjustment for age). Residents had a lower risk of recurrence than did nonresidents, and MDs had a lower risk than did DOs.
Using all 915,564 active physicians in the United States as a denominator, the authors calculated that over the 10-year study period, only 6% of physicians had a paid claim. Note that the 6% figure refers to paid claims reported to the NPDB, which can be expected to be lower than statistics derived from published surveys. These latter studies typically feature self-reported malpractice claims made over a given time period; but it is well known that the majority of such claims are dropped or decided in favor of the doctor, and so will not be reported to the NPDB.
For example, in 2010, the American Medical Association found that 42.2% of 5,825 physicians who responded to its Physician Practice Information survey reported having been sued, with 22.4% sued twice or more.2 The report headlined that by mid career, 61% of doctor have been sued.
Rates varied by specialty, with general surgeons and obstetrician-gynecologists being most likely to be sued (69.2%). Family physicians and general internists had similar rates (38.9% and 34%), and pediatricians and psychiatrists were sued the least.
In that report, male doctors were twice as likely to be sued as were their female counterparts, and physicians in solo and specialty practices were sued more often than those in multispecialty practices. Physicians who had an ownership interest in a practice were also at greater risk, with 47.5% reporting being sued, compared with 33.4% for those with no ownership interest.
The second recent study, reported by Dr. Jena of Harvard Medical School, Boston, and his colleagues, analyzed Florida hospital admissions data covering some 24,000 physicians.3 They found that higher spending by physicians was associated with reduced malpractice claims made the following year.
This pattern held true for physicians in all specialties but one (family practice). For example, among internists, the malpractice risk probability was 1.5% in the bottom spending fifth ($19,725 per admission) and 0.3% in the top fifth ($39,379 per admission). Among obstetricians, the comparable figures were 1.9% and 0.4% respectively.
In addition, a separate subgroup analysis of cesarean-section rates revealed that malpractice claims were approximately halved among obstetricians with rates in the highest fifth, compared with the lowest fifth.
Unfortunately, the Jena study lacked information on illness severity and past malpractice history, and it remains speculative whether increased resource utilization could be attributed entirely to defensive medical practice.4
As interesting as these new reports may be, it is worth remembering that what prompts a lawsuit are poor communication and patient perception that the physician is uncaring and at fault for the bad result.
It is well known that quality of medical care correlates poorly with the filing of malpractice lawsuits, as illustrated in the conclusion of the landmark Harvard study that “medical malpractice litigation infrequently compensates patients injured by medical negligence and rarely identifies, and holds providers accountable for, substandard care.”5 The authors estimated that there was only 1 malpractice claim for every 7.6 adverse events caused by negligence.
In another retrospective chart review study, the quality of treatment as judged by independent peer review was no different in frequently sued versus never-sued obstetricians.6
Communication problems exist in more than 70% of malpractice cases, centering around four themes: 1) deserting the patient; 2) devaluing patient/family views; 3) delivering information poorly; and 4) failing to understand the patient/family perspective.7
Anger, either from the adverse result itself or perceived lack of caring, turns an injured patient into a plaintiff, and lies at the root of all malpractice claims. The patients may not even have a serious injury or a meritorious claim, but they are so frustrated with their physician or the hospital that they contact an attorney to vent their anger.
One experienced attorney volunteered that close to half his malpractice cases could have been avoided through disclosure or apology, noting: “What the patients really wanted was simply an honest explanation of what happened, and, if appropriate, an apology. Unfortunately, when they were not only offered neither, but were rejected as well, they felt doubly wronged and then sought legal counsel.”8
Communicating well begins with active listening. Patients want their doctors to listen to them and to explain their conditions and treatment plans in simple, understandable language. The physician should give them ample opportunity to tell their story and to ask questions.
In one well-publicized study, only 23% of patients were able to complete their opening statement before the doctor interrupted, which occurred, on the average, 18 seconds after the patient began to speak!9
References
1. N Engl J Med. 2016 Jan 28;374(4):354-62.
2. “Medical liability: By late career, 61% of doctors have been sued,” Aug. 16, 2010, American Medical News.
4. “Law & Medicine: Health care costs and defensive medicine,” Jan. 19, 2016, Internal Medicine News.
5. N Engl J Med. 1991 Jul 25;325(4):245-51.
6. JAMA. 1994 Nov 23-30;272(20):1588-91.
7. Arch Intern Med. 1994 Jun 27;154(12):1365-70.
8. Ann Intern Med. 1999 Dec 21;131(12):970-2.
9. Ann Intern Med. 1984 Nov;101(5):692-6.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected]
Question: Doctors are more prone to lawsuits if they:
A. Have been sued before.
B. Spend fewer dollars per hospitalized patient.
C. Show poor communication skills.
D. A and C only.
E. A, B, and C.
Answer: E. Two very recent studies, one by David M. Studdert and the other by Dr. Anupam B. Jena, offer fresh insights into factors linked to the likelihood of a malpractice lawsuit.
The Studdert study concluded that doctors with prior paid claims are at increased risk of incurring yet another lawsuit.1 Instead of simply relying on data from a single insurer or state, the researchers accessed the National Practitioner Data Bank (NPDB) from 2005 through 2014 and identified 66,426 claims paid against 54,099 physicians.
Over that 10-year period, only 1% of physicians accounted for 32% of paid claims. Of all the physicians, 84% incurred only one paid claim during the study period, and 16% had at least two. Four percent of the physicians had at least three. In adjusted analyses, the risk of recurrence increased with the number of previous paid claims.
For example, compared with physicians with a single claim, the 2,160 physicians who had three paid claims had three times the risk of incurring another (hazard ratio, 3.11); this corresponded in absolute terms to a 24% risk within 2 years.
Likelihood of recurrence also varied widely according to specialty. For example, the risk among neurosurgeons was four times greater than that of psychiatrists. As for internists, the risk of recurrence was approximately double that of neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, or obstetrician-gynecologists. The lowest risks of recurrence were seen among psychiatrists (HR, 0.60) and pediatricians (HR, 0.71).
Male physicians had a 38% higher risk of recurrence than did female physicians, and the risk among physicians younger than 35 years was approximately one-third that of their older colleagues (after adjustment for age). Residents had a lower risk of recurrence than did nonresidents, and MDs had a lower risk than did DOs.
Using all 915,564 active physicians in the United States as a denominator, the authors calculated that over the 10-year study period, only 6% of physicians had a paid claim. Note that the 6% figure refers to paid claims reported to the NPDB, which can be expected to be lower than statistics derived from published surveys. These latter studies typically feature self-reported malpractice claims made over a given time period; but it is well known that the majority of such claims are dropped or decided in favor of the doctor, and so will not be reported to the NPDB.
For example, in 2010, the American Medical Association found that 42.2% of 5,825 physicians who responded to its Physician Practice Information survey reported having been sued, with 22.4% sued twice or more.2 The report headlined that by mid career, 61% of doctor have been sued.
Rates varied by specialty, with general surgeons and obstetrician-gynecologists being most likely to be sued (69.2%). Family physicians and general internists had similar rates (38.9% and 34%), and pediatricians and psychiatrists were sued the least.
In that report, male doctors were twice as likely to be sued as were their female counterparts, and physicians in solo and specialty practices were sued more often than those in multispecialty practices. Physicians who had an ownership interest in a practice were also at greater risk, with 47.5% reporting being sued, compared with 33.4% for those with no ownership interest.
The second recent study, reported by Dr. Jena of Harvard Medical School, Boston, and his colleagues, analyzed Florida hospital admissions data covering some 24,000 physicians.3 They found that higher spending by physicians was associated with reduced malpractice claims made the following year.
This pattern held true for physicians in all specialties but one (family practice). For example, among internists, the malpractice risk probability was 1.5% in the bottom spending fifth ($19,725 per admission) and 0.3% in the top fifth ($39,379 per admission). Among obstetricians, the comparable figures were 1.9% and 0.4% respectively.
In addition, a separate subgroup analysis of cesarean-section rates revealed that malpractice claims were approximately halved among obstetricians with rates in the highest fifth, compared with the lowest fifth.
Unfortunately, the Jena study lacked information on illness severity and past malpractice history, and it remains speculative whether increased resource utilization could be attributed entirely to defensive medical practice.4
As interesting as these new reports may be, it is worth remembering that what prompts a lawsuit are poor communication and patient perception that the physician is uncaring and at fault for the bad result.
It is well known that quality of medical care correlates poorly with the filing of malpractice lawsuits, as illustrated in the conclusion of the landmark Harvard study that “medical malpractice litigation infrequently compensates patients injured by medical negligence and rarely identifies, and holds providers accountable for, substandard care.”5 The authors estimated that there was only 1 malpractice claim for every 7.6 adverse events caused by negligence.
In another retrospective chart review study, the quality of treatment as judged by independent peer review was no different in frequently sued versus never-sued obstetricians.6
Communication problems exist in more than 70% of malpractice cases, centering around four themes: 1) deserting the patient; 2) devaluing patient/family views; 3) delivering information poorly; and 4) failing to understand the patient/family perspective.7
Anger, either from the adverse result itself or perceived lack of caring, turns an injured patient into a plaintiff, and lies at the root of all malpractice claims. The patients may not even have a serious injury or a meritorious claim, but they are so frustrated with their physician or the hospital that they contact an attorney to vent their anger.
One experienced attorney volunteered that close to half his malpractice cases could have been avoided through disclosure or apology, noting: “What the patients really wanted was simply an honest explanation of what happened, and, if appropriate, an apology. Unfortunately, when they were not only offered neither, but were rejected as well, they felt doubly wronged and then sought legal counsel.”8
Communicating well begins with active listening. Patients want their doctors to listen to them and to explain their conditions and treatment plans in simple, understandable language. The physician should give them ample opportunity to tell their story and to ask questions.
In one well-publicized study, only 23% of patients were able to complete their opening statement before the doctor interrupted, which occurred, on the average, 18 seconds after the patient began to speak!9
References
1. N Engl J Med. 2016 Jan 28;374(4):354-62.
2. “Medical liability: By late career, 61% of doctors have been sued,” Aug. 16, 2010, American Medical News.
4. “Law & Medicine: Health care costs and defensive medicine,” Jan. 19, 2016, Internal Medicine News.
5. N Engl J Med. 1991 Jul 25;325(4):245-51.
6. JAMA. 1994 Nov 23-30;272(20):1588-91.
7. Arch Intern Med. 1994 Jun 27;154(12):1365-70.
8. Ann Intern Med. 1999 Dec 21;131(12):970-2.
9. Ann Intern Med. 1984 Nov;101(5):692-6.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected]
Law & Medicine: Health care costs and defensive medicine
Question: Which of the following choices is best?
A. Controversy exists over whether defensive medicine is widely practiced and whether it raises health care costs.
B. Everyone agrees that defensive medicine is widely practiced.
C. Doctors who spend more for their hospitalized patients have been reported to face a lower malpractice risk.
D. A and C.
E. B and C.
Answer: D. Virtually all doctors admit they practice defensive medicine, which describes medical care specifically directed to attenuate the threat of malpractice liability rather than for a proper medical indication. Survey studies generally put the prevalence at greater than 90%, but what separates true defensive medicine from careful practice or patient expectation/demand remains controversial.
A mail survey of 824 physicians in high-risk specialties in Pennsylvania, a state where doctors pay high malpractice premiums, revealed that nearly all reported practicing defensive medicine. The respondents admitted to both assurance behavior – such as ordering more tests, especially imaging studies – as well as avoidance behavior – that is, restricting or eliminating complex procedures or perceived litigious patients.1
In another study, emergency physicians in the upper third of “malpractice fear” used more diagnostic tests and were more likely to hospitalize patients at low risk for coronary artery disease.2
On the other hand, a report using simulated clinical scenarios concluded that the extent of defensive medicine was at most 8%, and another found no correlation between individual malpractice claims experience and resource use, physician concern about malpractice, tolerance for uncertainty, or perception of risk.3
Another area of contention is whether some of our soaring health care costs may reflect defensive medicine at play.
A recent survey of 2,000 U.S. orthopedic surgeons found that 96% admitted practicing defensive medicine, with 24% of all ordered tests being for defensive reasons. The authors estimated that this amounted to about $100,000 per surgeon per year, or a total annual sum of $2 billion for the 20,400 orthopedic surgeons in the U.S.4
By correlating professional liability insurance with cost of services, the AMA estimated that in the 1980s, defensive medicine cost $12.1 billion to $13.7 billion each year.5 In an oft-cited study by Kessler and McClellan, the authors measured the effects of malpractice liability reforms using data from elderly Medicare beneficiaries treated for serious heart disease.6 They found that reforms that directly reduced provider liability pressure led to reductions of 5%-9% in medical expenditures. If such Medicare savings, which amounted to $600 million per year for cardiac disease, were extrapolated across the health care system, the annual savings would total $50 billion.
A more conservative study estimated that systemwide savings from aggressive malpractice reform would approach $41 billion over 5 years.7
Dr. Anupam B. Jena and his coauthors are the latest investigators seeking to clarify the correlation between defensive medicine and health care costs.8 Using Florida hospital admission data from 2000-2009, which covered some 24,000 physicians in seven separate specialties, the authors found that higher spending by physicians was associated with reduced malpractice claims the following year. This pattern held true for six of the seven specialties, family practitioners being the sole exception.
For example, among internists, the malpractice risk probability was reduced from 1.5% in the bottom spending fifth ($19,725 per admission) to 0.3% in the top fifth ($39,379 per admission). Among obstetricians, a separate subgroup analysis of cesarean-section rates revealed that malpractice claims were approximately halved among obstetricians with rates in the highest fifth, compared with the lowest fifth. These results comport with previous reports of higher C-section rates in obstetricians who perceived themselves at higher malpractice risk, although other studies have found no correlation or an actual lower rate.
In concluding that higher resource use by physicians was associated with fewer malpractice claims, the authors acknowledged that a principal limitation of the study was the lack of information on illness severity. Importantly, they were unable to state whether higher spending was defensively motivated. A companion editorial questioned whether increased resource expenditure was a bona fide reflection of defensive medicine or may simply have resulted in fewer errors and adverse events.9
Unfortunately, the past malpractice experience of the doctors, which could provide insight into more defensive postures, better communication, etc., was not measured in the study. In addition, claims made just 1 year after an incident may not accurately reflect the real-world situation, where the filing of a lawsuit may lag any alleged negligence by a much longer period, especially in obstetric cases.
Worryingly, the results of this timely study may be used to imply that the more doctors spend, the less likely they are to be sued – a troubling notion in our current race to stem rising health care costs.
References
1. JAMA. 2005 Jun 1;293(21):2609-17.
2. Ann Emerg Med. 2005 Dec;46(6):525-33.
3. J Health Polit Policy Law. 1996 Summer;21(2):267-88.
4. Am J Orthop (Belle Mead NJ). 2012 Feb;41(2):69-73.
5. JAMA. 1987 May 22-29;257(20):2776-81.
6. Q J Econ. 1996 May; 111(2):353-90.
7. J Am Health Policy. 1994 Jul-Aug;4(4):7-15.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: Which of the following choices is best?
A. Controversy exists over whether defensive medicine is widely practiced and whether it raises health care costs.
B. Everyone agrees that defensive medicine is widely practiced.
C. Doctors who spend more for their hospitalized patients have been reported to face a lower malpractice risk.
D. A and C.
E. B and C.
Answer: D. Virtually all doctors admit they practice defensive medicine, which describes medical care specifically directed to attenuate the threat of malpractice liability rather than for a proper medical indication. Survey studies generally put the prevalence at greater than 90%, but what separates true defensive medicine from careful practice or patient expectation/demand remains controversial.
A mail survey of 824 physicians in high-risk specialties in Pennsylvania, a state where doctors pay high malpractice premiums, revealed that nearly all reported practicing defensive medicine. The respondents admitted to both assurance behavior – such as ordering more tests, especially imaging studies – as well as avoidance behavior – that is, restricting or eliminating complex procedures or perceived litigious patients.1
In another study, emergency physicians in the upper third of “malpractice fear” used more diagnostic tests and were more likely to hospitalize patients at low risk for coronary artery disease.2
On the other hand, a report using simulated clinical scenarios concluded that the extent of defensive medicine was at most 8%, and another found no correlation between individual malpractice claims experience and resource use, physician concern about malpractice, tolerance for uncertainty, or perception of risk.3
Another area of contention is whether some of our soaring health care costs may reflect defensive medicine at play.
A recent survey of 2,000 U.S. orthopedic surgeons found that 96% admitted practicing defensive medicine, with 24% of all ordered tests being for defensive reasons. The authors estimated that this amounted to about $100,000 per surgeon per year, or a total annual sum of $2 billion for the 20,400 orthopedic surgeons in the U.S.4
By correlating professional liability insurance with cost of services, the AMA estimated that in the 1980s, defensive medicine cost $12.1 billion to $13.7 billion each year.5 In an oft-cited study by Kessler and McClellan, the authors measured the effects of malpractice liability reforms using data from elderly Medicare beneficiaries treated for serious heart disease.6 They found that reforms that directly reduced provider liability pressure led to reductions of 5%-9% in medical expenditures. If such Medicare savings, which amounted to $600 million per year for cardiac disease, were extrapolated across the health care system, the annual savings would total $50 billion.
A more conservative study estimated that systemwide savings from aggressive malpractice reform would approach $41 billion over 5 years.7
Dr. Anupam B. Jena and his coauthors are the latest investigators seeking to clarify the correlation between defensive medicine and health care costs.8 Using Florida hospital admission data from 2000-2009, which covered some 24,000 physicians in seven separate specialties, the authors found that higher spending by physicians was associated with reduced malpractice claims the following year. This pattern held true for six of the seven specialties, family practitioners being the sole exception.
For example, among internists, the malpractice risk probability was reduced from 1.5% in the bottom spending fifth ($19,725 per admission) to 0.3% in the top fifth ($39,379 per admission). Among obstetricians, a separate subgroup analysis of cesarean-section rates revealed that malpractice claims were approximately halved among obstetricians with rates in the highest fifth, compared with the lowest fifth. These results comport with previous reports of higher C-section rates in obstetricians who perceived themselves at higher malpractice risk, although other studies have found no correlation or an actual lower rate.
In concluding that higher resource use by physicians was associated with fewer malpractice claims, the authors acknowledged that a principal limitation of the study was the lack of information on illness severity. Importantly, they were unable to state whether higher spending was defensively motivated. A companion editorial questioned whether increased resource expenditure was a bona fide reflection of defensive medicine or may simply have resulted in fewer errors and adverse events.9
Unfortunately, the past malpractice experience of the doctors, which could provide insight into more defensive postures, better communication, etc., was not measured in the study. In addition, claims made just 1 year after an incident may not accurately reflect the real-world situation, where the filing of a lawsuit may lag any alleged negligence by a much longer period, especially in obstetric cases.
Worryingly, the results of this timely study may be used to imply that the more doctors spend, the less likely they are to be sued – a troubling notion in our current race to stem rising health care costs.
References
1. JAMA. 2005 Jun 1;293(21):2609-17.
2. Ann Emerg Med. 2005 Dec;46(6):525-33.
3. J Health Polit Policy Law. 1996 Summer;21(2):267-88.
4. Am J Orthop (Belle Mead NJ). 2012 Feb;41(2):69-73.
5. JAMA. 1987 May 22-29;257(20):2776-81.
6. Q J Econ. 1996 May; 111(2):353-90.
7. J Am Health Policy. 1994 Jul-Aug;4(4):7-15.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: Which of the following choices is best?
A. Controversy exists over whether defensive medicine is widely practiced and whether it raises health care costs.
B. Everyone agrees that defensive medicine is widely practiced.
C. Doctors who spend more for their hospitalized patients have been reported to face a lower malpractice risk.
D. A and C.
E. B and C.
Answer: D. Virtually all doctors admit they practice defensive medicine, which describes medical care specifically directed to attenuate the threat of malpractice liability rather than for a proper medical indication. Survey studies generally put the prevalence at greater than 90%, but what separates true defensive medicine from careful practice or patient expectation/demand remains controversial.
A mail survey of 824 physicians in high-risk specialties in Pennsylvania, a state where doctors pay high malpractice premiums, revealed that nearly all reported practicing defensive medicine. The respondents admitted to both assurance behavior – such as ordering more tests, especially imaging studies – as well as avoidance behavior – that is, restricting or eliminating complex procedures or perceived litigious patients.1
In another study, emergency physicians in the upper third of “malpractice fear” used more diagnostic tests and were more likely to hospitalize patients at low risk for coronary artery disease.2
On the other hand, a report using simulated clinical scenarios concluded that the extent of defensive medicine was at most 8%, and another found no correlation between individual malpractice claims experience and resource use, physician concern about malpractice, tolerance for uncertainty, or perception of risk.3
Another area of contention is whether some of our soaring health care costs may reflect defensive medicine at play.
A recent survey of 2,000 U.S. orthopedic surgeons found that 96% admitted practicing defensive medicine, with 24% of all ordered tests being for defensive reasons. The authors estimated that this amounted to about $100,000 per surgeon per year, or a total annual sum of $2 billion for the 20,400 orthopedic surgeons in the U.S.4
By correlating professional liability insurance with cost of services, the AMA estimated that in the 1980s, defensive medicine cost $12.1 billion to $13.7 billion each year.5 In an oft-cited study by Kessler and McClellan, the authors measured the effects of malpractice liability reforms using data from elderly Medicare beneficiaries treated for serious heart disease.6 They found that reforms that directly reduced provider liability pressure led to reductions of 5%-9% in medical expenditures. If such Medicare savings, which amounted to $600 million per year for cardiac disease, were extrapolated across the health care system, the annual savings would total $50 billion.
A more conservative study estimated that systemwide savings from aggressive malpractice reform would approach $41 billion over 5 years.7
Dr. Anupam B. Jena and his coauthors are the latest investigators seeking to clarify the correlation between defensive medicine and health care costs.8 Using Florida hospital admission data from 2000-2009, which covered some 24,000 physicians in seven separate specialties, the authors found that higher spending by physicians was associated with reduced malpractice claims the following year. This pattern held true for six of the seven specialties, family practitioners being the sole exception.
For example, among internists, the malpractice risk probability was reduced from 1.5% in the bottom spending fifth ($19,725 per admission) to 0.3% in the top fifth ($39,379 per admission). Among obstetricians, a separate subgroup analysis of cesarean-section rates revealed that malpractice claims were approximately halved among obstetricians with rates in the highest fifth, compared with the lowest fifth. These results comport with previous reports of higher C-section rates in obstetricians who perceived themselves at higher malpractice risk, although other studies have found no correlation or an actual lower rate.
In concluding that higher resource use by physicians was associated with fewer malpractice claims, the authors acknowledged that a principal limitation of the study was the lack of information on illness severity. Importantly, they were unable to state whether higher spending was defensively motivated. A companion editorial questioned whether increased resource expenditure was a bona fide reflection of defensive medicine or may simply have resulted in fewer errors and adverse events.9
Unfortunately, the past malpractice experience of the doctors, which could provide insight into more defensive postures, better communication, etc., was not measured in the study. In addition, claims made just 1 year after an incident may not accurately reflect the real-world situation, where the filing of a lawsuit may lag any alleged negligence by a much longer period, especially in obstetric cases.
Worryingly, the results of this timely study may be used to imply that the more doctors spend, the less likely they are to be sued – a troubling notion in our current race to stem rising health care costs.
References
1. JAMA. 2005 Jun 1;293(21):2609-17.
2. Ann Emerg Med. 2005 Dec;46(6):525-33.
3. J Health Polit Policy Law. 1996 Summer;21(2):267-88.
4. Am J Orthop (Belle Mead NJ). 2012 Feb;41(2):69-73.
5. JAMA. 1987 May 22-29;257(20):2776-81.
6. Q J Econ. 1996 May; 111(2):353-90.
7. J Am Health Policy. 1994 Jul-Aug;4(4):7-15.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Oral contraception and medical liability
Question: Oral contraceptives are prescription drugs sold with highly specific manufacturer instructions on how and when to take them, because the sequence of pill ingestion is critical to their anovulatory efficacy.
Suppose a manufacturing mishap resulted in improper labeling and sequencing of the pills, and some women, relying on the product, became pregnant. In a lawsuit against the manufacturer, which of the following choices is best?
A. This is a case of product liability.
B. Affected plaintiffs should consider filing a class-action lawsuit.
C. Mothers can sue for wrongful pregnancy.
D. Children can sue for wrongful life.
E. All are possible legal causes of action.
Answer: E. This hypothetical is adapted from a recent report that the use of mispackaged oral contraceptives had resulted in more than 100 women becoming pregnant. The prescription drugs, available in blister packs, were erroneously sequenced such that the daily use of active or inactive drug was asynchronous with the woman’s ovulatory cycle, thus foiling the drug’s pregnancy prevention efficacy.
Typically, each packet of oral contraceptives comes with 28 days’ worth of color-coded pills, with the first 21 containing the active principle to inhibit ovulation, followed by 7 inert pills. Each monthly pack begins with the same strict pill sequence.
In 2011, the manufacturer of several brands of oral contraceptives recalled half a million such packs when it was discovered that some of them had the pill sequence reversed. Foreseeably, this debacle resulted in a number of unplanned pregnancies – and live births. Legal action soon followed.
▶ Product liability: A simple negligence lawsuit would typically cover a situation in which a wrongdoer has breached the requisite standard of care, as appears to be the case here. However, when a product such as a prescription drug leads to “harm,” an injured party, using the law of product liability, can sue the manufacturer that had placed it into the stream of commerce. This allows the plaintiff to rely on legal theories other than negligence, including breach of warranty and strict liability.
Under the latter legal theory, there is no need to prove fault or contractual breach, and the significant part of the complaint is whether the product is both defective and unreasonably dangerous. “Defective” is usually defined as product quality that is less than what a reasonable consumer expects, and “unreasonably dangerous” is a conclusion that the risks that result from its condition outweigh the product’s advantages.
Although the medication itself in this case is not defective or unreasonably dangerous, the assembly and labeling fiasco would suffice to keep the lawsuit within the product liability category. According to Section 102(2) of the Uniform Product Liability Act, product liability includes “all claims or action brought for personal injury, death, or property damage caused by the manufacture, design, formula, preparation, assembly, installation, testing, warnings, instructions, marketing, packaging, or labeling of any product.”
▶ Class action: A class action lawsuit, governed by Rule 23 of the Federal Rules of Civil Procedure, describes a legal cause of action where a representative plaintiff asserts claims on behalf of a large class of similarly injured members, who then give up their rights to pursue an individual lawsuit. It confers several advantages upon the plaintiffs, including the potential of higher damages.
However, four prerequisites must be present before a lawsuit can be certified a class action: numerosity, commonality, typicality, and adequacy.
Although there is the possibility of going forward with a class action suit, a federal judge in Georgia refused to certify class action status in the 2011 recall case. The judge stated that only 53 of the half-million recalled blister packs had the pills arranged in reverse order, and each woman’s case should be individually adjudicated given the controlling laws in her state, the need to prove use of the product, and whether she became pregnant and carried the pregnancy to term.
▶ Wrongful life: Strictly speaking, tort issues in this case can be divided into two categories: wrongful pregnancy (sometimes confusingly referred to as wrongful birth) alleged by the mother, and wrongful life by the child. Unfortunately, these claims are frequently lumped together under the rubric of wrongful life.
The women affected by this mix-up are reportedly seeking damages for lost income, medical costs, and, in some cases, the cost of raising their children, including the cost of college. However, the common law has traditionally barred a wrongful life action, although state laws have evolved over the years. So, court decisions and statutes in each state should be carefully consulted for any individual case.
The prime reason for disallowing a wrongful life action is that life, even if imperfect, is always preferable to non-life. Besides, it will be impossible to assess the quantum of damages, because this necessarily requires placing a monetary worth on human existence.
The seminal case is the 1967 New Jersey decision of Gleitman v. Cosgrove (227 A.2d 689 [N.J. 1967]), but the state’s position has since changed. In Berman v. Allan (404 A.2d 8 [N.J. 1979]), the court allowed damages for maternal emotional distress, though not for medical and other expenses of raising the child.
Overall, the law of wrongful life appears to be increasingly willing to award damages to the mother for the physical, emotional, and financial costs of pregnancy and delivery, but not the cost associated with the normal rearing of a healthy child.
The legal situation is quite different for a lawsuit filed by the child, who in essence is arguing that he/she should not have been born at all. Courts continue to refuse a claim brought by a healthy infant for wrongful life, adopting the reasoning in Berman that the infant has not suffered any damage cognizable at law by being brought into existence. Even an infant with birth disabilities will not prevail in the majority of jurisdictions, with California being a notable exception.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: Oral contraceptives are prescription drugs sold with highly specific manufacturer instructions on how and when to take them, because the sequence of pill ingestion is critical to their anovulatory efficacy.
Suppose a manufacturing mishap resulted in improper labeling and sequencing of the pills, and some women, relying on the product, became pregnant. In a lawsuit against the manufacturer, which of the following choices is best?
A. This is a case of product liability.
B. Affected plaintiffs should consider filing a class-action lawsuit.
C. Mothers can sue for wrongful pregnancy.
D. Children can sue for wrongful life.
E. All are possible legal causes of action.
Answer: E. This hypothetical is adapted from a recent report that the use of mispackaged oral contraceptives had resulted in more than 100 women becoming pregnant. The prescription drugs, available in blister packs, were erroneously sequenced such that the daily use of active or inactive drug was asynchronous with the woman’s ovulatory cycle, thus foiling the drug’s pregnancy prevention efficacy.
Typically, each packet of oral contraceptives comes with 28 days’ worth of color-coded pills, with the first 21 containing the active principle to inhibit ovulation, followed by 7 inert pills. Each monthly pack begins with the same strict pill sequence.
In 2011, the manufacturer of several brands of oral contraceptives recalled half a million such packs when it was discovered that some of them had the pill sequence reversed. Foreseeably, this debacle resulted in a number of unplanned pregnancies – and live births. Legal action soon followed.
▶ Product liability: A simple negligence lawsuit would typically cover a situation in which a wrongdoer has breached the requisite standard of care, as appears to be the case here. However, when a product such as a prescription drug leads to “harm,” an injured party, using the law of product liability, can sue the manufacturer that had placed it into the stream of commerce. This allows the plaintiff to rely on legal theories other than negligence, including breach of warranty and strict liability.
Under the latter legal theory, there is no need to prove fault or contractual breach, and the significant part of the complaint is whether the product is both defective and unreasonably dangerous. “Defective” is usually defined as product quality that is less than what a reasonable consumer expects, and “unreasonably dangerous” is a conclusion that the risks that result from its condition outweigh the product’s advantages.
Although the medication itself in this case is not defective or unreasonably dangerous, the assembly and labeling fiasco would suffice to keep the lawsuit within the product liability category. According to Section 102(2) of the Uniform Product Liability Act, product liability includes “all claims or action brought for personal injury, death, or property damage caused by the manufacture, design, formula, preparation, assembly, installation, testing, warnings, instructions, marketing, packaging, or labeling of any product.”
▶ Class action: A class action lawsuit, governed by Rule 23 of the Federal Rules of Civil Procedure, describes a legal cause of action where a representative plaintiff asserts claims on behalf of a large class of similarly injured members, who then give up their rights to pursue an individual lawsuit. It confers several advantages upon the plaintiffs, including the potential of higher damages.
However, four prerequisites must be present before a lawsuit can be certified a class action: numerosity, commonality, typicality, and adequacy.
Although there is the possibility of going forward with a class action suit, a federal judge in Georgia refused to certify class action status in the 2011 recall case. The judge stated that only 53 of the half-million recalled blister packs had the pills arranged in reverse order, and each woman’s case should be individually adjudicated given the controlling laws in her state, the need to prove use of the product, and whether she became pregnant and carried the pregnancy to term.
▶ Wrongful life: Strictly speaking, tort issues in this case can be divided into two categories: wrongful pregnancy (sometimes confusingly referred to as wrongful birth) alleged by the mother, and wrongful life by the child. Unfortunately, these claims are frequently lumped together under the rubric of wrongful life.
The women affected by this mix-up are reportedly seeking damages for lost income, medical costs, and, in some cases, the cost of raising their children, including the cost of college. However, the common law has traditionally barred a wrongful life action, although state laws have evolved over the years. So, court decisions and statutes in each state should be carefully consulted for any individual case.
The prime reason for disallowing a wrongful life action is that life, even if imperfect, is always preferable to non-life. Besides, it will be impossible to assess the quantum of damages, because this necessarily requires placing a monetary worth on human existence.
The seminal case is the 1967 New Jersey decision of Gleitman v. Cosgrove (227 A.2d 689 [N.J. 1967]), but the state’s position has since changed. In Berman v. Allan (404 A.2d 8 [N.J. 1979]), the court allowed damages for maternal emotional distress, though not for medical and other expenses of raising the child.
Overall, the law of wrongful life appears to be increasingly willing to award damages to the mother for the physical, emotional, and financial costs of pregnancy and delivery, but not the cost associated with the normal rearing of a healthy child.
The legal situation is quite different for a lawsuit filed by the child, who in essence is arguing that he/she should not have been born at all. Courts continue to refuse a claim brought by a healthy infant for wrongful life, adopting the reasoning in Berman that the infant has not suffered any damage cognizable at law by being brought into existence. Even an infant with birth disabilities will not prevail in the majority of jurisdictions, with California being a notable exception.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: Oral contraceptives are prescription drugs sold with highly specific manufacturer instructions on how and when to take them, because the sequence of pill ingestion is critical to their anovulatory efficacy.
Suppose a manufacturing mishap resulted in improper labeling and sequencing of the pills, and some women, relying on the product, became pregnant. In a lawsuit against the manufacturer, which of the following choices is best?
A. This is a case of product liability.
B. Affected plaintiffs should consider filing a class-action lawsuit.
C. Mothers can sue for wrongful pregnancy.
D. Children can sue for wrongful life.
E. All are possible legal causes of action.
Answer: E. This hypothetical is adapted from a recent report that the use of mispackaged oral contraceptives had resulted in more than 100 women becoming pregnant. The prescription drugs, available in blister packs, were erroneously sequenced such that the daily use of active or inactive drug was asynchronous with the woman’s ovulatory cycle, thus foiling the drug’s pregnancy prevention efficacy.
Typically, each packet of oral contraceptives comes with 28 days’ worth of color-coded pills, with the first 21 containing the active principle to inhibit ovulation, followed by 7 inert pills. Each monthly pack begins with the same strict pill sequence.
In 2011, the manufacturer of several brands of oral contraceptives recalled half a million such packs when it was discovered that some of them had the pill sequence reversed. Foreseeably, this debacle resulted in a number of unplanned pregnancies – and live births. Legal action soon followed.
▶ Product liability: A simple negligence lawsuit would typically cover a situation in which a wrongdoer has breached the requisite standard of care, as appears to be the case here. However, when a product such as a prescription drug leads to “harm,” an injured party, using the law of product liability, can sue the manufacturer that had placed it into the stream of commerce. This allows the plaintiff to rely on legal theories other than negligence, including breach of warranty and strict liability.
Under the latter legal theory, there is no need to prove fault or contractual breach, and the significant part of the complaint is whether the product is both defective and unreasonably dangerous. “Defective” is usually defined as product quality that is less than what a reasonable consumer expects, and “unreasonably dangerous” is a conclusion that the risks that result from its condition outweigh the product’s advantages.
Although the medication itself in this case is not defective or unreasonably dangerous, the assembly and labeling fiasco would suffice to keep the lawsuit within the product liability category. According to Section 102(2) of the Uniform Product Liability Act, product liability includes “all claims or action brought for personal injury, death, or property damage caused by the manufacture, design, formula, preparation, assembly, installation, testing, warnings, instructions, marketing, packaging, or labeling of any product.”
▶ Class action: A class action lawsuit, governed by Rule 23 of the Federal Rules of Civil Procedure, describes a legal cause of action where a representative plaintiff asserts claims on behalf of a large class of similarly injured members, who then give up their rights to pursue an individual lawsuit. It confers several advantages upon the plaintiffs, including the potential of higher damages.
However, four prerequisites must be present before a lawsuit can be certified a class action: numerosity, commonality, typicality, and adequacy.
Although there is the possibility of going forward with a class action suit, a federal judge in Georgia refused to certify class action status in the 2011 recall case. The judge stated that only 53 of the half-million recalled blister packs had the pills arranged in reverse order, and each woman’s case should be individually adjudicated given the controlling laws in her state, the need to prove use of the product, and whether she became pregnant and carried the pregnancy to term.
▶ Wrongful life: Strictly speaking, tort issues in this case can be divided into two categories: wrongful pregnancy (sometimes confusingly referred to as wrongful birth) alleged by the mother, and wrongful life by the child. Unfortunately, these claims are frequently lumped together under the rubric of wrongful life.
The women affected by this mix-up are reportedly seeking damages for lost income, medical costs, and, in some cases, the cost of raising their children, including the cost of college. However, the common law has traditionally barred a wrongful life action, although state laws have evolved over the years. So, court decisions and statutes in each state should be carefully consulted for any individual case.
The prime reason for disallowing a wrongful life action is that life, even if imperfect, is always preferable to non-life. Besides, it will be impossible to assess the quantum of damages, because this necessarily requires placing a monetary worth on human existence.
The seminal case is the 1967 New Jersey decision of Gleitman v. Cosgrove (227 A.2d 689 [N.J. 1967]), but the state’s position has since changed. In Berman v. Allan (404 A.2d 8 [N.J. 1979]), the court allowed damages for maternal emotional distress, though not for medical and other expenses of raising the child.
Overall, the law of wrongful life appears to be increasingly willing to award damages to the mother for the physical, emotional, and financial costs of pregnancy and delivery, but not the cost associated with the normal rearing of a healthy child.
The legal situation is quite different for a lawsuit filed by the child, who in essence is arguing that he/she should not have been born at all. Courts continue to refuse a claim brought by a healthy infant for wrongful life, adopting the reasoning in Berman that the infant has not suffered any damage cognizable at law by being brought into existence. Even an infant with birth disabilities will not prevail in the majority of jurisdictions, with California being a notable exception.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Law & Medicine: To whom do doctors owe a duty?
Question: A doctor may owe a duty of care in the setting of:
A. A cyber relationship.
B. A special relationship.
C. Both A and B.
D. Neither A nor B.
Answer: C. Ascertaining whether a defendant owes a duty to a claimant is the first inquiry in the tort of negligence. To say there is no duty owed is to deny liability altogether, however obvious the breach or horrendous the foreseeable injuries.
Thus, duty is used as a filter mechanism to reduce frivolous suits or otherwise control the tide of litigation, to prevent “liability in an indeterminate amount for an indeterminate time to an indeterminate class.”
Duty in the context of medical negligence is not usually in dispute, as it is plainly owed by a doctor to his or her patient. It arises out of the doctor-patient relationship. Whether a relationship has been formed in the first place is a threshold inquiry. Where a doctor accepts a patient who is seeking his or her services, the relationship is readily evident. Duty is also established when the doctor begins the evaluation process in a typical encounter.
However, a phone inquiry by a potential patient, without more, may be insufficient to create this relationship, although this may depend on the nature of the phone conversation and the doctor’s response.
Likewise, a “curbside” consultation sought by a colleague does not normally translate into a duty for the doctor offering the opinion. Presumably casual advice given freely and understood as such at social gatherings does not add up to a doctor-patient relationship, and courts will look to reasonableness as the touchstone in deciding whether such a relationship was ever formed.
Still, there are some medical situations where a legitimate question of duty can be raised. With the growth of electronic medical records and communication, medical encounters in cyberspace will emerge as an increasing source of litigation.
Internet liability can be far reaching. In addition to risks governing negligence, informed consent, and privacy/confidentiality, there are additional issues of product liability, cross-border jurisdictional conflicts, and others.
The threshold question when assessing cyberspace liability arising, for example, from the use of doctor-operated medical websites concerns duty, because its existence or denial will determine whether the case can go forward in the first place. Although not the typical office or hospital patient, a plaintiff may argue successfully that a doctor-patient relationship had nonetheless been formed in cyberspace.
It is possible that such a relationship will be found in some circumstances, relevant factors being knowledge of names of subscribers, frequency of interactions, specificity of queries, and so on. In particular, a subscription fee is likely to be construed as evidence of soliciting and accepting a more committed interaction, so it places the operator of the website at greater legal risk. A specific disclaimer is a standard precaution but may not be enough to definitively protect against a lawsuit.
Courts have ruled in favor of plaintiffs despite the absence of face-to-face interaction with a physician. In one case, a doctor speaking to a patient from the emergency department was deemed to have formed a doctor-patient relationship (O’Neill v. Montefiore Hospital, 11 A.D.2d 132 (N.Y.A.D. 1 Dept. 1960). In another, an on-call neurologist’s telephone advice to the treating doctor likewise raised the issue of legal duty (Lection v. Dyll, 65 S.W.3d 696 (Tex. App. Dallas 2001).
The state of Hawaii now permits telehealth services to be reimbursable, notwithstanding the absence of face-to-face contact (HI Rev Stat § 431:10A-116.3[a]). With this law, an online encounter will likely translate into a professional relationship – with corresponding legal duty of due care.
In the case of a Good Samaritan physician – i.e., one who offers gratuitous aid to a stranger in need of medical assistance – courts are unlikely to find a professional relationship, because there is no common law duty to help a stranger.
However, once treatment has begun, there is a duty not to make matters worse. So, all 50 states have enacted Good Samaritan statutes, which protect against liability arising out of negligent rescue. Note that statutory protection is generally excluded for Good Samaritan acts performed within a hospital setting, under the theory that doctors have an ongoing relationship with the hospital and are already obligated to provide emergency care within its walls.
Another category of legal duty concerns nonpatient third parties. The complaint may relate to a failure to warn family members of a patient’s contagious disease, or the transmissible condition may have been missed and an innocent third party was injured as a result.
Another situation where duty to a third party might arise is the learning of a credible threat of harm directed at a named individual. This is famously known as the Tarasoff doctrine, after a California case in which the court imposed a duty on a college psychologist to directly warn an intended victim of harm by his patient – even though that meant breaching confidentiality of a professional relationship, and the victim was a nonpatient third party (Tarasoff v. Regents of University of California, 551 P.2d 334 [Cal. 1976]).
A doctor may also incur liability for automobile injuries sustained by one other than his or her own patient. In a Hawaii case, a car suddenly veered across five lanes of traffic, striking an 11-year-old bystander. The driver alleged that the prescription medication prazosin caused him to lose control of the car.
In ruling that the health care provider was liable to the injured bystander, the Hawaii Supreme Court held that physicians have a duty to warn their patients of potential adverse medication effects, and this responsibility should extend to third parties (McKenzie v. Hawaii Permanente Medical Group, 47 P.3d 1209 [Haw. 2002]).
A foreseeable and unreasonable risk of harm is an important factor, but not the only decisive factor, in construing the existence of a legal duty. Under some circumstances, the term “special relationship” has been employed based on a consideration of “existing social values, customs, and considerations of policy.”
In a Massachusetts case, a family practitioner had failed to warn his patient of the risk of diabetic drugs when operating a vehicle. Just 45 minutes after the patient’s discharge from the hospital, he developed hypoglycemia, losing consciousness and injuring a motorcyclist who then sued the doctor. The court used the “special relationship” rationale in ruling that the doctor owed a duty to the motorcyclist (Arsenault v. McConarty, 21 Mass. L. Rptr. 500 [2006]).
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: A doctor may owe a duty of care in the setting of:
A. A cyber relationship.
B. A special relationship.
C. Both A and B.
D. Neither A nor B.
Answer: C. Ascertaining whether a defendant owes a duty to a claimant is the first inquiry in the tort of negligence. To say there is no duty owed is to deny liability altogether, however obvious the breach or horrendous the foreseeable injuries.
Thus, duty is used as a filter mechanism to reduce frivolous suits or otherwise control the tide of litigation, to prevent “liability in an indeterminate amount for an indeterminate time to an indeterminate class.”
Duty in the context of medical negligence is not usually in dispute, as it is plainly owed by a doctor to his or her patient. It arises out of the doctor-patient relationship. Whether a relationship has been formed in the first place is a threshold inquiry. Where a doctor accepts a patient who is seeking his or her services, the relationship is readily evident. Duty is also established when the doctor begins the evaluation process in a typical encounter.
However, a phone inquiry by a potential patient, without more, may be insufficient to create this relationship, although this may depend on the nature of the phone conversation and the doctor’s response.
Likewise, a “curbside” consultation sought by a colleague does not normally translate into a duty for the doctor offering the opinion. Presumably casual advice given freely and understood as such at social gatherings does not add up to a doctor-patient relationship, and courts will look to reasonableness as the touchstone in deciding whether such a relationship was ever formed.
Still, there are some medical situations where a legitimate question of duty can be raised. With the growth of electronic medical records and communication, medical encounters in cyberspace will emerge as an increasing source of litigation.
Internet liability can be far reaching. In addition to risks governing negligence, informed consent, and privacy/confidentiality, there are additional issues of product liability, cross-border jurisdictional conflicts, and others.
The threshold question when assessing cyberspace liability arising, for example, from the use of doctor-operated medical websites concerns duty, because its existence or denial will determine whether the case can go forward in the first place. Although not the typical office or hospital patient, a plaintiff may argue successfully that a doctor-patient relationship had nonetheless been formed in cyberspace.
It is possible that such a relationship will be found in some circumstances, relevant factors being knowledge of names of subscribers, frequency of interactions, specificity of queries, and so on. In particular, a subscription fee is likely to be construed as evidence of soliciting and accepting a more committed interaction, so it places the operator of the website at greater legal risk. A specific disclaimer is a standard precaution but may not be enough to definitively protect against a lawsuit.
Courts have ruled in favor of plaintiffs despite the absence of face-to-face interaction with a physician. In one case, a doctor speaking to a patient from the emergency department was deemed to have formed a doctor-patient relationship (O’Neill v. Montefiore Hospital, 11 A.D.2d 132 (N.Y.A.D. 1 Dept. 1960). In another, an on-call neurologist’s telephone advice to the treating doctor likewise raised the issue of legal duty (Lection v. Dyll, 65 S.W.3d 696 (Tex. App. Dallas 2001).
The state of Hawaii now permits telehealth services to be reimbursable, notwithstanding the absence of face-to-face contact (HI Rev Stat § 431:10A-116.3[a]). With this law, an online encounter will likely translate into a professional relationship – with corresponding legal duty of due care.
In the case of a Good Samaritan physician – i.e., one who offers gratuitous aid to a stranger in need of medical assistance – courts are unlikely to find a professional relationship, because there is no common law duty to help a stranger.
However, once treatment has begun, there is a duty not to make matters worse. So, all 50 states have enacted Good Samaritan statutes, which protect against liability arising out of negligent rescue. Note that statutory protection is generally excluded for Good Samaritan acts performed within a hospital setting, under the theory that doctors have an ongoing relationship with the hospital and are already obligated to provide emergency care within its walls.
Another category of legal duty concerns nonpatient third parties. The complaint may relate to a failure to warn family members of a patient’s contagious disease, or the transmissible condition may have been missed and an innocent third party was injured as a result.
Another situation where duty to a third party might arise is the learning of a credible threat of harm directed at a named individual. This is famously known as the Tarasoff doctrine, after a California case in which the court imposed a duty on a college psychologist to directly warn an intended victim of harm by his patient – even though that meant breaching confidentiality of a professional relationship, and the victim was a nonpatient third party (Tarasoff v. Regents of University of California, 551 P.2d 334 [Cal. 1976]).
A doctor may also incur liability for automobile injuries sustained by one other than his or her own patient. In a Hawaii case, a car suddenly veered across five lanes of traffic, striking an 11-year-old bystander. The driver alleged that the prescription medication prazosin caused him to lose control of the car.
In ruling that the health care provider was liable to the injured bystander, the Hawaii Supreme Court held that physicians have a duty to warn their patients of potential adverse medication effects, and this responsibility should extend to third parties (McKenzie v. Hawaii Permanente Medical Group, 47 P.3d 1209 [Haw. 2002]).
A foreseeable and unreasonable risk of harm is an important factor, but not the only decisive factor, in construing the existence of a legal duty. Under some circumstances, the term “special relationship” has been employed based on a consideration of “existing social values, customs, and considerations of policy.”
In a Massachusetts case, a family practitioner had failed to warn his patient of the risk of diabetic drugs when operating a vehicle. Just 45 minutes after the patient’s discharge from the hospital, he developed hypoglycemia, losing consciousness and injuring a motorcyclist who then sued the doctor. The court used the “special relationship” rationale in ruling that the doctor owed a duty to the motorcyclist (Arsenault v. McConarty, 21 Mass. L. Rptr. 500 [2006]).
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: A doctor may owe a duty of care in the setting of:
A. A cyber relationship.
B. A special relationship.
C. Both A and B.
D. Neither A nor B.
Answer: C. Ascertaining whether a defendant owes a duty to a claimant is the first inquiry in the tort of negligence. To say there is no duty owed is to deny liability altogether, however obvious the breach or horrendous the foreseeable injuries.
Thus, duty is used as a filter mechanism to reduce frivolous suits or otherwise control the tide of litigation, to prevent “liability in an indeterminate amount for an indeterminate time to an indeterminate class.”
Duty in the context of medical negligence is not usually in dispute, as it is plainly owed by a doctor to his or her patient. It arises out of the doctor-patient relationship. Whether a relationship has been formed in the first place is a threshold inquiry. Where a doctor accepts a patient who is seeking his or her services, the relationship is readily evident. Duty is also established when the doctor begins the evaluation process in a typical encounter.
However, a phone inquiry by a potential patient, without more, may be insufficient to create this relationship, although this may depend on the nature of the phone conversation and the doctor’s response.
Likewise, a “curbside” consultation sought by a colleague does not normally translate into a duty for the doctor offering the opinion. Presumably casual advice given freely and understood as such at social gatherings does not add up to a doctor-patient relationship, and courts will look to reasonableness as the touchstone in deciding whether such a relationship was ever formed.
Still, there are some medical situations where a legitimate question of duty can be raised. With the growth of electronic medical records and communication, medical encounters in cyberspace will emerge as an increasing source of litigation.
Internet liability can be far reaching. In addition to risks governing negligence, informed consent, and privacy/confidentiality, there are additional issues of product liability, cross-border jurisdictional conflicts, and others.
The threshold question when assessing cyberspace liability arising, for example, from the use of doctor-operated medical websites concerns duty, because its existence or denial will determine whether the case can go forward in the first place. Although not the typical office or hospital patient, a plaintiff may argue successfully that a doctor-patient relationship had nonetheless been formed in cyberspace.
It is possible that such a relationship will be found in some circumstances, relevant factors being knowledge of names of subscribers, frequency of interactions, specificity of queries, and so on. In particular, a subscription fee is likely to be construed as evidence of soliciting and accepting a more committed interaction, so it places the operator of the website at greater legal risk. A specific disclaimer is a standard precaution but may not be enough to definitively protect against a lawsuit.
Courts have ruled in favor of plaintiffs despite the absence of face-to-face interaction with a physician. In one case, a doctor speaking to a patient from the emergency department was deemed to have formed a doctor-patient relationship (O’Neill v. Montefiore Hospital, 11 A.D.2d 132 (N.Y.A.D. 1 Dept. 1960). In another, an on-call neurologist’s telephone advice to the treating doctor likewise raised the issue of legal duty (Lection v. Dyll, 65 S.W.3d 696 (Tex. App. Dallas 2001).
The state of Hawaii now permits telehealth services to be reimbursable, notwithstanding the absence of face-to-face contact (HI Rev Stat § 431:10A-116.3[a]). With this law, an online encounter will likely translate into a professional relationship – with corresponding legal duty of due care.
In the case of a Good Samaritan physician – i.e., one who offers gratuitous aid to a stranger in need of medical assistance – courts are unlikely to find a professional relationship, because there is no common law duty to help a stranger.
However, once treatment has begun, there is a duty not to make matters worse. So, all 50 states have enacted Good Samaritan statutes, which protect against liability arising out of negligent rescue. Note that statutory protection is generally excluded for Good Samaritan acts performed within a hospital setting, under the theory that doctors have an ongoing relationship with the hospital and are already obligated to provide emergency care within its walls.
Another category of legal duty concerns nonpatient third parties. The complaint may relate to a failure to warn family members of a patient’s contagious disease, or the transmissible condition may have been missed and an innocent third party was injured as a result.
Another situation where duty to a third party might arise is the learning of a credible threat of harm directed at a named individual. This is famously known as the Tarasoff doctrine, after a California case in which the court imposed a duty on a college psychologist to directly warn an intended victim of harm by his patient – even though that meant breaching confidentiality of a professional relationship, and the victim was a nonpatient third party (Tarasoff v. Regents of University of California, 551 P.2d 334 [Cal. 1976]).
A doctor may also incur liability for automobile injuries sustained by one other than his or her own patient. In a Hawaii case, a car suddenly veered across five lanes of traffic, striking an 11-year-old bystander. The driver alleged that the prescription medication prazosin caused him to lose control of the car.
In ruling that the health care provider was liable to the injured bystander, the Hawaii Supreme Court held that physicians have a duty to warn their patients of potential adverse medication effects, and this responsibility should extend to third parties (McKenzie v. Hawaii Permanente Medical Group, 47 P.3d 1209 [Haw. 2002]).
A foreseeable and unreasonable risk of harm is an important factor, but not the only decisive factor, in construing the existence of a legal duty. Under some circumstances, the term “special relationship” has been employed based on a consideration of “existing social values, customs, and considerations of policy.”
In a Massachusetts case, a family practitioner had failed to warn his patient of the risk of diabetic drugs when operating a vehicle. Just 45 minutes after the patient’s discharge from the hospital, he developed hypoglycemia, losing consciousness and injuring a motorcyclist who then sued the doctor. The court used the “special relationship” rationale in ruling that the doctor owed a duty to the motorcyclist (Arsenault v. McConarty, 21 Mass. L. Rptr. 500 [2006]).
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Was this CT with contrast unnecessary—and harmful? ... Patient dies after being prescribed opioids right after detoxification
Was this CT with contrast unnecessary—and harmful?
A 52-YEAR-OLD WOMAN presented to the emergency department (ED) with leg pain and vaginal bleeding. The ED physicians ordered a computed tomography (CT) scan with contrast. Following the administration of the contrast dye, the patient’s blood pressure spiked and a brain aneurysm ruptured. The patient immediately underwent cranial surgery and recovered well. However, she still suffers from paralysis, cognitive issues, and weakness in her left arm and leg. She has been unable to return to her job.
PLAINTIFF’S CLAIM The doctors ran several unnecessary tests, including the CT scan, which caused her to have an allergic reaction.
THE DEFENSE The CT scan was necessary to rule out a stomach abscess, and the ruptured aneurysm was caused by her medical condition and not the dye.
VERDICT $3.62 million New Jersey verdict.
COMMENT Here is a sober reminder that doing more tests does not protect one from litigation. We are not told enough in this short report to know if there was a legitimate indication for a CT scan, but the large award suggests there was not. The Choosing Wisely campaign (http://www.choosingwisely.org), which has a goal of “advancing a national dialogue on avoiding wasteful or unnecessary medical tests, treatments and procedures,” is not just about saving money—it is about practicing medicine appropriately.
Patient dies after being prescribed opioids right after detoxification
A 52-YEAR-OLD WOMAN had been going to the same physician for 17 years. While she was under his care, she had been prescribed various narcotics, benzodiazepines, and barbiturates, and she had become addicted to them. The patient suffered a fall at home that was allegedly caused by an overdose of these medications. During a 3-week hospitalization after her fall, the woman went through a detoxification protocol to ease her dependence on the drugs. During her next appointment with her physician, he prescribed alprazolam and morphine sulfate daily. A week later, the woman died, allegedly due to an overdose of the alprazolam and morphine sulfate.
PLAINTIFF’S CLAIM The defendant’s failure to investigate the reason for the decedent’s hospitalization violated the standard of care. If the physician had inquired about his patient’s recent hospitalization, he would have been told about her detoxification, and wouldn’t have prescribed her any potentially addictive drugs.
THE DEFENSE The physician admitted that if he had known about his patient’s detoxification, he would not have prescribed her any medication. However, the doctor in charge of overseeing the detoxification told the patient not to see the defendant again, and not to take any prescriptions from him.
VERDICT $156,853 Illinois verdict.
COMMENT There is good reason to be wary of prescribing strong opioids and benzodiazepines for chronic pain in primary care practice. With the sharp increase in overdose deaths from opioids and the marginal evidence, at best, that supports the use of opioids for chronic, nonmalignant pain, such patients should—in my opinion—be managed directly in a pain/addiction program, or in close collaboration with one.
State Boards of Medicine are becoming appropriately stringent about opioids, so don’t risk losing your medical license or being sued. Use narcotic-use contracts, random drug testing, and co-management, and check your state narcotic prescribing database regularly if you treat chronic pain patients.
Was this CT with contrast unnecessary—and harmful?
A 52-YEAR-OLD WOMAN presented to the emergency department (ED) with leg pain and vaginal bleeding. The ED physicians ordered a computed tomography (CT) scan with contrast. Following the administration of the contrast dye, the patient’s blood pressure spiked and a brain aneurysm ruptured. The patient immediately underwent cranial surgery and recovered well. However, she still suffers from paralysis, cognitive issues, and weakness in her left arm and leg. She has been unable to return to her job.
PLAINTIFF’S CLAIM The doctors ran several unnecessary tests, including the CT scan, which caused her to have an allergic reaction.
THE DEFENSE The CT scan was necessary to rule out a stomach abscess, and the ruptured aneurysm was caused by her medical condition and not the dye.
VERDICT $3.62 million New Jersey verdict.
COMMENT Here is a sober reminder that doing more tests does not protect one from litigation. We are not told enough in this short report to know if there was a legitimate indication for a CT scan, but the large award suggests there was not. The Choosing Wisely campaign (http://www.choosingwisely.org), which has a goal of “advancing a national dialogue on avoiding wasteful or unnecessary medical tests, treatments and procedures,” is not just about saving money—it is about practicing medicine appropriately.
Patient dies after being prescribed opioids right after detoxification
A 52-YEAR-OLD WOMAN had been going to the same physician for 17 years. While she was under his care, she had been prescribed various narcotics, benzodiazepines, and barbiturates, and she had become addicted to them. The patient suffered a fall at home that was allegedly caused by an overdose of these medications. During a 3-week hospitalization after her fall, the woman went through a detoxification protocol to ease her dependence on the drugs. During her next appointment with her physician, he prescribed alprazolam and morphine sulfate daily. A week later, the woman died, allegedly due to an overdose of the alprazolam and morphine sulfate.
PLAINTIFF’S CLAIM The defendant’s failure to investigate the reason for the decedent’s hospitalization violated the standard of care. If the physician had inquired about his patient’s recent hospitalization, he would have been told about her detoxification, and wouldn’t have prescribed her any potentially addictive drugs.
THE DEFENSE The physician admitted that if he had known about his patient’s detoxification, he would not have prescribed her any medication. However, the doctor in charge of overseeing the detoxification told the patient not to see the defendant again, and not to take any prescriptions from him.
VERDICT $156,853 Illinois verdict.
COMMENT There is good reason to be wary of prescribing strong opioids and benzodiazepines for chronic pain in primary care practice. With the sharp increase in overdose deaths from opioids and the marginal evidence, at best, that supports the use of opioids for chronic, nonmalignant pain, such patients should—in my opinion—be managed directly in a pain/addiction program, or in close collaboration with one.
State Boards of Medicine are becoming appropriately stringent about opioids, so don’t risk losing your medical license or being sued. Use narcotic-use contracts, random drug testing, and co-management, and check your state narcotic prescribing database regularly if you treat chronic pain patients.
Was this CT with contrast unnecessary—and harmful?
A 52-YEAR-OLD WOMAN presented to the emergency department (ED) with leg pain and vaginal bleeding. The ED physicians ordered a computed tomography (CT) scan with contrast. Following the administration of the contrast dye, the patient’s blood pressure spiked and a brain aneurysm ruptured. The patient immediately underwent cranial surgery and recovered well. However, she still suffers from paralysis, cognitive issues, and weakness in her left arm and leg. She has been unable to return to her job.
PLAINTIFF’S CLAIM The doctors ran several unnecessary tests, including the CT scan, which caused her to have an allergic reaction.
THE DEFENSE The CT scan was necessary to rule out a stomach abscess, and the ruptured aneurysm was caused by her medical condition and not the dye.
VERDICT $3.62 million New Jersey verdict.
COMMENT Here is a sober reminder that doing more tests does not protect one from litigation. We are not told enough in this short report to know if there was a legitimate indication for a CT scan, but the large award suggests there was not. The Choosing Wisely campaign (http://www.choosingwisely.org), which has a goal of “advancing a national dialogue on avoiding wasteful or unnecessary medical tests, treatments and procedures,” is not just about saving money—it is about practicing medicine appropriately.
Patient dies after being prescribed opioids right after detoxification
A 52-YEAR-OLD WOMAN had been going to the same physician for 17 years. While she was under his care, she had been prescribed various narcotics, benzodiazepines, and barbiturates, and she had become addicted to them. The patient suffered a fall at home that was allegedly caused by an overdose of these medications. During a 3-week hospitalization after her fall, the woman went through a detoxification protocol to ease her dependence on the drugs. During her next appointment with her physician, he prescribed alprazolam and morphine sulfate daily. A week later, the woman died, allegedly due to an overdose of the alprazolam and morphine sulfate.
PLAINTIFF’S CLAIM The defendant’s failure to investigate the reason for the decedent’s hospitalization violated the standard of care. If the physician had inquired about his patient’s recent hospitalization, he would have been told about her detoxification, and wouldn’t have prescribed her any potentially addictive drugs.
THE DEFENSE The physician admitted that if he had known about his patient’s detoxification, he would not have prescribed her any medication. However, the doctor in charge of overseeing the detoxification told the patient not to see the defendant again, and not to take any prescriptions from him.
VERDICT $156,853 Illinois verdict.
COMMENT There is good reason to be wary of prescribing strong opioids and benzodiazepines for chronic pain in primary care practice. With the sharp increase in overdose deaths from opioids and the marginal evidence, at best, that supports the use of opioids for chronic, nonmalignant pain, such patients should—in my opinion—be managed directly in a pain/addiction program, or in close collaboration with one.
State Boards of Medicine are becoming appropriately stringent about opioids, so don’t risk losing your medical license or being sued. Use narcotic-use contracts, random drug testing, and co-management, and check your state narcotic prescribing database regularly if you treat chronic pain patients.
Midair medical emergencies
Question: One hour into an Air France international flight out of New York, Dr. Internist responded to a call for emergency medical assistance. A U.S. passenger had briefly passed out but then appeared to recover. Dr. Internist made a tentative diagnosis of a transient ischemic attack, but did not think an immediate divert was necessary. Based on the doctor’s assessment, the pilot continued on the previously scheduled flight path, landing several hours later in Paris. Meanwhile, the passenger’s condition worsened, and he expired shortly after arrival.
Which of the following statements is correct?
A. Under the common law, there is no legal duty to aid a stranger in distress; but under French law, a doctor is legally obligated to provide emergency assistance.
B. The U.S. federal Aviation Medical Assistance Act may immunize the doctor against liability for negligence during a midair medical emergency.
C. A tort action may still lie against the airline, notwithstanding the doctor’s advice not to divert.
D. Expect jurisdictional conflicts in the event there is a lawsuit.
E. All are correct.
Answer: E. Under the common law, there is no legal duty for anyone, even a doctor, to come to the aid of a stranger. However, doctors are generally held to have an ethical duty to offer emergency care. The American Medical Association’s Code of Medical Ethics states: “Physicians are free to choose whom they will serve. The physician should, however, respond to the best of his or her ability in cases of emergency where first aid treatment is essential.”1
In contrast, Australia and most civil law jurisdictions, e.g., many European countries, impose a legal obligation to render assistance. Under French law, for example, failure to render assistance to a person in urgent need of help can be met with fines of up to 75,000 euros and 5 years imprisonment.
Medical “emergencies” occur in roughly 1 of every 600 flights, which may be an underestimate because of underreporting. The most common medical reasons for aircraft diversion are cardiac, respiratory, and neurologic emergencies. According to a recent review in the New England Journal of Medicine, the decision to divert lies solely with the captain of the aircraft, who must also consider factors such as fuel, costs, the ability to land, and the medical resources available at that airport.2 The review also summarizes medical steps to be taken during midair medical emergencies.
Two related laws other than international aviation treaties govern medical liability during commercial flights: the generic “Good Samaritan” statute, which all 50 U.S. states have enacted, and the more specific federal Aviation Medical Assistance Act.
In 1959, California enacted the first Good Samaritan statute, whose intent is to encourage the helping of people in distress. In general, the law protects against liability arising out of nonreimbursed negligent rescue, but it does not affirmatively require doctors to come to the aid of strangers. Vermont, however, is an exception, and imposes a legal duty to assist a victim in need.
Typically, there is legal immunity against ordinary negligence but not gross misconduct, although California appears to excuse even gross negligence so long as the act was done in good faith. In a litigated case, a California court eloquently declared: “The goodness of the Samaritan is a description of the quality of his or her intention, not the quality of the aid delivered.”3
There is no universal definition of gross negligence, but the term frequently is equated with willful, wanton, or reckless conduct. One can think of gross negligence as aggravated negligence, involving more than mere mistake, inadvertence, or inattention, and representing highly unreasonable conduct or an extreme departure from ordinary care where a high degree of danger is apparent.4 An example may be an obviously inebriated physician attempting to provide treatment and causing harm to the victim.
However, the Good Samaritan statute, being state based, may not be applicable to scenarios with cross-border jurisdictional issues. The specific law that incorporates Good Samaritan assistance during commercial flights is the federal Aviation Medical Assistance Act (AMAA), which Congress enacted in 1998. In addition to Federal Aviation Administration mandates such as requisite medical supplies on board and training of flight crew, this federal law shields providers who respond to in-flight medical emergencies.
The AMAA covers claims arising from domestic flights and those arising from international flights involving U.S. carriers or residents, but it does not protect a provider who exhibits flagrant disregard for the patient’s health and safety. Liability is generally determined under the law of the country in which the aircraft is registered, but the citizenship status of the parties and where the incident occurs are also relevant.5
Under the facts of the hypothetical given above, one can expect jurisdictional conflicts in the event the plaintiff files a lawsuit, because it is unclear whether the AMAA is applicable where a foreign airline is on an international flight over the Atlantic, even one out of New York involving a U.S. citizen.
There does not appear to be an appellate court opinion on physician negligence during an in-flight medical emergency, but there have been lower court decisions and settlements adverse to the airline.6
For example, Northwest Airlines reportedly settled out of court following the death of a passenger on a flight from Manila to Tokyo, despite its claim that three doctors on board the aircraft did not feel an emergency landing was warranted. In a similar case, a Miami federal judge ordered Lufthansa German Airlines to pay damages of $2.7 million to a passenger having a heart attack during a 9-hour flight, after the captain heeded the recommendation from a doctor on board against diverting. In neither case were the doctors apparently named as defendants.
In summary, a doctor is ethically obligated to provide medical assistance in a midair emergency situation. It is highly unlikely that any adverse legal repercussion will ensue. Good Samaritan statutes and, more specifically, the AMAA, properly provide immunity against any allegation of ordinary negligence. Finally, one should be mindful of the need for the patient’s consent before examination and treatment, and, as always, keep written notes of what you have done.
References
1. AMA Code of Medical Ethics §8.11, 2012-2013 edition.
2. N Engl J Med. 2015 Sep 3;373(10):939-45.
3. Perkins v. Howard, 232 Cal.App.3d 708 (1991).
4. Prosser and Keeton on Torts, 5th ed. 1984, p. 211-4.
5. Aviation Medical Assistance Act of 1998, Pub L. No. 105-170. Washington, DC.
6. Aviat Space Environ Med. 1997 Dec;68(12):1134-8.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: One hour into an Air France international flight out of New York, Dr. Internist responded to a call for emergency medical assistance. A U.S. passenger had briefly passed out but then appeared to recover. Dr. Internist made a tentative diagnosis of a transient ischemic attack, but did not think an immediate divert was necessary. Based on the doctor’s assessment, the pilot continued on the previously scheduled flight path, landing several hours later in Paris. Meanwhile, the passenger’s condition worsened, and he expired shortly after arrival.
Which of the following statements is correct?
A. Under the common law, there is no legal duty to aid a stranger in distress; but under French law, a doctor is legally obligated to provide emergency assistance.
B. The U.S. federal Aviation Medical Assistance Act may immunize the doctor against liability for negligence during a midair medical emergency.
C. A tort action may still lie against the airline, notwithstanding the doctor’s advice not to divert.
D. Expect jurisdictional conflicts in the event there is a lawsuit.
E. All are correct.
Answer: E. Under the common law, there is no legal duty for anyone, even a doctor, to come to the aid of a stranger. However, doctors are generally held to have an ethical duty to offer emergency care. The American Medical Association’s Code of Medical Ethics states: “Physicians are free to choose whom they will serve. The physician should, however, respond to the best of his or her ability in cases of emergency where first aid treatment is essential.”1
In contrast, Australia and most civil law jurisdictions, e.g., many European countries, impose a legal obligation to render assistance. Under French law, for example, failure to render assistance to a person in urgent need of help can be met with fines of up to 75,000 euros and 5 years imprisonment.
Medical “emergencies” occur in roughly 1 of every 600 flights, which may be an underestimate because of underreporting. The most common medical reasons for aircraft diversion are cardiac, respiratory, and neurologic emergencies. According to a recent review in the New England Journal of Medicine, the decision to divert lies solely with the captain of the aircraft, who must also consider factors such as fuel, costs, the ability to land, and the medical resources available at that airport.2 The review also summarizes medical steps to be taken during midair medical emergencies.
Two related laws other than international aviation treaties govern medical liability during commercial flights: the generic “Good Samaritan” statute, which all 50 U.S. states have enacted, and the more specific federal Aviation Medical Assistance Act.
In 1959, California enacted the first Good Samaritan statute, whose intent is to encourage the helping of people in distress. In general, the law protects against liability arising out of nonreimbursed negligent rescue, but it does not affirmatively require doctors to come to the aid of strangers. Vermont, however, is an exception, and imposes a legal duty to assist a victim in need.
Typically, there is legal immunity against ordinary negligence but not gross misconduct, although California appears to excuse even gross negligence so long as the act was done in good faith. In a litigated case, a California court eloquently declared: “The goodness of the Samaritan is a description of the quality of his or her intention, not the quality of the aid delivered.”3
There is no universal definition of gross negligence, but the term frequently is equated with willful, wanton, or reckless conduct. One can think of gross negligence as aggravated negligence, involving more than mere mistake, inadvertence, or inattention, and representing highly unreasonable conduct or an extreme departure from ordinary care where a high degree of danger is apparent.4 An example may be an obviously inebriated physician attempting to provide treatment and causing harm to the victim.
However, the Good Samaritan statute, being state based, may not be applicable to scenarios with cross-border jurisdictional issues. The specific law that incorporates Good Samaritan assistance during commercial flights is the federal Aviation Medical Assistance Act (AMAA), which Congress enacted in 1998. In addition to Federal Aviation Administration mandates such as requisite medical supplies on board and training of flight crew, this federal law shields providers who respond to in-flight medical emergencies.
The AMAA covers claims arising from domestic flights and those arising from international flights involving U.S. carriers or residents, but it does not protect a provider who exhibits flagrant disregard for the patient’s health and safety. Liability is generally determined under the law of the country in which the aircraft is registered, but the citizenship status of the parties and where the incident occurs are also relevant.5
Under the facts of the hypothetical given above, one can expect jurisdictional conflicts in the event the plaintiff files a lawsuit, because it is unclear whether the AMAA is applicable where a foreign airline is on an international flight over the Atlantic, even one out of New York involving a U.S. citizen.
There does not appear to be an appellate court opinion on physician negligence during an in-flight medical emergency, but there have been lower court decisions and settlements adverse to the airline.6
For example, Northwest Airlines reportedly settled out of court following the death of a passenger on a flight from Manila to Tokyo, despite its claim that three doctors on board the aircraft did not feel an emergency landing was warranted. In a similar case, a Miami federal judge ordered Lufthansa German Airlines to pay damages of $2.7 million to a passenger having a heart attack during a 9-hour flight, after the captain heeded the recommendation from a doctor on board against diverting. In neither case were the doctors apparently named as defendants.
In summary, a doctor is ethically obligated to provide medical assistance in a midair emergency situation. It is highly unlikely that any adverse legal repercussion will ensue. Good Samaritan statutes and, more specifically, the AMAA, properly provide immunity against any allegation of ordinary negligence. Finally, one should be mindful of the need for the patient’s consent before examination and treatment, and, as always, keep written notes of what you have done.
References
1. AMA Code of Medical Ethics §8.11, 2012-2013 edition.
2. N Engl J Med. 2015 Sep 3;373(10):939-45.
3. Perkins v. Howard, 232 Cal.App.3d 708 (1991).
4. Prosser and Keeton on Torts, 5th ed. 1984, p. 211-4.
5. Aviation Medical Assistance Act of 1998, Pub L. No. 105-170. Washington, DC.
6. Aviat Space Environ Med. 1997 Dec;68(12):1134-8.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: One hour into an Air France international flight out of New York, Dr. Internist responded to a call for emergency medical assistance. A U.S. passenger had briefly passed out but then appeared to recover. Dr. Internist made a tentative diagnosis of a transient ischemic attack, but did not think an immediate divert was necessary. Based on the doctor’s assessment, the pilot continued on the previously scheduled flight path, landing several hours later in Paris. Meanwhile, the passenger’s condition worsened, and he expired shortly after arrival.
Which of the following statements is correct?
A. Under the common law, there is no legal duty to aid a stranger in distress; but under French law, a doctor is legally obligated to provide emergency assistance.
B. The U.S. federal Aviation Medical Assistance Act may immunize the doctor against liability for negligence during a midair medical emergency.
C. A tort action may still lie against the airline, notwithstanding the doctor’s advice not to divert.
D. Expect jurisdictional conflicts in the event there is a lawsuit.
E. All are correct.
Answer: E. Under the common law, there is no legal duty for anyone, even a doctor, to come to the aid of a stranger. However, doctors are generally held to have an ethical duty to offer emergency care. The American Medical Association’s Code of Medical Ethics states: “Physicians are free to choose whom they will serve. The physician should, however, respond to the best of his or her ability in cases of emergency where first aid treatment is essential.”1
In contrast, Australia and most civil law jurisdictions, e.g., many European countries, impose a legal obligation to render assistance. Under French law, for example, failure to render assistance to a person in urgent need of help can be met with fines of up to 75,000 euros and 5 years imprisonment.
Medical “emergencies” occur in roughly 1 of every 600 flights, which may be an underestimate because of underreporting. The most common medical reasons for aircraft diversion are cardiac, respiratory, and neurologic emergencies. According to a recent review in the New England Journal of Medicine, the decision to divert lies solely with the captain of the aircraft, who must also consider factors such as fuel, costs, the ability to land, and the medical resources available at that airport.2 The review also summarizes medical steps to be taken during midair medical emergencies.
Two related laws other than international aviation treaties govern medical liability during commercial flights: the generic “Good Samaritan” statute, which all 50 U.S. states have enacted, and the more specific federal Aviation Medical Assistance Act.
In 1959, California enacted the first Good Samaritan statute, whose intent is to encourage the helping of people in distress. In general, the law protects against liability arising out of nonreimbursed negligent rescue, but it does not affirmatively require doctors to come to the aid of strangers. Vermont, however, is an exception, and imposes a legal duty to assist a victim in need.
Typically, there is legal immunity against ordinary negligence but not gross misconduct, although California appears to excuse even gross negligence so long as the act was done in good faith. In a litigated case, a California court eloquently declared: “The goodness of the Samaritan is a description of the quality of his or her intention, not the quality of the aid delivered.”3
There is no universal definition of gross negligence, but the term frequently is equated with willful, wanton, or reckless conduct. One can think of gross negligence as aggravated negligence, involving more than mere mistake, inadvertence, or inattention, and representing highly unreasonable conduct or an extreme departure from ordinary care where a high degree of danger is apparent.4 An example may be an obviously inebriated physician attempting to provide treatment and causing harm to the victim.
However, the Good Samaritan statute, being state based, may not be applicable to scenarios with cross-border jurisdictional issues. The specific law that incorporates Good Samaritan assistance during commercial flights is the federal Aviation Medical Assistance Act (AMAA), which Congress enacted in 1998. In addition to Federal Aviation Administration mandates such as requisite medical supplies on board and training of flight crew, this federal law shields providers who respond to in-flight medical emergencies.
The AMAA covers claims arising from domestic flights and those arising from international flights involving U.S. carriers or residents, but it does not protect a provider who exhibits flagrant disregard for the patient’s health and safety. Liability is generally determined under the law of the country in which the aircraft is registered, but the citizenship status of the parties and where the incident occurs are also relevant.5
Under the facts of the hypothetical given above, one can expect jurisdictional conflicts in the event the plaintiff files a lawsuit, because it is unclear whether the AMAA is applicable where a foreign airline is on an international flight over the Atlantic, even one out of New York involving a U.S. citizen.
There does not appear to be an appellate court opinion on physician negligence during an in-flight medical emergency, but there have been lower court decisions and settlements adverse to the airline.6
For example, Northwest Airlines reportedly settled out of court following the death of a passenger on a flight from Manila to Tokyo, despite its claim that three doctors on board the aircraft did not feel an emergency landing was warranted. In a similar case, a Miami federal judge ordered Lufthansa German Airlines to pay damages of $2.7 million to a passenger having a heart attack during a 9-hour flight, after the captain heeded the recommendation from a doctor on board against diverting. In neither case were the doctors apparently named as defendants.
In summary, a doctor is ethically obligated to provide medical assistance in a midair emergency situation. It is highly unlikely that any adverse legal repercussion will ensue. Good Samaritan statutes and, more specifically, the AMAA, properly provide immunity against any allegation of ordinary negligence. Finally, one should be mindful of the need for the patient’s consent before examination and treatment, and, as always, keep written notes of what you have done.
References
1. AMA Code of Medical Ethics §8.11, 2012-2013 edition.
2. N Engl J Med. 2015 Sep 3;373(10):939-45.
3. Perkins v. Howard, 232 Cal.App.3d 708 (1991).
4. Prosser and Keeton on Torts, 5th ed. 1984, p. 211-4.
5. Aviation Medical Assistance Act of 1998, Pub L. No. 105-170. Washington, DC.
6. Aviat Space Environ Med. 1997 Dec;68(12):1134-8.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].