User login
Simulation could help guide MM treatment
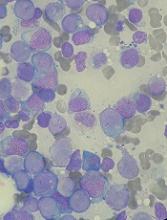
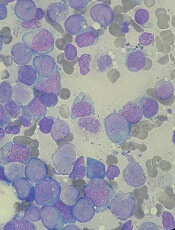
A simulation could help personalize therapy for multiple myeloma (MM), according to researchers.
With the help of gene expression signatures, a simulated treatment learning model identified which MM patients would have the greatest progression-free survival (PFS) benefit from treatment with bortezomib or lenalidomide.
Joske Ubels, of University Medical Center Utrecht in the Netherlands, and her colleagues described this research in Nature Communications.
“The key idea of simulated treatment learning is that a patient’s treatment benefit can be estimated by comparing [his or her] survival to a set of genetically similar patients [who] received the comparator treatment,” the researchers noted.
For this study, the team applied a simulated treatment learning model called GESTURE to two MM gene expression datasets. One set included patients who received bortezomib (and other therapies). The other included patients who received lenalidomide (and other therapies).
For the bortezomib dataset, the researchers combined data from three randomized, phase 3 trials of 910 MM patients (total therapy 2, total therapy 3, and HOVON-65/GMMG-HD4).
The model suggested that, in 19.8% of these patients, bortezomib would produce a two-fold greater PFS benefit than in the patient population as a whole.
For the lenalidomide dataset, the researchers obtained data on 662 MM patients in the CoMMpass trial.
The model suggested that, in 31.1% of these patients, lenalidomide would produce a three-fold greater PFS benefit than that observed in the patient population as a whole.
Based on these results, the researchers concluded that GESTURE “can derive clinically actionable gene expression signatures that enable a more personalized approach to treatment.”
The method requires a large dataset but could be useful for trials that have missed their primary endpoint, according to the researchers.
The team’s next step is to see if GESTURE makes useful treatment predictions for other cancers. The code needed to train and validate the model is available at github.com/jubels/GESTURE.
The Van Herk Fellowship provided support for this research. The lenalidomide dataset was created as part of the Multiple Myeloma Research Foundation Personalized Medicine Initiative.
Dr. Ubels and one co-investigator are employees of SkylineDx. Another co-investigator served on the company’s advisory board. All other study authors reported having no relevant conflicts of interest.
A simulation could help personalize therapy for multiple myeloma (MM), according to researchers.
With the help of gene expression signatures, a simulated treatment learning model identified which MM patients would have the greatest progression-free survival (PFS) benefit from treatment with bortezomib or lenalidomide.
Joske Ubels, of University Medical Center Utrecht in the Netherlands, and her colleagues described this research in Nature Communications.
“The key idea of simulated treatment learning is that a patient’s treatment benefit can be estimated by comparing [his or her] survival to a set of genetically similar patients [who] received the comparator treatment,” the researchers noted.
For this study, the team applied a simulated treatment learning model called GESTURE to two MM gene expression datasets. One set included patients who received bortezomib (and other therapies). The other included patients who received lenalidomide (and other therapies).
For the bortezomib dataset, the researchers combined data from three randomized, phase 3 trials of 910 MM patients (total therapy 2, total therapy 3, and HOVON-65/GMMG-HD4).
The model suggested that, in 19.8% of these patients, bortezomib would produce a two-fold greater PFS benefit than in the patient population as a whole.
For the lenalidomide dataset, the researchers obtained data on 662 MM patients in the CoMMpass trial.
The model suggested that, in 31.1% of these patients, lenalidomide would produce a three-fold greater PFS benefit than that observed in the patient population as a whole.
Based on these results, the researchers concluded that GESTURE “can derive clinically actionable gene expression signatures that enable a more personalized approach to treatment.”
The method requires a large dataset but could be useful for trials that have missed their primary endpoint, according to the researchers.
The team’s next step is to see if GESTURE makes useful treatment predictions for other cancers. The code needed to train and validate the model is available at github.com/jubels/GESTURE.
The Van Herk Fellowship provided support for this research. The lenalidomide dataset was created as part of the Multiple Myeloma Research Foundation Personalized Medicine Initiative.
Dr. Ubels and one co-investigator are employees of SkylineDx. Another co-investigator served on the company’s advisory board. All other study authors reported having no relevant conflicts of interest.
A simulation could help personalize therapy for multiple myeloma (MM), according to researchers.
With the help of gene expression signatures, a simulated treatment learning model identified which MM patients would have the greatest progression-free survival (PFS) benefit from treatment with bortezomib or lenalidomide.
Joske Ubels, of University Medical Center Utrecht in the Netherlands, and her colleagues described this research in Nature Communications.
“The key idea of simulated treatment learning is that a patient’s treatment benefit can be estimated by comparing [his or her] survival to a set of genetically similar patients [who] received the comparator treatment,” the researchers noted.
For this study, the team applied a simulated treatment learning model called GESTURE to two MM gene expression datasets. One set included patients who received bortezomib (and other therapies). The other included patients who received lenalidomide (and other therapies).
For the bortezomib dataset, the researchers combined data from three randomized, phase 3 trials of 910 MM patients (total therapy 2, total therapy 3, and HOVON-65/GMMG-HD4).
The model suggested that, in 19.8% of these patients, bortezomib would produce a two-fold greater PFS benefit than in the patient population as a whole.
For the lenalidomide dataset, the researchers obtained data on 662 MM patients in the CoMMpass trial.
The model suggested that, in 31.1% of these patients, lenalidomide would produce a three-fold greater PFS benefit than that observed in the patient population as a whole.
Based on these results, the researchers concluded that GESTURE “can derive clinically actionable gene expression signatures that enable a more personalized approach to treatment.”
The method requires a large dataset but could be useful for trials that have missed their primary endpoint, according to the researchers.
The team’s next step is to see if GESTURE makes useful treatment predictions for other cancers. The code needed to train and validate the model is available at github.com/jubels/GESTURE.
The Van Herk Fellowship provided support for this research. The lenalidomide dataset was created as part of the Multiple Myeloma Research Foundation Personalized Medicine Initiative.
Dr. Ubels and one co-investigator are employees of SkylineDx. Another co-investigator served on the company’s advisory board. All other study authors reported having no relevant conflicts of interest.
Role of SES in childhood cancer survival disparities
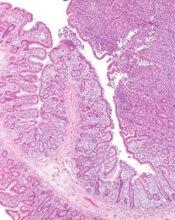
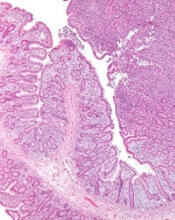
Socioeconomic status (SES) may explain some racial/ethnic disparities in childhood cancer survival, according to new research.
The study showed that whites had a significant survival advantage over blacks and Hispanics for several childhood cancers.
SES significantly mediated the association between race/ethnicity and survival for acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), neuroblastoma, and non-Hodgkin lymphoma (NHL).
Rebecca Kehm, PhD, of Columbia University in New York, New York, and her colleagues reported these findings in Cancer alongside a related editorial.
The researchers examined population-based cancer survival data from the Surveillance, Epidemiology, and End Results database.
The team collected information on 31,866 patients, ages 0 to 19, who were diagnosed with cancer between 2000 and 2011.
Survival differences by race/ethnicity
The researchers found that whites had a significant survival advantage over blacks for the cancers listed in the following table.
| Survival—black vs white | |||
| Cancer | Mortality hazard ratio | 95% confidence interval | P value |
| ALL | 1.43 | 1.15-1.77 | <0.01 |
| AML | 1.68 | 1.36-2.07 | <0.001 |
| Neuroblastoma | 1.38 | 1.08-1.75 | 0.01 |
| NHL | 1.53 | 1.14-2.07 | 0.01 |
| Hodgkin lymphoma | 1.66 | 1.06-2.60 | 0.03 |
| Astrocytoma | 1.95 | 1.57-2.43 | <0.001 |
| Non-astrocytoma CNS tumor | 1.53 | 1.25-1.88 | <0.001 |
| Non-rhabdomyosarcoma STS | 1.40 | 1.06-1.84 | 0.02 |
| Rhabdomyosarcoma | 1.44 | 1.10-1.88 | 0.01 |
In addition, whites had a significant survival advantage over Hispanics for the following cancers.
| Survival—Hispanic vs white | |||
| Cancer | Mortality hazard ratio | 95% confidence interval | P value |
| ALL | 1.63 | 1.43-1.86 | <0.001 |
| Neuroblastoma | 1.31 | 1.04-1.65 | 0.02 |
| NHL | 1.65 | 1.29-2.12 | <0.001 |
| Astrocytoma | 1.34 | 1.10-1.64 | <0.01 |
| Wilms tumor | 1.60 | 1.04-2.45 | 0.03 |
| Germ cell tumor | 1.63 | 1.19-2.24 | <0.01 |
Impact of SES
SES significantly mediated the association between race/ethnicity and survival for ALL, AML, neuroblastoma, and NHL but not for Hodgkin lymphoma or other cancers.
For black versus white patients, SES reduced the original association between race/ethnicity and survival by:
- 44% for ALL
- 28% for AML
- 49% for neuroblastoma
- 34% for NHL.
For Hispanics versus whites, SES reduced the original association between race/ethnicity and survival by:
- 31% for ALL
- 73% for AML
- 48% for neuroblastoma
- 28% for NHL.
“These findings provide insight for future intervention efforts aimed at closing the survival gap,” Dr Kehm said.
“For cancers in which socioeconomic status is a key factor in explaining racial and ethnic survival disparities, behavioral and supportive interventions that address social and economic barriers to effective care are warranted. However, for cancers in which survival is less influenced by socioeconomic status, more research is needed on underlying differences in tumor biology and drug processing.”
This research was supported by a grant from the National Institutes of Health, and the study’s authors made no disclosures.
Socioeconomic status (SES) may explain some racial/ethnic disparities in childhood cancer survival, according to new research.
The study showed that whites had a significant survival advantage over blacks and Hispanics for several childhood cancers.
SES significantly mediated the association between race/ethnicity and survival for acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), neuroblastoma, and non-Hodgkin lymphoma (NHL).
Rebecca Kehm, PhD, of Columbia University in New York, New York, and her colleagues reported these findings in Cancer alongside a related editorial.
The researchers examined population-based cancer survival data from the Surveillance, Epidemiology, and End Results database.
The team collected information on 31,866 patients, ages 0 to 19, who were diagnosed with cancer between 2000 and 2011.
Survival differences by race/ethnicity
The researchers found that whites had a significant survival advantage over blacks for the cancers listed in the following table.
| Survival—black vs white | |||
| Cancer | Mortality hazard ratio | 95% confidence interval | P value |
| ALL | 1.43 | 1.15-1.77 | <0.01 |
| AML | 1.68 | 1.36-2.07 | <0.001 |
| Neuroblastoma | 1.38 | 1.08-1.75 | 0.01 |
| NHL | 1.53 | 1.14-2.07 | 0.01 |
| Hodgkin lymphoma | 1.66 | 1.06-2.60 | 0.03 |
| Astrocytoma | 1.95 | 1.57-2.43 | <0.001 |
| Non-astrocytoma CNS tumor | 1.53 | 1.25-1.88 | <0.001 |
| Non-rhabdomyosarcoma STS | 1.40 | 1.06-1.84 | 0.02 |
| Rhabdomyosarcoma | 1.44 | 1.10-1.88 | 0.01 |
In addition, whites had a significant survival advantage over Hispanics for the following cancers.
| Survival—Hispanic vs white | |||
| Cancer | Mortality hazard ratio | 95% confidence interval | P value |
| ALL | 1.63 | 1.43-1.86 | <0.001 |
| Neuroblastoma | 1.31 | 1.04-1.65 | 0.02 |
| NHL | 1.65 | 1.29-2.12 | <0.001 |
| Astrocytoma | 1.34 | 1.10-1.64 | <0.01 |
| Wilms tumor | 1.60 | 1.04-2.45 | 0.03 |
| Germ cell tumor | 1.63 | 1.19-2.24 | <0.01 |
Impact of SES
SES significantly mediated the association between race/ethnicity and survival for ALL, AML, neuroblastoma, and NHL but not for Hodgkin lymphoma or other cancers.
For black versus white patients, SES reduced the original association between race/ethnicity and survival by:
- 44% for ALL
- 28% for AML
- 49% for neuroblastoma
- 34% for NHL.
For Hispanics versus whites, SES reduced the original association between race/ethnicity and survival by:
- 31% for ALL
- 73% for AML
- 48% for neuroblastoma
- 28% for NHL.
“These findings provide insight for future intervention efforts aimed at closing the survival gap,” Dr Kehm said.
“For cancers in which socioeconomic status is a key factor in explaining racial and ethnic survival disparities, behavioral and supportive interventions that address social and economic barriers to effective care are warranted. However, for cancers in which survival is less influenced by socioeconomic status, more research is needed on underlying differences in tumor biology and drug processing.”
This research was supported by a grant from the National Institutes of Health, and the study’s authors made no disclosures.
Socioeconomic status (SES) may explain some racial/ethnic disparities in childhood cancer survival, according to new research.
The study showed that whites had a significant survival advantage over blacks and Hispanics for several childhood cancers.
SES significantly mediated the association between race/ethnicity and survival for acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), neuroblastoma, and non-Hodgkin lymphoma (NHL).
Rebecca Kehm, PhD, of Columbia University in New York, New York, and her colleagues reported these findings in Cancer alongside a related editorial.
The researchers examined population-based cancer survival data from the Surveillance, Epidemiology, and End Results database.
The team collected information on 31,866 patients, ages 0 to 19, who were diagnosed with cancer between 2000 and 2011.
Survival differences by race/ethnicity
The researchers found that whites had a significant survival advantage over blacks for the cancers listed in the following table.
| Survival—black vs white | |||
| Cancer | Mortality hazard ratio | 95% confidence interval | P value |
| ALL | 1.43 | 1.15-1.77 | <0.01 |
| AML | 1.68 | 1.36-2.07 | <0.001 |
| Neuroblastoma | 1.38 | 1.08-1.75 | 0.01 |
| NHL | 1.53 | 1.14-2.07 | 0.01 |
| Hodgkin lymphoma | 1.66 | 1.06-2.60 | 0.03 |
| Astrocytoma | 1.95 | 1.57-2.43 | <0.001 |
| Non-astrocytoma CNS tumor | 1.53 | 1.25-1.88 | <0.001 |
| Non-rhabdomyosarcoma STS | 1.40 | 1.06-1.84 | 0.02 |
| Rhabdomyosarcoma | 1.44 | 1.10-1.88 | 0.01 |
In addition, whites had a significant survival advantage over Hispanics for the following cancers.
| Survival—Hispanic vs white | |||
| Cancer | Mortality hazard ratio | 95% confidence interval | P value |
| ALL | 1.63 | 1.43-1.86 | <0.001 |
| Neuroblastoma | 1.31 | 1.04-1.65 | 0.02 |
| NHL | 1.65 | 1.29-2.12 | <0.001 |
| Astrocytoma | 1.34 | 1.10-1.64 | <0.01 |
| Wilms tumor | 1.60 | 1.04-2.45 | 0.03 |
| Germ cell tumor | 1.63 | 1.19-2.24 | <0.01 |
Impact of SES
SES significantly mediated the association between race/ethnicity and survival for ALL, AML, neuroblastoma, and NHL but not for Hodgkin lymphoma or other cancers.
For black versus white patients, SES reduced the original association between race/ethnicity and survival by:
- 44% for ALL
- 28% for AML
- 49% for neuroblastoma
- 34% for NHL.
For Hispanics versus whites, SES reduced the original association between race/ethnicity and survival by:
- 31% for ALL
- 73% for AML
- 48% for neuroblastoma
- 28% for NHL.
“These findings provide insight for future intervention efforts aimed at closing the survival gap,” Dr Kehm said.
“For cancers in which socioeconomic status is a key factor in explaining racial and ethnic survival disparities, behavioral and supportive interventions that address social and economic barriers to effective care are warranted. However, for cancers in which survival is less influenced by socioeconomic status, more research is needed on underlying differences in tumor biology and drug processing.”
This research was supported by a grant from the National Institutes of Health, and the study’s authors made no disclosures.
Marzeptacog alfa may prevent bleeds in hemophilia A/B with inhibitors
BOSTON—The activated factor VIIa variant marzeptacog alfa has demonstrated efficacy as prophylaxis for patients with hemophilia A or B who also have inhibitors, according to researchers.
Three patients have completed dosing with marzeptacog alfa in a phase 2/3 study.
None of these patients experienced bleeding during treatment, and none have developed antidrug antibodies or reported injection site reactions.
As for the other 2 patients enrolled in this study, 1 withdrew consent, and 1 died of an adverse event unrelated to marzeptacog alfa.
Howard Levy, chief medical officer of Catalyst Biosciences, Inc., presented these data at the 2018 Hemophilia Drug Development Summit.
The trial is sponsored by Catalyst Biosciences, the company developing marzeptacog alfa.
Results
The goal of this ongoing trial is to determine whether daily subcutaneous injections of marzeptacog alfa can eliminate or minimize spontaneous bleeding episodes. The primary endpoint is a reduction in annualized bleed rate (ABR) compared to each individual’s recorded historical ABR.
Thus far, the trial has enrolled 5 patients with hemophilia A or B and inhibitors. (Catalyst would not disclose how many patients have hemophilia A and how many have hemophilia B).
One patient with a historic ABR of 26.7 completed the trial with no bleeds after 50 days of treatment with marzeptacog alfa at 60 µg/kg.
This patient had previously experienced a bleed on day 46 when receiving marzeptacog alfa at 30 µg/kg, and the patient experienced another bleed 16 days after the end of dosing at 60 µg/kg.
A second patient with a historic ABR of 16.6 had no bleeds when receiving marzeptacog alfa at 30 µg/kg for 50 days.
And a third patient with a historic ABR of 15.9 had no bleeds when receiving marzeptacog alfa at 30 µg/kg for 44 days.
“The data from these 3 individuals support the efficacy of [marzeptacog alfa] to reduce annualized bleed rates after daily subcutaneous injections,” said Nassim Usman, PhD, chief executive officer of Catalyst Biosciences.
“Importantly, to date, we have not observed any injection site reactions nor any anti-drug antibodies after more than 200 subcutaneous doses of [marzeptacog alfa].”
A fourth patient with a historic ABR of 18.3 had a fatal hemorrhagic stroke on day 11 that was considered unrelated to marzeptacog alfa. The patient had previously treated hypertension that was going untreated at the time of death.
A fifth patient with a historic ABR of 12.2 withdrew consent.
BOSTON—The activated factor VIIa variant marzeptacog alfa has demonstrated efficacy as prophylaxis for patients with hemophilia A or B who also have inhibitors, according to researchers.
Three patients have completed dosing with marzeptacog alfa in a phase 2/3 study.
None of these patients experienced bleeding during treatment, and none have developed antidrug antibodies or reported injection site reactions.
As for the other 2 patients enrolled in this study, 1 withdrew consent, and 1 died of an adverse event unrelated to marzeptacog alfa.
Howard Levy, chief medical officer of Catalyst Biosciences, Inc., presented these data at the 2018 Hemophilia Drug Development Summit.
The trial is sponsored by Catalyst Biosciences, the company developing marzeptacog alfa.
Results
The goal of this ongoing trial is to determine whether daily subcutaneous injections of marzeptacog alfa can eliminate or minimize spontaneous bleeding episodes. The primary endpoint is a reduction in annualized bleed rate (ABR) compared to each individual’s recorded historical ABR.
Thus far, the trial has enrolled 5 patients with hemophilia A or B and inhibitors. (Catalyst would not disclose how many patients have hemophilia A and how many have hemophilia B).
One patient with a historic ABR of 26.7 completed the trial with no bleeds after 50 days of treatment with marzeptacog alfa at 60 µg/kg.
This patient had previously experienced a bleed on day 46 when receiving marzeptacog alfa at 30 µg/kg, and the patient experienced another bleed 16 days after the end of dosing at 60 µg/kg.
A second patient with a historic ABR of 16.6 had no bleeds when receiving marzeptacog alfa at 30 µg/kg for 50 days.
And a third patient with a historic ABR of 15.9 had no bleeds when receiving marzeptacog alfa at 30 µg/kg for 44 days.
“The data from these 3 individuals support the efficacy of [marzeptacog alfa] to reduce annualized bleed rates after daily subcutaneous injections,” said Nassim Usman, PhD, chief executive officer of Catalyst Biosciences.
“Importantly, to date, we have not observed any injection site reactions nor any anti-drug antibodies after more than 200 subcutaneous doses of [marzeptacog alfa].”
A fourth patient with a historic ABR of 18.3 had a fatal hemorrhagic stroke on day 11 that was considered unrelated to marzeptacog alfa. The patient had previously treated hypertension that was going untreated at the time of death.
A fifth patient with a historic ABR of 12.2 withdrew consent.
BOSTON—The activated factor VIIa variant marzeptacog alfa has demonstrated efficacy as prophylaxis for patients with hemophilia A or B who also have inhibitors, according to researchers.
Three patients have completed dosing with marzeptacog alfa in a phase 2/3 study.
None of these patients experienced bleeding during treatment, and none have developed antidrug antibodies or reported injection site reactions.
As for the other 2 patients enrolled in this study, 1 withdrew consent, and 1 died of an adverse event unrelated to marzeptacog alfa.
Howard Levy, chief medical officer of Catalyst Biosciences, Inc., presented these data at the 2018 Hemophilia Drug Development Summit.
The trial is sponsored by Catalyst Biosciences, the company developing marzeptacog alfa.
Results
The goal of this ongoing trial is to determine whether daily subcutaneous injections of marzeptacog alfa can eliminate or minimize spontaneous bleeding episodes. The primary endpoint is a reduction in annualized bleed rate (ABR) compared to each individual’s recorded historical ABR.
Thus far, the trial has enrolled 5 patients with hemophilia A or B and inhibitors. (Catalyst would not disclose how many patients have hemophilia A and how many have hemophilia B).
One patient with a historic ABR of 26.7 completed the trial with no bleeds after 50 days of treatment with marzeptacog alfa at 60 µg/kg.
This patient had previously experienced a bleed on day 46 when receiving marzeptacog alfa at 30 µg/kg, and the patient experienced another bleed 16 days after the end of dosing at 60 µg/kg.
A second patient with a historic ABR of 16.6 had no bleeds when receiving marzeptacog alfa at 30 µg/kg for 50 days.
And a third patient with a historic ABR of 15.9 had no bleeds when receiving marzeptacog alfa at 30 µg/kg for 44 days.
“The data from these 3 individuals support the efficacy of [marzeptacog alfa] to reduce annualized bleed rates after daily subcutaneous injections,” said Nassim Usman, PhD, chief executive officer of Catalyst Biosciences.
“Importantly, to date, we have not observed any injection site reactions nor any anti-drug antibodies after more than 200 subcutaneous doses of [marzeptacog alfa].”
A fourth patient with a historic ABR of 18.3 had a fatal hemorrhagic stroke on day 11 that was considered unrelated to marzeptacog alfa. The patient had previously treated hypertension that was going untreated at the time of death.
A fifth patient with a historic ABR of 12.2 withdrew consent.
Inhibitor receives orphan designation for AML
The US Food and Drug Administration (FDA) has granted orphan drug designation to ASLAN003 as a treatment for acute myeloid leukemia (AML).
ASLAN003 is a small molecule inhibitor of the human dihydroorotate dehydrogenase (DHODH) enzyme.
This second-generation DHODH inhibitor is being developed by ASLAN Pharmaceuticals.
The company is currently conducting a phase 2 trial (NCT03451084) of ASLAN003 in patients with newly diagnosed or relapsed/refractory AML.
The goals of this trial are to determine the optimum dose of ASLAN003 as monotherapy and assess the drug’s efficacy by overall complete remission rate. ASLAN expects to report interim data from this trial in the second half of this year.
ASLAN has already completed a phase 1 trial (NCT01992367) of ASLAN003 in healthy volunteers.
Results suggested that ASLAN003 has an “excellent” pharmacokinetic profile, according to ASLAN, and the drug was considered well tolerated in the volunteers.
ASLAN003 has also demonstrated “potent” inhibition of DHODH, according to ASLAN. In fact, the company said the binding affinity of ASLAN003 to DHODH has proven to be up to 2 orders of magnitude stronger than first-generation DHODH inhibitors such as leflunomide and teriflunomide.
ASLAN also said ASLAN003 should not confer the same toxicities as first-generation DHODH inhibitors and other novel AML therapies.
For example, leflunomide and teriflunomide, which may cause significant liver toxicity, take between 3 and 4 weeks to build to therapeutic levels and 2 years to be cleared completely after treatment is stopped.
ASLAN003, on the other hand, reaches full exposure in 24 hours and has a half-life of 18 hours.
Finally, ASLAN003 has been shown to differentiate blast cells into granulocytes in AML cell lines that do not respond to all-trans retinoic acid. These results were published in Cell in 2016.
Because of this research, ASLAN believes ASLAN003 may be effective in patients who do not respond to all-trans retinoic acid.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to ASLAN003 as a treatment for acute myeloid leukemia (AML).
ASLAN003 is a small molecule inhibitor of the human dihydroorotate dehydrogenase (DHODH) enzyme.
This second-generation DHODH inhibitor is being developed by ASLAN Pharmaceuticals.
The company is currently conducting a phase 2 trial (NCT03451084) of ASLAN003 in patients with newly diagnosed or relapsed/refractory AML.
The goals of this trial are to determine the optimum dose of ASLAN003 as monotherapy and assess the drug’s efficacy by overall complete remission rate. ASLAN expects to report interim data from this trial in the second half of this year.
ASLAN has already completed a phase 1 trial (NCT01992367) of ASLAN003 in healthy volunteers.
Results suggested that ASLAN003 has an “excellent” pharmacokinetic profile, according to ASLAN, and the drug was considered well tolerated in the volunteers.
ASLAN003 has also demonstrated “potent” inhibition of DHODH, according to ASLAN. In fact, the company said the binding affinity of ASLAN003 to DHODH has proven to be up to 2 orders of magnitude stronger than first-generation DHODH inhibitors such as leflunomide and teriflunomide.
ASLAN also said ASLAN003 should not confer the same toxicities as first-generation DHODH inhibitors and other novel AML therapies.
For example, leflunomide and teriflunomide, which may cause significant liver toxicity, take between 3 and 4 weeks to build to therapeutic levels and 2 years to be cleared completely after treatment is stopped.
ASLAN003, on the other hand, reaches full exposure in 24 hours and has a half-life of 18 hours.
Finally, ASLAN003 has been shown to differentiate blast cells into granulocytes in AML cell lines that do not respond to all-trans retinoic acid. These results were published in Cell in 2016.
Because of this research, ASLAN believes ASLAN003 may be effective in patients who do not respond to all-trans retinoic acid.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to ASLAN003 as a treatment for acute myeloid leukemia (AML).
ASLAN003 is a small molecule inhibitor of the human dihydroorotate dehydrogenase (DHODH) enzyme.
This second-generation DHODH inhibitor is being developed by ASLAN Pharmaceuticals.
The company is currently conducting a phase 2 trial (NCT03451084) of ASLAN003 in patients with newly diagnosed or relapsed/refractory AML.
The goals of this trial are to determine the optimum dose of ASLAN003 as monotherapy and assess the drug’s efficacy by overall complete remission rate. ASLAN expects to report interim data from this trial in the second half of this year.
ASLAN has already completed a phase 1 trial (NCT01992367) of ASLAN003 in healthy volunteers.
Results suggested that ASLAN003 has an “excellent” pharmacokinetic profile, according to ASLAN, and the drug was considered well tolerated in the volunteers.
ASLAN003 has also demonstrated “potent” inhibition of DHODH, according to ASLAN. In fact, the company said the binding affinity of ASLAN003 to DHODH has proven to be up to 2 orders of magnitude stronger than first-generation DHODH inhibitors such as leflunomide and teriflunomide.
ASLAN also said ASLAN003 should not confer the same toxicities as first-generation DHODH inhibitors and other novel AML therapies.
For example, leflunomide and teriflunomide, which may cause significant liver toxicity, take between 3 and 4 weeks to build to therapeutic levels and 2 years to be cleared completely after treatment is stopped.
ASLAN003, on the other hand, reaches full exposure in 24 hours and has a half-life of 18 hours.
Finally, ASLAN003 has been shown to differentiate blast cells into granulocytes in AML cell lines that do not respond to all-trans retinoic acid. These results were published in Cell in 2016.
Because of this research, ASLAN believes ASLAN003 may be effective in patients who do not respond to all-trans retinoic acid.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
Access to care drives disparity between urban, rural cancer patients
New research suggests that better access to quality care may reduce disparities in survival between cancer patients living in rural areas of the US and those living in urban areas.
The study showed that urban and rural cancer patients had similar survival outcomes when they were enrolled in clinical trials.
These results, published in JAMA Network Open, cast new light on decades of research showing that cancer patients living in rural areas don’t live as long as urban cancer patients.
“These findings were a surprise, since we thought we might find the same disparities others had found,” said study author Joseph Unger, PhD, of Fred Hutchinson Cancer Research Center in Seattle, Washington.
“But clinical trials are a key difference here. In trials, patients are uniformly assessed, treated, and followed under a strict, guideline-driven protocol. This suggests that giving people with cancer access to uniform treatment strategies could help resolve the disparities in outcomes that we see between rural and urban patients.”
Dr Unger and his colleagues studied data on 36,995 patients who were enrolled in 44 phase 3 or phase 2/3 SWOG trials from 1986 through 2012. All 50 states were represented.
Patients had 17 different cancer types, including acute myeloid leukemia (AML), non-Hodgkin lymphoma (NHL), and multiple myeloma (MM).
Using US Department of Agriculture population classifications known as Rural-Urban Continuum Codes, the researchers categorized the patients as either rural or urban and analyzed their outcomes.
A minority of patients (19.4%, n=7184) were from rural locations. They were significantly more likely than urban patients to be 65 or older (P<0.001) and significantly less likely to be black (vs all other races; P<0.001).
However, there was no significant between-group difference in sex (P=0.53), and all major US geographic regions (West, Midwest, South, and Northeast) were represented.
Results
The researchers limited their analysis of survival to the first 5 years after trial enrollment to emphasize outcomes related to cancer and its treatment. They looked at overall survival (OS) as well as cancer-specific survival.
The team found no meaningful difference in OS or cancer-specific survival between rural and urban patients for 16 of the 17 cancer types.
The exception was estrogen receptor-negative, progesterone receptor-negative breast cancer. Rural patients with this cancer didn’t live as long as their urban counterparts. The hazard ratio (HR) was 1.27 (95% CI, 1.06-1.51; P=0.008) for OS and 1.26 (95% CI, 1.04-1.52; P=0.02) for cancer-specific survival.
The researchers believe this finding could be attributed to a few factors, including timely access to follow-up chemotherapy after patients’ first round of cancer treatment.
Although there were no significant survival differences for patients with hematologic malignancies, rural patients had slightly better OS if they had advanced indolent NHL or AML but slightly worse OS if they had MM or advanced aggressive NHL. The HRs were as follows:
- Advanced indolent NHL—HR=0.91 (95% CI, 0.64-1.29; P=0.60)
- AML—HR=0.94 (95% CI, 0.83-1.06; P=0.29)
- MM—HR=1.05 (95% CI, 0.93-1.18, P=0.46)
- Advanced aggressive NHL—HR=1.05 (95% CI, 0.87-1.27; P=0.60).
Rural patients had slightly better cancer-specific survival if they had advanced indolent NHL but slightly worse cancer-specific survival if they had AML, MM, or advanced aggressive NHL. The HRs were as follows:
- Advanced indolent NHL—HR=0.98 (95% CI, 0.66-1.45; P=0.90)
- AML—HR=1.01 (95% CI, 0.86-1.20; P=0.87)
- MM—HR=1.04 (95% CI, 0.90-1.20; P=0.60)
- Advanced aggressive NHL—HR=1.08 (95% CI, 0.87-1.34; P=0.50).
The researchers said these findings suggest it is access to care, and not other characteristics, that drive the survival disparities typically observed between urban and rural cancer patients.
“If people diagnosed with cancer, regardless of where they live, receive similar care and have similar outcomes, then a reasonable inference is that the best way to improve outcomes for rural patients is to improve their access to quality care,” Dr Unger said.
This research was supported by the National Cancer Institute and the HOPE Foundation. The researchers reported financial relationships with various pharmaceutical companies.
New research suggests that better access to quality care may reduce disparities in survival between cancer patients living in rural areas of the US and those living in urban areas.
The study showed that urban and rural cancer patients had similar survival outcomes when they were enrolled in clinical trials.
These results, published in JAMA Network Open, cast new light on decades of research showing that cancer patients living in rural areas don’t live as long as urban cancer patients.
“These findings were a surprise, since we thought we might find the same disparities others had found,” said study author Joseph Unger, PhD, of Fred Hutchinson Cancer Research Center in Seattle, Washington.
“But clinical trials are a key difference here. In trials, patients are uniformly assessed, treated, and followed under a strict, guideline-driven protocol. This suggests that giving people with cancer access to uniform treatment strategies could help resolve the disparities in outcomes that we see between rural and urban patients.”
Dr Unger and his colleagues studied data on 36,995 patients who were enrolled in 44 phase 3 or phase 2/3 SWOG trials from 1986 through 2012. All 50 states were represented.
Patients had 17 different cancer types, including acute myeloid leukemia (AML), non-Hodgkin lymphoma (NHL), and multiple myeloma (MM).
Using US Department of Agriculture population classifications known as Rural-Urban Continuum Codes, the researchers categorized the patients as either rural or urban and analyzed their outcomes.
A minority of patients (19.4%, n=7184) were from rural locations. They were significantly more likely than urban patients to be 65 or older (P<0.001) and significantly less likely to be black (vs all other races; P<0.001).
However, there was no significant between-group difference in sex (P=0.53), and all major US geographic regions (West, Midwest, South, and Northeast) were represented.
Results
The researchers limited their analysis of survival to the first 5 years after trial enrollment to emphasize outcomes related to cancer and its treatment. They looked at overall survival (OS) as well as cancer-specific survival.
The team found no meaningful difference in OS or cancer-specific survival between rural and urban patients for 16 of the 17 cancer types.
The exception was estrogen receptor-negative, progesterone receptor-negative breast cancer. Rural patients with this cancer didn’t live as long as their urban counterparts. The hazard ratio (HR) was 1.27 (95% CI, 1.06-1.51; P=0.008) for OS and 1.26 (95% CI, 1.04-1.52; P=0.02) for cancer-specific survival.
The researchers believe this finding could be attributed to a few factors, including timely access to follow-up chemotherapy after patients’ first round of cancer treatment.
Although there were no significant survival differences for patients with hematologic malignancies, rural patients had slightly better OS if they had advanced indolent NHL or AML but slightly worse OS if they had MM or advanced aggressive NHL. The HRs were as follows:
- Advanced indolent NHL—HR=0.91 (95% CI, 0.64-1.29; P=0.60)
- AML—HR=0.94 (95% CI, 0.83-1.06; P=0.29)
- MM—HR=1.05 (95% CI, 0.93-1.18, P=0.46)
- Advanced aggressive NHL—HR=1.05 (95% CI, 0.87-1.27; P=0.60).
Rural patients had slightly better cancer-specific survival if they had advanced indolent NHL but slightly worse cancer-specific survival if they had AML, MM, or advanced aggressive NHL. The HRs were as follows:
- Advanced indolent NHL—HR=0.98 (95% CI, 0.66-1.45; P=0.90)
- AML—HR=1.01 (95% CI, 0.86-1.20; P=0.87)
- MM—HR=1.04 (95% CI, 0.90-1.20; P=0.60)
- Advanced aggressive NHL—HR=1.08 (95% CI, 0.87-1.34; P=0.50).
The researchers said these findings suggest it is access to care, and not other characteristics, that drive the survival disparities typically observed between urban and rural cancer patients.
“If people diagnosed with cancer, regardless of where they live, receive similar care and have similar outcomes, then a reasonable inference is that the best way to improve outcomes for rural patients is to improve their access to quality care,” Dr Unger said.
This research was supported by the National Cancer Institute and the HOPE Foundation. The researchers reported financial relationships with various pharmaceutical companies.
New research suggests that better access to quality care may reduce disparities in survival between cancer patients living in rural areas of the US and those living in urban areas.
The study showed that urban and rural cancer patients had similar survival outcomes when they were enrolled in clinical trials.
These results, published in JAMA Network Open, cast new light on decades of research showing that cancer patients living in rural areas don’t live as long as urban cancer patients.
“These findings were a surprise, since we thought we might find the same disparities others had found,” said study author Joseph Unger, PhD, of Fred Hutchinson Cancer Research Center in Seattle, Washington.
“But clinical trials are a key difference here. In trials, patients are uniformly assessed, treated, and followed under a strict, guideline-driven protocol. This suggests that giving people with cancer access to uniform treatment strategies could help resolve the disparities in outcomes that we see between rural and urban patients.”
Dr Unger and his colleagues studied data on 36,995 patients who were enrolled in 44 phase 3 or phase 2/3 SWOG trials from 1986 through 2012. All 50 states were represented.
Patients had 17 different cancer types, including acute myeloid leukemia (AML), non-Hodgkin lymphoma (NHL), and multiple myeloma (MM).
Using US Department of Agriculture population classifications known as Rural-Urban Continuum Codes, the researchers categorized the patients as either rural or urban and analyzed their outcomes.
A minority of patients (19.4%, n=7184) were from rural locations. They were significantly more likely than urban patients to be 65 or older (P<0.001) and significantly less likely to be black (vs all other races; P<0.001).
However, there was no significant between-group difference in sex (P=0.53), and all major US geographic regions (West, Midwest, South, and Northeast) were represented.
Results
The researchers limited their analysis of survival to the first 5 years after trial enrollment to emphasize outcomes related to cancer and its treatment. They looked at overall survival (OS) as well as cancer-specific survival.
The team found no meaningful difference in OS or cancer-specific survival between rural and urban patients for 16 of the 17 cancer types.
The exception was estrogen receptor-negative, progesterone receptor-negative breast cancer. Rural patients with this cancer didn’t live as long as their urban counterparts. The hazard ratio (HR) was 1.27 (95% CI, 1.06-1.51; P=0.008) for OS and 1.26 (95% CI, 1.04-1.52; P=0.02) for cancer-specific survival.
The researchers believe this finding could be attributed to a few factors, including timely access to follow-up chemotherapy after patients’ first round of cancer treatment.
Although there were no significant survival differences for patients with hematologic malignancies, rural patients had slightly better OS if they had advanced indolent NHL or AML but slightly worse OS if they had MM or advanced aggressive NHL. The HRs were as follows:
- Advanced indolent NHL—HR=0.91 (95% CI, 0.64-1.29; P=0.60)
- AML—HR=0.94 (95% CI, 0.83-1.06; P=0.29)
- MM—HR=1.05 (95% CI, 0.93-1.18, P=0.46)
- Advanced aggressive NHL—HR=1.05 (95% CI, 0.87-1.27; P=0.60).
Rural patients had slightly better cancer-specific survival if they had advanced indolent NHL but slightly worse cancer-specific survival if they had AML, MM, or advanced aggressive NHL. The HRs were as follows:
- Advanced indolent NHL—HR=0.98 (95% CI, 0.66-1.45; P=0.90)
- AML—HR=1.01 (95% CI, 0.86-1.20; P=0.87)
- MM—HR=1.04 (95% CI, 0.90-1.20; P=0.60)
- Advanced aggressive NHL—HR=1.08 (95% CI, 0.87-1.34; P=0.50).
The researchers said these findings suggest it is access to care, and not other characteristics, that drive the survival disparities typically observed between urban and rural cancer patients.
“If people diagnosed with cancer, regardless of where they live, receive similar care and have similar outcomes, then a reasonable inference is that the best way to improve outcomes for rural patients is to improve their access to quality care,” Dr Unger said.
This research was supported by the National Cancer Institute and the HOPE Foundation. The researchers reported financial relationships with various pharmaceutical companies.
Partial hold placed on trial of drug for AML, MDS
The US Food and Drug Administration (FDA) has placed a partial clinical hold on a phase 1b/2 study of OXi4503, a vascular disrupting agent.
In this trial (NCT02576301), researchers are evaluating OXi4503, alone and in combination with cytarabine, in patients with relapsed/refractory acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS).
The partial clinical hold applies to the 12.2 mg/m2 dose of OXi4503.
The FDA is allowing the continued treatment and enrollment of patients using a dose of 9.76 mg/m2.
The agency said additional data on patients receiving OXi4503 at 9.76 mg/m2 must be evaluated before dosing at 12.2 mg/m2 can be resumed.
The partial clinical hold is a result of 2 potential dose-limiting toxicities (DLTs) observed at the 12.2 mg/m2 dose level.
One DLT was hypotension, which occurred shortly after initial treatment with OXi4503. The other DLT was acute hypoxic respiratory failure, which occurred approximately 2 weeks after receiving OXi4503 and cytarabine.
Both events were deemed “possibly related” to OXi4503, and both patients recovered following treatment.
The study protocol generally defines a DLT as any grade 3 serious adverse event where a relationship to OXi4503 cannot be ruled out.
“Although it is disappointing that we are not currently continuing with the higher dose of OXi4503, we look forward to gathering more safety and efficacy data at the previous dose level, where we observed 2 complete remissions in the 4 patients that we treated,” said William D. Schwieterman, MD, chief executive officer of Mateon Therapeutics, Inc., the company developing OXi4503.
About OXi4503
According to Mateon Therapeutics, OXi4503 has a dual mechanism of action that disrupts the shape of tumor bone marrow endothelial cells through reversible binding to tubulin at the colchicine binding site, downregulating intercellular adhesion molecules.
This alters the endothelial cell shape, releasing quiescent adherent tumor cells from bone marrow endothelial cells and activating the cell cycle, which makes the tumor cells vulnerable to chemotherapy.
OXi4503 also kills tumor cells directly via myeloperoxidase activation of an orthoquinone cytotoxic mediator.
In preclinical research, OXi4503 demonstrated activity against AML, both when given alone and in combination with bevacizumab. These results were published in Blood in 2010.
Clinical trials
In a phase 1 trial (NCT01085656), researchers evaluated OXi4503 in patients with relapsed or refractory AML or MDS. The goals were to determine the safety profile, maximum tolerated dose, and biologic activity of OXi4503.
The researchers said OXi4503 demonstrated preliminary evidence of disease response in heavily pre-treated, refractory AML and advanced MDS.
The maximum tolerated dose of OXi4503 was not identified, but adverse events attributable to the drug included hypertension, bone pain, fever, anemia, thrombocytopenia, and coagulopathies.
Results from this study were presented at the 2013 ASH Annual Meeting.
In 2015, Mateon Therapeutics initiated the phase 1b/2 study of OXi4503 (NCT02576301) that is now on partial clinical hold.
The phase 1 portion of this study was designed to assess the safety, pharmacokinetics, pharmacodynamics, and preliminary efficacy of single-agent OXi4503 in patients with relapsed/refractory AML and MDS.
The phase 1 portion was also intended to determine the safety, pharmacokinetics, and pharmacodynamics of OXi4503 plus intermediate-dose cytarabine.
The goal of the phase 2 portion is to assess the preliminary efficacy of OXi4503 and cytarabine in patients with AML and MDS.
The US Food and Drug Administration (FDA) has placed a partial clinical hold on a phase 1b/2 study of OXi4503, a vascular disrupting agent.
In this trial (NCT02576301), researchers are evaluating OXi4503, alone and in combination with cytarabine, in patients with relapsed/refractory acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS).
The partial clinical hold applies to the 12.2 mg/m2 dose of OXi4503.
The FDA is allowing the continued treatment and enrollment of patients using a dose of 9.76 mg/m2.
The agency said additional data on patients receiving OXi4503 at 9.76 mg/m2 must be evaluated before dosing at 12.2 mg/m2 can be resumed.
The partial clinical hold is a result of 2 potential dose-limiting toxicities (DLTs) observed at the 12.2 mg/m2 dose level.
One DLT was hypotension, which occurred shortly after initial treatment with OXi4503. The other DLT was acute hypoxic respiratory failure, which occurred approximately 2 weeks after receiving OXi4503 and cytarabine.
Both events were deemed “possibly related” to OXi4503, and both patients recovered following treatment.
The study protocol generally defines a DLT as any grade 3 serious adverse event where a relationship to OXi4503 cannot be ruled out.
“Although it is disappointing that we are not currently continuing with the higher dose of OXi4503, we look forward to gathering more safety and efficacy data at the previous dose level, where we observed 2 complete remissions in the 4 patients that we treated,” said William D. Schwieterman, MD, chief executive officer of Mateon Therapeutics, Inc., the company developing OXi4503.
About OXi4503
According to Mateon Therapeutics, OXi4503 has a dual mechanism of action that disrupts the shape of tumor bone marrow endothelial cells through reversible binding to tubulin at the colchicine binding site, downregulating intercellular adhesion molecules.
This alters the endothelial cell shape, releasing quiescent adherent tumor cells from bone marrow endothelial cells and activating the cell cycle, which makes the tumor cells vulnerable to chemotherapy.
OXi4503 also kills tumor cells directly via myeloperoxidase activation of an orthoquinone cytotoxic mediator.
In preclinical research, OXi4503 demonstrated activity against AML, both when given alone and in combination with bevacizumab. These results were published in Blood in 2010.
Clinical trials
In a phase 1 trial (NCT01085656), researchers evaluated OXi4503 in patients with relapsed or refractory AML or MDS. The goals were to determine the safety profile, maximum tolerated dose, and biologic activity of OXi4503.
The researchers said OXi4503 demonstrated preliminary evidence of disease response in heavily pre-treated, refractory AML and advanced MDS.
The maximum tolerated dose of OXi4503 was not identified, but adverse events attributable to the drug included hypertension, bone pain, fever, anemia, thrombocytopenia, and coagulopathies.
Results from this study were presented at the 2013 ASH Annual Meeting.
In 2015, Mateon Therapeutics initiated the phase 1b/2 study of OXi4503 (NCT02576301) that is now on partial clinical hold.
The phase 1 portion of this study was designed to assess the safety, pharmacokinetics, pharmacodynamics, and preliminary efficacy of single-agent OXi4503 in patients with relapsed/refractory AML and MDS.
The phase 1 portion was also intended to determine the safety, pharmacokinetics, and pharmacodynamics of OXi4503 plus intermediate-dose cytarabine.
The goal of the phase 2 portion is to assess the preliminary efficacy of OXi4503 and cytarabine in patients with AML and MDS.
The US Food and Drug Administration (FDA) has placed a partial clinical hold on a phase 1b/2 study of OXi4503, a vascular disrupting agent.
In this trial (NCT02576301), researchers are evaluating OXi4503, alone and in combination with cytarabine, in patients with relapsed/refractory acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS).
The partial clinical hold applies to the 12.2 mg/m2 dose of OXi4503.
The FDA is allowing the continued treatment and enrollment of patients using a dose of 9.76 mg/m2.
The agency said additional data on patients receiving OXi4503 at 9.76 mg/m2 must be evaluated before dosing at 12.2 mg/m2 can be resumed.
The partial clinical hold is a result of 2 potential dose-limiting toxicities (DLTs) observed at the 12.2 mg/m2 dose level.
One DLT was hypotension, which occurred shortly after initial treatment with OXi4503. The other DLT was acute hypoxic respiratory failure, which occurred approximately 2 weeks after receiving OXi4503 and cytarabine.
Both events were deemed “possibly related” to OXi4503, and both patients recovered following treatment.
The study protocol generally defines a DLT as any grade 3 serious adverse event where a relationship to OXi4503 cannot be ruled out.
“Although it is disappointing that we are not currently continuing with the higher dose of OXi4503, we look forward to gathering more safety and efficacy data at the previous dose level, where we observed 2 complete remissions in the 4 patients that we treated,” said William D. Schwieterman, MD, chief executive officer of Mateon Therapeutics, Inc., the company developing OXi4503.
About OXi4503
According to Mateon Therapeutics, OXi4503 has a dual mechanism of action that disrupts the shape of tumor bone marrow endothelial cells through reversible binding to tubulin at the colchicine binding site, downregulating intercellular adhesion molecules.
This alters the endothelial cell shape, releasing quiescent adherent tumor cells from bone marrow endothelial cells and activating the cell cycle, which makes the tumor cells vulnerable to chemotherapy.
OXi4503 also kills tumor cells directly via myeloperoxidase activation of an orthoquinone cytotoxic mediator.
In preclinical research, OXi4503 demonstrated activity against AML, both when given alone and in combination with bevacizumab. These results were published in Blood in 2010.
Clinical trials
In a phase 1 trial (NCT01085656), researchers evaluated OXi4503 in patients with relapsed or refractory AML or MDS. The goals were to determine the safety profile, maximum tolerated dose, and biologic activity of OXi4503.
The researchers said OXi4503 demonstrated preliminary evidence of disease response in heavily pre-treated, refractory AML and advanced MDS.
The maximum tolerated dose of OXi4503 was not identified, but adverse events attributable to the drug included hypertension, bone pain, fever, anemia, thrombocytopenia, and coagulopathies.
Results from this study were presented at the 2013 ASH Annual Meeting.
In 2015, Mateon Therapeutics initiated the phase 1b/2 study of OXi4503 (NCT02576301) that is now on partial clinical hold.
The phase 1 portion of this study was designed to assess the safety, pharmacokinetics, pharmacodynamics, and preliminary efficacy of single-agent OXi4503 in patients with relapsed/refractory AML and MDS.
The phase 1 portion was also intended to determine the safety, pharmacokinetics, and pharmacodynamics of OXi4503 plus intermediate-dose cytarabine.
The goal of the phase 2 portion is to assess the preliminary efficacy of OXi4503 and cytarabine in patients with AML and MDS.
Some PE patients don’t require hospitalization
A new study suggests that certain patients with acute pulmonary embolism (PE) may be better off receiving outpatient treatment.
Researchers tested outpatient anticoagulant therapy in 200 PE patients with a low risk of mortality.
At 90 days of follow-up, there were no deaths or recurrences of venous thromboembolism (VTE), but 1 patient experienced major bleeding after a traumatic injury.
A majority of patients said they were satisfied with outpatient care.
Joseph Bledsoe, MD, of Intermountain Medical Center in Salt Lake City, Utah, and his colleagues reported these results in CHEST.
The researchers tracked patients who were treated for acute PE in 5 Intermountain Healthcare emergency departments (EDs) from 2013 to 2016.
The patients had to have a low risk of mortality according to the Pulmonary Embolism Severity Index score (<86), echocardiography (no signs of right heart strain), and whole-leg compression ultrasound.
Patients could not have deep vein thrombosis proximal to the popliteal vein, hypoxia, hypotension, hepatic failure, or renal failure. They had to be eligible for therapeutic anticoagulation and not have any condition requiring hospitalization.
With these criteria, the researchers selected 200 patients. They were observed in the ED or hospital for 12 to 24 hours and then discharged with anticoagulant therapy.
Patients received rivaroxaban (n=149), enoxaparin transitioned to warfarin (n=26), apixaban (n=24), or enoxaparin alone (n=1).
Results
The study’s primary outcome was the 90-day composite rate of all-cause mortality, recurrent symptomatic VTE, and major bleeding.
There were no deaths and no cases of recurrent VTE. One patient did experience major bleeding at day 61 due to a traumatic thigh injury.
Within 7 days of study enrollment, there were 19 patients (9.5%) who returned to the ED and 2 patients (1%) who were admitted to the hospital. One patient with pulmonary infarct was admitted for pain control (day 2), and another was admitted for an elective coronary intervention (day 7) due to a positive cardiac stress test.
Within 30 days, 32 patients (16%) returned to the ED, and 5 (3%) were admitted to the hospital for events unrelated to their PE.
The study also showed that patients were largely satisfied with outpatient care. Of the 146 patients who completed a satisfaction survey at 90 days, 89% said they would choose outpatient management if they had another PE in the future.
“We found a large subset of patients with blood clots who’d do well at home; in fact, who probably did better at home,” Dr Bledsoe said. “When patients are sent home versus staying in the hospital, they’re at lower risk of getting another infection. It’s a lot less expensive, too.”
Currently, the standard of care in the US for acute PE is hospitalization for all patients. That’s recommended, in part, because their overall mortality rate is 17%.
However, the lower mortality rate among some appropriately risk-stratified patients suggests that at-home care, which has become the norm in some European countries, leads to better outcomes for those patients overall and less chance of a hospital-introduced infection, according to Dr Bledsoe.
“Our findings show that, if you appropriately risk-stratify patients, there are a lot of people with blood clots who are safe to go home,” he said.
Dr Bledsoe added that similar research should be conducted outside of the Intermountain Healthcare system to confirm the results of this study, and a larger group of patients should be studied.
A new study suggests that certain patients with acute pulmonary embolism (PE) may be better off receiving outpatient treatment.
Researchers tested outpatient anticoagulant therapy in 200 PE patients with a low risk of mortality.
At 90 days of follow-up, there were no deaths or recurrences of venous thromboembolism (VTE), but 1 patient experienced major bleeding after a traumatic injury.
A majority of patients said they were satisfied with outpatient care.
Joseph Bledsoe, MD, of Intermountain Medical Center in Salt Lake City, Utah, and his colleagues reported these results in CHEST.
The researchers tracked patients who were treated for acute PE in 5 Intermountain Healthcare emergency departments (EDs) from 2013 to 2016.
The patients had to have a low risk of mortality according to the Pulmonary Embolism Severity Index score (<86), echocardiography (no signs of right heart strain), and whole-leg compression ultrasound.
Patients could not have deep vein thrombosis proximal to the popliteal vein, hypoxia, hypotension, hepatic failure, or renal failure. They had to be eligible for therapeutic anticoagulation and not have any condition requiring hospitalization.
With these criteria, the researchers selected 200 patients. They were observed in the ED or hospital for 12 to 24 hours and then discharged with anticoagulant therapy.
Patients received rivaroxaban (n=149), enoxaparin transitioned to warfarin (n=26), apixaban (n=24), or enoxaparin alone (n=1).
Results
The study’s primary outcome was the 90-day composite rate of all-cause mortality, recurrent symptomatic VTE, and major bleeding.
There were no deaths and no cases of recurrent VTE. One patient did experience major bleeding at day 61 due to a traumatic thigh injury.
Within 7 days of study enrollment, there were 19 patients (9.5%) who returned to the ED and 2 patients (1%) who were admitted to the hospital. One patient with pulmonary infarct was admitted for pain control (day 2), and another was admitted for an elective coronary intervention (day 7) due to a positive cardiac stress test.
Within 30 days, 32 patients (16%) returned to the ED, and 5 (3%) were admitted to the hospital for events unrelated to their PE.
The study also showed that patients were largely satisfied with outpatient care. Of the 146 patients who completed a satisfaction survey at 90 days, 89% said they would choose outpatient management if they had another PE in the future.
“We found a large subset of patients with blood clots who’d do well at home; in fact, who probably did better at home,” Dr Bledsoe said. “When patients are sent home versus staying in the hospital, they’re at lower risk of getting another infection. It’s a lot less expensive, too.”
Currently, the standard of care in the US for acute PE is hospitalization for all patients. That’s recommended, in part, because their overall mortality rate is 17%.
However, the lower mortality rate among some appropriately risk-stratified patients suggests that at-home care, which has become the norm in some European countries, leads to better outcomes for those patients overall and less chance of a hospital-introduced infection, according to Dr Bledsoe.
“Our findings show that, if you appropriately risk-stratify patients, there are a lot of people with blood clots who are safe to go home,” he said.
Dr Bledsoe added that similar research should be conducted outside of the Intermountain Healthcare system to confirm the results of this study, and a larger group of patients should be studied.
A new study suggests that certain patients with acute pulmonary embolism (PE) may be better off receiving outpatient treatment.
Researchers tested outpatient anticoagulant therapy in 200 PE patients with a low risk of mortality.
At 90 days of follow-up, there were no deaths or recurrences of venous thromboembolism (VTE), but 1 patient experienced major bleeding after a traumatic injury.
A majority of patients said they were satisfied with outpatient care.
Joseph Bledsoe, MD, of Intermountain Medical Center in Salt Lake City, Utah, and his colleagues reported these results in CHEST.
The researchers tracked patients who were treated for acute PE in 5 Intermountain Healthcare emergency departments (EDs) from 2013 to 2016.
The patients had to have a low risk of mortality according to the Pulmonary Embolism Severity Index score (<86), echocardiography (no signs of right heart strain), and whole-leg compression ultrasound.
Patients could not have deep vein thrombosis proximal to the popliteal vein, hypoxia, hypotension, hepatic failure, or renal failure. They had to be eligible for therapeutic anticoagulation and not have any condition requiring hospitalization.
With these criteria, the researchers selected 200 patients. They were observed in the ED or hospital for 12 to 24 hours and then discharged with anticoagulant therapy.
Patients received rivaroxaban (n=149), enoxaparin transitioned to warfarin (n=26), apixaban (n=24), or enoxaparin alone (n=1).
Results
The study’s primary outcome was the 90-day composite rate of all-cause mortality, recurrent symptomatic VTE, and major bleeding.
There were no deaths and no cases of recurrent VTE. One patient did experience major bleeding at day 61 due to a traumatic thigh injury.
Within 7 days of study enrollment, there were 19 patients (9.5%) who returned to the ED and 2 patients (1%) who were admitted to the hospital. One patient with pulmonary infarct was admitted for pain control (day 2), and another was admitted for an elective coronary intervention (day 7) due to a positive cardiac stress test.
Within 30 days, 32 patients (16%) returned to the ED, and 5 (3%) were admitted to the hospital for events unrelated to their PE.
The study also showed that patients were largely satisfied with outpatient care. Of the 146 patients who completed a satisfaction survey at 90 days, 89% said they would choose outpatient management if they had another PE in the future.
“We found a large subset of patients with blood clots who’d do well at home; in fact, who probably did better at home,” Dr Bledsoe said. “When patients are sent home versus staying in the hospital, they’re at lower risk of getting another infection. It’s a lot less expensive, too.”
Currently, the standard of care in the US for acute PE is hospitalization for all patients. That’s recommended, in part, because their overall mortality rate is 17%.
However, the lower mortality rate among some appropriately risk-stratified patients suggests that at-home care, which has become the norm in some European countries, leads to better outcomes for those patients overall and less chance of a hospital-introduced infection, according to Dr Bledsoe.
“Our findings show that, if you appropriately risk-stratify patients, there are a lot of people with blood clots who are safe to go home,” he said.
Dr Bledsoe added that similar research should be conducted outside of the Intermountain Healthcare system to confirm the results of this study, and a larger group of patients should be studied.
Drug coverage linked to OS in myeloma
Prescription drug coverage at diagnosis is associated with outcomes among Medicare beneficiaries with myeloma, according to new research.
Patients enrolled in a Medicare Part D plan (PDP) and those with other creditable prescription drug coverage (OCC) at the time of myeloma diagnosis were more likely to receive active care and had better overall survival (OS) than Medicare beneficiaries with no drug coverage.
Adam Olszewski, MD, of Rhode Island Hospital in Providence, and his colleagues reported these findings in the Journal of Clinical Oncology.
The researchers looked at 9755 patients diagnosed with myeloma from 2006 to 2011, assessing the patients’ first-line treatment and OS.
The team classified patients according to the prescription drug coverage they had at myeloma diagnosis. There were 1460 patients with no prescription drug coverage, 3283 with PDP, 3607 with OCC, and 1405 with dual eligibility for Medicare and Medicaid coverage.
Treatment
In a multivariate analysis, PDP beneficiaries were 6% more likely than beneficiaries with no drug coverage to receive active care for myeloma.
However, PDP beneficiaries were 14% less likely to receive parenteral chemotherapy and 38% less likely to receive classic cytotoxic agents. The use of bortezomib-based regimens was similar between PDP patients and those with no drug coverage.
Beneficiaries with OCC were 3% more likely than those with no drug coverage to receive active myeloma care. The use of parenteral chemotherapy, classic cytotoxic agents, and bortezomib-based regimens was similar between the OCC group and the group without drug coverage.
Medicare/Medicaid dual enrollees were about as likely as beneficiaries with no drug coverage to receive active myeloma care. However, the dual enrollees were less likely to receive parenteral chemotherapy, classic cytotoxic agents, and bortezomib-based regimens.
Survival
The median follow-up was 4.9 years. The median survival for all myeloma patients was 2.3 years, and the 3-year OS was 43.1%.
The researchers noted that, among the beneficiaries without drug coverage at diagnosis, 41% had obtained PDP or OCC by the following January. Even so, their OS was significantly worse than beneficiaries who had PDP or OCC at diagnosis.
In a multivariate analysis, OS was 16% longer in both the PDP group and the OCC group than in the group without drug coverage at diagnosis. OS was 8% longer for dual enrollees than for patients without drug coverage.
Dr Olszewski and his colleagues noted that survival differences were largest during the first year and decreased over time as more patients without drug coverage obtained coverage.
The researchers said they couldn’t determine whether the worse OS in the group without drug coverage was the result of not receiving therapy, lack of access to immunomodulatory drugs, or other medical issues.
The team also said their findings should be interpreted with caution because the survival results are “confounded by multiple baseline factors and mediated by the quality of cancer treatment.”
Still, the results “strongly suggest that patients with myeloma without prescription drug coverage may not have received the most effective first-line therapy,” Dr Olszewski and his colleagues wrote.
“Survival for PDP and OCC groups remained identical, which supports the notion that having any prescription drug coverage contributed to optimal treatment and outcomes.”
Prescription drug coverage at diagnosis is associated with outcomes among Medicare beneficiaries with myeloma, according to new research.
Patients enrolled in a Medicare Part D plan (PDP) and those with other creditable prescription drug coverage (OCC) at the time of myeloma diagnosis were more likely to receive active care and had better overall survival (OS) than Medicare beneficiaries with no drug coverage.
Adam Olszewski, MD, of Rhode Island Hospital in Providence, and his colleagues reported these findings in the Journal of Clinical Oncology.
The researchers looked at 9755 patients diagnosed with myeloma from 2006 to 2011, assessing the patients’ first-line treatment and OS.
The team classified patients according to the prescription drug coverage they had at myeloma diagnosis. There were 1460 patients with no prescription drug coverage, 3283 with PDP, 3607 with OCC, and 1405 with dual eligibility for Medicare and Medicaid coverage.
Treatment
In a multivariate analysis, PDP beneficiaries were 6% more likely than beneficiaries with no drug coverage to receive active care for myeloma.
However, PDP beneficiaries were 14% less likely to receive parenteral chemotherapy and 38% less likely to receive classic cytotoxic agents. The use of bortezomib-based regimens was similar between PDP patients and those with no drug coverage.
Beneficiaries with OCC were 3% more likely than those with no drug coverage to receive active myeloma care. The use of parenteral chemotherapy, classic cytotoxic agents, and bortezomib-based regimens was similar between the OCC group and the group without drug coverage.
Medicare/Medicaid dual enrollees were about as likely as beneficiaries with no drug coverage to receive active myeloma care. However, the dual enrollees were less likely to receive parenteral chemotherapy, classic cytotoxic agents, and bortezomib-based regimens.
Survival
The median follow-up was 4.9 years. The median survival for all myeloma patients was 2.3 years, and the 3-year OS was 43.1%.
The researchers noted that, among the beneficiaries without drug coverage at diagnosis, 41% had obtained PDP or OCC by the following January. Even so, their OS was significantly worse than beneficiaries who had PDP or OCC at diagnosis.
In a multivariate analysis, OS was 16% longer in both the PDP group and the OCC group than in the group without drug coverage at diagnosis. OS was 8% longer for dual enrollees than for patients without drug coverage.
Dr Olszewski and his colleagues noted that survival differences were largest during the first year and decreased over time as more patients without drug coverage obtained coverage.
The researchers said they couldn’t determine whether the worse OS in the group without drug coverage was the result of not receiving therapy, lack of access to immunomodulatory drugs, or other medical issues.
The team also said their findings should be interpreted with caution because the survival results are “confounded by multiple baseline factors and mediated by the quality of cancer treatment.”
Still, the results “strongly suggest that patients with myeloma without prescription drug coverage may not have received the most effective first-line therapy,” Dr Olszewski and his colleagues wrote.
“Survival for PDP and OCC groups remained identical, which supports the notion that having any prescription drug coverage contributed to optimal treatment and outcomes.”
Prescription drug coverage at diagnosis is associated with outcomes among Medicare beneficiaries with myeloma, according to new research.
Patients enrolled in a Medicare Part D plan (PDP) and those with other creditable prescription drug coverage (OCC) at the time of myeloma diagnosis were more likely to receive active care and had better overall survival (OS) than Medicare beneficiaries with no drug coverage.
Adam Olszewski, MD, of Rhode Island Hospital in Providence, and his colleagues reported these findings in the Journal of Clinical Oncology.
The researchers looked at 9755 patients diagnosed with myeloma from 2006 to 2011, assessing the patients’ first-line treatment and OS.
The team classified patients according to the prescription drug coverage they had at myeloma diagnosis. There were 1460 patients with no prescription drug coverage, 3283 with PDP, 3607 with OCC, and 1405 with dual eligibility for Medicare and Medicaid coverage.
Treatment
In a multivariate analysis, PDP beneficiaries were 6% more likely than beneficiaries with no drug coverage to receive active care for myeloma.
However, PDP beneficiaries were 14% less likely to receive parenteral chemotherapy and 38% less likely to receive classic cytotoxic agents. The use of bortezomib-based regimens was similar between PDP patients and those with no drug coverage.
Beneficiaries with OCC were 3% more likely than those with no drug coverage to receive active myeloma care. The use of parenteral chemotherapy, classic cytotoxic agents, and bortezomib-based regimens was similar between the OCC group and the group without drug coverage.
Medicare/Medicaid dual enrollees were about as likely as beneficiaries with no drug coverage to receive active myeloma care. However, the dual enrollees were less likely to receive parenteral chemotherapy, classic cytotoxic agents, and bortezomib-based regimens.
Survival
The median follow-up was 4.9 years. The median survival for all myeloma patients was 2.3 years, and the 3-year OS was 43.1%.
The researchers noted that, among the beneficiaries without drug coverage at diagnosis, 41% had obtained PDP or OCC by the following January. Even so, their OS was significantly worse than beneficiaries who had PDP or OCC at diagnosis.
In a multivariate analysis, OS was 16% longer in both the PDP group and the OCC group than in the group without drug coverage at diagnosis. OS was 8% longer for dual enrollees than for patients without drug coverage.
Dr Olszewski and his colleagues noted that survival differences were largest during the first year and decreased over time as more patients without drug coverage obtained coverage.
The researchers said they couldn’t determine whether the worse OS in the group without drug coverage was the result of not receiving therapy, lack of access to immunomodulatory drugs, or other medical issues.
The team also said their findings should be interpreted with caution because the survival results are “confounded by multiple baseline factors and mediated by the quality of cancer treatment.”
Still, the results “strongly suggest that patients with myeloma without prescription drug coverage may not have received the most effective first-line therapy,” Dr Olszewski and his colleagues wrote.
“Survival for PDP and OCC groups remained identical, which supports the notion that having any prescription drug coverage contributed to optimal treatment and outcomes.”
CPI-613 receives orphan designation for PTCL
The US Food and Drug Administration (FDA) has granted orphan drug designation to CPI-613 for the treatment of peripheral T-cell lymphoma (PTCL).
CPI-613 is a novel lipoic acid analogue that inhibits multiple enzyme targets within the tricarboxylic acid cycle.
Rafael Pharmaceuticals, Inc., is developing CPI-613 as a treatment for hematologic malignancies and solid tumors.
CPI-613 is currently under investigation in combination with bendamustine in a phase 1 study of patients with relapsed or refractory T-cell lymphoma or classical Hodgkin lymphoma.
Results from this trial were presented at the 2016 ASH Annual Meeting.*
CPI-613 was given at escalating doses starting at 2000 mg/m2 over 2 hours on days 1-4 as well as on days 8, 11, 15, and 18. Bendamustine was infused at 90 mg/m2 on days 4 and 5 of each 4-week treatment cycle. The treatment cycles were repeated for up to 6 cycles. There was no intra-patient dose-escalation.
The ASH presentation included safety data on 8 patients. The most common grade 3 or higher toxicities—lymphopenia and neutropenia—occurred in 4 patients.
A patient dosed at 2750 mg/m2 had a dose-limiting toxicity of grade 3 acute kidney injury and grade 4 lactic acidosis. Because of this, the study protocol was amended to discontinue dose-escalation at doses of 2750 mg/m2 or higher and to expand the 2500 mg/m2 cohort.
Six patients were evaluable for efficacy, and the overall response rate was 83% (5/6).
There were 3 complete responses in patients with PTCL not otherwise specified, a partial response in a patient with mycosis fungoides, and a partial response in a patient with angioimmunoblastic T-cell lymphoma.
One patient with T-cell acute lymphoblastic leukemia experienced progressive disease.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
*The data presented differ from the abstract.
The US Food and Drug Administration (FDA) has granted orphan drug designation to CPI-613 for the treatment of peripheral T-cell lymphoma (PTCL).
CPI-613 is a novel lipoic acid analogue that inhibits multiple enzyme targets within the tricarboxylic acid cycle.
Rafael Pharmaceuticals, Inc., is developing CPI-613 as a treatment for hematologic malignancies and solid tumors.
CPI-613 is currently under investigation in combination with bendamustine in a phase 1 study of patients with relapsed or refractory T-cell lymphoma or classical Hodgkin lymphoma.
Results from this trial were presented at the 2016 ASH Annual Meeting.*
CPI-613 was given at escalating doses starting at 2000 mg/m2 over 2 hours on days 1-4 as well as on days 8, 11, 15, and 18. Bendamustine was infused at 90 mg/m2 on days 4 and 5 of each 4-week treatment cycle. The treatment cycles were repeated for up to 6 cycles. There was no intra-patient dose-escalation.
The ASH presentation included safety data on 8 patients. The most common grade 3 or higher toxicities—lymphopenia and neutropenia—occurred in 4 patients.
A patient dosed at 2750 mg/m2 had a dose-limiting toxicity of grade 3 acute kidney injury and grade 4 lactic acidosis. Because of this, the study protocol was amended to discontinue dose-escalation at doses of 2750 mg/m2 or higher and to expand the 2500 mg/m2 cohort.
Six patients were evaluable for efficacy, and the overall response rate was 83% (5/6).
There were 3 complete responses in patients with PTCL not otherwise specified, a partial response in a patient with mycosis fungoides, and a partial response in a patient with angioimmunoblastic T-cell lymphoma.
One patient with T-cell acute lymphoblastic leukemia experienced progressive disease.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
*The data presented differ from the abstract.
The US Food and Drug Administration (FDA) has granted orphan drug designation to CPI-613 for the treatment of peripheral T-cell lymphoma (PTCL).
CPI-613 is a novel lipoic acid analogue that inhibits multiple enzyme targets within the tricarboxylic acid cycle.
Rafael Pharmaceuticals, Inc., is developing CPI-613 as a treatment for hematologic malignancies and solid tumors.
CPI-613 is currently under investigation in combination with bendamustine in a phase 1 study of patients with relapsed or refractory T-cell lymphoma or classical Hodgkin lymphoma.
Results from this trial were presented at the 2016 ASH Annual Meeting.*
CPI-613 was given at escalating doses starting at 2000 mg/m2 over 2 hours on days 1-4 as well as on days 8, 11, 15, and 18. Bendamustine was infused at 90 mg/m2 on days 4 and 5 of each 4-week treatment cycle. The treatment cycles were repeated for up to 6 cycles. There was no intra-patient dose-escalation.
The ASH presentation included safety data on 8 patients. The most common grade 3 or higher toxicities—lymphopenia and neutropenia—occurred in 4 patients.
A patient dosed at 2750 mg/m2 had a dose-limiting toxicity of grade 3 acute kidney injury and grade 4 lactic acidosis. Because of this, the study protocol was amended to discontinue dose-escalation at doses of 2750 mg/m2 or higher and to expand the 2500 mg/m2 cohort.
Six patients were evaluable for efficacy, and the overall response rate was 83% (5/6).
There were 3 complete responses in patients with PTCL not otherwise specified, a partial response in a patient with mycosis fungoides, and a partial response in a patient with angioimmunoblastic T-cell lymphoma.
One patient with T-cell acute lymphoblastic leukemia experienced progressive disease.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
*The data presented differ from the abstract.
FDA approves assay to screen blood for Zika
The US Food and Drug Administration (FDA) has approved the Procleix® Zika Virus Assay for blood screening.
The assay is approved to detect Zika virus in individual or pooled plasma specimens from human donors, including volunteer donors of whole blood and blood components for transfusion.
The assay is also approved for testing plasma or serum specimens to screen other living or cadaveric organ donors and human cells, tissues, and cellular and tissue-based products.
The Procleix Zika Virus Assay, which was developed by Hologic, Inc. and Grifols, is designed to run on the Procleix Panther System. The Procleix Panther System automates all aspects of nucleic acid technology-based blood screening on a single, integrated platform.
The Procleix Zika Virus Assay has been in use in the US since June 2016, when it was authorized under an investigational new drug protocol to screen donated blood collected in the US.
Also in 2016, the assay was CE-marked for use in European countries conforming to CE Mark regulations.
The US Food and Drug Administration (FDA) has approved the Procleix® Zika Virus Assay for blood screening.
The assay is approved to detect Zika virus in individual or pooled plasma specimens from human donors, including volunteer donors of whole blood and blood components for transfusion.
The assay is also approved for testing plasma or serum specimens to screen other living or cadaveric organ donors and human cells, tissues, and cellular and tissue-based products.
The Procleix Zika Virus Assay, which was developed by Hologic, Inc. and Grifols, is designed to run on the Procleix Panther System. The Procleix Panther System automates all aspects of nucleic acid technology-based blood screening on a single, integrated platform.
The Procleix Zika Virus Assay has been in use in the US since June 2016, when it was authorized under an investigational new drug protocol to screen donated blood collected in the US.
Also in 2016, the assay was CE-marked for use in European countries conforming to CE Mark regulations.
The US Food and Drug Administration (FDA) has approved the Procleix® Zika Virus Assay for blood screening.
The assay is approved to detect Zika virus in individual or pooled plasma specimens from human donors, including volunteer donors of whole blood and blood components for transfusion.
The assay is also approved for testing plasma or serum specimens to screen other living or cadaveric organ donors and human cells, tissues, and cellular and tissue-based products.
The Procleix Zika Virus Assay, which was developed by Hologic, Inc. and Grifols, is designed to run on the Procleix Panther System. The Procleix Panther System automates all aspects of nucleic acid technology-based blood screening on a single, integrated platform.
The Procleix Zika Virus Assay has been in use in the US since June 2016, when it was authorized under an investigational new drug protocol to screen donated blood collected in the US.
Also in 2016, the assay was CE-marked for use in European countries conforming to CE Mark regulations.